Chapter 28 The Female Reproductive System 28 1
- Slides: 57
Chapter 28: The Female Reproductive System 28 -1
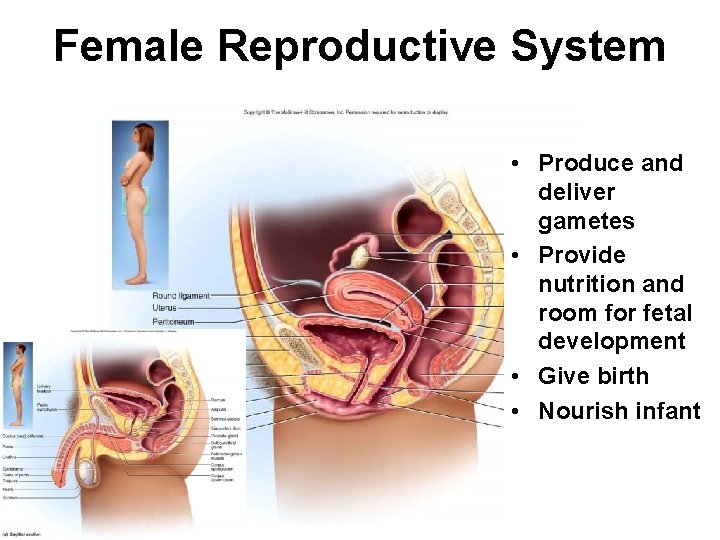
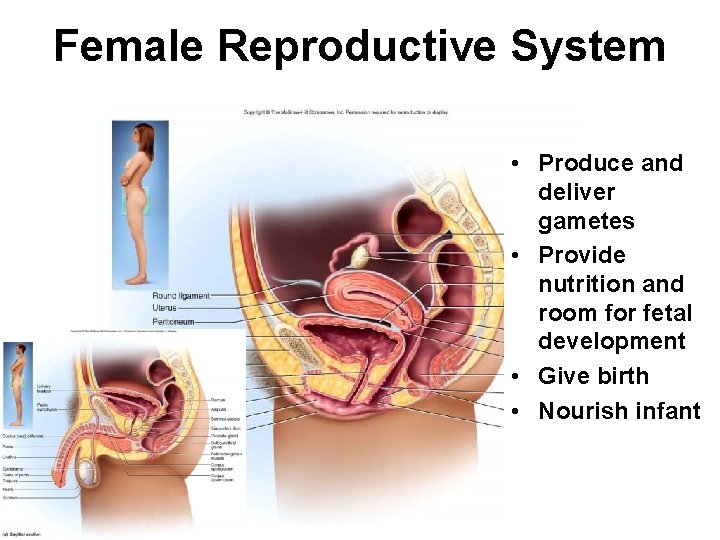
Female Reproductive System • Produce and deliver gametes • Provide nutrition and room for fetal development • Give birth • Nourish infant 28 -2
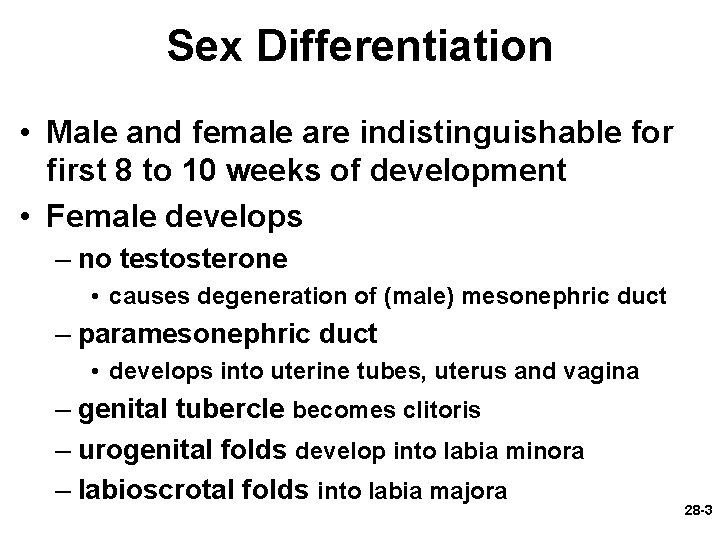
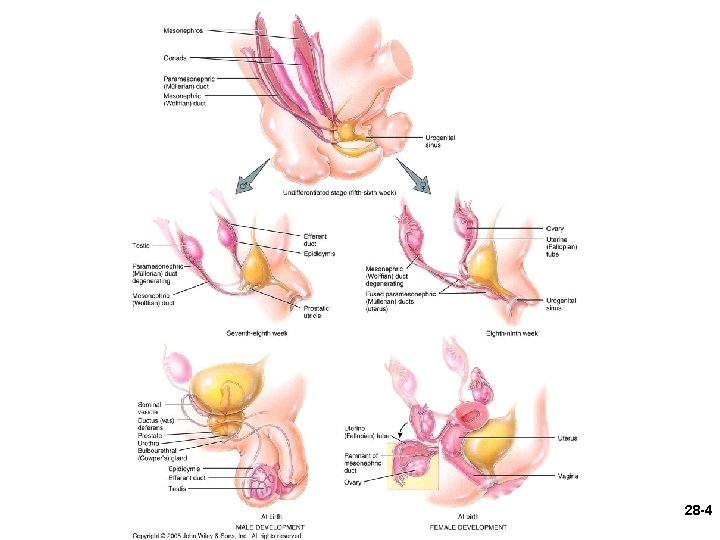
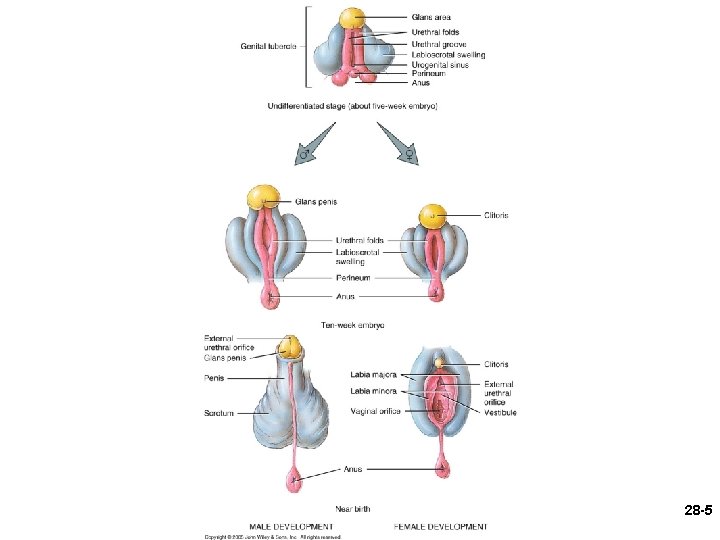
Sex Differentiation • Male and female are indistinguishable for first 8 to 10 weeks of development • Female develops – no testosterone • causes degeneration of (male) mesonephric duct – paramesonephric duct • develops into uterine tubes, uterus and vagina – genital tubercle becomes clitoris – urogenital folds develop into labia minora – labioscrotal folds into labia majora 28 -3
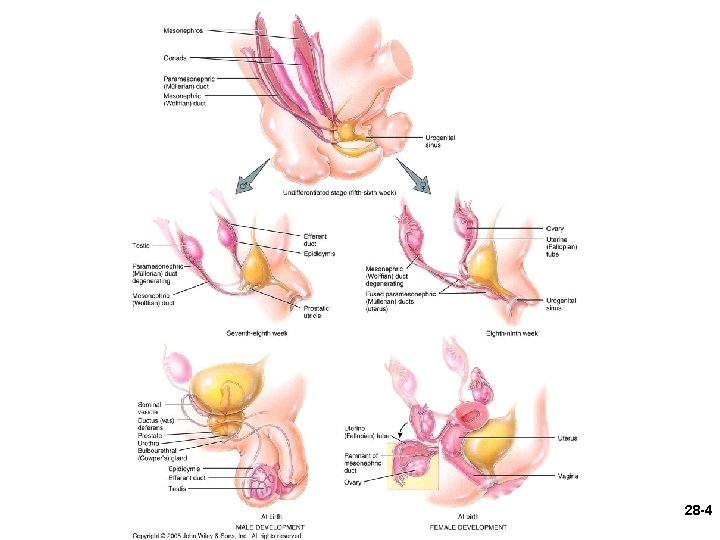
28 -4
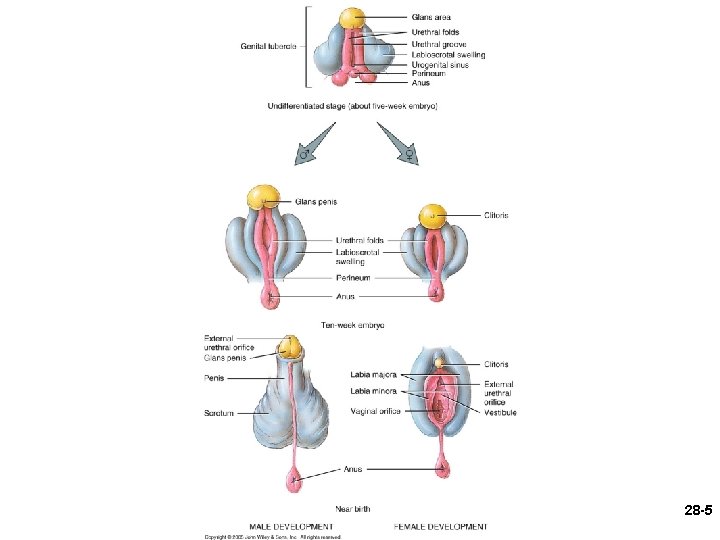
28 -5
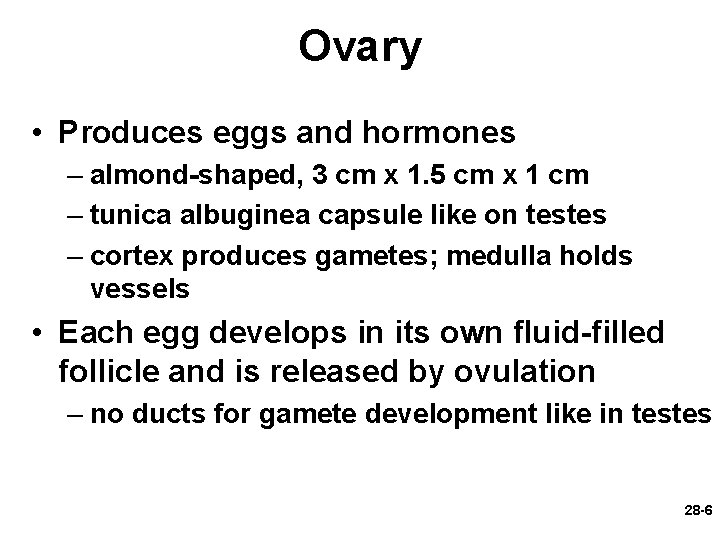
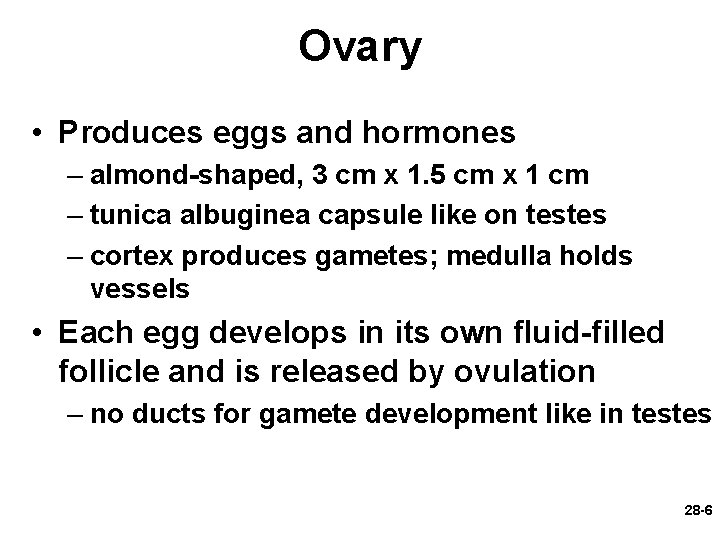
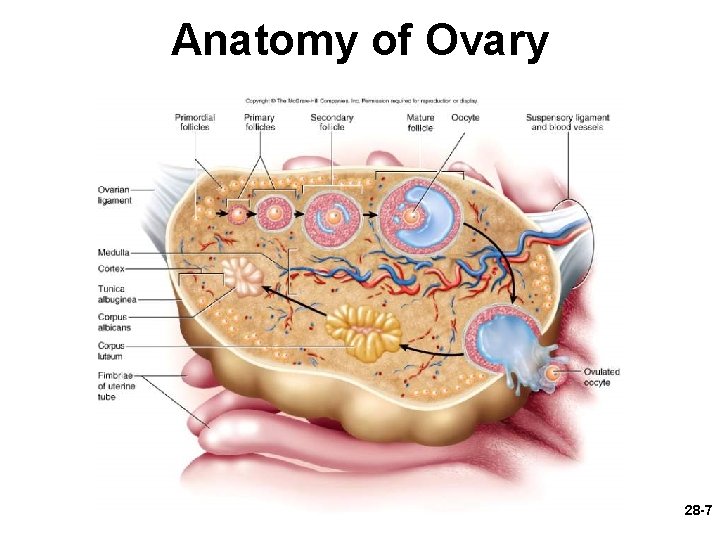
Ovary • Produces eggs and hormones – almond-shaped, 3 cm x 1. 5 cm x 1 cm – tunica albuginea capsule like on testes – cortex produces gametes; medulla holds vessels • Each egg develops in its own fluid-filled follicle and is released by ovulation – no ducts for gamete development like in testes 28 -6
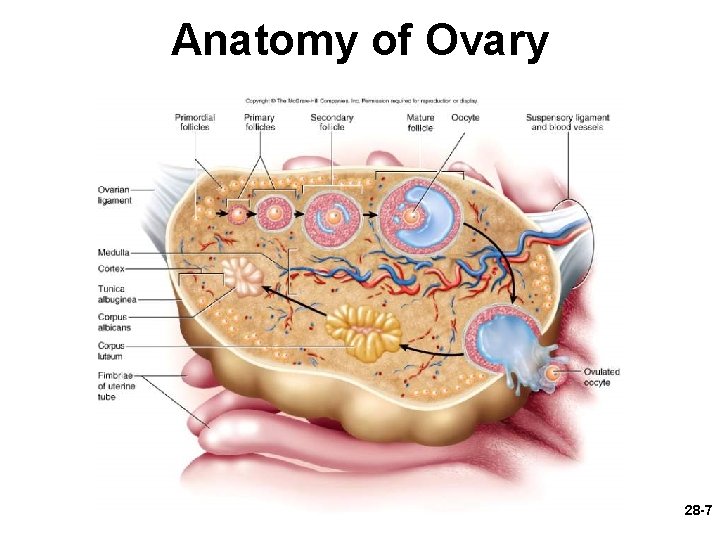
Anatomy of Ovary 28 -7
Secondary Sex Organs • Internal genitalia – duct system of uterine tubes, uterus, vagina • External genitalia – clitoris, labia minora, and labia majora – occupy perineum – accessory glands beneath skin provide lubrication 28 -8
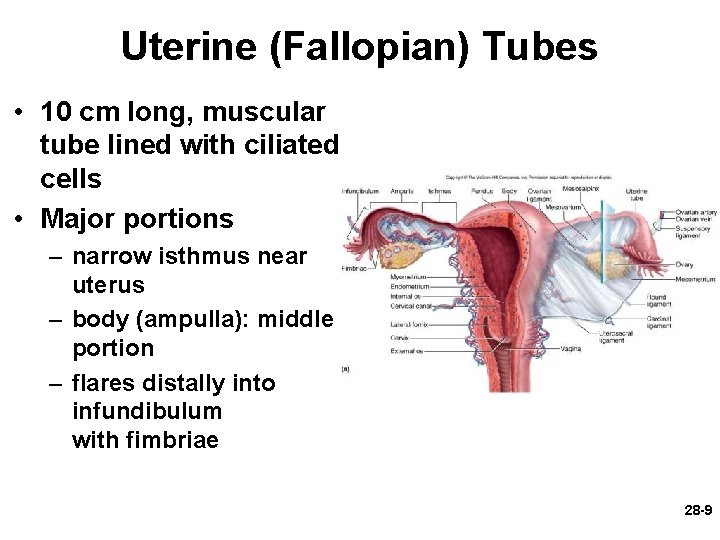
