Chapter 22 Processes Stages of Labor and Birth
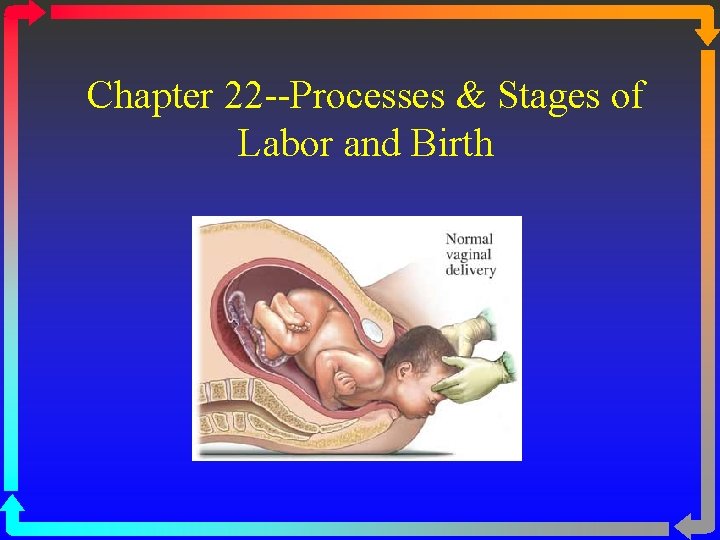
Chapter 22 --Processes & Stages of Labor and Birth
Critical Factors In Labor • The Four P’s: passage, passenger, powers & psyche • Passage: • adequate pelvis? • cephalopelvic disproportion (CPD) • Suspect if presenting part does not engage in pelvis (0 station)
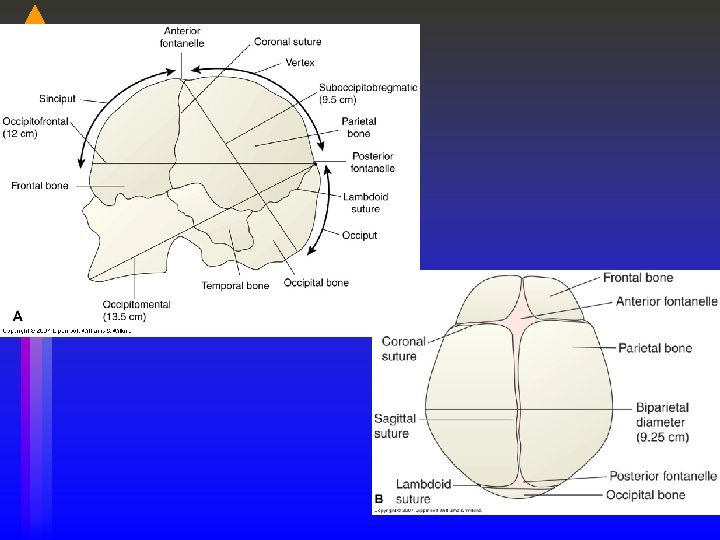
Passenger • The fetus: head is largest diameter • Fetal head: 4 bones with 3 membranous interspaces (sutures) that allow bones to move & overlap to diminish size of skull • Molding: head becomes narrower, longer, sutures can overlap--normal--resolves 1 -2 days after birth • Fontanelles: at junctures of skull bones
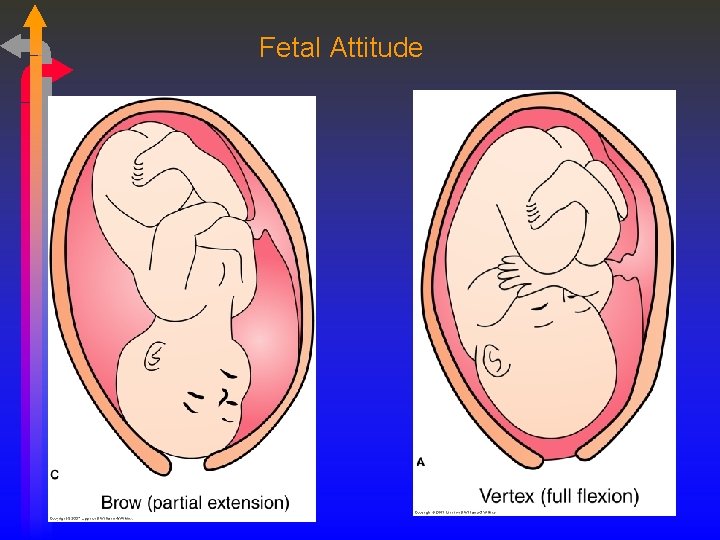
Fetal Attitude
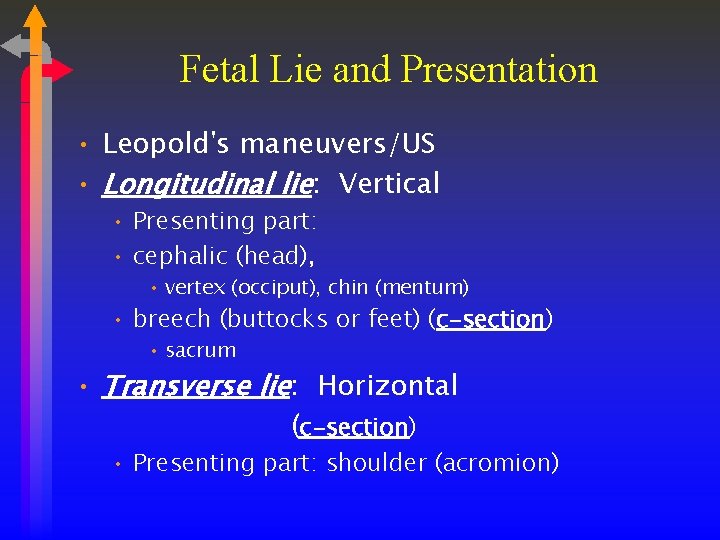
Fetal Lie and Presentation • Leopold's maneuvers/US • Longitudinal lie: Vertical • Presenting part: • cephalic (head), • vertex (occiput), chin (mentum) • breech (buttocks or feet) (c-section) • sacrum • Transverse lie: Horizontal (c-section) • Presenting part: shoulder (acromion)
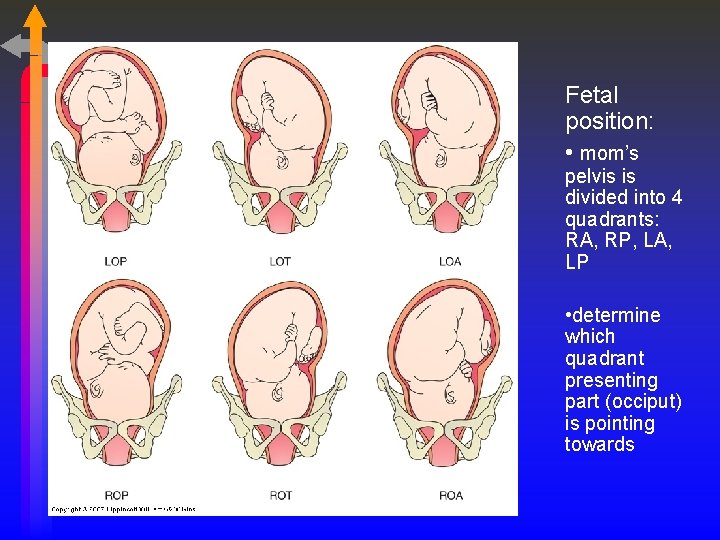
Fetal position: • mom’s pelvis is divided into 4 quadrants: RA, RP, LA, LP • determine which quadrant presenting part (occiput) is pointing towards
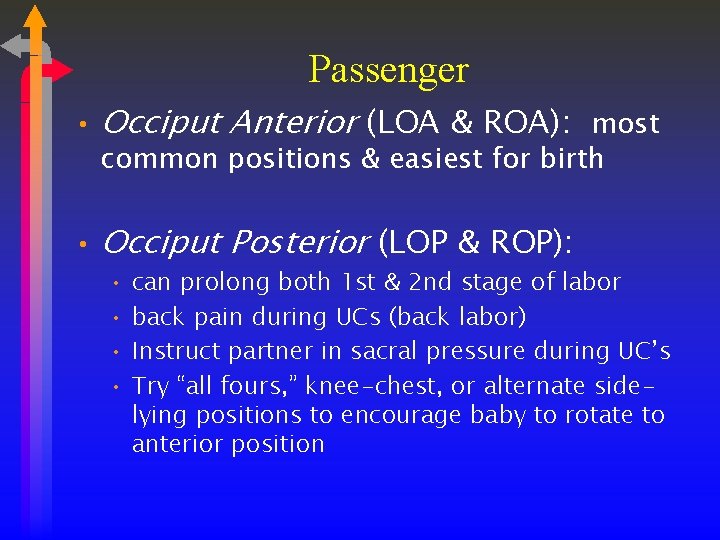
Passenger • Occiput Anterior (LOA & ROA): most common positions & easiest for birth • Occiput Posterior (LOP & ROP): • can prolong both 1 st & 2 nd stage of labor • back pain during UCs (back labor) • Instruct partner in sacral pressure during UC’s • Try “all fours, ” knee-chest, or alternate sidelying positions to encourage baby to rotate to anterior position
