Chapter 26 Digestive System Part 2 Stomach Intestines

- Slides: 49
Chapter 26 Digestive System Part 2, Stomach, Intestines, Rectum

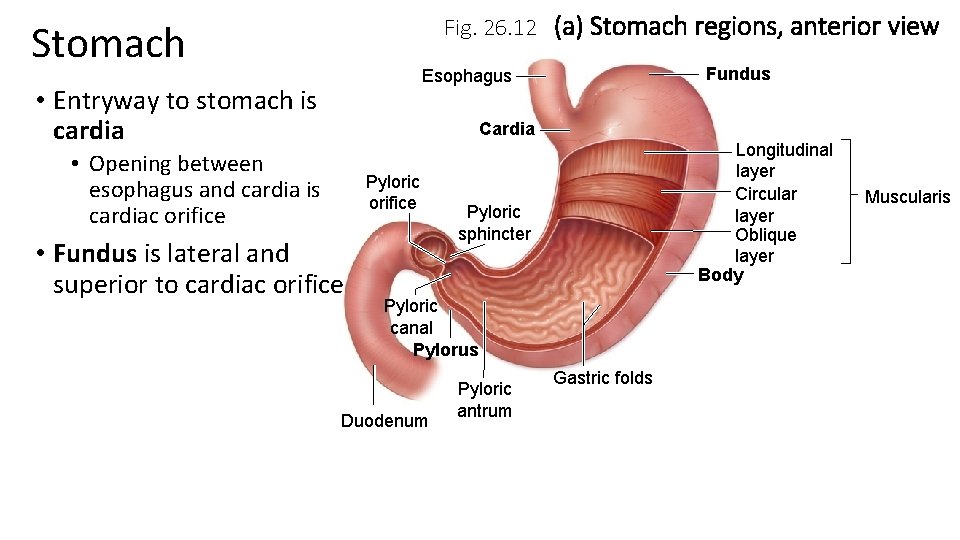
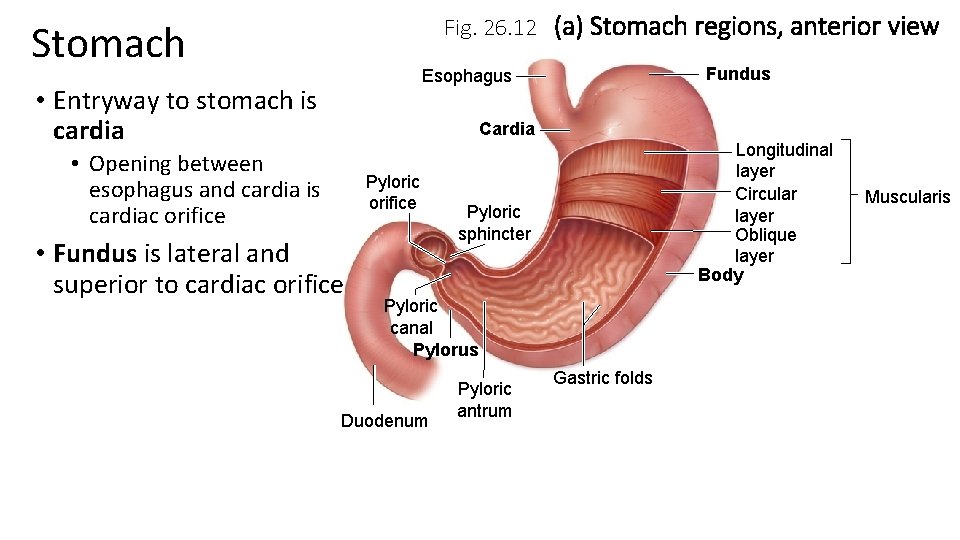
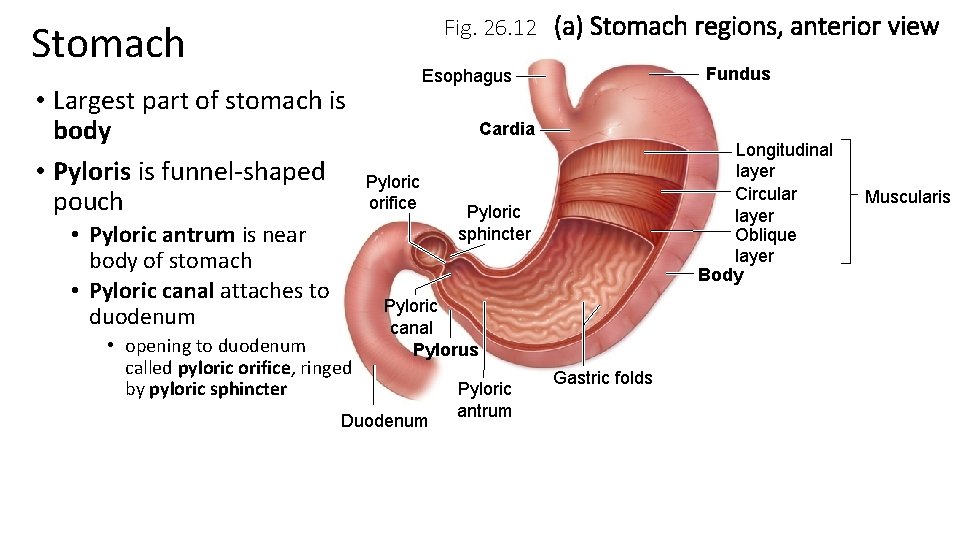
Fig. 26. 12 (a) Stomach regions, anterior view Stomach Fundus Esophagus • Entryway to stomach is cardia Cardia • Opening between esophagus and cardia is cardiac orifice Pyloric orifice • Fundus is lateral and superior to cardiac orifice Longitudinal layer Circular layer Oblique layer Body Pyloric sphincter Pyloric canal Pylorus Duodenum Pyloric antrum Gastric folds Muscularis
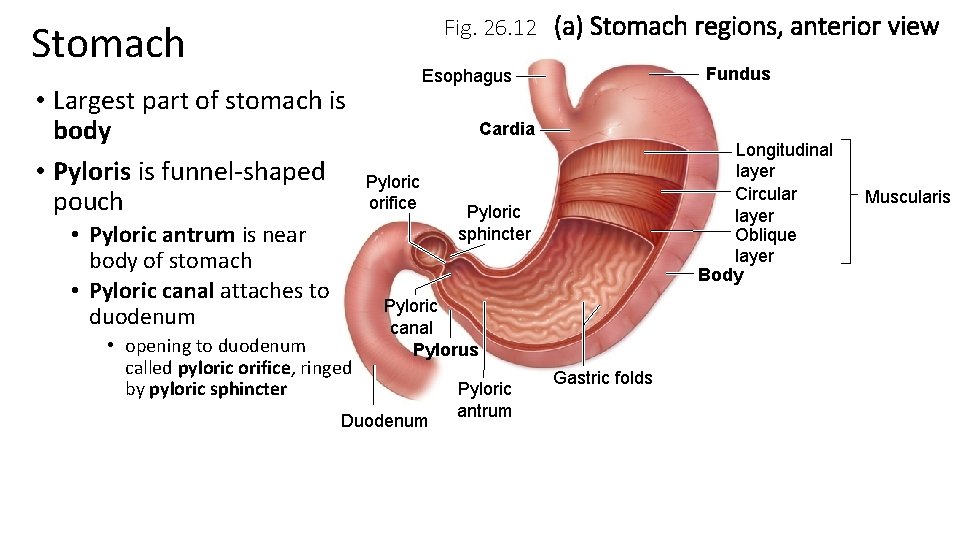
Fig. 26. 12 (a) Stomach regions, anterior view Stomach • Largest part of stomach is body • Pyloris is funnel-shaped pouch • Pyloric antrum is near body of stomach • Pyloric canal attaches to duodenum • opening to duodenum called pyloric orifice, ringed by pyloric sphincter Fundus Esophagus Cardia Pyloric orifice Longitudinal layer Circular layer Oblique layer Body Pyloric sphincter Pyloric canal Pylorus Duodenum Pyloric antrum Gastric folds Muscularis
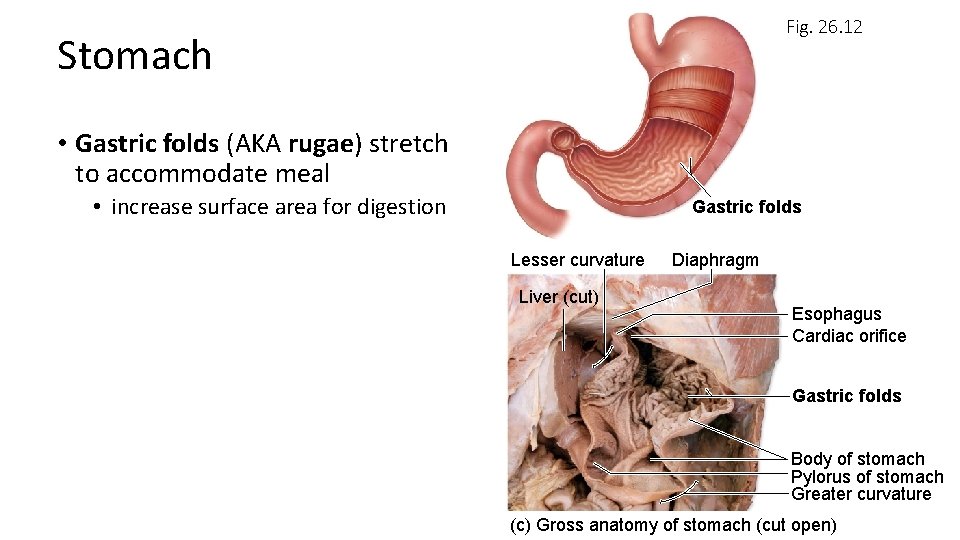
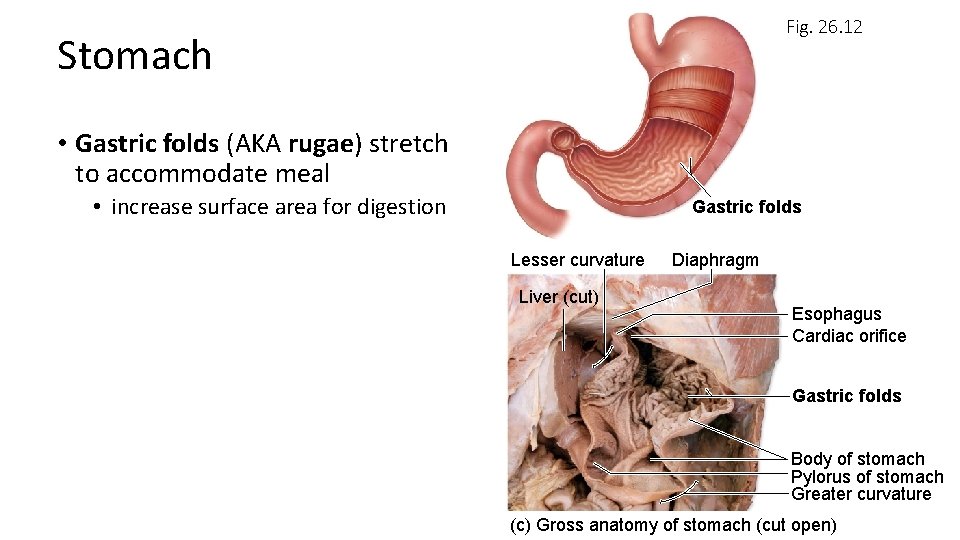
Fig. 26. 12 Stomach • Gastric folds (AKA rugae) stretch to accommodate meal • increase surface area for digestion Gastric folds Lesser curvature Liver (cut) Diaphragm Esophagus Cardiac orifice Gastric folds Body of stomach Pylorus of stomach Greater curvature (c) Gross anatomy of stomach (cut open)
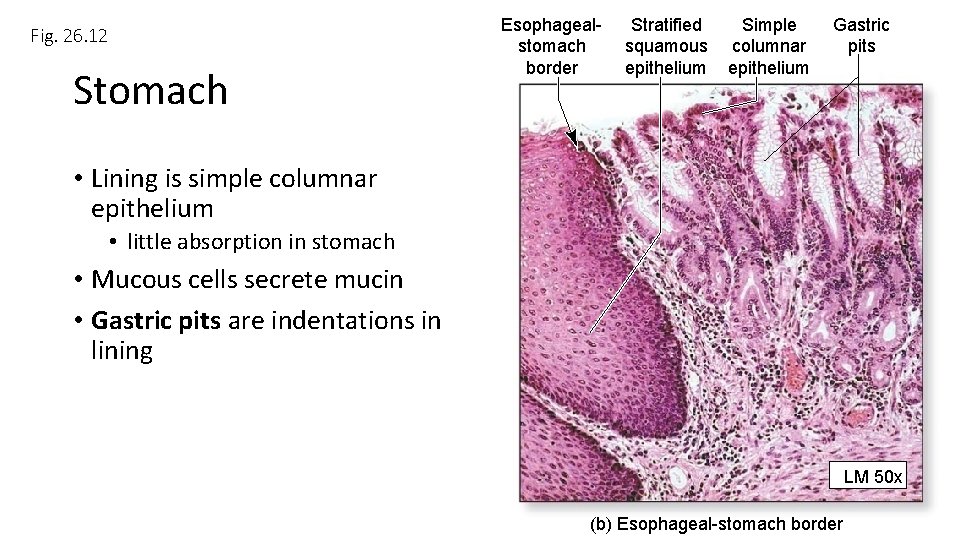
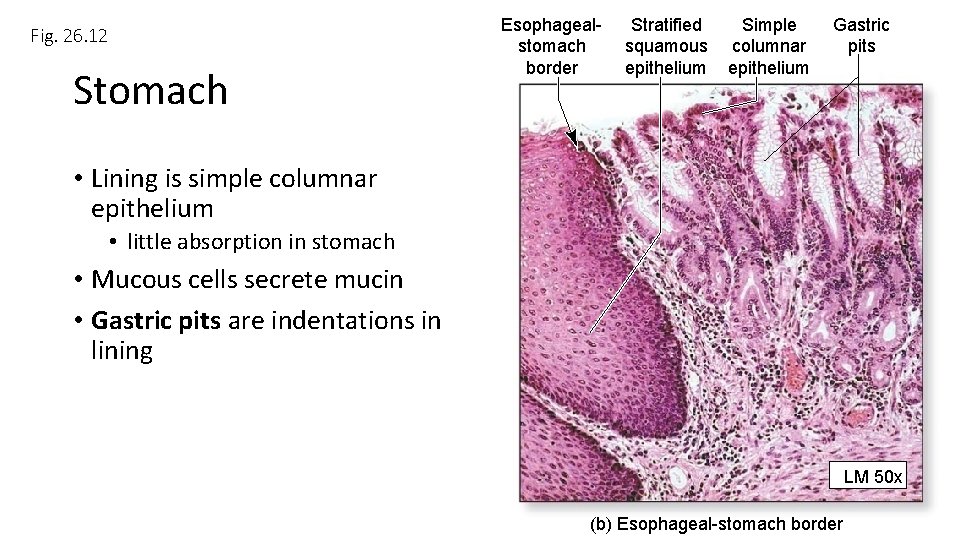
Fig. 26. 12 Stomach Esophagealstomach border Stratified Simple squamous columnar epithelium Gastric pits • Lining is simple columnar epithelium • little absorption in stomach • Mucous cells secrete mucin • Gastric pits are indentations in lining LM 50 x (b) Esophageal-stomach border
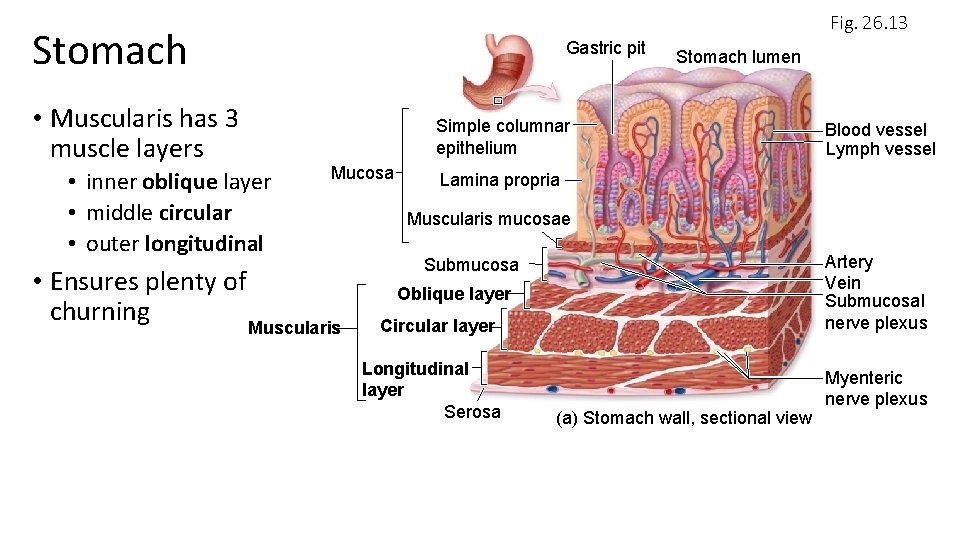
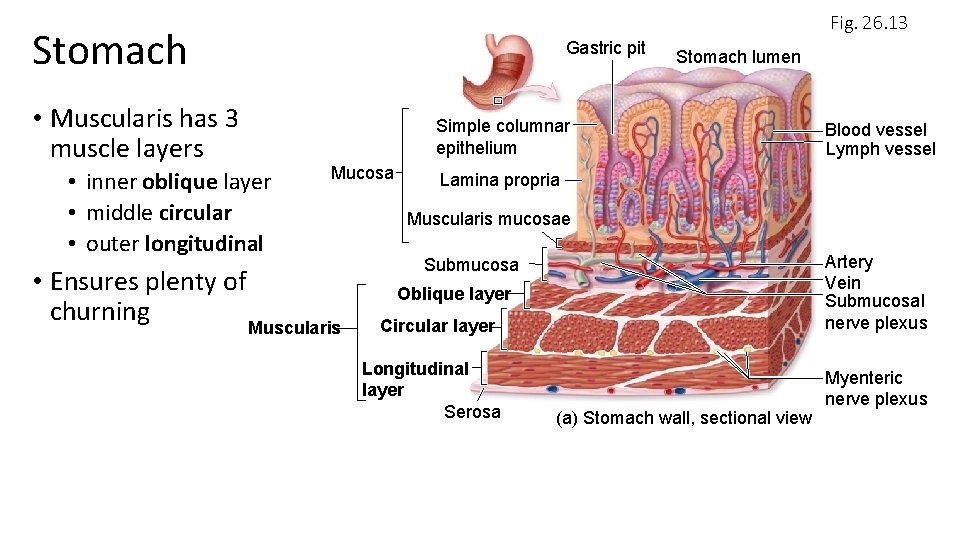
Fig. 26. 13 Stomach • Muscularis has 3 muscle layers • inner oblique layer • middle circular • outer longitudinal Gastric pit Stomach lumen Simple columnar epithelium Mucosa • Ensures plenty of churning Muscularis Blood vessel Lymph vessel Lamina propria Muscularis mucosae Artery Vein Submucosal nerve plexus Submucosa Oblique layer Circular layer Longitudinal layer Serosa (a) Stomach wall, sectional view Myenteric nerve plexus
