Chapter 22 Part A The Respiratory System Annie

- Slides: 56
Chapter 22 Part A The Respiratory System © Annie Leibovitz/Contact Press Images © 2016 Pearson Education, Inc. Power. Point® Lecture Slides prepared by Karen Dunbar Kareiva Ivy Tech Community College
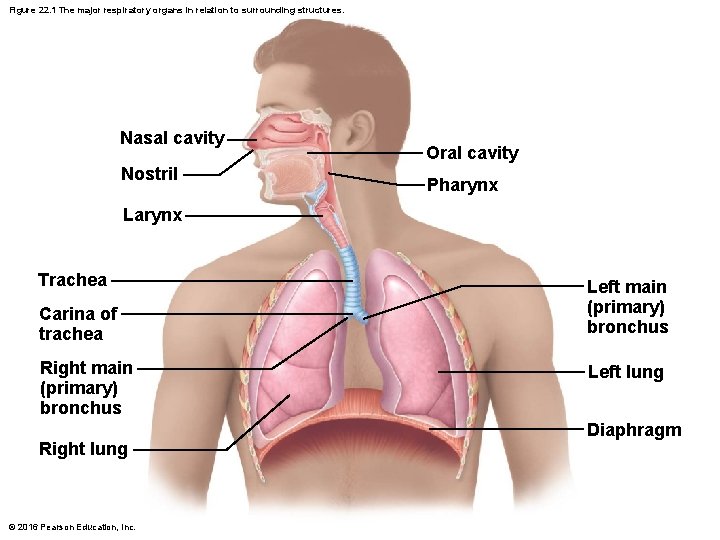
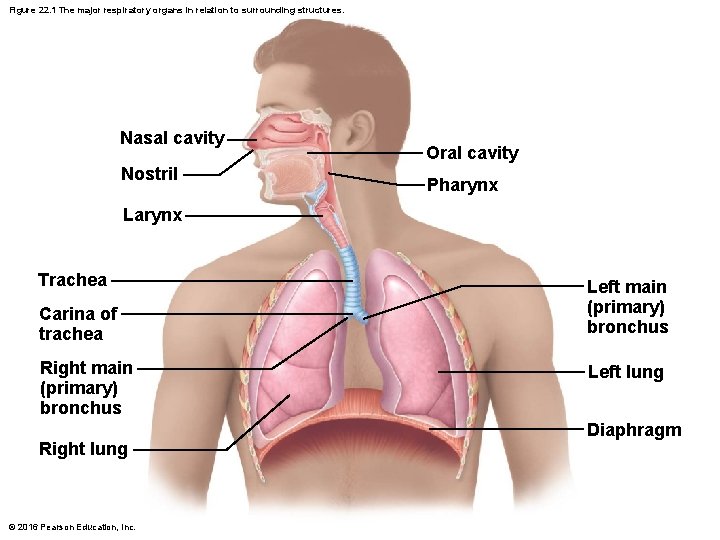
Figure 22. 1 The major respiratory organs in relation to surrounding structures. Nasal cavity Nostril Oral cavity Pharynx Larynx Trachea Carina of trachea Right main (primary) bronchus Right lung © 2016 Pearson Education, Inc. Left main (primary) bronchus Left lung Diaphragm
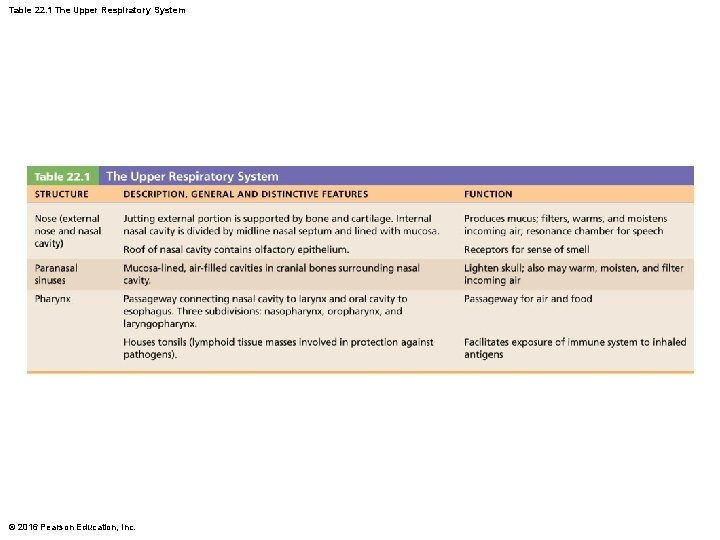
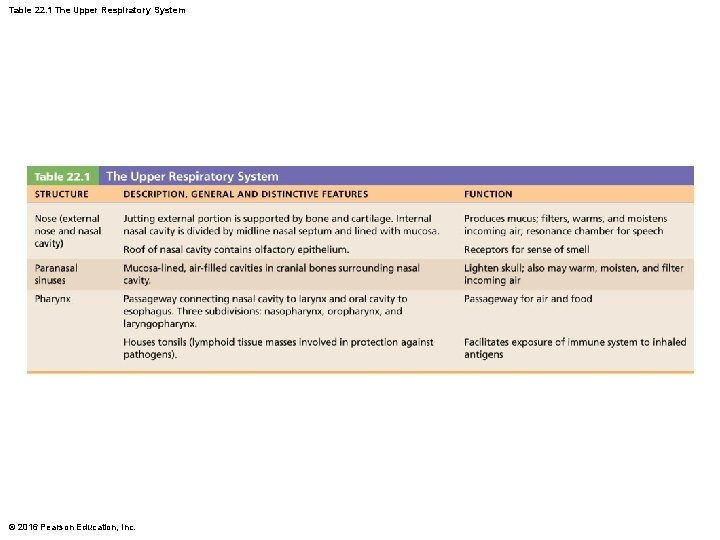
Table 22. 1 The Upper Respiratory System © 2016 Pearson Education, Inc.
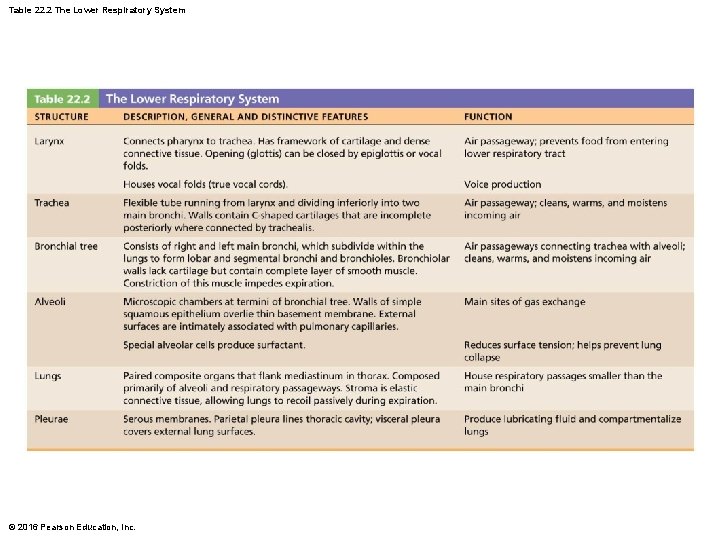
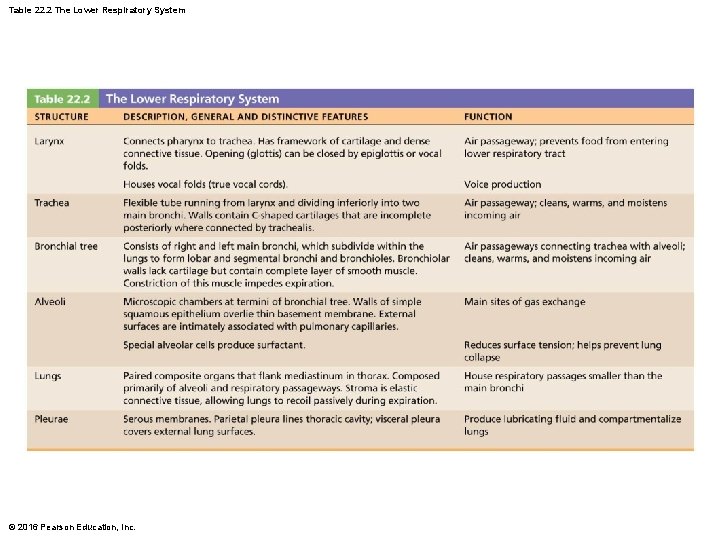
Table 22. 2 The Lower Respiratory System © 2016 Pearson Education, Inc.
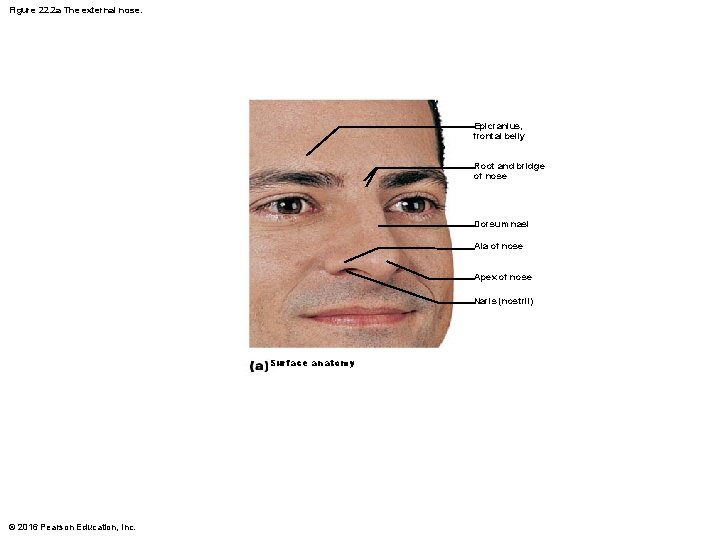
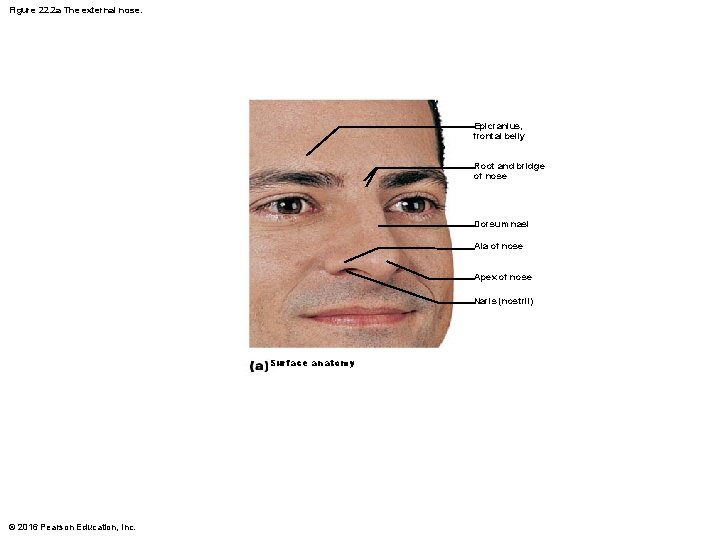
Figure 22. 2 a The external nose. Epicranius, frontal belly Root and bridge of nose Dorsum nasi Ala of nose Apex of nose Naris (nostril) Surface anatomy © 2016 Pearson Education, Inc.
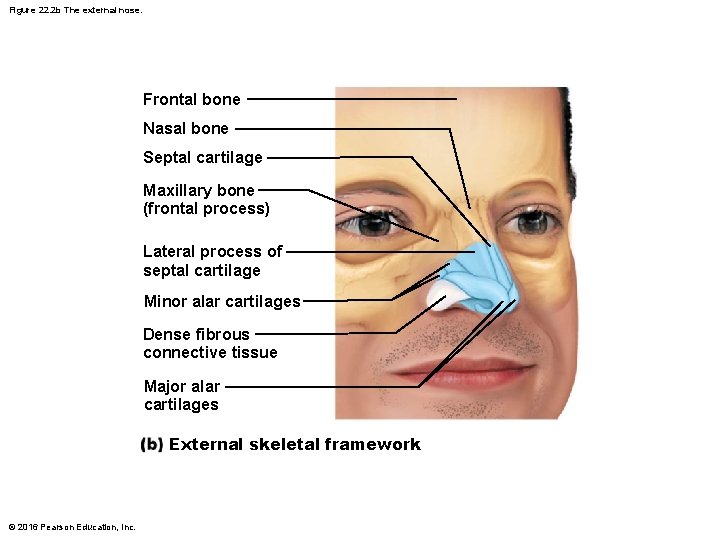
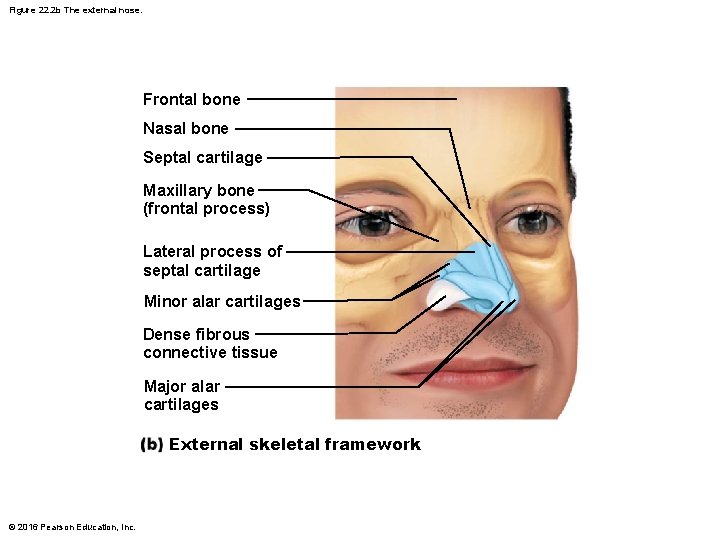
Figure 22. 2 b The external nose. Frontal bone Nasal bone Septal cartilage Maxillary bone (frontal process) Lateral process of septal cartilage Minor alar cartilages Dense fibrous connective tissue Major alar cartilages External skeletal framework © 2016 Pearson Education, Inc.
