Chapter 23 The Respiratory System Cells continually use
- Slides: 77
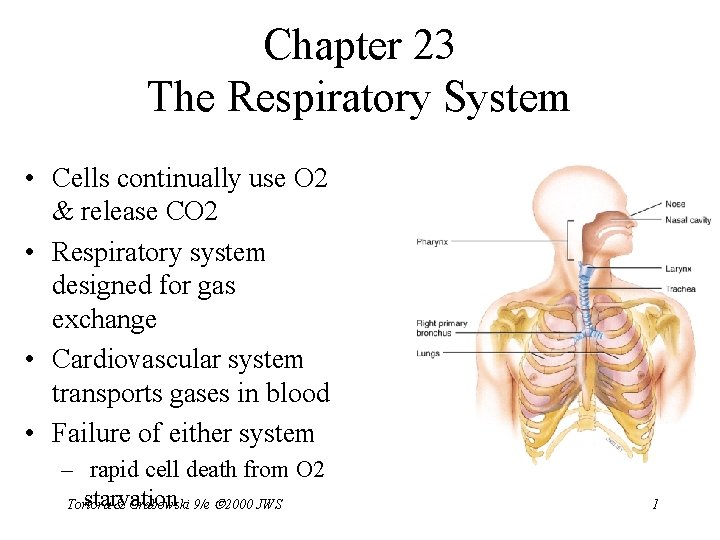
Chapter 23 The Respiratory System • Cells continually use O 2 & release CO 2 • Respiratory system designed for gas exchange • Cardiovascular system transports gases in blood • Failure of either system – rapid cell death from O 2 starvation Tortora & Grabowski 9/e 2000 JWS 1
Respiratory System Anatomy • • Nose Pharynx = throat Larynx = voicebox Trachea = windpipe Bronchi = airways Lungs Locations of infections – upper respiratory tract is above vocal cords – lower respiratory tract is below vocal cords Tortora & Grabowski 9/e 2000 JWS 2
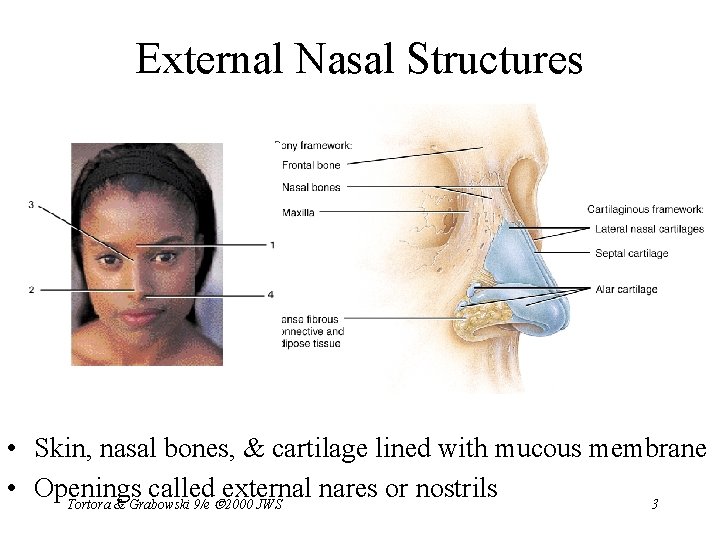
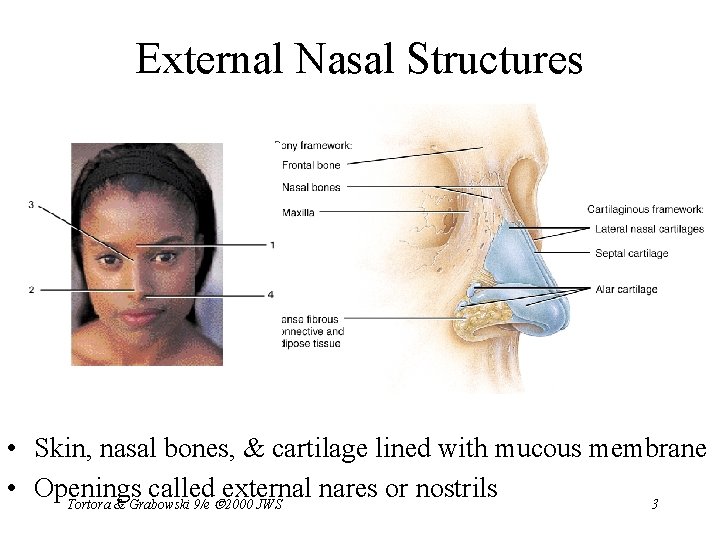
External Nasal Structures • Skin, nasal bones, & cartilage lined with mucous membrane • Openings called external nares or nostrils Tortora & Grabowski 9/e 2000 JWS 3
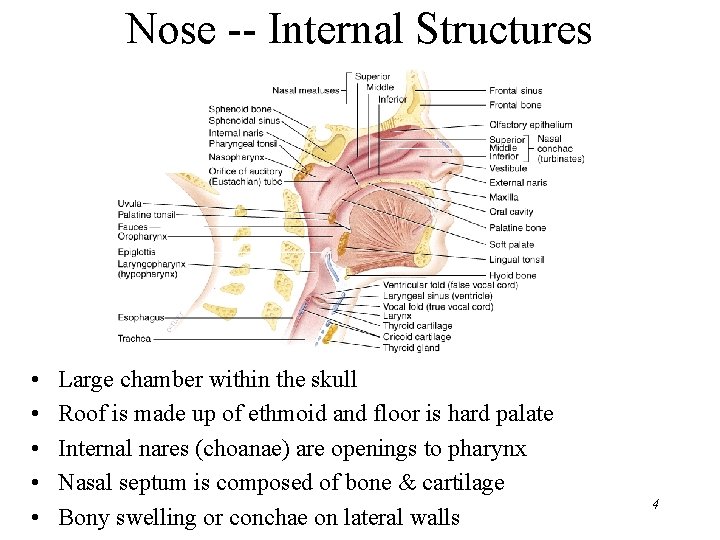
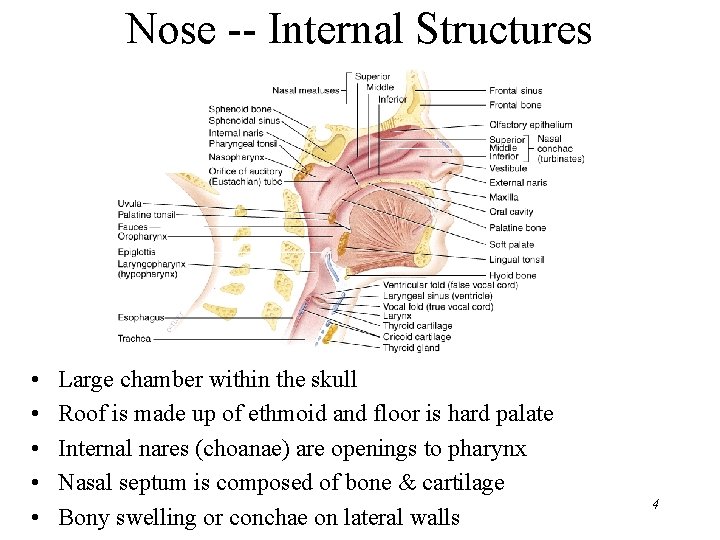
Nose -- Internal Structures • • • Large chamber within the skull Roof is made up of ethmoid and floor is hard palate Internal nares (choanae) are openings to pharynx Nasal septum is composed of bone & cartilage Bony swelling or conchae on lateral walls 4
Functions of the Nasal Structures • Olfactory epithelium for sense of smell • Pseudostratified ciliated columnar with goblet cells lines nasal cavity – warms air due to high vascularity – mucous moistens air & traps dust – cilia move mucous towards pharynx • Paranasal sinuses open into nasal cavity – found in ethmoid, sphenoid, frontal & maxillary – lighten skull & resonate voice Tortora & Grabowski 9/e 2000 JWS 5
Rhinoplasty • Commonly called a “nose job” • Surgical procedure done for cosmetic reasons / fracture or septal repair • Procedure – local and general anesthetic – nasal cartilage is reshaped through nostrils – bones fractured and repositioned – internal packing & splint while healing Tortora & Grabowski 9/e 2000 JWS 6
Pharynx • Muscular tube (5 inch long) hanging from skull – skeletal muscle & mucous membrane • Extends from internal nares to cricoid cartilage • Functions – passageway for food and air – resonating chamber for speech production – tonsil (lymphatic tissue) in the walls protects entryway into body Tortora & Grabowski 9/e 2000 JWS 7
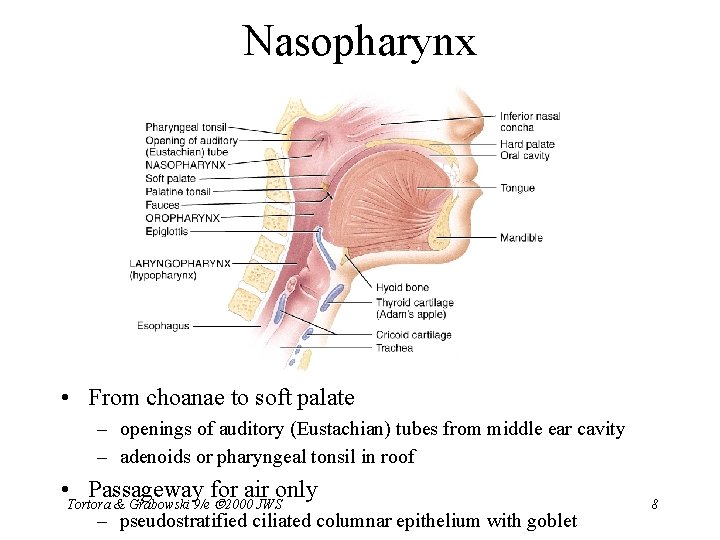
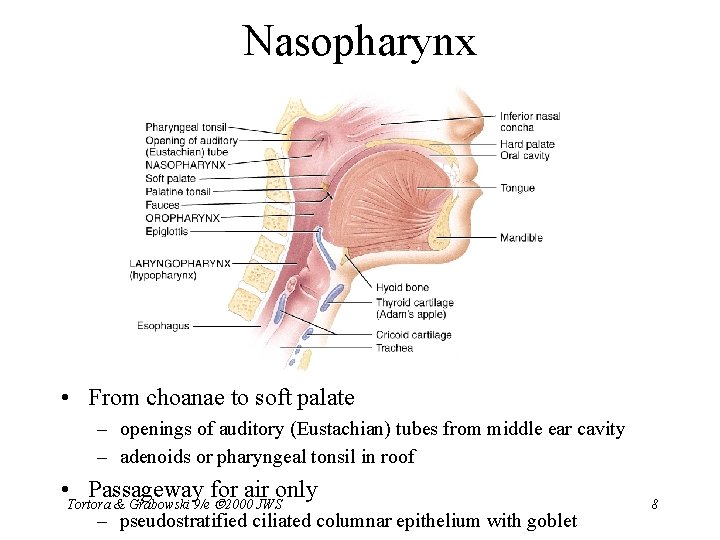
Nasopharynx • From choanae to soft palate – openings of auditory (Eustachian) tubes from middle ear cavity – adenoids or pharyngeal tonsil in roof • Tortora Passageway for air only & Grabowski 9/e 2000 JWS – pseudostratified ciliated columnar epithelium with goblet 8
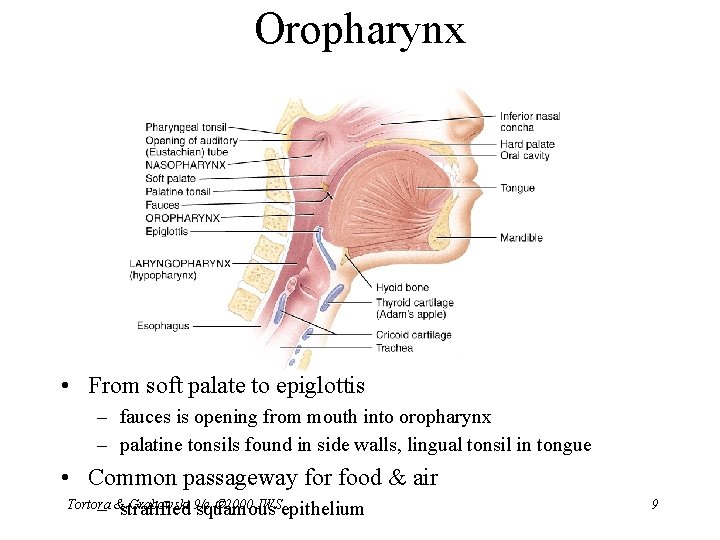
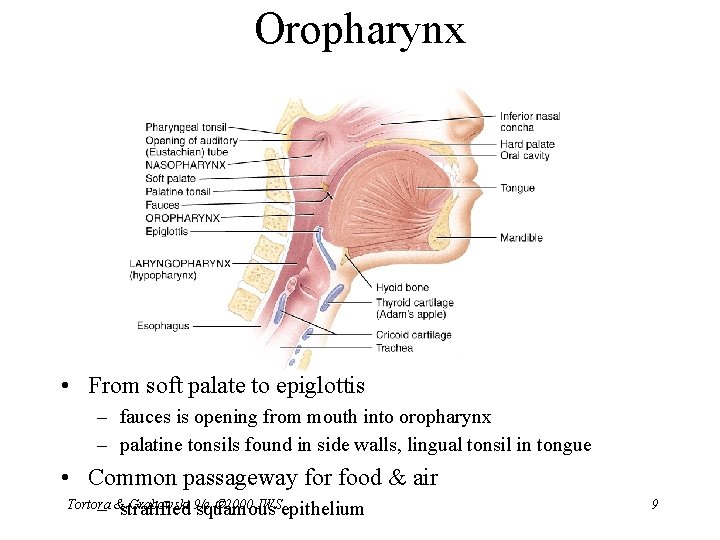
Oropharynx • From soft palate to epiglottis – fauces is opening from mouth into oropharynx – palatine tonsils found in side walls, lingual tonsil in tongue • Common passageway for food & air Tortora Grabowski 9/e 2000 JWSepithelium – &stratified squamous 9
