Chapter 27 The Reproductive System Lecture Presentation by
Chapter 27 The Reproductive System Lecture Presentation by Steven Bassett Southeast Community College © 2015 Pearson Education, Inc.
Introduction • The reproductive system is designed to perpetuate the species • The male produces gametes called sperm cells • The female produces gametes called ova • The joining of a sperm cell and an ovum is fertilization • Fertilization results in the formation of a zygote © 2015 Pearson Education, Inc.

Organization of the Reproductive System • The reproductive system includes: • Gonads • Testes / Ovaries • Reproductive tract • Accessory glands • Perineal structures • External genitalia © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Principal structures of the male reproductive system are: • External genitalia • Scrotum • Penis © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Principal structures of the male reproductive system are (continued): • • Testis Epididymis Ductus deferens Ejaculatory duct Spongy urethra (penile urethra) Seminal gland Prostate gland Bulbo-urethral gland © 2015 Pearson Education, Inc.
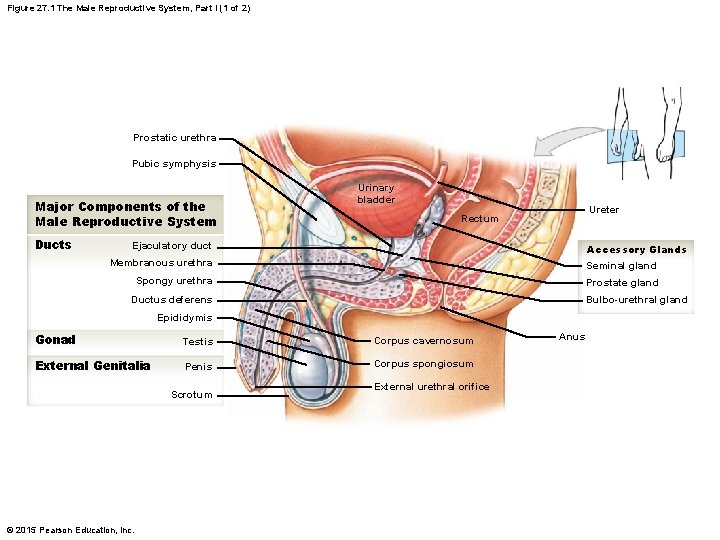
Figure 27. 1 The Male Reproductive System, Part I (1 of 2) Prostatic urethra Pubic symphysis Major Components of the Male Reproductive System Ducts Urinary bladder Ureter Rectum Ejaculatory duct Accessory Glands Membranous urethra Seminal gland Spongy urethra Prostate gland Bulbo-urethral gland Ductus deferens Epididymis Gonad Testis Corpus cavernosum External Genitalia Penis Corpus spongiosum Scrotum © 2015 Pearson Education, Inc. External urethral orifice Anus
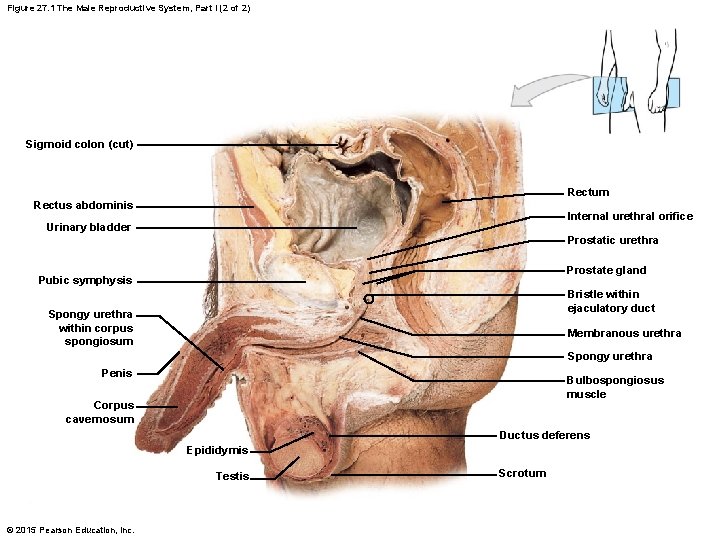
Figure 27. 1 The Male Reproductive System, Part I (2 of 2) Sigmoid colon (cut) Rectum Rectus abdominis Internal urethral orifice Urinary bladder Prostatic urethra Prostate gland Pubic symphysis Bristle within ejaculatory duct Spongy urethra within corpus spongiosum Membranous urethra Spongy urethra Penis Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Testis © 2015 Pearson Education, Inc. Scrotum
Anatomy of the Male Reproductive System • The Testes • Testes hang inside a pouch called the scrotum, which is on the outside of the body • Testicle size • • 5 cm long 3 cm wide 2. 5 cm thick 10– 15 g © 2015 Pearson Education, Inc.
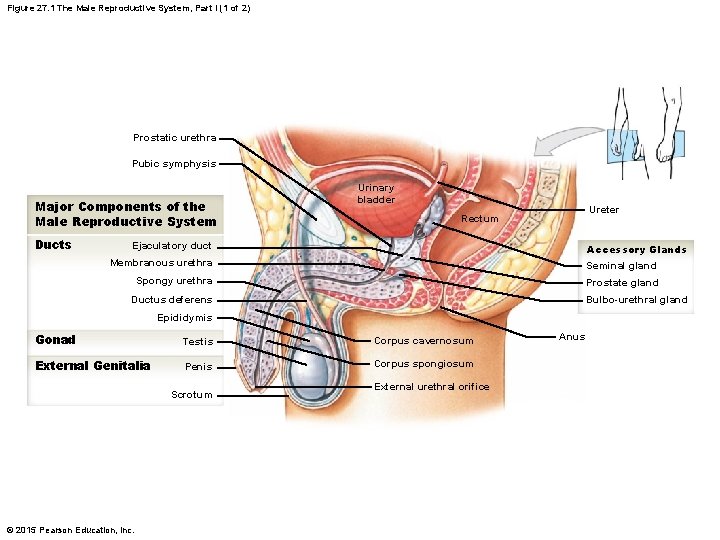
Figure 27. 1 The Male Reproductive System, Part I (1 of 2) Prostatic urethra Pubic symphysis Major Components of the Male Reproductive System Ducts Urinary bladder Ureter Rectum Ejaculatory duct Accessory Glands Membranous urethra Seminal gland Spongy urethra Prostate gland Bulbo-urethral gland Ductus deferens Epididymis Gonad Testis Corpus cavernosum External Genitalia Penis Corpus spongiosum Scrotum © 2015 Pearson Education, Inc. External urethral orifice Anus
Anatomy of the Male Reproductive System • Descent of the Testes • During development, the testes form inside the abdominal cavity near the kidneys • Testes descend toward the scrotum by passing through the inguinal canals • The ductus deferens, blood vessels, lymphatics, and nerves remain bundled to the testes in the spermatic cords © 2015 Pearson Education, Inc.

Anatomy of the Male Reproductive System • Descent of the Testes • Testicle development requires a temperature approximately 98. 6°F • Hence the development of the testicles within the abdominal cavity • Sperm development requires a temperature approximately 96. 6°F • Hence the development of sperm cells outside the abdominal cavity © 2015 Pearson Education, Inc.
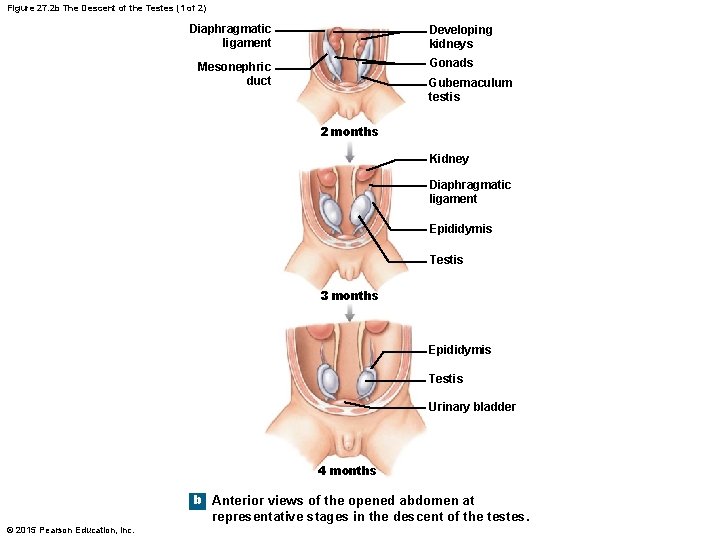
Figure 27. 2 b The Descent of the Testes (1 of 2) Diaphragmatic ligament Developing kidneys Gonads Mesonephric duct Gubernaculum testis 2 months Kidney Diaphragmatic ligament Epididymis Testis 3 months Epididymis Testis Urinary bladder 4 months b Anterior views of the opened abdomen at representative stages in the descent of the testes. © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • The Spermatic Cords • Consist of: • • Ilionguinal nerve Genitofemoral nerve Deferential artery Ductus deferens Pampiniform plexus Testicular artery Testicular vein © 2015 Pearson Education, Inc.
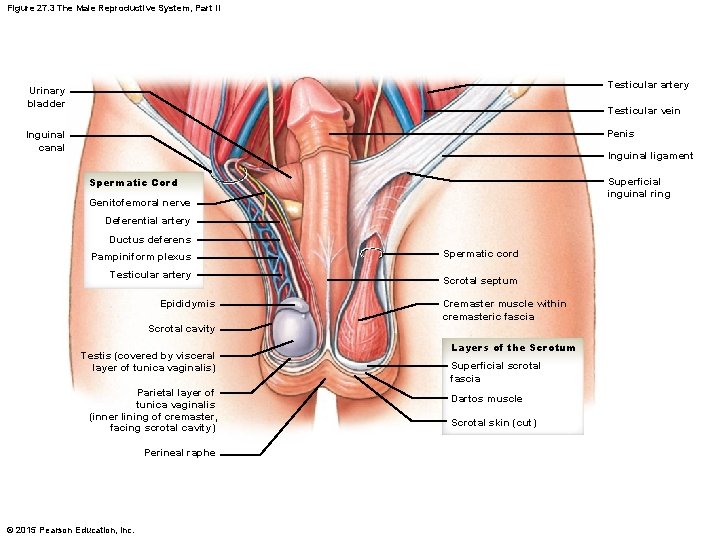
Figure 27. 3 The Male Reproductive System, Part II Testicular artery Urinary bladder Testicular vein Penis Inguinal canal Inguinal ligament Spermatic Cord Superficial inguinal ring Genitofemoral nerve Deferential artery Ductus deferens Pampiniform plexus Testicular artery Epididymis Spermatic cord Scrotal septum Cremaster muscle within cremasteric fascia Scrotal cavity Testis (covered by visceral layer of tunica vaginalis) Parietal layer of tunica vaginalis (inner lining of cremaster, facing scrotal cavity) Perineal raphe © 2015 Pearson Education, Inc. Layers of the Scrotum Superficial scrotal fascia Dartos muscle Scrotal skin (cut)
Anatomy of the Male Reproductive System • The Scrotum and the Position of the Testes • Divided into two chambers (scrotal cavities) • Chambers are separated by the perineal raphe • Can be seen as thickened tissue that extends from the anus, across the scrotum, and along the anterior surface of the penis • Tunica vaginalis • A serous membrane that covers the outside of each testis and covers the inside lining of each scrotal cavity © 2015 Pearson Education, Inc.
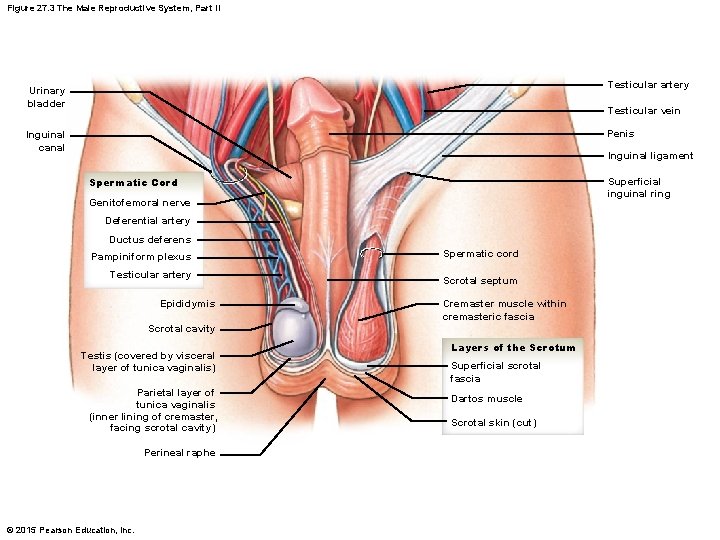
Figure 27. 3 The Male Reproductive System, Part II Testicular artery Urinary bladder Testicular vein Penis Inguinal canal Inguinal ligament Spermatic Cord Superficial inguinal ring Genitofemoral nerve Deferential artery Ductus deferens Pampiniform plexus Testicular artery Epididymis Spermatic cord Scrotal septum Cremaster muscle within cremasteric fascia Scrotal cavity Testis (covered by visceral layer of tunica vaginalis) Parietal layer of tunica vaginalis (inner lining of cremaster, facing scrotal cavity) Perineal raphe © 2015 Pearson Education, Inc. Layers of the Scrotum Superficial scrotal fascia Dartos muscle Scrotal skin (cut)
Anatomy of the Male Reproductive System • The Scrotum and the Position of the Testes (continued) • Muscles of the scrotum • Dartos muscle • Contraction causes the wrinkling of the scrotal surface • Cremaster muscle • Contraction tenses the scrotal sac and pulls it closer to the body • The temperature for sperm development is 2°F cooler than body temperature • Therefore, if the temperature is cold outside, the testes move closer to the abdomen to maintain the proper temperature © 2015 Pearson Education, Inc.
