Chapter 26 Urinary System Urinary System Functions Filtering
- Slides: 48
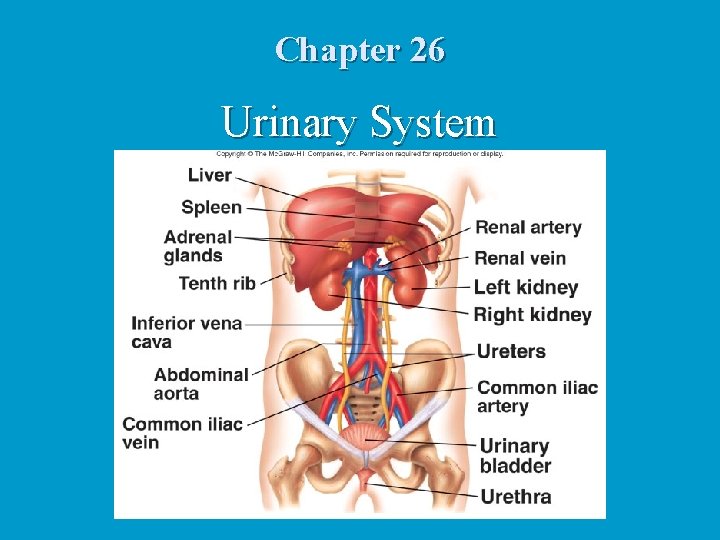
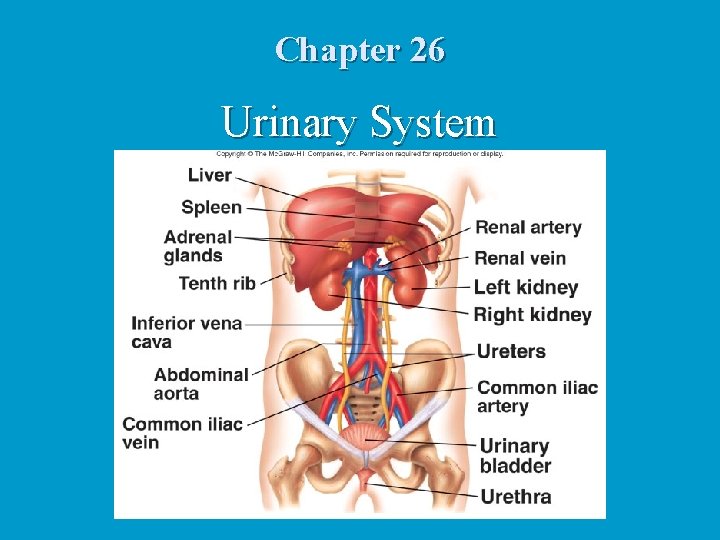
Chapter 26 Urinary System
Urinary System Functions Filtering of blood n Regulation of n blood volume n concentration of blood solutes n p. H of extracellular fluid n blood cell synthesis n n Synthesis of Vitamin D
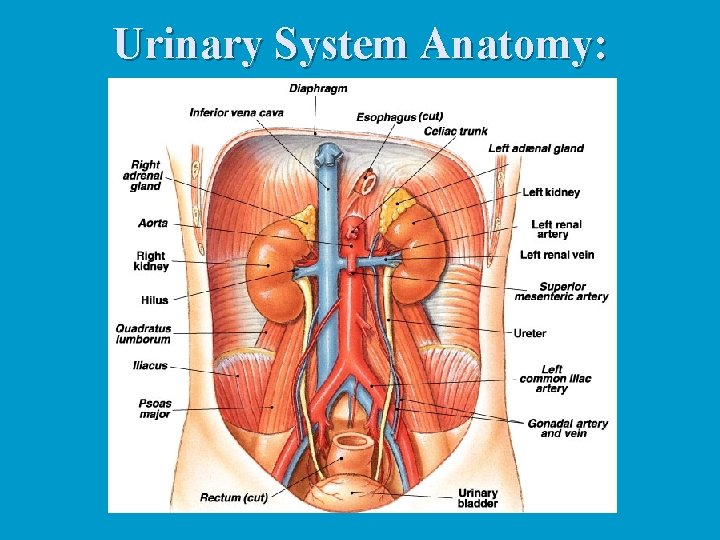
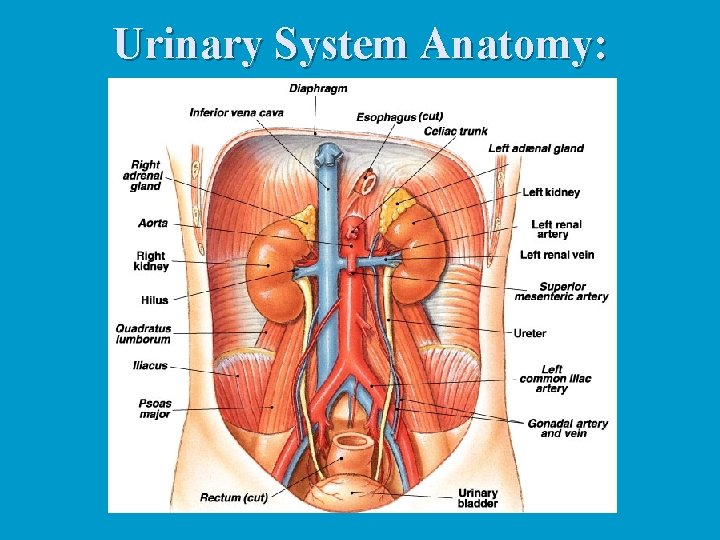
Urinary System Anatomy:
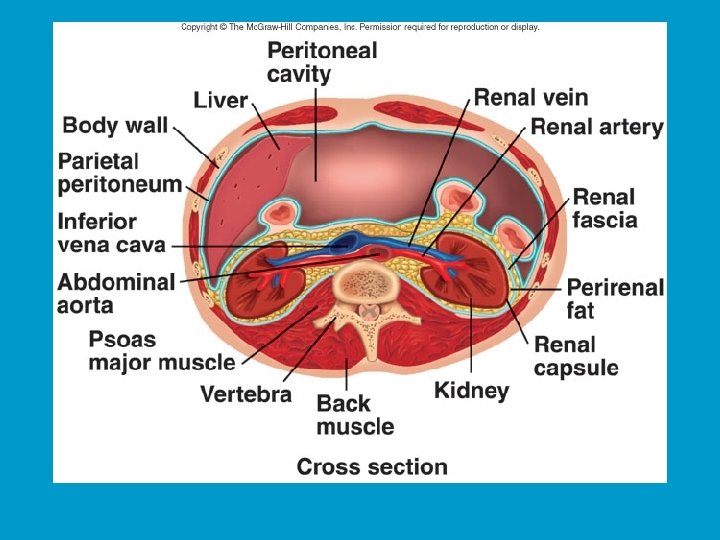
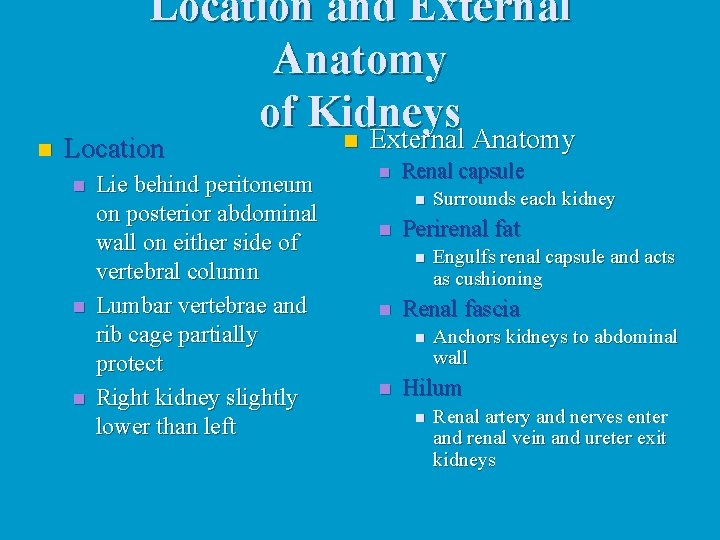
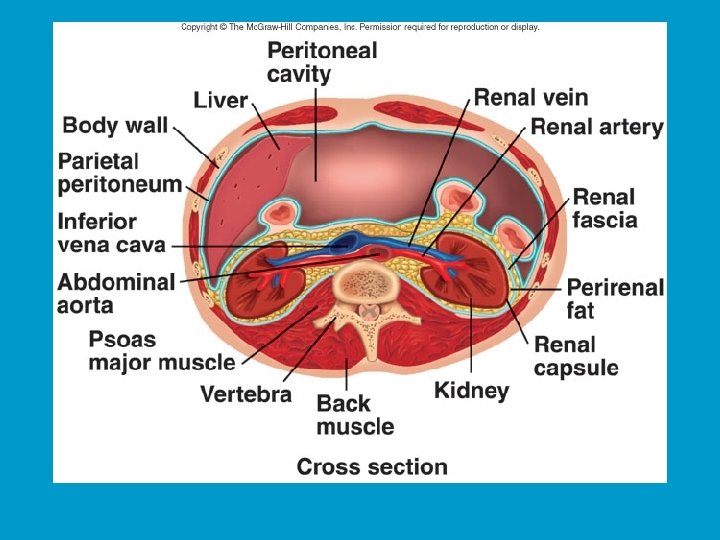
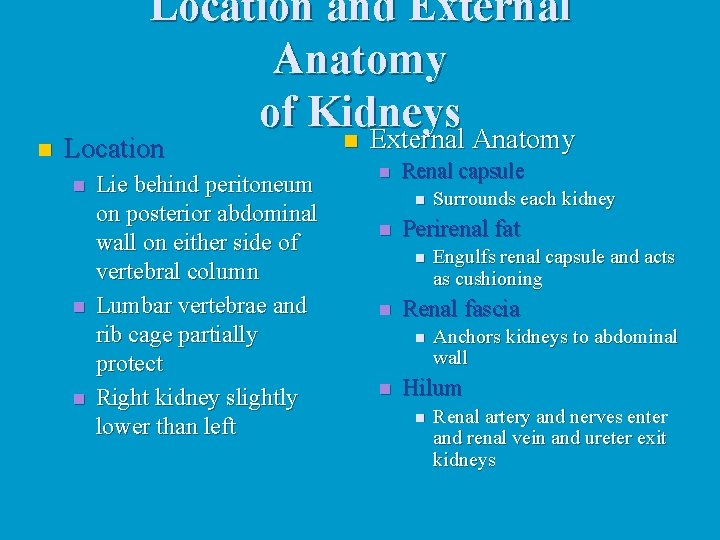
n Location and External Anatomy of Kidneys n External Anatomy Location n Lie behind peritoneum on posterior abdominal wall on either side of vertebral column Lumbar vertebrae and rib cage partially protect Right kidney slightly lower than left n Renal capsule n n Perirenal fat n n Engulfs renal capsule and acts as cushioning Renal fascia n n Surrounds each kidney Anchors kidneys to abdominal wall Hilum n Renal artery and nerves enter and renal vein and ureter exit kidneys
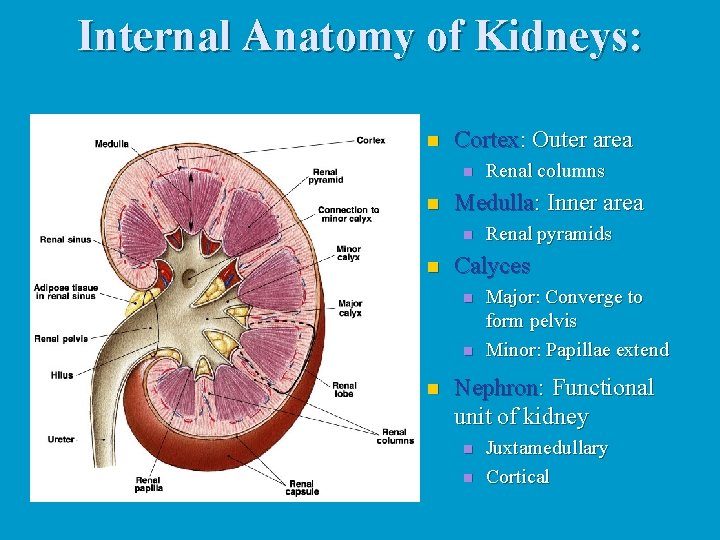
