Chapter 32 Red Blood Cells Anemia and Polycythemia
Chapter 32: Red Blood Cells, Anemia, and Polycythemia
Function of Red Blood Cells Transport of Hemoglobin Transport of Carbon Dioxide Acid-base buffer
Definitions Hematocrit: % volume of blood that is red cells Men ~45% Women ~40% Hemoglobin: 34 gm/100 ml red cells 15 -16 (male) gm Hb/100 ml blood 13 -14 (female) gm Hb/100 ml blood Oxygen carrying capacity: gm Hg/100 ml blood * 1. 34 ml O 2/gm Hb ~21 ml O 2/ 100 ml blood for men ~19 ml O 2/ 100 ml blood for women

Normal Values WBC count RBC count x 103 7. 8 ± 3 x 106 5. 4 ± 0. 7 male x 106 4. 8 ± 0. 6 female Hemoglobin 16 ± 2 male 14 ± 2 female 47 ± 5 male 42 ± 5 female hematocrit RBC indices MCV MCHC RDW-sd Platelet count fl pg % fl x 103 90 ± 9 32 ± 2 33 ± 3 42 ± 5 140 -440
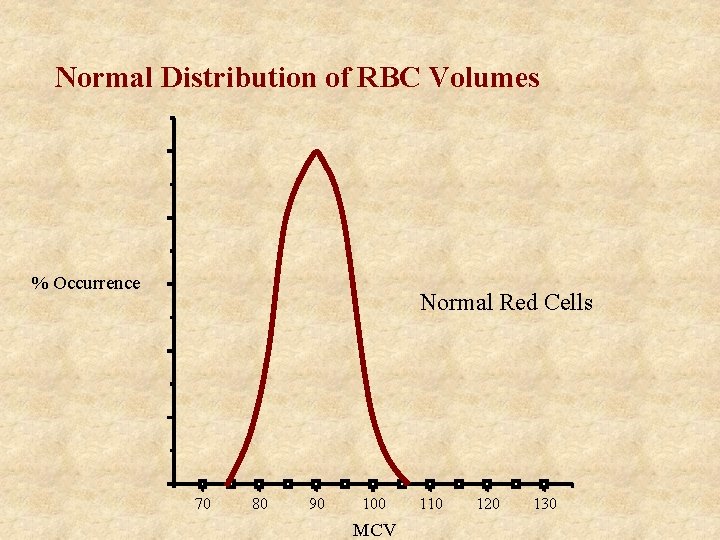
Normal Distribution of RBC Volumes % Occurrence Normal Red Cells 70 80 90 100 MCV 110 120 130
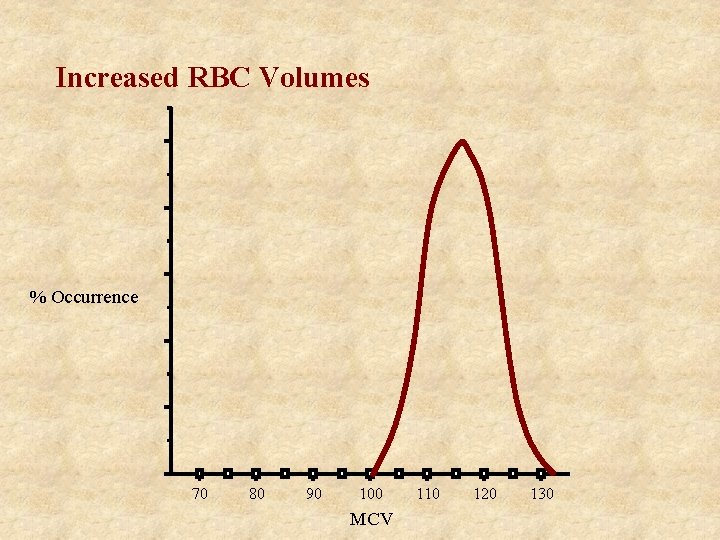
Increased RBC Volumes % Occurrence 70 80 90 100 MCV 110 120 130

Increased Distribution of RBC Volumes % Occurrence 70 80 90 100 MCV 110 120 130