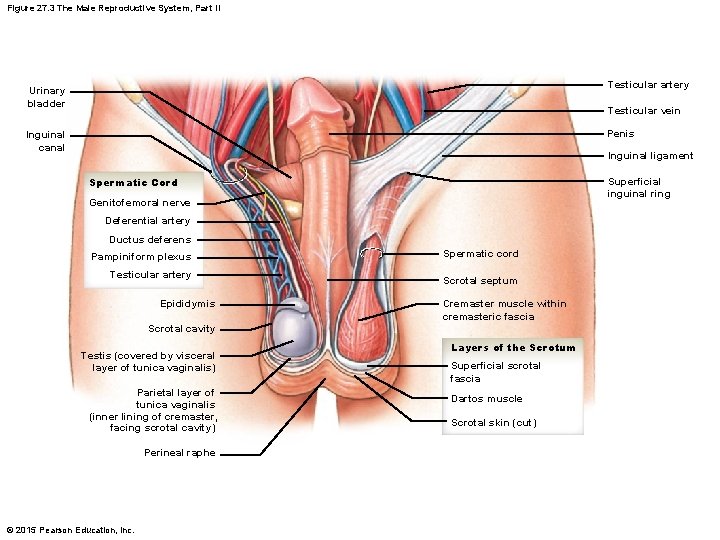
Figure 27. 3 The Male Reproductive System, Part II Testicular artery Urinary bladder Testicular vein Penis Inguinal canal Inguinal ligament Spermatic Cord Superficial inguinal ring Genitofemoral nerve Deferential artery Ductus deferens Pampiniform plexus Testicular artery Epididymis Spermatic cord Scrotal septum Cremaster muscle within cremasteric fascia Scrotal cavity Testis (covered by visceral layer of tunica vaginalis) Parietal layer of tunica vaginalis (inner lining of cremaster, facing scrotal cavity) Perineal raphe © 2015 Pearson Education, Inc. Layers of the Scrotum Superficial scrotal fascia Dartos muscle Scrotal skin (cut)
Anatomy of the Male Reproductive System • The Scrotum and the Position of the Testes (continued) • The scrotum is highly vascularized by the: • Internal pudendal arteries • A branch from the internal iliac artery • External pudendal arteries • A branch from the femoral artery • Inferior epigastric arteries • A branch from the external iliac artery © 2015 Pearson Education, Inc.

Anatomy of the Male Reproductive System • The Scrotum and the Position of the Testes (continued) • The scrotum has nerves from the: • • Hypogastric plexus Ilioinguinal nerves Genitofemoral nerves Pudendal nerves © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Structure of the Testes • Tunica albuginea • • A tough fibrous lining of the testes Extends deep into the testes and forms septa Septa converge toward the mediastinum Mediastinum supports ducts that move material toward the epididymis • Tunica vaginalis • Fibrous tissue that surrounds the tunica albuginea and is continuous with the surrounding tissue of the epididymis © 2015 Pearson Education, Inc.
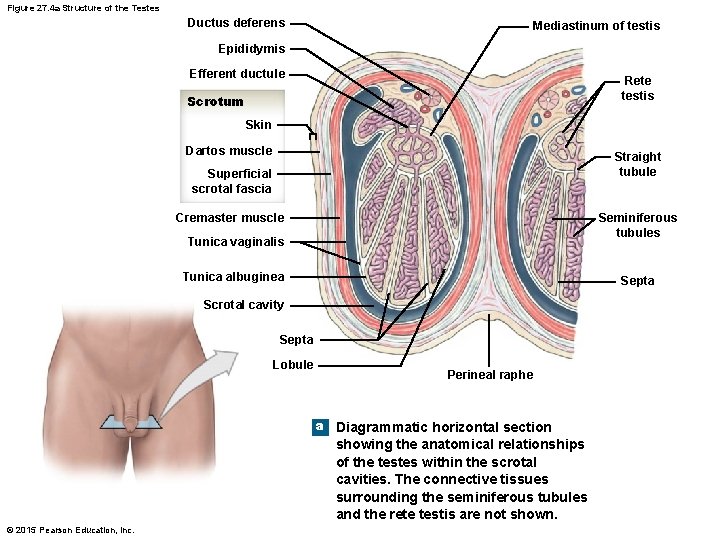
Figure 27. 4 a Structure of the Testes Ductus deferens Mediastinum of testis Epididymis Efferent ductule Rete testis Scrotum Skin Dartos muscle Straight tubule Superficial scrotal fascia Cremaster muscle Seminiferous tubules Tunica vaginalis Tunica albuginea Septa Scrotal cavity Septa Lobule Perineal raphe a Diagrammatic horizontal section showing the anatomical relationships of the testes within the scrotal cavities. The connective tissues surrounding the seminiferous tubules and the rete testis are not shown. © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Histology of the Testes • The septa of the testes separate the testes into lobules • Each lobule contains seminiferous tubules • Seminiferous tubules begin to uncoil leading to the straight tubules in the mediastinum area • The straight tubules interconnect with each other forming the rete testis • Rete testis connects to the efferent ductules • Efferent ductules lead to the epididymis © 2015 Pearson Education, Inc.
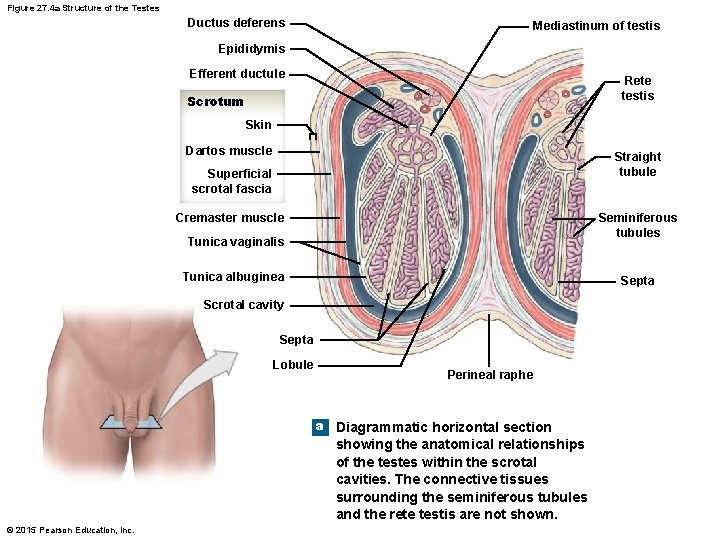
Figure 27. 4 a Structure of the Testes Ductus deferens Mediastinum of testis Epididymis Efferent ductule Rete testis Scrotum Skin Dartos muscle Straight tubule Superficial scrotal fascia Cremaster muscle Seminiferous tubules Tunica vaginalis Tunica albuginea Septa Scrotal cavity Septa Lobule Perineal raphe a Diagrammatic horizontal section showing the anatomical relationships of the testes within the scrotal cavities. The connective tissues surrounding the seminiferous tubules and the rete testis are not shown. © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Histology of the Testes (continued) • There is a space between the coils of the seminiferous tubules • The cells within this space are the interstitial cells • Interstitial cells produce and release testosterone © 2015 Pearson Education, Inc.
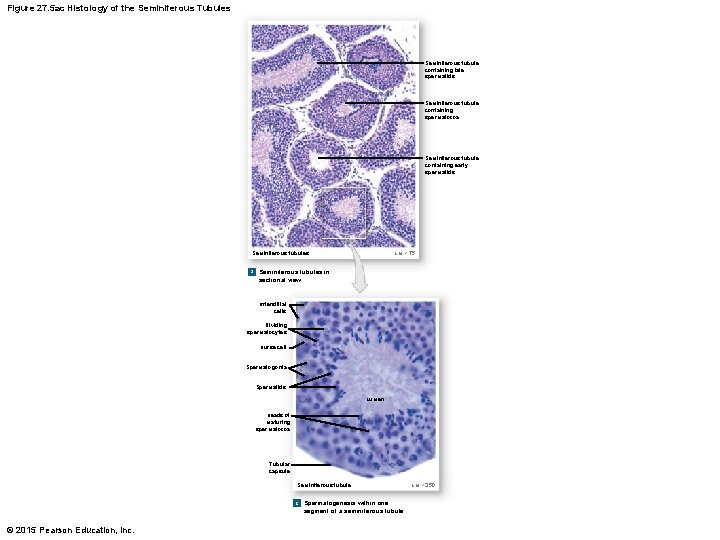
Figure 27. 5 ac Histology of the Seminiferous Tubules Seminiferous tubule containing late spermatids Seminiferous tubule containing spermatozoa Seminiferous tubule containing early spermatids LM × 75 Seminiferous tubules a Seminiferous tubules in sectional view Interstitial cells Dividing spermatocytes Nurse cell Spermatogonia Spermatids Lumen Heads of maturing spermatozoa Tubular capsule Seminiferous tubule c Spermatogenesis within one segment of a seminiferous tubule © 2015 Pearson Education, Inc. LM × 350
Anatomy of the Male Reproductive System • Histology of the Testes (continued) • Testosterone • • • Stimulates spermatogenesis Promotes sperm maturation Maintains the accessory organs Develops secondary sex characteristics Stimulates growth and development Stimulates sexual behavior and sexual drive © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Spermatogenesis and Meiosis • Spermatogenesis • Formation of sperm cells • Meiosis • Set of events involved in producing the sperm cells • Meiosis begins in the outer layer of the seminiferous tubules • Spermatogonia • Stem cells that will become sperm cells © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Spermatogenesis and Meiosis (continued) • At sexual maturation, spermatogonia divide • One of the cells produced by this division remains in the outer layer of the seminiferous tubules as a stem cell • The other cell produced by this division differentiates to become a primary spermatocyte • The primary spermatocyte begins to undergo meiosis © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Meiosis associated with the formation of sperm cells is called spermatogenesis • The primary spermatocyte undergoes division to produce two secondary spermatocytes • Each secondary spermatocyte undergoes meiosis to produce four haploid spermatids • Each spermatid matures to become a haploid sperm cell • Haploid sperm cells contain 23 chromosomes © 2015 Pearson Education, Inc.
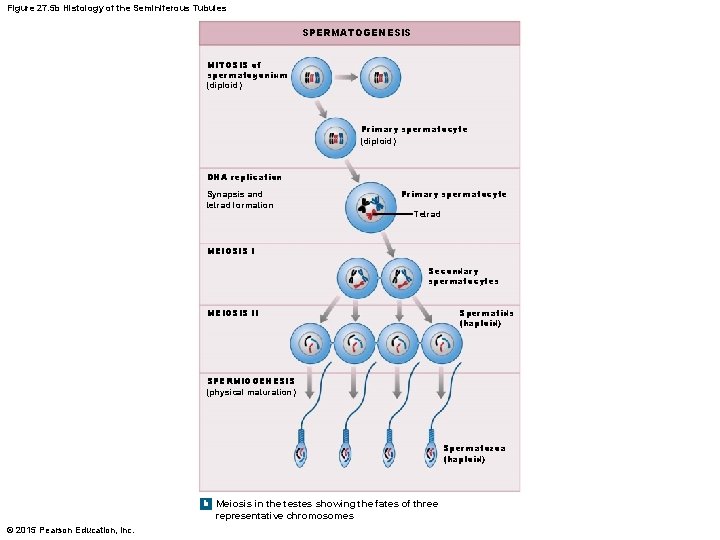
Figure 27. 5 b Histology of the Seminiferous Tubules SPERMATOGENESIS MITOSIS of spermatogonium (diploid) Primary spermatocyte (diploid) DNA replication Synapsis and tetrad formation Primary spermatocyte Tetrad MEIOSIS I Secondary spermatocytes MEIOSIS II Spermatids (haploid) SPERMIOGENESIS (physical maturation) Spermatozoa (haploid) b Meiosis in the testes showing the fates of three representative chromosomes © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Spermiogenesis • Spermatids will mature to form a spermatozoon (sperm cell) • This maturation process is called spermiogenesis • While the spermatids are maturing, they become embedded in nurse cells • Upon maturation, the spermatids (now sperm cells) enter into the lumen of the seminiferous tubules © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Nurse Cells • Function of Nurse Cells • • Maintenance of the blood–testis barrier Support of spermatogenesis Support of spermiogenesis Secretion of inhibin • Controls the rate of sperm formation • Secretion of androgen-binding protein (ABP) • Binds testosterone within the seminiferous tubules so testosterone will continue to have an effect on spermiogenesis © 2015 Pearson Education, Inc.
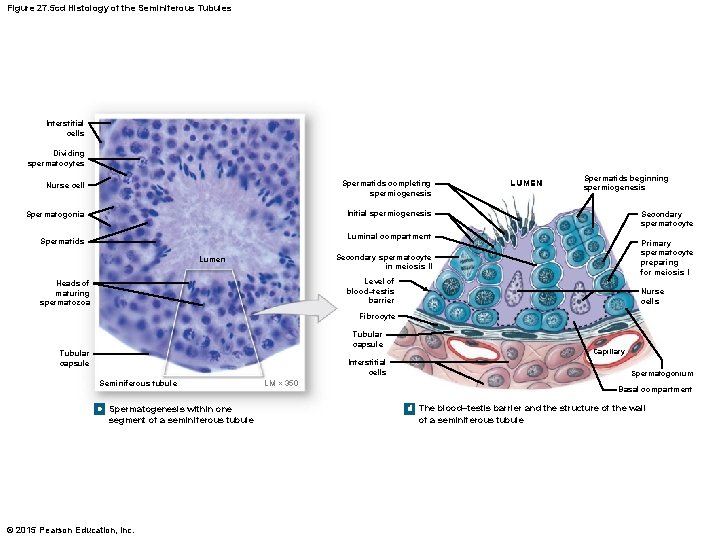
Figure 27. 5 cd Histology of the Seminiferous Tubules Interstitial cells Dividing spermatocytes Nurse cell Spermatids completing spermiogenesis Spermatogonia Initial spermiogenesis LUMEN Spermatids beginning spermiogenesis Secondary spermatocyte Luminal compartment Spermatids Primary spermatocyte preparing for meiosis I Secondary spermatocyte in meiosis II Lumen Level of blood–testis barrier Heads of maturing spermatozoa Nurse cells Fibrocyte Tubular capsule Capillary Interstitial cells Seminiferous tubule c Spermatogenesis within one segment of a seminiferous tubule © 2015 Pearson Education, Inc. Spermatogonium LM × 350 Basal compartment d The blood–testis barrier and the structure of the wall of a seminiferous tubule
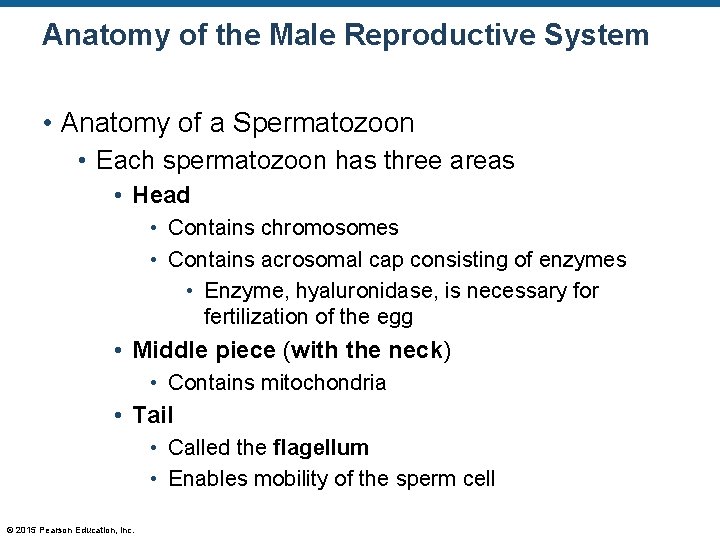
Anatomy of the Male Reproductive System • Anatomy of a Spermatozoon • Each spermatozoon has three areas • Head • Contains chromosomes • Contains acrosomal cap consisting of enzymes • Enzyme, hyaluronidase, is necessary for fertilization of the egg • Middle piece (with the neck) • Contains mitochondria • Tail • Called the flagellum • Enables mobility of the sperm cell © 2015 Pearson Education, Inc.