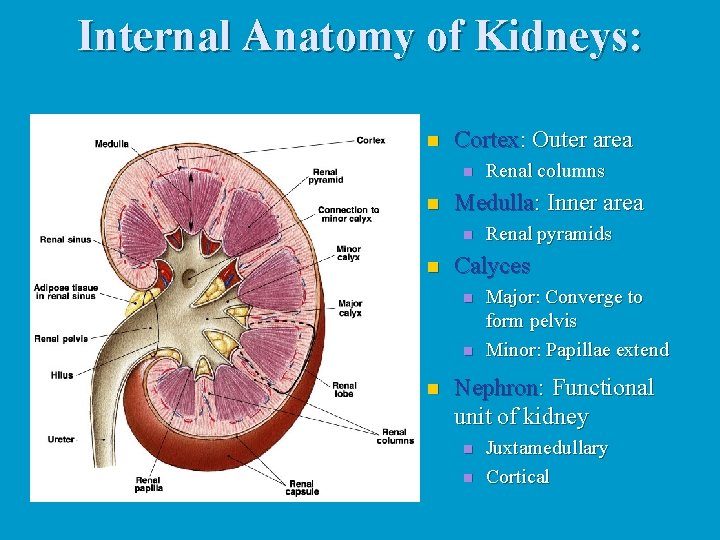
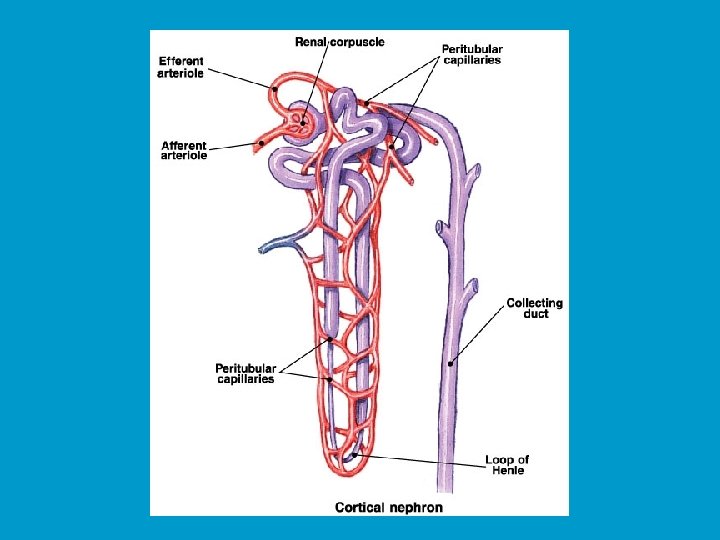
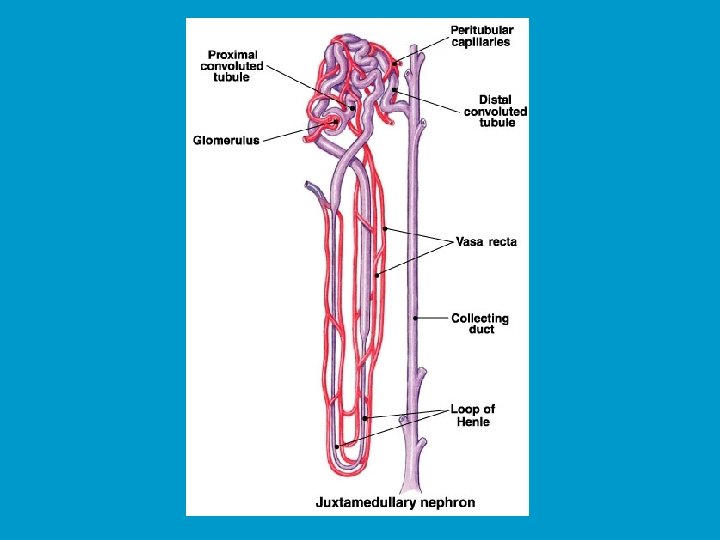
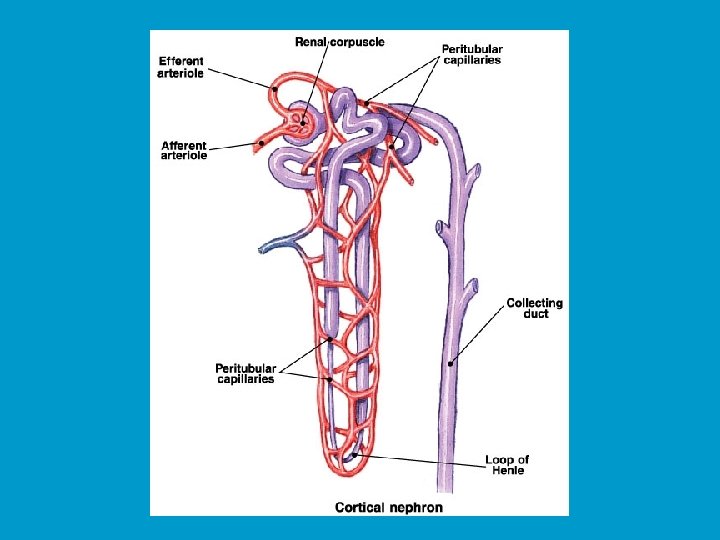
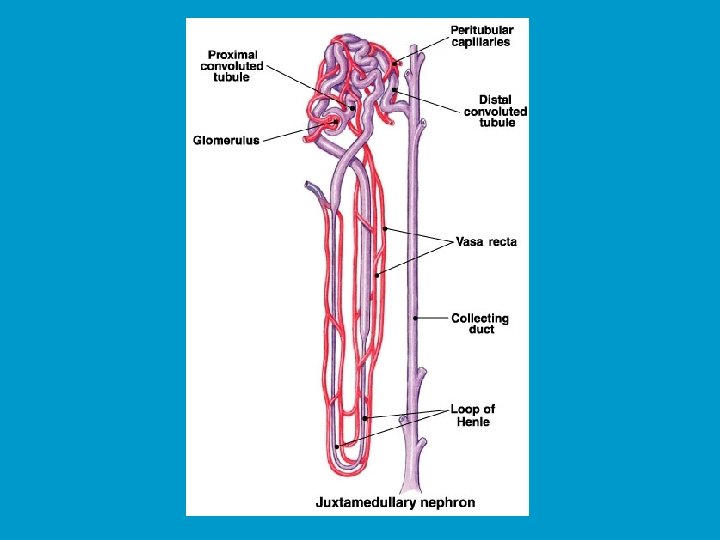
Internal Anatomy of Kidneys: n Cortex: Outer area n n Medulla: Inner area n n Renal pyramids Calyces n n n Renal columns Major: Converge to form pelvis Minor: Papillae extend Nephron: Functional unit of kidney n n Juxtamedullary Cortical
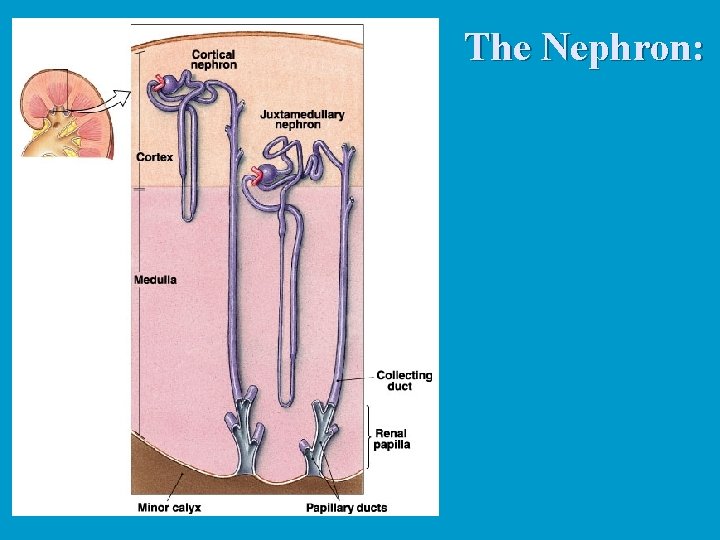
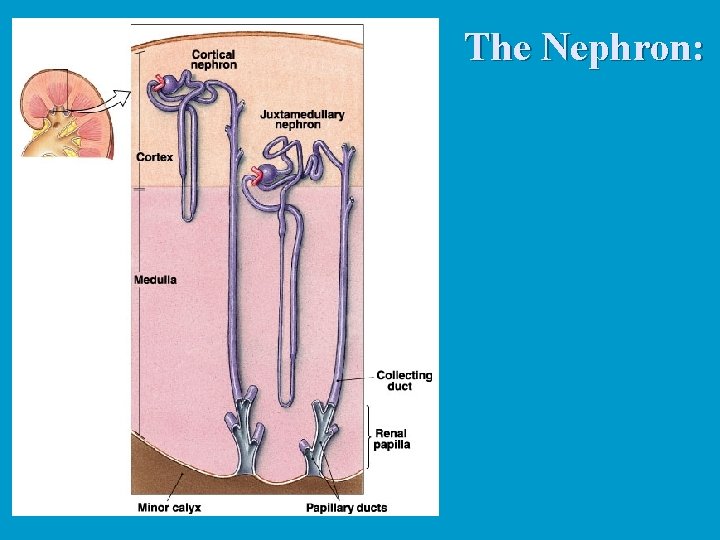
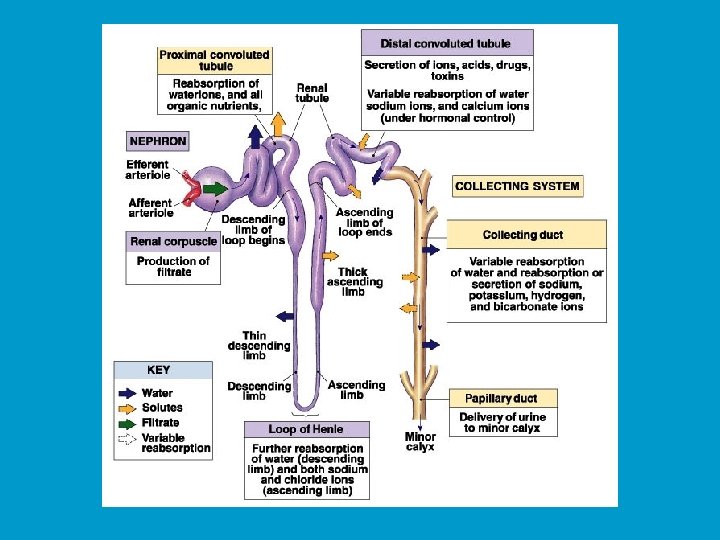
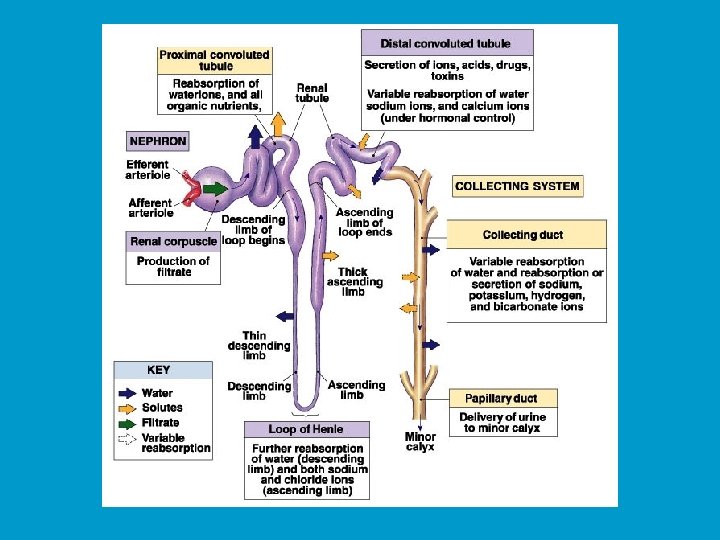
The Nephron:
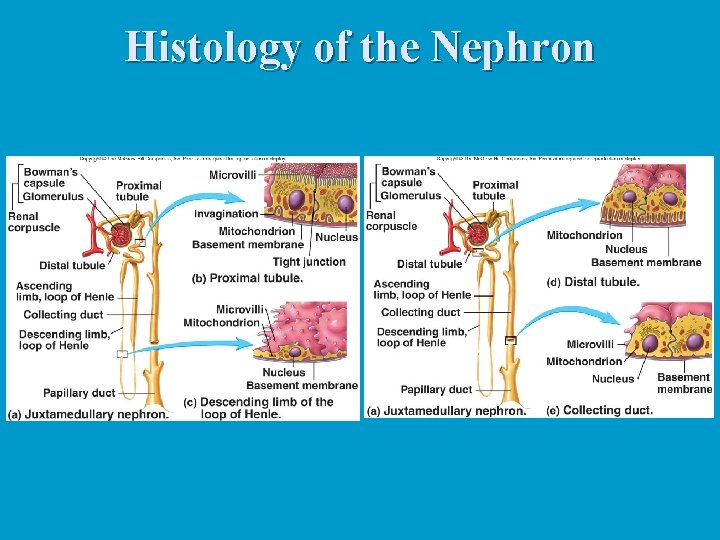
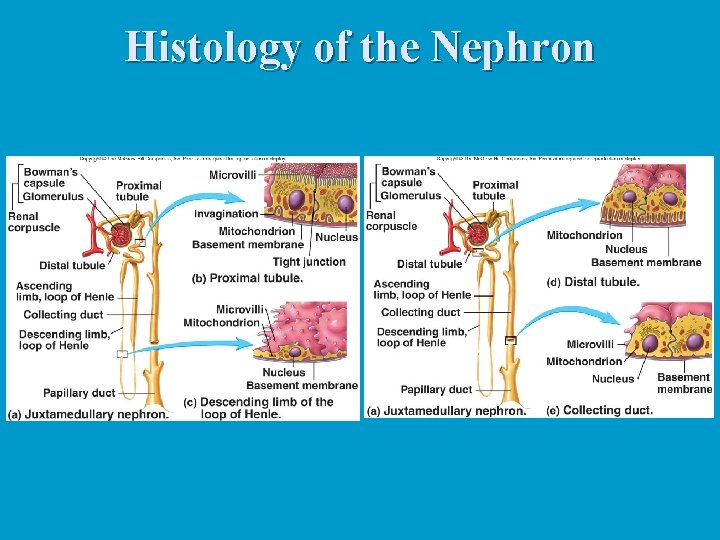
Histology of the Nephron
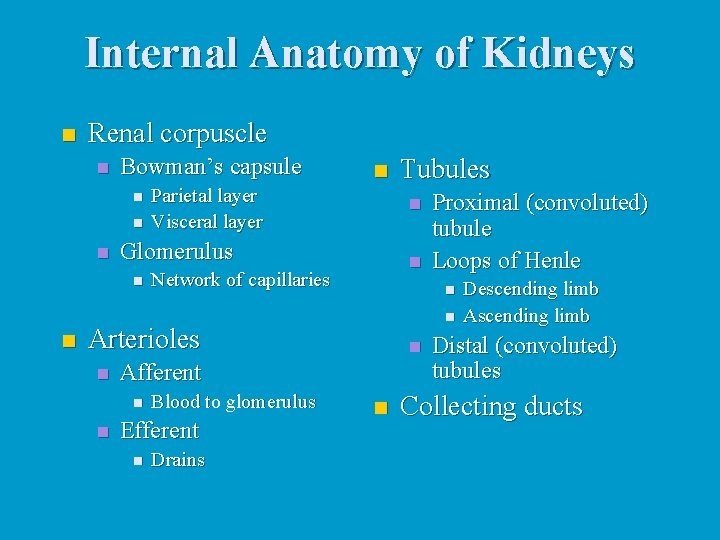
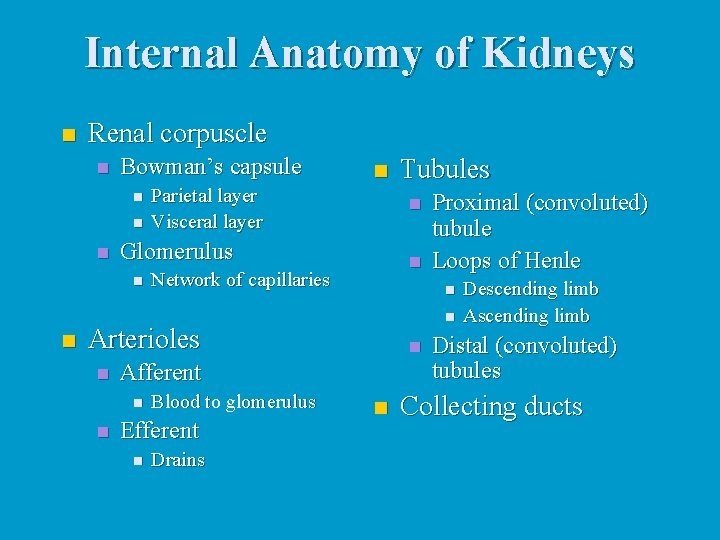
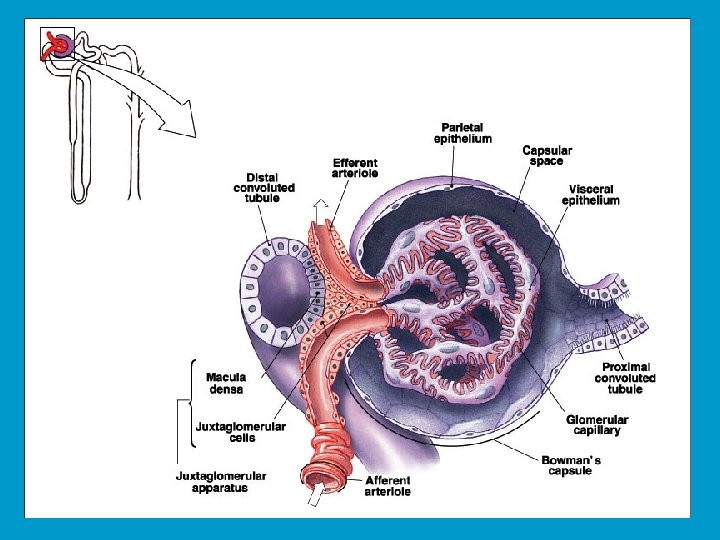
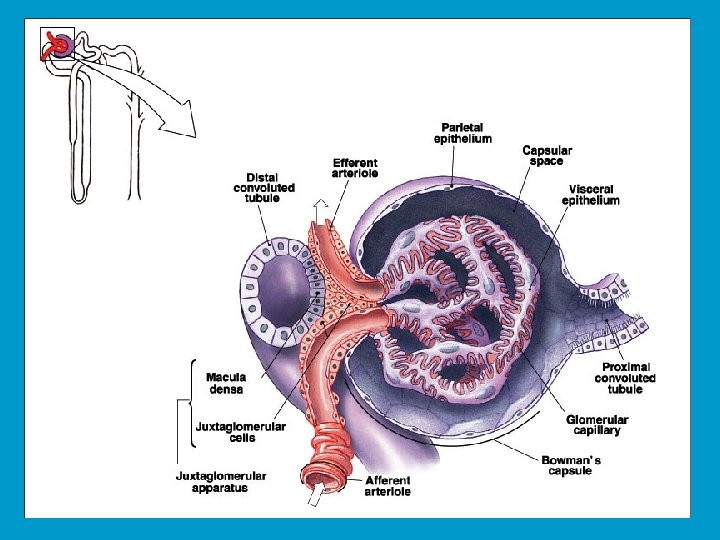
Internal Anatomy of Kidneys n Renal corpuscle n Bowman’s capsule n n n Parietal layer Visceral layer n Network of capillaries n n n Afferent n Blood to glomerulus Efferent n Drains Proximal (convoluted) tubule Loops of Henle n Arterioles n Tubules n Glomerulus n n Descending limb Ascending limb Distal (convoluted) tubules Collecting ducts