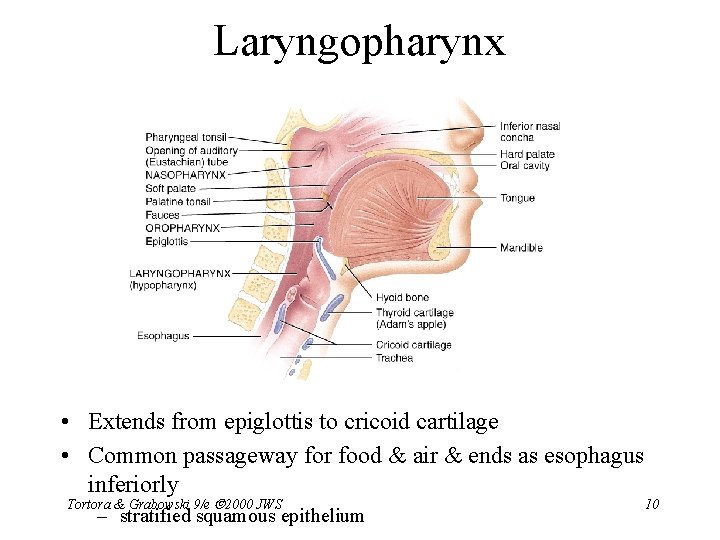
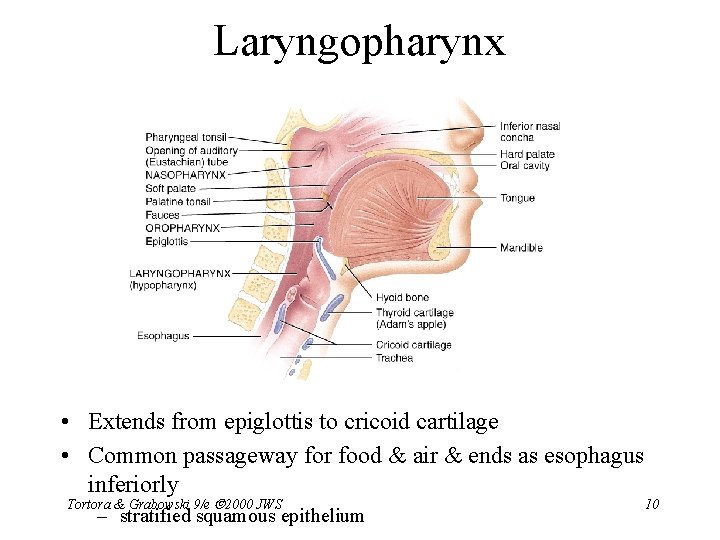
Laryngopharynx • Extends from epiglottis to cricoid cartilage • Common passageway for food & air & ends as esophagus inferiorly Tortora & Grabowski 9/e 2000 JWS – stratified squamous epithelium 10
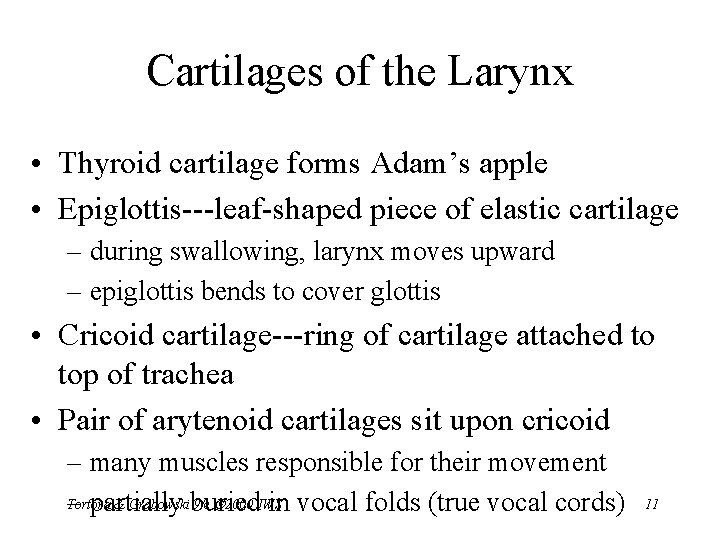
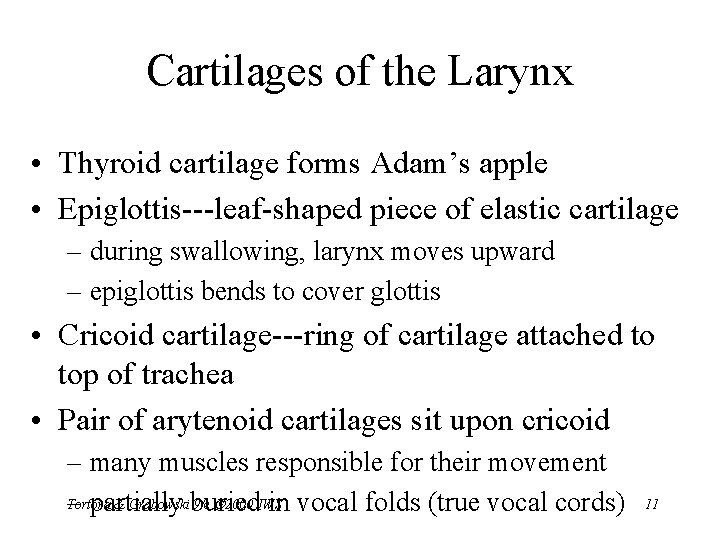
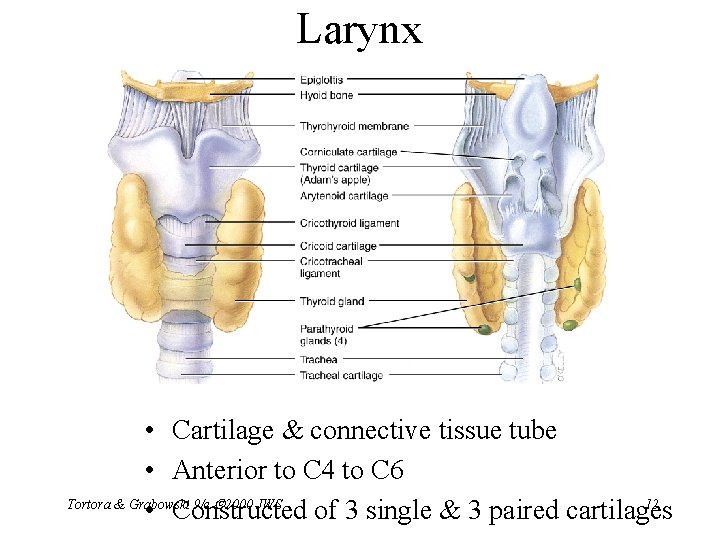
Cartilages of the Larynx • Thyroid cartilage forms Adam’s apple • Epiglottis---leaf-shaped piece of elastic cartilage – during swallowing, larynx moves upward – epiglottis bends to cover glottis • Cricoid cartilage---ring of cartilage attached to top of trachea • Pair of arytenoid cartilages sit upon cricoid – many muscles responsible for their movement Tortora & Grabowskiburied 9/e 2000 JWS – partially in vocal folds (true vocal cords) 11
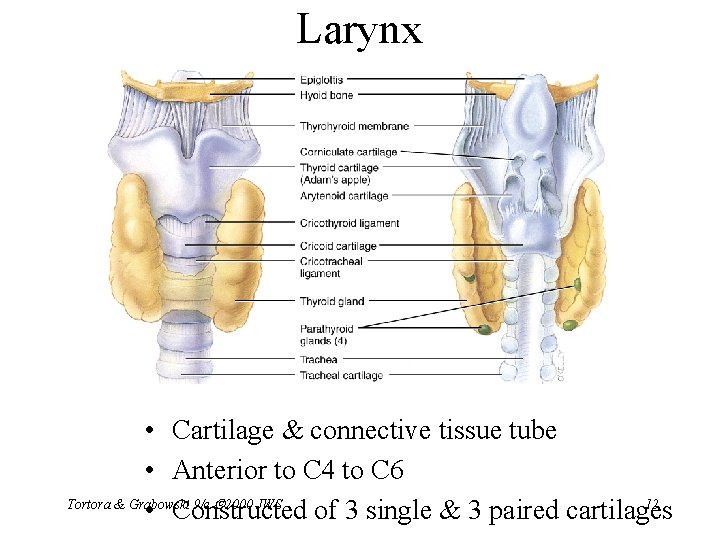
Larynx • Cartilage & connective tissue tube • Anterior to C 4 to C 6 Tortora & Grabowski 9/e 2000 JWS 12 • Constructed of 3 single & 3 paired cartilages
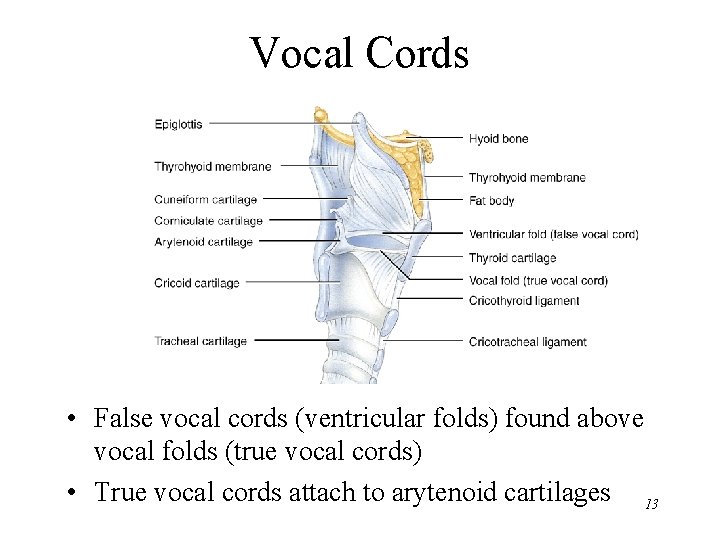
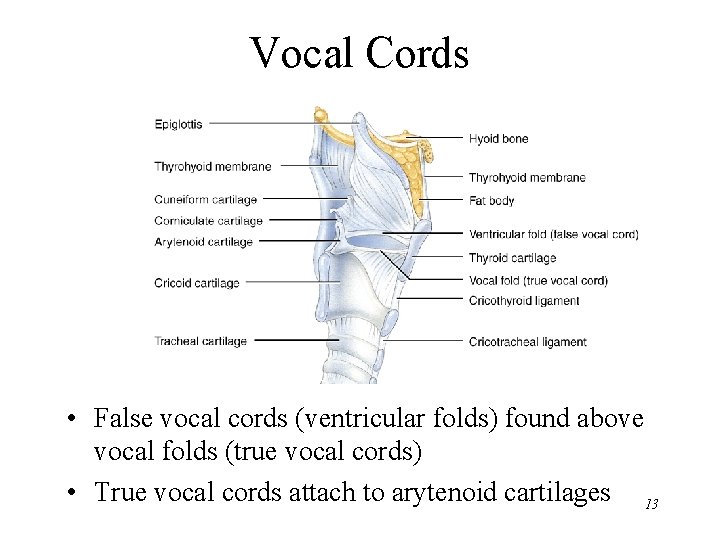
Vocal Cords • False vocal cords (ventricular folds) found above vocal folds (true vocal cords) • True vocal cords attach to arytenoid cartilages 13
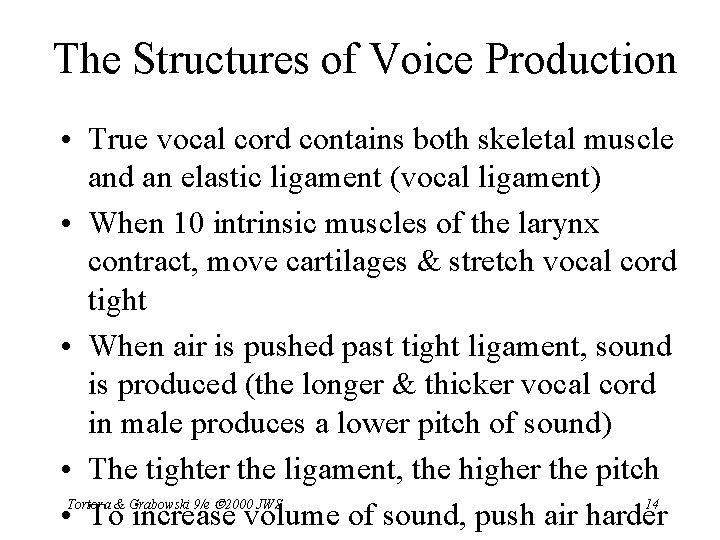
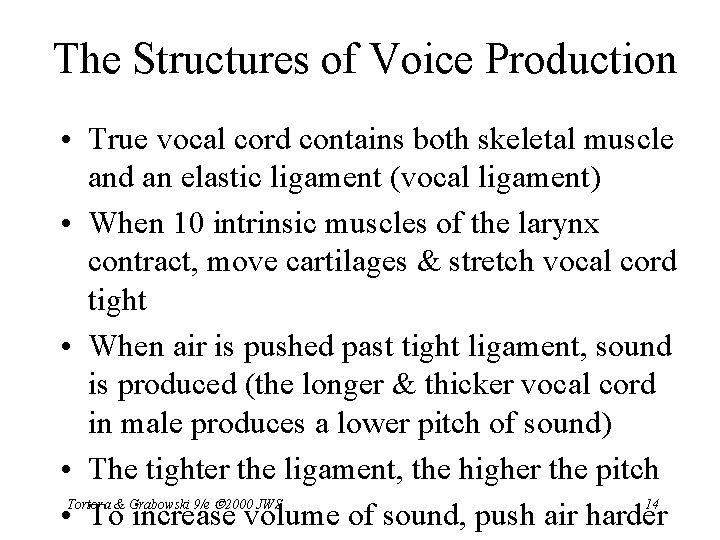
The Structures of Voice Production • True vocal cord contains both skeletal muscle and an elastic ligament (vocal ligament) • When 10 intrinsic muscles of the larynx contract, move cartilages & stretch vocal cord tight • When air is pushed past tight ligament, sound is produced (the longer & thicker vocal cord in male produces a lower pitch of sound) • The tighter the ligament, the higher the pitch Tortora & Grabowski 9/e 2000 JWS 14 • To increase volume of sound, push air harder
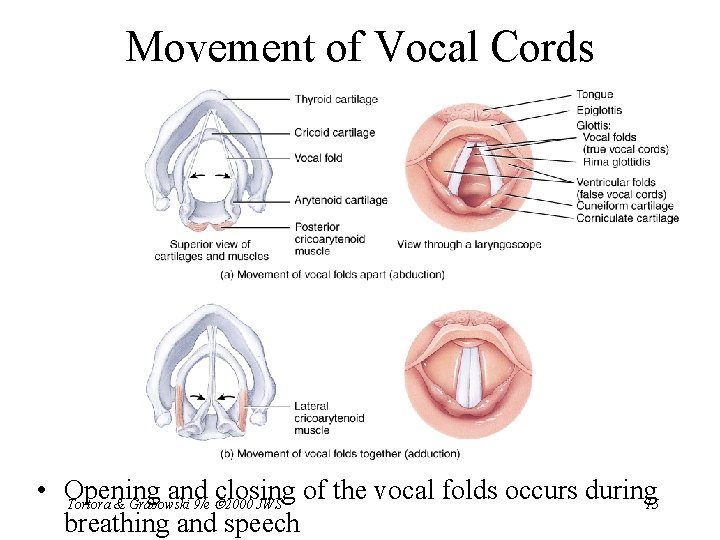
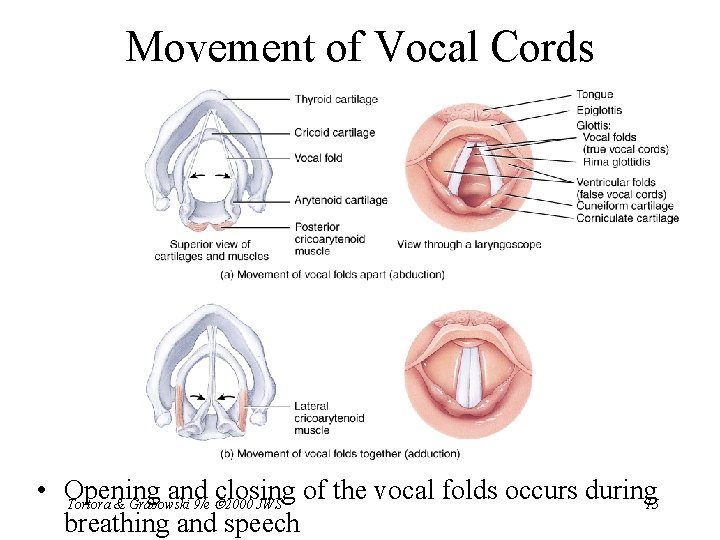
Movement of Vocal Cords • Opening and closing of the vocal folds occurs during 15 Tortora & Grabowski 9/e 2000 JWS breathing and speech
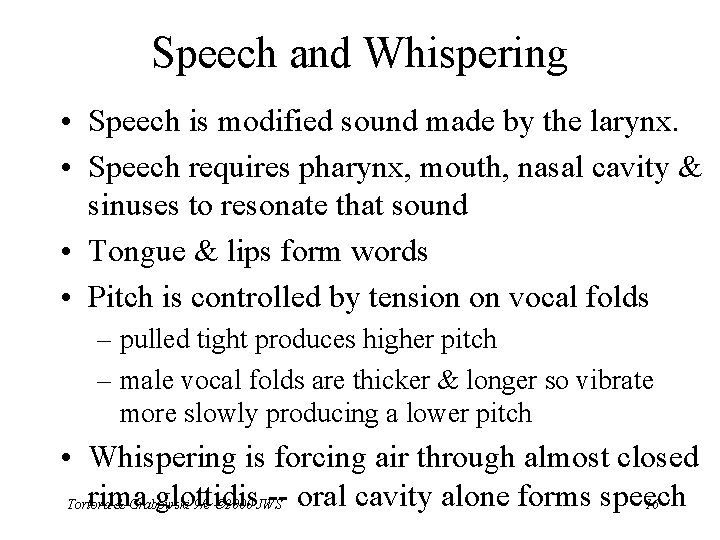
Speech and Whispering • Speech is modified sound made by the larynx. • Speech requires pharynx, mouth, nasal cavity & sinuses to resonate that sound • Tongue & lips form words • Pitch is controlled by tension on vocal folds – pulled tight produces higher pitch – male vocal folds are thicker & longer so vibrate more slowly producing a lower pitch • Whispering is forcing air through almost closed rima glottidis -- oral cavity alone forms speech Tortora & Grabowski 9/e 2000 JWS 16
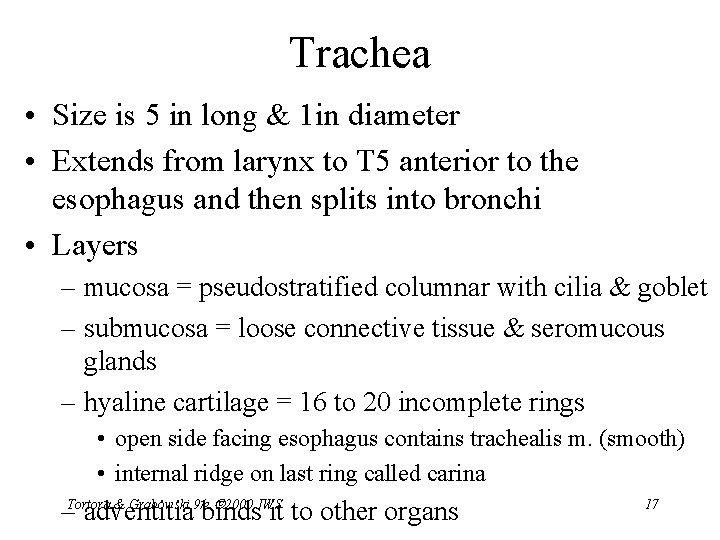