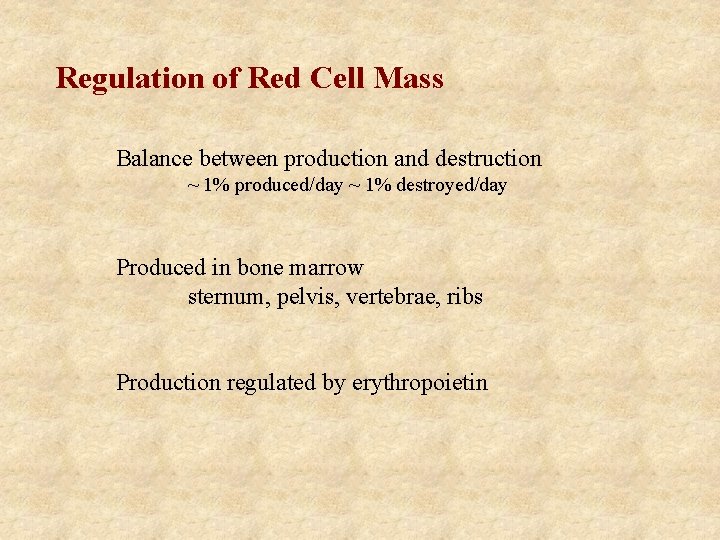
Regulation of Red Cell Mass Balance between production and destruction ~ 1% produced/day ~ 1% destroyed/day Produced in bone marrow sternum, pelvis, vertebrae, ribs Production regulated by erythropoietin
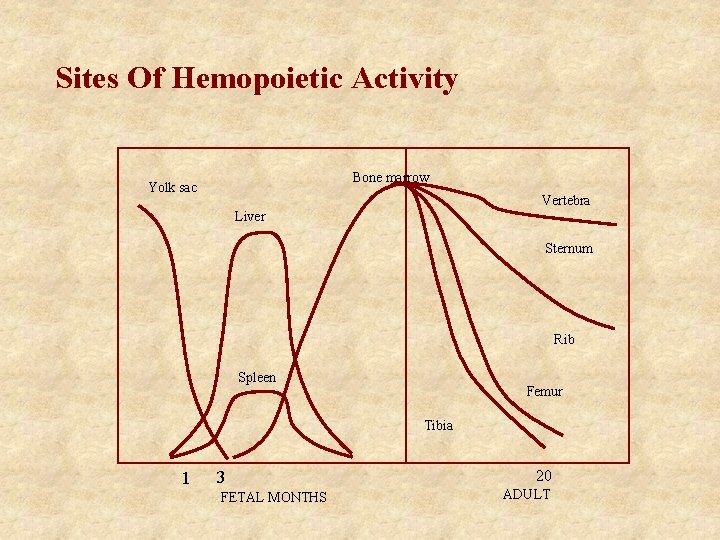
Sites Of Hemopoietic Activity Bone marrow Yolk sac Vertebra Liver Sternum Rib Spleen Femur Tibia 1 3 FETAL MONTHS 20 ADULT

Genesis of Blood Products T-Cell CFU-T B-Cell CFU-B Pluripotent Stem Cell Lymphoid Stem Cell eosinophil CFU-Eosin basophil CFU-Bas neutrophil CFU-GM Myeloid Stem Cell monocyte macrophage platelets CFU-MEG BFU-E erythrocyte
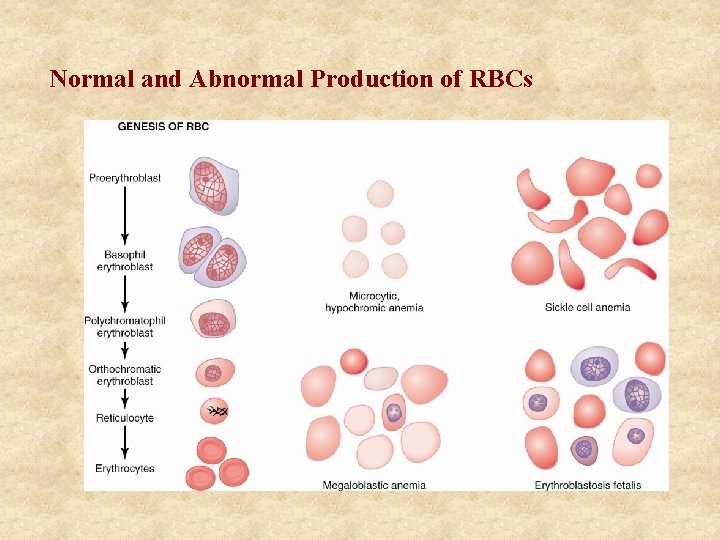
Normal and Abnormal Production of RBCs
Erythropoietin Hormone released from kidney in response to low renal oxygenation Stimulates stem cells to form pronormoblasts Promotes release of reticulocytes Red cell production increases within 24 hours Erythropoietin life span is 4 -12 hours Increase in red cell number in 5 days