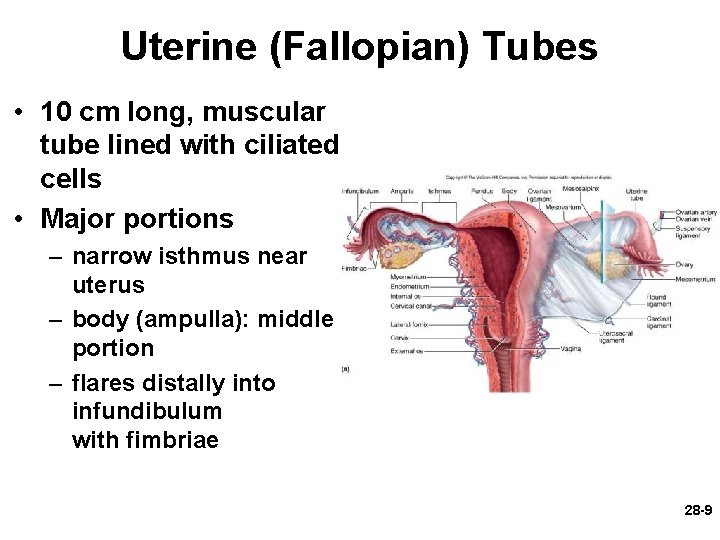
Uterine (Fallopian) Tubes • 10 cm long, muscular tube lined with ciliated cells • Major portions – narrow isthmus near uterus – body (ampulla): middle portion – flares distally into infundibulum with fimbriae 28 -9
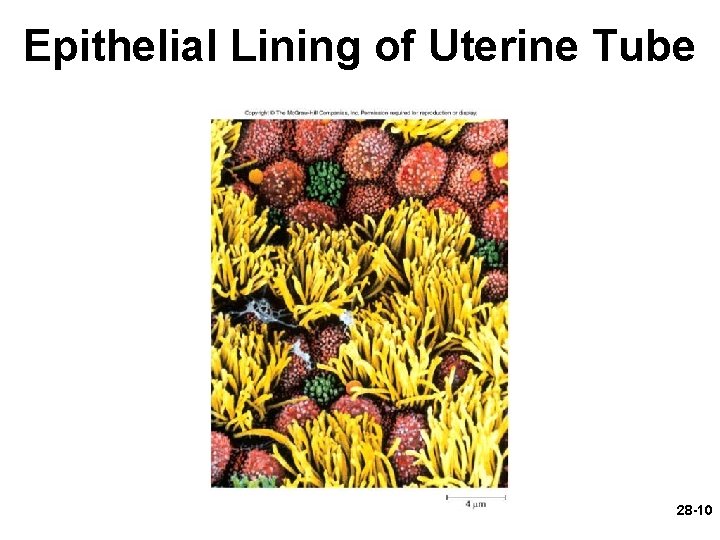
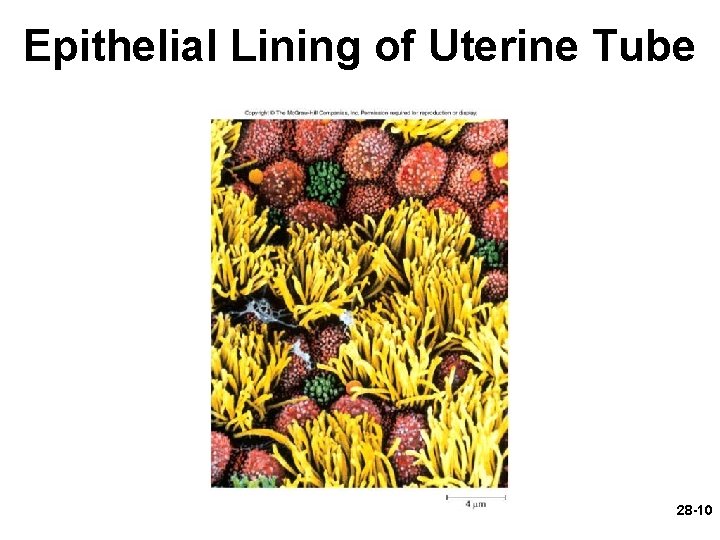
Epithelial Lining of Uterine Tube 28 -10
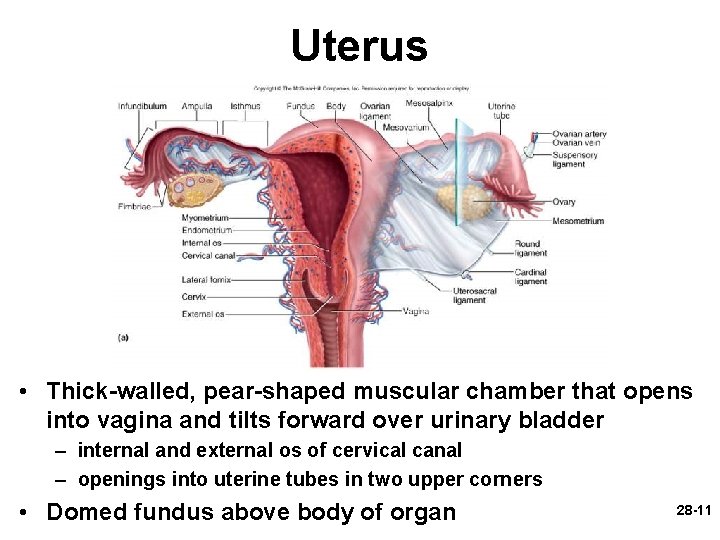
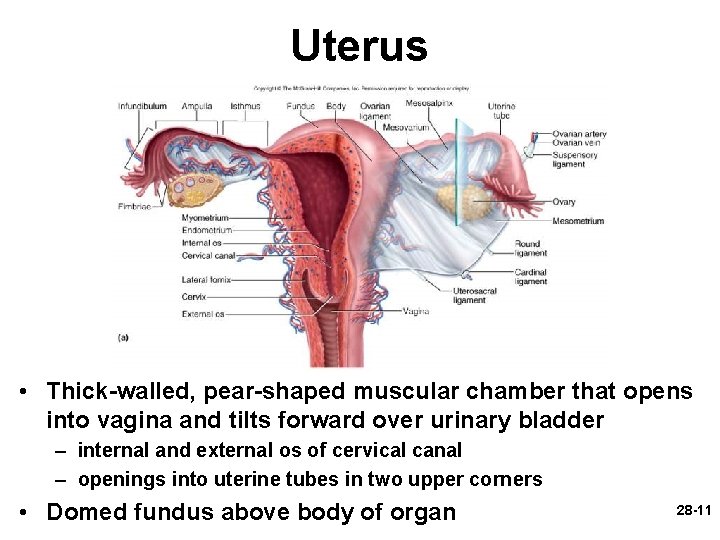
Uterus • Thick-walled, pear-shaped muscular chamber that opens into vagina and tilts forward over urinary bladder – internal and external os of cervical canal – openings into uterine tubes in two upper corners • Domed fundus above body of organ 28 -11
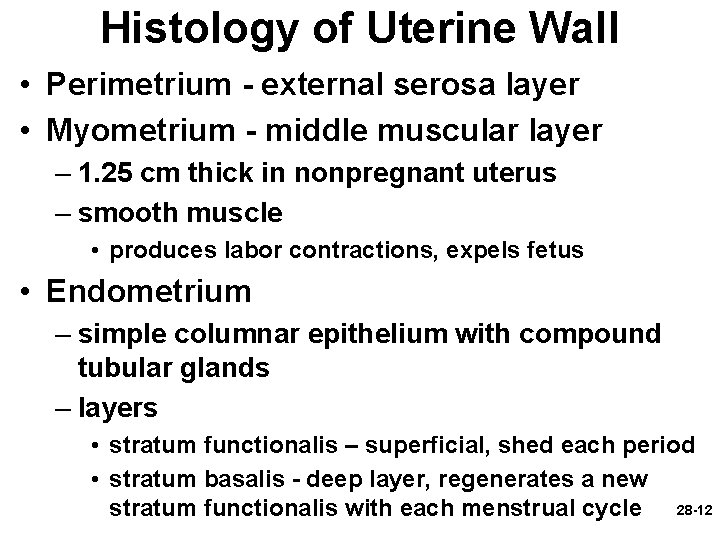
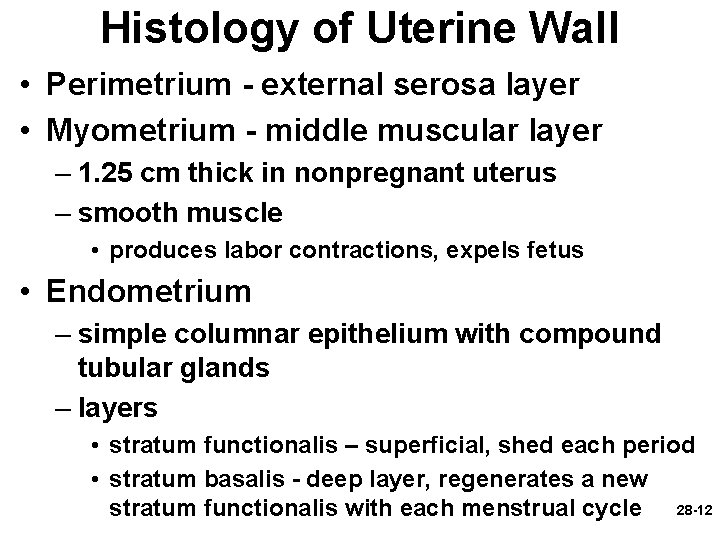
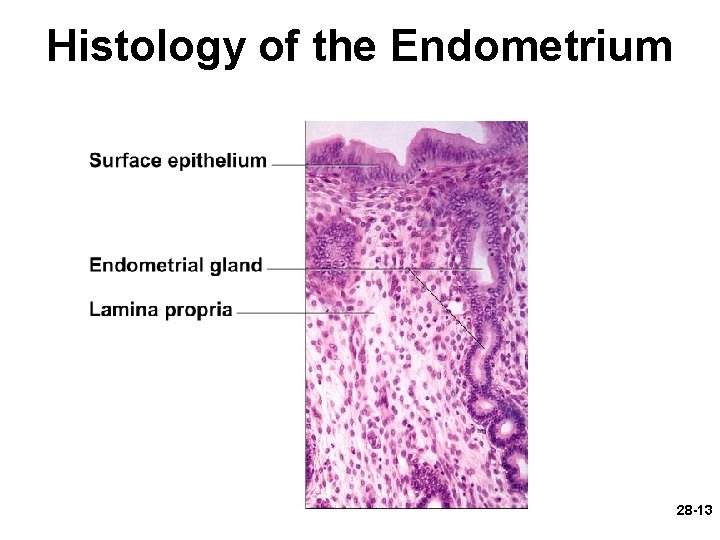
Histology of Uterine Wall • Perimetrium - external serosa layer • Myometrium - middle muscular layer – 1. 25 cm thick in nonpregnant uterus – smooth muscle • produces labor contractions, expels fetus • Endometrium – simple columnar epithelium with compound tubular glands – layers • stratum functionalis – superficial, shed each period • stratum basalis - deep layer, regenerates a new stratum functionalis with each menstrual cycle 28 -12
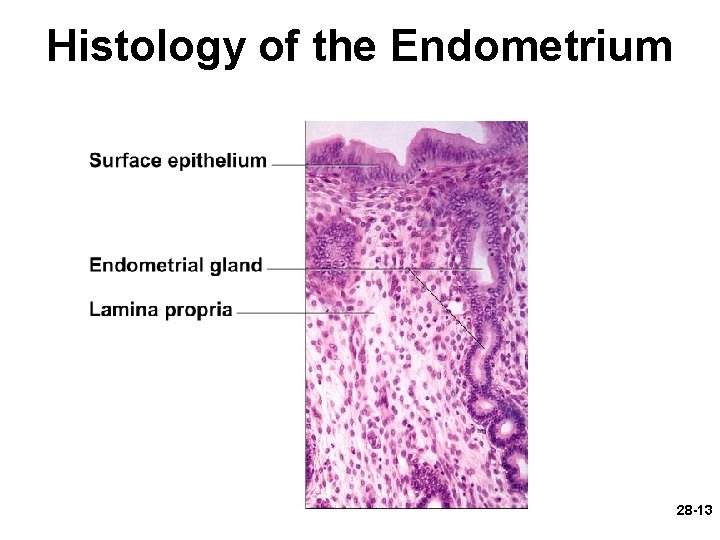
Histology of the Endometrium 28 -13
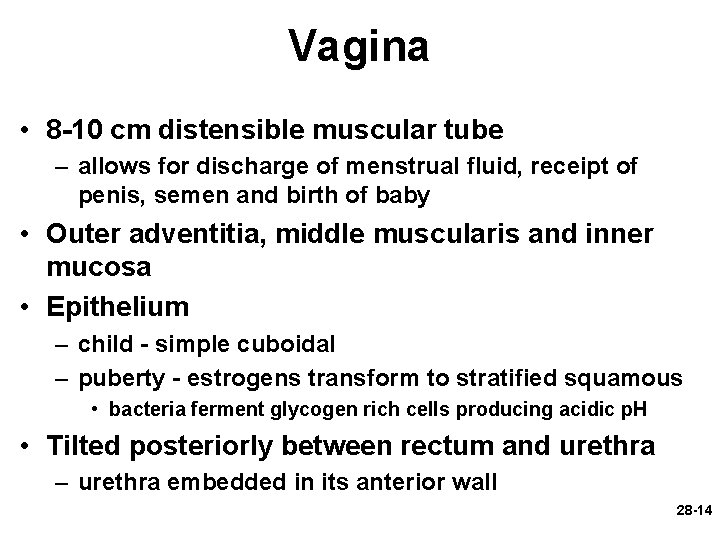
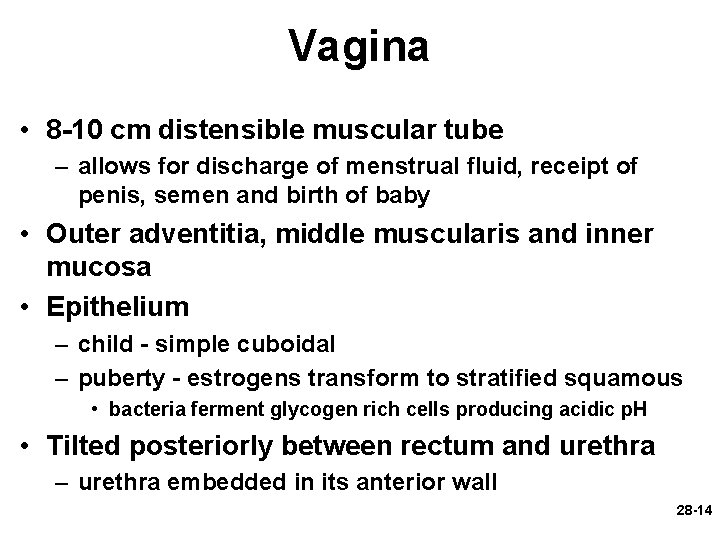
Vagina • 8 -10 cm distensible muscular tube – allows for discharge of menstrual fluid, receipt of penis, semen and birth of baby • Outer adventitia, middle muscularis and inner mucosa • Epithelium – child - simple cuboidal – puberty - estrogens transform to stratified squamous • bacteria ferment glycogen rich cells producing acidic p. H • Tilted posteriorly between rectum and urethra – urethra embedded in its anterior wall 28 -14