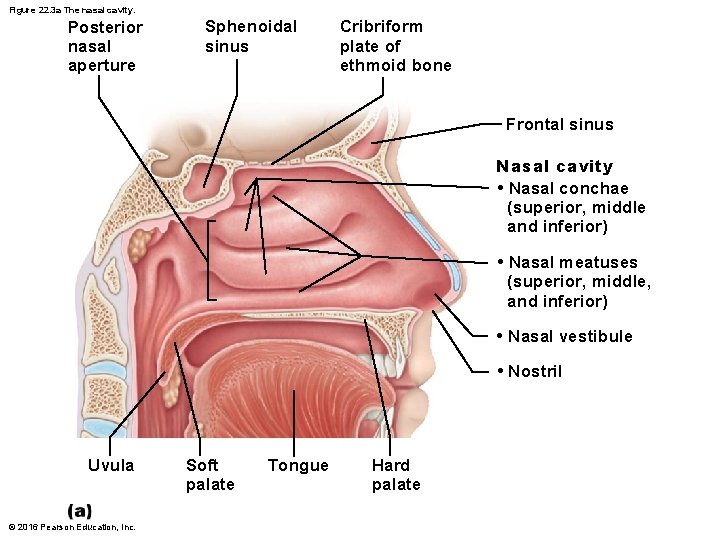
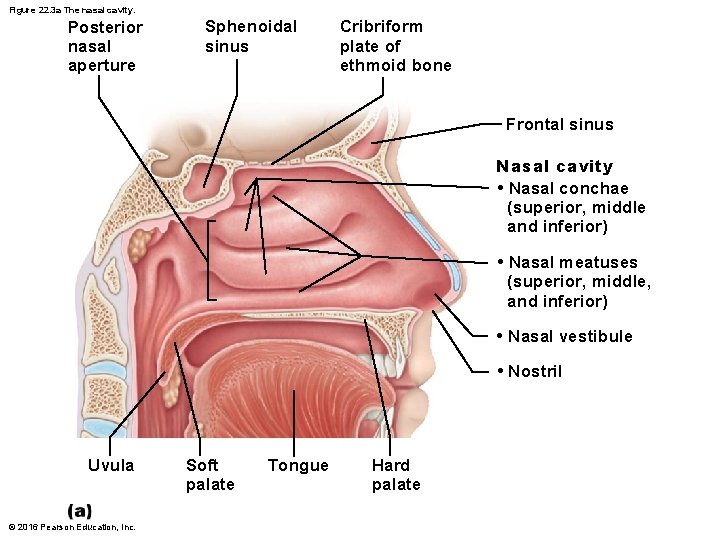
Figure 22. 3 a The nasal cavity. Posterior nasal aperture Sphenoidal sinus Cribriform plate of ethmoid bone Frontal sinus Nasal cavity • Nasal conchae (superior, middle and inferior) • Nasal meatuses (superior, middle, and inferior) • Nasal vestibule • Nostril Uvula © 2016 Pearson Education, Inc. Soft palate Tongue Hard palate
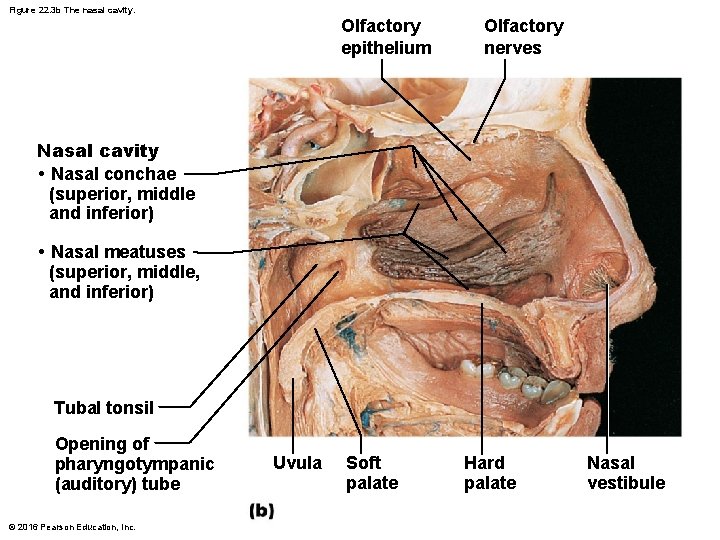
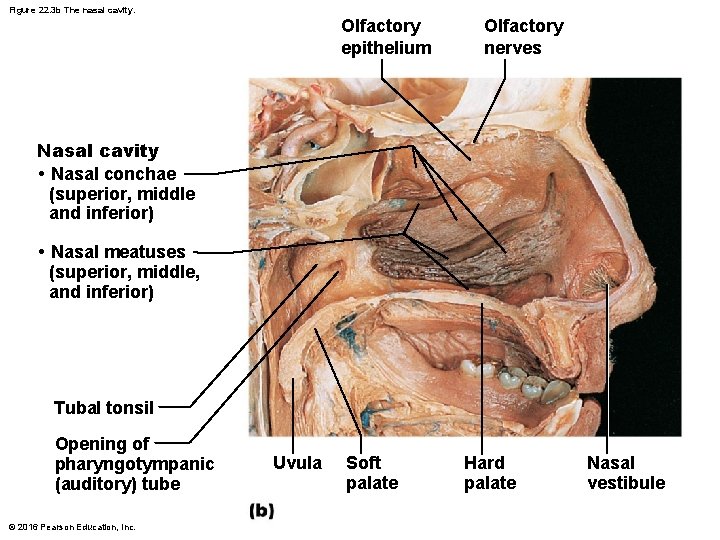
Figure 22. 3 b The nasal cavity. Olfactory epithelium Olfactory nerves Nasal cavity • Nasal conchae (superior, middle and inferior) • Nasal meatuses (superior, middle, and inferior) Tubal tonsil Opening of pharyngotympanic (auditory) tube © 2016 Pearson Education, Inc. Uvula Soft palate Hard palate Nasal vestibule
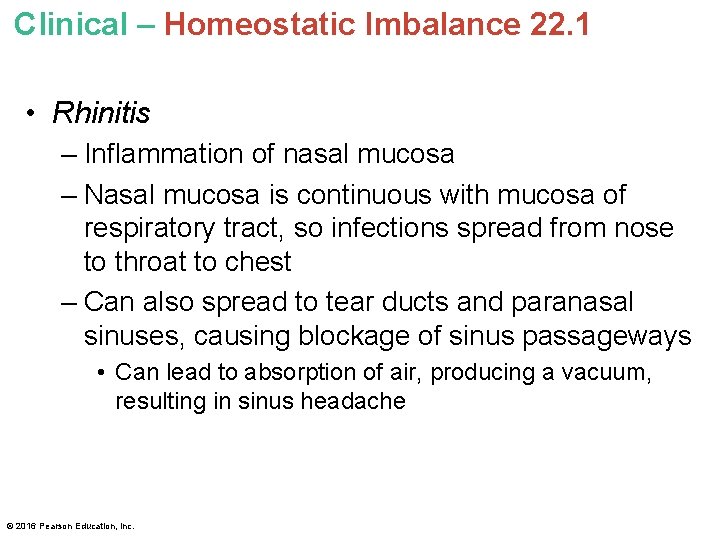
Clinical – Homeostatic Imbalance 22. 1 • Rhinitis – Inflammation of nasal mucosa – Nasal mucosa is continuous with mucosa of respiratory tract, so infections spread from nose to throat to chest – Can also spread to tear ducts and paranasal sinuses, causing blockage of sinus passageways • Can lead to absorption of air, producing a vacuum, resulting in sinus headache © 2016 Pearson Education, Inc.
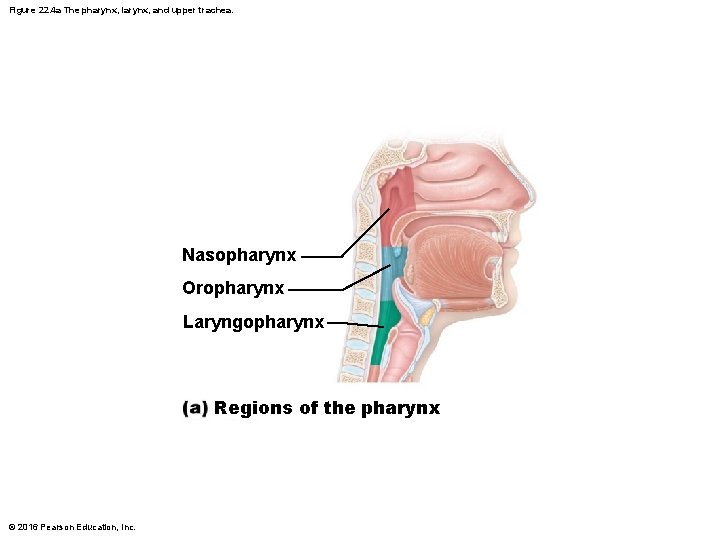
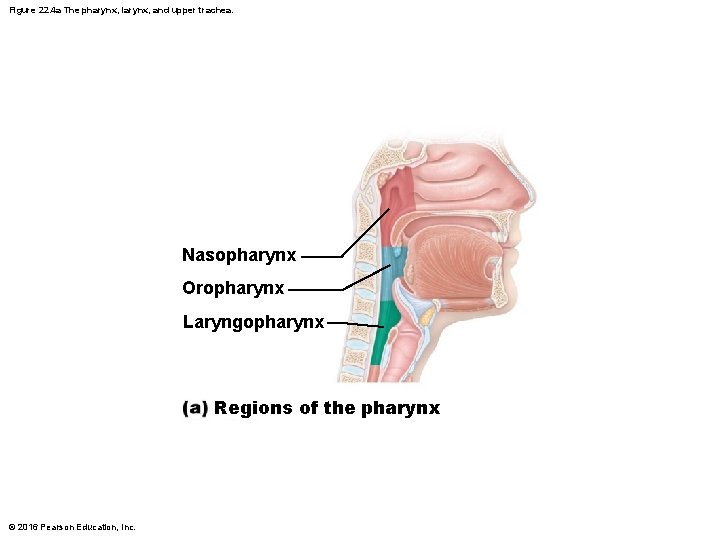
Figure 22. 4 a The pharynx, larynx, and upper trachea. Nasopharynx Oropharynx Laryngopharynx Regions of the pharynx © 2016 Pearson Education, Inc.
