Chapter 26 Digestive System Part 1 Overview Mouth
- Slides: 37
Chapter 26 Digestive System Part 1 Overview, Mouth, Esophagus
Functions of the digestive system • Ingestion • Digestion = breakdown of food into small structures and molecules • Mechanical digestion = physical breakdown by teeth, tongue, muscles • Chemical digestion = breakdown using enzymes • Propulsion • Secretion = production and release of mucin and fluids to aid digestion • Absorption = movement of electrolytes, fats, proteins, vitamins, water across GI tract into blood and lymph vessels • Elimination = get rid of waste
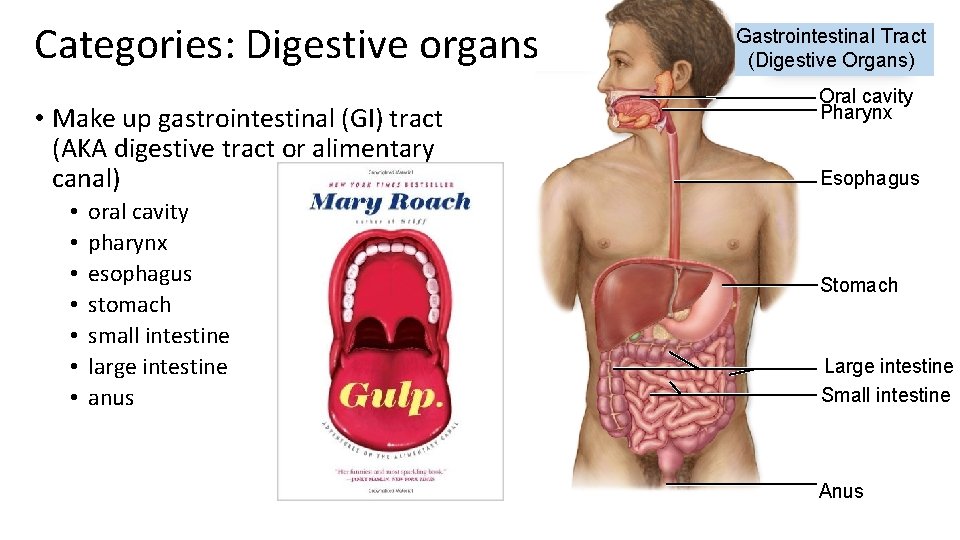
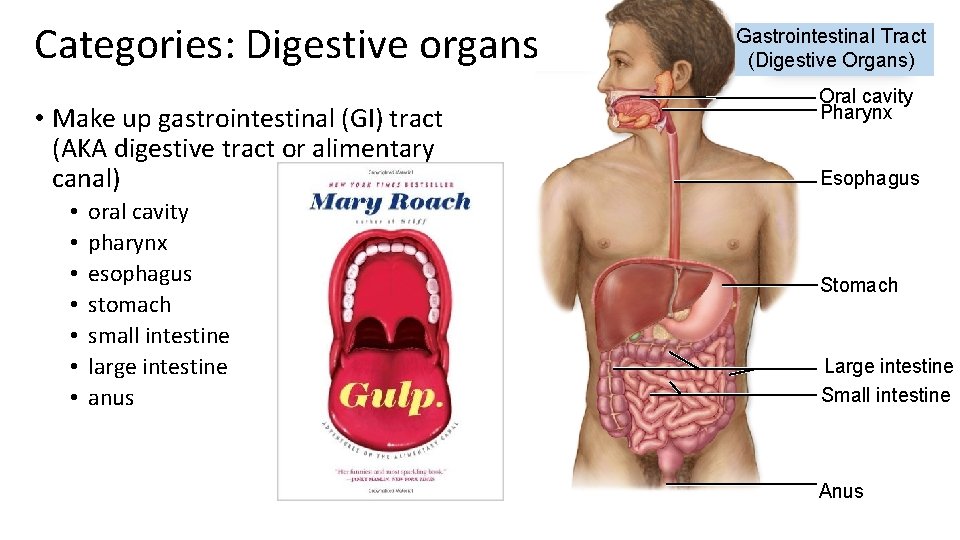
Categories: Digestive organs • Make up gastrointestinal (GI) tract (AKA digestive tract or alimentary canal) • • oral cavity pharynx esophagus stomach small intestine large intestine anus Gastrointestinal Tract (Digestive Organs) Oral cavity Pharynx Esophagus Stomach Large intestine Small intestine Anus
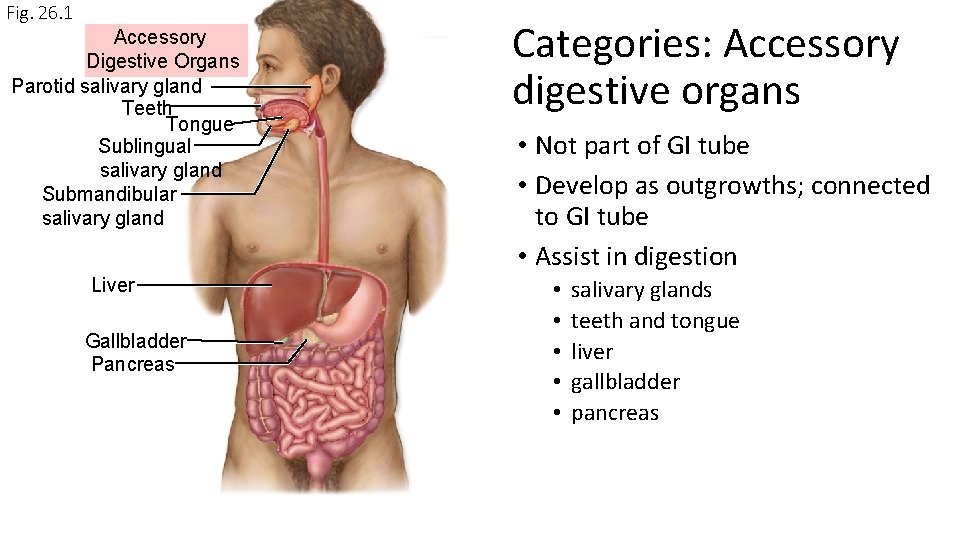
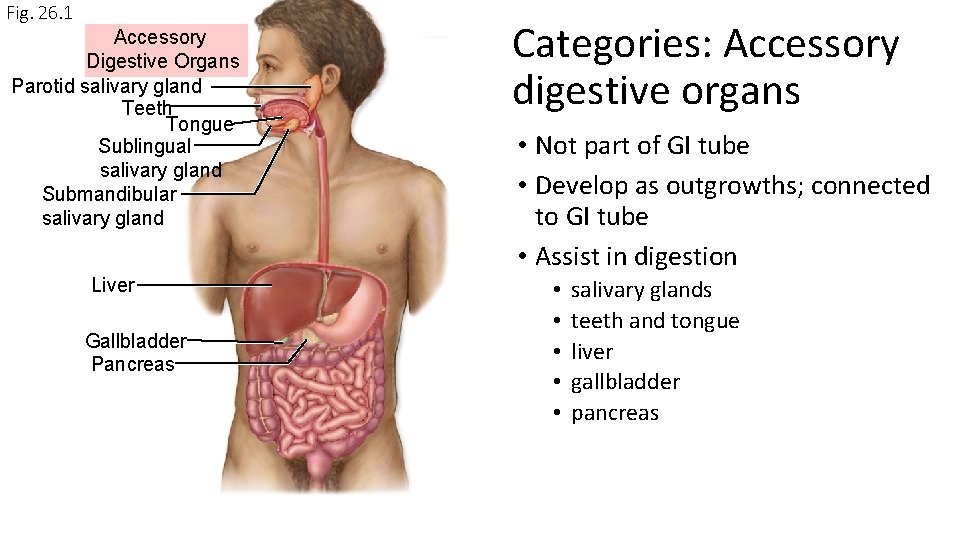
Fig. 26. 1 Accessory Digestive Organs Parotid salivary gland Teeth Tongue Sublingual salivary gland Submandibular salivary gland Liver Gallbladder Pancreas Categories: Accessory digestive organs • Not part of GI tube • Develop as outgrowths; connected to GI tube • Assist in digestion • • • salivary glands teeth and tongue liver gallbladder pancreas
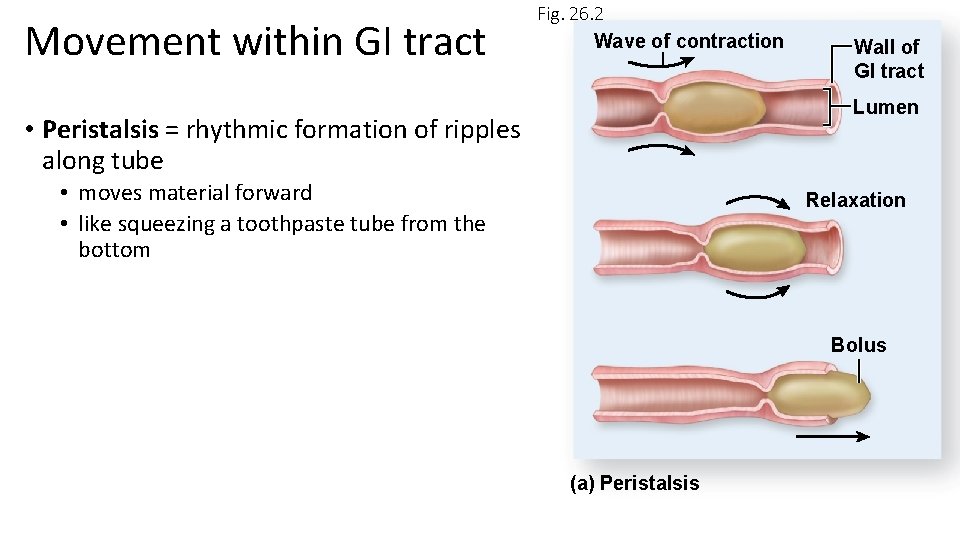
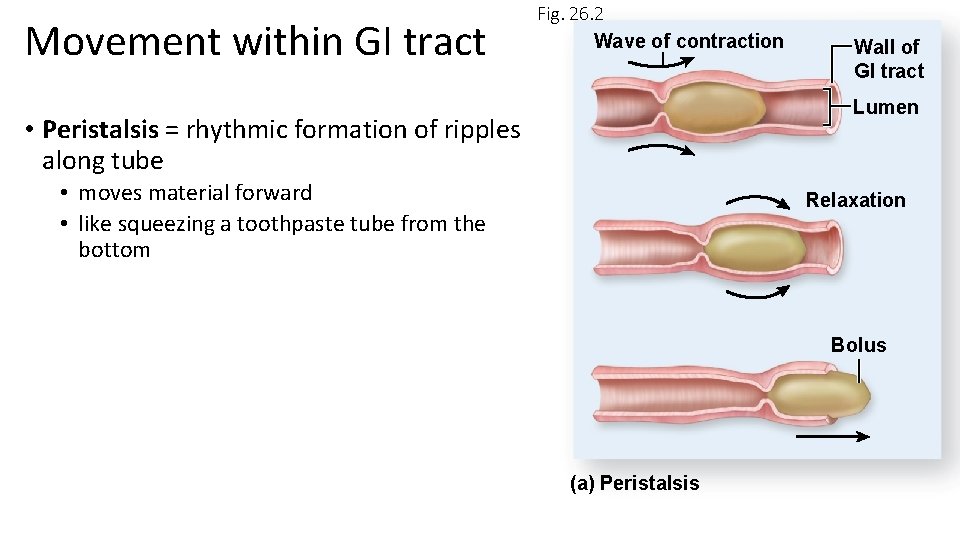
Movement within GI tract Fig. 26. 2 Wave of contraction Wall of GI tract Lumen • Peristalsis = rhythmic formation of ripples along tube • moves material forward • like squeezing a toothpaste tube from the bottom Relaxation Bolus (a) Peristalsis
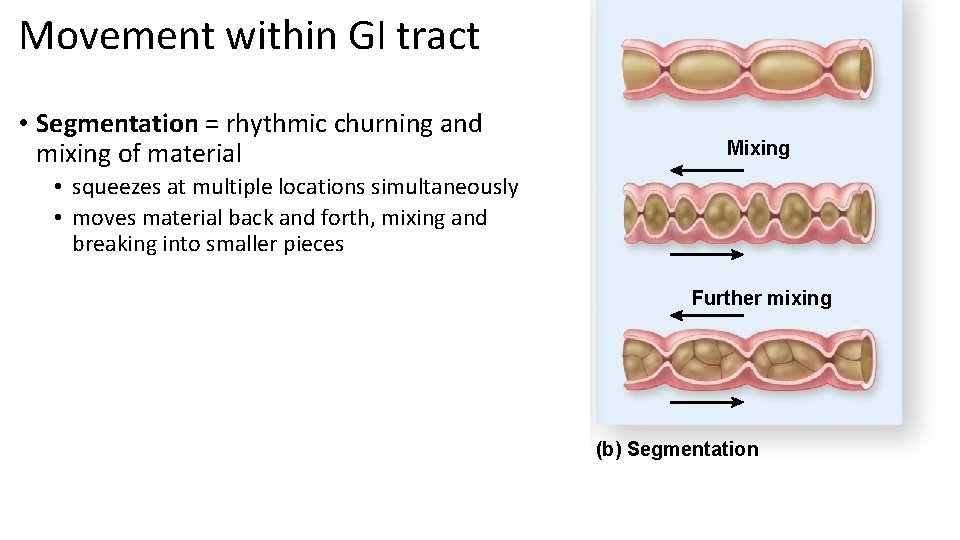
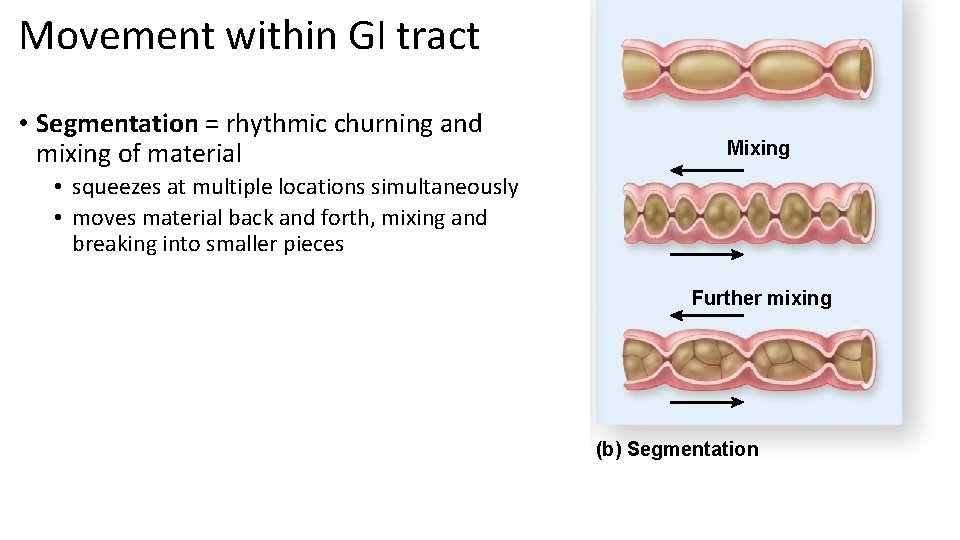
Movement within GI tract • Segmentation = rhythmic churning and mixing of material Mixing • squeezes at multiple locations simultaneously • moves material back and forth, mixing and breaking into smaller pieces Further mixing (b) Segmentation