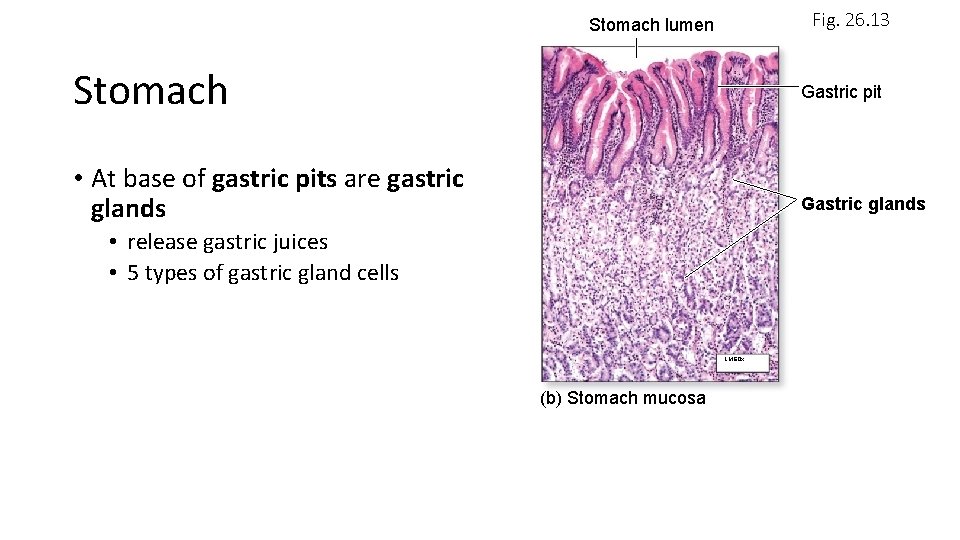
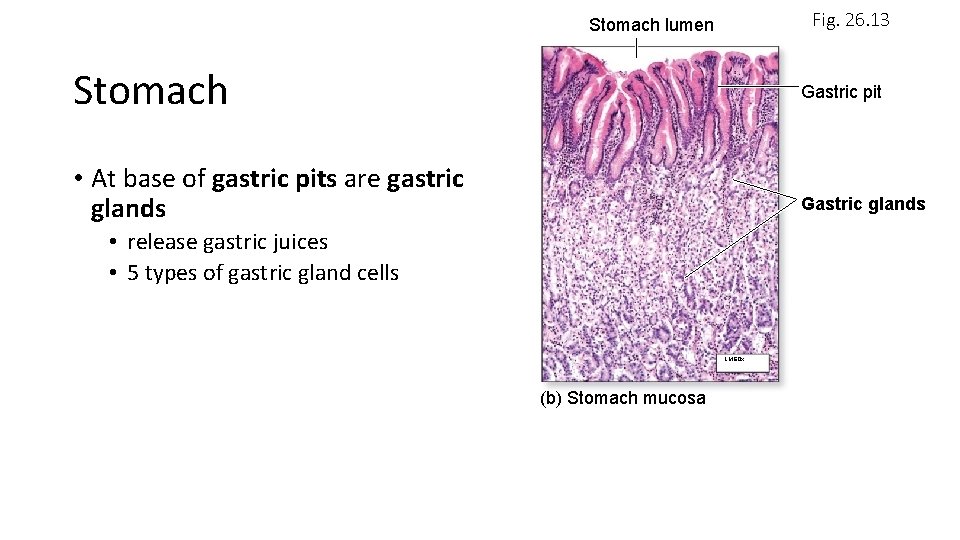
Fig. 26. 13 Stomach lumen Stomach Gastric pit • At base of gastric pits are gastric glands Gastric glands • release gastric juices • 5 types of gastric gland cells LM 60 x (b) Stomach mucosa
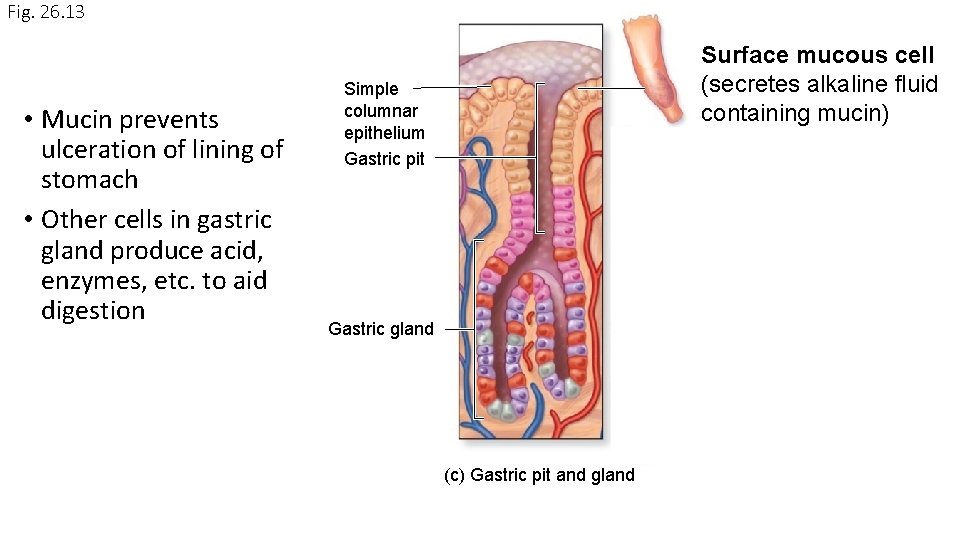
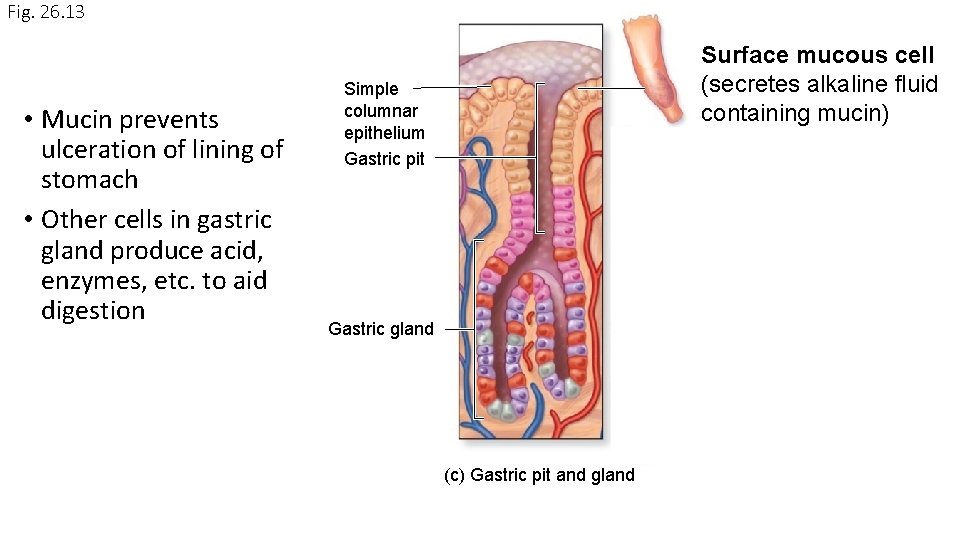
Fig. 26. 13 • Mucin prevents ulceration of lining of stomach • Other cells in gastric gland produce acid, enzymes, etc. to aid digestion Surface mucous cell (secretes alkaline fluid containing mucin) Simple columnar epithelium Gastric pit Gastric gland (c) Gastric pit and gland
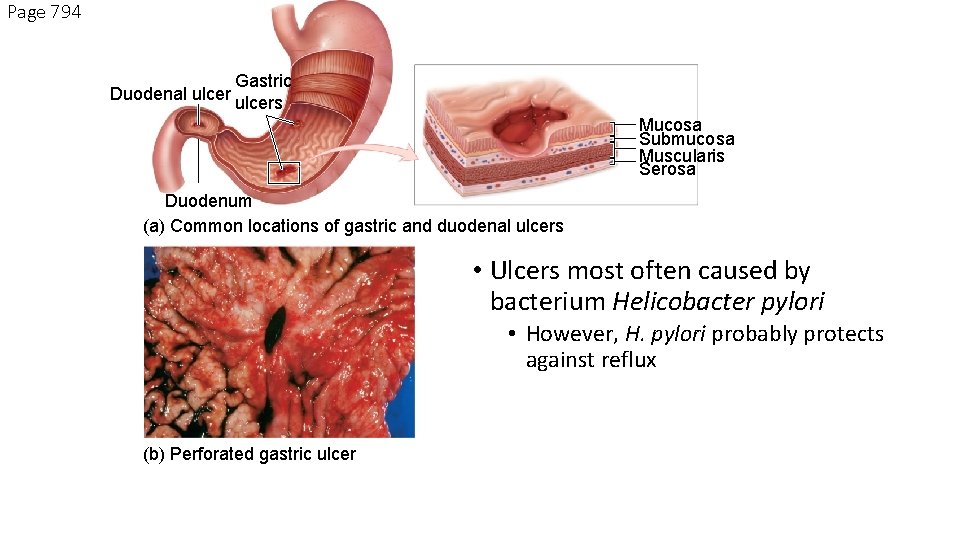
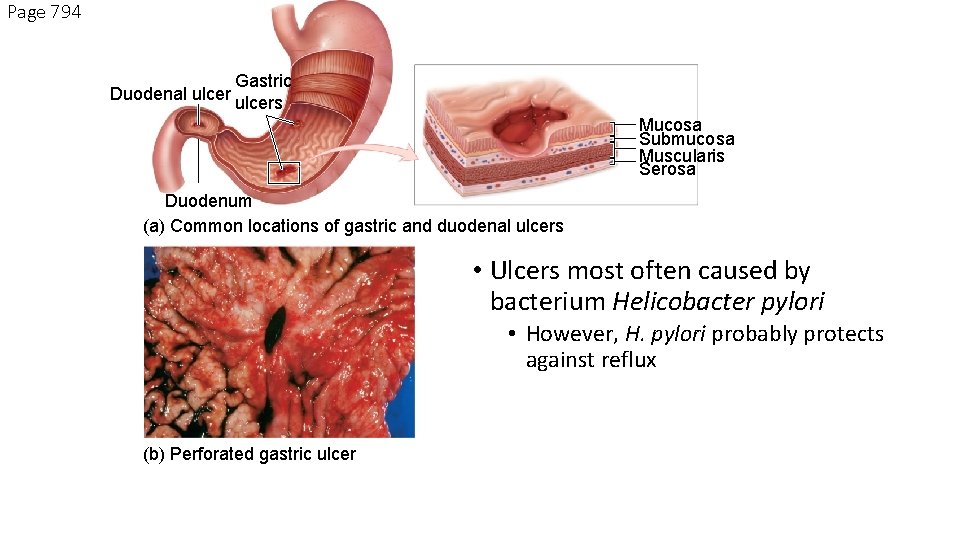
Page 794 Gastric Duodenal ulcers Mucosa Submucosa Muscularis Serosa Duodenum (a) Common locations of gastric and duodenal ulcers • Ulcers most often caused by bacterium Helicobacter pylori • However, H. pylori probably protects against reflux (b) Perforated gastric ulcer
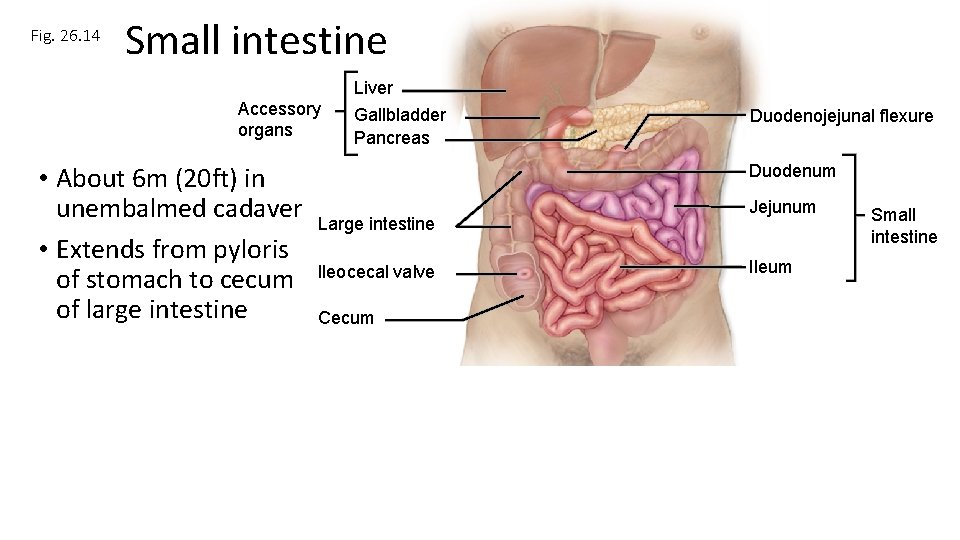
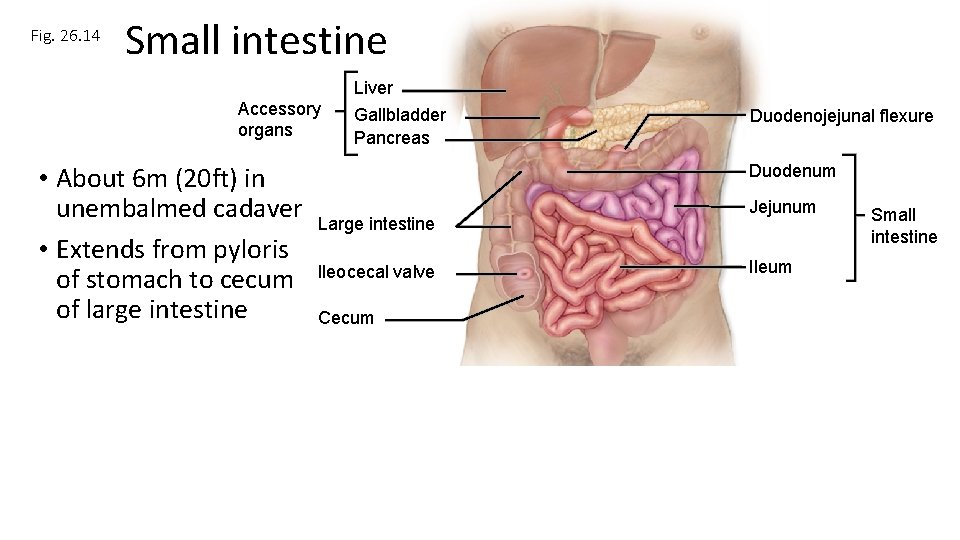
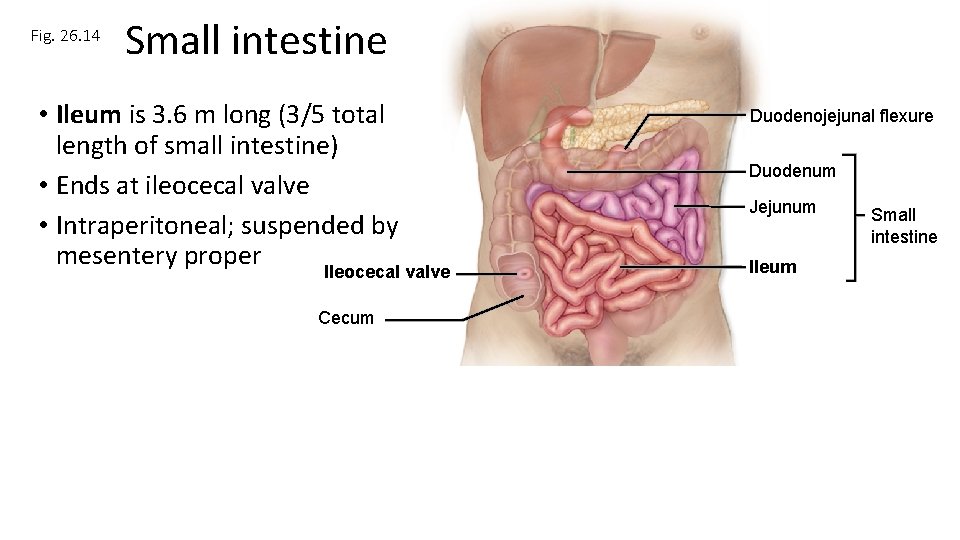
Fig. 26. 14 Small intestine Liver Accessory organs • About 6 m (20 ft) in unembalmed cadaver • Extends from pyloris of stomach to cecum of large intestine Gallbladder Pancreas Duodenojejunal flexure Duodenum Large intestine Ileocecal valve Cecum Jejunum Ileum Small intestine
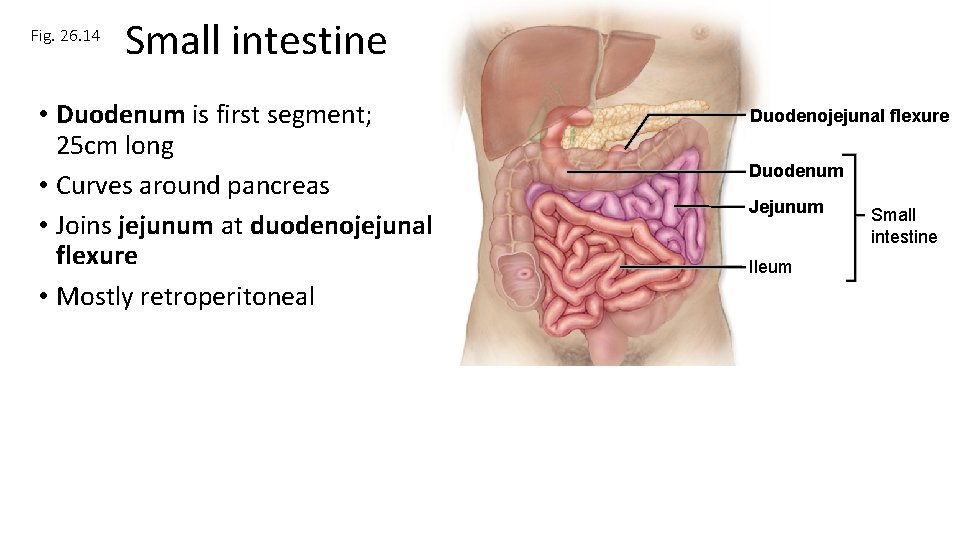
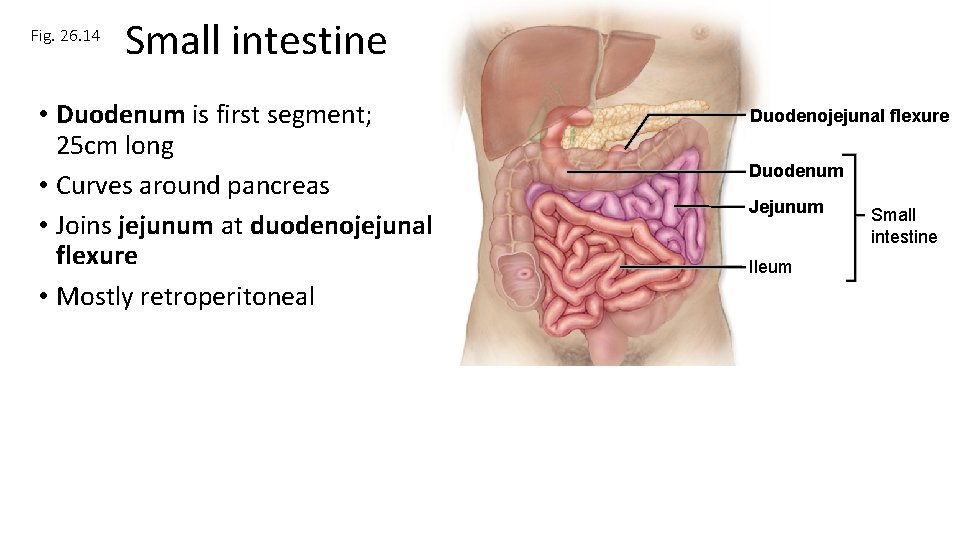
Fig. 26. 14 Small intestine • Duodenum is first segment; 25 cm long • Curves around pancreas • Joins jejunum at duodenojejunal flexure • Mostly retroperitoneal Duodenojejunal flexure Duodenum Jejunum Ileum Small intestine
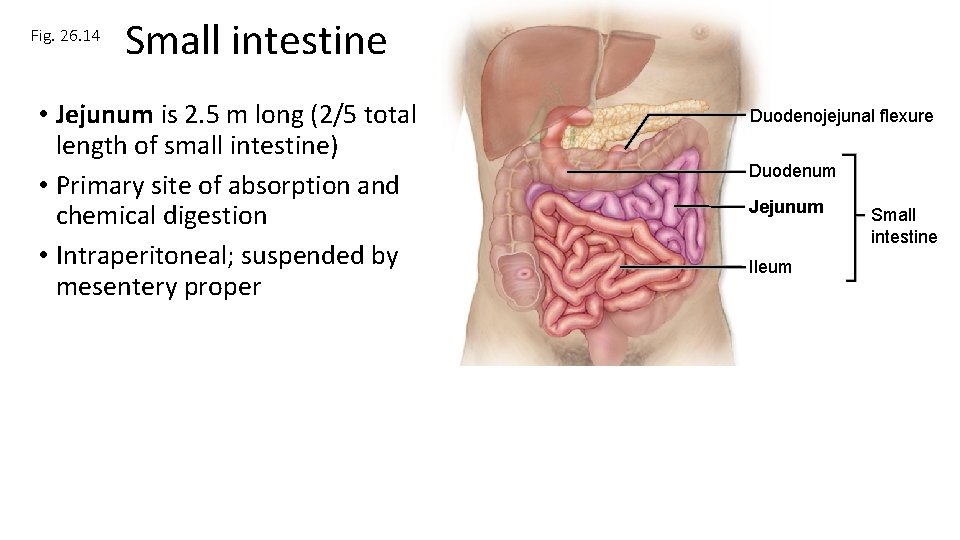
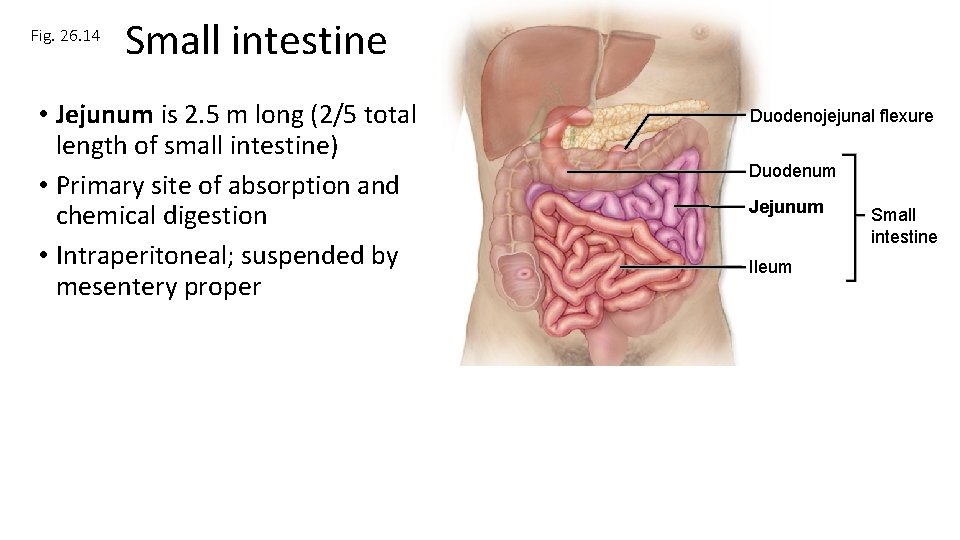
Fig. 26. 14 Small intestine • Jejunum is 2. 5 m long (2/5 total length of small intestine) • Primary site of absorption and chemical digestion • Intraperitoneal; suspended by mesentery proper Duodenojejunal flexure Duodenum Jejunum Ileum Small intestine
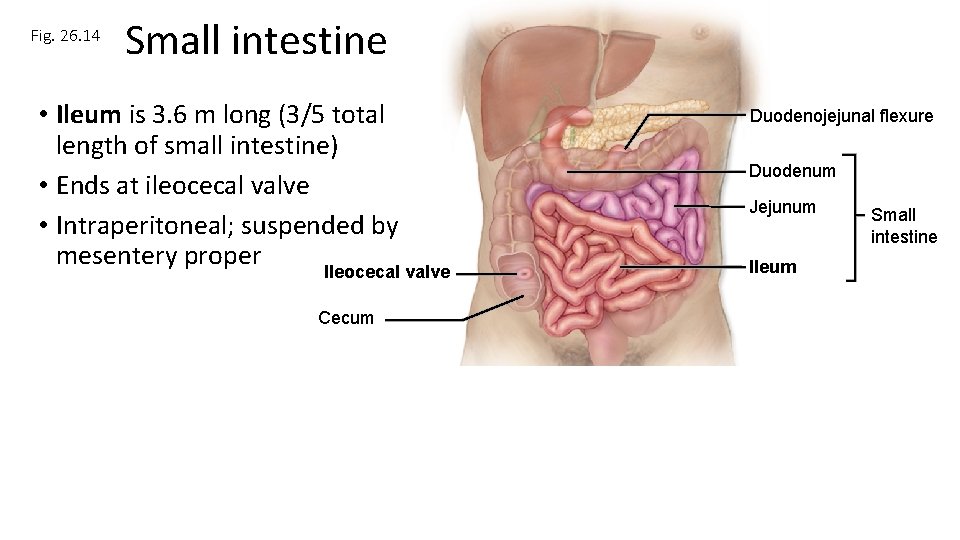
