chapter 24 Hip Hip A common site for
- Slides: 87
chapter 24 Hip
Hip • A common site for pain referral – – – Lumbar disc Organ disease Myofascial pain SI dysfunction Knee Reassess if no change after 2 weeks of treatment • Force transmitter for upper and lower extremities • Stability for upper- and lower-extremity activities • experiences repetitive, microtraumatic injuries more often than acute, macrotraumatic injuries
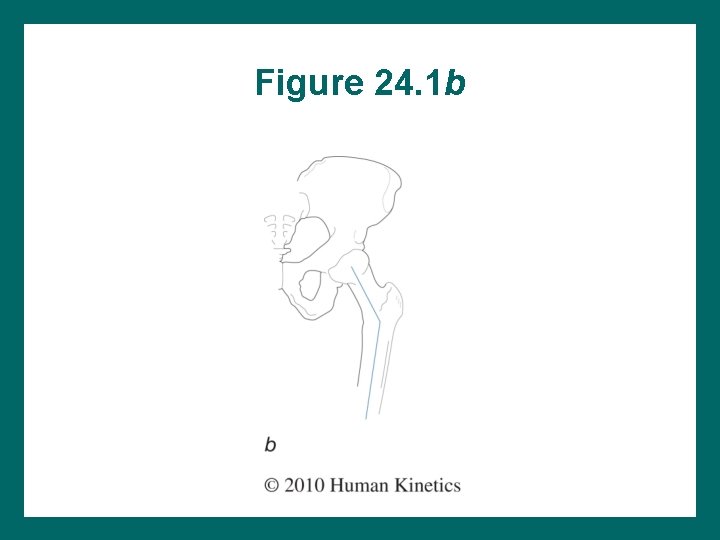
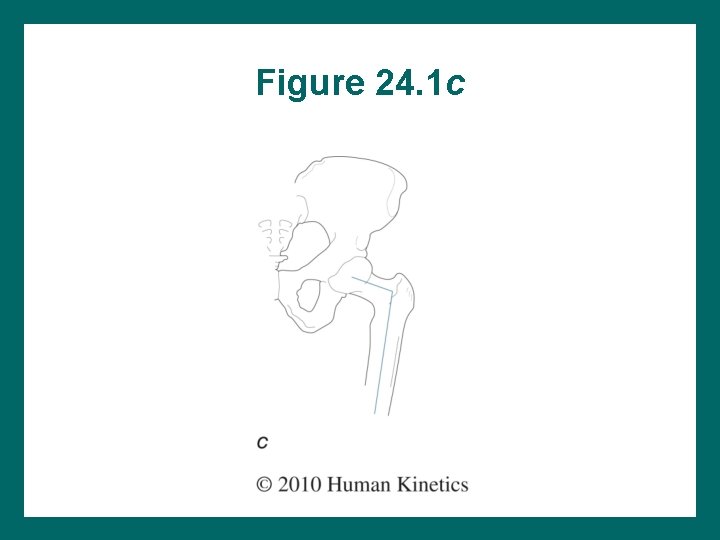
Hip Alignment Coxa valga (see figure 24. 1 b) – – Angle between neck and shaft = >125° Femoral head load, femoral neck stress Lengthens the limb Hip abductor effectiveness Coxa vara (see figure 24. 1 c) – – Angle between neck and shaft = <125° Femoral neck stress, femoral head load Shortens the limb Hip abductor effectiveness
Figure 24. 1 b
Figure 24. 1 c
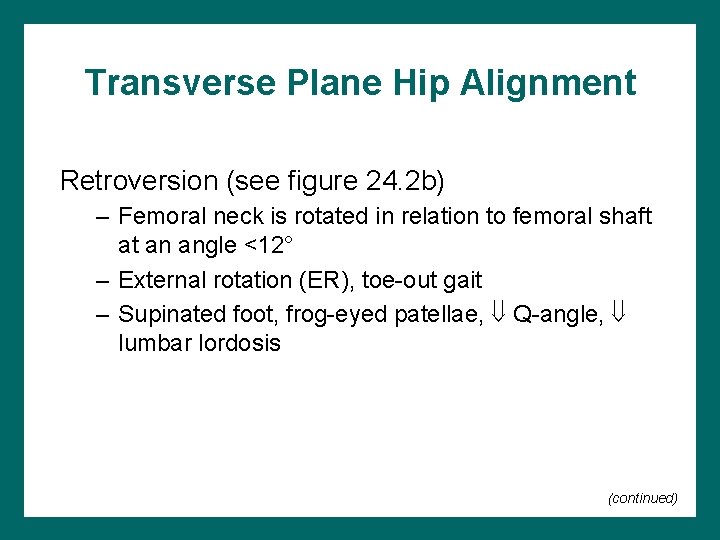
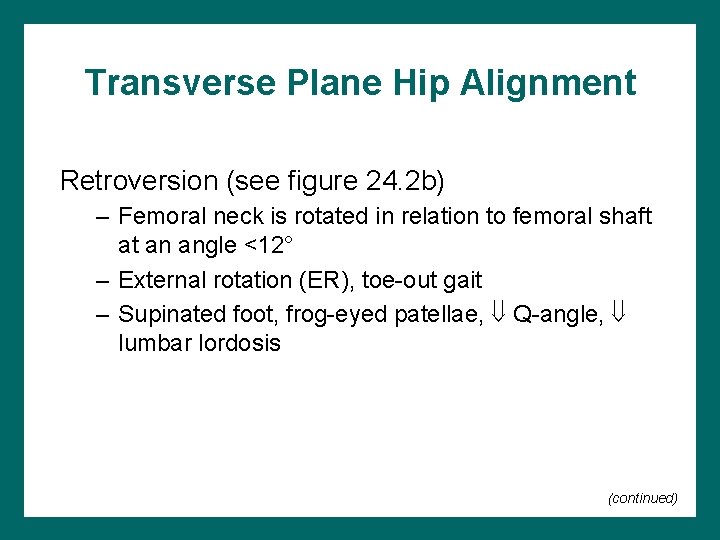
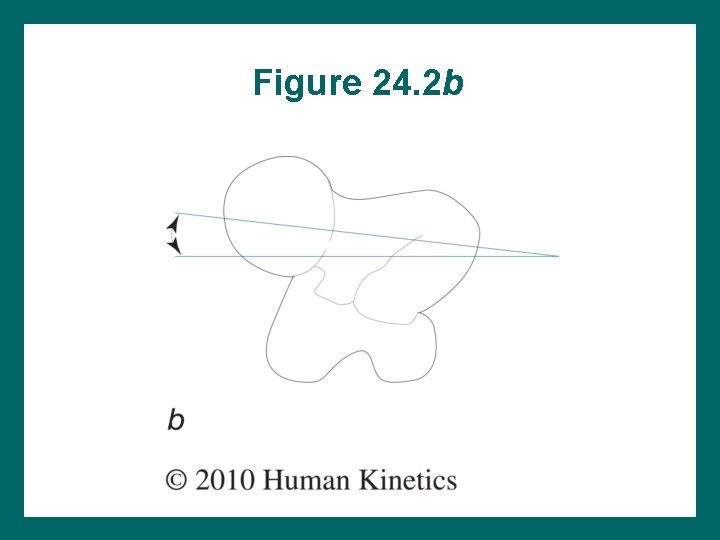
Transverse Plane Hip Alignment Retroversion (see figure 24. 2 b) – Femoral neck is rotated in relation to femoral shaft at an angle <12° – External rotation (ER), toe-out gait – Supinated foot, frog-eyed patellae, Q-angle, lumbar lordosis (continued)
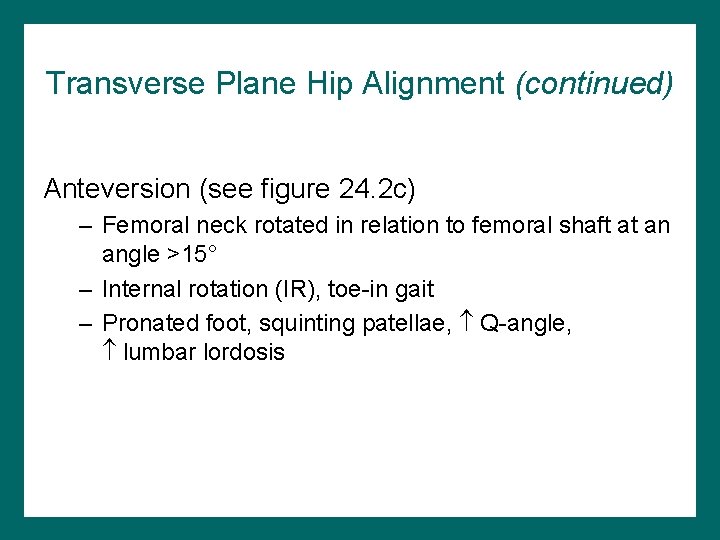
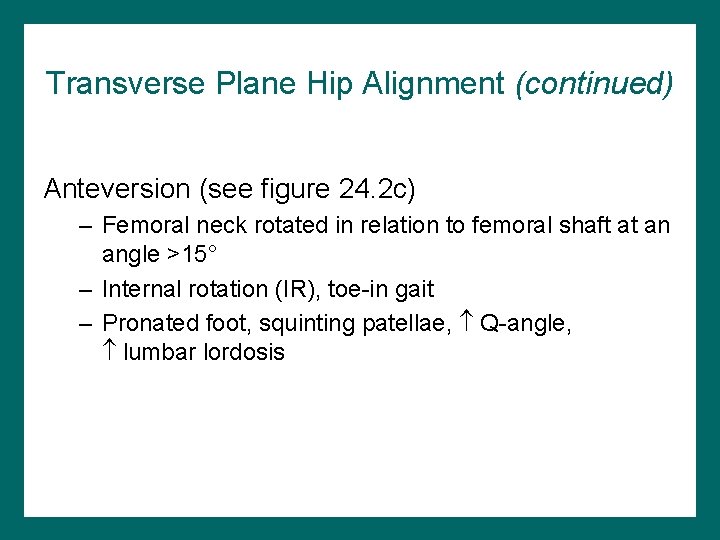
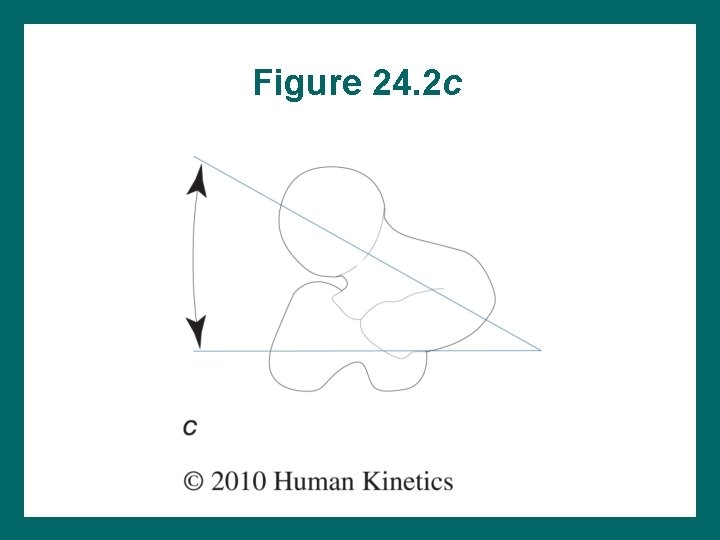
Transverse Plane Hip Alignment (continued) Anteversion (see figure 24. 2 c) – Femoral neck rotated in relation to femoral shaft at an angle >15° – Internal rotation (IR), toe-in gait – Pronated foot, squinting patellae, Q-angle, lumbar lordosis
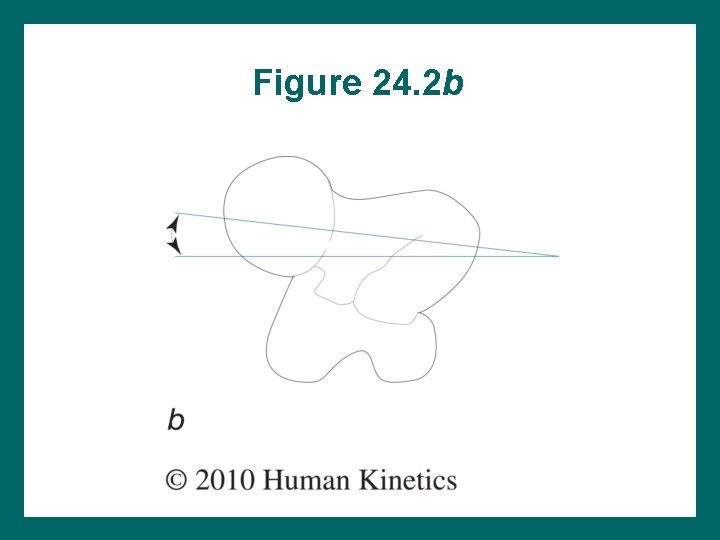
Figure 24. 2 b