Trachea • Size is 5 in long & 1 in diameter • Extends from larynx to T 5 anterior to the esophagus and then splits into bronchi • Layers – mucosa = pseudostratified columnar with cilia & goblet – submucosa = loose connective tissue & seromucous glands – hyaline cartilage = 16 to 20 incomplete rings • open side facing esophagus contains trachealis m. (smooth) • internal ridge on last ring called carina & Grabowski 9/e 2000 JWS –Tortora adventitia binds it to other organs 17
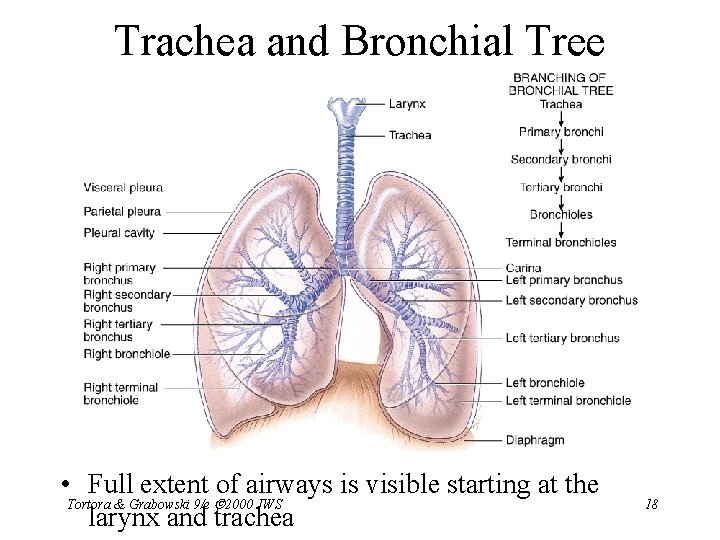
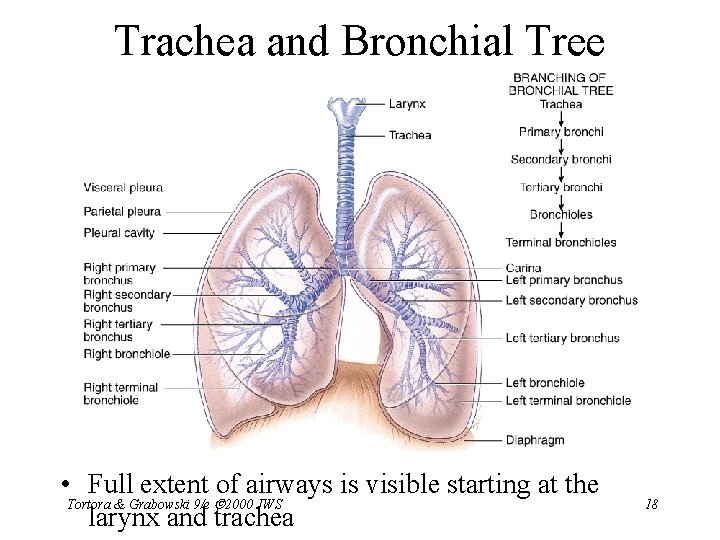
Trachea and Bronchial Tree • Full extent of airways is visible starting at the Tortora & Grabowski 9/e 2000 JWS larynx and trachea 18
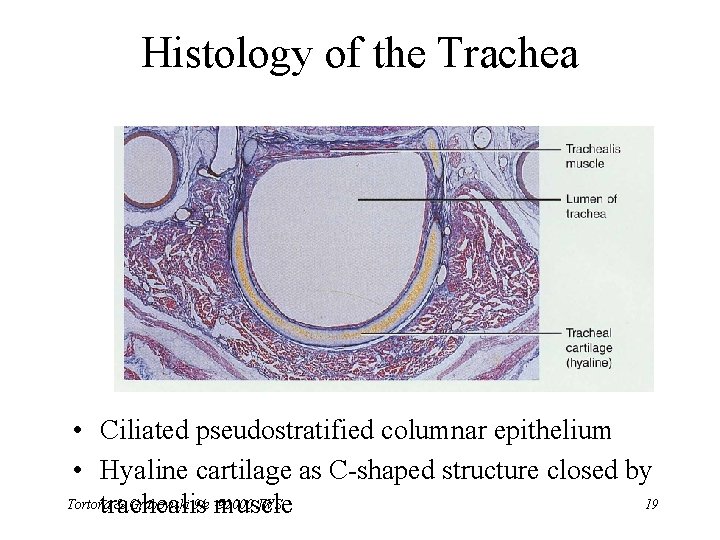
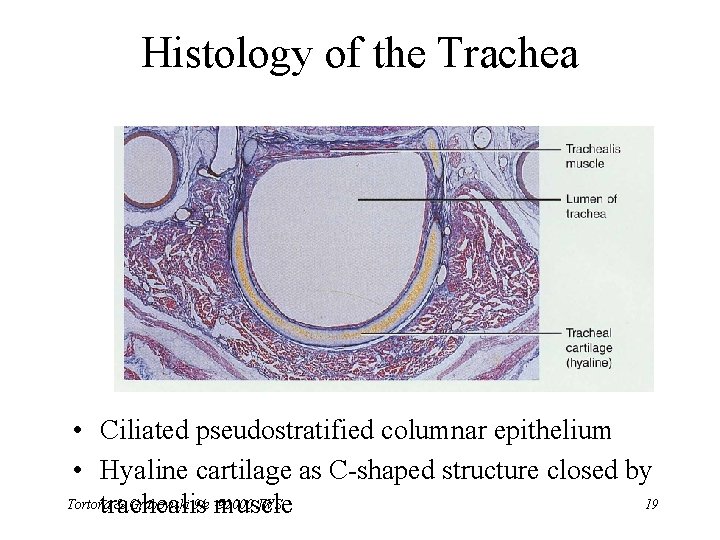
Histology of the Trachea • Ciliated pseudostratified columnar epithelium • Hyaline cartilage as C-shaped structure closed by Tortora & Grabowski 9/e 2000 JWS 19 trachealis muscle
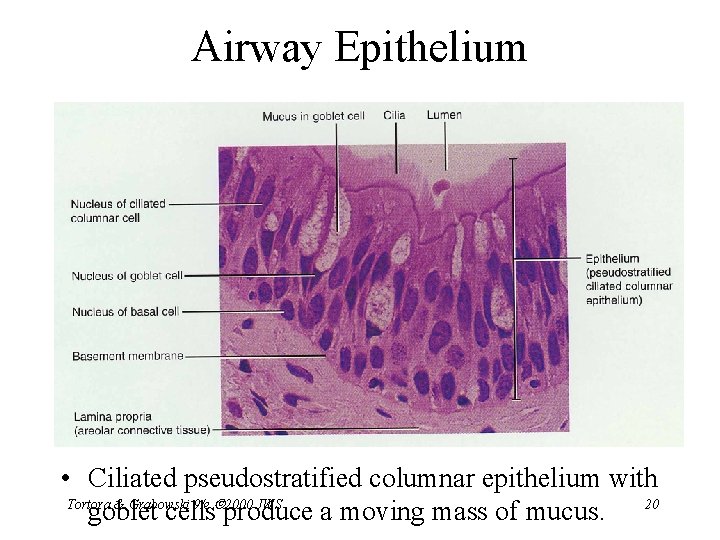
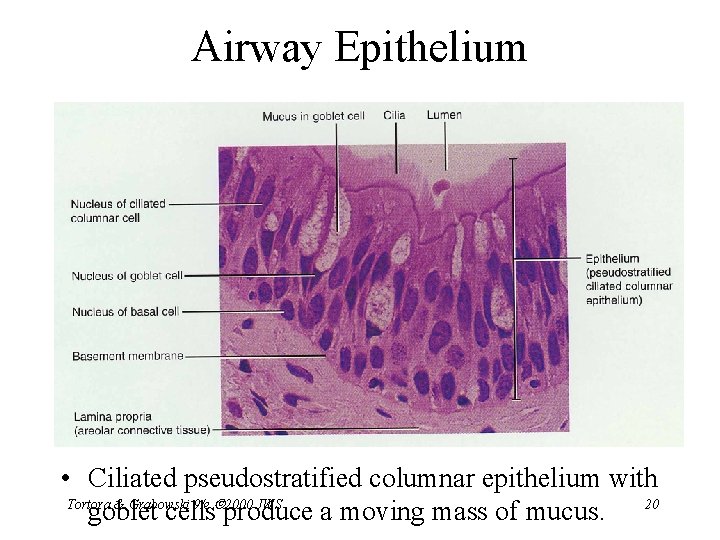
Airway Epithelium • Ciliated pseudostratified columnar epithelium with Tortora & Grabowski 9/e 2000 JWS goblet cells produce a moving mass of mucus. 20
Tracheostomy and Intubation • Reestablishing airflow past an airway obstruction – crushing injury to larynx or chest – swelling that closes airway – vomit or foreign object • Tracheostomy is incision in trachea below cricoid cartilage if larynx is obstructed • Intubation is passing a tube from mouth or nose through larynx and trachea Tortora & Grabowski 9/e 2000 JWS 21
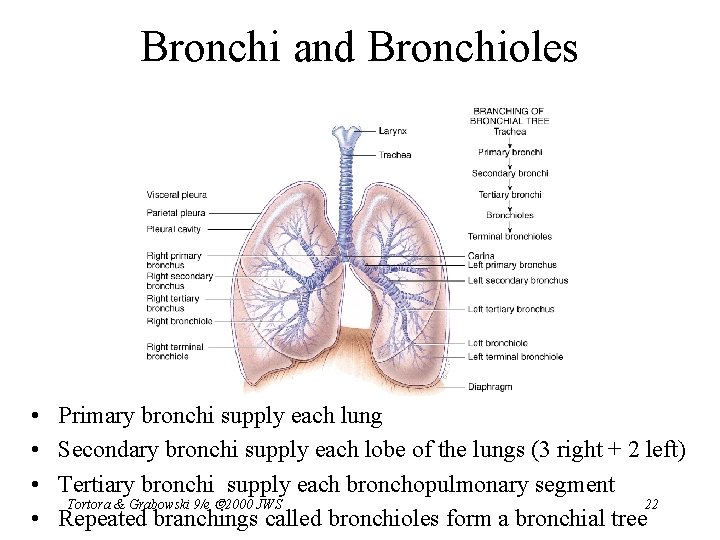
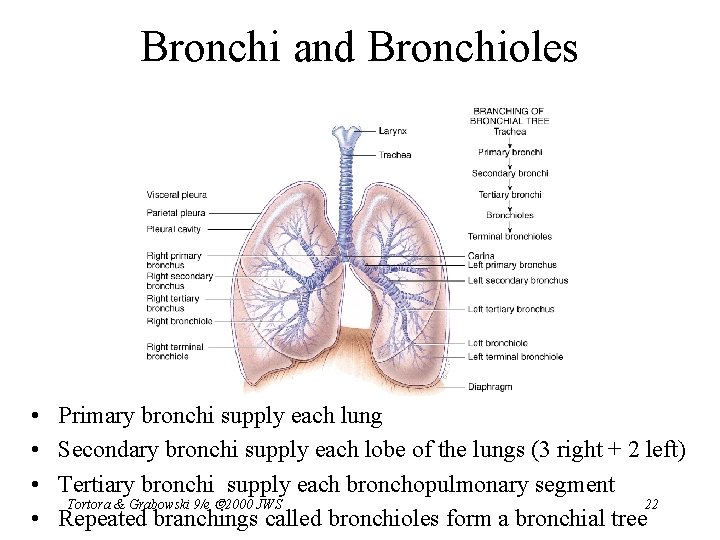
Bronchi and Bronchioles • • Primary bronchi supply each lung Secondary bronchi supply each lobe of the lungs (3 right + 2 left) Tertiary bronchi supply each bronchopulmonary segment Tortora & Grabowski 9/e 2000 JWS 22 Repeated branchings called bronchioles form a bronchial tree
Histology of Bronchial Tree • Epithelium changes from pseudostratified ciliated columnar to nonciliated simple cuboidal as pass deeper into lungs • Incomplete rings of cartilage replaced by rings of smooth muscle & then connective tissue – sympathetic NS & adrenal gland release epinephrine that relaxes smooth muscle & dilates airways – asthma attack or allergic reactions constrict distal bronchiole smooth muscle – nebulization therapy = inhale mist with chemicals that Tortora & Grabowski 9/e 2000 JWS 23 relax muscle & reduce thickness of mucus
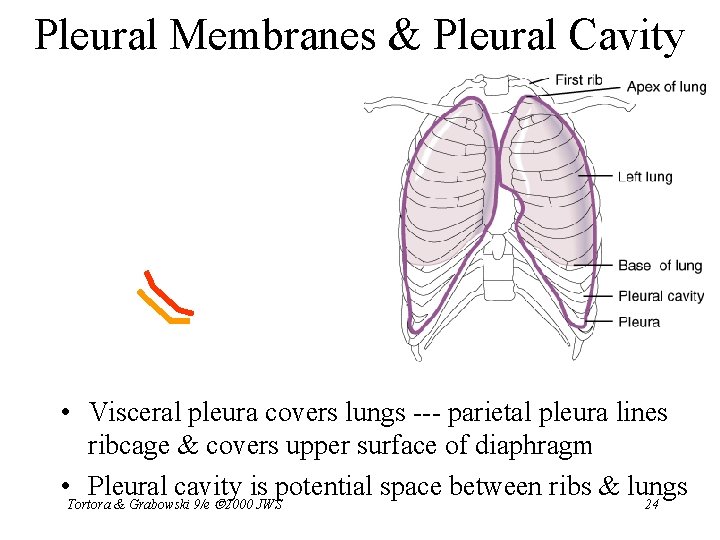
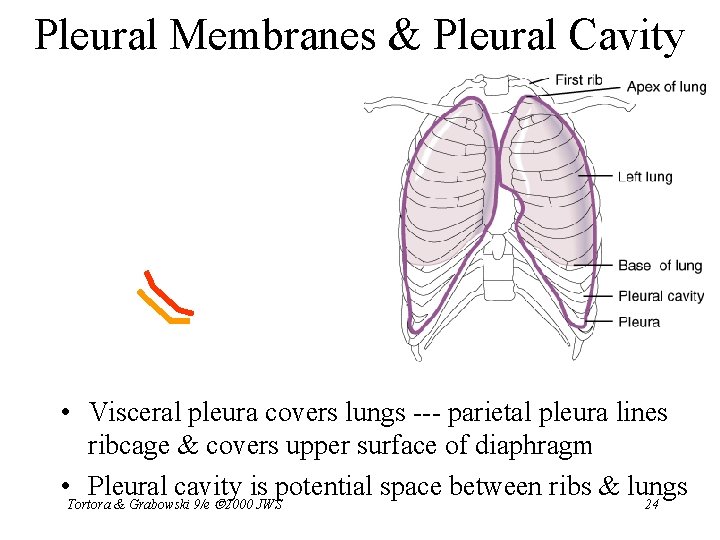
Pleural Membranes & Pleural Cavity • Visceral pleura covers lungs --- parietal pleura lines ribcage & covers upper surface of diaphragm • Pleural cavity is potential space between ribs & lungs Tortora & Grabowski 9/e 2000 JWS 24
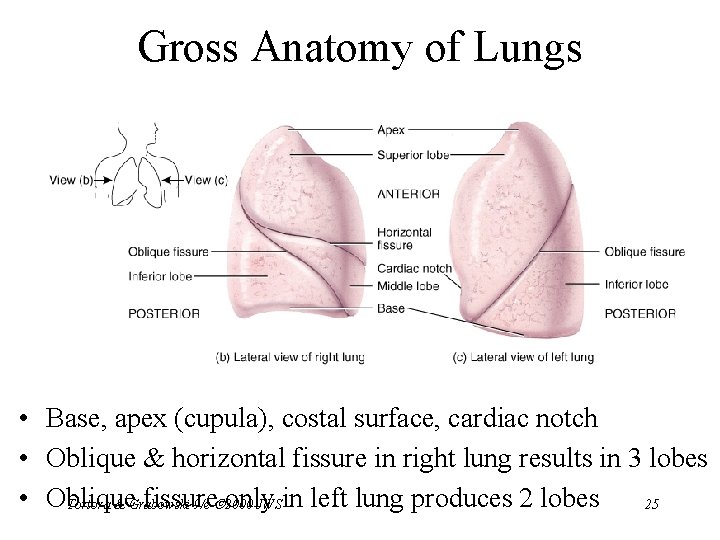
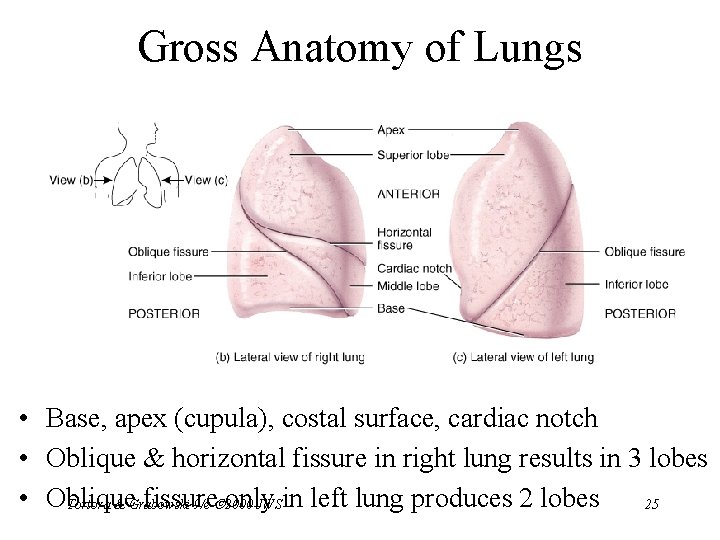
Gross Anatomy of Lungs • Base, apex (cupula), costal surface, cardiac notch • Oblique & horizontal fissure in right lung results in 3 lobes • Oblique fissure Tortora & Grabowski 9/e only 2000 JWSin left lung produces 2 lobes 25