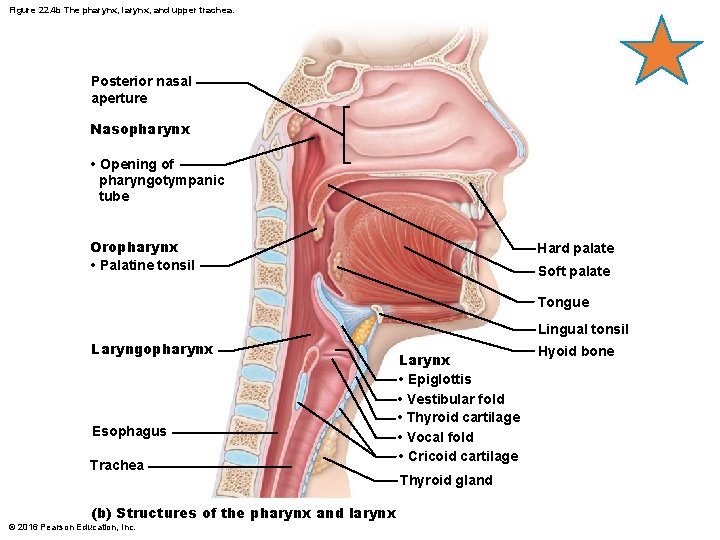
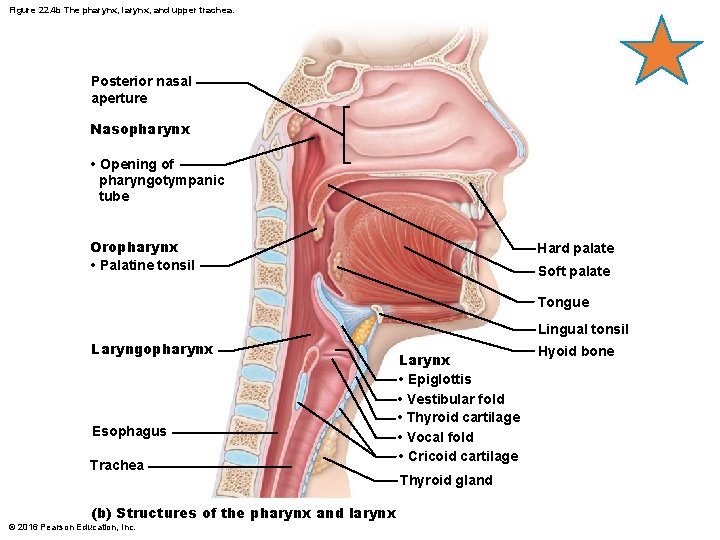
Figure 22. 4 b The pharynx, larynx, and upper trachea. Posterior nasal aperture Nasopharynx • Opening of pharyngotympanic tube Oropharynx • Palatine tonsil Hard palate Soft palate Tongue Lingual tonsil Laryngopharynx Esophagus Trachea (b) Structures of the pharynx and larynx © 2016 Pearson Education, Inc. Larynx • Epiglottis • Vestibular fold • Thyroid cartilage • Vocal fold • Cricoid cartilage Thyroid gland Hyoid bone
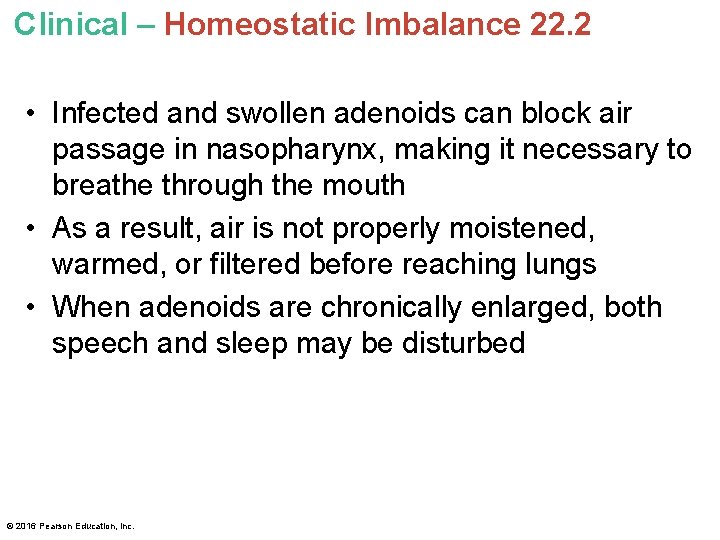
Clinical – Homeostatic Imbalance 22. 2 • Infected and swollen adenoids can block air passage in nasopharynx, making it necessary to breathe through the mouth • As a result, air is not properly moistened, warmed, or filtered before reaching lungs • When adenoids are chronically enlarged, both speech and sleep may be disturbed © 2016 Pearson Education, Inc.
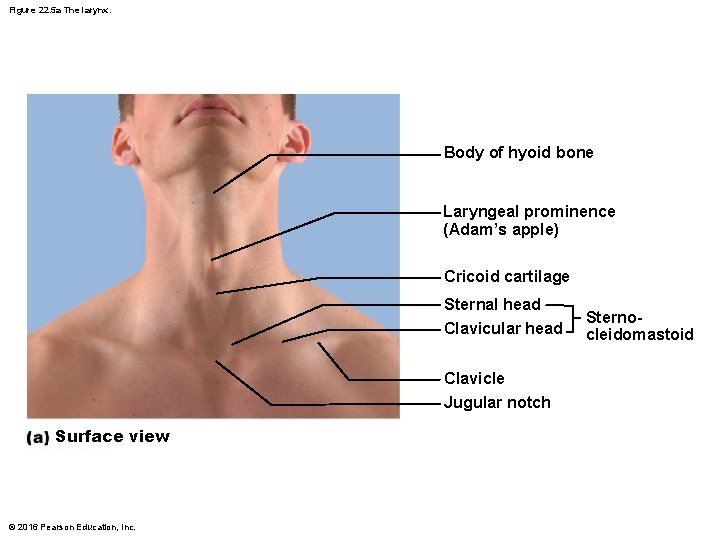
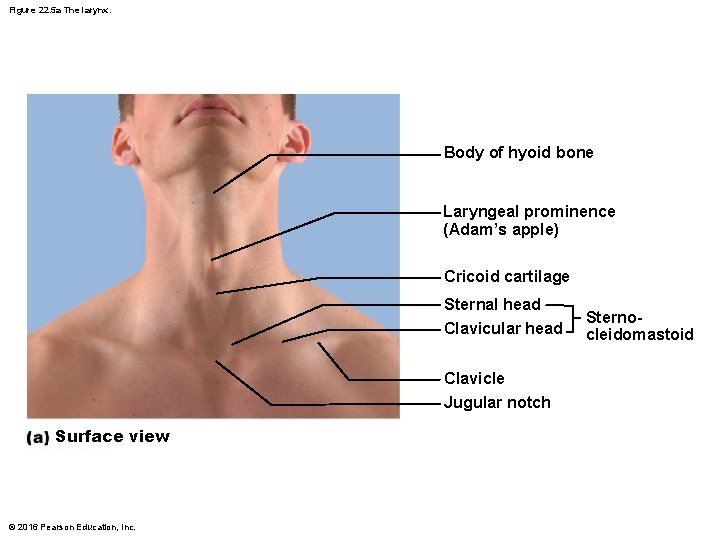
Figure 22. 5 a The larynx. Body of hyoid bone Laryngeal prominence (Adam’s apple) Cricoid cartilage Sternal head Clavicular head Clavicle Jugular notch Surface view © 2016 Pearson Education, Inc. Sternocleidomastoid
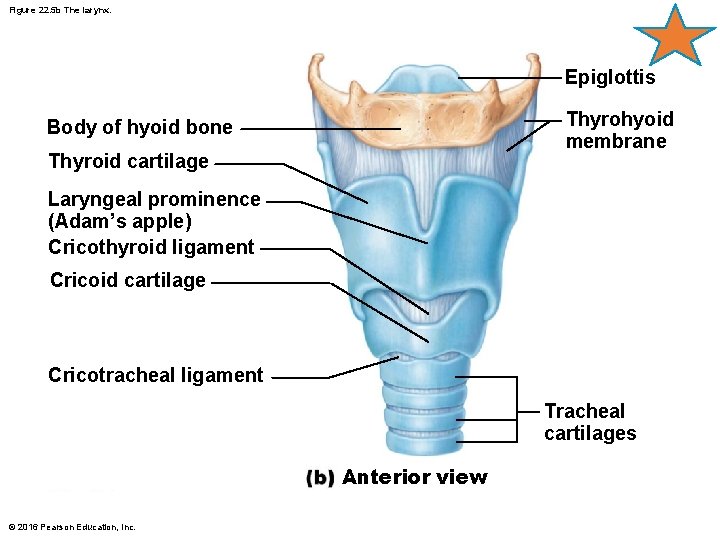
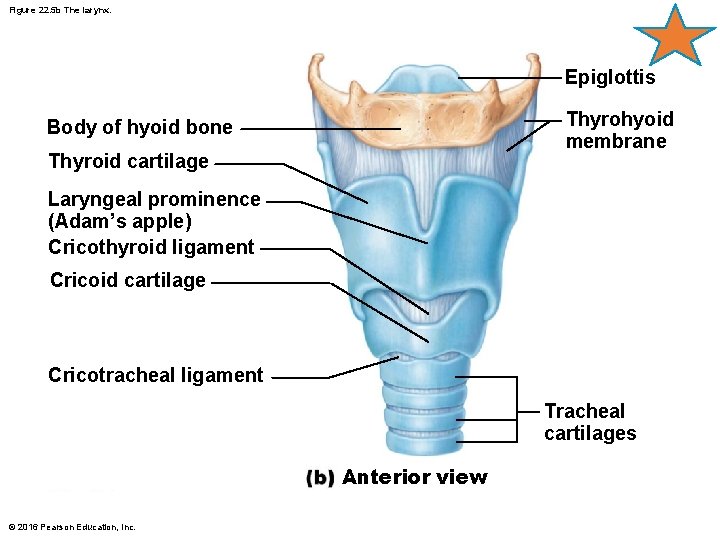
Figure 22. 5 b The larynx. Epiglottis Thyrohyoid membrane Body of hyoid bone Thyroid cartilage Laryngeal prominence (Adam’s apple) Cricothyroid ligament Cricoid cartilage Cricotracheal ligament Tracheal cartilages Anterior view © 2016 Pearson Education, Inc.
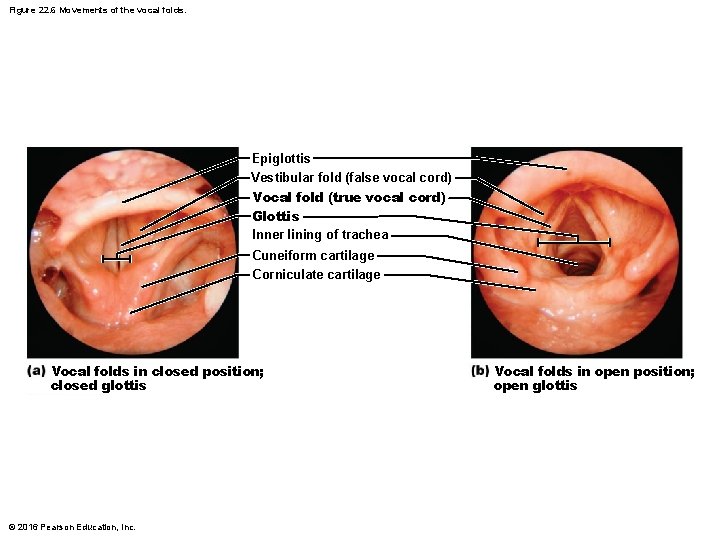
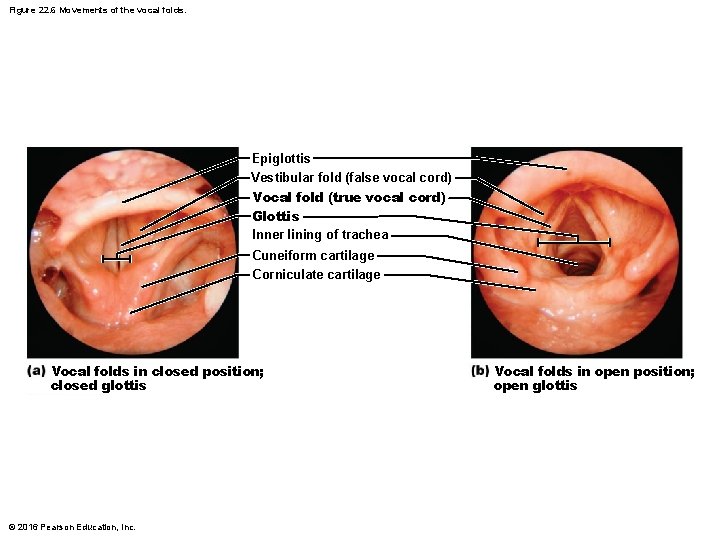
Figure 22. 6 Movements of the vocal folds. Epiglottis Vestibular fold (false vocal cord) Vocal fold (true vocal cord) Glottis Inner lining of trachea Cuneiform cartilage Corniculate cartilage Vocal folds in closed position; closed glottis © 2016 Pearson Education, Inc. Vocal folds in open position; open glottis
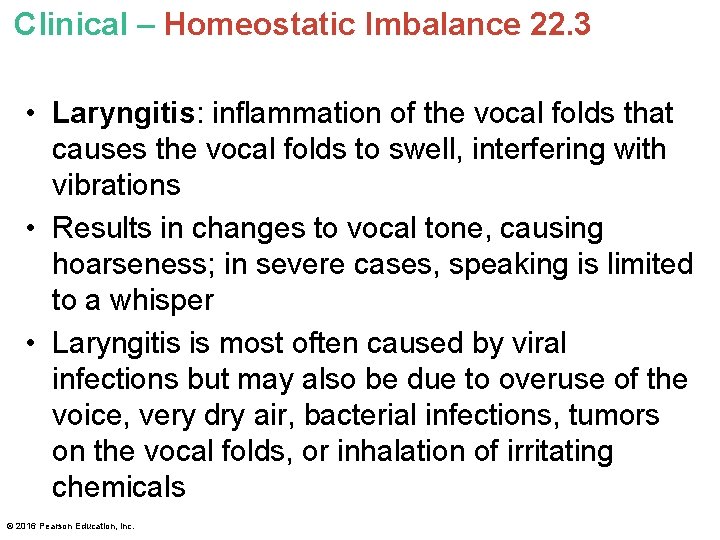
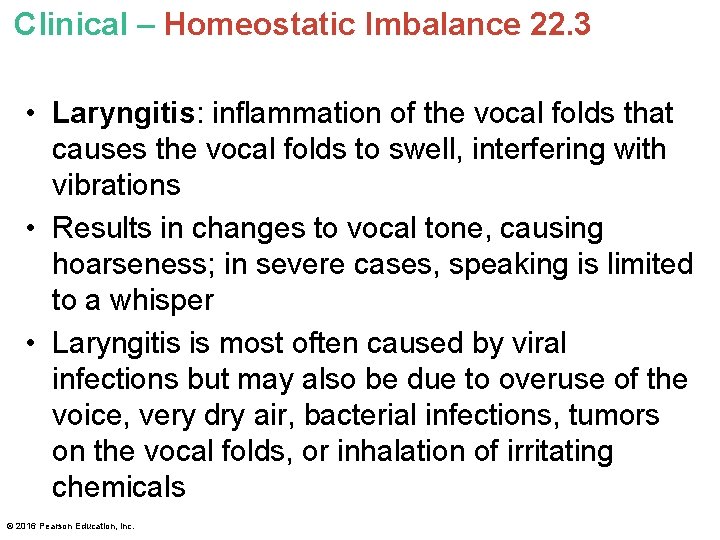
Clinical – Homeostatic Imbalance 22. 3 • Laryngitis: inflammation of the vocal folds that causes the vocal folds to swell, interfering with vibrations • Results in changes to vocal tone, causing hoarseness; in severe cases, speaking is limited to a whisper • Laryngitis is most often caused by viral infections but may also be due to overuse of the voice, very dry air, bacterial infections, tumors on the vocal folds, or inhalation of irritating chemicals © 2016 Pearson Education, Inc.