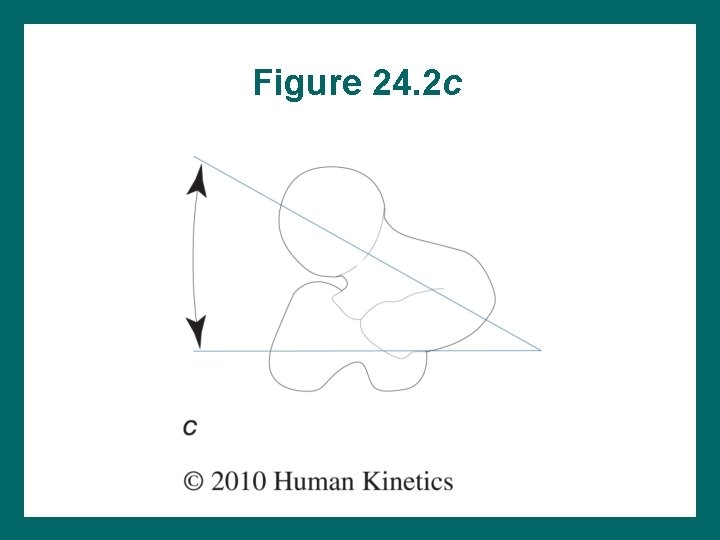
Figure 24. 2 c
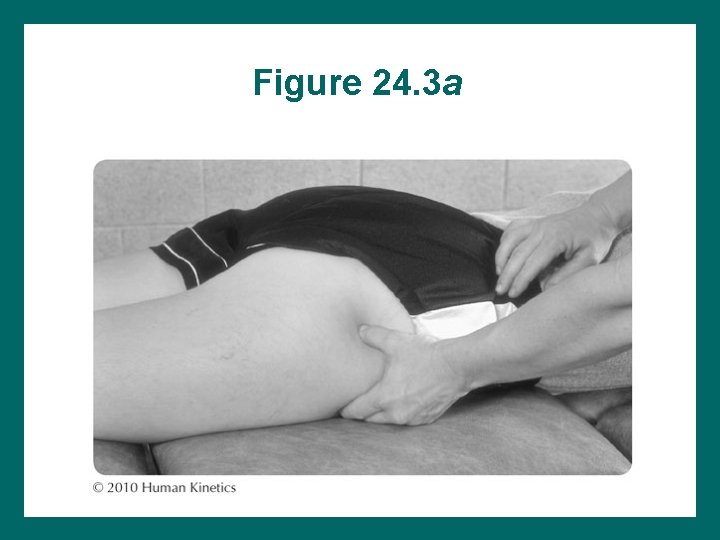
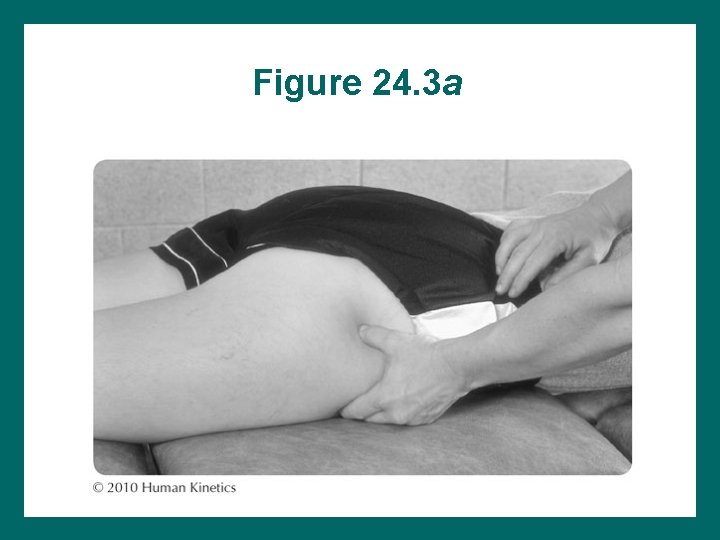
Figure 24. 3 a
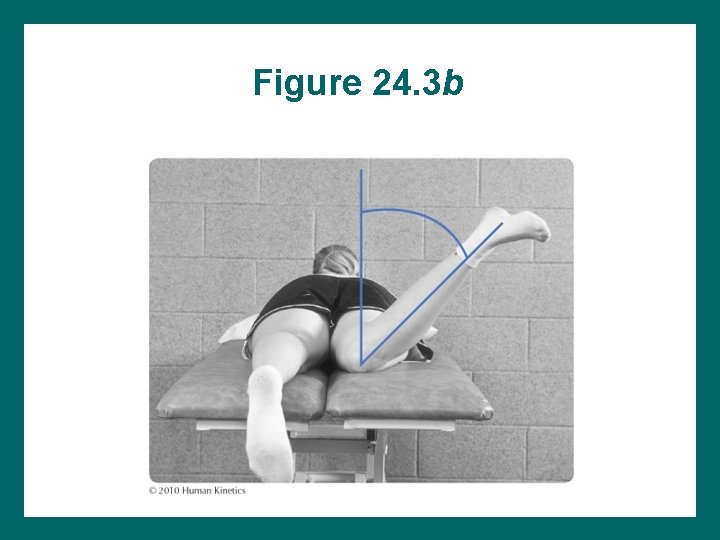
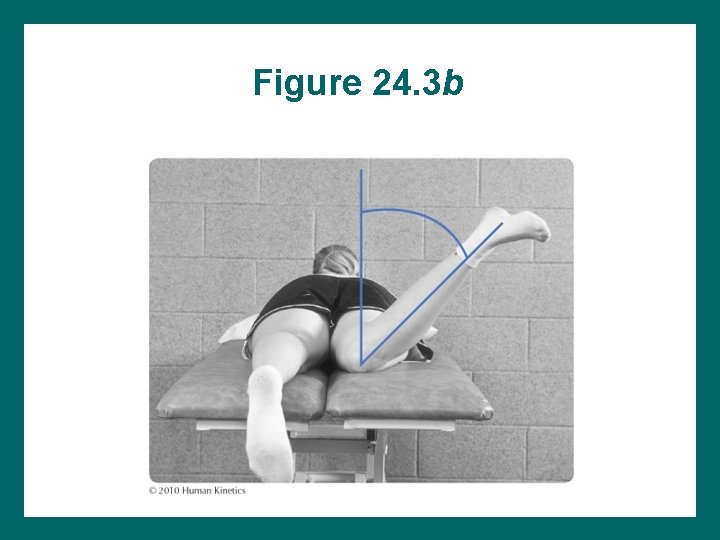
Figure 24. 3 b
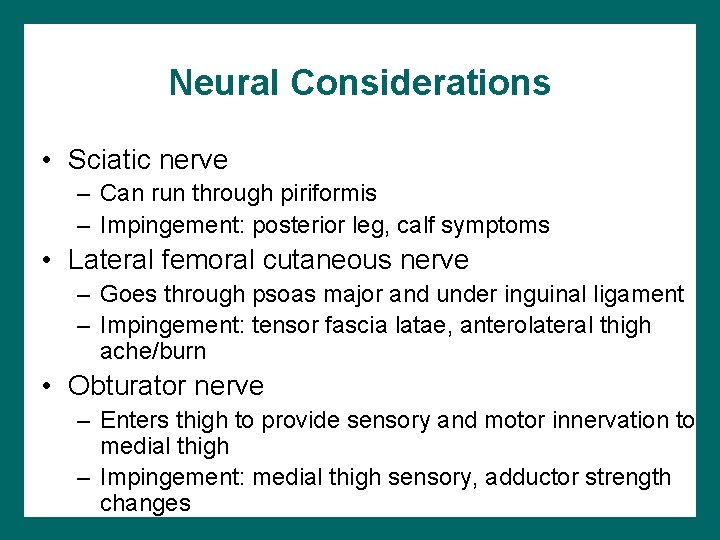
Neural Considerations • Sciatic nerve – Can run through piriformis – Impingement: posterior leg, calf symptoms • Lateral femoral cutaneous nerve – Goes through psoas major and under inguinal ligament – Impingement: tensor fascia latae, anterolateral thigh ache/burn • Obturator nerve – Enters thigh to provide sensory and motor innervation to medial thigh – Impingement: medial thigh sensory, adductor strength changes
Joint Mobility • Convex on concave rule • Resting position: 30° flexion, 30° abduction, slight lateral rotation • Close-packed position: full extension, abduction, and internal rotation • Capsular pattern: – ER = normal – IR = most restricted – Loss of motion: IR > flexion and abduction > extension
Influence of Pelvis • Pelvis movement influences hip movement • Anterior pelvic tilt – Moves anterior pelvis closer to anterior femur – Hip flexion • Posterior pelvic tilt – Moves posterior pelvis closer to posterior femur – Hip extension
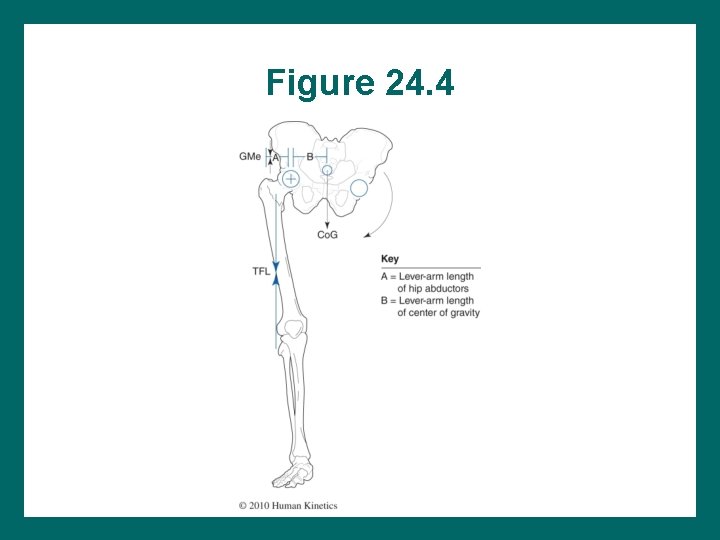
Unilateral Weight Bearing • In one-leg stance: – Rotation stress on hip – Hip abductors prevent contralateral pelvic drop • Necessary abductor force – >BW 2° LAL (lever-arm length) – If weak, hip will drop or patient must lean to BW LAL
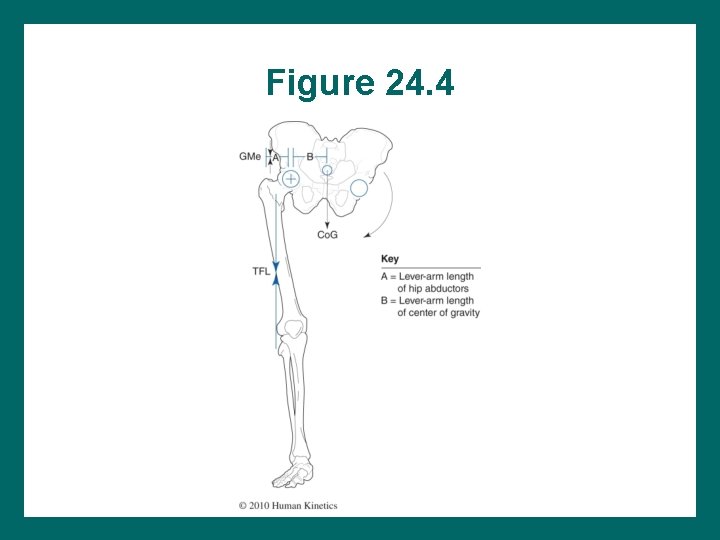
Figure 24. 4
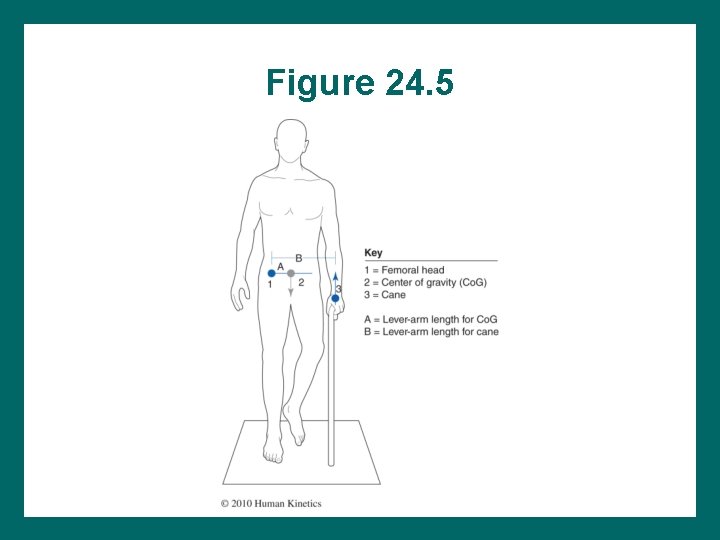
