Chapter 24 Structure and Function of the Kidney
- Slides: 32
Chapter 24 Structure and Function of the Kidney Copyright © 2015 Wolters Kluwer Health | Lippincott Williams & Wilkins
Kidney Functions • Filter the blood • Remove water-soluble wastes • Help control blood pressure • Help maintain red blood cell levels • Convert vitamin D Copyright © 2015 Wolters Kluwer • All Rights Reserved
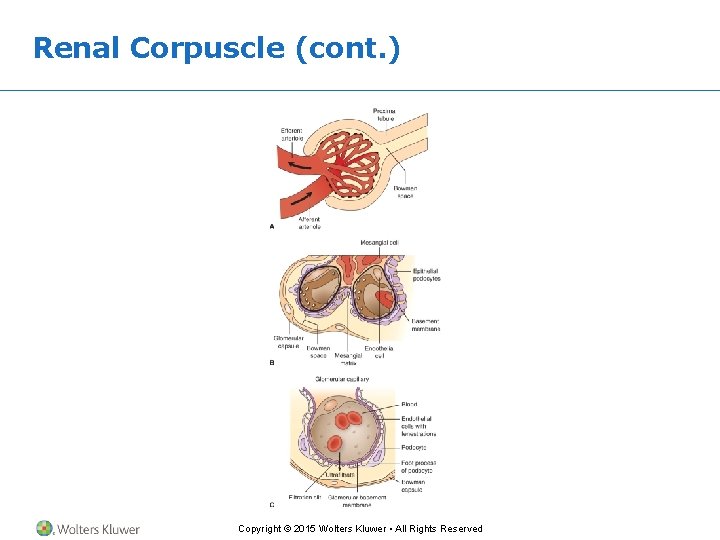
Renal Corpuscle • Glomerular capillary cells sit along a basement membrane. • Bowman capsule epithelium cells sit along the same basement membrane. • They stand up away from the membrane on pseudopods. • Fluid filters across the basement membrane and between the pseudopods. Copyright © 2015 Wolters Kluwer • All Rights Reserved
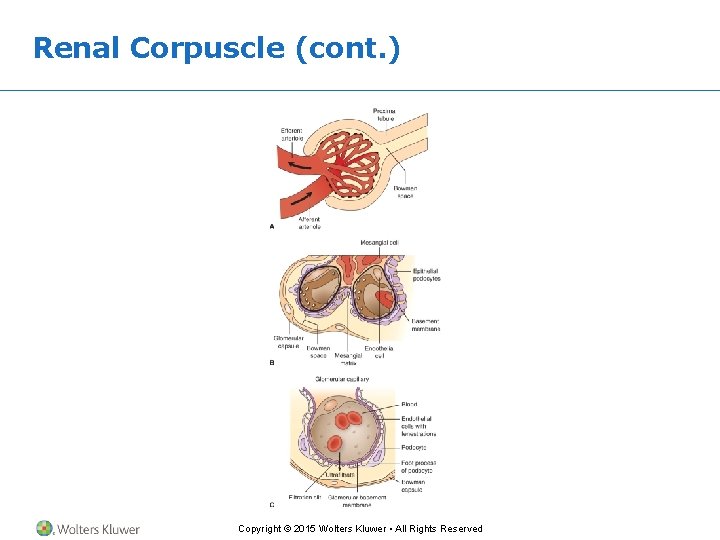
Renal Corpuscle (cont. ) Copyright © 2015 Wolters Kluwer • All Rights Reserved
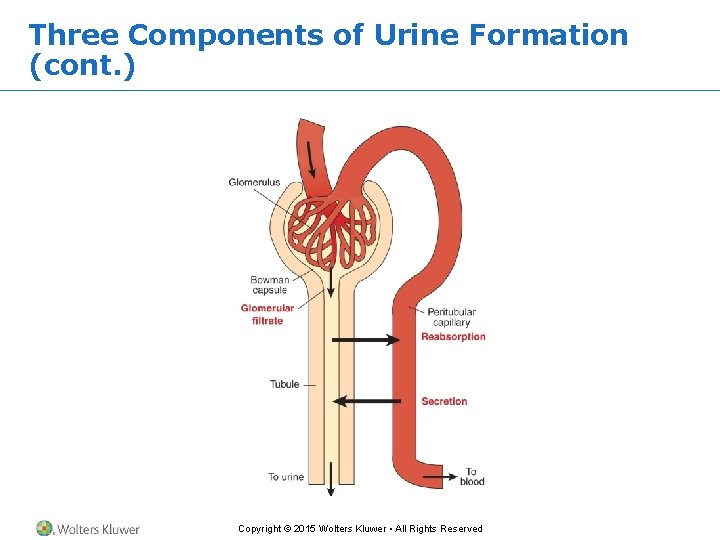
Three Components of Urine Formation • Filtration • Reabsorption • Secretion Copyright © 2015 Wolters Kluwer • All Rights Reserved
Glomerular Filtration Rate • Glomerular filtration rate = 125 m. L/minute Discussion: • How would it change if your – Efferent arterioles are constricted? – Afferent arterioles are constricted? – Blood pressure is decreased? • Which of the following will increase GFR? - Epinephrine - Prostaglandins - NO Copyright © 2015 Wolters Kluwer • All Rights Reserved - Endothelin
Question • True or false? • If GFR increases, urine output (UO) will decrease. Copyright © 2015 Wolters Kluwer • All Rights Reserved
Answer • False • Rationale: If GFR increases, it means that fluid is moving more quickly across the basement membrane/through the pseudopods. This means that more fluid will become filtrate and less fluid will be reabsorbed into the blood. If less fluid is reabsorbed, more fluid is left to be excreted (increasing UO). Copyright © 2015 Wolters Kluwer • All Rights Reserved
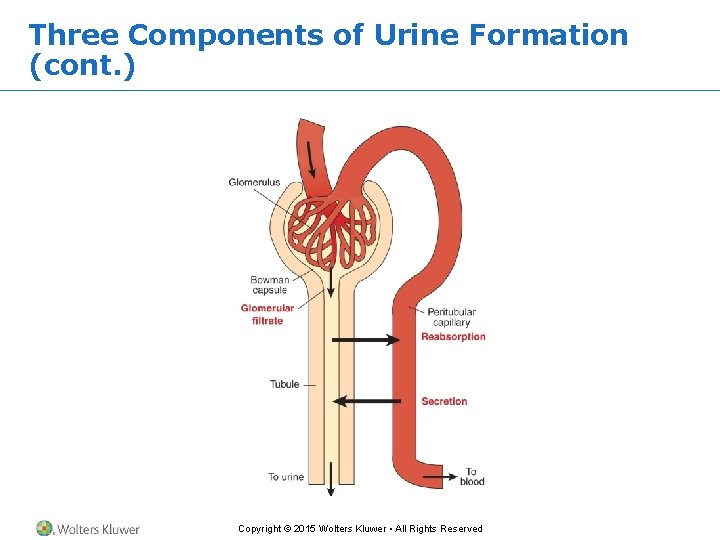
