Chapter 28 The Reproductive System The Reproductive Systems
- Slides: 88
Chapter 28 The Reproductive System
The Reproductive Systems Reproductive organs grouped by function Gonads - testes and ovaries u produce gametes and secrete hormones u production of gametes, fluid, discharge into ducts indicate exocrine glands u production of hormones indicate endocrine glands Ducts - transport, store, receive gametes Accessory sex glands - gamete support Supporting structures - various reproductive roles
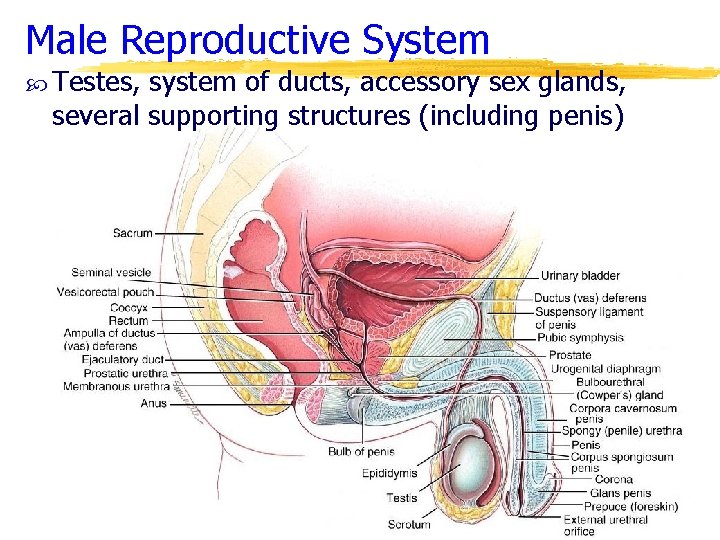
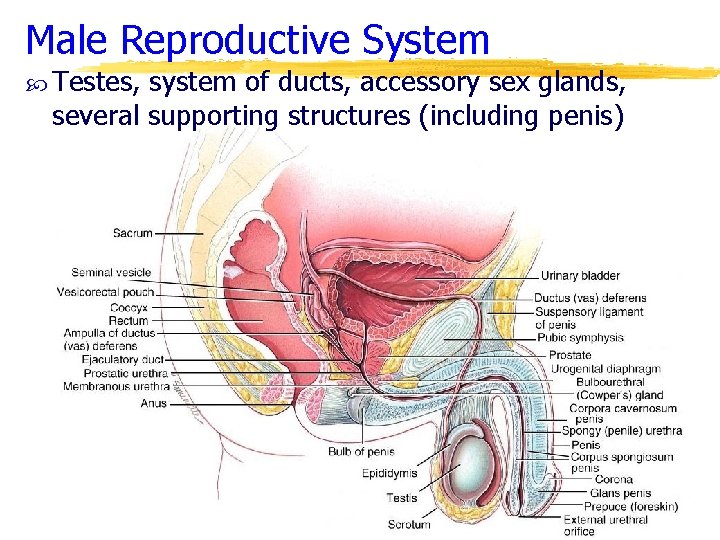
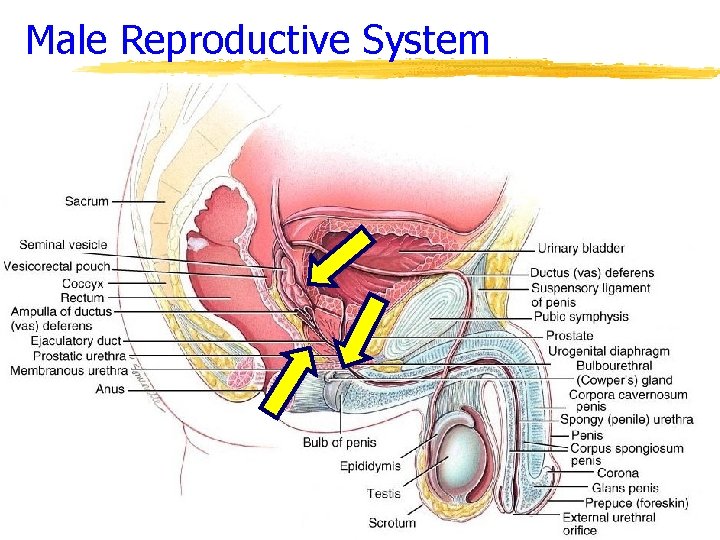
Male Reproductive System Testes, system of ducts, accessory sex glands, several supporting structures (including penis)
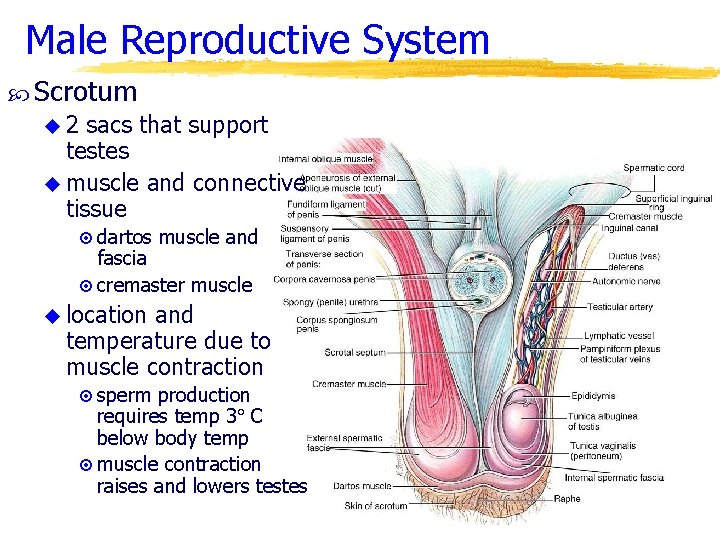
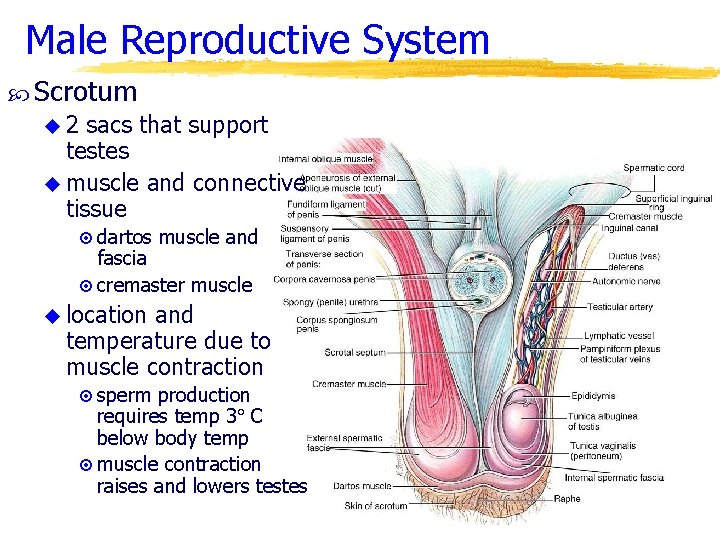
Male Reproductive System Scrotum u 2 sacs that support testes u muscle and connective tissue ¤ dartos muscle and fascia ¤ cremaster muscle u location and temperature due to muscle contraction ¤ sperm production requires temp 3 C below body temp ¤ muscle contraction raises and lowers testes
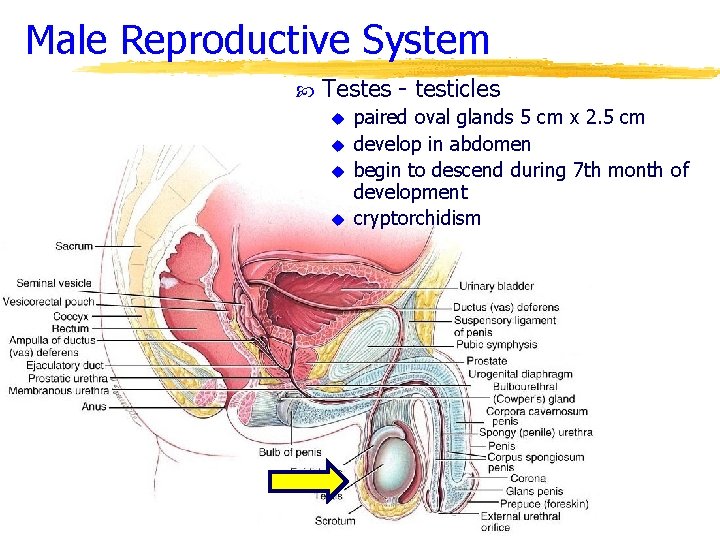
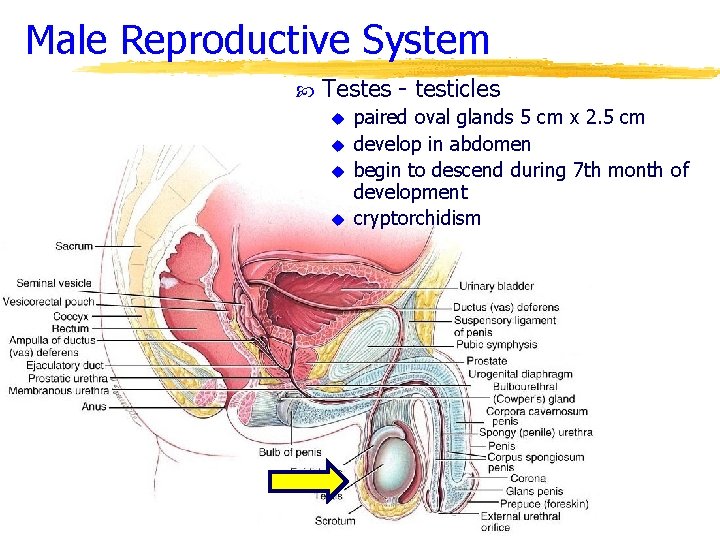
Male Reproductive System Testes - testicles u u paired oval glands 5 cm x 2. 5 cm develop in abdomen begin to descend during 7 th month of development cryptorchidism
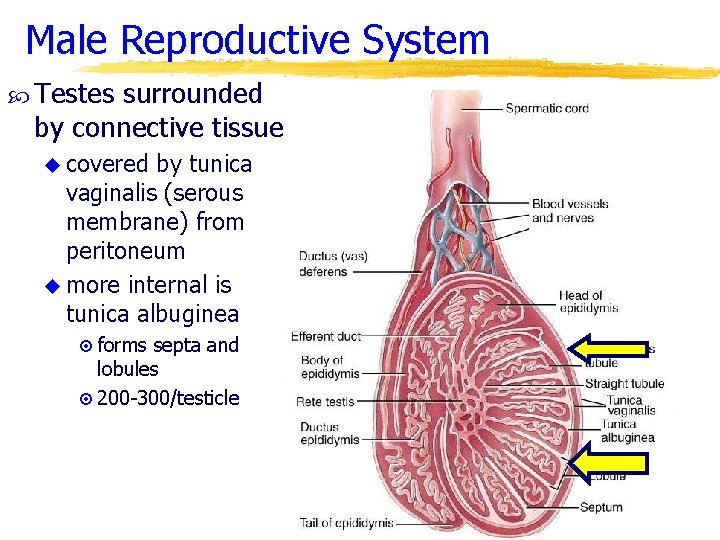
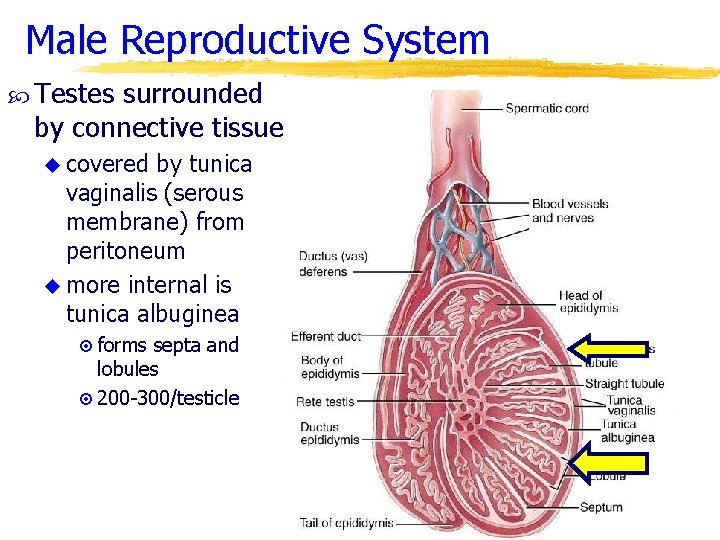
Male Reproductive System Testes surrounded by connective tissue u covered by tunica vaginalis (serous membrane) from peritoneum u more internal is tunica albuginea ¤ forms septa and lobules ¤ 200 -300/testicle
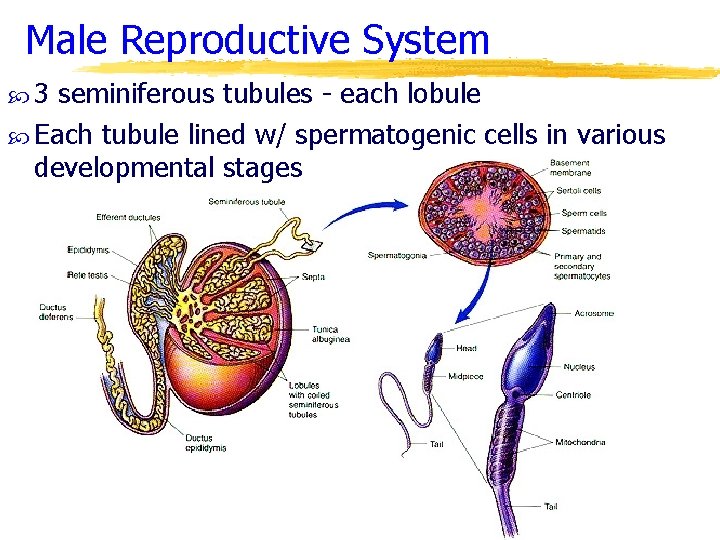
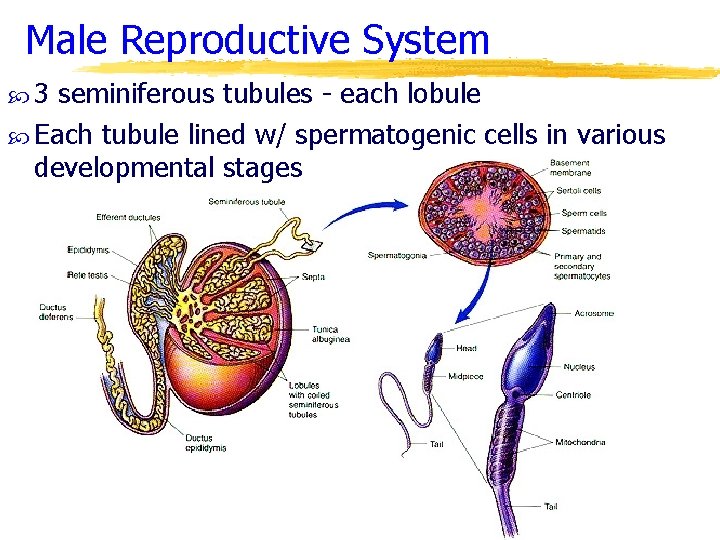
Male Reproductive System 3 seminiferous tubules - each lobule Each tubule lined w/ spermatogenic cells in various developmental stages
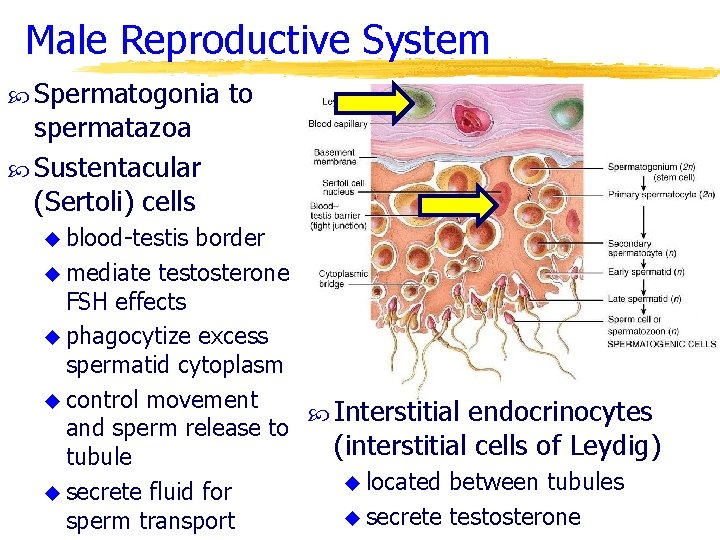
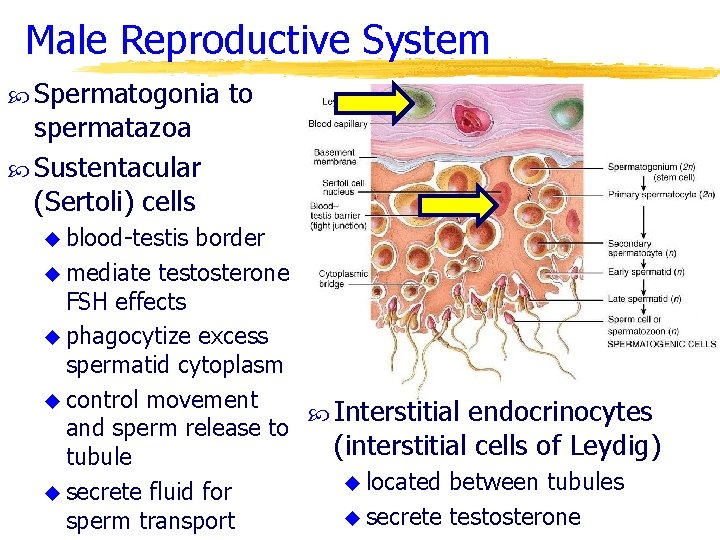
Male Reproductive System Spermatogonia spermatazoa Sustentacular (Sertoli) cells u blood-testis to border u mediate testosterone FSH effects u phagocytize excess spermatid cytoplasm u control movement Interstitial endocrinocytes and sperm release to (interstitial cells of Leydig) tubule u located between tubules u secrete fluid for u secrete testosterone sperm transport
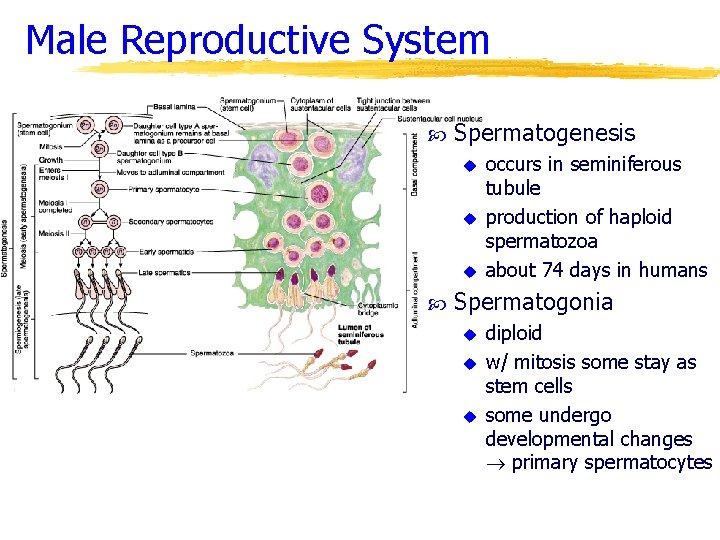
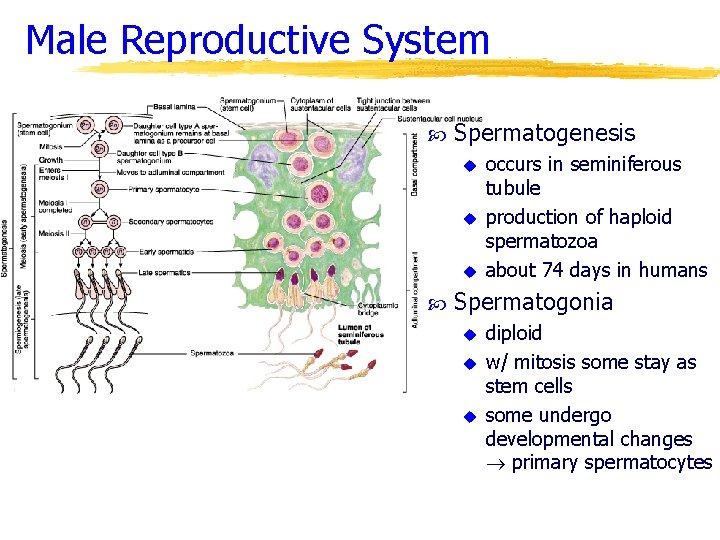
Male Reproductive System Spermatogenesis u u u occurs in seminiferous tubule production of haploid spermatozoa about 74 days in humans Spermatogonia u u u diploid w/ mitosis some stay as stem cells some undergo developmental changes primary spermatocytes
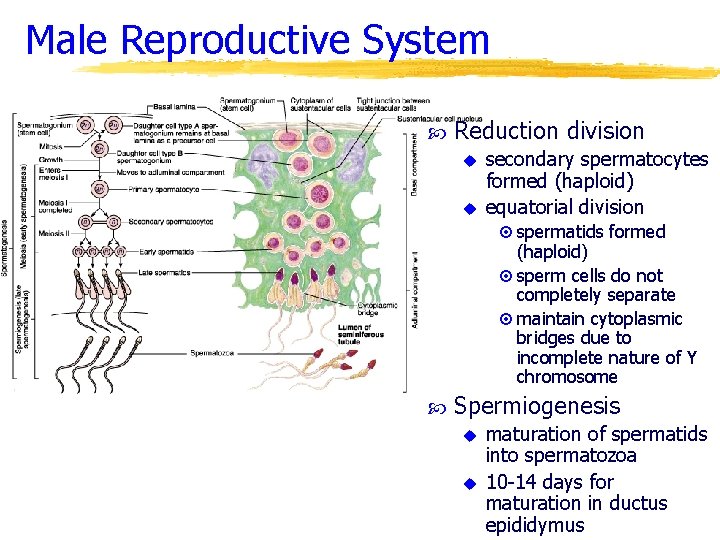
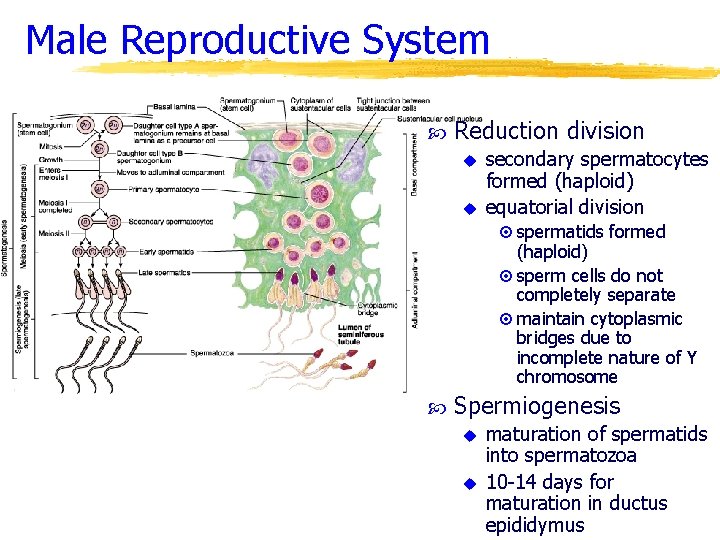