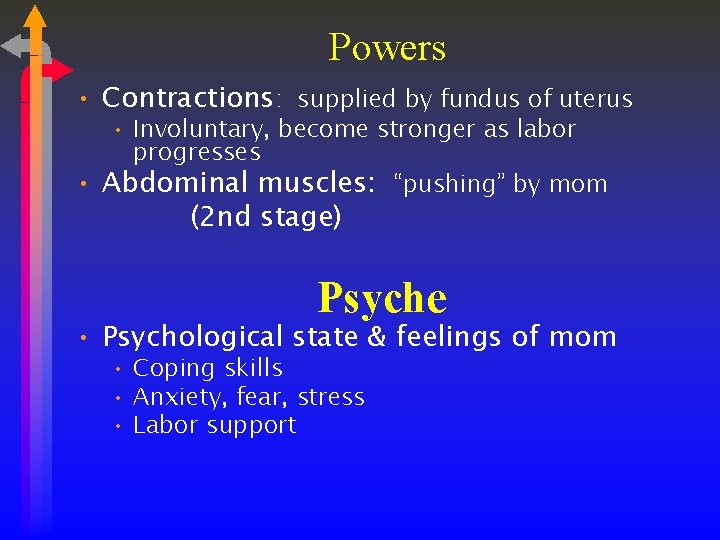
Powers • Contractions: supplied by fundus of uterus • Involuntary, become stronger as labor progresses • Abdominal muscles: “pushing” by mom (2 nd stage) Psyche • Psychological state & feelings of mom • Coping skills • Anxiety, fear, stress • Labor support
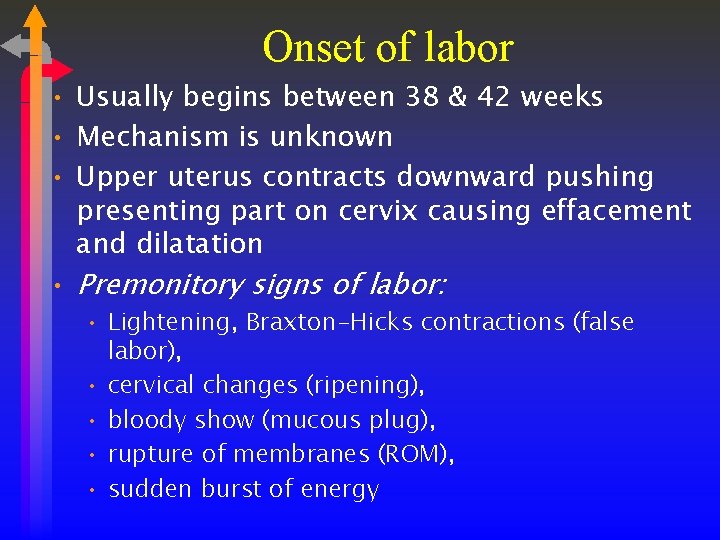
Onset of labor • Usually begins between 38 & 42 weeks • Mechanism is unknown • Upper uterus contracts downward pushing presenting part on cervix causing effacement and dilatation • Premonitory signs of labor: • Lightening, Braxton-Hicks contractions (false labor), • cervical changes (ripening), • bloody show (mucous plug), • rupture of membranes (ROM), • sudden burst of energy
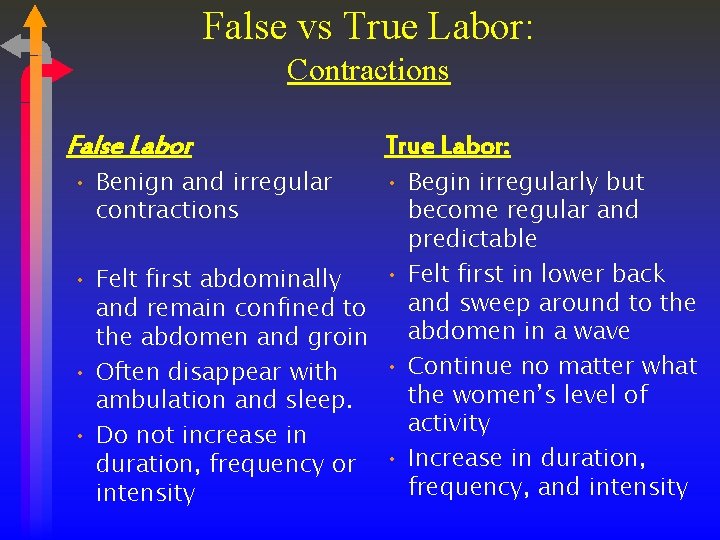
False vs True Labor: Contractions False Labor • Benign and irregular contractions True Labor: • Begin irregularly but become regular and predictable • Felt first in lower back • Felt first abdominally and sweep around to the and remain confined to abdomen in a wave the abdomen and groin • Continue no matter what • Often disappear with the women’s level of ambulation and sleep. activity • Do not increase in duration, frequency or • Increase in duration, frequency, and intensity
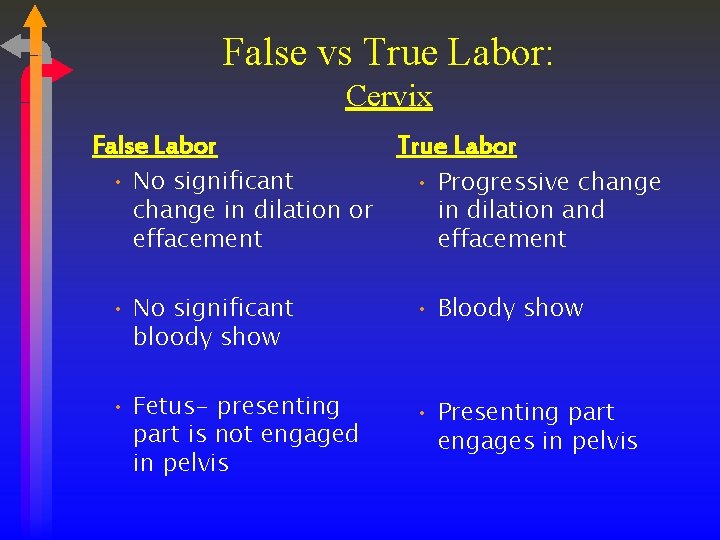
