Chapter 23 The Respiratory System 2015 Pearson Education

- Slides: 56
Chapter 23: The Respiratory System © 2015 Pearson Education, Inc.
Homeostasis • Provides for exchange of gases, O 2 & CO 2, between atmospheric air, blood, & tissue cells • Also helps adjust p. H of body fluids • Also participates in – – Sense of smell Filters inspired air Produces sound Rids body of some water & heat © 2015 Pearson Education, Inc.
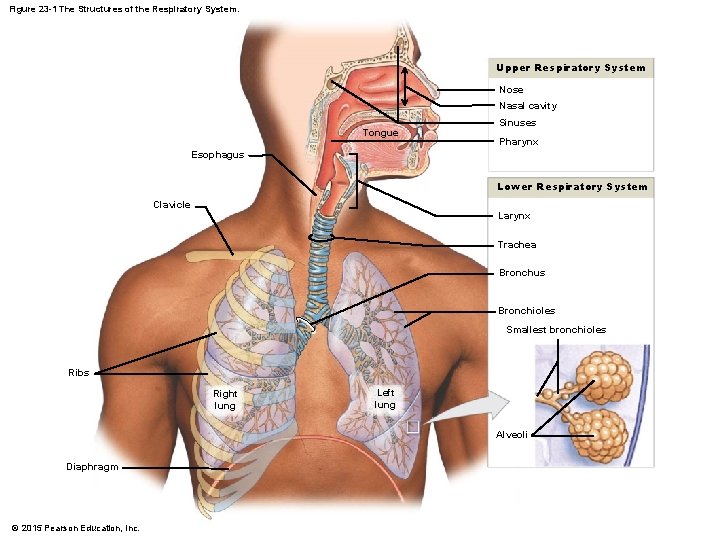
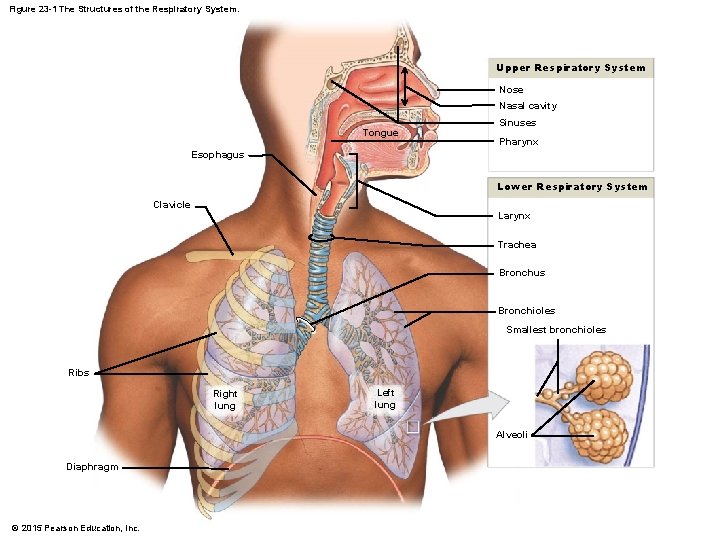
Figure 23 -1 The Structures of the Respiratory System. Upper Respiratory System Nose Nasal cavity Tongue Sinuses Pharynx Esophagus Lower Respiratory System Clavicle Larynx Trachea Bronchus Bronchioles Smallest bronchioles Ribs Right lung Left lung Alveoli Diaphragm © 2015 Pearson Education, Inc.
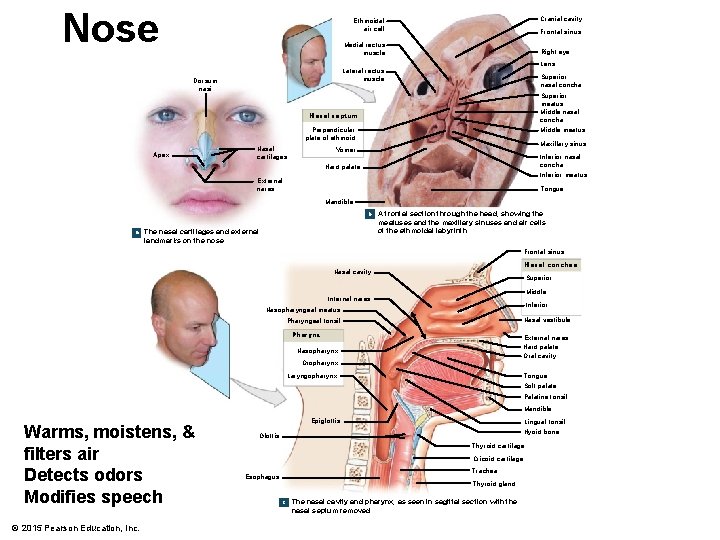
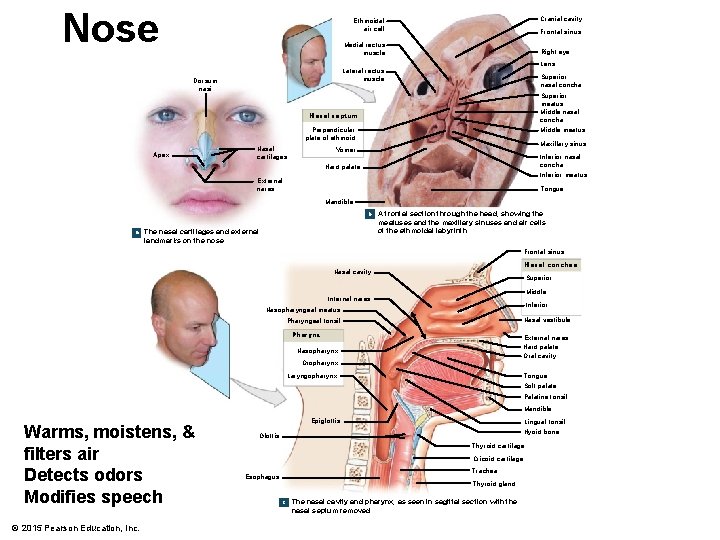
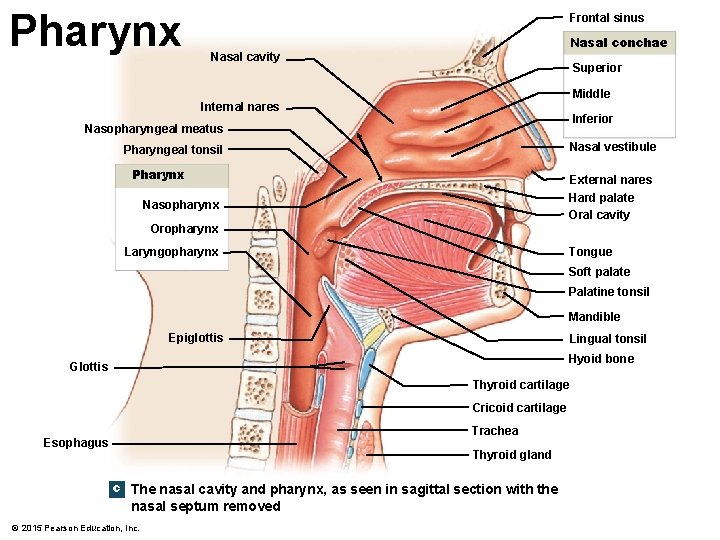
Nose Cranial cavity Ethmoidal air cell Frontal sinus Medial rectus muscle Right eye Lens Lateral rectus muscle Dorsum nasi Superior nasal concha Superior meatus Middle nasal concha Nasal septum Perpendicular plate of ethmoid Apex Nasal cartilages Middle meatus Maxillary sinus Vomer Inferior nasal concha Hard palate Inferior meatus External nares Tongue Mandible b a The nasal cartilages and external landmarks on the nose A frontal section through the head, showing the meatuses and the maxillary sinuses and air cells of the ethmoidal labyrinth Frontal sinus Nasal conchae Nasal cavity Superior Middle Internal nares Inferior Nasopharyngeal meatus Nasal vestibule Pharyngeal tonsil Pharynx External nares Hard palate Oral cavity Nasopharynx Oropharynx Laryngopharynx Tongue Soft palate Palatine tonsil Mandible Warms, moistens, & filters air Detects odors Modifies speech © 2015 Pearson Education, Inc. Epiglottis Lingual tonsil Hyoid bone Glottis Thyroid cartilage Cricoid cartilage Trachea Esophagus Thyroid gland c The nasal cavity and pharynx, as seen in sagittal section with the nasal septum removed
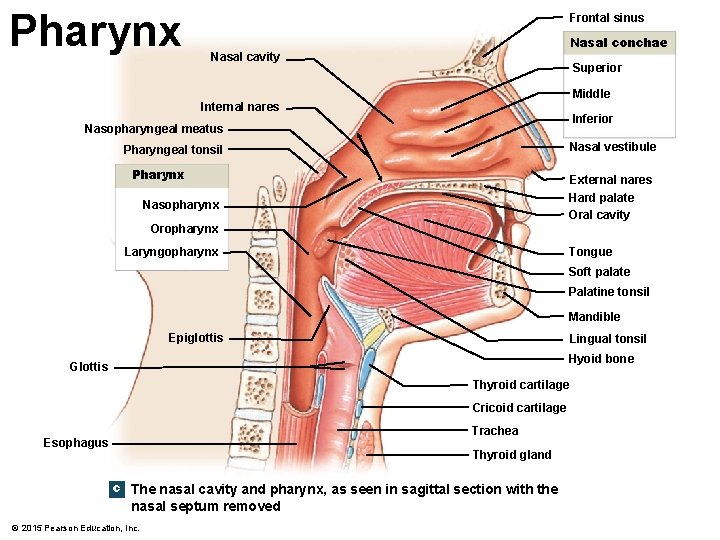
Pharynx Frontal sinus Nasal conchae Nasal cavity Superior Middle Internal nares Inferior Nasopharyngeal meatus Nasal vestibule Pharyngeal tonsil Pharynx External nares Hard palate Oral cavity Nasopharynx Oropharynx Laryngopharynx Tongue Soft palate Palatine tonsil Mandible Epiglottis Lingual tonsil Hyoid bone Glottis Thyroid cartilage Cricoid cartilage Trachea Esophagus Thyroid gland c The nasal cavity and pharynx, as seen in sagittal section with the nasal septum removed © 2015 Pearson Education, Inc.
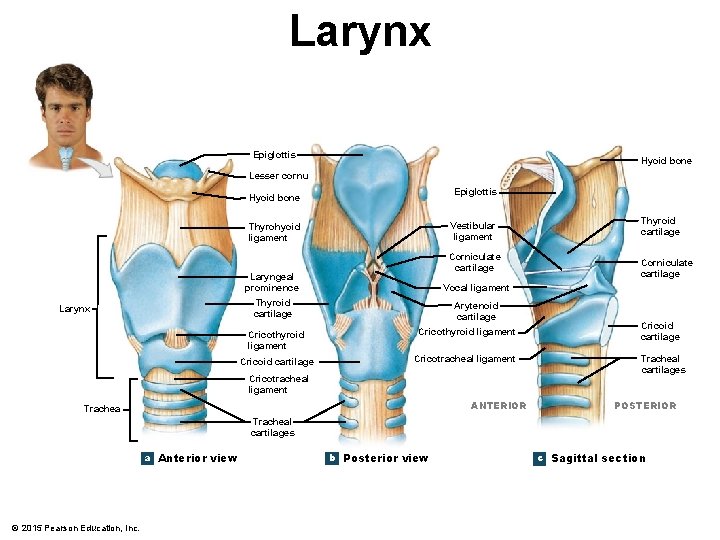
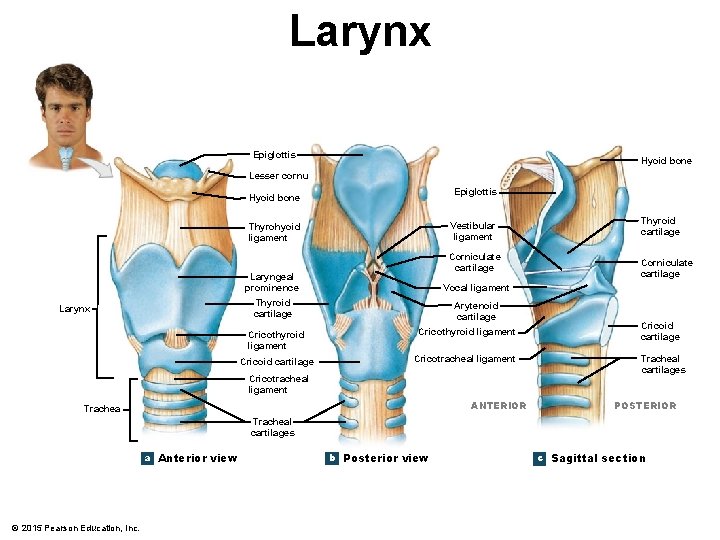
Larynx Epiglottis Hyoid bone Lesser cornu Epiglottis Hyoid bone Vestibular ligament Thyrohyoid ligament Larynx Corniculate cartilage Laryngeal prominence Vocal ligament Thyroid cartilage Arytenoid cartilage Cricothyroid ligament Cricoid cartilage Cricotracheal ligament ANTERIOR Trachea Thyroid cartilage Corniculate cartilage Cricoid cartilage Tracheal cartilages POSTERIOR Tracheal cartilages a Anterior view © 2015 Pearson Education, Inc. b Posterior view c Sagittal section
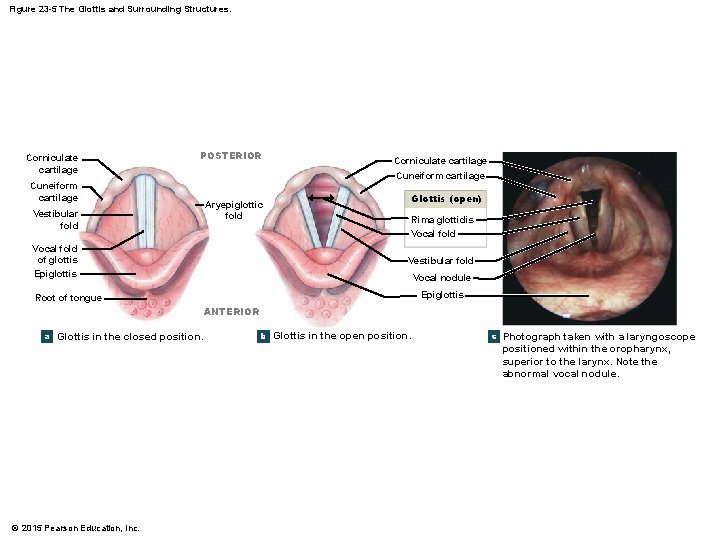
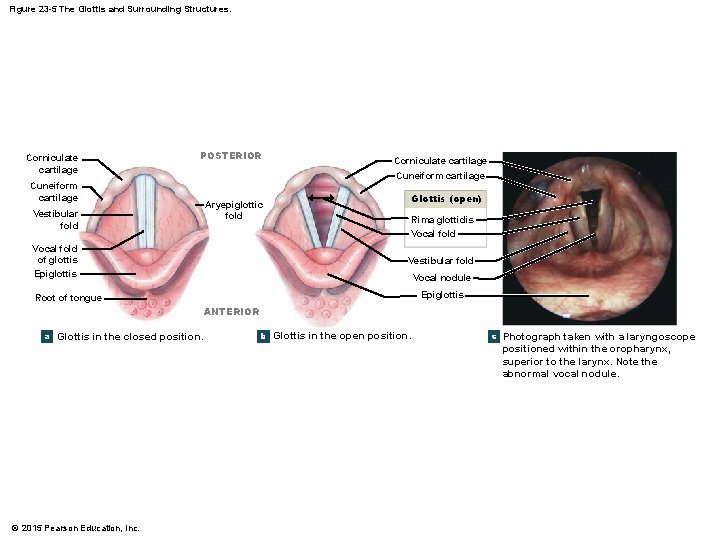
Figure 23 -5 The Glottis and Surrounding Structures. Corniculate cartilage POSTERIOR Corniculate cartilage Cuneiform cartilage Aryepiglottic fold Vestibular fold Vocal fold of glottis Epiglottis Glottis (open) Rima glottidis Vocal fold Vestibular fold Vocal nodule Epiglottis Root of tongue ANTERIOR a Glottis in the closed position. b Glottis in the open position. c Photograph taken with a laryngoscope positioned within the oropharynx, superior to the larynx. Note the abnormal vocal nodule. © 2015 Pearson Education, Inc.