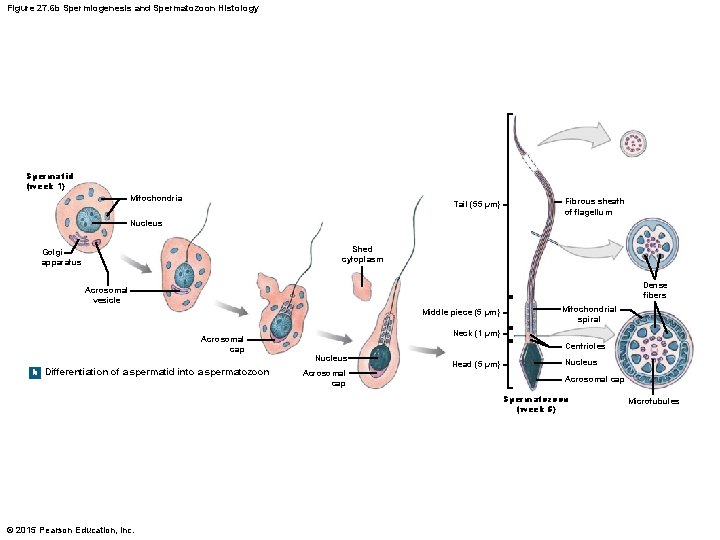
Figure 27. 6 b Spermiogenesis and Spermatozoon Histology Spermatid (week 1) Mitochondria Tail (55 µm) Fibrous sheath of flagellum Nucleus Shed cytoplasm Golgi apparatus Dense fibers Acrosomal vesicle Middle piece (5 µm) Acrosomal cap b Differentiation of a spermatid into a spermatozoon Mitochondrial spiral Neck (1 µm) Centrioles Nucleus Acrosomal cap Head (5 µm) Nucleus Acrosomal cap Spermatozoon (week 5) © 2015 Pearson Education, Inc. Microtubules
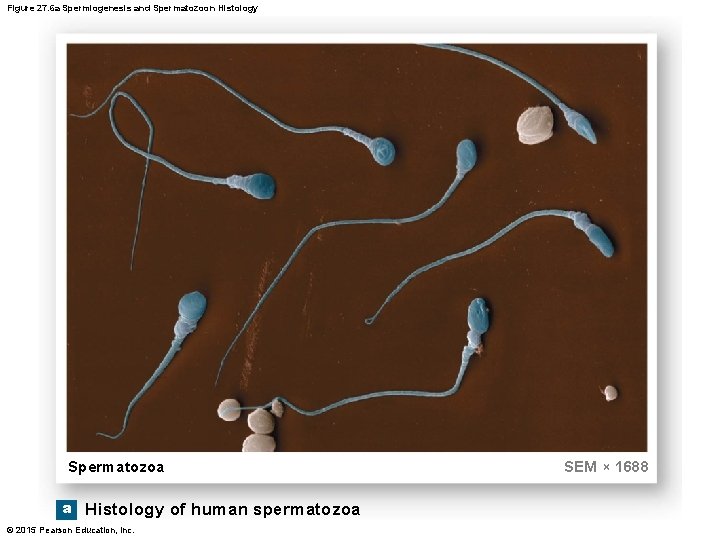
Figure 27. 6 a Spermiogenesis and Spermatozoon Histology Spermatozoa a Histology of human spermatozoa © 2015 Pearson Education, Inc. SEM × 1688
Anatomy of the Male Reproductive System • The Male Reproductive Tract • Epididymis • Ductus deferens • Urethra © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • The Epididymis • Sperm cells move from the seminiferous tubules (via fluid movement) eventually to the epididymis to mature a little longer • The epididymis consists of three parts • Head • Receives spermatozoa via the efferent ducts • Body • Coiled tubes pass through the body • Tail • Tubes begin to uncoil to become a single tube called the ductus deferens © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Functions of the Epididymis • Monitors the composition of the fluid in the seminiferous tubules • Recycling center for damaged spermatozoa • Stores spermatozoa for further maturation (about two weeks) • Mature sperm cells are not active until they become capacitated © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Functions of the Epididymis (continued) • The process of capacitation • Sperm cells become motile when mixed with secretions from the seminal glands • Become capable of fertilizing an egg when exposed to the female reproductive tract © 2015 Pearson Education, Inc.
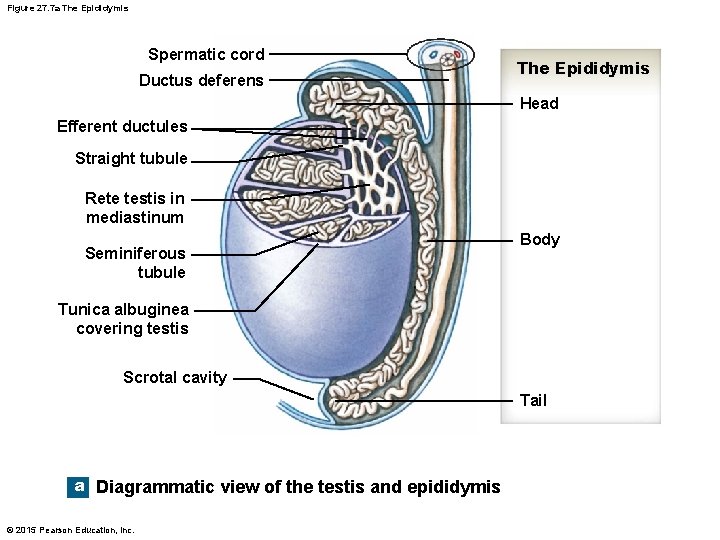
Figure 27. 7 a The Epididymis Spermatic cord Ductus deferens The Epididymis Head Efferent ductules Straight tubule Rete testis in mediastinum Seminiferous tubule Body Tunica albuginea covering testis Scrotal cavity Tail a Diagrammatic view of the testis and epididymis © 2015 Pearson Education, Inc.
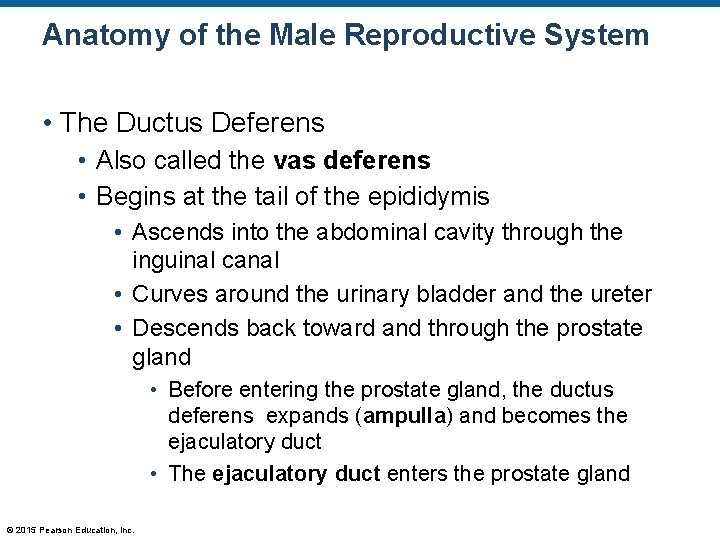
Anatomy of the Male Reproductive System • The Ductus Deferens • Also called the vas deferens • Begins at the tail of the epididymis • Ascends into the abdominal cavity through the inguinal canal • Curves around the urinary bladder and the ureter • Descends back toward and through the prostate gland • Before entering the prostate gland, the ductus deferens expands (ampulla) and becomes the ejaculatory duct • The ejaculatory duct enters the prostate gland © 2015 Pearson Education, Inc.
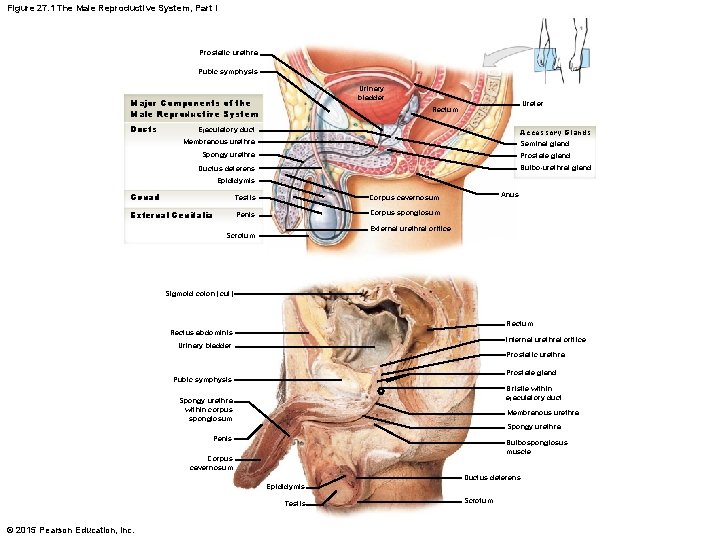
Figure 27. 1 The Male Reproductive System, Part I Prostatic urethra Pubic symphysis Urinary bladder Major Components of the Male Reproductive System Ducts Ureter Rectum Ejaculatory duct Accessory Glands Seminal gland Membranous urethra Spongy urethra Prostate gland Bulbo-urethral gland Ductus deferens Epididymis Gonad Testis Corpus cavernosum External Genitalia Penis Corpus spongiosum Anus External urethral orifice Scrotum Sigmoid colon (cut) Rectum Rectus abdominis Internal urethral orifice Urinary bladder Prostatic urethra Prostate gland Pubic symphysis Bristle within ejaculatory duct Spongy urethra within corpus spongiosum Membranous urethra Spongy urethra Penis Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Testis © 2015 Pearson Education, Inc. Scrotum
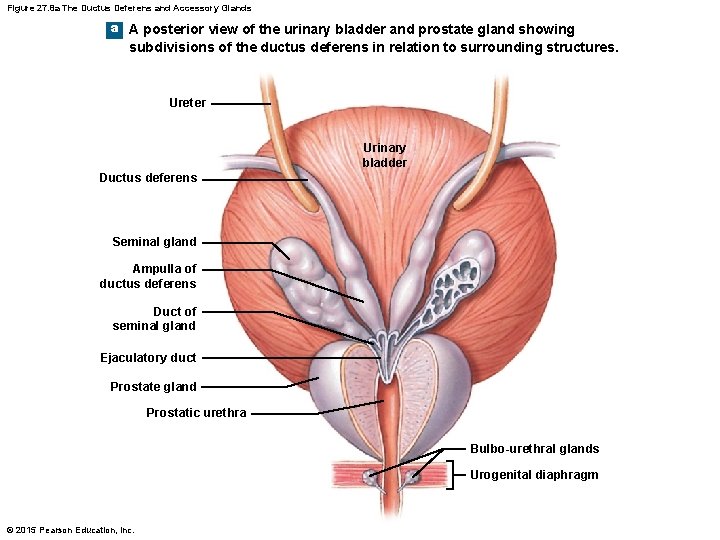
Figure 27. 8 a The Ductus Deferens and Accessory Glands a A posterior view of the urinary bladder and prostate gland showing subdivisions of the ductus deferens in relation to surrounding structures. Ureter Urinary bladder Ductus deferens Seminal gland Ampulla of ductus deferens Duct of seminal gland Ejaculatory duct Prostate gland Prostatic urethra Bulbo-urethral glands Urogenital diaphragm © 2015 Pearson Education, Inc.
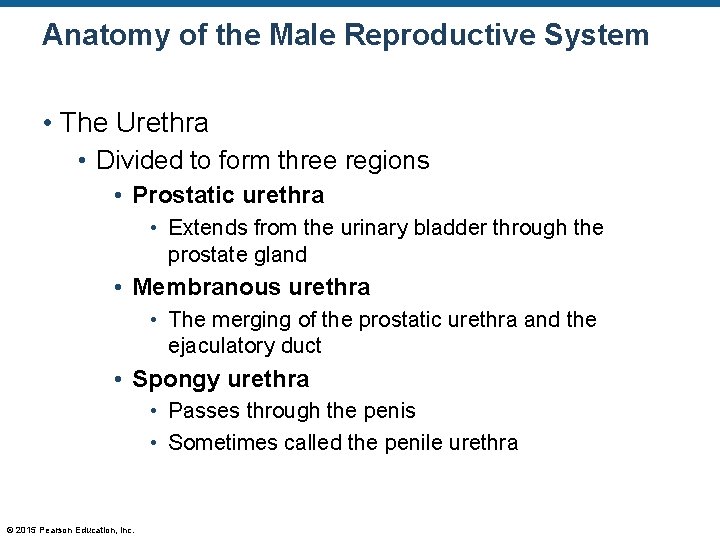
Anatomy of the Male Reproductive System • The Urethra • Divided to form three regions • Prostatic urethra • Extends from the urinary bladder through the prostate gland • Membranous urethra • The merging of the prostatic urethra and the ejaculatory duct • Spongy urethra • Passes through the penis • Sometimes called the penile urethra © 2015 Pearson Education, Inc.