Fig. 26. 14 Small intestine • Ileum is 3. 6 m long (3/5 total length of small intestine) • Ends at ileocecal valve • Intraperitoneal; suspended by mesentery proper Ileocecal valve Cecum Duodenojejunal flexure Duodenum Jejunum Ileum Small intestine
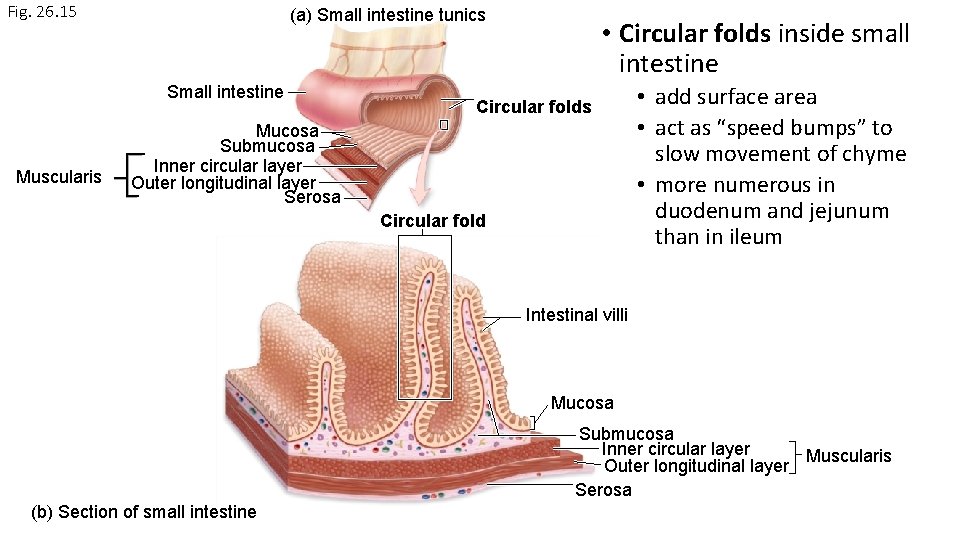
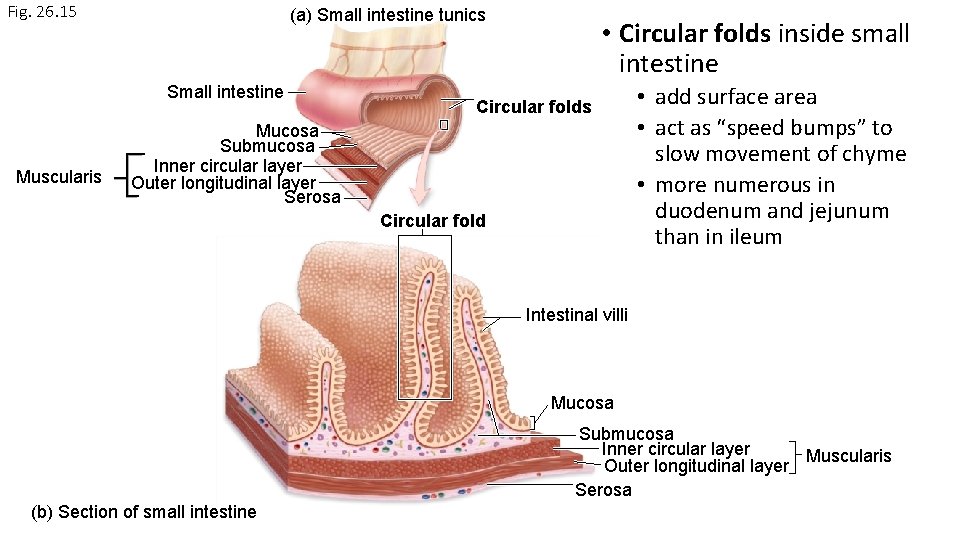
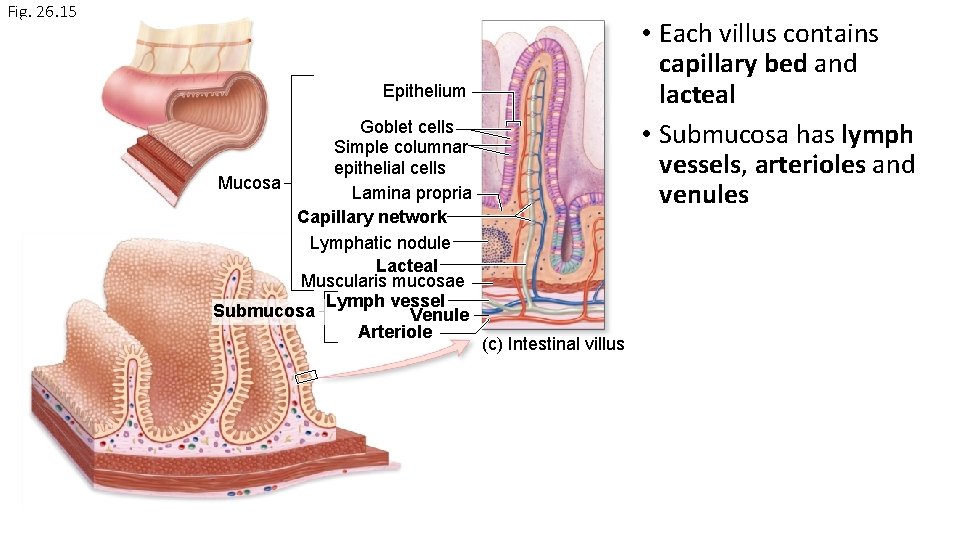
Fig. 26. 15 (a) Small intestine tunics Small intestine Muscularis • Circular folds inside small intestine Circular folds Mucosa Submucosa Inner circular layer Outer longitudinal layer Serosa Circular fold • add surface area • act as “speed bumps” to slow movement of chyme • more numerous in duodenum and jejunum than in ileum Intestinal villi Mucosa Submucosa Inner circular layer Muscularis Outer longitudinal layer Serosa (b) Section of small intestine
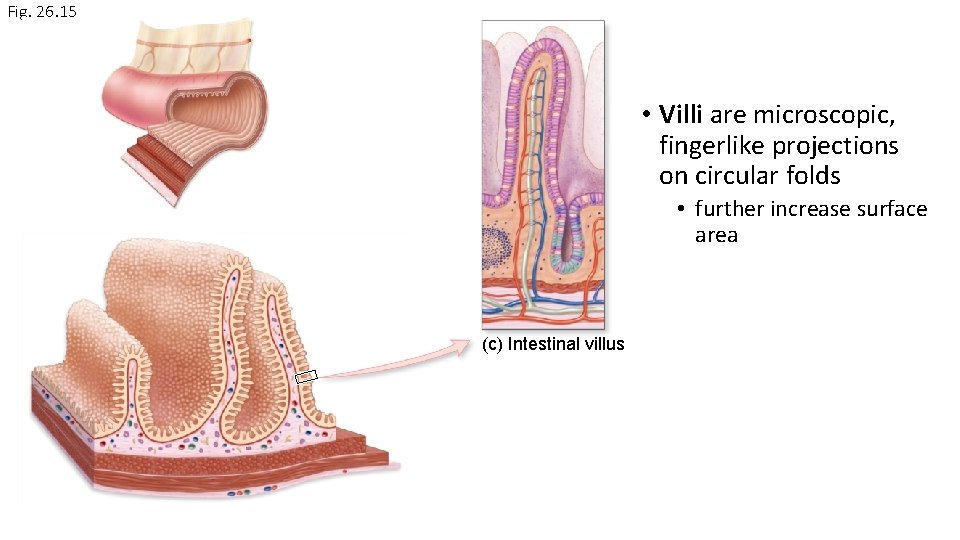
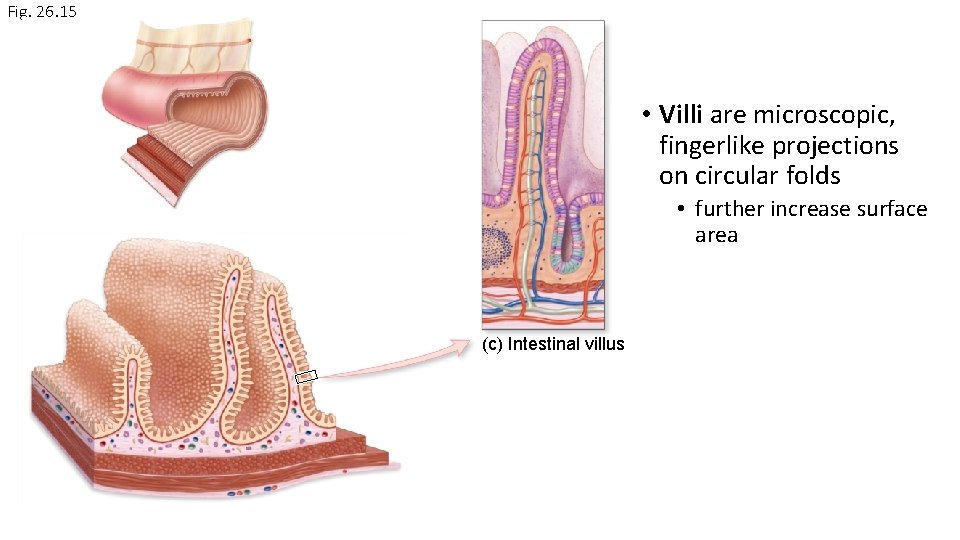
Fig. 26. 15 • Villi are microscopic, fingerlike projections on circular folds • further increase surface area (c) Intestinal villus
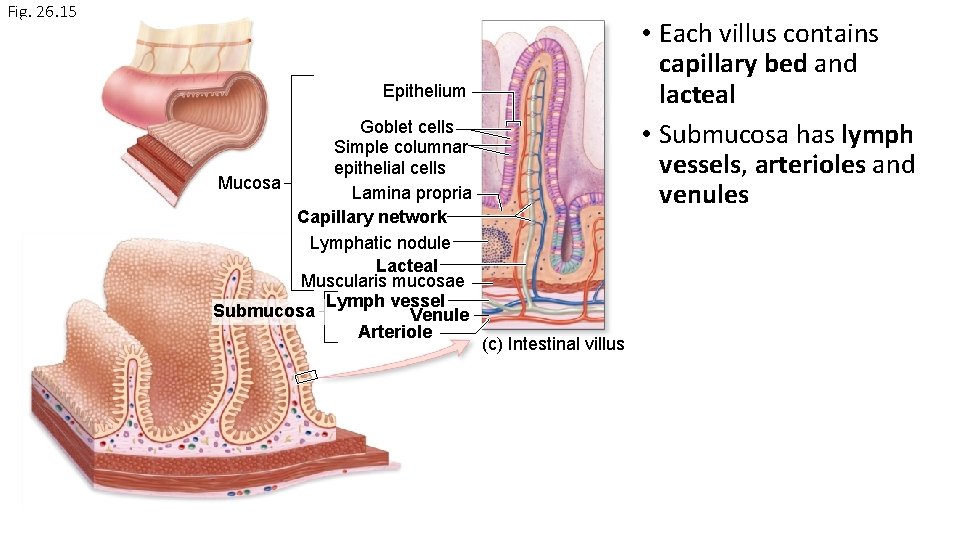
Fig. 26. 15 • Each villus contains capillary bed and lacteal • Submucosa has lymph vessels, arterioles and venules Epithelium Goblet cells Simple columnar epithelial cells Mucosa Lamina propria Capillary network Lymphatic nodule Lacteal Muscularis mucosae Lymph vessel Submucosa Venule Arteriole (c) Intestinal villus
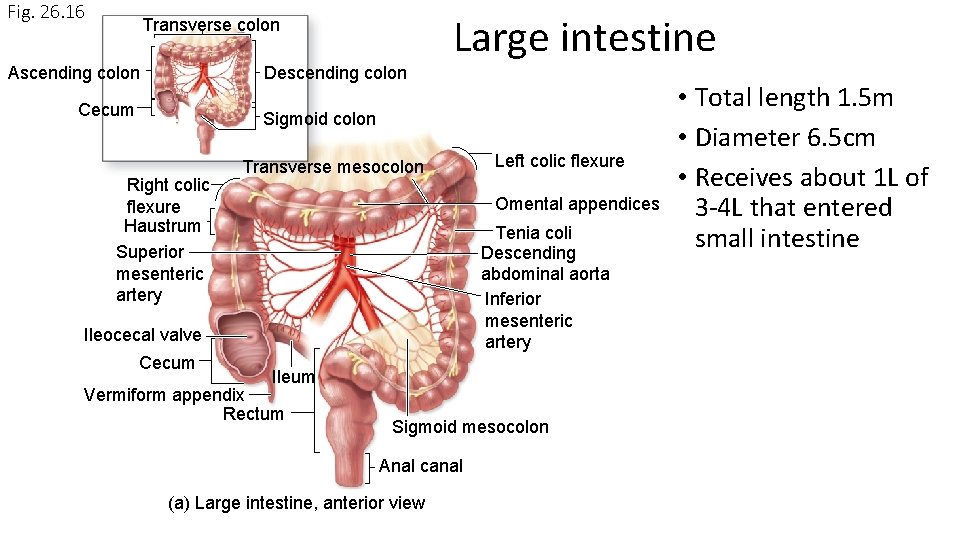
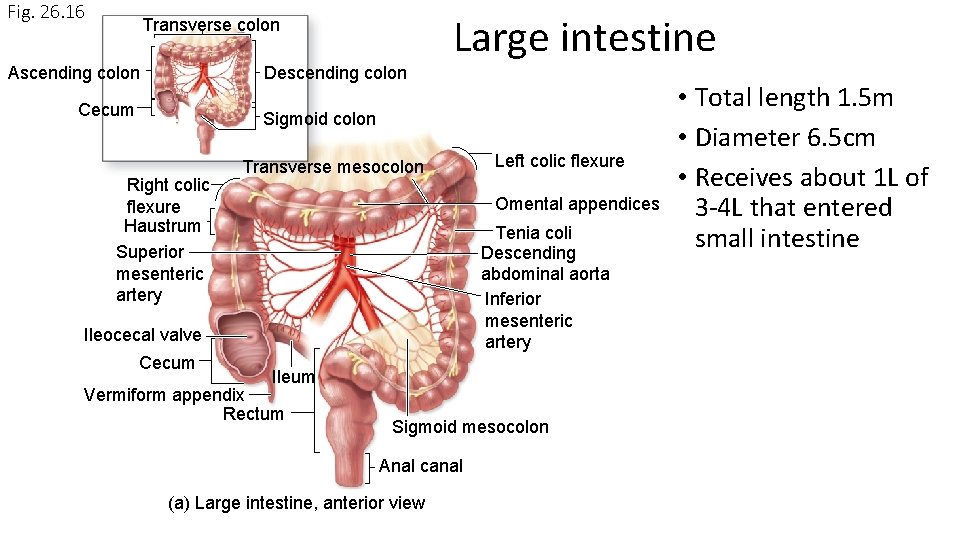
Fig. 26. 16 Transverse colon Ascending colon Descending colon Cecum Large intestine Sigmoid colon Right colic flexure Haustrum Superior mesenteric artery Transverse mesocolon Omental appendices Tenia coli Descending abdominal aorta Inferior mesenteric artery Ileocecal valve Cecum Left colic flexure Ileum Vermiform appendix Rectum Sigmoid mesocolon Anal canal (a) Large intestine, anterior view • Total length 1. 5 m • Diameter 6. 5 cm • Receives about 1 L of 3 -4 L that entered small intestine
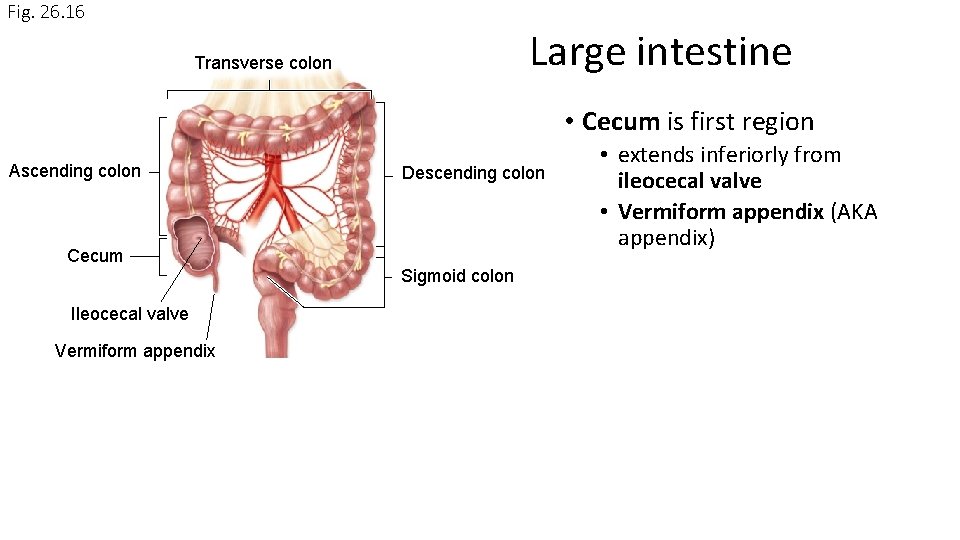
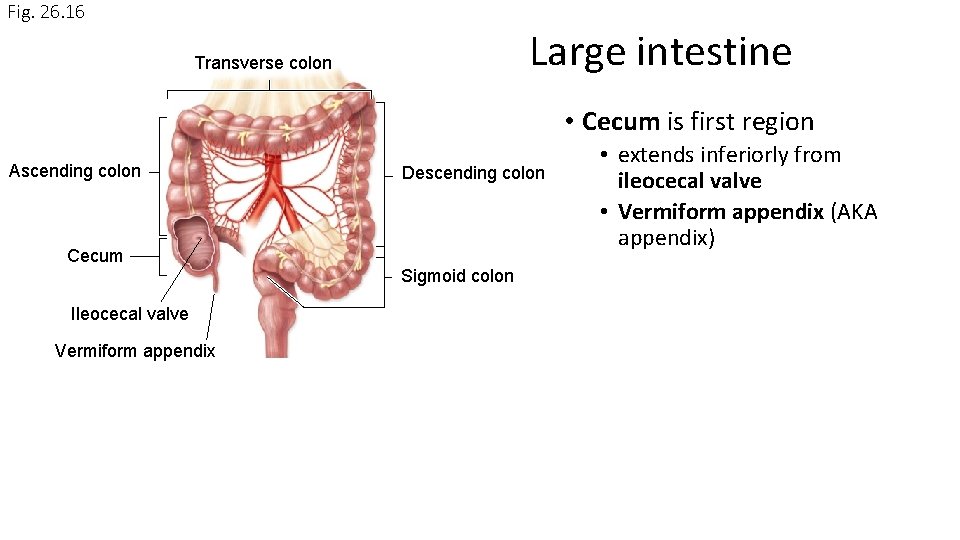
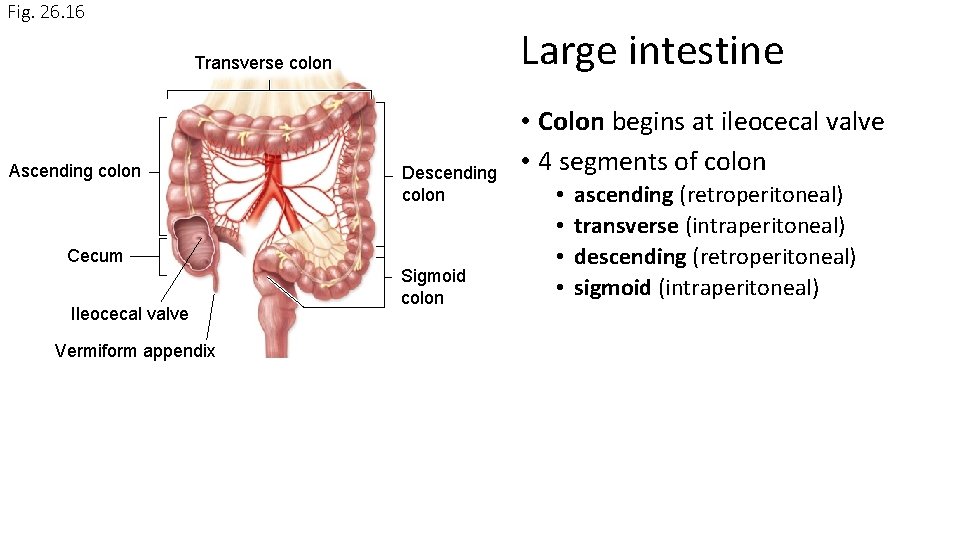