Male Reproductive System Reduction division u u secondary spermatocytes formed (haploid) equatorial division ¤ spermatids formed (haploid) ¤ sperm cells do not completely separate ¤ maintain cytoplasmic bridges due to incomplete nature of Y chromosome Spermiogenesis u u maturation of spermatids into spermatozoa 10 -14 days for maturation in ductus epididymus
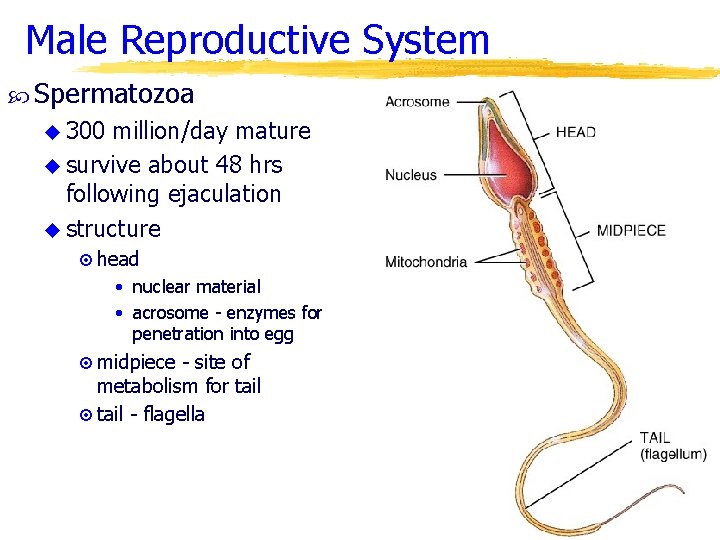
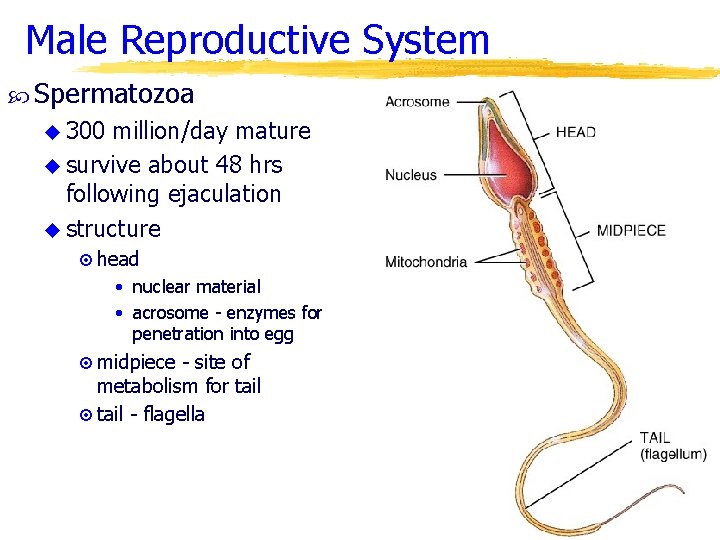
Male Reproductive System Spermatozoa u 300 million/day mature u survive about 48 hrs following ejaculation u structure ¤ head • nuclear material • acrosome - enzymes for penetration into egg ¤ midpiece - site of metabolism for tail ¤ tail - flagella
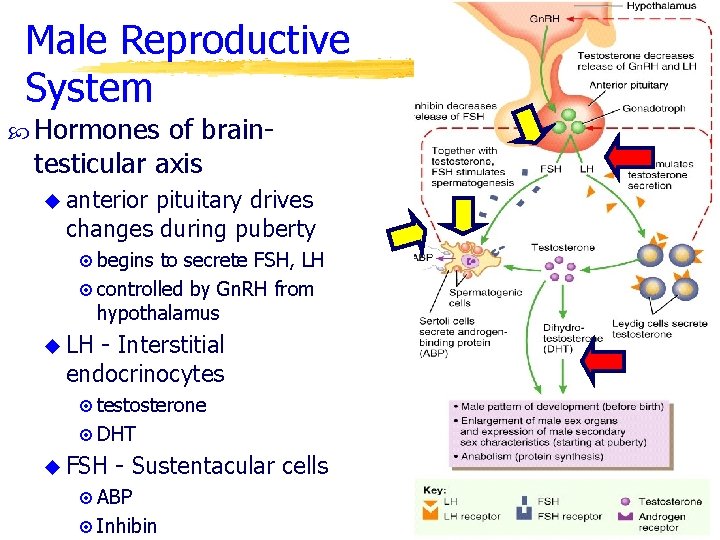
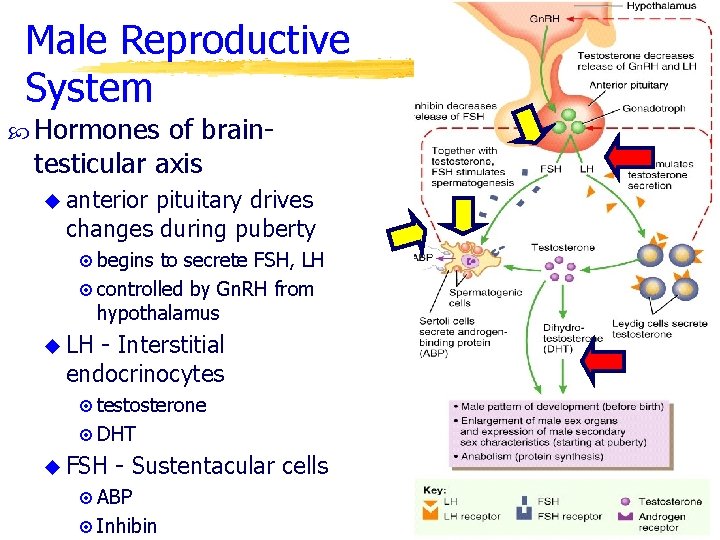
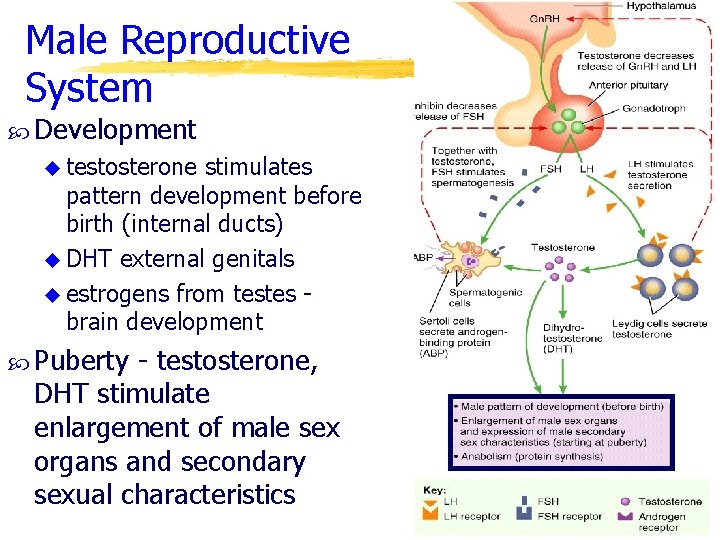
Male Reproductive System Hormones of braintesticular axis u anterior pituitary drives changes during puberty ¤ begins to secrete FSH, LH ¤ controlled by Gn. RH from hypothalamus u LH - Interstitial endocrinocytes ¤ testosterone ¤ DHT u FSH - Sustentacular cells ¤ ABP ¤ Inhibin
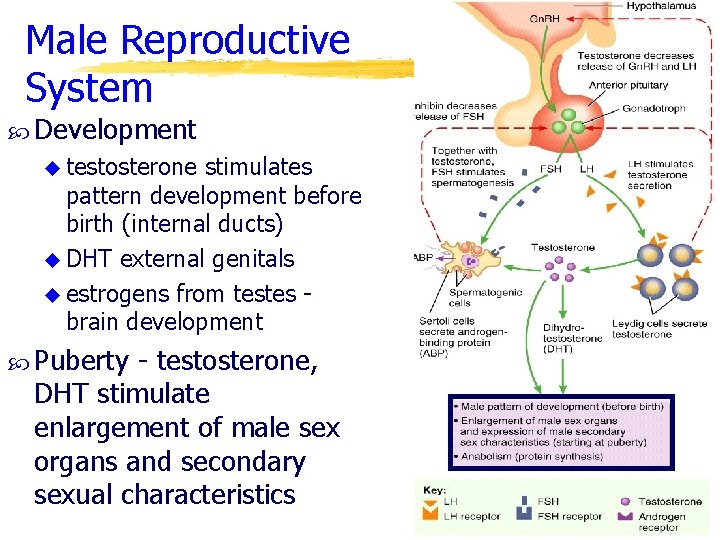
Male Reproductive System Development u testosterone stimulates pattern development before birth (internal ducts) u DHT external genitals u estrogens from testes brain development Puberty - testosterone, DHT stimulate enlargement of male sex organs and secondary sexual characteristics
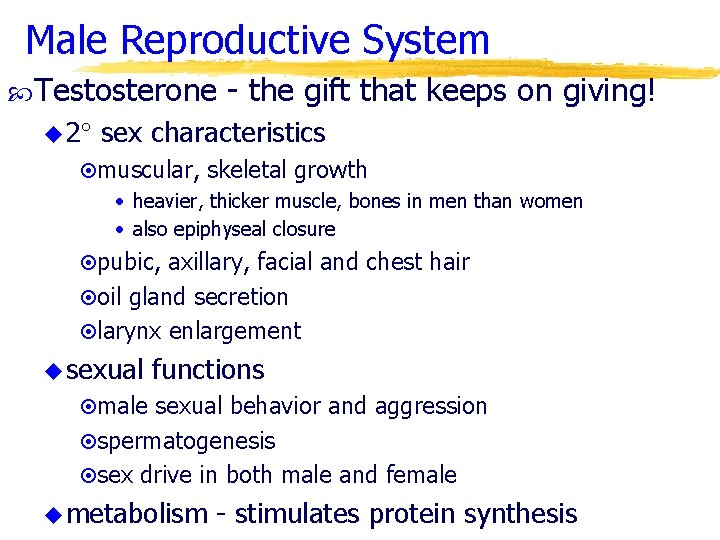
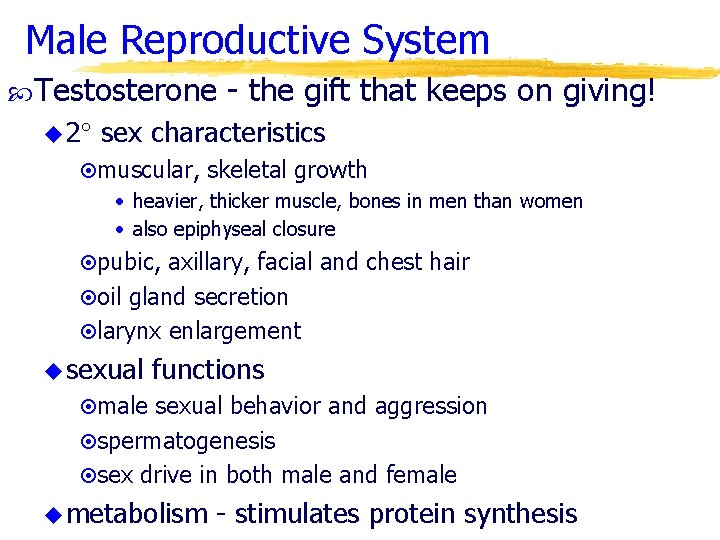
Male Reproductive System Testosterone u 2 - the gift that keeps on giving! sex characteristics ¤muscular, skeletal growth • heavier, thicker muscle, bones in men than women • also epiphyseal closure ¤pubic, axillary, facial and chest hair ¤oil gland secretion ¤larynx enlargement u sexual functions ¤male sexual behavior and aggression ¤spermatogenesis ¤sex drive in both male and female u metabolism - stimulates protein synthesis
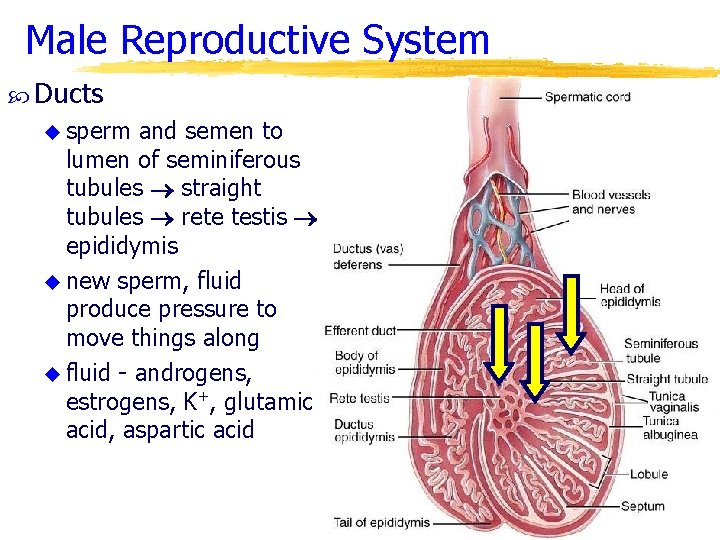
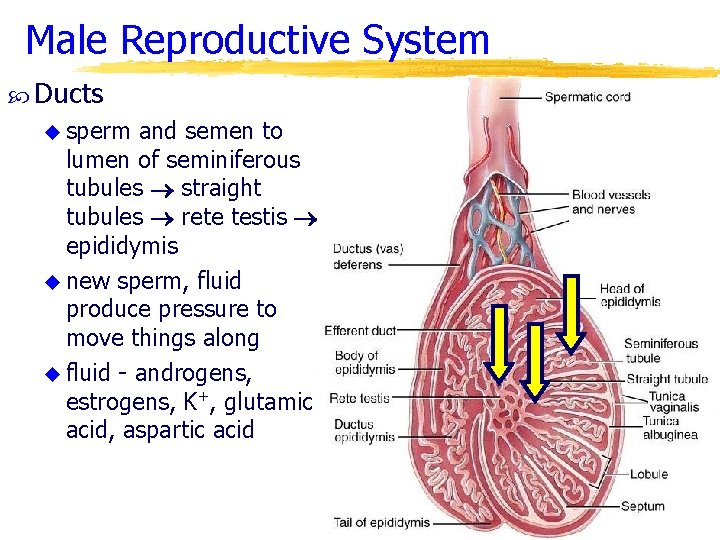
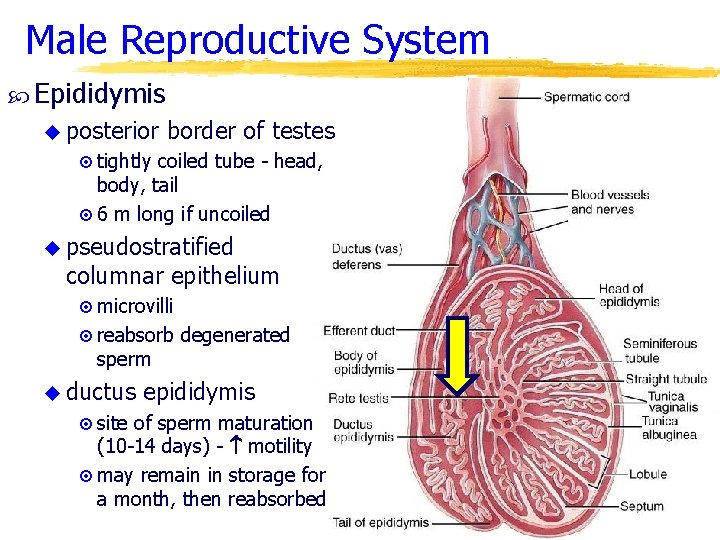
Male Reproductive System Ducts u sperm and semen to lumen of seminiferous tubules straight tubules rete testis epididymis u new sperm, fluid produce pressure to move things along u fluid - androgens, estrogens, K+, glutamic acid, aspartic acid
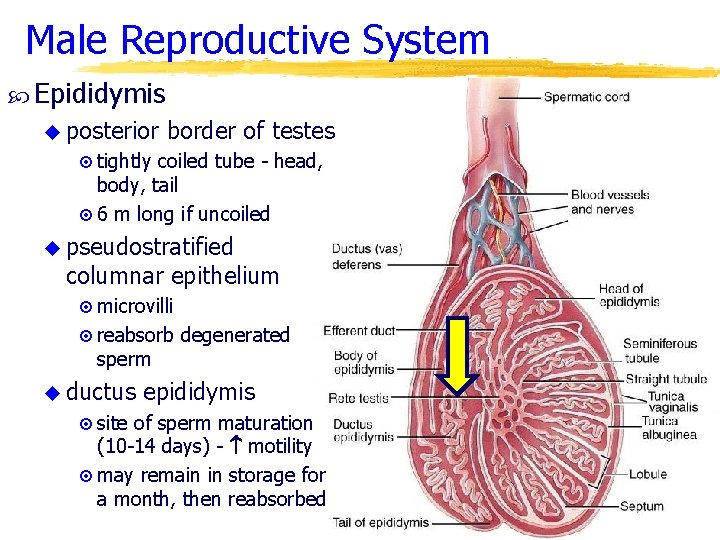
Male Reproductive System Epididymis u posterior border of testes ¤ tightly coiled tube - head, body, tail ¤ 6 m long if uncoiled u pseudostratified columnar epithelium ¤ microvilli ¤ reabsorb degenerated sperm u ductus epididymis ¤ site of sperm maturation (10 -14 days) - motility ¤ may remain in storage for a month, then reabsorbed
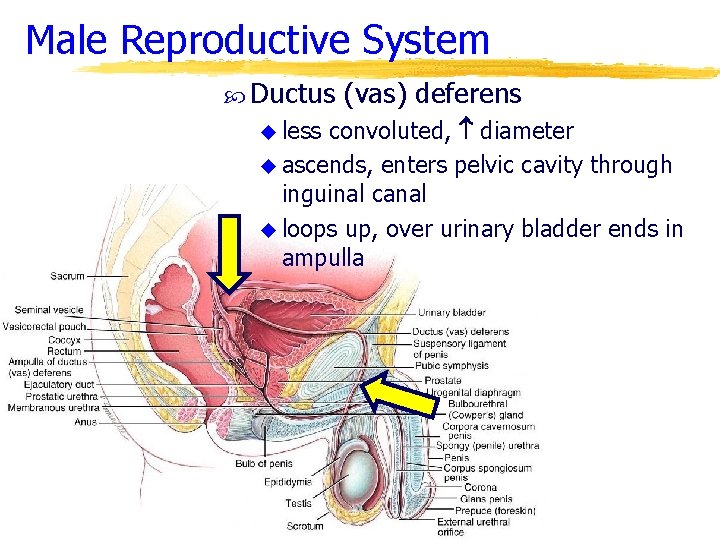
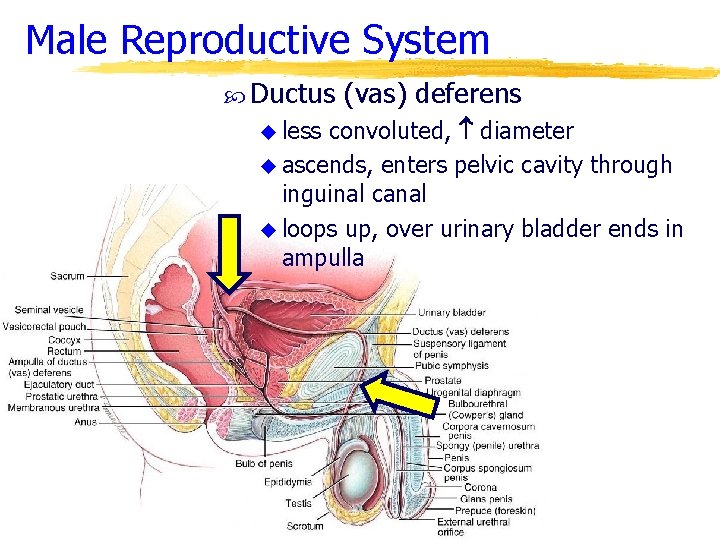
Male Reproductive System Ductus (vas) deferens convoluted, diameter u ascends, enters pelvic cavity through inguinal canal u loops up, over urinary bladder ends in ampulla u less
