Chapter 22 Part C The Respiratory System Annie
- Slides: 32
Chapter 22 Part C The Respiratory System © Annie Leibovitz/Contact Press Images © 2016 Pearson Education, Inc. Power. Point® Lecture Slides prepared by Karen Dunbar Kareiva Ivy Tech Community College
Clinical – Homeostatic Imbalance 22. 14 • Hypoxia: inadequate O 2 delivery to tissues; can result in cyanosis • Hypoxia is based on cause: – Anemic hypoxia: too few RBCs or abnormal or too little Hb – Ischemic hypoxia: impaired or blocked circulation © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 14 – Histotoxic hypoxia: cells unable to use O 2, as in metabolic poisons – Hypoxemic hypoxia: abnormal ventilation; pulmonary disease – Carbon monoxide poisoning: especially from fire • Hb has a 200 greater affinity for carbon monoxide than oxygen © 2016 Pearson Education, Inc.
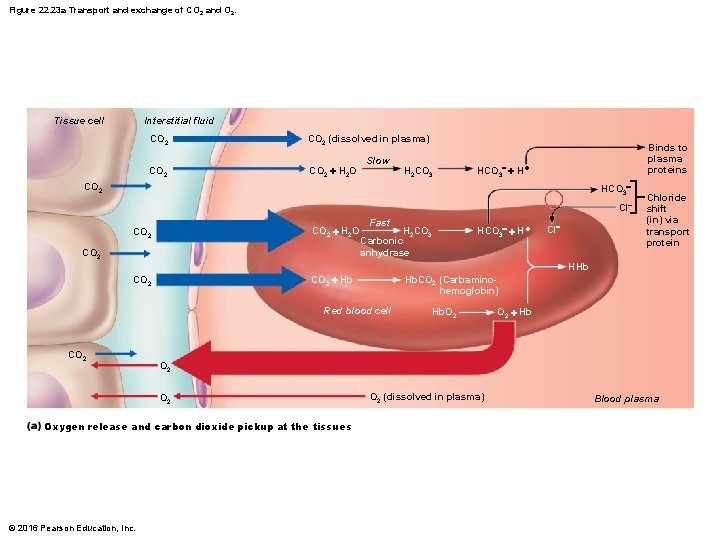
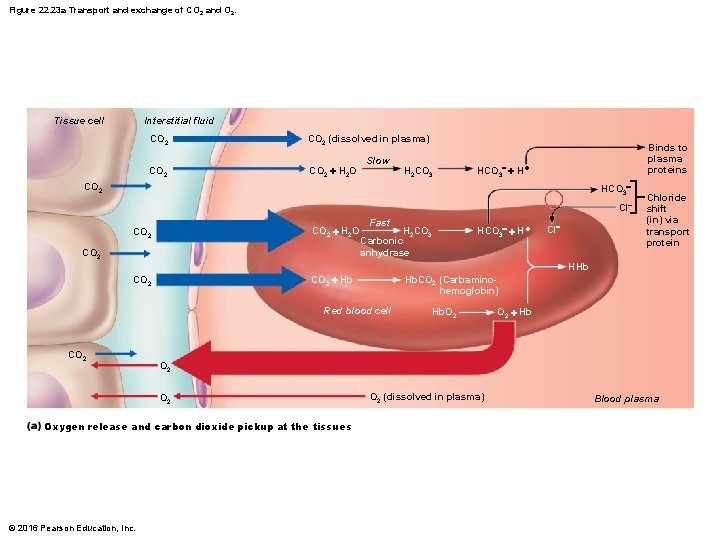
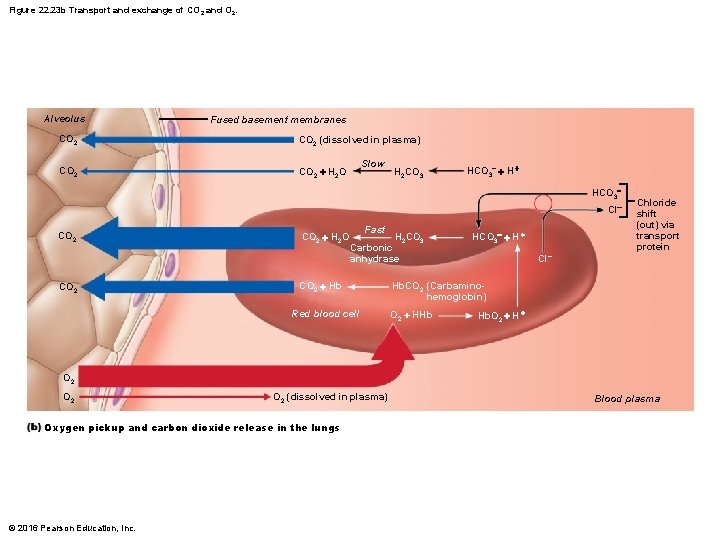
Figure 22. 23 a Transport and exchange of CO 2 and O 2. Interstitial fluid Tissue cell CO 2 (dissolved in plasma) CO 2 + H 2 O Slow H 2 CO 3 Binds to plasma proteins HCO 3 + H + CO 2 HCO 3 Cl CO 2 + H 2 O CO 2 + Hb CO 2 Fast H 2 CO 3 Carbonic anhydrase HCO 3 + H + Cl Chloride shift (in) via transport protein HHb Hb. CO 2 (Carbaminohemoglobin) Red blood cell CO 2 + Hb O 2 Oxygen release and carbon dioxide pickup at the tissues © 2016 Pearson Education, Inc. Hb. O 2 (dissolved in plasma) Blood plasma
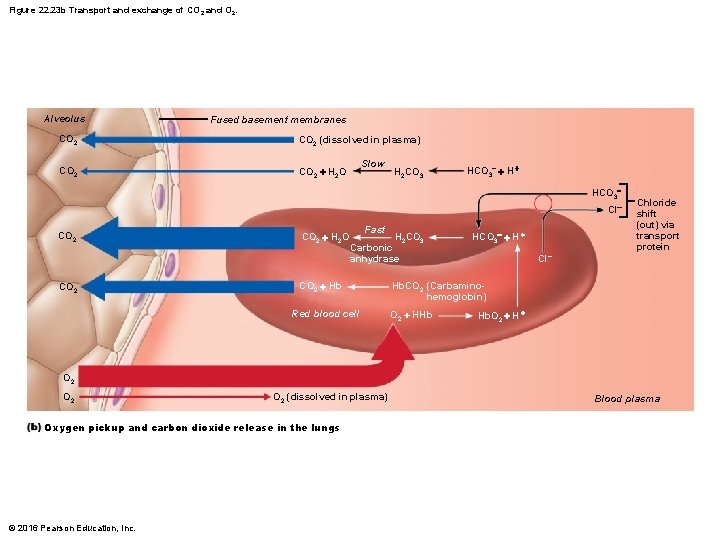
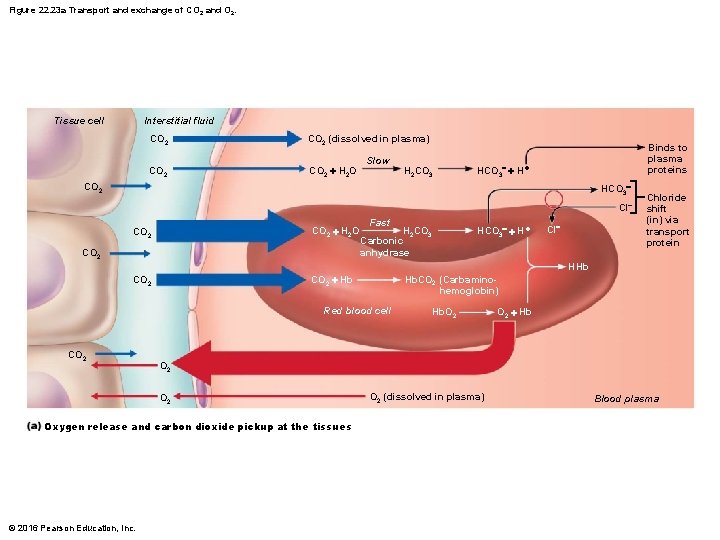
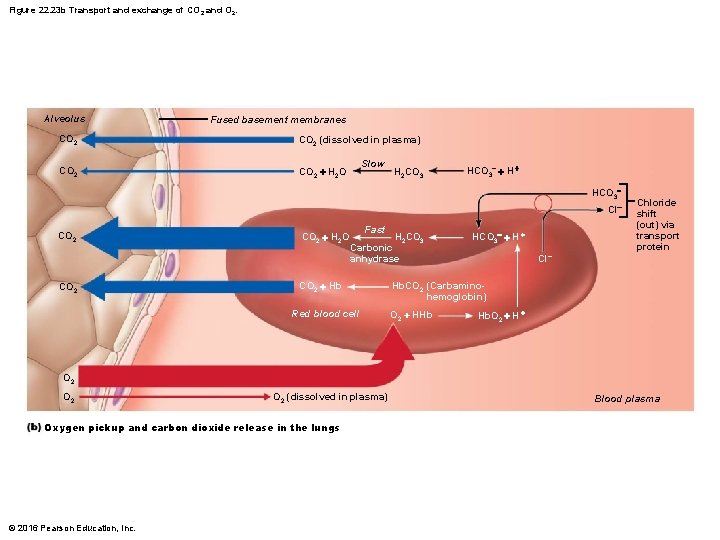
Figure 22. 23 b Transport and exchange of CO 2 and O 2. Alveolus Fused basement membranes CO 2 (dissolved in plasma) CO 2 + H 2 O Slow H 2 CO 3 HCO 3 + HCO 3 Cl CO 2 + H 2 O Fast H 2 CO 3 Carbonic anhydrase CO 2 + Hb Red blood cell HCO 3 + H + Cl Chloride shift (out) via transport protein Hb. CO 2 (Carbaminohemoglobin) O 2 + HHb Hb. O 2 + H + O 2 O 2 (dissolved in plasma) Oxygen pickup and carbon dioxide release in the lungs © 2016 Pearson Education, Inc. Blood plasma
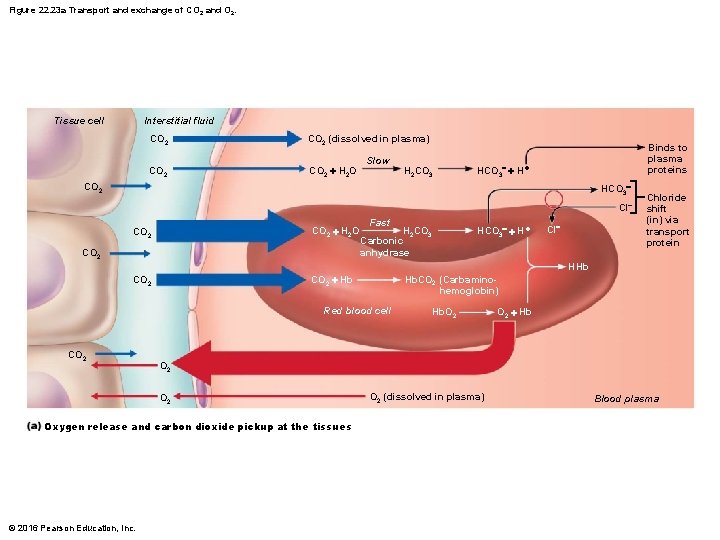
Figure 22. 23 a Transport and exchange of CO 2 and O 2. Interstitial fluid Tissue cell CO 2 (dissolved in plasma) CO 2 + H 2 O Slow H 2 CO 3 Binds to plasma proteins HCO 3 + H + CO 2 HCO 3 Cl CO 2 + H 2 O CO 2 + Hb CO 2 Fast H 2 CO 3 Carbonic anhydrase HCO 3 + H + Cl Chloride shift (in) via transport protein HHb Hb. CO 2 (Carbaminohemoglobin) Red blood cell CO 2 + Hb O 2 Oxygen release and carbon dioxide pickup at the tissues © 2016 Pearson Education, Inc. Hb. O 2 (dissolved in plasma) Blood plasma