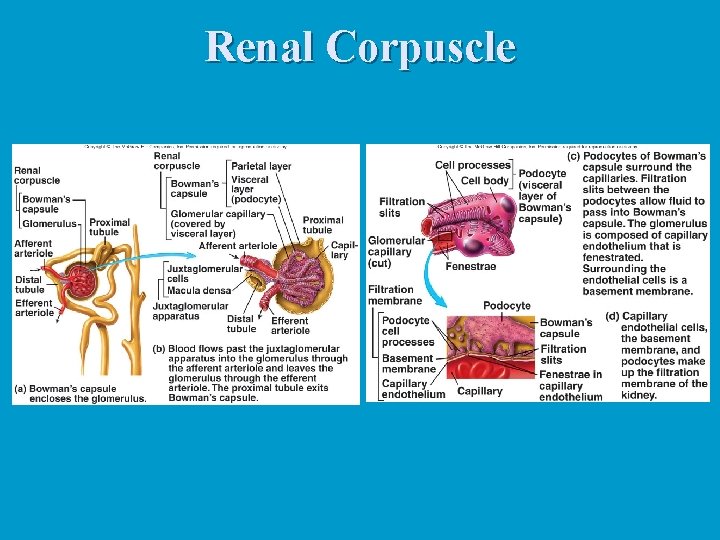
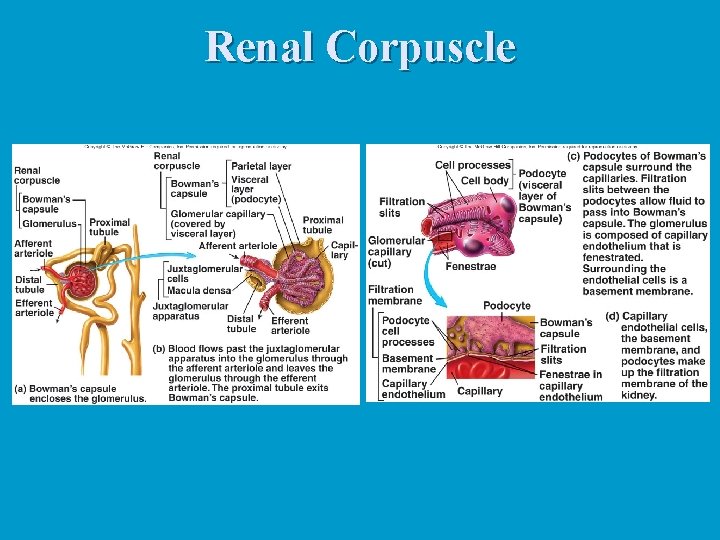
Renal Corpuscle
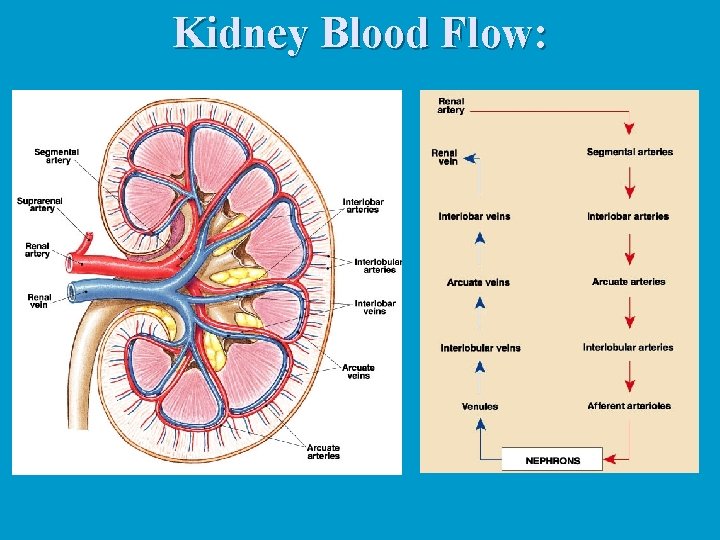
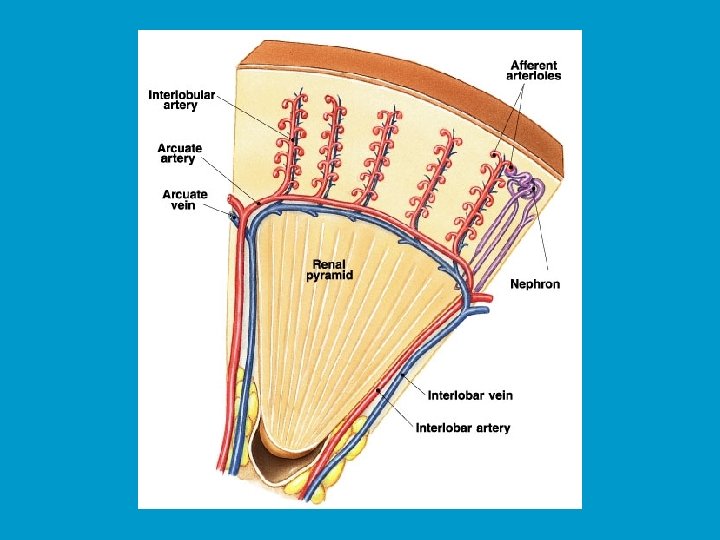
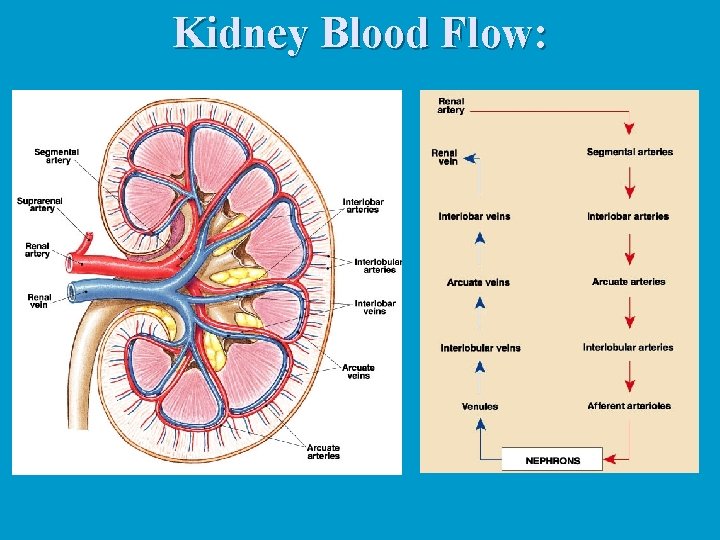
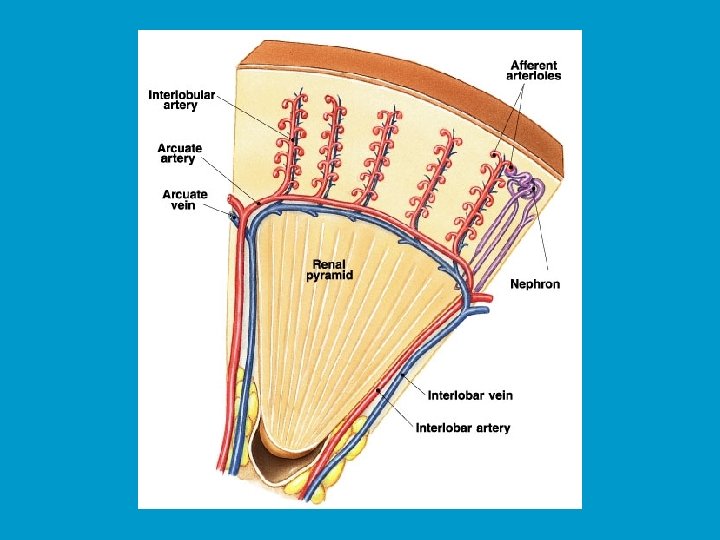
Kidney Blood Flow:
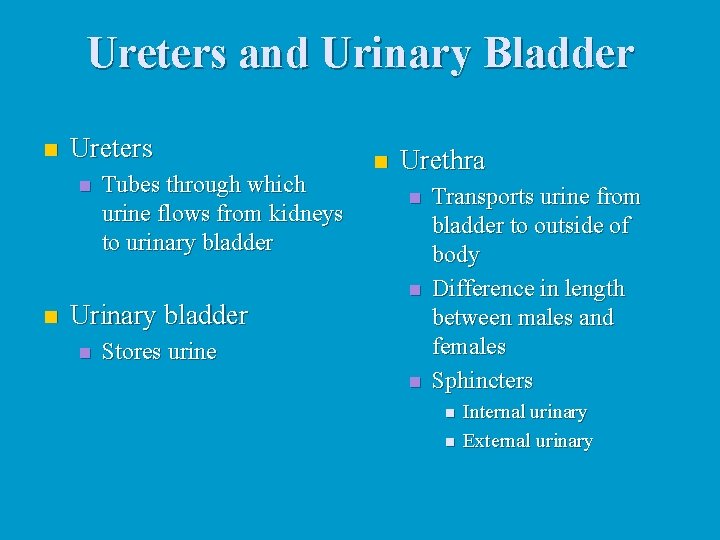
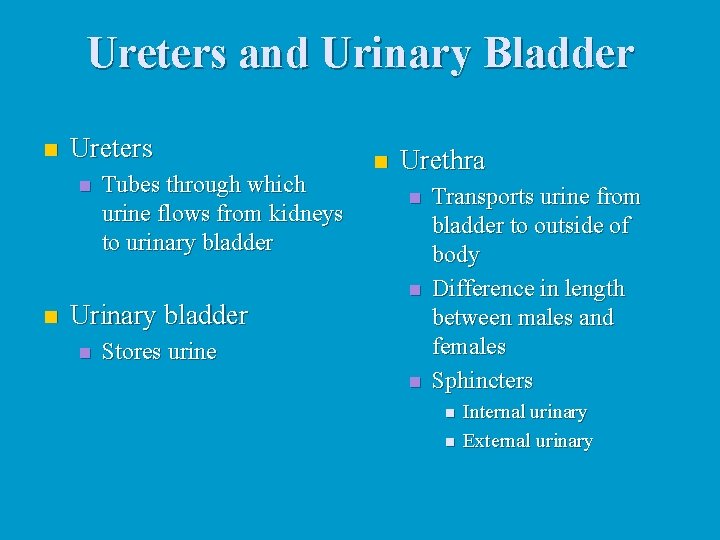
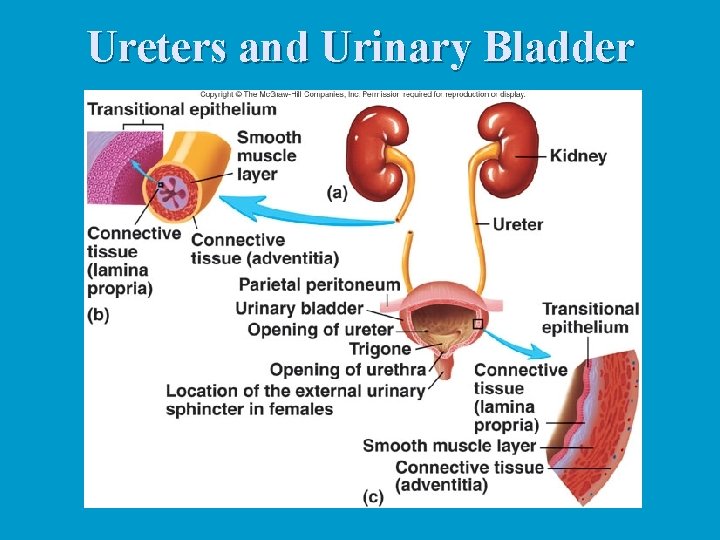
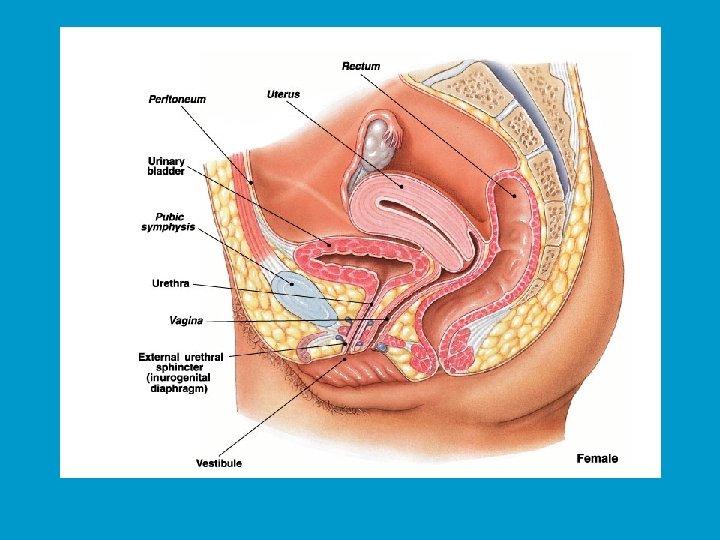
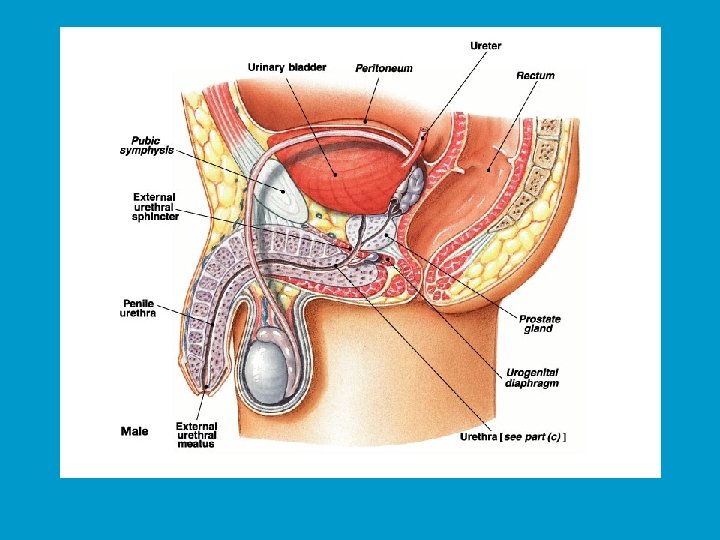
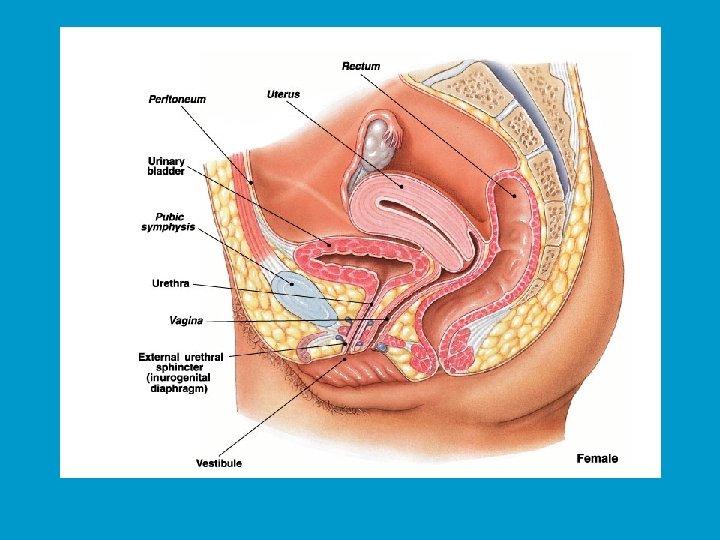
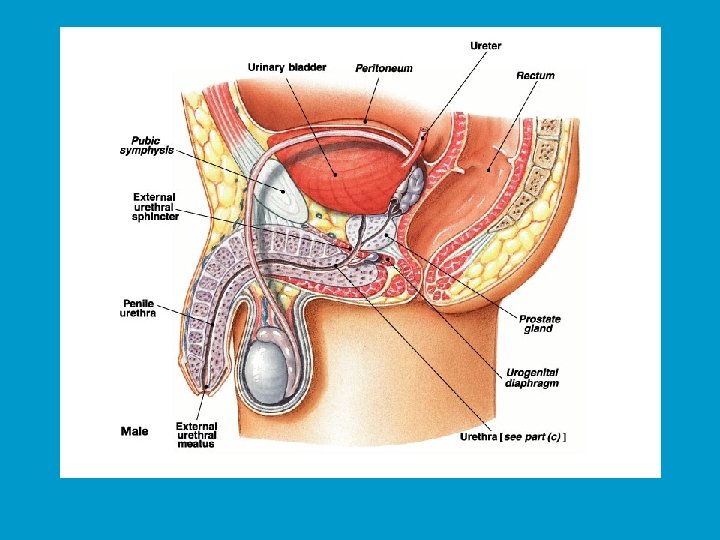
Ureters and Urinary Bladder n Ureters n n Tubes through which urine flows from kidneys to urinary bladder Urinary bladder n n Urethra n n Stores urine n Transports urine from bladder to outside of body Difference in length between males and females Sphincters n n Internal urinary External urinary
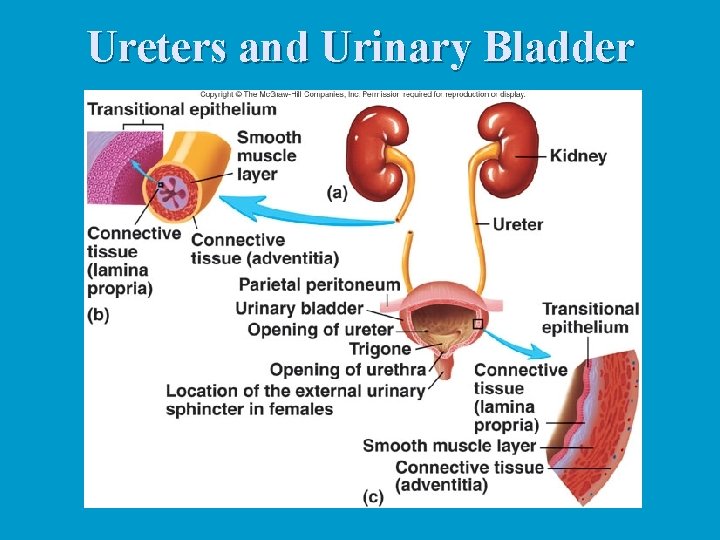
Ureters and Urinary Bladder
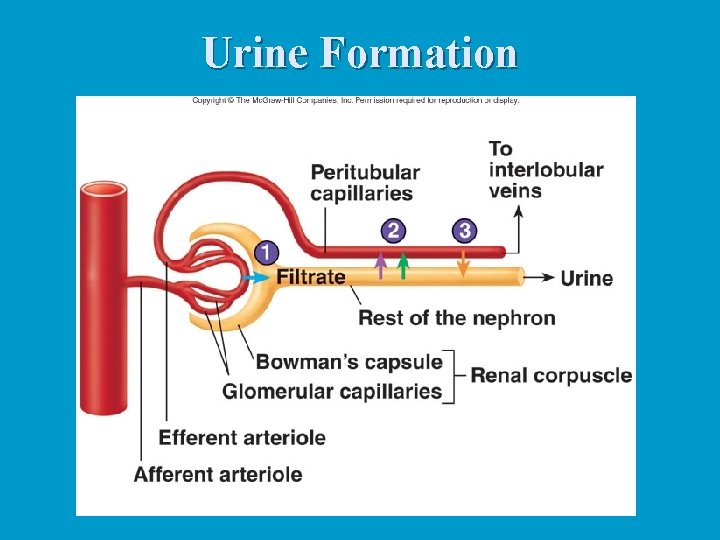
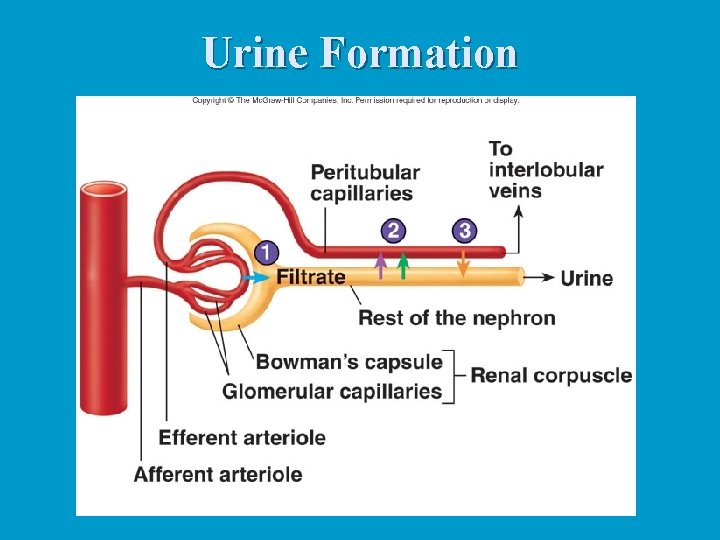
Urine Formation
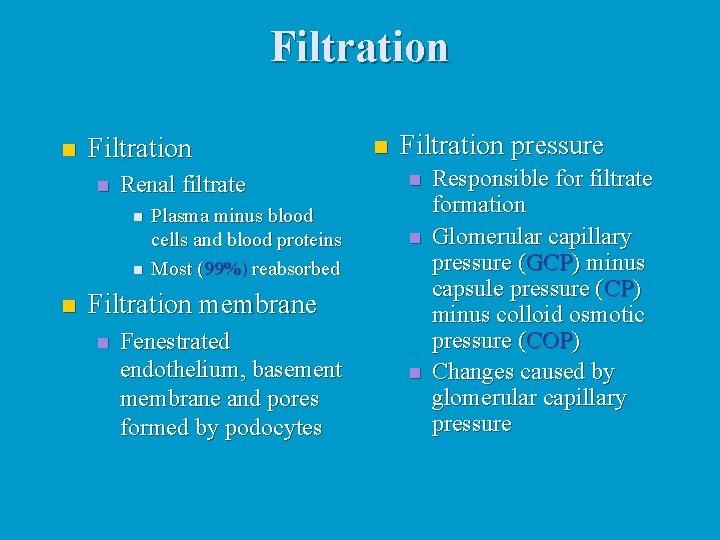
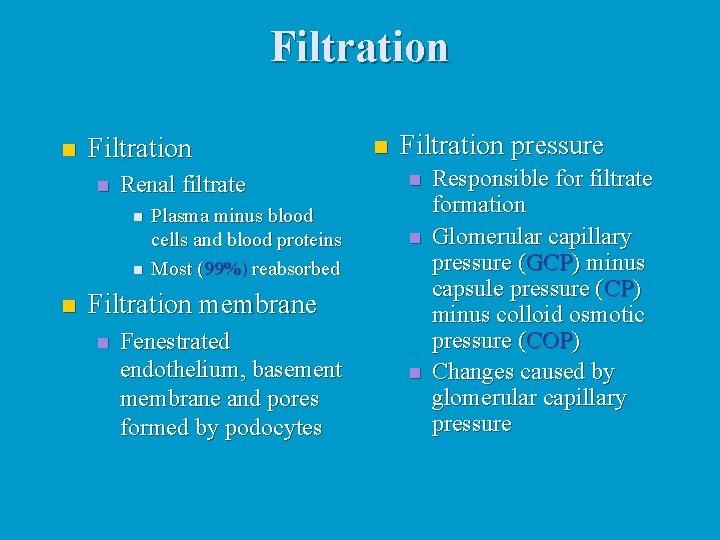