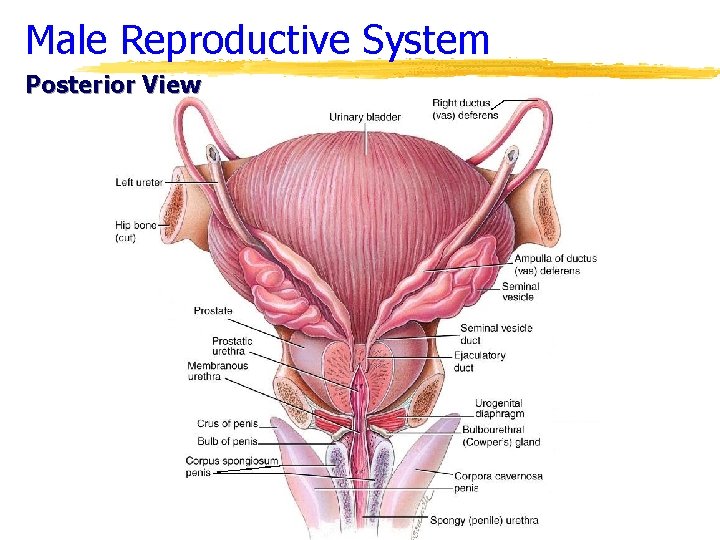
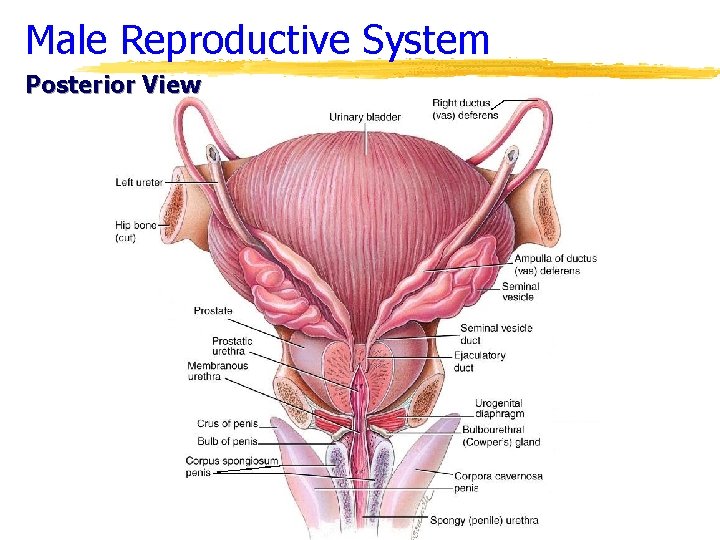
Male Reproductive System Posterior View
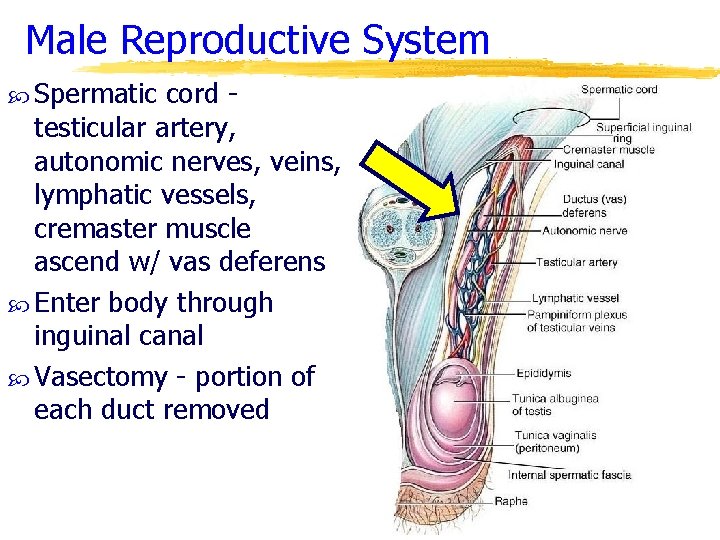
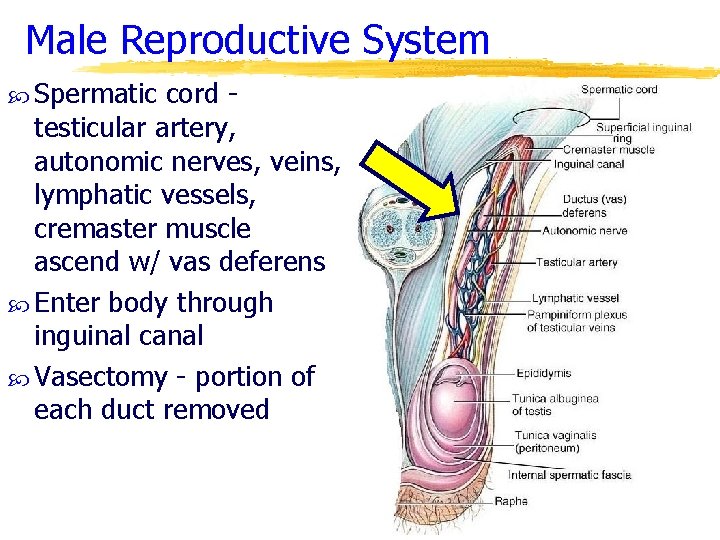
Male Reproductive System Spermatic cord testicular artery, autonomic nerves, veins, lymphatic vessels, cremaster muscle ascend w/ vas deferens Enter body through inguinal canal Vasectomy - portion of each duct removed
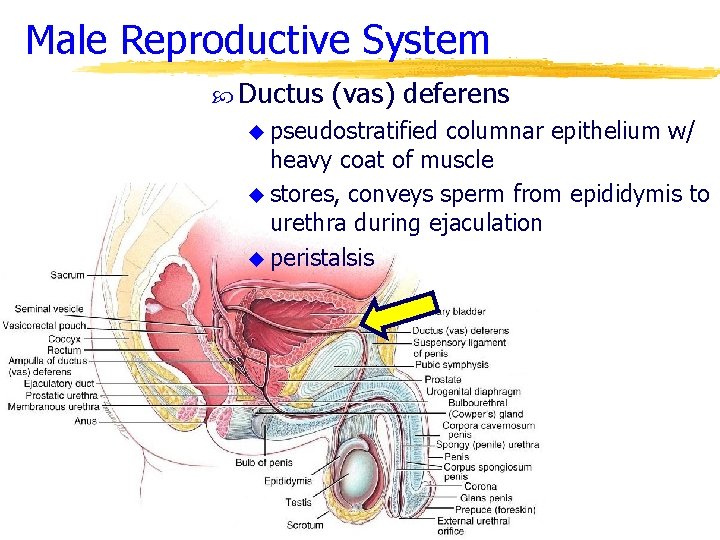
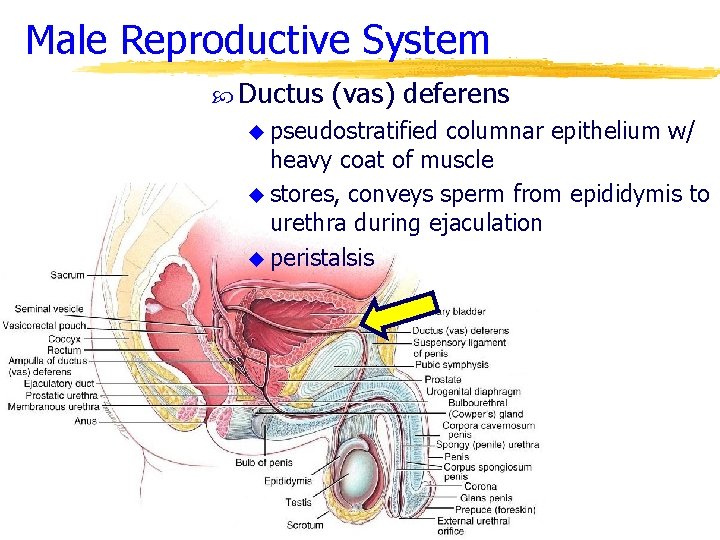
Male Reproductive System Ductus (vas) deferens u pseudostratified columnar epithelium w/ heavy coat of muscle u stores, conveys sperm from epididymis to urethra during ejaculation u peristalsis
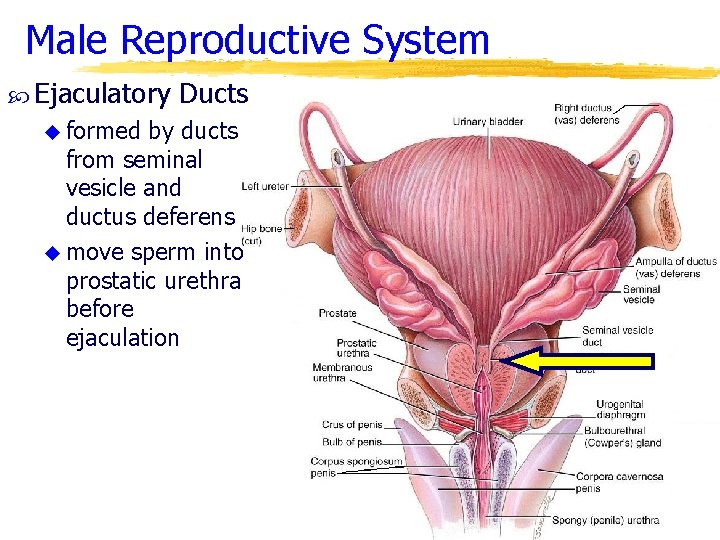
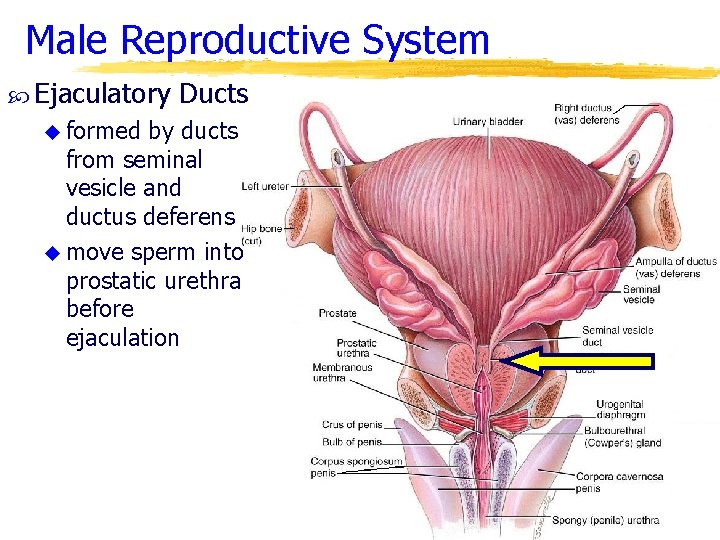
Male Reproductive System Ejaculatory u formed Ducts by ducts from seminal vesicle and ductus deferens u move sperm into prostatic urethra before ejaculation
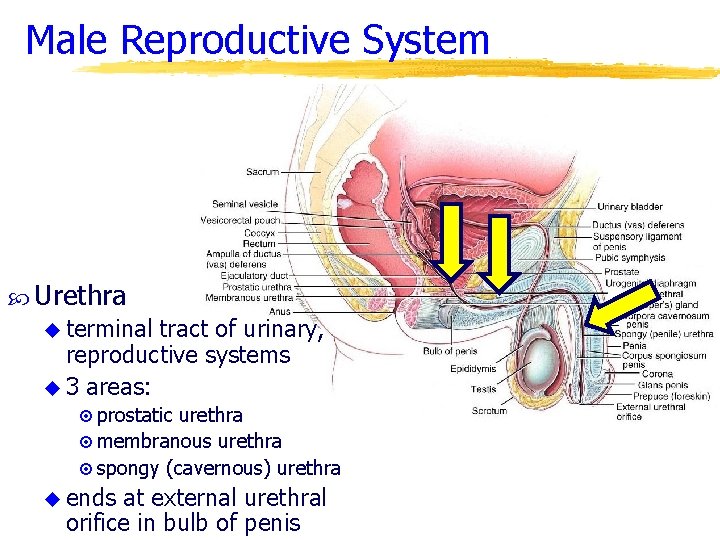
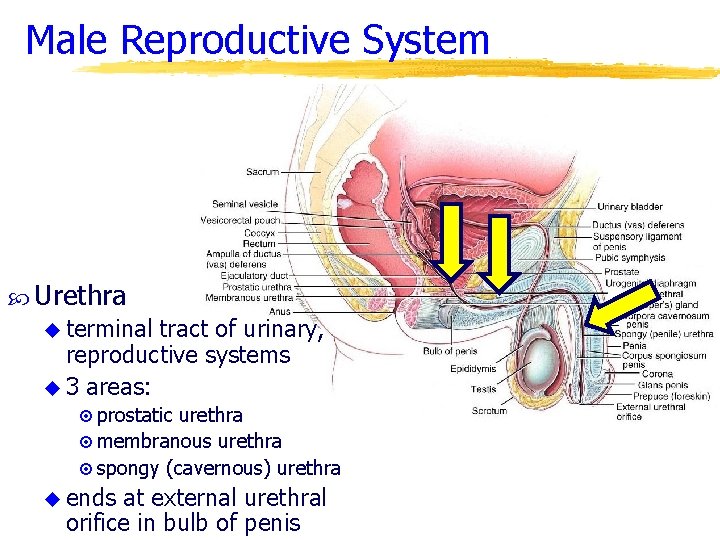
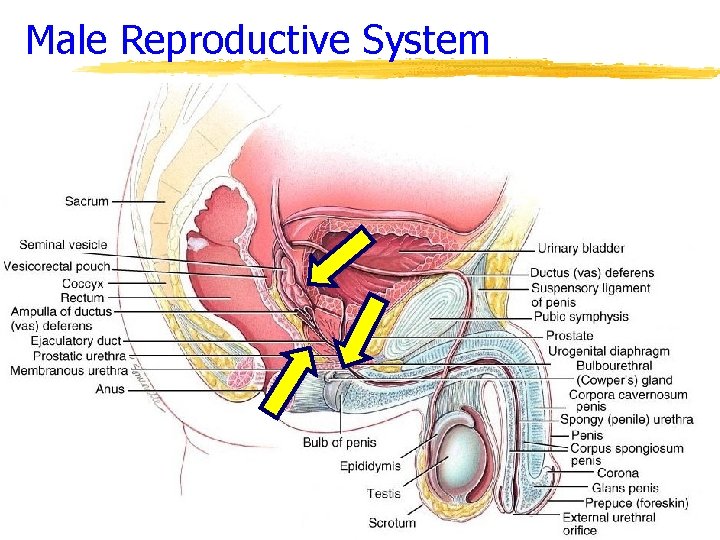
Male Reproductive System Urethra u terminal tract of urinary, reproductive systems u 3 areas: ¤ prostatic urethra ¤ membranous urethra ¤ spongy (cavernous) urethra u ends at external urethral orifice in bulb of penis
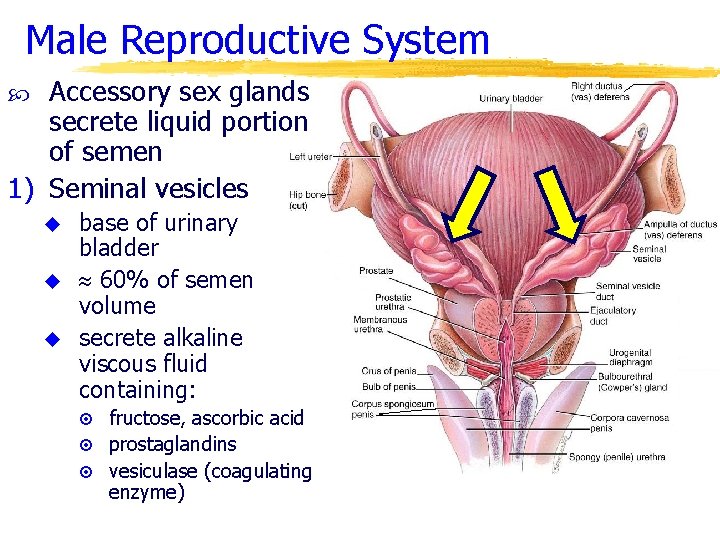
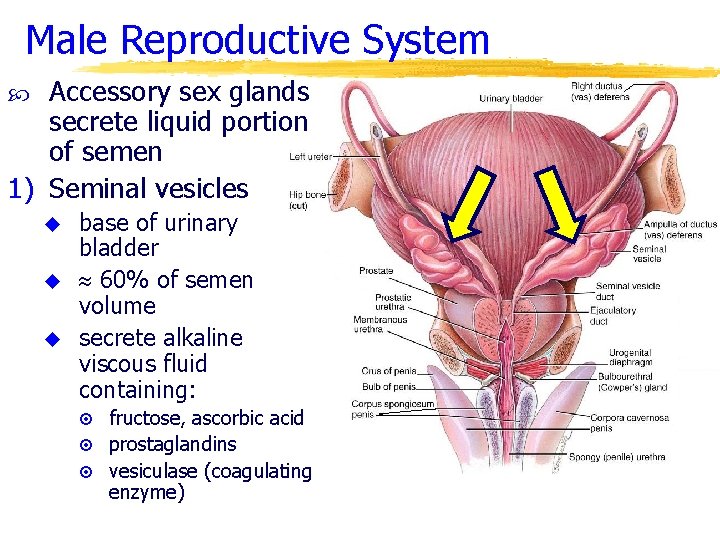
Male Reproductive System Accessory sex glands secrete liquid portion of semen 1) Seminal vesicles u u u base of urinary bladder 60% of semen volume secrete alkaline viscous fluid containing: ¤ fructose, ascorbic acid ¤ prostaglandins ¤ vesiculase (coagulating enzyme)
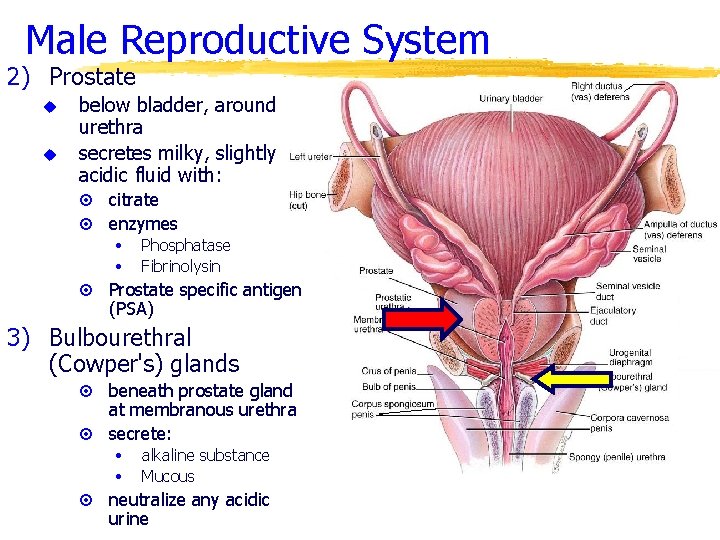
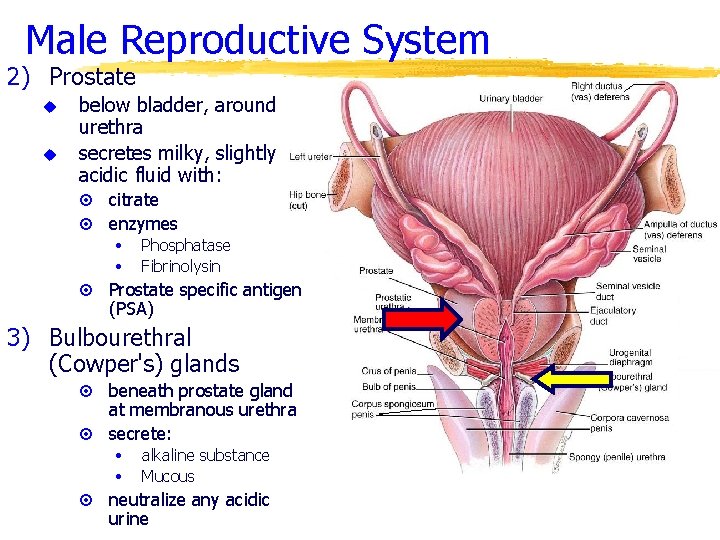
Male Reproductive System 2) Prostate u u below bladder, around urethra secretes milky, slightly acidic fluid with: citrate ¤ enzymes ¤ • • ¤ Phosphatase Fibrinolysin Prostate specific antigen (PSA) 3) Bulbourethral (Cowper's) glands beneath prostate gland at membranous urethra ¤ secrete: ¤ • • ¤ alkaline substance Mucous neutralize any acidic urine
Male Reproductive System
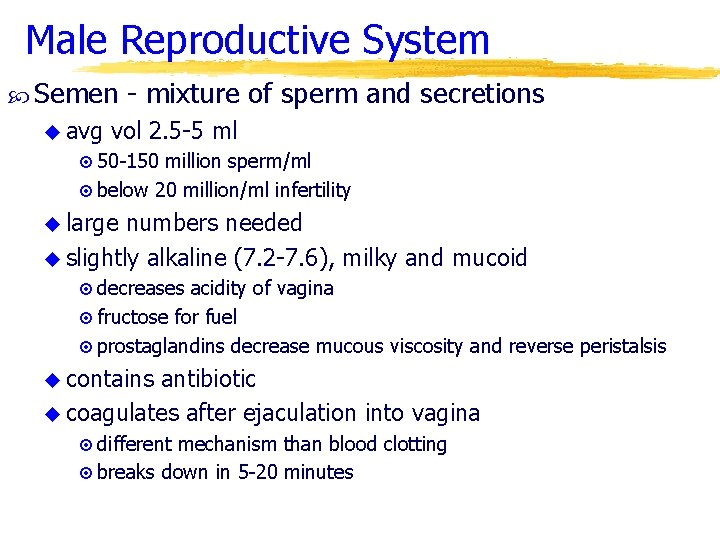
Male Reproductive System Semen u avg - mixture of sperm and secretions vol 2. 5 -5 ml ¤ 50 -150 million sperm/ml ¤ below 20 million/ml infertility u large numbers needed u slightly alkaline (7. 2 -7. 6), milky and mucoid ¤ decreases acidity of vagina ¤ fructose for fuel ¤ prostaglandins decrease mucous viscosity and reverse peristalsis u contains antibiotic u coagulates after ejaculation into vagina ¤ different mechanism than blood clotting ¤ breaks down in 5 -20 minutes
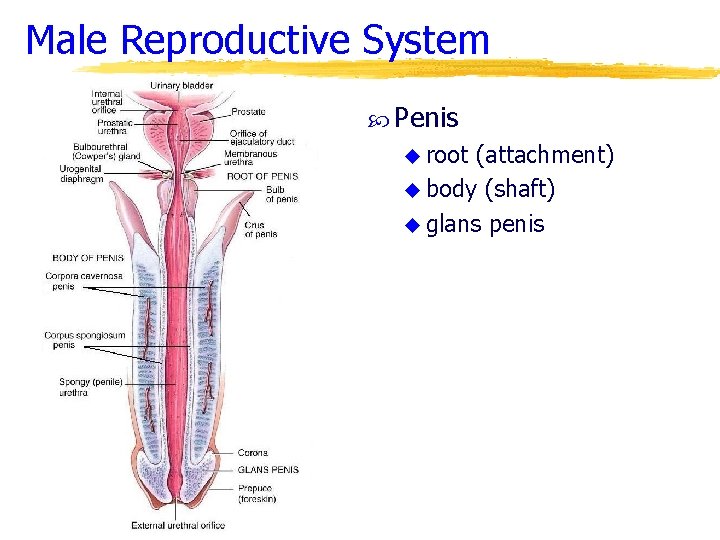
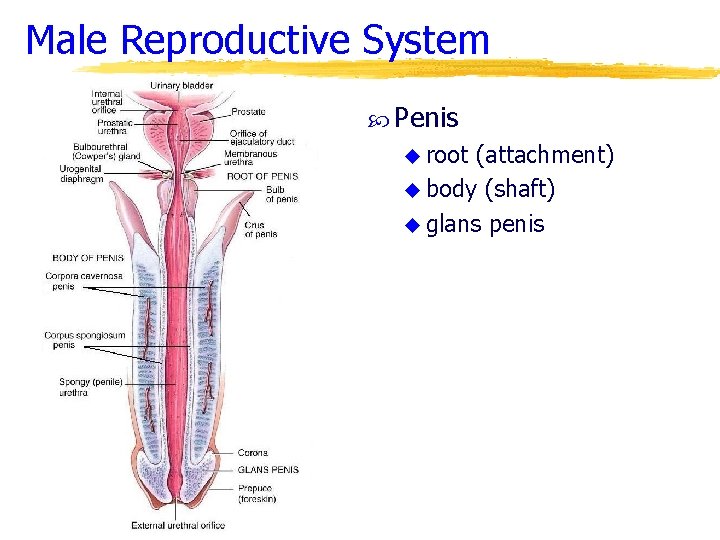
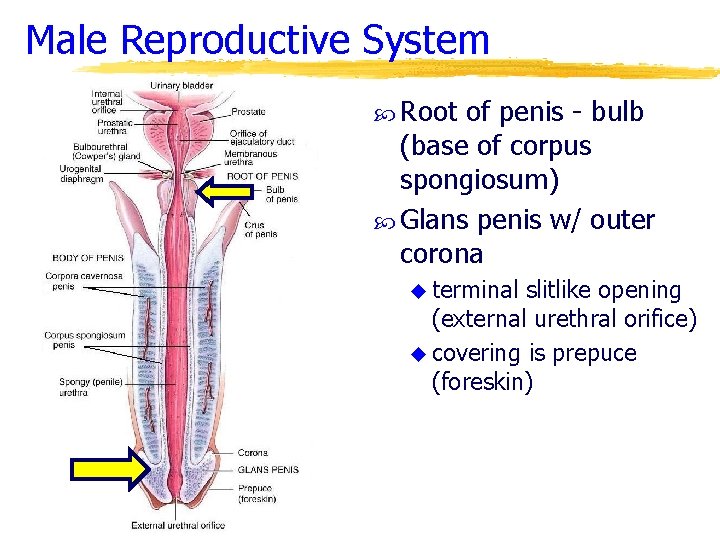
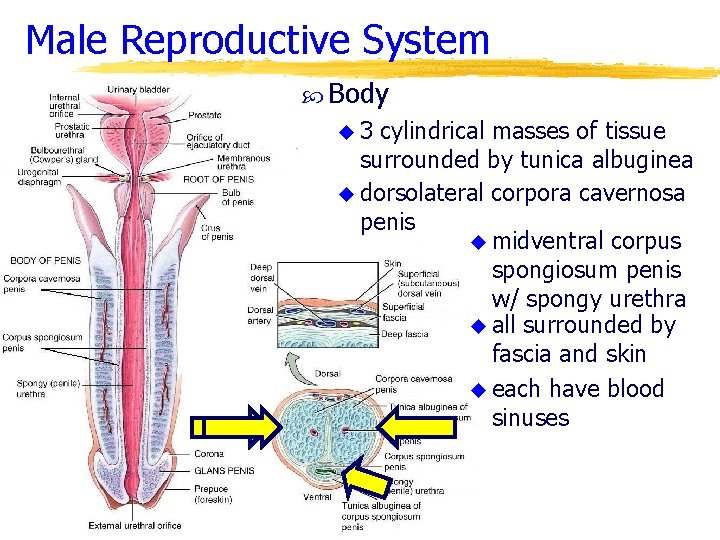