Assistive Devices in Ambulation • Assistive devices used to assist weak hip abductors • Cane on opposite side upward counterbalance force • Force through cane is small (~15%): cane LAL = >Co. G LAL
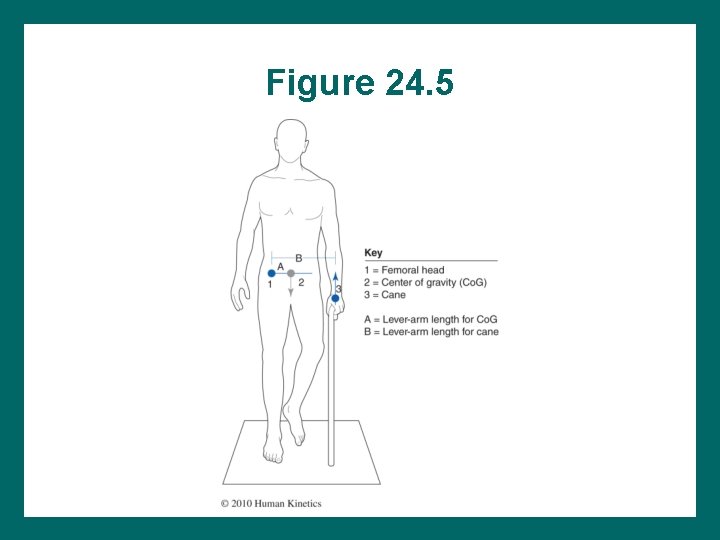
Figure 24. 5
Leg-Length Discrepancies • Can be caused by true length or soft-tissue differences • Pelvis drops on shorter side; trunk bends away from the short leg in weight bearing • Uneven shoe wear most obvious indication • Can lead to osteoarthritis of longer leg
Reducing Hip Stress in Acute Lower-Extremity Injuries • Goal post-injury: normal gait • Antalgic gait: requires assistive devices until normal ambulation is possible • Stride length during walking or running – Smaller stride reduces the force and motion demands – Spica wrap
Rehabilitation Considerations • Hip pain can be difficult to interpret since there are several referring sources of pain – – Hip: to groin, medial anterior thigh Spine: to anterior hip, buttock, thigh Sacrum: buttock, posterior thigh, lateral thigh Organs and abdomen: to groin • Differential diagnosis may be needed (continued)
Rehabilitation Considerations (continued) • Some hip injuries are self-limiting. • Predisposing factors must be corrected to reduce recurrence. • Inclusion exercises: – Hip stabilization – Knee and ankle weakness – Trunk stabilization
Soft-Tissue Mobilization • If Rx is not effective, reassess: • Soft-tissue techniques – – Deep-tissue massage Scar-tissue massage Cross-friction mobilization Myofascial release (i. e. , trigger point and ice-andstretch) • End with active stretches • Home exercise program: Stretches, selfmobilization
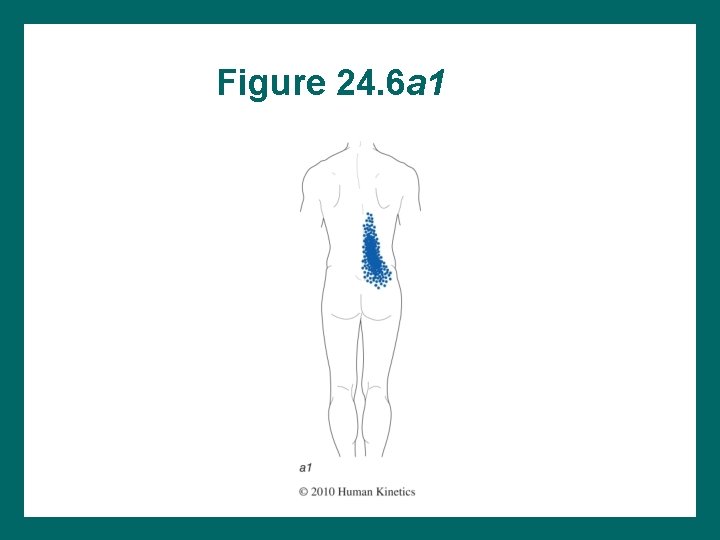
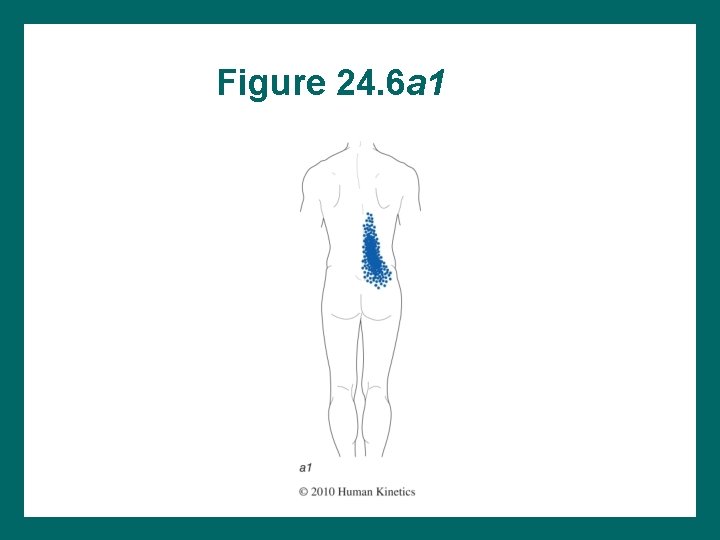