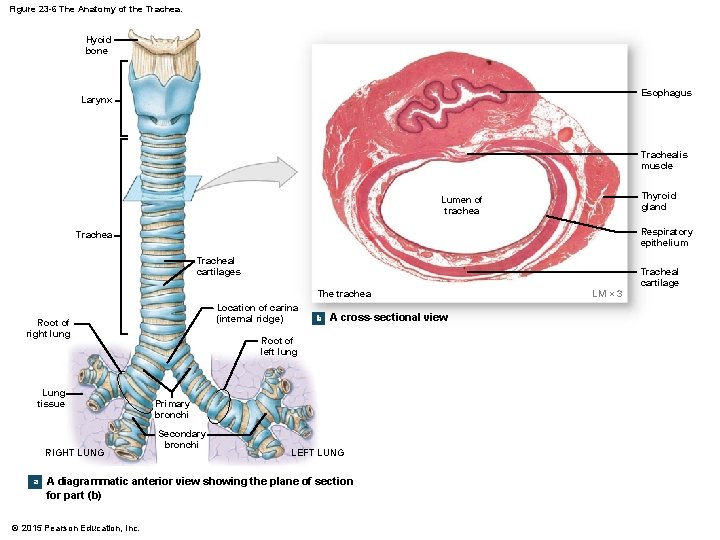
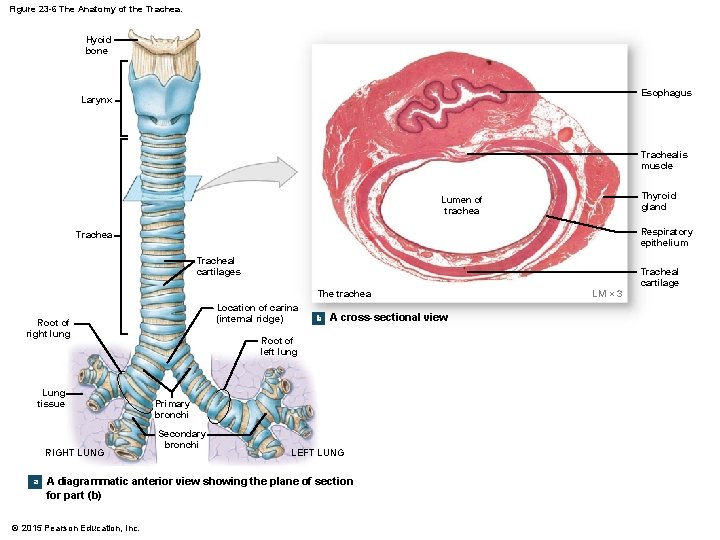
Figure 23 -6 The Anatomy of the Trachea. Hyoid bone Esophagus Larynx Trachealis muscle Thyroid gland Lumen of trachea Respiratory epithelium Tracheal cartilages The trachea Location of carina (internal ridge) Root of right lung Lung tissue RIGHT LUNG a b A cross-sectional view Root of left lung Primary bronchi Secondary bronchi LEFT LUNG A diagrammatic anterior view showing the plane of section for part (b) © 2015 Pearson Education, Inc. LM × 3 Tracheal cartilage
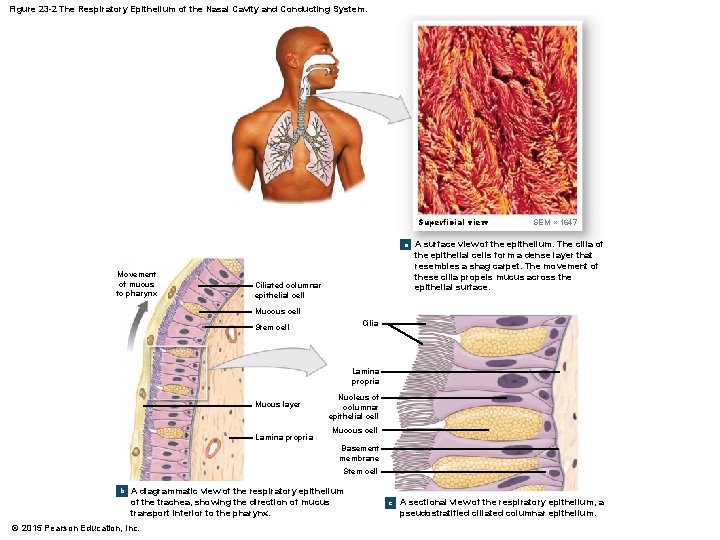
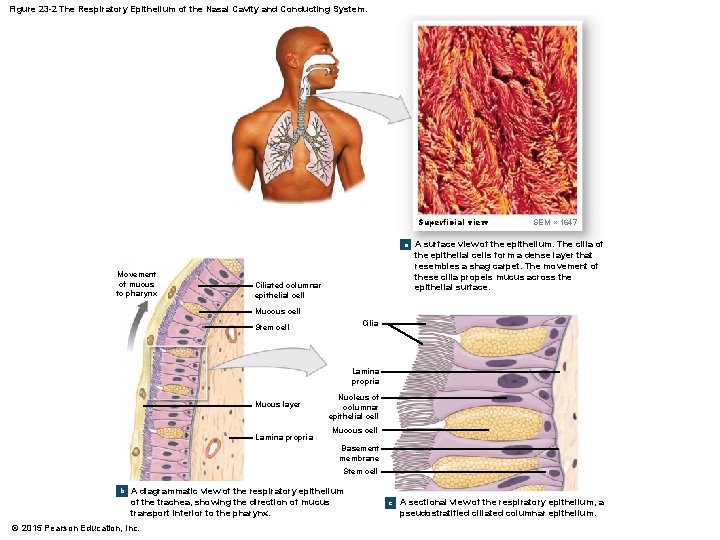
Figure 23 -2 The Respiratory Epithelium of the Nasal Cavity and Conducting System. Superficial view a Movement of mucus to pharynx Ciliated columnar epithelial cell SEM × 1647 A surface view of the epithelium. The cilia of the epithelial cells form a dense layer that resembles a shag carpet. The movement of these cilia propels mucus across the epithelial surface. Mucous cell Cilia Stem cell Lamina propria Mucus layer Lamina propria Nucleus of columnar epithelial cell Mucous cell Basement membrane Stem cell b A diagrammatic view of the respiratory epithelium of the trachea, showing the direction of mucus transport inferior to the pharynx. © 2015 Pearson Education, Inc. c A sectional view of the respiratory epithelium, a pseudostratified ciliated columnar epithelium.
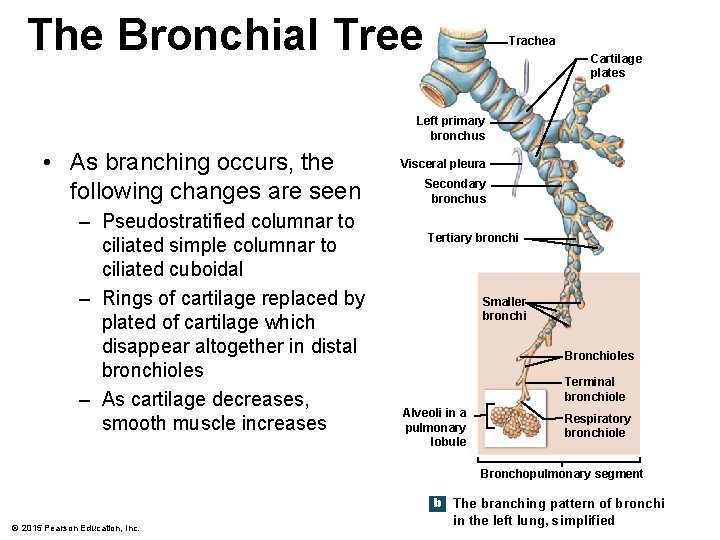
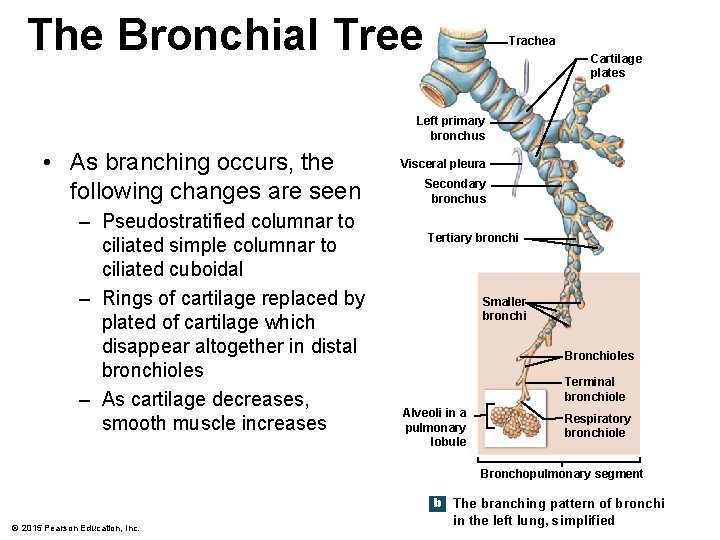
The Bronchial Tree Trachea Cartilage plates Left primary bronchus • As branching occurs, the following changes are seen – Pseudostratified columnar to ciliated simple columnar to ciliated cuboidal – Rings of cartilage replaced by plated of cartilage which disappear altogether in distal bronchioles – As cartilage decreases, smooth muscle increases Visceral pleura Secondary bronchus Tertiary bronchi Smaller bronchi Bronchioles Terminal bronchiole Alveoli in a pulmonary lobule Respiratory bronchiole Bronchopulmonary segment b The branching pattern of bronchi © 2015 Pearson Education, Inc. in the left lung, simplified
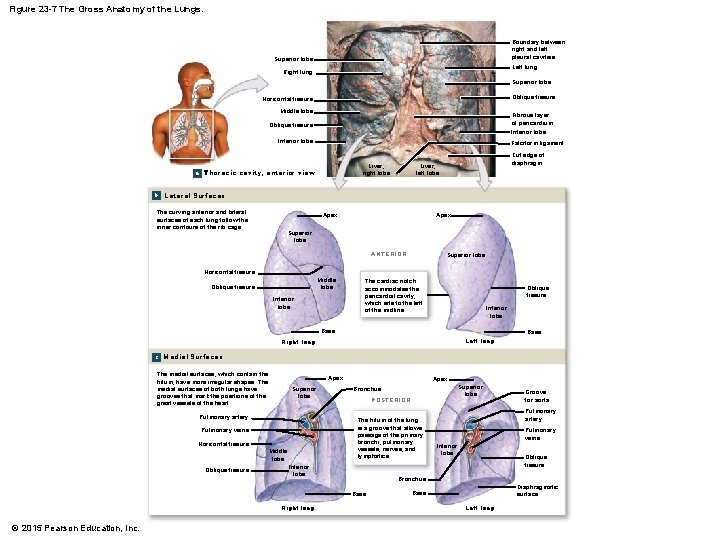
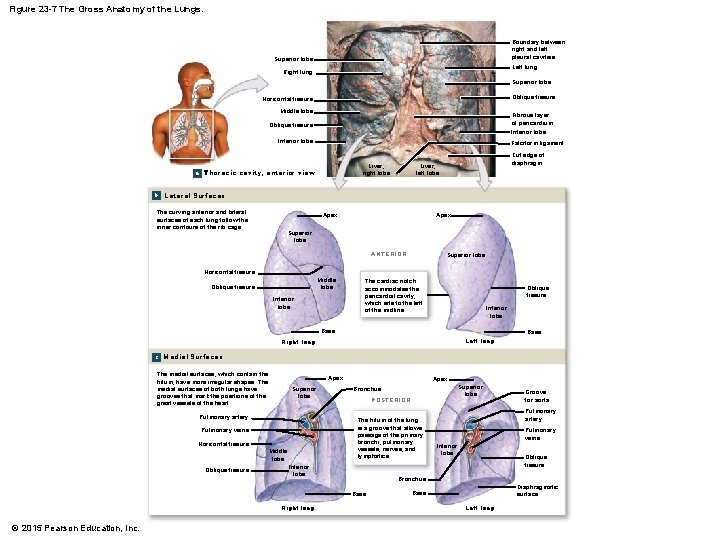
Figure 23 -7 The Gross Anatomy of the Lungs. Boundary between right and left pleural cavities Superior lobe Left lung Right lung Superior lobe Oblique fissure Horizontal fissure Middle lobe Fibrous layer of pericardium Oblique fissure Inferior lobe Falciform ligament Liver, right lobe a Thoracic cavity, anterior view Cut edge of diaphragm Liver, left lobe b Lateral Surfaces The curving anterior and lateral surfaces of each lung follow the inner contours of the rib cage. Apex Superior lobe ANTERIOR Superior lobe Horizontal fissure Middle lobe Oblique fissure Inferior lobe The cardiac notch accommodates the pericardial cavity, which sits to the left of the midline. Oblique fissure Inferior lobe Base Left lung Right lung c Medial Surfaces The medial surfaces, which contain the hilum, have more irregular shapes. The medial surfaces of both lungs have grooves that mark the positions of the great vessels of the heart. Apex Superior lobe Pulmonary artery Horizontal fissure Middle lobe Inferior lobe Right lung Groove for aorta Pulmonary artery Pulmonary veins Inferior lobe Oblique fissure Bronchus Base © 2015 Pearson Education, Inc. Superior lobe POSTERIOR The hilum of the lung is a groove that allows passage of the primary bronchi, pulmonary vessels, nerves, and lymphatics. Pulmonary veins Oblique fissure Apex Bronchus Diaphragmatic surface Base Left lung