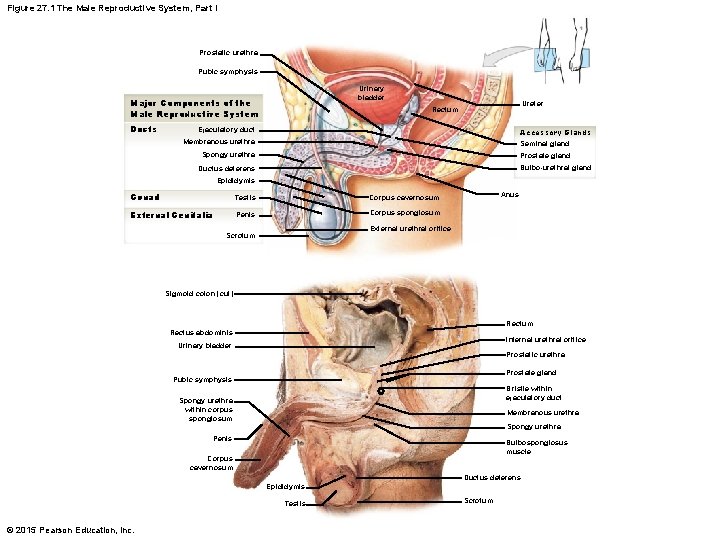
Figure 27. 1 The Male Reproductive System, Part I Prostatic urethra Pubic symphysis Urinary bladder Major Components of the Male Reproductive System Ducts Ureter Rectum Ejaculatory duct Accessory Glands Seminal gland Membranous urethra Spongy urethra Prostate gland Bulbo-urethral gland Ductus deferens Epididymis Gonad Testis Corpus cavernosum External Genitalia Penis Corpus spongiosum Anus External urethral orifice Scrotum Sigmoid colon (cut) Rectum Rectus abdominis Internal urethral orifice Urinary bladder Prostatic urethra Prostate gland Pubic symphysis Bristle within ejaculatory duct Spongy urethra within corpus spongiosum Membranous urethra Spongy urethra Penis Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Testis © 2015 Pearson Education, Inc. Scrotum
Anatomy of the Male Reproductive System • The Accessory Glands • There are three glands associated with the male reproductive system • Seminal glands (or seminal vesicles) • Prostate gland • Bulbo-urethral glands (or Cowper’s glands) © 2015 Pearson Education, Inc.
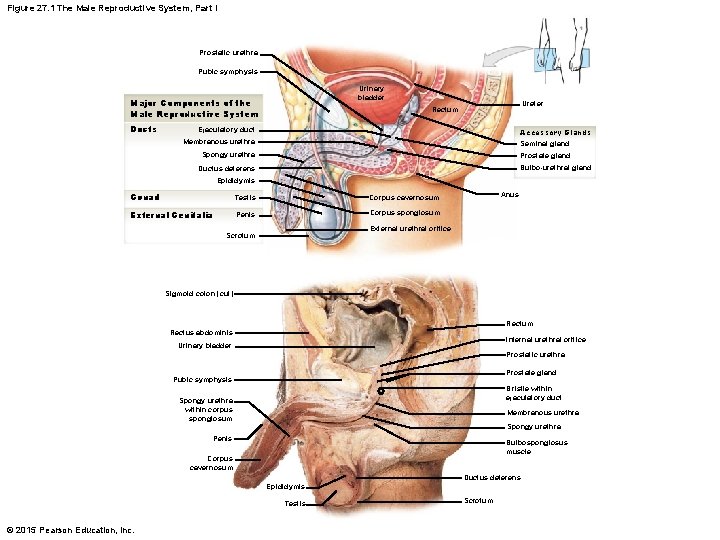
Figure 27. 1 The Male Reproductive System, Part I Prostatic urethra Pubic symphysis Urinary bladder Major Components of the Male Reproductive System Ducts Ureter Rectum Ejaculatory duct Accessory Glands Seminal gland Membranous urethra Spongy urethra Prostate gland Bulbo-urethral gland Ductus deferens Epididymis Gonad Testis Corpus cavernosum External Genitalia Penis Corpus spongiosum Anus External urethral orifice Scrotum Sigmoid colon (cut) Rectum Rectus abdominis Internal urethral orifice Urinary bladder Prostatic urethra Prostate gland Pubic symphysis Bristle within ejaculatory duct Spongy urethra within corpus spongiosum Membranous urethra Spongy urethra Penis Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Testis © 2015 Pearson Education, Inc. Scrotum
Anatomy of the Male Reproductive System • The Accessory Glands (continued) • The seminal glands • Produce 60 percent of the semen volume • Seminal fluid consists of • A high concentration of fructose • Prostaglandins • Clotting factors • Contents empty into the ductus deferens © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • The Accessory Glands (continued) • The prostate gland • • Contents empty into the prostatic urethra Produces 20– 30 percent of the semen volume Weakly acidic Secretions consist of seminalplasmin • This is an antibiotic believed to prevent UTIs in males © 2015 Pearson Education, Inc.
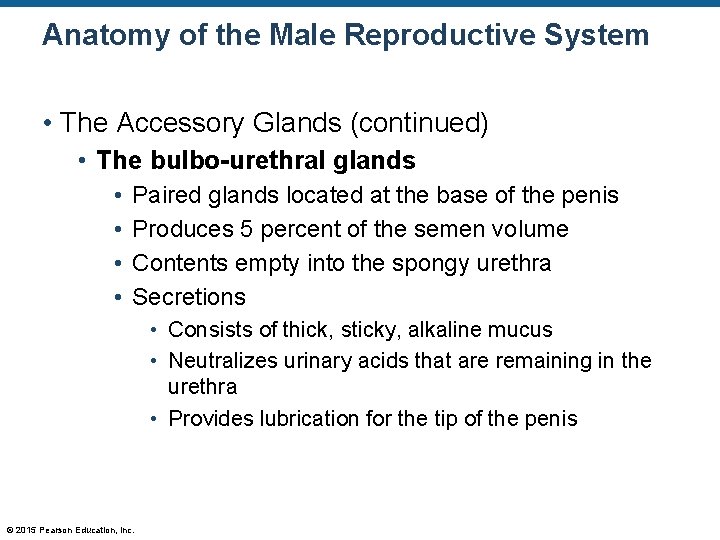
Anatomy of the Male Reproductive System • The Accessory Glands (continued) • The bulbo-urethral glands • • Paired glands located at the base of the penis Produces 5 percent of the semen volume Contents empty into the spongy urethra Secretions • Consists of thick, sticky, alkaline mucus • Neutralizes urinary acids that are remaining in the urethra • Provides lubrication for the tip of the penis © 2015 Pearson Education, Inc.
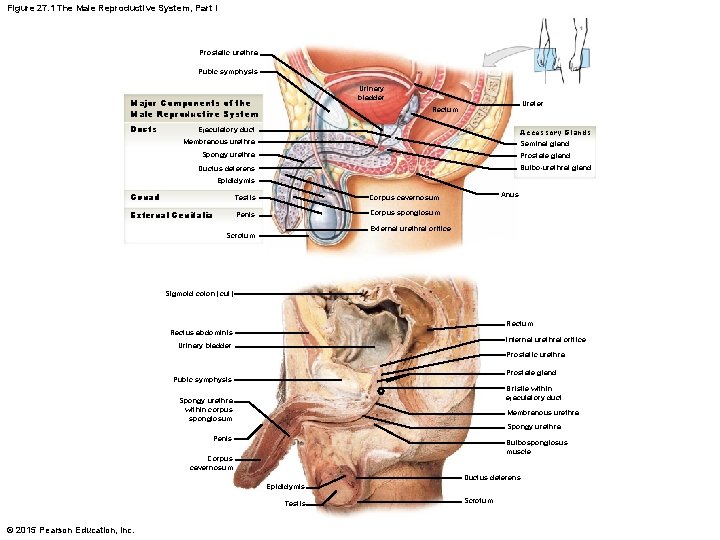
Figure 27. 1 The Male Reproductive System, Part I Prostatic urethra Pubic symphysis Urinary bladder Major Components of the Male Reproductive System Ducts Ureter Rectum Ejaculatory duct Accessory Glands Seminal gland Membranous urethra Spongy urethra Prostate gland Bulbo-urethral gland Ductus deferens Epididymis Gonad Testis Corpus cavernosum External Genitalia Penis Corpus spongiosum Anus External urethral orifice Scrotum Sigmoid colon (cut) Rectum Rectus abdominis Internal urethral orifice Urinary bladder Prostatic urethra Prostate gland Pubic symphysis Bristle within ejaculatory duct Spongy urethra within corpus spongiosum Membranous urethra Spongy urethra Penis Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Testis © 2015 Pearson Education, Inc. Scrotum
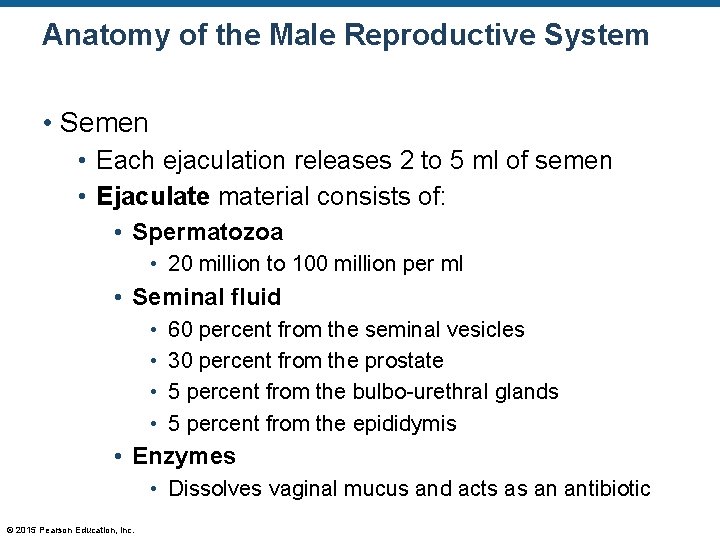
Anatomy of the Male Reproductive System • Semen • Each ejaculation releases 2 to 5 ml of semen • Ejaculate material consists of: • Spermatozoa • 20 million to 100 million per ml • Seminal fluid • • 60 percent from the seminal vesicles 30 percent from the prostate 5 percent from the bulbo-urethral glands 5 percent from the epididymis • Enzymes • Dissolves vaginal mucus and acts as an antibiotic © 2015 Pearson Education, Inc.
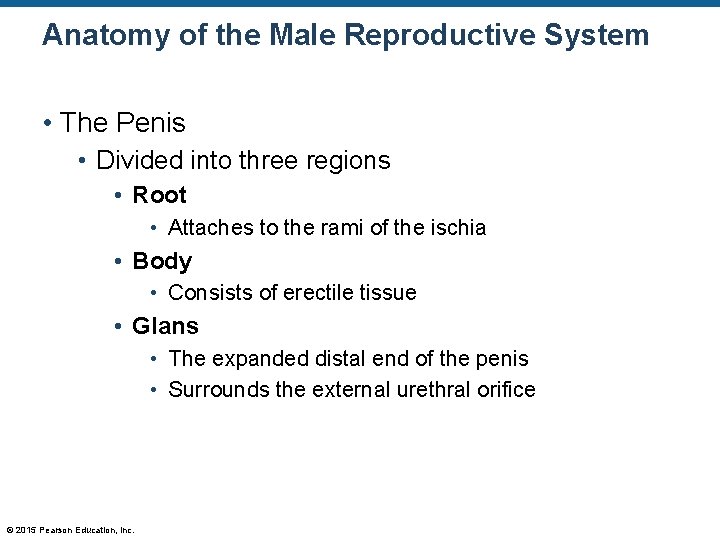
Anatomy of the Male Reproductive System • The Penis • Divided into three regions • Root • Attaches to the rami of the ischia • Body • Consists of erectile tissue • Glans • The expanded distal end of the penis • Surrounds the external urethral orifice © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • The Penis • Consists of three cylindrical columns of erectile tissue and blood vessels • Two corpora cavernosa • One corpus spongiosum © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • The Penis • The corpora cavernosa • Deep artery of the penis is in the center of this tissue • Each corpus cavernosum extends posteriorly forming a crus of the penis • Each crus is bound to the ramus of the ischium • The corpus spongiosum • Consists of the spongy urethra © 2015 Pearson Education, Inc.
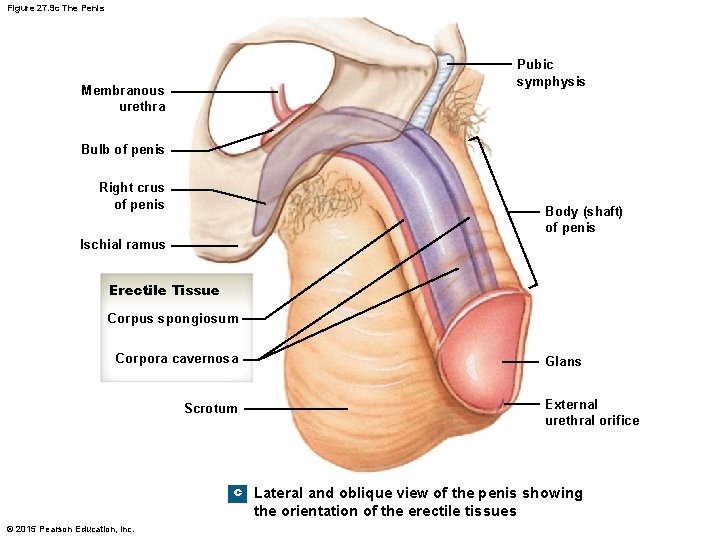
Figure 27. 9 c The Penis Pubic symphysis Membranous urethra Bulb of penis Right crus of penis Body (shaft) of penis Ischial ramus Erectile Tissue Corpus spongiosum Corpora cavernosa Glans External urethral orifice Scrotum c Lateral and oblique view of the penis showing the orientation of the erectile tissues © 2015 Pearson Education, Inc.