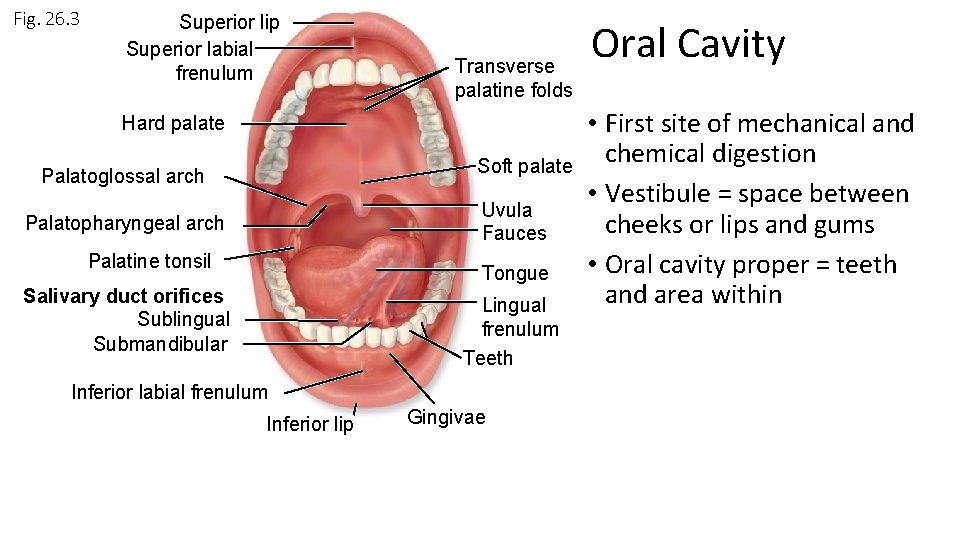
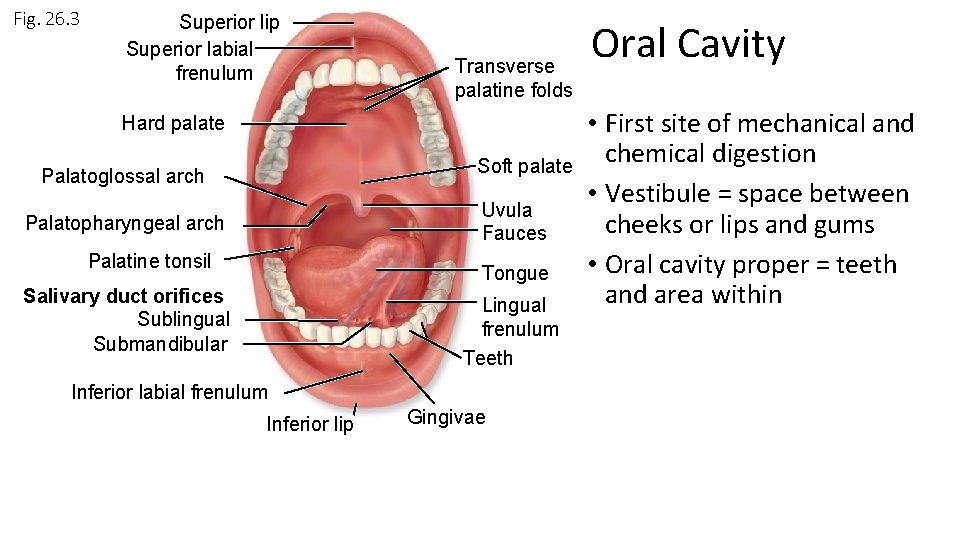
Fig. 26. 3 Superior lip Superior labial frenulum Transverse palatine folds Hard palate Soft palate Palatoglossal arch Uvula Fauces Palatopharyngeal arch Palatine tonsil Tongue Salivary duct orifices Sublingual Submandibular Lingual frenulum Teeth Inferior labial frenulum Inferior lip Gingivae Oral Cavity • First site of mechanical and chemical digestion • Vestibule = space between cheeks or lips and gums • Oral cavity proper = teeth and area within
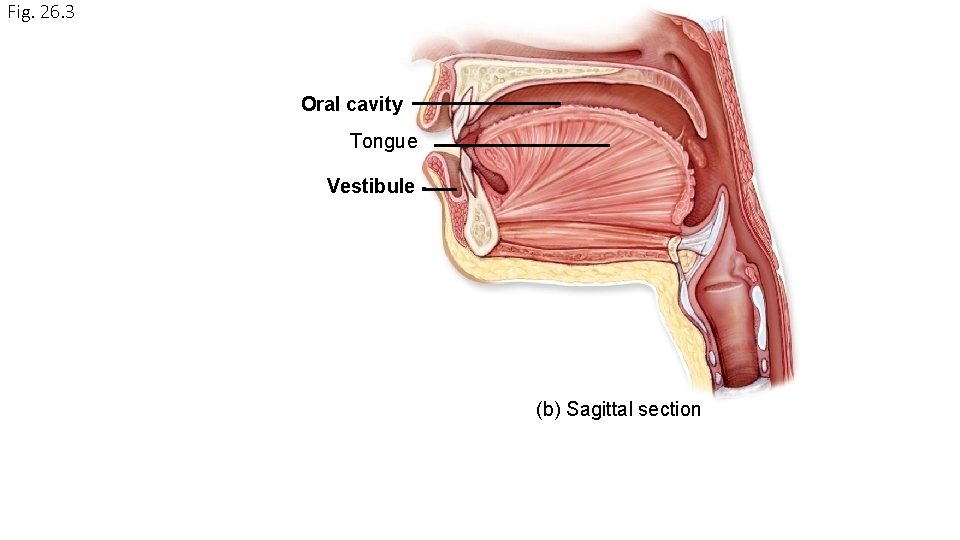
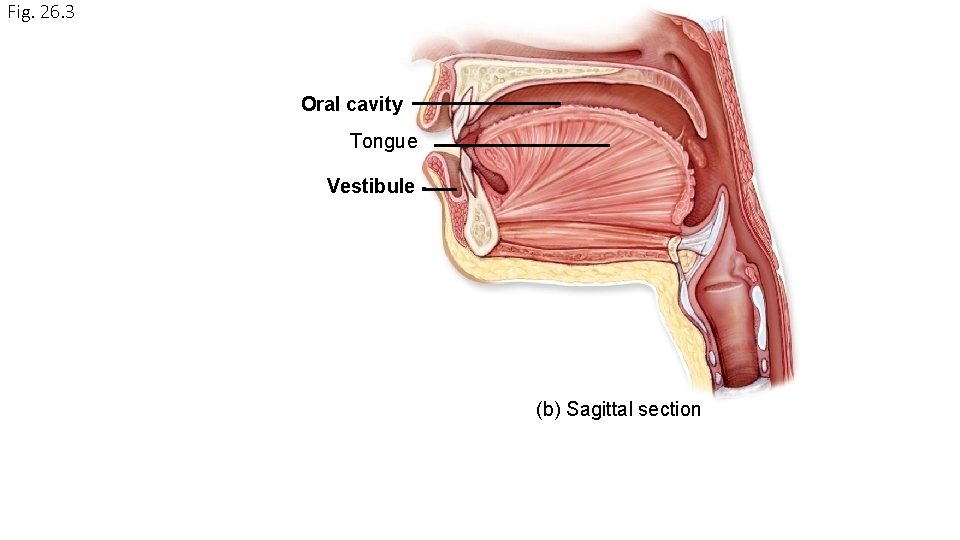
Fig. 26. 3 Oral cavity Tongue Vestibule (b) Sagittal section
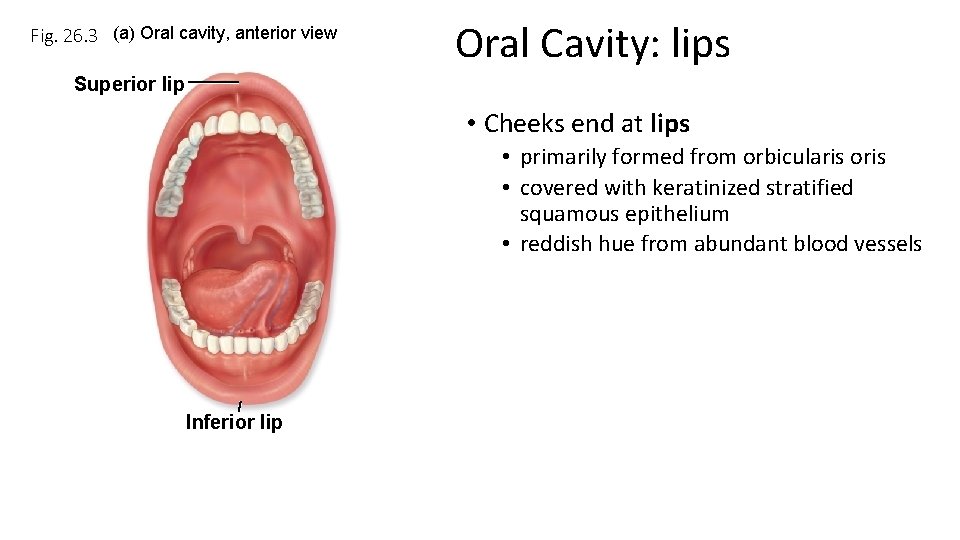
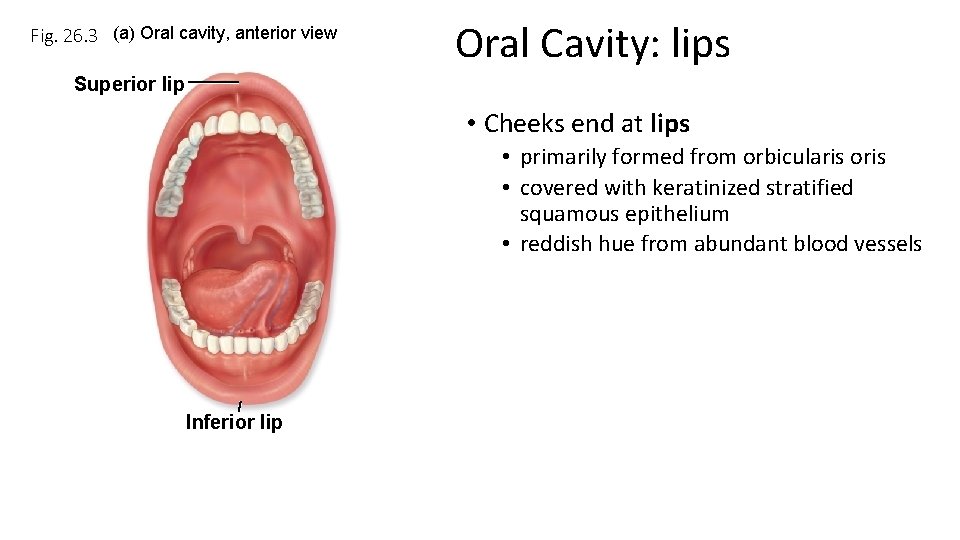
Fig. 26. 3 (a) Oral cavity, anterior view Oral Cavity: lips Superior lip • Cheeks end at lips • primarily formed from orbicularis oris • covered with keratinized stratified squamous epithelium • reddish hue from abundant blood vessels Inferior lip
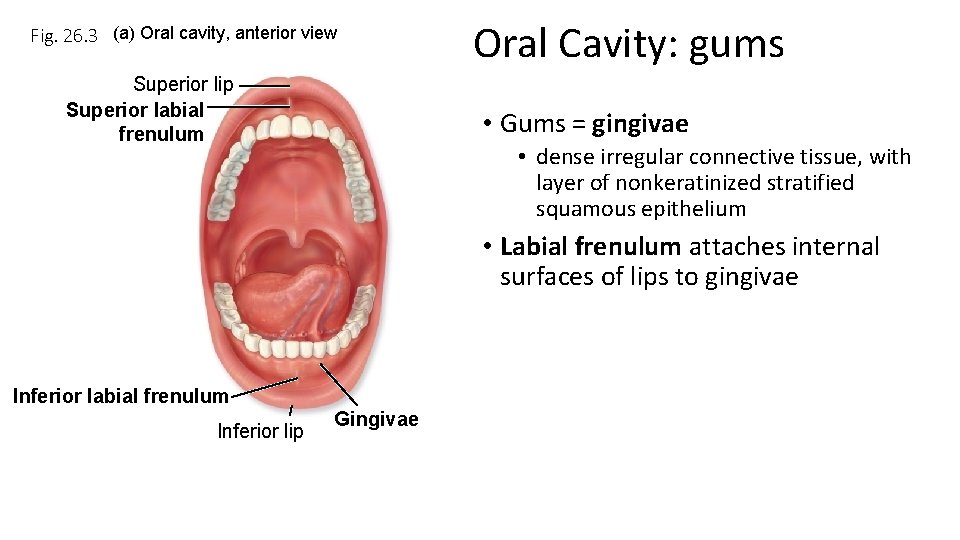
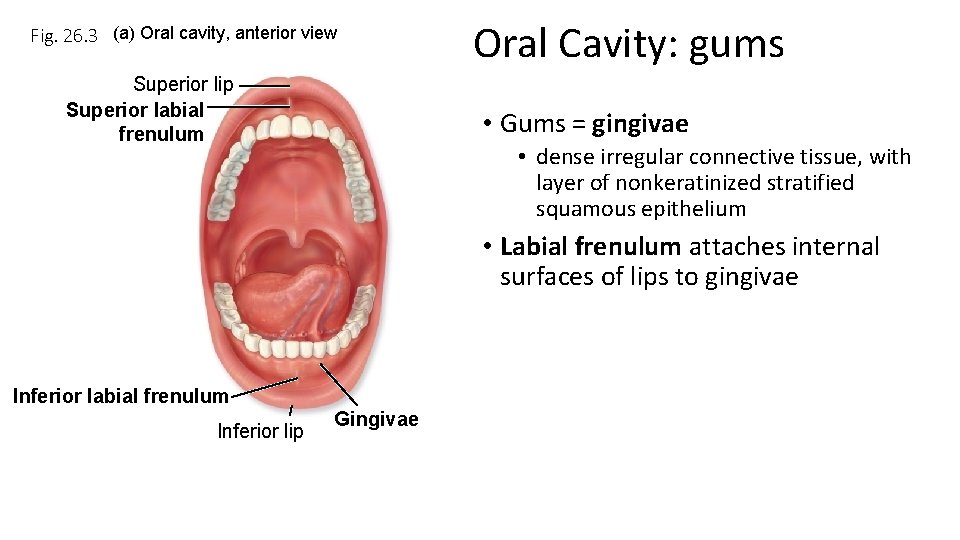
Fig. 26. 3 (a) Oral cavity, anterior view Superior lip Superior labial frenulum Oral Cavity: gums • Gums = gingivae • dense irregular connective tissue, with layer of nonkeratinized stratified squamous epithelium • Labial frenulum attaches internal surfaces of lips to gingivae Inferior labial frenulum Inferior lip Gingivae
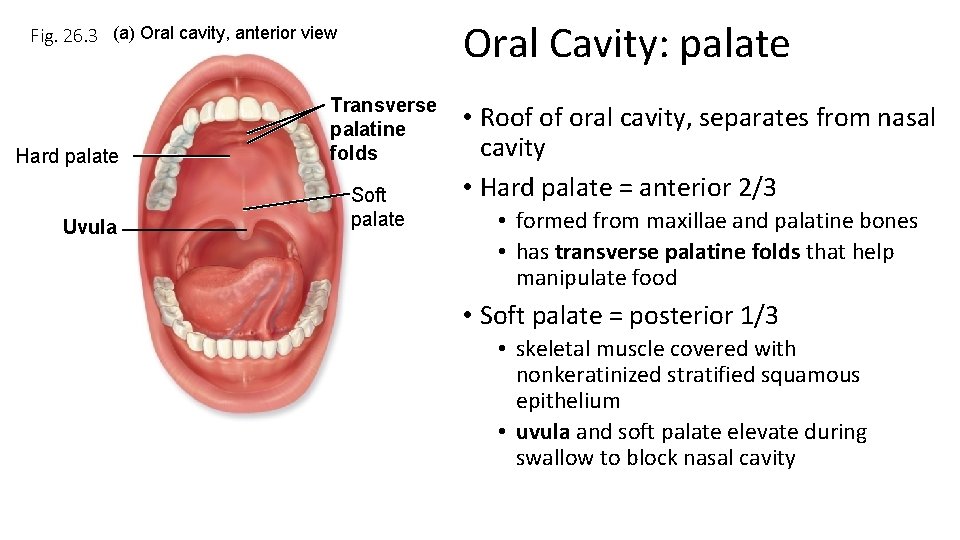
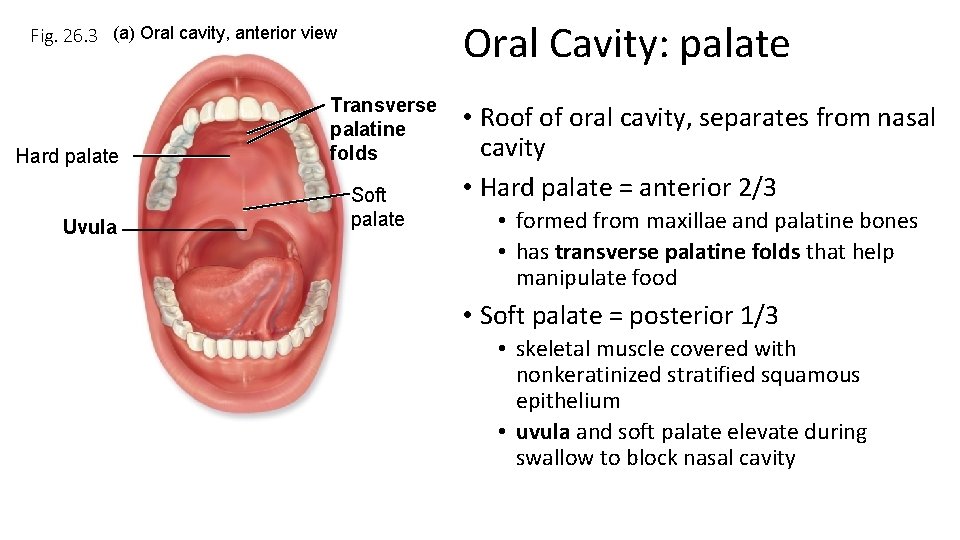
Oral Cavity: palate Fig. 26. 3 (a) Oral cavity, anterior view Hard palate Uvula Transverse palatine folds Soft palate • Roof of oral cavity, separates from nasal cavity • Hard palate = anterior 2/3 • formed from maxillae and palatine bones • has transverse palatine folds that help manipulate food • Soft palate = posterior 1/3 • skeletal muscle covered with nonkeratinized stratified squamous epithelium • uvula and soft palate elevate during swallow to block nasal cavity