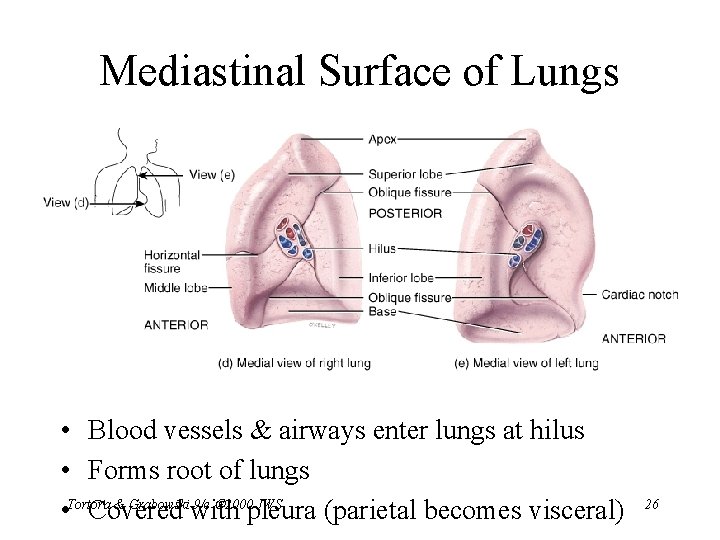
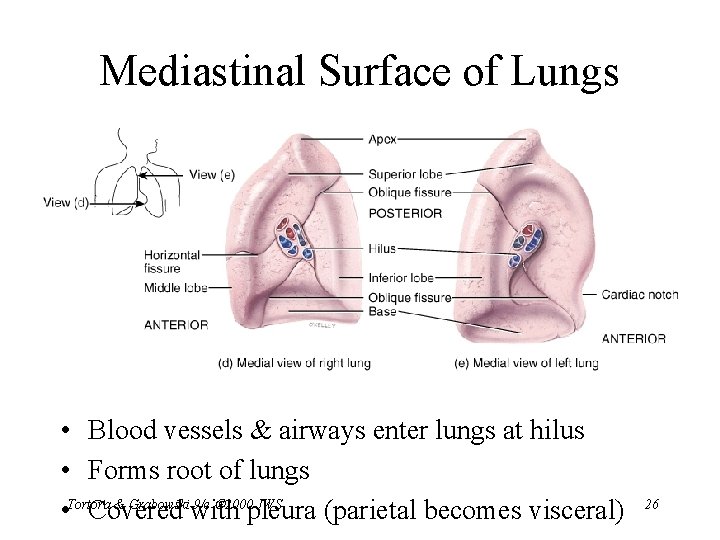
Mediastinal Surface of Lungs • Blood vessels & airways enter lungs at hilus • Forms root of lungs & Grabowski 9/e 2000 JWS • Tortora Covered with pleura (parietal becomes visceral) 26
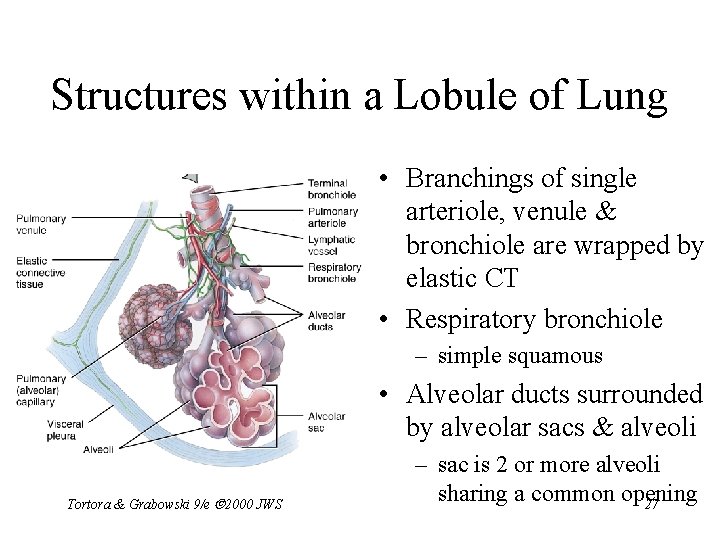
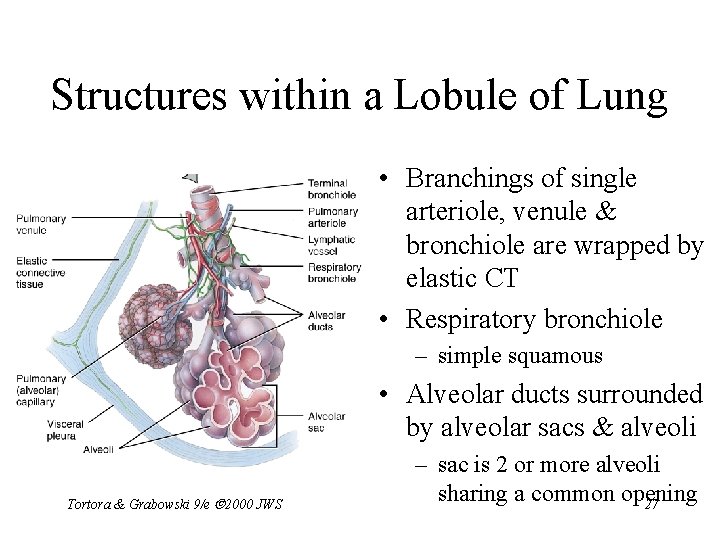
Structures within a Lobule of Lung • Branchings of single arteriole, venule & bronchiole are wrapped by elastic CT • Respiratory bronchiole – simple squamous • Alveolar ducts surrounded by alveolar sacs & alveoli Tortora & Grabowski 9/e 2000 JWS – sac is 2 or more alveoli sharing a common opening 27
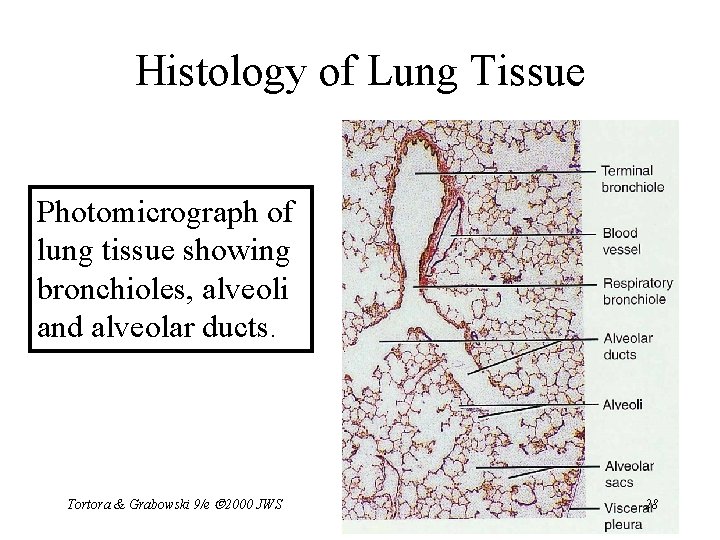
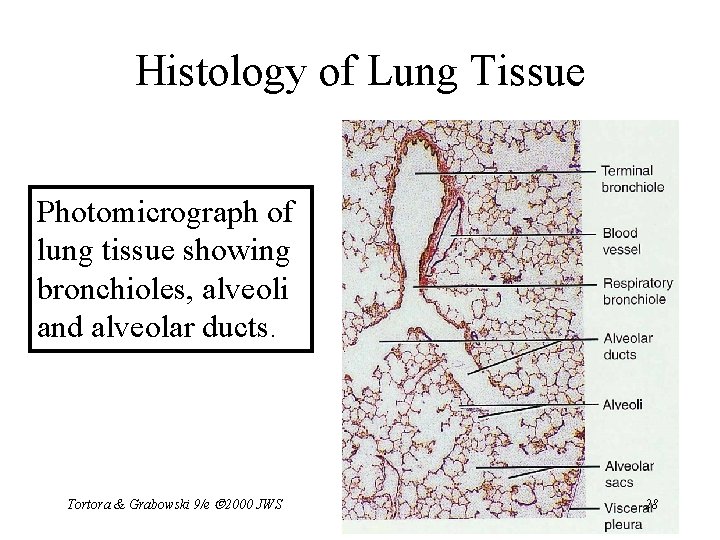
Histology of Lung Tissue Photomicrograph of lung tissue showing bronchioles, alveoli and alveolar ducts. Tortora & Grabowski 9/e 2000 JWS 28
Cells Types of the Alveoli • Type I alveolar cells – simple squamous cells where gas exchange occurs • Type II alveolar cells (septal cells) – free surface has microvilli – secrete alveolar fluid containing surfactant • Alveolar dust cells – wandering macrophages remove debris Tortora & Grabowski 9/e 2000 JWS 29
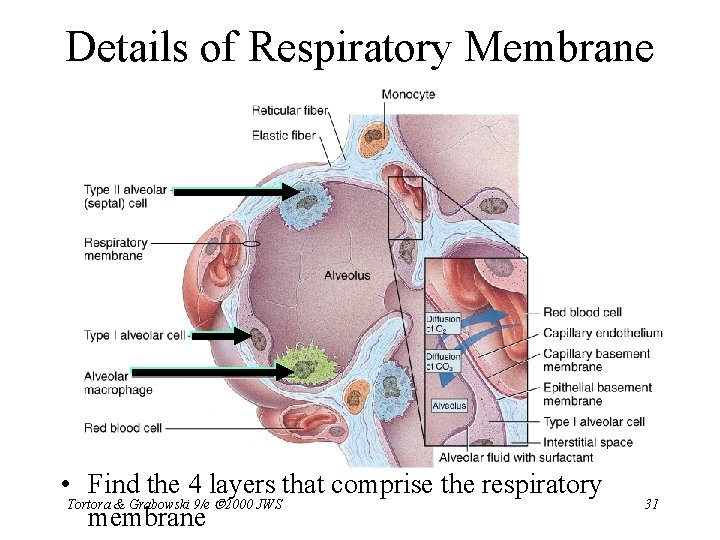
Alveolar-Capillary Membrane • Respiratory membrane = 1/2 micron thick • Exchange of gas from alveoli to blood • 4 Layers of membrane to cross – alveolar epithelial wall of type I cells – alveolar epithelial basement membrane – capillary basement membrane – endothelial cells of capillary • Vast surface area = handball court Tortora & Grabowski 9/e 2000 JWS 30
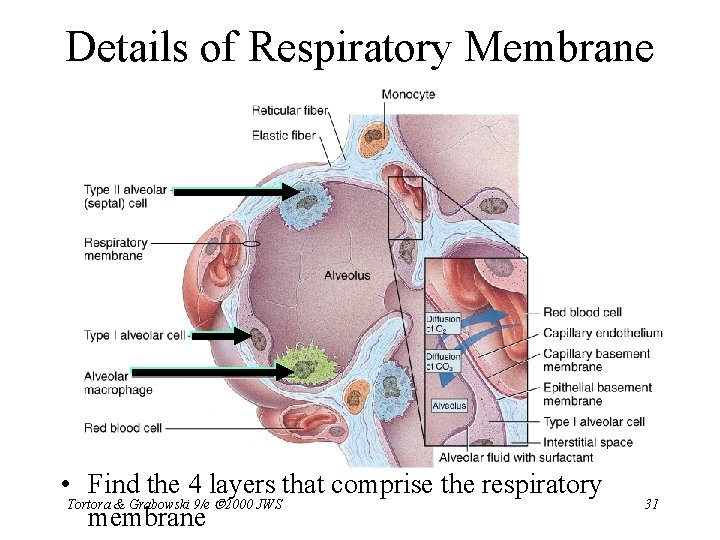
Details of Respiratory Membrane • Find the 4 layers that comprise the respiratory Tortora & Grabowski 9/e 2000 JWS membrane 31
Double Blood Supply to the Lungs • Deoxygenated blood arrives through pulmonary trunk from the right ventricle • Bronchial arteries branch off of the aorta to supply oxygenated blood to lung tissue • Venous drainage returns all blood to heart • Less pressure in venous system • Pulmonary blood vessels constrict in response to low O 2 levels so as not to pick up CO 2 on Tortora & Grabowski 9/e 2000 JWS 32 there way through the lungs
Breathing or Pulmonary Ventilation • Air moves into lungs when pressure inside lungs is less than atmospheric pressure – How is this accomplished? • Air moves out of the lungs when pressure inside lungs is greater than atmospheric pressure – How is this accomplished? • Atmospheric pressure = 1 atm or 760 mm Hg Tortora & Grabowski 9/e 2000 JWS 33
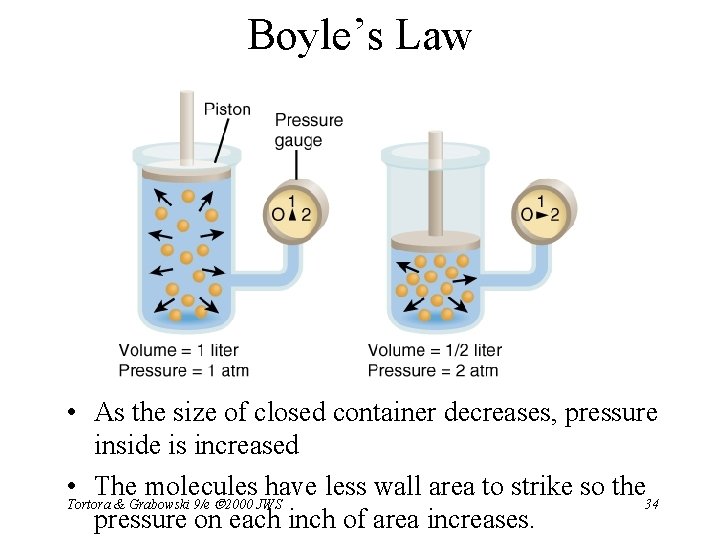
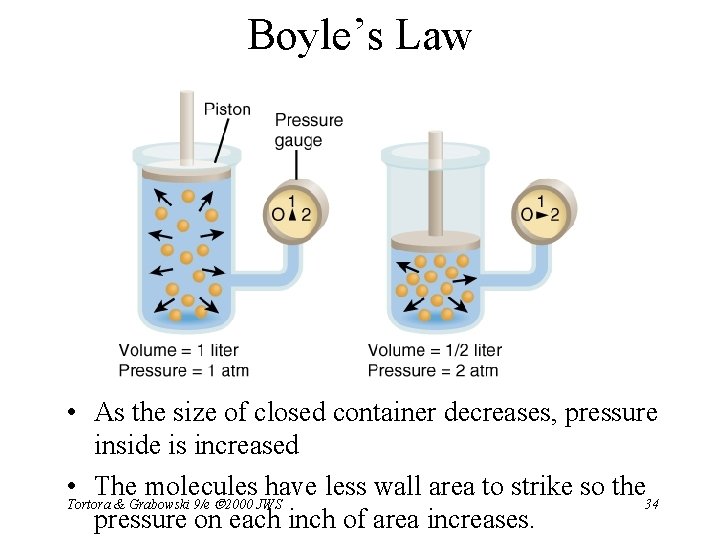
Boyle’s Law • As the size of closed container decreases, pressure inside is increased • The molecules have less wall area to strike so the Tortora & Grabowski 9/e 2000 JWS 34 pressure on each inch of area increases.