Male Reproductive System Penis u root (attachment) u body (shaft) u glans penis
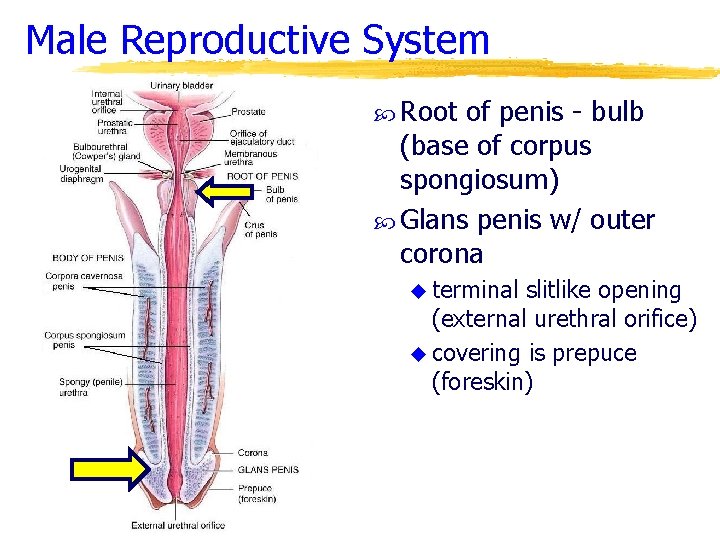
Male Reproductive System Root of penis - bulb (base of corpus spongiosum) Glans penis w/ outer corona u terminal slitlike opening (external urethral orifice) u covering is prepuce (foreskin)
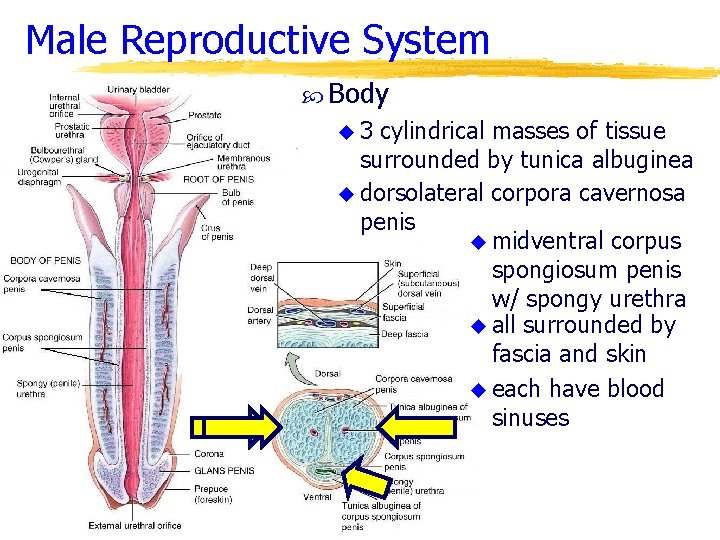
Male Reproductive System Body u 3 cylindrical masses of tissue surrounded by tunica albuginea u dorsolateral corpora cavernosa penis u midventral corpus spongiosum penis w/ spongy urethra u all surrounded by fascia and skin u each have blood sinuses
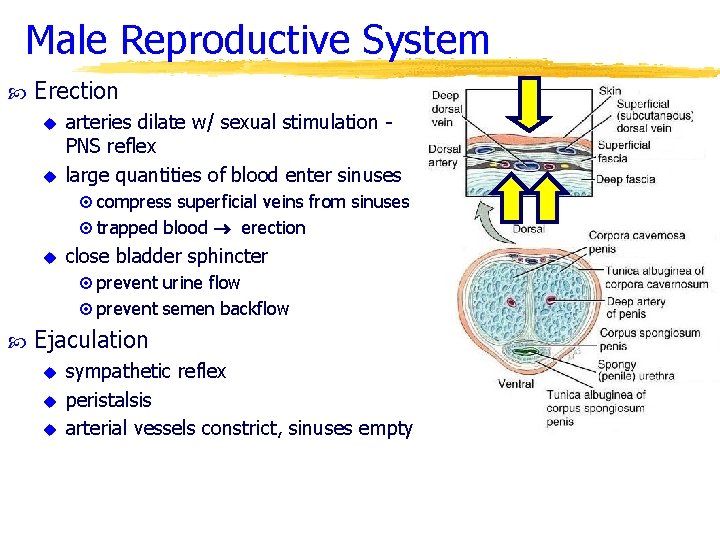
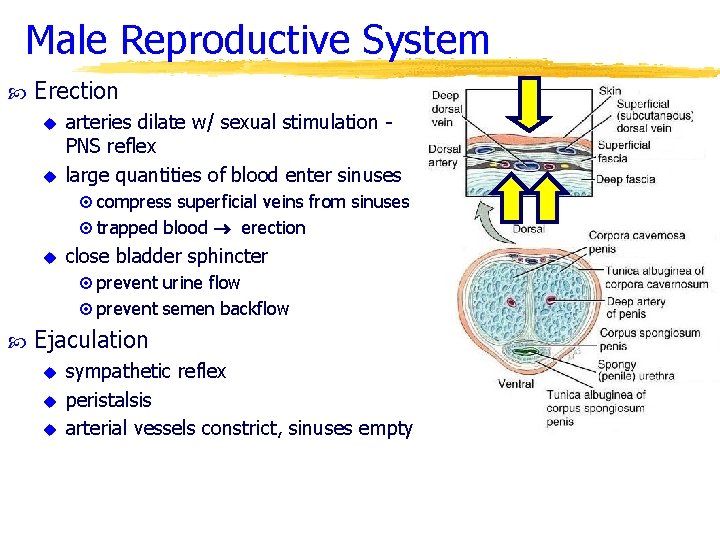
Male Reproductive System Erection u u arteries dilate w/ sexual stimulation PNS reflex large quantities of blood enter sinuses ¤ compress superficial veins from sinuses ¤ trapped blood erection u close bladder sphincter ¤ prevent urine flow ¤ prevent semen backflow Ejaculation u u u sympathetic reflex peristalsis arterial vessels constrict, sinuses empty
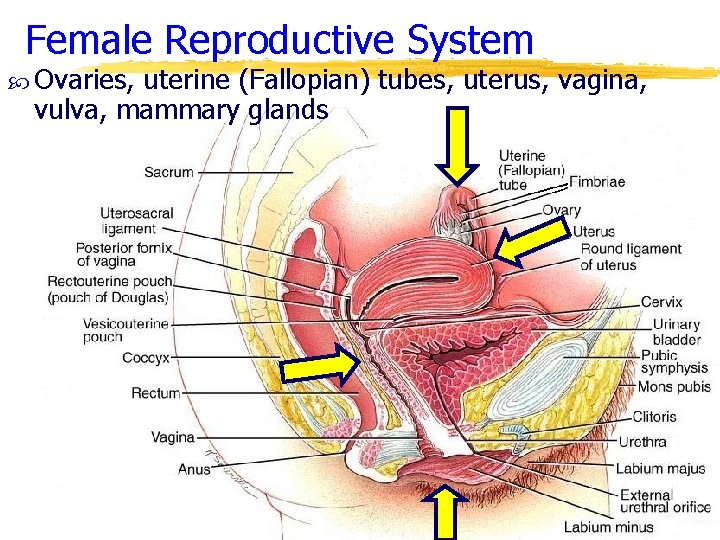
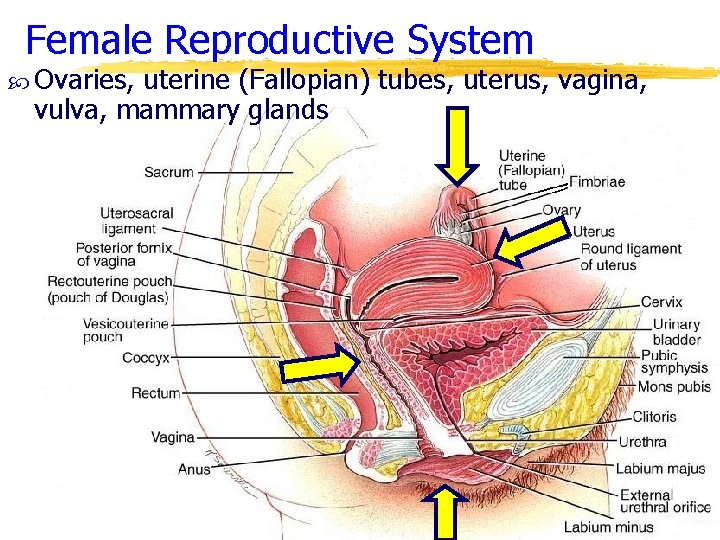
Female Reproductive System Ovaries, uterine (Fallopian) tubes, uterus, vagina, vulva, mammary glands
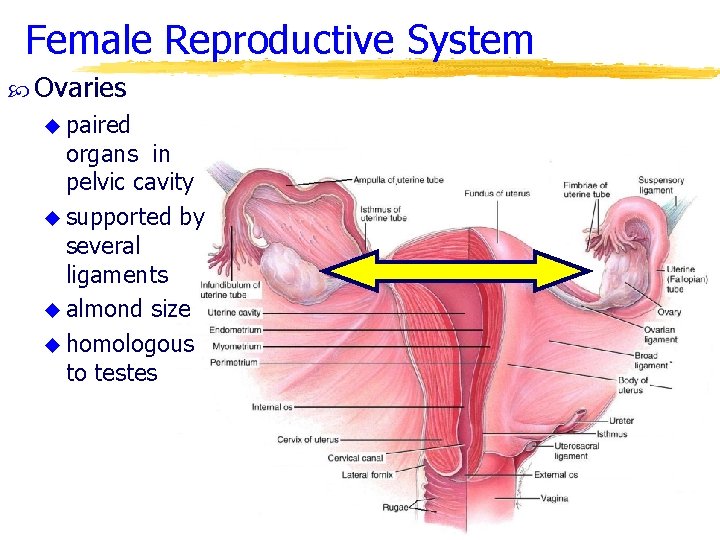
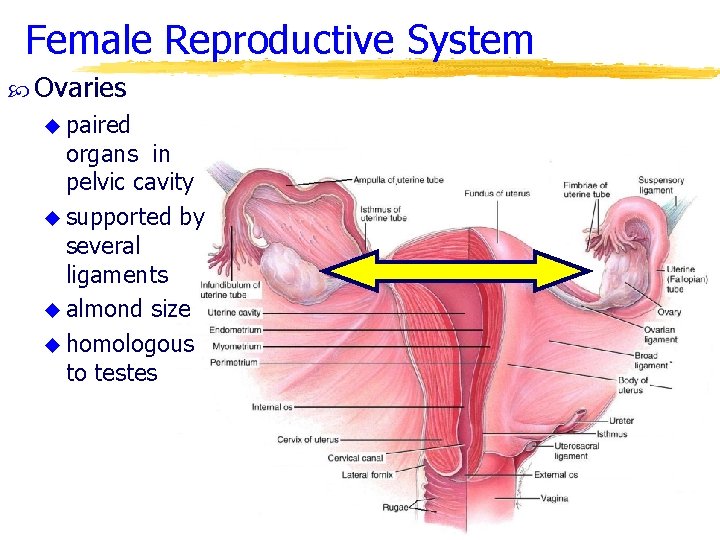
Female Reproductive System Ovaries u paired organs in pelvic cavity u supported by several ligaments u almond size u homologous to testes
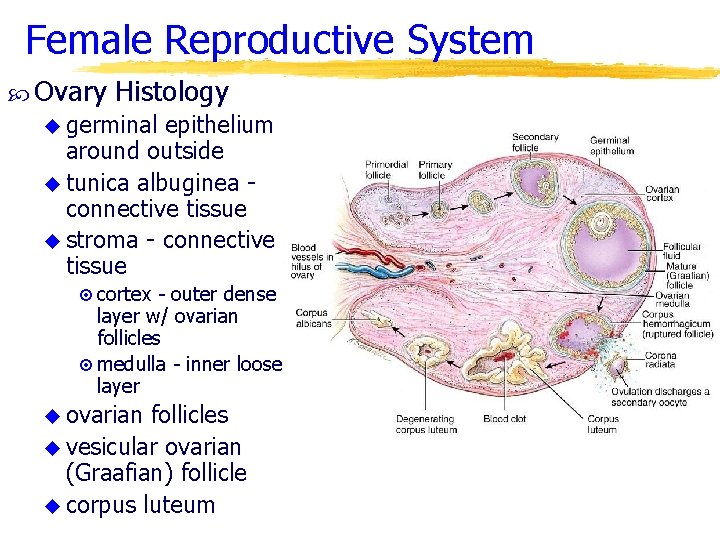
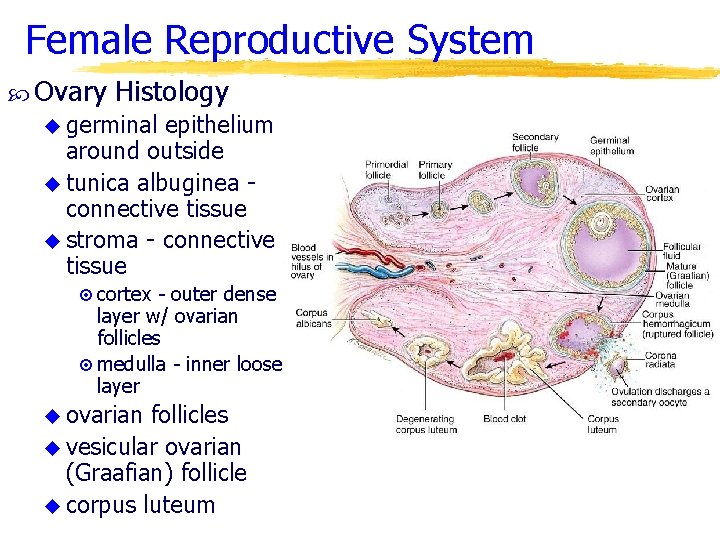
Female Reproductive System Ovary Histology u germinal epithelium around outside u tunica albuginea connective tissue u stroma - connective tissue ¤ cortex - outer dense layer w/ ovarian follicles ¤ medulla - inner loose layer u ovarian follicles u vesicular ovarian (Graafian) follicle u corpus luteum
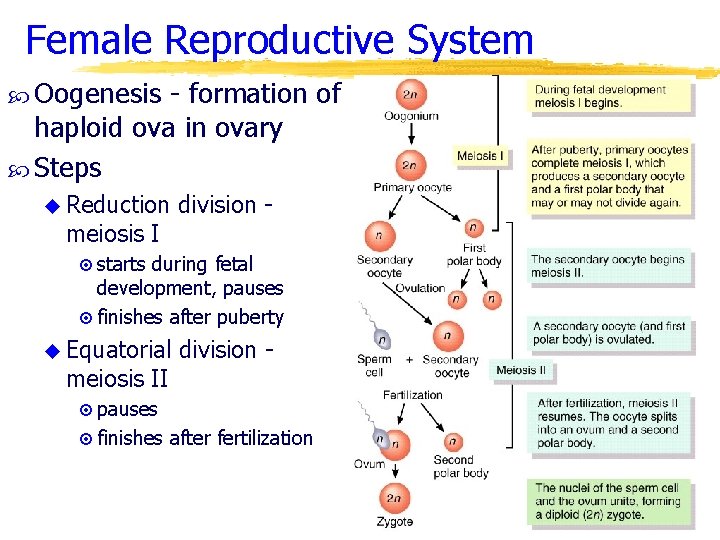
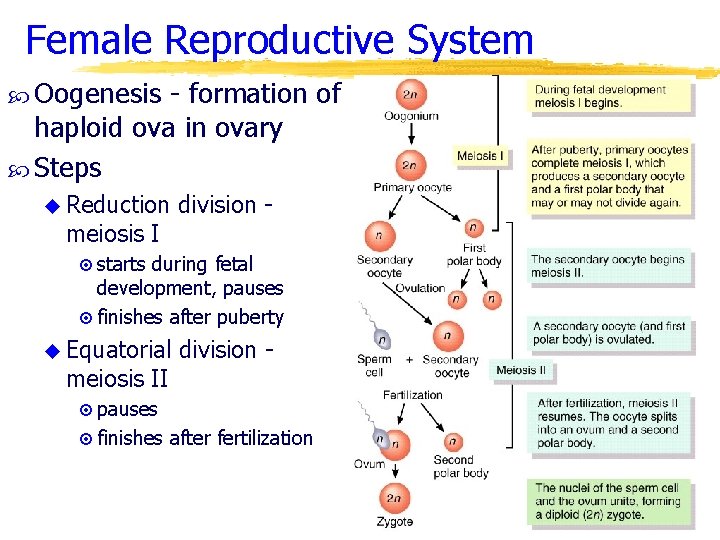
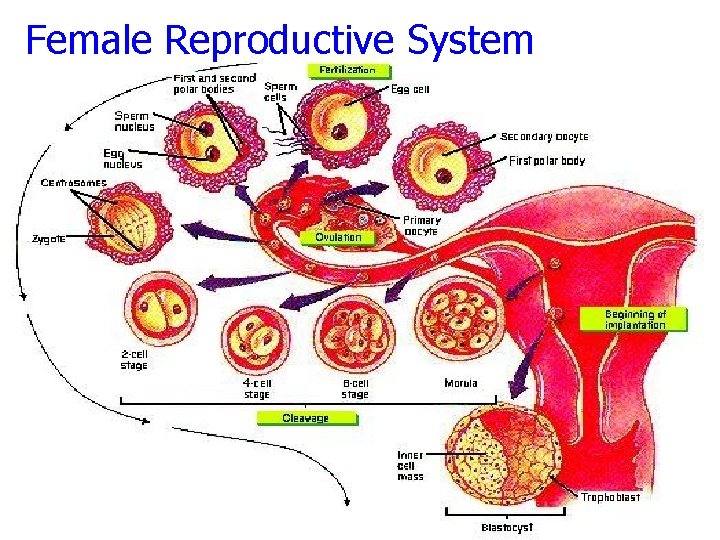
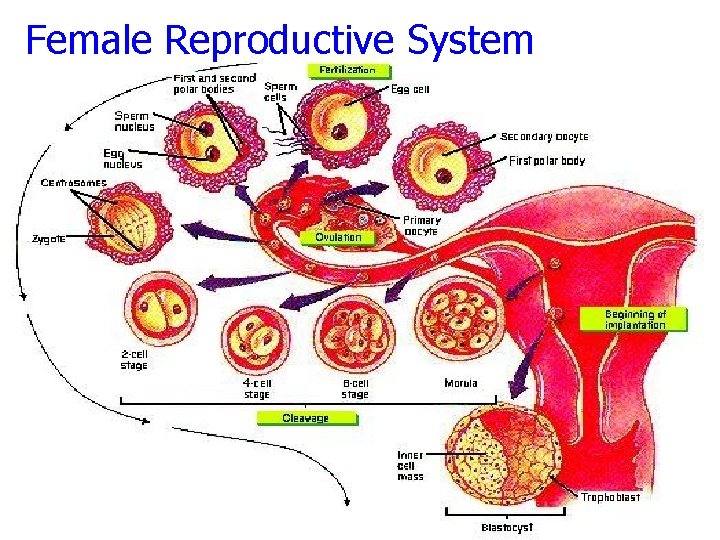
Female Reproductive System Oogenesis - formation of haploid ova in ovary Steps u Reduction meiosis I division - ¤ starts during fetal development, pauses ¤ finishes after puberty u Equatorial meiosis II division - ¤ pauses ¤ finishes after fertilization
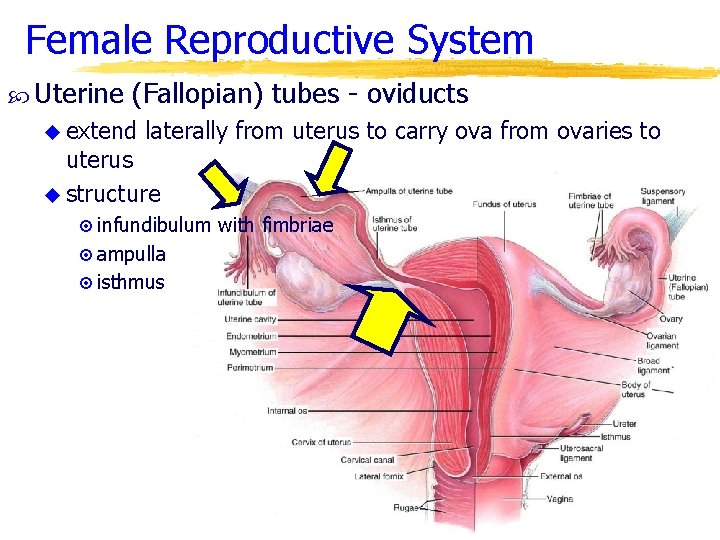
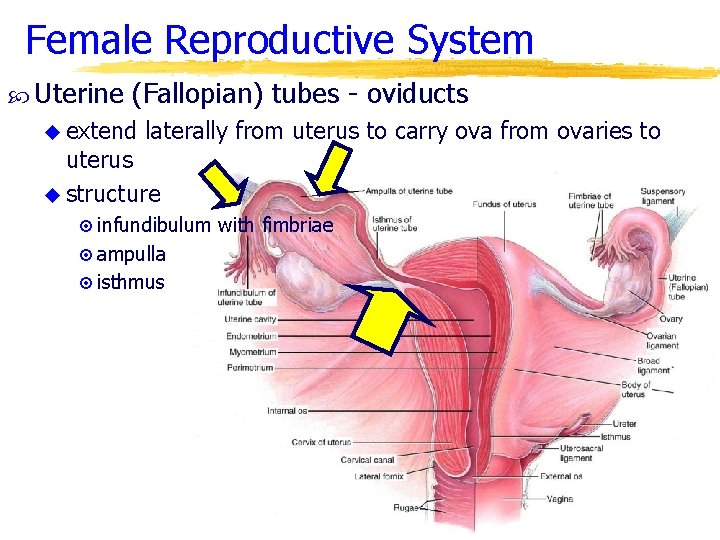
Female Reproductive System Uterine (Fallopian) tubes - oviducts u extend laterally from uterus to carry ova from ovaries to uterus u structure ¤ infundibulum with fimbriae ¤ ampulla ¤ isthmus
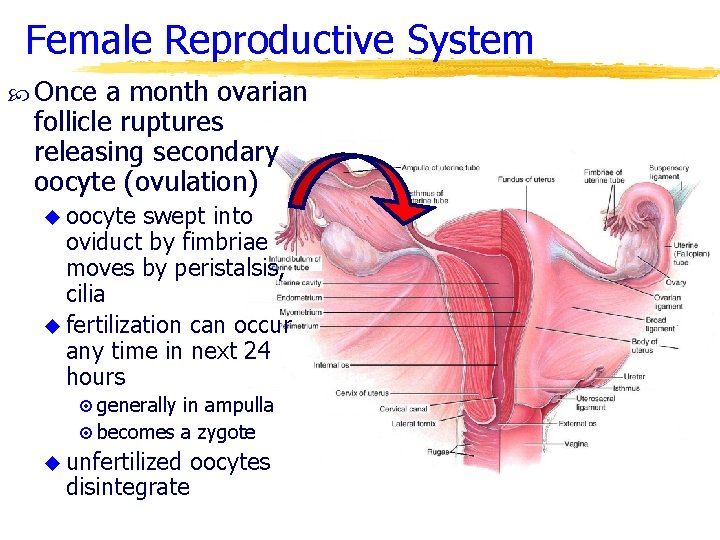
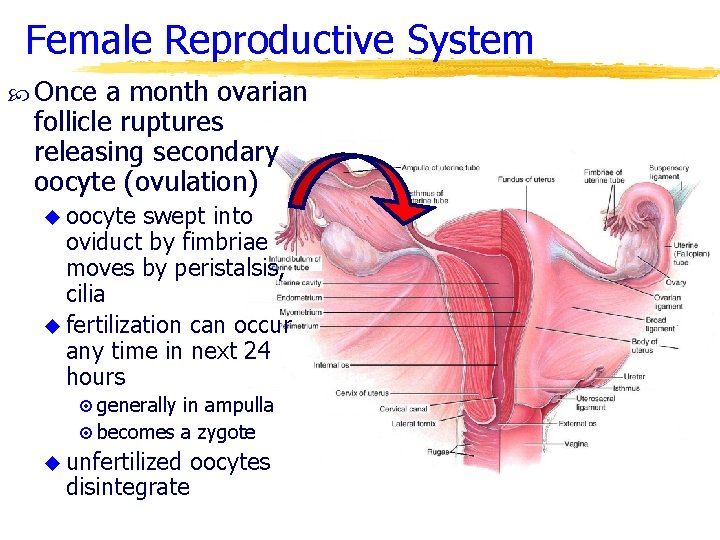
Female Reproductive System Once a month ovarian follicle ruptures releasing secondary oocyte (ovulation) u oocyte swept into oviduct by fimbriae moves by peristalsis, cilia u fertilization can occur any time in next 24 hours ¤ generally in ampulla ¤ becomes a zygote u unfertilized disintegrate oocytes