Erythropoietin Produced in peritubular interstitial cells of the kidney Produced in the liver ~10% No preformed stores of erythropoietin Erythrocytosis suppresses erythropoietin production but does not abolish it Erythropoietin is always present in the plasma

Destruction of Red Blood Cells < 100 days survival hemolysis Decrease in enzyme activity, ATP levels, and MCH Decreased deformability (spherocytosis) Binding by Ig. G Ingested by macrophage in spleen extravascular hemolysis Iron release to transferrin Hemoglobin excreted as bilirubin
Iron Metabolism • 7 mg/1000 calories ~ 10% absorbed, 1 -1. 5 mg/day • absorption enhanced by meat, poultry, fish • inhibited by carbonates, tannate (tea), oxalate (spinach, rhubarb), phosphates (vegetables), clay • duodenum and upper jejunum major site absorption • HCl promotes absorption • loss 1 mg/day males average • menstruating women additional 14 mg/period loss
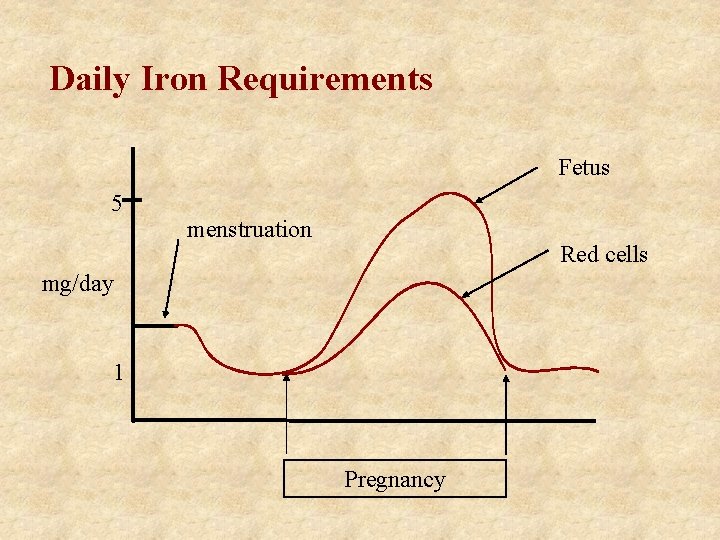
Daily Iron Requirements Fetus 5 menstruation Red cells mg/day 1 Pregnancy
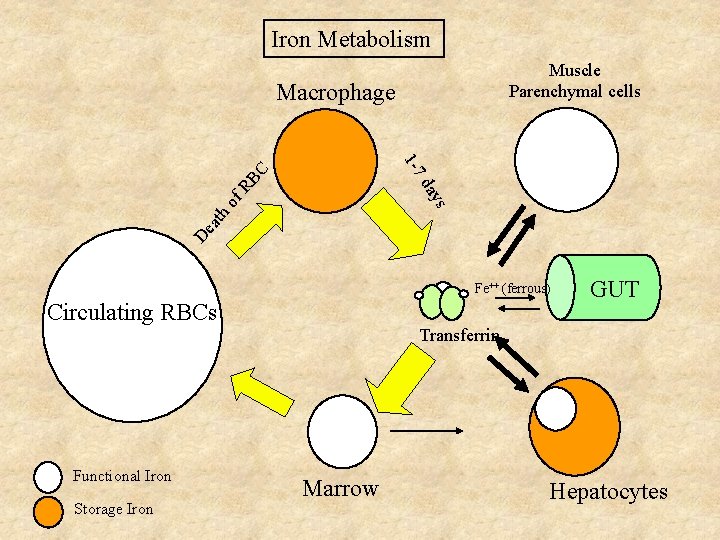
Iron Metabolism Muscle Parenchymal cells Macrophage da RB C 1 -7 De ath of ys Fe++ (ferrous) Circulating RBCs Functional Iron Storage Iron GUT Transferrin Marrow Hepatocytes