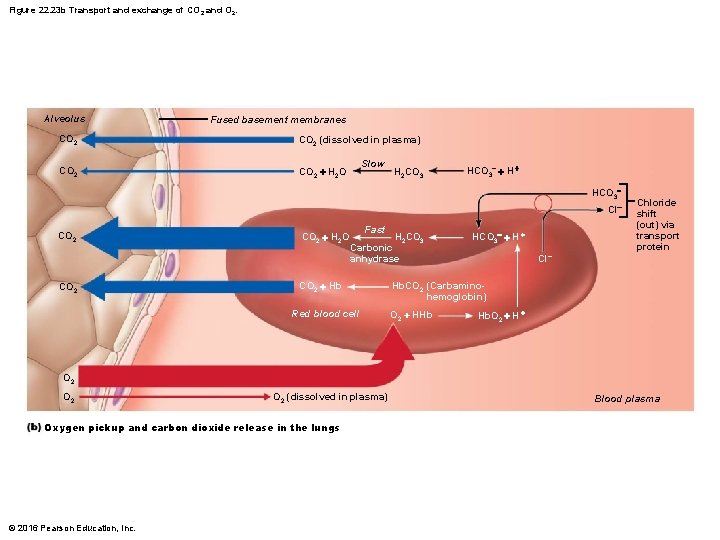
Figure 22. 23 b Transport and exchange of CO 2 and O 2. Alveolus Fused basement membranes CO 2 (dissolved in plasma) CO 2 + H 2 O Slow H 2 CO 3 HCO 3 + HCO 3 Cl CO 2 + H 2 O Fast H 2 CO 3 Carbonic anhydrase CO 2 + Hb Red blood cell HCO 3 + H + Cl Chloride shift (out) via transport protein Hb. CO 2 (Carbaminohemoglobin) O 2 + HHb Hb. O 2 + H + O 2 O 2 (dissolved in plasma) Oxygen pickup and carbon dioxide release in the lungs © 2016 Pearson Education, Inc. Blood plasma
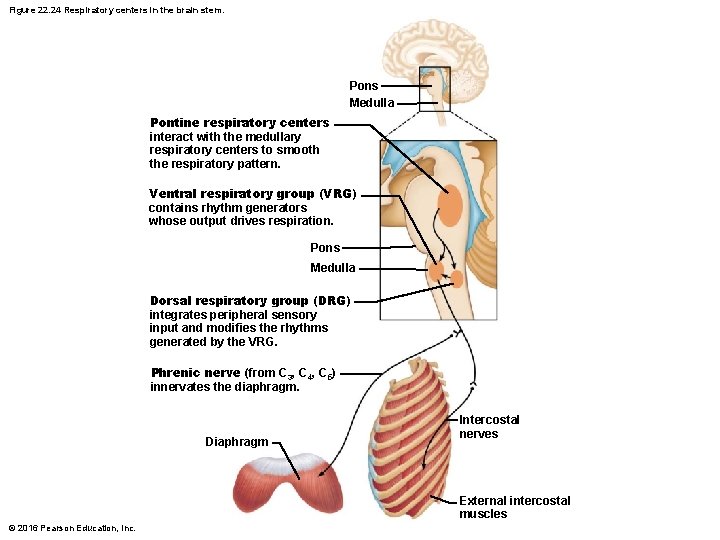
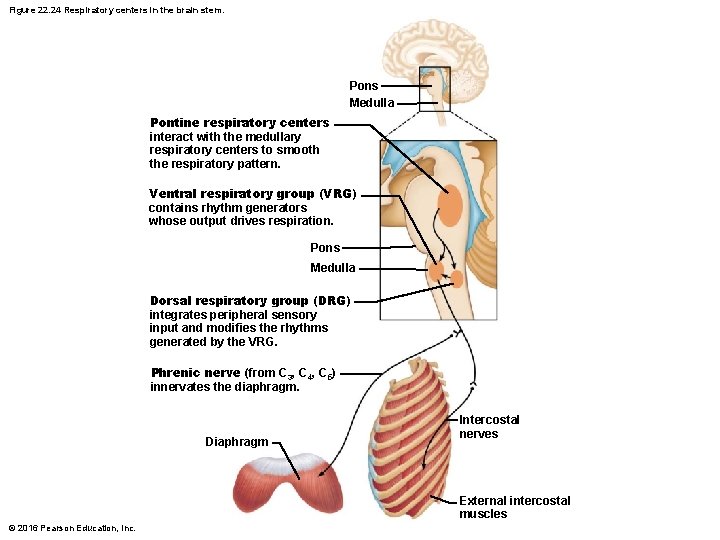
Figure 22. 24 Respiratory centers in the brain stem. Pons Medulla Pontine respiratory centers interact with the medullary respiratory centers to smooth the respiratory pattern. Ventral respiratory group (VRG) contains rhythm generators whose output drives respiration. Pons Medulla Dorsal respiratory group (DRG) integrates peripheral sensory input and modifies the rhythms generated by the VRG. Phrenic nerve (from C 3, C 4, C 5) innervates the diaphragm. Diaphragm Intercostal nerves External intercostal muscles © 2016 Pearson Education, Inc.