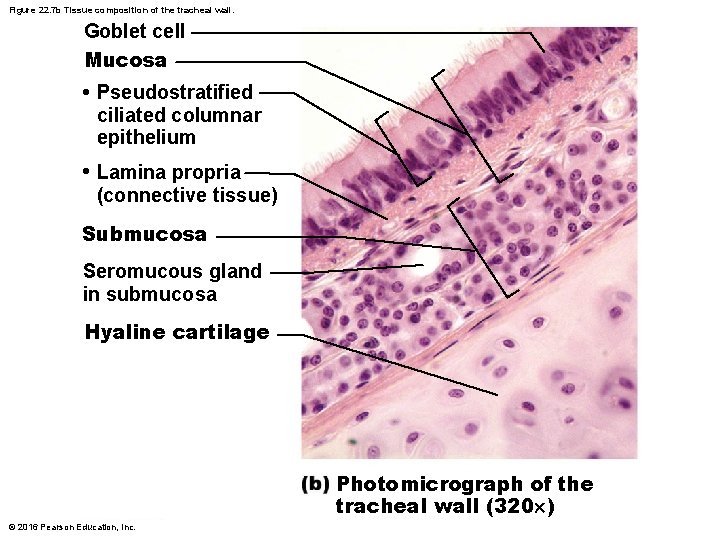
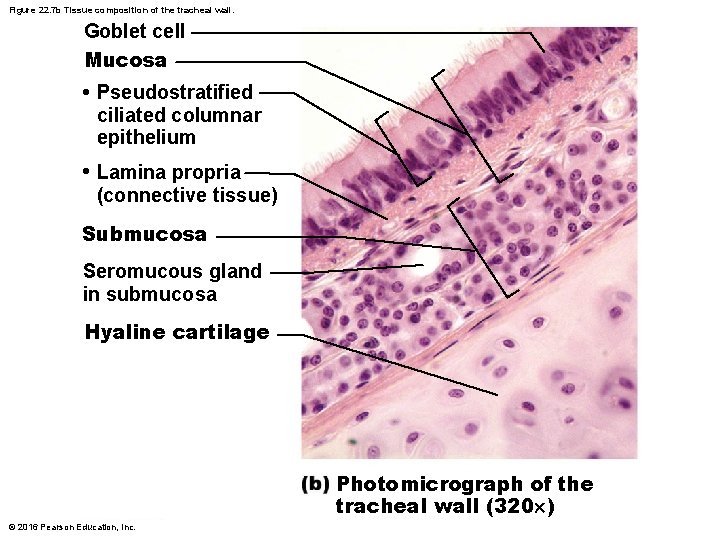
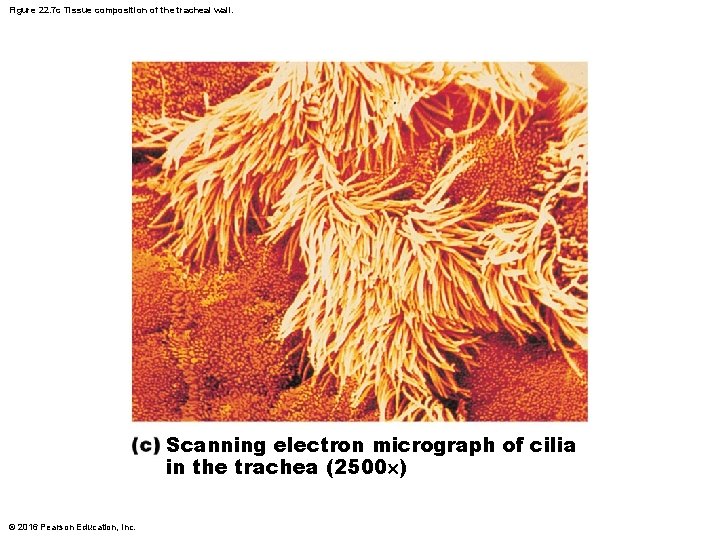
Figure 22. 7 b Tissue composition of the tracheal wall. Goblet cell Mucosa • Pseudostratified ciliated columnar epithelium • Lamina propria (connective tissue) Submucosa Seromucous gland in submucosa Hyaline cartilage Photomicrograph of the tracheal wall (320 ) © 2016 Pearson Education, Inc.
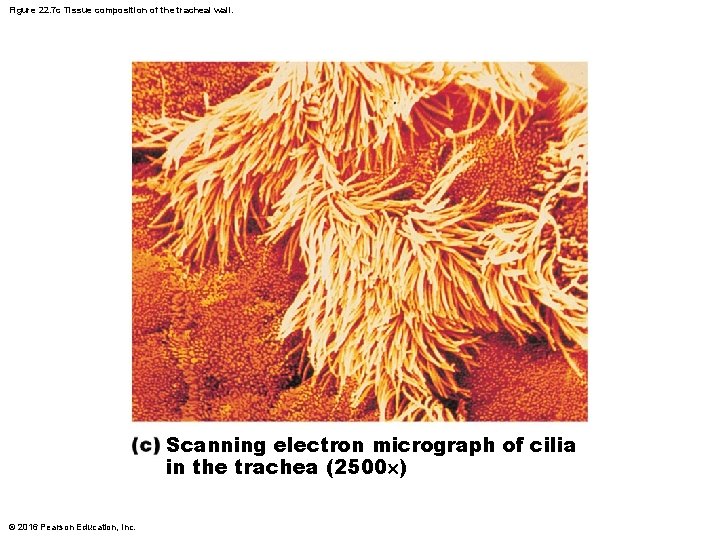
Figure 22. 7 c Tissue composition of the tracheal wall. Scanning electron micrograph of cilia in the trachea (2500 ) © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 4 • Smoking inhibits and ultimately destroys cilia • Without ciliary activity, coughing is only way to prevent mucus from accumulating in lungs – Reason smokers with respiratory congestion should avoid medications that inhibit cough reflex © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 5 • Tracheal obstruction is life threatening: many people have suffocated after choking on a piece of food that suddenly closed off their trachea • Heimlich maneuver: procedure in which air in victim’s lungs is used to “pop out, ” or expel, an obstructing piece of food • Maneuver is simple to learn and easy to do but is best learned by demonstration; when done incorrectly, may lead to cracked ribs © 2016 Pearson Education, Inc.

Figure 22. 8 Conducting zone passages. Trachea Superior lobe of left lung Left main (primary) bronchus Superior lobe of right lung Lobar (secondary) bronchus Middle lobe of right lung Segmental (tertiary) bronchus Inferior lobe of right lung Inferior lobe of left lung © 2016 Pearson Education, Inc.
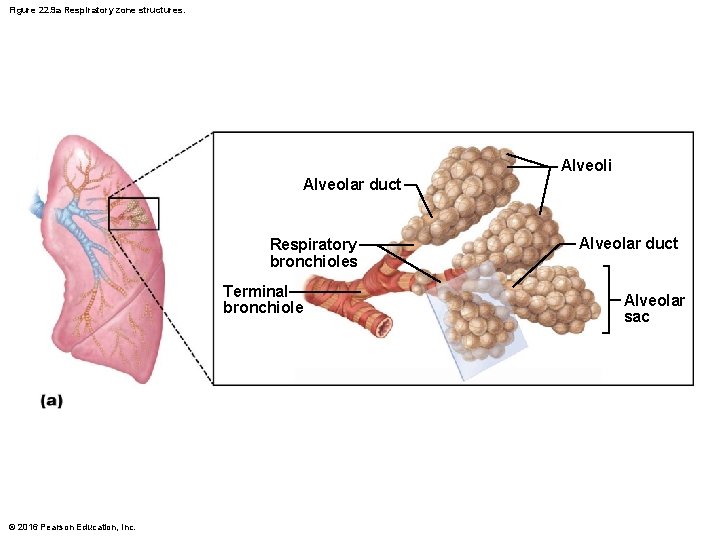
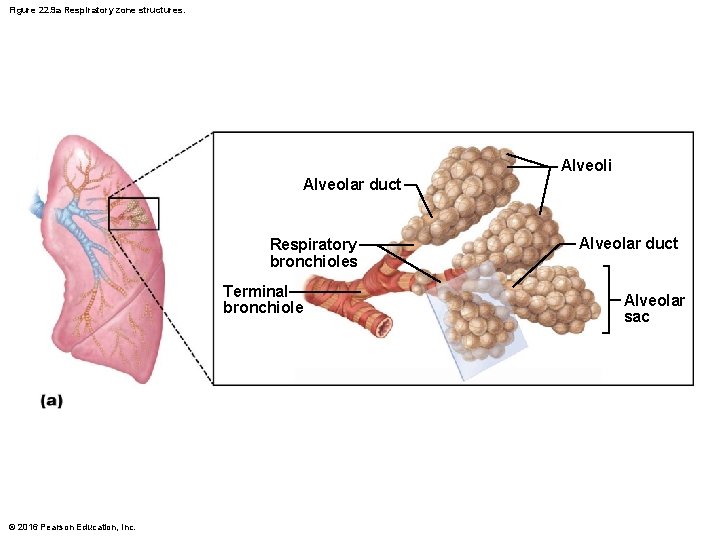
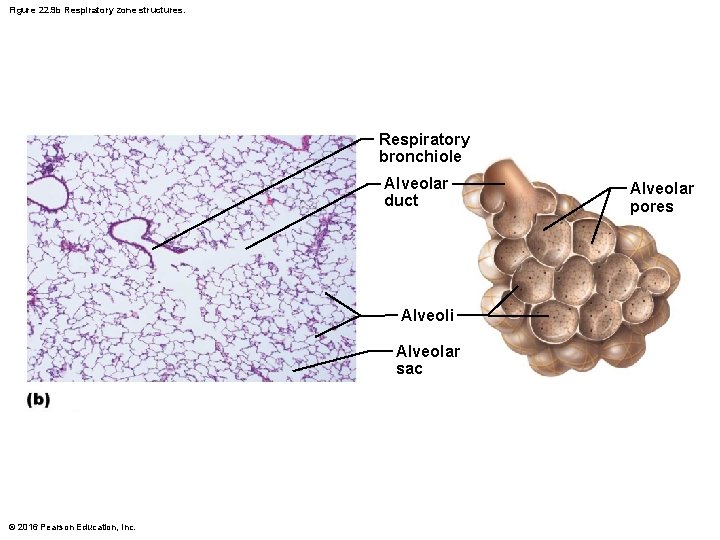
Figure 22. 9 a Respiratory zone structures. Alveoli Alveolar duct Respiratory bronchioles Terminal bronchiole © 2016 Pearson Education, Inc. Alveolar duct Alveolar sac