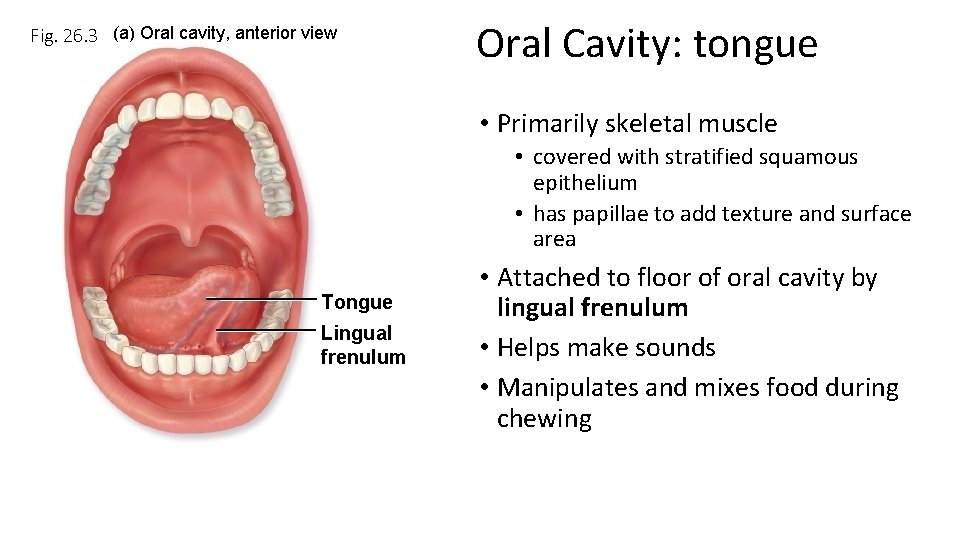
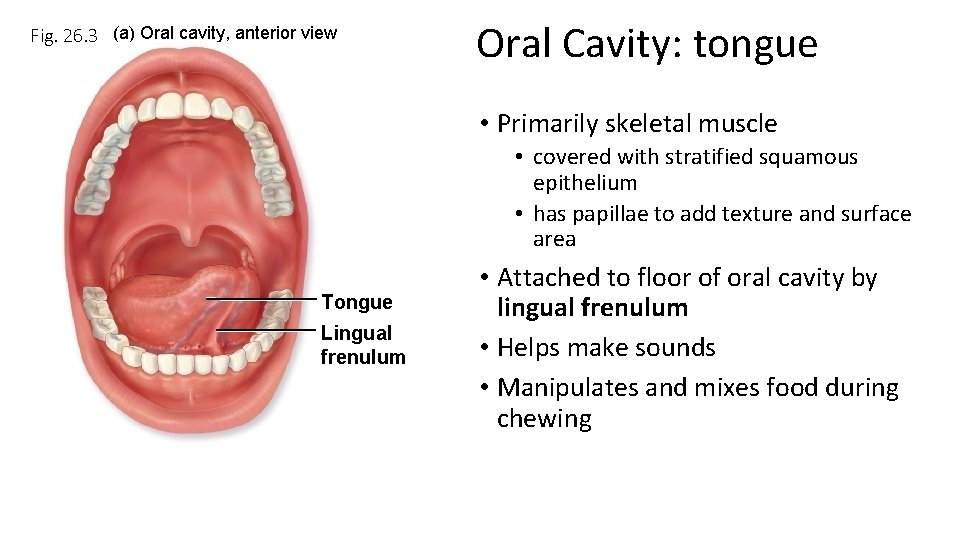
Fig. 26. 3 (a) Oral cavity, anterior view Oral Cavity: tongue • Primarily skeletal muscle • covered with stratified squamous epithelium • has papillae to add texture and surface area Tongue Lingual frenulum • Attached to floor of oral cavity by lingual frenulum • Helps make sounds • Manipulates and mixes food during chewing
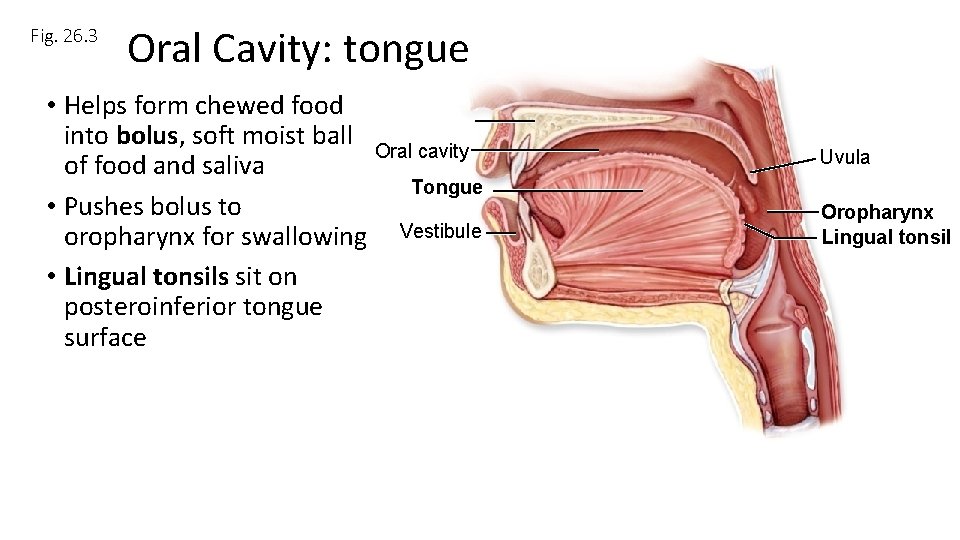
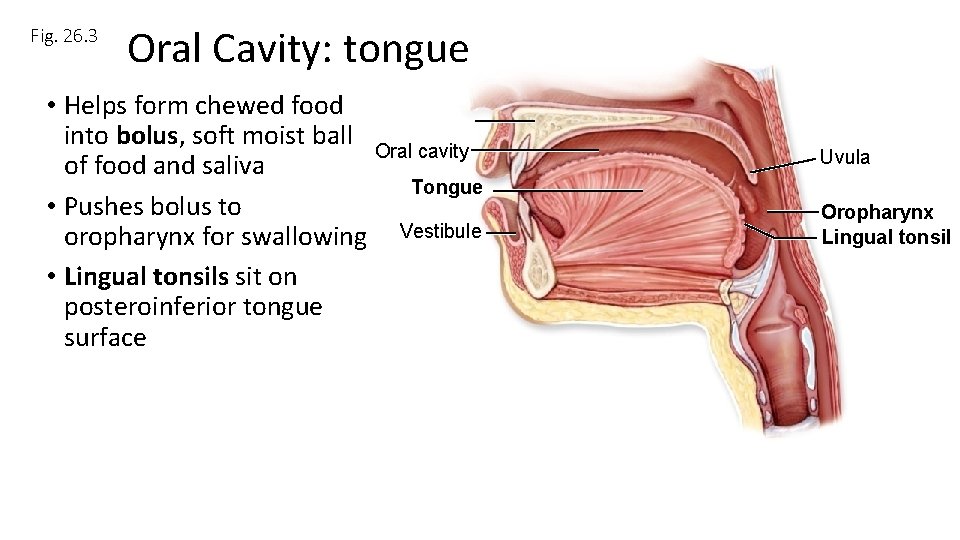
Fig. 26. 3 Oral Cavity: tongue • Helps form chewed food into bolus, soft moist ball Oral cavity of food and saliva Tongue • Pushes bolus to oropharynx for swallowing Vestibule • Lingual tonsils sit on posteroinferior tongue surface Uvula Oropharynx Lingual tonsil
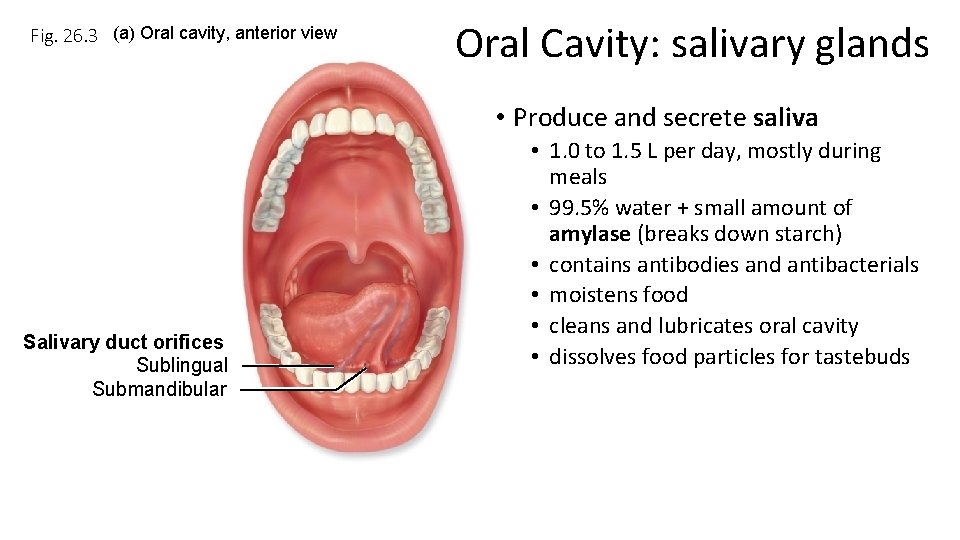
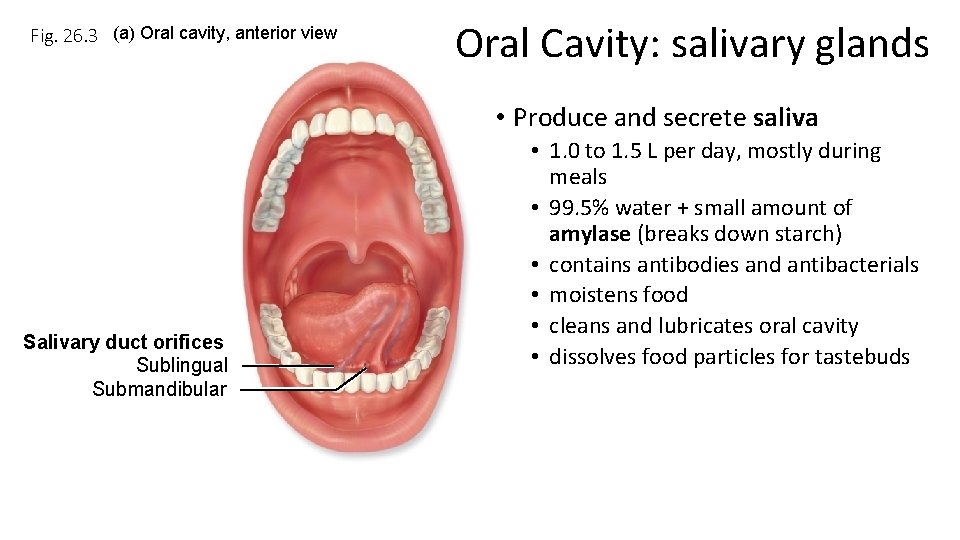
Fig. 26. 3 (a) Oral cavity, anterior view Oral Cavity: salivary glands • Produce and secrete saliva Salivary duct orifices Sublingual Submandibular • 1. 0 to 1. 5 L per day, mostly during meals • 99. 5% water + small amount of amylase (breaks down starch) • contains antibodies and antibacterials • moistens food • cleans and lubricates oral cavity • dissolves food particles for tastebuds
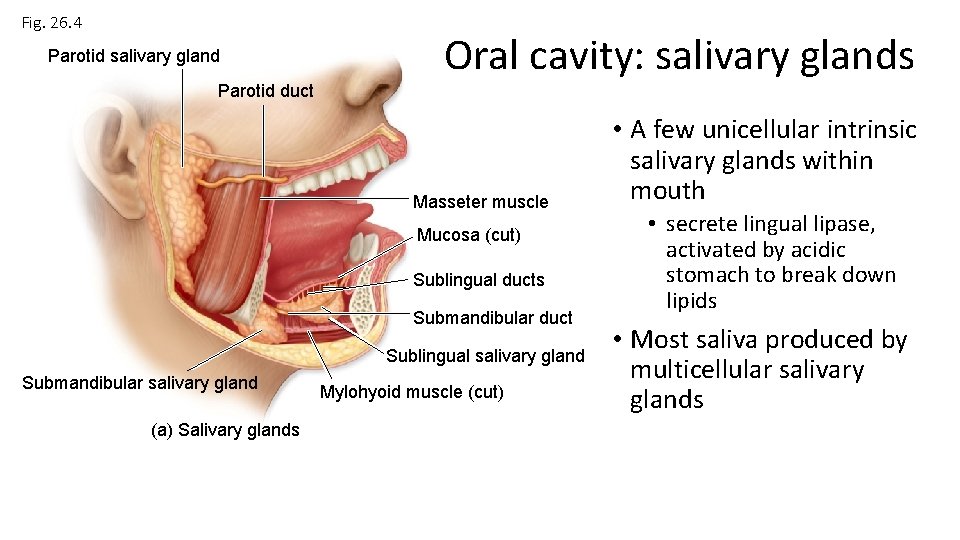
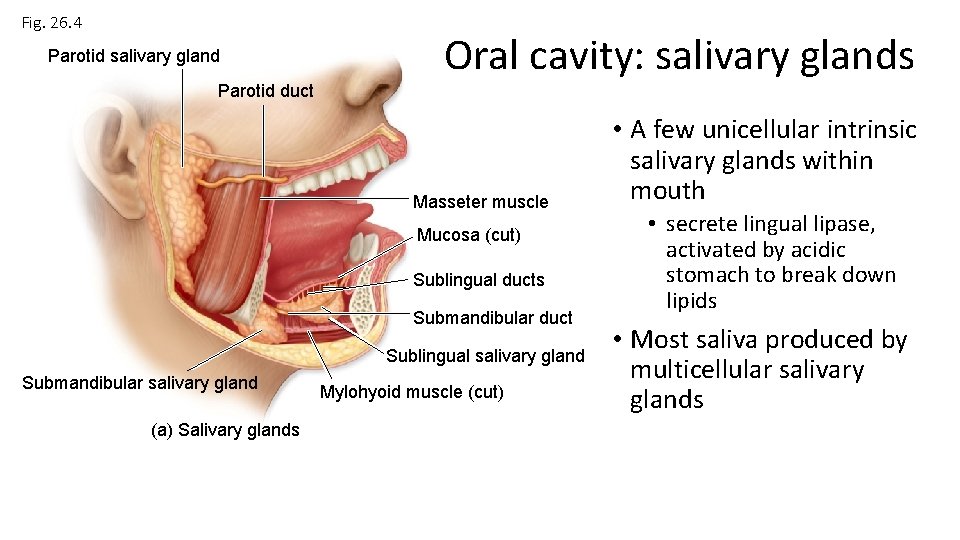
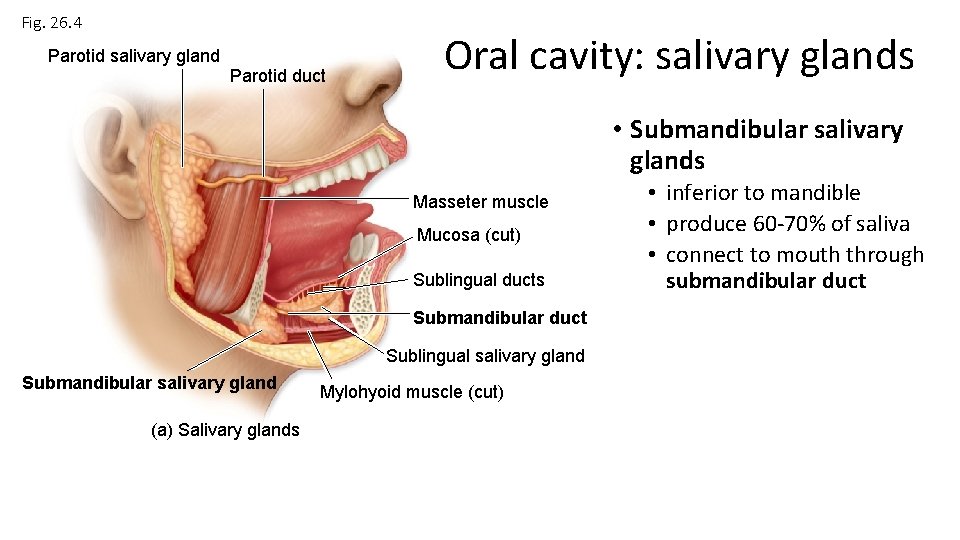
Fig. 26. 4 Parotid salivary gland Parotid duct Oral cavity: salivary glands Masseter muscle Mucosa (cut) Sublingual ducts Submandibular duct Sublingual salivary gland Submandibular salivary gland (a) Salivary glands Mylohyoid muscle (cut) • A few unicellular intrinsic salivary glands within mouth • secrete lingual lipase, activated by acidic stomach to break down lipids • Most saliva produced by multicellular salivary glands
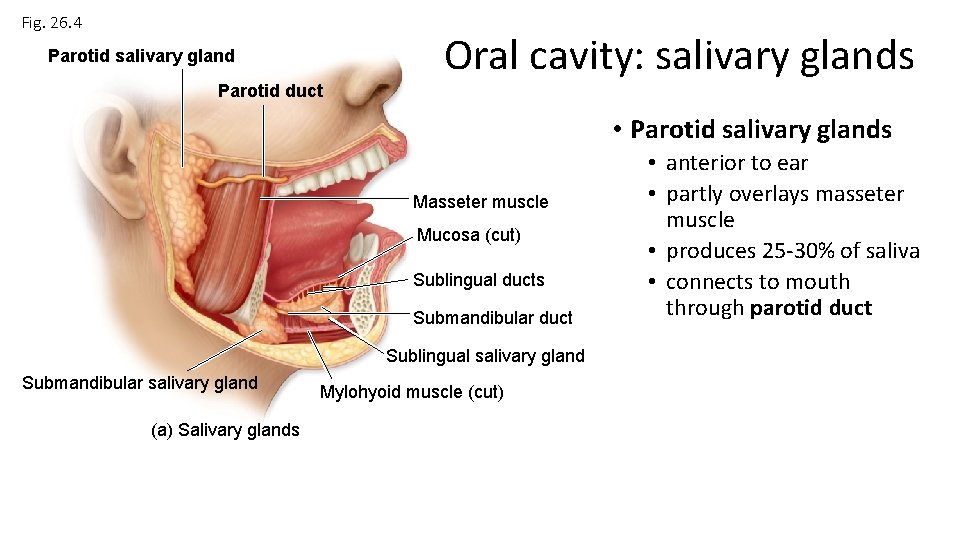
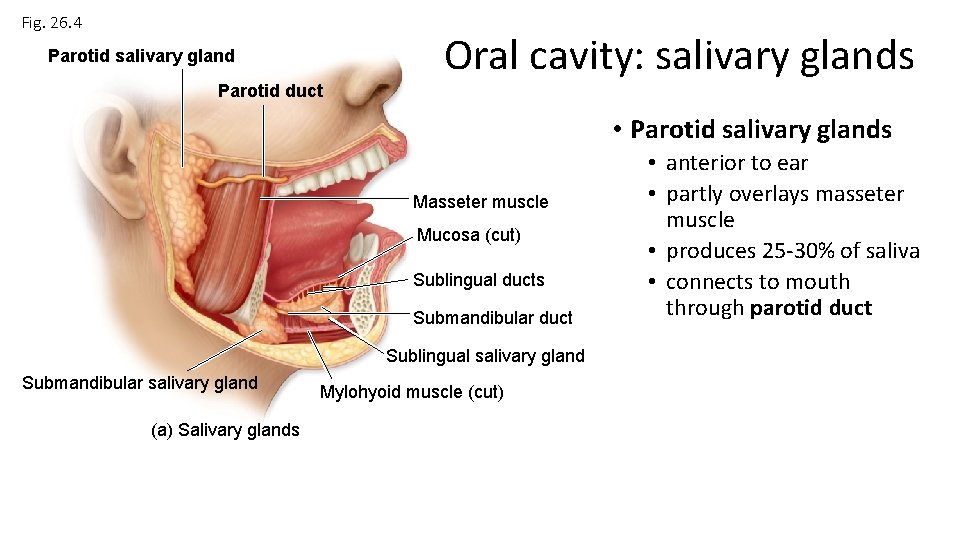