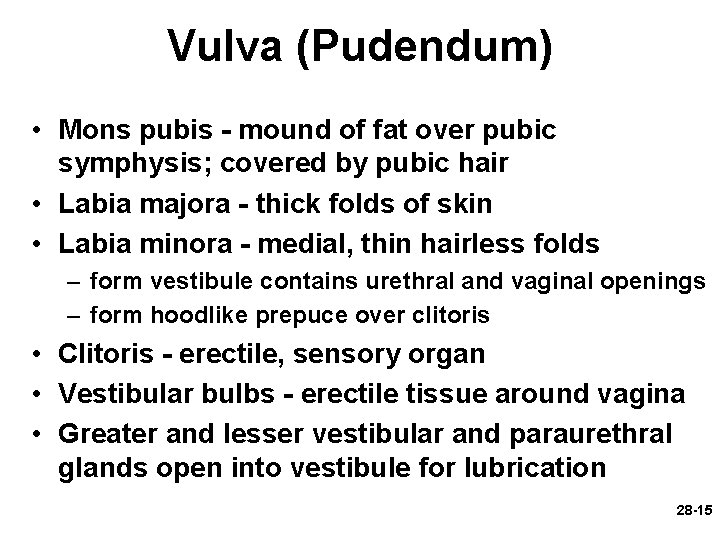
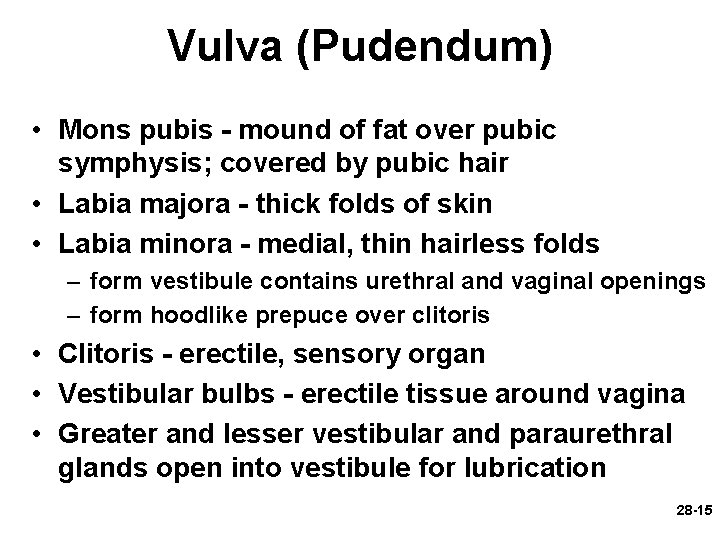
Vulva (Pudendum) • Mons pubis - mound of fat over pubic symphysis; covered by pubic hair • Labia majora - thick folds of skin • Labia minora - medial, thin hairless folds – form vestibule contains urethral and vaginal openings – form hoodlike prepuce over clitoris • Clitoris - erectile, sensory organ • Vestibular bulbs - erectile tissue around vagina • Greater and lesser vestibular and paraurethral glands open into vestibule for lubrication 28 -15
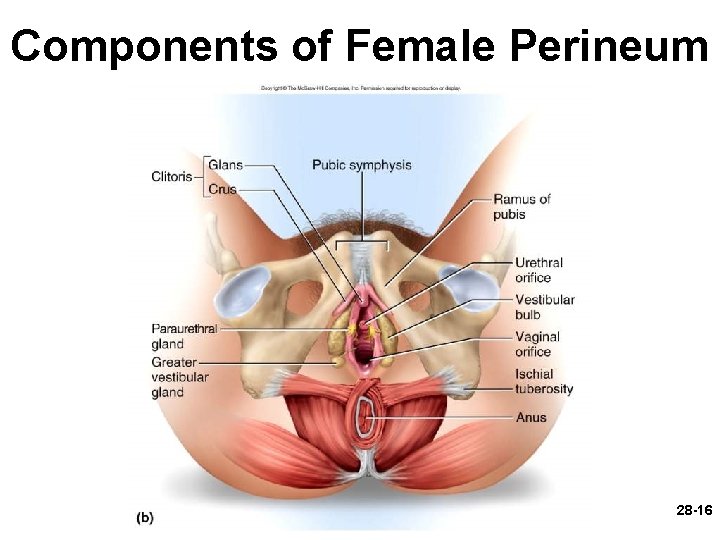
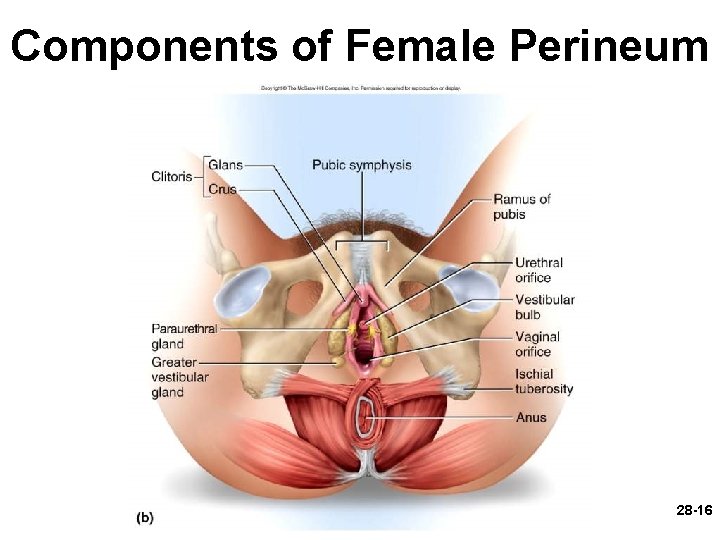
Components of Female Perineum 28 -16
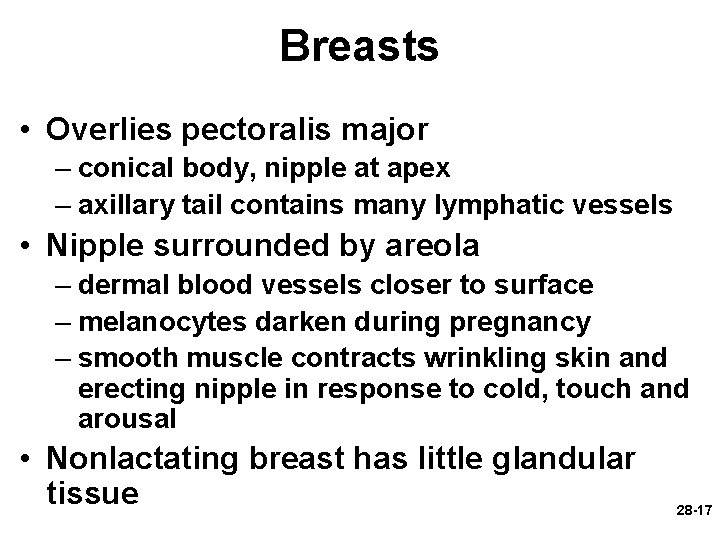
Breasts • Overlies pectoralis major – conical body, nipple at apex – axillary tail contains many lymphatic vessels • Nipple surrounded by areola – dermal blood vessels closer to surface – melanocytes darken during pregnancy – smooth muscle contracts wrinkling skin and erecting nipple in response to cold, touch and arousal • Nonlactating breast has little glandular tissue 28 -17
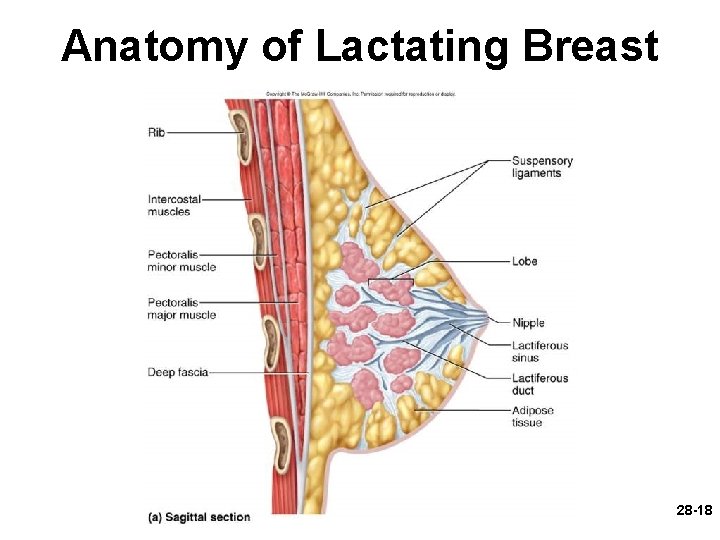
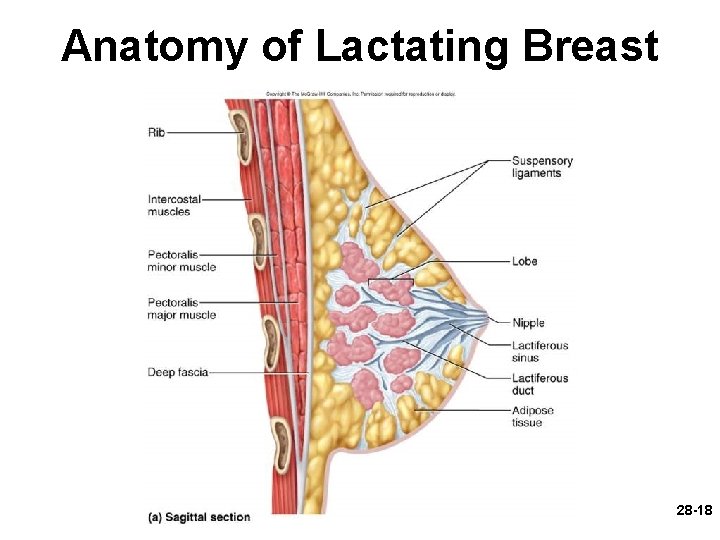
Anatomy of Lactating Breast 28 -18
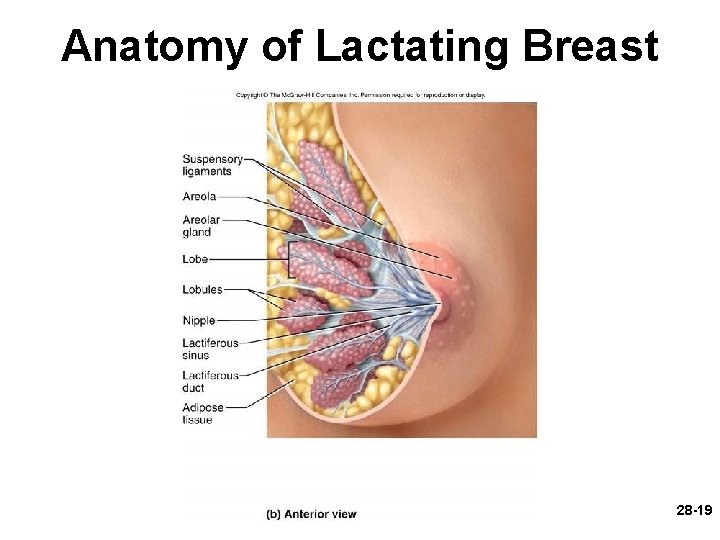
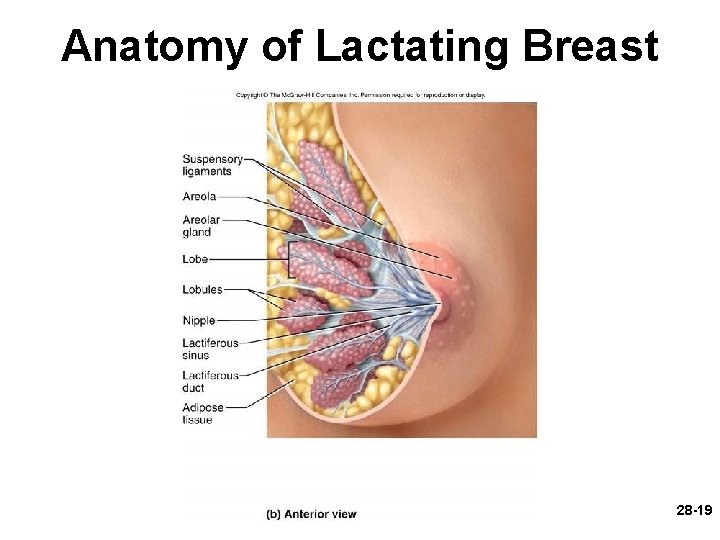
Anatomy of Lactating Breast 28 -19
Puberty • Begins at age 9 -10 (US) • Triggered by rising levels of Gn. RH – stimulates anterior lobe of pituitary to produce • follicle-stimulating hormone (FSH) • luteinizing hormone (LH) • Follicles develop and begin to secrete estrogen and progesterone 28 -20