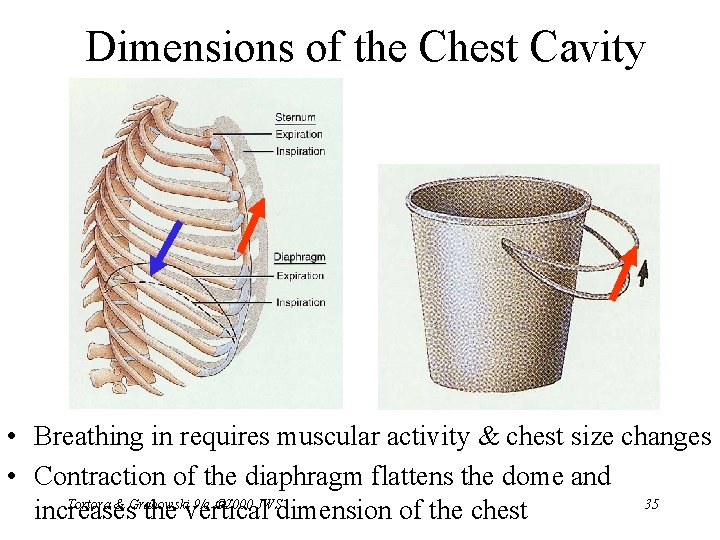
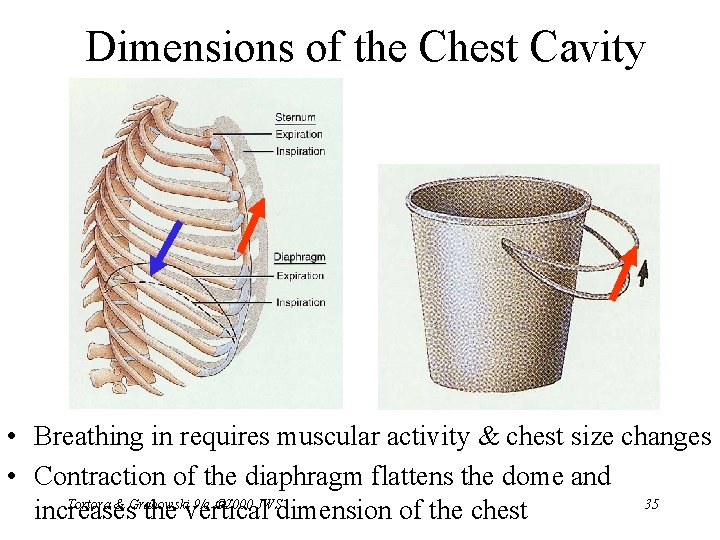
Dimensions of the Chest Cavity • Breathing in requires muscular activity & chest size changes • Contraction of the diaphragm flattens the dome and Tortora & Grabowski 9/e 2000 JWS 35 increases the vertical dimension of the chest
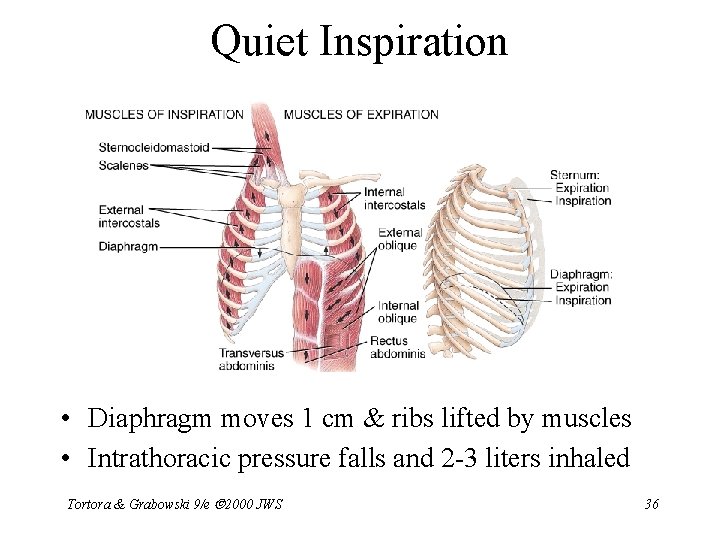
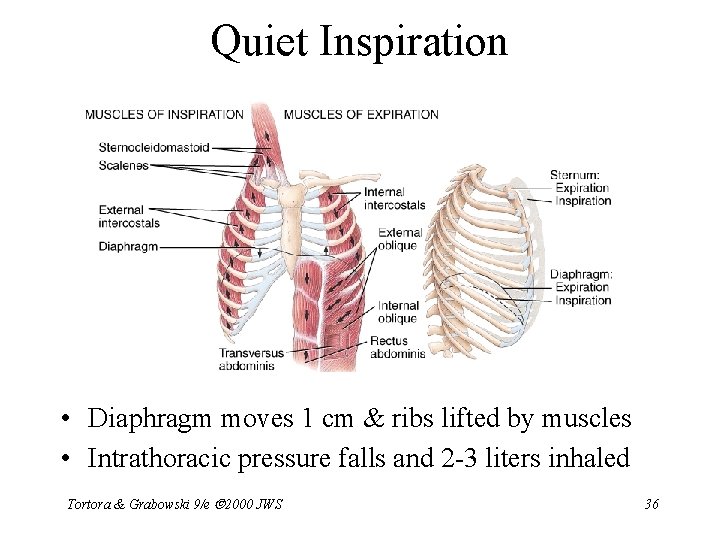
Quiet Inspiration • Diaphragm moves 1 cm & ribs lifted by muscles • Intrathoracic pressure falls and 2 -3 liters inhaled Tortora & Grabowski 9/e 2000 JWS 36
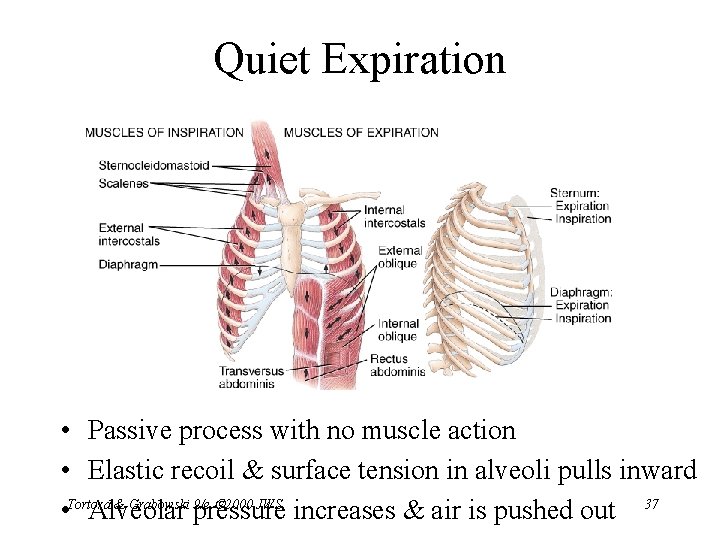
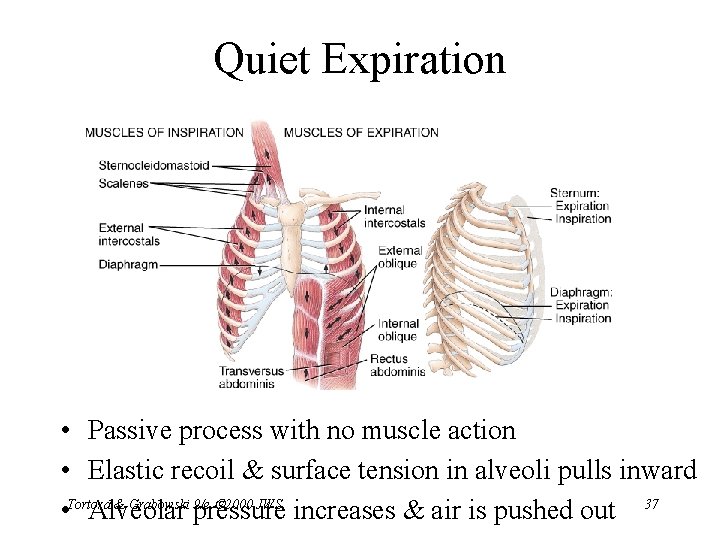
Quiet Expiration • Passive process with no muscle action • Elastic recoil & surface tension in alveoli pulls inward & Grabowski 9/e 2000 JWS • Tortora Alveolar pressure increases & air is pushed out 37
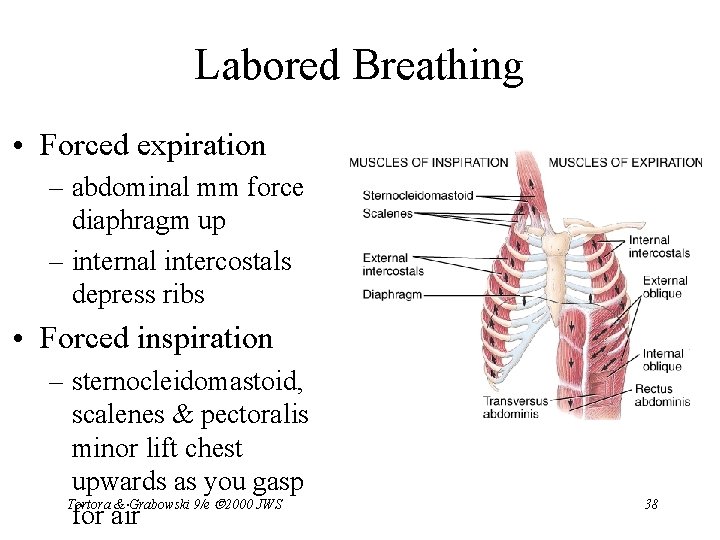
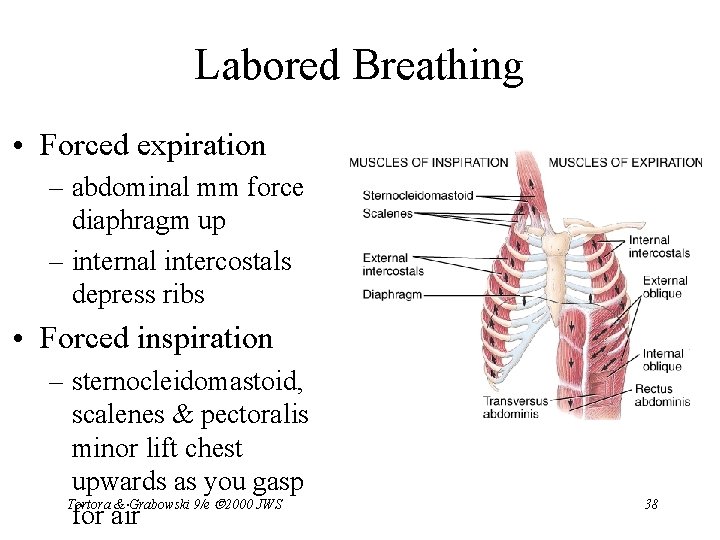
Labored Breathing • Forced expiration – abdominal mm force diaphragm up – internal intercostals depress ribs • Forced inspiration – sternocleidomastoid, scalenes & pectoralis minor lift chest upwards as you gasp Tortora & Grabowski 9/e 2000 JWS for air 38
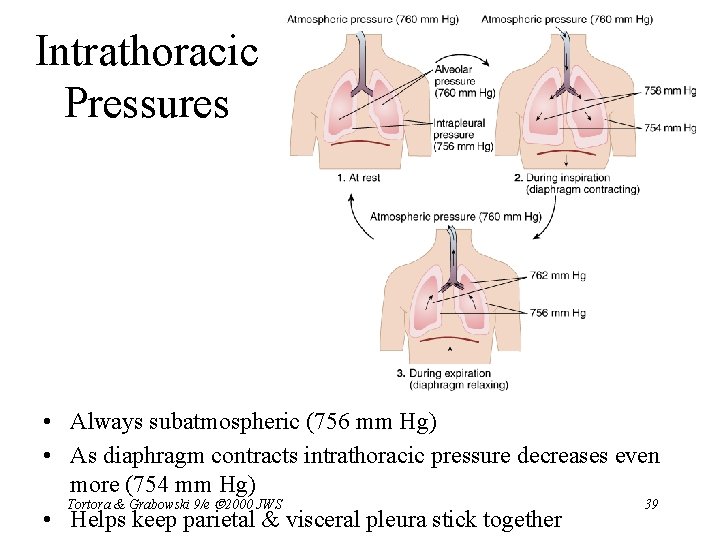
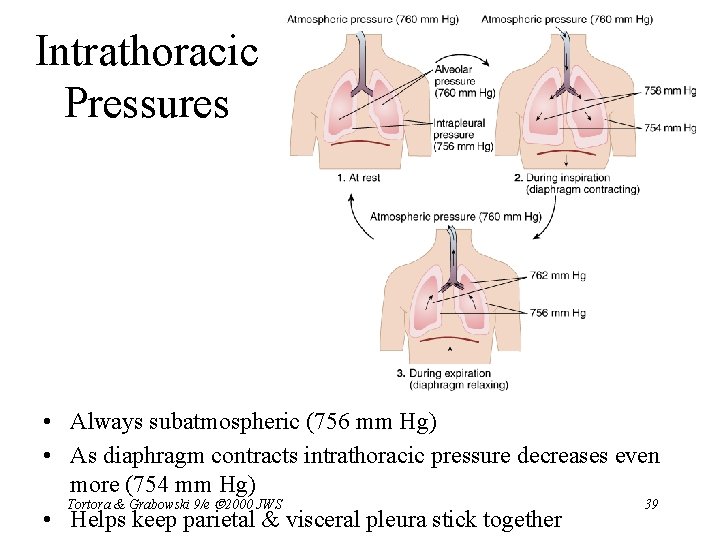
Intrathoracic Pressures • Always subatmospheric (756 mm Hg) • As diaphragm contracts intrathoracic pressure decreases even more (754 mm Hg) Tortora & Grabowski 9/e 2000 JWS 39 • Helps keep parietal & visceral pleura stick together
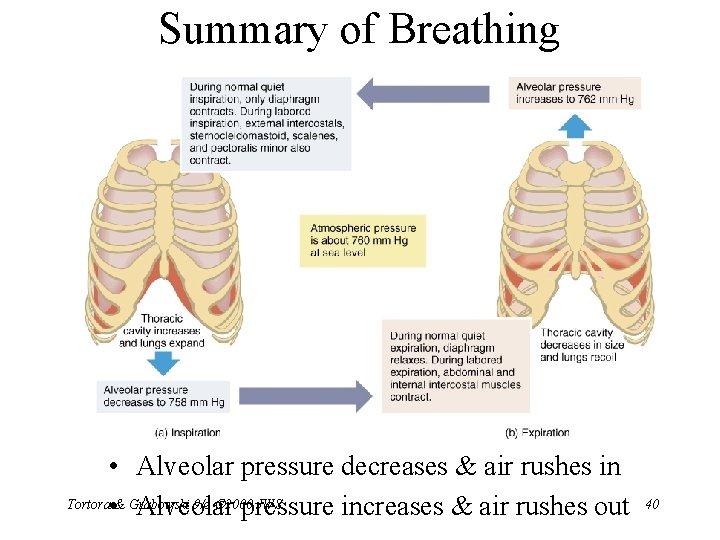
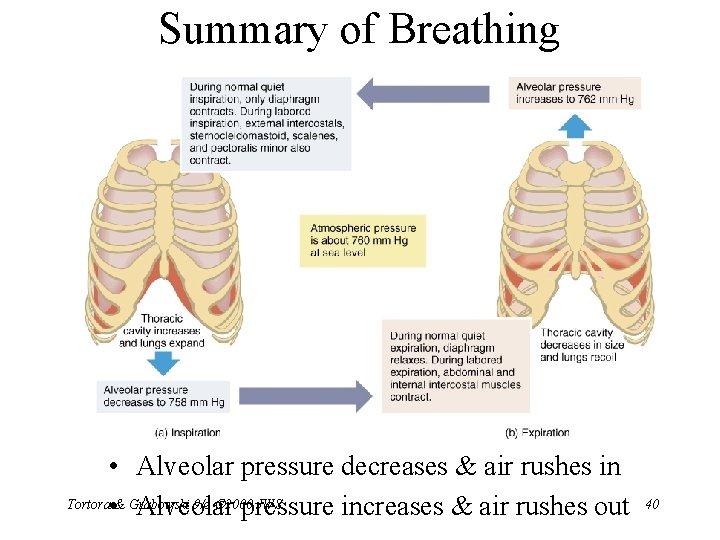
Summary of Breathing • Alveolar pressure decreases & air rushes in Tortora • & Grabowski 9/e 2000 JWS Alveolar pressure increases & air rushes out 40
Alveolar Surface Tension • Thin layer of fluid in alveoli causes inwardly directed force = surface tension – water molecules strongly attracted to each other • Causes alveoli to remain as small as possible • Detergent-like substance called surfactant produced by Type II alveolar cells – lowers alveolar surface tension – insufficient in premature babies so that alveoli collapse at end of each exhalation Tortora & Grabowski 9/e 2000 JWS 41
Pneumothorax • Pleural cavities are sealed cavities not open to the outside • Injuries to the chest wall that let air enter the intrapleural space – causes a pneumothorax – collapsed lung on same side as injury – surface tension and recoil of elastic fibers causes the lung to collapse Tortora & Grabowski 9/e 2000 JWS 42
Compliance of the Lungs • Ease with which lungs & chest wall expand depends upon elasticity of lungs & surface tension • Some diseases reduce compliance – tuberculosis forms scar tissue – pulmonary edema --- fluid in lungs & reduced surfactant – paralysis Tortora & Grabowski 9/e 2000 JWS 43
Airway Resistance • Resistance to airflow depends upon airway size – increase size of chest • airways increase in diameter – contract smooth muscles in airways • decreases in diameter Tortora & Grabowski 9/e 2000 JWS 44
Breathing Patterns • • • Eupnea = normal quiet breathing Apnea = temporary cessation of breathing Dyspnea =difficult or labored breathing Tachypnea = rapid breathing Diaphragmatic breathing = descent of diaphragm causes stomach to bulge during inspiration • Costal breathing = just rib activity involved Tortora & Grabowski 9/e 2000 JWS 45
Modified Respiratory Movements • Coughing – deep inspiration, closure of rima glottidis & strong expiration blasts air out to clear respiratory passages • Hiccuping – spasmodic contraction of diaphragm & quick closure of rima glottidis produce sharp inspiratory sound • Chart of others on page 794 Tortora & Grabowski 9/e 2000 JWS 46
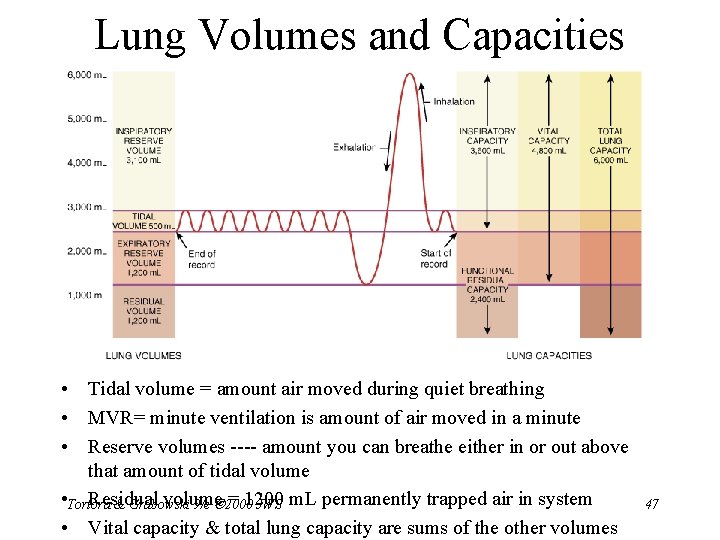
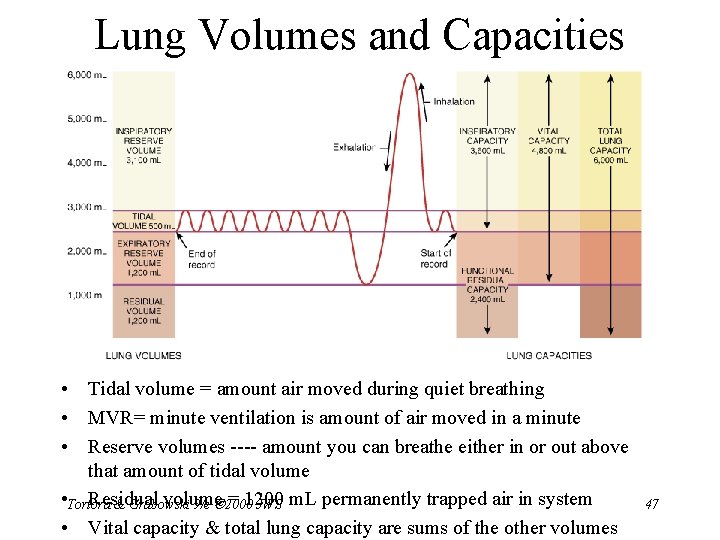