Three Components of Urine Formation (cont. ) Copyright © 2015 Wolters Kluwer • All Rights Reserved
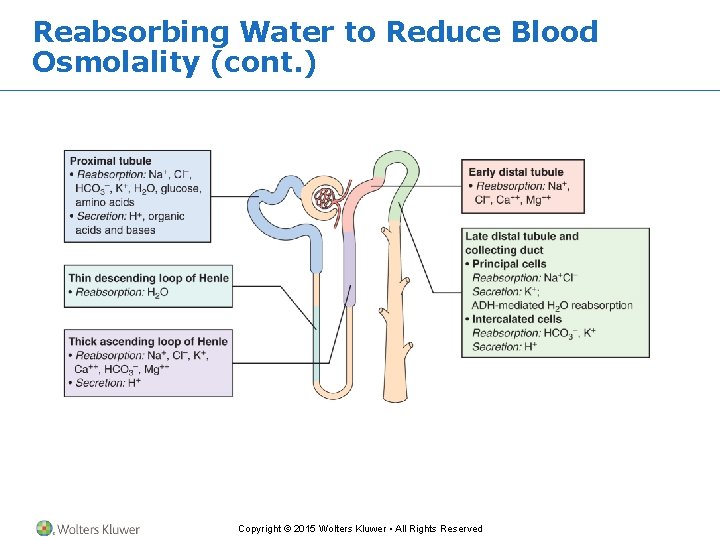
Reabsorbing Water to Reduce Blood Osmolality • This happens in the inner layer of the kidney, the medulla. • The loop of Henle contains ion pumps. Copyright © 2015 Wolters Kluwer • All Rights Reserved
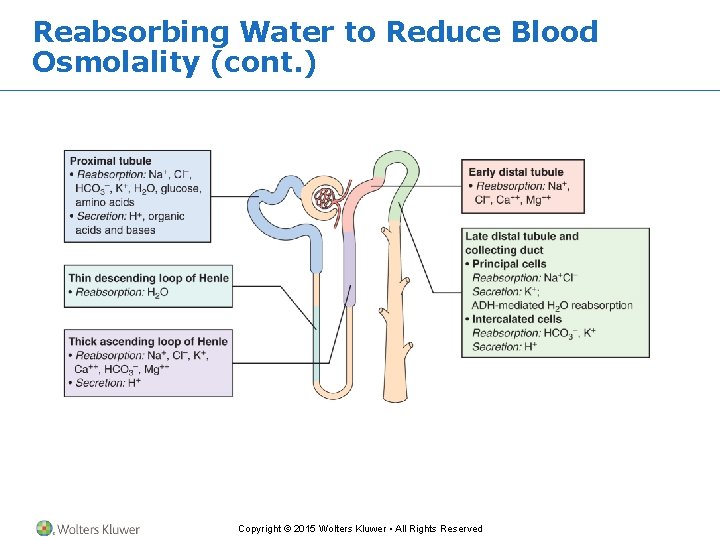
Reabsorbing Water to Reduce Blood Osmolality (cont. ) Copyright © 2015 Wolters Kluwer • All Rights Reserved
Reabsorbing Water to Reduce Blood Osmolality (cont. ) • The Na. Cl pumped into the medulla makes it salty. • It is hypertonic to the urine in the collecting duct. • Water moves from the collecting duct into the salty medulla and enters the blood. Copyright © 2015 Wolters Kluwer • All Rights Reserved
Question • Which renal structure reabsorbs water? A. Proximal loop B. Distal loop C. Collecting duct D. Glomerulus Copyright © 2015 Wolters Kluwer • All Rights Reserved
Answer • C. Collecting duct • Rationale: Reabsorption of water occurs in the medulla (the inner layer of the kidney). Na+Cl− leaves the loop of Henle, which makes it hypertonic to the urine in the collecting duct. Water moves from the collecting duct into the blood (reabsorption). Copyright © 2015 Wolters Kluwer • All Rights Reserved
Amount of Water Absorbed • Depends on how much can move out of the collecting duct. • Antidiuretic hormone makes the duct permeable to water. Copyright © 2015 Wolters Kluwer • All Rights Reserved
Antidiuretic Hormone (ADH) • Makes the collecting duct more permeable to water. • More water can be reabsorbed from the urine into the blood. • Blood osmolarity decreases. Copyright © 2015 Wolters Kluwer • All Rights Reserved
Question • True or false? • Increased ADH decreases urine output (UO). Copyright © 2015 Wolters Kluwer • All Rights Reserved