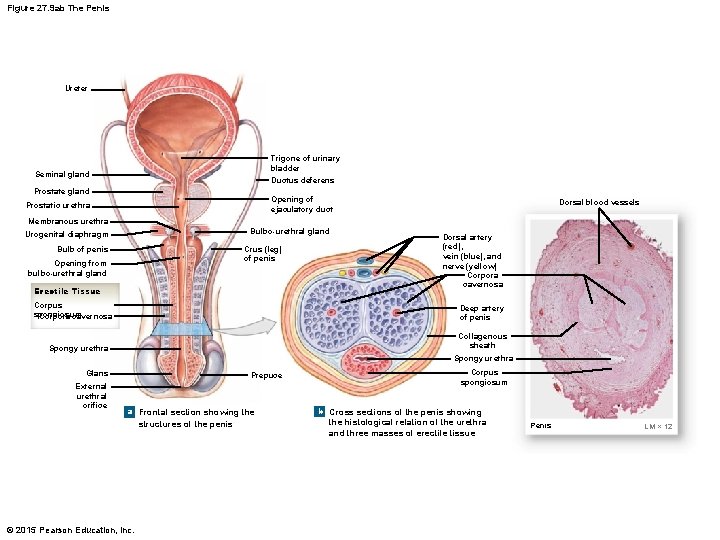
Figure 27. 9 ab The Penis Ureter Trigone of urinary bladder Ductus deferens Seminal gland Prostate gland Opening of ejaculatory duct Prostatic urethra Dorsal blood vessels Membranous urethra Bulbo-urethral gland Urogenital diaphragm Crus (leg) of penis Bulb of penis Opening from bulbo-urethral gland Erectile Tissue Corpus spongiosum Corpora cavernosa Dorsal artery (red), vein (blue), and nerve (yellow) Corpora cavernosa Deep artery of penis Collagenous sheath Spongy urethra Glans External urethral orifice Prepuce a Frontal section showing the structures of the penis © 2015 Pearson Education, Inc. Corpus spongiosum b Cross sections of the penis showing the histological relation of the urethra and three masses of erectile tissue Penis LM × 12
Anatomy of the Male Reproductive System • Erection of the Penis • • Parasympathetic nerves are activated Smooth muscles in the arterial walls relax Arterial vessels dilate Arterial vessels and vascular channels within the corpora cavernosa become engorged with blood • Erection occurs © 2015 Pearson Education, Inc.
Anatomy of the Male Reproductive System • Semen Release and Ejaculation • The sympathetic nerves cause peristaltic action in the: • • Ductus deferens Seminal glands Prostate gland Bulbo-urethral glands • Ejaculation occurs © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Overview of the Female Reproductive System • • • Ovaries Fimbriae Uterine tubes Uterus Vagina © 2015 Pearson Education, Inc.
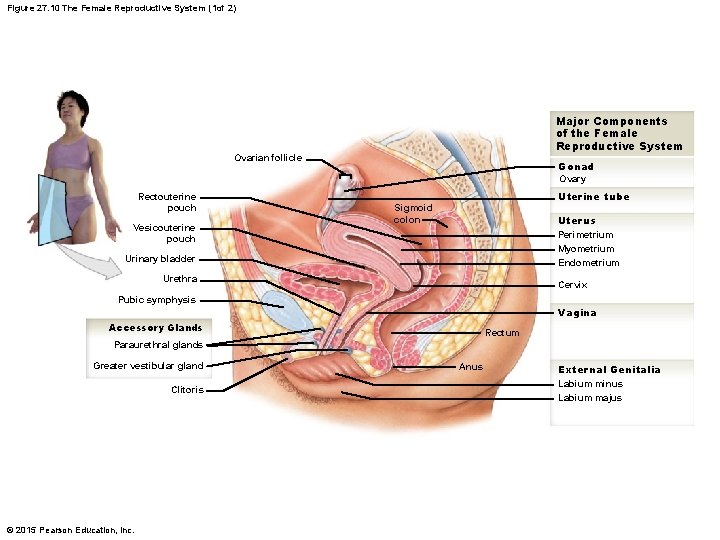
Figure 27. 10 The Female Reproductive System (1 of 2) Major Components of the Female Reproductive System Ovarian follicle Gonad Ovary Rectouterine pouch Vesicouterine pouch Uterine tube Sigmoid colon Uterus Perimetrium Myometrium Endometrium Urinary bladder Urethra Cervix Pubic symphysis Vagina Accessory Glands Rectum Paraurethral glands Greater vestibular gland Clitoris © 2015 Pearson Education, Inc. Anus External Genitalia Labium minus Labium majus
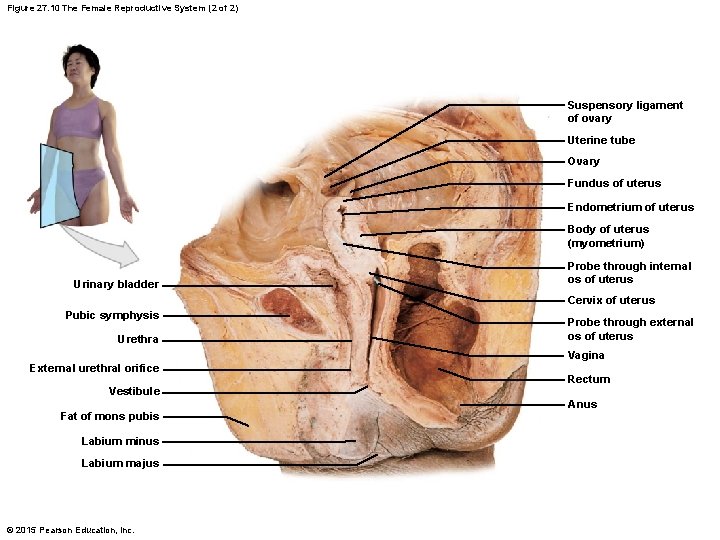
Figure 27. 10 The Female Reproductive System (2 of 2) Suspensory ligament of ovary Uterine tube Ovary Fundus of uterus Endometrium of uterus Body of uterus (myometrium) Urinary bladder Probe through internal os of uterus Cervix of uterus Pubic symphysis Urethra External urethral orifice Vestibule Fat of mons pubis Labium minus Labium majus © 2015 Pearson Education, Inc. Probe through external os of uterus Vagina Rectum Anus
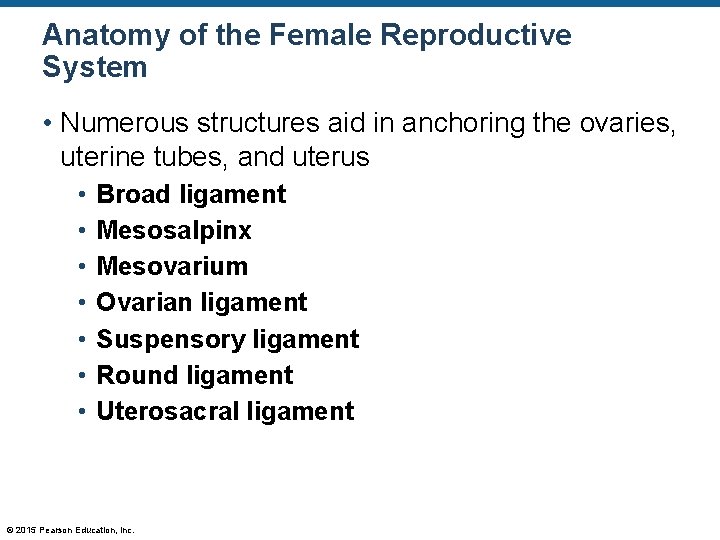
Anatomy of the Female Reproductive System • Numerous structures aid in anchoring the ovaries, uterine tubes, and uterus • • Broad ligament Mesosalpinx Mesovarium Ovarian ligament Suspensory ligament Round ligament Uterosacral ligament © 2015 Pearson Education, Inc.
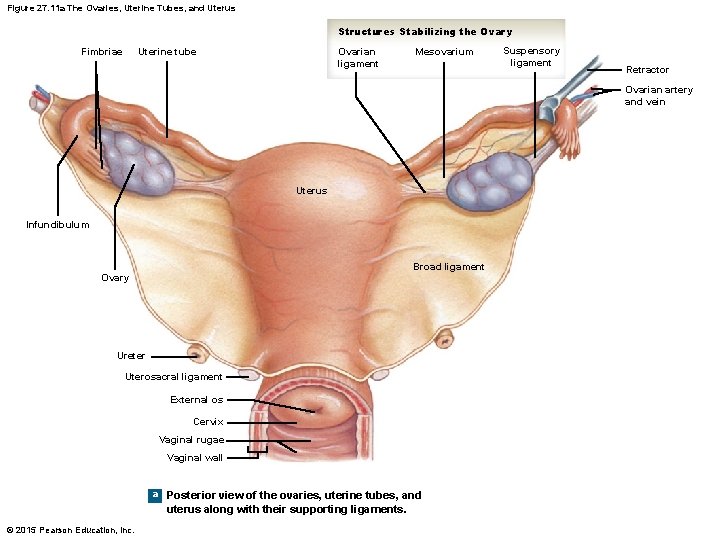
Figure 27. 11 a The Ovaries, Uterine Tubes, and Uterus Structures Stabilizing the Ovary Fimbriae Ovarian ligament Uterine tube Mesovarium Suspensory ligament Retractor Ovarian artery and vein Uterus Infundibulum Broad ligament Ovary Ureter Uterosacral ligament External os Cervix Vaginal rugae Vaginal wall a Posterior view of the ovaries, uterine tubes, and uterus along with their supporting ligaments. © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Ovaries • Consist of: • Cortex • Gamete production occurs here • Medulla © 2015 Pearson Education, Inc.
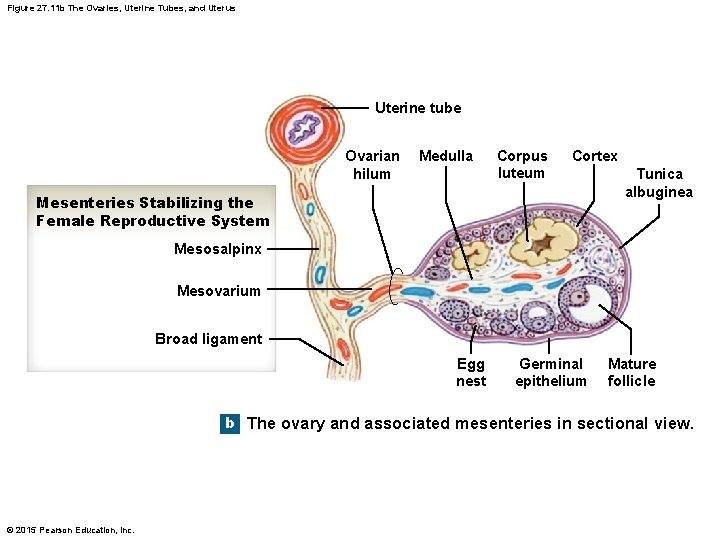
Figure 27. 11 b The Ovaries, Uterine Tubes, and Uterus Uterine tube Ovarian hilum Medulla Corpus luteum Cortex Mesenteries Stabilizing the Female Reproductive System Tunica albuginea Mesosalpinx Mesovarium Broad ligament Egg nest Germinal epithelium Mature follicle b The ovary and associated mesenteries in sectional view. © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Ovarian Cycle and Oogenesis • Oogenesis is the production of female gametes • Previous thoughts: • Unlike the males, this process begins before birth • Current research: • This might not be the case © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Ovarian Cycle and Oogenesis (details) • At puberty, the follicle-stimulating hormone (FSH) from the pituitary gland initiates the cycle • Primordial follicles develop into primary follicles • During this development, several layers of cells form around the follicles • Zona pellucida • This layer consists of granulosa cells • These cells form interdigitating microvilli to the oocyte • These cells also produce estrogen © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Ovarian Cycle and Oogenesis (details) • The layer surrounding the zona pellucida: • Thecal cells • These cells also release estrogen • Estrogen functions • • Stimulates bone and muscle growth Maintains female secondary sex characteristics Affects sex-related behaviors and drives Maintains function of reproductive glands and organs • Initiates repair and growth of uterine lining © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Ovarian Cycle and Oogenesis (details) • The primary follicles develop to form secondary follicles • Secondary follicles enlarge greatly due to fluid production by the follicular cells © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Ovarian Cycle and Oogenesis (details) • The secondary follicles become tertiary follicles • This is the mature follicle (also called Graafian follicle) • This follicle is large enough to cause the ovarian walls to stretch • The tertiary follicle is preparing to ovulate the egg © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Ovarian Cycle and Oogenesis (details) • Ovulation: gamete release • The follicular cells around the oocyte are now called the corona radiata • There is a rise in the concentration of the luteinizing hormone (LH)—this causes a weakening in the follicular wall • The egg is released eventually into the uterine tube © 2015 Pearson Education, Inc.