Female Reproductive System
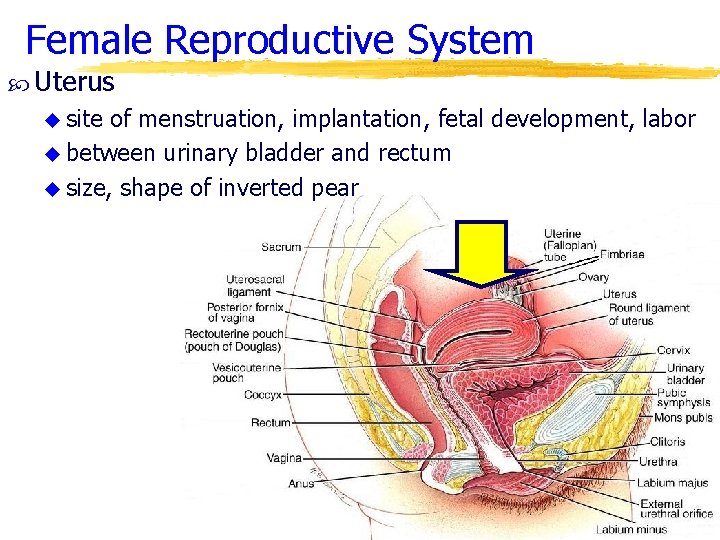
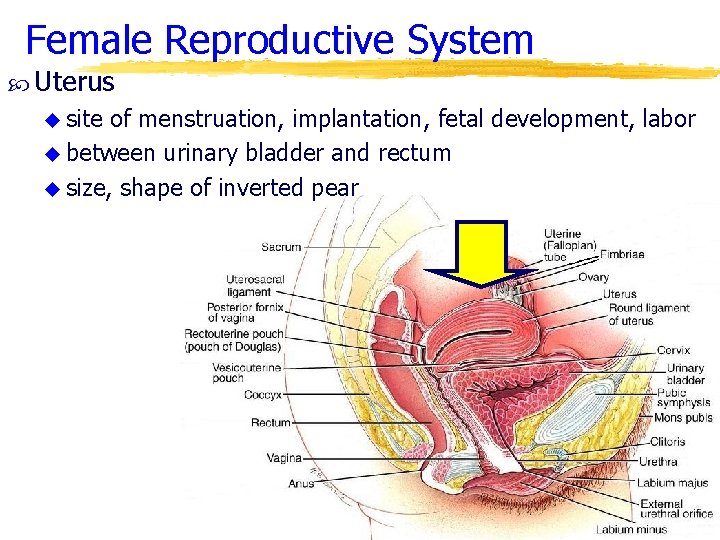
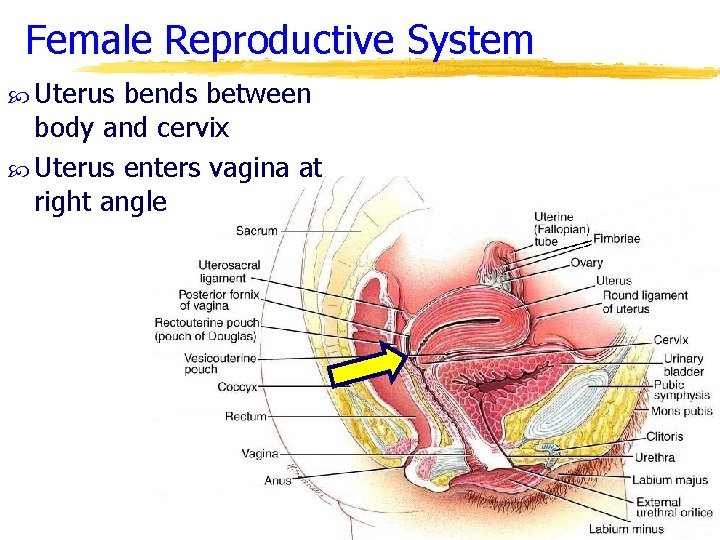
Female Reproductive System Uterus u site of menstruation, implantation, fetal development, labor u between urinary bladder and rectum u size, shape of inverted pear
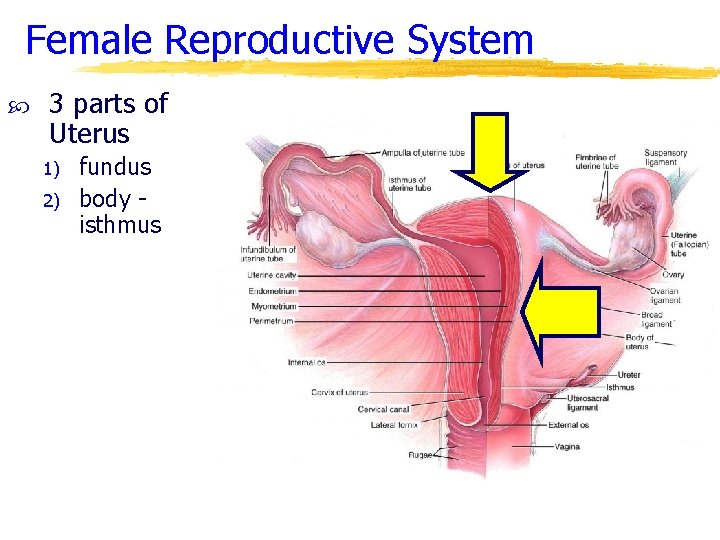
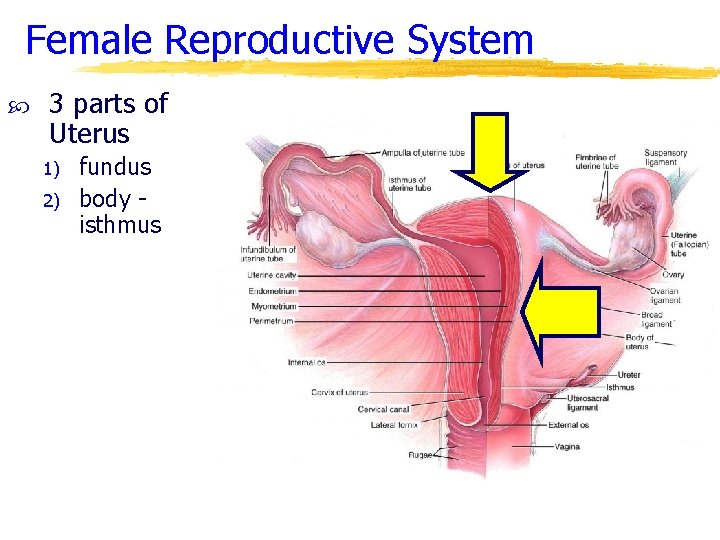
Female Reproductive System 3 parts of Uterus 1) 2) fundus body isthmus
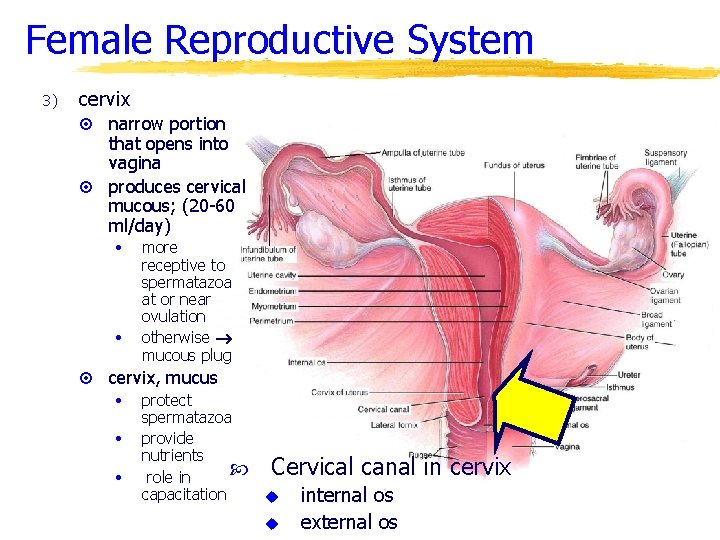
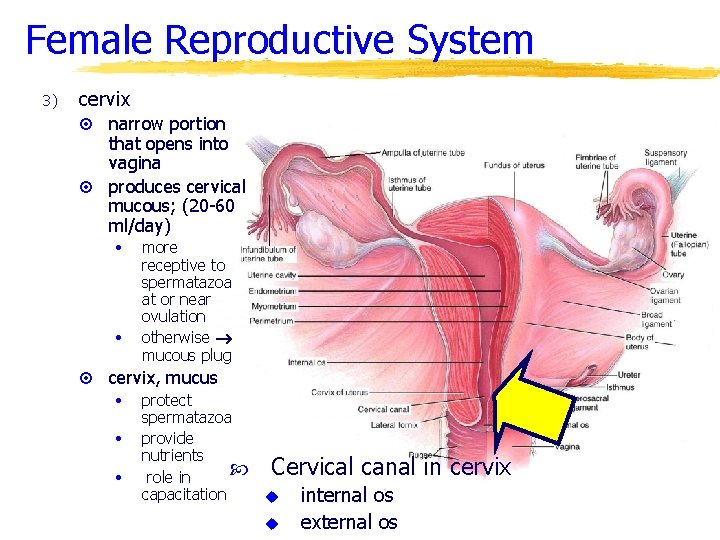
Female Reproductive System 3) cervix narrow portion that opens into vagina ¤ produces cervical mucous; (20 -60 ml/day) ¤ • • ¤ more receptive to spermatazoa at or near ovulation otherwise mucous plug cervix, mucus • • • protect spermatazoa provide nutrients role in capacitation Cervical canal in cervix u u internal os external os
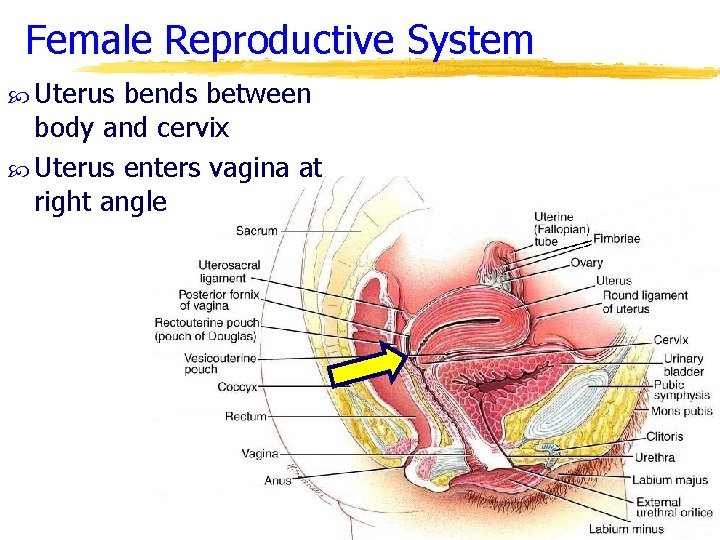
Female Reproductive System Uterus bends between body and cervix Uterus enters vagina at right angle
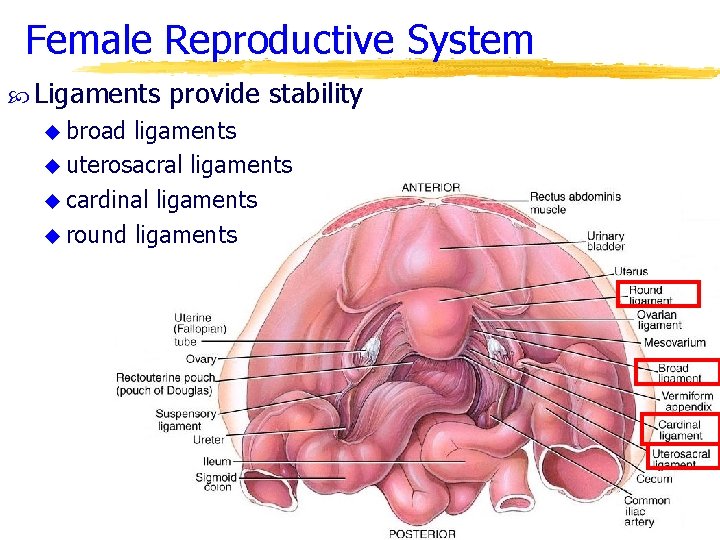
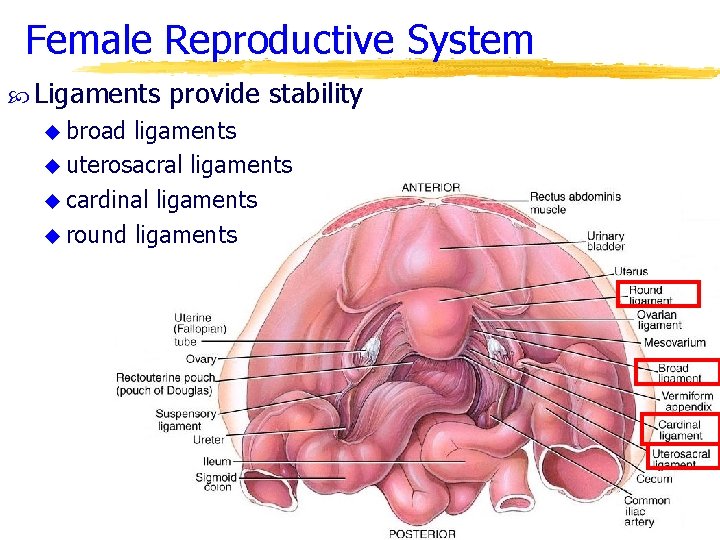
Female Reproductive System Ligaments u broad provide stability ligaments u uterosacral ligaments u cardinal ligaments u round ligaments
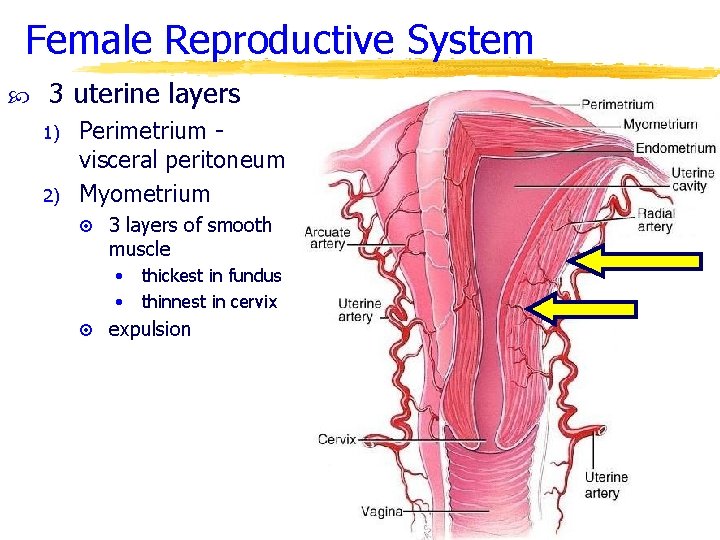
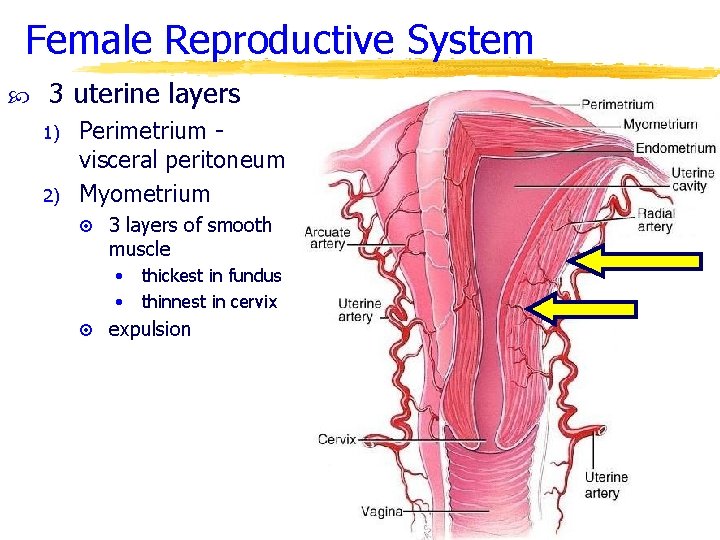
Female Reproductive System 3 uterine layers 1) 2) Perimetrium visceral peritoneum Myometrium ¤ 3 layers of smooth muscle • • thickest in fundus thinnest in cervix ¤ expulsion
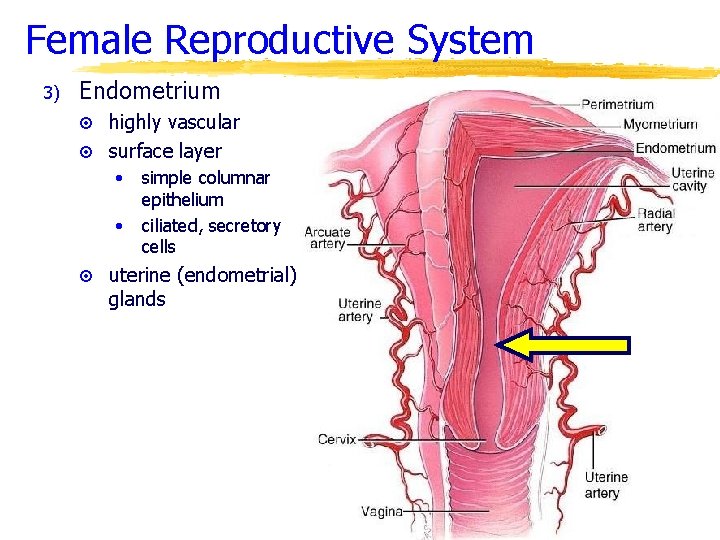
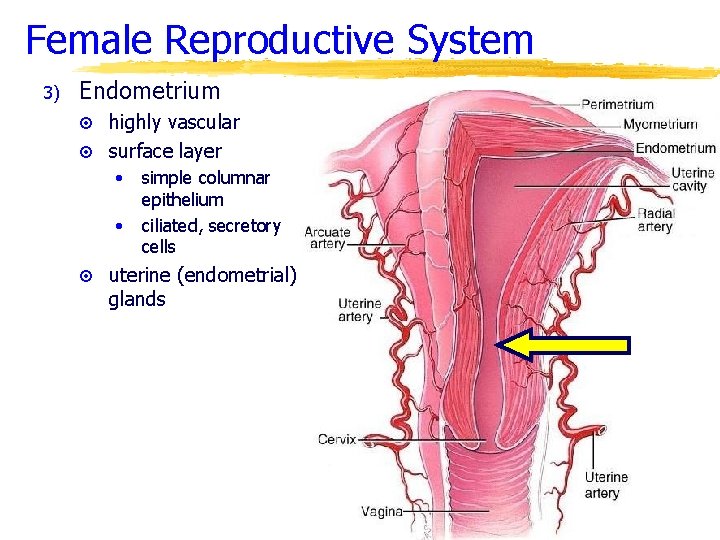
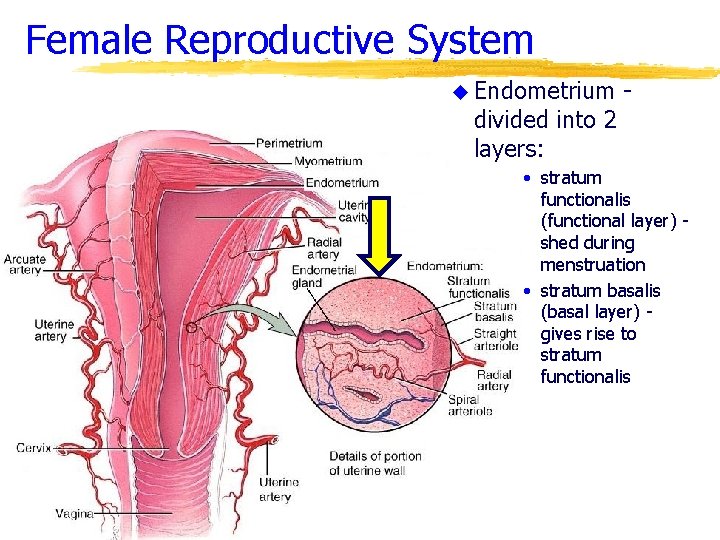
Female Reproductive System 3) Endometrium ¤ highly vascular ¤ surface layer • • simple columnar epithelium ciliated, secretory cells ¤ uterine (endometrial) glands
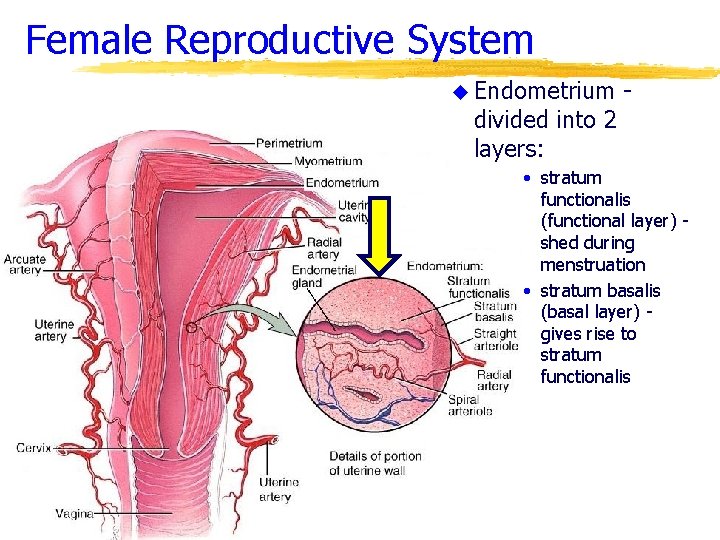
Female Reproductive System u Endometrium divided into 2 layers: - • stratum functionalis (functional layer) shed during menstruation • stratum basalis (basal layer) gives rise to stratum functionalis
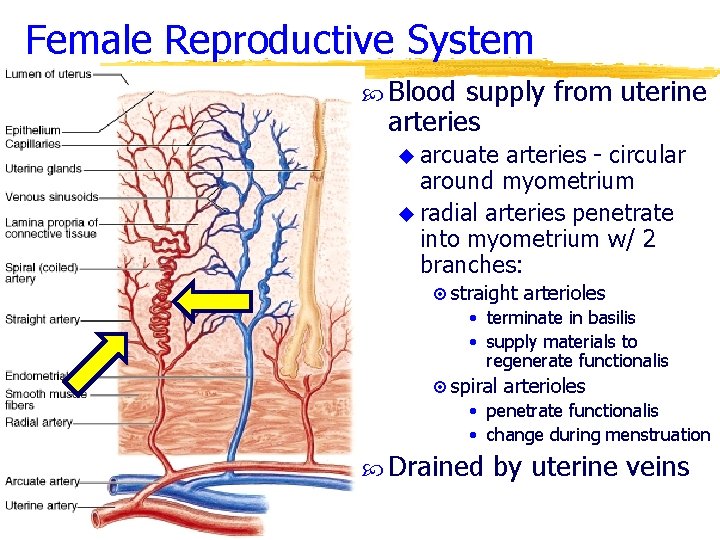
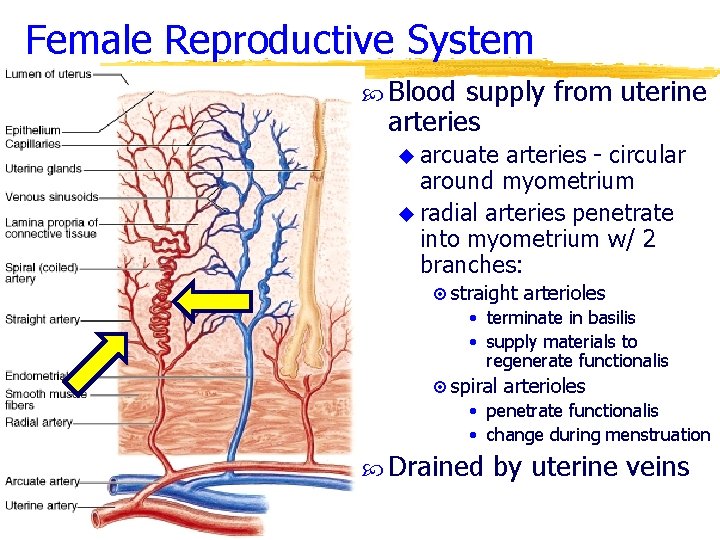
Female Reproductive System Blood supply from uterine arteries u arcuate arteries - circular around myometrium u radial arteries penetrate into myometrium w/ 2 branches: ¤ straight arterioles • terminate in basilis • supply materials to regenerate functionalis ¤ spiral arterioles • penetrate functionalis • change during menstruation Drained by uterine veins
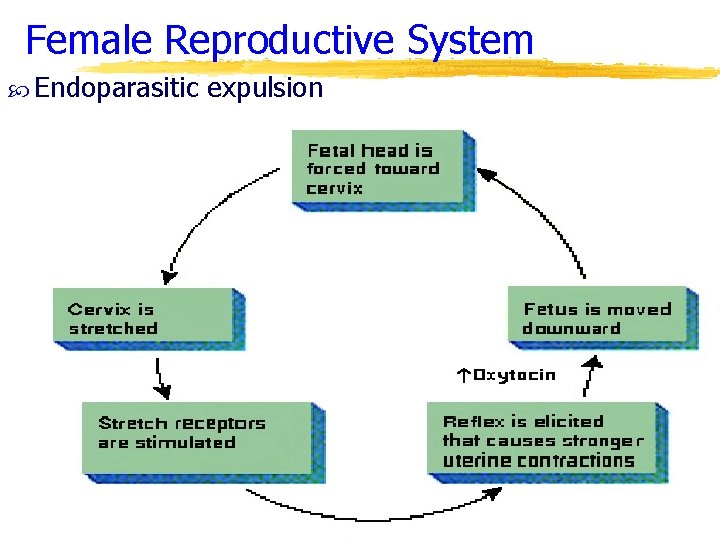
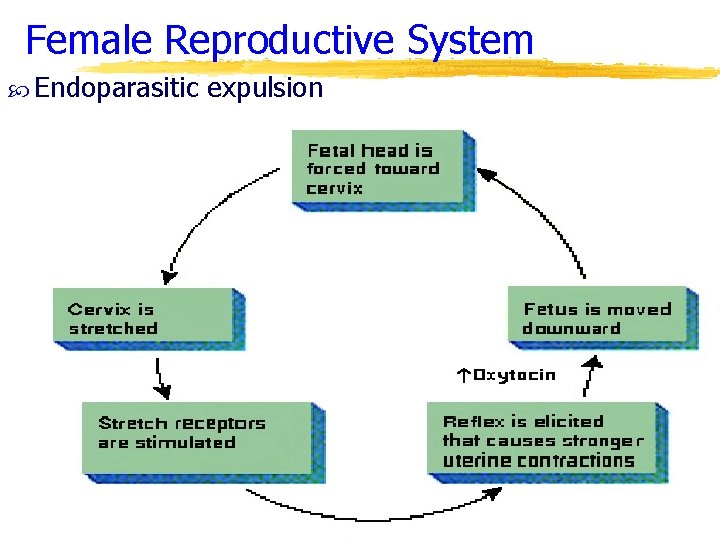
Female Reproductive System Endoparasitic expulsion
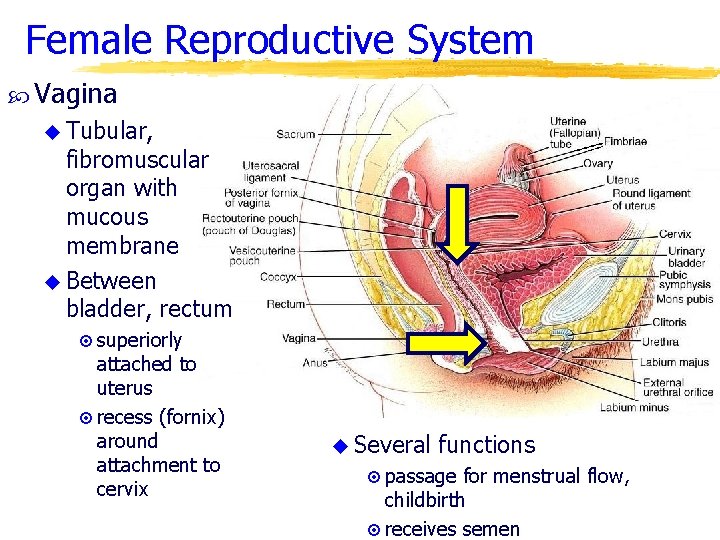
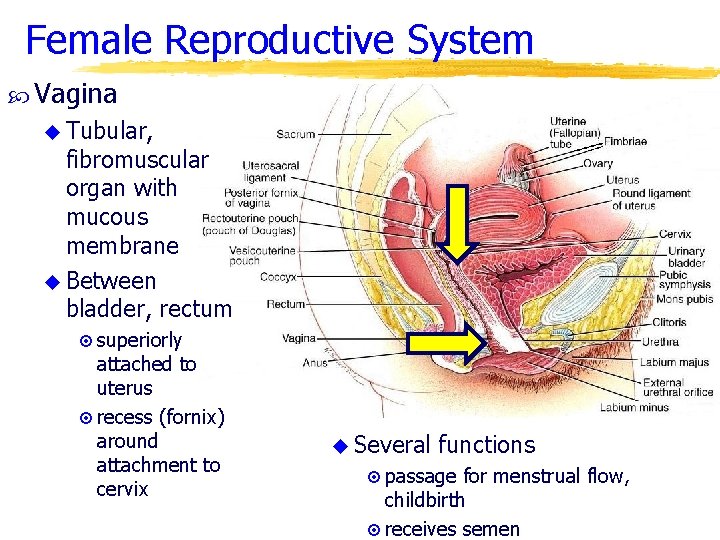
