Chapter 3 Communication Skills ROOSEVELT HEALTH SCIENCE CLINICAL


- Slides: 53
Chapter 3: Communication Skills ROOSEVELT HEALTH SCIENCE CLINICAL ROTATIONS SUCCESSFUL NURSING ASSISTANT CARE, 2 ND ED. (CH. 3) SIMMERS DHO HEALTH SCIENCE, 8 TH ED. (CH. 4) MEDICAL ASSISTING: ADMINISTRATIVE & CLINICAL COMPETENCIES, 7 TH ED (UNIT 4, 5)
Chapter 3 Objectives � Define important words � Explain the Minimum Data Set (MDS) � Explain types of communication � � Explain barriers to communication Describe how to observe and report accurately � List ways that cultures impact communication � Explain the nursing process � Identify the people you will communicate with in a facility � Discuss the nursing assistant’s role in care planning and at care conferences � Understand basic medical terminology and abbreviations � Describe incident reporting and recording � Explain proper telephone etiquette Explain how to convert regular time to military time � Describe the resident call system � Describe the nursing assistant’s role in change-of-shift reports and “rounds” � � Describe a standard resident/patient chart � Explain guidelines for documentation � � Describe the use of computers in documentation List the information found on an assignment sheet � Discuss how to organize your work and manage time.

Communication � Communication is the exchange of information with others. � Process of sending and receiving messages � People communicate with signs, symbols, and behavior. � Including words, drawings, and pictures
Verbal Communication � Communicating verbally means using words. � Speaking � and writing are examples Verbal communication also includes the way that words are spoken or written. � The tone of voice and specific words chosen are important. � Written communication should be legible.
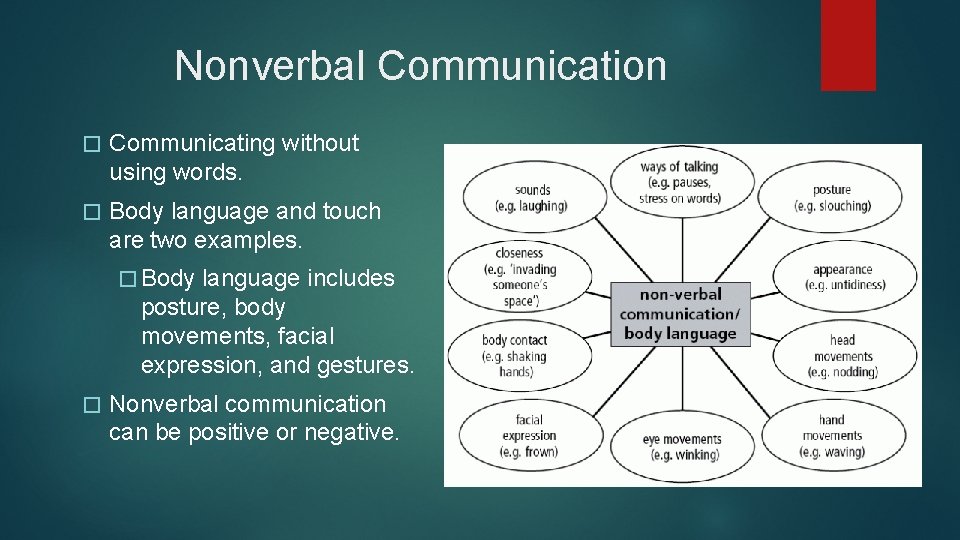
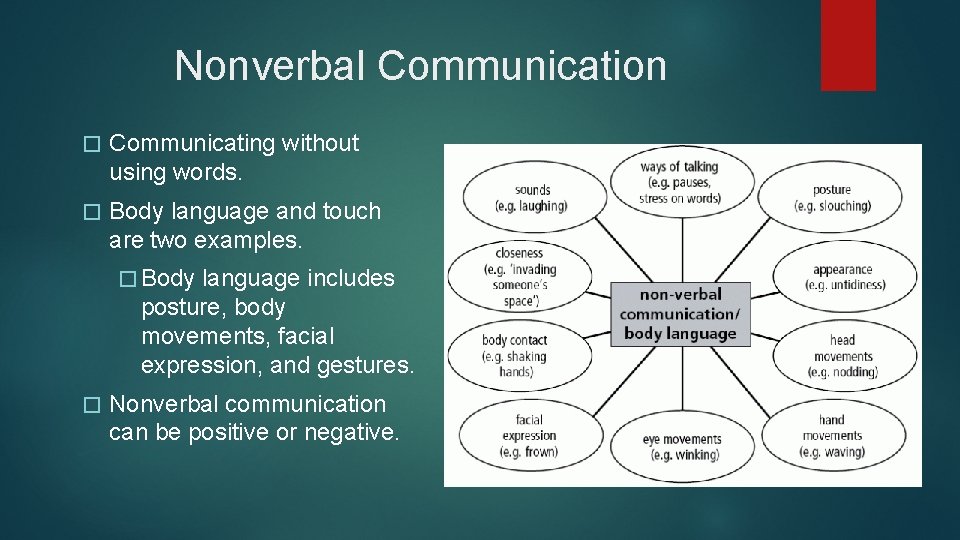
Nonverbal Communication � Communicating without using words. � Body language and touch are two examples. � Body language includes posture, body movements, facial expression, and gestures. � Nonverbal communication can be positive or negative.