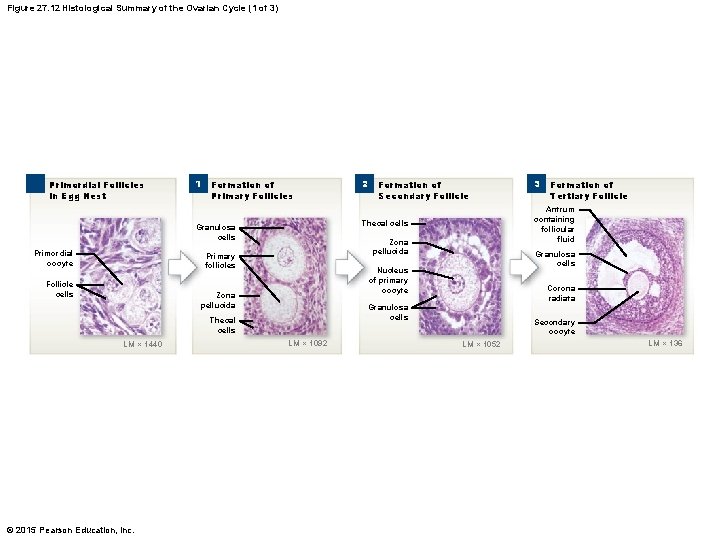
Figure 27. 12 Histological Summary of the Ovarian Cycle (1 of 3) Primordial Follicles in Egg Nest 1 Formation of Primary Follicles LM × 1440 © 2015 Pearson Education, Inc. Corona radiata Granulosa cells Thecal cells LM × 1092 Formation of Tertiary Follicle Granulosa cells Nucleus of primary oocyte Zona pellucida 3 Antrum containing follicular fluid Zona pellucida Primary follicles Follicle cells Formation of Secondary Follicle Thecal cells Granulosa cells Primordial oocyte 2 Secondary oocyte LM × 1052 LM × 136
Anatomy of the Female Reproductive System • The Ovarian Cycle and Oogenesis (details) • After the release of the egg, the empty follicle is called a corpus luteum • The corpus luteum produces progesterone • Progesterone is used to prepare the body for pregnancy • If pregnancy does not occur, the corpus luteum decomposes (about 12 days after ovulation) and becomes the corpus albicans © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Age and Oogenesis • At puberty, there about 200, 000 primordial follicles per ovary • Forty years later, only about 500 will have been ovulated • The rest decompose © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Uterine Tubes • Consist of four regions • • Infundibulum Ampulla Isthmus Uterine part © 2015 Pearson Education, Inc.
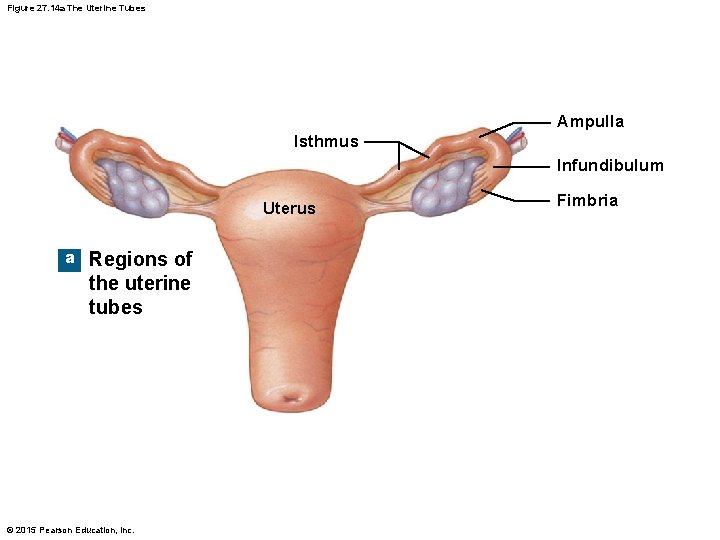
Figure 27. 14 a The Uterine Tubes Ampulla Isthmus Infundibulum Uterus a Regions of the uterine tubes © 2015 Pearson Education, Inc. Fimbria
Anatomy of the Female Reproductive System • Four Regions of the Uterine Tubes • Infundibulum • Has numerous fimbriae • Inner lining of infundibulum contains cilia • Ampulla • Isthmus • Uterine part • Opens into the uterus © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Histology of the Uterine Tube • Consists of • Ciliated and nonciliated columnar cells • Layers of smooth muscle • Used for peristaltic action • Successful fertilization • Occurs 12– 24 hours after ovulation • Occurs in the distal 2/3 of the uterine tube (ampulla region) © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Uterus • Provides protection for the embryo • Provides nutritional support for the embryo • Provides a means to remove waste produced by the embryo © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Uterus • Overall size • • Pear-shaped 7. 5 cm long 5 cm diameter 30– 40 g © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Suspensory Ligaments of the Uterus • These are in addition to the various regions of the broad ligament • Uterosacral ligaments • Round ligaments • Cardinal ligaments © 2015 Pearson Education, Inc.
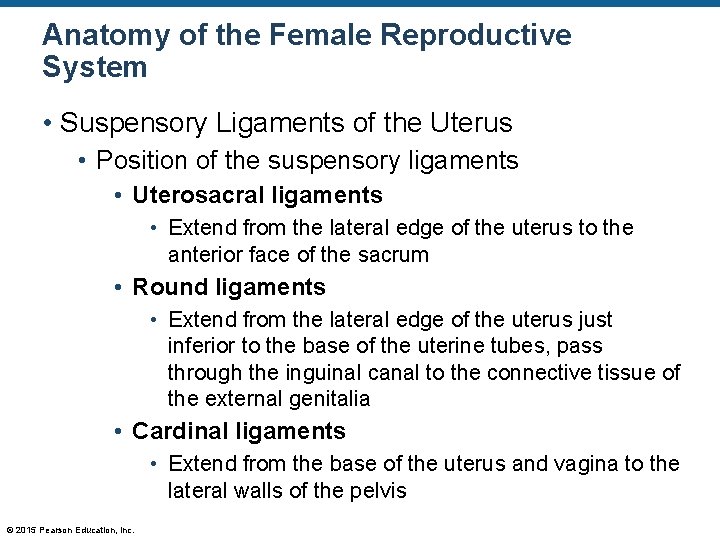
Anatomy of the Female Reproductive System • Suspensory Ligaments of the Uterus • Position of the suspensory ligaments • Uterosacral ligaments • Extend from the lateral edge of the uterus to the anterior face of the sacrum • Round ligaments • Extend from the lateral edge of the uterus just inferior to the base of the uterine tubes, pass through the inguinal canal to the connective tissue of the external genitalia • Cardinal ligaments • Extend from the base of the uterus and vagina to the lateral walls of the pelvis © 2015 Pearson Education, Inc.
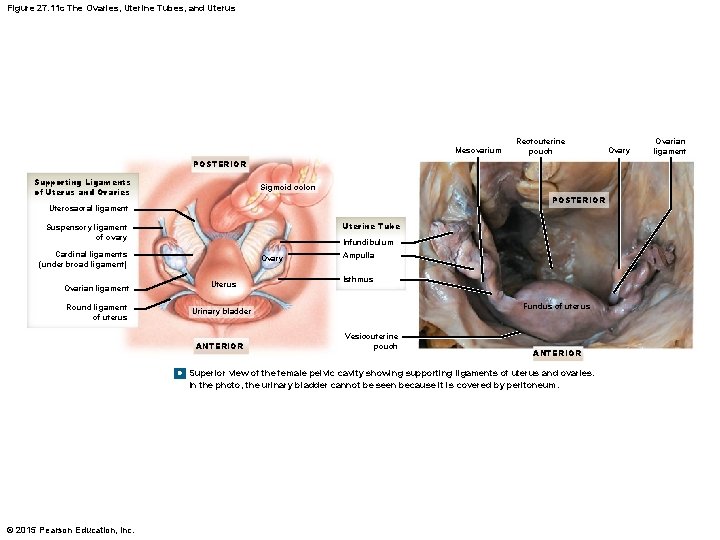
Figure 27. 11 c The Ovaries, Uterine Tubes, and Uterus Mesovarium Rectouterine pouch POSTERIOR Supporting Ligaments of Uterus and Ovaries Sigmoid colon POSTERIOR Uterosacral ligament Uterine Tube Suspensory ligament of ovary Infundibulum Cardinal ligaments (under broad ligament) Ovary Ovarian ligament Uterus Round ligament of uterus Urinary bladder ANTERIOR Ampulla Isthmus Fundus of uterus Vesicouterine pouch ANTERIOR c Superior view of the female pelvic cavity showing supporting ligaments of uterus and ovaries. In the photo, the urinary bladder cannot be seen because it is covered by peritoneum. © 2015 Pearson Education, Inc. Ovary Ovarian ligament
Anatomy of the Female Reproductive System • Internal Anatomy of the Uterus • Consists of: • • Body Fundus Cervix External os Cervical canal Uterine cavity Internal os © 2015 Pearson Education, Inc.
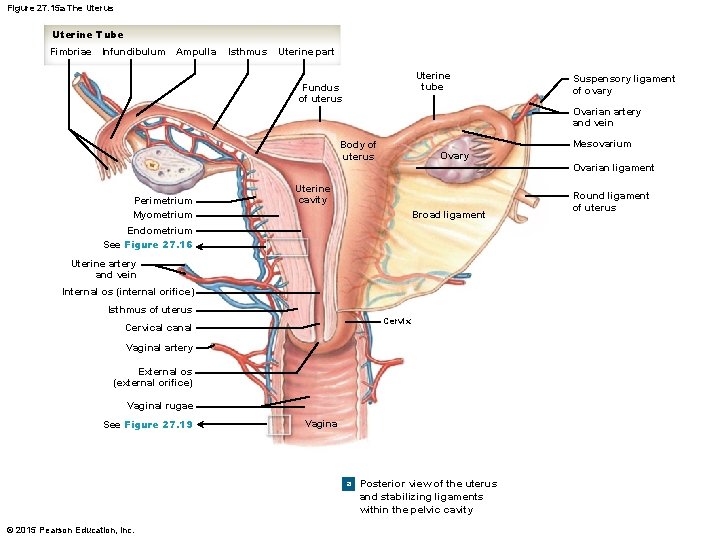
Figure 27. 15 a The Uterus Uterine Tube Fimbriae Infundibulum Ampulla Isthmus Uterine part Uterine tube Fundus of uterus Suspensory ligament of ovary Ovarian artery and vein Mesovarium Body of uterus Perimetrium Myometrium Ovary Ovarian ligament Uterine cavity Broad ligament Endometrium See Figure 27. 16 Uterine artery and vein Internal os (internal orifice) Isthmus of uterus Cervix Cervical canal Vaginal artery External os (external orifice) Vaginal rugae See Figure 27. 19 Vagina a Posterior view of the uterus and stabilizing ligaments within the pelvic cavity © 2015 Pearson Education, Inc. Round ligament of uterus
Anatomy of the Female Reproductive System • The Uterine Wall • The uterine wall consists of three layers • Endometrium • Myometrium • Consists of longitudinal, circular, and oblique smooth muscles • Perimetrium © 2015 Pearson Education, Inc.
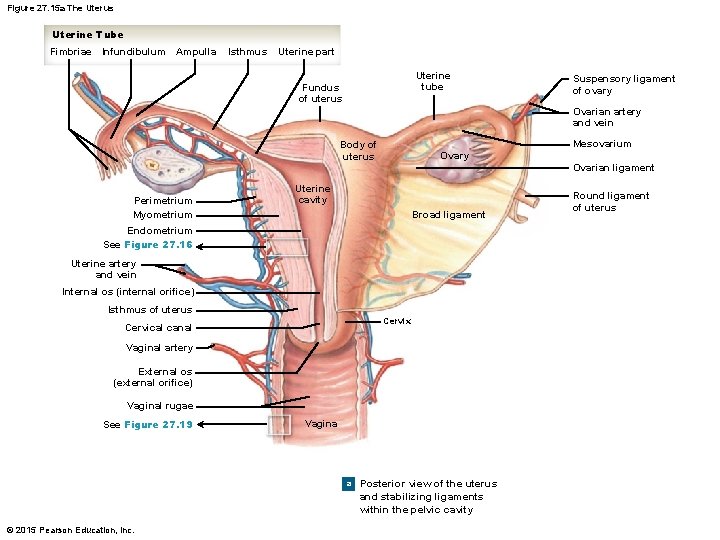
Figure 27. 15 a The Uterus Uterine Tube Fimbriae Infundibulum Ampulla Isthmus Uterine part Uterine tube Fundus of uterus Suspensory ligament of ovary Ovarian artery and vein Mesovarium Body of uterus Perimetrium Myometrium Ovary Ovarian ligament Uterine cavity Broad ligament Endometrium See Figure 27. 16 Uterine artery and vein Internal os (internal orifice) Isthmus of uterus Cervix Cervical canal Vaginal artery External os (external orifice) Vaginal rugae See Figure 27. 19 Vagina a Posterior view of the uterus and stabilizing ligaments within the pelvic cavity © 2015 Pearson Education, Inc. Round ligament of uterus
Anatomy of the Female Reproductive System • Blood Supply to the Uterus • Uterine arteries arise from the internal iliac arteries • Ovarian arteries arise from the abdominal aorta inferior to the renal arteries © 2015 Pearson Education, Inc.