Puberty • Thelarche (thee-LAR-kee) - development of breasts • Pubarche (pyu-BAR-kee) - growth of pubic and axillary hair; apocrine and sebaceous glands • Menarche (men-AR-kee) - first menstrual period – requires at least 17% body fat in teenager, 22% in adult • leptin stimulates gonadotropin secretion • improved nutrition ( body fat) has lowered avg. age of onset to 12 • Female hormones secreted cyclically and in sequence 28 -21
Climacteric • Midlife change in hormone secretion – due to age related depletion of follicles – occurs with menopause (cessation of menstruation); average of 52 • Results – atrophy of uterus, vagina and breasts – skin becomes thinner, bone mass declines, and risks of cardiovascular disease increase – hot flashes (sudden dilation of cutaneous arteries) occur several times a day • HRT = hormone replacement therapy 28 -22
Oogensis and Sexual Cycle • Reproductive cycle - events occurring between fertilization and birth • Sexual cycle - events recurring every month when pregnancy does not occur – ovarian cycle = events in ovaries – menstrual cycle = parallel changes in uterus 28 -23
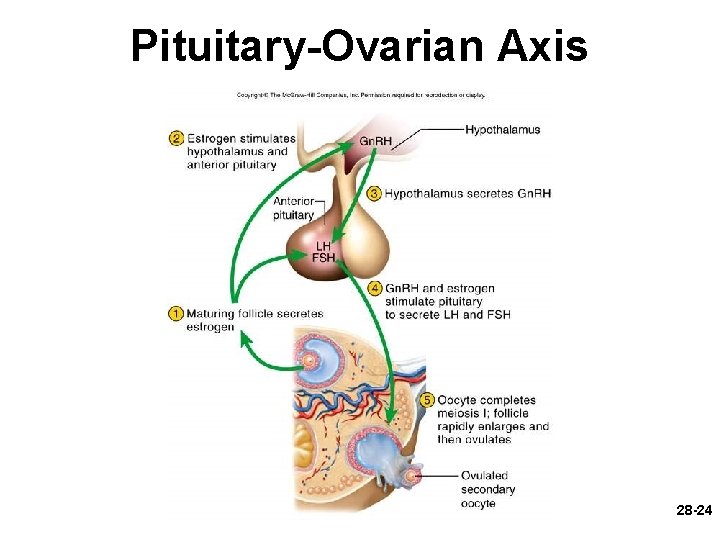
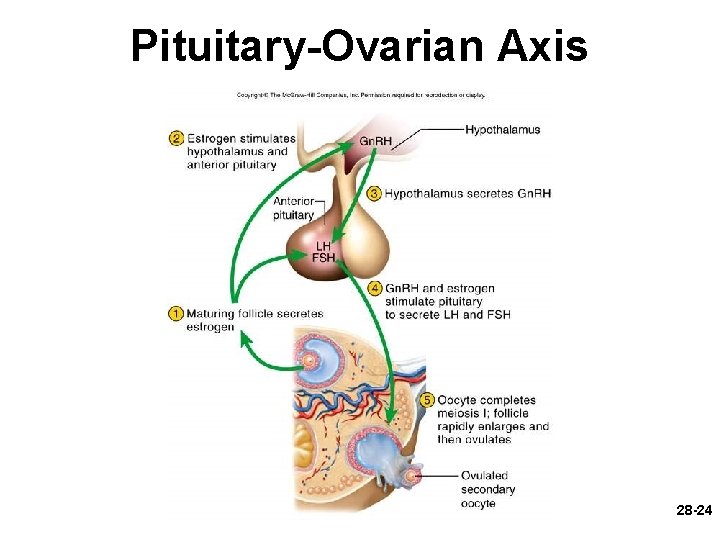
Pituitary-Ovarian Axis 28 -24
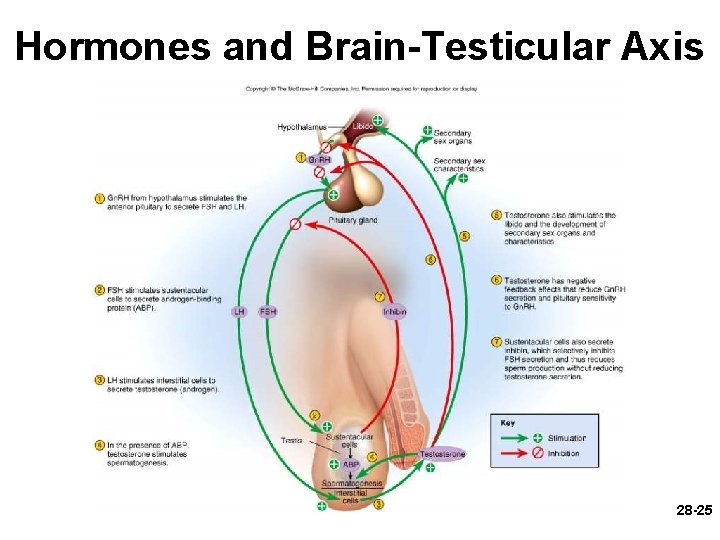
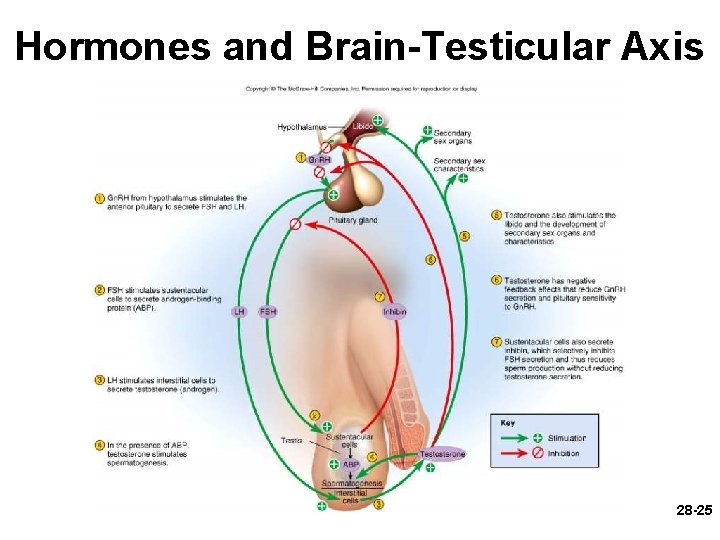
Hormones and Brain-Testicular Axis 28 -25
28 -26
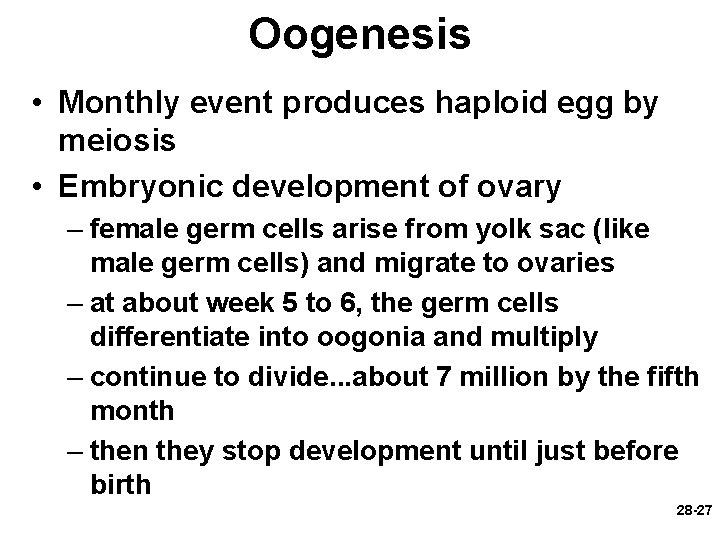
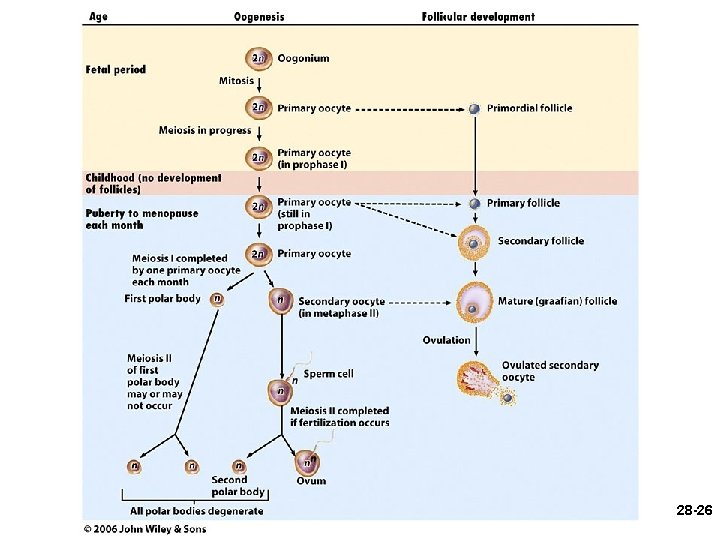
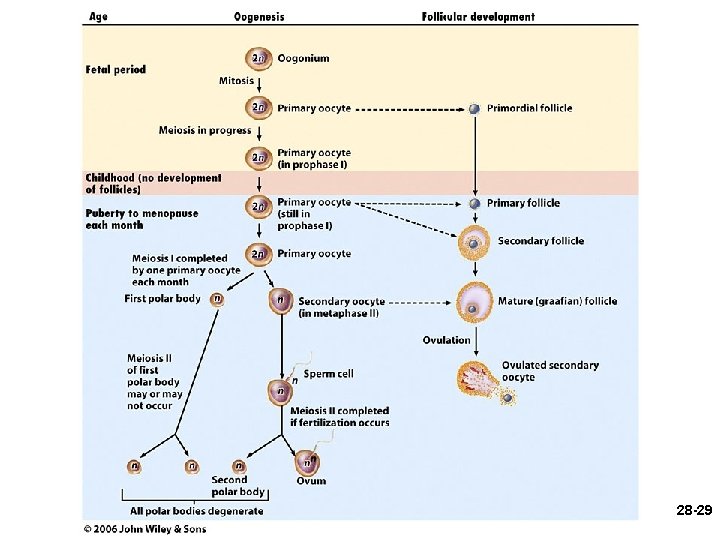
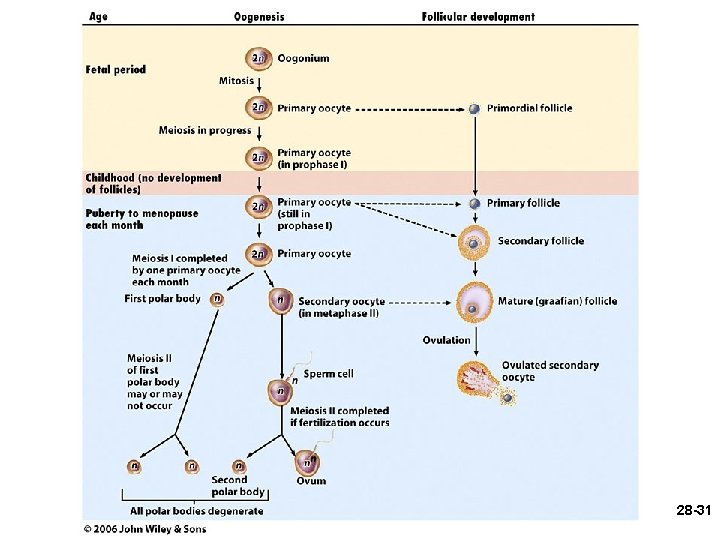
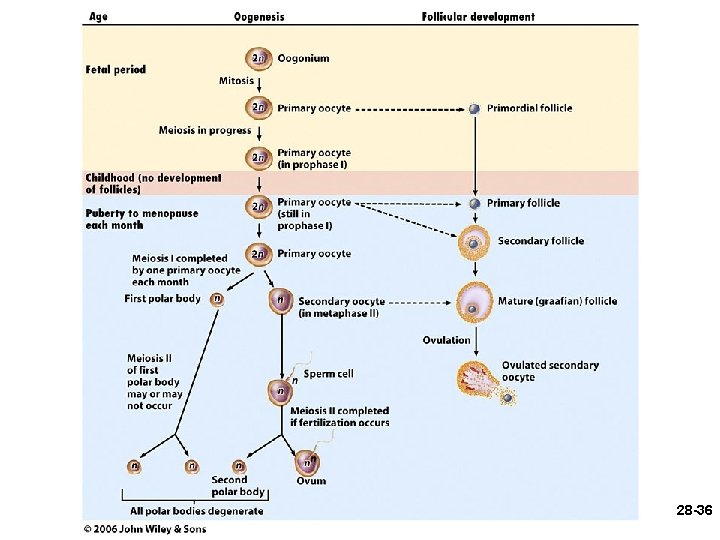
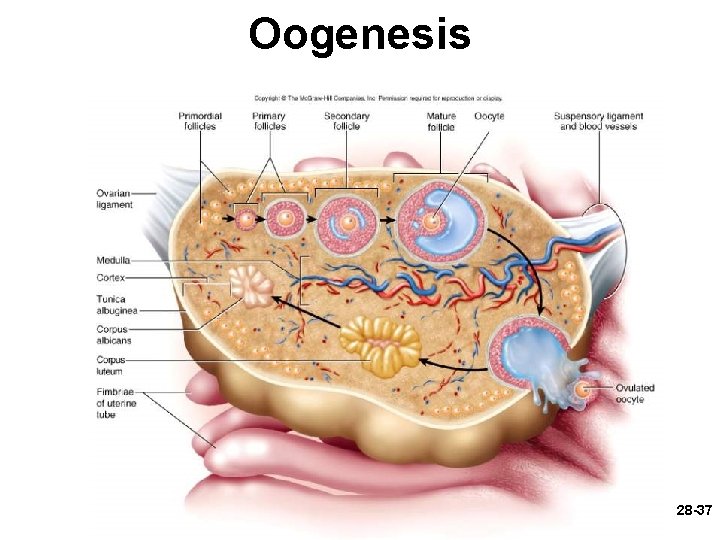
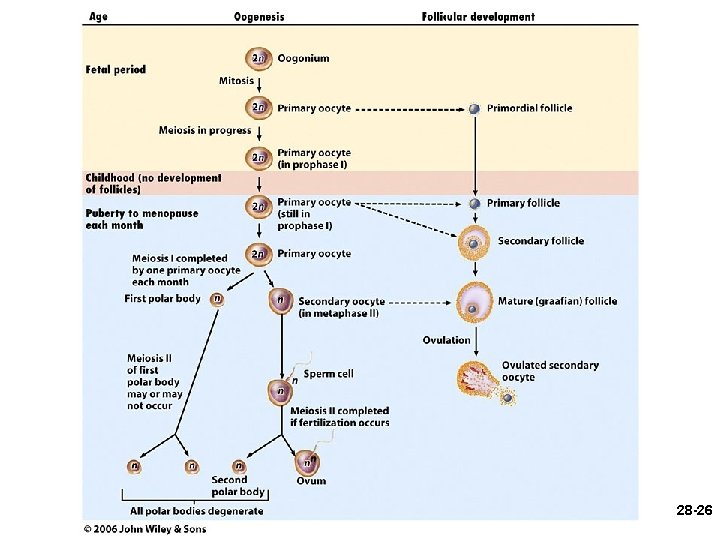