Nonverbal Communication � Positive Nonverbal Communication � Smiling in a friendly manner � Leaning � Negative Nonverbal Communication � Rolling your eyes or crossing your arms forward to listen � Tapping permission, putting your hand over a resident’s hand while listening to her � Pointing � With your foot at someone while speaking
Keys to Communicating Properly � Use appropriate words. Make sure that patients are able to understand what you say. Use proper words and terms with care team members. � Be aware of your body language! � Use an acceptable tone of voice. Communicate concern and caring. � Wait for responses. Let pauses happen. Do not interrupt or try to finish the person’s sentences. � Practice active listening. � Use facts when communicating.
Active Listening � Involves giving patients your full attention while they are speaking. � Maintain good eye contact � Use phrases that encourage them to keep speaking and to clarify their communication. � Examples: Yes, Hmm, I see, I understand, Go on � Repeat the patient’s message to show you have been listening closely. � Show patients you are really interested in what they have to say by nodding and smiling.
Communication Barriers � Some patients have trouble understanding or using verbal communication due to a barrier that prevents proper communication. �Barrier- a block or obstacle
What would you do if…… The patient does not hear you, does not hear correctly, or does not understand?
The patient does not hear you, does not hear correctly, or does not understand? � Stand directly facing the patient � Speak slowly, make sure each word is spoken clearly � Speak in a low, pleasant, and professional voice � If the patient wears a hearing aid, check to see that it is on and works properly.
What would you do if…… The patient is difficult to understand?
The patient is difficult to understand? � Be patient � Take � Ask the time to listen the patient to repeat or explain � State the message in your own words to make sure you have understood. � If the patient becomes frustrated, take a break and try again in a few minutes or find someone else to listen with you.
What would you do if…… The patient speaks a different language than you do?
The patient speaks a different language than you do? � Be patient � Speak � Keep � Be slowly and clearly message short and simple alert for words the patient understands � Use pictures and gestures to communicate � Look for signs that the patient is only pretending to understand � Ask the patient’s family, friends, or other staff members who speak the patient’s language for help.
Things to Avoid � Using words that the patient/family does not understand. � Do not use slang. Do not curse. � Avoid clichés. � Clichés are phrases that are used repeatedly and do not really mean anything. Ex: “Everything will be okay. ” � Asking � “why” Asking “why” makes the patient defensive. Try saying “Is there something else you want to do? ” instead of “Why not? ” when the patient does not want to participate in a specific activity.
Things to Avoid � Giving advice � Offering your opinion is inappropriate. Patients and families should make decisions on their own or with help from doctors. � Giving medical advice is not within the scope of your practice. � Asking � Yes/No questions Ask open-ended questions; yes/no end a conversation � Conflicting � verbal and nonverbal communication Be aware of your body language and the patient’s body language!
Culture �A set of learned beliefs, values, and behaviors shared by a social, ethnic or age group. � CULTURE � Cultures � Use �Is DOES NOT MEAN RACE communicate in different ways of eye contact it a sign of respect and honesty or rude and aggressive? � Touching �Always get permission �Explain your intentions
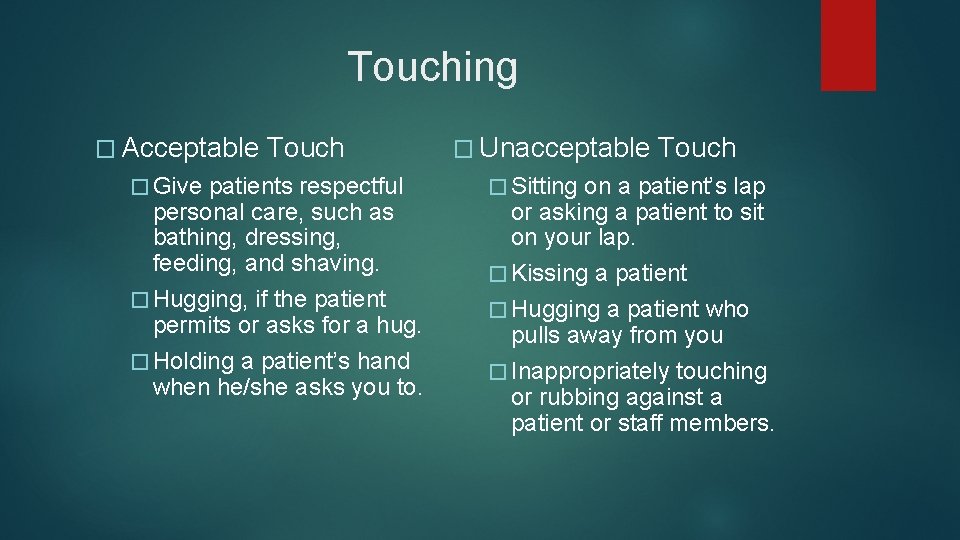
Touching � Acceptable � Give Touch patients respectful personal care, such as bathing, dressing, feeding, and shaving. � Hugging, if the patient permits or asks for a hug. � Holding a patient’s hand when he/she asks you to. � Unacceptable � Sitting Touch on a patient’s lap or asking a patient to sit on your lap. � Kissing a patient � Hugging a patient who pulls away from you � Inappropriately touching or rubbing against a patient or staff members.