False vs True Labor: Cervix False Labor • No significant change in dilation or effacement True Labor • Progressive change in dilation and effacement • No significant bloody show • Bloody show • Fetus- presenting part is not engaged in pelvis • Presenting part engages in pelvis
Critical Thinking • A. B. C. D. A primigravida client has just arrived in the birthing unit. What steps would be most important for the nurse to perform to gain an understanding of the physical status of the client and her fetus? Check for ruptured membranes, and apply a fetal scalp electrode Auscultate the fetal heart rate between and during contractions Palpate contractions and resting uterine tone Perform a vaginal exam for cervical dilation, and perform Leopold's maneuvers E. Determine gestational age of fetus
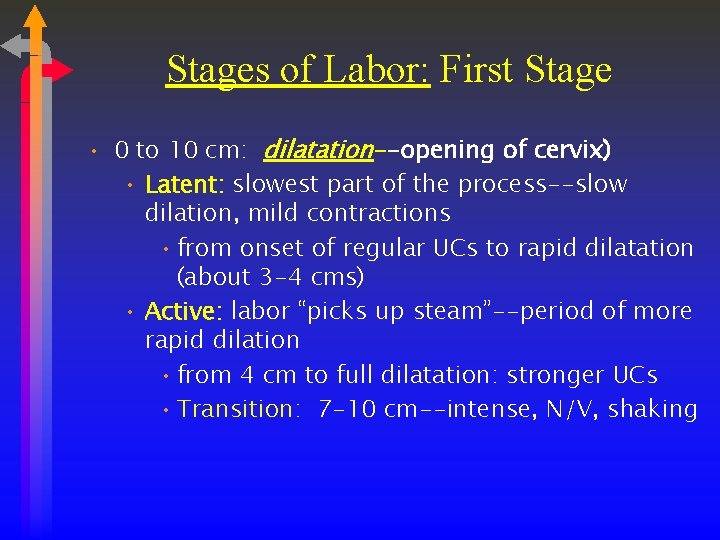
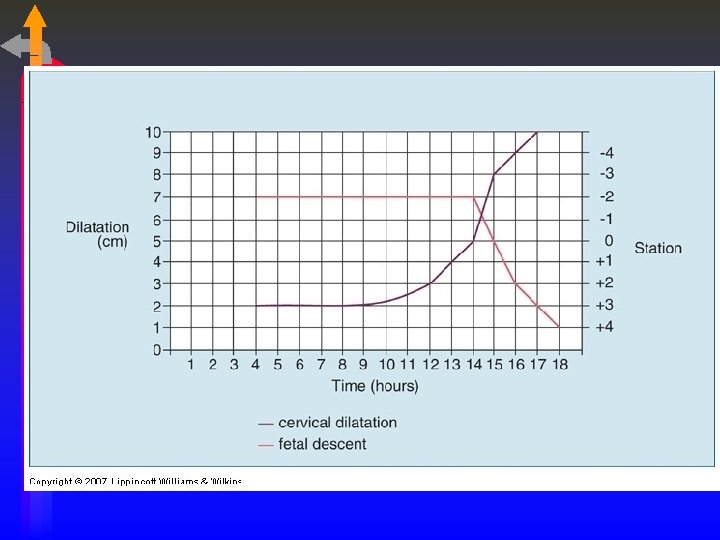
Stages of Labor: First Stage • 0 to 10 cm: dilatation--opening of cervix) • Latent: slowest part of the process--slow dilation, mild contractions • from onset of regular UCs to rapid dilatation (about 3 -4 cms) • Active: labor “picks up steam”--period of more rapid dilation • from 4 cm to full dilatation: stronger UCs • Transition: 7 -10 cm--intense, N/V, shaking
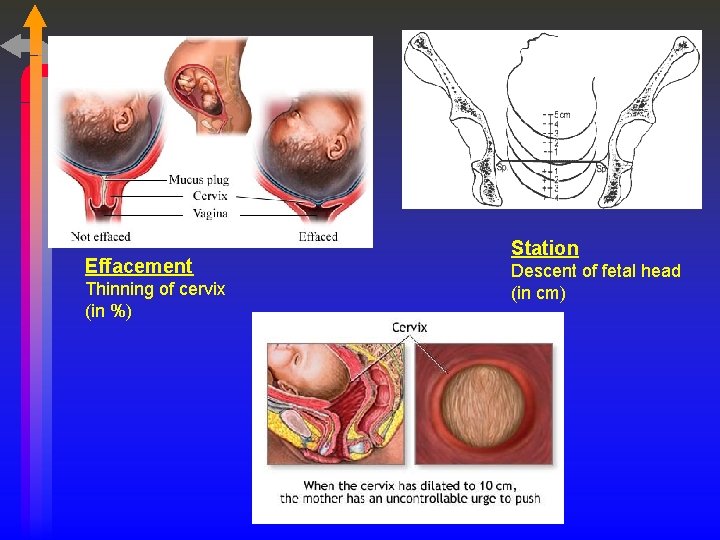
Effacement Thinning of cervix (in %) Station Descent of fetal head (in cm)
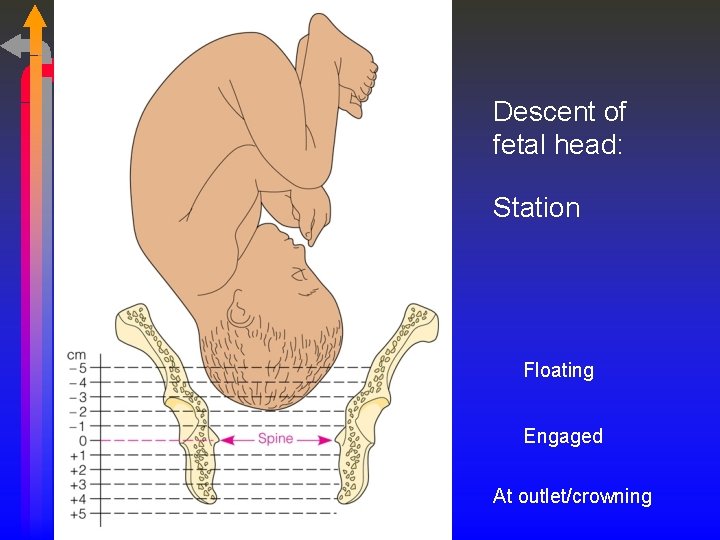
Descent of fetal head: Station Floating Engaged At outlet/crowning
Dilatation & Effacement
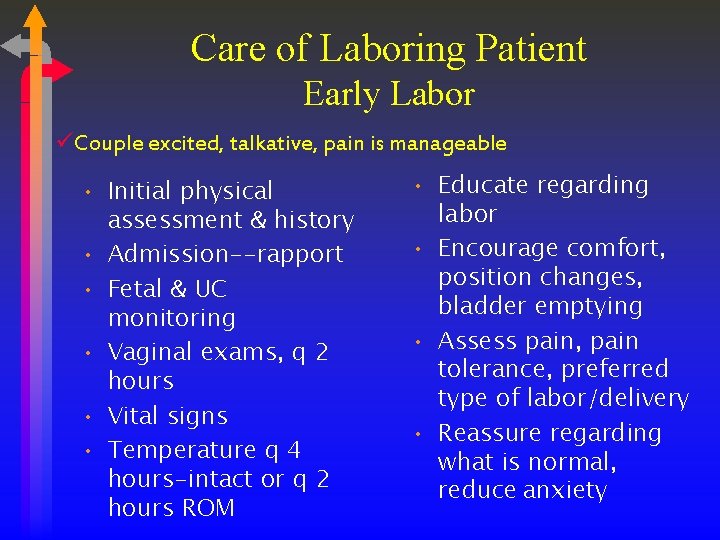