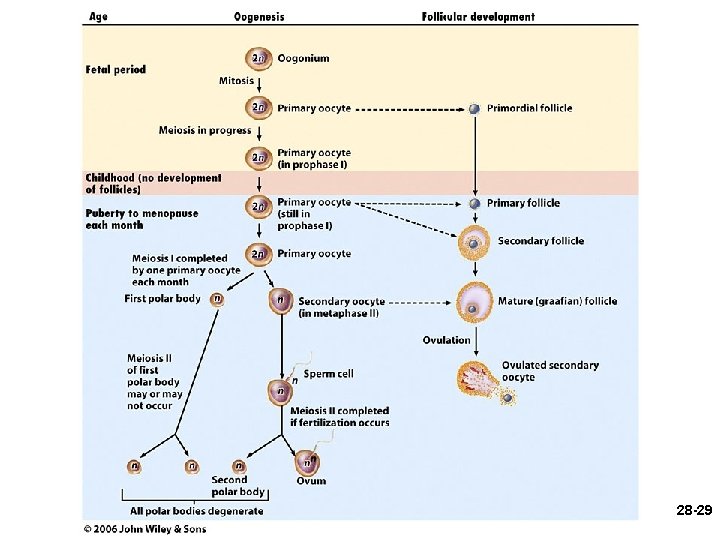
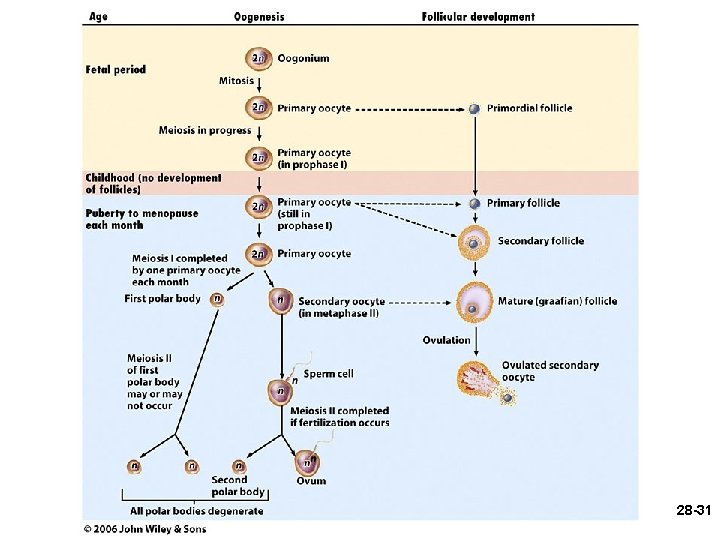
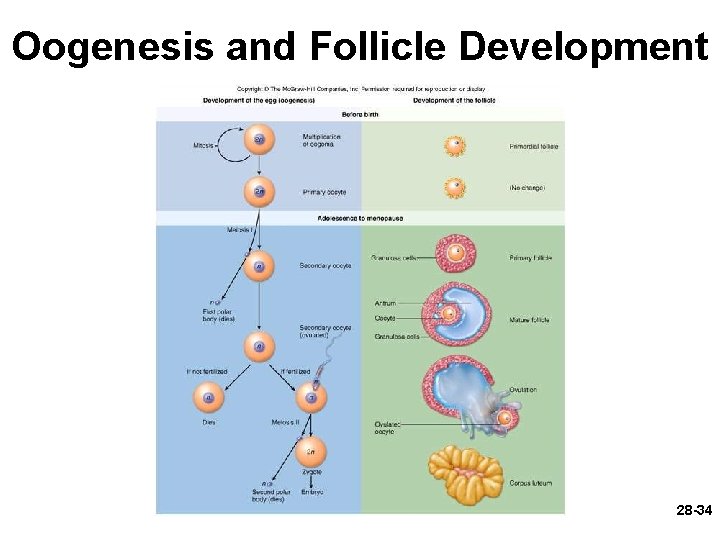
Oogenesis • Monthly event produces haploid egg by meiosis • Embryonic development of ovary – female germ cells arise from yolk sac (like male germ cells) and migrate to ovaries – at about week 5 to 6, the germ cells differentiate into oogonia and multiply – continue to divide. . . about 7 million by the fifth month – then they stop development until just before birth 28 -27
Oogenesis • Monthly event produces haploid egg by meiosis • Embryonic development of ovary – during this arrested phase of development, each primary oocyte is surrounded by a single layer of follicular cells. . . the entire structure is called a primordial follicle 28 -28
28 -29
Oogenesis • just before birth – oogonia transform into primary oocytes – complete early meiosis I • at birth – most primary oocytes degenerate (atresia) by childhood – about 2 million at the time of birth • at puberty – by puberty 40, 000 oocytes remain • ovulation every 28 days between the ages of 14 and 50 would require 480 eggs. . . there are many extra 28 -30 oocytes
28 -31
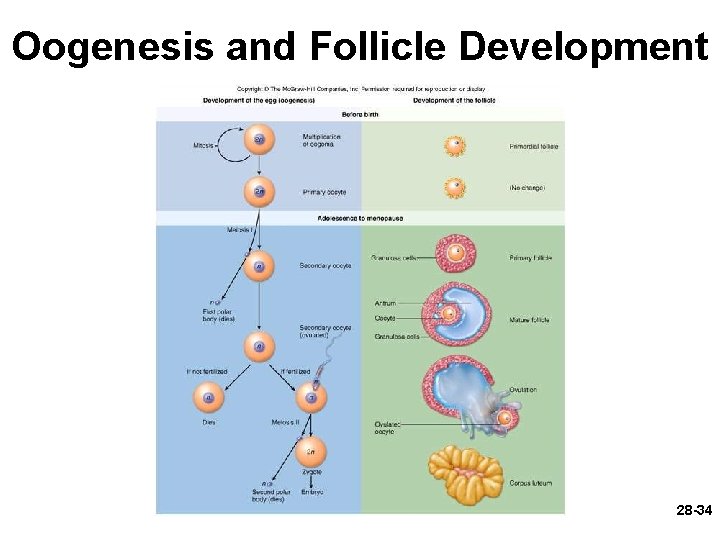
Oogenesis • beginning in adolescence, each month, FSH stimulates the development of a primordial follicle, which becomes a primary follicle • the oocyte completes meiosis I, producing a secondary oocyte and 1 st polar body 28 -32
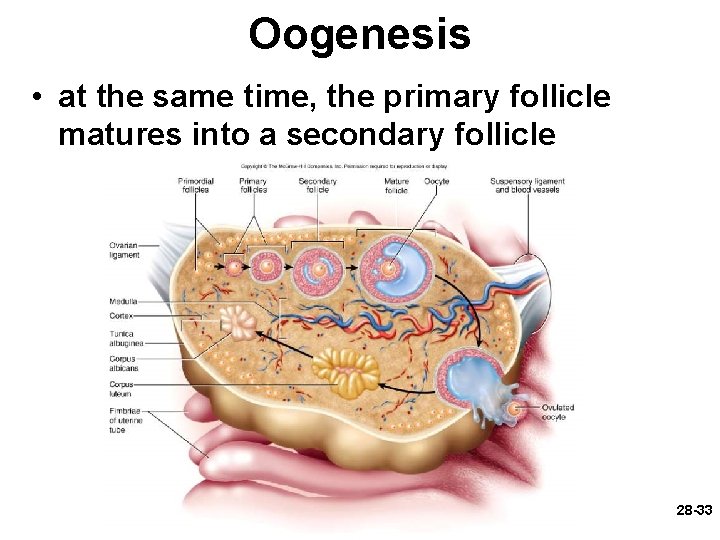
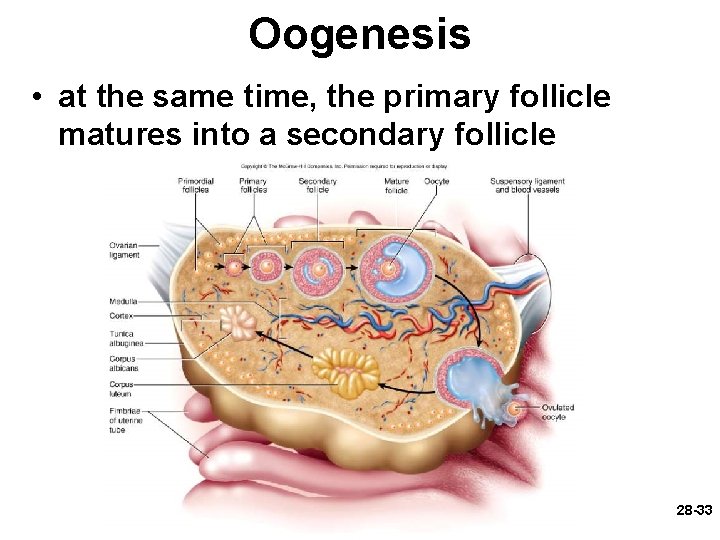
Oogenesis • at the same time, the primary follicle matures into a secondary follicle 28 -33
Oogenesis and Follicle Development 28 -34
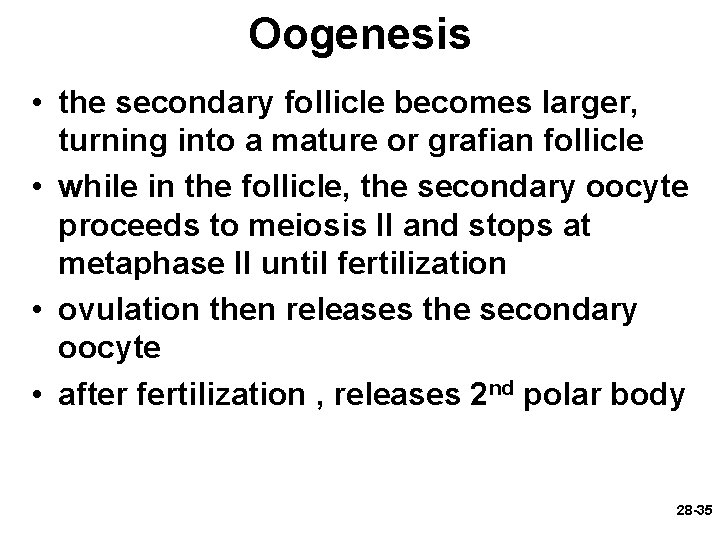