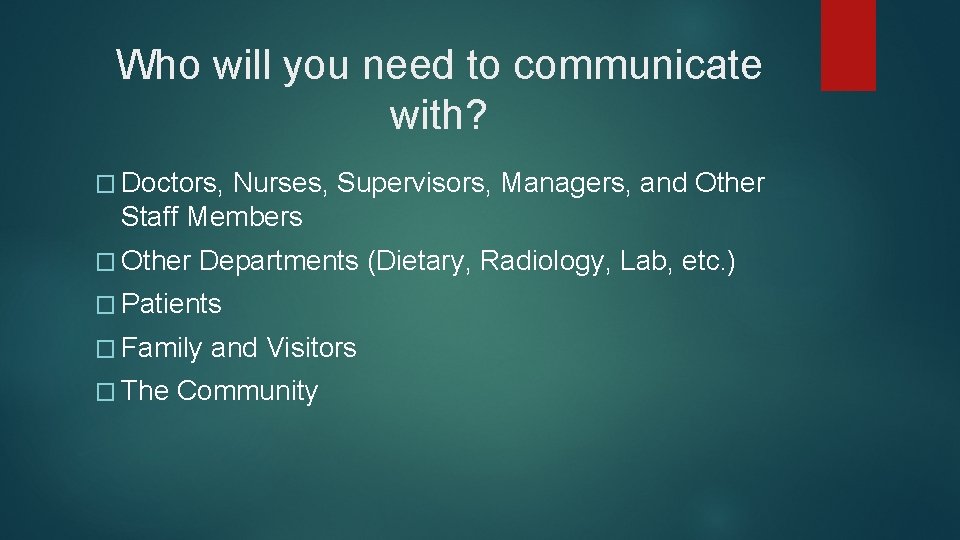
Who will you need to communicate with? � Doctors, Nurses, Supervisors, Managers, and Other Staff Members � Other Departments (Dietary, Radiology, Lab, etc. ) � Patients � Family � The and Visitors Community
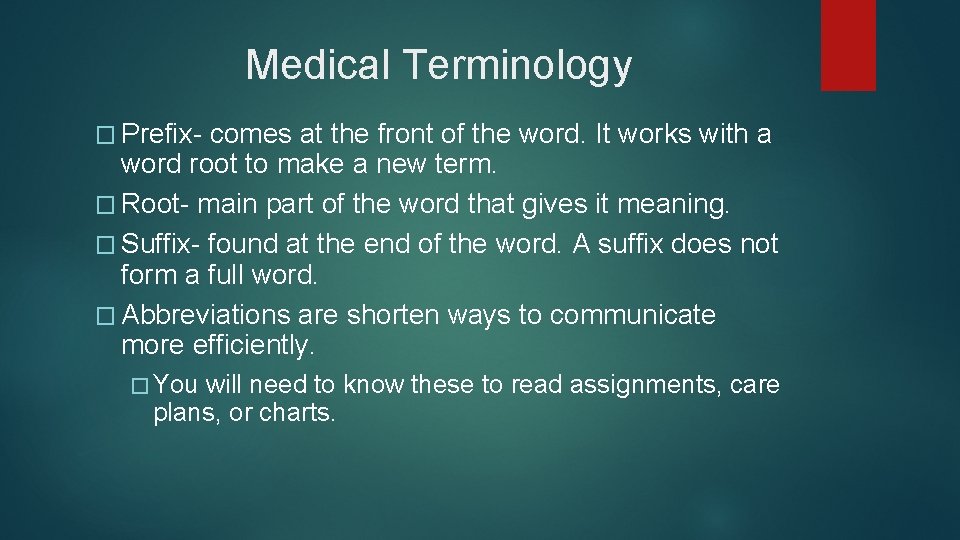
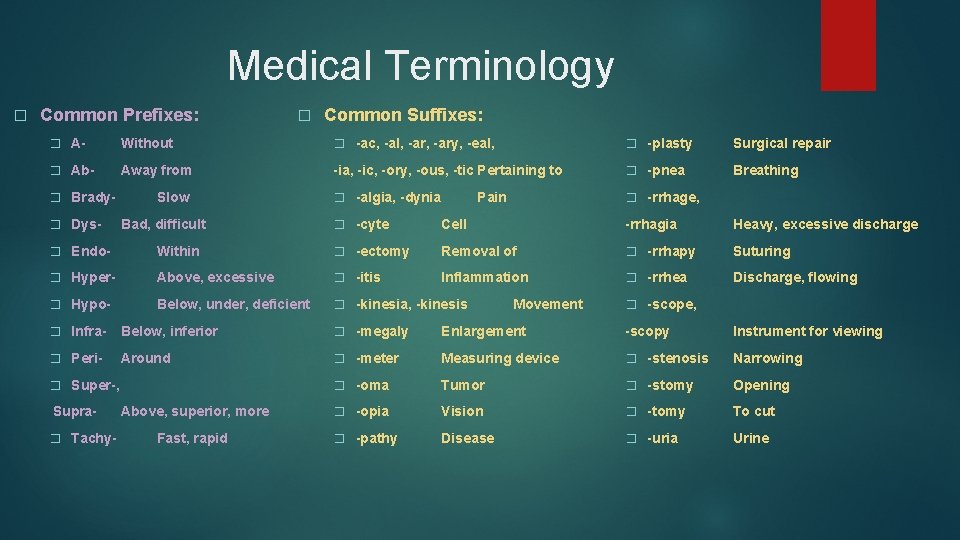
Medical Terminology � Prefix- comes at the front of the word. It works with a word root to make a new term. � Root- main part of the word that gives it meaning. � Suffix- found at the end of the word. A suffix does not form a full word. � Abbreviations are shorten ways to communicate more efficiently. � You will need to know these to read assignments, care plans, or charts.