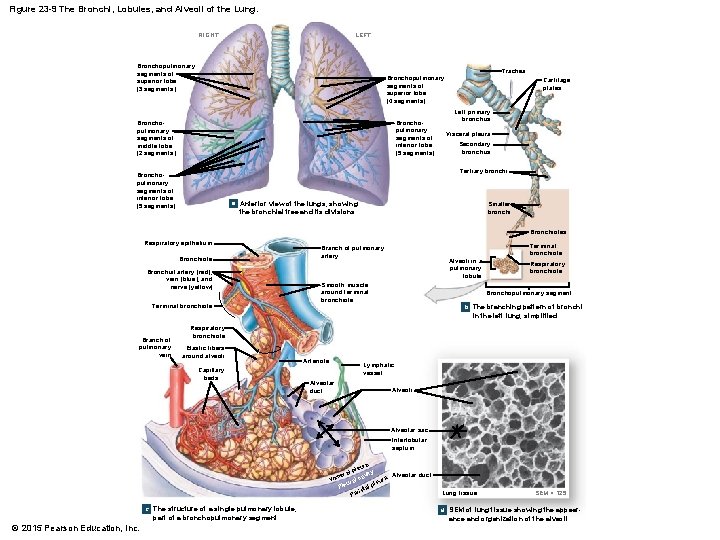
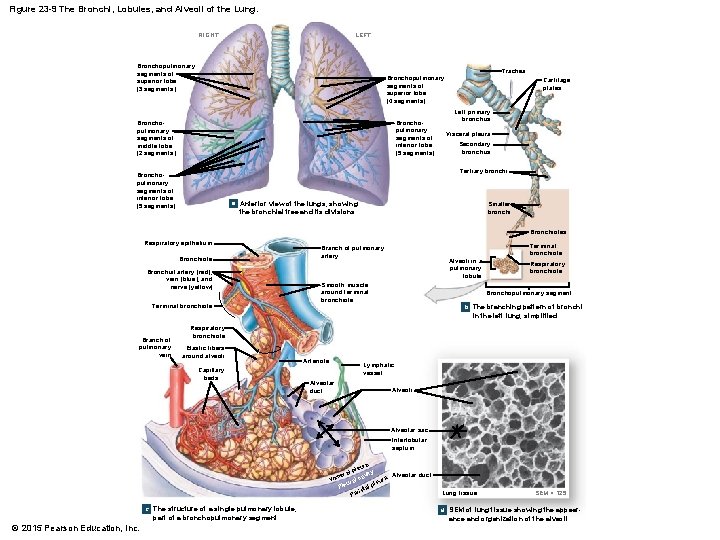
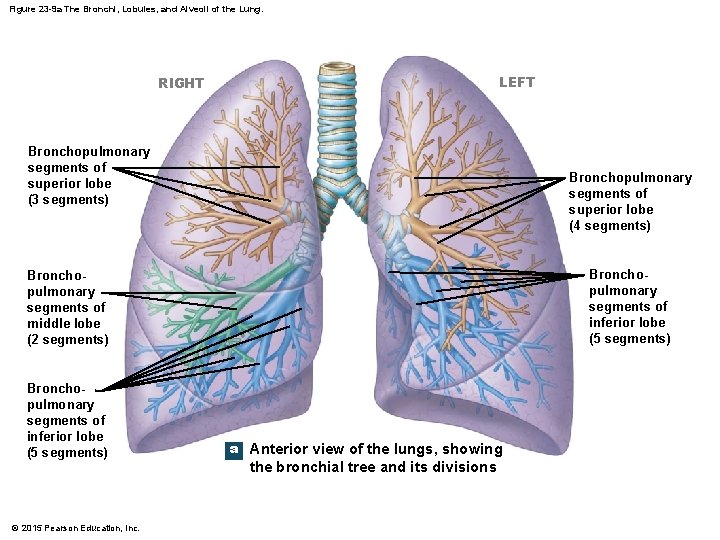
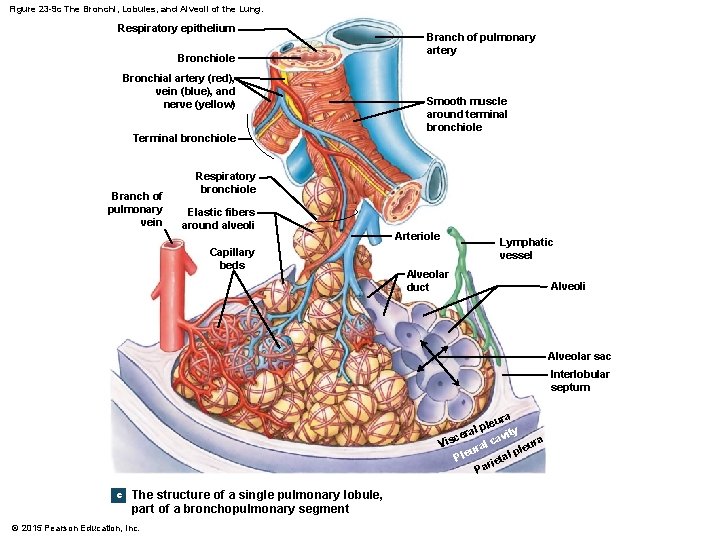
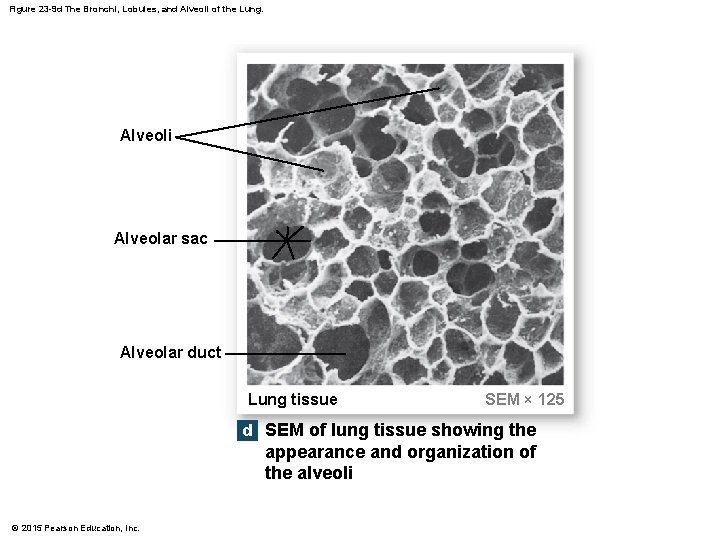
Figure 23 -9 The Bronchi, Lobules, and Alveoli of the Lung. LEFT RIGHT Bronchopulmonary segments of superior lobe (3 segments) Trachea Bronchopulmonary segments of superior lobe (4 segments) Bronchopulmonary segments of inferior lobe (5 segments) Bronchopulmonary segments of middle lobe (2 segments) Cartilage plates Left primary bronchus Visceral pleura Secondary bronchus Tertiary bronchi Bronchopulmonary segments of inferior lobe (5 segments) a Anterior view of the lungs, showing Smaller bronchi the bronchial tree and its divisions Bronchioles Respiratory epithelium Bronchiole Bronchial artery (red), vein (blue), and nerve (yellow) Terminal bronchiole Branch of pulmonary artery Alveoli in a pulmonary lobule Smooth muscle around terminal bronchiole Respiratory bronchiole Bronchopulmonary segment b The branching pattern of bronchi in the left lung, simplified Branch of pulmonary vein Respiratory bronchiole Elastic fibers around alveoli Capillary beds Arteriole Lymphatic vessel Alveolar duct Alveoli Alveolar sac Interlobular septum a eur l pl ity Alveolar duct era v c a s lc Vi ura ple e l P al t e ri Pa c The structure of a single pulmonary lobule, part of a bronchopulmonary segment © 2015 Pearson Education, Inc. Lung tissue SEM × 125 d SEM of lung tissue showing the appear- ance and organization of the alveoli
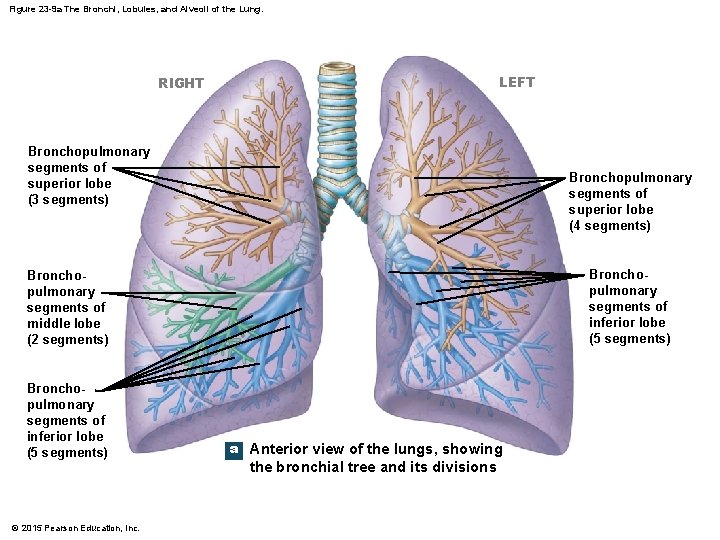
Figure 23 -9 a The Bronchi, Lobules, and Alveoli of the Lung. LEFT RIGHT Bronchopulmonary segments of superior lobe (3 segments) Bronchopulmonary segments of superior lobe (4 segments) Bronchopulmonary segments of inferior lobe (5 segments) Bronchopulmonary segments of middle lobe (2 segments) Bronchopulmonary segments of inferior lobe (5 segments) © 2015 Pearson Education, Inc. a Anterior view of the lungs, showing the bronchial tree and its divisions
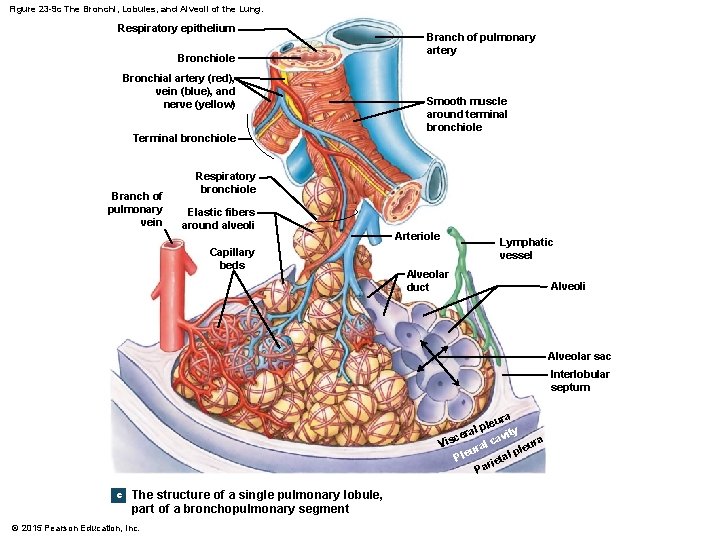
Figure 23 -9 c The Bronchi, Lobules, and Alveoli of the Lung. Respiratory epithelium Bronchiole Bronchial artery (red), vein (blue), and nerve (yellow) Terminal bronchiole Branch of pulmonary vein Branch of pulmonary artery Smooth muscle around terminal bronchiole Respiratory bronchiole Elastic fibers around alveoli Capillary beds Arteriole Lymphatic vessel Alveolar duct Alveoli Alveolar sac Interlobular septum ura ple ty l a i cer cav ra Vis l a leu ur p e l l P ta rie Pa c The structure of a single pulmonary lobule, part of a bronchopulmonary segment © 2015 Pearson Education, Inc.
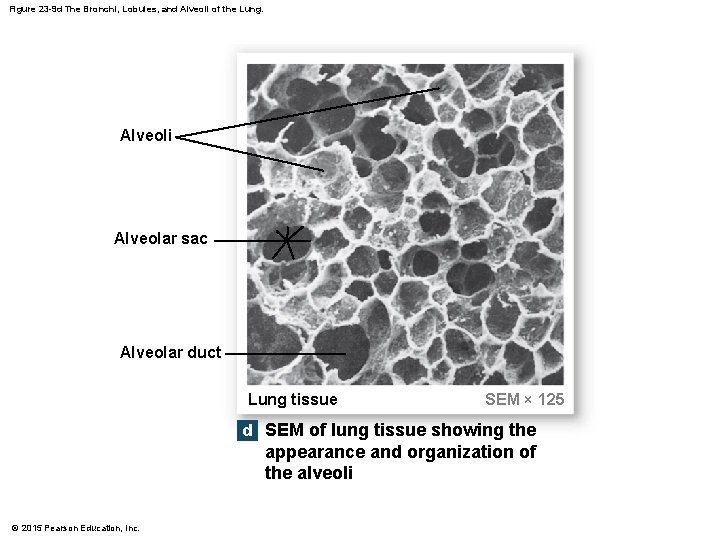
Figure 23 -9 d The Bronchi, Lobules, and Alveoli of the Lung. Alveoli Alveolar sac Alveolar duct Lung tissue SEM × 125 d SEM of lung tissue showing the appearance and organization of the alveoli © 2015 Pearson Education, Inc.