Answer • True • Rationale: ADH makes the collecting duct more permeable to water, so that more water can leave the duct and be reabsorbed into the blood. More reabsorption means that there is less fluid to be excreted (↓ UO). Copyright © 2015 Wolters Kluwer • All Rights Reserved
When Urine Reaches Distal Tubule • Juxtaglomerular cells measure blood flow in the afferent arteriole and urine flow and composition. • They can release renin, which turns on the Na+/K+ ATPase in the distal tubule. • Na+ and water are reabsorbed. • K+ is secreted. Copyright © 2015 Wolters Kluwer • All Rights Reserved
Renin-Angiotensin-Aldosterone Pathway • Na+ and water are reabsorbed. – Raises blood volume – Does not change blood osmolarity • K+ is secreted. – Lowers blood K+ Copyright © 2015 Wolters Kluwer • All Rights Reserved
Discussion • Which changes in these variables would increase renin secretion? – Increased blood volume – Decreased blood volume – Increased blood pressure – Decreased blood pressure Copyright © 2015 Wolters Kluwer • All Rights Reserved
Scenario • A man was given a drug that stopped the ion pumps in the loop of Henle. Questions: • What happened to – Medulla osmolarity? – Na+ levels in the distal convoluted tubule? – Amount of water reabsorbed? – Renin levels? – Blood K+? Copyright © 2015 Wolters Kluwer • All Rights Reserved
Removing Na. Cl and Water from Your Blood • Atrial natriuretic peptide – Made by overstretched atria • Causes the kidneys to stop reabsorbing Na. Cl. • The Na. Cl and water are lost in the urine, reducing blood volume and decreasing the stretch and workload of the heart. Copyright © 2015 Wolters Kluwer • All Rights Reserved
Discussion • What will happen to urine if: – Aldosterone is given? – ADH levels are high? Copyright © 2015 Wolters Kluwer • All Rights Reserved
Discussion • A man has severe renal disease. Questions: • Why does he develop: – Anemia? – Weak bones? Copyright © 2015 Wolters Kluwer • All Rights Reserved
Question • What hormone secreted by the kidneys stimulates RBC formation in the bone marrow? A. Renin B. Erythropoietin C. Aldosterone D. Angiotensin Copyright © 2015 Wolters Kluwer • All Rights Reserved