Care of Laboring Patient Early Labor üCouple excited, talkative, pain is manageable • Initial physical assessment & history • Admission--rapport • Fetal & UC monitoring • Vaginal exams, q 2 hours • Vital signs • Temperature q 4 hours-intact or q 2 hours ROM • Educate regarding labor • Encourage comfort, position changes, bladder emptying • Assess pain, pain tolerance, preferred type of labor/delivery • Reassure regarding what is normal, reduce anxiety
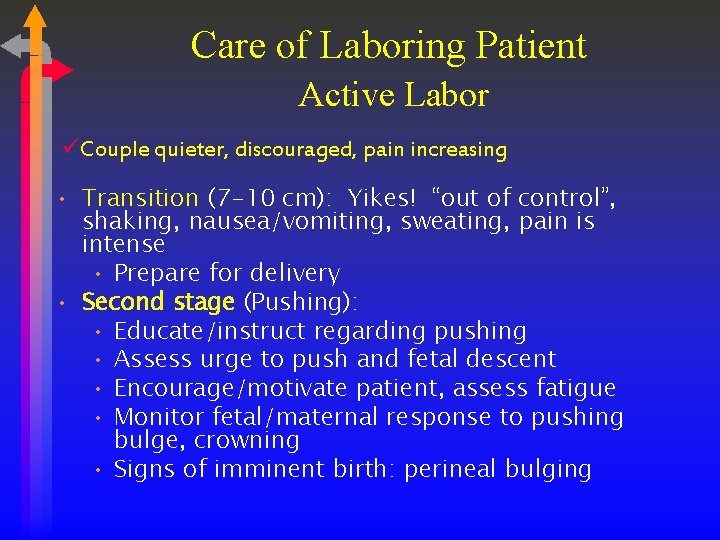
Care of Laboring Patient Active Labor üCouple quieter, discouraged, pain increasing • Transition (7 -10 cm): Yikes! “out of control”, shaking, nausea/vomiting, sweating, pain is intense • Prepare for delivery • Second stage (Pushing): • Educate/instruct regarding pushing • Assess urge to push and fetal descent • Encourage/motivate patient, assess fatigue • Monitor fetal/maternal response to pushing bulge, crowning • Signs of imminent birth: perineal bulging
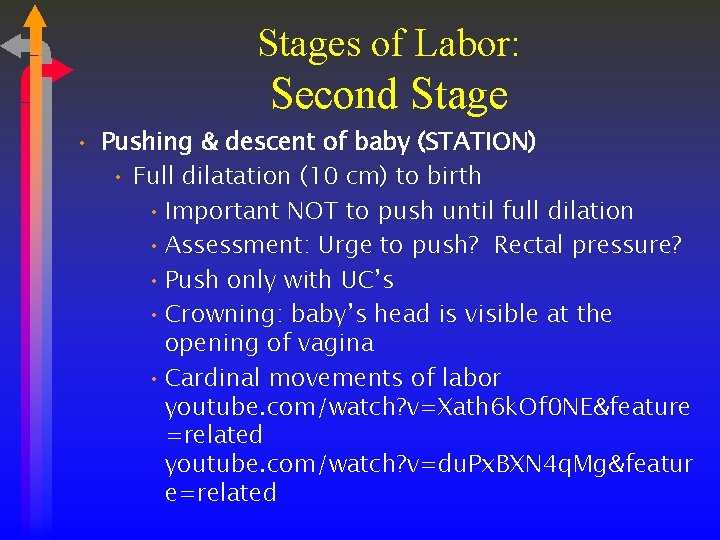
Stages of Labor: Second Stage • Pushing & descent of baby (STATION) • Full dilatation (10 cm) to birth • Important NOT to push until full dilation • Assessment: Urge to push? Rectal pressure? • Push only with UC’s • Crowning: baby’s head is visible at the opening of vagina • Cardinal movements of labor youtube. com/watch? v=Xath 6 k. Of 0 NE&feature =related youtube. com/watch? v=du. Px. BXN 4 q. Mg&featur e=related
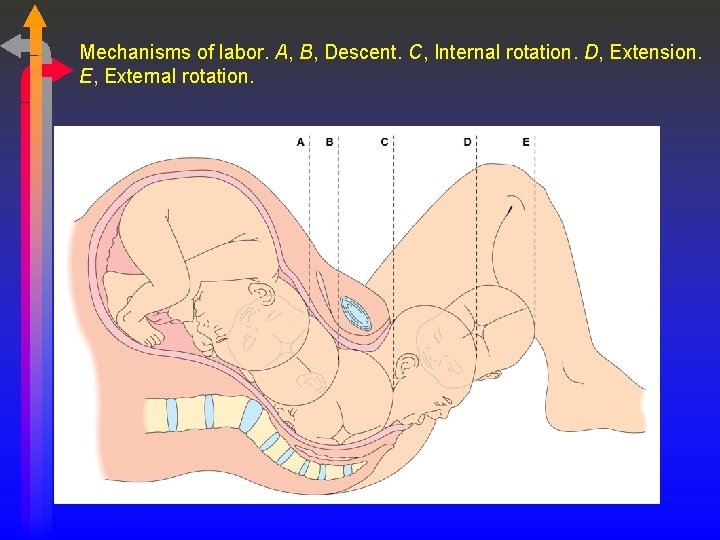
Mechanisms of labor. A, B, Descent. C, Internal rotation. D, Extension. E, External rotation.