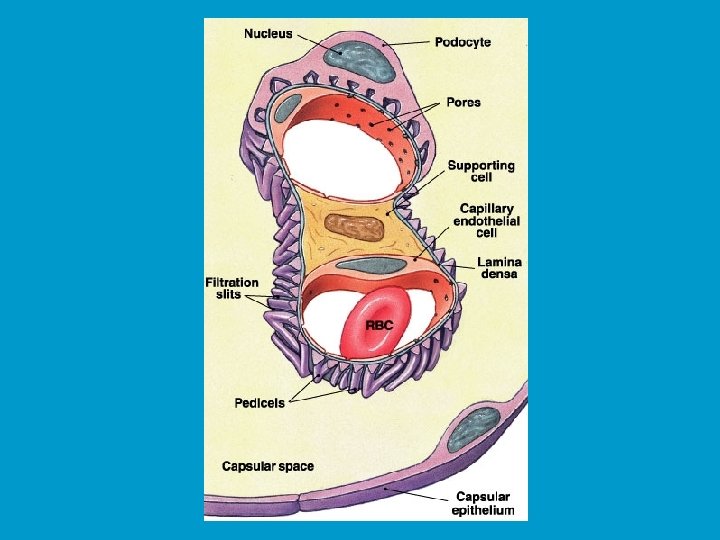
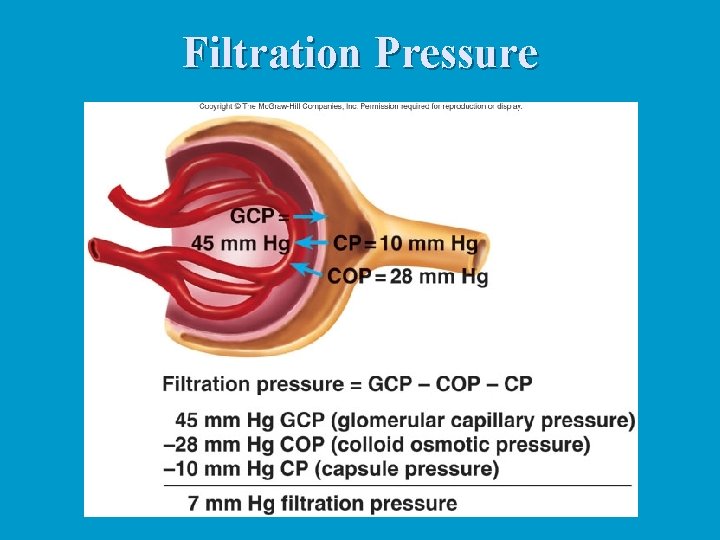
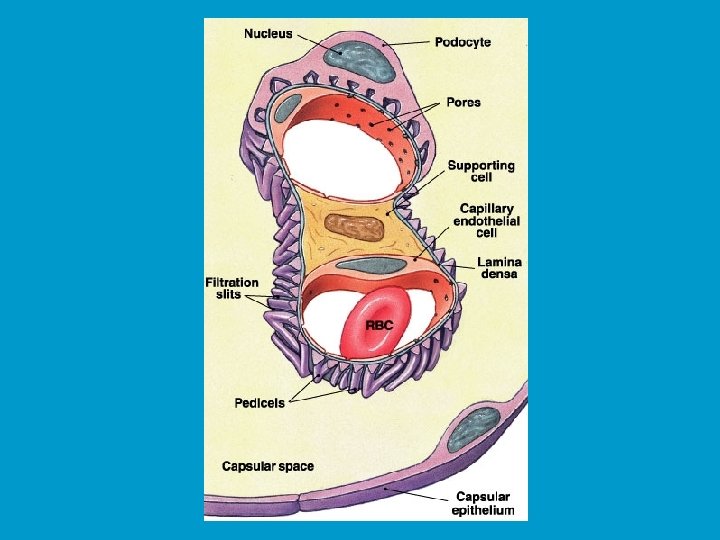
Filtration n Renal filtrate n n n Plasma minus blood cells and blood proteins Most (99%) reabsorbed n Filtration pressure n n Filtration membrane n Fenestrated endothelium, basement membrane and pores formed by podocytes n Responsible for filtrate formation Glomerular capillary pressure (GCP) minus capsule pressure (CP) minus colloid osmotic pressure (COP) Changes caused by glomerular capillary pressure
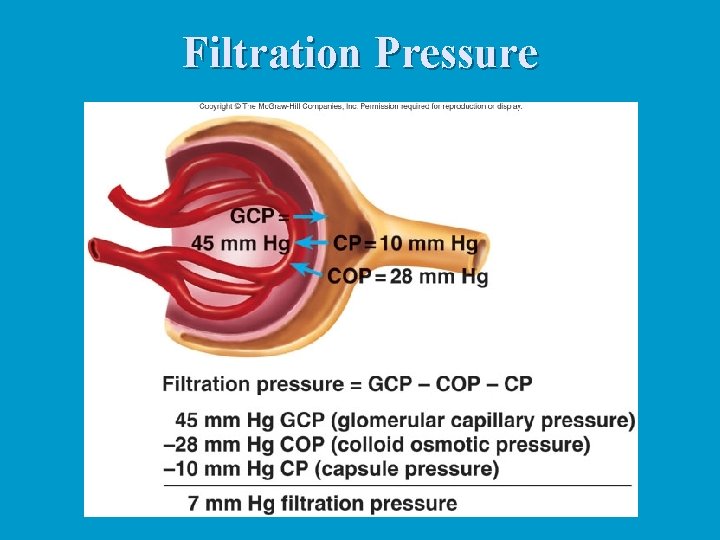
Filtration Pressure
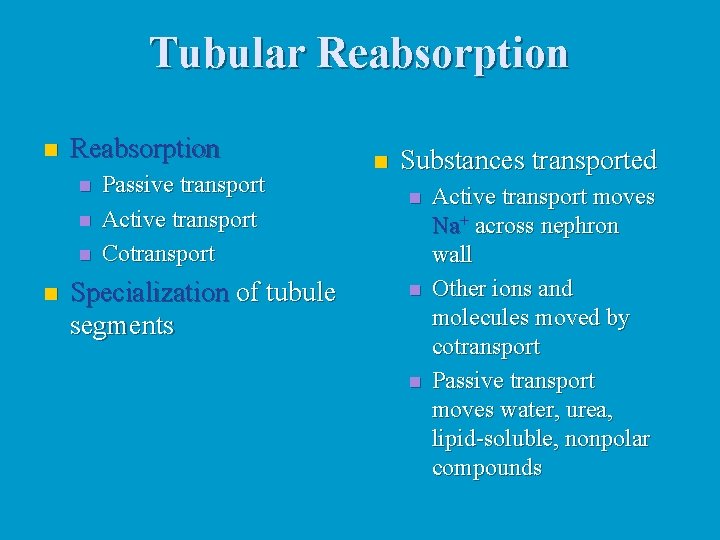
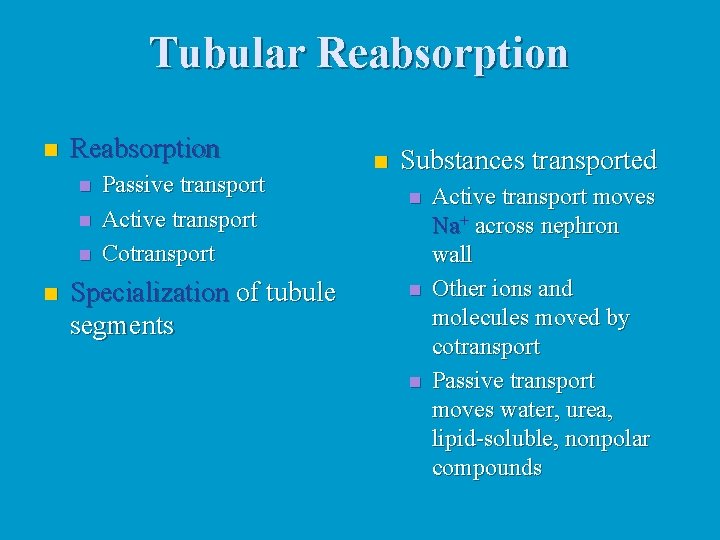
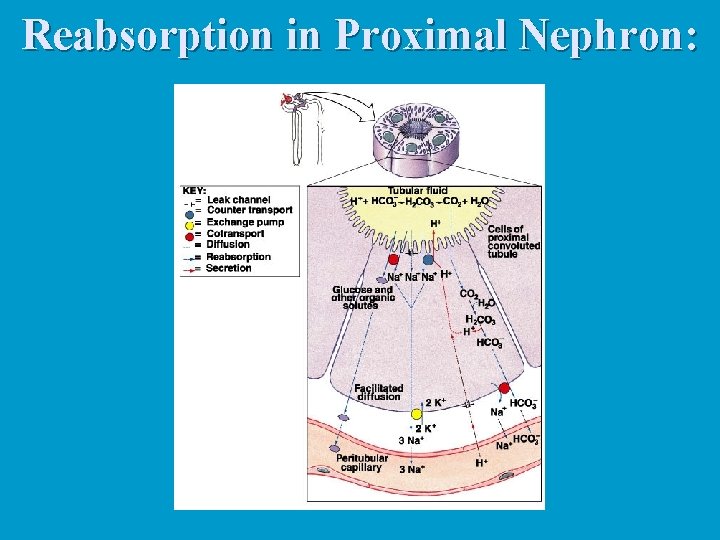
Tubular Reabsorption n n n n Passive transport Active transport Cotransport Specialization of tubule segments n Substances transported n n n Active transport moves Na+ across nephron wall Other ions and molecules moved by cotransport Passive transport moves water, urea, lipid-soluble, nonpolar compounds
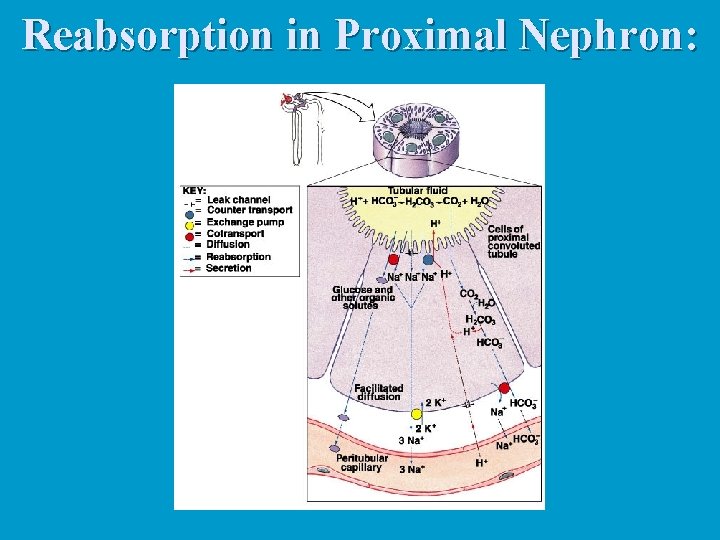
Reabsorption in Proximal Nephron:
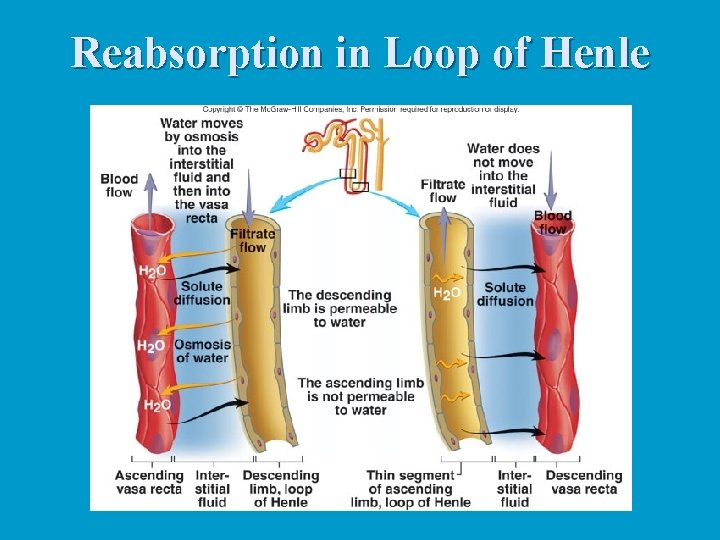
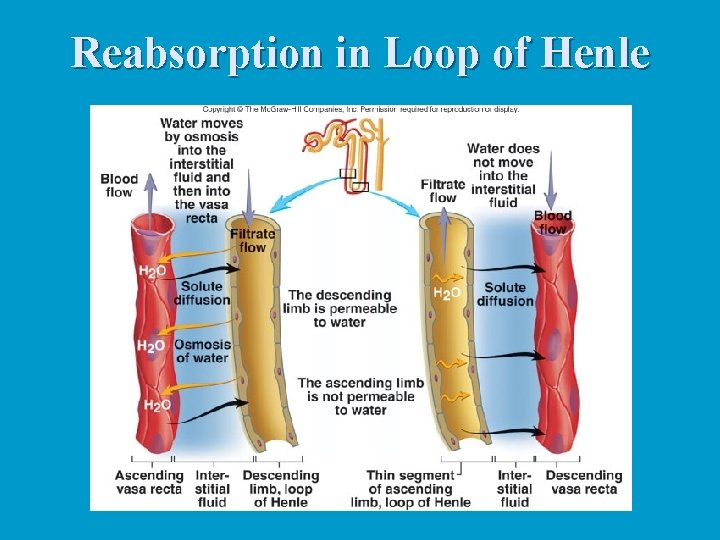