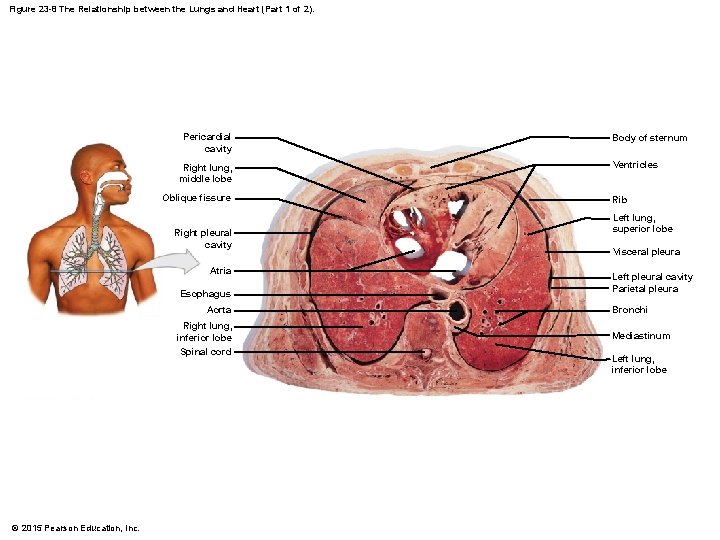
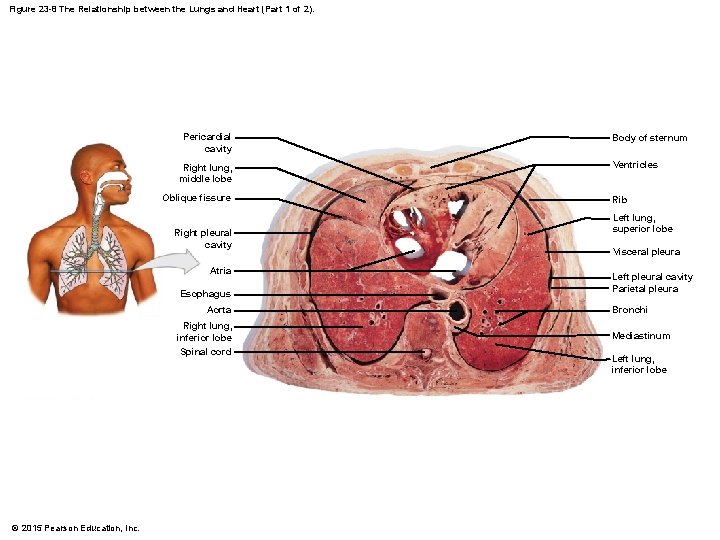
Figure 23 -8 The Relationship between the Lungs and Heart (Part 1 of 2). Pericardial cavity Right lung, middle lobe Oblique fissure Right pleural cavity Atria Esophagus Aorta Right lung, inferior lobe Spinal cord © 2015 Pearson Education, Inc. Body of sternum Ventricles Rib Left lung, superior lobe Visceral pleura Left pleural cavity Parietal pleura Bronchi Mediastinum Left lung, inferior lobe
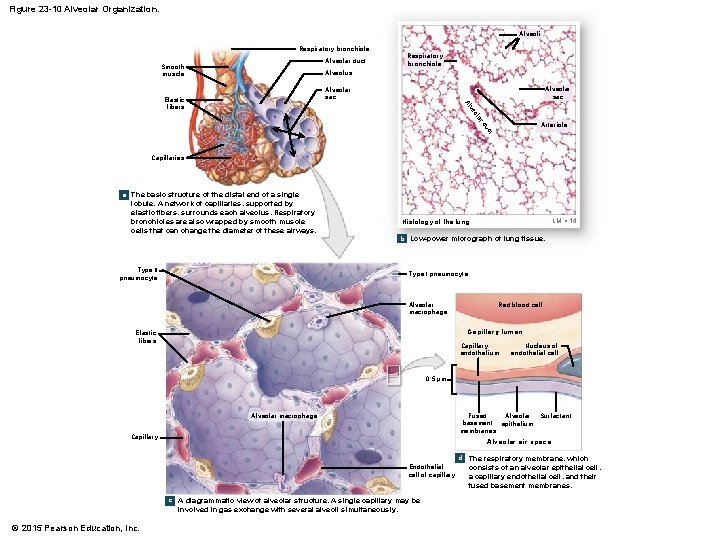
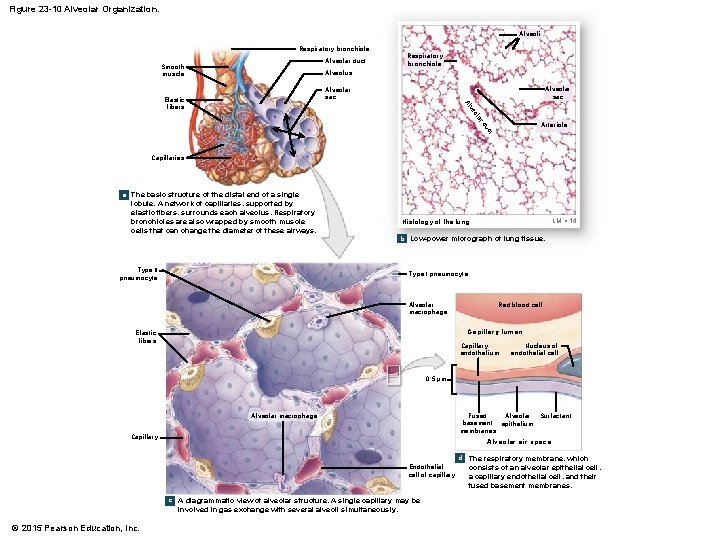
Figure 23 -10 Alveolar Organization. Alveoli Respiratory bronchiole Alveolar duct Smooth muscle Respiratory bronchiole Alveolus Alveolar sac ar ol ve Al Elastic fibers ct du Arteriole Capillaries a The basic structure of the distal end of a single lobule. A network of capillaries, supported by elastic fibers, surrounds each alveolus. Respiratory bronchioles are also wrapped by smooth muscle cells that can change the diameter of these airways. Type II pneumocyte LM × 14 Histology of the lung b Low-power micrograph of lung tissue. Type I pneumocyte Alveolar macrophage Red blood cell Capillary lumen Elastic fibers Capillary endothelium Nucleus of endothelial cell 0. 5 μm Alveolar macrophage Fused Alveolar Surfactant basement epithelium membranes Capillary Alveolar air space d The respiratory membrane, which Endothelial cell of capillary c A diagrammatic view of alveolar structure. A single capillary may be involved in gas exchange with several alveoli simultaneously. © 2015 Pearson Education, Inc. consists of an alveolar epithelial cell, a capillary endothelial cell, and their fused basement membranes.
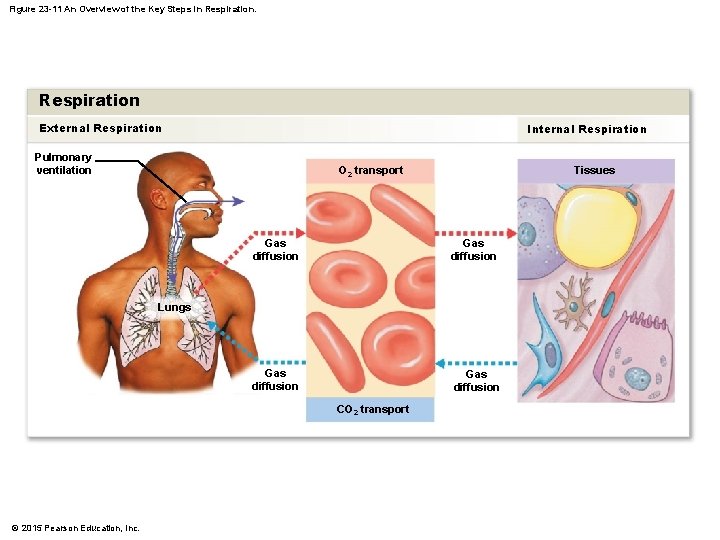
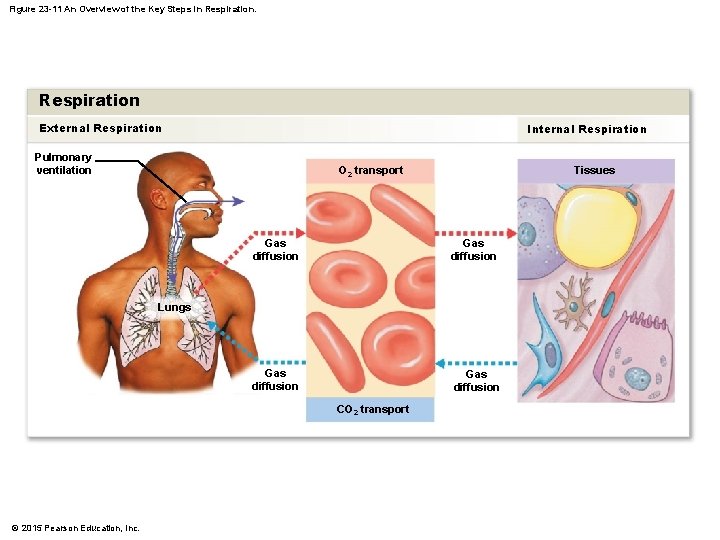
Figure 23 -11 An Overview of the Key Steps in Respiration External Respiration Internal Respiration Pulmonary ventilation O 2 transport Tissues Gas diffusion Lungs CO 2 transport © 2015 Pearson Education, Inc.
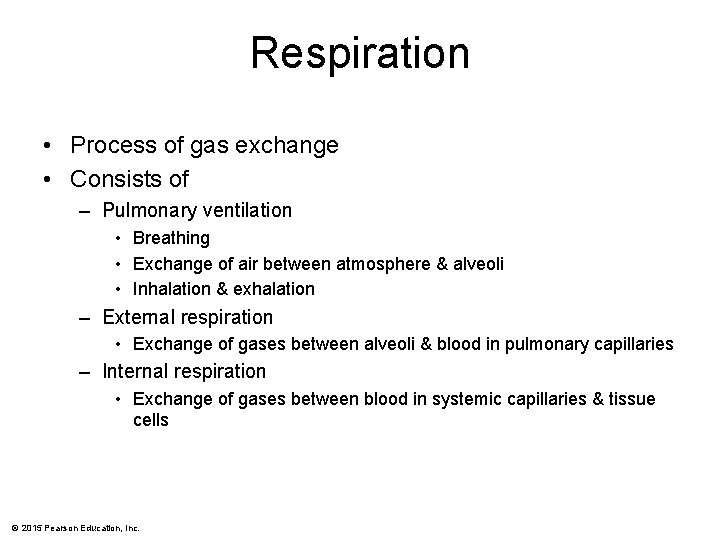
Respiration • Process of gas exchange • Consists of – Pulmonary ventilation • Breathing • Exchange of air between atmosphere & alveoli • Inhalation & exhalation – External respiration • Exchange of gases between alveoli & blood in pulmonary capillaries – Internal respiration • Exchange of gases between blood in systemic capillaries & tissue cells © 2015 Pearson Education, Inc.
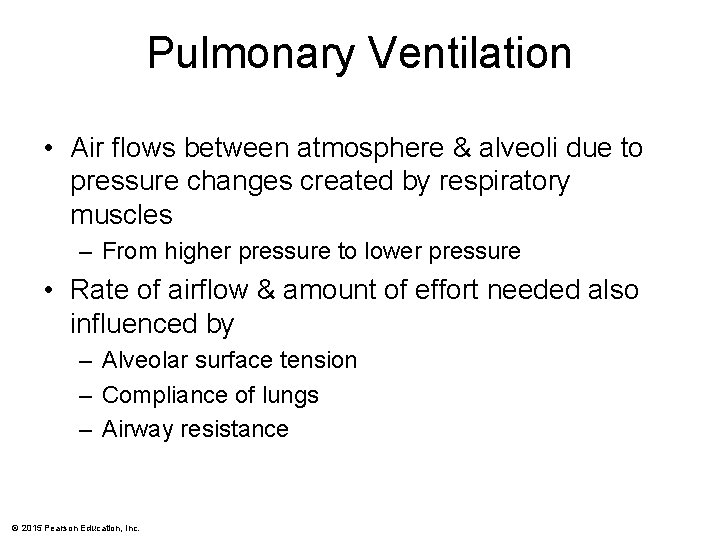
Pulmonary Ventilation • Air flows between atmosphere & alveoli due to pressure changes created by respiratory muscles – From higher pressure to lower pressure • Rate of airflow & amount of effort needed also influenced by – Alveolar surface tension – Compliance of lungs – Airway resistance © 2015 Pearson Education, Inc.
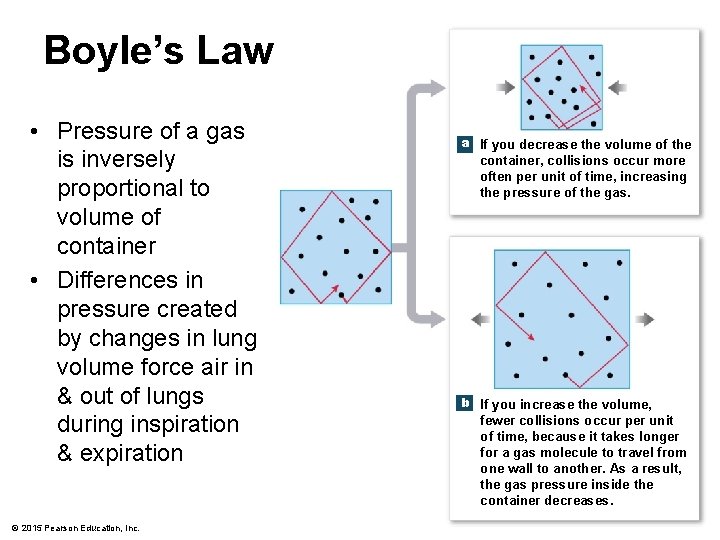
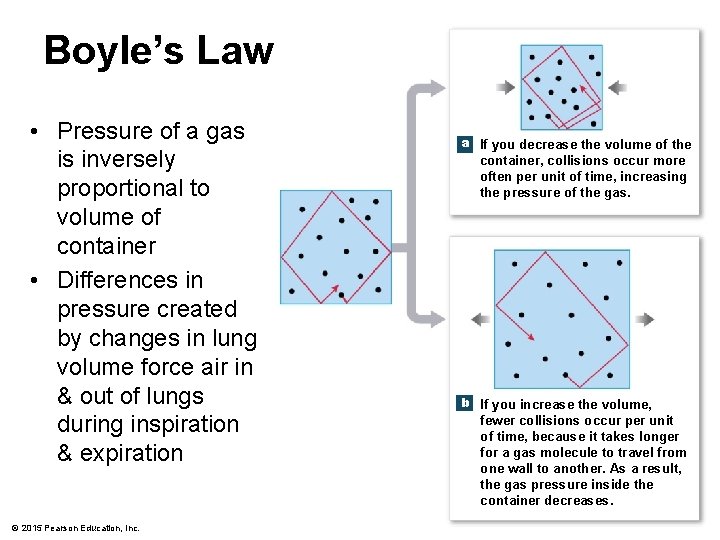
Boyle’s Law • Pressure of a gas is inversely proportional to volume of container • Differences in pressure created by changes in lung volume force air in & out of lungs during inspiration & expiration © 2015 Pearson Education, Inc. a If you decrease the volume of the container, collisions occur more often per unit of time, increasing the pressure of the gas. b If you increase the volume, fewer collisions occur per unit of time, because it takes longer for a gas molecule to travel from one wall to another. As a result, the gas pressure inside the container decreases.