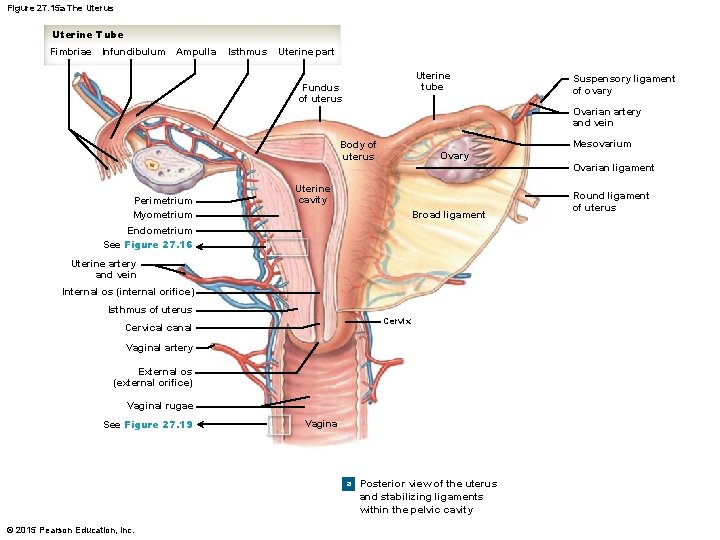
Figure 27. 15 a The Uterus Uterine Tube Fimbriae Infundibulum Ampulla Isthmus Uterine part Uterine tube Fundus of uterus Suspensory ligament of ovary Ovarian artery and vein Mesovarium Body of uterus Perimetrium Myometrium Ovary Ovarian ligament Uterine cavity Broad ligament Endometrium See Figure 27. 16 Uterine artery and vein Internal os (internal orifice) Isthmus of uterus Cervix Cervical canal Vaginal artery External os (external orifice) Vaginal rugae See Figure 27. 19 Vagina a Posterior view of the uterus and stabilizing ligaments within the pelvic cavity © 2015 Pearson Education, Inc. Round ligament of uterus
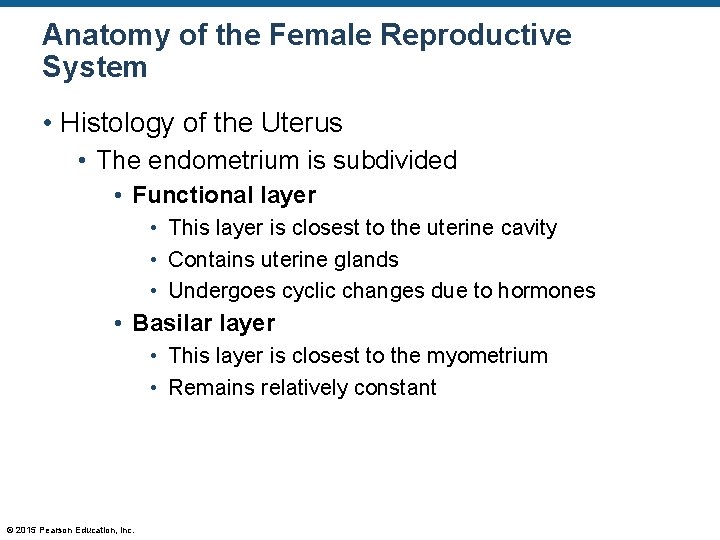
Anatomy of the Female Reproductive System • Histology of the Uterus • The endometrium is subdivided • Functional layer • This layer is closest to the uterine cavity • Contains uterine glands • Undergoes cyclic changes due to hormones • Basilar layer • This layer is closest to the myometrium • Remains relatively constant © 2015 Pearson Education, Inc.
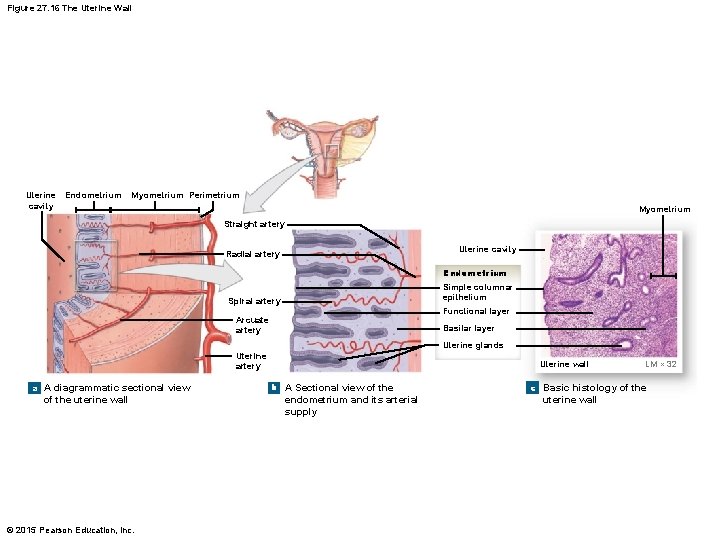
Figure 27. 16 The Uterine Wall Uterine cavity Endometrium Myometrium Perimetrium Myometrium Straight artery Uterine cavity Radial artery Endometrium Simple columnar epithelium Spiral artery Functional layer Arcuate artery Basilar layer Uterine glands Uterine artery a A diagrammatic sectional view of the uterine wall © 2015 Pearson Education, Inc. Uterine wall b A Sectional view of the endometrium and its arterial supply LM × 32 c Basic histology of the uterine wall
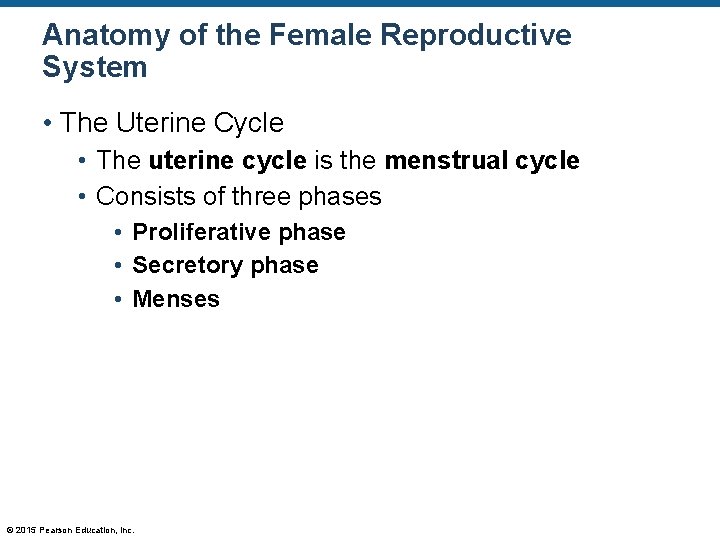
Anatomy of the Female Reproductive System • The Uterine Cycle • The uterine cycle is the menstrual cycle • Consists of three phases • Proliferative phase • Secretory phase • Menses © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Phases of the Uterine Cycle • Menarche • This is the first uterine cycle at puberty • Proliferative phase • Endometrial lining thickens preparing the body for the implantation of a fertilized egg • Secretory phase • Endometrial glands enlarge and blood vessels elongate • An egg is ready to implant (if an egg is present) © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Phases of the Uterine Cycle • Menses • Begins due to a decrease in progestin and estrogen levels • This causes constriction of blood vessels • This causes a loss of the excess endometrial cells • This is menstruation • Menopause • The last uterine cycle © 2015 Pearson Education, Inc.
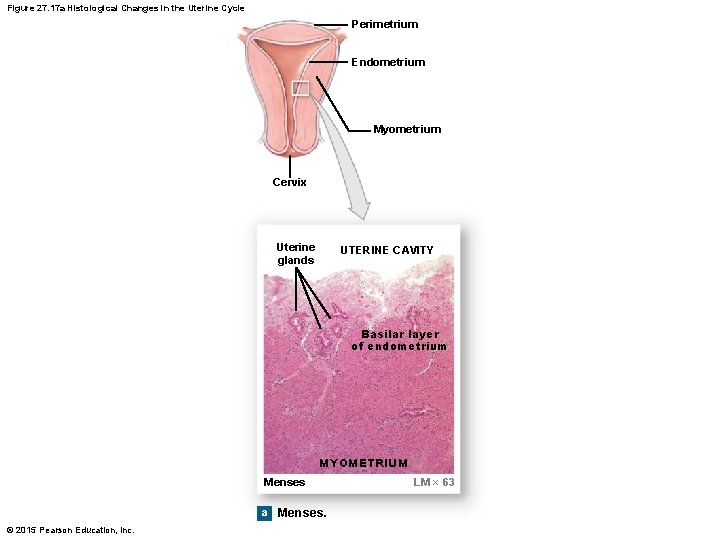
Figure 27. 17 a Histological Changes in the Uterine Cycle Perimetrium Endometrium Myometrium Cervix Uterine glands UTERINE CAVITY Basilar layer of endometrium MYOMETRIUM Menses a Menses. © 2015 Pearson Education, Inc. LM × 63
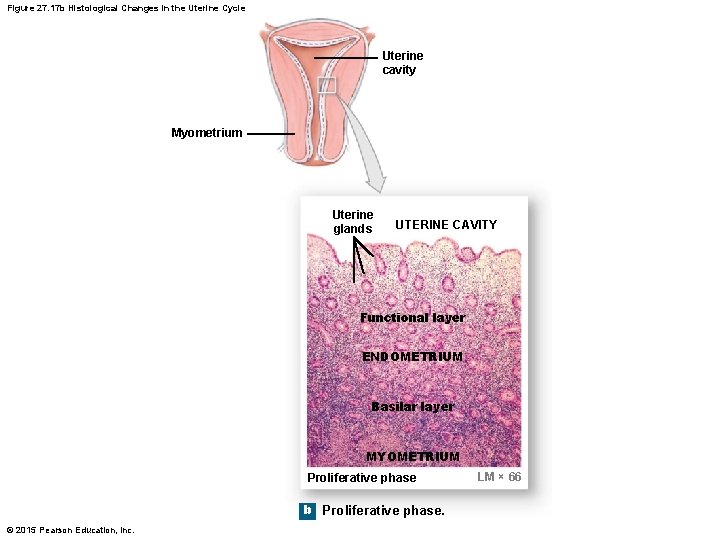
Figure 27. 17 b Histological Changes in the Uterine Cycle Uterine cavity Myometrium Uterine glands UTERINE CAVITY Functional layer ENDOMETRIUM Basilar layer MYOMETRIUM Proliferative phase b Proliferative phase. © 2015 Pearson Education, Inc. LM × 66
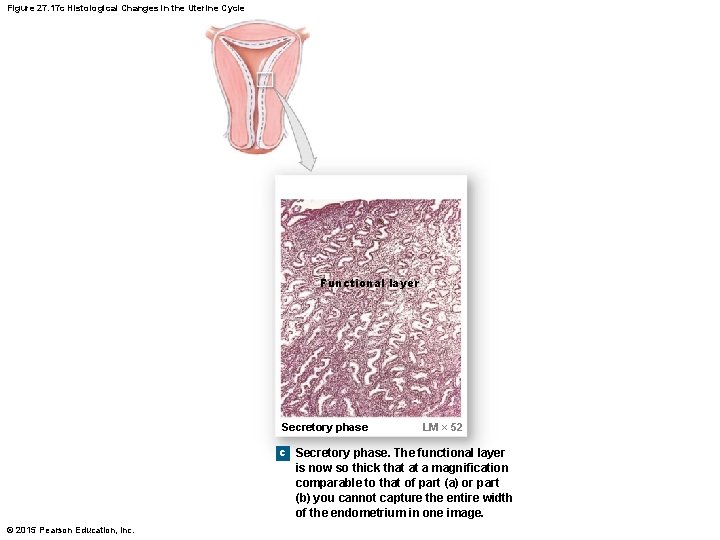
Figure 27. 17 c Histological Changes in the Uterine Cycle Functional layer Secretory phase LM × 52 c Secretory phase. The functional layer is now so thick that at a magnification comparable to that of part (a) or part (b) you cannot capture the entire width of the endometrium in one image. © 2015 Pearson Education, Inc.
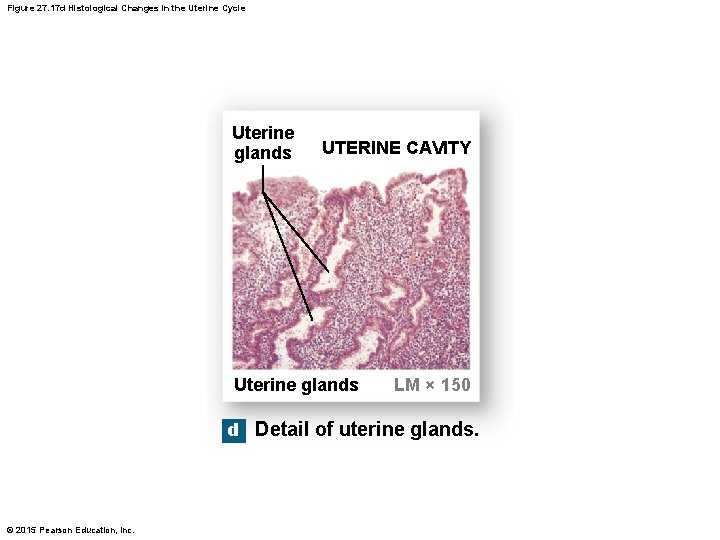
Figure 27. 17 d Histological Changes in the Uterine Cycle Uterine glands UTERINE CAVITY Uterine glands LM × 150 d Detail of uterine glands. © 2015 Pearson Education, Inc.
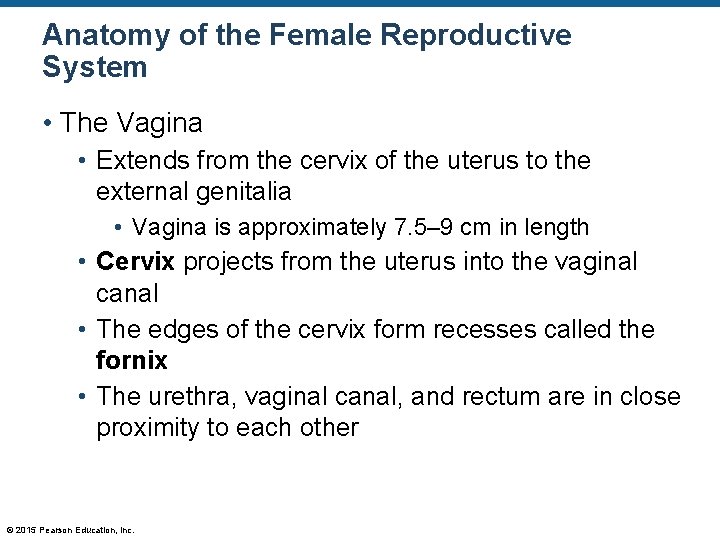
Anatomy of the Female Reproductive System • The Vagina • Extends from the cervix of the uterus to the external genitalia • Vagina is approximately 7. 5– 9 cm in length • Cervix projects from the uterus into the vaginal canal • The edges of the cervix form recesses called the fornix • The urethra, vaginal canal, and rectum are in close proximity to each other © 2015 Pearson Education, Inc.