Fig. 26. 16 Large intestine Transverse colon • Cecum is first region Ascending colon Descending colon Cecum Sigmoid colon Ileocecal valve Vermiform appendix • extends inferiorly from ileocecal valve • Vermiform appendix (AKA appendix)
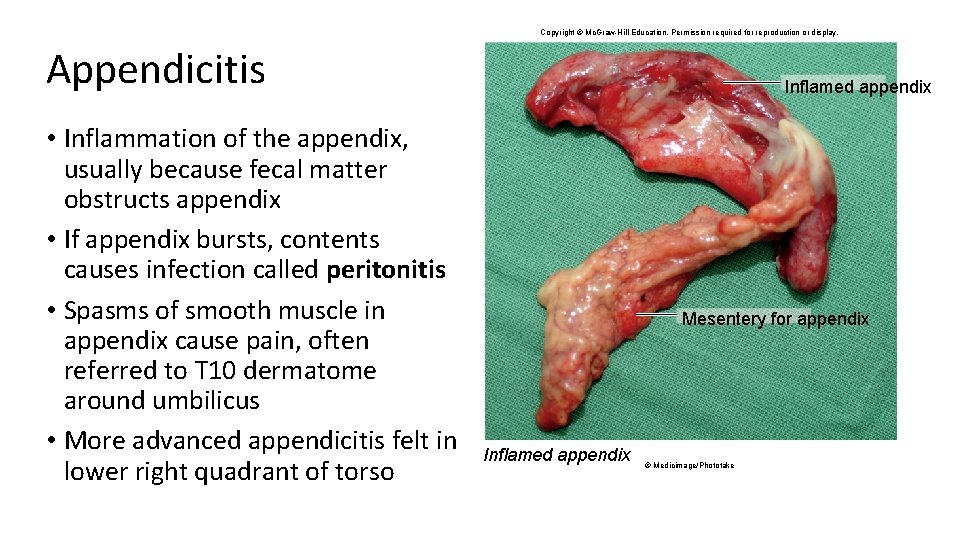
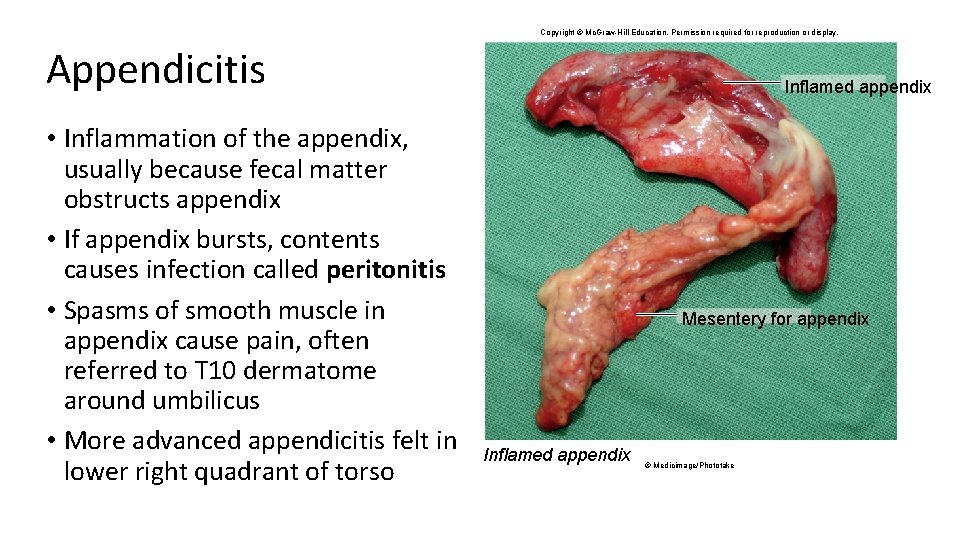
Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display. Appendicitis • Inflammation of the appendix, usually because fecal matter obstructs appendix • If appendix bursts, contents causes infection called peritonitis • Spasms of smooth muscle in appendix cause pain, often referred to T 10 dermatome around umbilicus • More advanced appendicitis felt in lower right quadrant of torso Inflamed appendix Mesentery for appendix Inflamed appendix © Medicimage/Phototake
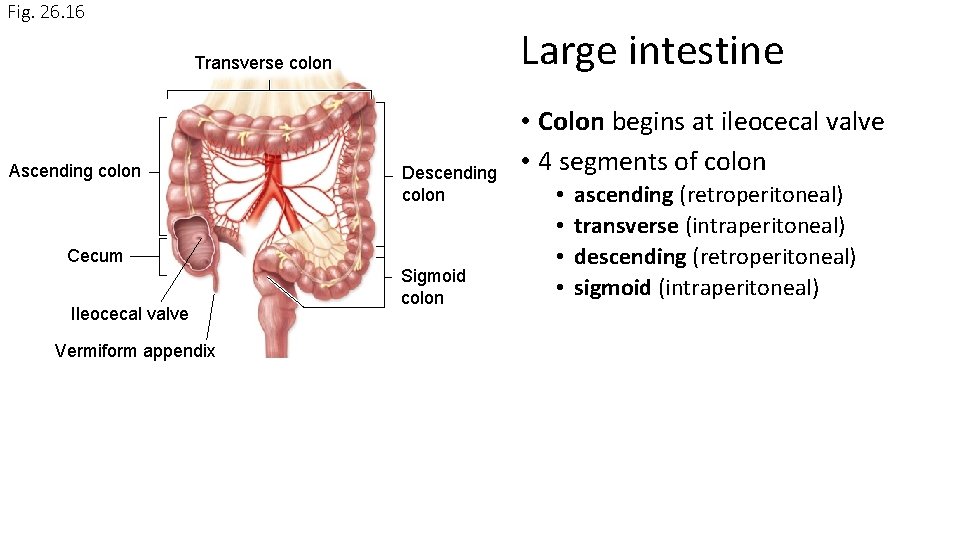
Fig. 26. 16 Large intestine Transverse colon Ascending colon Descending colon Cecum Ileocecal valve Vermiform appendix Sigmoid colon • Colon begins at ileocecal valve • 4 segments of colon • • ascending (retroperitoneal) transverse (intraperitoneal) descending (retroperitoneal) sigmoid (intraperitoneal)
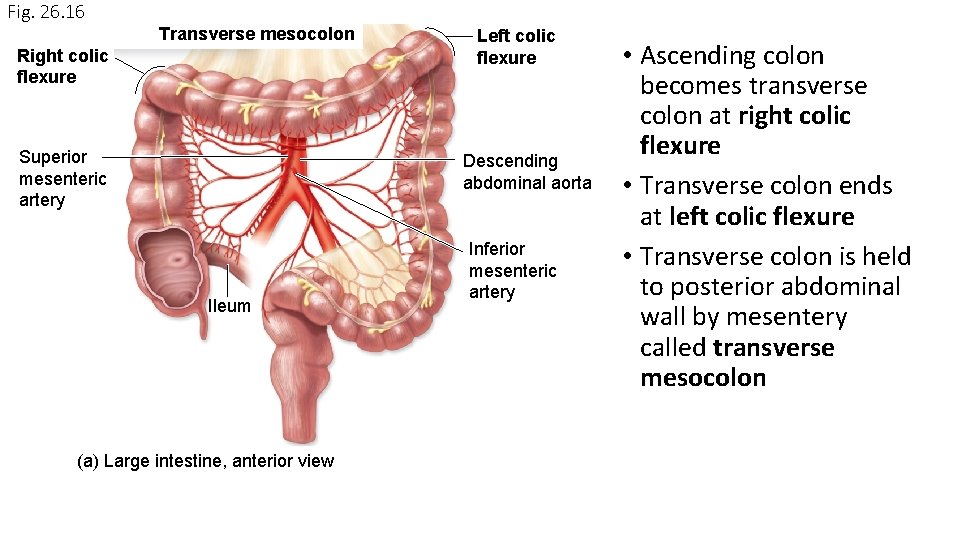
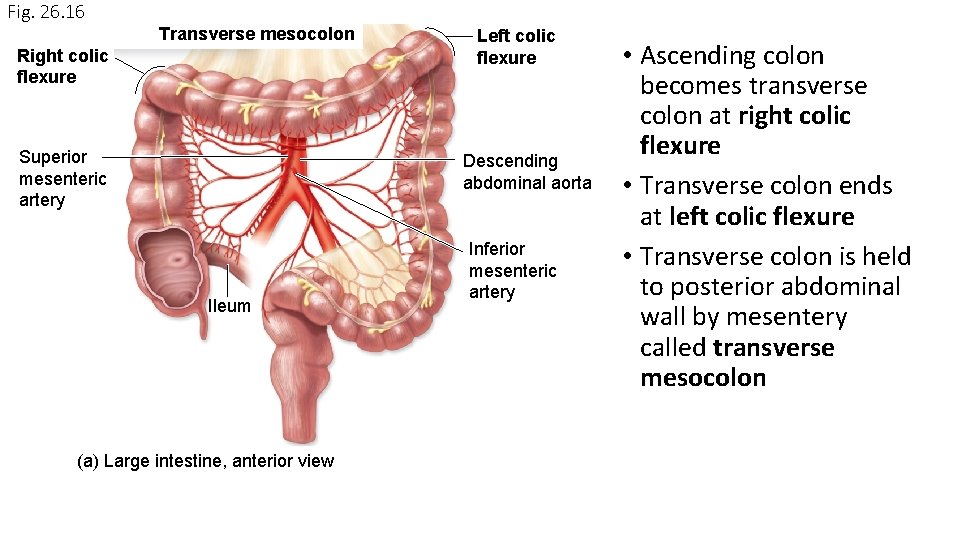
Fig. 26. 16 Transverse mesocolon Right colic flexure Superior mesenteric artery Left colic flexure Descending abdominal aorta Ileum (a) Large intestine, anterior view Inferior mesenteric artery • Ascending colon becomes transverse colon at right colic flexure • Transverse colon ends at left colic flexure • Transverse colon is held to posterior abdominal wall by mesentery called transverse mesocolon
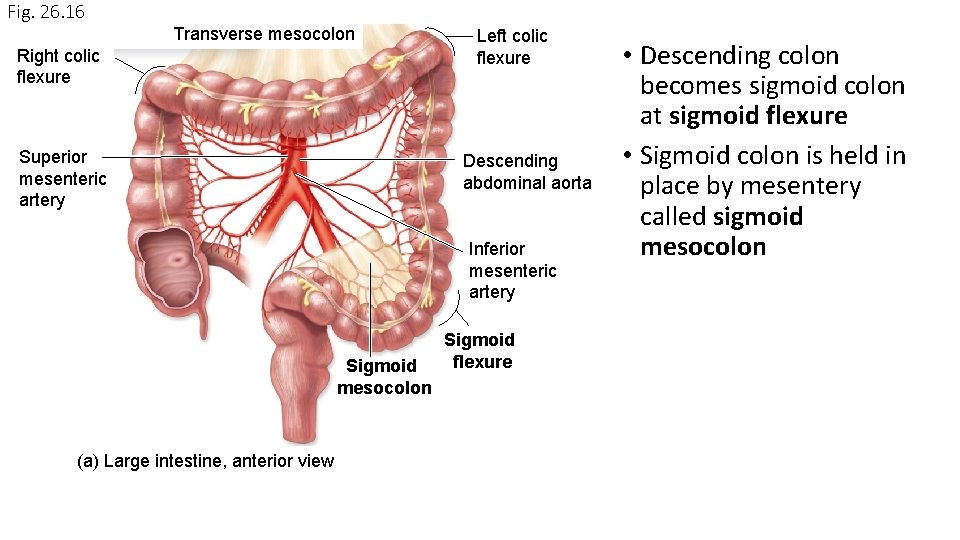
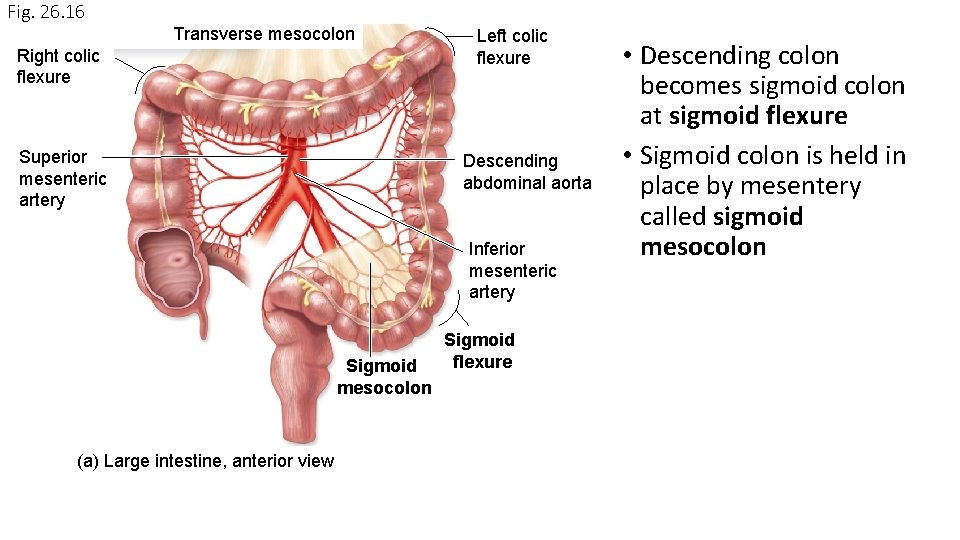
Fig. 26. 16 Transverse mesocolon Right colic flexure Superior mesenteric artery Left colic flexure Descending abdominal aorta Inferior mesenteric artery Sigmoid mesocolon (a) Large intestine, anterior view Sigmoid flexure • Descending colon becomes sigmoid colon at sigmoid flexure • Sigmoid colon is held in place by mesentery called sigmoid mesocolon
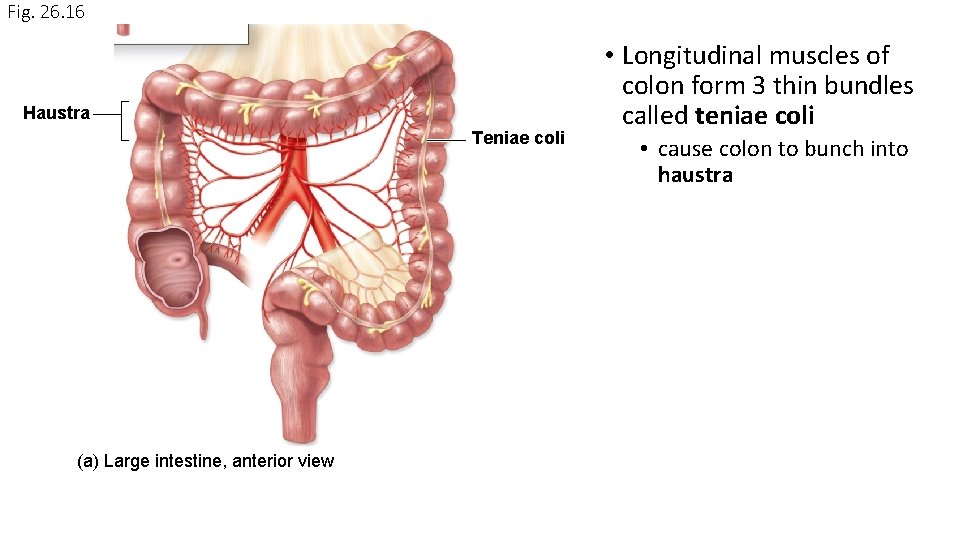
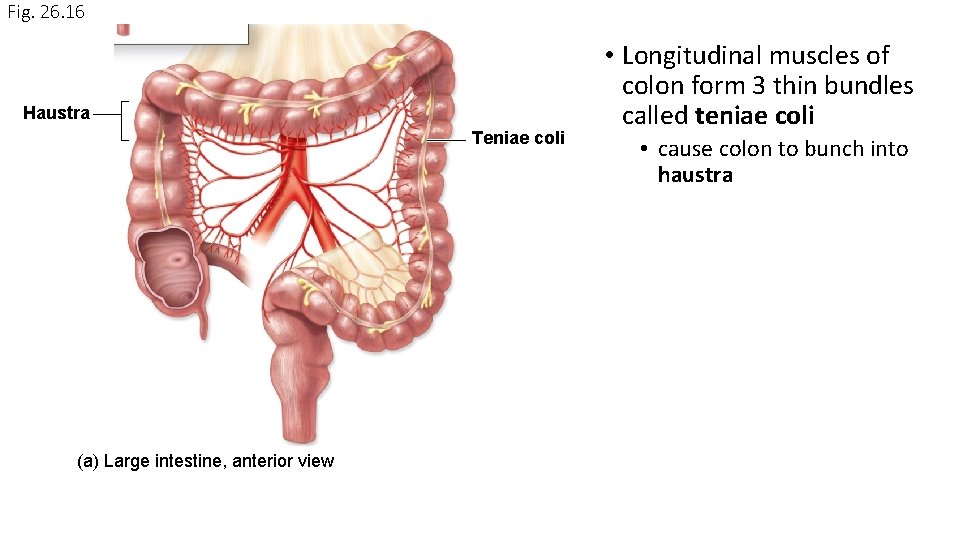
Fig. 26. 16 Haustra Teniae coli (a) Large intestine, anterior view • Longitudinal muscles of colon form 3 thin bundles called teniae coli • cause colon to bunch into haustra