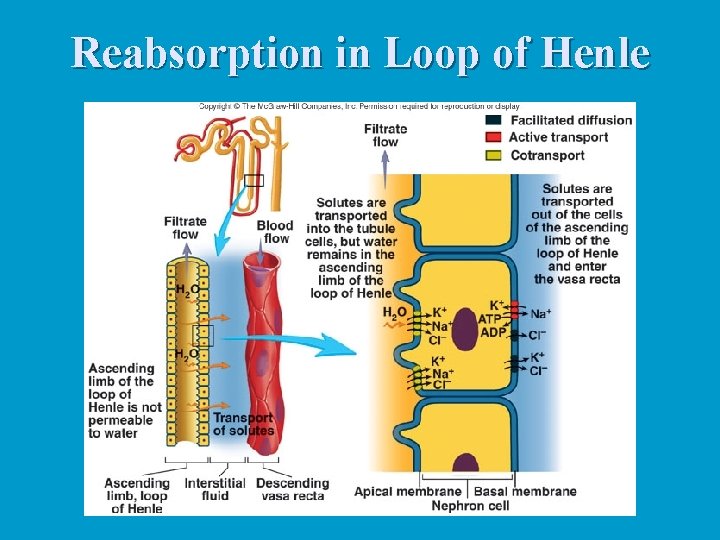
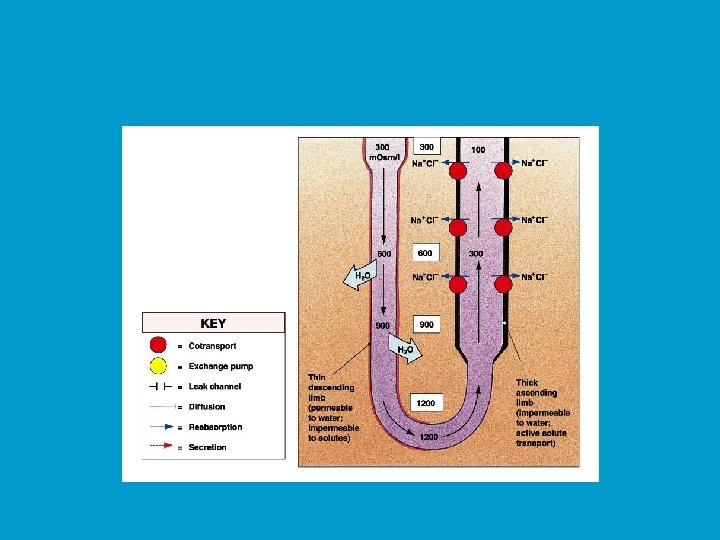
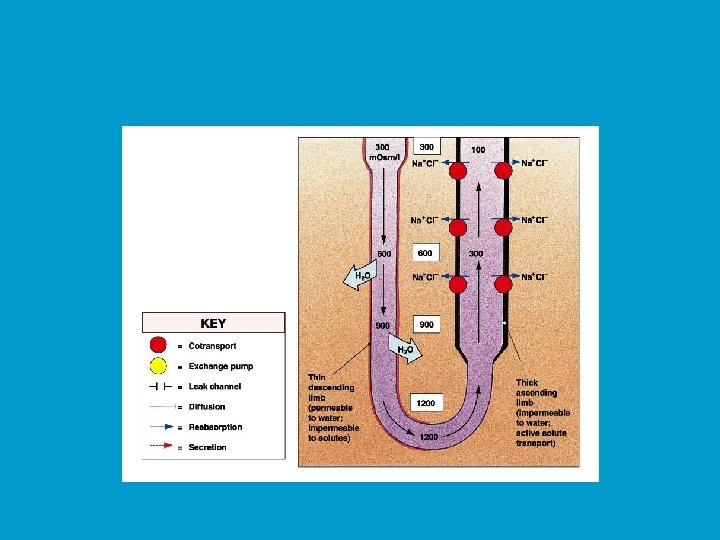
Reabsorption in Loop of Henle
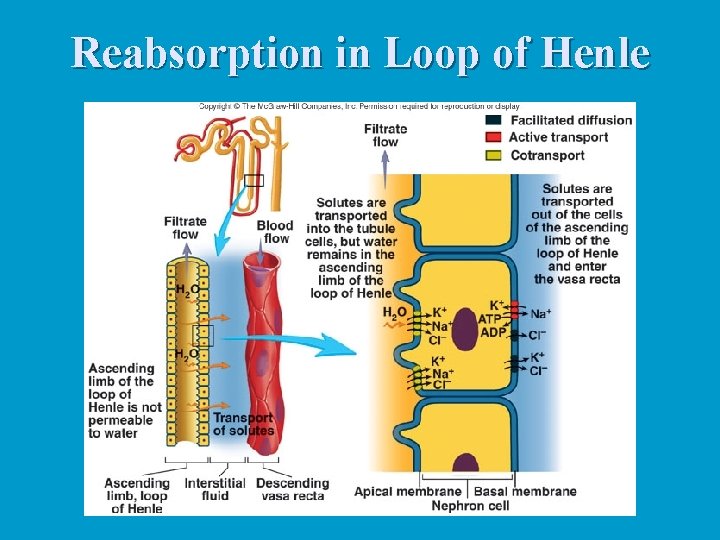
Reabsorption in Loop of Henle
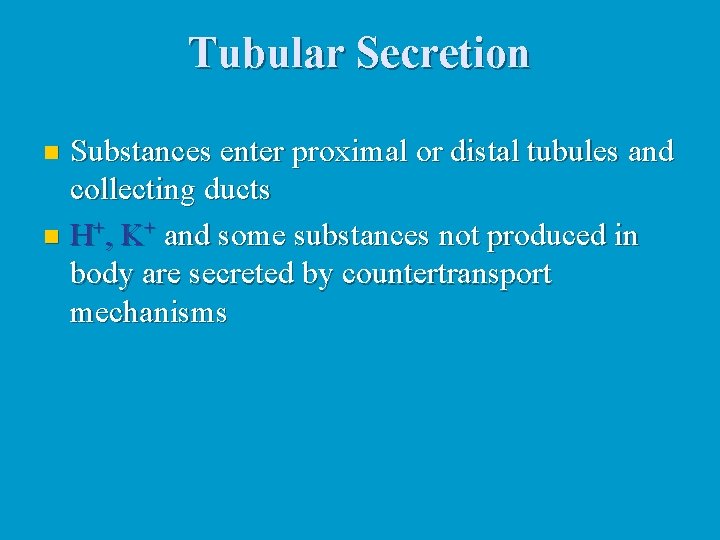
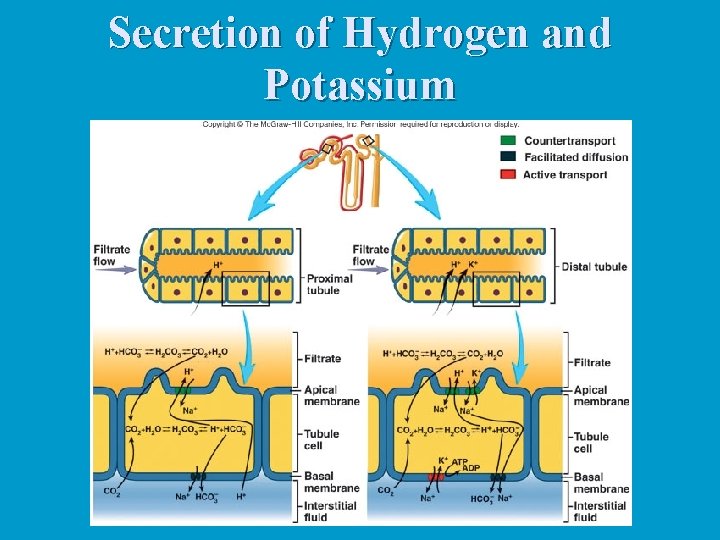
Tubular Secretion Substances enter proximal or distal tubules and collecting ducts n H+, K+ and some substances not produced in body are secreted by countertransport mechanisms n
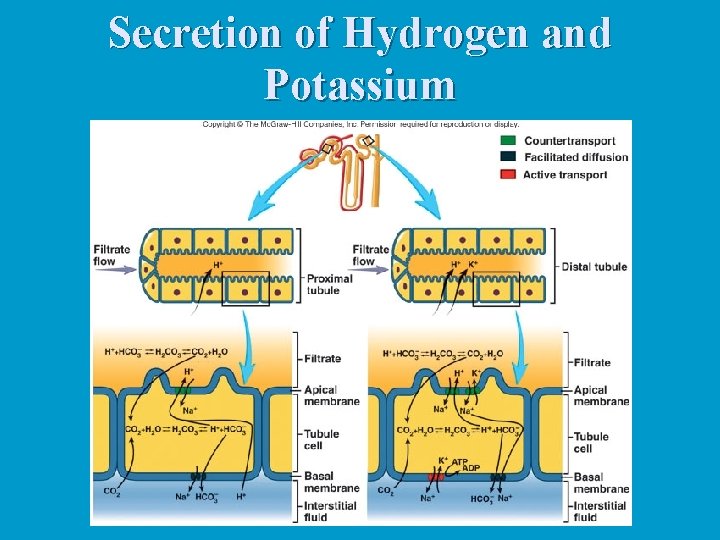
Secretion of Hydrogen and Potassium
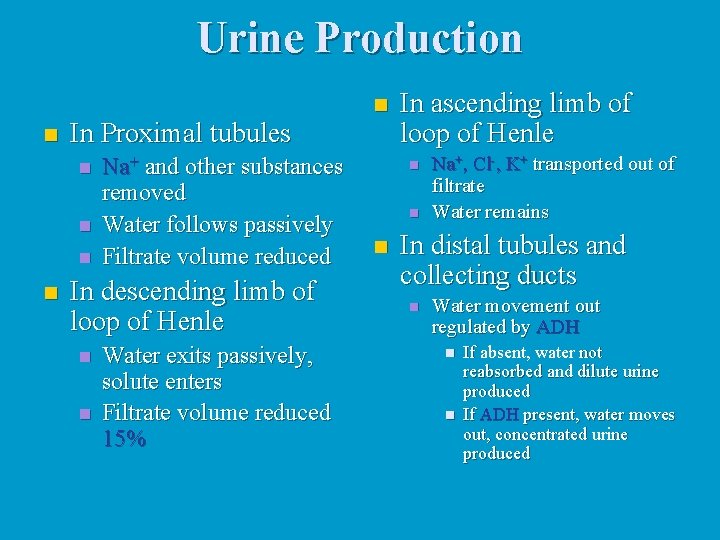
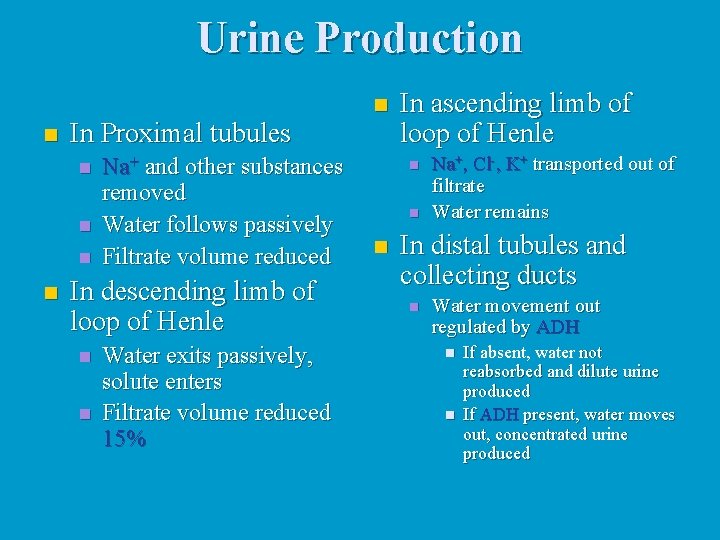
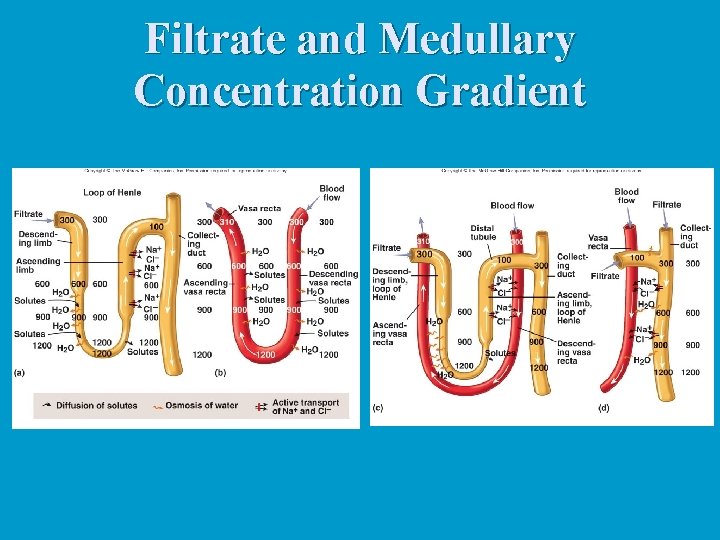
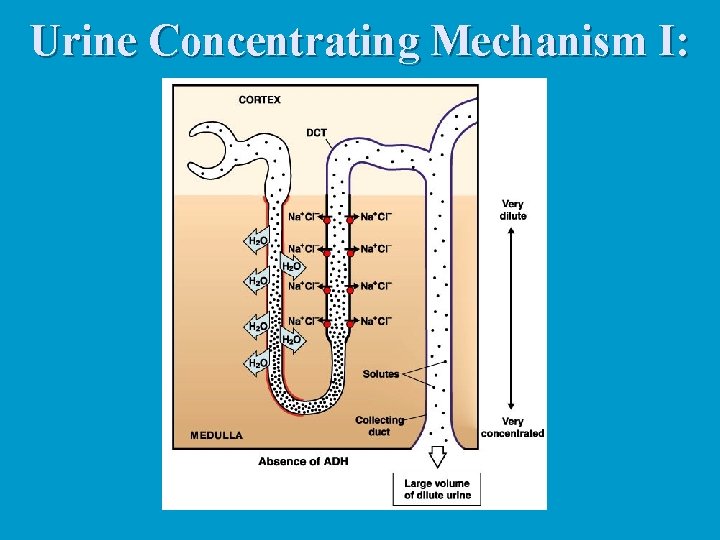
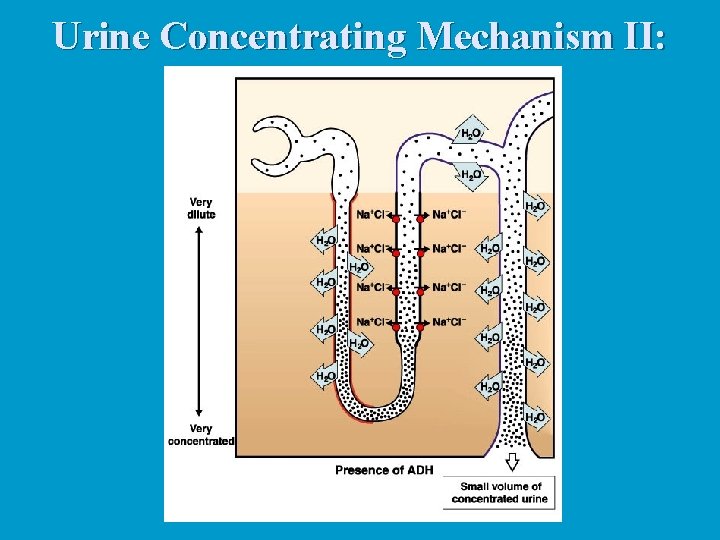
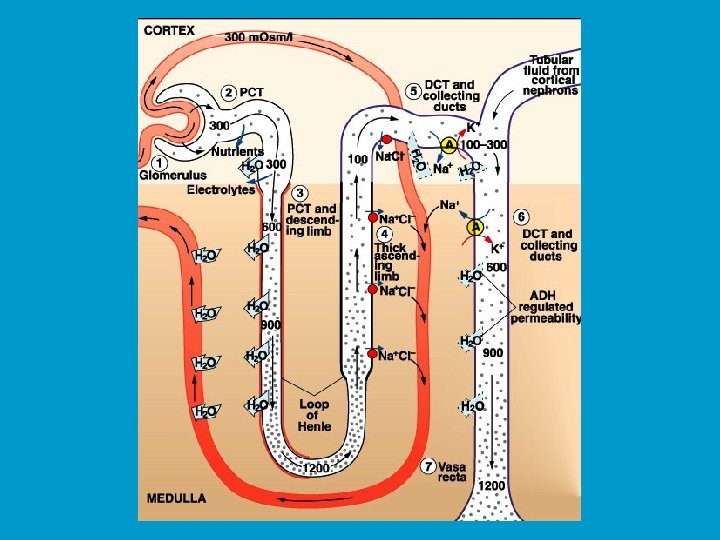
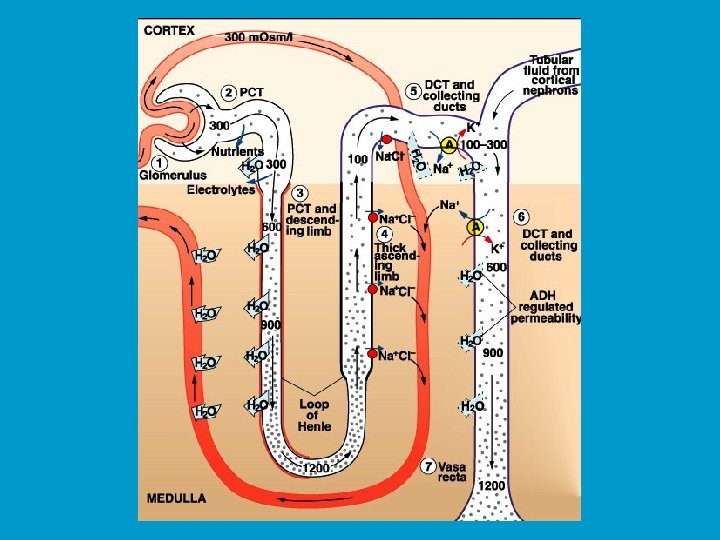
Urine Production n n In Proximal tubules n n Na+ and other substances removed Water follows passively Filtrate volume reduced In descending limb of loop of Henle n n Water exits passively, solute enters Filtrate volume reduced 15% In ascending limb of loop of Henle n n n Na+, Cl-, K+ transported out of