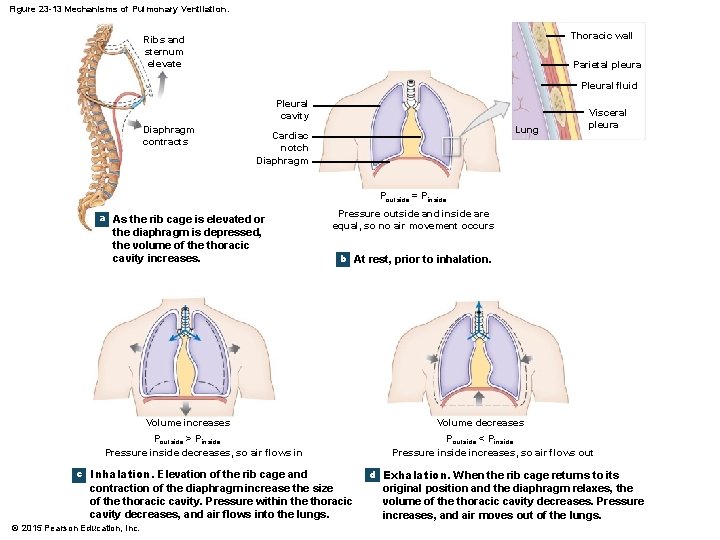
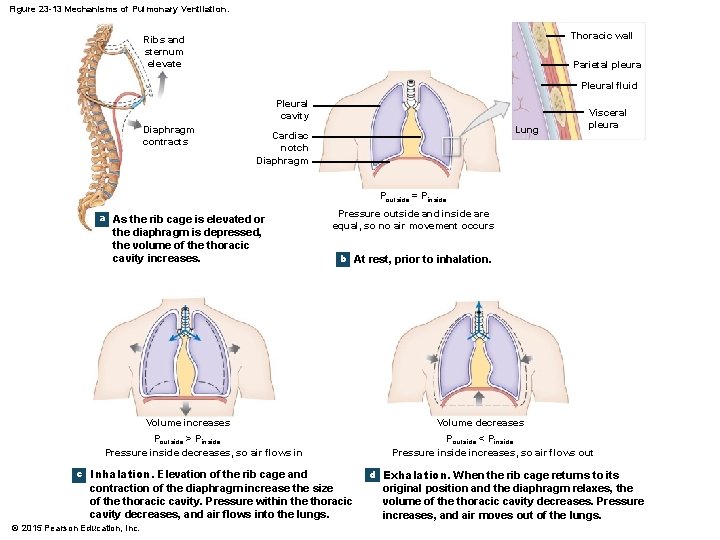
Figure 23 -13 Mechanisms of Pulmonary Ventilation. Thoracic wall Ribs and sternum elevate Parietal pleura Pleural fluid Pleural cavity Diaphragm contracts Lung Cardiac notch Diaphragm Visceral pleura Poutside = Pinside a As the rib cage is elevated or the diaphragm is depressed, the volume of the thoracic cavity increases. Pressure outside and inside are equal, so no air movement occurs b At rest, prior to inhalation. Volume increases Poutside > Pinside Pressure inside decreases, so air flows in c Inhalation. Elevation of the rib cage and contraction of the diaphragm increase the size of the thoracic cavity. Pressure within the thoracic cavity decreases, and air flows into the lungs. © 2015 Pearson Education, Inc. Volume decreases Poutside < Pinside Pressure inside increases, so air flows out d Exhalation. When the rib cage returns to its original position and the diaphragm relaxes, the volume of the thoracic cavity decreases. Pressure increases, and air moves out of the lungs.
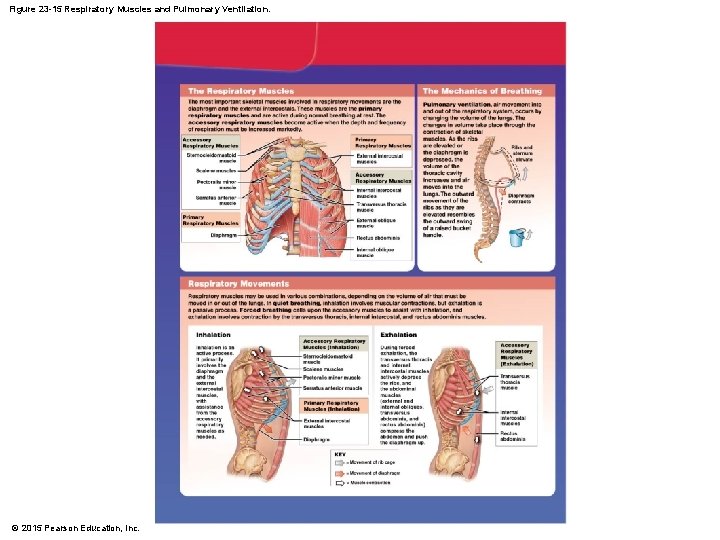
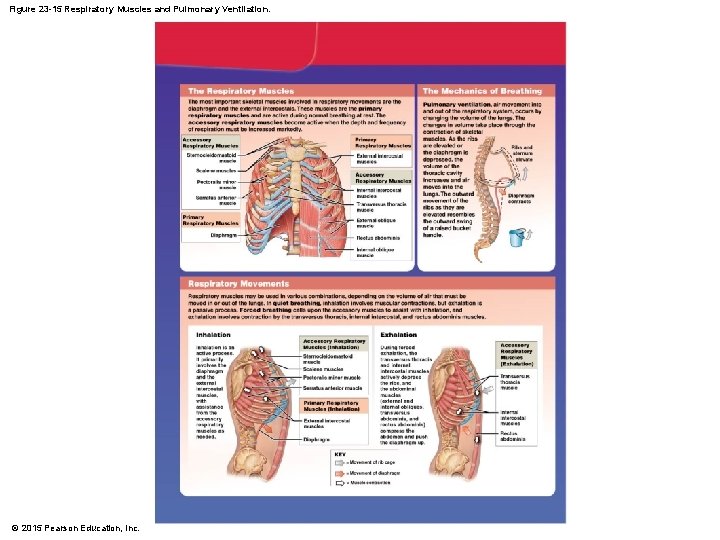
Figure 23 -15 Respiratory Muscles and Pulmonary Ventilation. © 2015 Pearson Education, Inc.
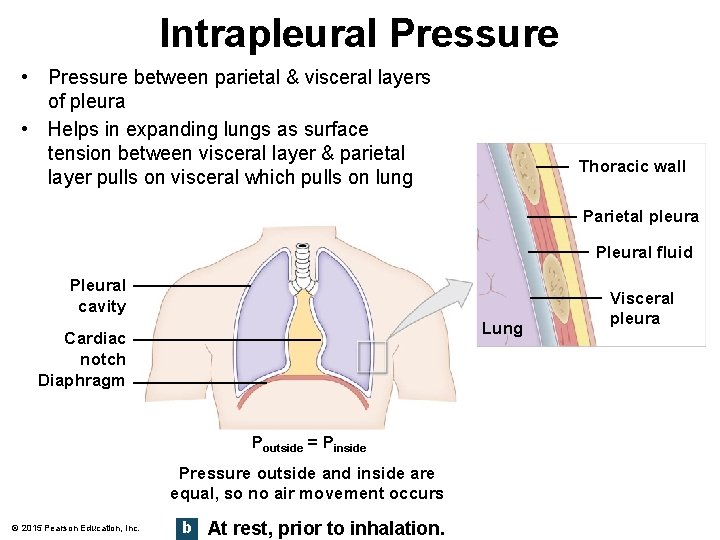
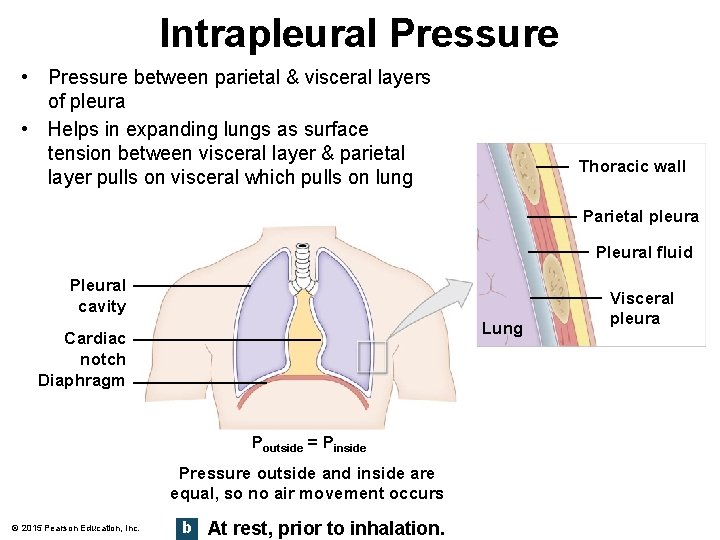
Intrapleural Pressure • Pressure between parietal & visceral layers of pleura • Helps in expanding lungs as surface tension between visceral layer & parietal layer pulls on visceral which pulls on lung Thoracic wall Parietal pleura Pleural fluid Pleural cavity Lung Cardiac notch Diaphragm Poutside = Pinside Pressure outside and inside are equal, so no air movement occurs © 2015 Pearson Education, Inc. b At rest, prior to inhalation. Visceral pleura
Other Factors Affecting Breathing • Surface tension – Alveolar fluid creates surface tension – H 2 O molecules more strongly attracted to each other than to air & so produces an inward force – Causes alveoli to assume smallest diameter possible – Must be overcome during inhalation – Accounts for 2/3 of elastic recoil – Surfactant reduces surface tension • Compliance • Airway resistance © 2015 Pearson Education, Inc.
Other Factors Affecting Breathing • Surface tension • Compliance – – Effort needed to stretch lungs & chest wall High means expand easily & low means they resist expansion Related to elasticity & surface tension Normally have high compliance because elastic fibers in lungs allow for easy stretch & surfactant reduces surface tension – Decreased compliance when • • There is scar tissue (TB) There is edema (pulmonary edema) There is a deficit of surfactant There is anything that can impede expansion (paralysis or loss of elasticity) • Airway resistance © 2015 Pearson Education, Inc.
Other Factors Affecting Breathing • Surface tension • Compliance • Airway resistance – Related to diameter of airways or obstructions in airways – Larger the diameter, the less resistance to airflow © 2015 Pearson Education, Inc.
Breathing Patterns • Eupnea – Normal quiet breathing • Dyspnea – Difficult or labored breathing • Costal breathing – Shallow breathing • Diaphragmatic breathing – Deep breathing © 2015 Pearson Education, Inc. • Modified respiratory movements include – – – – Laughing Crying Coughing Sneezing Yawning Sighing Hiccupping
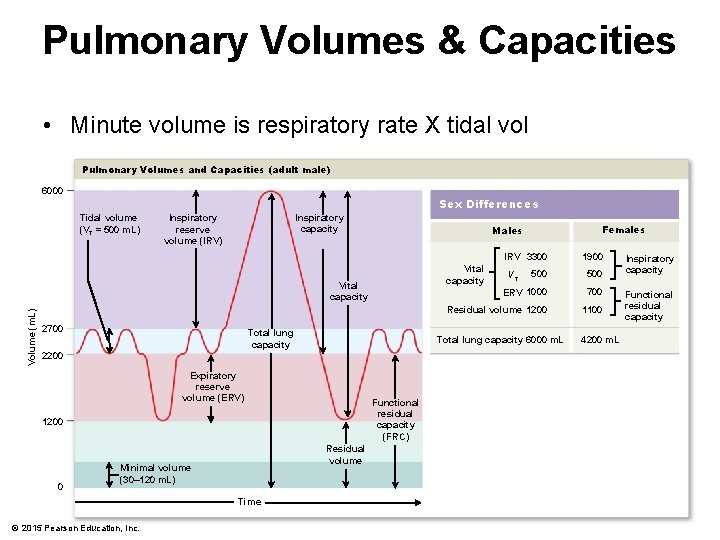
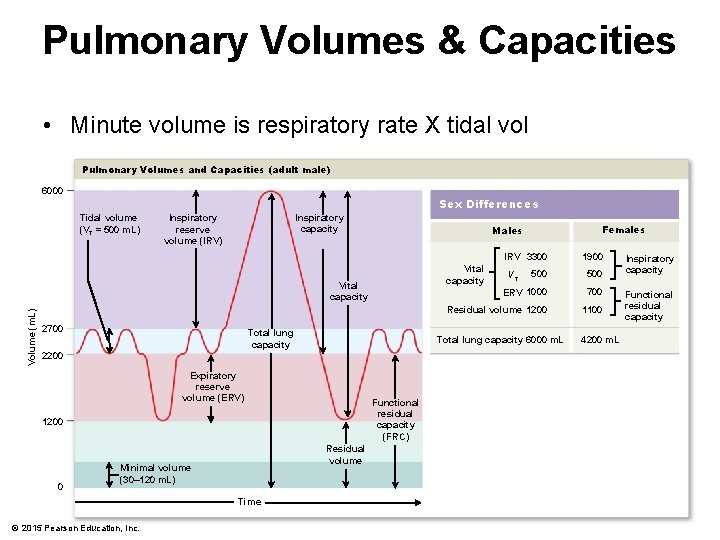
Pulmonary Volumes & Capacities • Minute volume is respiratory rate X tidal vol Pulmonary Volumes and Capacities (adult male) 6000 Sex Differences Tidal volume (VT = 500 m. L) Inspiratory capacity Inspiratory reserve volume (IRV) Volume (m. L) Total lung capacity Expiratory reserve volume (ERV) Functional residual capacity (FRC) 1200 0 Residual volume Time © 2015 Pearson Education, Inc. 1900 500 ERV 1000 700 Residual volume 1200 1100 VT Total lung capacity 6000 m. L 2200 Minimal volume (30– 120 m. L) IRV 3300 Vital capacity 2700 Females Males 4200 m. L Inspiratory capacity Functional residual capacity
Exchange of O 2 & CO 2 • Passive diffusion governed by 2 gas laws – Dalton’s • In a mixture of gases, each gas exerts its own pressure as if no other gases were present • Called partial pressure – Henry’s • Quantity of gas that will dissolve in a liquid is proportional to partial pressure of gas & its solubility • CO 2 is much more soluble in plasma than O 2 © 2015 Pearson Education, Inc.