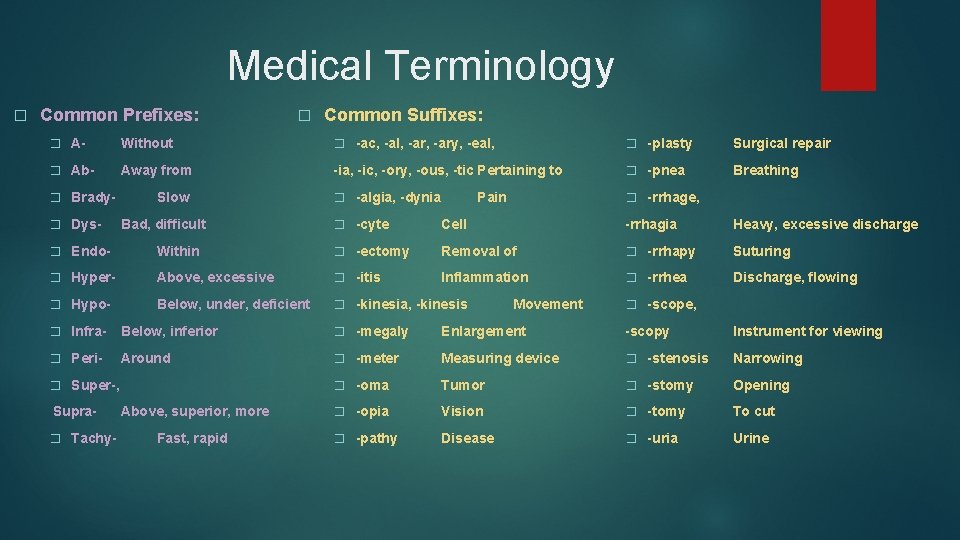
Medical Terminology � Common Prefixes: � Common Suffixes: � A- Without � -ac, -al, -ary, -eal, � -plasty Surgical repair � Ab- Away from -ia, -ic, -ory, -ous, -tic Pertaining to � -pnea Breathing � -algia, -dynia � -rrhage, � Brady� Dys- Slow Bad, difficult Pain � -cyte Cell -rrhagia Heavy, excessive discharge � Endo- Within � -ectomy Removal of � -rrhapy Suturing � Hyper- Above, excessive � -itis Inflammation � -rrhea Discharge, flowing � Hypo- Below, under, deficient � -kinesia, -kinesis Movement � -scope, � Infra- Below, inferior � -megaly Enlargement -scopy Instrument for viewing � Peri- Around � -meter Measuring device � -stenosis Narrowing � -oma Tumor � -stomy Opening � -opia Vision � -tomy To cut � -pathy Disease � -uria Urine � Super-, Supra� Tachy- Above, superior, more Fast, rapid
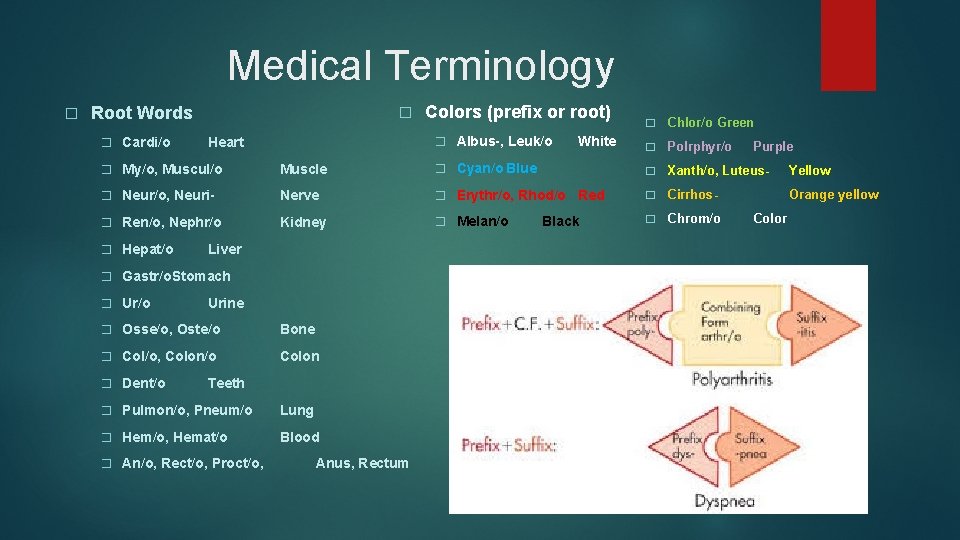
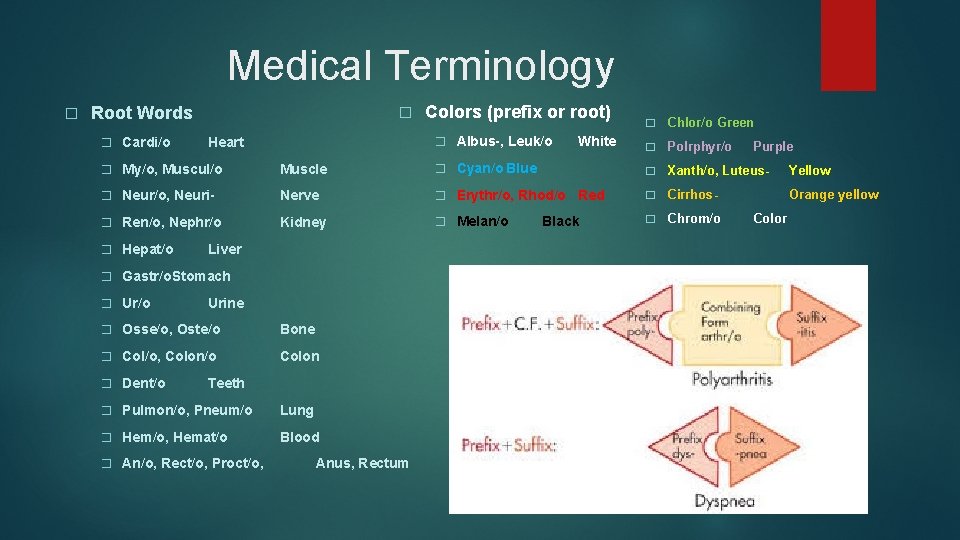