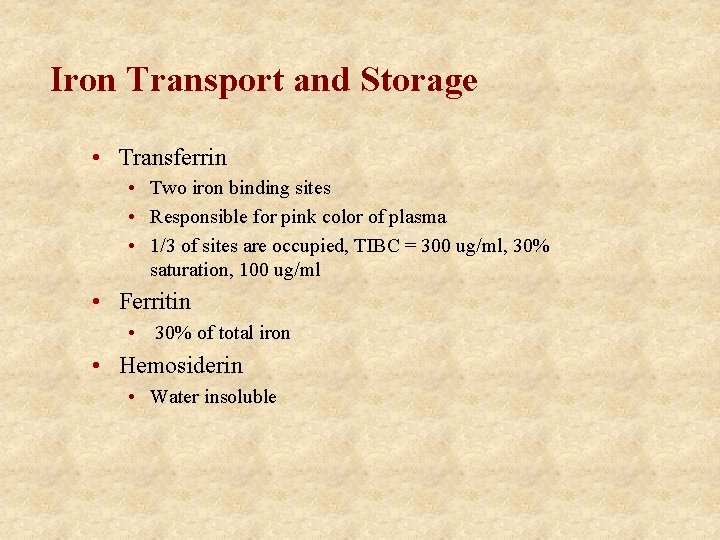
Iron Transport and Storage • Transferrin • Two iron binding sites • Responsible for pink color of plasma • 1/3 of sites are occupied, TIBC = 300 ug/ml, 30% saturation, 100 ug/ml • Ferritin • 30% of total iron • Hemosiderin • Water insoluble

Reticulocyte Index Retic = relative percent of cells that are reticulocytes Need to correct to get absolute percentage RI= Retic (%) * Hc(patients)/Hc (normal) Hc = 50 Retic = 1% (50, 000/ul) Hc = 25 Retic = 2% (50, 000/ul)
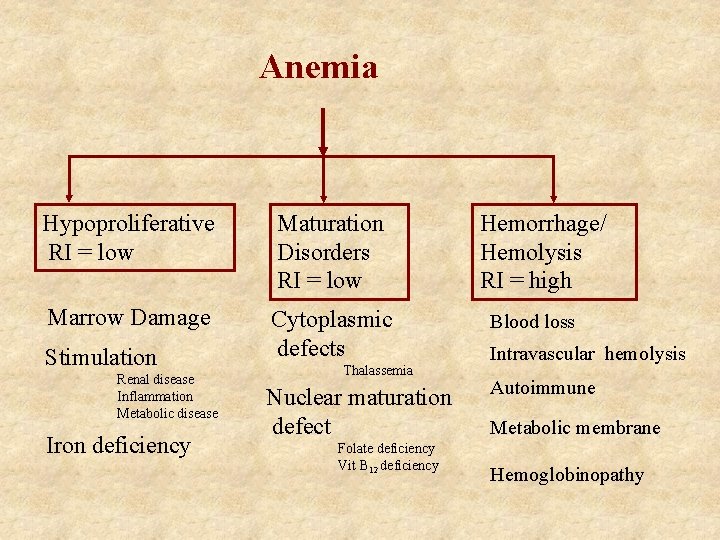
Anemia Hypoproliferative RI = low Maturation Disorders RI = low Marrow Damage Cytoplasmic defects Stimulation Renal disease Inflammation Metabolic disease Iron deficiency Thalassemia Nuclear maturation defect Folate deficiency Vit B 12 deficiency Hemorrhage/ Hemolysis RI = high Blood loss Intravascular hemolysis Autoimmune Metabolic membrane Hemoglobinopathy
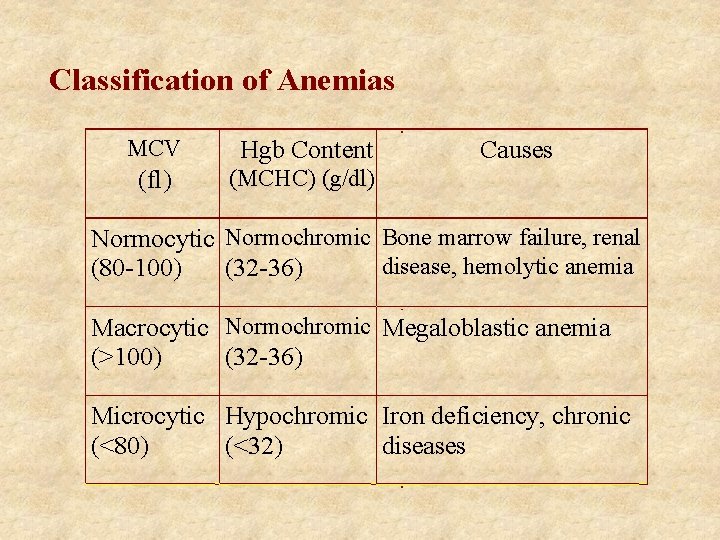