Figure 24. 6 a 1
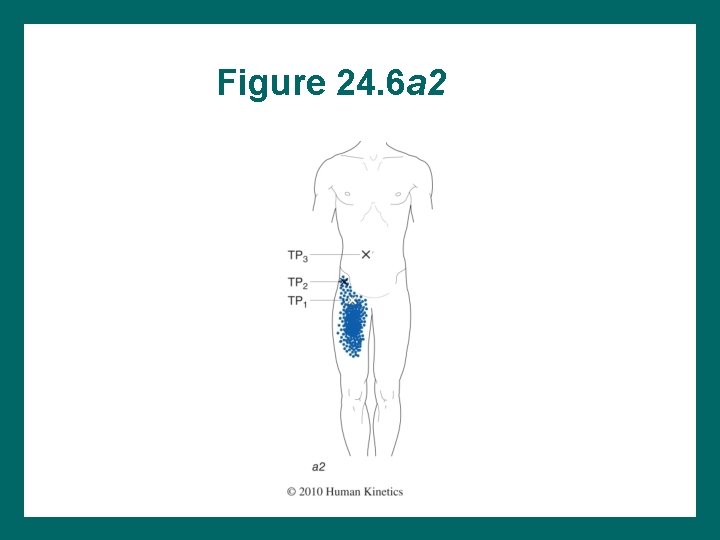
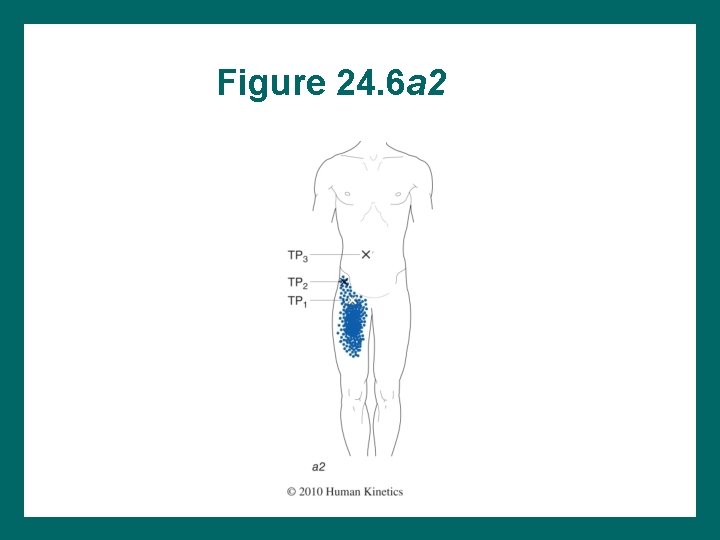
Figure 24. 6 a 2
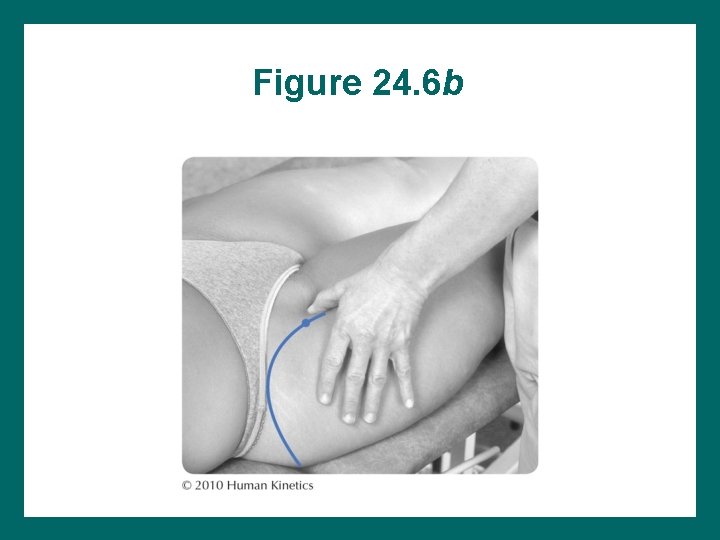
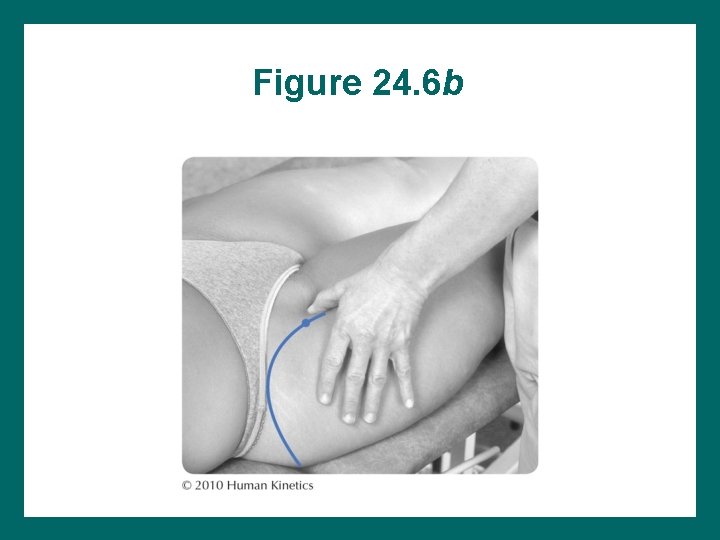
Figure 24. 6 b
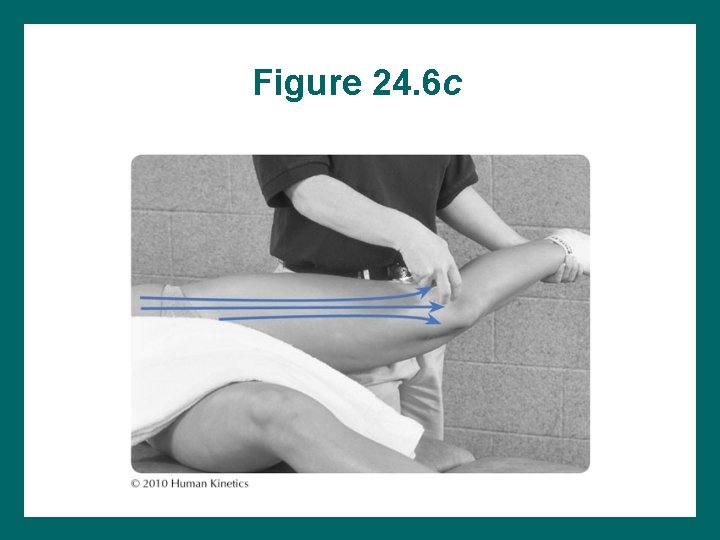
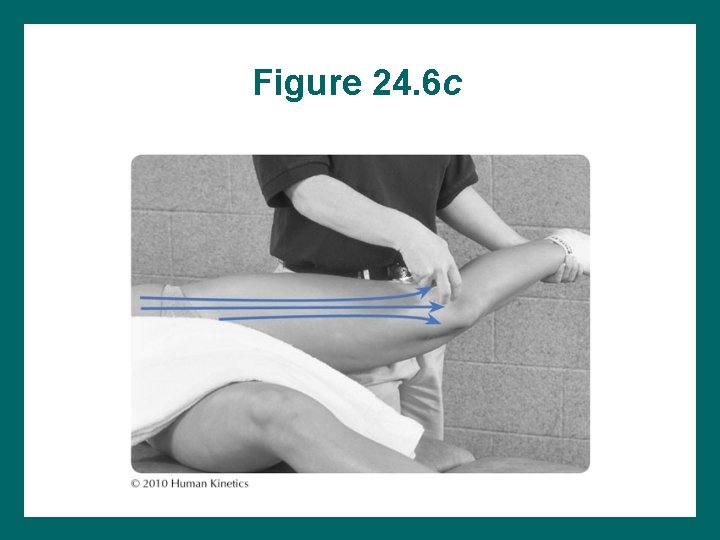
Figure 24. 6 c
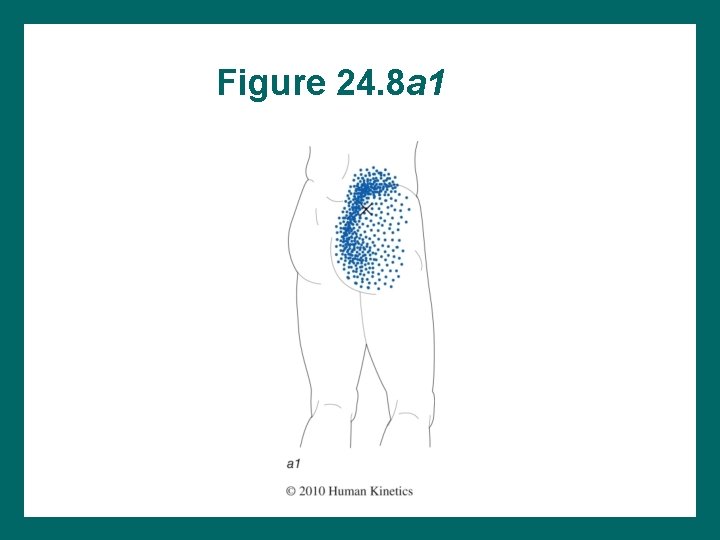
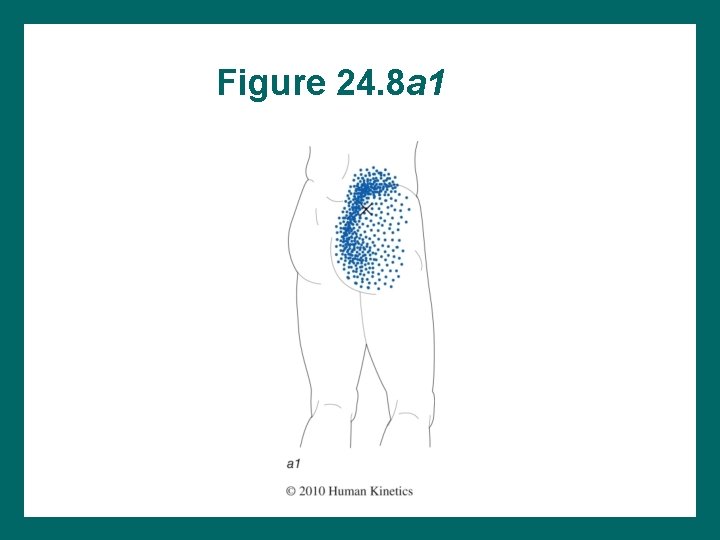
Figure 24. 8 a 1
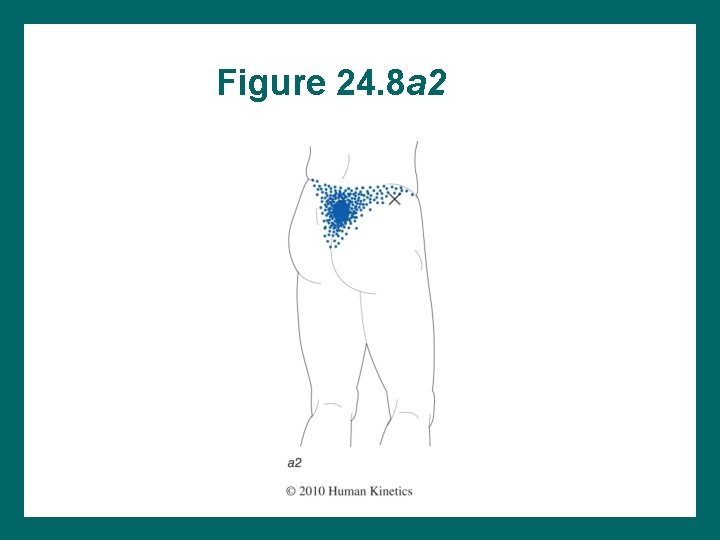
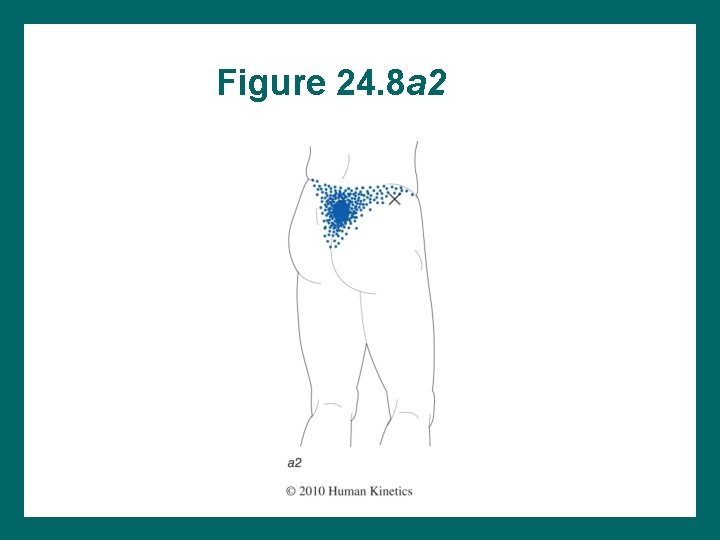
Figure 24. 8 a 2
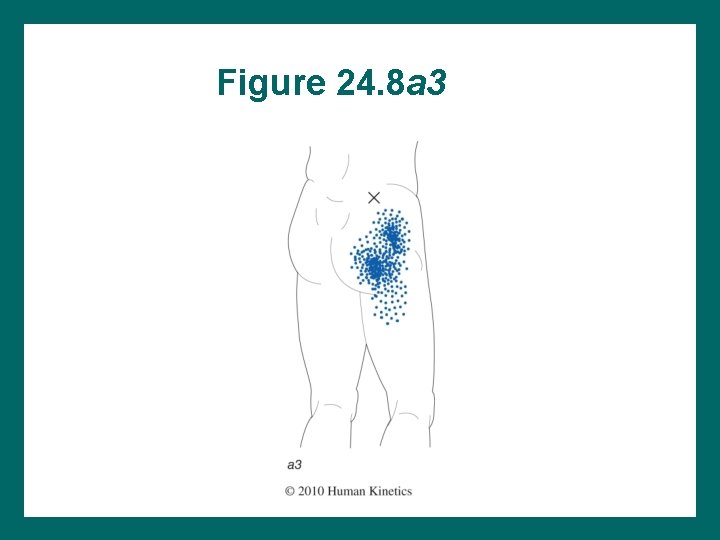
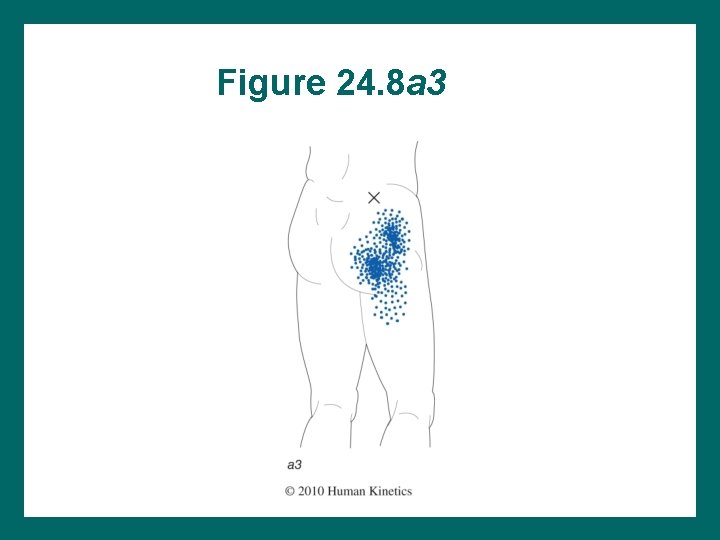
Figure 24. 8 a 3
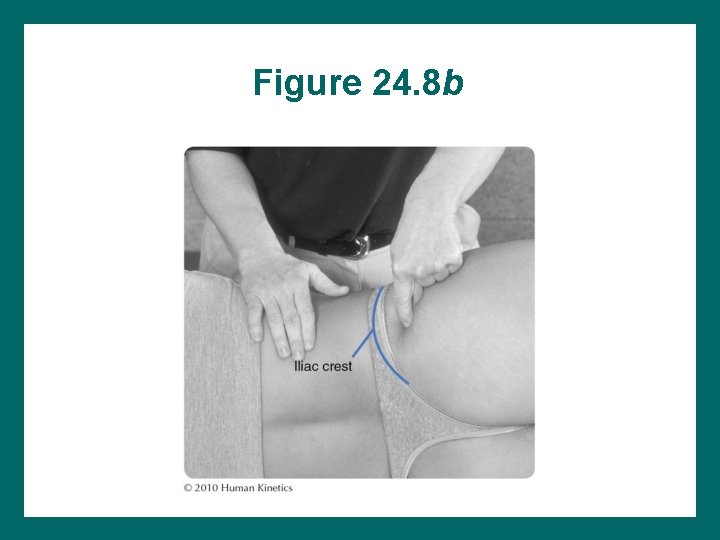
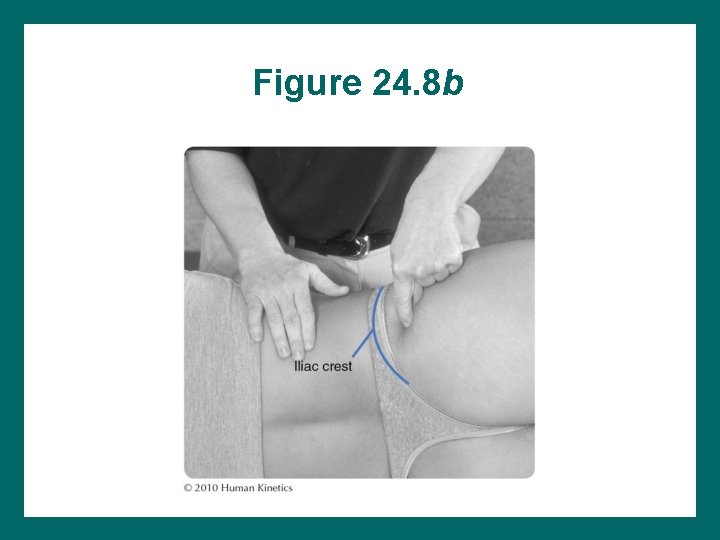
Figure 24. 8 b
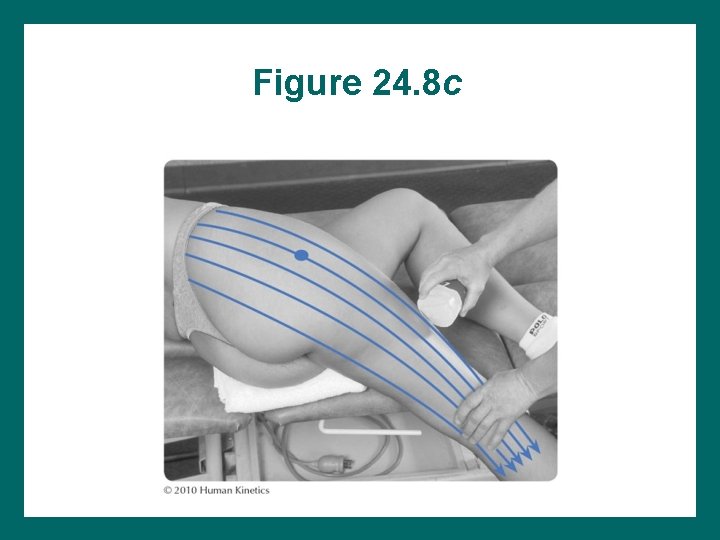
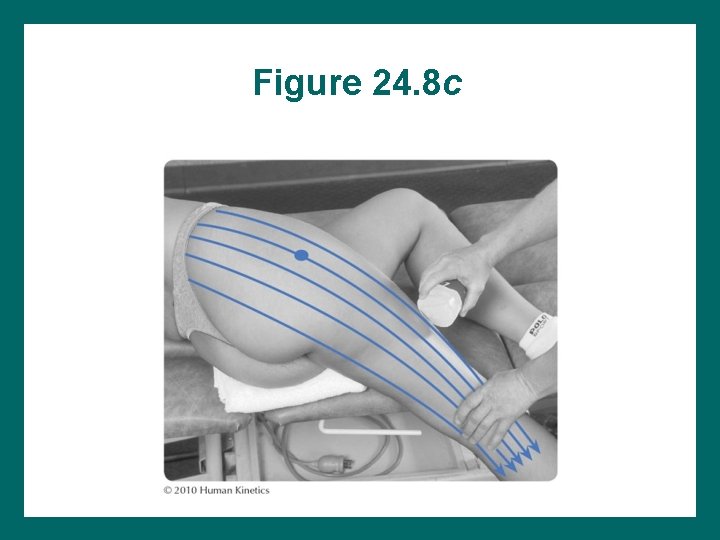
Figure 24. 8 c
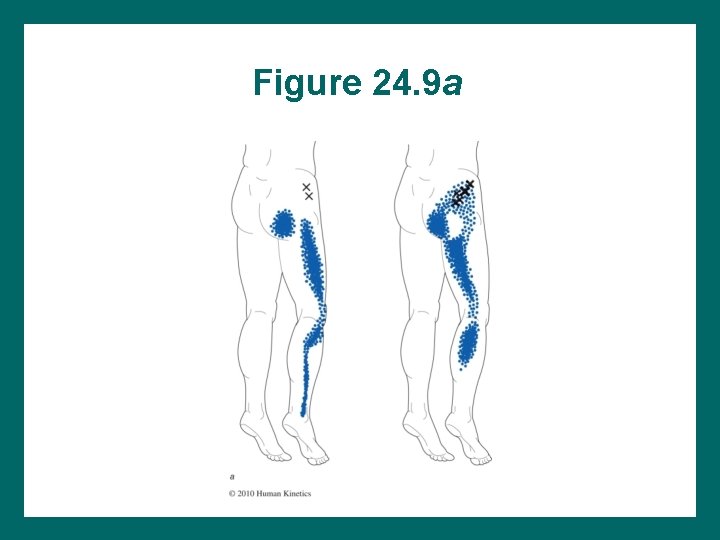
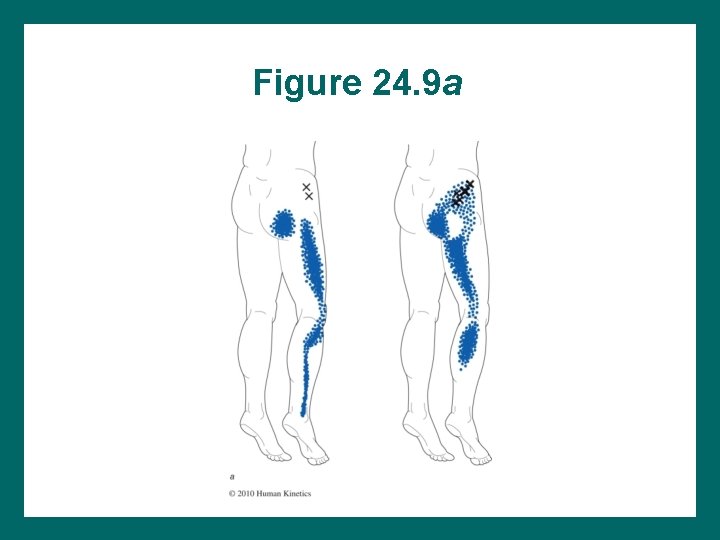
Figure 24. 9 a
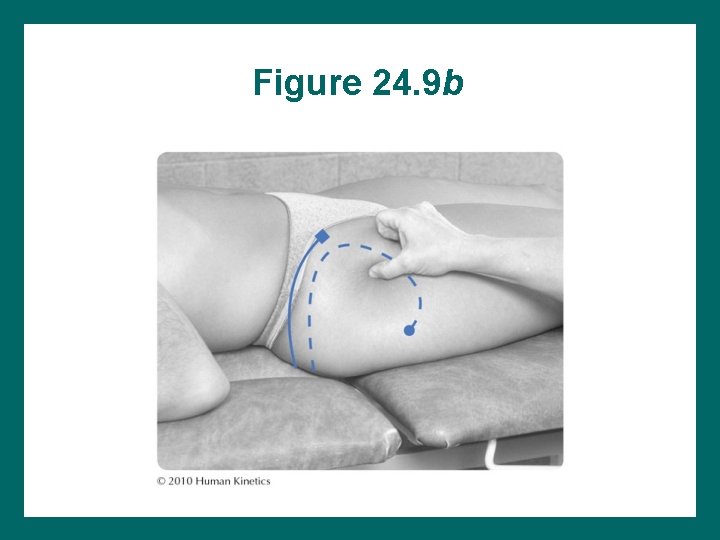
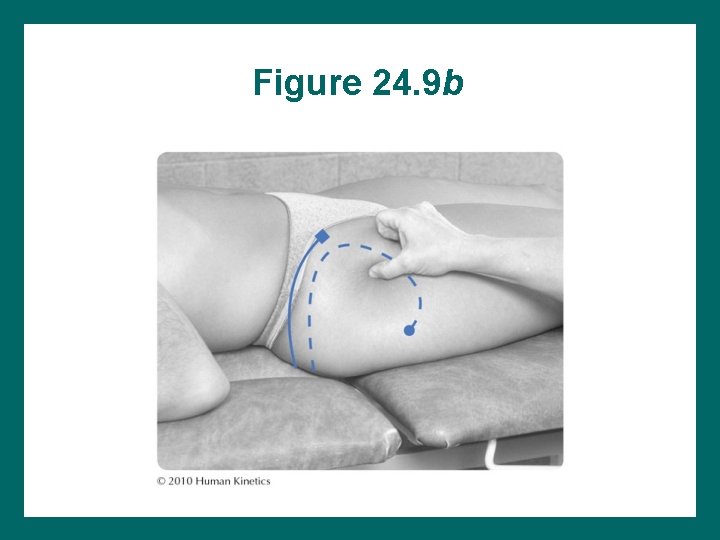
Figure 24. 9 b
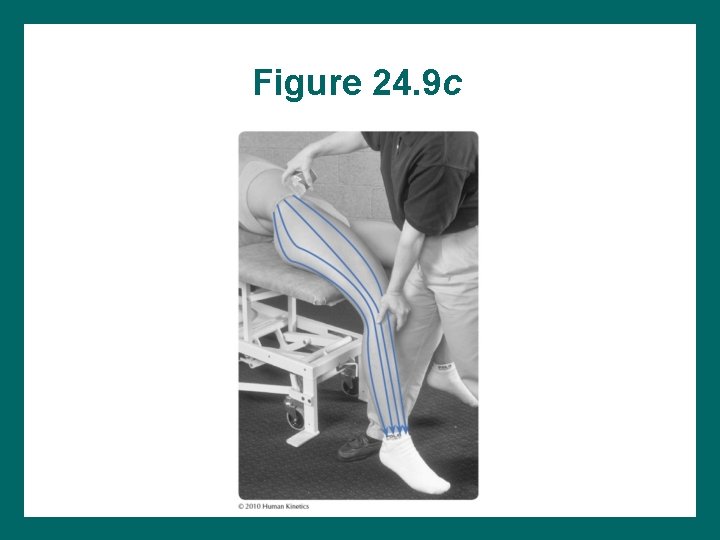
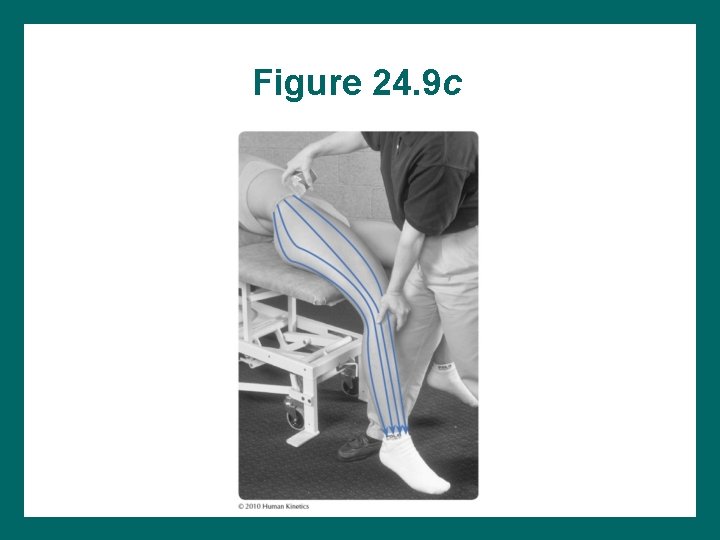
Figure 24. 9 c
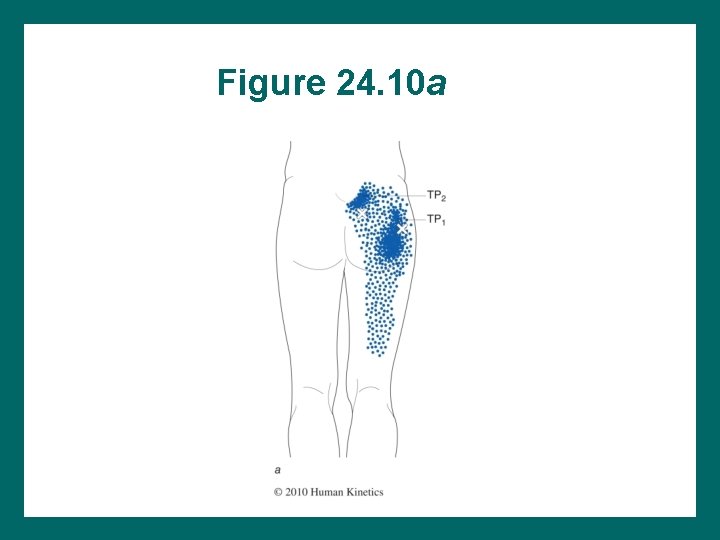
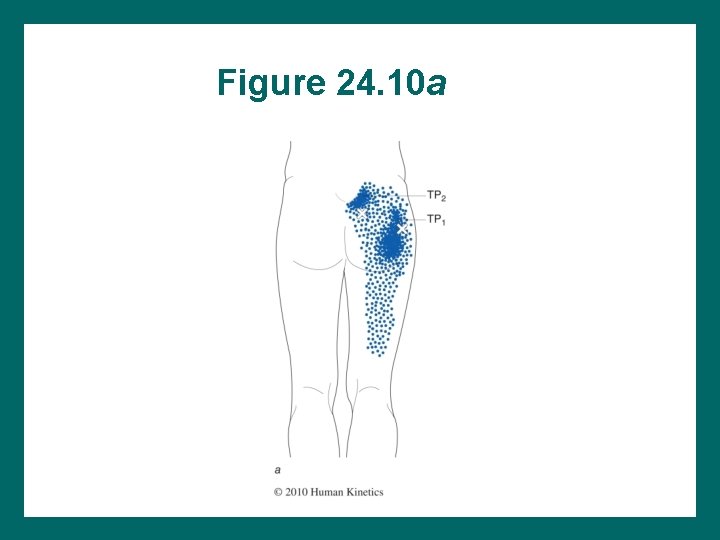
Figure 24. 10 a
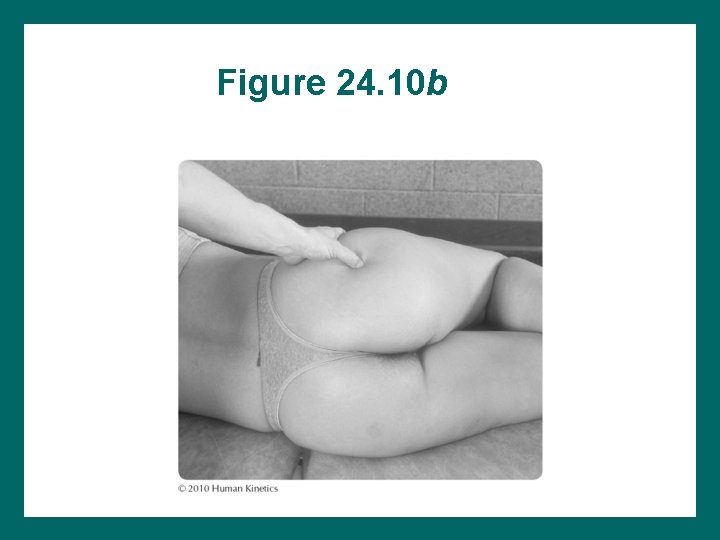
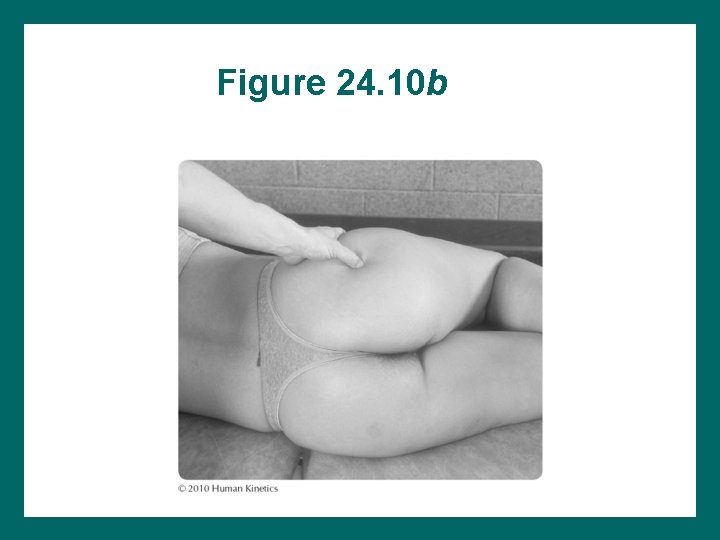
Figure 24. 10 b
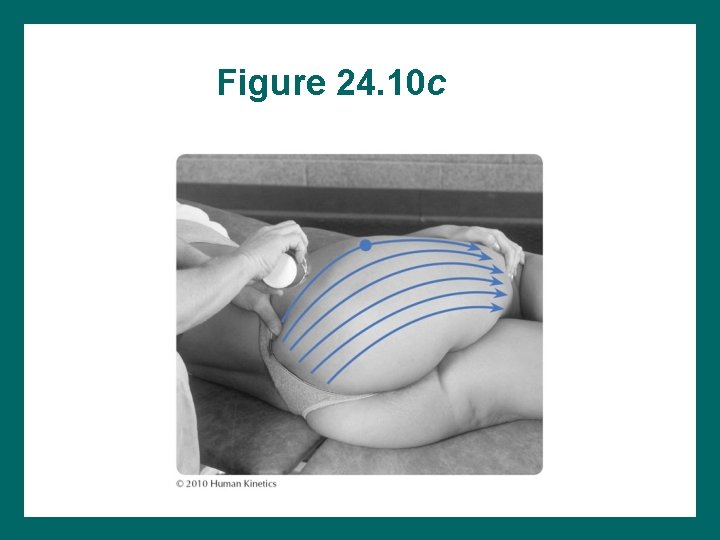
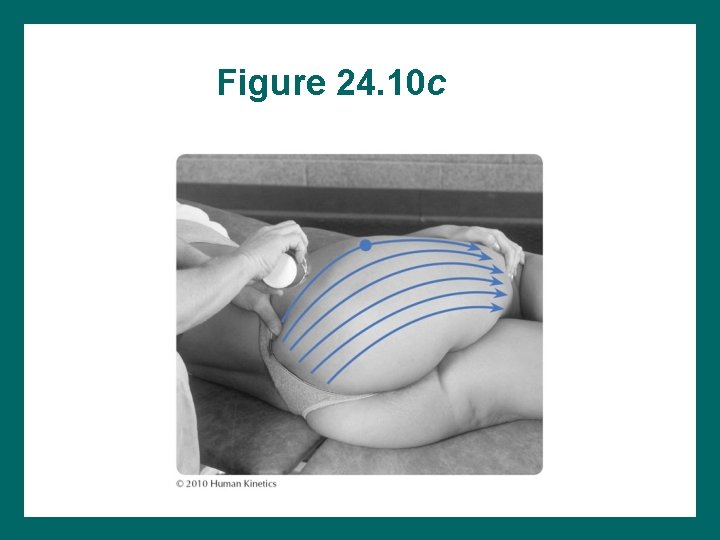
Figure 24. 10 c
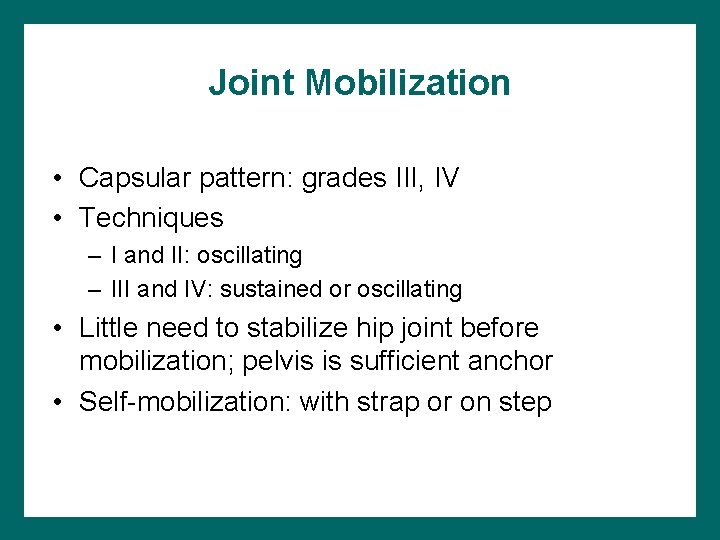
Joint Mobilization • Capsular pattern: grades III, IV • Techniques – I and II: oscillating – III and IV: sustained or oscillating • Little need to stabilize hip joint before mobilization; pelvis is sufficient anchor • Self-mobilization: with strap or on step