Medical Terminology � Root Words � Cardi/o � Colors (prefix or root) � Albus-, Leuk/o Heart � My/o, Muscul/o Muscle � Cyan/o Blue � Neur/o, Neuri- Nerve � Erythr/o, Rhod/o � Ren/o, Nephr/o Kidney � Melan/o � Hepat/o Liver � Gastr/o. Stomach � Ur/o Urine � Osse/o, Oste/o Bone � Col/o, Colon/o Colon � Dent/o Teeth � Pulmon/o, Pneum/o Lung � Hem/o, Hemat/o Blood � An/o, Rect/o, Proct/o, Anus, Rectum White Red Black � Chlor/o Green � Polrphyr/o � Xanth/o, Luteus- Yellow � Cirrhos- Orange yellow � Chrom/o Purple Color
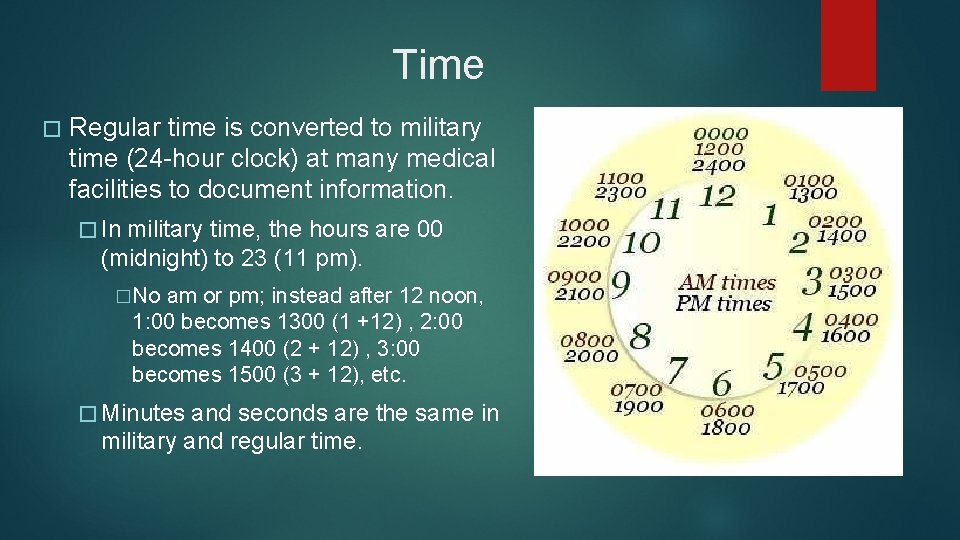
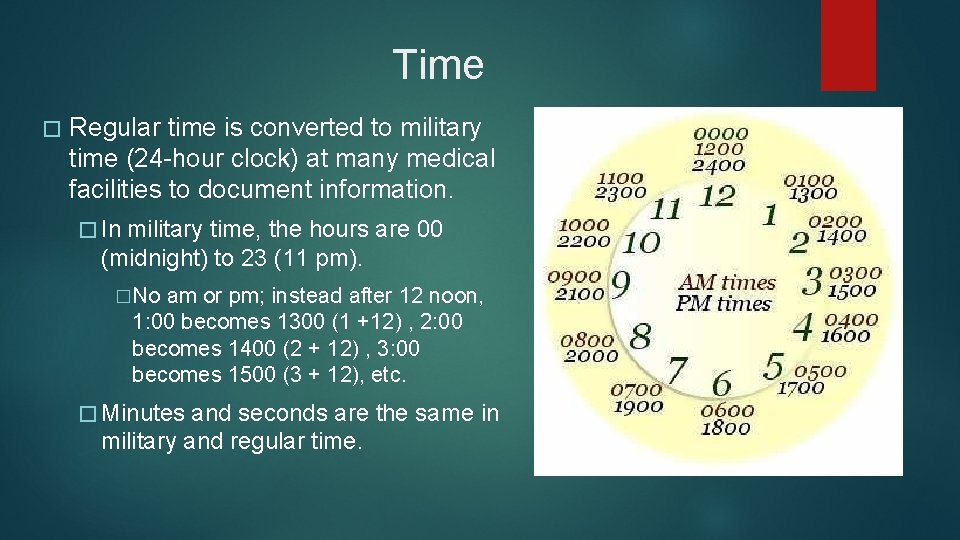
Time � Regular time is converted to military time (24 -hour clock) at many medical facilities to document information. � In military time, the hours are 00 (midnight) to 23 (11 pm). �No am or pm; instead after 12 noon, 1: 00 becomes 1300 (1 +12) , 2: 00 becomes 1400 (2 + 12) , 3: 00 becomes 1500 (3 + 12), etc. � Minutes and seconds are the same in military and regular time.