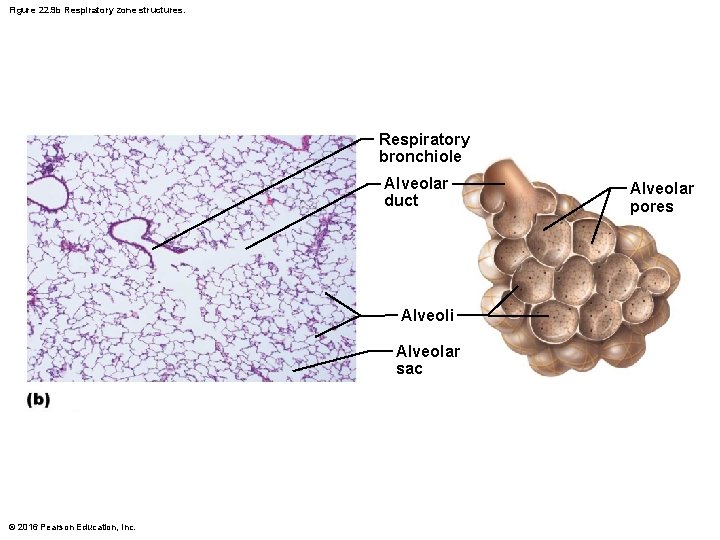
Figure 22. 9 b Respiratory zone structures. Respiratory bronchiole Alveolar duct Alveoli Alveolar sac © 2016 Pearson Education, Inc. Alveolar pores
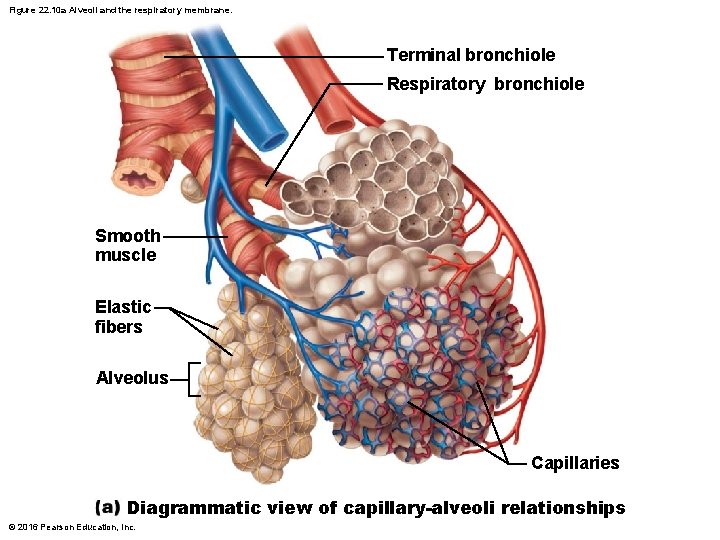
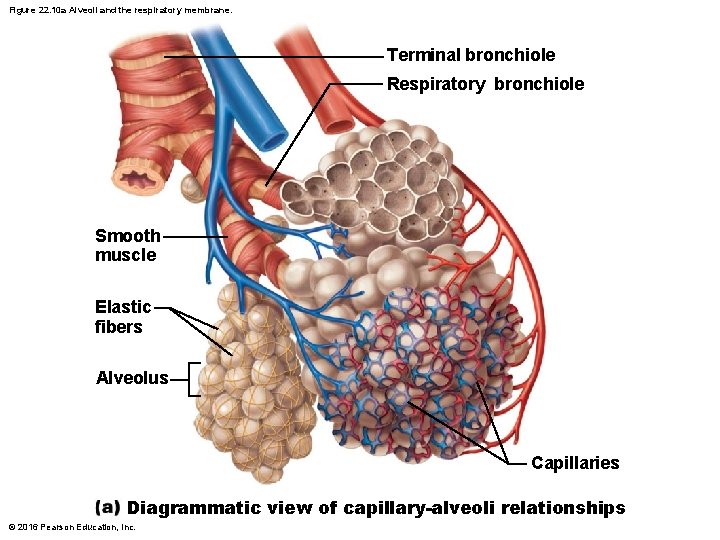
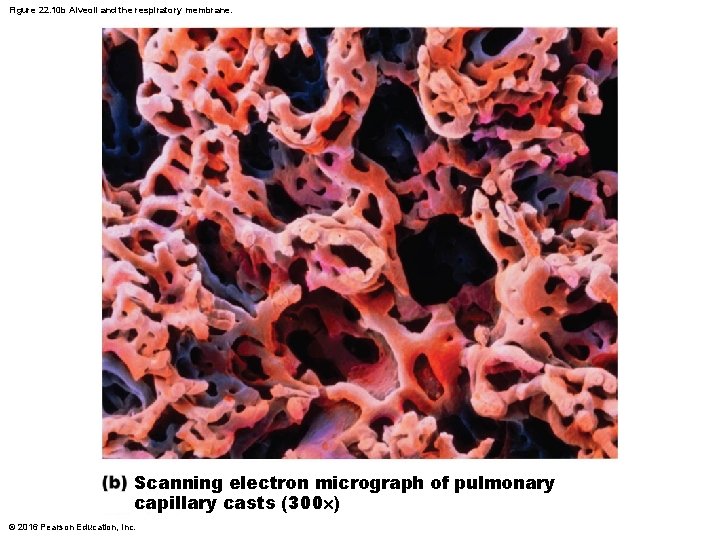
Figure 22. 10 a Alveoli and the respiratory membrane. Terminal bronchiole Respiratory bronchiole Smooth muscle Elastic fibers Alveolus Capillaries Diagrammatic view of capillary-alveoli relationships © 2016 Pearson Education, Inc.
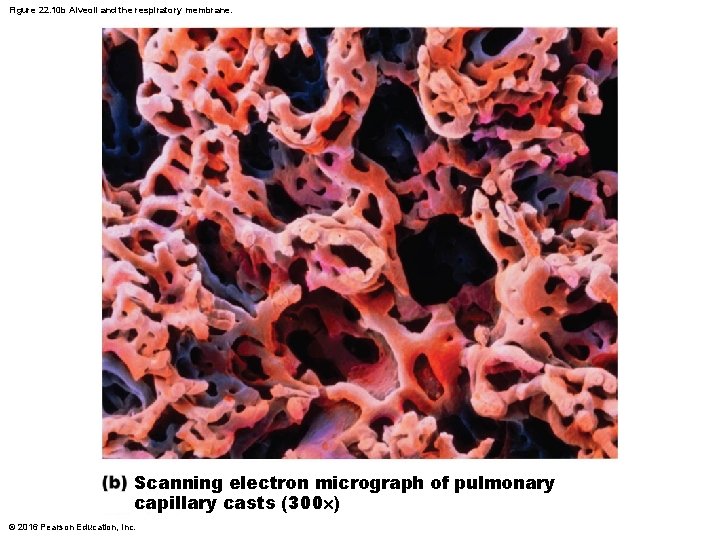
Figure 22. 10 b Alveoli and the respiratory membrane. Scanning electron micrograph of pulmonary capillary casts (300 ) © 2016 Pearson Education, Inc.
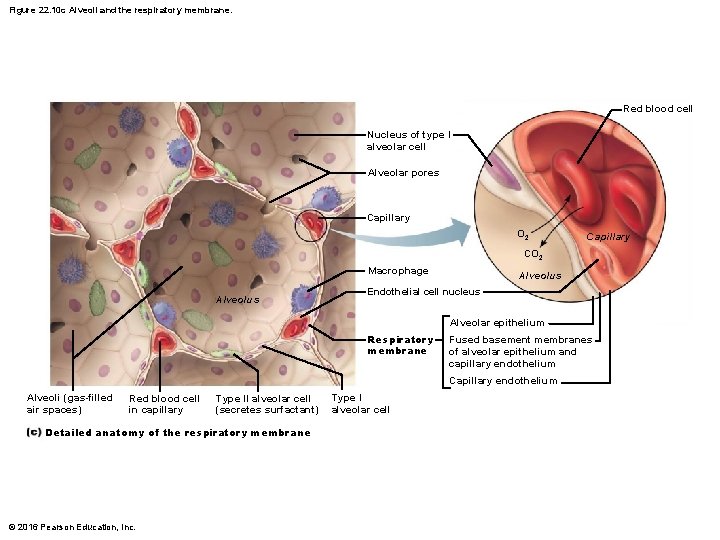
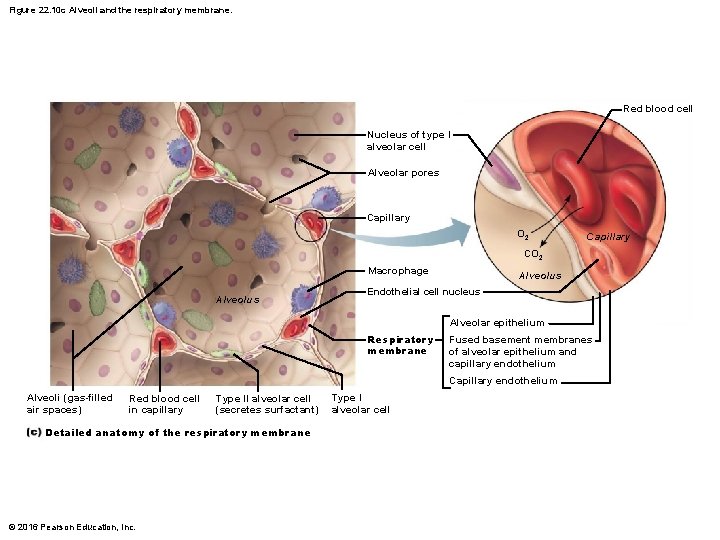
Figure 22. 10 c Alveoli and the respiratory membrane. Red blood cell Nucleus of type I alveolar cell Alveolar pores Capillary O 2 Capillary CO 2 Macrophage Alveolus Endothelial cell nucleus Alveolar epithelium Respiratory membrane Fused basement membranes of alveolar epithelium and capillary endothelium Capillary endothelium Alveoli (gas-filled air spaces) Red blood cell in capillary Type II alveolar cell (secretes surfactant) Detailed anatomy of the respiratory membrane © 2016 Pearson Education, Inc. Type I alveolar cell
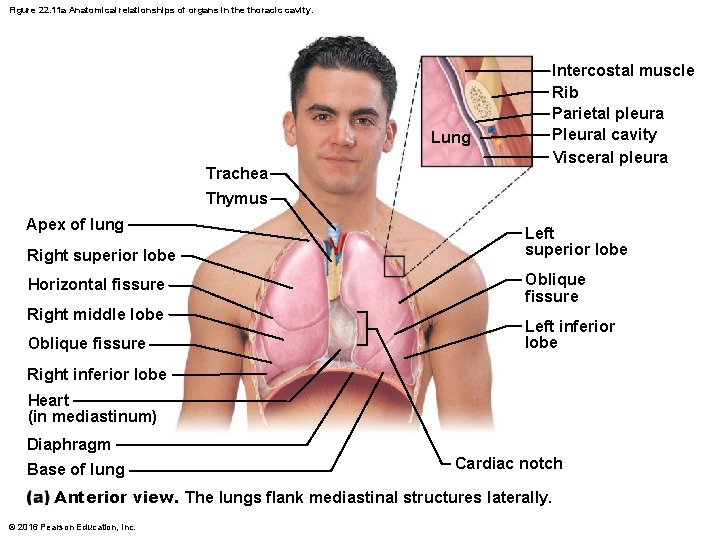
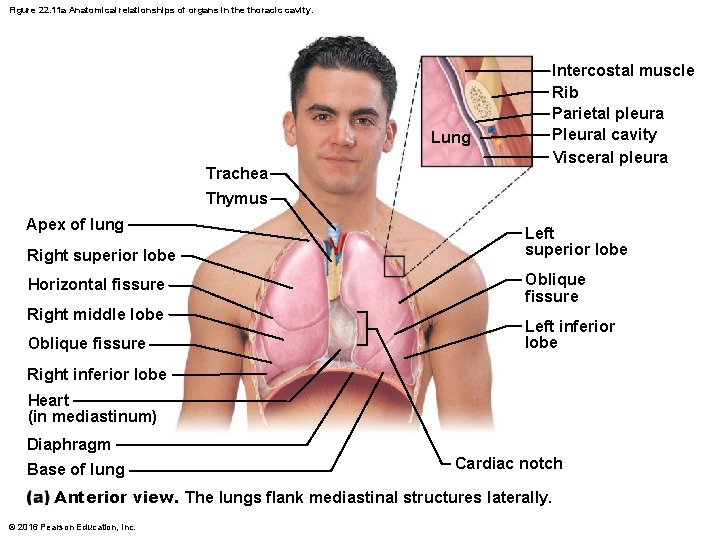
Figure 22. 11 a Anatomical relationships of organs in the thoracic cavity. Lung Trachea Thymus Apex of lung Right superior lobe Horizontal fissure Right middle lobe Oblique fissure Intercostal muscle Rib Parietal pleura Pleural cavity Visceral pleura Left superior lobe Oblique fissure Left inferior lobe Right inferior lobe Heart (in mediastinum) Diaphragm Base of lung Cardiac notch Anterior view. The lungs flank mediastinal structures laterally. © 2016 Pearson Education, Inc.