filtrate Water remains In distal tubules and collecting ducts n Water movement out regulated by ADH n n If absent, water not reabsorbed and dilute urine produced If ADH present, water moves out, concentrated urine produced
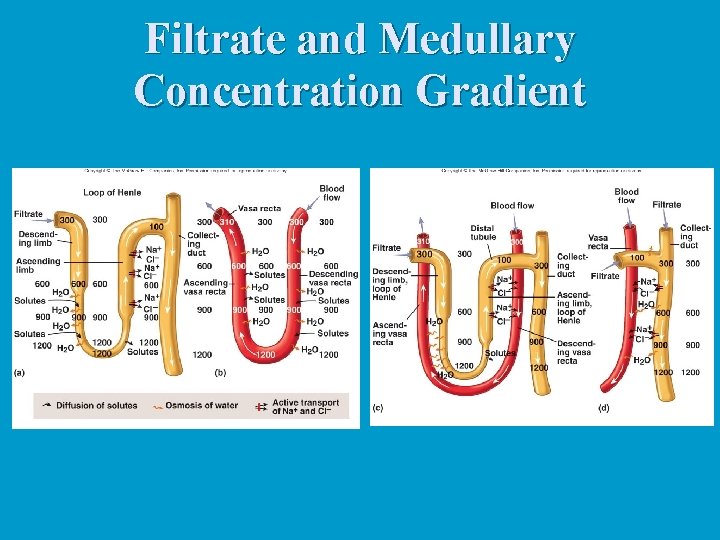
Filtrate and Medullary Concentration Gradient
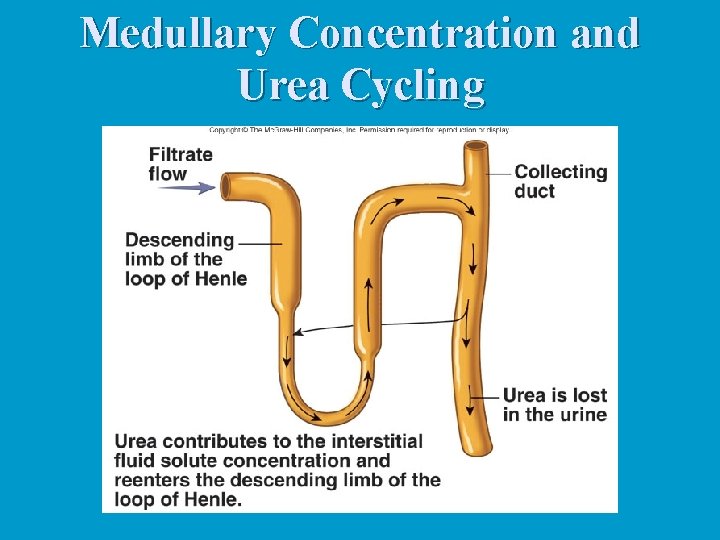
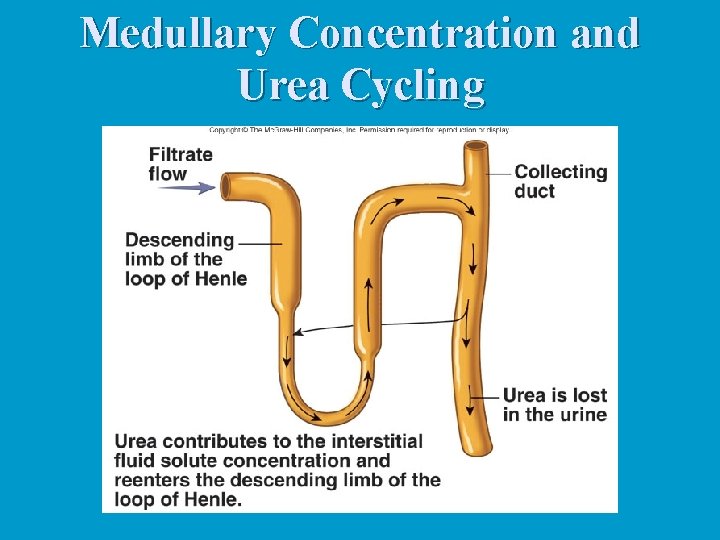
Medullary Concentration and Urea Cycling
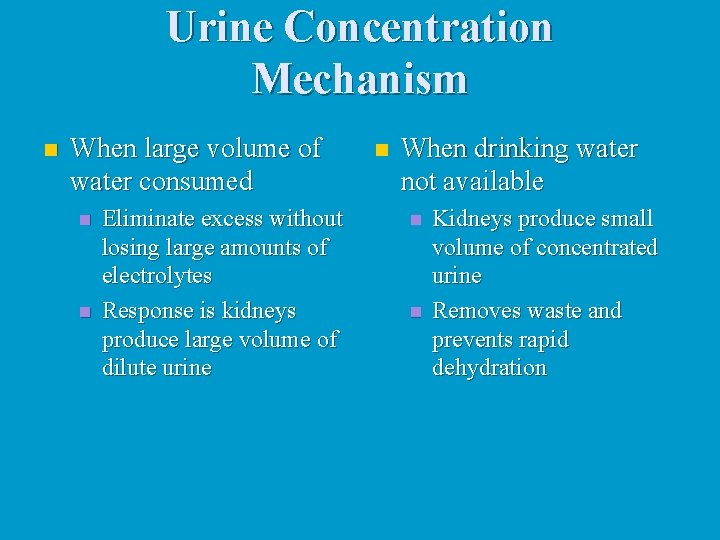
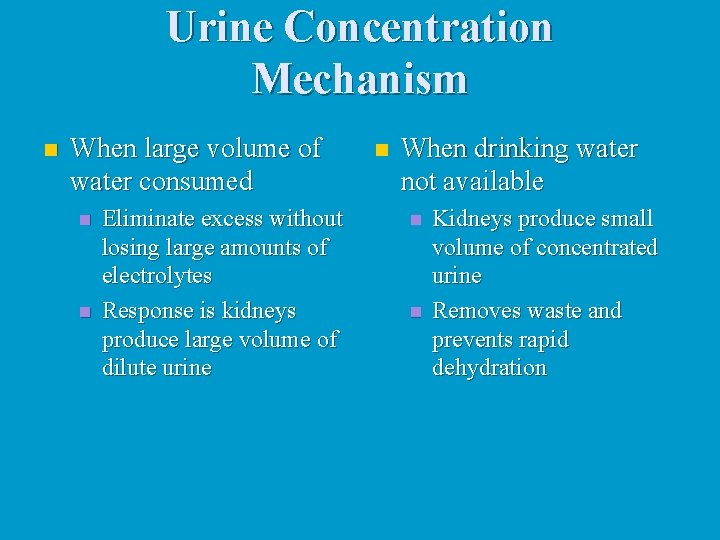
Urine Concentration Mechanism n When large volume of water consumed n n Eliminate excess without losing large amounts of electrolytes Response is kidneys produce large volume of dilute urine n When drinking water not available n n Kidneys produce small volume of concentrated urine Removes waste and prevents rapid dehydration
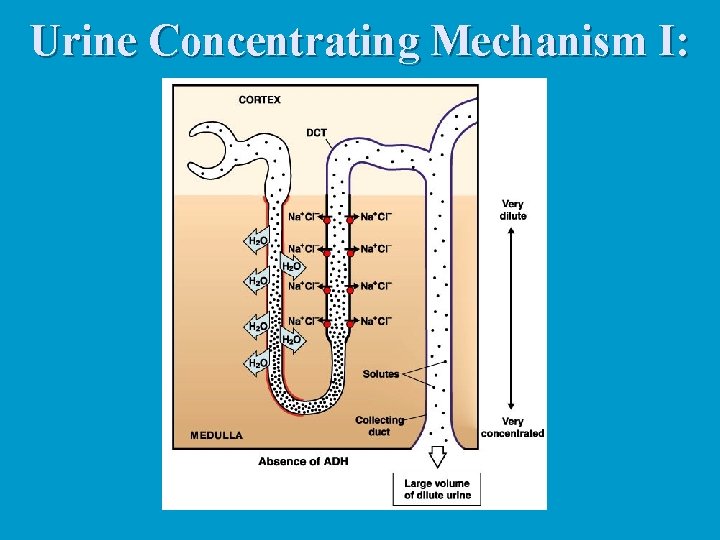
Urine Concentrating Mechanism I:
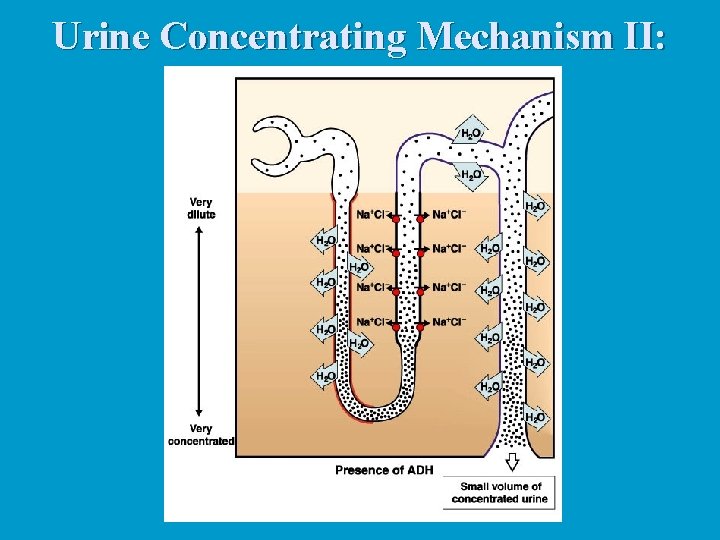
Urine Concentrating Mechanism II:
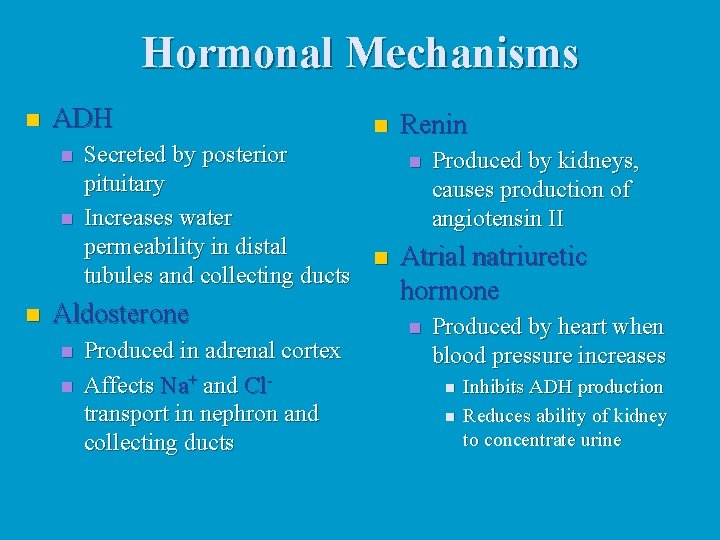
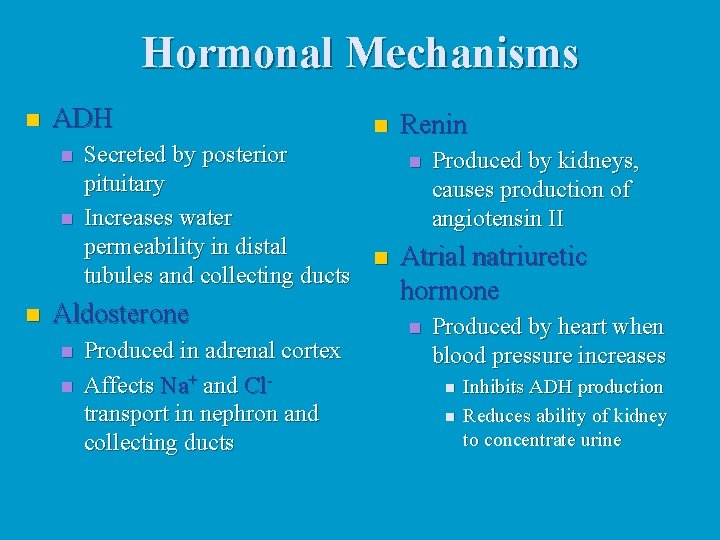
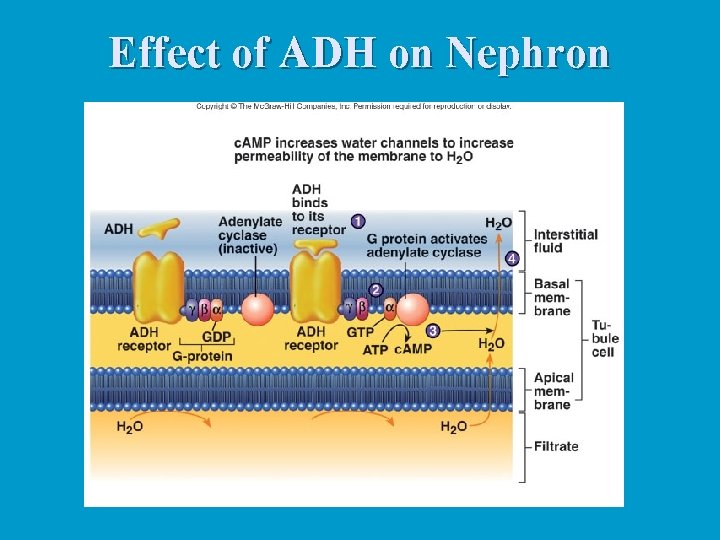
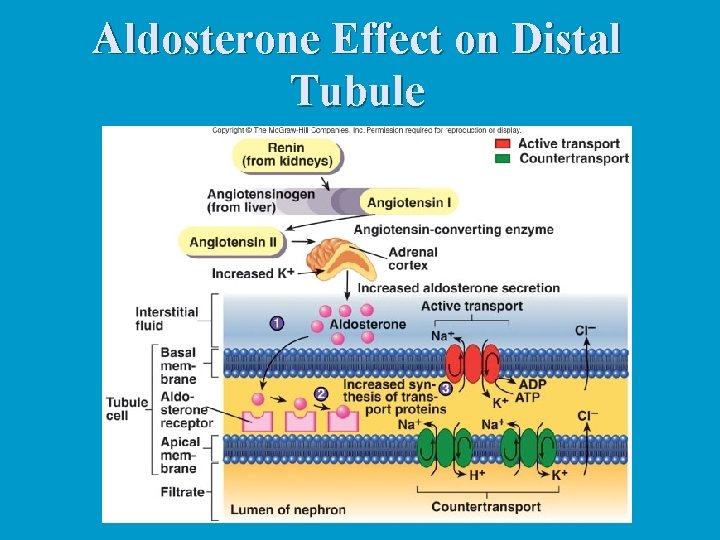