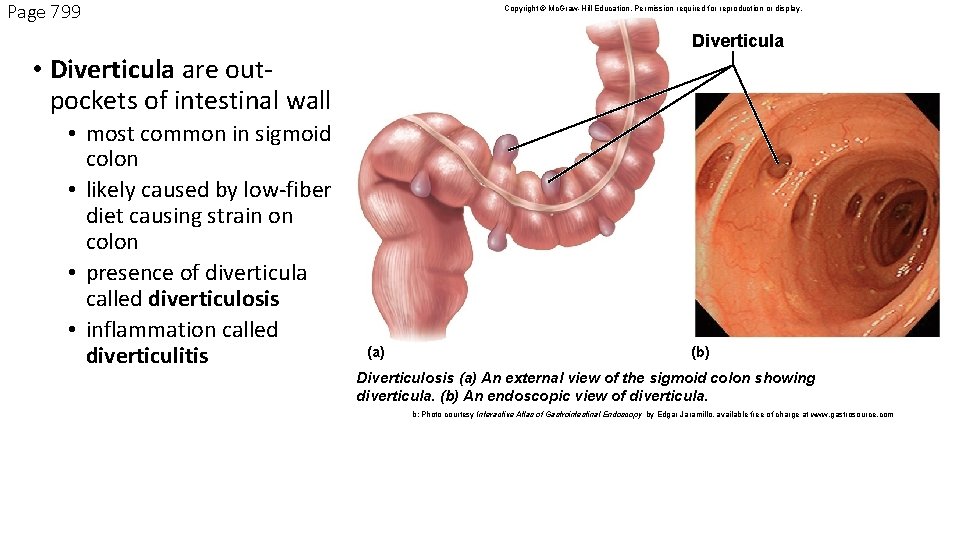
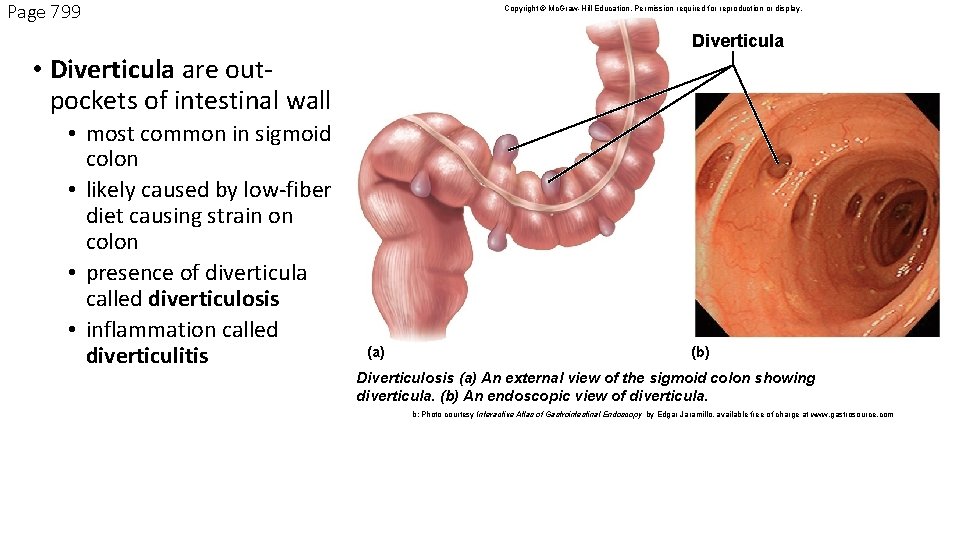
Page 799 Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display. Diverticula • Diverticula are outpockets of intestinal wall • most common in sigmoid colon • likely caused by low-fiber diet causing strain on colon • presence of diverticula called diverticulosis • inflammation called diverticulitis (a) (b) Diverticulosis (a) An external view of the sigmoid colon showing diverticula. (b) An endoscopic view of diverticula. b: Photo courtesy Interactive Atlas of Gastrointestinal Endoscopy by Edgar Jaramillo, available free of charge at www. gastrosource. com
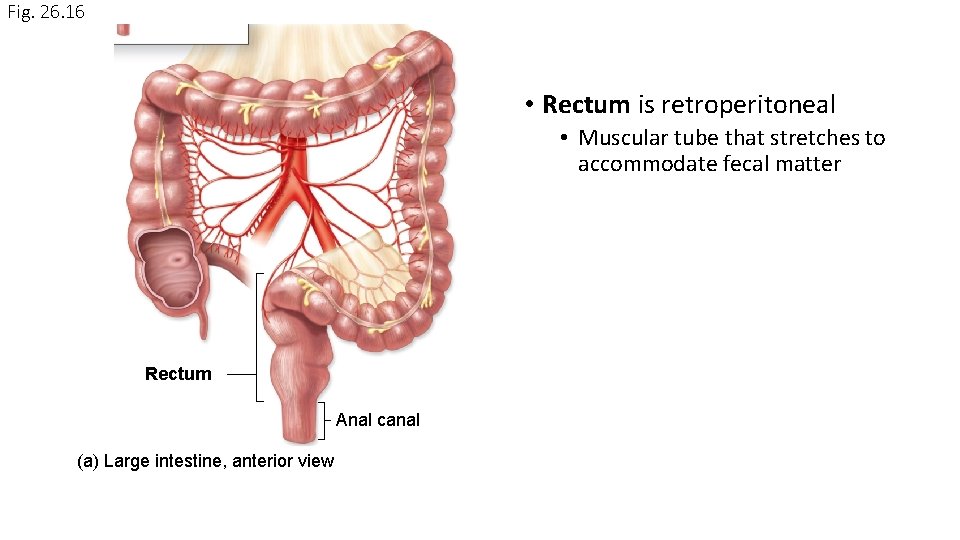
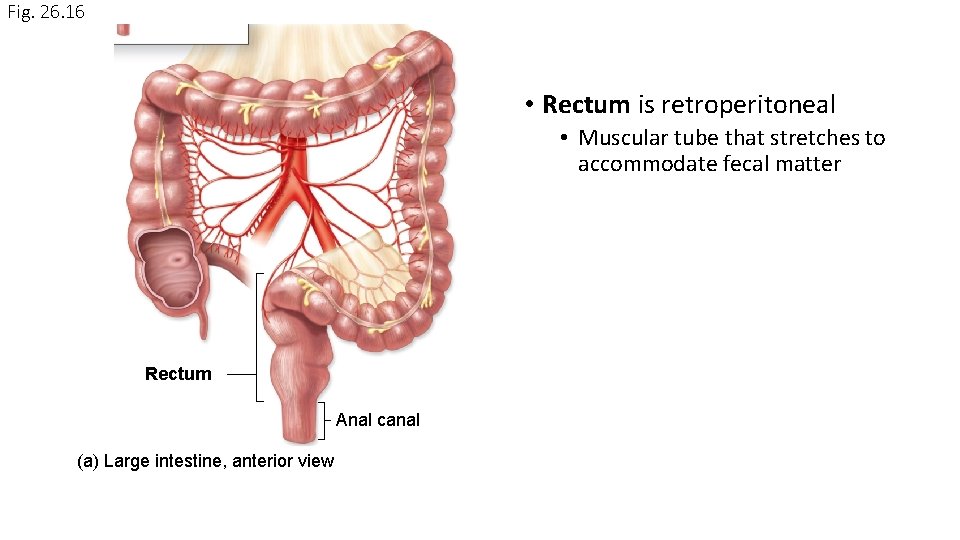
Fig. 26. 16 • Rectum is retroperitoneal • Muscular tube that stretches to accommodate fecal matter Rectum Anal canal (a) Large intestine, anterior view
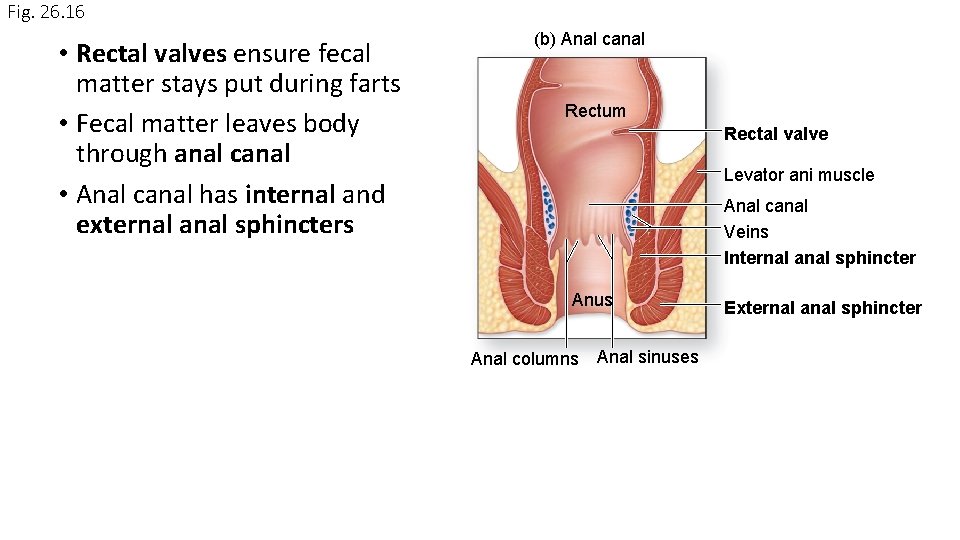
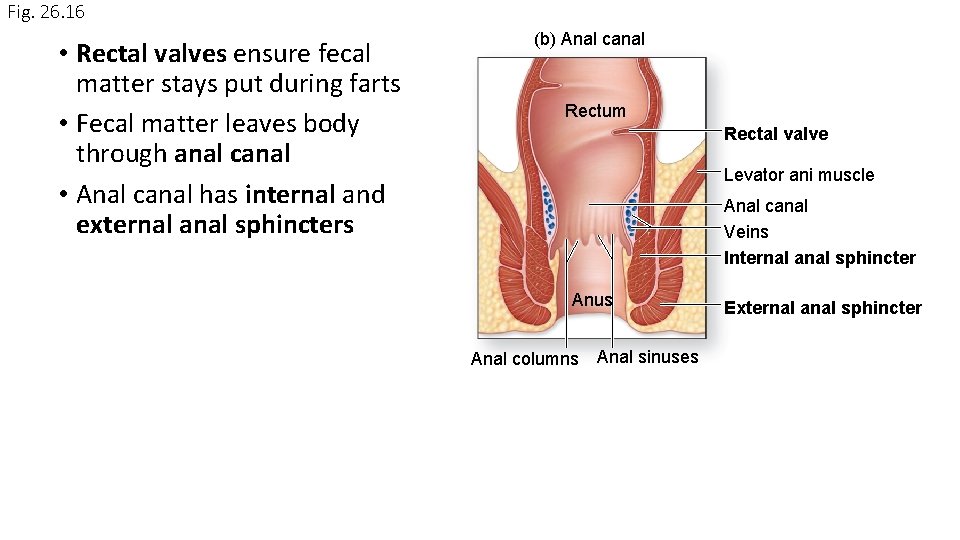
Fig. 26. 16 • Rectal valves ensure fecal matter stays put during farts • Fecal matter leaves body through anal canal • Anal canal has internal and external anal sphincters (b) Anal canal Rectum Rectal valve Levator ani muscle Anal canal Veins Internal anal sphincter Anus Anal columns Anal sinuses External anal sphincter
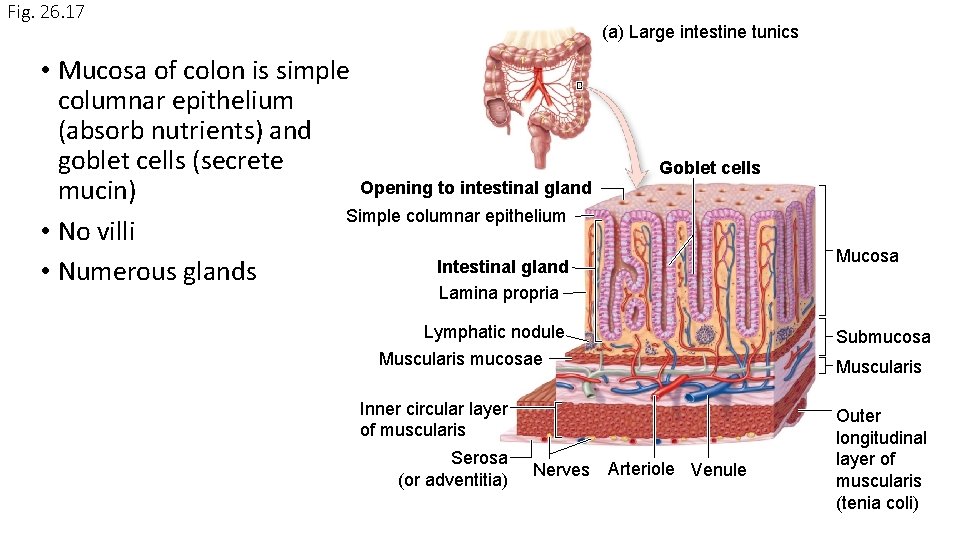
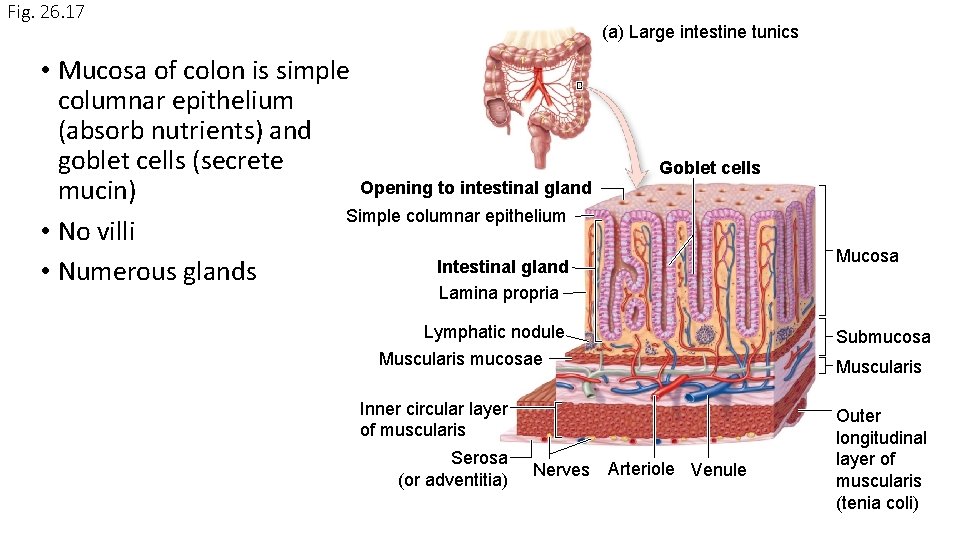
Fig. 26. 17 (a) Large intestine tunics • Mucosa of colon is simple columnar epithelium (absorb nutrients) and goblet cells (secrete Opening to intestinal gland mucin) Simple columnar epithelium • No villi Intestinal gland • Numerous glands Goblet cells Mucosa Lamina propria Lymphatic nodule Muscularis mucosae Inner circular layer of muscularis Serosa (or adventitia) Nerves Arteriole Venule Submucosa Muscularis Outer longitudinal layer of muscularis (tenia coli)
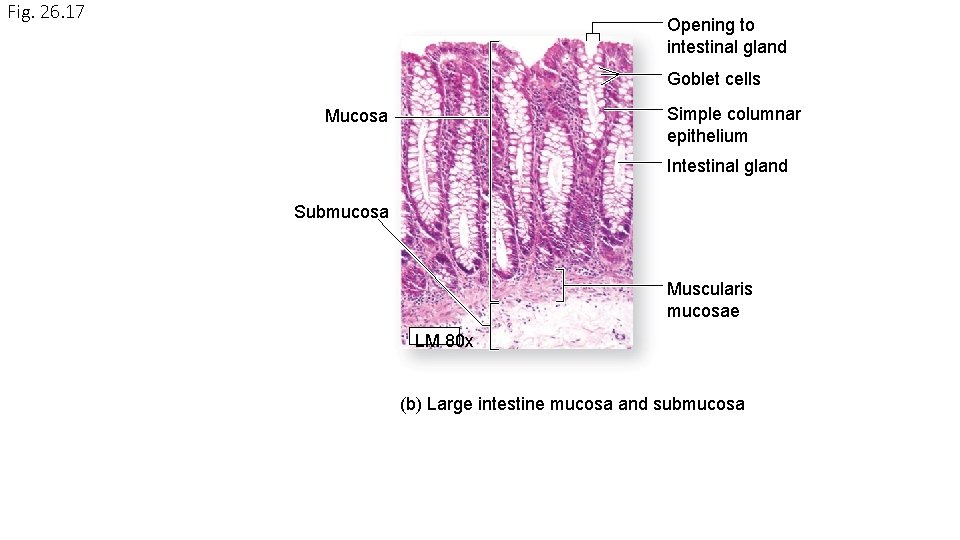
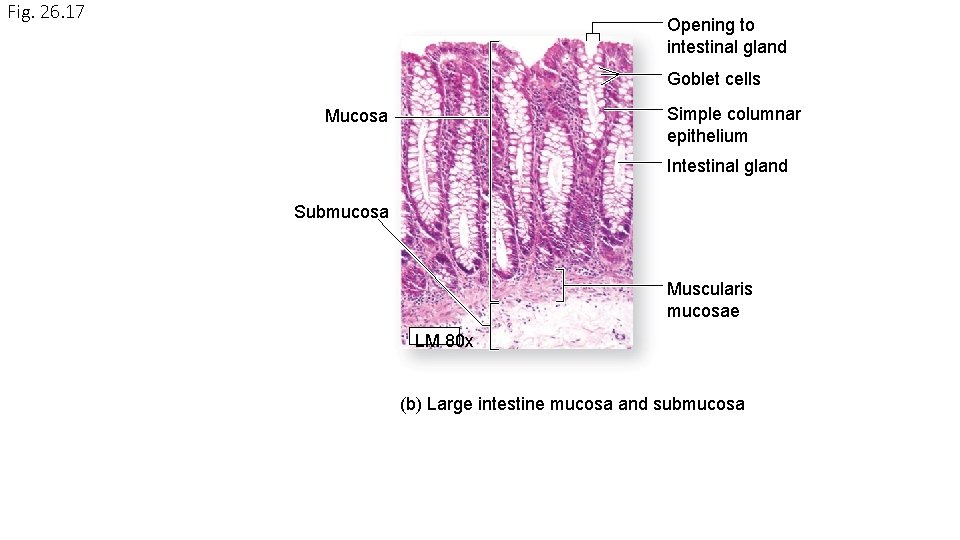
Fig. 26. 17 Opening to intestinal gland Goblet cells Simple columnar epithelium Mucosa Intestinal gland Submucosa Muscularis mucosae LM 80 x (b) Large intestine mucosa and submucosa
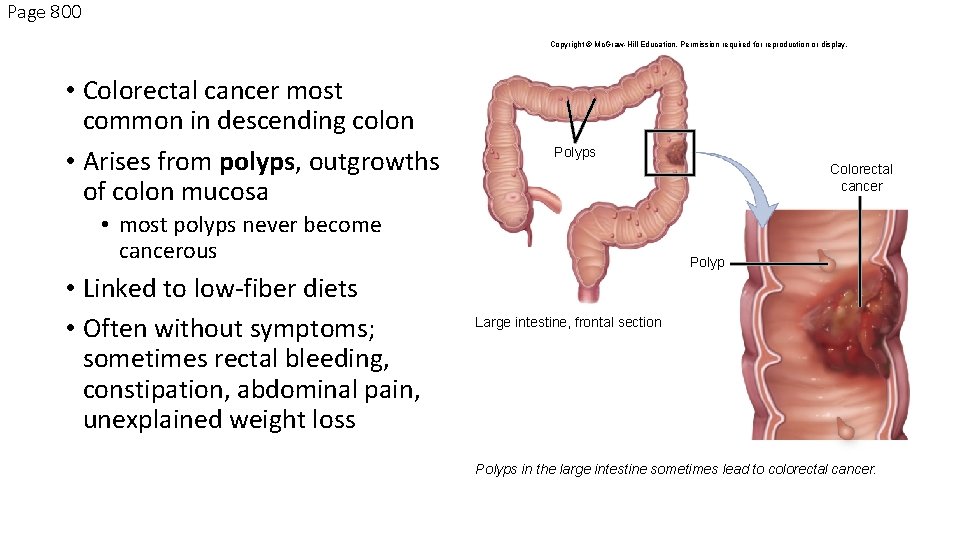
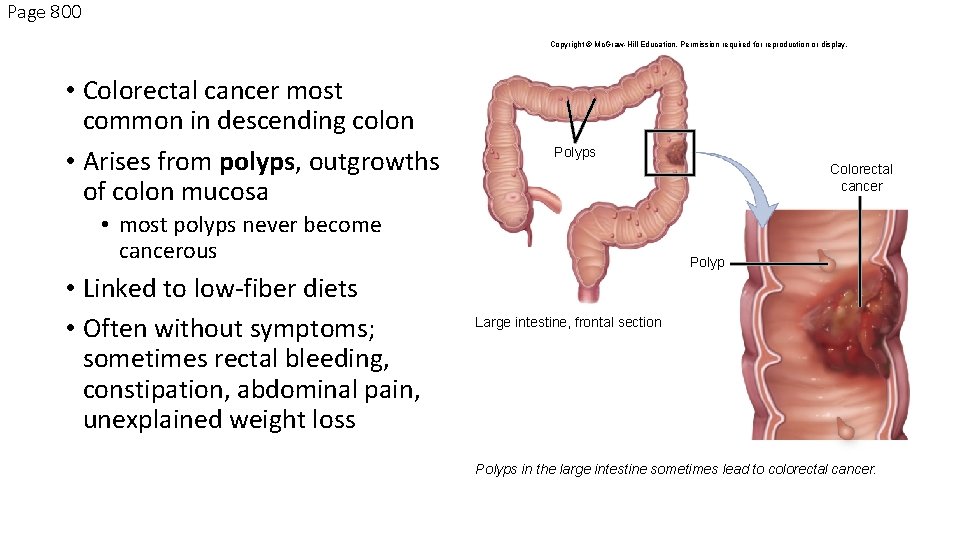