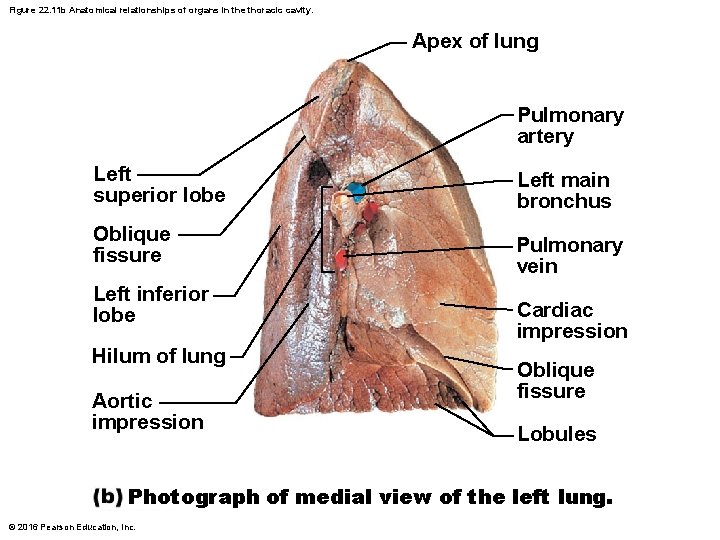
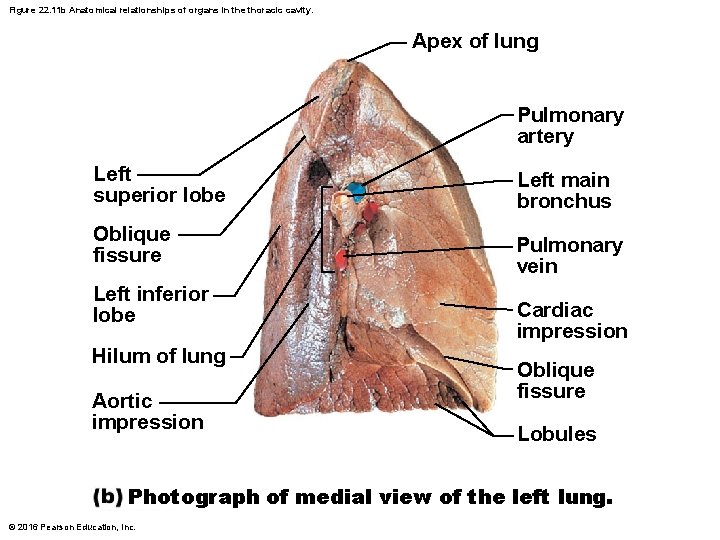
Figure 22. 11 b Anatomical relationships of organs in the thoracic cavity. Apex of lung Pulmonary artery Left superior lobe Oblique fissure Left inferior lobe Hilum of lung Aortic impression Left main bronchus Pulmonary vein Cardiac impression Oblique fissure Lobules Photograph of medial view of the left lung. © 2016 Pearson Education, Inc.
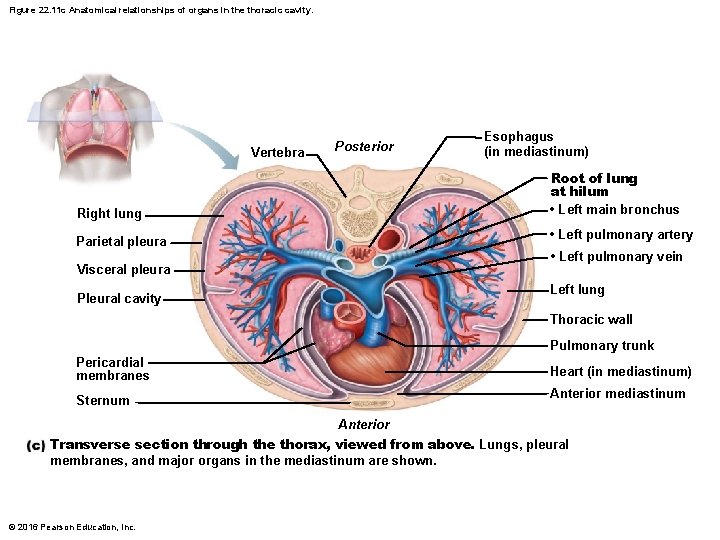
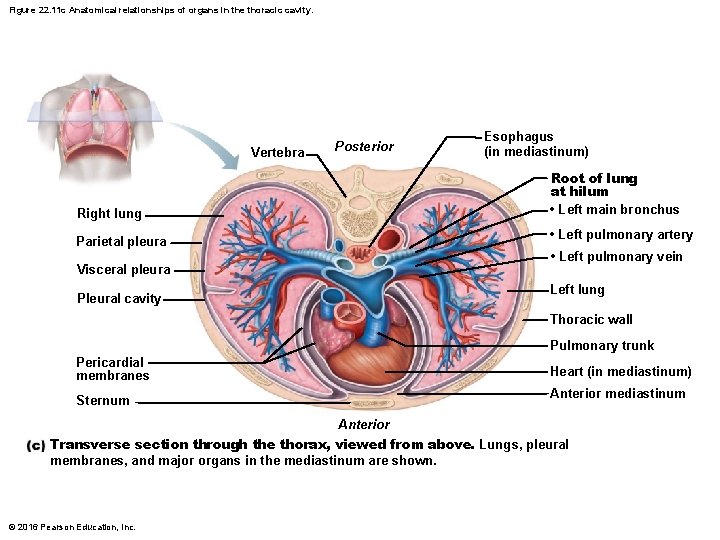
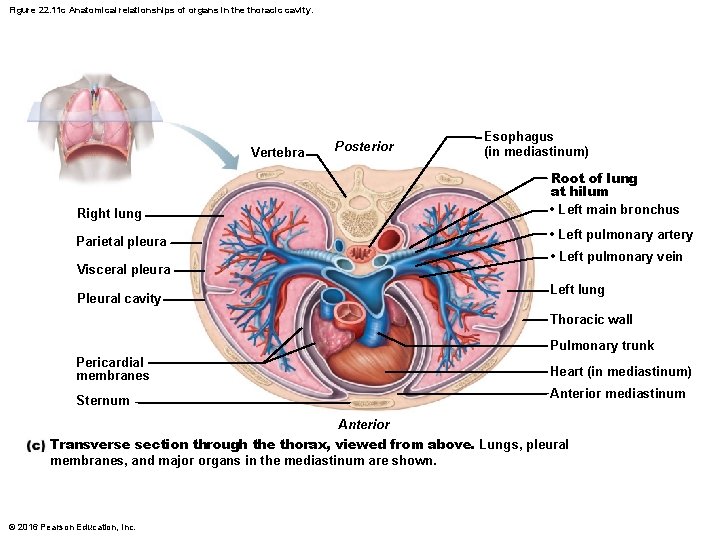
Figure 22. 11 c Anatomical relationships of organs in the thoracic cavity. Vertebra Posterior Esophagus (in mediastinum) Root of lung at hilum • Left main bronchus Right lung • Left pulmonary artery Parietal pleura • Left pulmonary vein Visceral pleura Left lung Pleural cavity Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Anterior mediastinum Sternum Anterior Transverse section through the thorax, viewed from above. Lungs, pleural membranes, and major organs in the mediastinum are shown. © 2016 Pearson Education, Inc.
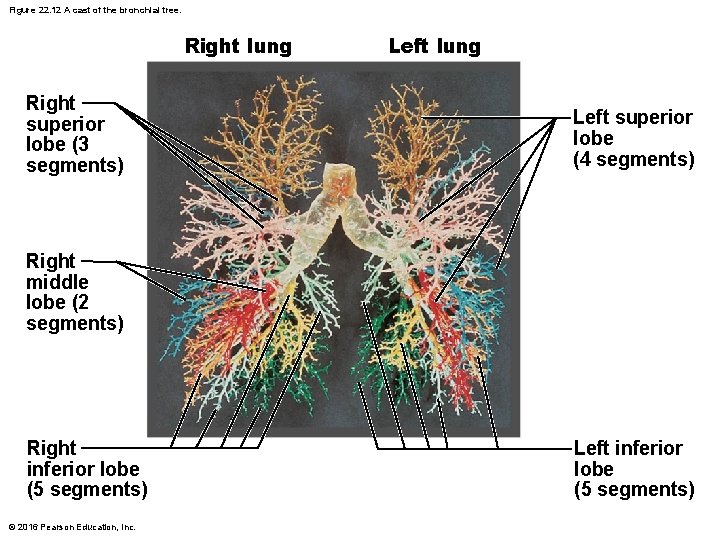
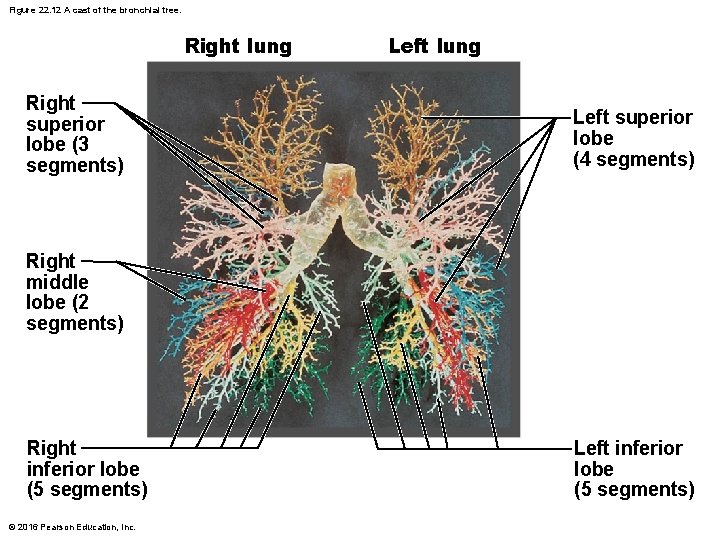
Figure 22. 12 A cast of the bronchial tree. Right lung Right superior lobe (3 segments) Left lung Left superior lobe (4 segments) Right middle lobe (2 segments) Right inferior lobe (5 segments) © 2016 Pearson Education, Inc. Left inferior lobe (5 segments)
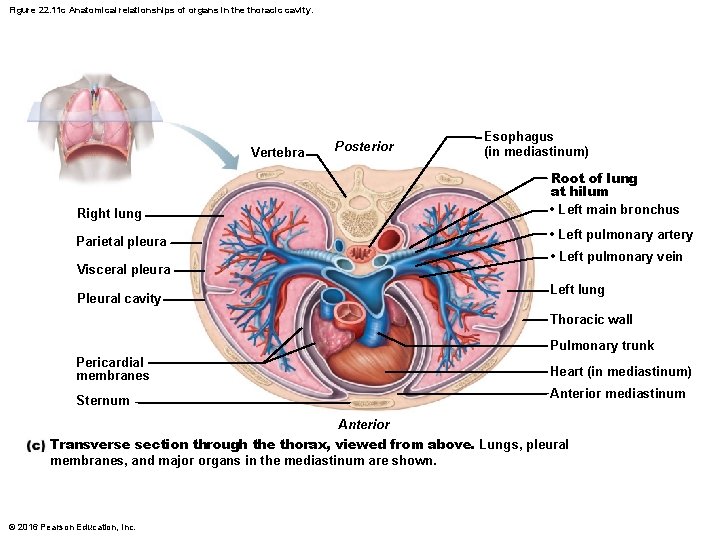
Figure 22. 11 c Anatomical relationships of organs in the thoracic cavity. Vertebra Posterior Esophagus (in mediastinum) Root of lung at hilum • Left main bronchus Right lung • Left pulmonary artery Parietal pleura • Left pulmonary vein Visceral pleura Left lung Pleural cavity Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Anterior mediastinum Sternum Anterior Transverse section through the thorax, viewed from above. Lungs, pleural membranes, and major organs in the mediastinum are shown. © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 6 • Pleurisy: inflammation of pleurae that often results from pneumonia • Inflamed pleurae become rough, resulting in friction and stabbing pain with each breath • Pleurae may produce excessive amounts of fluid, which may exert pressure on lungs, hindering breathing © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 6 • Other fluids that may accumulate in pleural cavity – Blood: leaked from damaged blood vessels – Blood filtrate: watery fluid that oozes from lung capillaries when left-sided heart failure occurs • Pleural effusion: fluid accumulation in pleural cavity © 2016 Pearson Education, Inc.