Classification of Anemias MCV Hgb Content (fl) (MCHC) (g/dl) Causes Normocytic Normochromic Bone marrow failure, renal disease, hemolytic anemia (80 -100) (32 -36) Macrocytic Normochromic Megaloblastic anemia (>100) (32 -36) Microcytic Hypochromic Iron deficiency, chronic (<80) (<32) diseases

Hypoproliferative • Aplastic anemia • Primary • idiopathic • Secondary • Drugs - chemotherapy, antibiotics, antidepressants, ethanol • Chemicals - benzene • Radiation • Immune suppression of stem cell • Malignancy (non-hematopoietic tumors and transformation of hematopoietic stem cells) • Therapy
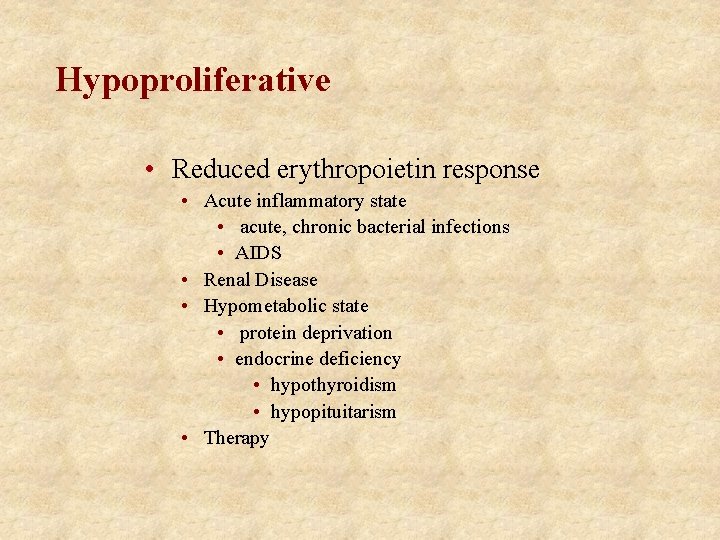
Hypoproliferative • Reduced erythropoietin response • Acute inflammatory state • acute, chronic bacterial infections • AIDS • Renal Disease • Hypometabolic state • protein deprivation • endocrine deficiency • hypothyroidism • hypopituitarism • Therapy

Hypoproliferative • Iron deficiency • almost always blood loss • exceptions (children, adults poor absorption) • Men and post menopausal women • GI blood loss • depletion of stores • decrease iron - microcytic, hypochromic • major deficiency misshapen RBCs
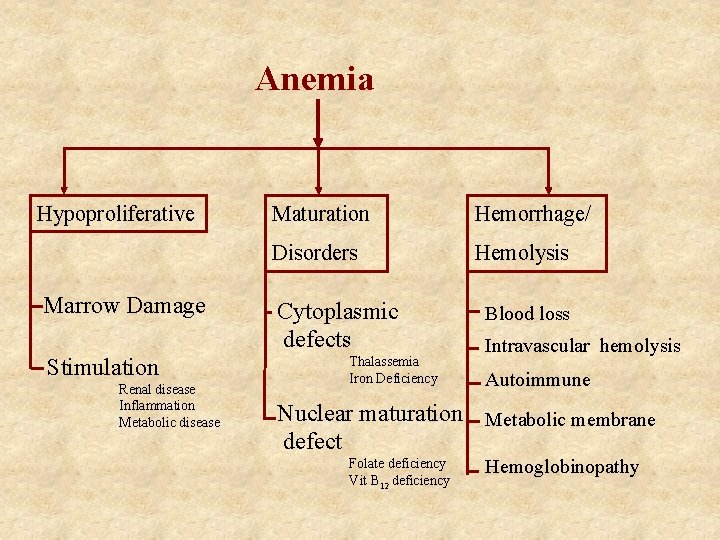