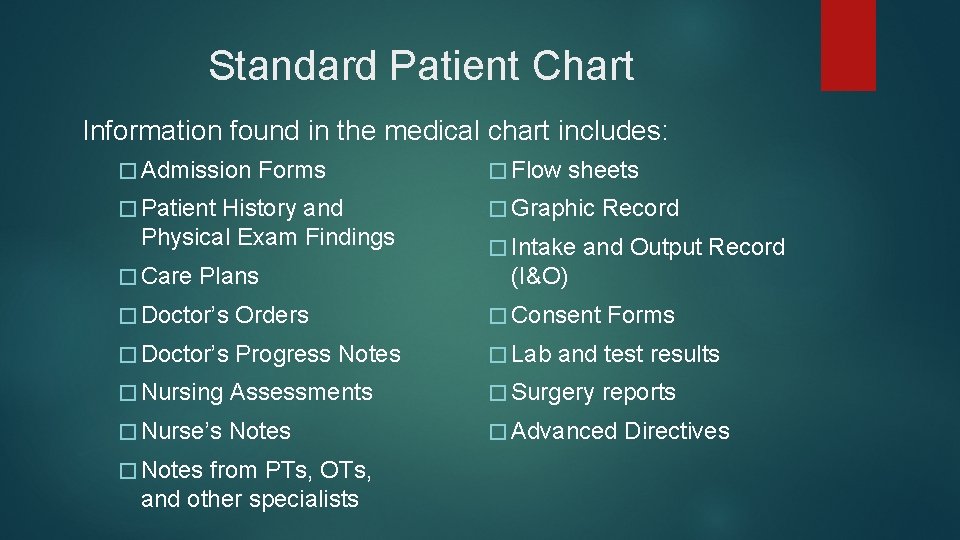
Standard Patient Chart �A chart is a legal record of a patient’s care, it is also called a medical record. � What is written in the chart is considered in court to be what actually happened. � It is the nursing assistant’s job to gather info and report it to the nurse. Writing down your observations and care is known as charting. �A computer is often used for charting, these are called Electronic Medical Records. � Charts and other medical info cannot be shared with anyone except for the care team (HIPAA).
Standard Patient Chart Information found in the medical chart includes: � Admission Forms � Patient History and Physical Exam Findings � Care Plans � Flow sheets � Graphic � Intake Record and Output Record (I&O) � Doctor’s Orders � Consent � Doctor’s Progress Notes � Lab � Nursing Assessments � Surgery � Nurse’s Notes � Advanced � Notes from PTs, OTs, and other specialists Forms and test results reports Directives
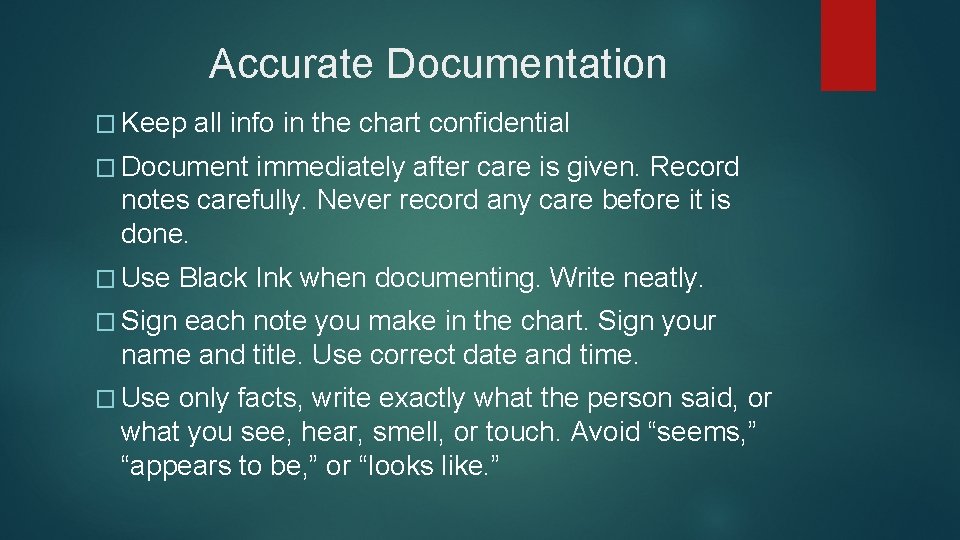
Accurate Documentation � Keep all info in the chart confidential � Document immediately after care is given. Record notes carefully. Never record any care before it is done. � Use Black Ink when documenting. Write neatly. � Sign each note you make in the chart. Sign your name and title. Use correct date and time. � Use only facts, write exactly what the person said, or what you see, hear, smell, or touch. Avoid “seems, ” “appears to be, ” or “looks like. ”
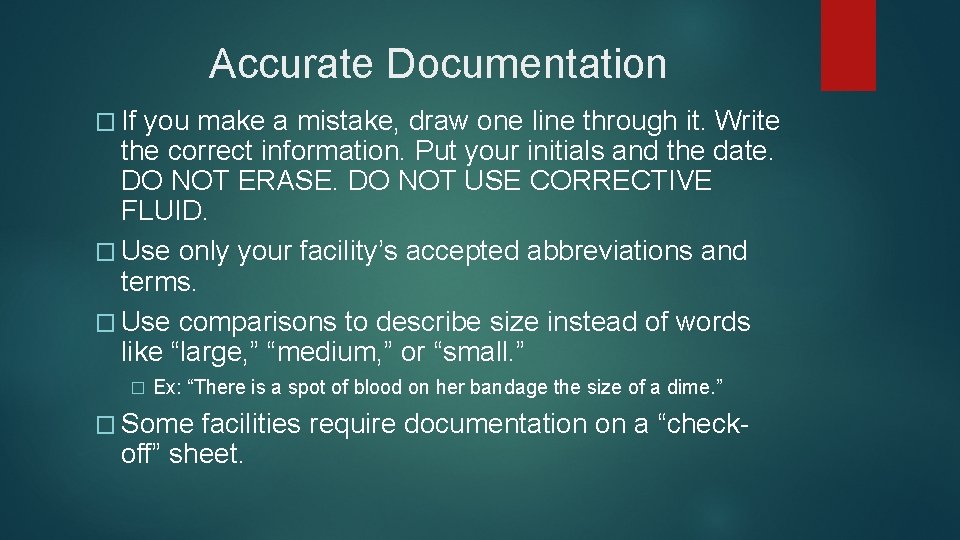
Accurate Documentation � If you make a mistake, draw one line through it. Write the correct information. Put your initials and the date. DO NOT ERASE. DO NOT USE CORRECTIVE FLUID. � Use only your facility’s accepted abbreviations and terms. � Use comparisons to describe size instead of words like “large, ” “medium, ” or “small. ” � Ex: “There is a spot of blood on her bandage the size of a dime. ” � Some facilities require documentation on a “checkoff” sheet.