Lung Volumes and Capacities • Tidal volume = amount air moved during quiet breathing • MVR= minute ventilation is amount of air moved in a minute • Reserve volumes ---- amount you can breathe either in or out above that amount of tidal volume • Tortora Residual volume = 1200 & Grabowski 9/e 2000 JWS m. L permanently trapped air in system • Vital capacity & total lung capacity are sums of the other volumes 47
Dalton’s Law • Each gas in a mixture of gases exerts its own pressure – as if all other gases were not present – partial pressures denoted as p • Total pressure is sum of all partial pressures – atmospheric pressure (760 mm Hg) = p. O 2 + p. CO 2 + p. N 2 + p. H 2 O – to determine partial pressure of O 2 -- multiply 760 by % of air that is O 2 (21%) = 160 mm Hg Tortora & Grabowski 9/e 2000 JWS 48
What is Composition of Air? • • Air = 21% O 2, 79% N 2 and. 04% CO 2 Alveolar air = 14% O 2, 79% N 2 and 5. 2% CO 2 Expired air = 16% O 2, 79% N 2 and 4. 5% CO 2 Observations – alveolar air has less O 2 since absorbed by blood – mystery-----expired air has more O 2 & less CO 2 than alveolar air? – Anatomical dead space = 150 ml of 500 ml of tidal Tortora & Grabowski 9/e 2000 JWS 49 volume
Henry’s Law • Quantity of a gas that will dissolve in a liquid depends upon the amount of gas present and its solubility coefficient – explains why you can breathe compressed air while scuba diving despite 79% Nitrogen • N 2 has very low solubility unlike CO 2 (soda cans) • dive deep & increased pressure forces more N 2 to dissolve in the blood (nitrogen narcosis) • decompression sickness if come back to surface too fast or stay deep too long • Breathing O 2 under pressure dissolves more O 2 in Tortora & Grabowski 9/e 2000 JWS 50 blood
Hyperbaric Oxygenation • Clinical application of Henry’s law • Use of pressure to dissolve more O 2 in the blood – treatment for patients with anaerobic bacterial infections (tetanus and gangrene) – anaerobic bacteria die in the presence of O 2 • Hyperbaric chamber pressure raised to 3 to 4 atmospheres so that tissues absorb more O 2 • Used to treat heart disorders, carbon monoxide poisoning, cerebral edema, bone infections, gas embolisms & crush injuries Tortora & Grabowski 9/e 2000 JWS 51
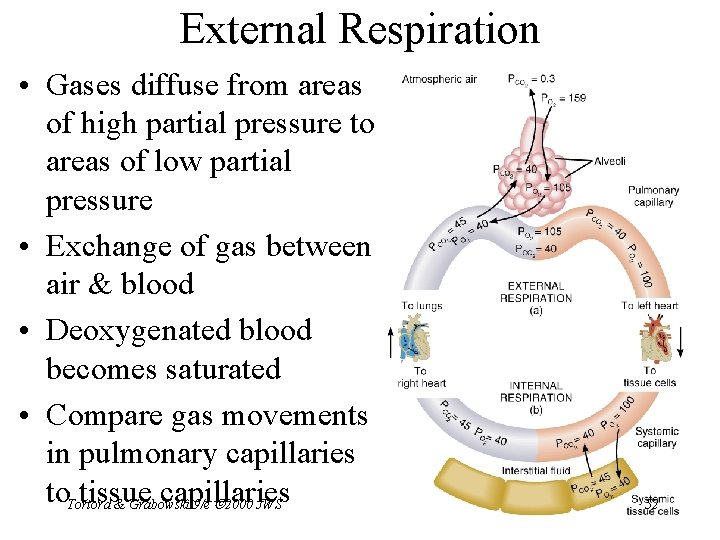
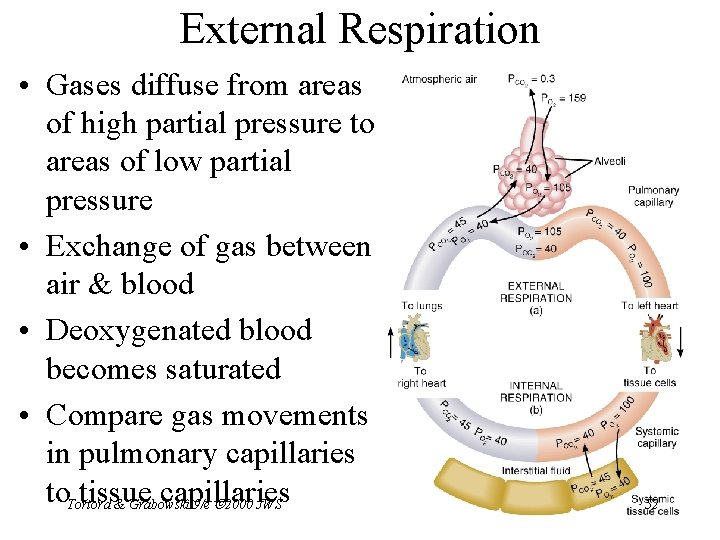
External Respiration • Gases diffuse from areas of high partial pressure to areas of low partial pressure • Exchange of gas between air & blood • Deoxygenated blood becomes saturated • Compare gas movements in pulmonary capillaries to. Tortora tissue capillaries & Grabowski 9/e 2000 JWS 52
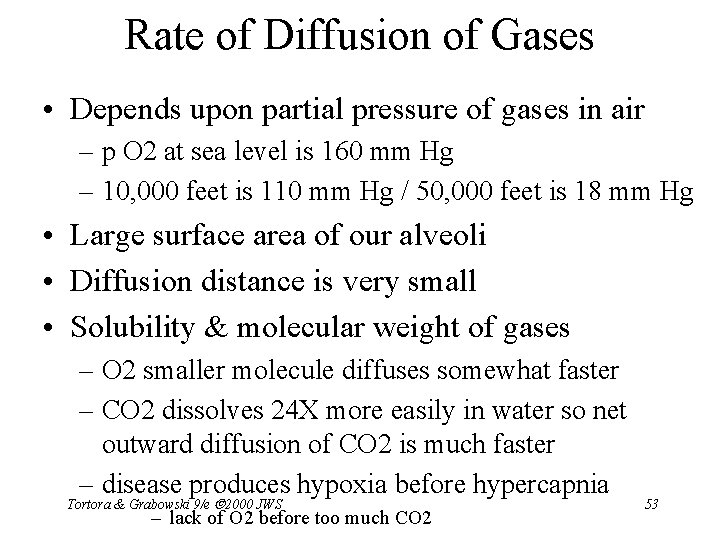
Rate of Diffusion of Gases • Depends upon partial pressure of gases in air – p O 2 at sea level is 160 mm Hg – 10, 000 feet is 110 mm Hg / 50, 000 feet is 18 mm Hg • Large surface area of our alveoli • Diffusion distance is very small • Solubility & molecular weight of gases – O 2 smaller molecule diffuses somewhat faster – CO 2 dissolves 24 X more easily in water so net outward diffusion of CO 2 is much faster – disease produces hypoxia before hypercapnia Tortora & Grabowski 9/e 2000 JWS – lack of O 2 before too much CO 2 53
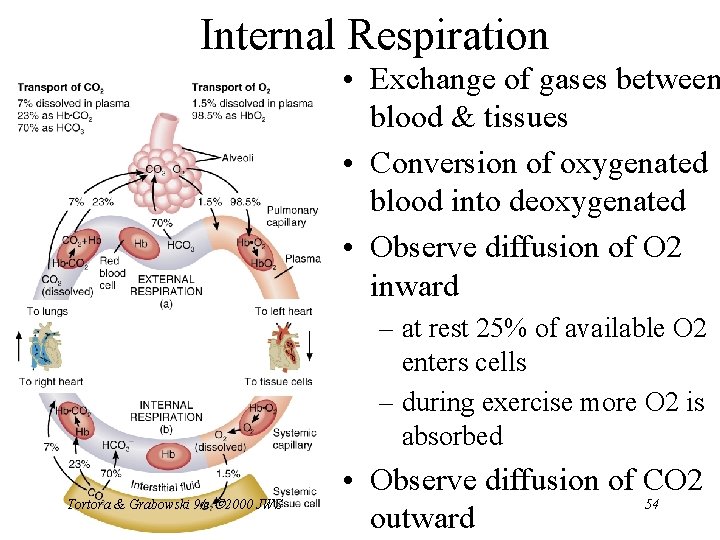
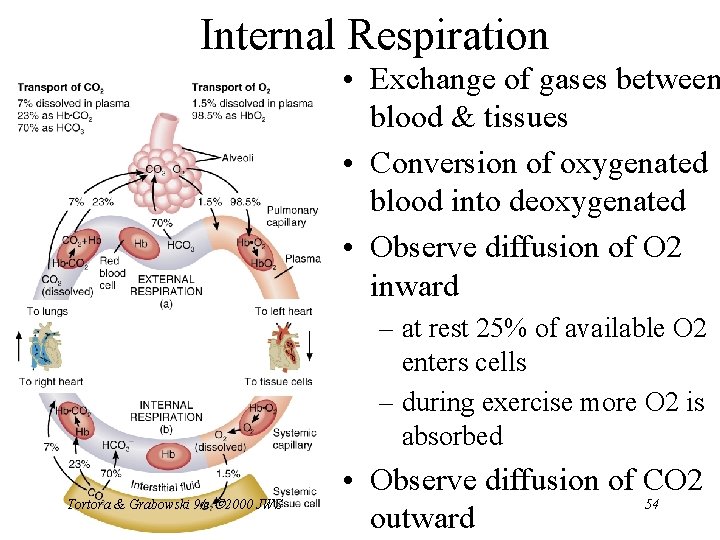
Internal Respiration • Exchange of gases between blood & tissues • Conversion of oxygenated blood into deoxygenated • Observe diffusion of O 2 inward – at rest 25% of available O 2 enters cells – during exercise more O 2 is absorbed Tortora & Grabowski 9/e 2000 JWS • Observe diffusion of CO 2 54 outward
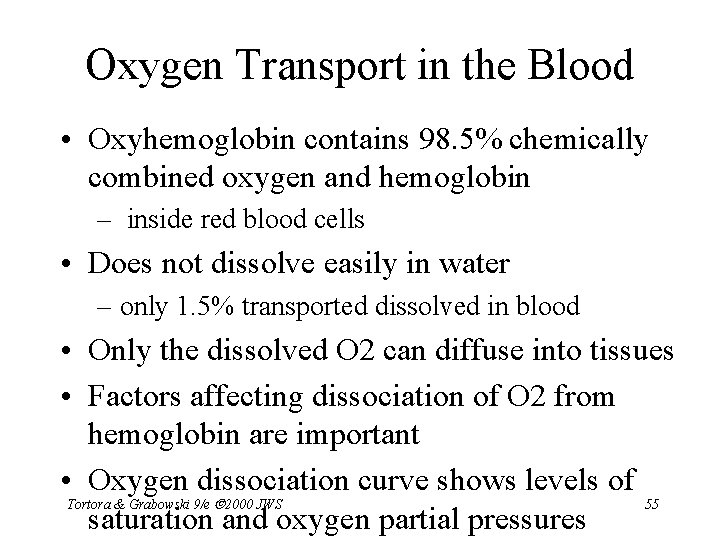
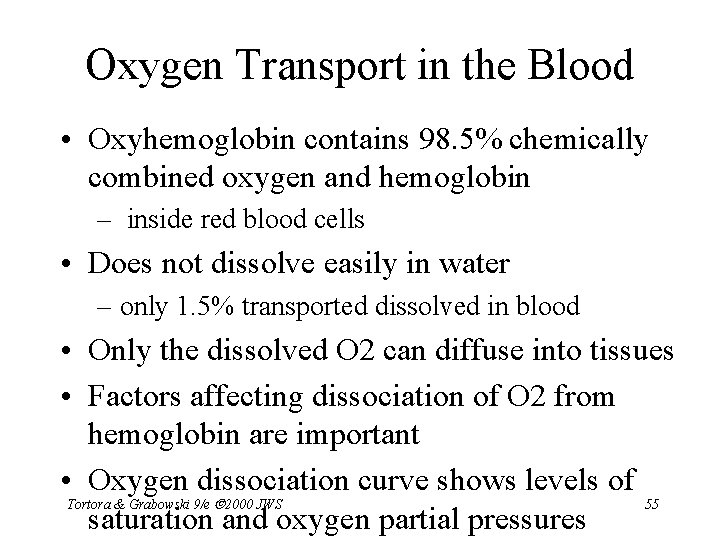