Fig. 26. 4 Parotid salivary gland Parotid duct Oral cavity: salivary glands • Parotid salivary glands Masseter muscle Mucosa (cut) Sublingual ducts Submandibular duct Sublingual salivary gland Submandibular salivary gland (a) Salivary glands Mylohyoid muscle (cut) • anterior to ear • partly overlays masseter muscle • produces 25 -30% of saliva • connects to mouth through parotid duct
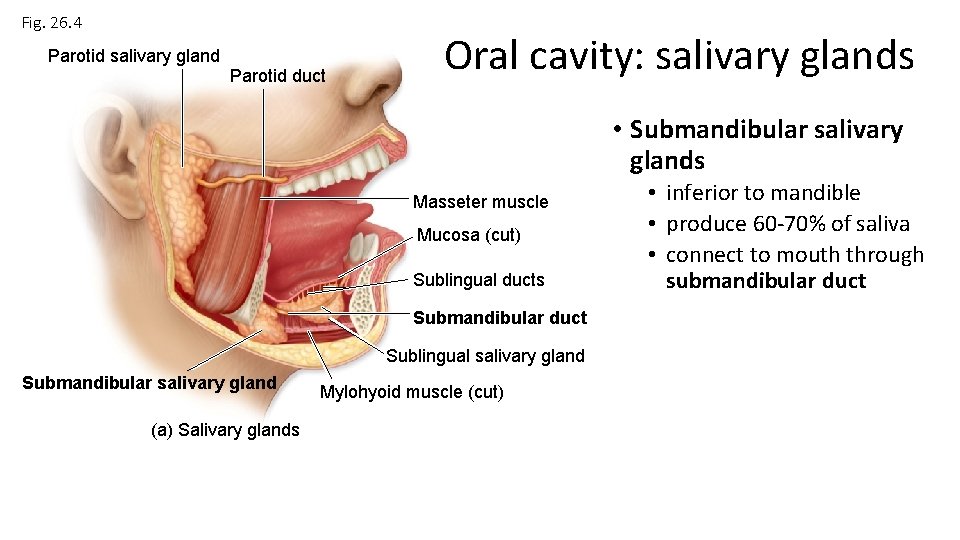
Fig. 26. 4 Parotid salivary gland Parotid duct Oral cavity: salivary glands • Submandibular salivary glands Masseter muscle Mucosa (cut) Sublingual ducts Submandibular duct Sublingual salivary gland Submandibular salivary gland (a) Salivary glands Mylohyoid muscle (cut) • inferior to mandible • produce 60 -70% of saliva • connect to mouth through submandibular duct
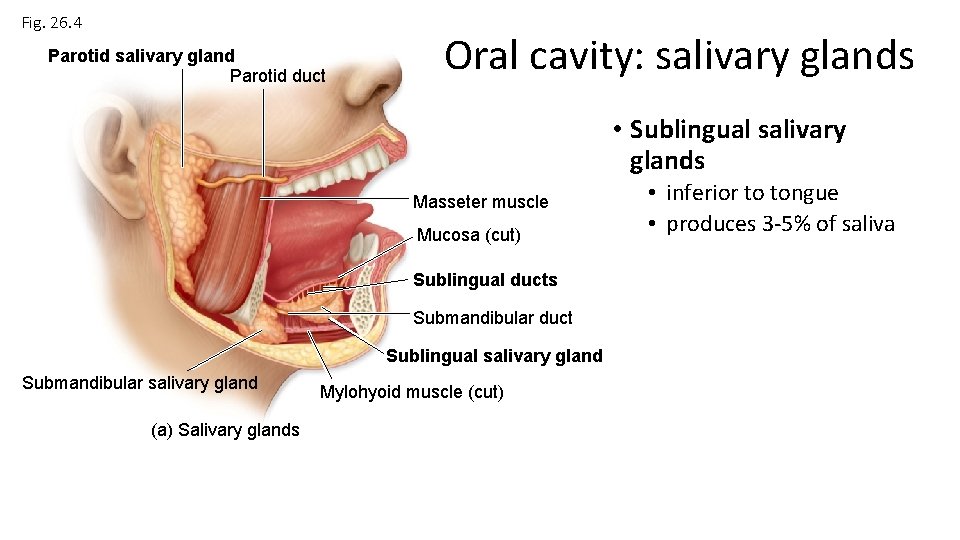
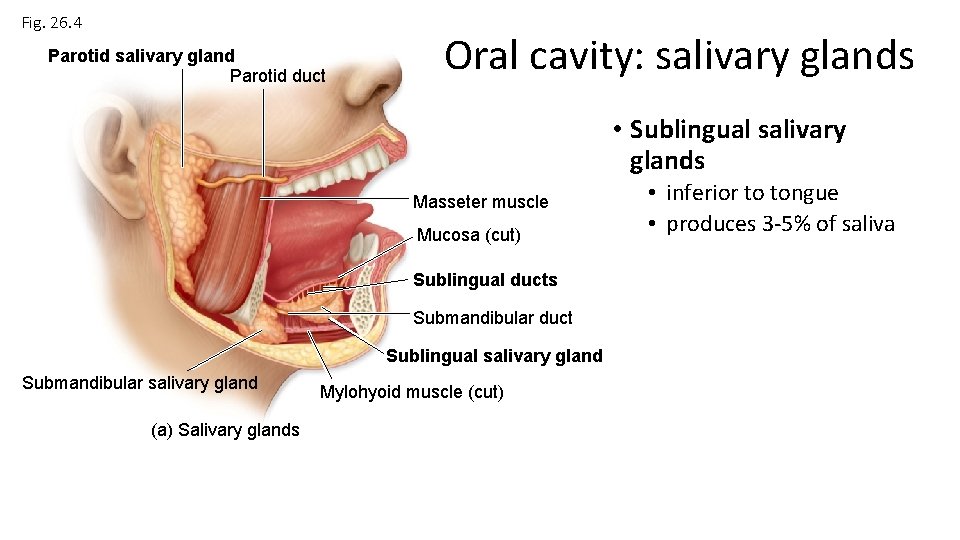
Fig. 26. 4 Parotid salivary gland Parotid duct Oral cavity: salivary glands • Sublingual salivary glands Masseter muscle Mucosa (cut) Sublingual ducts Submandibular duct Sublingual salivary gland Submandibular salivary gland (a) Salivary glands Mylohyoid muscle (cut) • inferior to tongue • produces 3 -5% of saliva
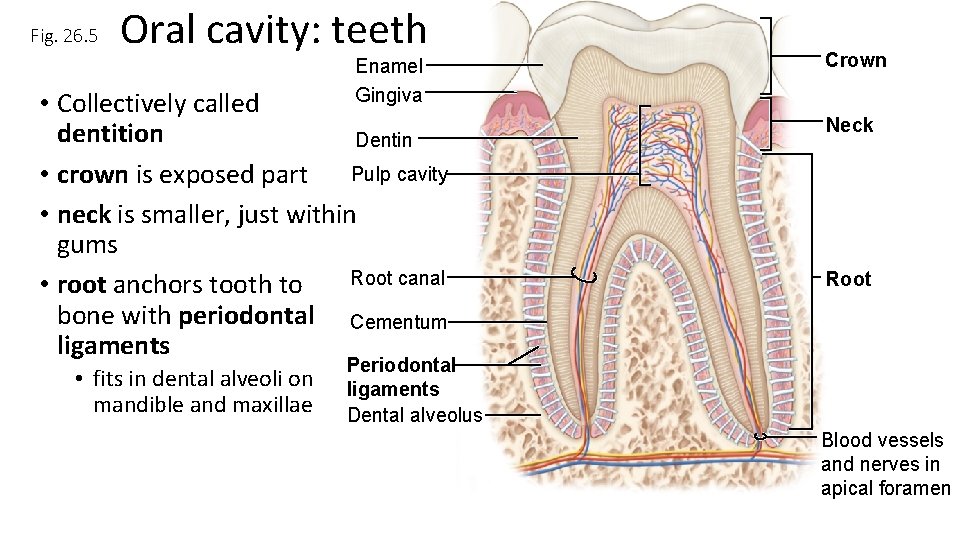
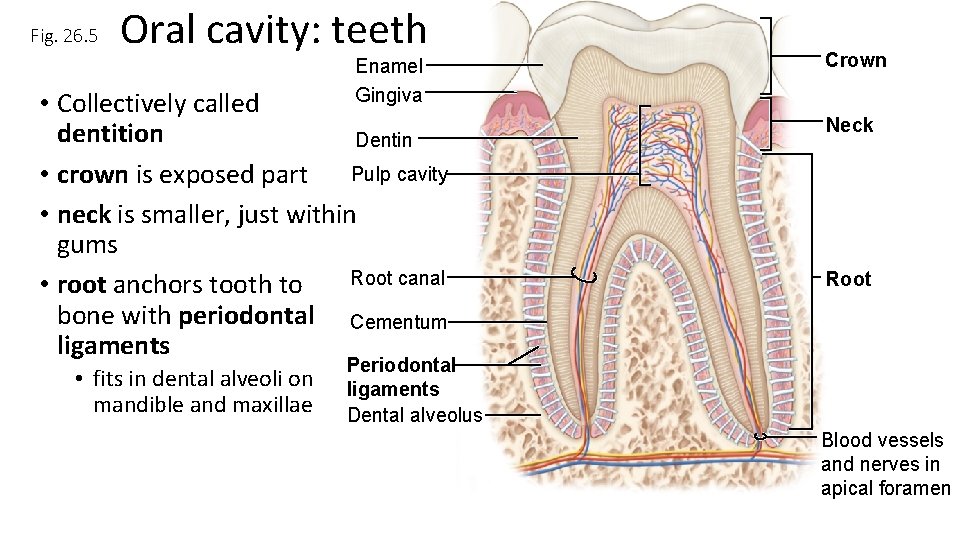
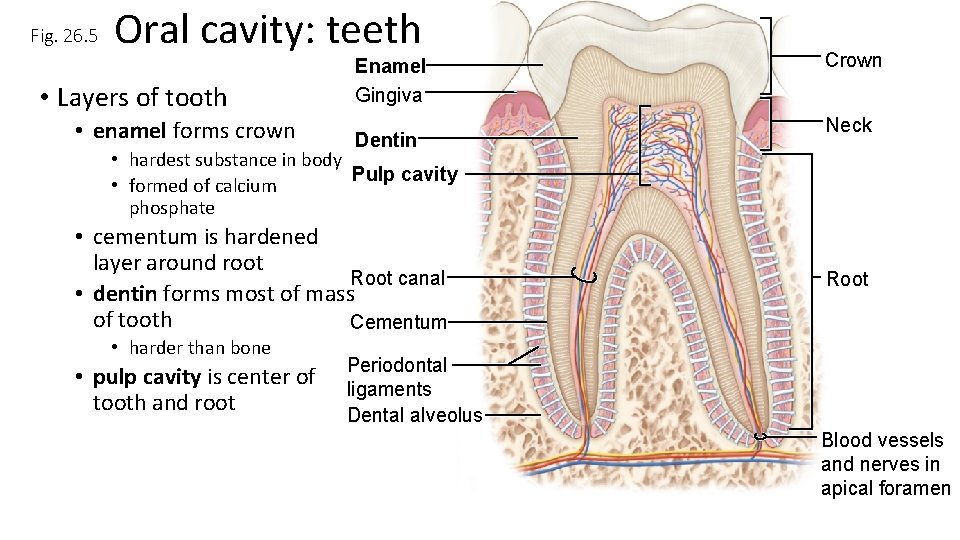
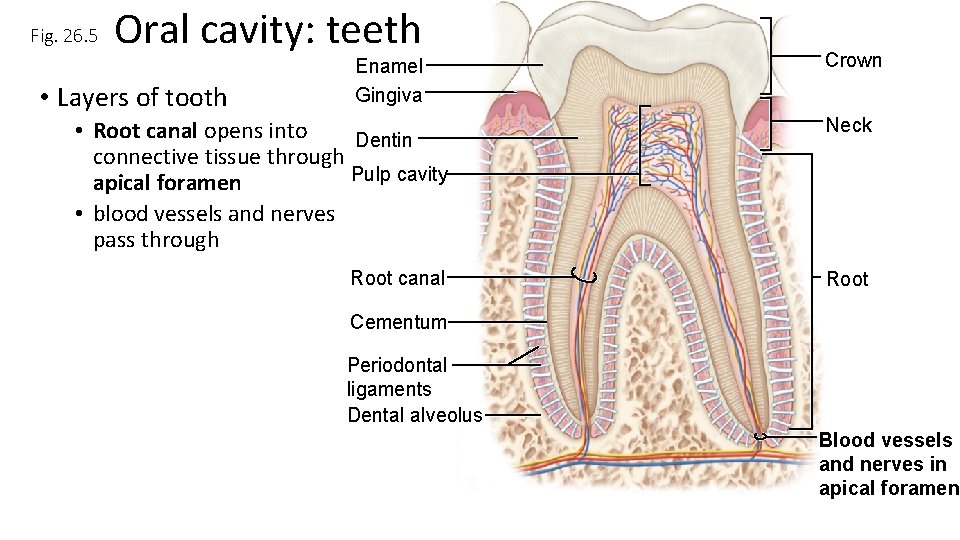
Fig. 26. 5 Oral cavity: teeth Enamel Gingiva • Collectively called dentition Dentin Pulp cavity • crown is exposed part • neck is smaller, just within gums Root canal • root anchors tooth to bone with periodontal Cementum ligaments • fits in dental alveoli on mandible and maxillae Crown Neck Root Periodontal ligaments Dental alveolus Blood vessels and nerves in apical foramen
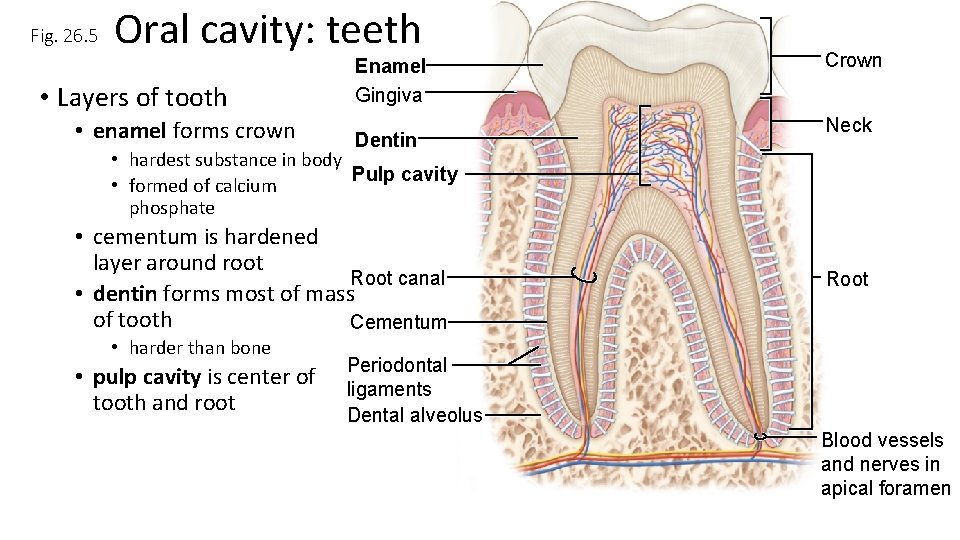
Fig. 26. 5 Oral cavity: teeth • Layers of tooth • enamel forms crown Enamel Gingiva Dentin Crown Neck • hardest substance in body Pulp cavity • formed of calcium phosphate • cementum is hardened layer around root Root canal • dentin forms most of mass of tooth Cementum • harder than bone • pulp cavity is center of tooth and root Root Periodontal ligaments Dental alveolus Blood vessels and nerves in apical foramen