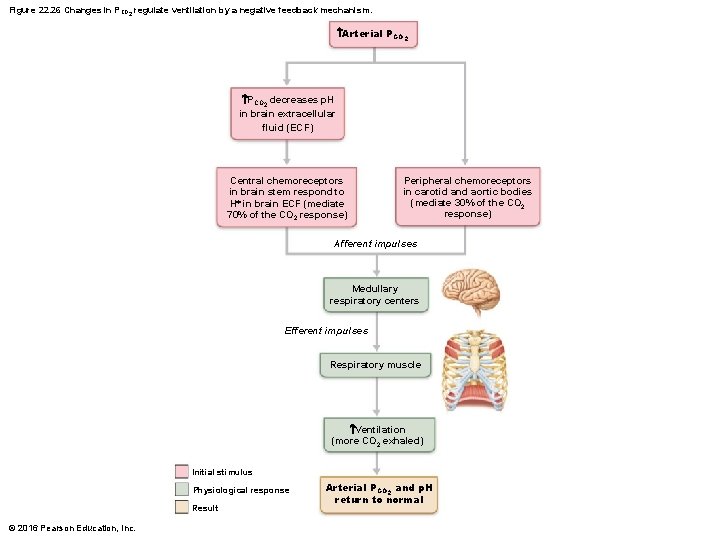
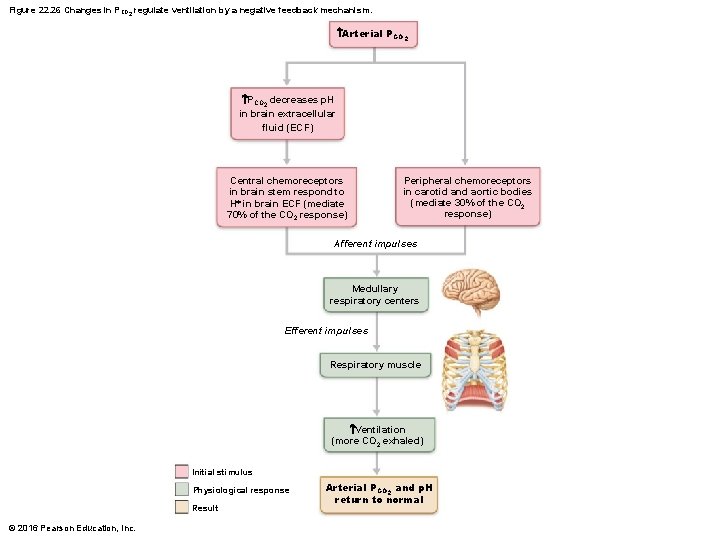
Figure 22. 26 Changes in PCO 2 regulate ventilation by a negative feedback mechanism. Arterial PCO 2 decreases p. H in brain extracellular fluid (ECF) Central chemoreceptors in brain stem respond to H+ in brain ECF (mediate 70% of the CO 2 response) Peripheral chemoreceptors in carotid and aortic bodies (mediate 30% of the CO 2 response) Afferent impulses Medullary respiratory centers Efferent impulses Respiratory muscle Ventilation (more CO 2 exhaled) Initial stimulus Physiological response Result © 2016 Pearson Education, Inc. Arterial PCO 2 and p. H return to normal
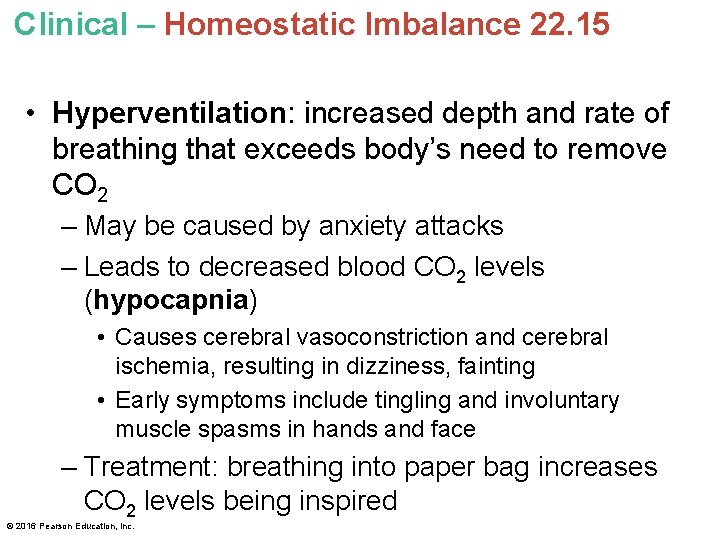
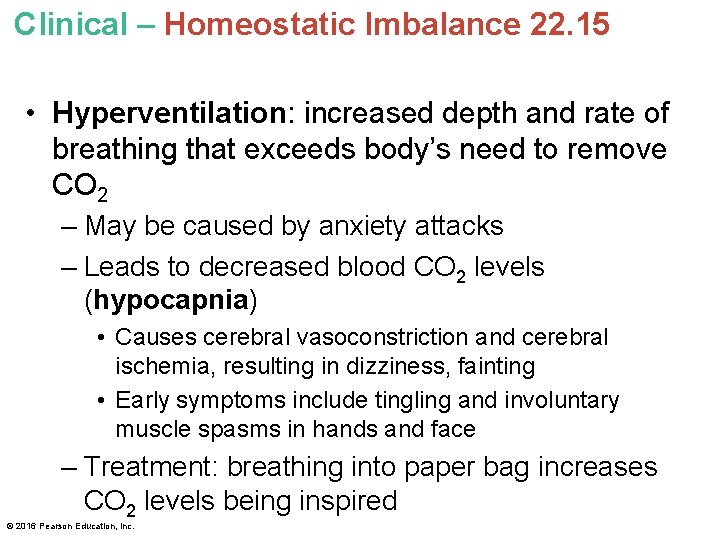
Clinical – Homeostatic Imbalance 22. 