Computers in Documentation � Many facilities use computers to document information about the patient. � They will train staff on computer use. � Computers can easily store information that can be retrieved when needed. � Vital signs, laboratory results, radiologic reports, and comments from other physicians. � Using a computer for charting is faster and more legible than writing by hand. � Staff input information each time they enter and leave the room. � Some facilities have a computer in every resident’s room.
Computers in Documentation � General rules for computer use: � Do not share your personal password or login ID with anyone � Do not access personal e-mail accounts at work � Do not view inappropriate websites from work � Log off the computer when you are done with charting or using the computer � HIPAA guidelines apply to computer use. Be careful about who can see private or protected health information on the computer screen.
Minimum Data Set (MDS) � MDS is a manual that is used as an assessment tool for long-term care facilities. � Developed by the Federal Government in 1990, and is updated periodically. � Gives detailed guidelines for assessing residents, and provides a protocol when problems are identified. � Gives facilities a structured, standardized approach to care. � Facilities must complete the MDS for each resident within 14 days of admission, and again each year. They must also be reviewed for each patient every 3 months. � A new MDS is done when there is any major change in a resident’s condition. �
Nursing Assistants!
Care Plans � Care Plan- written plan for each patient created by the nurse. � Outlines steps and tasks that the care team must perform to help the patient reach his/her goals. � To plan care, nurses must collect info from staff. �Includes objective and subjective information
Signs v. Symptoms � Objective Information � Based on what you see, touch, or smell. � Also called signs � FACT � Subjective Information � Info collected from something that patients or their families report to you. � May not be accurate � Also called symptoms � OPINION
Using the 4 senses � Sight: look for changes in appearance, such as redness, swelling, rashes, discharge, changes in the eyes or ears or ability to move. � Hearing: Listen to what the resident tells you. Make sure he is making sense. Check to see if his breathing is normal. Note if he is coughing or gasping. Report if he is showing emotions, such as anger or sadness. � Smell: Check for odors coming from the resident’s body or mouth. Odors can indicate an infection, a need for bathing, or poor mouth care. � Touch: Note if the skin seems hot or cool. Check to see if it is dry or moist.
Other Observations � Note any changes in orientation. Does the patient know who she is, who you are, where she is, and what year it is? � Check to see if the patient’s vital signs are normal or abnormal. � Report any changes in ability. Has there been a change in the patient’s ability to move a part of her body? � Report other important changes, such as changes in weight or overall appetite, changes in ability to go to the bathroom, and changes in mood.
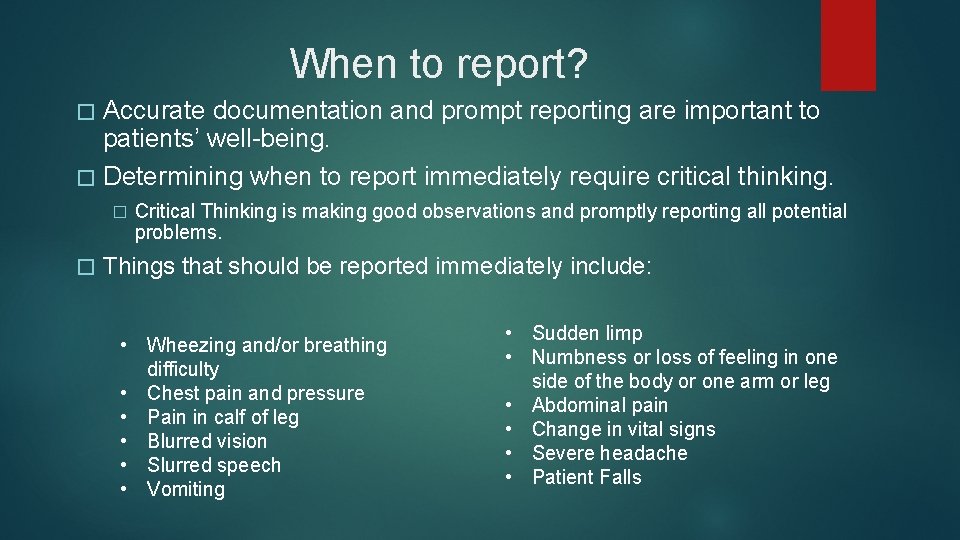
When to report? � Accurate documentation and prompt reporting are important to patients’ well-being. � Determining when to report immediately require critical thinking. � � Critical Thinking is making good observations and promptly reporting all potential problems. Things that should be reported immediately include: • Wheezing and/or breathing difficulty • Chest pain and pressure • Pain in calf of leg • Blurred vision • Slurred speech • Vomiting • Sudden limp • Numbness or loss of feeling in one side of the body or one arm or leg • Abdominal pain • Change in vital signs • Severe headache • Patient Falls
Nursing Process � Organized method used by nurses to determine patients’ needs, plan the appropriate care to meet those needs, and evaluate how well the care plan is working. � 5 steps � Assessment � Diagnosis � Planning � Implementation � Evaluation
Assessment and Diagnosis � Assessment � Getting information from many sources, such as medical history and a physical assessment, and reviewing it; the purpose is to identify actual or potential problems. � Diagnosis � The identification of health problems after looking at all the patient’s needs; complete to make a care plan.