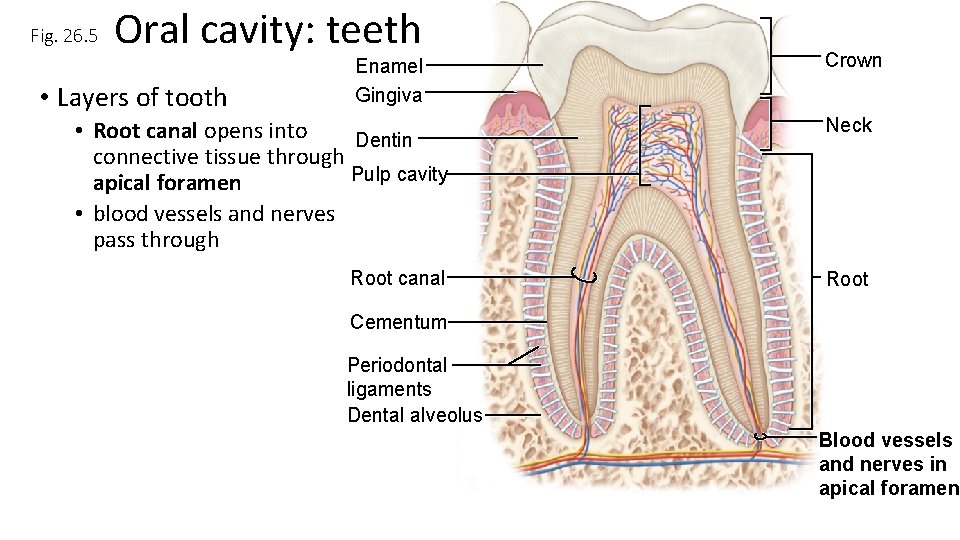
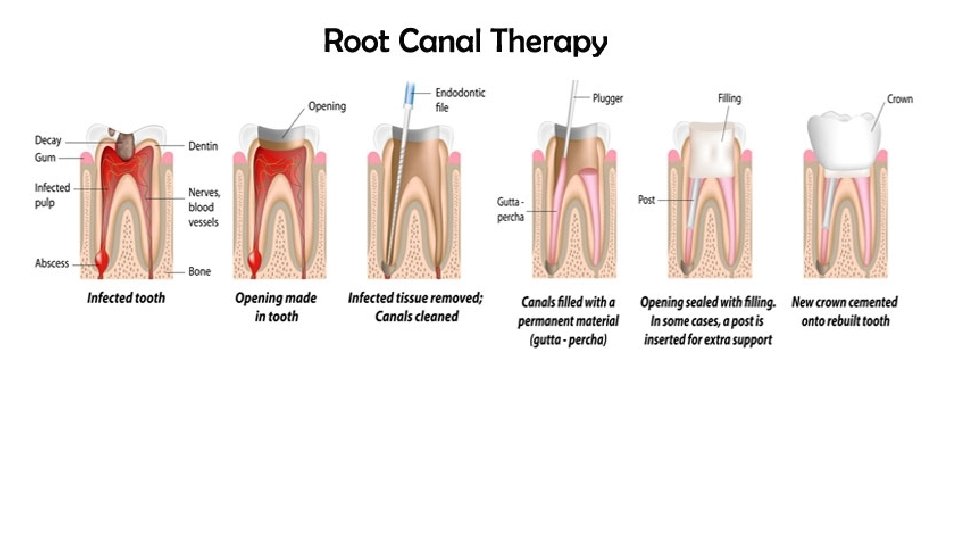
Fig. 26. 5 Oral cavity: teeth • Layers of tooth Enamel Gingiva Crown • Root canal opens into Dentin connective tissue through Pulp cavity apical foramen • blood vessels and nerves pass through Neck Root canal Root Cementum Periodontal ligaments Dental alveolus Blood vessels and nerves in apical foramen
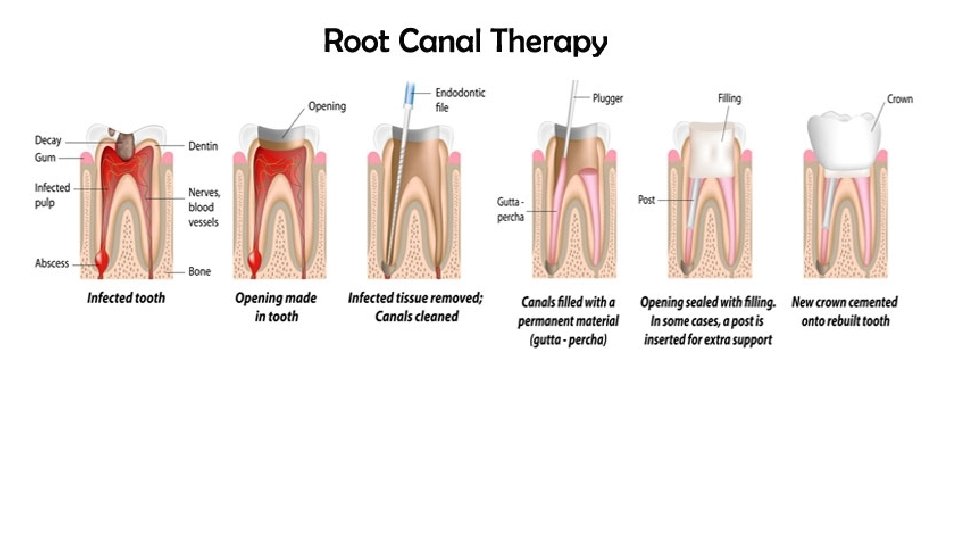
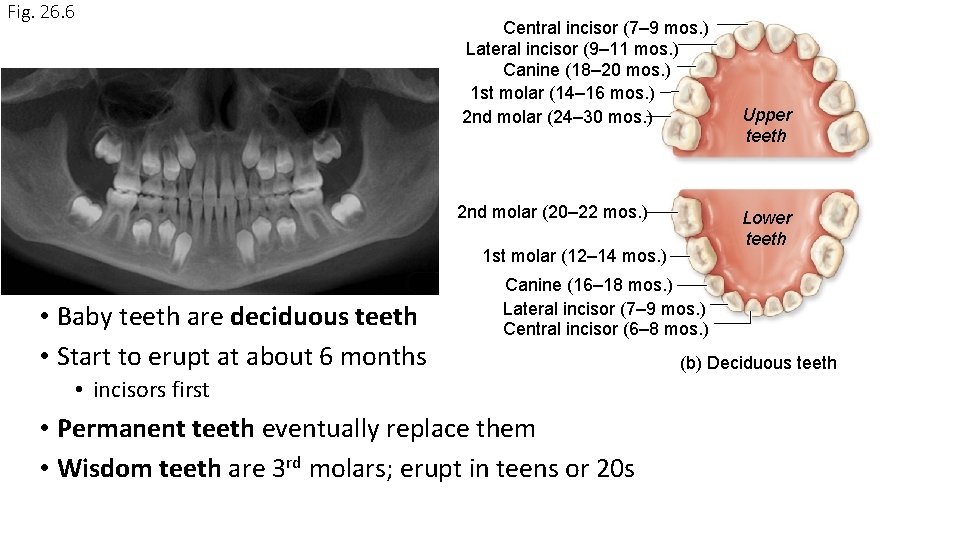
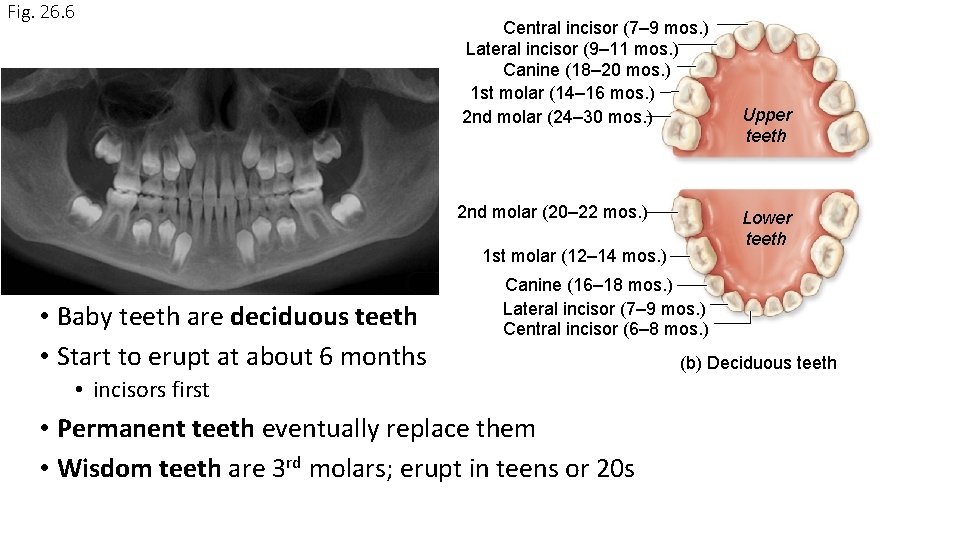
Fig. 26. 6 Central incisor (7– 9 mos. ) Lateral incisor (9– 11 mos. ) Canine (18– 20 mos. ) 1 st molar (14– 16 mos. ) 2 nd molar (24– 30 mos. ) 2 nd molar (20– 22 mos. ) Lower teeth 1 st molar (12– 14 mos. ) • Baby teeth are deciduous teeth • Start to erupt at about 6 months Upper teeth Canine (16– 18 mos. ) Lateral incisor (7– 9 mos. ) Central incisor (6– 8 mos. ) • incisors first • Permanent teeth eventually replace them • Wisdom teeth are 3 rd molars; erupt in teens or 20 s (b) Deciduous teeth
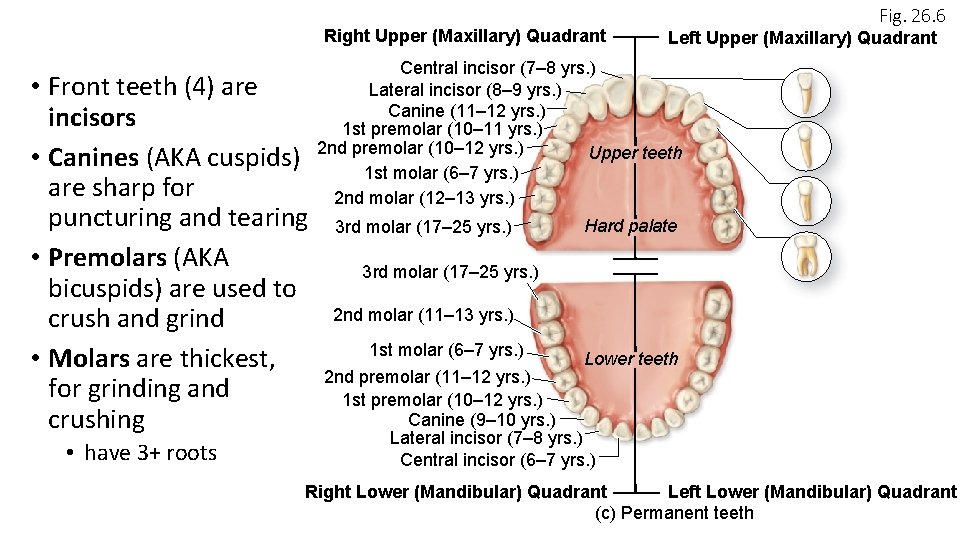
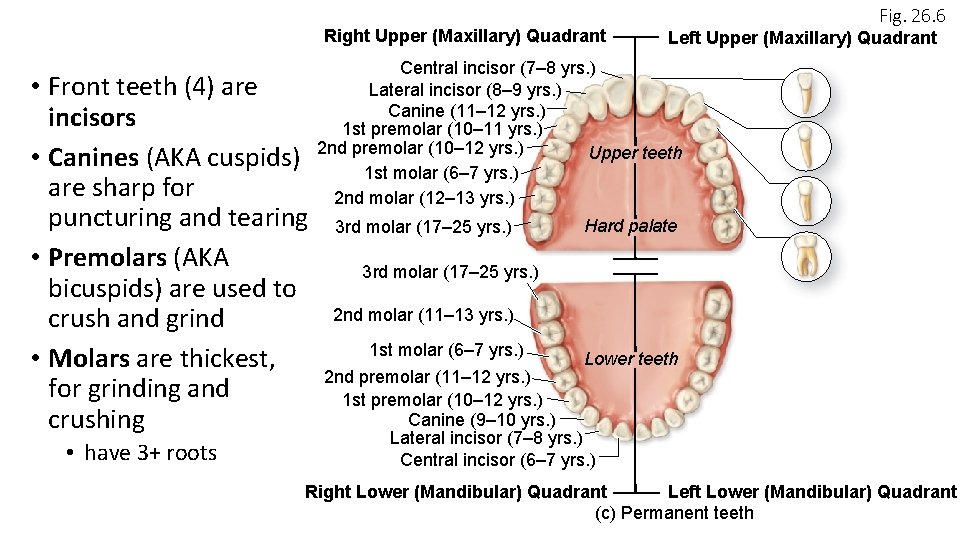
Right Upper (Maxillary) Quadrant • Front teeth (4) are incisors • Canines (AKA cuspids) are sharp for puncturing and tearing • Premolars (AKA bicuspids) are used to crush and grind • Molars are thickest, for grinding and crushing • have 3+ roots Fig. 26. 6 Left Upper (Maxillary) Quadrant Central incisor (7– 8 yrs. ) Lateral incisor (8– 9 yrs. ) Canine (11– 12 yrs. ) 1 st premolar (10– 11 yrs. ) 2 nd premolar (10– 12 yrs. ) Upper teeth 1 st molar (6– 7 yrs. ) 2 nd molar (12– 13 yrs. ) 3 rd molar (17– 25 yrs. ) Hard palate 3 rd molar (17– 25 yrs. ) 2 nd molar (11– 13 yrs. ) 1 st molar (6– 7 yrs. ) Lower teeth 2 nd premolar (11– 12 yrs. ) 1 st premolar (10– 12 yrs. ) Canine (9– 10 yrs. ) Lateral incisor (7– 8 yrs. ) Central incisor (6– 7 yrs. ) Right Lower (Mandibular) Quadrant Left Lower (Mandibular) Quadrant (c) Permanent teeth