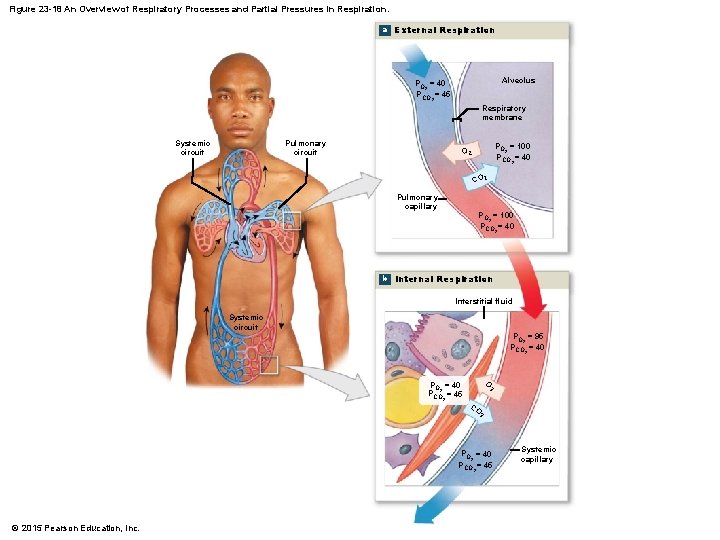
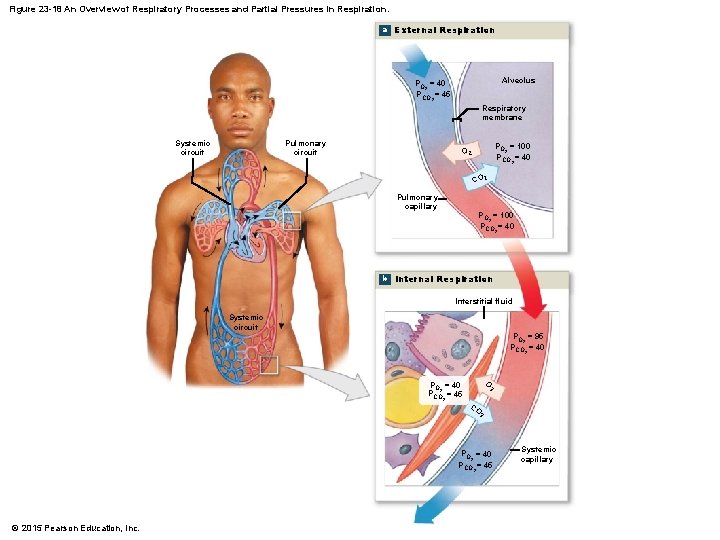
Figure 23 -18 An Overview of Respiratory Processes and Partial Pressures in Respiration. a External Respiration Alveolus PO = 40 2 PCO = 45 2 Respiratory membrane Systemic circuit Pulmonary circuit PO = 100 2 PCO = 40 O 2 2 CO 2 Pulmonary capillary PO = 100 2 PCO = 40 2 b Internal Respiration Interstitial fluid Systemic circuit PO = 95 2 PCO = 40 2 O PO = 40 2 PCO = 45 2 2 CO 2 PO = 40 2 PCO = 45 2 © 2015 Pearson Education, Inc. Systemic capillary
Rate of Exchange • Depends on – Partial pressure differences of gases • Larger the difference the faster the diffusion – Surface area available for exchange • Any decrease in surface area of respiratory membrane slow rate of exchange – Diffusion distance • As distances increases, rate slows – Molecular weight & solubility of gases • O 2 has lower molecular weight but CO 2 is far more soluble than O 2 © 2015 Pearson Education, Inc.
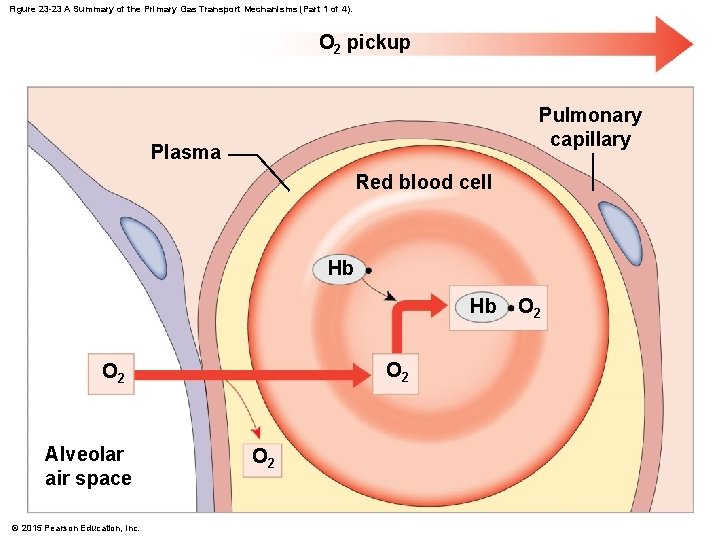
O 2 Transport • Since O 2 doesn’t dissolve in water easily, only about 1. 5% is dissolved in plasma • Most O 2 is carried by Hgb – O 2 binding site is on Fe 2+ so each Hgb can carry maximum of 4 O 2 © 2015 Pearson Education, Inc.
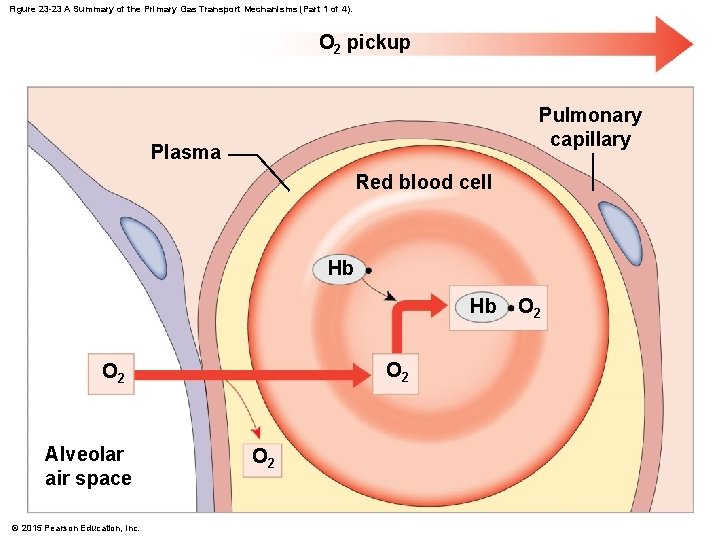
Figure 23 -23 A Summary of the Primary Gas Transport Mechanisms (Part 1 of 4). O 2 pickup Pulmonary capillary Plasma Red blood cell Hb Hb O 2 Alveolar air space © 2015 Pearson Education, Inc. O 2
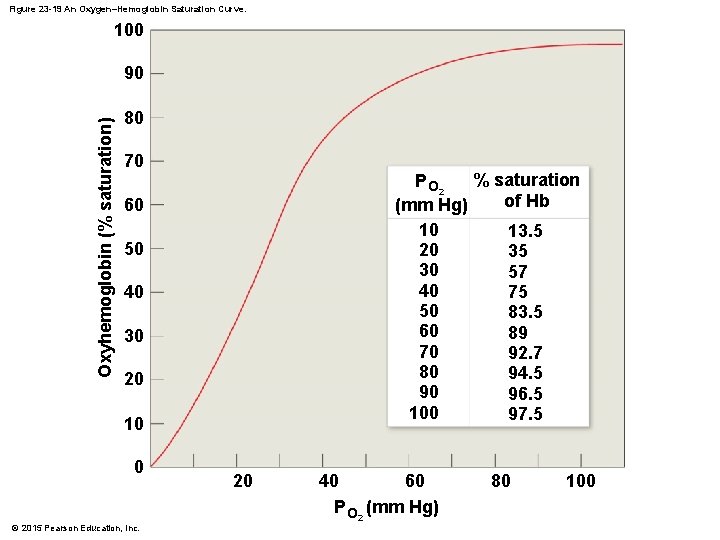
Hgb Affinity for O 2 • Most important factor that determines how much O 2 binds to Hgb is the p. O 2 – The higher the p. O 2 the more O 2 combines with Hgb © 2015 Pearson Education, Inc.
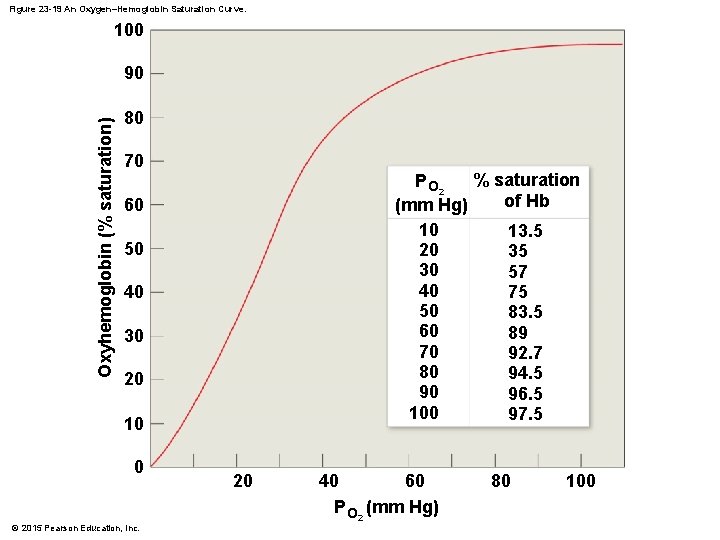
Figure 23 -19 An Oxygen–Hemoglobin Saturation Curve. 100 Oxyhemoglobin (% saturation) 90 80 70 % saturation P O 2 of Hb (mm Hg) 10 13. 5 20 35 30 57 40 75 50 83. 5 60 89 70 92. 7 80 94. 5 90 96. 5 100 97. 5 60 50 40 30 20 10 0 © 2015 Pearson Education, Inc. 20 40 60 P O 2 (mm Hg) 80 100
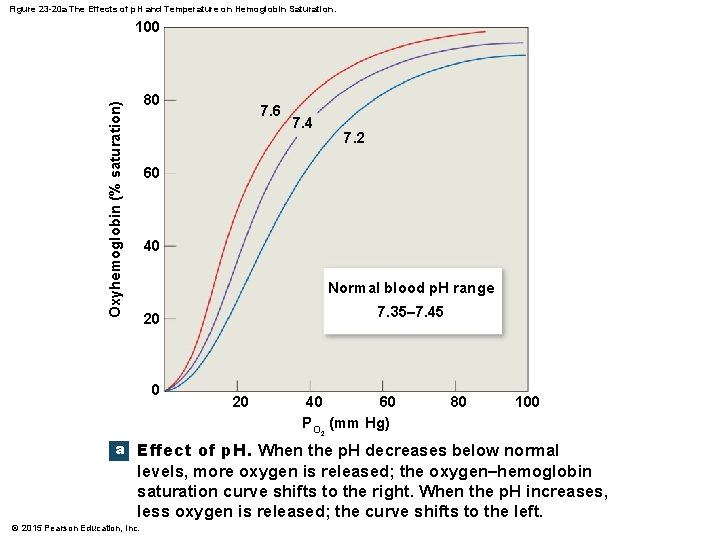
Hgb Affinity for O 2 • Most important factor that determines how much O 2 binds to Hgb is the p. O 2 • Acidity (p. H) – As acidity increases, affinity of Hgb for O 2 decreases & O 2 dissociates more readily © 2015 Pearson Education, Inc.
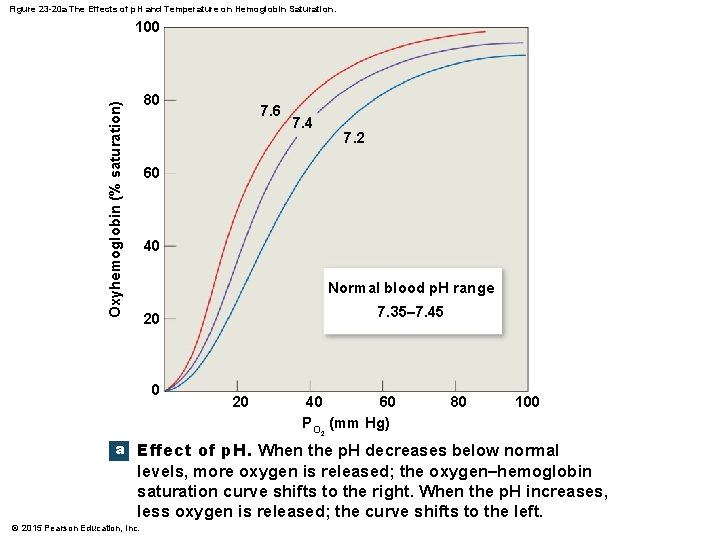
Figure 23 -20 a The Effects of p. H and Temperature on Hemoglobin Saturation. 100 Oxyhemoglobin (% saturation) 80 7. 6 7. 4 7. 2 60 40 Normal blood p. H range 7. 35– 7. 45 20 0 20 40 60 P O 2 (mm Hg) 80 100 a Effect of p. H. When the p. H decreases below normal levels, more oxygen is released; the oxygen–hemoglobin saturation curve shifts to the right. When the p. H increases, less oxygen is released; the curve shifts to the left. © 2015 Pearson Education, Inc.
Hgb Affinity for O 2 • Most important factor that determines how much O 2 binds to Hgb is the p. O 2 • Acidity (p. H) • p. CO 2 – As p. CO 2 rises, Hgb releases O 2 more readily – p. CO 2 & p. H are related as low blood p. H results from high p. CO 2 CA – CO 2 + H 2 O H 2 CO 3 H+ + HCO 3 - © 2015 Pearson Education, Inc.