Page 800 Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display. • Colorectal cancer most common in descending colon • Arises from polyps, outgrowths of colon mucosa Polyps Colorectal cancer • most polyps never become cancerous • Linked to low-fiber diets • Often without symptoms; sometimes rectal bleeding, constipation, abdominal pain, unexplained weight loss Polyp Large intestine, frontal section Polyps in the large intestine sometimes lead to colorectal cancer.
Liver celebrates New Year’s Eve
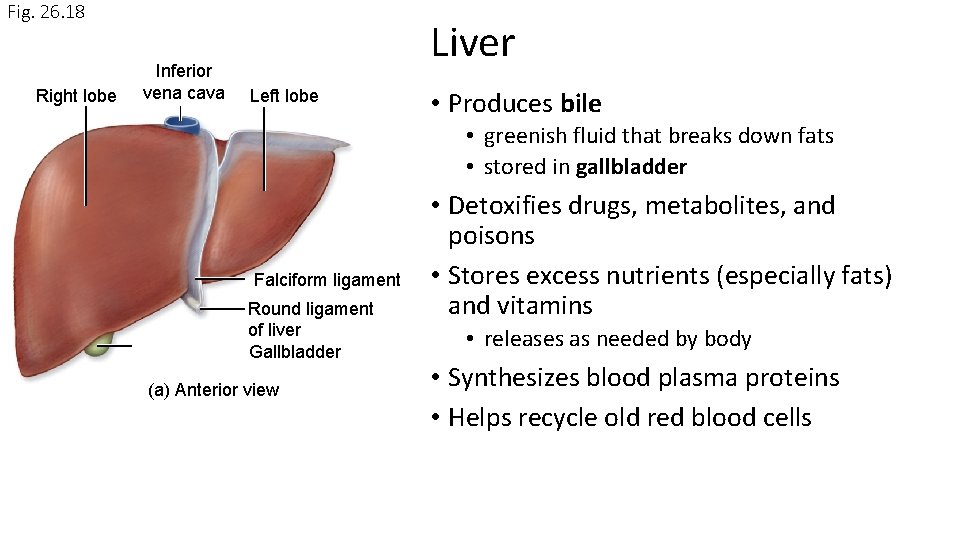
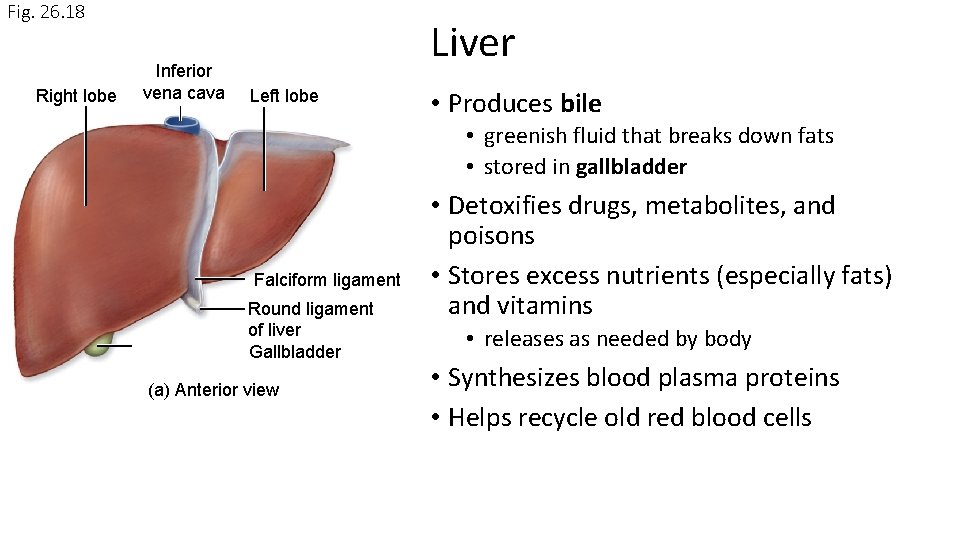
Fig. 26. 18 Right lobe Inferior vena cava Liver Left lobe • Produces bile • greenish fluid that breaks down fats • stored in gallbladder Falciform ligament Round ligament of liver Gallbladder (a) Anterior view • Detoxifies drugs, metabolites, and poisons • Stores excess nutrients (especially fats) and vitamins • releases as needed by body • Synthesizes blood plasma proteins • Helps recycle old red blood cells
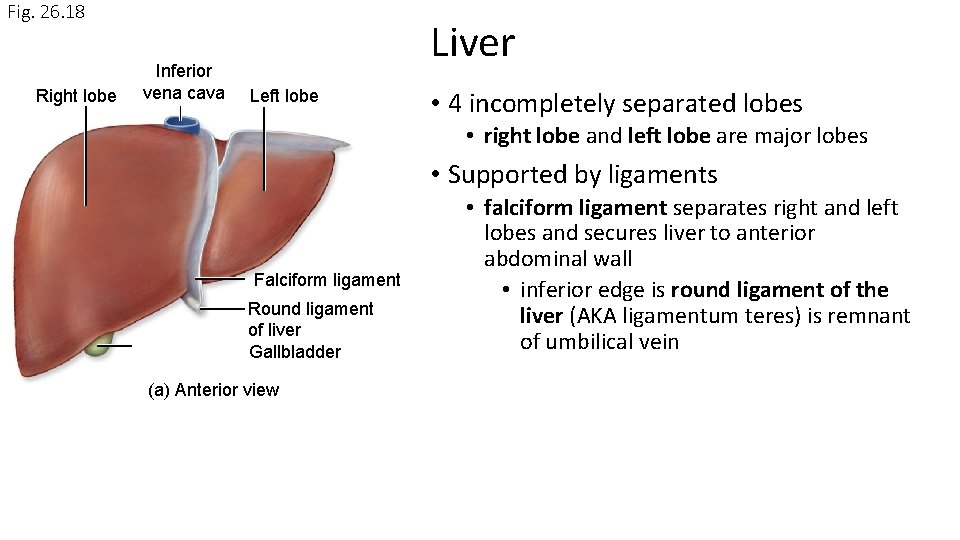
Fig. 26. 18 Right lobe Inferior vena cava Liver Left lobe • 4 incompletely separated lobes • right lobe and left lobe are major lobes • Supported by ligaments Falciform ligament Round ligament of liver Gallbladder (a) Anterior view • falciform ligament separates right and left lobes and secures liver to anterior abdominal wall • inferior edge is round ligament of the liver (AKA ligamentum teres) is remnant of umbilical vein
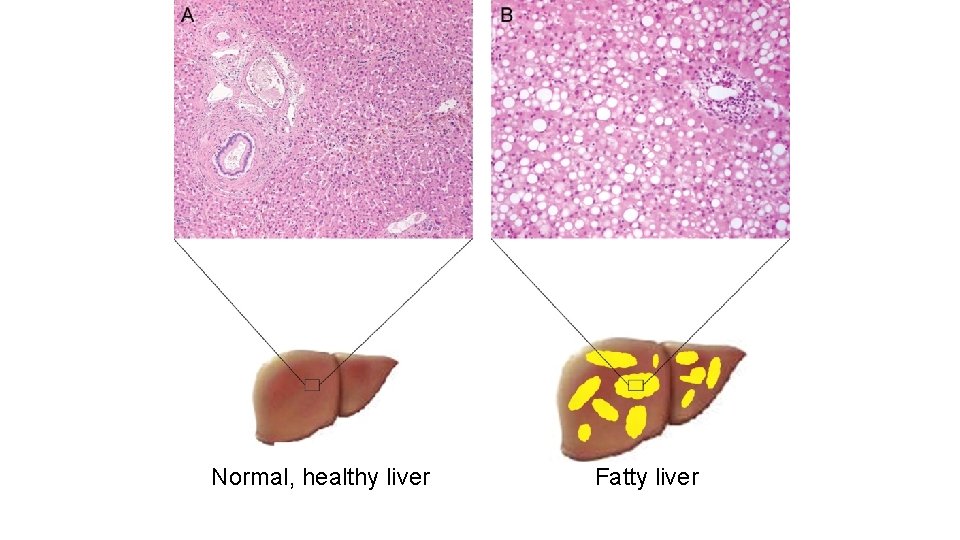
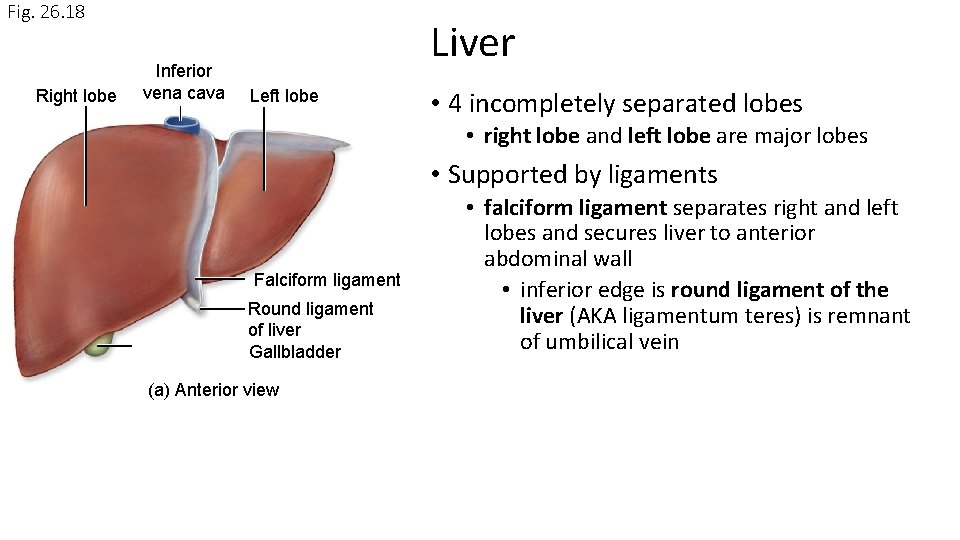
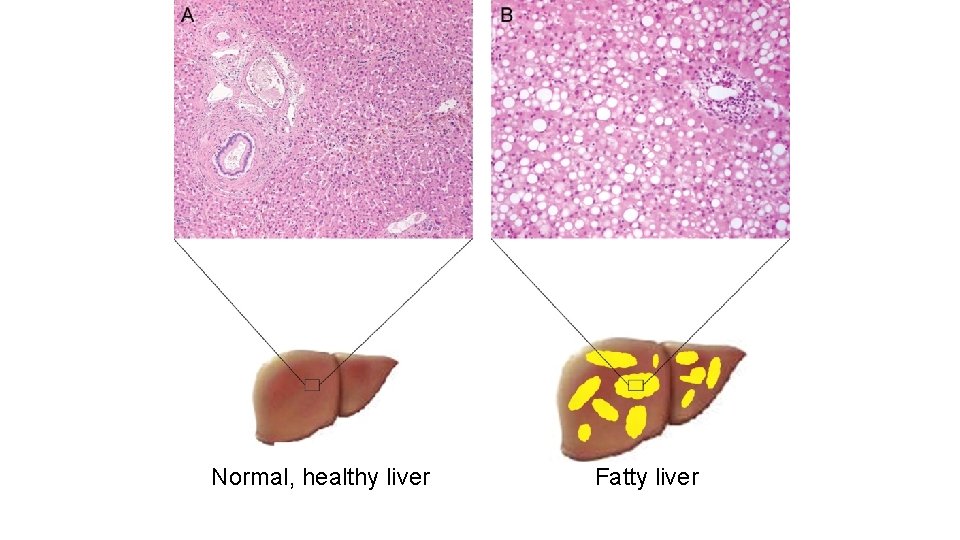
Normal, healthy liver Fatty liver
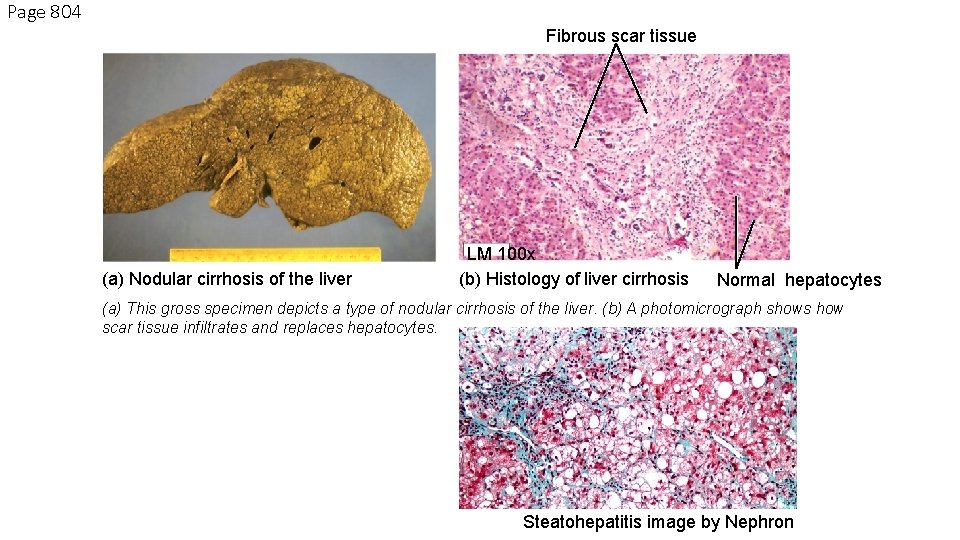
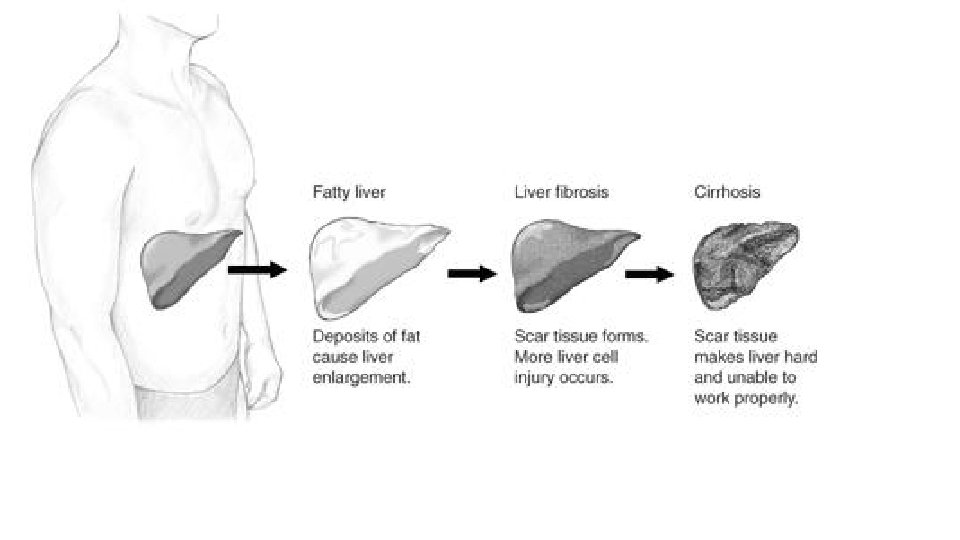
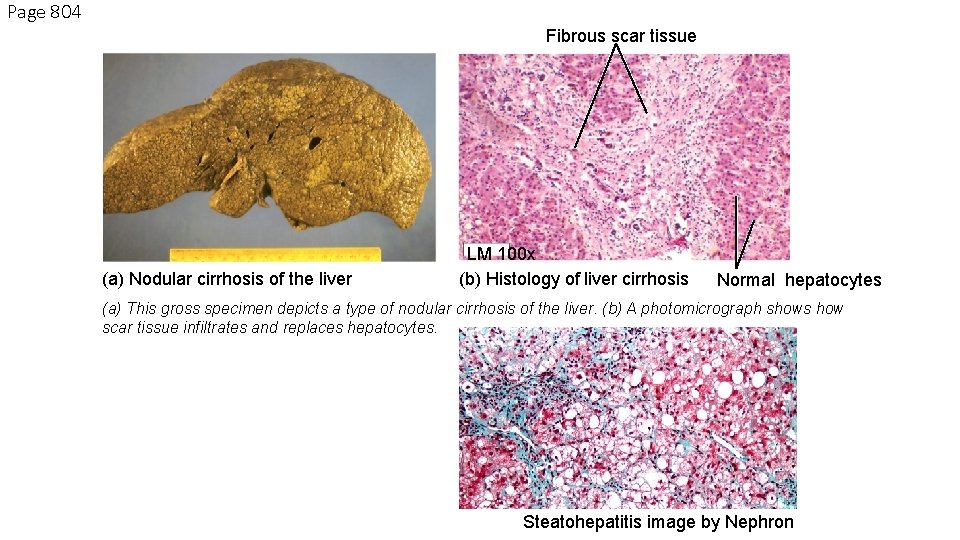
Page 804 Fibrous scar tissue (a) Nodular cirrhosis of the liver LM 100 x (b) Histology of liver cirrhosis Normal hepatocytes (a) This gross specimen depicts a type of nodular cirrhosis of the liver. (b) A photomicrograph shows how scar tissue infiltrates and replaces hepatocytes. Steatohepatitis image by Nephron
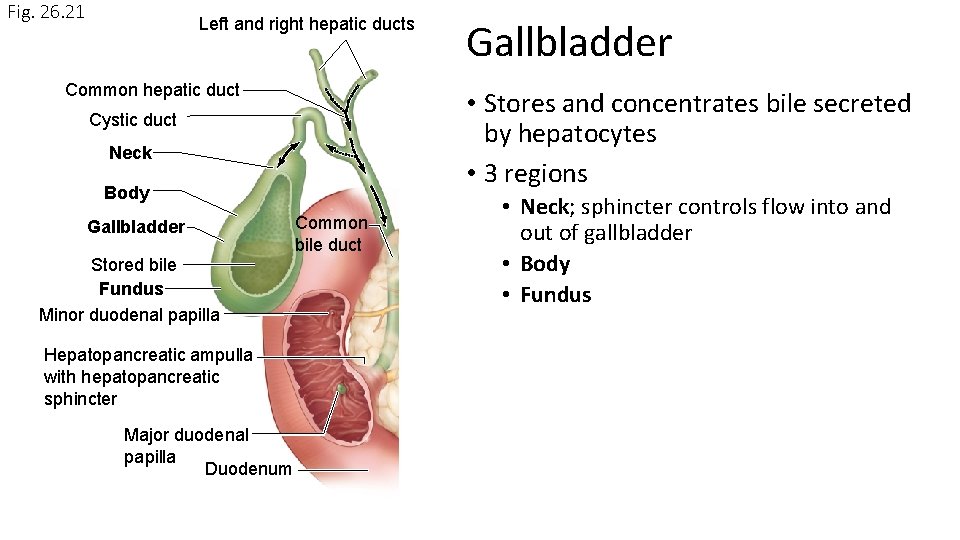
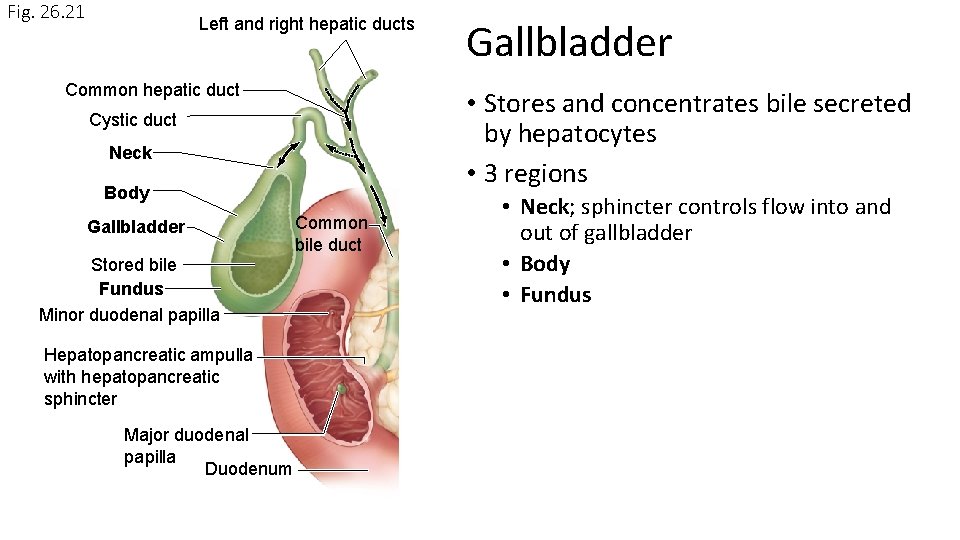
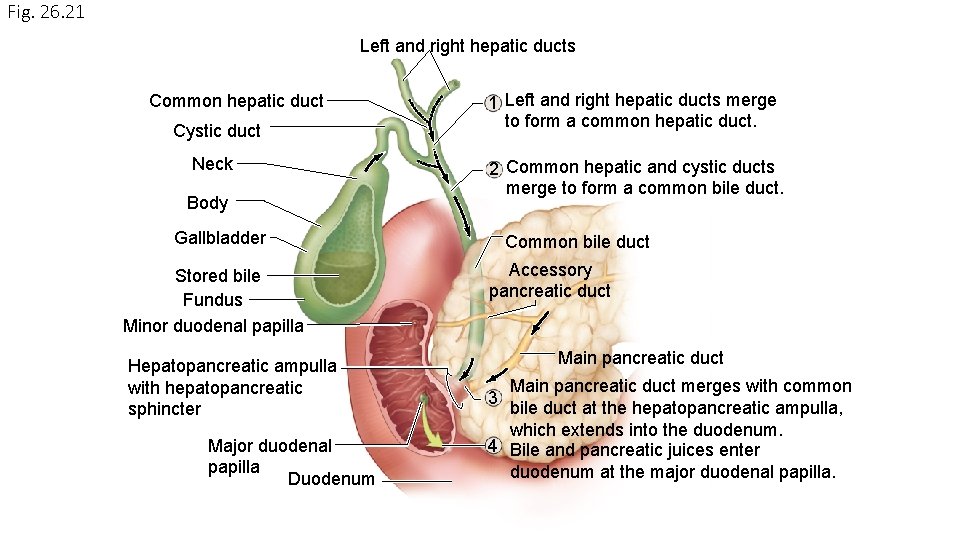