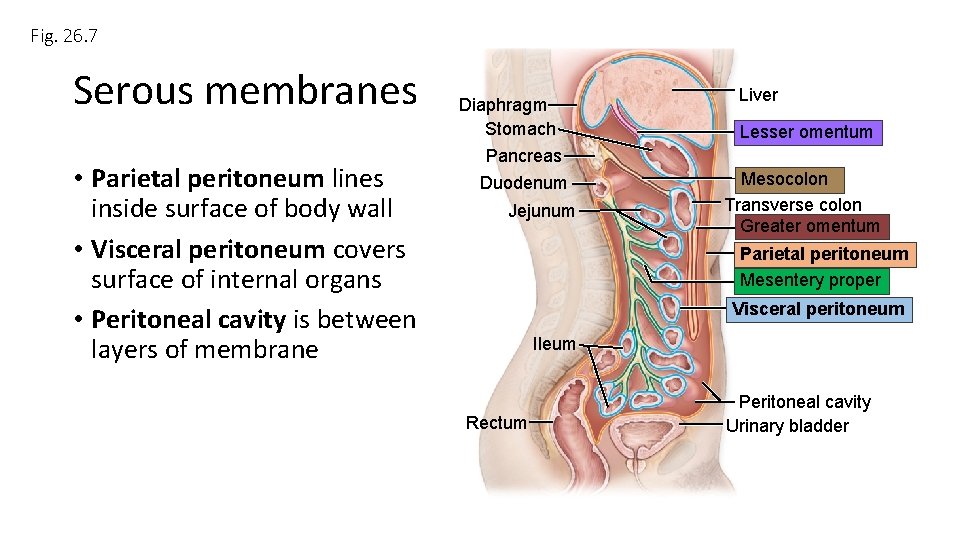
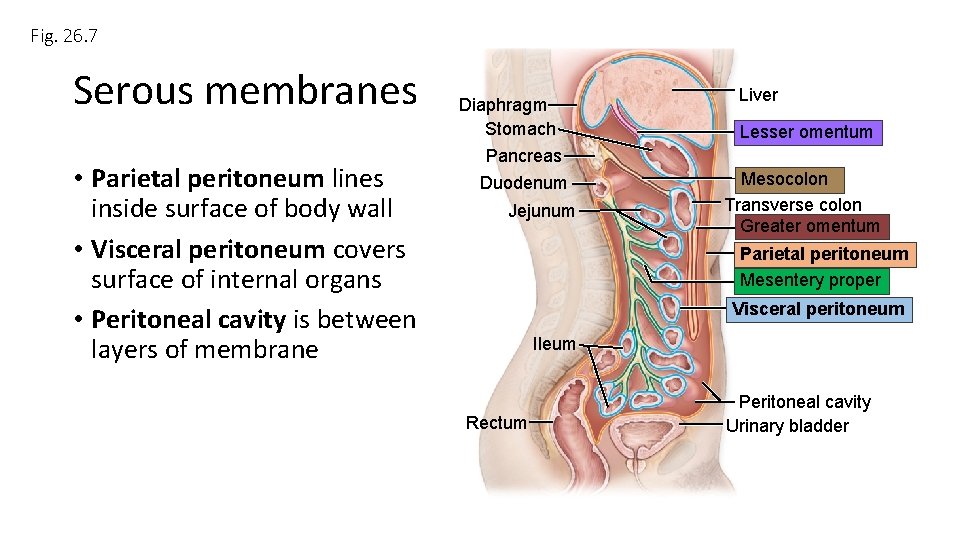
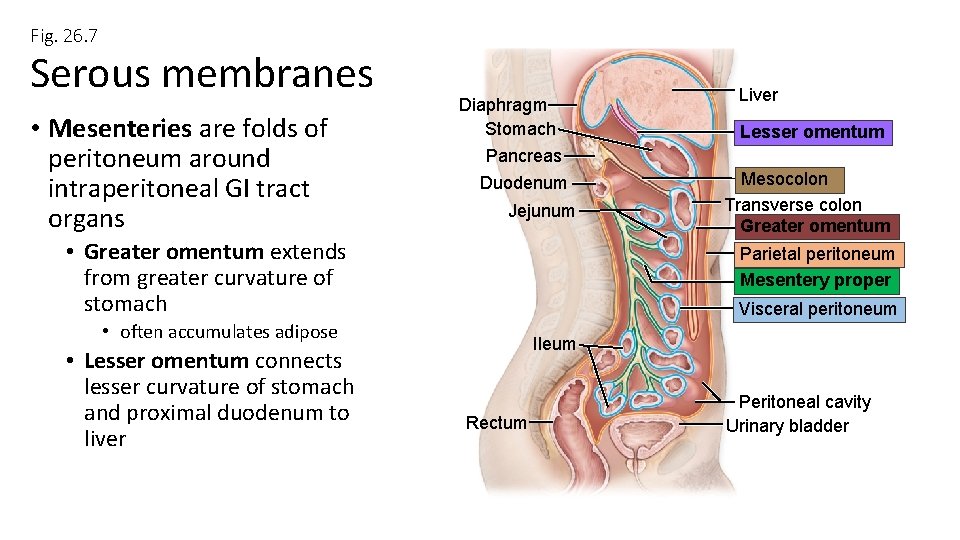
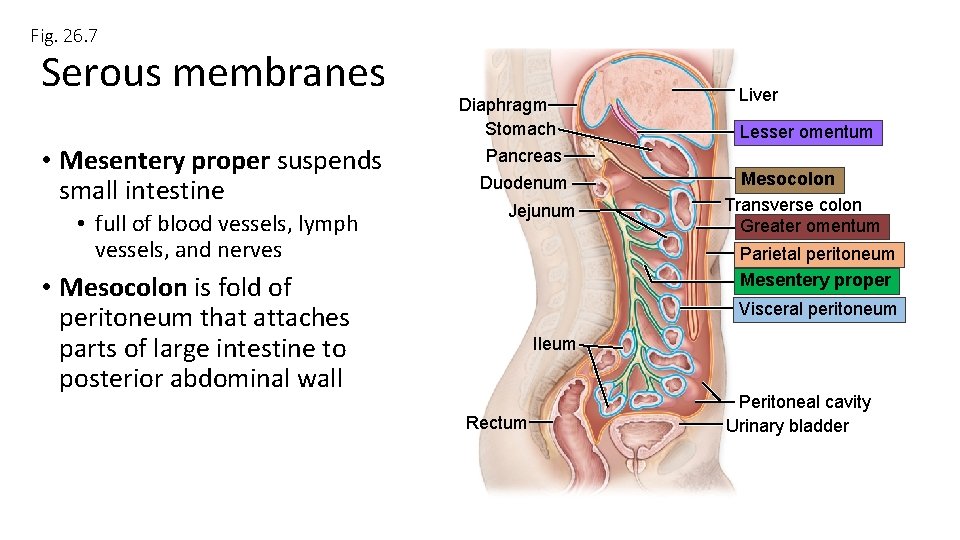
Fig. 26. 7 Serous membranes • Parietal peritoneum lines inside surface of body wall • Visceral peritoneum covers surface of internal organs • Peritoneal cavity is between layers of membrane Diaphragm Stomach Pancreas Duodenum Jejunum Liver Lesser omentum Mesocolon Transverse colon Greater omentum Parietal peritoneum Mesentery proper Visceral peritoneum Ileum Rectum Peritoneal cavity Urinary bladder
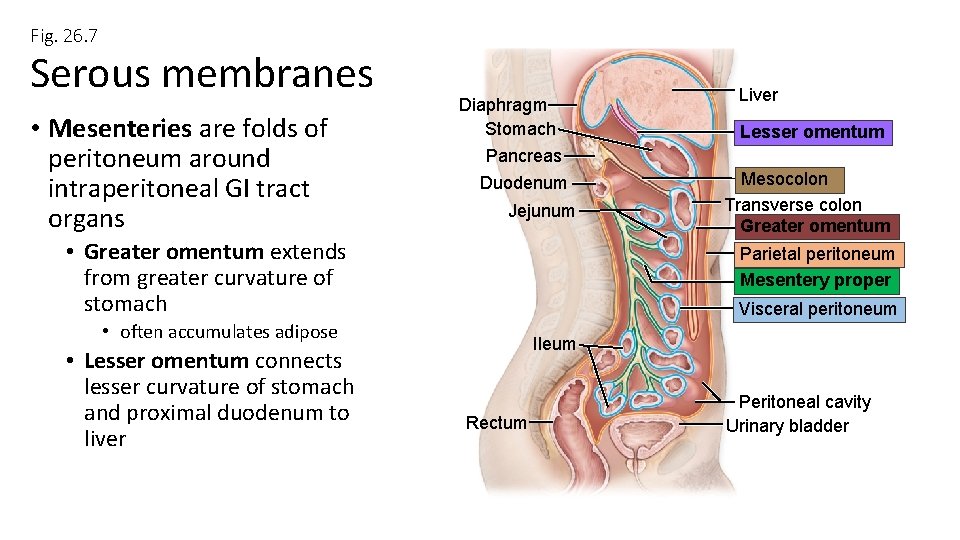
Fig. 26. 7 Serous membranes • Mesenteries are folds of peritoneum around intraperitoneal GI tract organs Diaphragm Stomach Pancreas Duodenum Jejunum • Greater omentum extends from greater curvature of stomach Lesser omentum Mesocolon Transverse colon Greater omentum Parietal peritoneum Mesentery proper Visceral peritoneum • often accumulates adipose • Lesser omentum connects lesser curvature of stomach and proximal duodenum to liver Liver Ileum Rectum Peritoneal cavity Urinary bladder
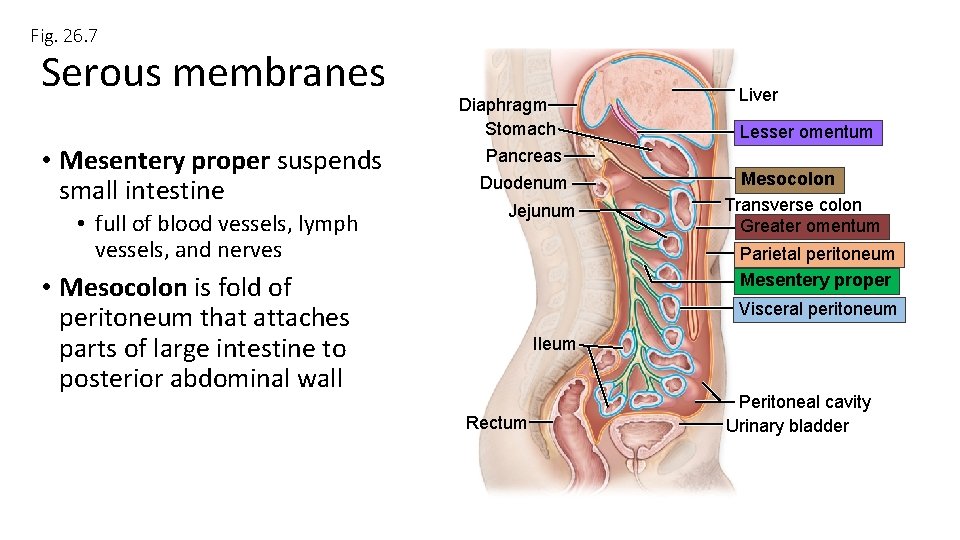
Fig. 26. 7 Serous membranes • Mesentery proper suspends small intestine • full of blood vessels, lymph vessels, and nerves Diaphragm Stomach Pancreas Duodenum Jejunum Liver Lesser omentum Mesocolon Transverse colon Greater omentum Parietal peritoneum Mesentery proper • Mesocolon is fold of peritoneum that attaches parts of large intestine to posterior abdominal wall Visceral peritoneum Ileum Rectum Peritoneal cavity Urinary bladder
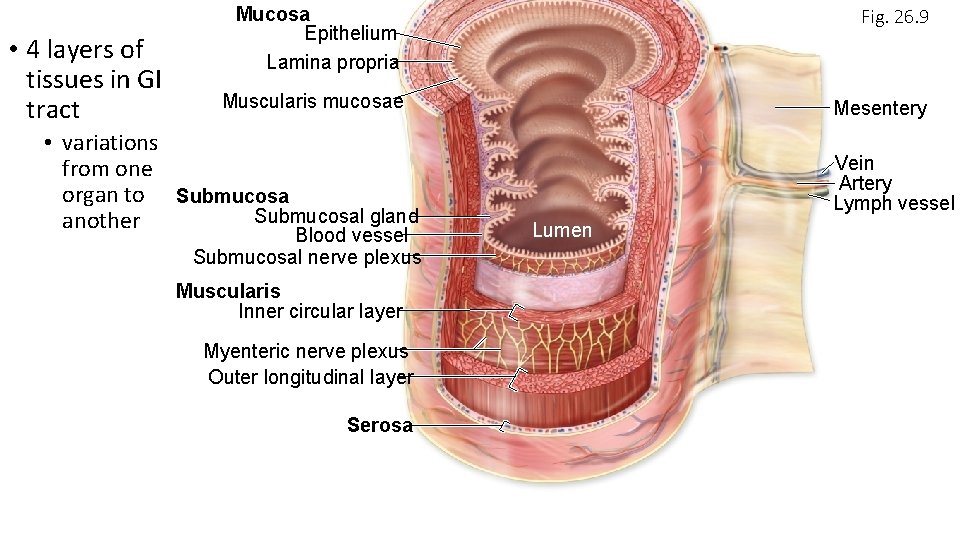
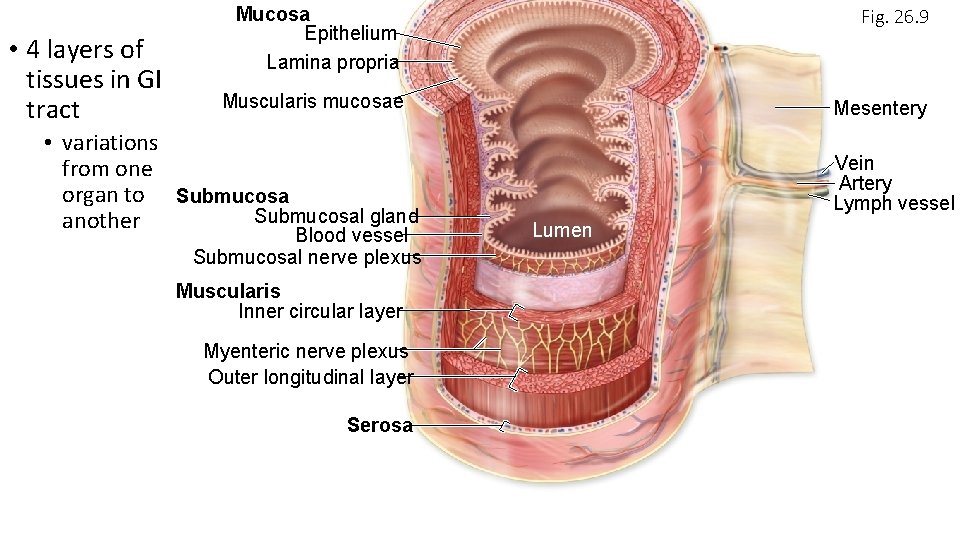
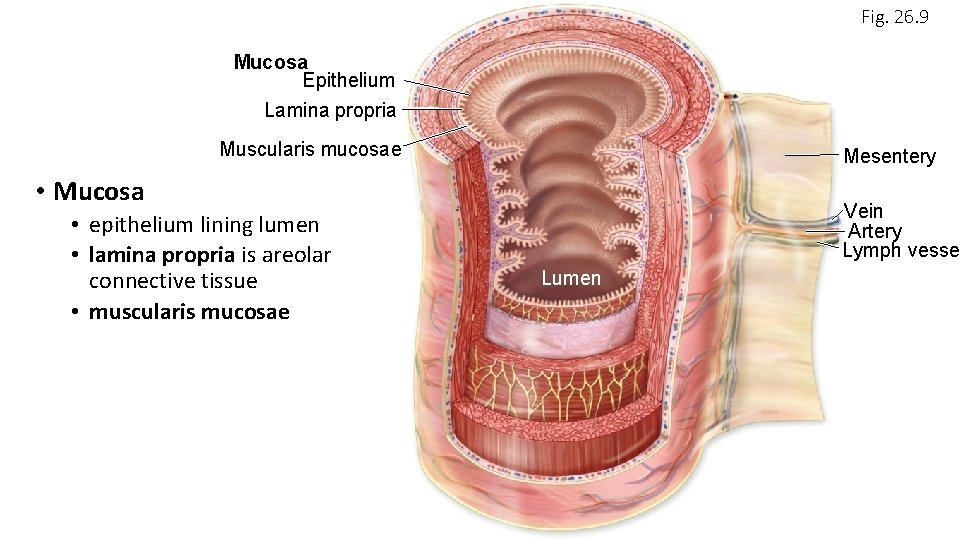
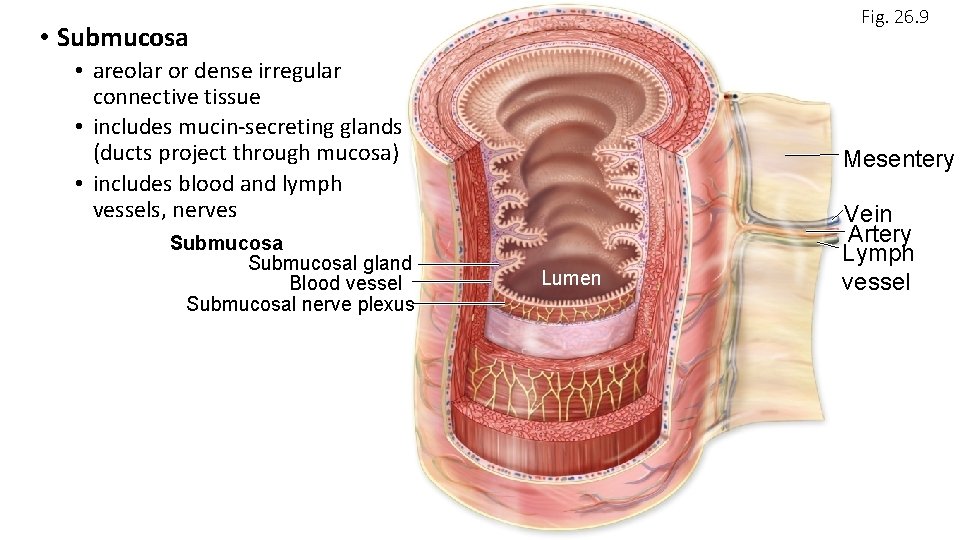
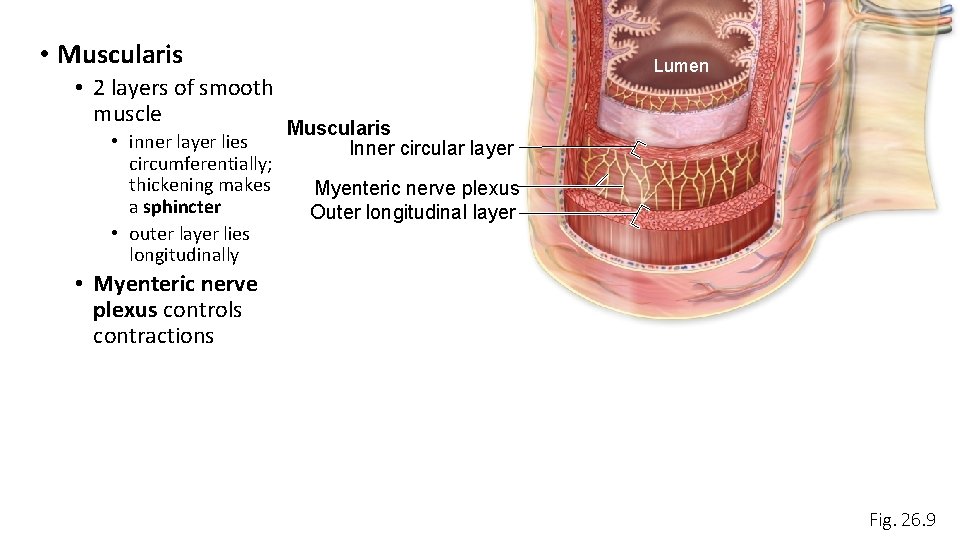
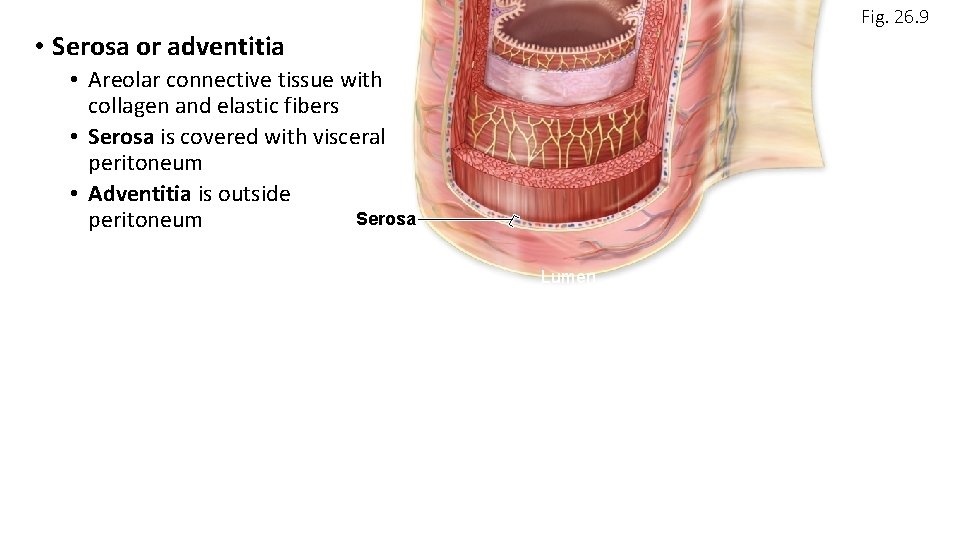
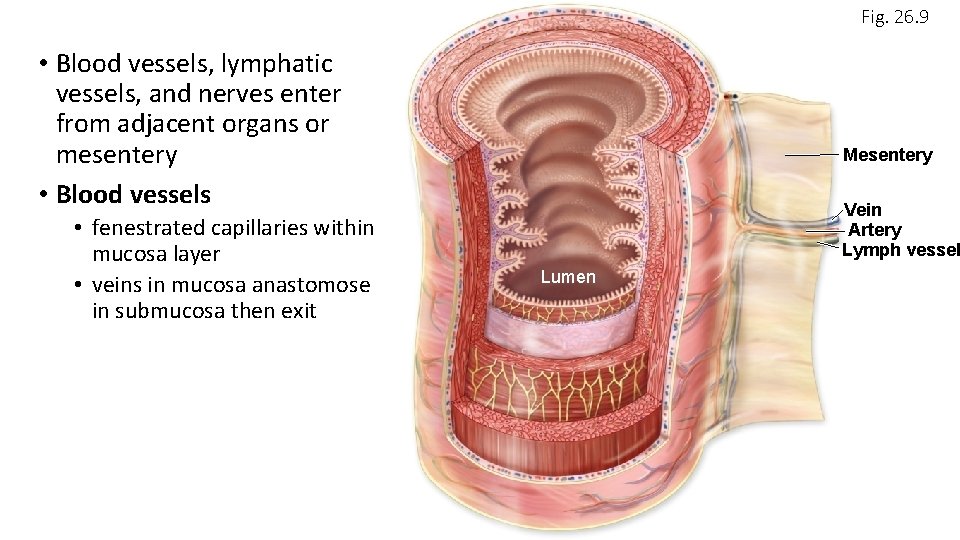