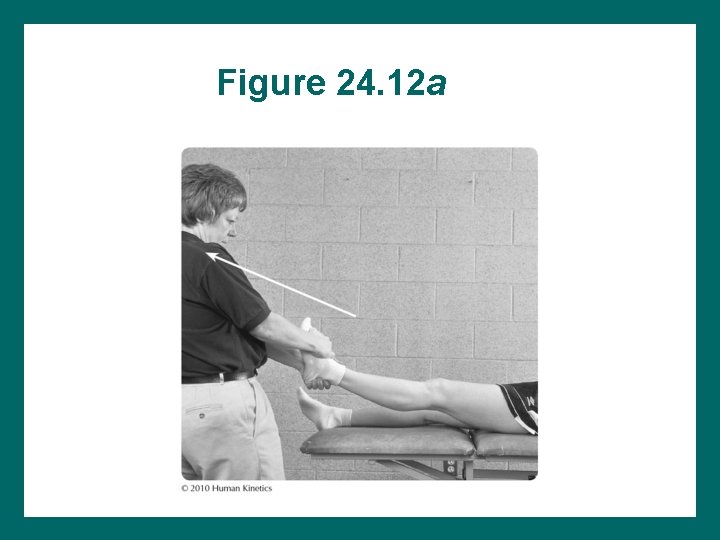
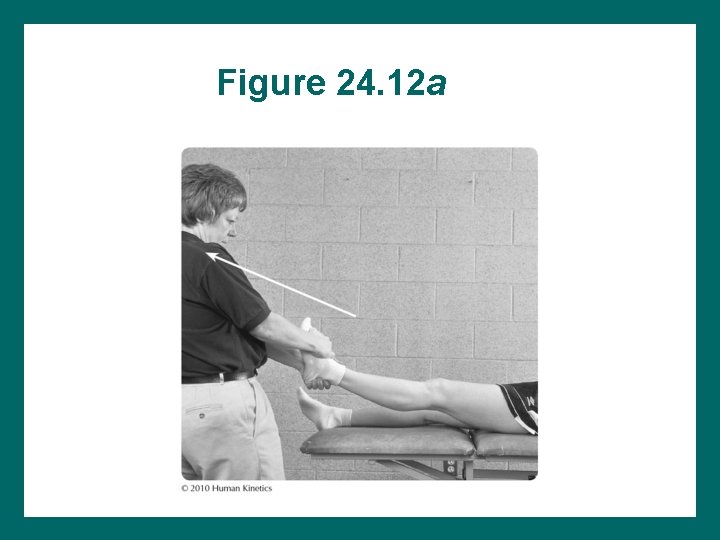
Figure 24. 12 a
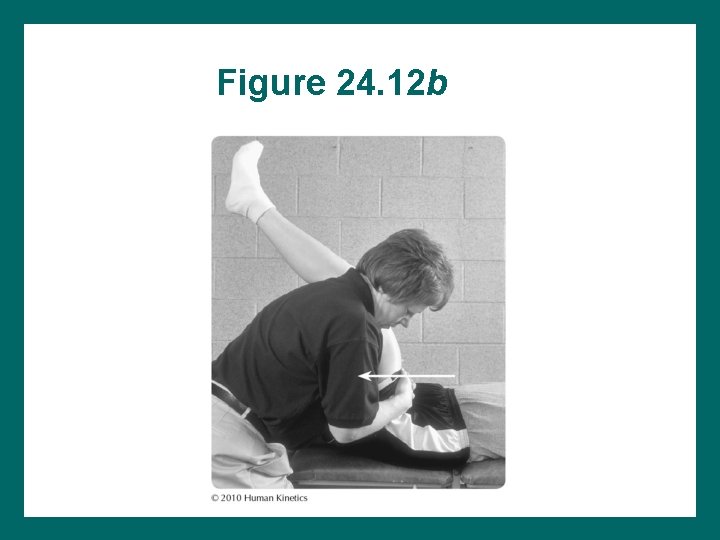
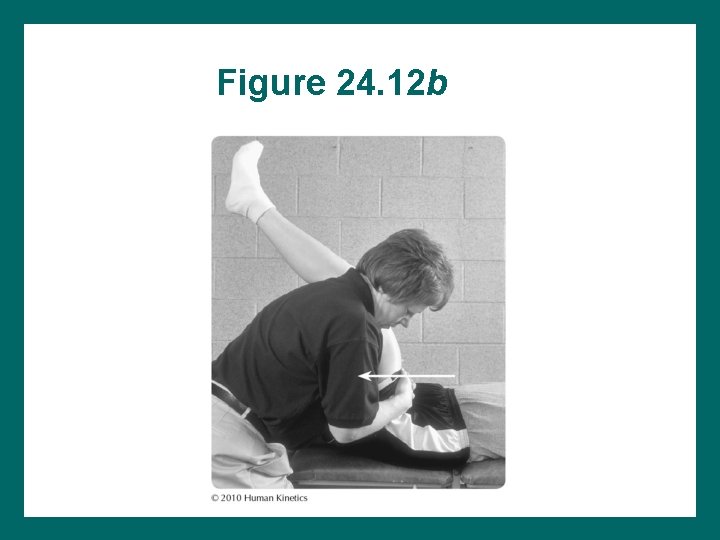
Figure 24. 12 b
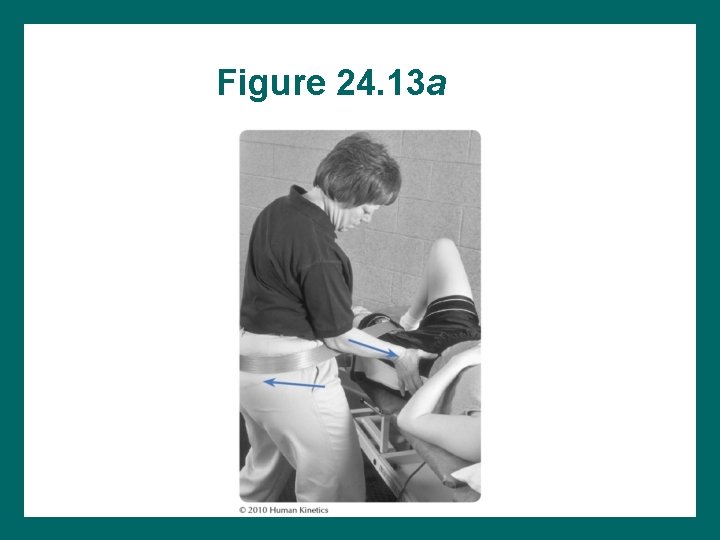
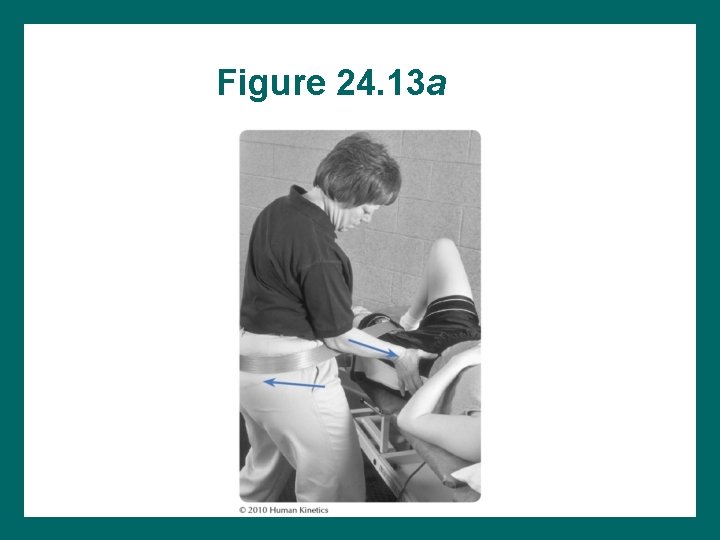
Figure 24. 13 a
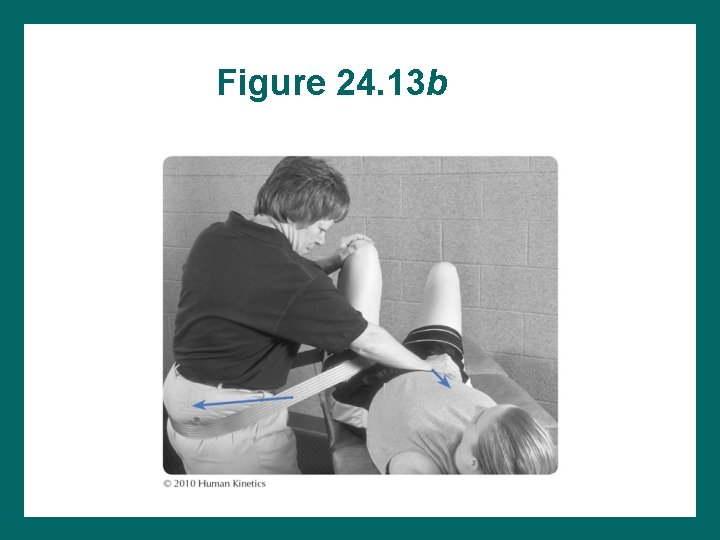
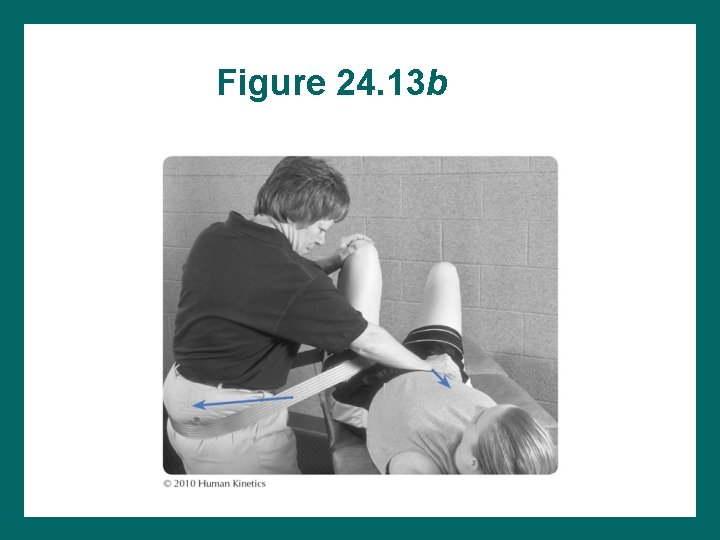
Figure 24. 13 b
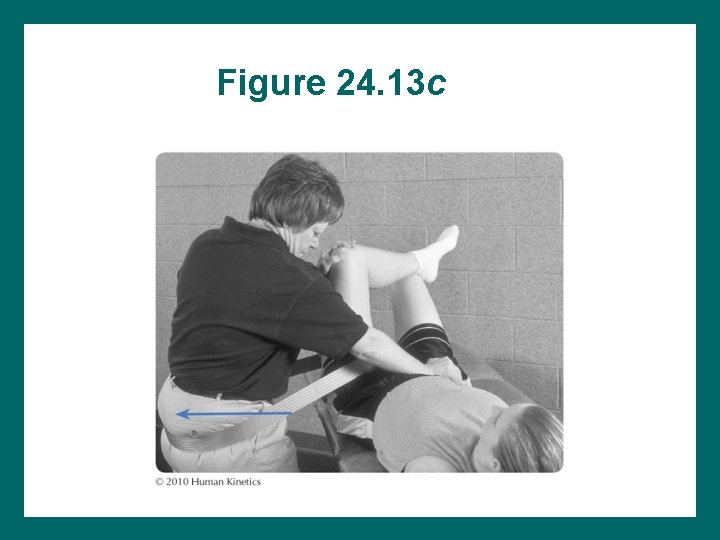
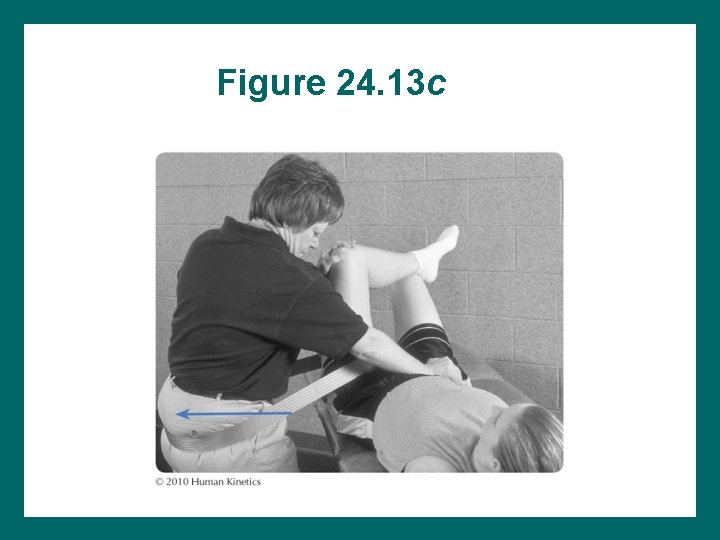
Figure 24. 13 c
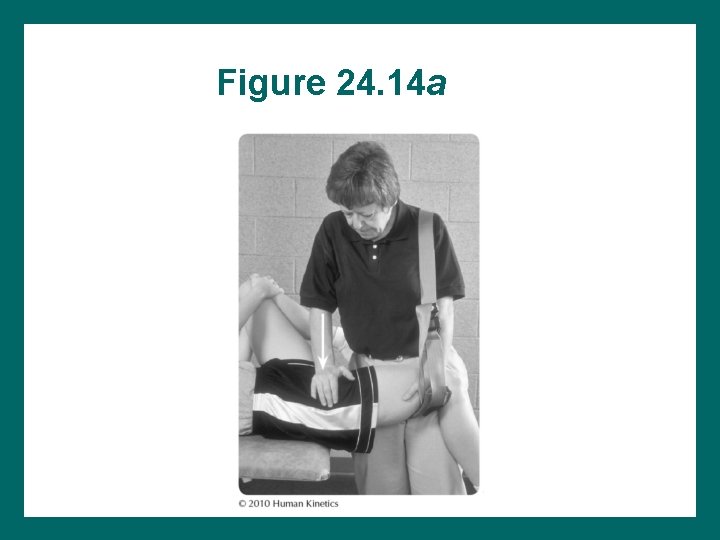
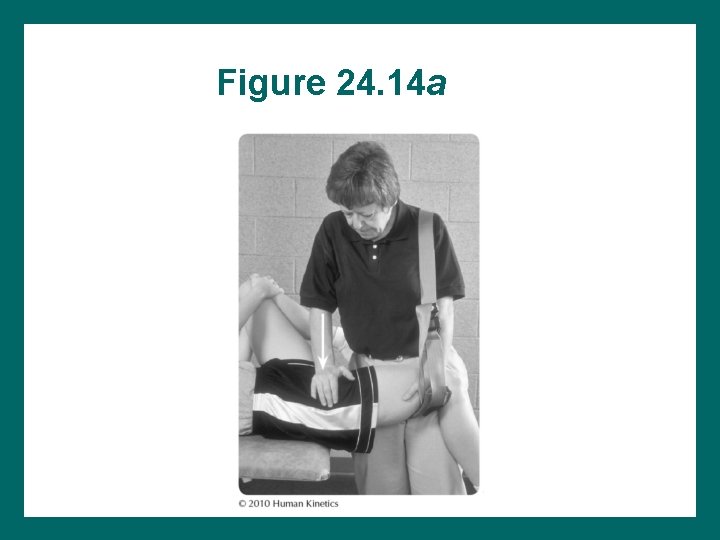
Figure 24. 14 a
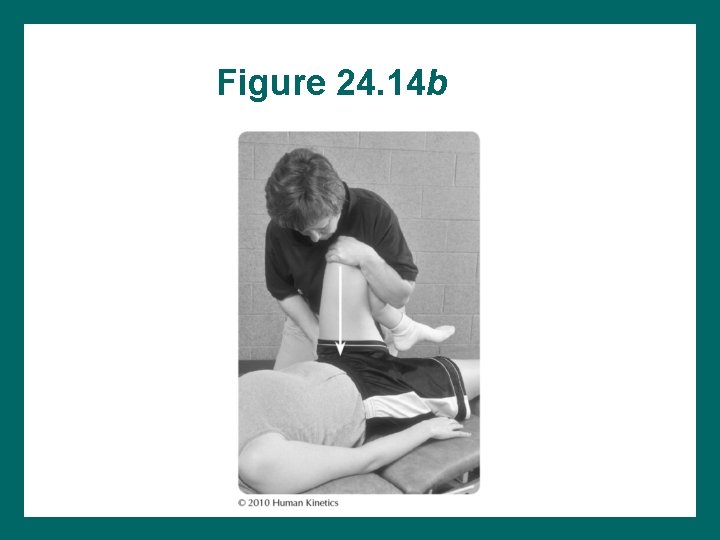
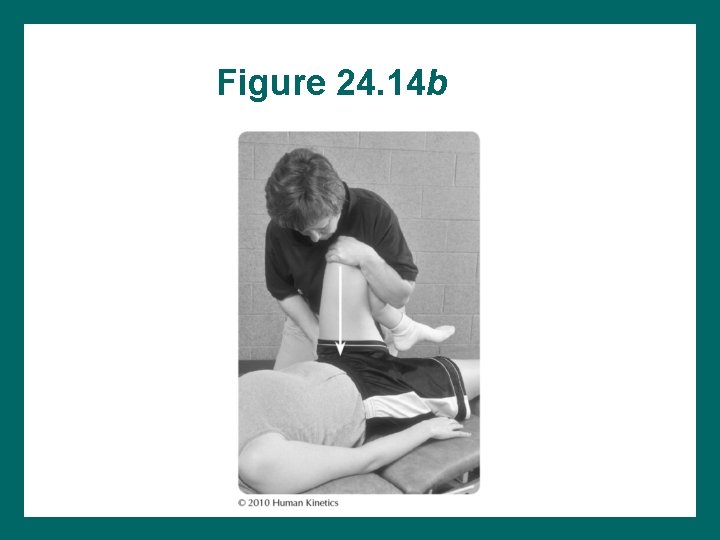
Figure 24. 14 b
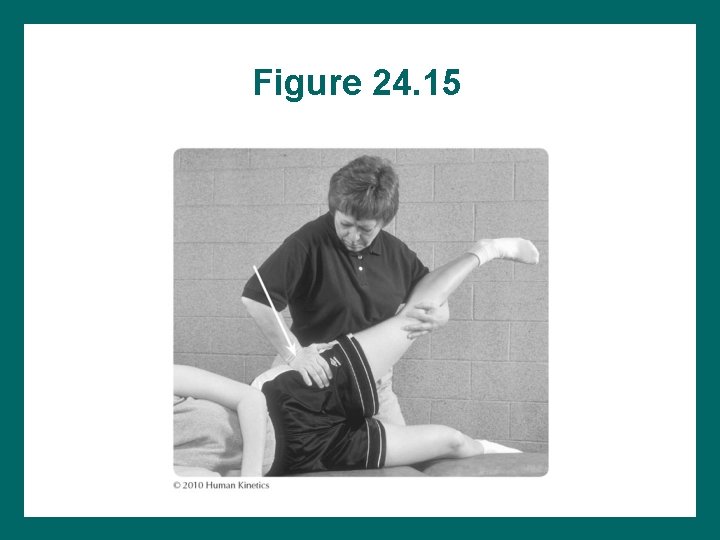
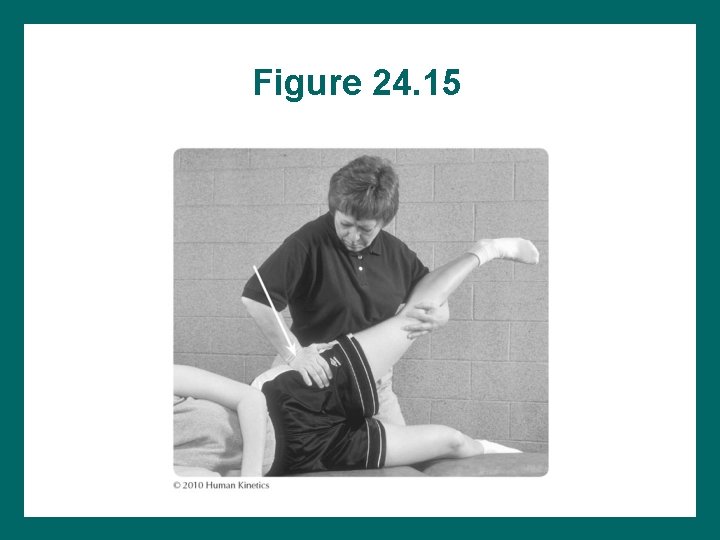
Figure 24. 15
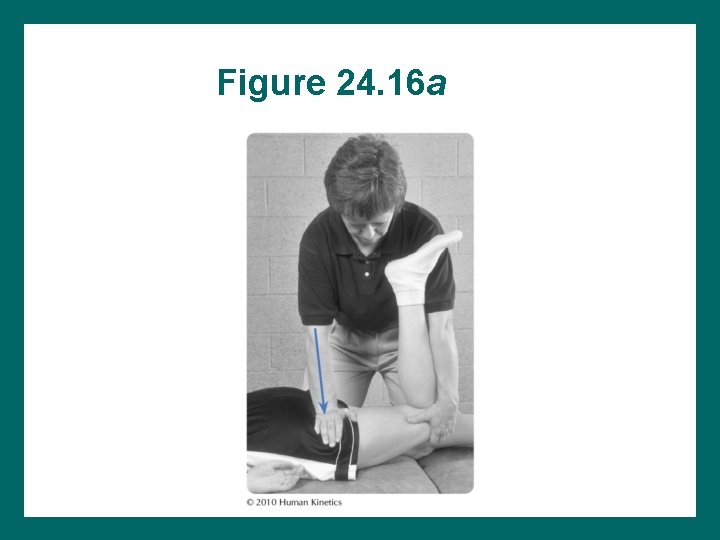
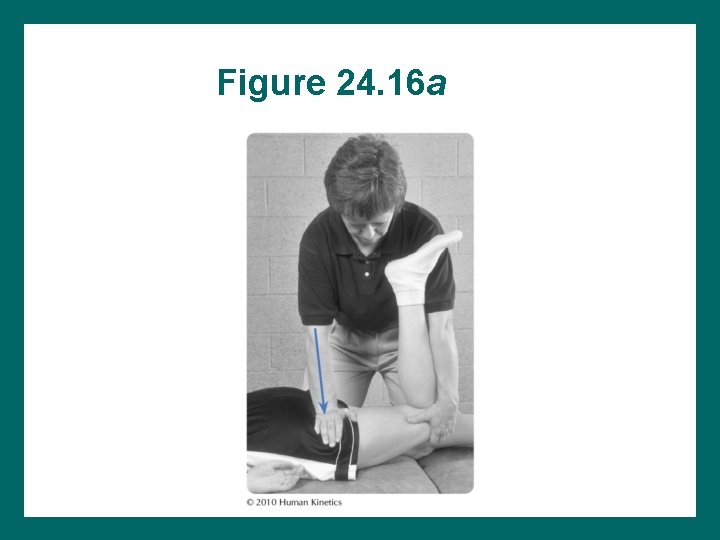
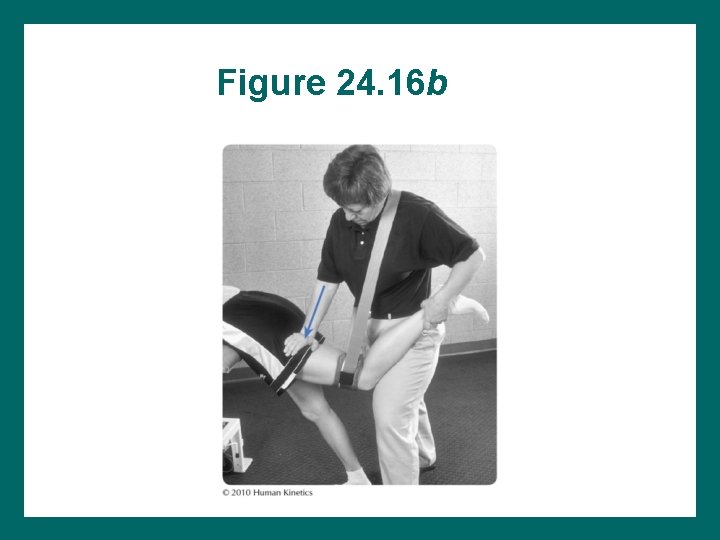
Figure 24. 16 a
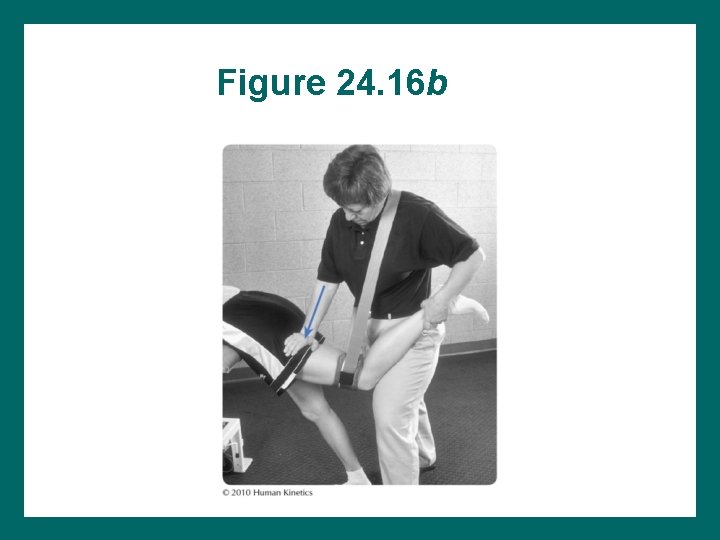
Figure 24. 16 b
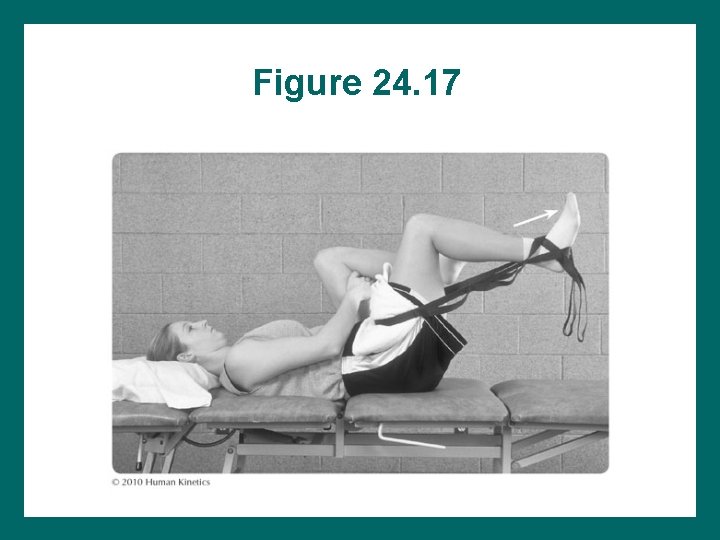
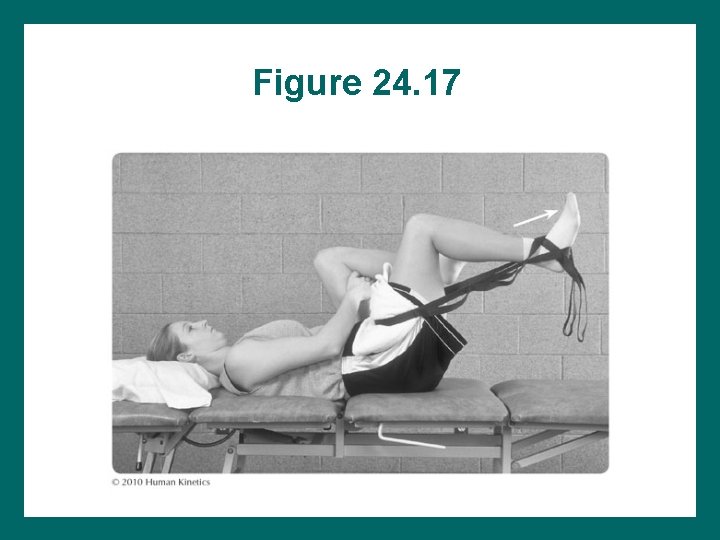
Figure 24. 17
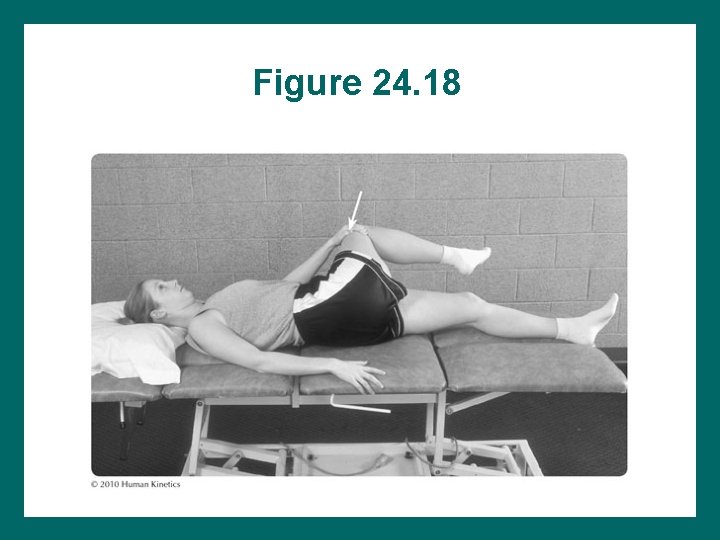
Flexibility Exercises • Knee, back, and pelvis must be positioned appropriately. • Active contraction of opposing muscles leads to improved results. • Prolonged stretches are most effective for aged scar tissue or thick collagen tissue structures.
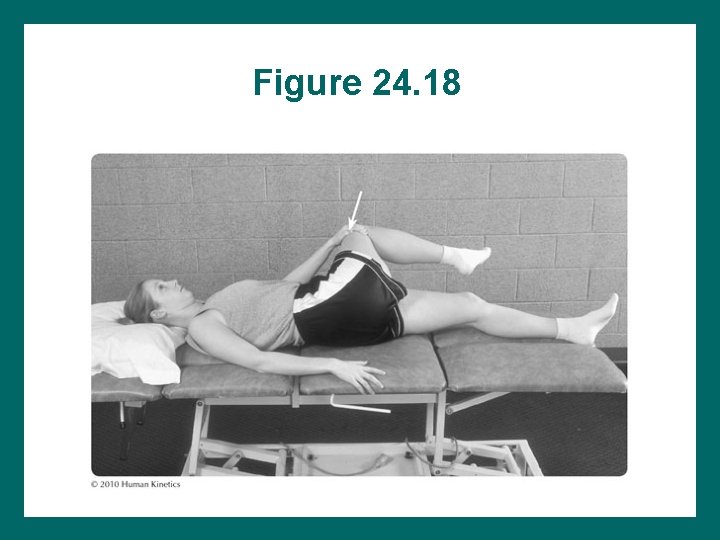
Figure 24. 18
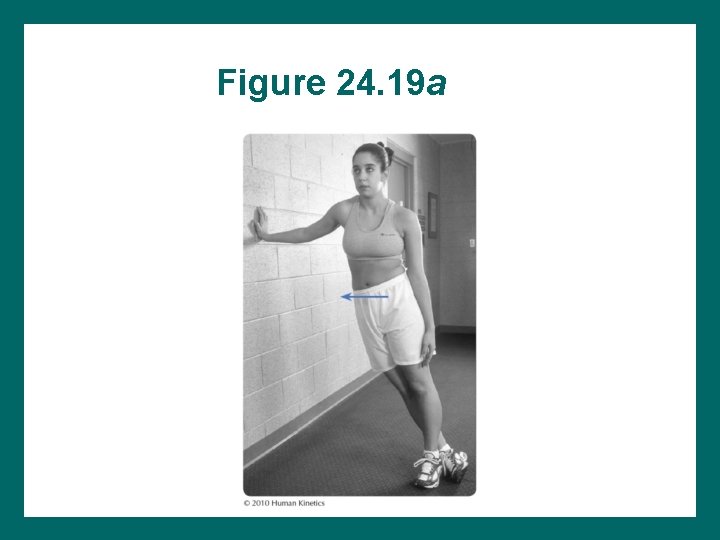
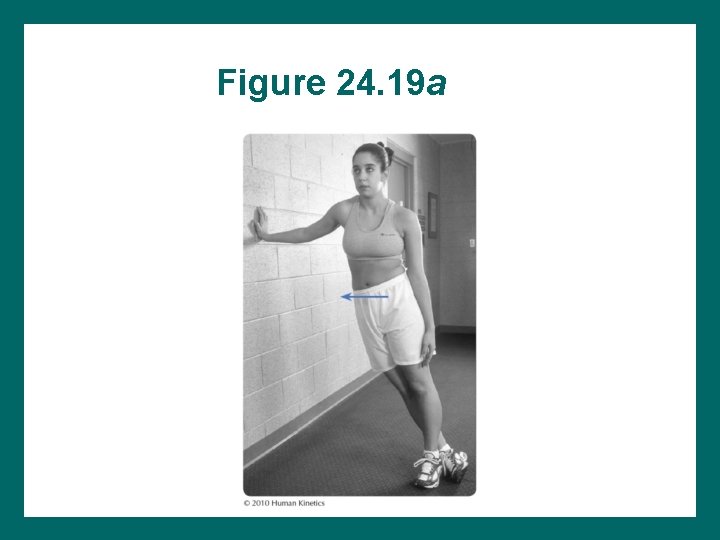
Figure 24. 19 a
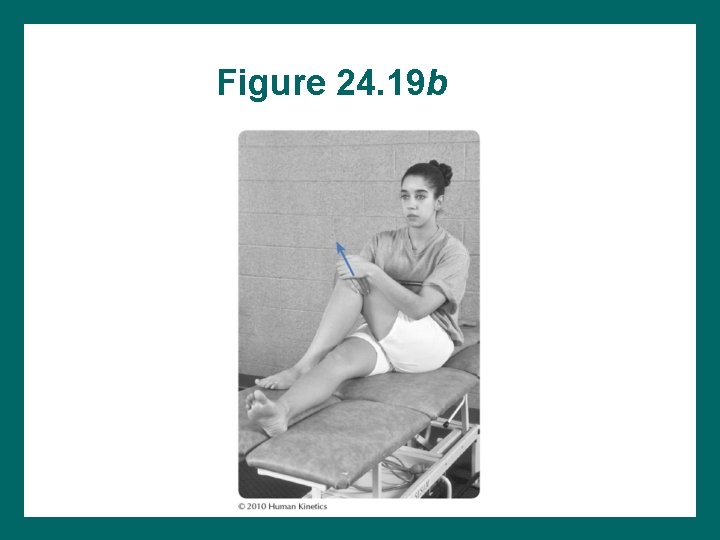
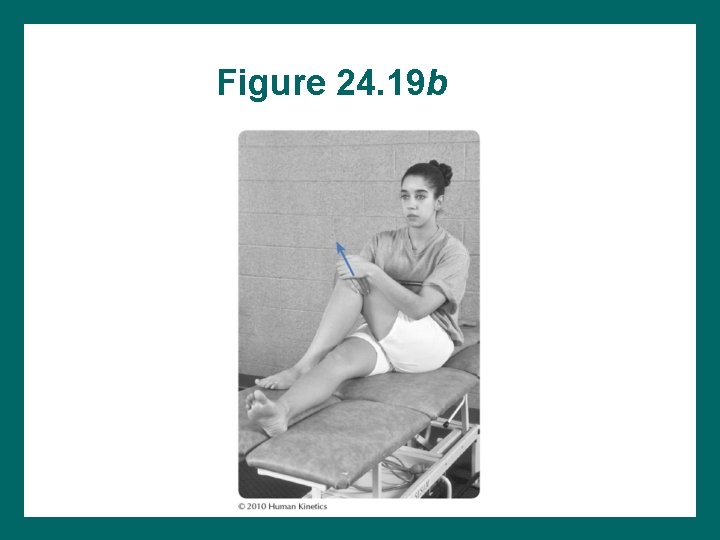
Figure 24. 19 b