Oogenesis • the secondary follicle becomes larger, turning into a mature or grafian follicle • while in the follicle, the secondary oocyte proceeds to meiosis II and stops at metaphase II until fertilization • ovulation then releases the secondary oocyte • after fertilization , releases 2 nd polar body 28 -35
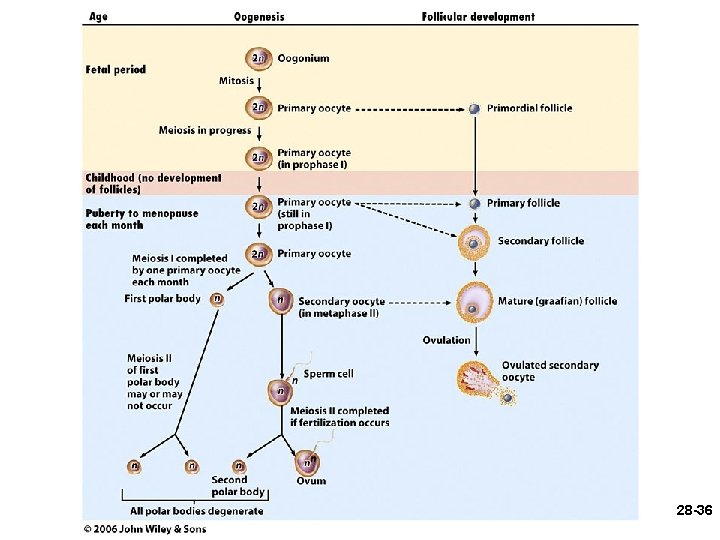
28 -36
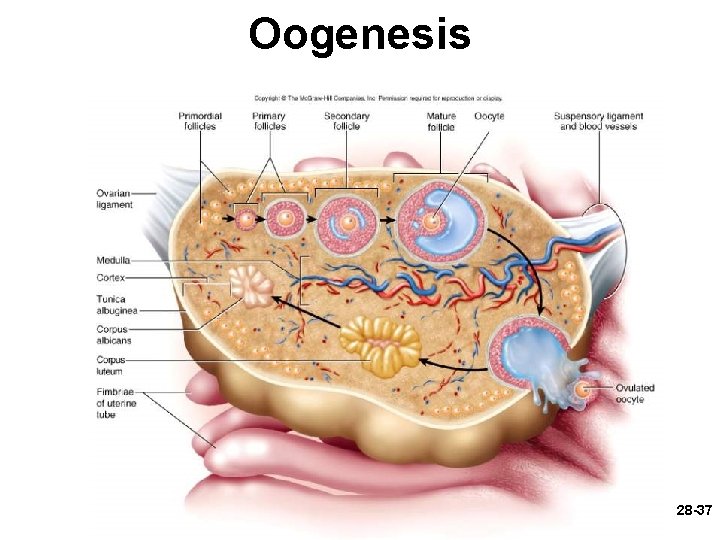
Oogenesis 28 -37
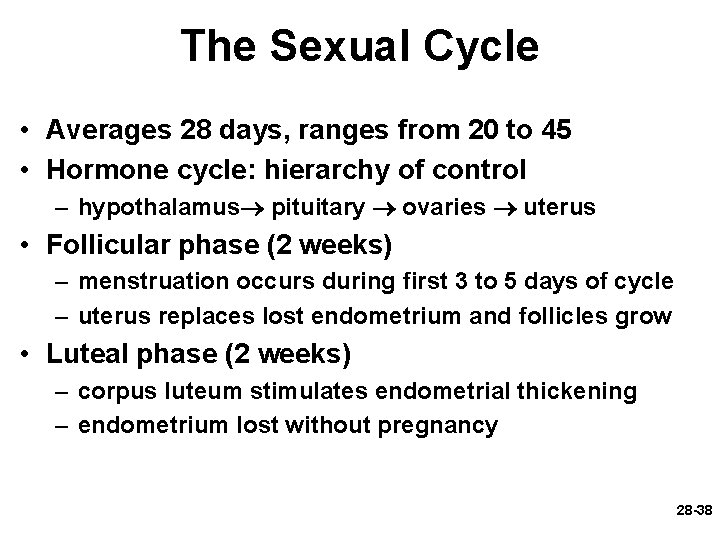
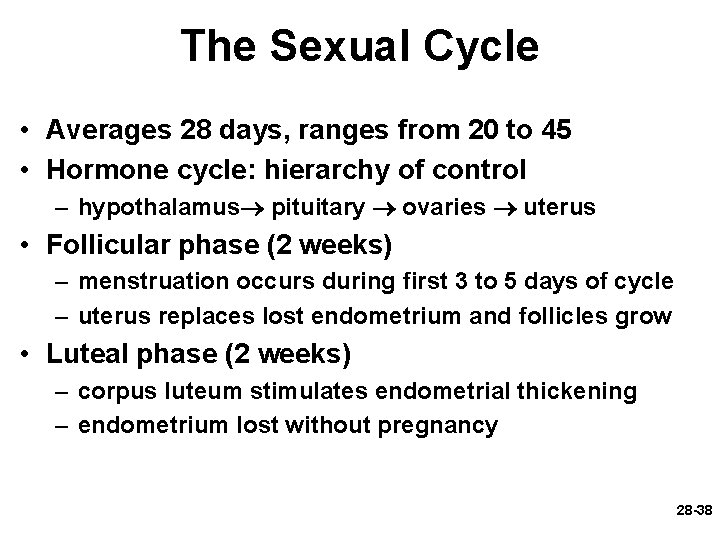
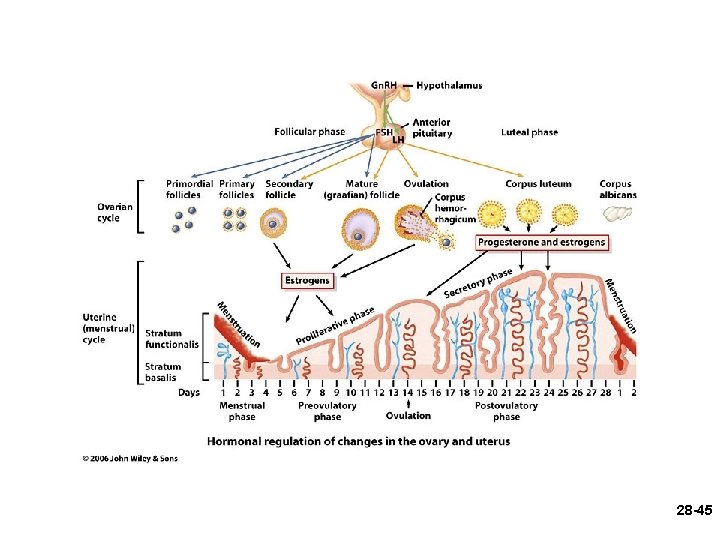
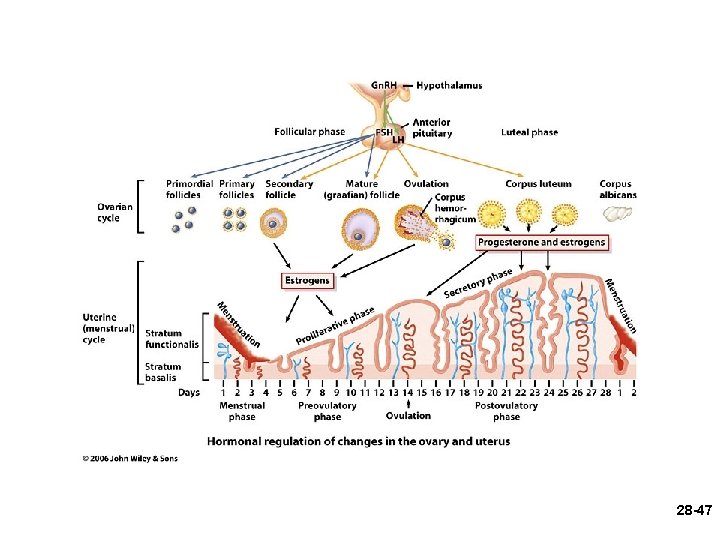
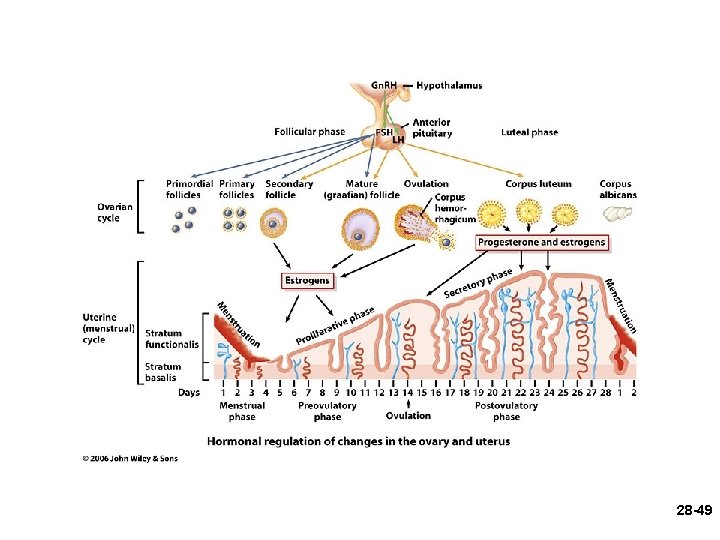
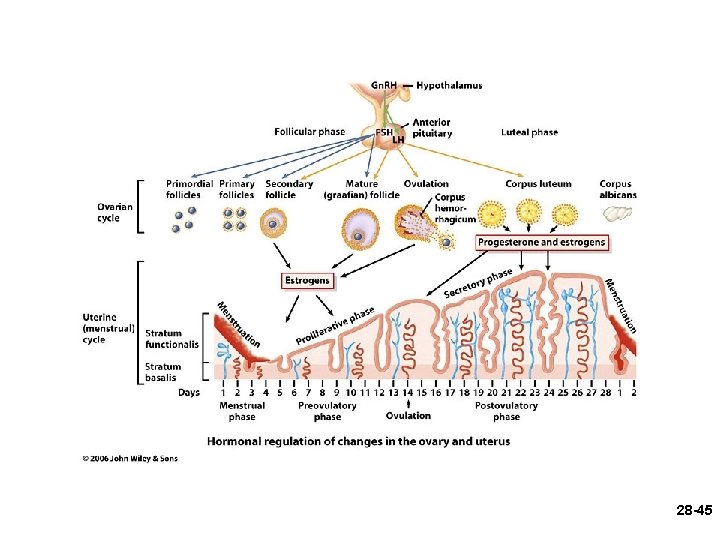
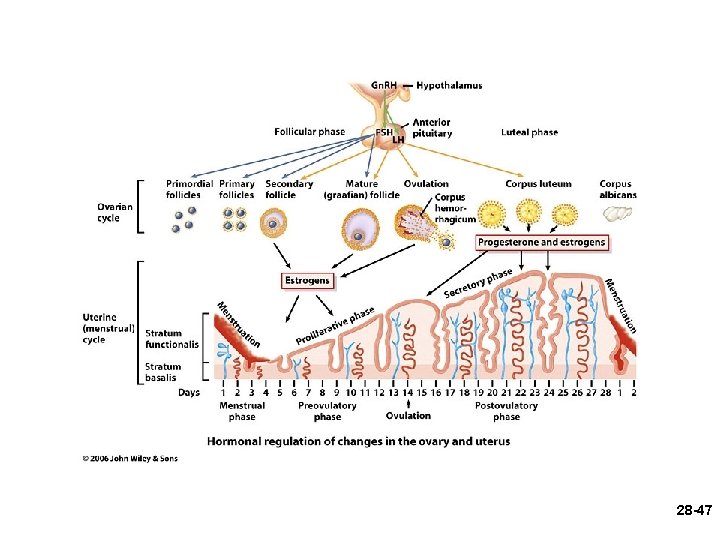
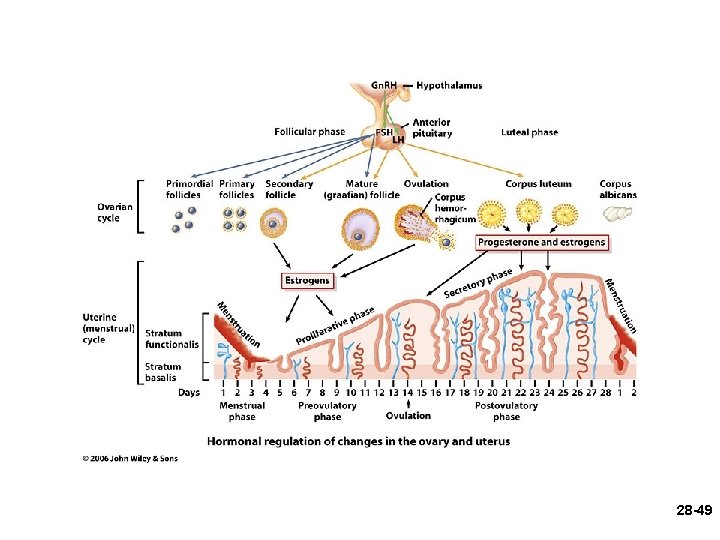
The Sexual Cycle • Averages 28 days, ranges from 20 to 45 • Hormone cycle: hierarchy of control – hypothalamus pituitary ovaries uterus • Follicular phase (2 weeks) – menstruation occurs during first 3 to 5 days of cycle – uterus replaces lost endometrium and follicles grow • Luteal phase (2 weeks) – corpus luteum stimulates endometrial thickening – endometrium lost without pregnancy 28 -38
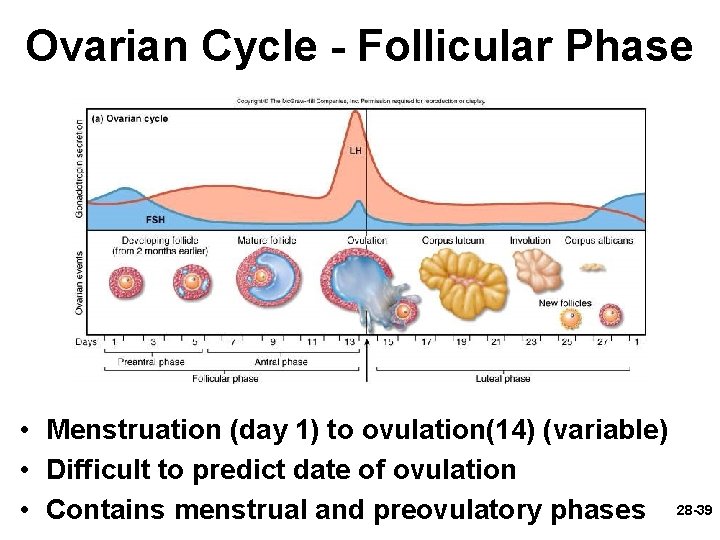
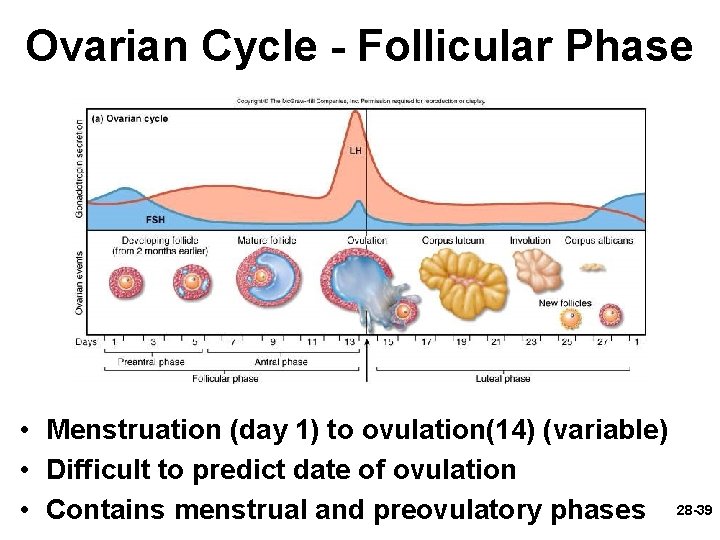
Ovarian Cycle - Follicular Phase • Menstruation (day 1) to ovulation(14) (variable) • Difficult to predict date of ovulation • Contains menstrual and preovulatory phases 28 -39
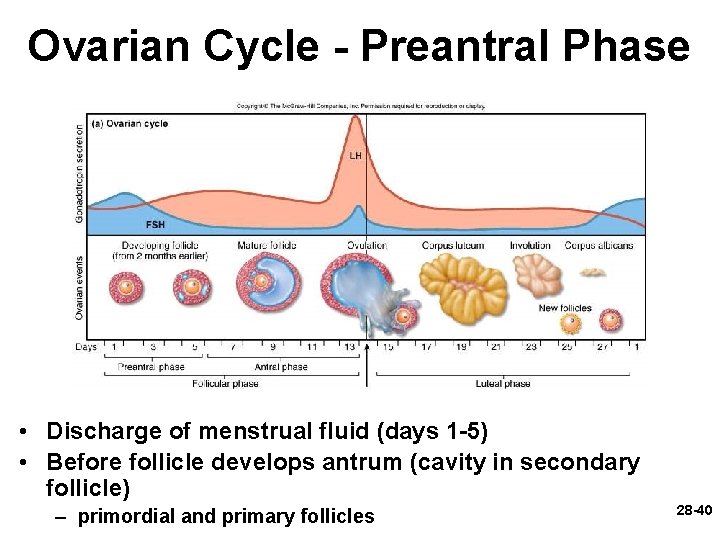
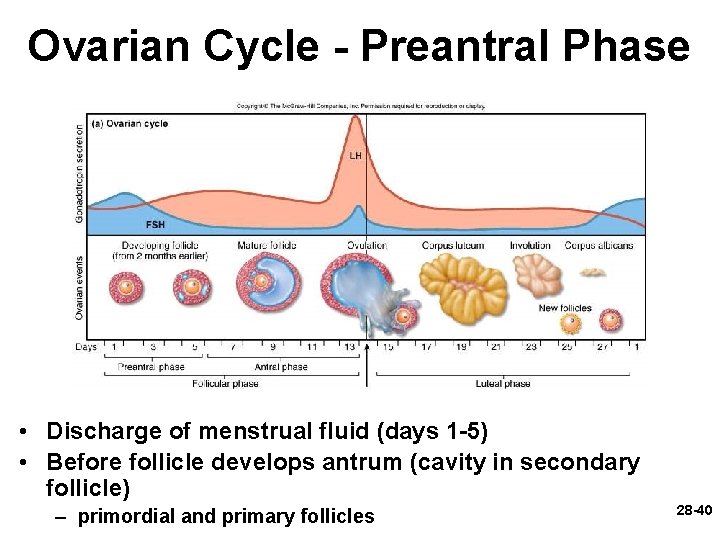
Ovarian Cycle - Preantral Phase • Discharge of menstrual fluid (days 1 -5) • Before follicle develops antrum (cavity in secondary follicle) – primordial and primary follicles 28 -40
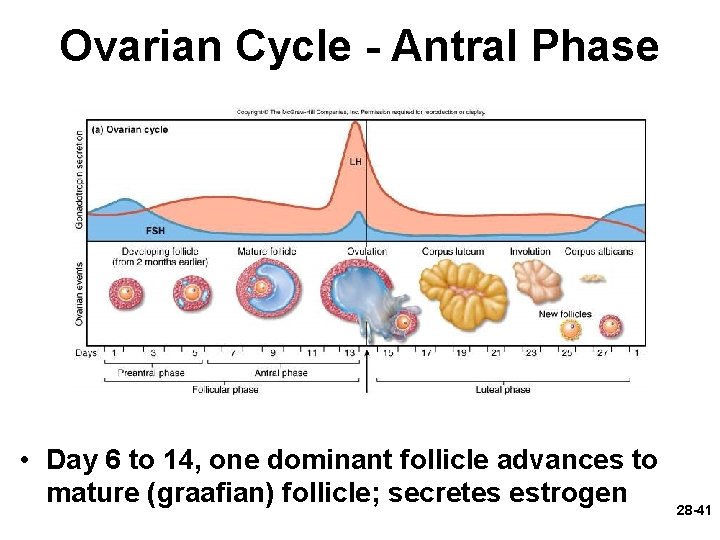