• 4 layers of tissues in GI tract Mucosa Epithelium Lamina propria Fig. 26. 9 Muscularis mucosae Mesentery • variations from one organ to Submucosal gland another Blood vessel Submucosal nerve plexus Muscularis Inner circular layer Myenteric nerve plexus Outer longitudinal layer Serosa Vein Artery Lymph vessel Lumen
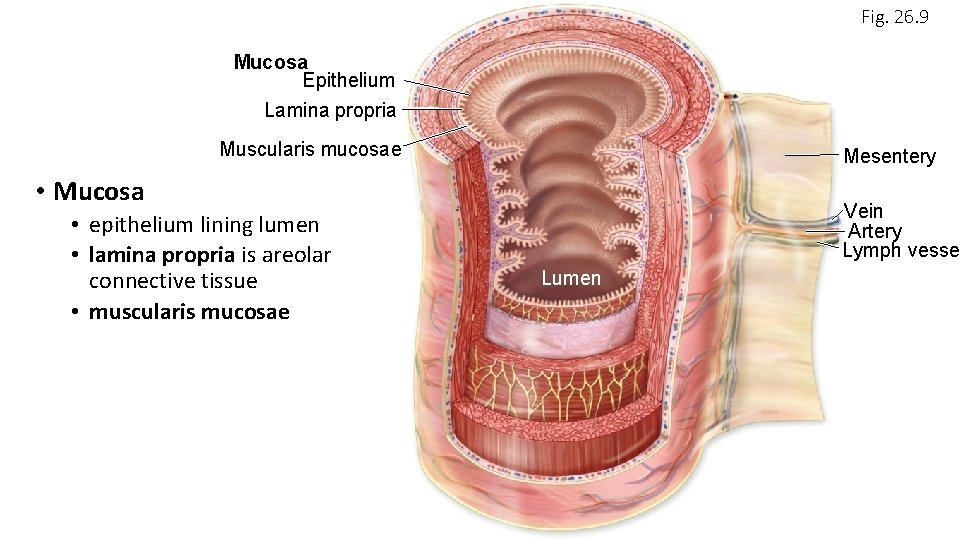
Fig. 26. 9 Mucosa Epithelium Lamina propria Muscularis mucosae Mesentery • Mucosa • epithelium lining lumen • lamina propria is areolar connective tissue • muscularis mucosae Vein Artery Lymph vesse Lumen
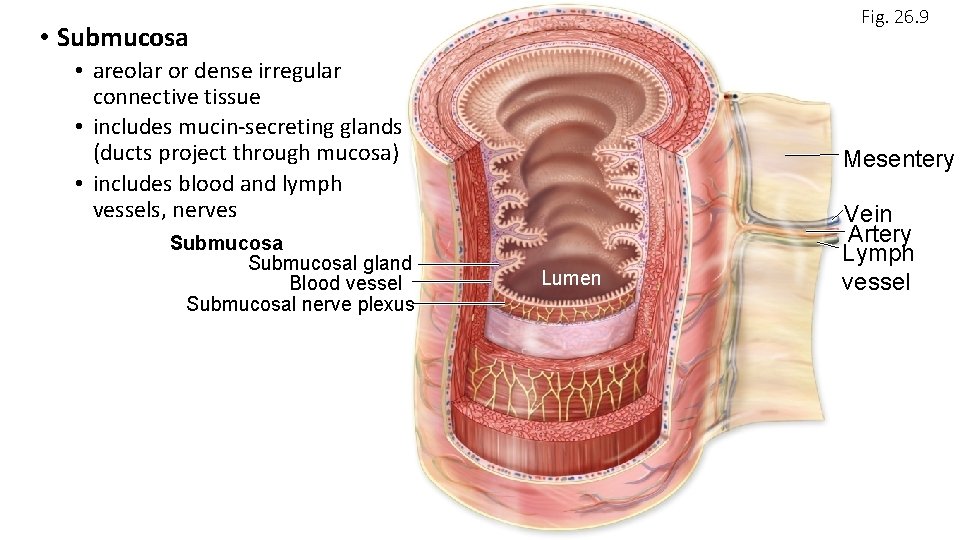
Fig. 26. 9 • Submucosa • areolar or dense irregular connective tissue • includes mucin-secreting glands (ducts project through mucosa) • includes blood and lymph vessels, nerves Submucosal gland Blood vessel Submucosal nerve plexus Mesentery Lumen Vein Artery Lymph vessel
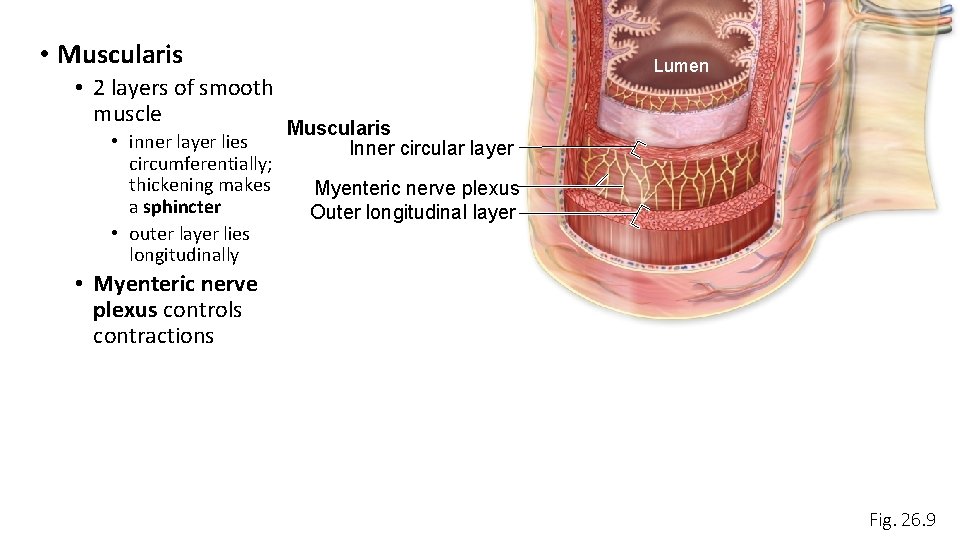
• Muscularis • 2 layers of smooth muscle • inner layer lies circumferentially; thickening makes a sphincter • outer layer lies longitudinally Lumen Muscularis Inner circular layer Myenteric nerve plexus Outer longitudinal layer • Myenteric nerve plexus controls contractions Fig. 26. 9
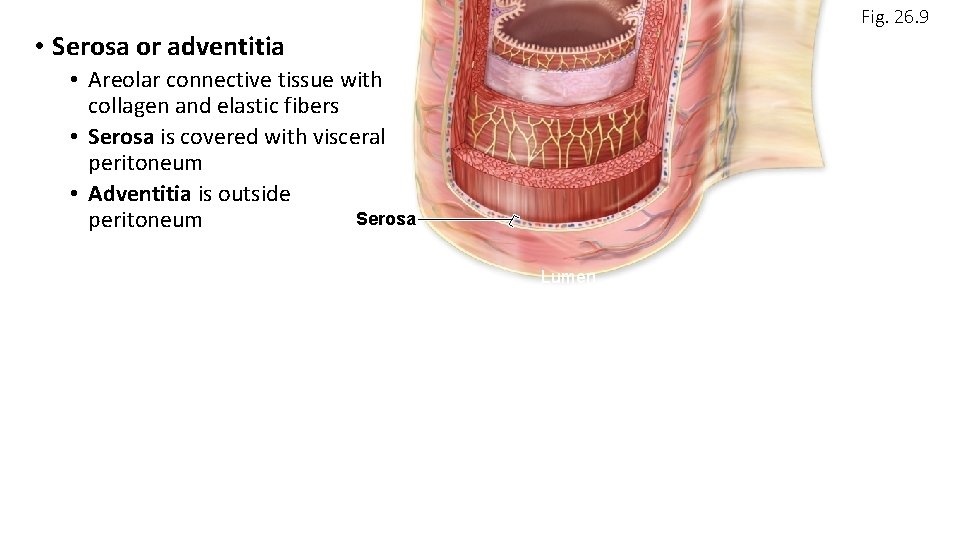
Fig. 26. 9 • Serosa or adventitia • Areolar connective tissue with collagen and elastic fibers • Serosa is covered with visceral peritoneum • Adventitia is outside Serosa peritoneum Lumen
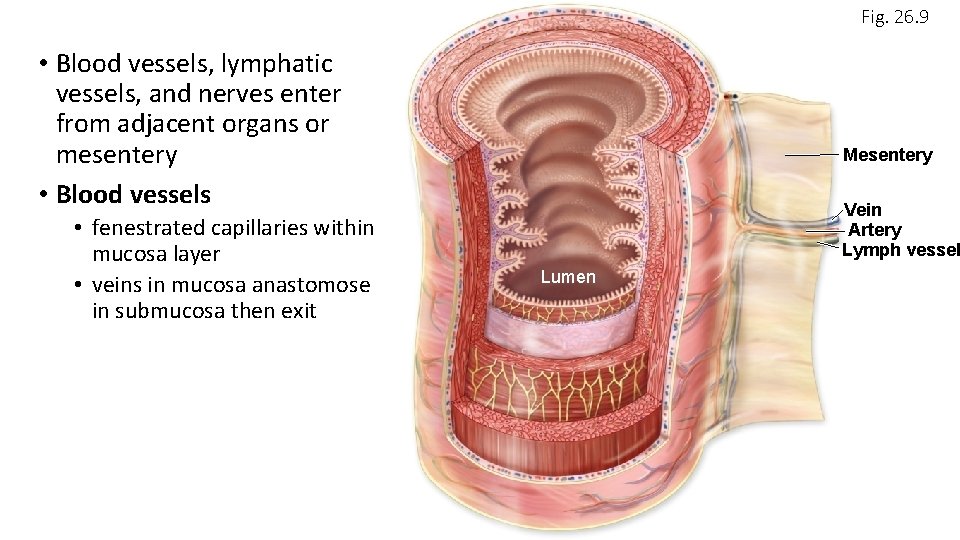
Fig. 26. 9 • Blood vessels, lymphatic vessels, and nerves enter from adjacent organs or mesentery • Blood vessels • fenestrated capillaries within mucosa layer • veins in mucosa anastomose in submucosa then exit Mesentery Vein Artery Lymph vessel Lumen
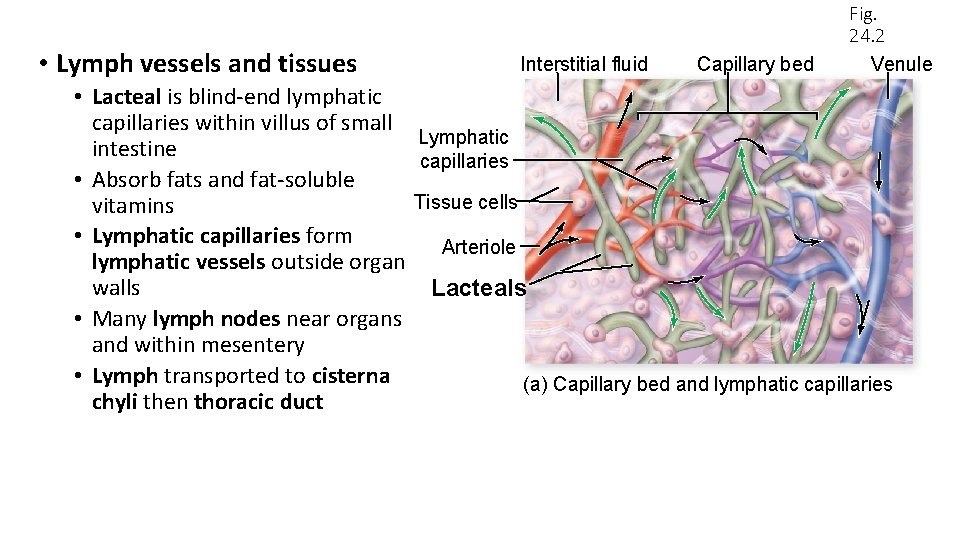
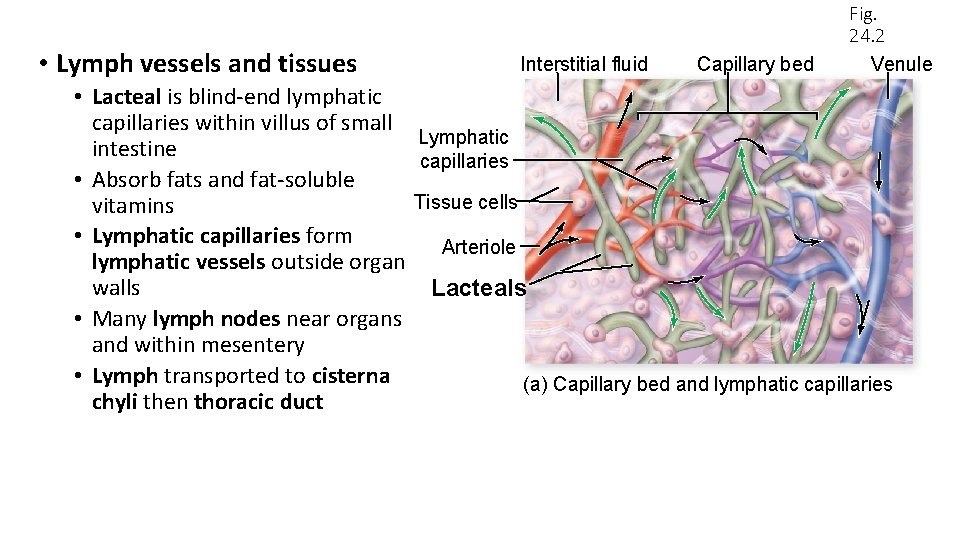
• Lymph vessels and tissues Interstitial fluid Capillary bed Fig. 24. 2 Venule • Lacteal is blind-end lymphatic capillaries within villus of small Lymphatic intestine capillaries • Absorb fats and fat-soluble Tissue cells vitamins • Lymphatic capillaries form Arteriole lymphatic vessels outside organ walls Lacteals • Many lymph nodes near organs and within mesentery • Lymph transported to cisterna (a) Capillary bed and lymphatic capillaries chyli then thoracic duct