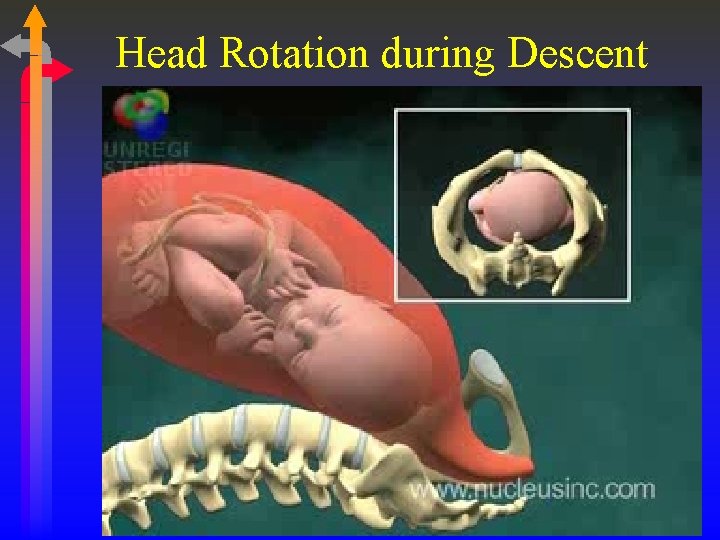
Head Rotation during Descent

Crowning Alternative settings In the hospital
Stages of Labor: Third Stage • Placental stage: from birth to delivery of placenta • Placental separation from uterine wall (rise of fundus, sudden gush of blood, lengthening of umbilical cord) • Entire lining of uterus shed • Expulsion of placenta • Normal blood loss: 300 -500 m. L • If placenta does not deliver spontaneously, can be delivered manually • Pitocin infusion started immediately post delivery of placenta
Critical Thinking • • • A client is admitted to the labor unit with contractions 2 to 3 minutes apart and lasting 60 to 90 seconds. The client is apprehensive and vomiting. This nurse understands this information to indicate that the client is most likely in what phase of labor? A) Active B) Transition C) Latent D) Second
Methods of Induction • Prostaglandins (Cervidil, prostin gel, Prepidil, Cytotec) applied intravaginally for cervical ripening • Pitocin (oxytocin) by IV • Amniotomy or stripping of membranes • Sexual intercourse • Nipple stimulation • Herbal preparations
Indications for induction of labor • Post-term pregnancy (≥ 42 weeks) • Premature or prolonged rupture of membranes • Maternal complications (Rh isoimmunization, Diabetes, Pulmonary disease, Pregnancy-induced hypertension) • Chorioamnionitis • Suspected fetal problems- Intrauterine Growth restriction (IUGR) and hydrops (fetal hemolytic disorder as result of Rh isoimmunization when maternal immune system attacks fetal red blood cells) • Fetal demise
Contraindications to Induction • • previous c-section placenta previa or abruption prolapsed cord fetal bradycardia, nonreassuring fetal status vaginal bleeding of unknown cause cephalopelvic disproportion active genital herpes
Cervical Ripening Assessment • Bishop Score- rating that determines if the cervix is ready for induction--Pg. 765 • Fetus must be in vertex position • Baseline data on fetal and maternal well-being (at least half an hour of monitoring) • Fetal monitoring and uterine contraction monitoring is imperative • Notify MD if hyperstimulation or fetal heart rate distress is noted
Oxytocin Induction pg 767 • Confirmation that the baby is in a cephalic (vertex) position (head down) • V/S done at least every 30 minutes and when dose is titrated • FHTs and UCs assessed every 30 minutes • Titration of oxytocin till UCs every 2 -3 minutes • Cervical dilation should be 2 cm/hr (ideally) • Reassuring FHTs between 110 -160 beats/min
When to Discontinue Oxytocin Hyperstimulation-frequency of UCs less than 2 minutes apart -Now being called tachysystole -Inadequate uterine relaxation between contractions <60 sec between UC’s Fetal Distress -any decelerations or decreased baseline variability
Childbirth at Risk (Ch. 26) Complications of Labor or Delivery
Critical Thinking The client in active labor is requesting pain relief. The physician orders epidural anesthesia for the client. Which of the following parameters should the nurse be prepared to assess immediately after administration of the epidural? • • • A) For headache. B) For urinary retention. C) The blood pressure. D) The maternal pulse rate.
Precipitous Labor & Birth • Labor in < 3 hours • Risk factors: • Multiparity, oxytocin or amniotomy, hx of precipitate labor • Risks for injury • Maternal: cervical, vaginal & perineal lacerations with possible hemorrhage, pain, anxiety • Fetal: Birth trauma (intracranial bleed, brachial palsy), meconium-stained fluid, fetal distress • Management: close monitoring for cervical changes, induction
Postterm Pregnancy • > 42 weeks • Maternal risks: trauma/hemorrhage due to larger baby, ↑operative delivery/csection • Fetal risks: placental changes that ↓oxygenation to baby and ↑mortality rate, oligohydramnios (↑cord compression during labor), LGA baby (↑birth trauma, shoulder dystocia), meconium aspiration • Management: > 40 wks, NST, BPP or modified BPP (NST & AFI), induction
Malpresentations • Occiput-posterior (OP) • Prolonged labor, back labor (sacral nerve compression), arrested dilatation/ descent, perineal tears • Usually vaginal, but may need C-Section if baby doesn’t rotate • Management: positioning (side-lying, kneechest or hand-knees), sacral pressure during UC’s • Transverse Lie • Associated with: pendulous abdomen, uterine masses/fibroids, congenital abnormalities of uterus, hydramnios • Attempt External Cephalic Version, if