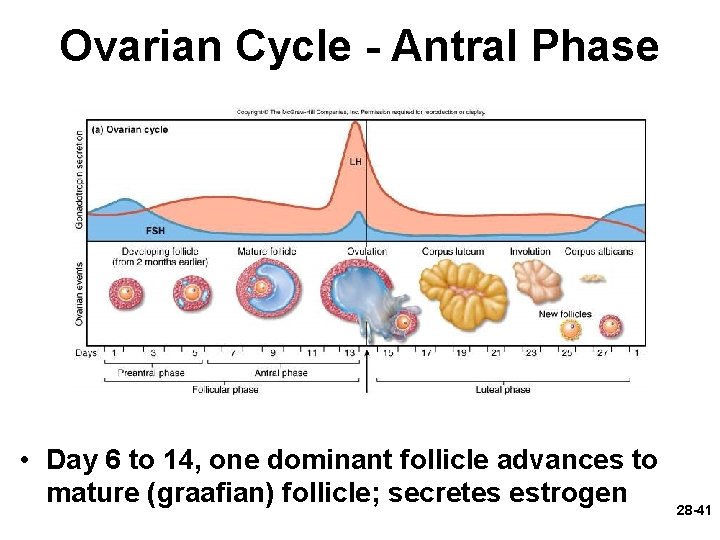
Ovarian Cycle - Antral Phase • Day 6 to 14, one dominant follicle advances to mature (graafian) follicle; secretes estrogen 28 -41
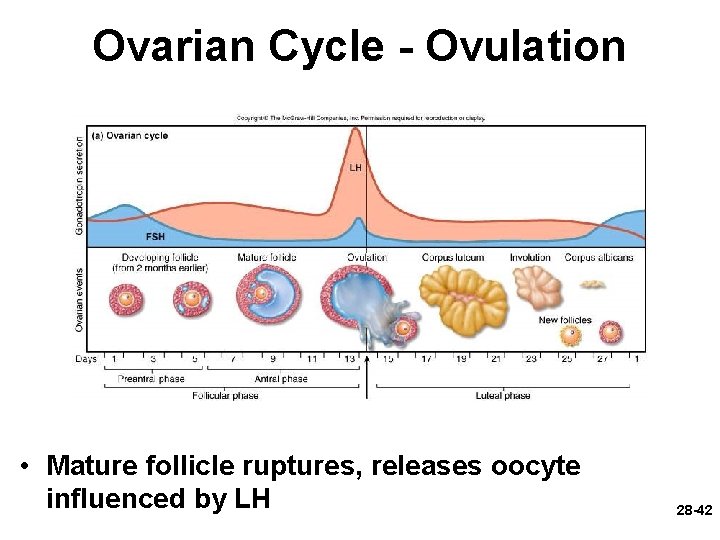
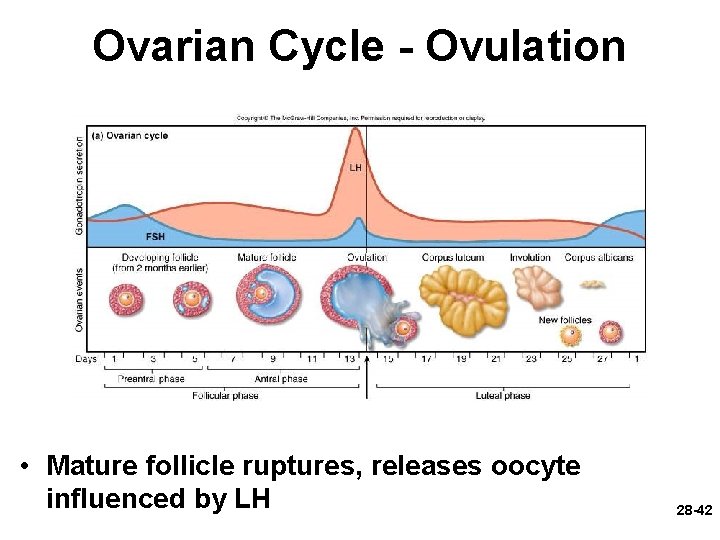
Ovarian Cycle - Ovulation • Mature follicle ruptures, releases oocyte influenced by LH 28 -42
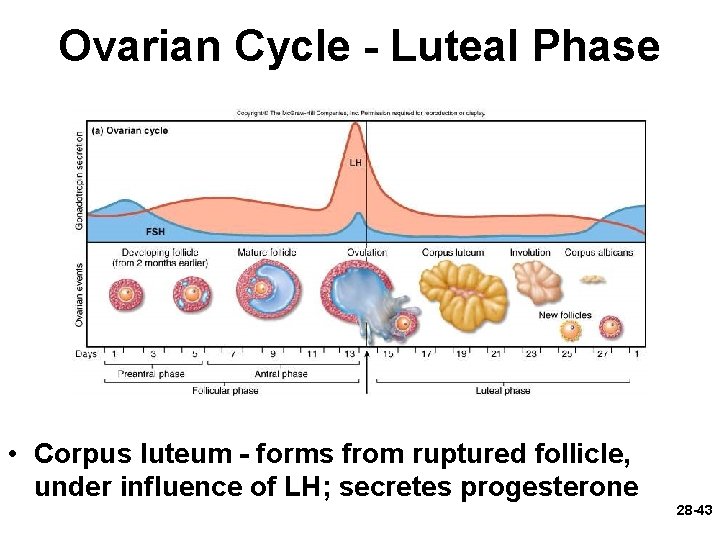
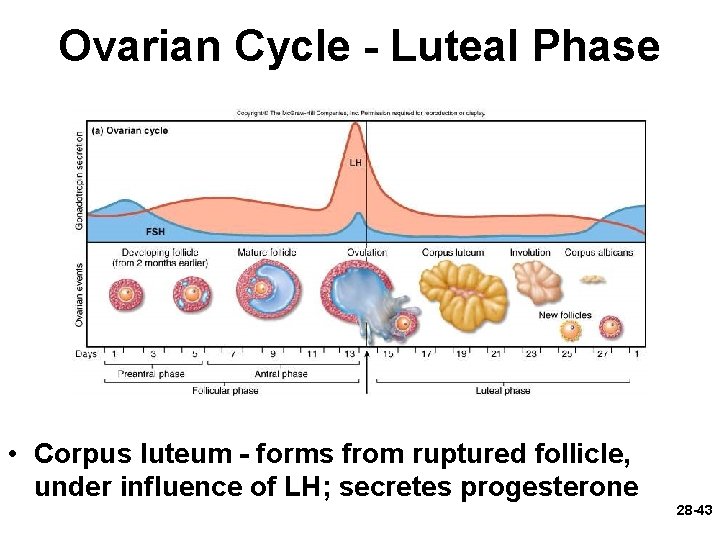
Ovarian Cycle - Luteal Phase • Corpus luteum - forms from ruptured follicle, under influence of LH; secretes progesterone 28 -43
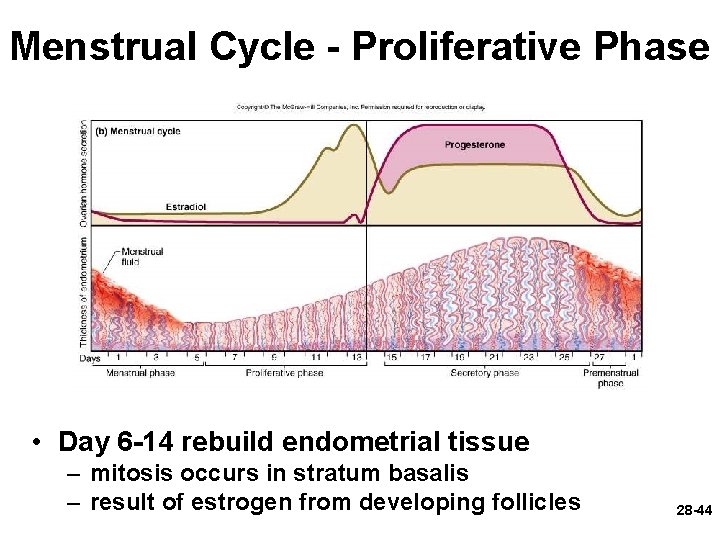
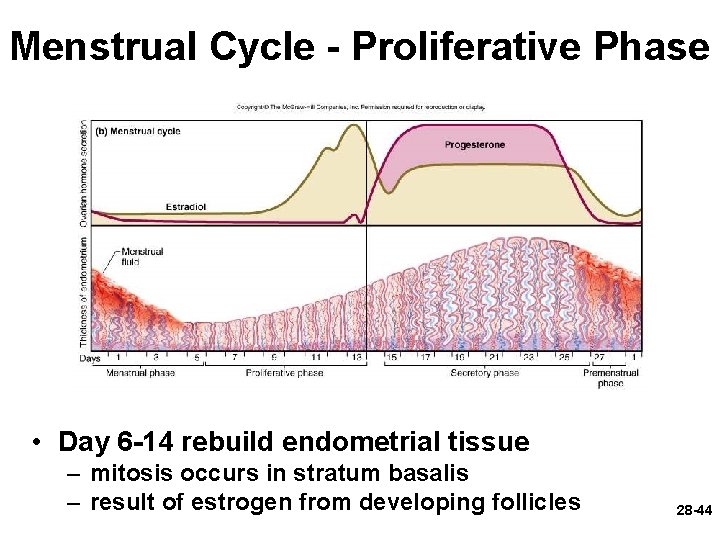
Menstrual Cycle - Proliferative Phase • Day 6 -14 rebuild endometrial tissue – mitosis occurs in stratum basalis – result of estrogen from developing follicles 28 -44
28 -45
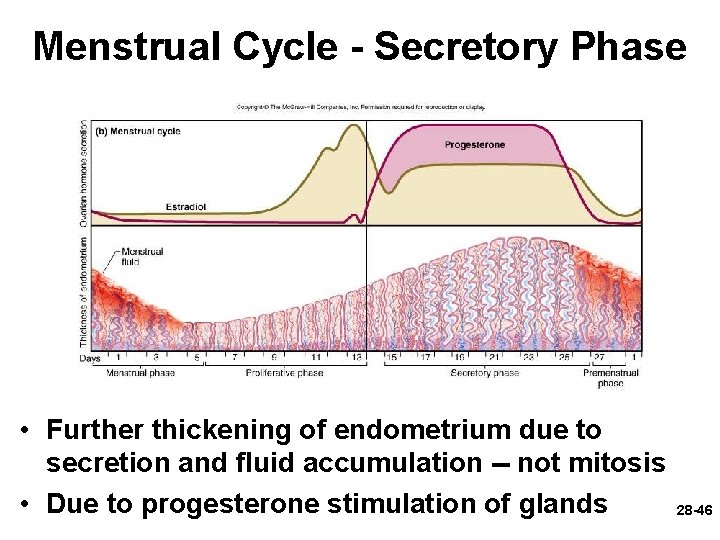
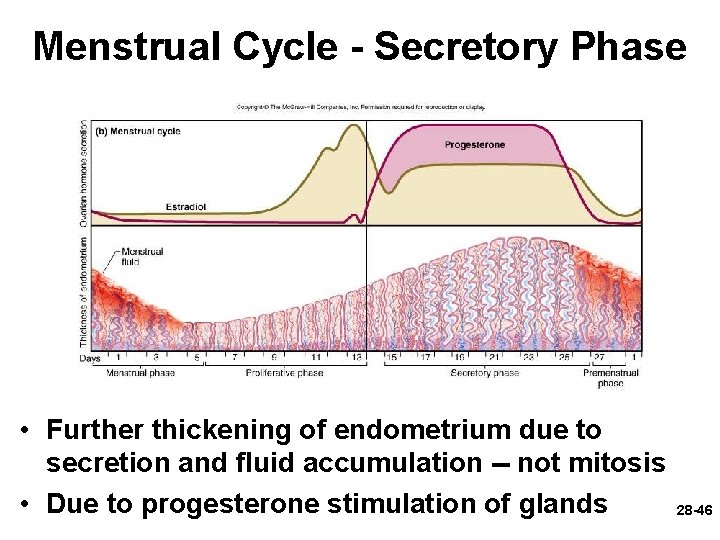
Menstrual Cycle - Secretory Phase • Further thickening of endometrium due to secretion and fluid accumulation -- not mitosis • Due to progesterone stimulation of glands 28 -46
28 -47
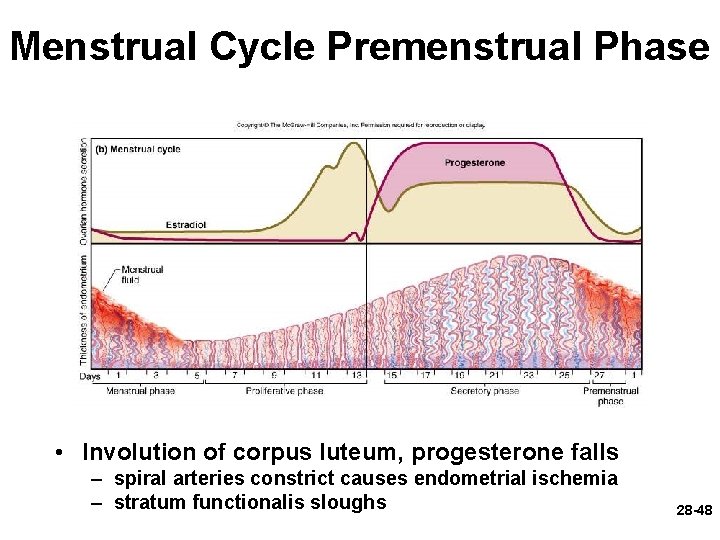
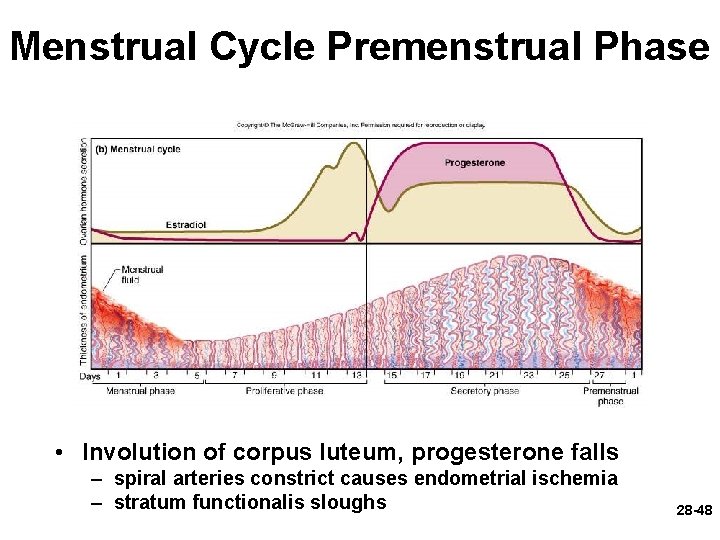
Menstrual Cycle Premenstrual Phase • Involution of corpus luteum, progesterone falls – spiral arteries constrict causes endometrial ischemia – stratum functionalis sloughs 28 -48
28 -49
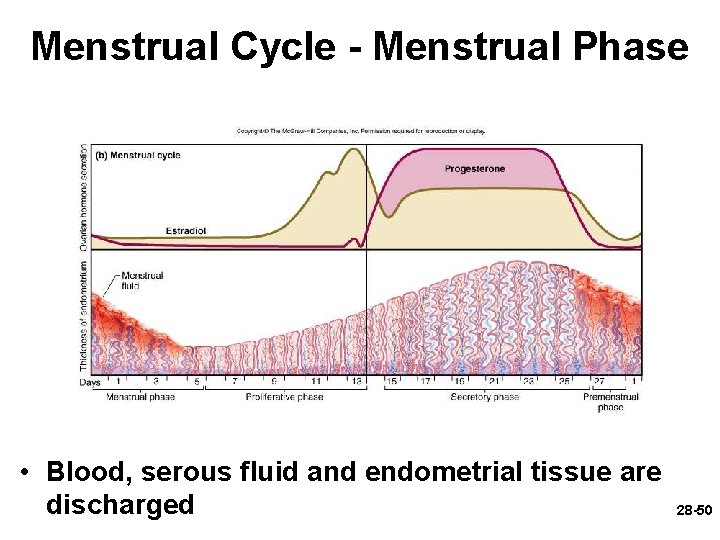
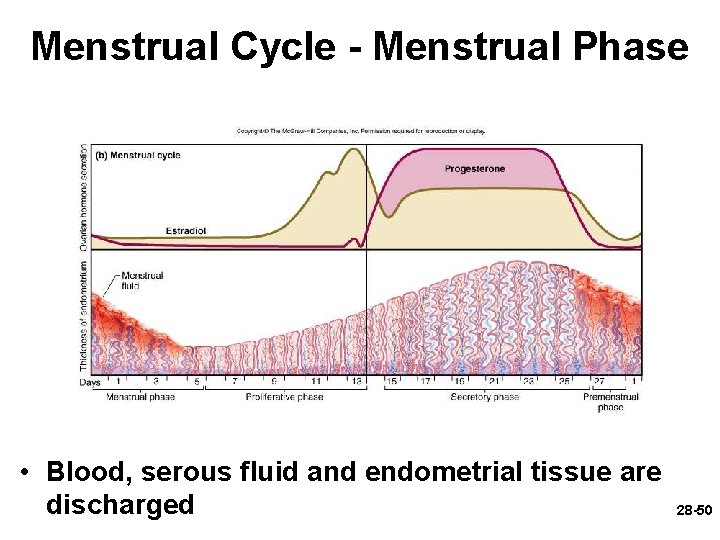
Menstrual Cycle - Menstrual Phase • Blood, serous fluid and endometrial tissue are discharged 28 -50
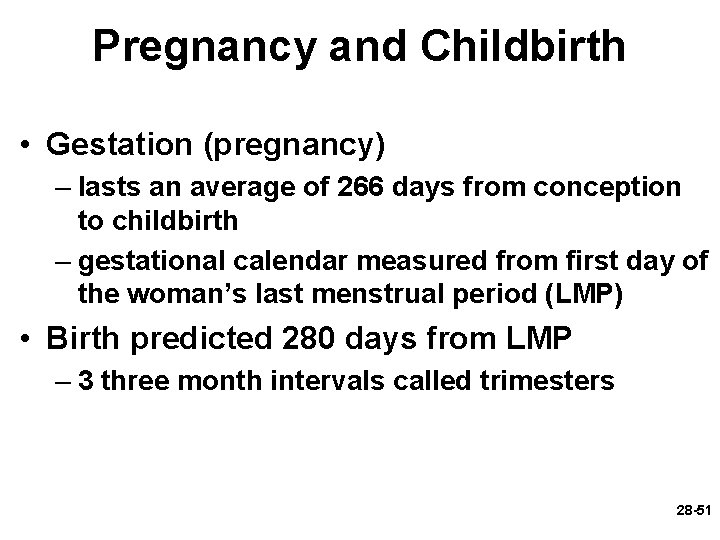