Anemia Hypoproliferative Marrow Damage Stimulation Renal disease Inflammation Metabolic disease Maturation Hemorrhage/ Disorders Hemolysis Cytoplasmic defects Thalassemia Iron Deficiency Blood loss Intravascular hemolysis Autoimmune Nuclear maturation Metabolic membrane defect Folate deficiency Vit B 12 deficiency Hemoglobinopathy
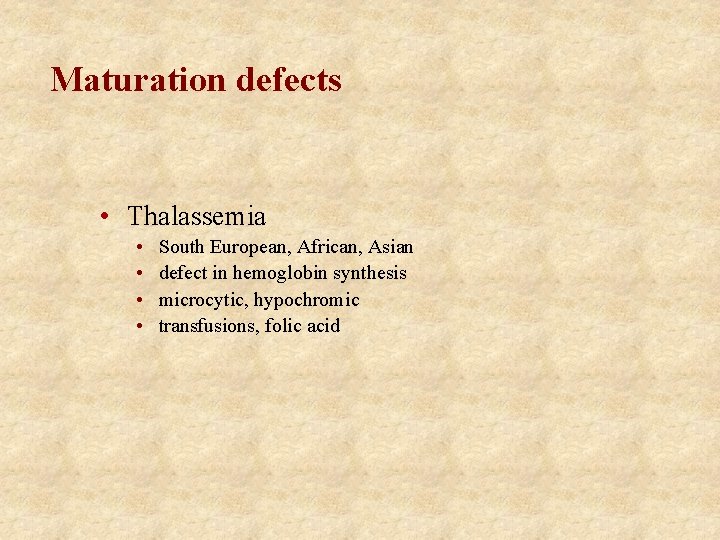
Maturation defects • Thalassemia • • South European, African, Asian defect in hemoglobin synthesis microcytic, hypochromic transfusions, folic acid
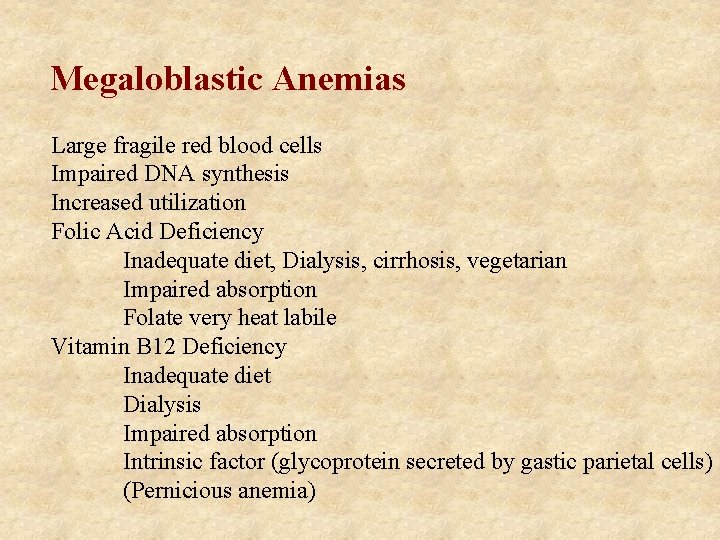
Megaloblastic Anemias Large fragile red blood cells Impaired DNA synthesis Increased utilization Folic Acid Deficiency Inadequate diet, Dialysis, cirrhosis, vegetarian Impaired absorption Folate very heat labile Vitamin B 12 Deficiency Inadequate diet Dialysis Impaired absorption Intrinsic factor (glycoprotein secreted by gastic parietal cells) (Pernicious anemia)
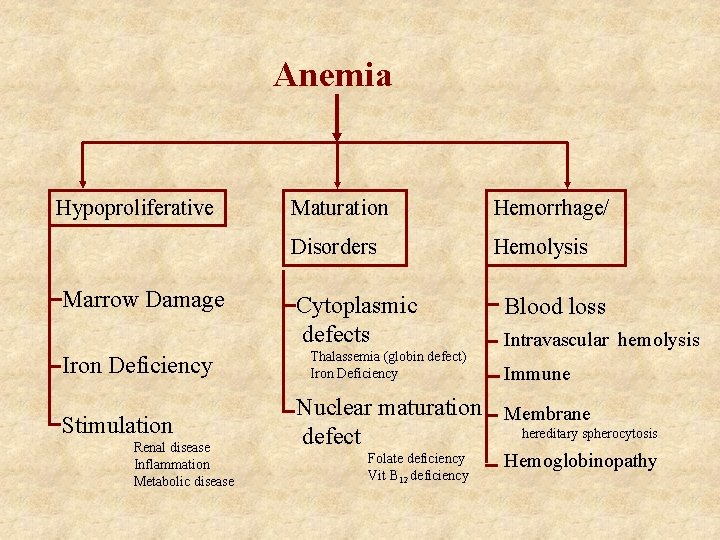
Anemia Hypoproliferative Marrow Damage Iron Deficiency Stimulation Renal disease Inflammation Metabolic disease Maturation Hemorrhage/ Disorders Hemolysis Cytoplasmic defects