Hormonal Mechanisms n ADH n n Renin Secreted by posterior n Produced by kidneys, pituitary causes production of Increases water angiotensin II permeability in distal n Atrial natriuretic tubules and collecting ducts Aldosterone n n Produced in adrenal cortex Affects Na+ and Cltransport in nephron and collecting ducts hormone n Produced by heart when blood pressure increases n n Inhibits ADH production Reduces ability of kidney to concentrate urine
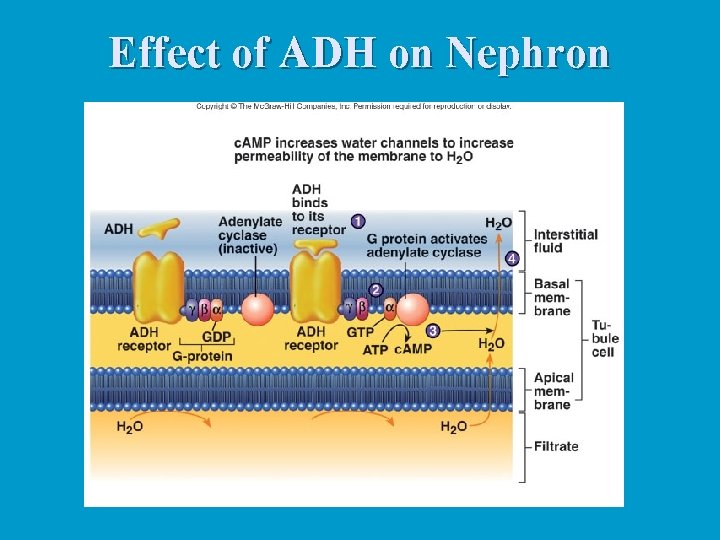
Effect of ADH on Nephron
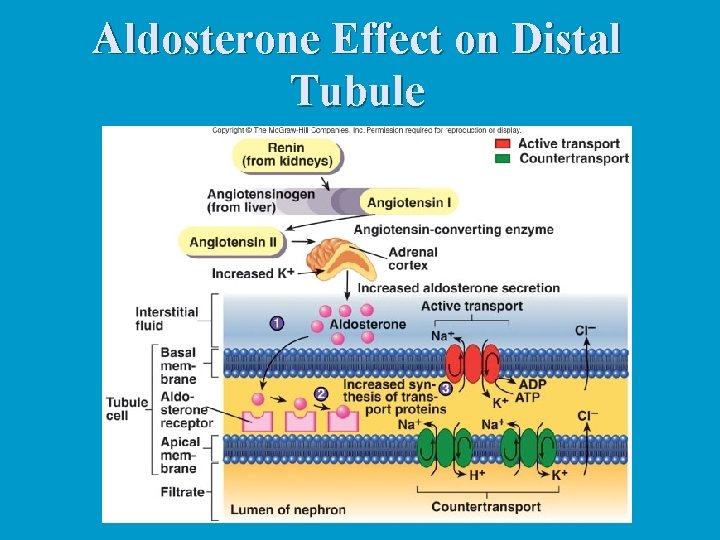
Aldosterone Effect on Distal Tubule
Autoregulation and Sympathetic Stimulation n Autoregulation n n Involves changes in degree of constriction in afferent arterioles As systemic BP increased, afferent arterioles constrict and prevent increase in renal blood flow n Sympathetic stimulation n n Constricts small arteries and afferent arterioles Decreases renal blood flow
Clearance and Tubular Load n Plasma clearance n n Volume of plasma cleared of a specific substance each minute Used to estimate GFR Used to calculate renal plasma flow Used to determine which drugs or other substances excreted by kidney n Tubular load n n Total amount of substance that passes through filtration membrane into nephrons each minute Normally glucose is almost completed reabsorbed