Answer • B. Erythropoietin • Rationale: Erythropoietin literally means “producing erythrocytes/RBCs. ” Decreased levels of this hormone lead to anemia; increased levels lead to polycythemia. Copyright © 2015 Wolters Kluwer • All Rights Reserved
Kidney Functions • The kidneys clear wastes out of the blood. • Renal clearance is a measurement of how much blood the kidneys clean in a minute – If the blood contains 1 mg waste/100 m. L blood – If the person produces 1 m. L urine per minute – And if the urine contains 1 mg waste/m. L Question: • How much blood did the kidney clean in 1 minute? Copyright © 2015 Wolters Kluwer • All Rights Reserved
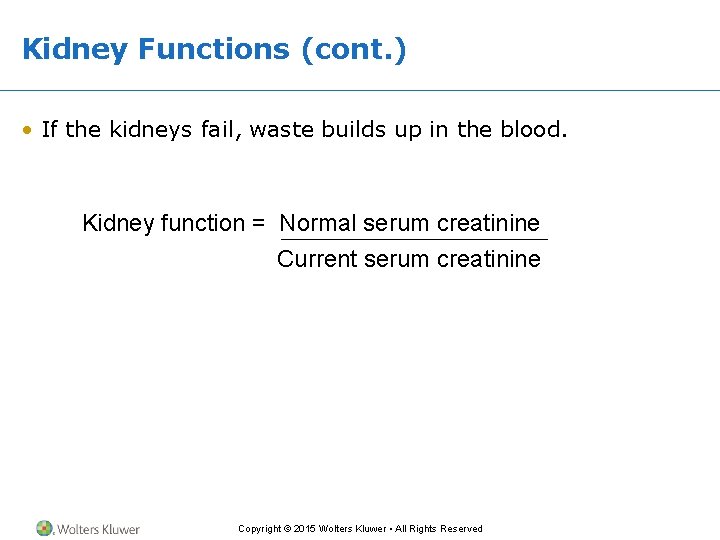
Kidney Functions (cont. ) • If the kidneys fail, waste builds up in the blood. • What is the percent of kidney function when serum creatinine is: − 2 mg/d. L? − 3 mg/d. L? − 10 mg/d. L? Copyright © 2015 Wolters Kluwer • All Rights Reserved
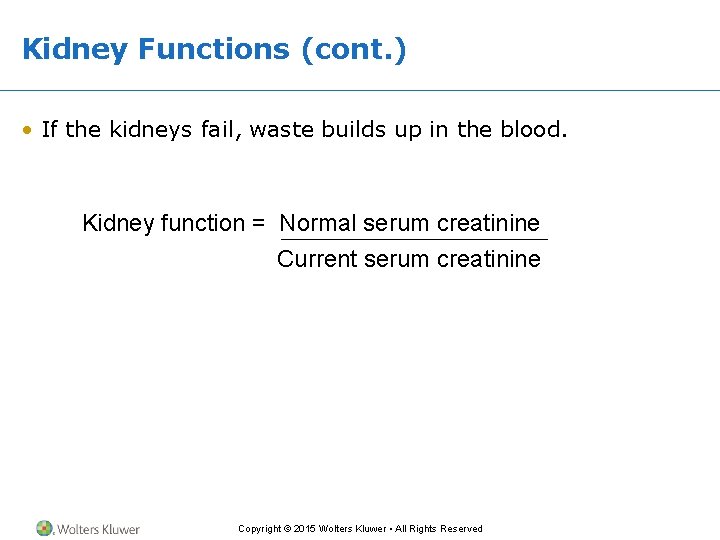
Kidney Functions (cont. ) • If the kidneys fail, waste builds up in the blood. Kidney function = Normal serum creatinine Current serum creatinine Copyright © 2015 Wolters Kluwer • All Rights Reserved
Discussion • What would each of these test results indicate? – Severe proteinuria – Casts with red blood cells in them – Low specific gravity – Serum creatinine = 6 mg/d. L – BUN = 35 mg/d. L; serum creatinine = 1. 2 mg/d. L Copyright © 2015 Wolters Kluwer • All Rights Reserved
If 125 m. L of Ultrafiltrate Is Formed Each Minute, How Much Is Formed in a Day? • Actual urine excretion is 1. 5 L a day. • Proximal convoluted tubule reabsorbs about 60% of nutrients and ions in the urine. – Absorbs at an automatic rate. – The amount of a solute it can reabsorb is the transport maximum. – Nutrients not reabsorbed pass out in the urine. • Water follows the solutes back into the blood. Copyright © 2015 Wolters Kluwer • All Rights Reserved