Female Reproductive System Vagina u Tubular, fibromuscular organ with mucous membrane u Between bladder, rectum ¤ superiorly attached to uterus ¤ recess (fornix) around attachment to cervix u Several functions ¤ passage for menstrual flow, childbirth ¤ receives semen
Female Reproductive System Vagina histology u Mucosa continuous w/ uterus ¤non-keratinized stratified squamous epithelium and connective tissue in folds (rugae) • mucosal cells have large stores of glycogen • upon decomposition produce organic acids - lo p. H ¤dendritic (APC) cells - AIDS? u Muscularis ¤smooth muscle - outer circular, inner longitudinal ¤stretches to receive penis and for childbirth u Adventitia - areolar connective tissue
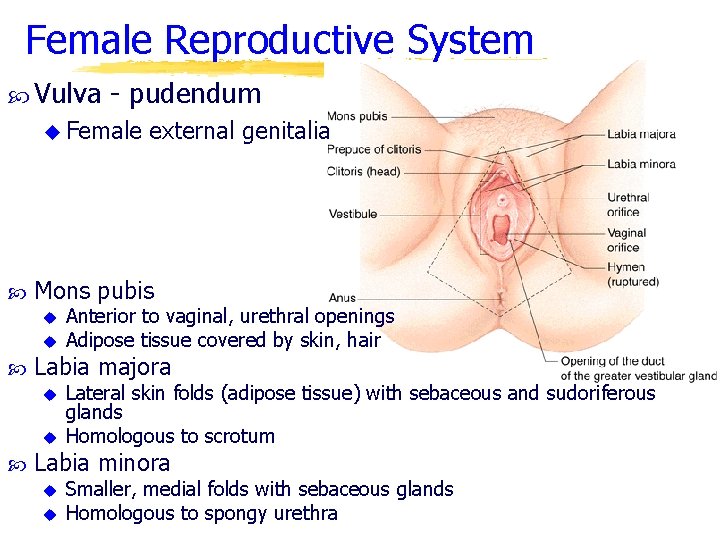
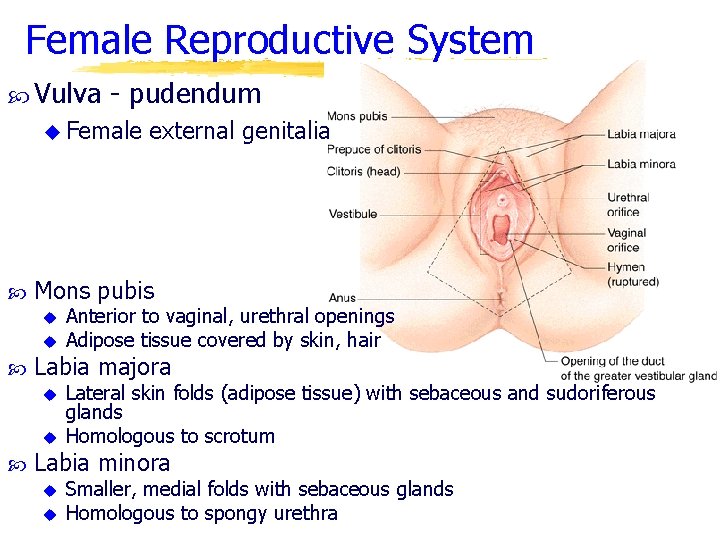
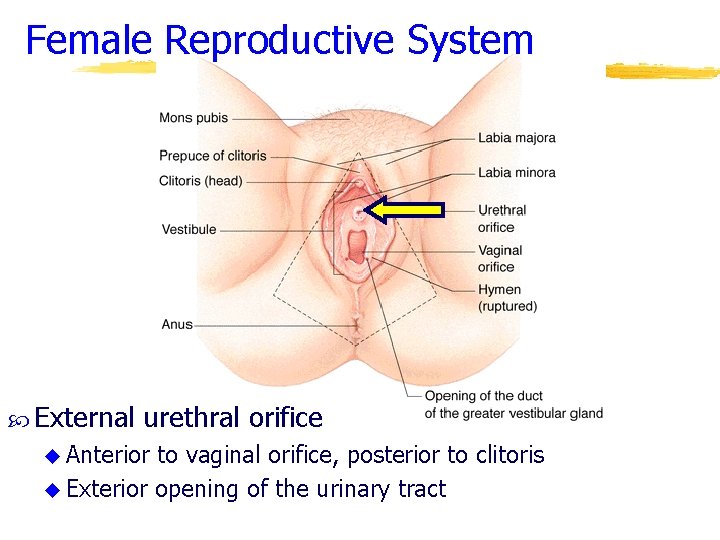
Female Reproductive System Vulva - pudendum u Female Mons pubis u Anterior to vaginal, urethral openings this is a test u Adipose tissue covered by skin, hair Labia majora u u external genitalia Lateral skin folds (adipose tissue) with sebaceous and sudoriferous glands Homologous to scrotum Labia minora u u Smaller, medial folds with sebaceous glands Homologous to spongy urethra
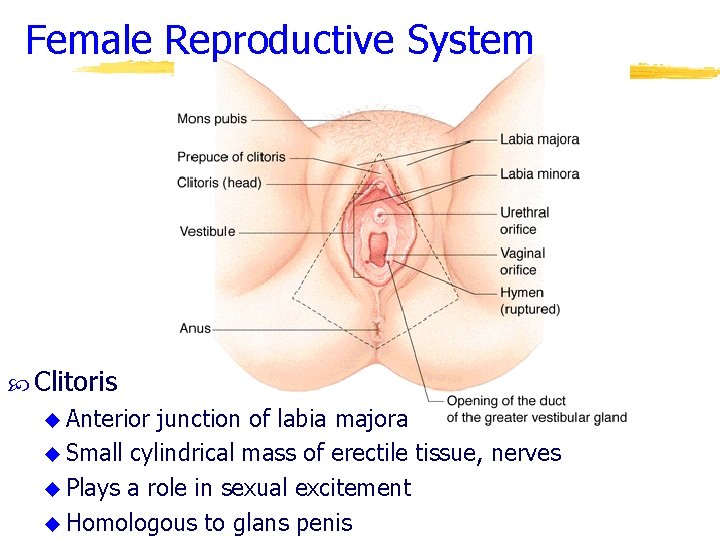
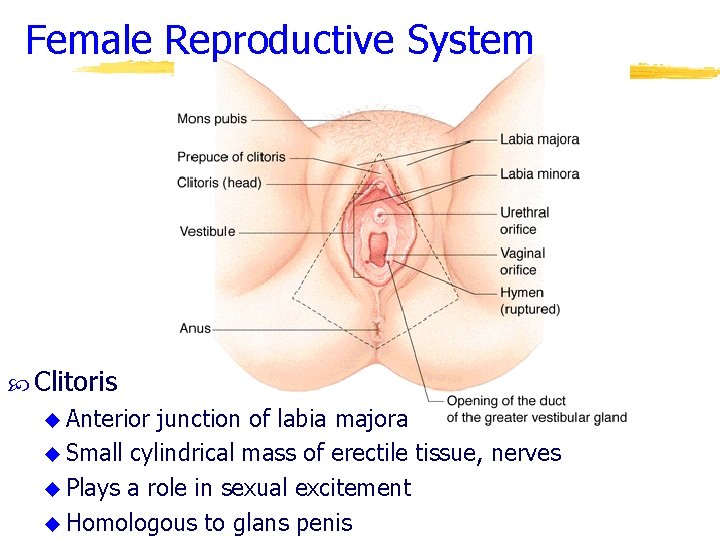
Female Reproductive System Clitoris u Anterior junction of labia majora u Small cylindrical mass of erectile tissue, nerves u Plays a role in sexual excitement u Homologous to glans penis
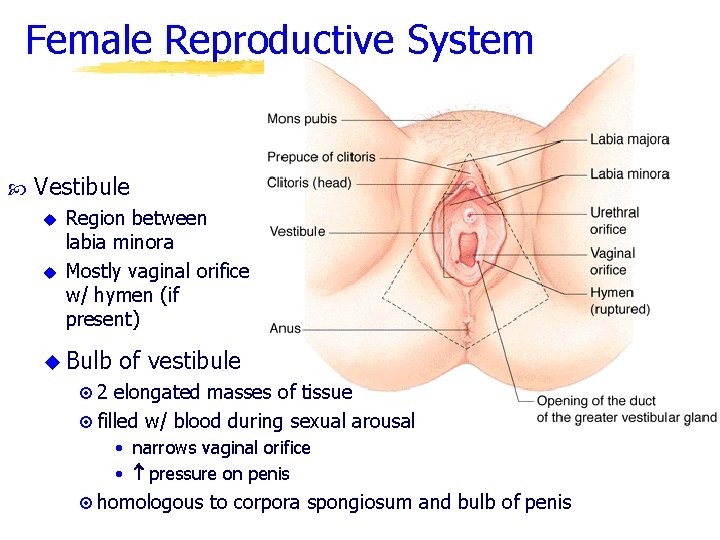
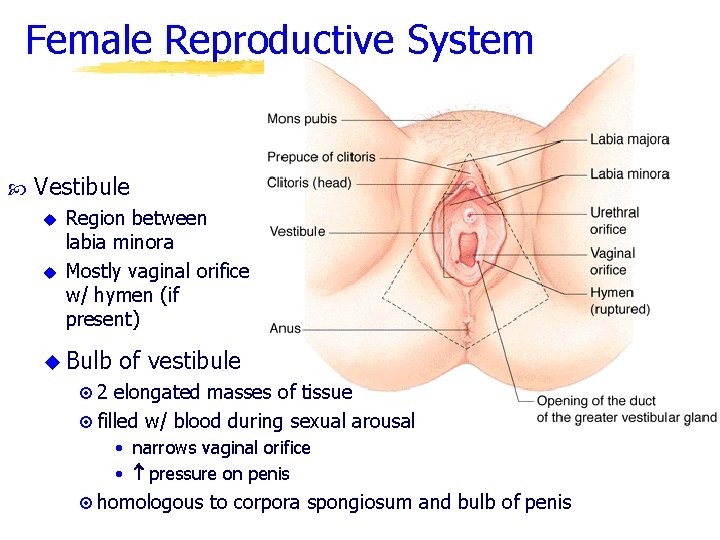
Female Reproductive System Vestibule u u Region between labia minora Mostly vaginal orifice w/ hymen (if present) u Bulb of vestibule ¤ 2 elongated masses of tissue ¤ filled w/ blood during sexual arousal • narrows vaginal orifice • pressure on penis ¤ homologous to corpora spongiosum and bulb of penis
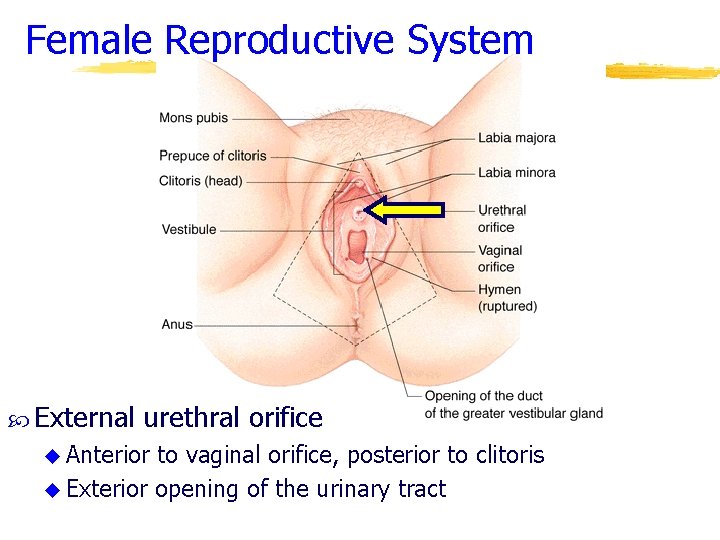
Female Reproductive System External urethral orifice u Anterior to vaginal orifice, posterior to clitoris u Exterior opening of the urinary tract
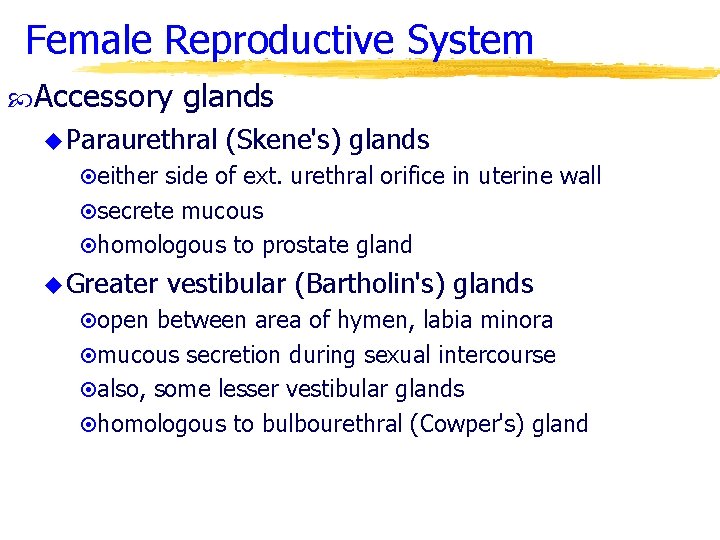
Female Reproductive System Accessory glands u Paraurethral (Skene's) glands ¤either side of ext. urethral orifice in uterine wall ¤secrete mucous ¤homologous to prostate gland u Greater vestibular (Bartholin's) glands ¤open between area of hymen, labia minora ¤mucous secretion during sexual intercourse ¤also, some lesser vestibular glands ¤homologous to bulbourethral (Cowper's) gland
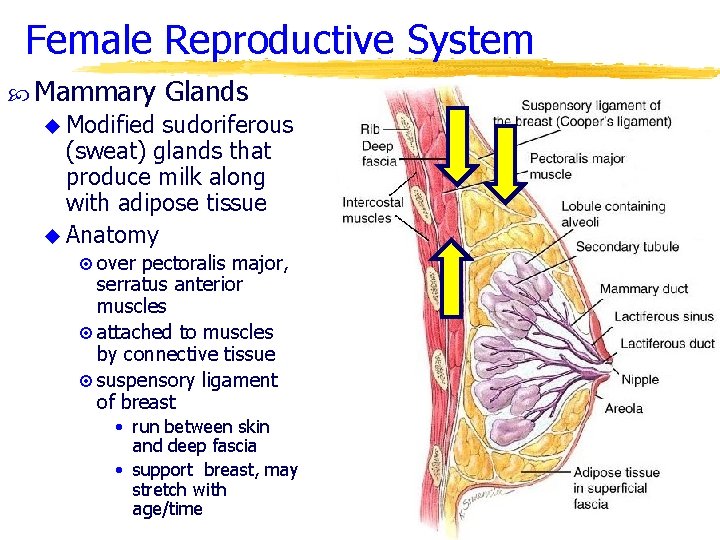
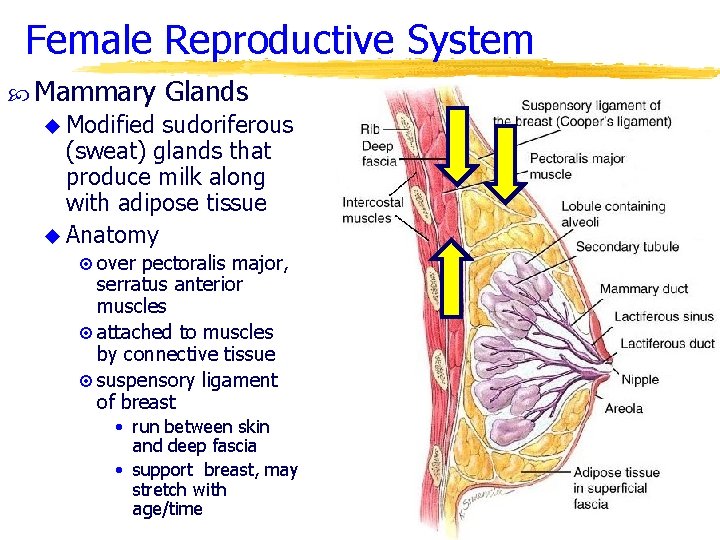
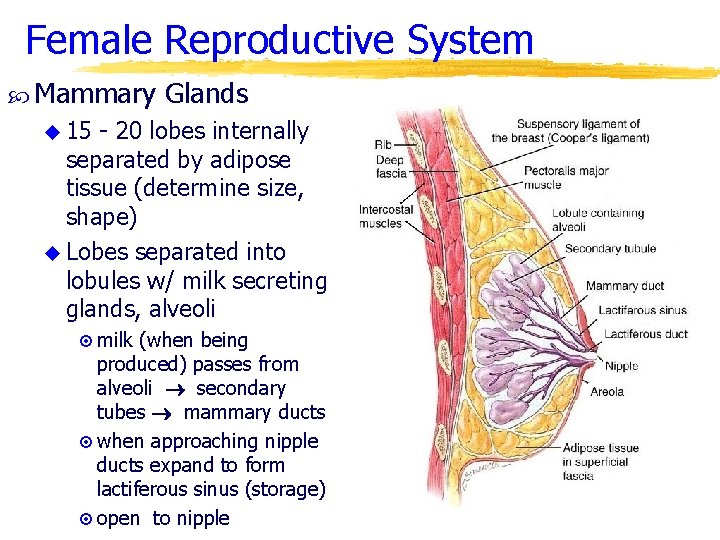
Female Reproductive System Mammary Glands u Modified sudoriferous (sweat) glands that produce milk along with adipose tissue u Anatomy ¤ over pectoralis major, serratus anterior muscles ¤ attached to muscles by connective tissue ¤ suspensory ligament of breast • run between skin and deep fascia • support breast, may stretch with age/time