Thalassemia (globin defect) Iron Deficiency Blood loss Intravascular hemolysis Immune Nuclear maturation Membrane hereditary spherocytosis defect Folate deficiency Vit B 12 deficiency Hemoglobinopathy
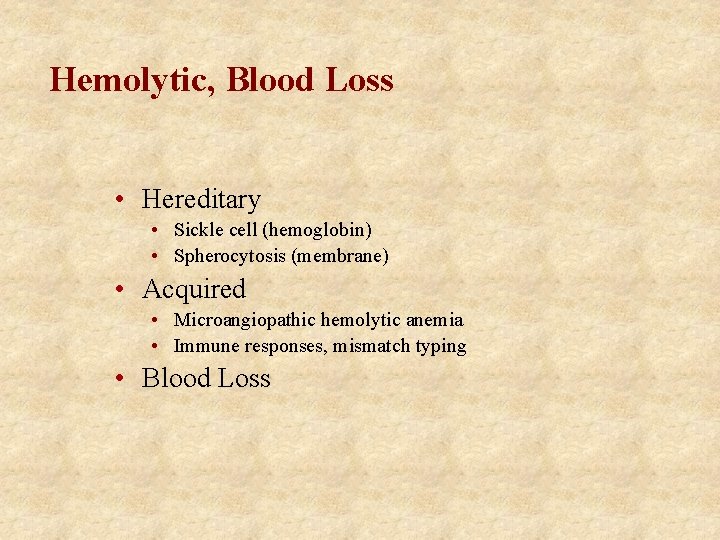
Hemolytic, Blood Loss • Hereditary • Sickle cell (hemoglobin) • Spherocytosis (membrane) • Acquired • Microangiopathic hemolytic anemia • Immune responses, mismatch typing • Blood Loss
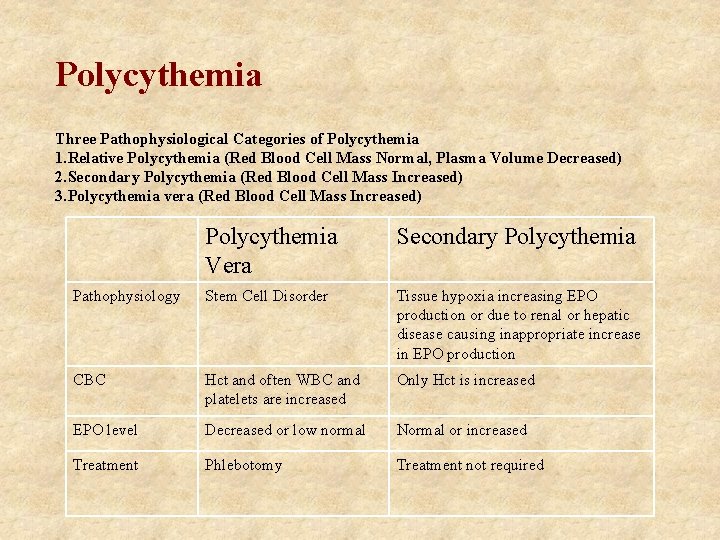
Polycythemia Three Pathophysiological Categories of Polycythemia 1. Relative Polycythemia (Red Blood Cell Mass Normal, Plasma Volume Decreased) 2. Secondary Polycythemia (Red Blood Cell Mass Increased) 3. Polycythemia vera (Red Blood Cell Mass Increased) Polycythemia Vera Secondary Polycythemia Pathophysiology Stem Cell Disorder Tissue hypoxia increasing EPO production or due to renal or hepatic disease causing inappropriate increase in EPO production CBC Hct and often WBC and platelets are increased Only Hct is increased EPO level Decreased or low normal Normal or increased Treatment Phlebotomy Treatment not required
- Slides: 30