Oxygen Transport in the Blood • Oxyhemoglobin contains 98. 5% chemically combined oxygen and hemoglobin – inside red blood cells • Does not dissolve easily in water – only 1. 5% transported dissolved in blood • Only the dissolved O 2 can diffuse into tissues • Factors affecting dissociation of O 2 from hemoglobin are important • Oxygen dissociation curve shows levels of Tortora & Grabowski 9/e 2000 JWS 55 saturation and oxygen partial pressures
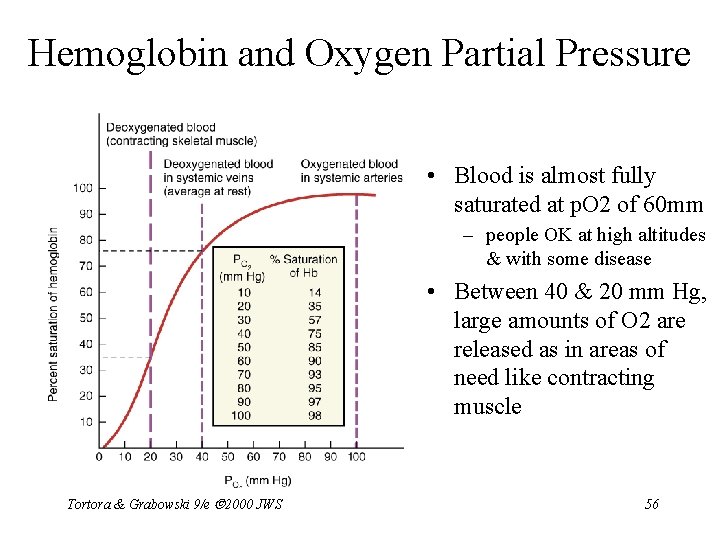
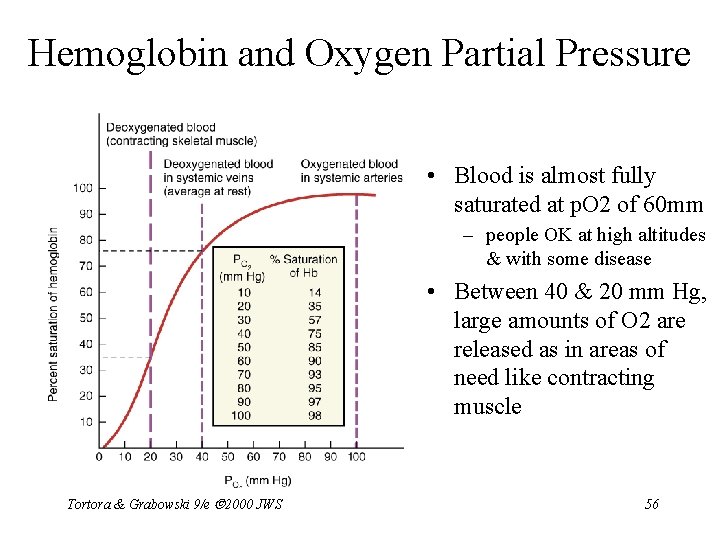
Hemoglobin and Oxygen Partial Pressure • Blood is almost fully saturated at p. O 2 of 60 mm – people OK at high altitudes & with some disease • Between 40 & 20 mm Hg, large amounts of O 2 are released as in areas of need like contracting muscle Tortora & Grabowski 9/e 2000 JWS 56
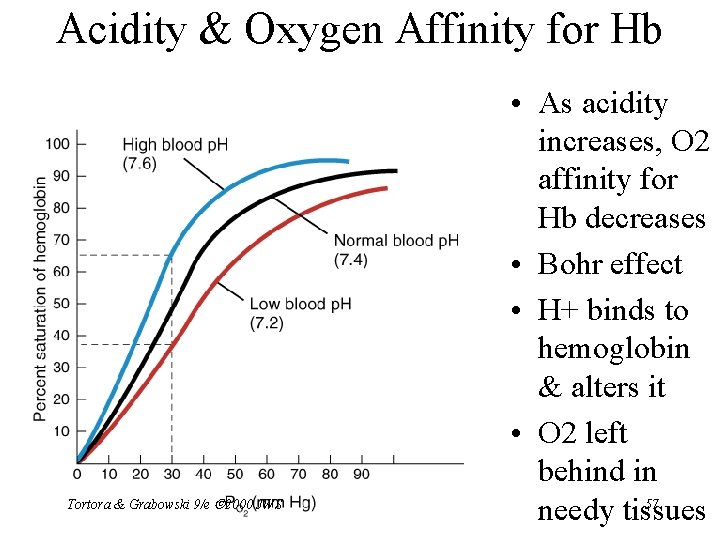
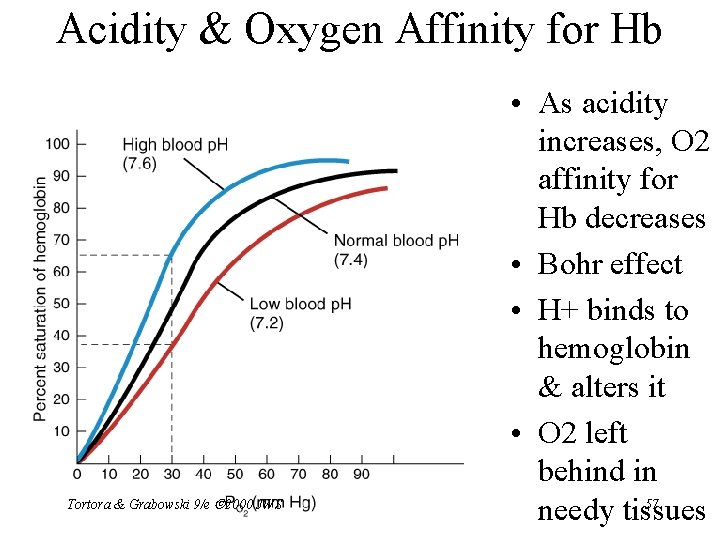
Acidity & Oxygen Affinity for Hb Tortora & Grabowski 9/e 2000 JWS • As acidity increases, O 2 affinity for Hb decreases • Bohr effect • H+ binds to hemoglobin & alters it • O 2 left behind in 57 needy tissues
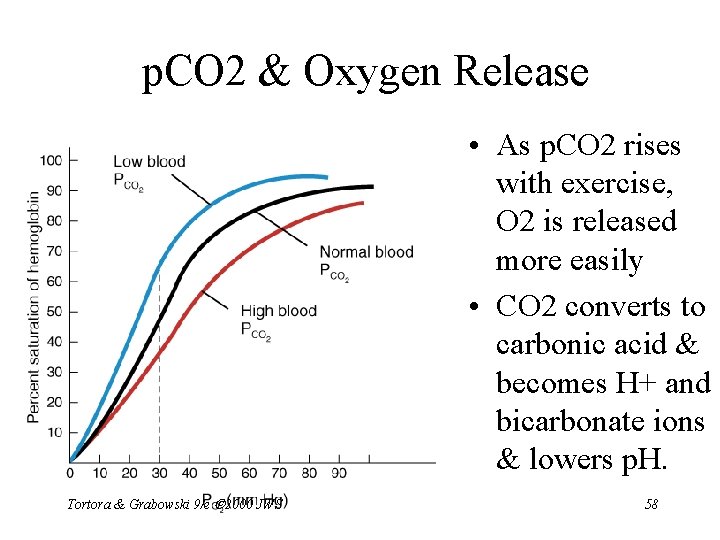
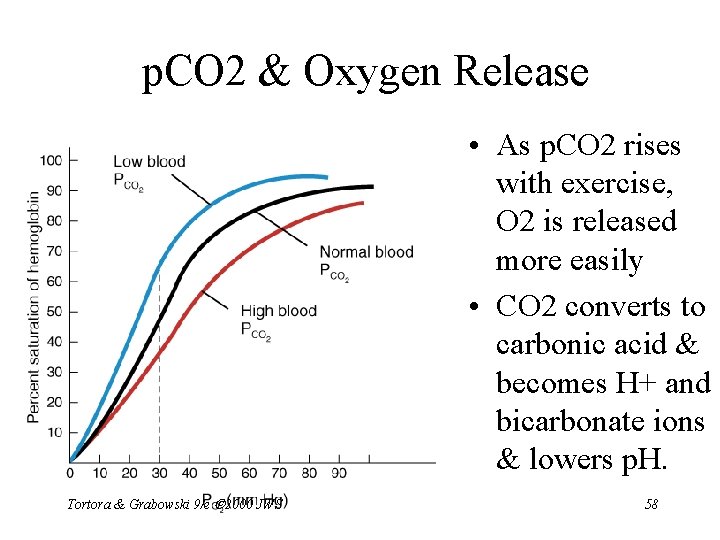
p. CO 2 & Oxygen Release • As p. CO 2 rises with exercise, O 2 is released more easily • CO 2 converts to carbonic acid & becomes H+ and bicarbonate ions & lowers p. H. Tortora & Grabowski 9/e 2000 JWS 58
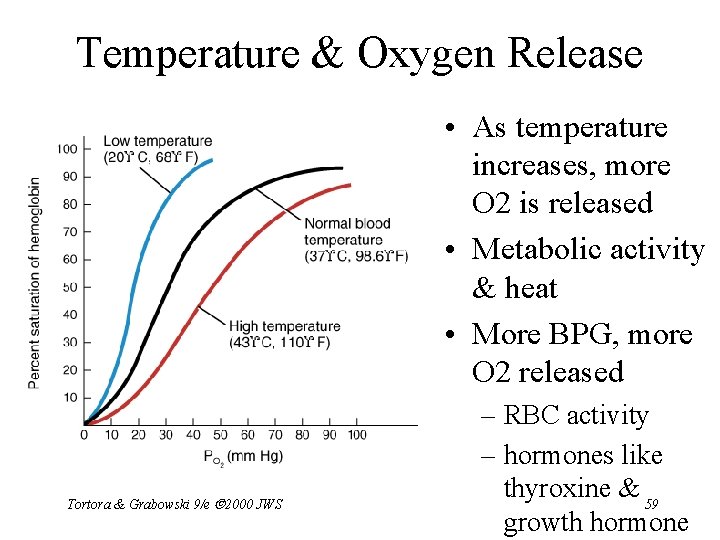
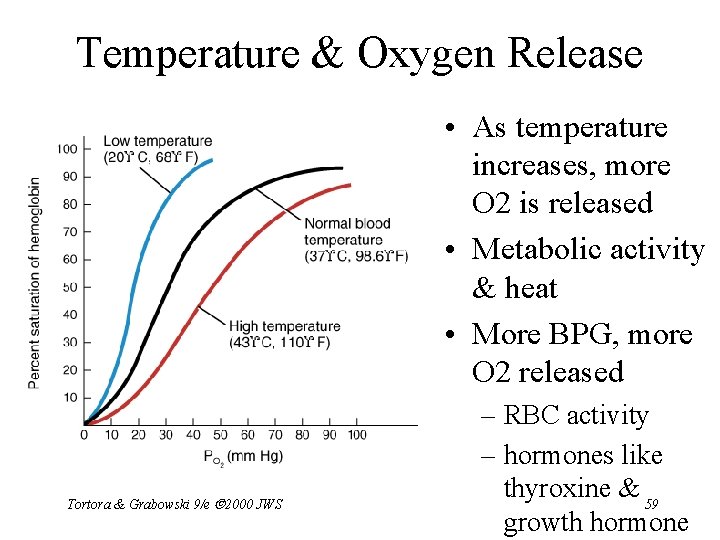
Temperature & Oxygen Release • As temperature increases, more O 2 is released • Metabolic activity & heat • More BPG, more O 2 released Tortora & Grabowski 9/e 2000 JWS – RBC activity – hormones like thyroxine & 59 growth hormone
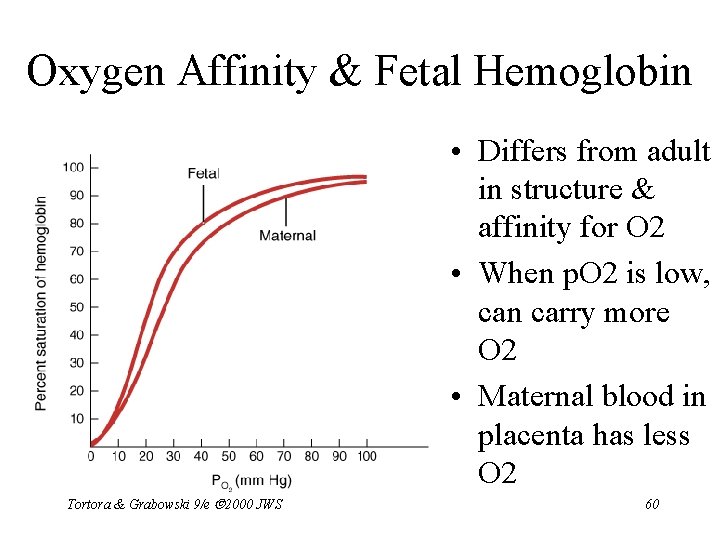
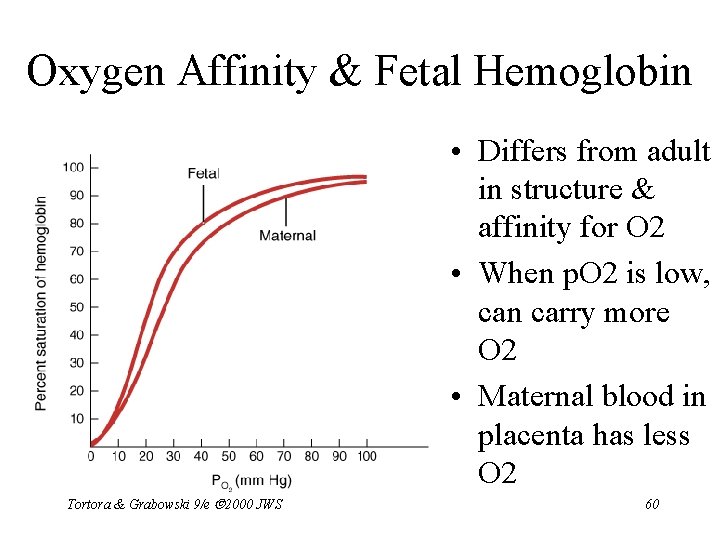
Oxygen Affinity & Fetal Hemoglobin • Differs from adult in structure & affinity for O 2 • When p. O 2 is low, can carry more O 2 • Maternal blood in placenta has less O 2 Tortora & Grabowski 9/e 2000 JWS 60
Carbon Monoxide Poisoning • CO from car exhaust & tobacco smoke • Binds to Hb heme group more successfully than O 2 • CO poisoning • Treat by administering pure O 2 Tortora & Grabowski 9/e 2000 JWS 61
Carbon Dioxide Transport • 100 ml of blood carries 55 ml of CO 2 • Is carried by the blood in 3 ways – dissolved in plasma – combined with the globin part of Hb molecule forming carbaminohemoglobin – as part of bicarbonate ion • CO 2 + H 2 O combine to form carbonic acid that dissociates into H+ and bicarbonate ion Tortora & Grabowski 9/e 2000 JWS 62
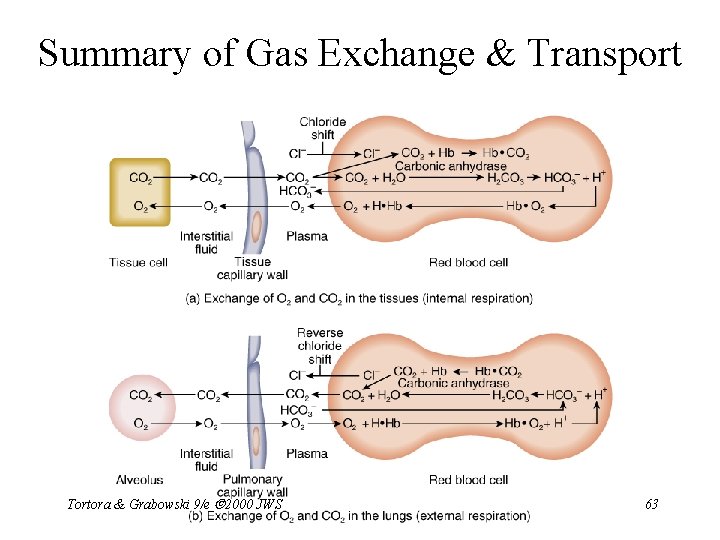
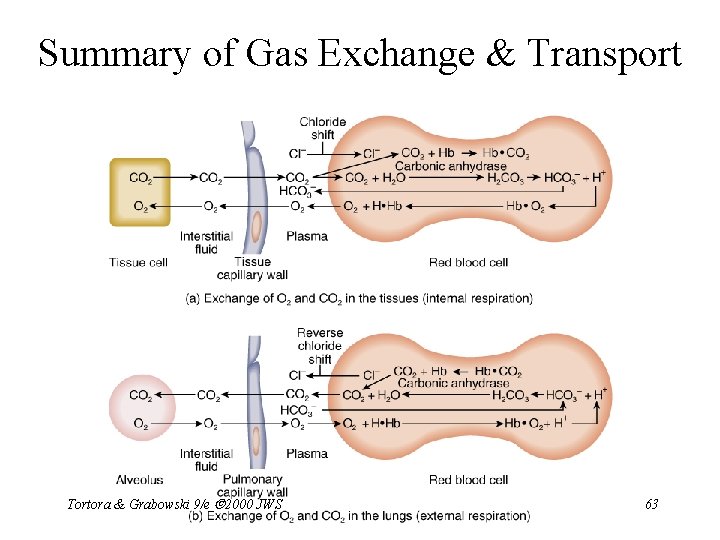
Summary of Gas Exchange & Transport Tortora & Grabowski 9/e 2000 JWS 63
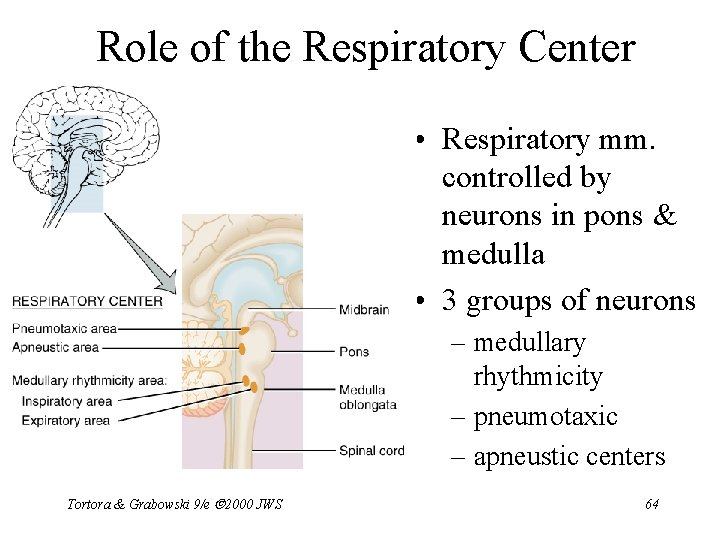
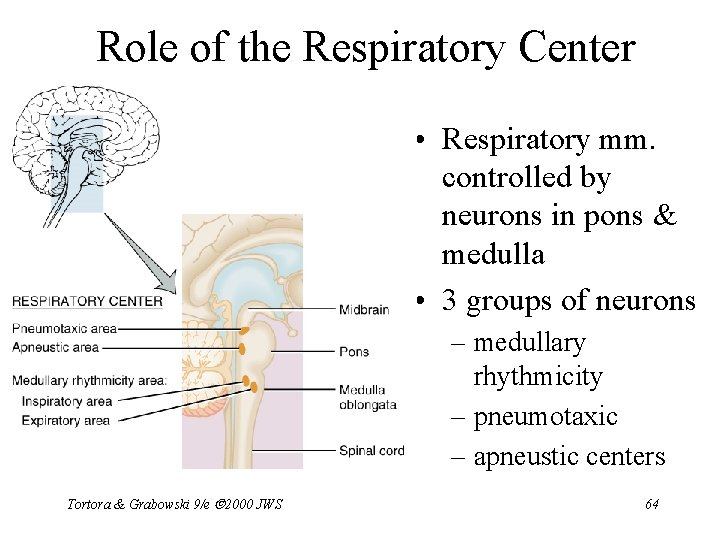
Role of the Respiratory Center • Respiratory mm. controlled by neurons in pons & medulla • 3 groups of neurons – medullary rhythmicity – pneumotaxic – apneustic centers Tortora & Grabowski 9/e 2000 JWS 64
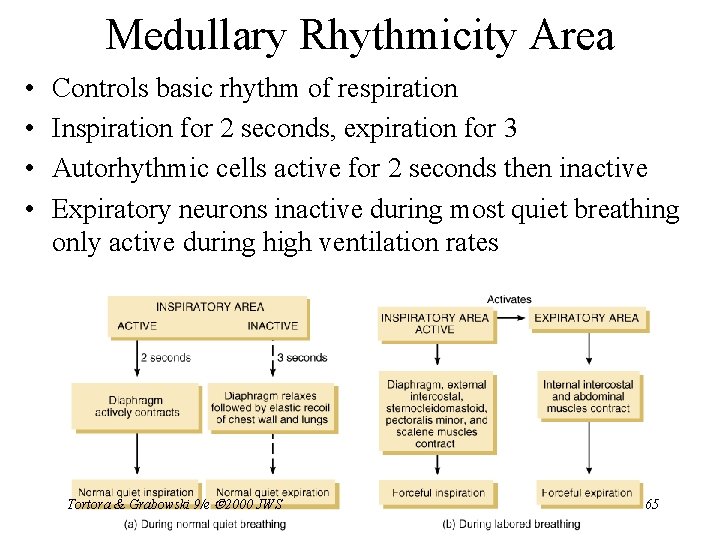
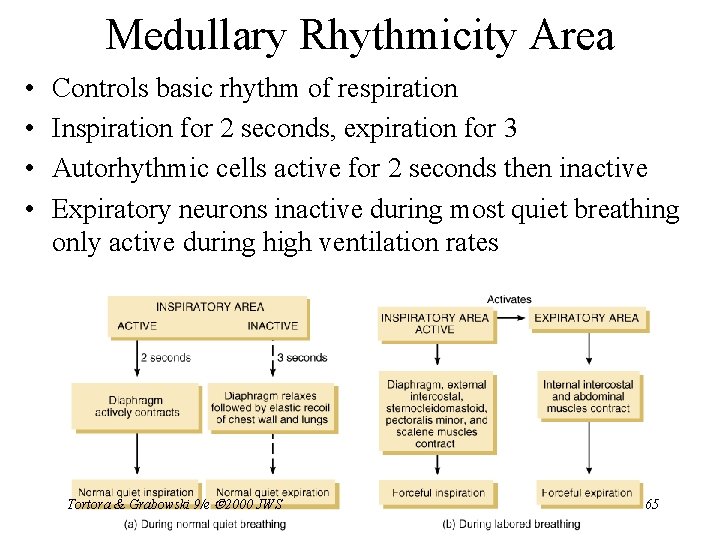
Medullary Rhythmicity Area • • Controls basic rhythm of respiration Inspiration for 2 seconds, expiration for 3 Autorhythmic cells active for 2 seconds then inactive Expiratory neurons inactive during most quiet breathing only active during high ventilation rates Tortora & Grabowski 9/e 2000 JWS 65
Pneumotaxic & Apneustic Areas • Pneumotaxic Area – constant inhibitory impulses to inspiratory area • neurons trying to turn off inspiration before lungs too expanded • Apneustic Area – stimulatory signals to inspiratory area to prolong inspiration – if pneumotaxic area is sick Tortora & Grabowski 9/e 2000 JWS 66
Regulation of Respiratory Center • Cortical Influences – voluntarily alter breathing patterns – limitations are buildup of CO 2 & H+ in blood – inspiratory center is stimulated by increase in either – if you hold breathe until you faint----breathing will resume Tortora & Grabowski 9/e 2000 JWS 67