Pregnancy and Childbirth • Gestation (pregnancy) – lasts an average of 266 days from conception to childbirth – gestational calendar measured from first day of the woman’s last menstrual period (LMP) • Birth predicted 280 days from LMP – 3 three month intervals called trimesters 28 -51
Prenatal Development • Age based terminology – blastocyst is less than 2 weeks old – embryo is from 2 to 8 weeks old – fetus is 9 weeks to birth – neonate - newborn to 6 weeks 28 -52
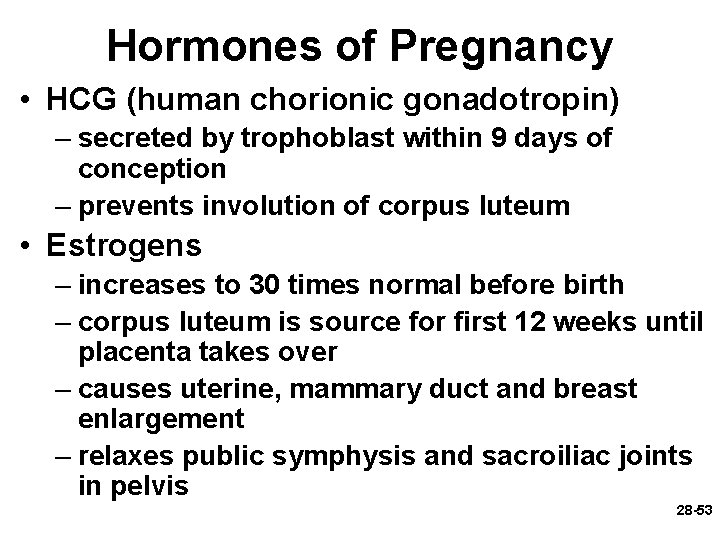
Hormones of Pregnancy • HCG (human chorionic gonadotropin) – secreted by trophoblast within 9 days of conception – prevents involution of corpus luteum • Estrogens – increases to 30 times normal before birth – corpus luteum is source for first 12 weeks until placenta takes over – causes uterine, mammary duct and breast enlargement – relaxes public symphysis and sacroiliac joints in pelvis 28 -53
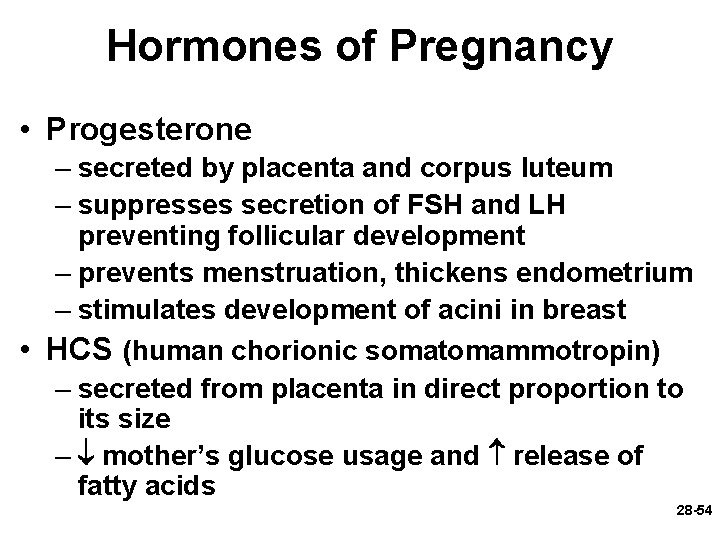
Hormones of Pregnancy • Progesterone – secreted by placenta and corpus luteum – suppresses secretion of FSH and LH preventing follicular development – prevents menstruation, thickens endometrium – stimulates development of acini in breast • HCS (human chorionic somatomammotropin) – secreted from placenta in direct proportion to its size – mother’s glucose usage and release of fatty acids 28 -54
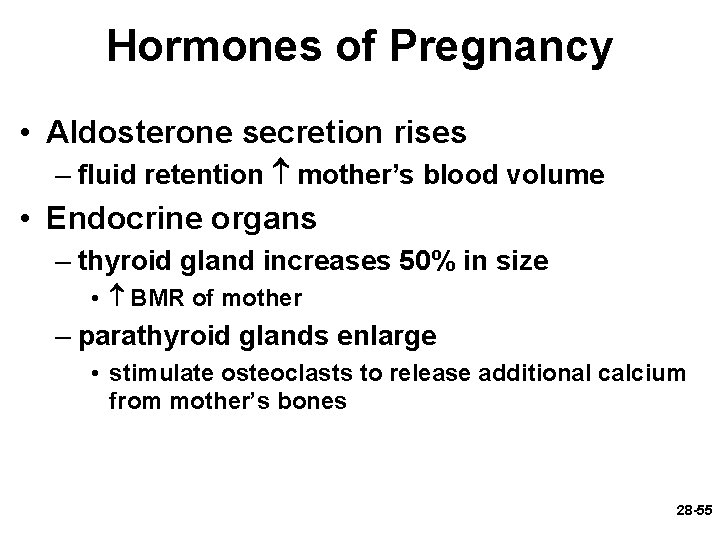
Hormones of Pregnancy • Aldosterone secretion rises – fluid retention mother’s blood volume • Endocrine organs – thyroid gland increases 50% in size • BMR of mother – parathyroid glands enlarge • stimulate osteoclasts to release additional calcium from mother’s bones 28 -55
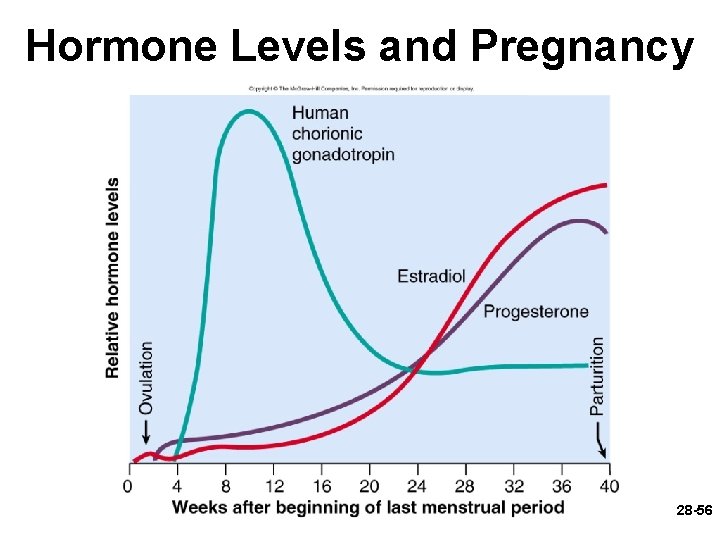
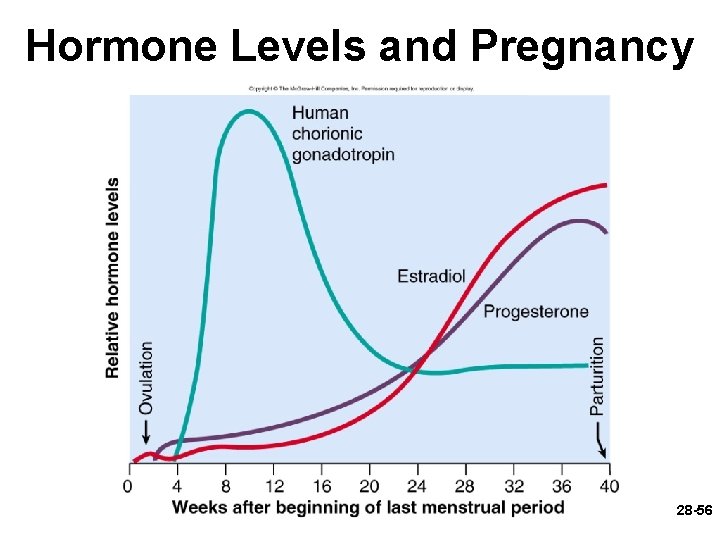
Hormone Levels and Pregnancy 28 -56
End 28 -57