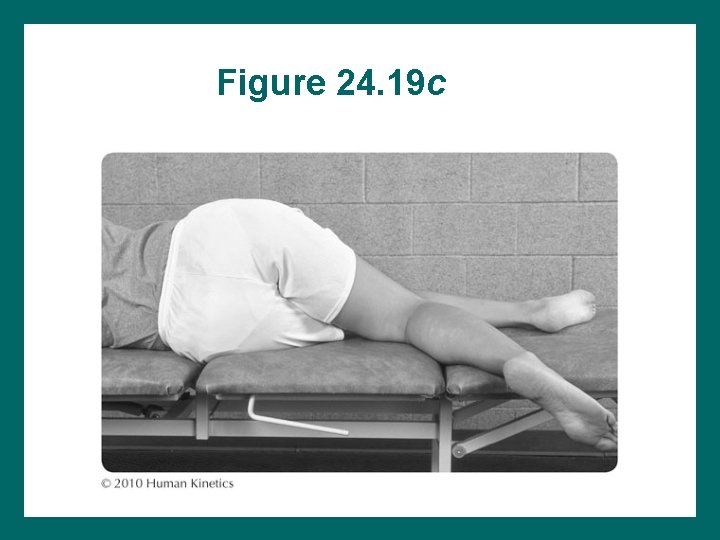
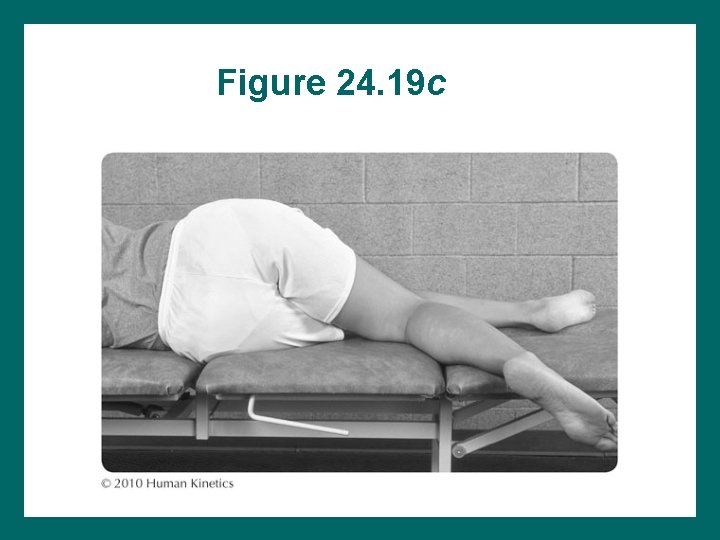
Figure 24. 19 c
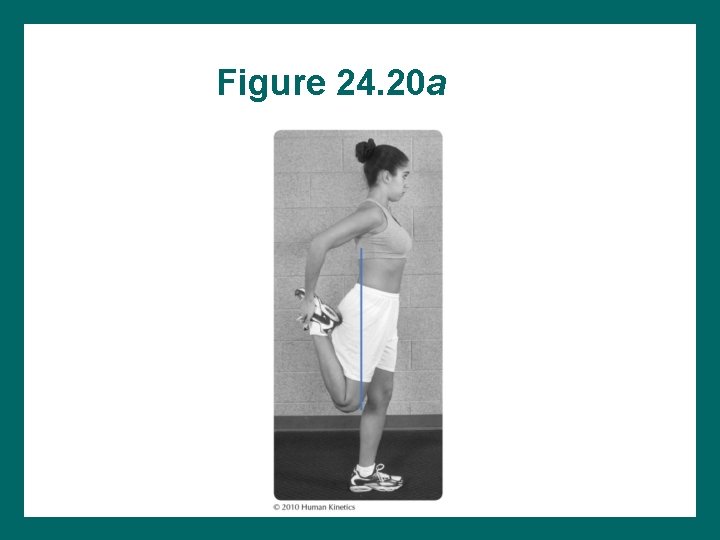
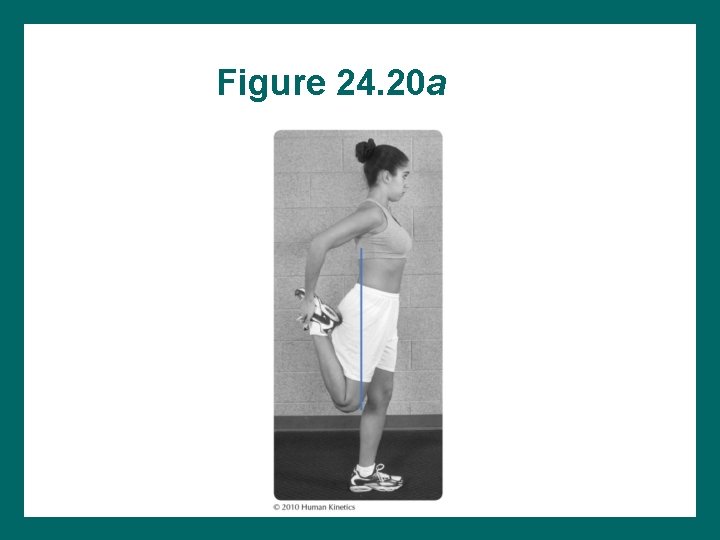
Figure 24. 20 a
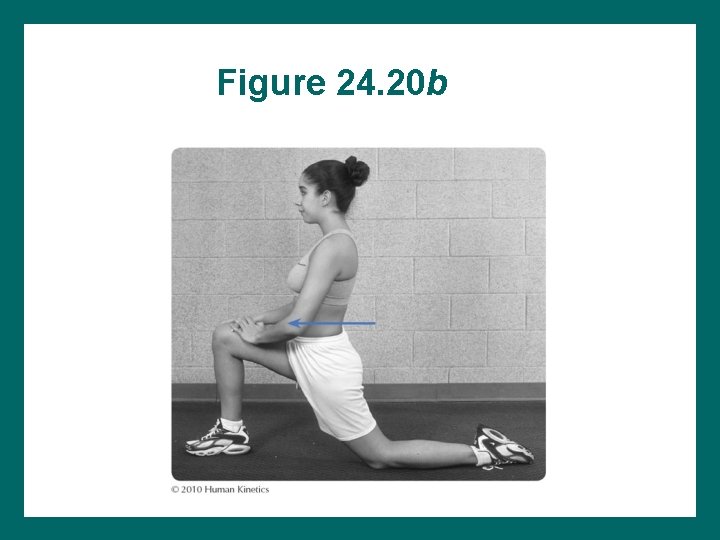
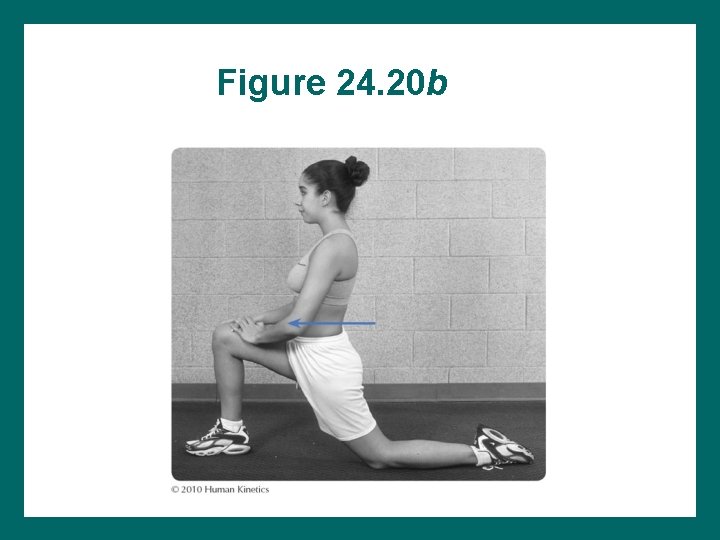
Figure 24. 20 b
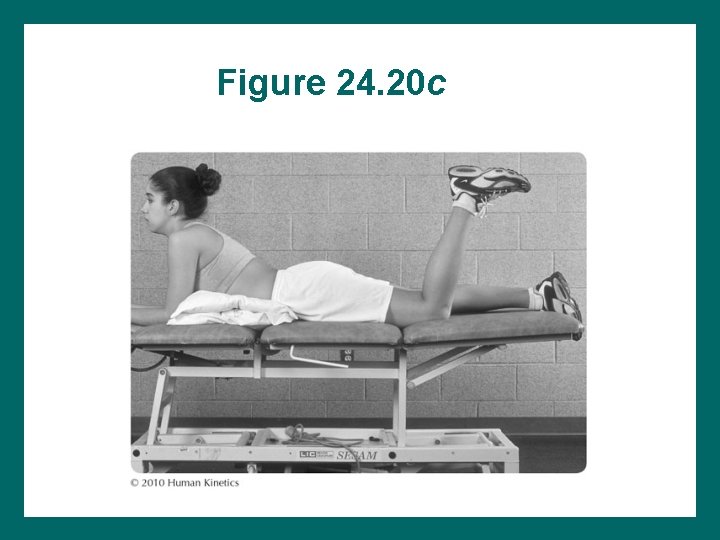
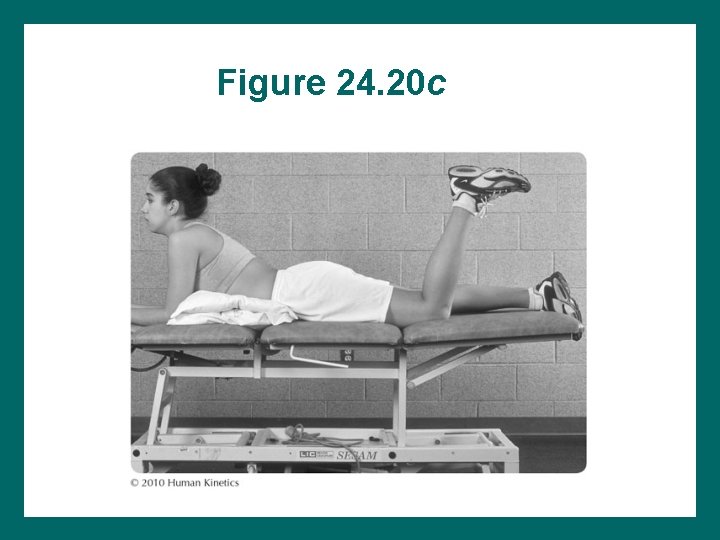
Figure 24. 20 c
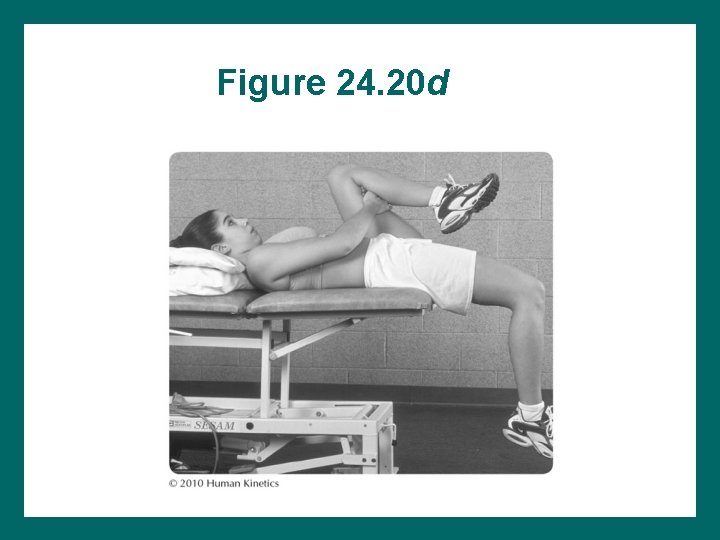
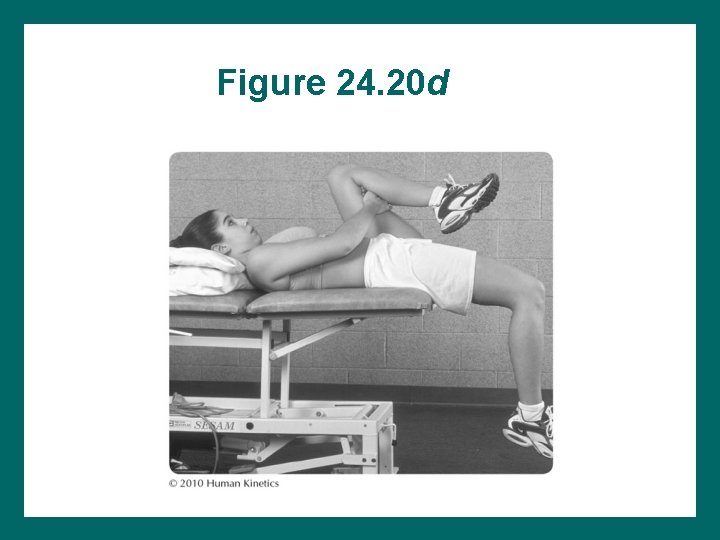
Figure 24. 20 d
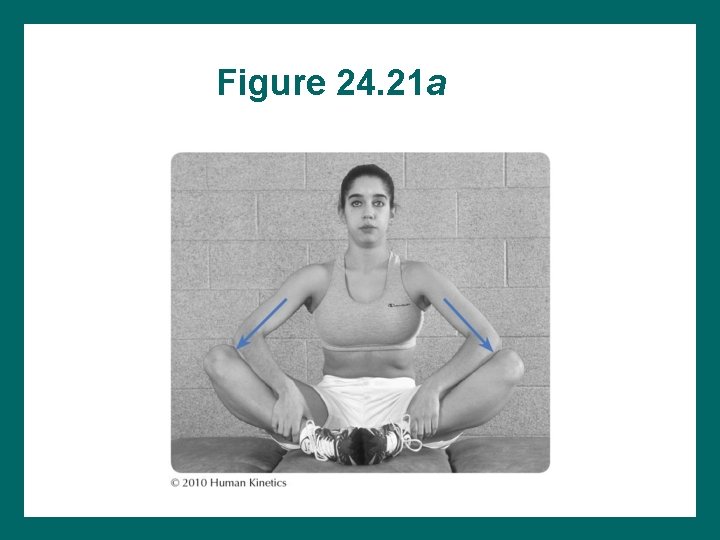
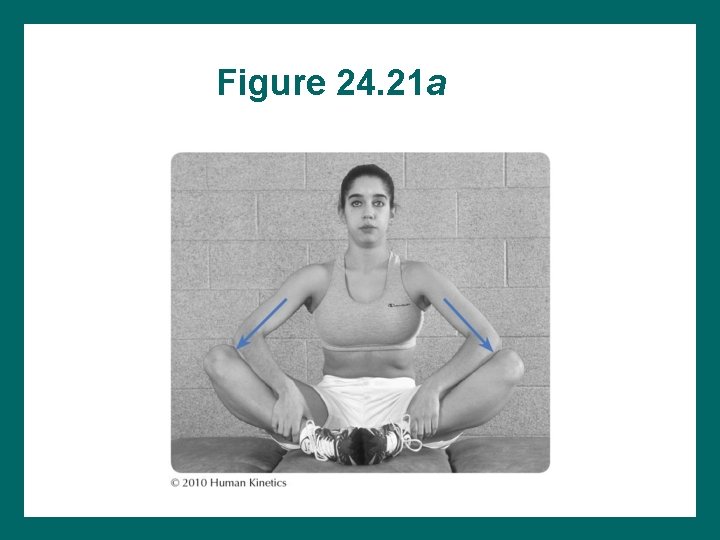
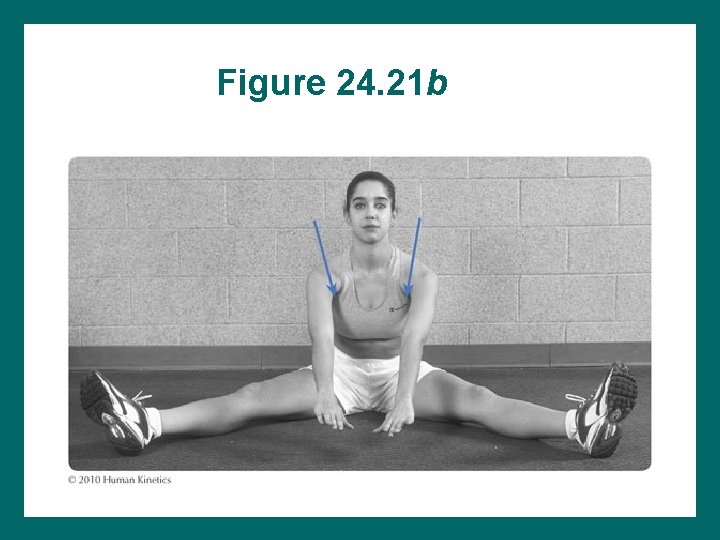
Figure 24. 21 a
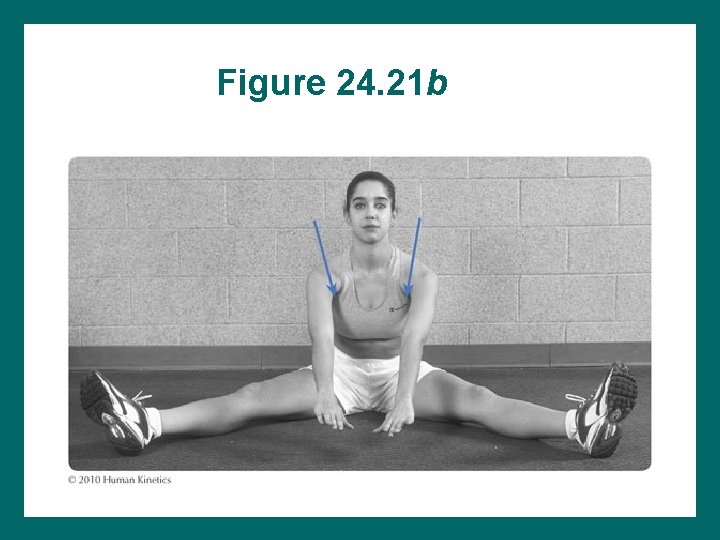
Figure 24. 21 b
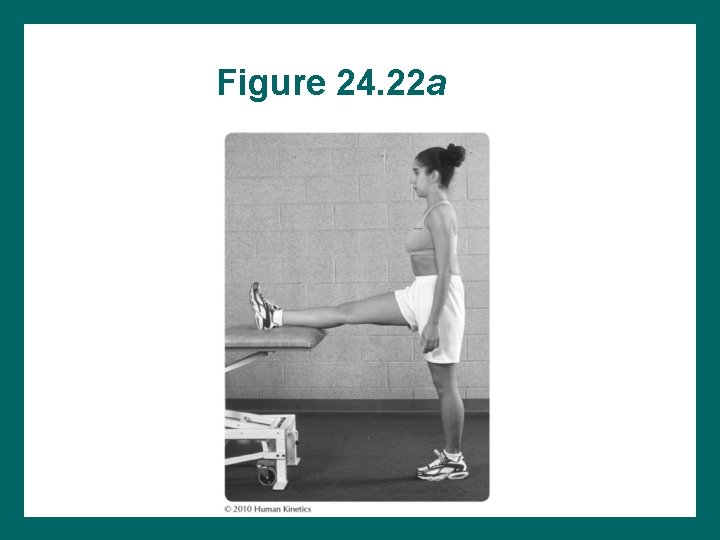
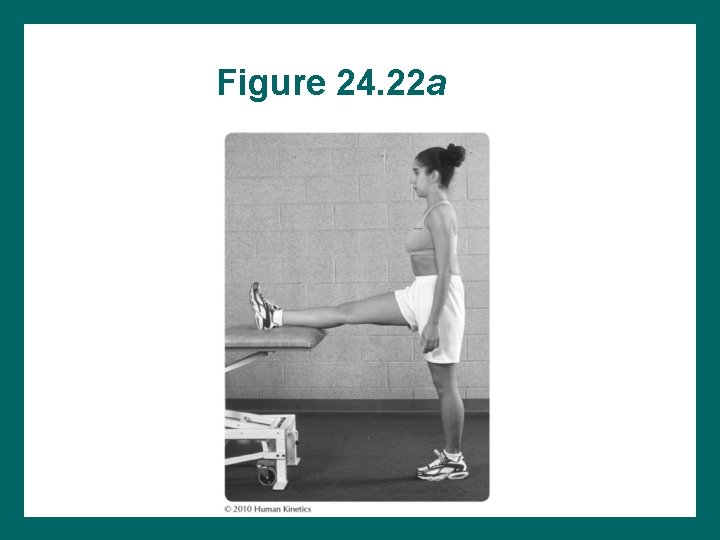
Figure 24. 22 a
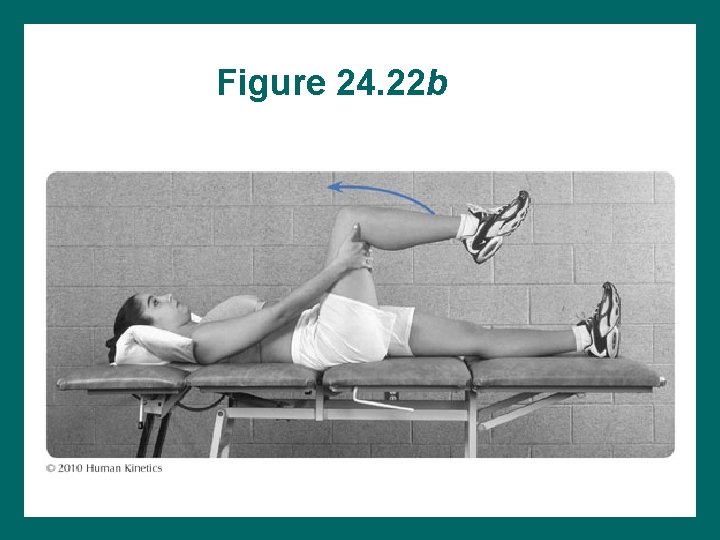
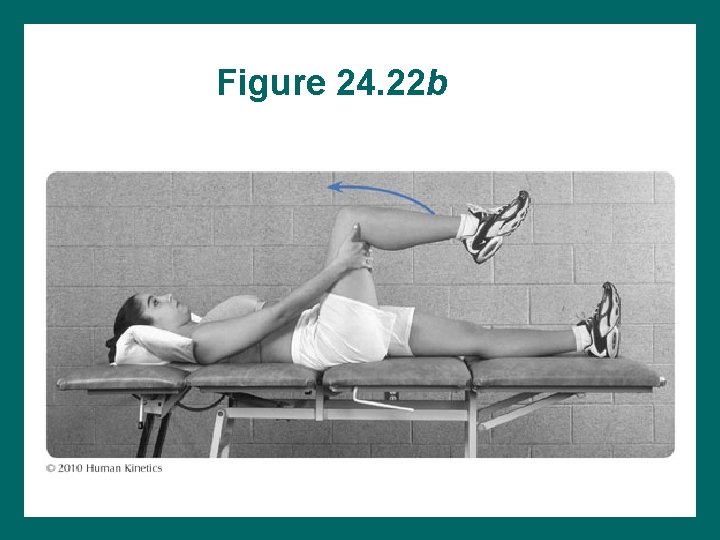
Figure 24. 22 b
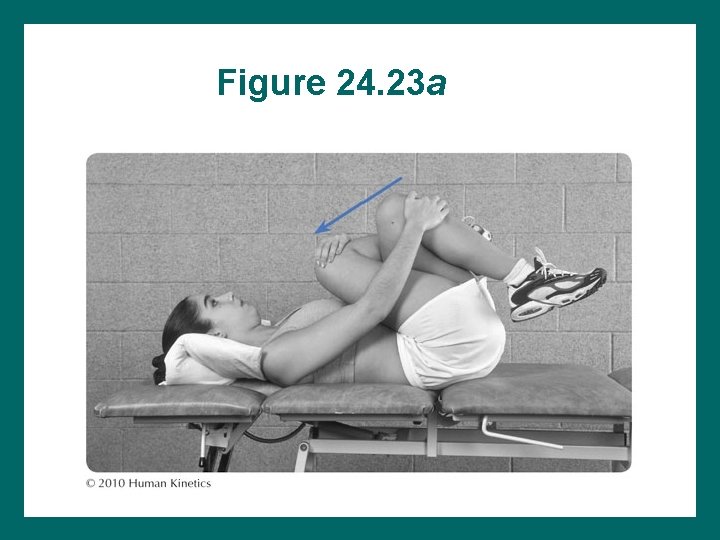
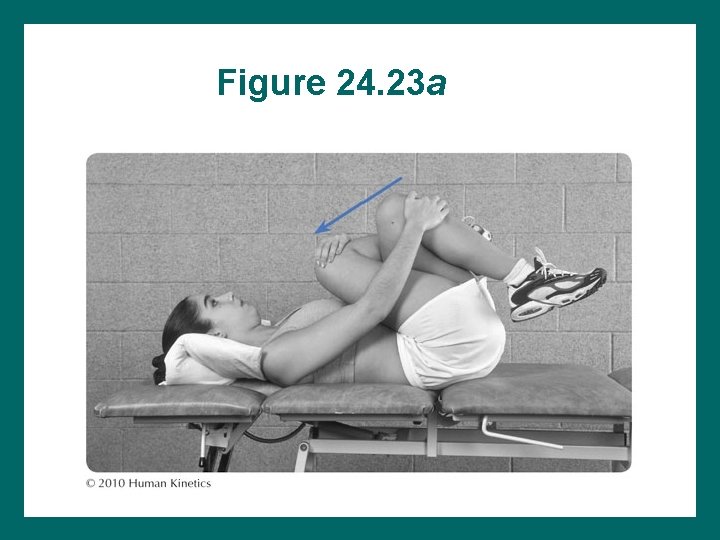
Figure 24. 23 a
Strengthening Exercises • Substitutions of other muscles occur easily in the hip and must be corrected. • Include exercises to strengthen trunk, knee, and ankle • Manual resistance and weight cuff resistance: applied anywhere along extremity
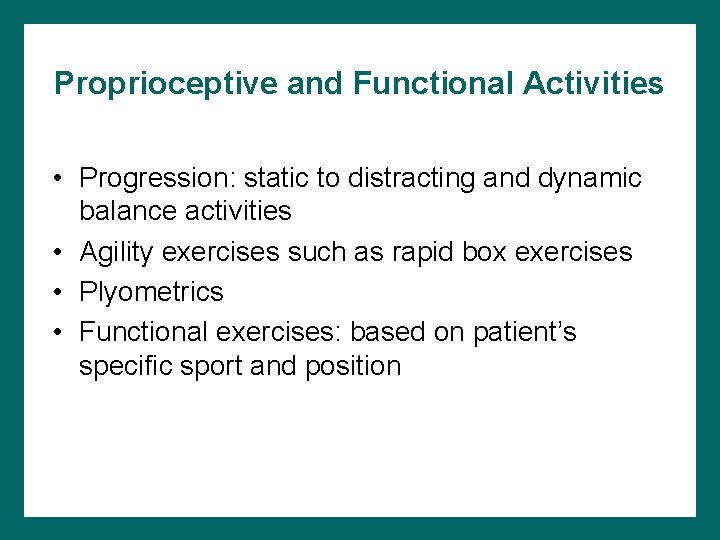
Proprioceptive and Functional Activities • Progression: static to distracting and dynamic balance activities • Agility exercises such as rapid box exercises • Plyometrics • Functional exercises: based on patient’s specific sport and position
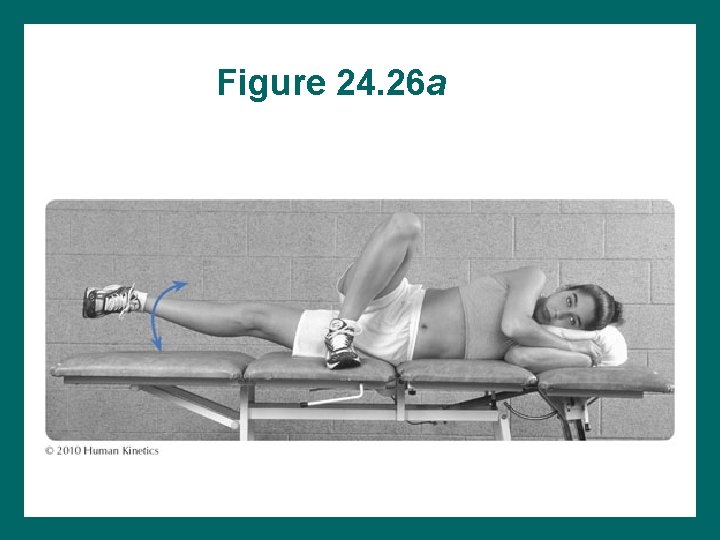
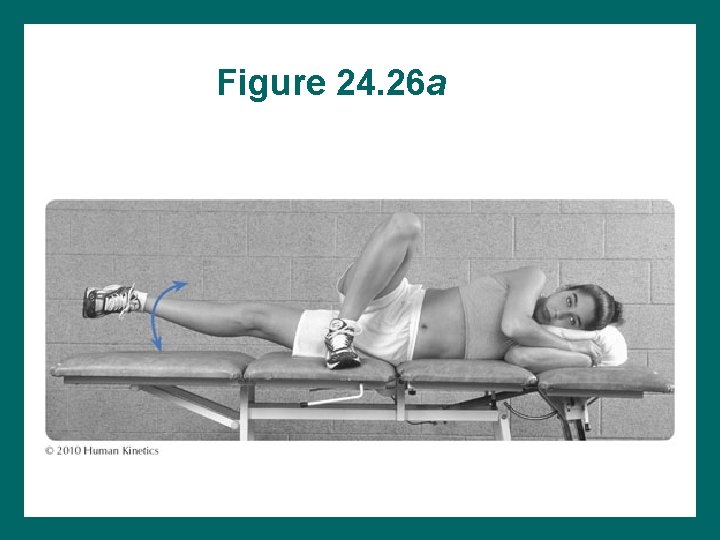
Figure 24. 26 a
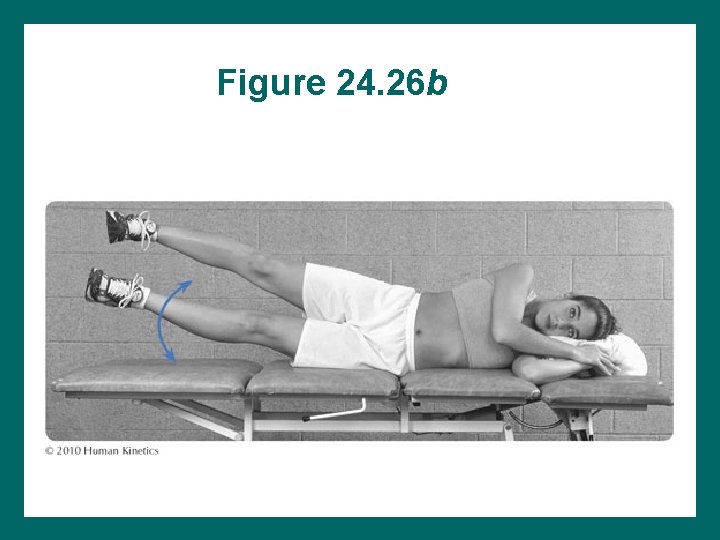
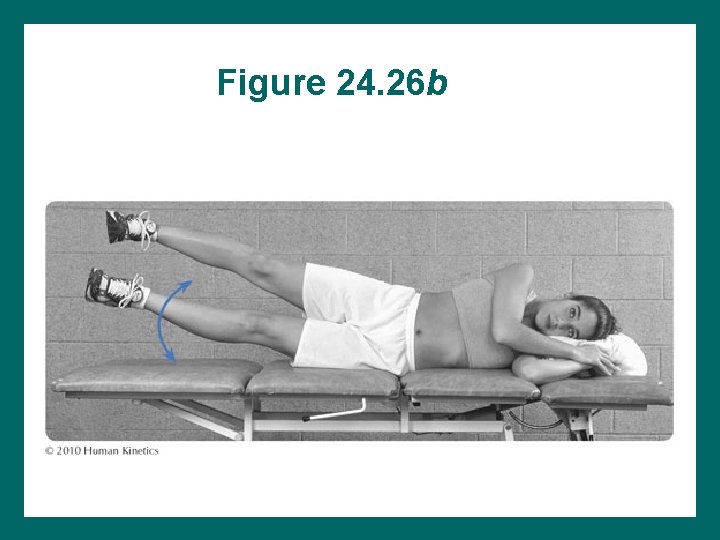