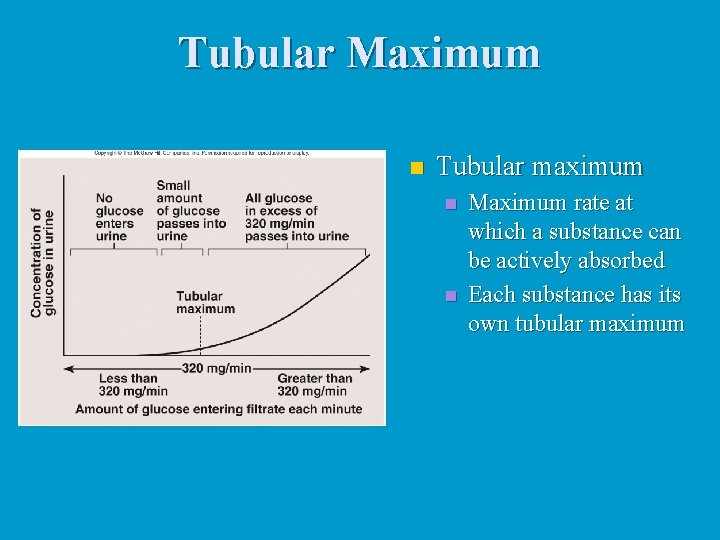
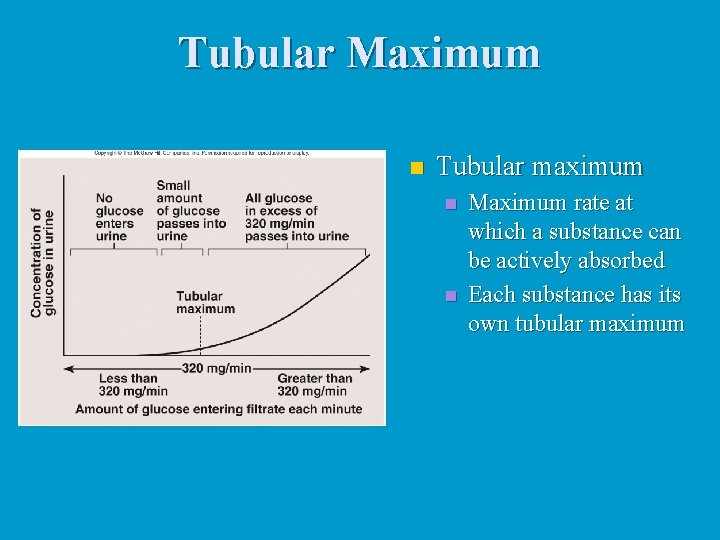
Tubular Maximum n Tubular maximum n n Maximum rate at which a substance can be actively absorbed Each substance has its own tubular maximum
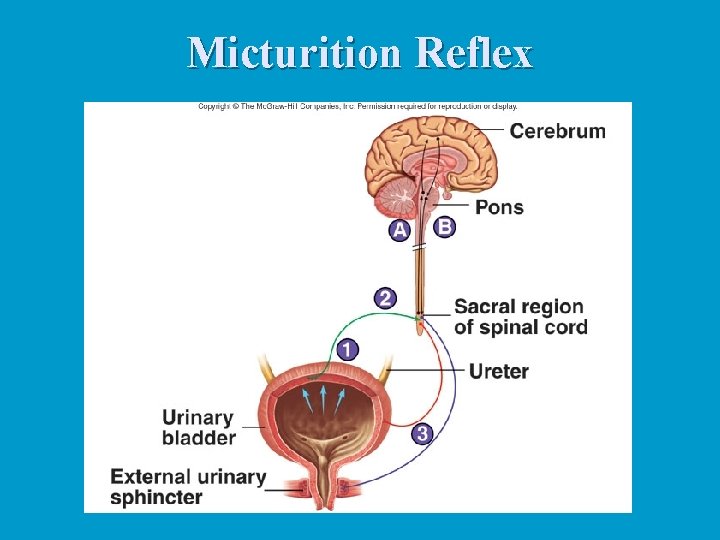
Urine Flow and Micturition Reflex n Urine flow n n Hydrostatic pressure forces urine through nephron Peristalsis moves urine through ureters n Micturition reflex n n Stretch of urinary bladder stimulates reflex causing bladder to contract, inhibiting urinary sphincters Higher brain centers can stimulate or inhibit reflex
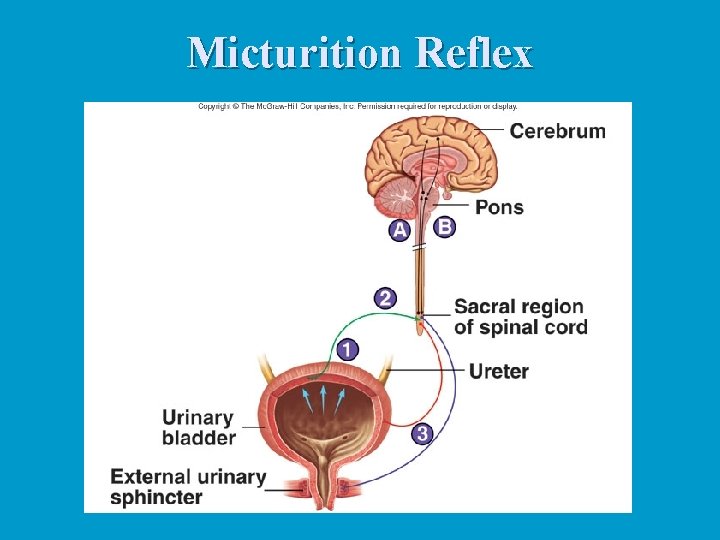
Micturition Reflex
Effects of Aging on Kidneys n Gradual decrease in size of kidney n Decrease in kidney size leads to decrease in renal blood flow Decrease in number of functional nephrons n Decrease in renin secretion and vitamin D synthesis n Decline in ability of nephron to secrete and absorb n
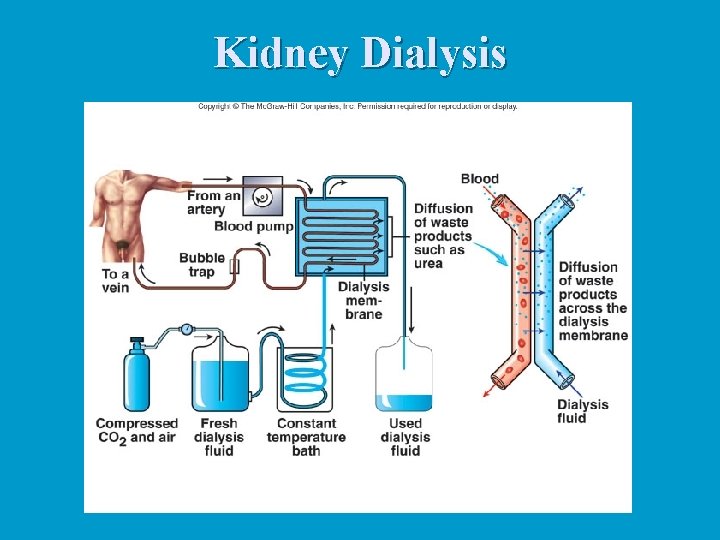
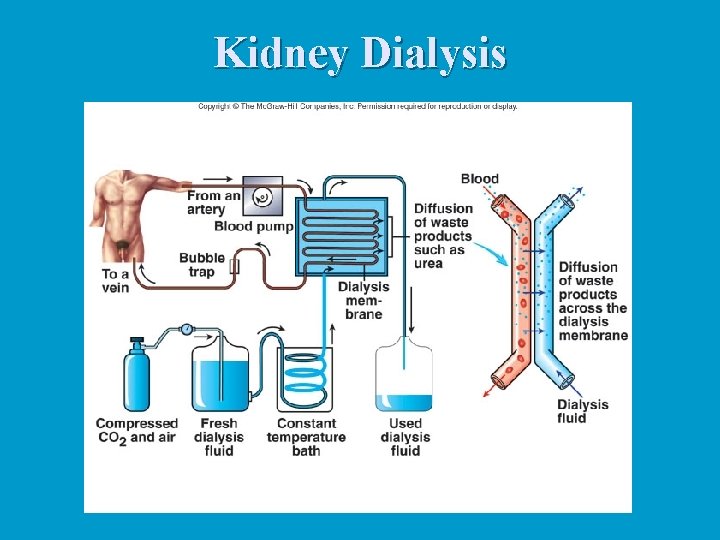
Kidney Dialysis