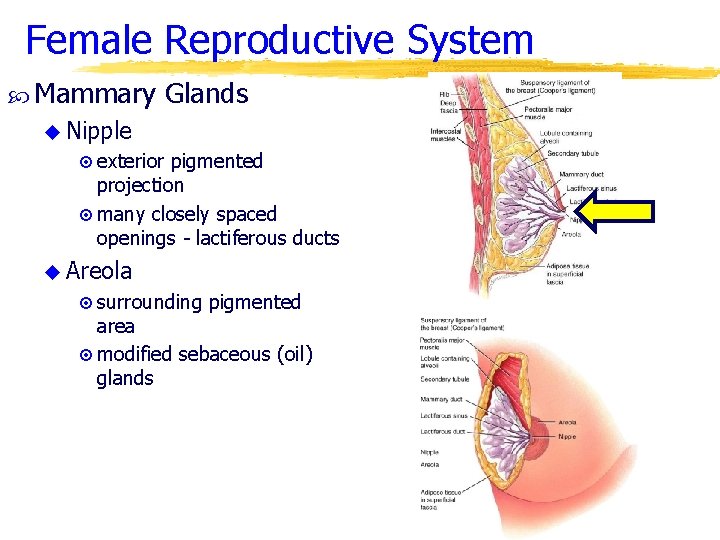
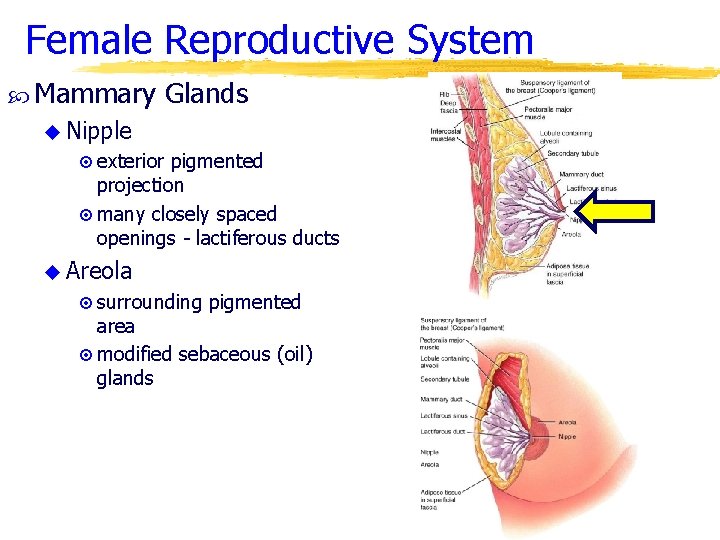
Female Reproductive System Mammary Glands u Nipple ¤ exterior pigmented projection ¤ many closely spaced openings - lactiferous ducts u Areola ¤ surrounding pigmented area ¤ modified sebaceous (oil) glands
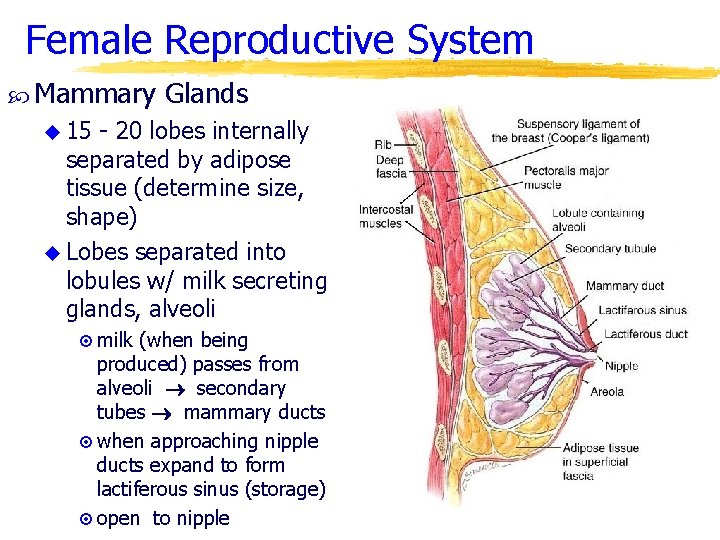
Female Reproductive System Mammary Glands u 15 - 20 lobes internally separated by adipose tissue (determine size, shape) u Lobes separated into lobules w/ milk secreting glands, alveoli ¤ milk (when being produced) passes from alveoli secondary tubes mammary ducts ¤ when approaching nipple ducts expand to form lactiferous sinus (storage) ¤ open to nipple
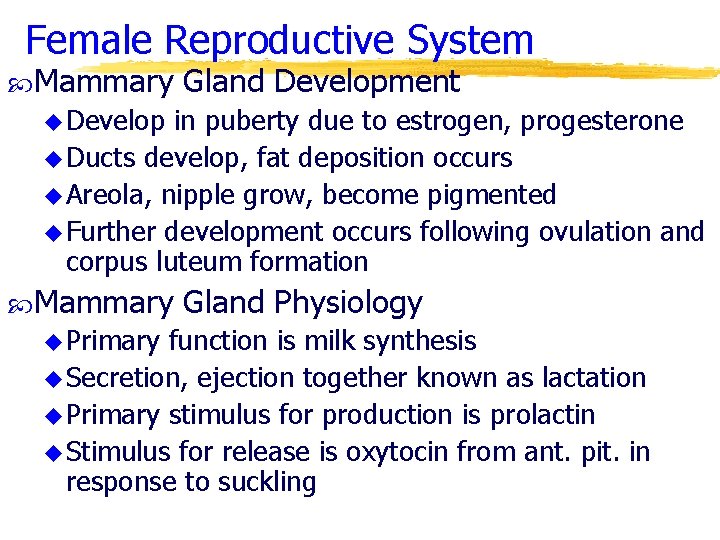
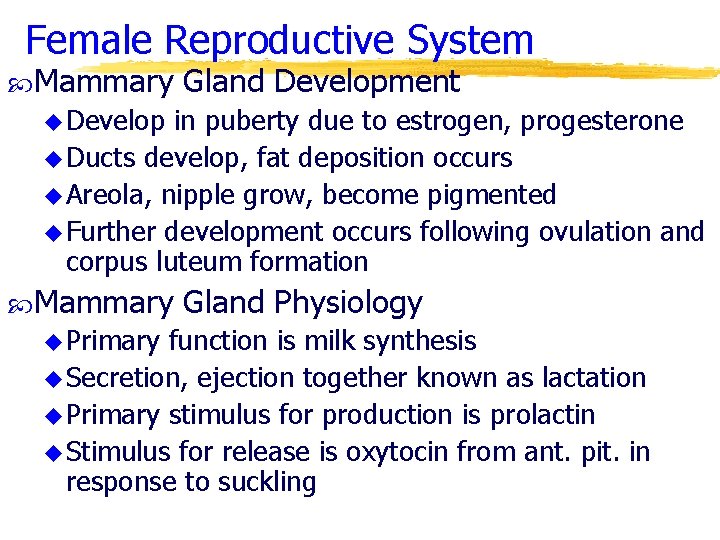
Female Reproductive System Mammary Gland Development u Develop in puberty due to estrogen, progesterone u Ducts develop, fat deposition occurs u Areola, nipple grow, become pigmented u Further development occurs following ovulation and corpus luteum formation Mammary u Primary Gland Physiology function is milk synthesis u Secretion, ejection together known as lactation u Primary stimulus for production is prolactin u Stimulus for release is oxytocin from ant. pit. in response to suckling
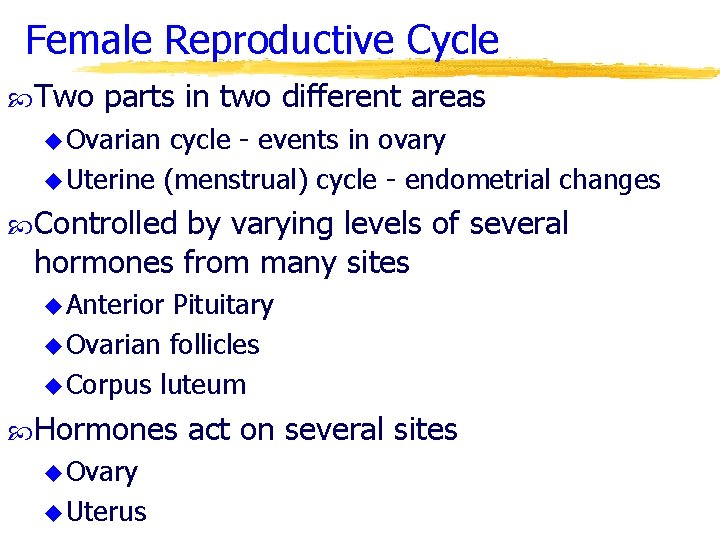
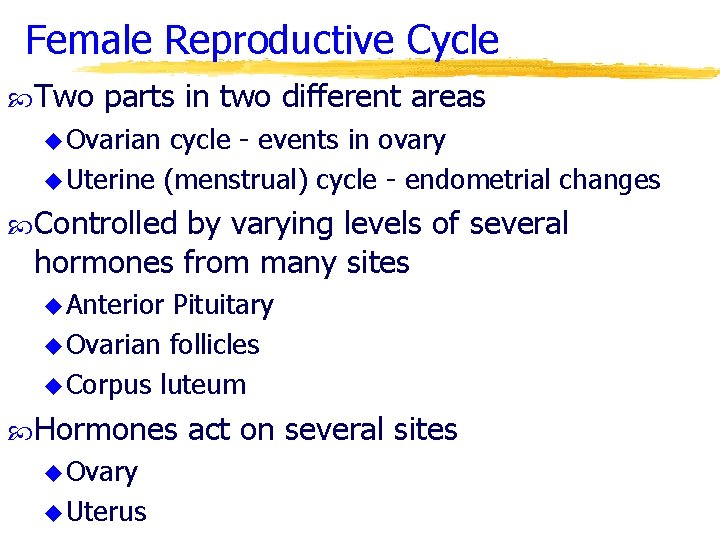
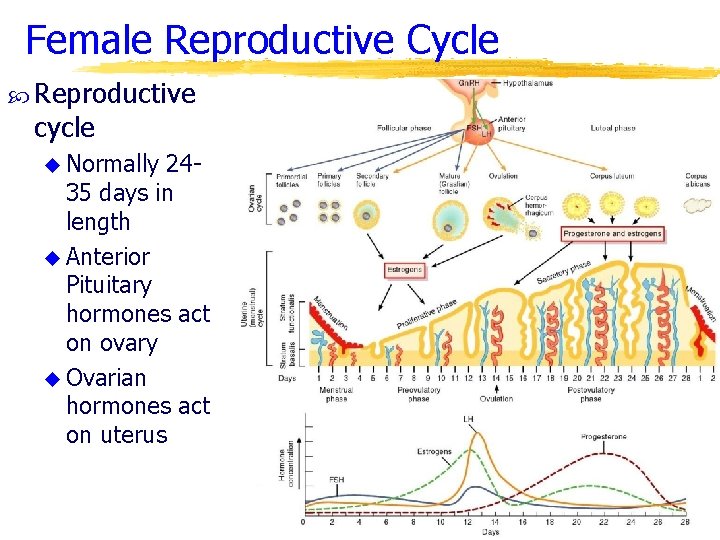
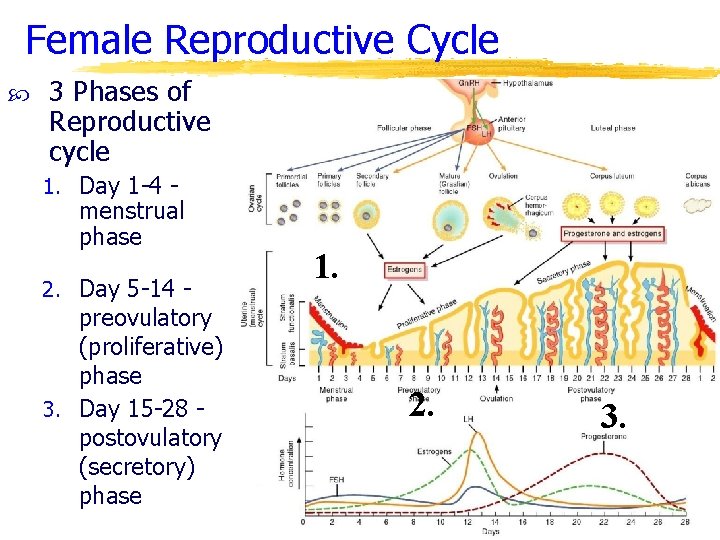
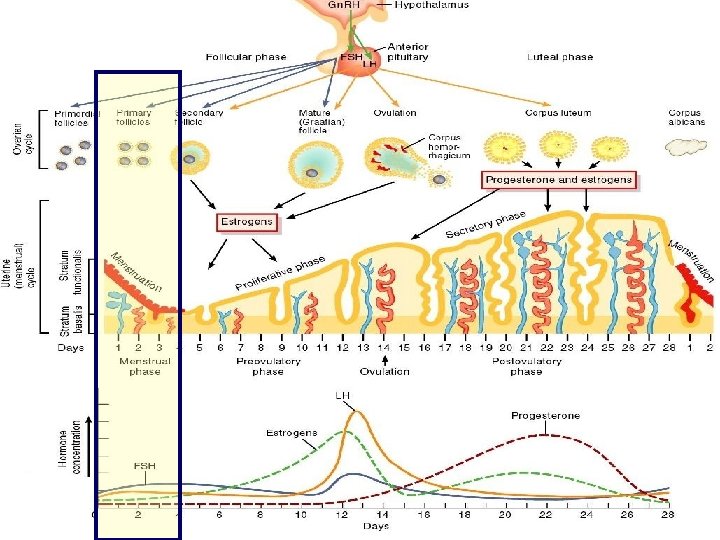
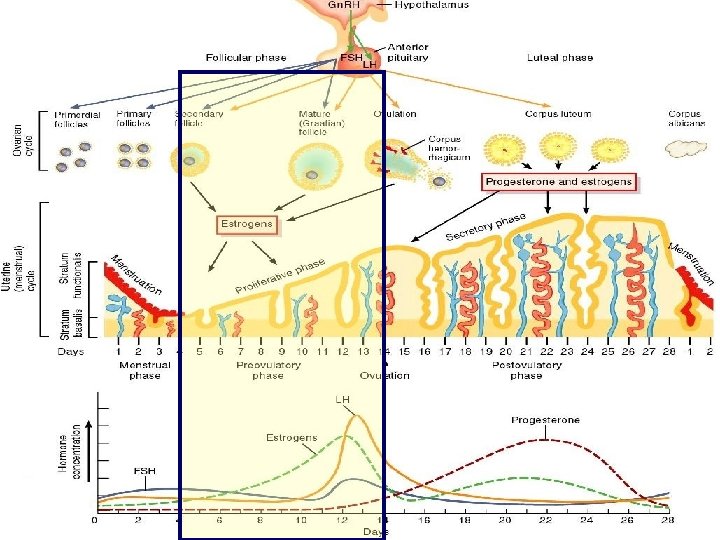
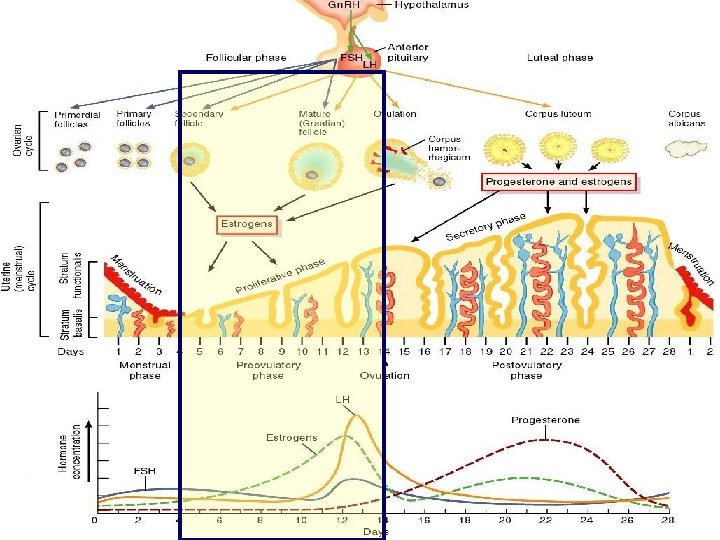
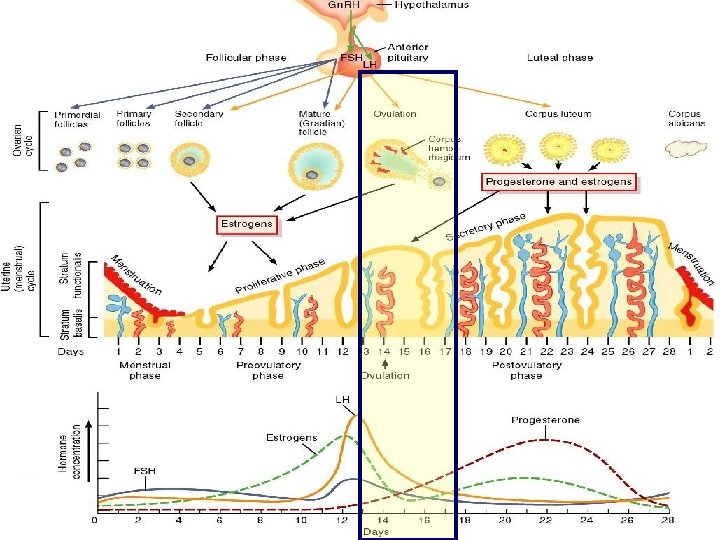
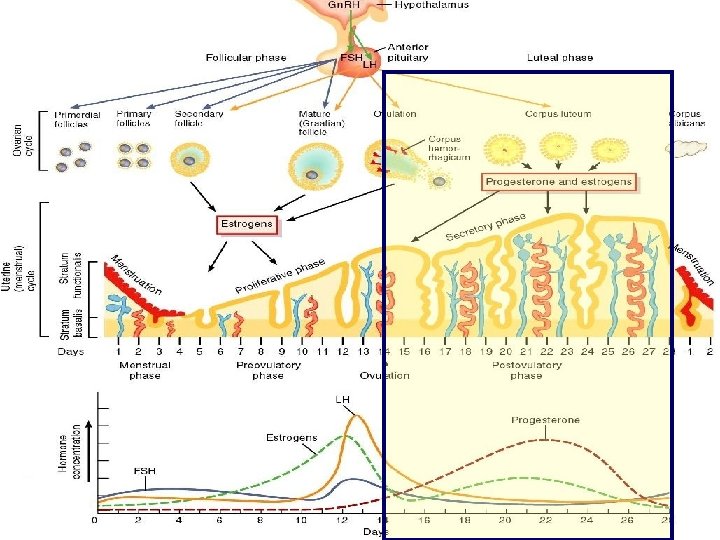
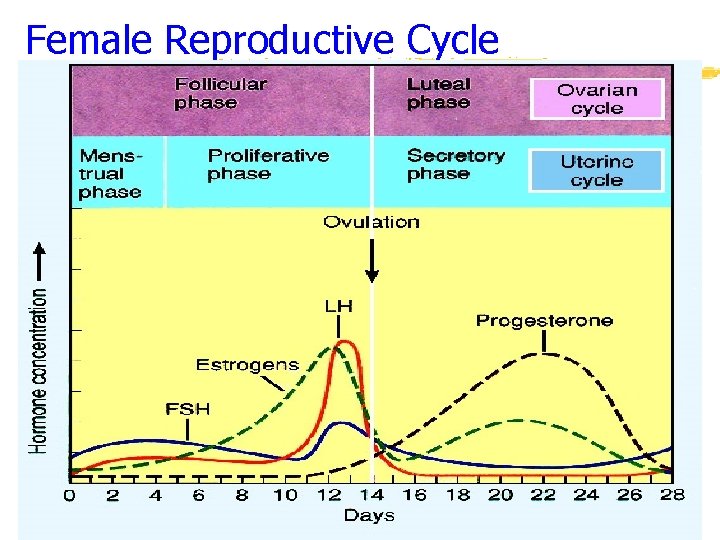
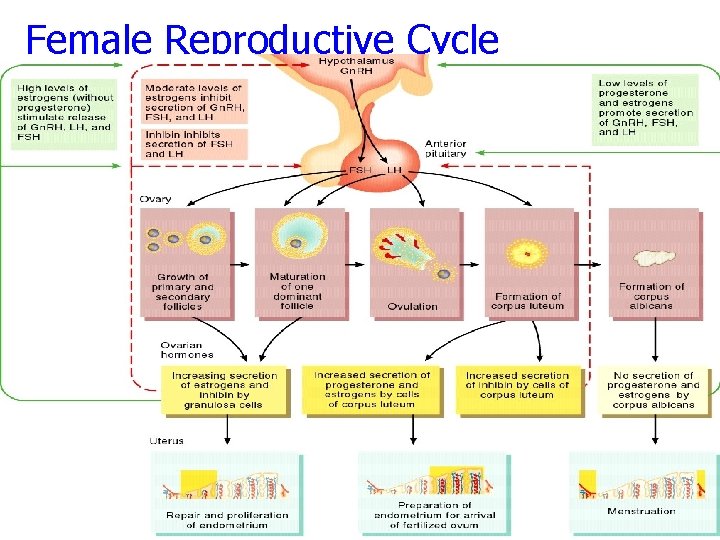
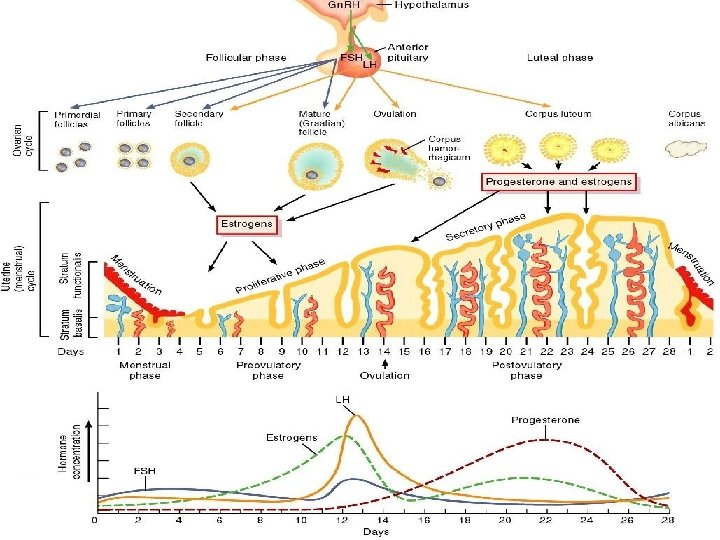
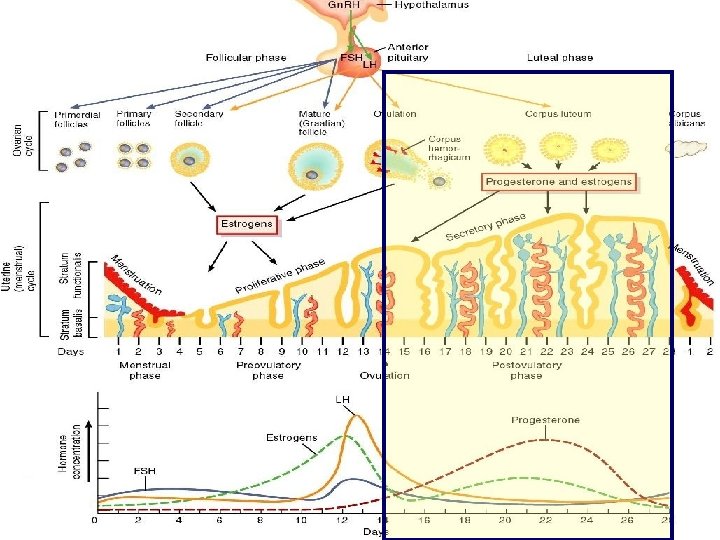
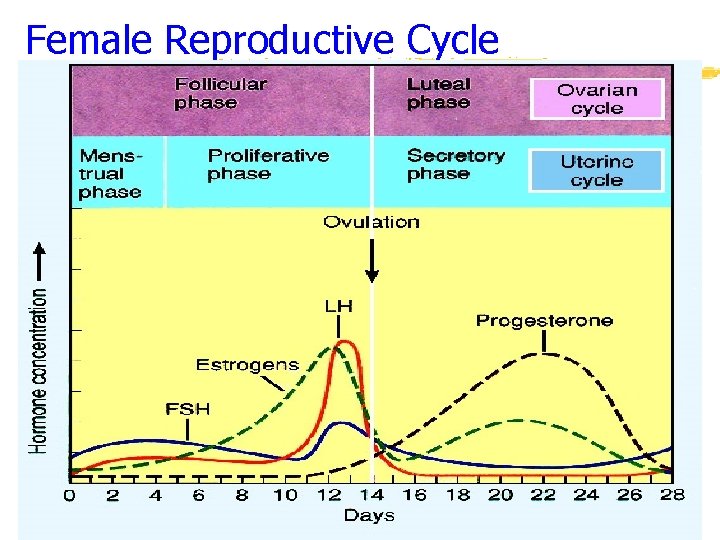
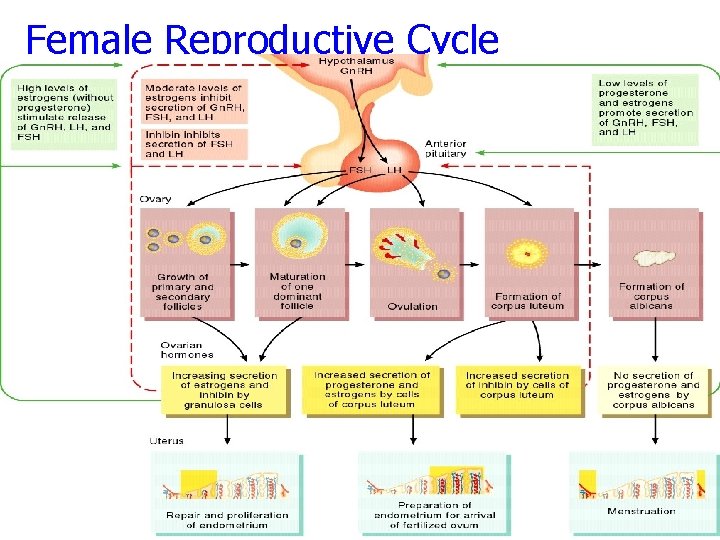
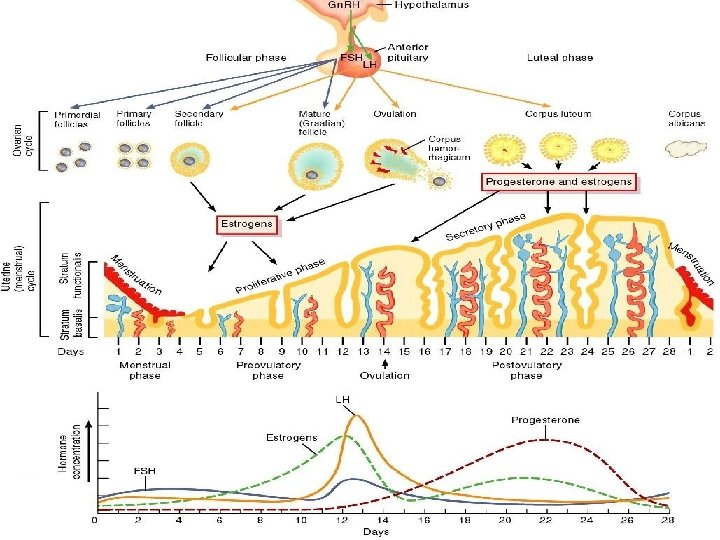
Female Reproductive Cycle Two parts in two different areas u Ovarian cycle - events in ovary u Uterine (menstrual) cycle - endometrial changes Controlled by varying levels of several hormones from many sites u Anterior Pituitary u Ovarian follicles u Corpus luteum Hormones u Ovary u Uterus act on several sites
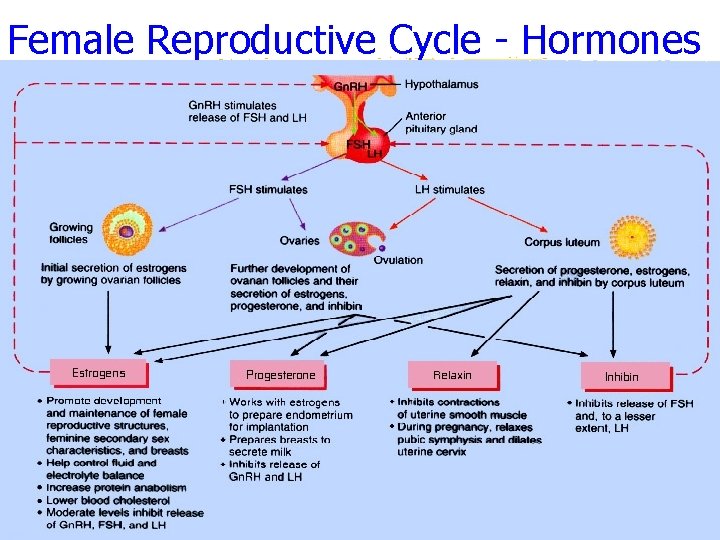
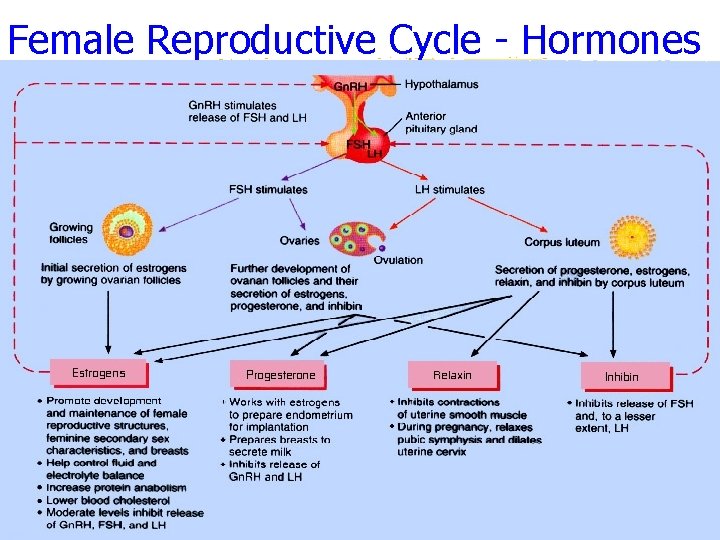
Female Reproductive Cycle - Hormones
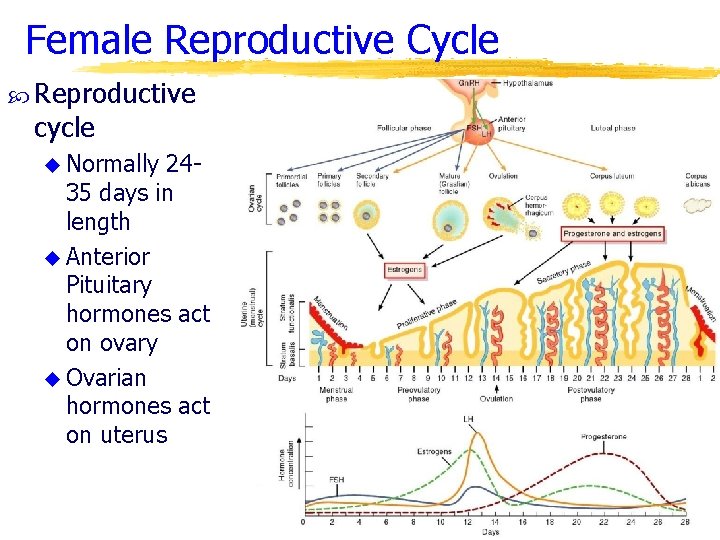
Female Reproductive Cycle Reproductive cycle u Normally 2435 days in length u Anterior Pituitary hormones act on ovary u Ovarian hormones act on uterus
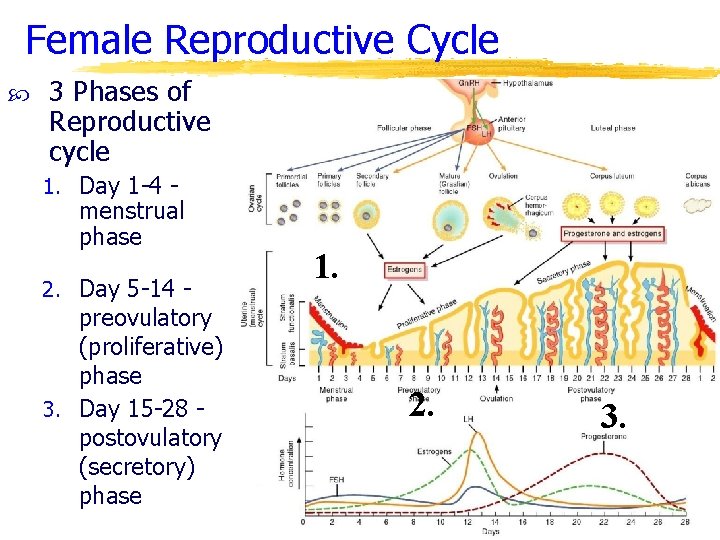
Female Reproductive Cycle 3 Phases of Reproductive cycle 1. Day 1 -4 - menstrual phase 2. Day 5 -14 - preovulatory (proliferative) phase 3. Day 15 -28 postovulatory (secretory) phase 1. 2. 3.