15 • Hyperventilation: increased depth and rate of breathing that exceeds body’s need to remove CO 2 – May be caused by anxiety attacks – Leads to decreased blood CO 2 levels (hypocapnia) • Causes cerebral vasoconstriction and cerebral ischemia, resulting in dizziness, fainting • Early symptoms include tingling and involuntary muscle spasms in hands and face – Treatment: breathing into paper bag increases CO 2 levels being inspired © 2016 Pearson Education, Inc.
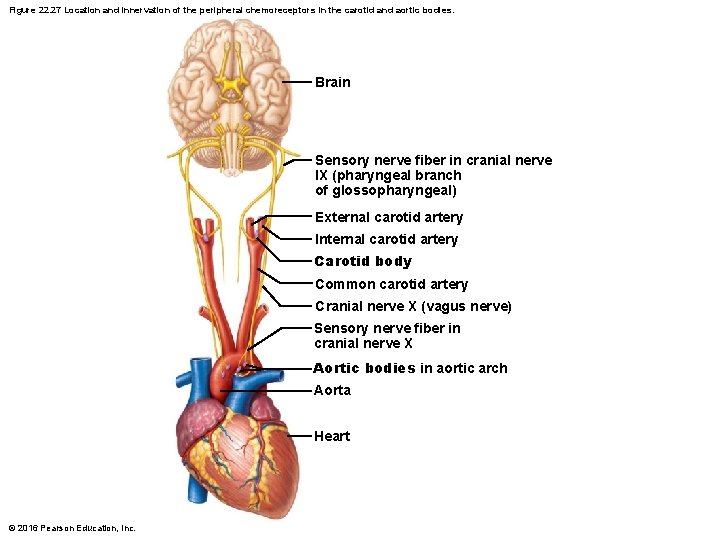
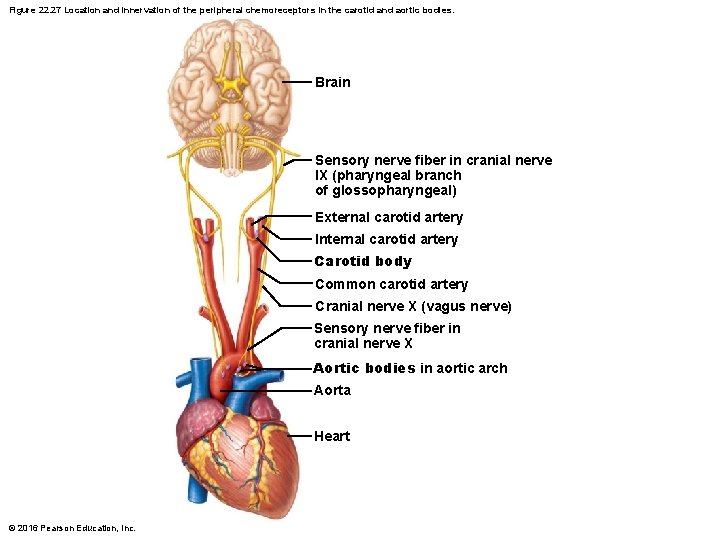
Figure 22. 27 Location and innervation of the peripheral chemoreceptors in the carotid and aortic bodies. Brain Sensory nerve fiber in cranial nerve IX (pharyngeal branch of glossopharyngeal) External carotid artery Internal carotid artery Carotid body Common carotid artery Cranial nerve X (vagus nerve) Sensory nerve fiber in cranial nerve X Aortic bodies in aortic arch Aorta Heart © 2016 Pearson Education, Inc.