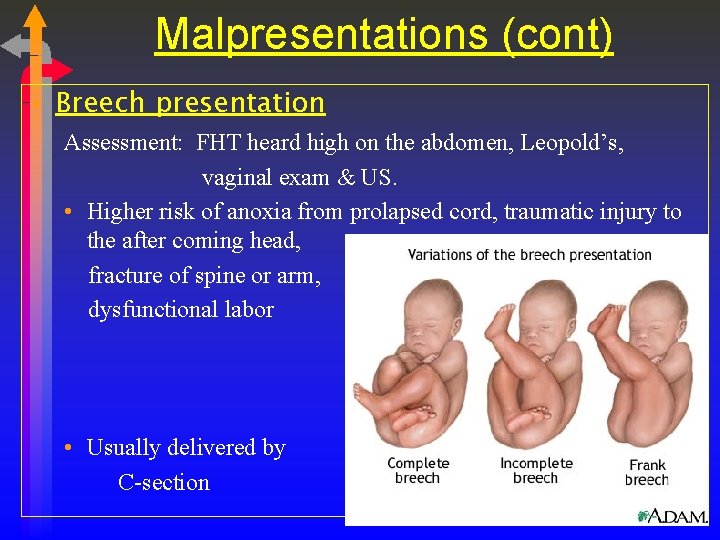
Malpresentations (cont) • Breech presentation Assessment: FHT heard high on the abdomen, Leopold’s, vaginal exam & US. • Higher risk of anoxia from prolapsed cord, traumatic injury to the after coming head, fracture of spine or arm, dysfunctional labor • Usually delivered by C-section
External Version • External cephalic version (37 -38 wks): abdominal manipulation to change fetal presentation • Contraindications: multiple gestation, fetal breech is engaged in pelvis, oligohydramnios, nonreactive NST, nuchal cord, vaginal bleeding, IUGR, ROM. • Risks: immediate cesarean birth • Nursing actions: NPO 8 hrs, NST, IV line, terbutaline, continuous FHR, US used to guide manipulations, assess for: labor, fetal distress. O- moms need Rhogam following the procedure
Macrosomia/Shoulder Dystocia • Wt. > 4500 gms (9 -10 lbs) • Associated with: • DM, Gestational DM, Multiparity, Postdates, obesity • Risks: • Shoulder dystocia, difficulty delivering the shoulders after head is delivered (obstetrical emergency) • Maternal: vaginal/cervical tears, pp hemorrhage, rupture • Fetal: compressed cord, fractured clavical, asphyxia & neurologic damage, brachial plexus injury (Erb’s. Palsy) • S/S: Turtle sign • Nursing interventions: Mc. Roberts maneuvers, suprapubic pressure. PP: assess for uterine atony/hemorrhage; trauma, cerebral or neurologic damage to baby
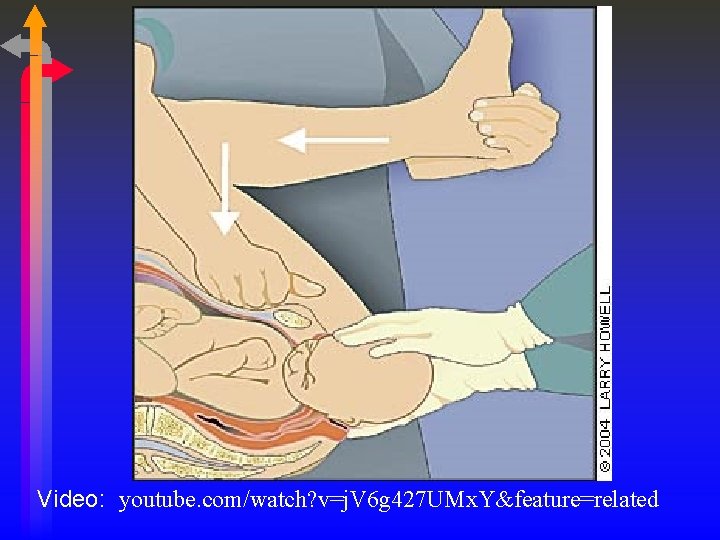
Video: youtube. com/watch? v=j. V 6 g 427 UMx. Y&feature=related

Mc. Roberts Maneuvers Video
Multiple Gestation • Monozygotic (identical) twins: can have 1 or 2 placentas, chorions, or amnions (↑risk if all shared) • Dizygotic (fraternal) twins: 2 of everything. • Dx: faster than usual growth of uterus, ↑AFP, HCG, Ultrasound • Risks: • Maternal: SAB, gestational DM, HTN/preeclampsia/HELLP, hydramnios, PT labor & delivery • Fetal: Preterm birth, twin-to-twin transfusion
Multiple Gestation (cont) • Management: • US to determine what type of twins • Prevention of PT labor/routine cervical measurements (US) • NST surveillance • Birth: depends on maternal & fetal complications and fetal position/ presentation • Examination of placenta • Close monitoring PP for hemorrhage (atony)
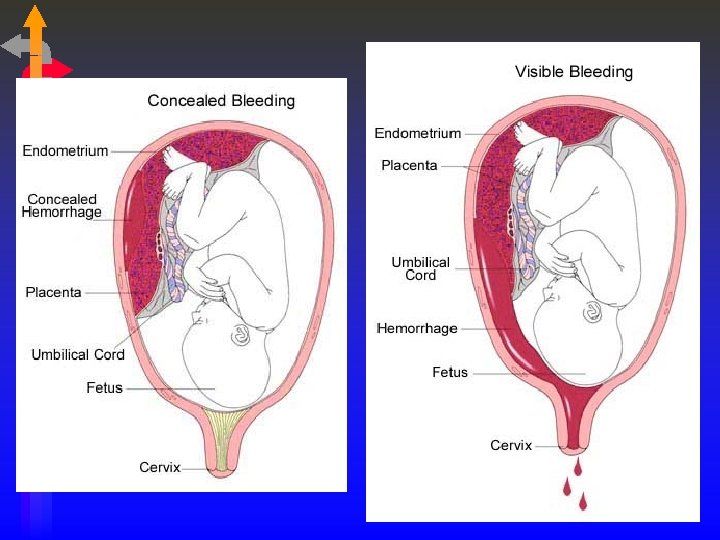
Abruptio Placentae • Premature separation of placenta from uterine wall • S/S: sharp, stabbing pain high in fundus, heavy bleeding (may be occult), hard, board-like uterus, tense, painful uterus, signs of shock due to blood loss, Port-Wine aminotic fluid if ROM. • Predisposing fx: ↑parity, adv. maternal age, short umbilical cord, chronic HTN, PIH, direct trauma, vasoconstriction from cocaine or cigarette use • Fetal distress on monitor. Can progress to DIC.
Abruptio Placentae (cont) • Management: • Emergency. Immediate c-section if birth not imminent. • Lg. gauge IV • O 2 via mask, fetal monitoring, maternal VS, lateral positioning, labs, blood transfusion (have 2 units avail) • CBC (H&H), Fibrinogen levels, platelet count, PT/PTT, fibrin degradation products ( sx of DIC)
Placenta Previa • Low implantation of placenta (1 in 200) • abrupt, painless, bright red bleeding • Associated with ↑parity, adv. maternal age, previous c -section or uterine curettage, multiple gestation • Dx: ultrasound. May resolve as pregnancy progresses • Bleeding common around 30 wks: Bedrest, VS, IV fluids, type & cross-match, observe for bleeding • Emergency: assess bleeding, hx, uc’s/labor, • NEVER do vaginal exam !!! C-Section delivery, possibly before 37 wks. Steroids for mom. Watch for pp hemorrhage. • Table 26 -6, pg 746, differential dx: abruptio/previa
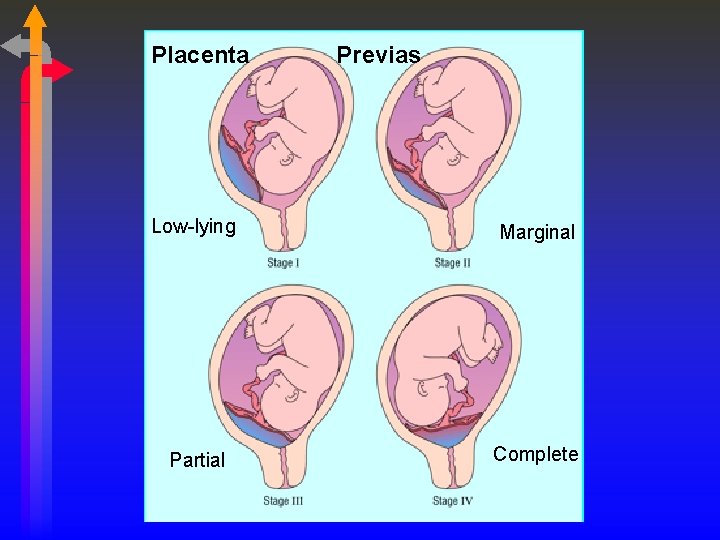
Placenta Previas Low-lying Marginal Partial Complete
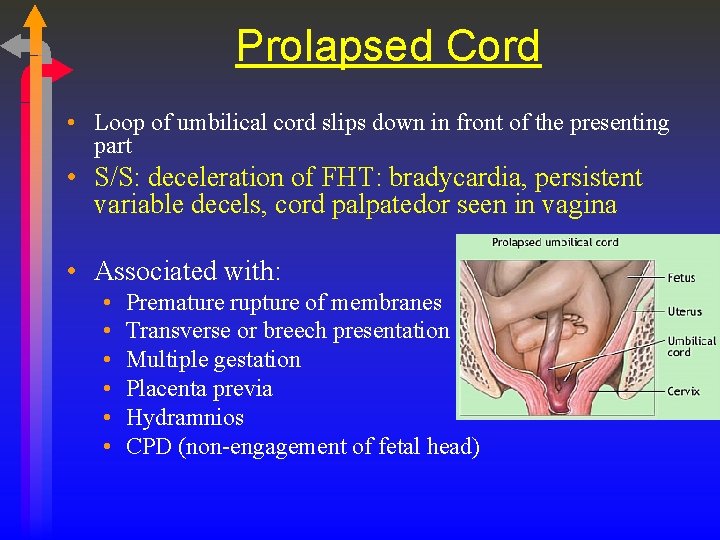
Prolapsed Cord • Loop of umbilical cord slips down in front of the presenting part • S/S: deceleration of FHT: bradycardia, persistent variable decels, cord palpatedor seen in vagina • Associated with: • • • Premature rupture of membranes Transverse or breech presentation Multiple gestation Placenta previa Hydramnios CPD (non-engagement of fetal head)
Prolapsed Cord • Management: Hold fetal head off cord, Trendelenburg or knee/chest position, immediate emergency c-section • Prevention • Watch fetal heart tones after rupture of membranes (SROM or AROM). Do VE if any sign of fetal distress. • If head not engaged, women with ruptured membranes should not ambulate.