Chemical Regulation of Respiration • Central chemoreceptors in medulla – respond to changes in H+ or p. CO 2 – hypercapnia = slight increase in p. CO 2 is noticed • Peripheral chemoreceptors – respond to changes in H+ , p. O 2 or PCO 2 – aortic body---in wall of aorta • nerves join vagus – carotid bodies--in walls of common carotid arteries • nerves join glossopharyngeal nerve Tortora & Grabowski 9/e 2000 JWS 68
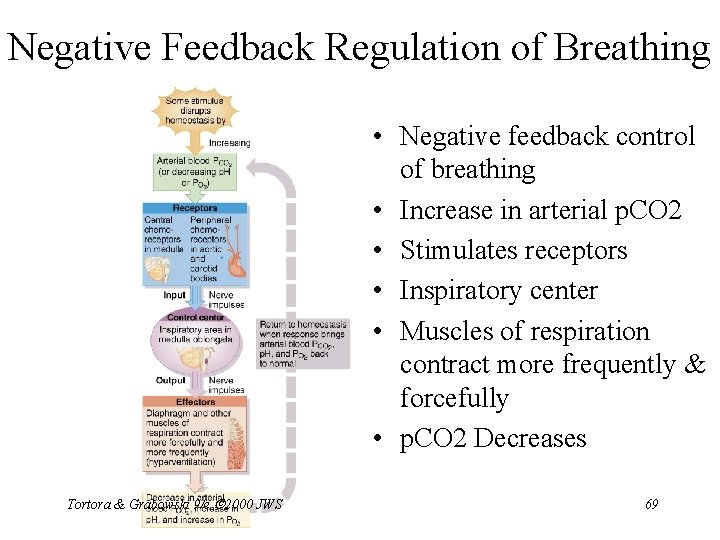
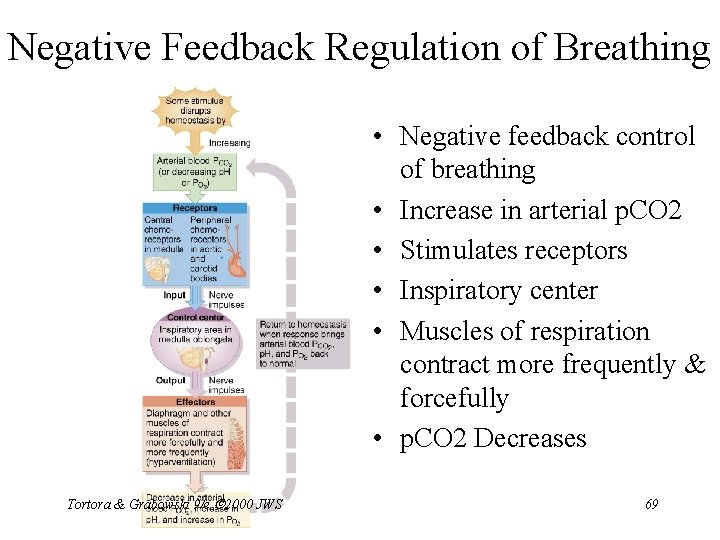
Negative Feedback Regulation of Breathing • Negative feedback control of breathing • Increase in arterial p. CO 2 • Stimulates receptors • Inspiratory center • Muscles of respiration contract more frequently & forcefully • p. CO 2 Decreases Tortora & Grabowski 9/e 2000 JWS 69
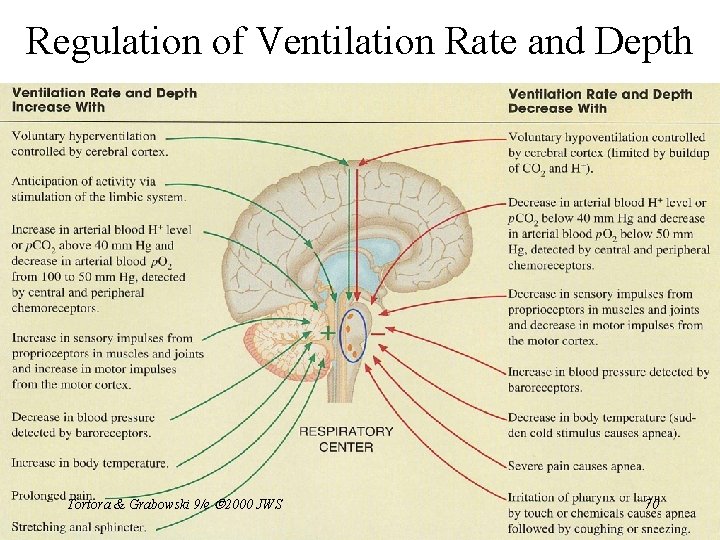
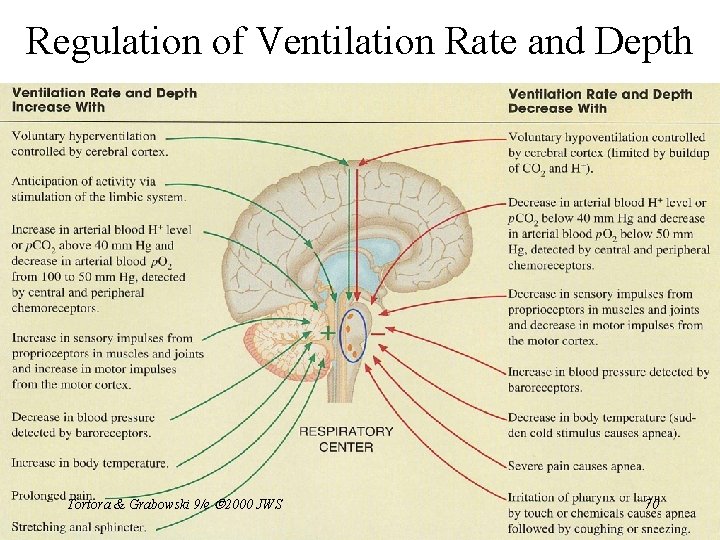
Regulation of Ventilation Rate and Depth Tortora & Grabowski 9/e 2000 JWS 70
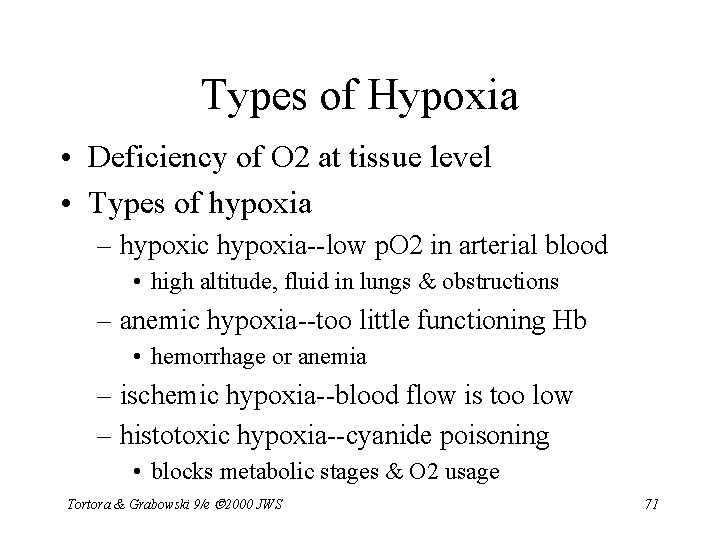
Types of Hypoxia • Deficiency of O 2 at tissue level • Types of hypoxia – hypoxic hypoxia--low p. O 2 in arterial blood • high altitude, fluid in lungs & obstructions – anemic hypoxia--too little functioning Hb • hemorrhage or anemia – ischemic hypoxia--blood flow is too low – histotoxic hypoxia--cyanide poisoning • blocks metabolic stages & O 2 usage Tortora & Grabowski 9/e 2000 JWS 71
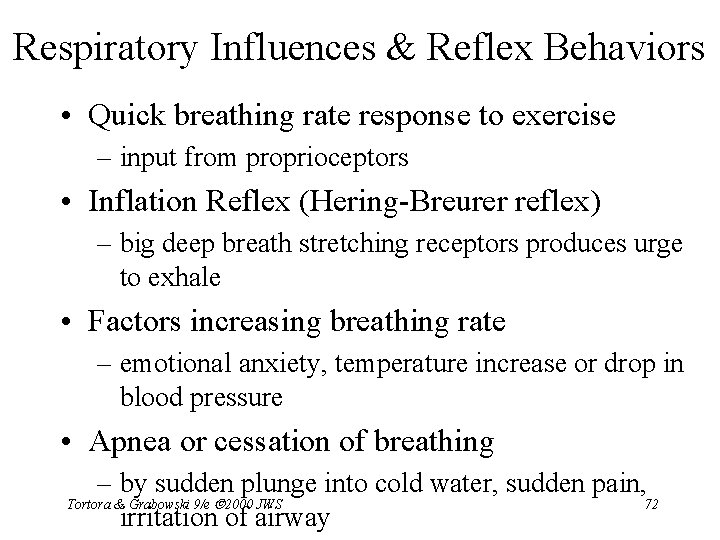
Respiratory Influences & Reflex Behaviors • Quick breathing rate response to exercise – input from proprioceptors • Inflation Reflex (Hering-Breurer reflex) – big deep breath stretching receptors produces urge to exhale • Factors increasing breathing rate – emotional anxiety, temperature increase or drop in blood pressure • Apnea or cessation of breathing – by sudden plunge into cold water, sudden pain, Tortora & Grabowski 9/e 2000 JWS 72 irritation of airway
Exercise and the Respiratory System • During exercise, muscles consume large amounts of O 2 & produce large amounts CO 2 • Pulmonary ventilation must increase – moderate exercise increases depth of breathing, – strenuous exercise also increases rate of breathing • Abrupt changes at start of exercise are neural – anticipation & sensory signals from proprioceptors – impulses from motor cortex • Chemical & physical changes are important – decrease in p. O 2, increase in p. CO 2 & increased 73 temperature Tortora & Grabowski 9/e 2000 JWS
Smokers Lowered Respiratory Efficiency • Smoker is easily “winded” with moderate exercise – nicotine constricts terminal bronchioles – carbon monoxide in smoke binds to hemoglobin – irritants in smoke cause excess mucus secretion – irritants inhibit movements of cilia – in time destroys elastic fibers in lungs & leads to emphysema • trapping of air in alveoli & reduced gas exchange Tortora & Grabowski 9/e 2000 JWS 74
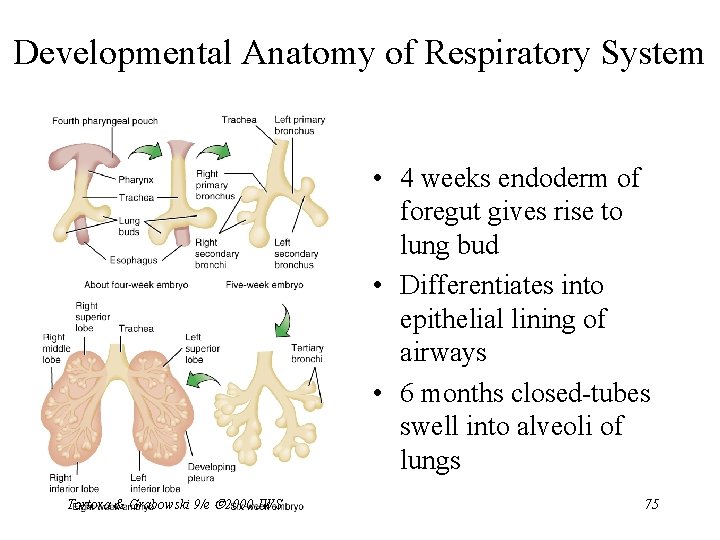
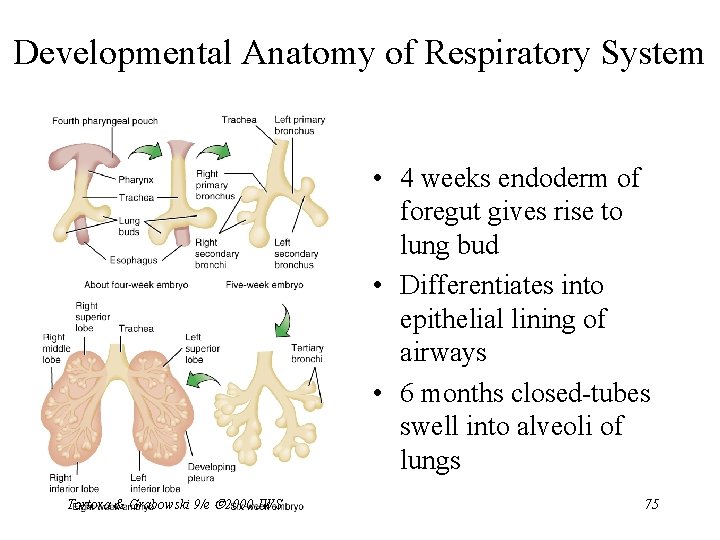
Developmental Anatomy of Respiratory System • 4 weeks endoderm of foregut gives rise to lung bud • Differentiates into epithelial lining of airways • 6 months closed-tubes swell into alveoli of lungs Tortora & Grabowski 9/e 2000 JWS 75
Aging & the Respiratory System • Respiratory tissues & chest wall become more rigid • Vital capacity decreases to 35% by age 70. • Decreases in macrophage activity • Diminished ciliary action • Decrease in blood levels of O 2 • Result is an age-related susceptibility to pneumonia or bronchitis Tortora & Grabowski 9/e 2000 JWS 76
Disorders of the Respiratory System • Asthma • Chronic obstructive pulmonary disease – Emphysema – Chronic bronchitis – Lung cancer • Pneumonia • Tuberculosis • Coryza and Influenza • Pulmonary Edema & Grabowski 9/e 2000 JWS • Tortora Cystic fibrosis 77