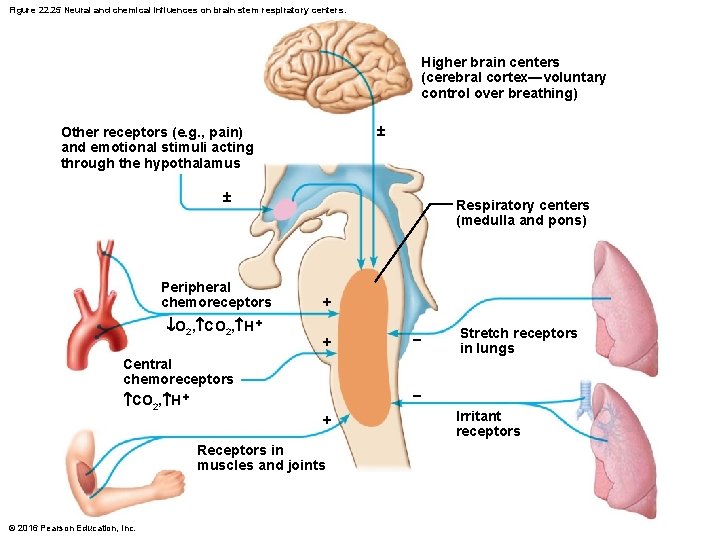
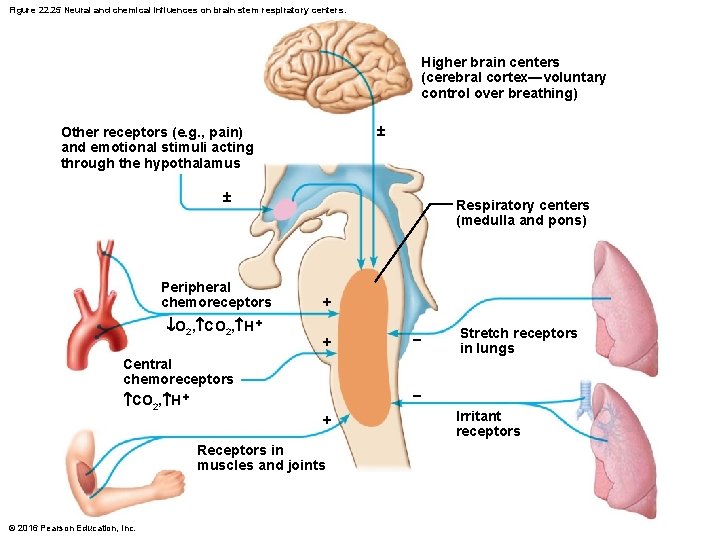
Figure 22. 25 Neural and chemical influences on brain stem respiratory centers. Higher brain centers (cerebral cortex—voluntary control over breathing) Other receptors (e. g. , pain) and emotional stimuli acting through the hypothalamus Peripheral chemoreceptors O 2, CO 2, H + Central chemoreceptors CO 2, H + Respiratory centers (medulla and pons) + + Stretch receptors in lungs + Receptors in muscles and joints © 2016 Pearson Education, Inc. Irritant receptors
High Altitude • Quick travel to altitudes above 2400 meters (8000 feet) may trigger symptoms of acute mountain sickness (AMS) – Atmospheric pressure and PO 2 levels are lower at high elevations – Symptoms: headaches, shortness of breath, nausea, and dizziness – In severe cases, lethal cerebral and pulmonary edema may occur © 2016 Pearson Education, Inc.
High Altitude (cont. ) • Acclimatization: respiratory and hematopoietic adjustments are made with long-term moves to high altitude – Chemoreceptors become more responsive to PCO 2 when PO 2 declines – Substantial decline in PO 2 directly stimulates peripheral chemoreceptors – Results in increases in minute ventilation that stabilize in few days to 2– 3 L/min higher than at sea level © 2016 Pearson Education, Inc.
High Altitude (cont. ) • High altitude conditions always result in lowerthan-normal Hb saturation levels – Due to availability of less O 2 • Decline in blood O 2 stimulates kidneys to accelerate production of EPO • RBC numbers increase slowly to provide longterm compensation © 2016 Pearson Education, Inc.
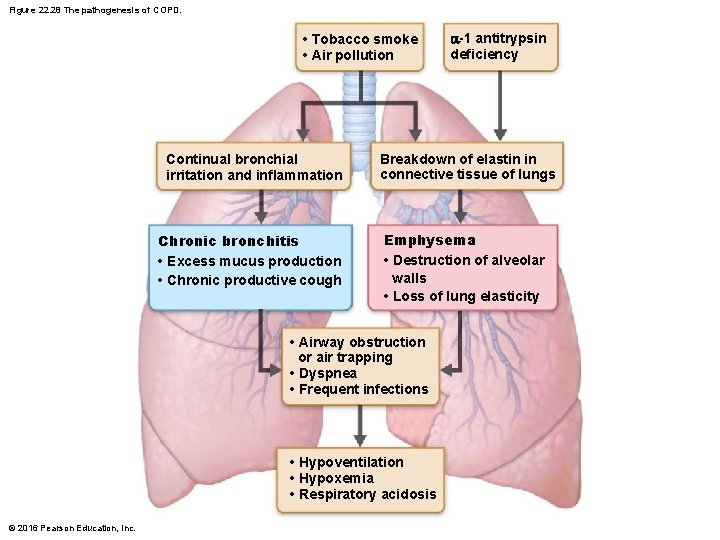
22. 10 Lung Diseases Chronic Obstructive Pulmonary Disease (COPD) • Exemplified by chronic emphysema and chronic bronchitis • Key feature is irreversible decrease in ability to force air out of lungs © 2016 Pearson Education, Inc.
Chronic Obstructive Pulmonary Disease (COPD) (cont. ) • Other common features: – History of smoking in 80% of patients – Dyspnea: labored breathing (“air hunger”) – Coughing and frequent pulmonary infections – Most patients develop hypoventilation accompanied by respiratory acidosis, hypoxemia © 2016 Pearson Education, Inc.