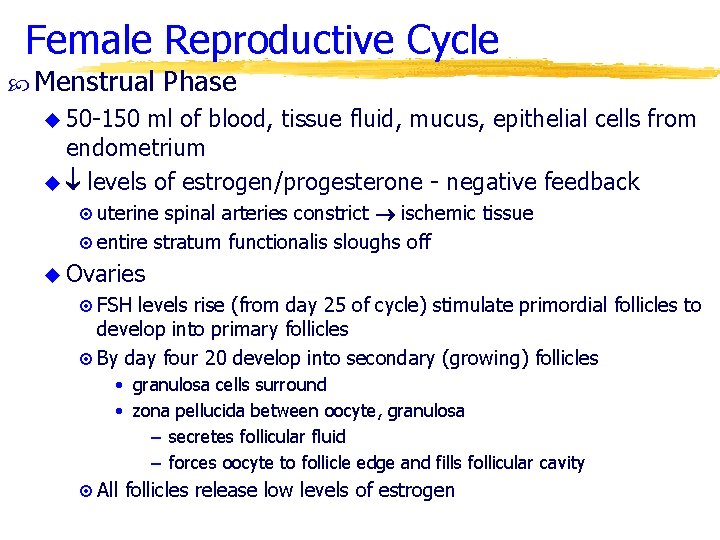
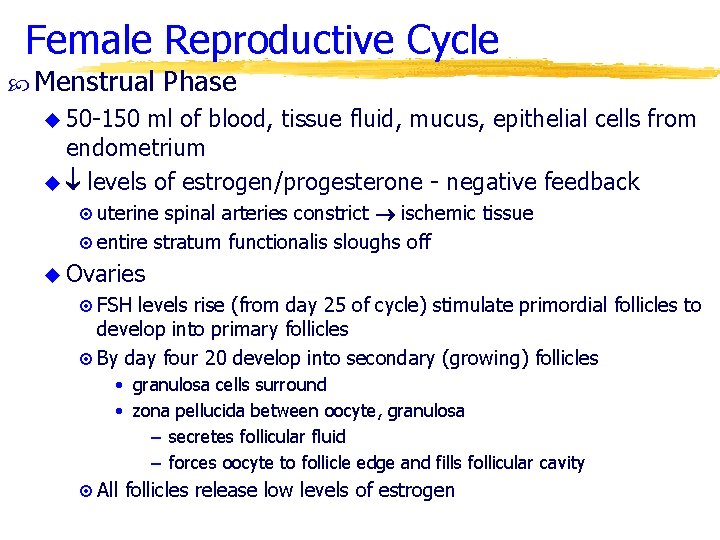
Female Reproductive Cycle Menstrual Phase u 50 -150 ml of blood, tissue fluid, mucus, epithelial cells from endometrium u levels of estrogen/progesterone - negative feedback ¤ uterine spinal arteries constrict ischemic tissue ¤ entire stratum functionalis sloughs off u Ovaries ¤ FSH levels rise (from day 25 of cycle) stimulate primordial follicles to develop into primary follicles ¤ By day four 20 develop into secondary (growing) follicles • granulosa cells surround • zona pellucida between oocyte, granulosa – secretes follicular fluid – forces oocyte to follicle edge and fills follicular cavity ¤ All follicles release low levels of estrogen
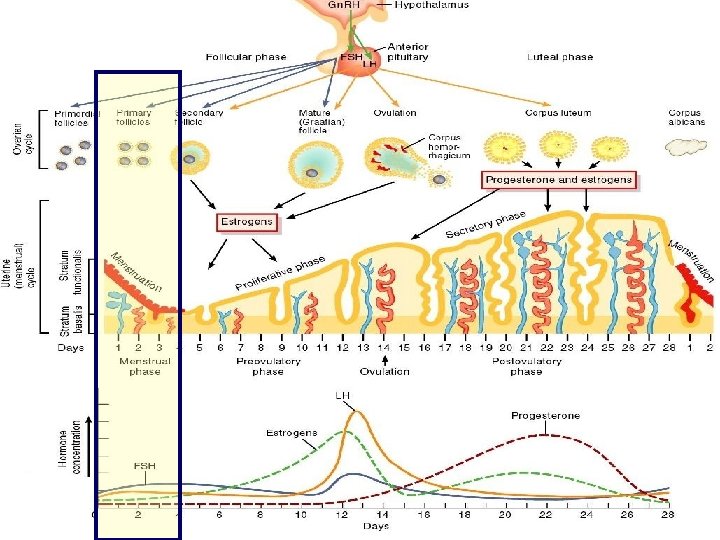
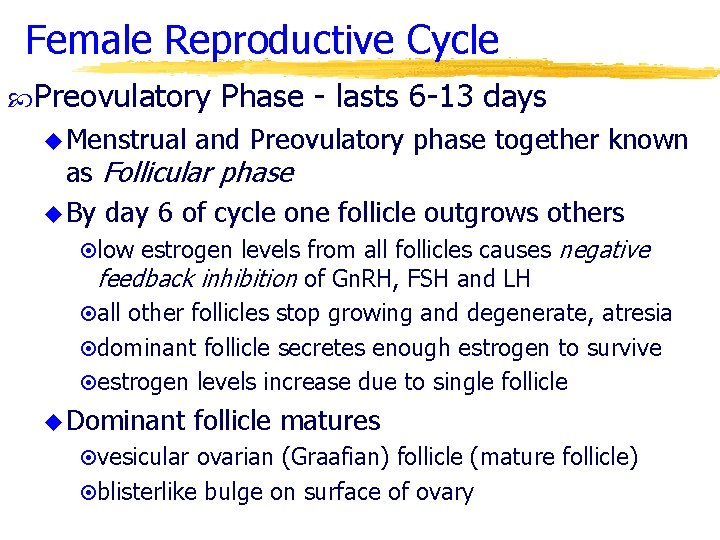
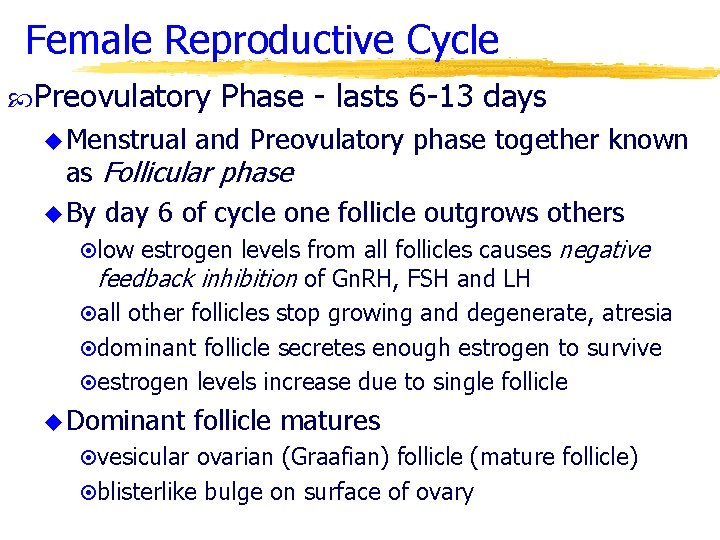
Female Reproductive Cycle Preovulatory u Menstrual Phase - lasts 6 -13 days and Preovulatory phase together known as Follicular phase u By day 6 of cycle one follicle outgrows others ¤low estrogen levels from all follicles causes feedback inhibition of Gn. RH, FSH and LH negative ¤all other follicles stop growing and degenerate, atresia ¤dominant follicle secretes enough estrogen to survive ¤estrogen levels increase due to single follicle u Dominant follicle matures ¤vesicular ovarian (Graafian) follicle (mature follicle) ¤blisterlike bulge on surface of ovary
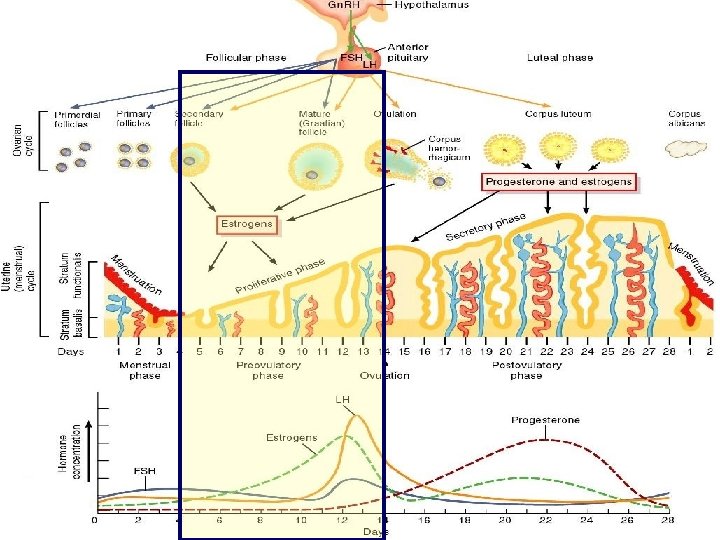
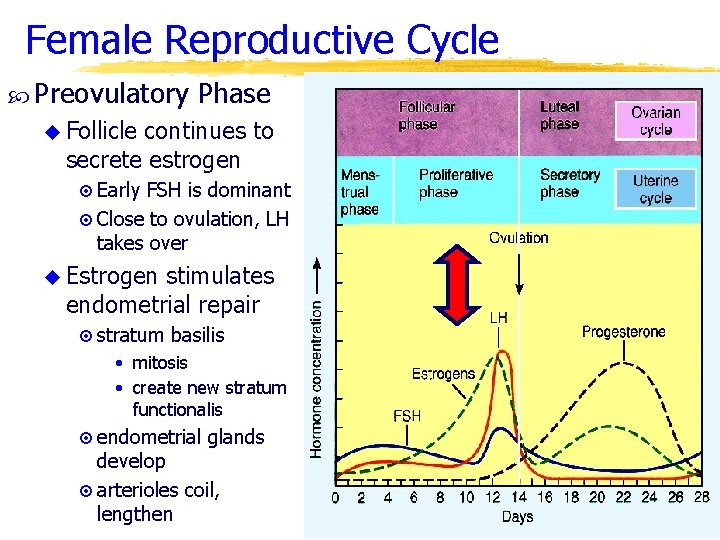
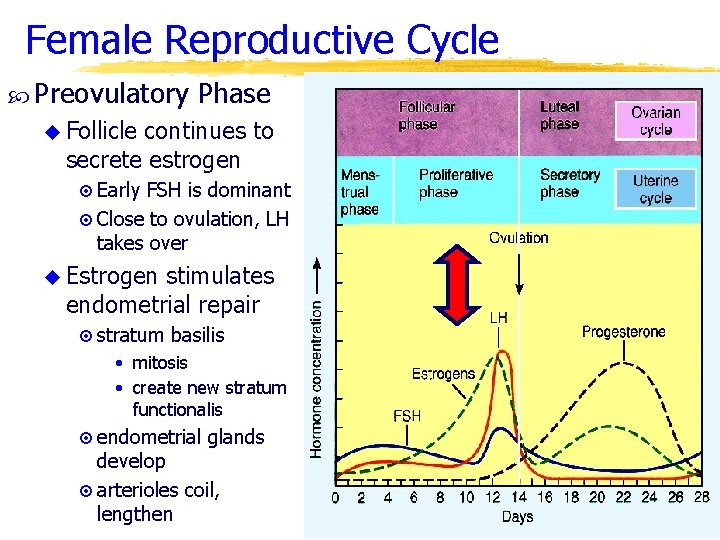
Female Reproductive Cycle Preovulatory Phase u Follicle continues to secrete estrogen ¤ Early FSH is dominant ¤ Close to ovulation, LH takes over u Estrogen stimulates endometrial repair ¤ stratum basilis • mitosis • create new stratum functionalis ¤ endometrial glands develop ¤ arterioles coil, lengthen
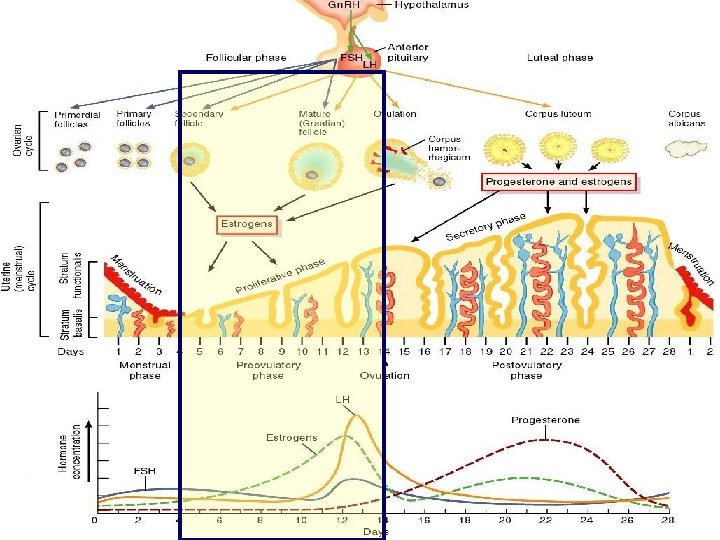
Female Reproductive Cycle Ovulation u Rupture of vesicular ovarian follicle and release into pelvic cavity occurs around day 14 u Secondary oocyte ¤surrounded by cells, corona radiata ¤secondary oocyte in metaphase II u Fimbrae become more active, create currents in fluid to carry oocyte into uterus u Changes in body temperature (estrogen) and cervical mucous (more stringy)
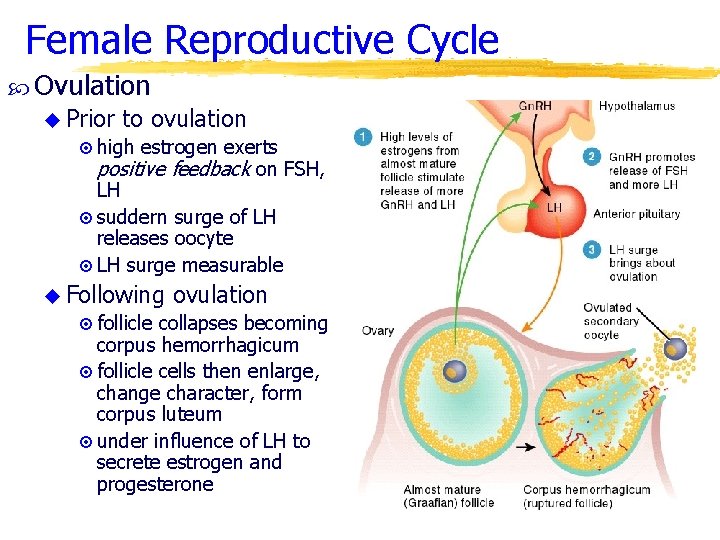
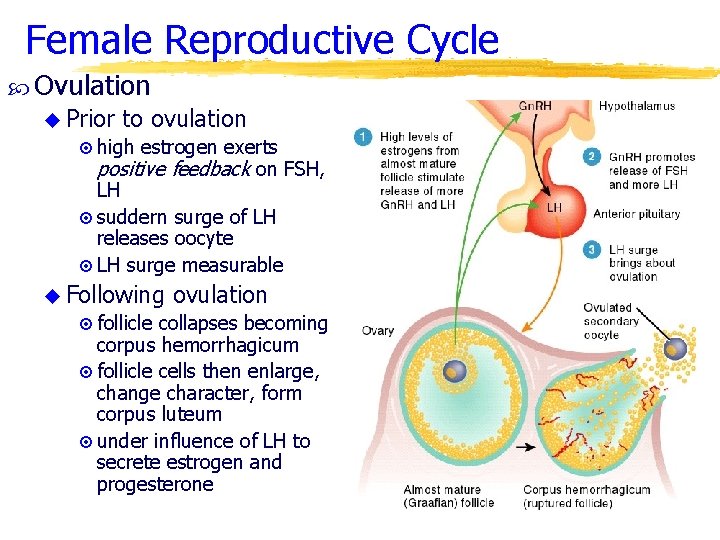
Female Reproductive Cycle Ovulation u Prior to ovulation ¤ high estrogen exerts positive feedback on FSH, LH ¤ suddern surge of LH releases oocyte ¤ LH surge measurable u Following ovulation ¤ follicle collapses becoming corpus hemorrhagicum ¤ follicle cells then enlarge, change character, form corpus luteum ¤ under influence of LH to secrete estrogen and progesterone
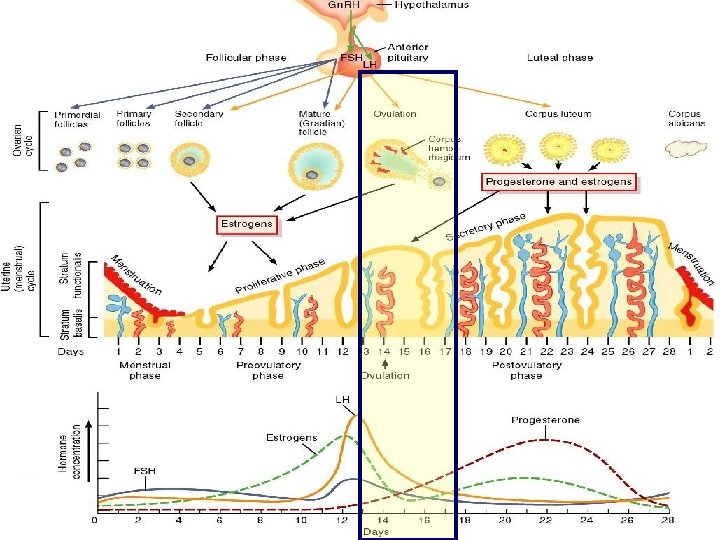
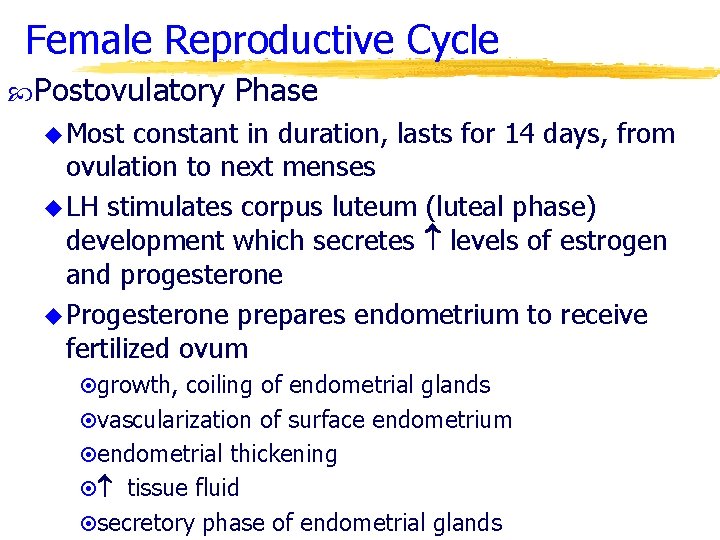
Female Reproductive Cycle Postovulatory Phase u Most constant in duration, lasts for 14 days, from ovulation to next menses u LH stimulates corpus luteum (luteal phase) development which secretes levels of estrogen and progesterone u Progesterone prepares endometrium to receive fertilized ovum ¤growth, coiling of endometrial glands ¤vascularization of surface endometrium ¤endometrial thickening ¤ tissue fluid ¤secretory phase of endometrial glands
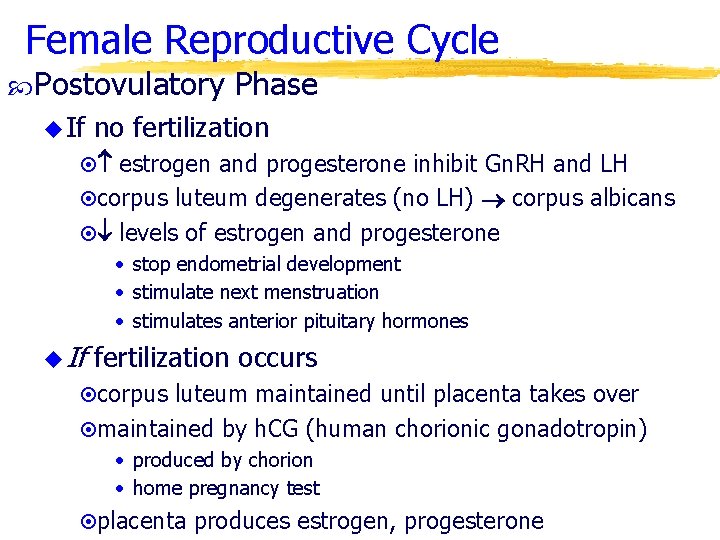
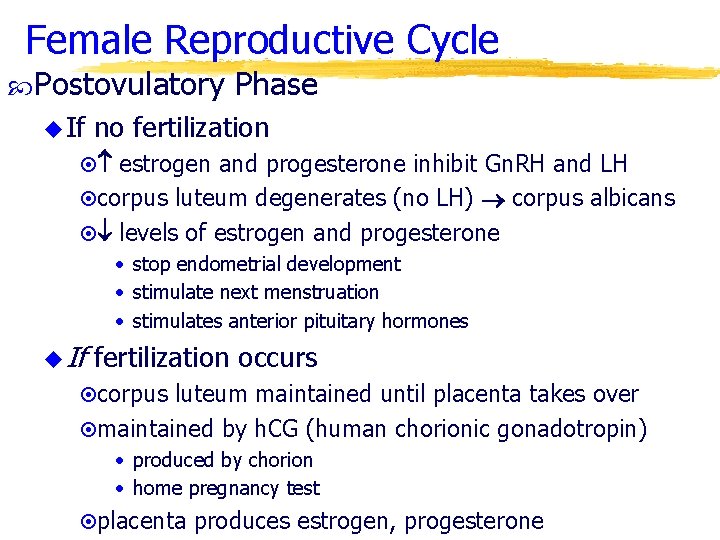
Female Reproductive Cycle Postovulatory u If Phase no fertilization ¤ estrogen and progesterone inhibit Gn. RH and LH ¤corpus luteum degenerates (no LH) corpus albicans ¤ levels of estrogen and progesterone • stop endometrial development • stimulate next menstruation • stimulates anterior pituitary hormones u If fertilization occurs ¤corpus luteum maintained until placenta takes over ¤maintained by h. CG (human chorionic gonadotropin) • produced by chorion • home pregnancy test ¤placenta produces estrogen, progesterone
Female Reproductive Cycle
Female Reproductive Cycle
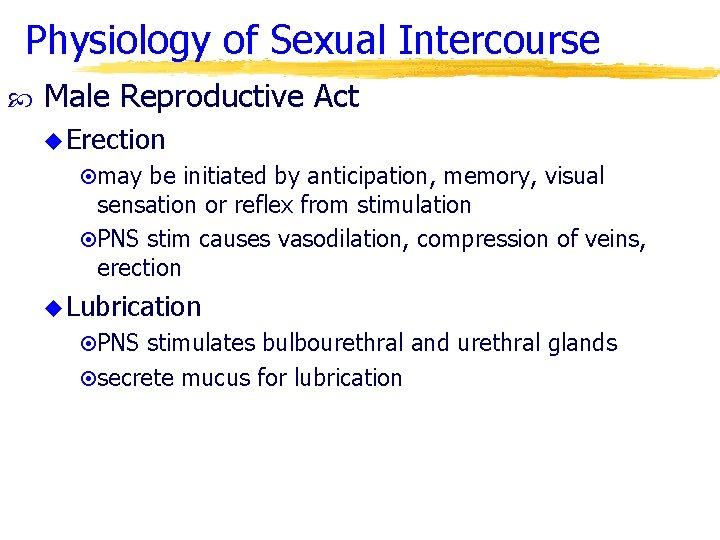
Physiology of Sexual Intercourse Male Reproductive Act u Erection ¤may be initiated by anticipation, memory, visual sensation or reflex from stimulation ¤PNS stim causes vasodilation, compression of veins, erection u Lubrication ¤PNS stimulates bulbourethral and urethral glands ¤secrete mucus for lubrication
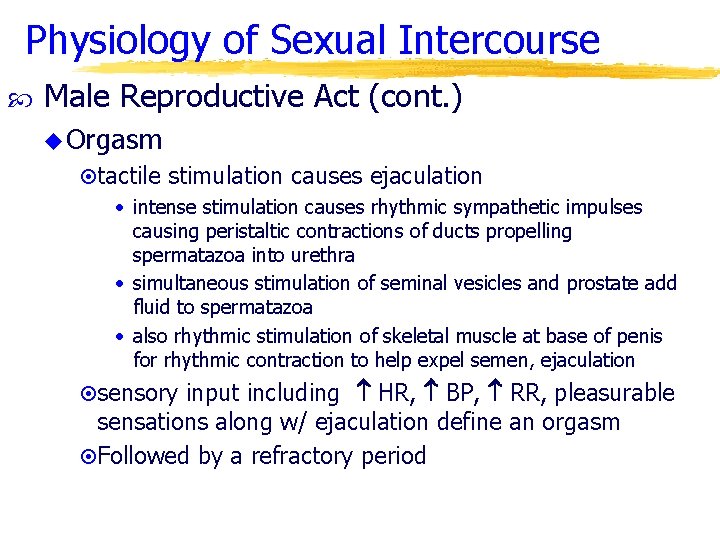
Physiology of Sexual Intercourse Male Reproductive Act (cont. ) u Orgasm ¤tactile stimulation causes ejaculation • intense stimulation causes rhythmic sympathetic impulses causing peristaltic contractions of ducts propelling spermatazoa into urethra • simultaneous stimulation of seminal vesicles and prostate add fluid to spermatazoa • also rhythmic stimulation of skeletal muscle at base of penis for rhythmic contraction to help expel semen, ejaculation ¤sensory input including HR, BP, RR, pleasurable sensations along w/ ejaculation define an orgasm ¤Followed by a refractory period
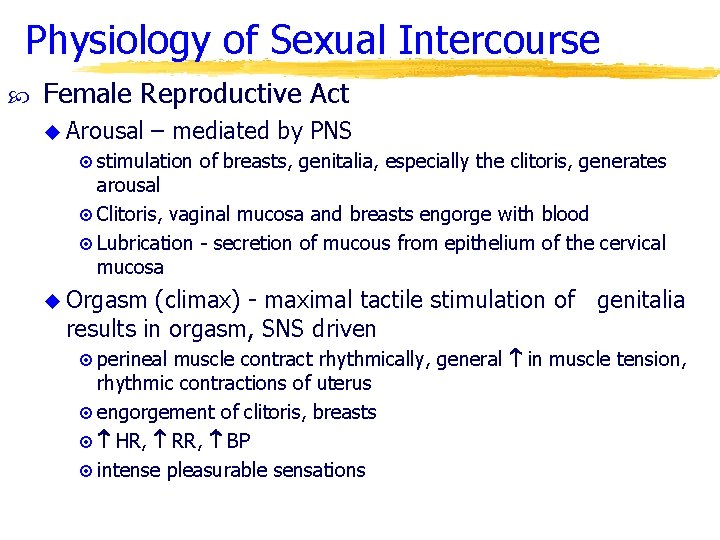
Physiology of Sexual Intercourse Female Reproductive Act u Arousal – mediated by PNS ¤ stimulation of breasts, genitalia, especially the clitoris, generates arousal ¤ Clitoris, vaginal mucosa and breasts engorge with blood ¤ Lubrication - secretion of mucous from epithelium of the cervical mucosa u Orgasm (climax) - maximal tactile stimulation of genitalia results in orgasm, SNS driven ¤ perineal muscle contract rhythmically, general in muscle tension, rhythmic contractions of uterus ¤ engorgement of clitoris, breasts ¤ HR, RR, BP ¤ intense pleasurable sensations
Female Reproductive System Breast u 1/9 Cancer women will have breast cancer u Early detection the most important aspect u Each month after menstrual period breasts should be examined for lumps, puckering of skin or nipple retraction or discharge
Female Reproductive System Breast u Risk Cancer factors ¤family history ¤no child or first child after 34 ¤previous cancer in breast ¤exposure to ionizing radiation (x-rays) ¤excess fat and alcohol intake, cigarette smoking u Detection - mammogram, flattening the key u Treatment ¤lumpectomy (removal of tumor and surrounding tissue) ¤radical mastectomy (breast, pectoral muscles, axillary lymph nodes)
Birth Control Sterilization u Vasectomy u Tubal ligation (uterine tubes cut and tied)
Birth Control Hormonal u Oral methods contraceptives ¤generally hi progesterone and low estrogen • negative feedback inhibition of FSH, LH and Gn. RH • preventing follicular development and ovulation • also alter cervical mucous and make endometrium less receptive to implantation ¤allows for regulation of length of menstrual cycles, menstrual flow, and prevention of ovarian cysts ¤not good for women w/ clotting problems, cerebral blood vessel damage, hypertension, liver malfunction or heart disease ¤also risk in women who smoke and drink for heart attack and stroke
Birth Control Hormonal methods u Norplant ¤ surgical implants under skin of progestin ¤ prevents ovulation and thickens cervical mucus ¤ no longer in widespread use u Depo-provera – IM injection every 3 months of progestin (similar to progesterone) u No male oral contraceptive currently available Intrauterine u Small devices plastic, copper or stainless steel device inserted into uterine cavity to prevent implantation u Danger of pelvic inflammatory disease, infertility and excess menstrual bleeding and pain
Birth Control Barrier methods u Condom ¤nonporous elastic (latex) preventing mechanical barrier to sperm deposition ¤reliable and prevents STD's when used correctly ¤both male and female (vaginal pouch) u Diaphragm ¤rubber dome-shaped device over cervix w/ spermicide to stop sperm passage ¤toxic shock syndrome and frequent urinary tract infections possible ¤does not prevent STD's
Birth Control Spermicides u Make vagina more inhospitable to sperm, inactivate HIV, decrease incidence of gonorrhea u More successful when used with barrier method Physiological u Rhythm methods method ¤abstention 3 days before and after ovulation ¤oocyte only viable for 24 hours after ovulation u Sympto-thermal method - abstention when signs of ovulation are present u Coitus interruptus (withdrawal)
Birth Control Induced abortion u RU 486 u blocks progesterone preventing proper endometrial development u menstruation occurs