Birth Related Procedures Chapter 27 Induction of labor • The deliberate initiation of uterine contractions, by chemical or mechanical means, to stimulate labor and birth before spontaneous onset of labor • Primary agent of induction: Pitocin by IV • Pitocin is also used to augment labor • If cervix not “ripe”, may need a preparatory stage of cervical ripening before pitocin can be started → Cervidil
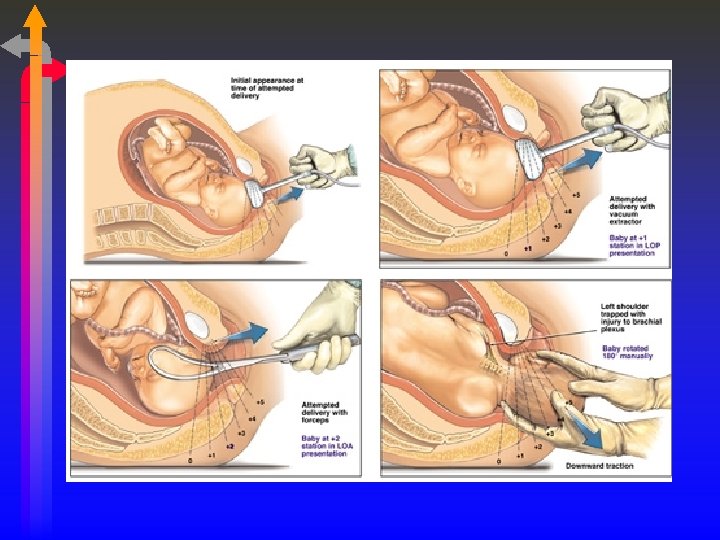
Operative Assisted Deliveries • Forceps • Indications: unable to push, arrested descent, need a quick delivery, breech • Associated with: maternal/fetal birth trauma, rectal sphincter tear, urinary stress incontinence • Vacuum extraction • Advantages: fewer lacerations, less anesthesia needed, • Disadvantages: marked caput, cephalhematomas, scalp laceration/bruising
Experiences of Pain • Etiology • Physiology • Perception • Factors influencing Anxiety Expectations Psychological factors Cultural factors Support Fetal position
Comfort and Pain Relief • Support from doula or coach • Alternative therapies • • • Relaxation/massage Focusing and imagery Breathing Herbal preparations/aromatherapy Hypnosis
Comfort and Pain Relief • Pharmacological Measures • Narcotic analgesics • Nubain/Stadol/Demerol (pg. 689) • Regional nerve blocks • Epidural/spinal • Local anesthetic blocks • Pudendal/perineal
Systemic Analgesia Table 25 -3, pg 690 • Pre-medication Assessment: • Pain level, VS, allergies, drug dependence (withdrawal), vaginal exam/progress in labor, UC pattern, fetal heart rate tracing • Post-medication Assessment: • VS, esp. RR, LOC, dizziness (bedpan), sedation, FHR • Reversal agent: Naloxone (Narcan) • Competes with narcotic for opiate receptors. Used in both mom and baby. (avoid with narcotic dependence)
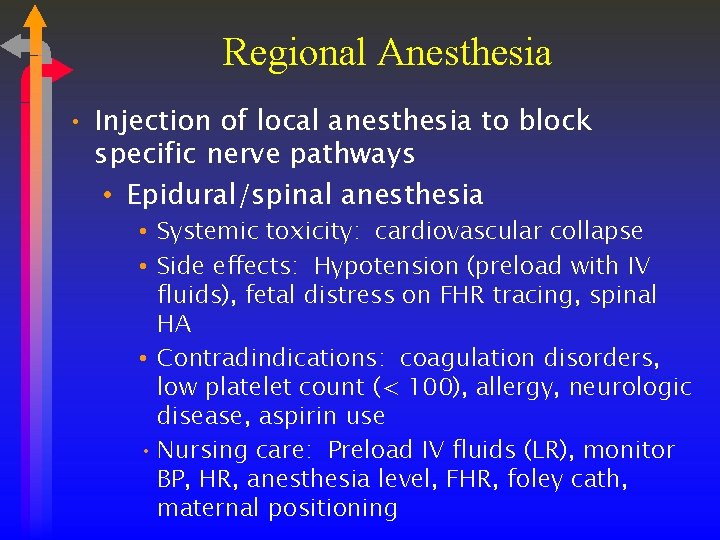
Regional Anesthesia • Injection of local anesthesia to block specific nerve pathways • Epidural/spinal anesthesia • Systemic toxicity: cardiovascular collapse • Side effects: Hypotension (preload with IV fluids), fetal distress on FHR tracing, spinal HA • Contradindications: coagulation disorders, low platelet count (< 100), allergy, neurologic disease, aspirin use • Nursing care: Preload IV fluids (LR), monitor BP, HR, anesthesia level, FHR, foley cath, maternal positioning
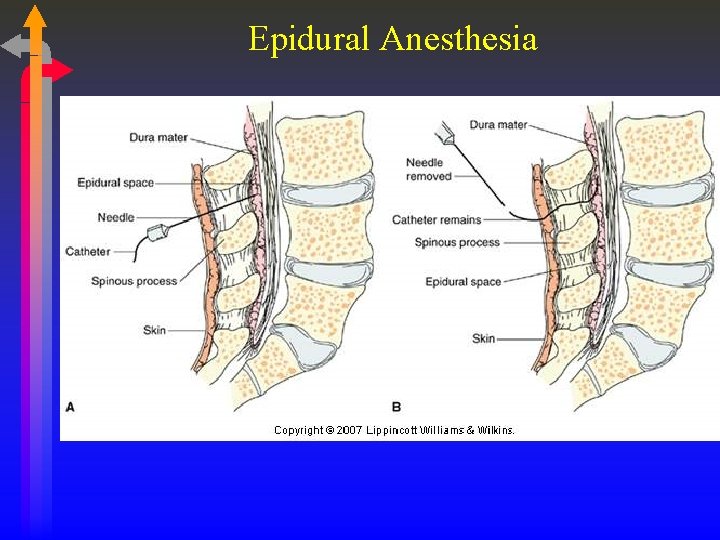
Epidural Anesthesia
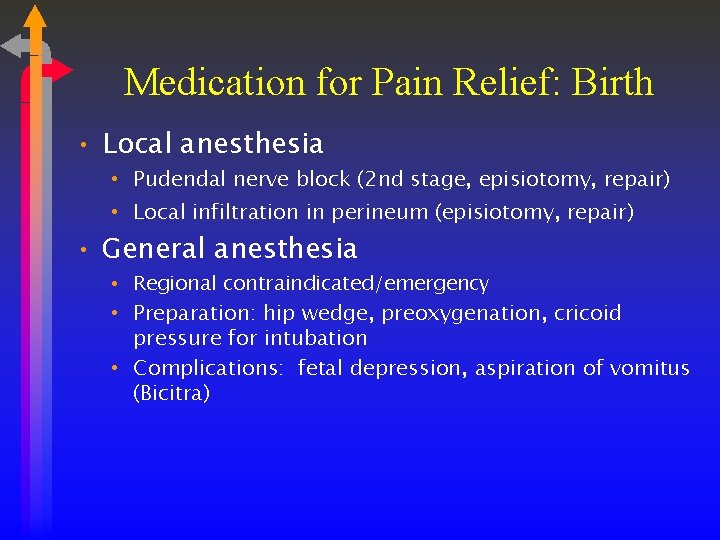