Chronic Obstructive Pulmonary Disease (COPD) (cont. ) • Emphysema – Permanent enlargement of alveoli and destruction of alveolar walls result in decreased lung elasticity, with three consequences: 1. Accessory muscles are necessary for breathing, leading to exhaustion from using 10– 15% more energy to breathe than normal 2. Trapped air causes hyperinflation, which flattens diaphragm and causes expanded barrel chest, both of which reduces ventilation efficiency 3. Damaged pulmonary capillaries lead to enlarged right ventricle – Hereditary factors for disease include alpha-1 antitrypsin deficiency © 2016 Pearson Education, Inc.
Chronic Obstructive Pulmonary Disease (COPD) (cont. ) • Chronic bronchitis – Inhaled irritants cause chronic excessive mucus – Mucosae of lower respiratory passageways become inflamed and fibrosed – Results in obstructed airways that impair lung ventilation and gas exchange – Symptoms include frequent pulmonary infections – Risk factors include smoking and environmental pollutants © 2016 Pearson Education, Inc.
Chronic Obstructive Pulmonary Disease (COPD) (cont. ) • COPD symptoms and treatment – Strength of patient’s innate respiratory drive is reason behind different symptoms seen • “Pink puffers”: patient usually thin because they burn large amount of energy breathing; near-normal blood gases are maintained, so skin color is normal • “Blue bloaters”: patient usually stocky; cyanosis is due to hypoxia, so skin color takes on bluish hue – Treatment: bronchodilators, corticosteroids, oxygen, sometimes lung volume reduction surgery; oxygen must be administered carefully © 2016 Pearson Education, Inc.
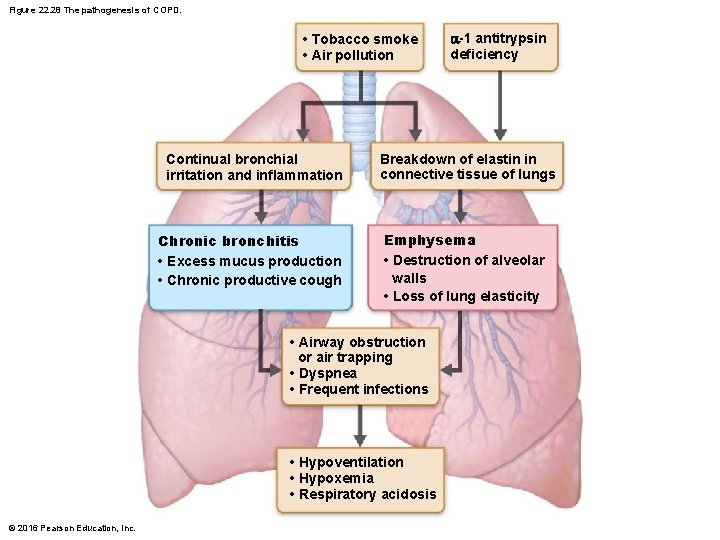
Figure 22. 28 The pathogenesis of COPD. • Tobacco smoke • Air pollution Continual bronchial irritation and inflammation Chronic bronchitis • Excess mucus production • Chronic productive cough Breakdown of elastin in connective tissue of lungs Emphysema • Destruction of alveolar walls • Loss of lung elasticity • Airway obstruction or air trapping • Dyspnea • Frequent infections • Hypoventilation • Hypoxemia • Respiratory acidosis © 2016 Pearson Education, Inc. -1 antitrypsin deficiency
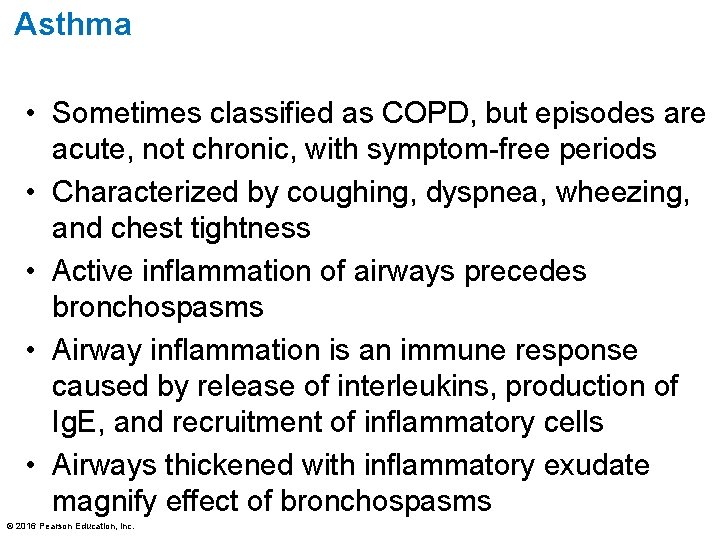
Asthma • Sometimes classified as COPD, but episodes are acute, not chronic, with symptom-free periods • Characterized by coughing, dyspnea, wheezing, and chest tightness • Active inflammation of airways precedes bronchospasms • Airway inflammation is an immune response caused by release of interleukins, production of Ig. E, and recruitment of inflammatory cells • Airways thickened with inflammatory exudate magnify effect of bronchospasms © 2016 Pearson Education, Inc.
Tuberculosis (TB) • Infectious disease caused by bacterium Mycobacterium tuberculosis • Symptoms: fever, night sweats, weight loss, racking cough, coughing up blood • Treatment: 12 -month course of antibiotics – Antibiotic-resistant strains have been seen, including multidrug-resistant strains © 2016 Pearson Education, Inc.
Lung Cancer • Leading cause of cancer deaths in North America • 90% of all cases are result of smoking © 2016 Pearson Education, Inc.