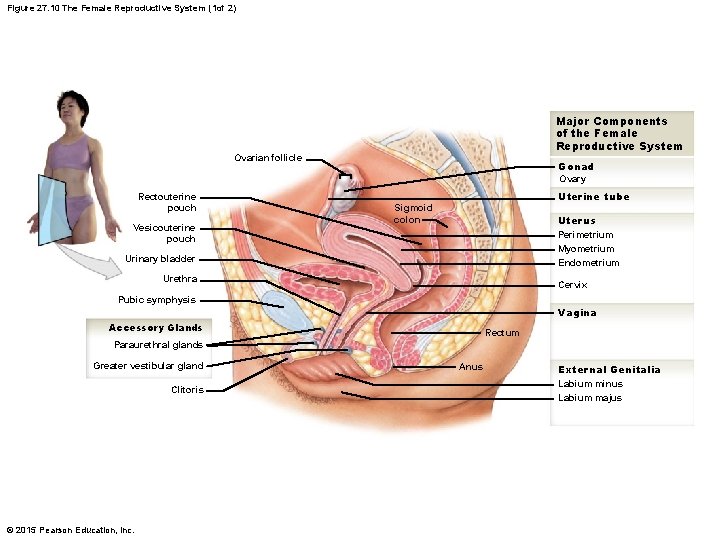
Figure 27. 10 The Female Reproductive System (1 of 2) Major Components of the Female Reproductive System Ovarian follicle Gonad Ovary Rectouterine pouch Vesicouterine pouch Uterine tube Sigmoid colon Uterus Perimetrium Myometrium Endometrium Urinary bladder Urethra Cervix Pubic symphysis Vagina Accessory Glands Rectum Paraurethral glands Greater vestibular gland Clitoris © 2015 Pearson Education, Inc. Anus External Genitalia Labium minus Labium majus
Anatomy of the Female Reproductive System • The Vagina • Serves three major functions • Passageway for elimination of menstrual fluids • Receives the penis and holds spermatozoa before they enter the uterus • Serves as a passageway for the fetus during vaginal birth © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The Vagina • Contains a normal population of bacteria • Bacteria are provided nutrients found in the cervical mucus • The bacteria create an acid environment • This reduces the growth of many pathogenic organisms • This also reduces sperm mobility • Buffers found in seminal fluid counteract this acidity © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Histology of the Vagina • Lined with stratified squamous epithelium • When relaxed, this tissue forms rugae • Lamina propria is thick and elastic • The muscular layer is continuous with the myometrium of the uterus © 2015 Pearson Education, Inc.
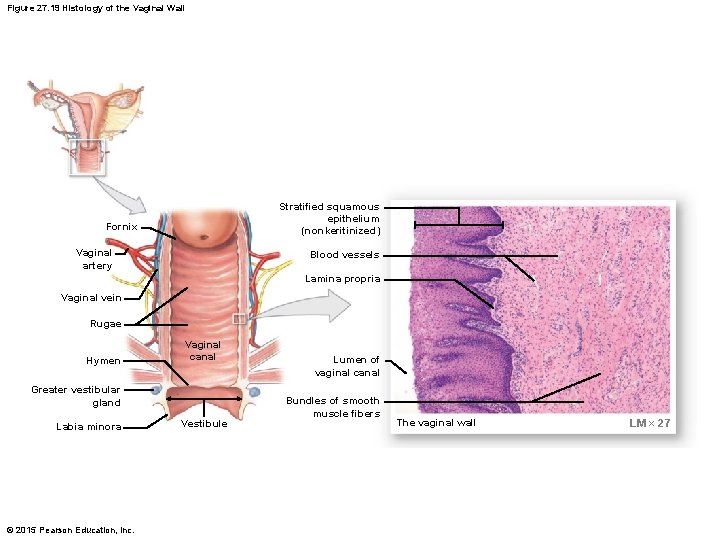
Figure 27. 19 Histology of the Vaginal Wall Stratified squamous epithelium (nonkeritinized) Fornix Vaginal artery Blood vessels Lamina propria Vaginal vein Rugae Hymen Vaginal canal Greater vestibular gland Labia minora © 2015 Pearson Education, Inc. Vestibule Lumen of vaginal canal Bundles of smooth muscle fibers The vaginal wall LM × 27
Anatomy of the Female Reproductive System • The External Genitalia • • Vulva Vestibule Labia minora Clitoris Prepuce Labia majora Mons pubis Hymen (when present) © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • The External Genitalia (details) • Vulva • The entire genitalia area • Vestibule • The opening into the vagina surrounded by the labia minora • Clitoris • Contains erectile tissue • Labia majora and mons pubis • Forms the lateral and superior edges of the vestibule © 2015 Pearson Education, Inc.
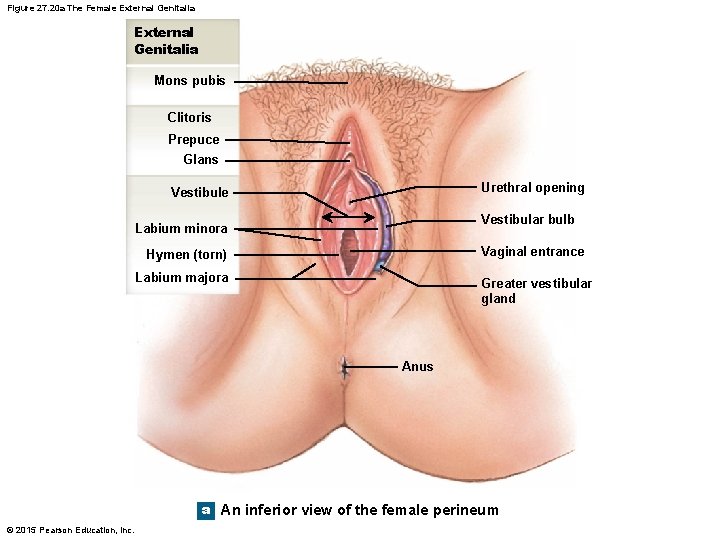
Figure 27. 20 a The Female External Genitalia Mons pubis Clitoris Prepuce Glans Urethral opening Vestibule Vestibular bulb Labium minora Vaginal entrance Hymen (torn) Labium majora Greater vestibular gland Anus a An inferior view of the female perineum © 2015 Pearson Education, Inc.
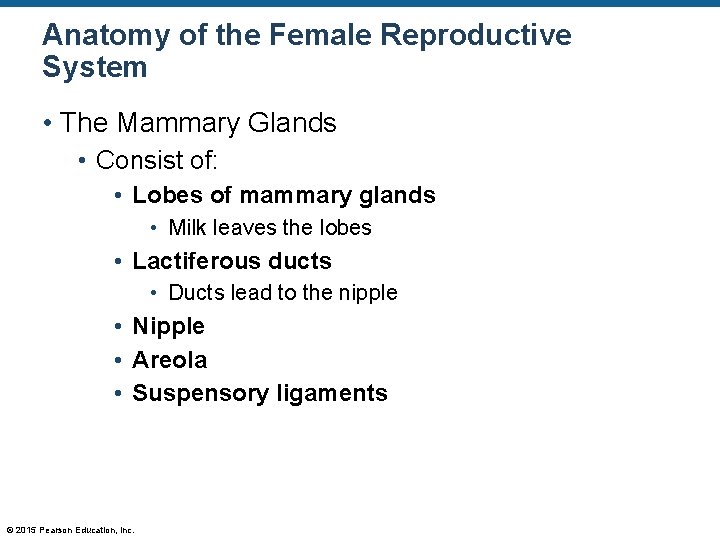
Anatomy of the Female Reproductive System • The Mammary Glands • Consist of: • Lobes of mammary glands • Milk leaves the lobes • Lactiferous ducts • Ducts lead to the nipple • Nipple • Areola • Suspensory ligaments © 2015 Pearson Education, Inc.
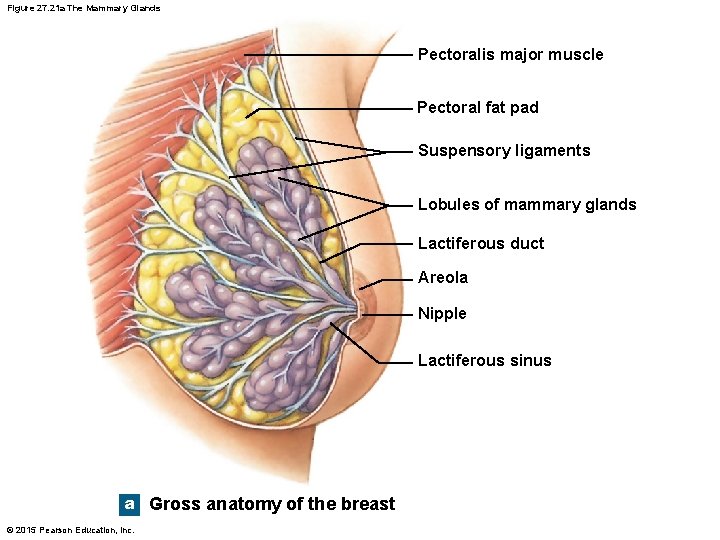
Figure 27. 21 a The Mammary Glands Pectoralis major muscle Pectoral fat pad Suspensory ligaments Lobules of mammary glands Lactiferous duct Areola Nipple Lactiferous sinus a Gross anatomy of the breast © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Development of the Mammary Glands during Pregnancy • Mammary gland ducts become mitotically active • Due to: • PRL / GH / HPL • Fully developed by 6 months of pregnancy • Milk is release when the infant sucks on the nipple • Pressure from nursing causes the release of oxytocin (OT) from the pituitary gland • OT causes the contraction of the lactiferous ducts, thus ejecting milk © 2015 Pearson Education, Inc.
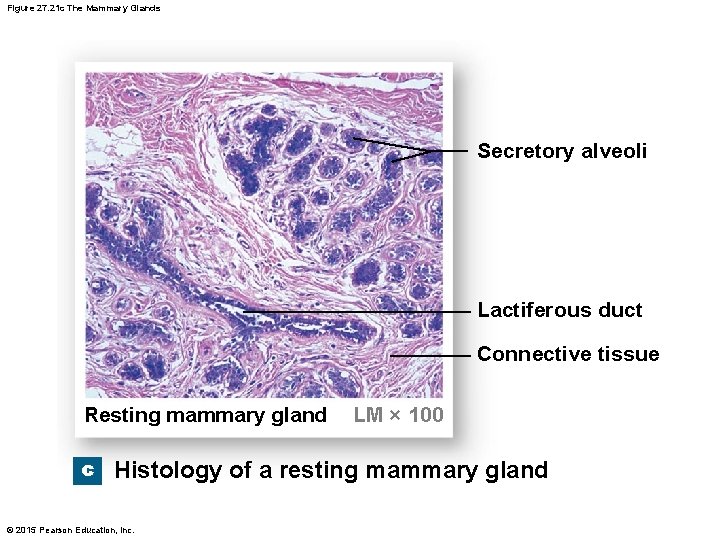
Figure 27. 21 c The Mammary Glands Secretory alveoli Lactiferous duct Connective tissue Resting mammary gland LM × 100 c Histology of a resting mammary gland © 2015 Pearson Education, Inc.
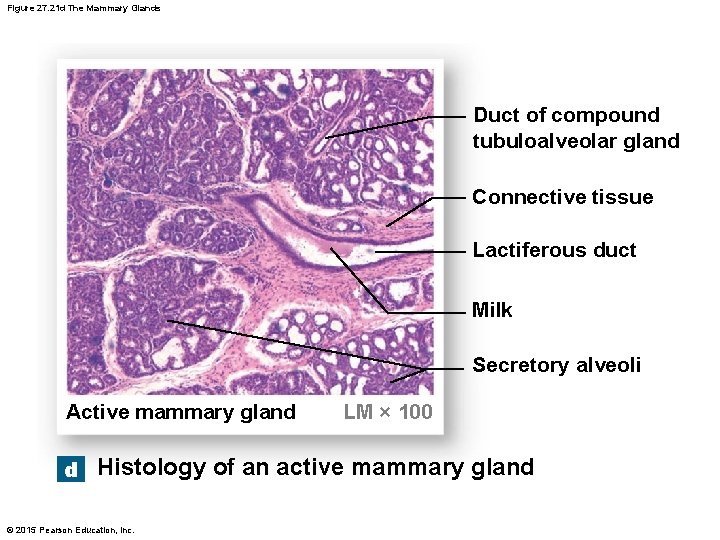
Figure 27. 21 d The Mammary Glands Duct of compound tubuloalveolar gland Connective tissue Lactiferous duct Milk Secretory alveoli Active mammary gland LM × 100 d Histology of an active mammary gland © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Pregnancy and the Female Reproductive System • Upon fertilization of the egg, changes occur • Blastocyst forms • Eventually implants in the endometrial lining • A placenta will form • Placenta releases HCG • HCG keeps the corpus luteum active • An active corpus luteum maintains a thick endometrial lining © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Pregnancy and the Female Reproductive System (continued) • In three months, the corpus luteum will decompose • A thick endometrial lining will continue due to: • The placenta produces progesterone, which maintains the thick endometrial lining • Placenta also produces • Relaxin • Human placental lactogen © 2015 Pearson Education, Inc.
Anatomy of the Female Reproductive System • Pregnancy and the Female Reproductive System (continued) • Relaxin • Increases pelvic flexibility during delivery • Dilation of the cervix during birth • Human placental lactogen • Helps prepare the mammary glands for milk production © 2015 Pearson Education, Inc.
Aging and the Reproductive System • Menopause • Decline in estrogen levels results in: • • Reduced size of the uterus Reduced size of the breasts Thinning of the vaginal walls Weakening of the supportive tissues of the reproductive organs • Osteoporosis • Hot flashes • Typically occurs at age 45– 55 © 2015 Pearson Education, Inc.
Aging and the Reproductive System • The Male Climacteric • Testosterone levels begin to decline (not as rapidly as estrogen however) • Occurs gradually between ages 50 and 60 • Reduction in sexual activity © 2015 Pearson Education, Inc.
- Slides: 120