Fig. 26. 21 Left and right hepatic ducts Common hepatic duct • Stores and concentrates bile secreted by hepatocytes • 3 regions Cystic duct Neck Body Gallbladder Stored bile Fundus Minor duodenal papilla Hepatopancreatic ampulla with hepatopancreatic sphincter Major duodenal papilla Duodenum Gallbladder Common bile duct • Neck; sphincter controls flow into and out of gallbladder • Body • Fundus
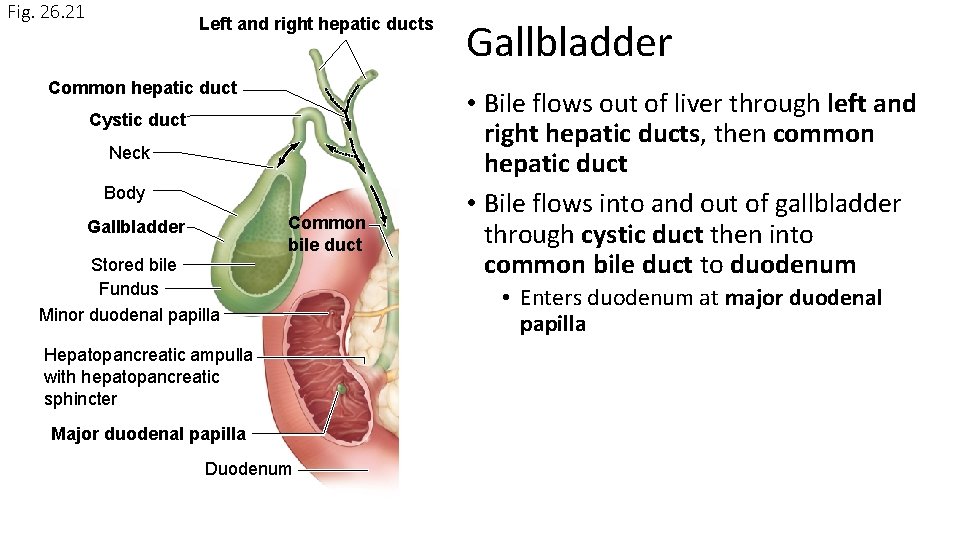
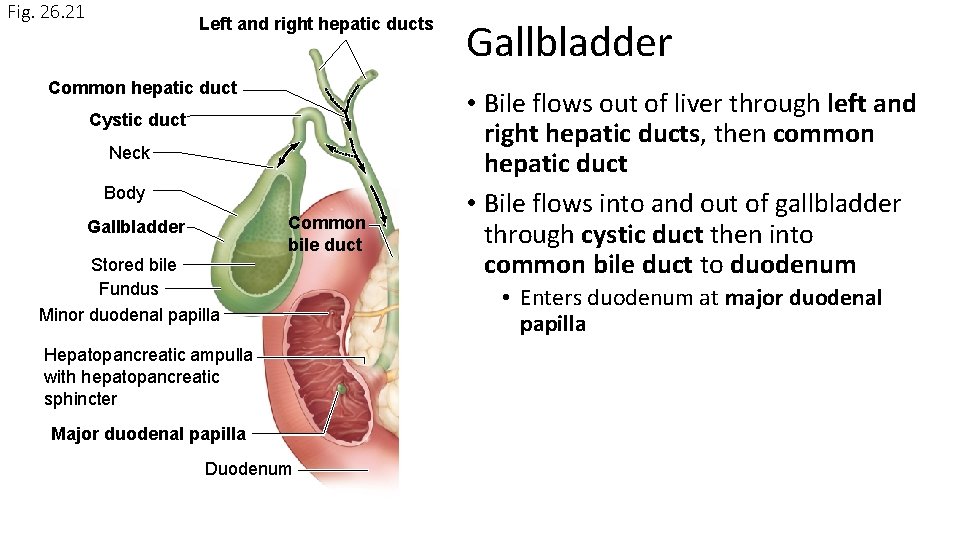
Fig. 26. 21 Left and right hepatic ducts Common hepatic duct Cystic duct Neck Body Common bile duct Gallbladder Stored bile Fundus Minor duodenal papilla Hepatopancreatic ampulla with hepatopancreatic sphincter Major duodenal papilla Duodenum Gallbladder • Bile flows out of liver through left and right hepatic ducts, then common hepatic duct • Bile flows into and out of gallbladder through cystic duct then into common bile duct to duodenum • Enters duodenum at major duodenal papilla
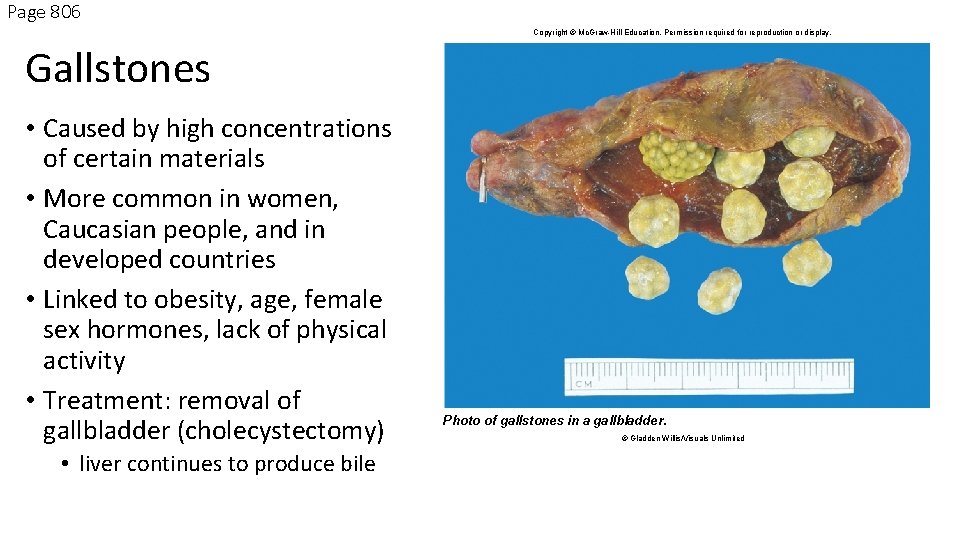
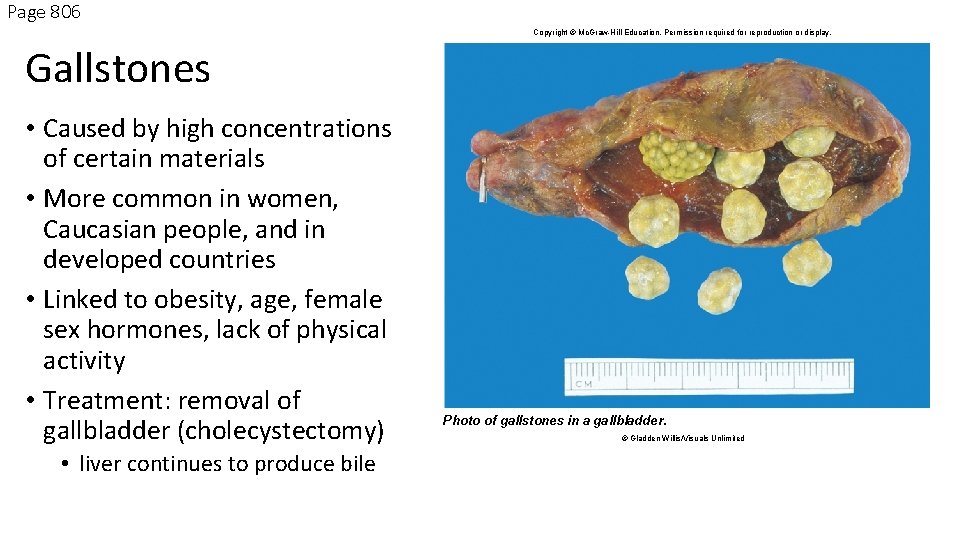
Page 806 Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display. Gallstones • Caused by high concentrations of certain materials • More common in women, Caucasian people, and in developed countries • Linked to obesity, age, female sex hormones, lack of physical activity • Treatment: removal of gallbladder (cholecystectomy) • liver continues to produce bile Photo of gallstones in a gallbladder. © Gladden Willis/Visuals Unlimited
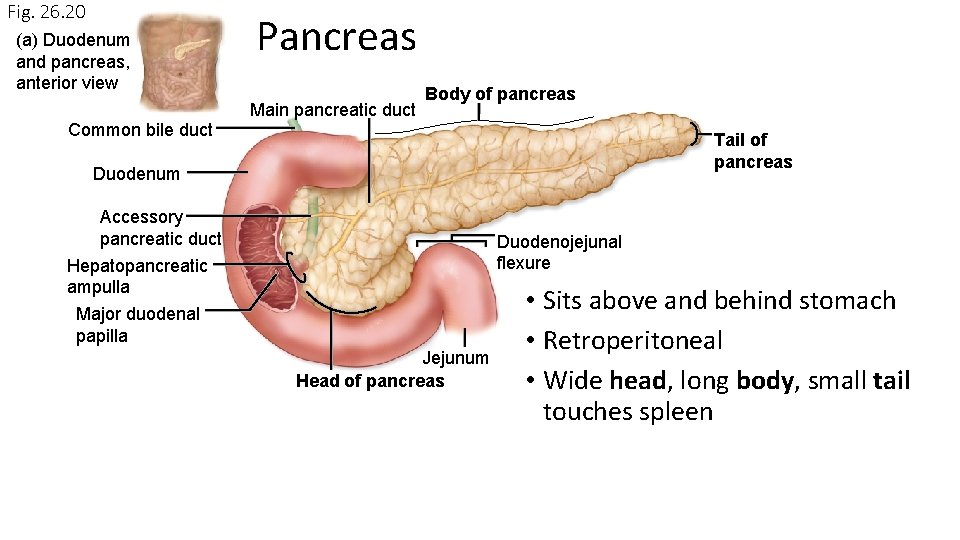
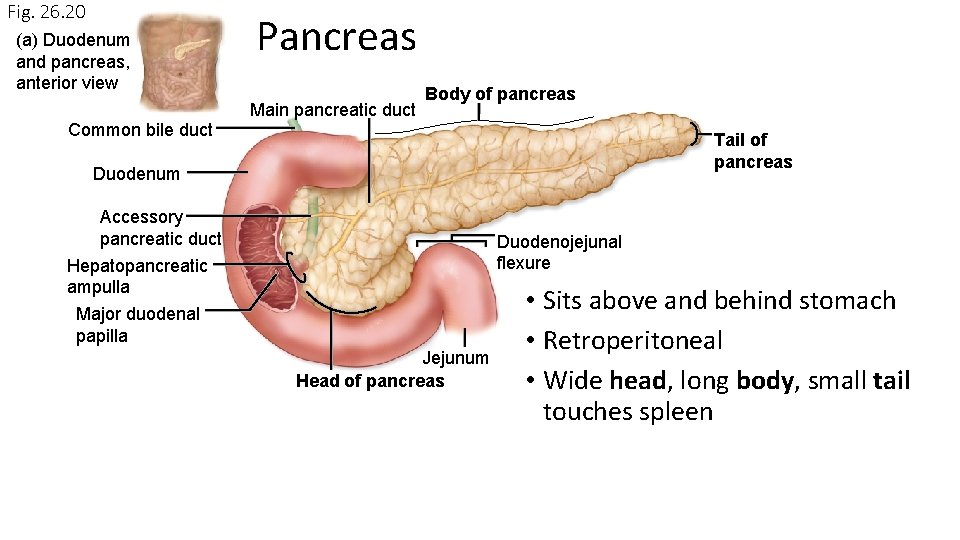
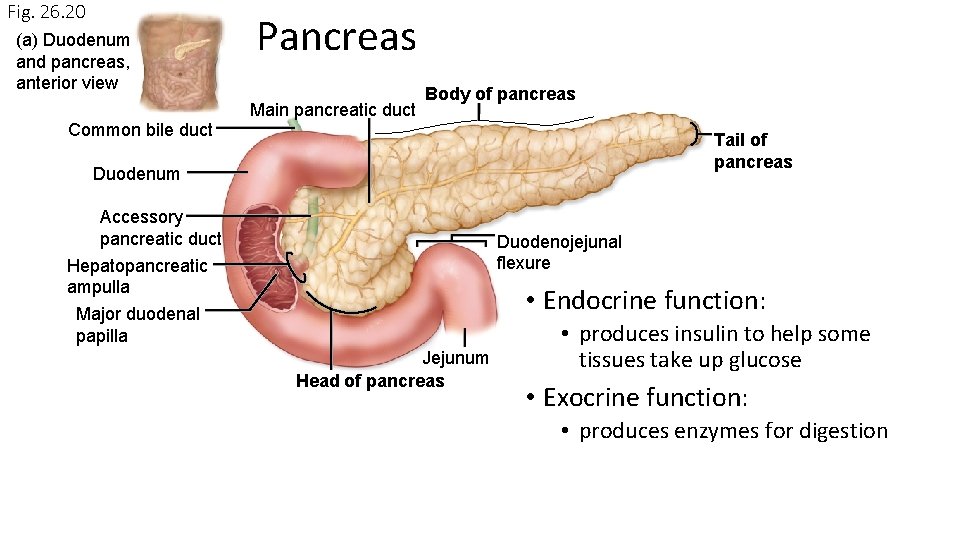
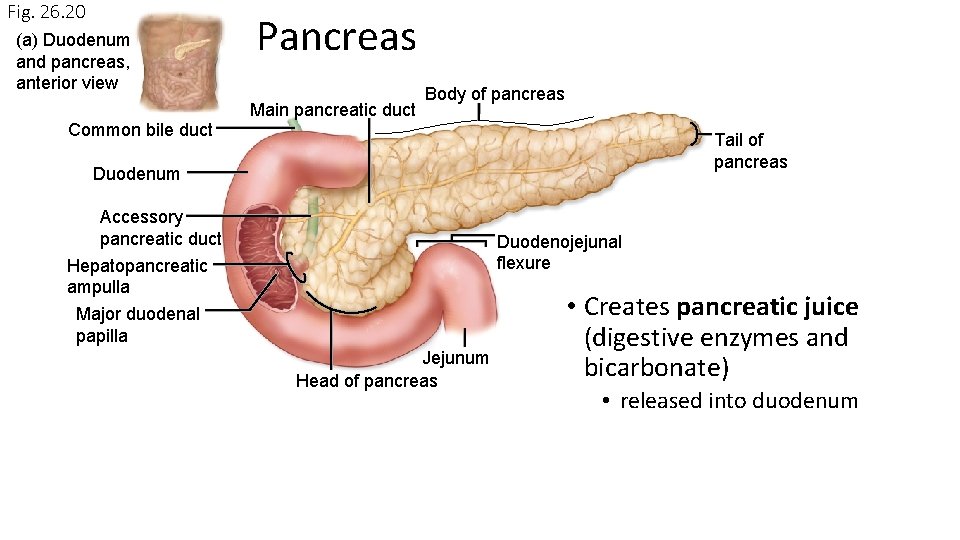
Fig. 26. 20 (a) Duodenum and pancreas, anterior view Common bile duct Pancreas Main pancreatic duct Body of pancreas Tail of pancreas Duodenum Accessory pancreatic duct Hepatopancreatic ampulla Duodenojejunal flexure Major duodenal papilla Jejunum Head of pancreas • Sits above and behind stomach • Retroperitoneal • Wide head, long body, small tail touches spleen
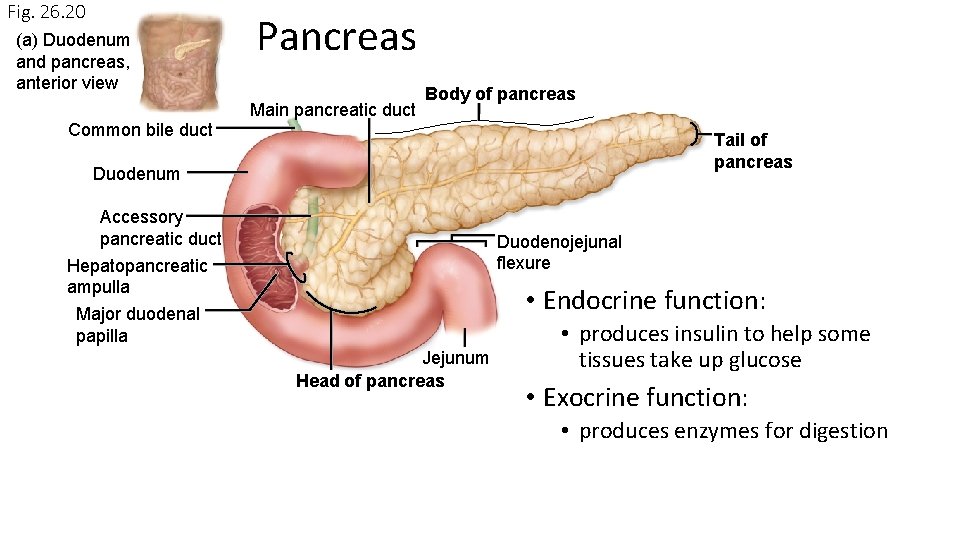
Fig. 26. 20 (a) Duodenum and pancreas, anterior view Common bile duct Pancreas Main pancreatic duct Body of pancreas Tail of pancreas Duodenum Accessory pancreatic duct Hepatopancreatic ampulla Duodenojejunal flexure • Endocrine function: Major duodenal papilla Jejunum Head of pancreas • produces insulin to help some tissues take up glucose • Exocrine function: • produces enzymes for digestion