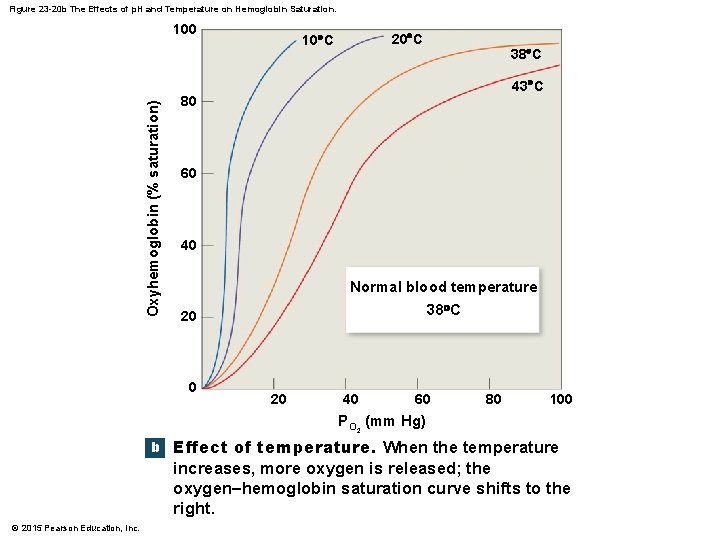
Hgb Affinity for O 2 • Most important factor that determines how much O 2 binds to Hgb is the p. O 2 • Acidity (p. H) • p. CO 2 • Temperature – As temperature increases, Hgb releases more O 2 © 2015 Pearson Education, Inc.
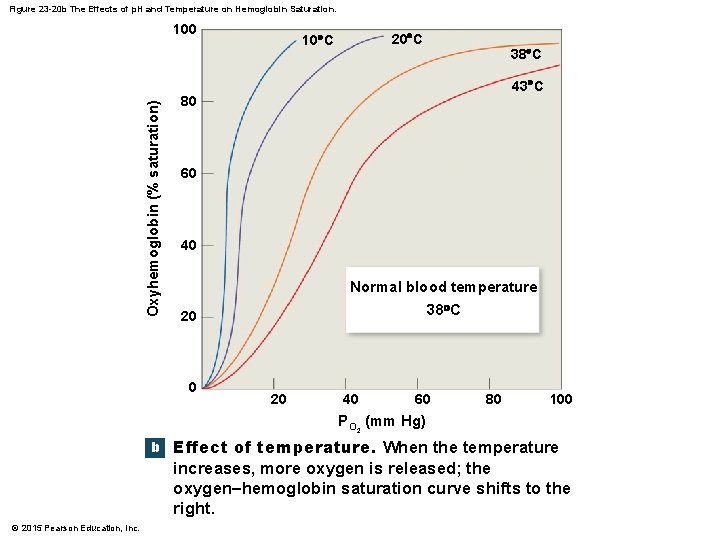
Figure 23 -20 b The Effects of p. H and Temperature on Hemoglobin Saturation. Oxyhemoglobin (% saturation) 100 20 C 10 C 38 C 43 C 80 60 40 Normal blood temperature 38 C 20 0 20 40 60 80 100 P O 2 (mm Hg) b Effect of temperature. When the temperature increases, more oxygen is released; the oxygen–hemoglobin saturation curve shifts to the right. © 2015 Pearson Education, Inc.
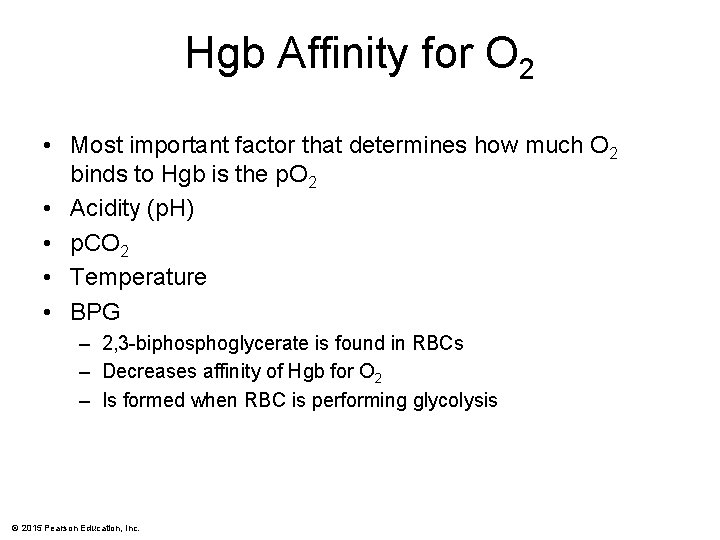
Hgb Affinity for O 2 • Most important factor that determines how much O 2 binds to Hgb is the p. O 2 • Acidity (p. H) • p. CO 2 • Temperature • BPG – 2, 3 -biphosphoglycerate is found in RBCs – Decreases affinity of Hgb for O 2 – Is formed when RBC is performing glycolysis © 2015 Pearson Education, Inc.
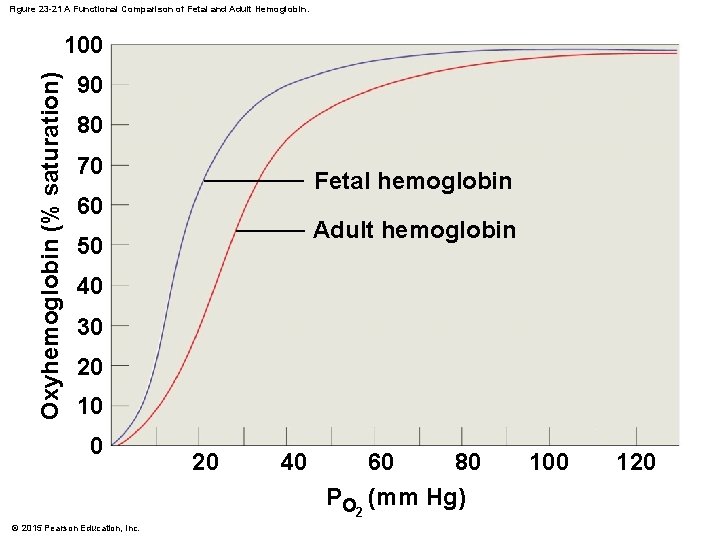
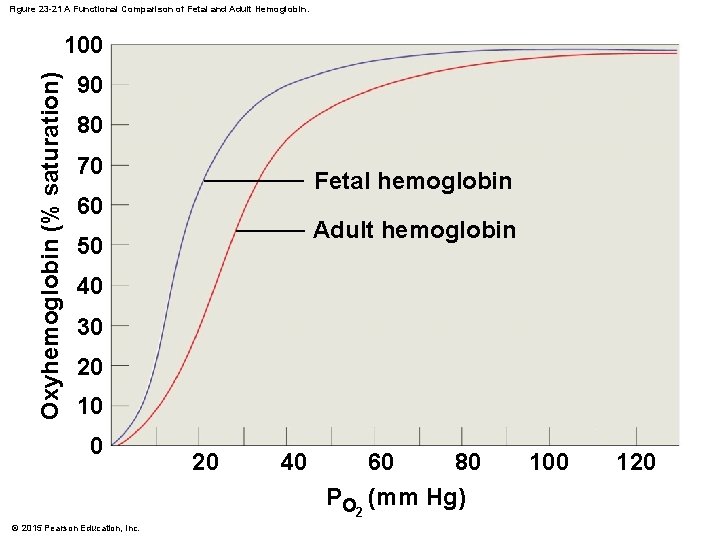
Figure 23 -21 A Functional Comparison of Fetal and Adult Hemoglobin. Oxyhemoglobin (% saturation) 100 90 80 70 Fetal hemoglobin 60 Adult hemoglobin 50 40 30 20 10 0 © 2015 Pearson Education, Inc. 20 40 60 80 PO 2 (mm Hg) 100 120
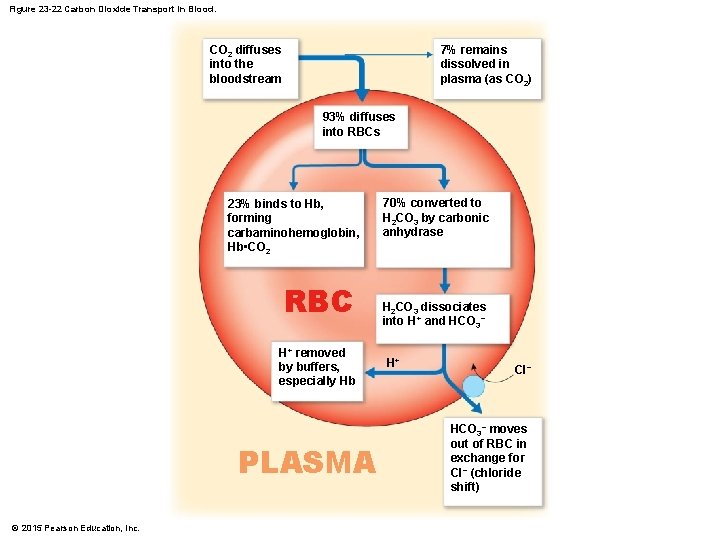
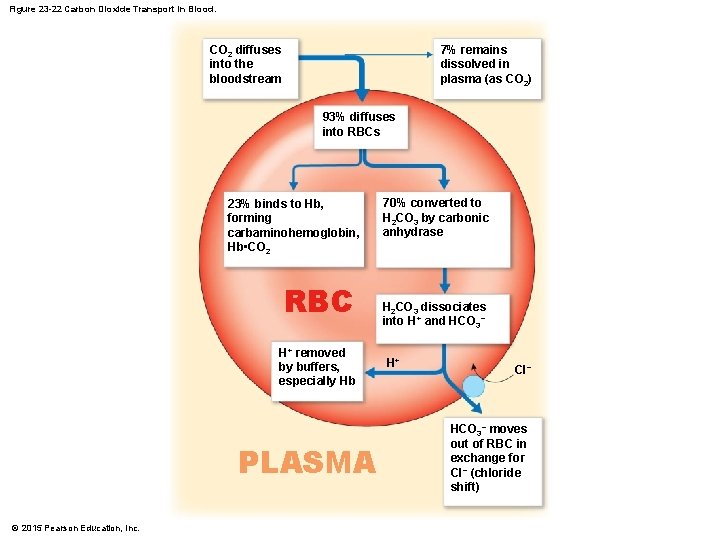
Figure 23 -22 Carbon Dioxide Transport in Blood. CO 2 diffuses into the bloodstream 7% remains dissolved in plasma (as CO 2) 93% diffuses into RBCs 23% binds to Hb, forming carbaminohemoglobin, Hb • CO 2 RBC H+ removed by buffers, especially Hb PLASMA © 2015 Pearson Education, Inc. 70% converted to H 2 CO 3 by carbonic anhydrase H 2 CO 3 dissociates into H+ and HCO 3− H+ Cl− HCO 3− moves out of RBC in exchange for Cl− (chloride shift)

Figure 23 -23 A Summary of the Primary Gas Transport Mechanisms. O 2 delivery O 2 pickup Pulmonary capillary Plasma Systemic capillary Red blood cell Hb Hb Hb O 2 O 2 Alveolar air space O 2 O 2 Hb Cells in peripheral tissues O 2 HCO 3− Cl− Alveolar air space HCO 3− Hb Hb H+ + HCO 3− Hb H+ H 2 CO 3 CO 2 Hb H 2 O CO 2 delivery CO 2 H 2 O Hb CO 2 Hb Pulmonary capillary © 2015 Pearson Education, Inc. H+ Hb Hb Cl− H+ + HCO 3− Chloride shift CO 2 Cells in peripheral tissues Systemic capillary CO 2 pickup
Respiratory Center • Located in the brainstem • 2 main areas – Medullary respiratory center • Dorsal respiratory group (DRG) • Ventral respiratory group (VRG) © 2015 Pearson Education, Inc.
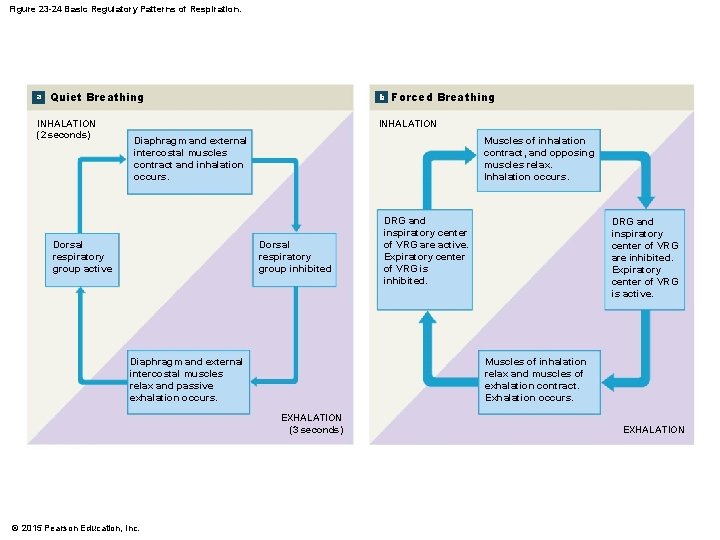
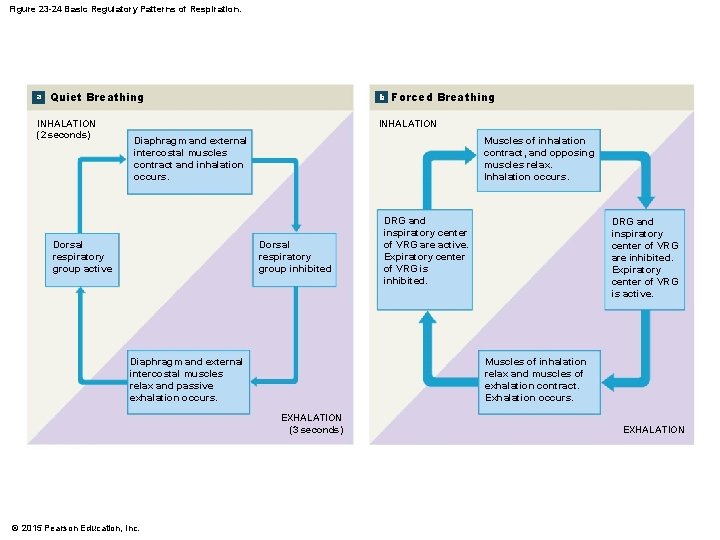
Figure 23 -24 Basic Regulatory Patterns of Respiration. a Quiet Breathing INHALATION (2 seconds) b Forced Breathing INHALATION Muscles of inhalation contract, and opposing muscles relax. Inhalation occurs. Diaphragm and external intercostal muscles contract and inhalation occurs. Dorsal respiratory group active Dorsal respiratory group inhibited Diaphragm and external intercostal muscles relax and passive exhalation occurs. DRG and inspiratory center of VRG are inhibited. Expiratory center of VRG is active. Muscles of inhalation relax and muscles of exhalation contract. Exhalation occurs. EXHALATION (3 seconds) © 2015 Pearson Education, Inc. DRG and inspiratory center of VRG are active. Expiratory center of VRG is inhibited. EXHALATION
Respiratory Center • Located in the brainstem • 2 main areas – Medullary respiratory center • Dorsal respiratory group (DRG) • Ventral respiratory group (VRG) – Pontine respiratory group • • Formerly known as pneumotaxic area Active during inhalation & exhalation Transmits impulses to DRG Modifies basic rhythm © 2015 Pearson Education, Inc.