Chapter 22 Part A The Respiratory System © Annie Leibovitz/Contact Press Images © 2016 Pearson Education, Inc. Power. Point® Lecture Slides prepared by Karen Dunbar Kareiva Ivy Tech Community College
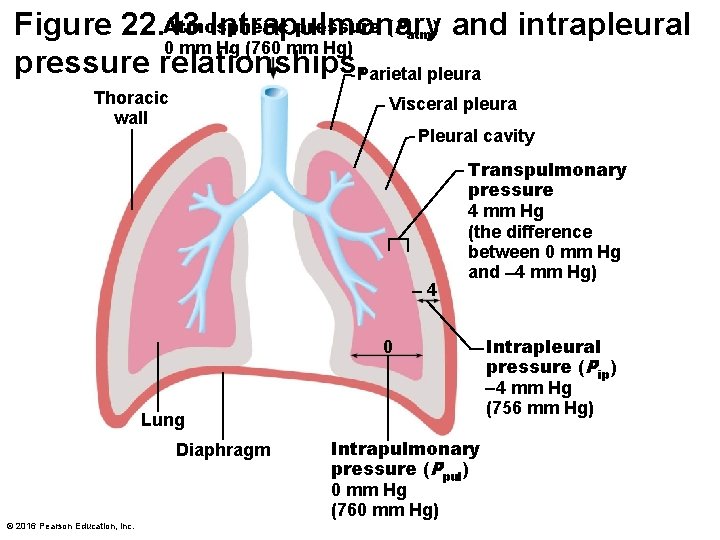
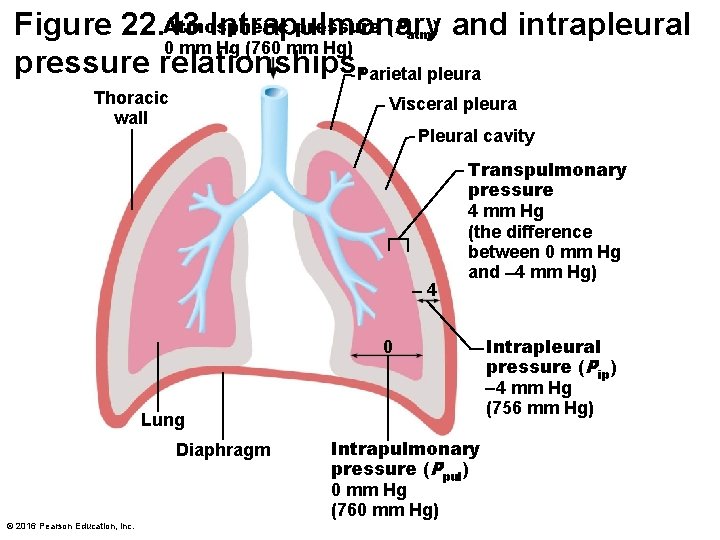
Atmospheric pressure (P ) and intrapleural Figure 22. 13 Intrapulmonary 0 mm Hg (760 mm Hg) pressure relationships. Parietal pleura atm Thoracic wall Visceral pleura Pleural cavity 4 Transpulmonary pressure 4 mm Hg (the difference between 0 mm Hg and 4 mm Hg) 0 Lung Diaphragm © 2016 Pearson Education, Inc. Intrapulmonary pressure (Ppul) 0 mm Hg (760 mm Hg) Intrapleural pressure (Pip) 4 mm Hg (756 mm Hg)
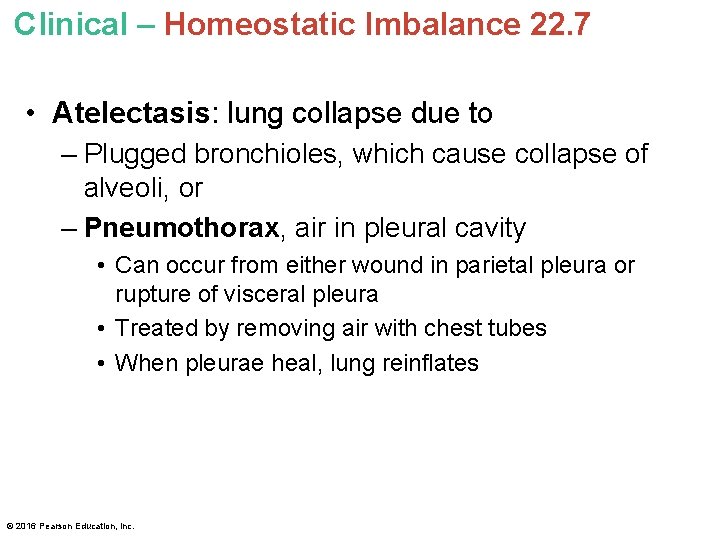
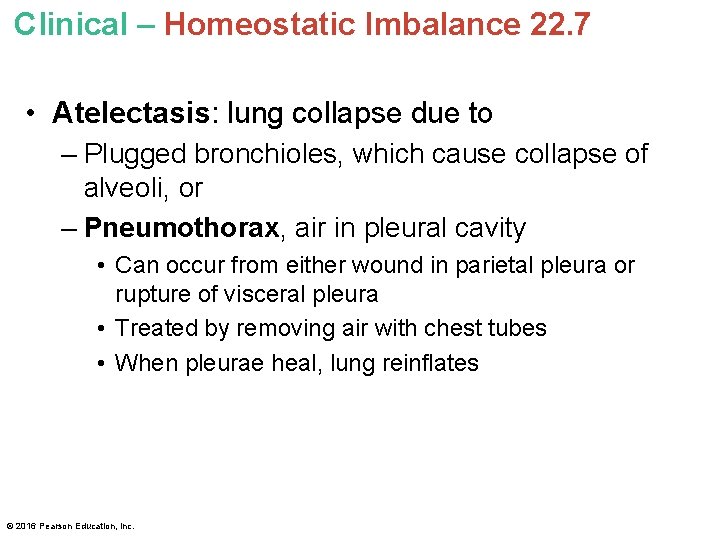
Clinical – Homeostatic Imbalance 22. 7 • Atelectasis: lung collapse due to – Plugged bronchioles, which cause collapse of alveoli, or – Pneumothorax, air in pleural cavity • Can occur from either wound in parietal pleura or rupture of visceral pleura • Treated by removing air with chest tubes • When pleurae heal, lung reinflates © 2016 Pearson Education, Inc.
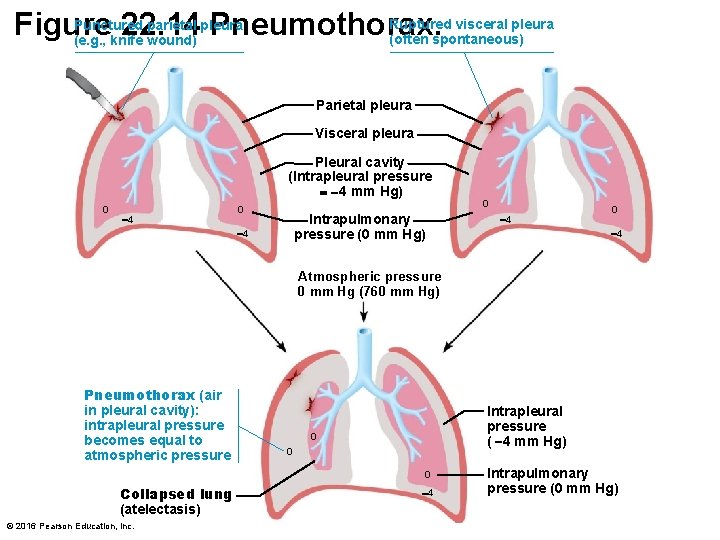
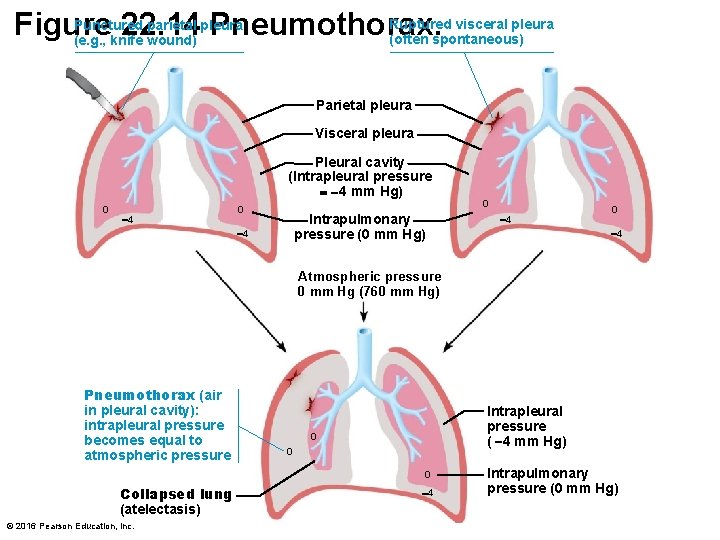
Ruptured visceral pleura Punctured parietal pleura Figure 22. 14 Pneumothorax. (often spontaneous) (e. g. , knife wound) Parietal pleura Visceral pleura Pleural cavity (Intrapleural pressure 4 mm Hg) 0 4 0 Intrapulmonary pressure (0 mm Hg) 4 0 4 Atmospheric pressure 0 mm Hg (760 mm Hg) Pneumothorax (air in pleural cavity): intrapleural pressure becomes equal to atmospheric pressure Intrapleural pressure ( 4 mm Hg) 0 0 0 Collapsed lung (atelectasis) © 2016 Pearson Education, Inc. 4 Intrapulmonary pressure (0 mm Hg)
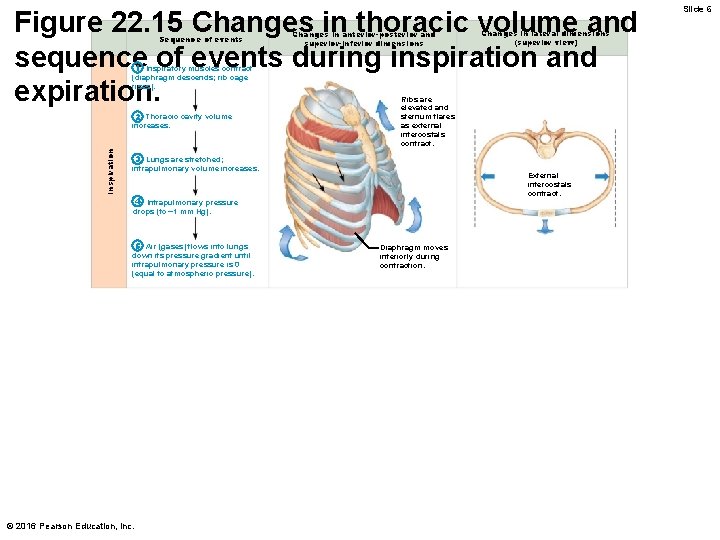
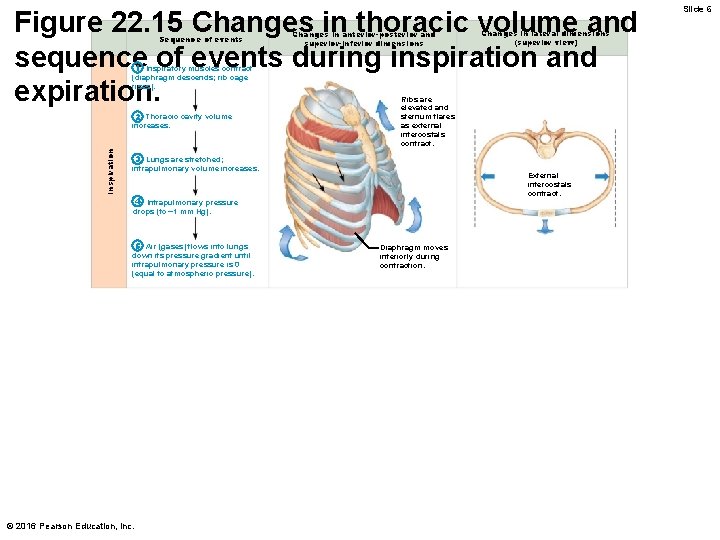
Figure 22. 15 Changes in thoracic volume and sequence of events during inspiration and expiration. Sequence of events Changes in anterior-posterior and superior-inferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles contract (diaphragm descends; rib cage rises). Inspiration 2 Thoracic cavity volume increases. Ribs are elevated and sternum flares as external intercostals contract. 3 Lungs are stretched; intrapulmonary volume increases. External intercostals contract. 4 Intrapulmonary pressure drops (to 1 mm Hg). 5 Air (gases) flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to atmospheric pressure). © 2016 Pearson Education, Inc. Diaphragm moves inferiorly during contraction. Slide 6
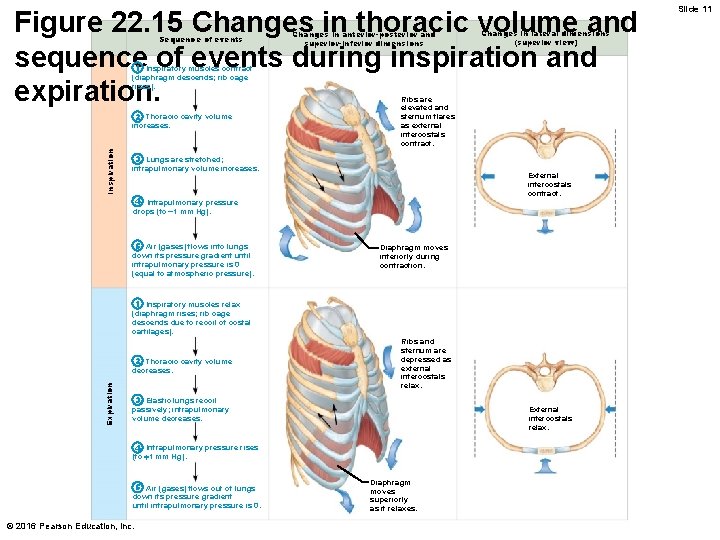
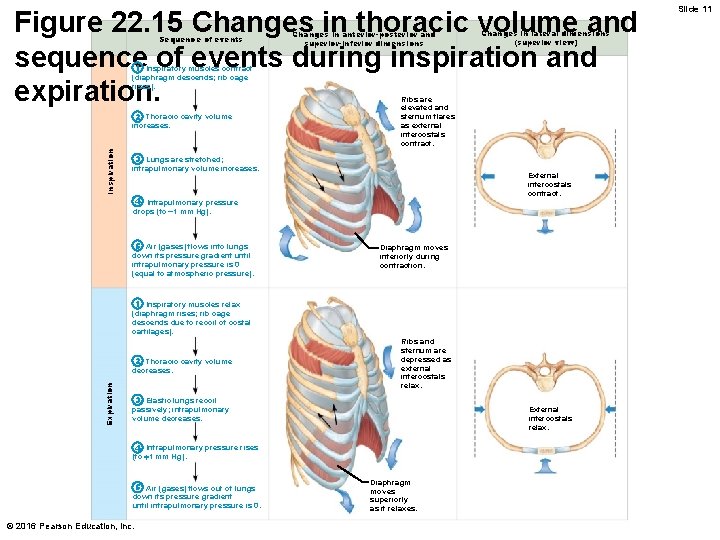
Figure 22. 15 Changes in thoracic volume and sequence of events during inspiration and expiration. Sequence of events Changes in anterior-posterior and superior-inferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles contract (diaphragm descends; rib cage rises). Inspiration 2 Thoracic cavity volume increases. Ribs are elevated and sternum flares as external intercostals contract. 3 Lungs are stretched; intrapulmonary volume increases. External intercostals contract. 4 Intrapulmonary pressure drops (to 1 mm Hg). 5 Air (gases) flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to atmospheric pressure). Diaphragm moves inferiorly during contraction. 