Figure 24. 26 b
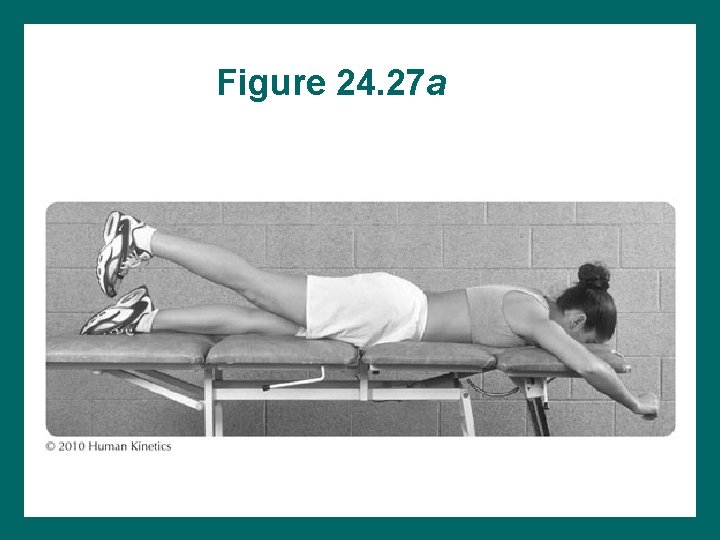
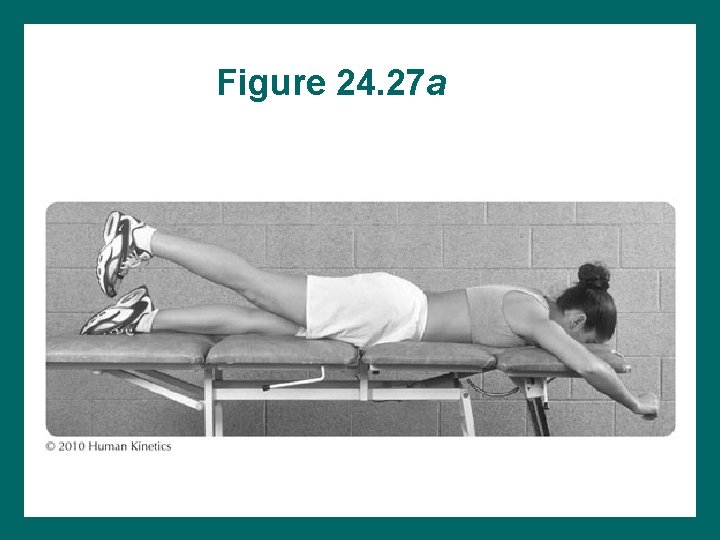
Figure 24. 27 a
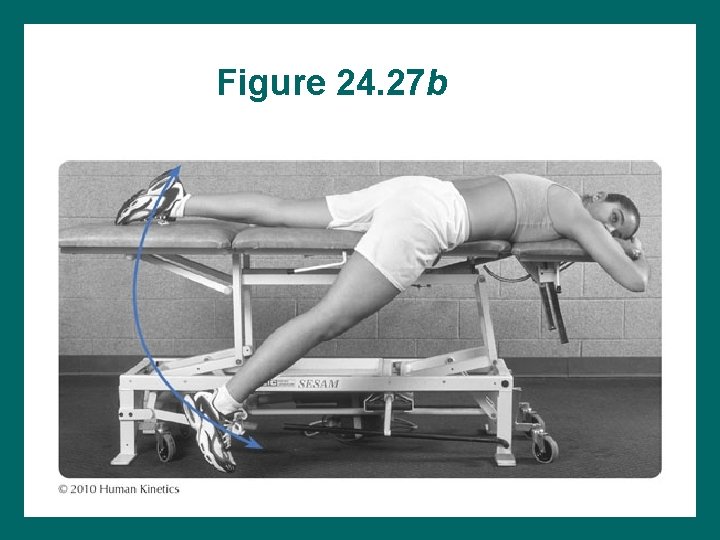
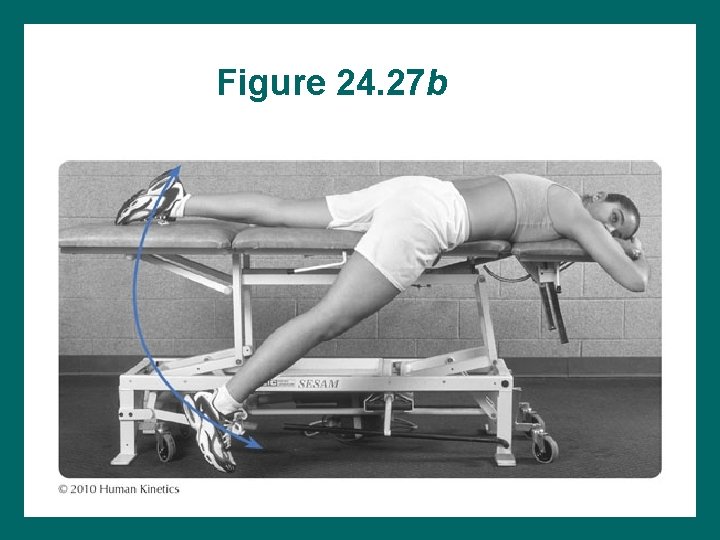
Figure 24. 27 b
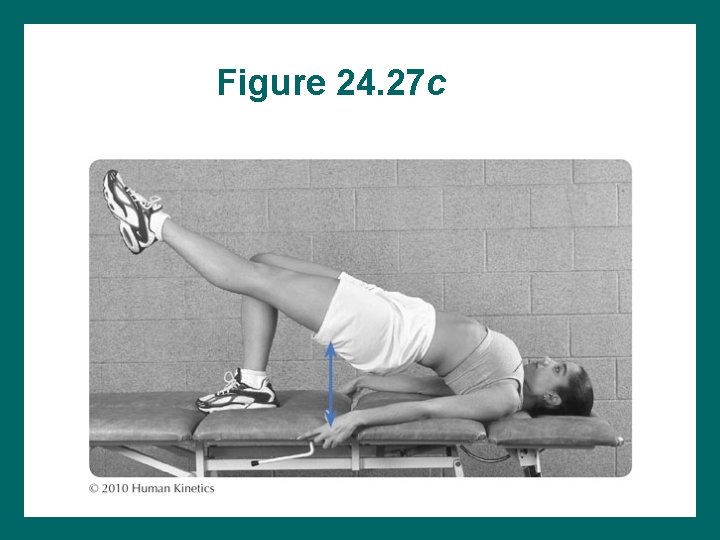
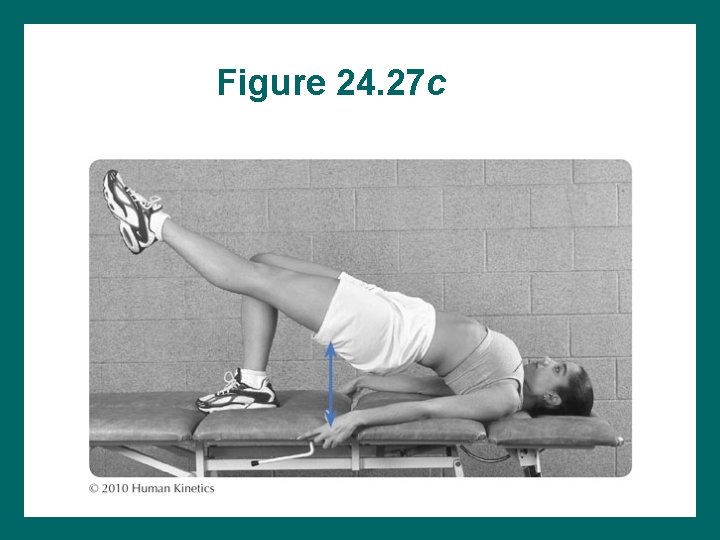
Figure 24. 27 c
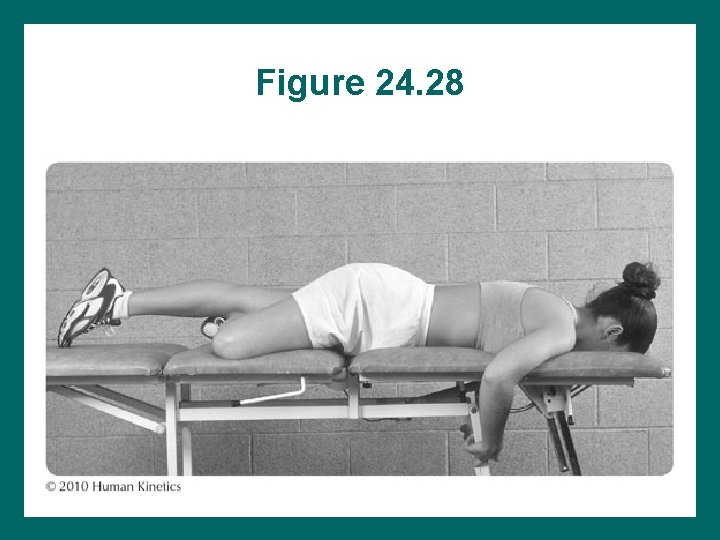
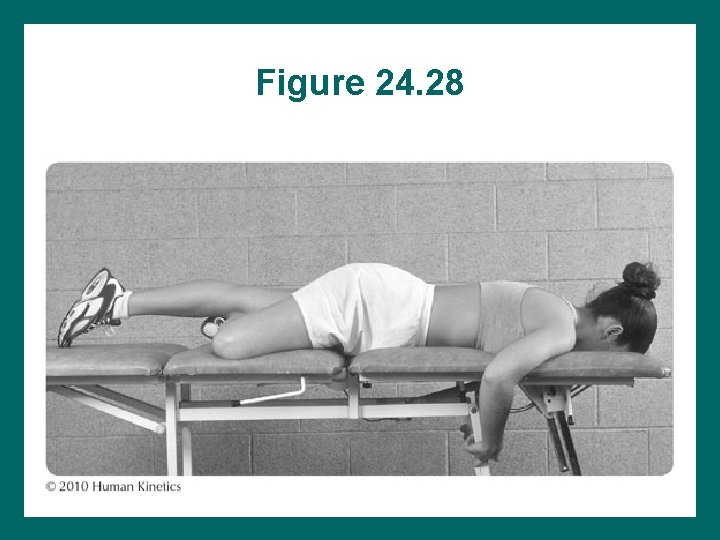
Figure 24. 28
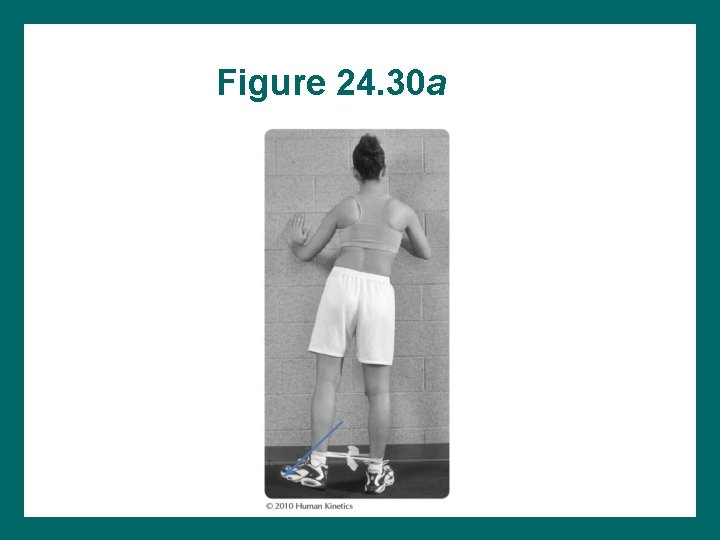
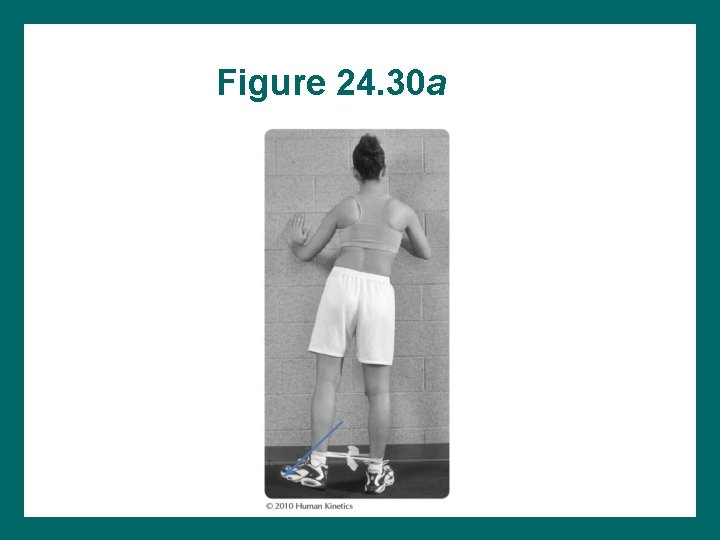
Figure 24. 30 a
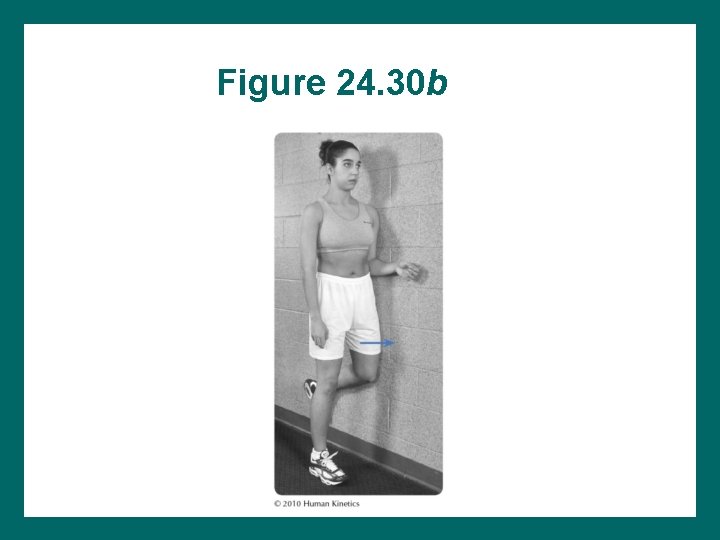
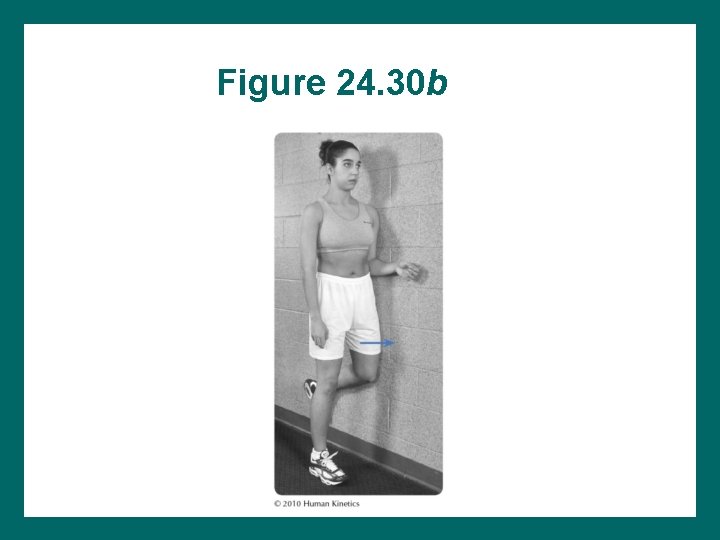
Figure 24. 30 b
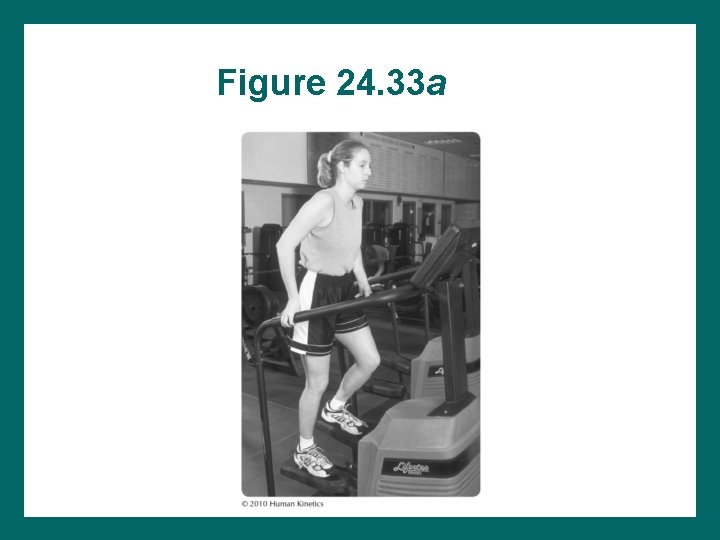
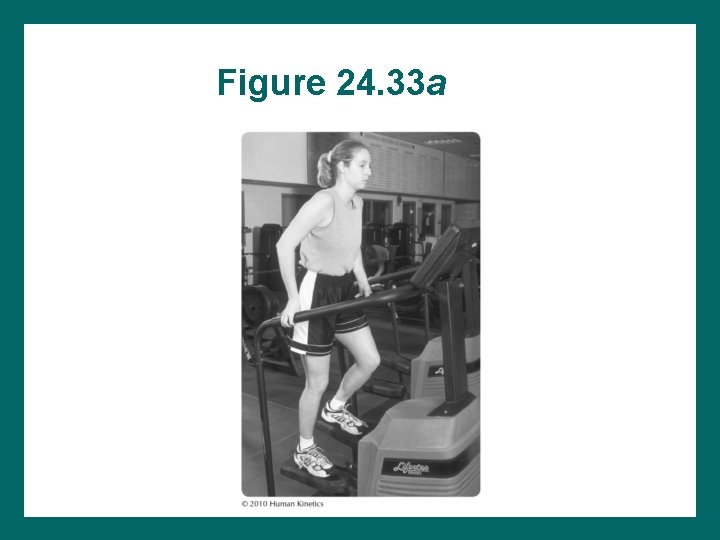
Figure 24. 33 a
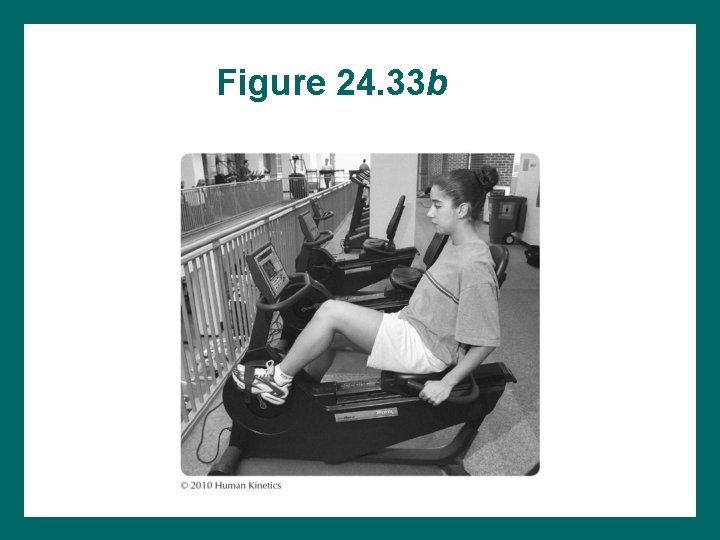
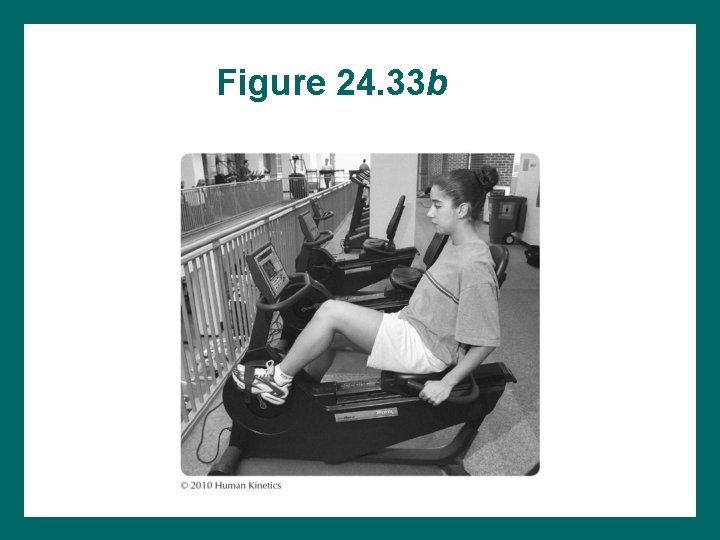
Figure 24. 33 b
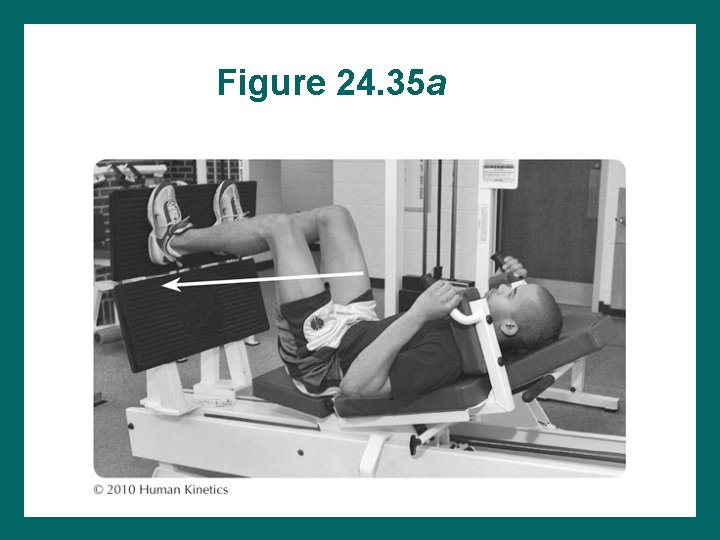
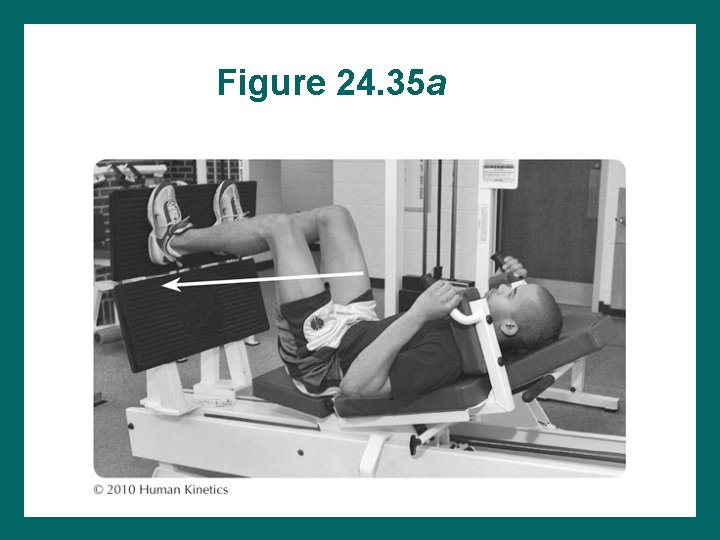
Figure 24. 35 a
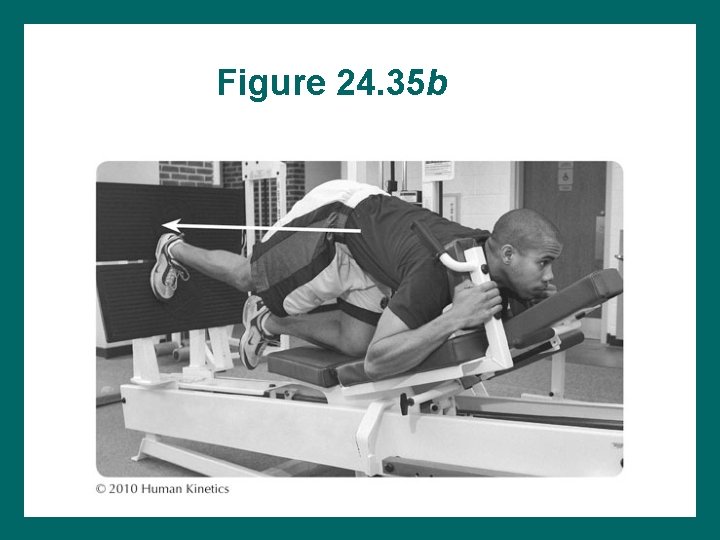
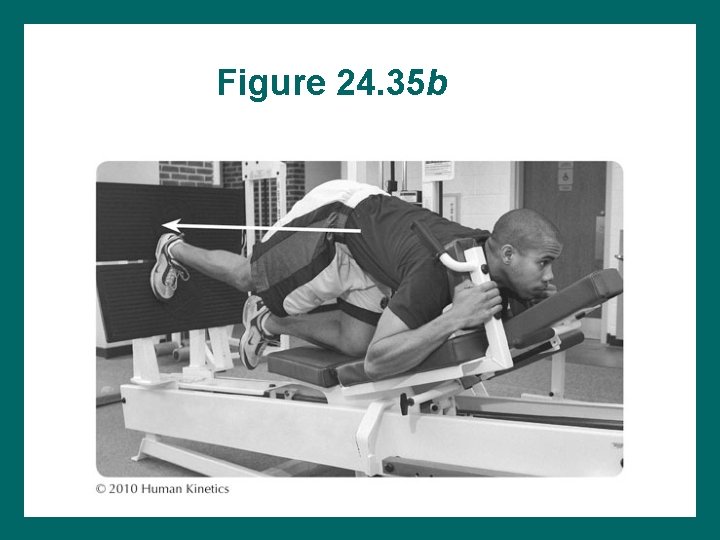
Figure 24. 35 b
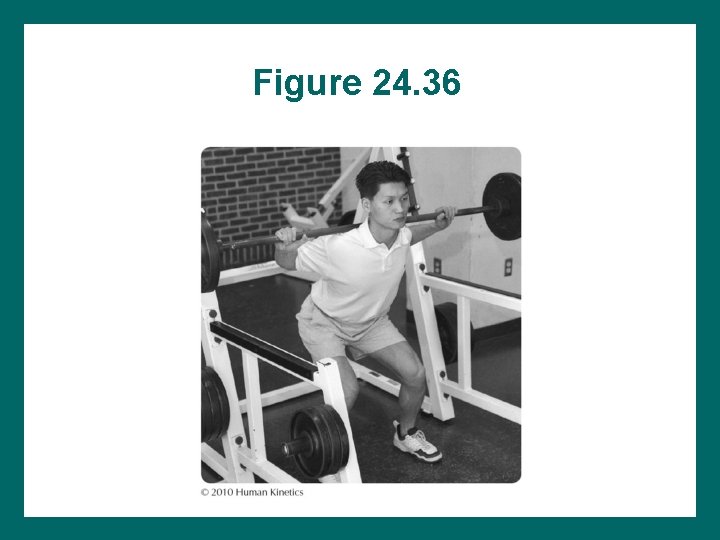
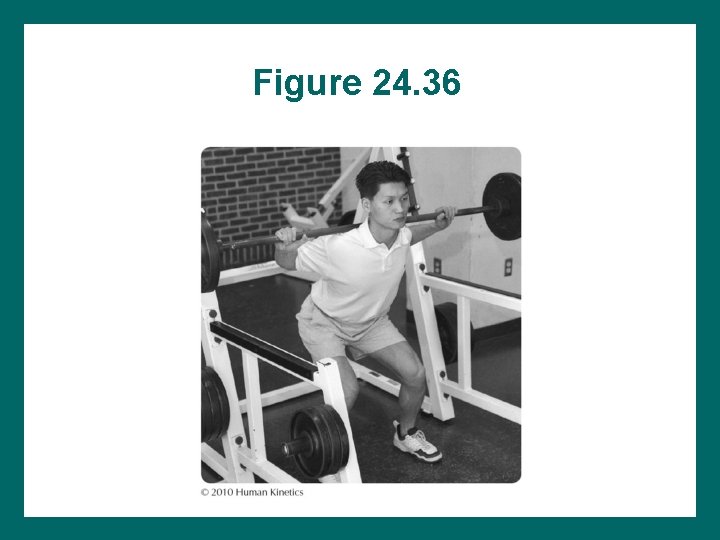
Figure 24. 36
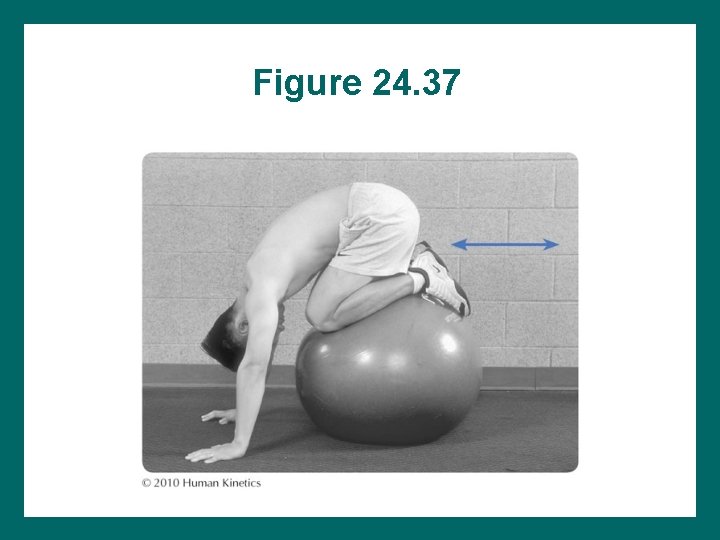
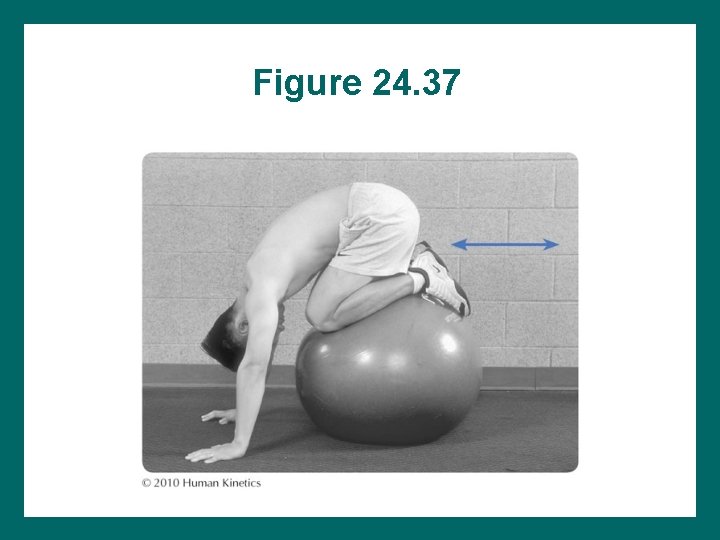
Figure 24. 37
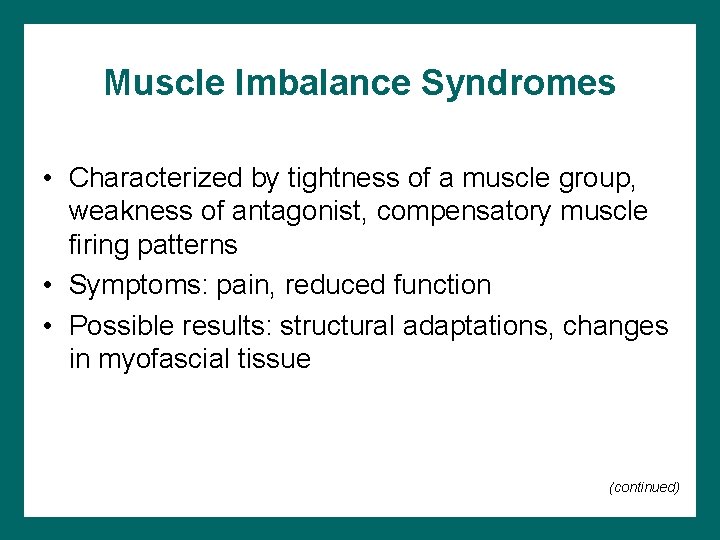
Muscle Imbalance Syndromes • Characterized by tightness of a muscle group, weakness of antagonist, compensatory muscle firing patterns • Symptoms: pain, reduced function • Possible results: structural adaptations, changes in myofascial tissue (continued)
Muscle Imbalance Syndromes (continued) Hip flexor tightness syndrome can lead to other pathology Normal muscle firing sequence in hip extension: 1. 2. 3. 4. 5. 6. hamstrings, gluteus maximus, contralateral lumbar spine, ipsilateral lumbar spine, contralateral thoracic spine, ipsilateral thoracic spine (not scapular muscles) (continued)