Medication for Pain Relief: Birth • Local anesthesia • Pudendal nerve block (2 nd stage, episiotomy, repair) • Local infiltration in perineum (episiotomy, repair) • General anesthesia • Regional contraindicated/emergency • Preparation: hip wedge, preoxygenation, cricoid pressure for intubation • Complications: fetal depression, aspiration of vomitus (Bicitra)
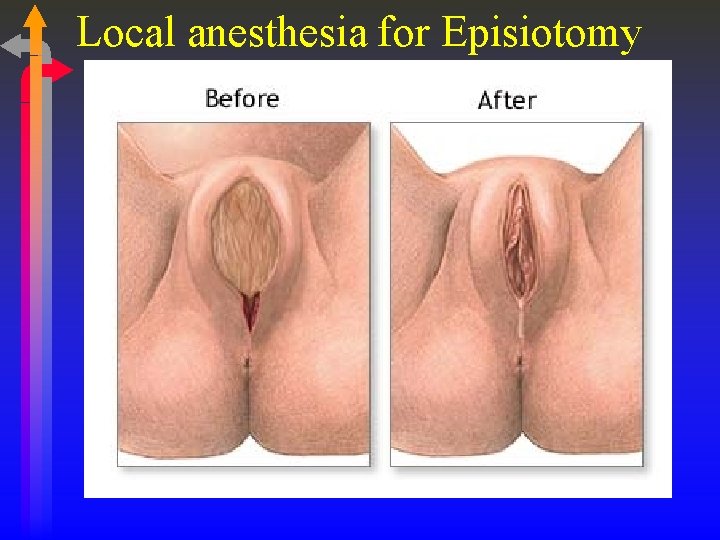
Local anesthesia for Episiotomy
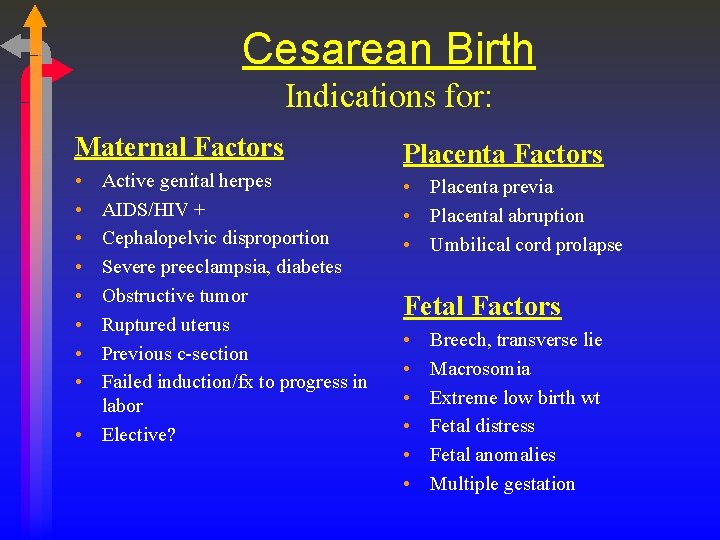
Cesarean Birth Indications for: Maternal Factors • • Active genital herpes AIDS/HIV + Cephalopelvic disproportion Severe preeclampsia, diabetes Obstructive tumor Ruptured uterus Previous c-section Failed induction/fx to progress in labor • Elective? Placenta Factors • Placenta previa • Placental abruption • Umbilical cord prolapse Fetal Factors • • • Breech, transverse lie Macrosomia Extreme low birth wt Fetal distress Fetal anomalies Multiple gestation
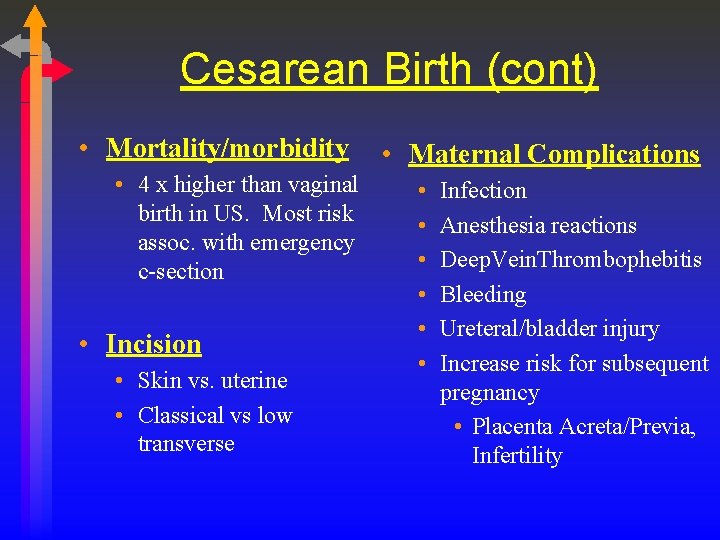
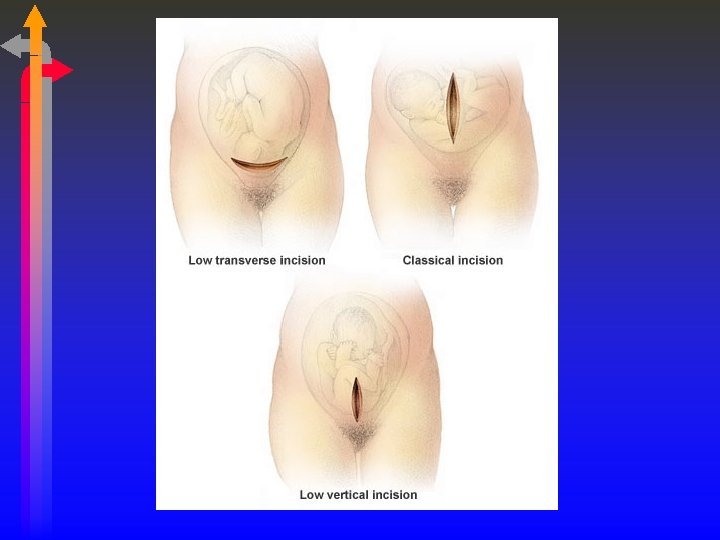
Cesarean Birth (cont) • Mortality/morbidity • 4 x higher than vaginal birth in US. Most risk assoc. with emergency c-section • Incision • Skin vs. uterine • Classical vs low transverse • Maternal Complications • • • Infection Anesthesia reactions Deep. Vein. Thrombophebitis Bleeding Ureteral/bladder injury Increase risk for subsequent pregnancy • Placenta Acreta/Previa, Infertility
Cesarean Birth • • Pre-op: CBC w/ platelets, hold clot, bicitra/antacid monitor baby Teaching: pre & post-op, anesthesia, recovery, breastfeeding • Psychosocial issues: • Fear • Self-image/self-esteem
Post-Op Care • Assess fundus/bleeding, vital signs, DVT. • Antibiotics. • Pain: Duramorph. Breakthrough pain meds. Benadryl for itching. Zofran for nausea. • Clear liquids and advance as tolerated. • Assess for GI function. Bowel sounds? Passing flatus? • Ambulation. Pre-medicate, teach splinting with pillow. • Stool softener
Critical Thinking • A laboring multipara is having intense uterine contractions with incomplete uterine relaxation between contractions. Vaginal examinations reveal rapid cervical dilation and fetal descent. What should the nurse do first? A) Notify the physician of these findings. B) Place the woman in knee-chest position. C) Turn off the lights to make it easier for the woman to relax. D) Assemble supplies to prepare for birth.
- Slides: 68