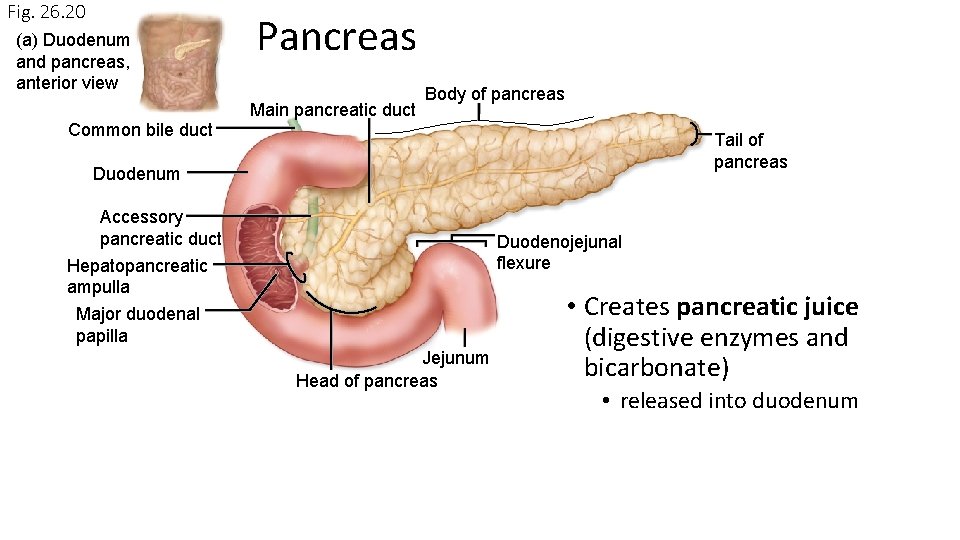
Fig. 26. 20 (a) Duodenum and pancreas, anterior view Common bile duct Pancreas Main pancreatic duct Body of pancreas Tail of pancreas Duodenum Accessory pancreatic duct Hepatopancreatic ampulla Duodenojejunal flexure Major duodenal papilla Jejunum Head of pancreas • Creates pancreatic juice (digestive enzymes and bicarbonate) • released into duodenum
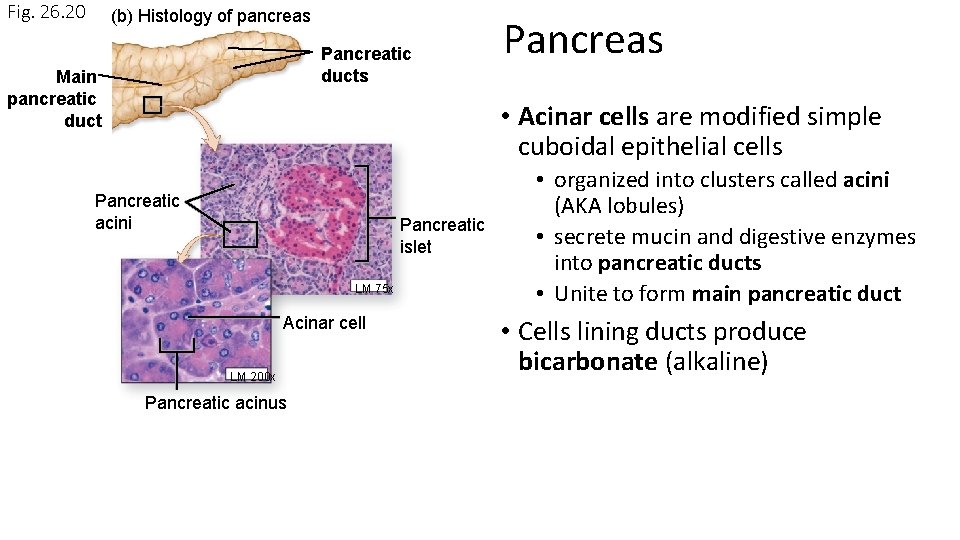
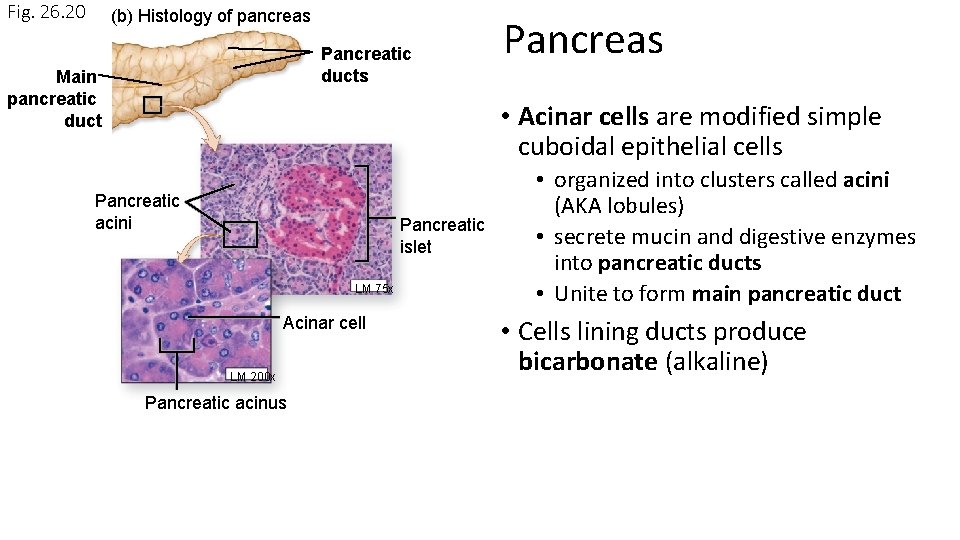
Fig. 26. 20 (b) Histology of pancreas Pancreatic ducts Main pancreatic duct Pancreas • Acinar cells are modified simple cuboidal epithelial cells Pancreatic acini Pancreatic islet LM 75 x Acinar cell LM 200 x Pancreatic acinus • organized into clusters called acini (AKA lobules) • secrete mucin and digestive enzymes into pancreatic ducts • Unite to form main pancreatic duct • Cells lining ducts produce bicarbonate (alkaline)
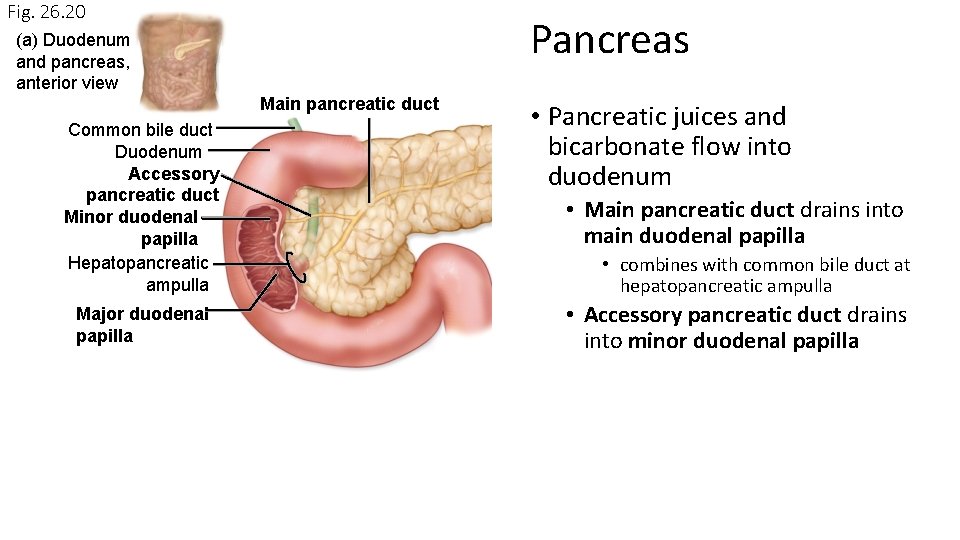
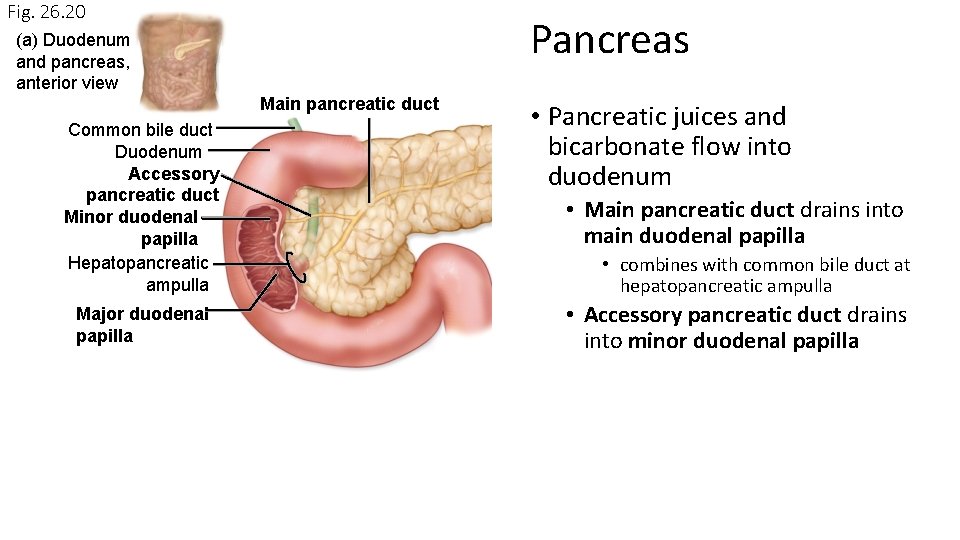
Fig. 26. 20 Pancreas (a) Duodenum and pancreas, anterior view Main pancreatic duct Common bile duct Duodenum Accessory pancreatic duct Minor duodenal papilla Hepatopancreatic ampulla Major duodenal papilla • Pancreatic juices and bicarbonate flow into duodenum • Main pancreatic duct drains into main duodenal papilla • combines with common bile duct at hepatopancreatic ampulla • Accessory pancreatic duct drains into minor duodenal papilla
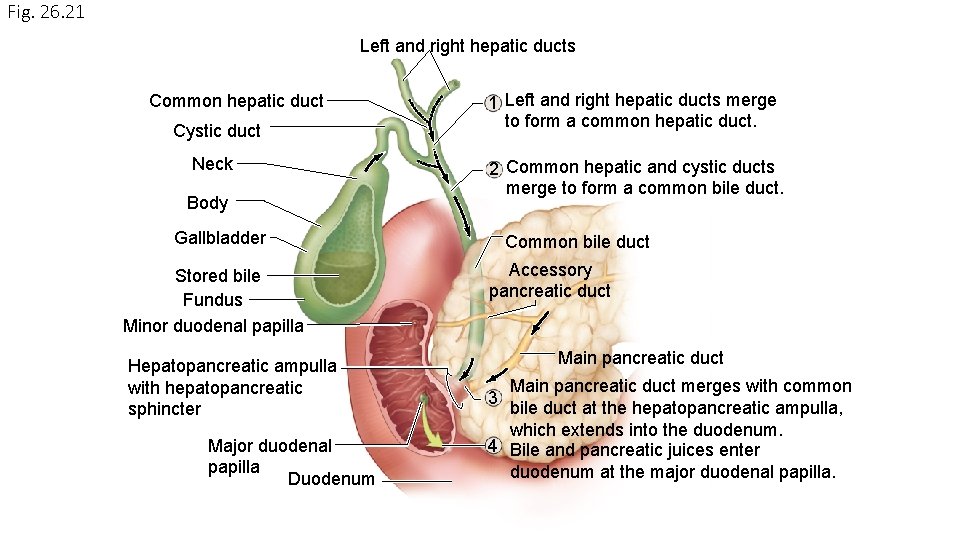
Fig. 26. 21 Left and right hepatic ducts Common hepatic duct Cystic duct Neck Body 1 Left and right hepatic ducts merge to form a common hepatic duct. 2 Common hepatic and cystic ducts merge to form a common bile duct. Gallbladder Stored bile Fundus Minor duodenal papilla Hepatopancreatic ampulla with hepatopancreatic sphincter Major duodenal papilla Duodenum Common bile duct Accessory pancreatic duct Main pancreatic duct merges with common bile duct at the hepatopancreatic ampulla, which extends into the duodenum. 4 Bile and pancreatic juices enter duodenum at the major duodenal papilla. 3