Planning, Implementation, and Evaluation � Planning � In agreement with the patient, goals are set and a care plan is created to meet the patient’s needs. � Implementation � Putting the care plan into action; giving care. � Evaluation �A careful examination to see if goals were met or progress was achieve; if progress is slow or if the problem worsened, the care plan must be changed.
Care Conference � Care plans may be written at a special care conference, where member of the care team meet to share and gather ideas. � CNA’s share observations from resident care. Always talk to the nurse before the care conference if you are not sure what to say. � Care plans are usually kept at the nurse’s station in a Kardex (type of card file) or by the resident’s room.
Incidents � An incident is an accident, problem, or unexpected event during the course of care. � Ex: Patient falls while being taken to the bathroom � Sentinel event- unexpected occurrence involving death or serious physical or psychological injury. � Ex: Patient falls out of bed and breaks hip � Incident reports- documentation reporting the incident and the response to it. � Confidential and based on facts � Give to Charge Nurse � Always fill one out, even if the event seemed minor � Complete as soon as possible after the incident occurs so that the details are not forgotten.

Telephone Etiquette � Greet the caller cheerfully, with “Good morning, ” “Good afternoon, ” or “Good evening. ” � Identify the facility: “Evergreen Skilled Nursing” � Identify yourself and your position � Listen closely to the caller’s request. Write down messages. Ask for correct spelling of names. � In � Say emergencies, take action immediately “Thank you, ” and “Goodbye”
Telephone Etiquette � Do not give out any information about staff or patients over the phone. � Refer patient status questions to a supervisor � Always ask someone to be hold, before you got get a supervisor or someone else. � You may need to transfer a call. You should be trained at the facility on how to do this � Follow specific phone, cell phone, and pager policies at the facility.
Patient Call System � Patients signal staff when they need them for whatever purpose through the call system. � Sometimes � Always called signal light or call light respond to call lights promptly, it can save someone’s life. � Do not ignore call lights, doing so can be considered neglect or abuse under the law. � Answer call lights for patients other than your own. � Always leave the call light within the patients’ reach before leaving the room.
Shift Change Reports � There are start-of-shift reports and end-of-shift reports. � CNAs � The go to start, Nurses go to both care team gather to discuss and plan patients’ care for a shift. � Shifts vary from 8, 10, or 12 hours � At start of shift reports, listen to important information about all of the residents in the area. � Examples of information passed on to the next shift are appetite problems, complaints of pain, or a change in the ability to move. � Special information shared during a report may include new admissions and transfers or discharges from the facility. � Before the end of shift report, tell the nurses about such things as changes in pulse or temperature and skin changes that could signal that start of pressure sores.
Rounds � Staff members move from room-to-room and discuss each patient and the care plan. � This is what you see on tv � Physicians � Nurses tend to make rounds may round, separately
Assignment Sheet � An assignment sheet lists all patients and has all of the tasks that you must do for them. � Certain tasks are done daily (ADLs) � You may asked to do range of motion (ROM), exercises done to bring joints through a full range of movement. � Code status- lists whether the patient has an advanced directive or not. �A “code” is when a group of specially-trained staff provide advanced life support during a medical emergency.
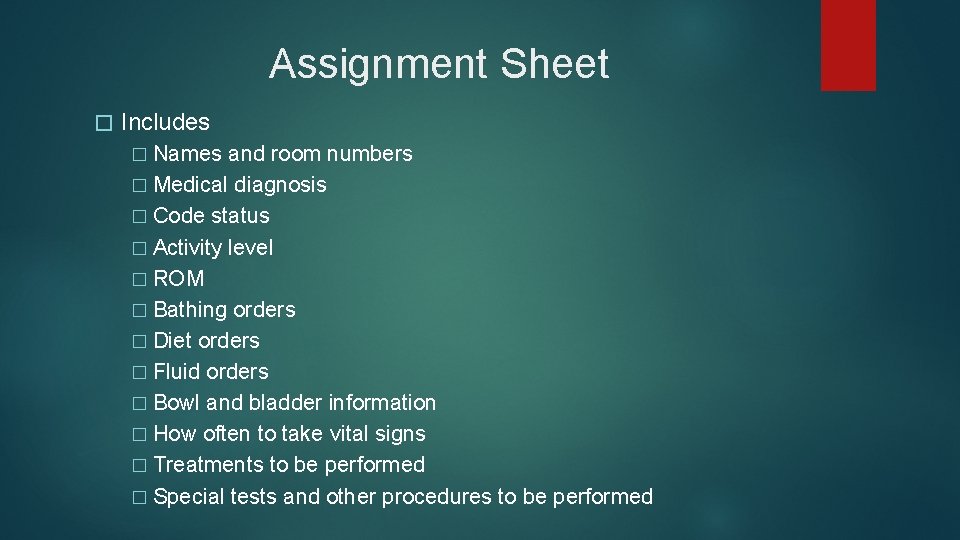
Assignment Sheet � Includes � Names and room numbers � Medical diagnosis � Code status � Activity level � ROM � Bathing orders � Diet orders � Fluid orders � Bowl and bladder information � How often to take vital signs � Treatments to be performed � Special tests and other procedures to be performed
Organizing In order to complete assignments each day, you must learn to organize your work. � After you receive your assignment, make rounds on all of your patients. � Check to see if any patients require immediate help or care. � Answer � Write call lights, make sure all patients can reach the call light. down any reminders on a notepad. Write down anything important on the assignment sheet.
Organizing � Decide the order of patients you will see. � Making a schedule will help you to be realistic about what can be done during the day. � Prioritize � Each � Do and combine activities. facility will have its own schedule of events and care. not be afraid to ask for help.
Communication � Super important � Includes � Ask spoken, written, and body language for help when you need it � Have a positive attitude and body language, so show that you are approachable.