Muscle Imbalance Syndromes (continued) • Piriformis syndrome can occur from sacroilium dysfunction, leg-length discrepancies, other muscle imbalances, running on canted surface • What do you recommend for rehabilitation of this condition?
Acute Soft-Tissue Injuries • Contusions – Hip pointer = iliac crest – No rehab unless weakness is disabling – Injury is self-limiting • Groin strain: adductors, flexors—rehab may take a week to several weeks • Sprains: rare in sports—occur in extremes of ROM • What are your rehabilitation recommendations?
Chronic Conditions • Bursitis: can occur in several bursae – Trochanteric, ischiogluteal, iliopectineal – Rule out disc, facet, fracture, nerve, organs, hip joint disease, tumors if Rx is unsuccessful • Tendinopathy – Most often affects adductor longus, iliopsoas, rectus femoris – Causes: leg-length discrepancy, tightness, canted surfaces, poor mechanics, muscle imbalance, too much too soon (continued)
Chronic Conditions (continued) • Are self-limiting • Clicking: torn labrum • Correction of underlying causes must be included in treatment program • What would you do for rehabilitation?
Fractures and Dislocations • Dislocations rare in sport; seen in high-energy sports: medical emergency • Traumatic fractures: rare in sports • Stress fractures: more common • Slipped capital femoral epiphysis – = Growth plate fracture in adolescents – Limited IR, rests in ER – Groin pain • Pool activities = beneficial • What would you include in your rehabilitation?