Lung Cancer (cont. ) • Three most common types: – Adenocarcinoma (~40% of cases) originates in peripheral lung areas; develops from bronchial glands and alveolar cells – Squamous cell carcinoma (20– 40% of cases) arises in bronchial epithelium – Small cell carcinoma (~20% of cases) contains lymphocyte-like cells that originate in primary bronchi and subsequently metastasize © 2016 Pearson Education, Inc.
Lung Cancer (cont. ) • Treatment for lung cancer – Early detection is key to survival – If metastasis has not occurred: surgery to remove diseased lung tissue – If metastasis has occurred: radiation and chemotherapy – Several new therapies are on horizon © 2016 Pearson Education, Inc.
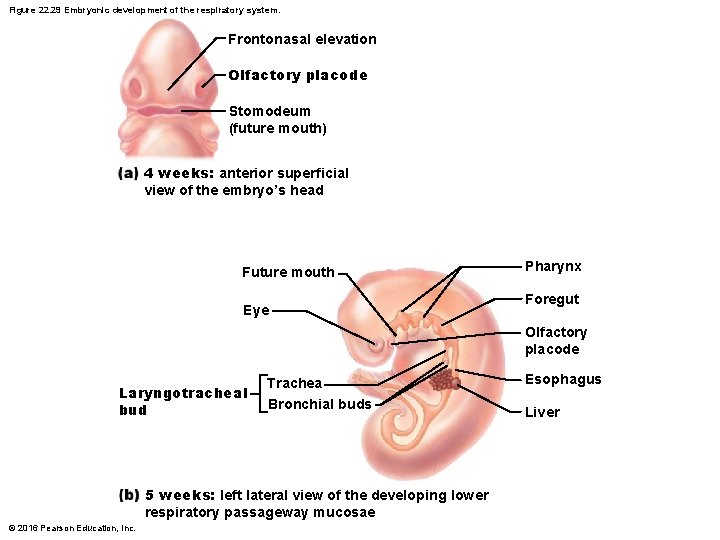
Developmental Aspects of Respiratory System • Upper respiratory structures develop first • Olfactory placodes invaginate into olfactory pits (form nasal cavities) present by week 4 • Laryngotracheal bud is present by week 5 • Mucosae of bronchi and lung alveoli are present by eighth week • By week 28, premature baby can breathe on its own • During fetal life, lungs are filled with fluid, and blood bypasses the lungs • Gas exchange takes place via placenta © 2016 Pearson Education, Inc.
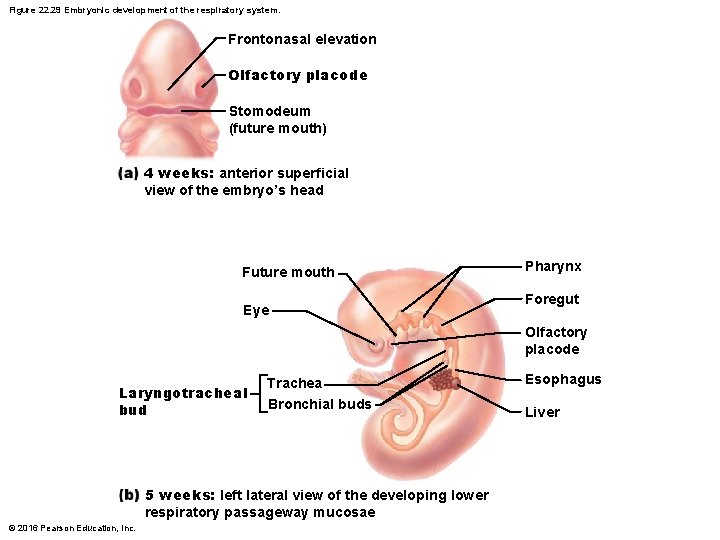
Figure 22. 29 Embryonic development of the respiratory system. Frontonasal elevation Olfactory placode Stomodeum (future mouth) 4 weeks: anterior superficial view of the embryo’s head Future mouth Eye Pharynx Foregut Olfactory placode Laryngotracheal bud Trachea Bronchial buds 5 weeks: left lateral view of the developing lower respiratory passageway mucosae © 2016 Pearson Education, Inc. Esophagus Liver
Developmental Aspects of Respiratory System • At birth, respiratory centers are activated, alveoli inflate, and lungs begin to function • Takes 2 weeks after birth before lungs are fully inflated • Respiratory rate is highest in newborns (40– 80 breaths/min) and slows until adulthood (12– 16 breaths/min) • Lungs continue to mature, and more alveoli are formed until young adulthood • Respiratory efficiency decreases in old age © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 16 • Cystic fibrosis – Most common lethal genetic disease in North America – Abnormal, viscous mucus clogs passageways, which can lead to bacterial infections • Affects lungs, pancreatic ducts, and reproductive ducts © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 16 • Cystic fibrosis (cont. ) – Caused by an abnormal gene for Cl membrane channel protein, cystic fibrosis transmembrane conductance regulator (CFTR) • Abnormal CFTR protein gets stuck in endoplasmic reticulum (ER), so never reaches cell membrane to carry out Cl transport function © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 16 • Treatments for cystic fibrosis – Mucus-dissolving drugs, manipulation to loosen mucus and antibiotics – Inhalation hypertonic saline to thin mucus – Ongoing research involves: 1. Introducing normal CFTR genes into respiratory tract mucosa cells 2. Prodding different protein to take over Cl channel protein duties 3. Freeing patient’s abnormal CFTR protein from ER © 2016 Pearson Education, Inc.