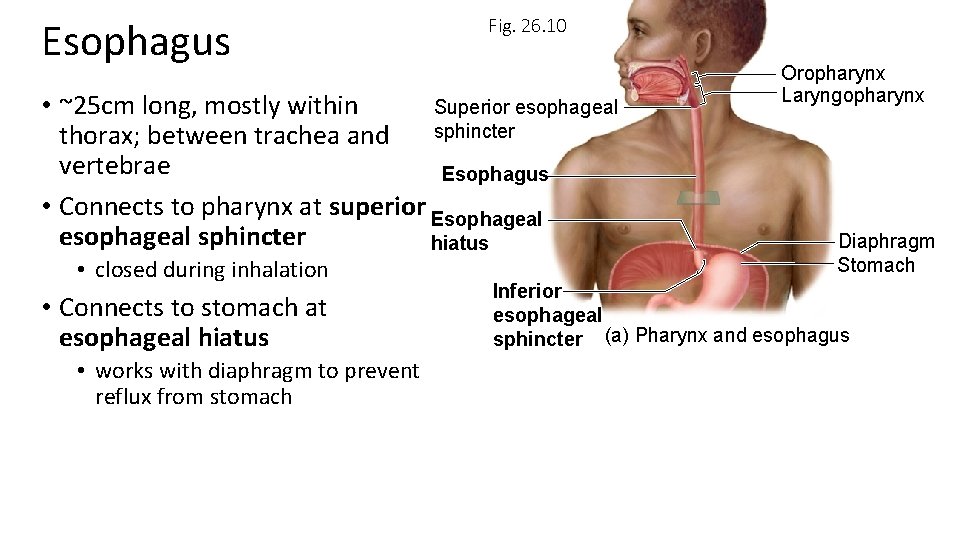
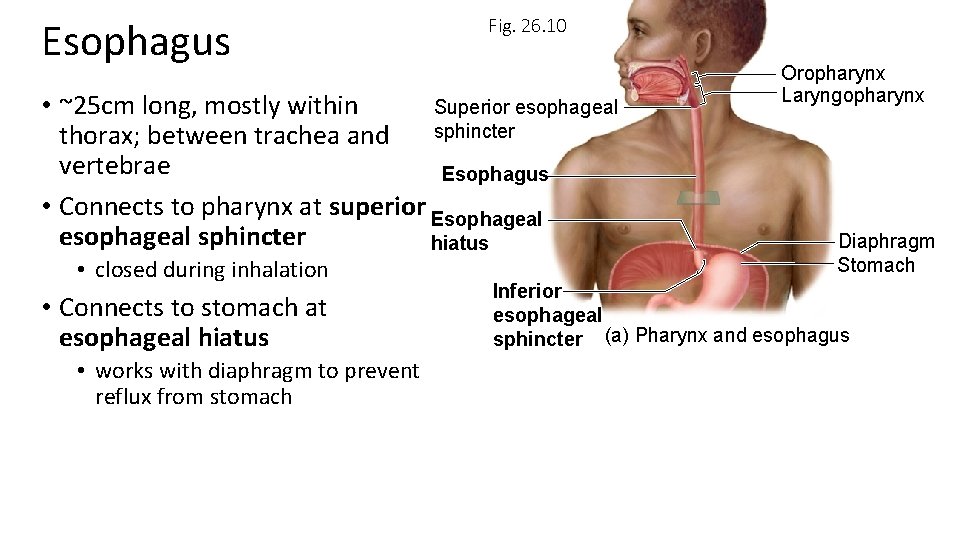
Esophagus Fig. 26. 10 • ~25 cm long, mostly within Superior esophageal sphincter thorax; between trachea and vertebrae Esophagus • Connects to pharynx at superior Esophageal esophageal sphincter hiatus • closed during inhalation • Connects to stomach at esophageal hiatus • works with diaphragm to prevent reflux from stomach Oropharynx Laryngopharynx Diaphragm Stomach Inferior esophageal sphincter (a) Pharynx and esophagus
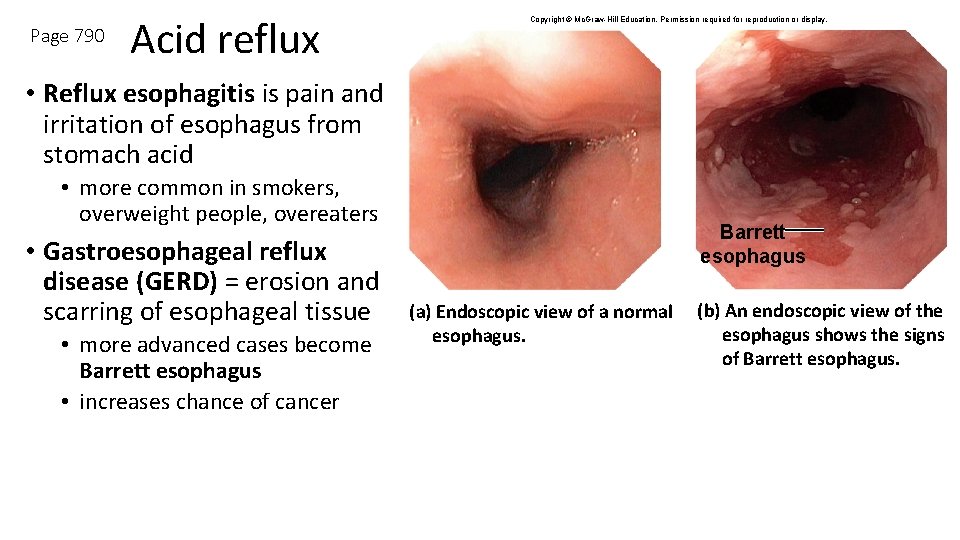
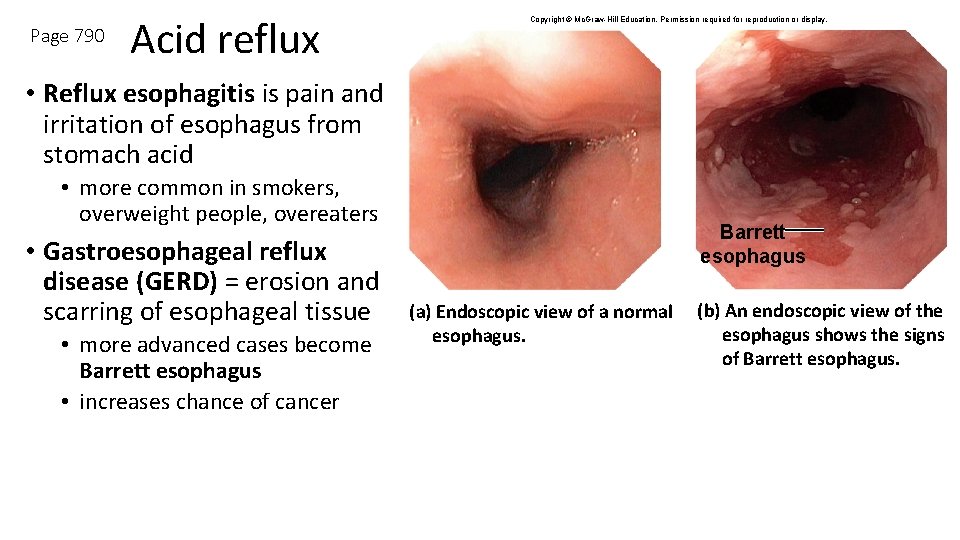
Page 790 Acid reflux Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display. • Reflux esophagitis is pain and irritation of esophagus from stomach acid • more common in smokers, overweight people, overeaters • Gastroesophageal reflux disease (GERD) = erosion and scarring of esophageal tissue • more advanced cases become Barrett esophagus • increases chance of cancer Barrett esophagus (a) Endoscopic view of a normal esophagus. (b) An endoscopic view of the esophagus shows the signs of Barrett esophagus.
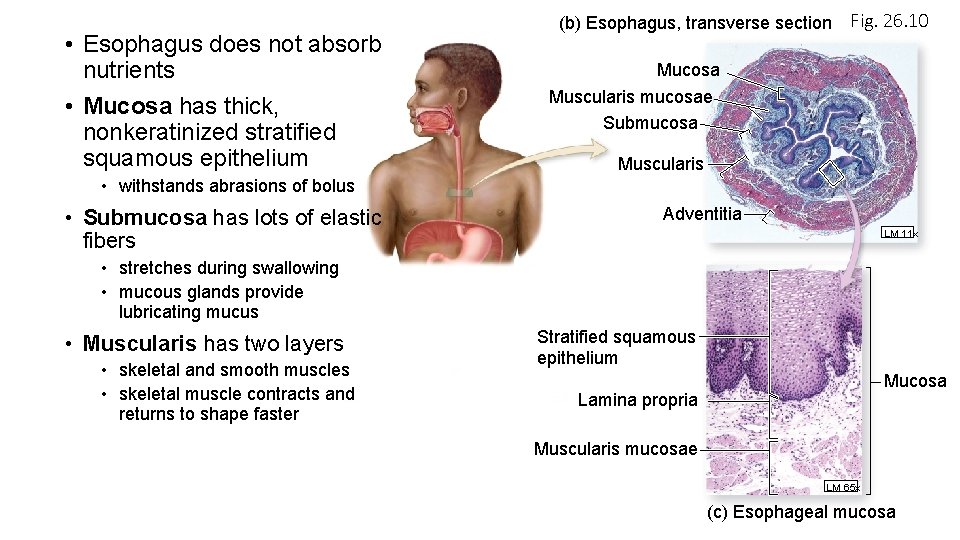
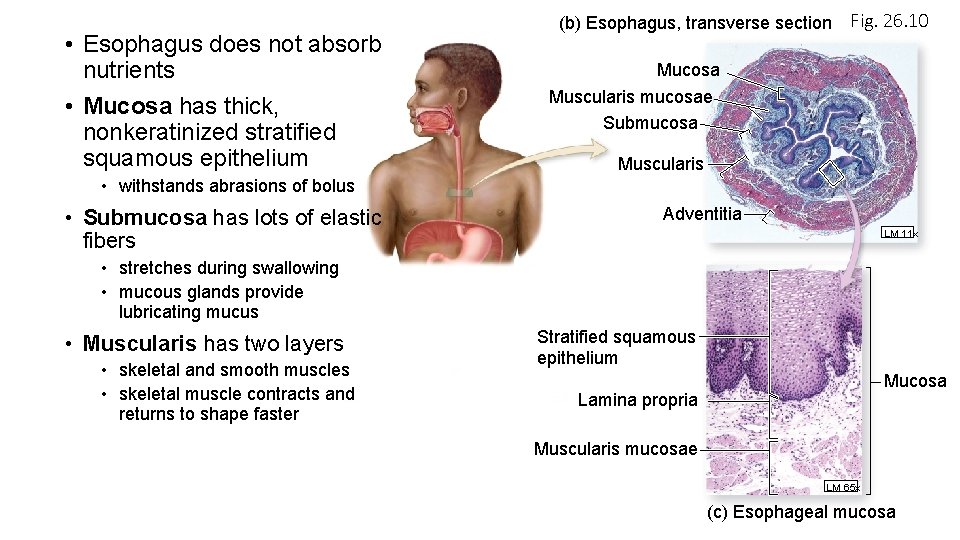
• Esophagus does not absorb nutrients • Mucosa has thick, nonkeratinized stratified squamous epithelium (b) Esophagus, transverse section Fig. 26. 10 Mucosa Muscularis mucosae Submucosa Muscularis • withstands abrasions of bolus • Submucosa has lots of elastic fibers Adventitia LM 11 x • stretches during swallowing • mucous glands provide lubricating mucus • Muscularis has two layers • skeletal and smooth muscles • skeletal muscle contracts and returns to shape faster Stratified squamous epithelium Mucosa Lamina propria Muscularis mucosae LM 65 x (c) Esophageal mucosa