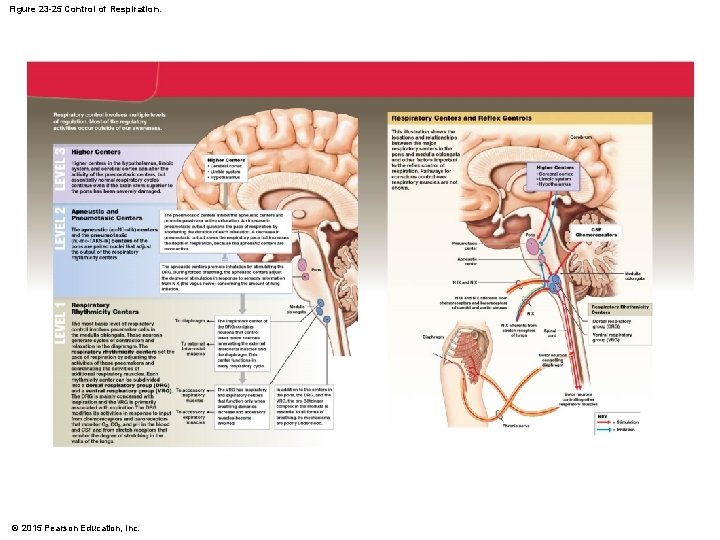
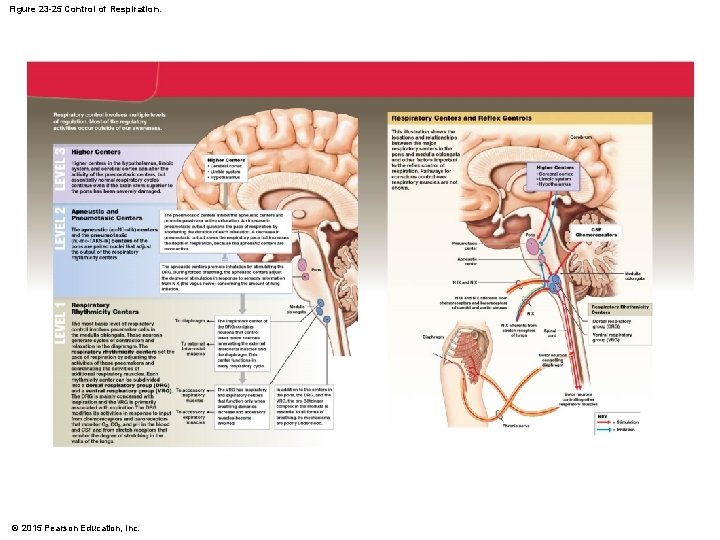
Figure 23 -25 Control of Respiration. © 2015 Pearson Education, Inc.
Cortical Influences on Breathing • Involves cerebral cortex, hypothalamus, & limbic system • Can voluntarily alter pattern of breathing • Limited though by buildup of CO 2 & H+ © 2015 Pearson Education, Inc.
Chemoreceptor Regulation • Central chemoreceptors – In or near medulla – Respond to changes in H+ or p. CO 2 in CSF • Peripheral chemoreceptors – Located in aortic bodies & carotid bodies – Respond to changes in H+, p. CO 2, & p. O 2 © 2015 Pearson Education, Inc.
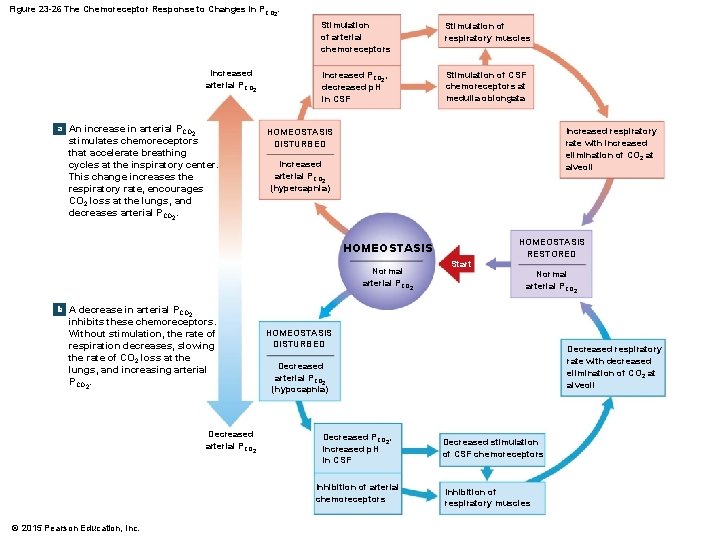
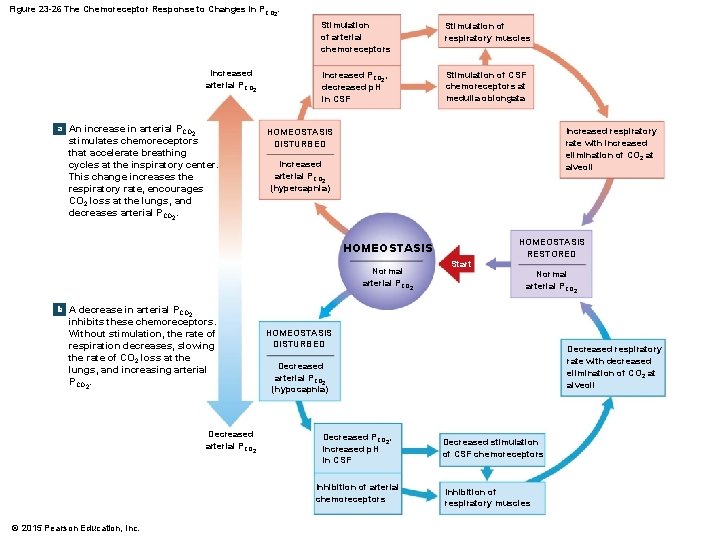
Figure 23 -26 The Chemoreceptor Response to Changes in PCO 2. Increased arterial PCO 2 a An increase in arterial PCO 2 stimulates chemoreceptors that accelerate breathing cycles at the inspiratory center. This change increases the respiratory rate, encourages CO 2 loss at the lungs, and decreases arterial PCO 2. Stimulation of arterial chemoreceptors Stimulation of respiratory muscles Increased PCO 2, decreased p. H in CSF Stimulation of CSF chemoreceptors at medulla oblongata Increased respiratory rate with increased elimination of CO 2 at alveoli HOMEOSTASIS DISTURBED Increased arterial PCO 2 (hypercapnia) HOMEOSTASIS Normal arterial PCO 2 Start HOMEOSTASIS RESTORED Normal arterial PCO 2 b A decrease in arterial PCO 2 inhibits these chemoreceptors. Without stimulation, the rate of respiration decreases, slowing the rate of CO 2 loss at the lungs, and increasing arterial PCO 2. Decreased arterial PCO 2 HOMEOSTASIS DISTURBED Decreased arterial PCO 2 (hypocapnia) Decreased PCO 2, increased p. H in CSF Inhibition of arterial chemoreceptors © 2015 Pearson Education, Inc. Decreased respiratory rate with decreased elimination of CO 2 at alveoli Decreased stimulation of CSF chemoreceptors Inhibition of respiratory muscles
Other Influences on Breathing • Proprioceptors – As you begin to exercise, proprioceptors send signals to DRG to increase rate & depth of breathing • Inflation reflex – Stretch receptors in walls of bronchi & bronchioles if overstretched will send impulses via CN X to DRG & inhibit it so inhalation stops & exhalation begins – Aka Hering-Breuer reflex • Limbic system – Anticipation of activity or emotional anxiety send input to DRG to increase rate & depth • Temperature – Increase in temp, increases rate • Pain – Sharp causes brief apnea – Prolonged causes increase • Stretching anal sphincter – Increases rate • Irritation of airways – Immediate cessation • Blood pressure – Sudden rise decreases rate & vice versa © 2015 Pearson Education, Inc.
Hypoxia • Deficiency of O 2 at the tissue level • Hypoxic hypoxia – Caused by low p. O 2 in arterial blood due to high altitude, airway obstruction, fluid in lungs • Anemic hypoxia – Not enough Hgb – Hemorrhage, anemia, CO poisoning • Ischemic hypoxia – Blood flow to tissue is reduced • Histotoxic hypoxia – Action of some toxic agent at tissue such as cyanide © 2015 Pearson Education, Inc.
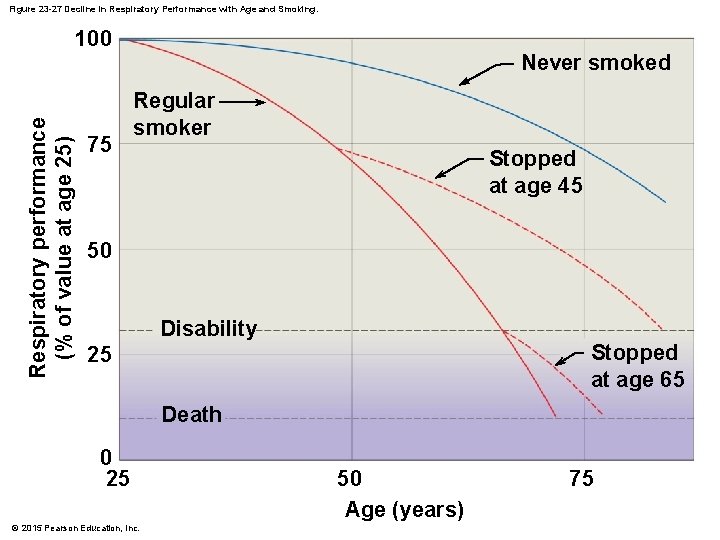
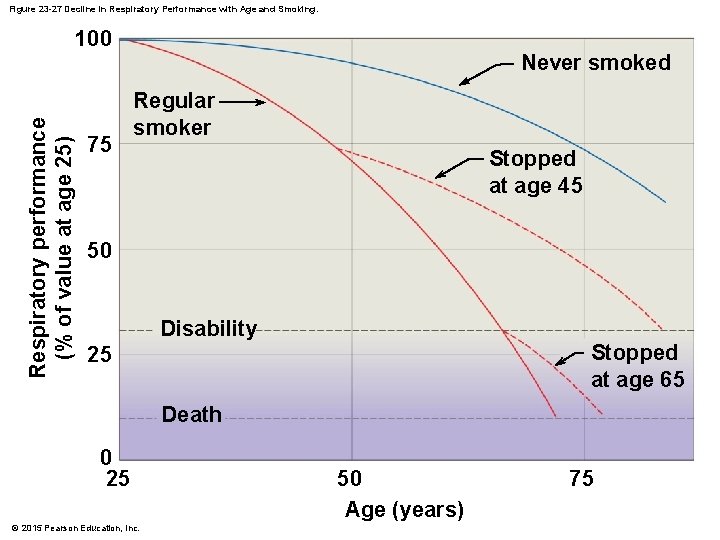
Figure 23 -27 Decline in Respiratory Performance with Age and Smoking. Respiratory performance (% of value at age 25) 100 75 Never smoked Regular smoker Stopped at age 45 50 Disability Stopped at age 65 25 Death 0 25 © 2015 Pearson Education, Inc. 50 Age (years) 75
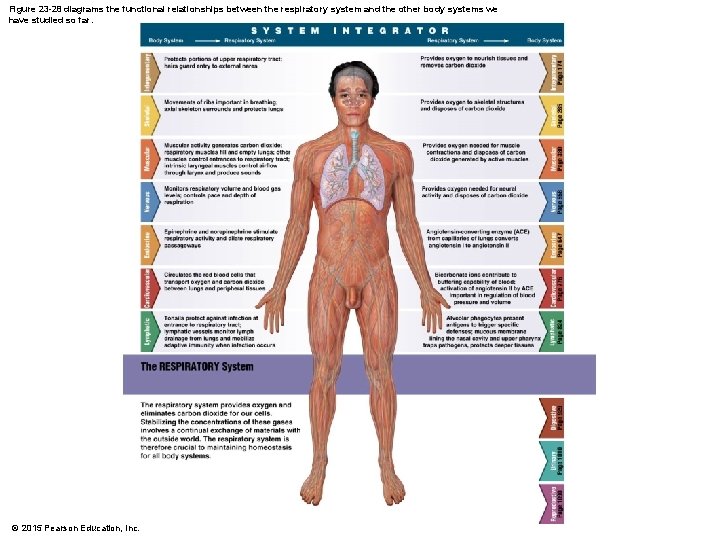
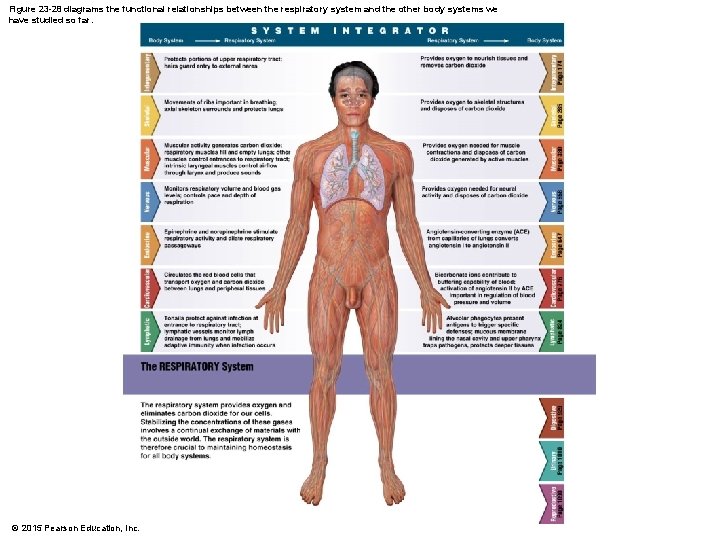
Figure 23 -28 diagrams the functional relationships between the respiratory system and the other body systems we have studied so far. © 2015 Pearson Education, Inc.