1 Inspiratory muscles relax (diaphragm rises; rib cage descends due to recoil of costal cartilages). Expiration 2 Thoracic cavity volume decreases. Ribs and sternum are depressed as external intercostals relax. 3 Elastic lungs recoil passively; intrapulmonary volume decreases. External intercostals relax. 4 Intrapulmonary pressure rises (to 1 mm Hg). 5 Air (gases) flows out of lungs down its pressure gradient until intrapulmonary pressure is 0. © 2016 Pearson Education, Inc. Diaphragm moves superiorly as it relaxes. Slide 11
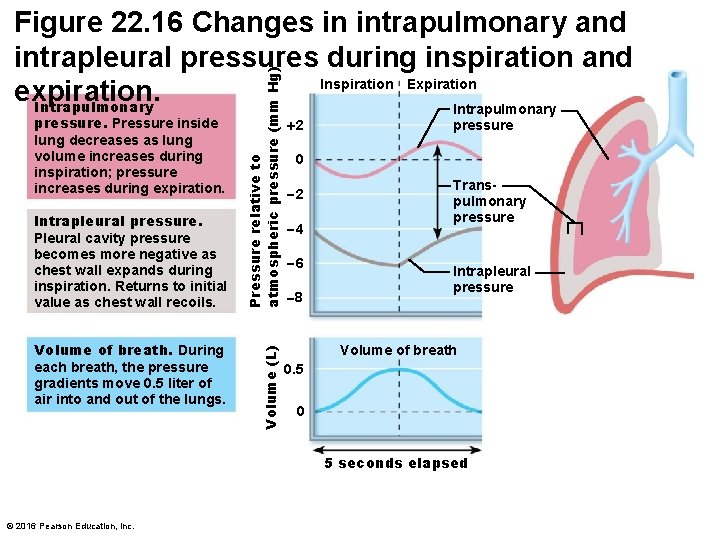
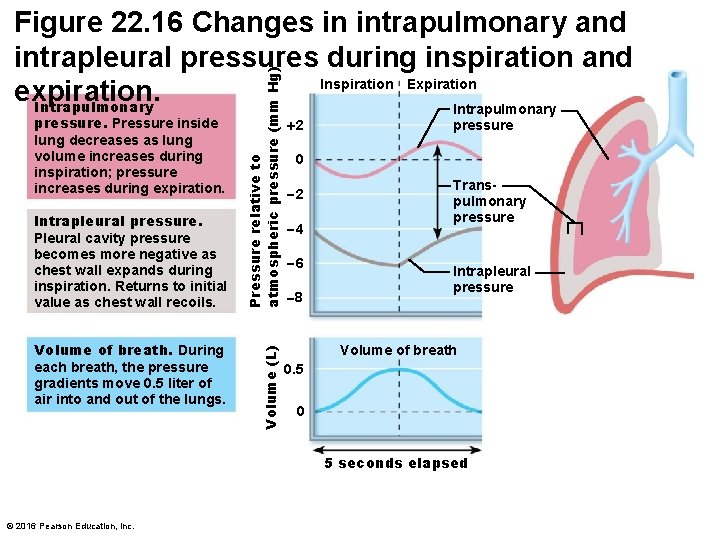
Intrapleural pressure. Pleural cavity pressure becomes more negative as chest wall expands during inspiration. Returns to initial value as chest wall recoils. Volume of breath. During each breath, the pressure gradients move 0. 5 liter of air into and out of the lungs. Volume (L) pressure. Pressure inside lung decreases as lung volume increases during inspiration; pressure increases during expiration. Pressure relative to atmospheric pressure (mm Hg) Figure 22. 16 Changes in intrapulmonary and intrapleural pressures during inspiration and Inspiration Expiration expiration. Intrapulmonary 2 pressure 0 2 4 6 8 Transpulmonary pressure Intrapleural pressure Volume of breath 0. 5 0 5 seconds elapsed © 2016 Pearson Education, Inc.
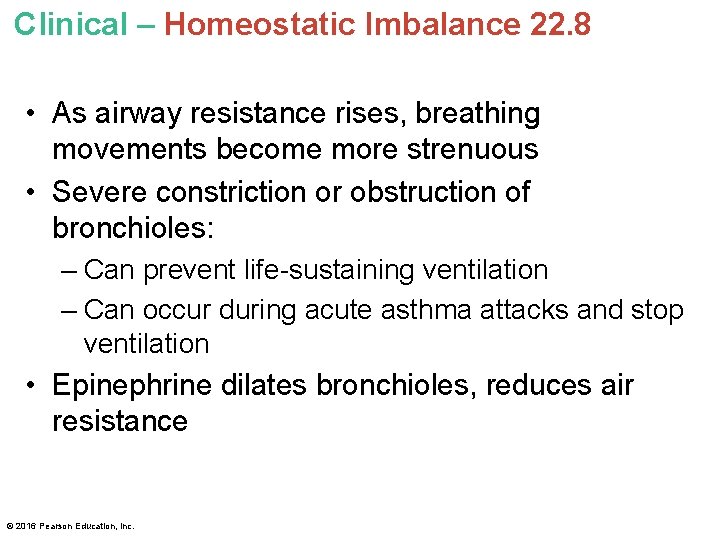
Clinical – Homeostatic Imbalance 22. 8 • As airway resistance rises, breathing movements become more strenuous • Severe constriction or obstruction of bronchioles: – Can prevent life-sustaining ventilation – Can occur during acute asthma attacks and stop ventilation • Epinephrine dilates bronchioles, reduces air resistance © 2016 Pearson Education, Inc.
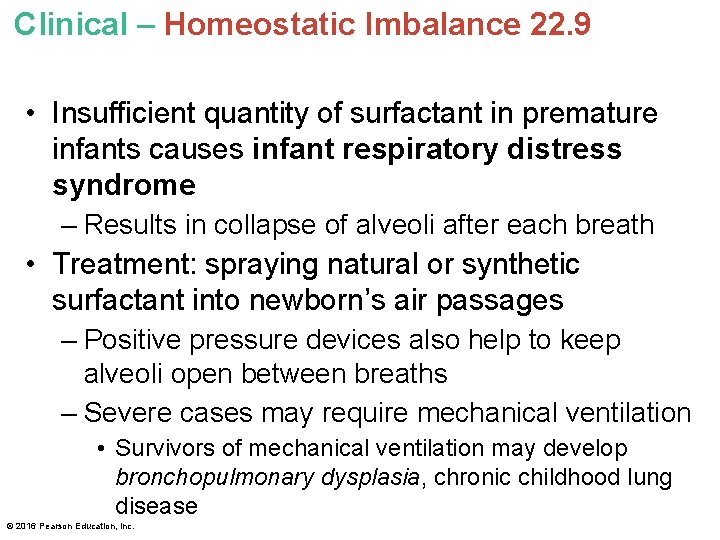
Clinical – Homeostatic Imbalance 22. 9 • Insufficient quantity of surfactant in premature infants causes infant respiratory distress syndrome – Results in collapse of alveoli after each breath • Treatment: spraying natural or synthetic surfactant into newborn’s air passages – Positive pressure devices also help to keep alveoli open between breaths – Severe cases may require mechanical ventilation • Survivors of mechanical ventilation may develop bronchopulmonary dysplasia, chronic childhood lung disease © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 10 • The total compliance of the respiratory system is also influenced by compliance (distensibility) of the thoracic wall, which is decreased by: – Deformities of thorax – Ossification of costal cartilage • Common in old age – Paralysis of intercostal muscles © 2016 Pearson Education, Inc.
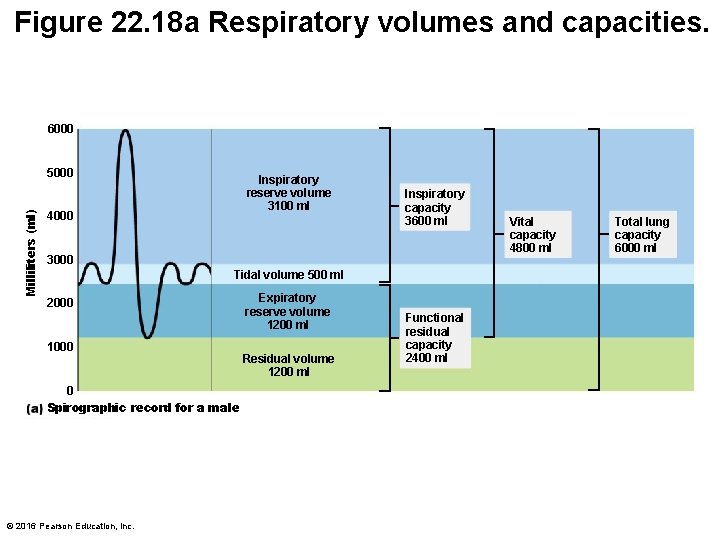
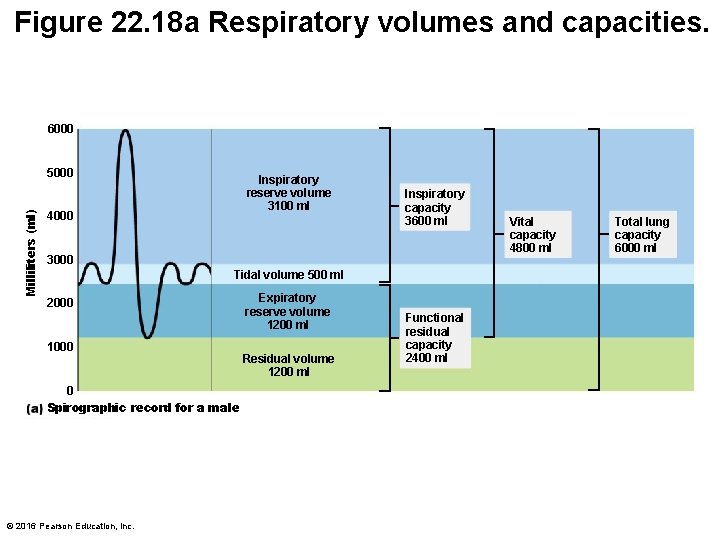
Figure 22. 18 a Respiratory volumes and capacities. 6000 Milliliters (ml) 5000 Inspiratory reserve volume 3100 ml 4000 Inspiratory capacity 3600 ml 3000 Tidal volume 500 ml 2000 1000 0 Spirographic record for a male © 2016 Pearson Education, Inc. Expiratory reserve volume 1200 ml Residual volume 1200 ml Functional residual capacity 2400 ml Vital capacity 4800 ml Total lung capacity 6000 ml
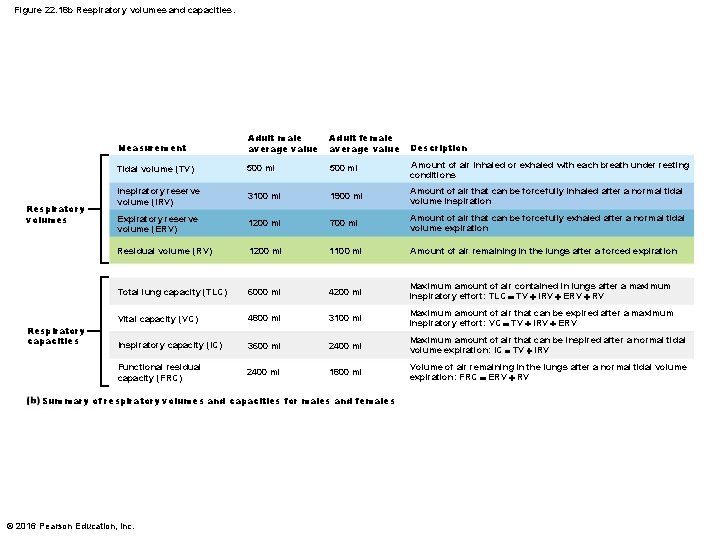
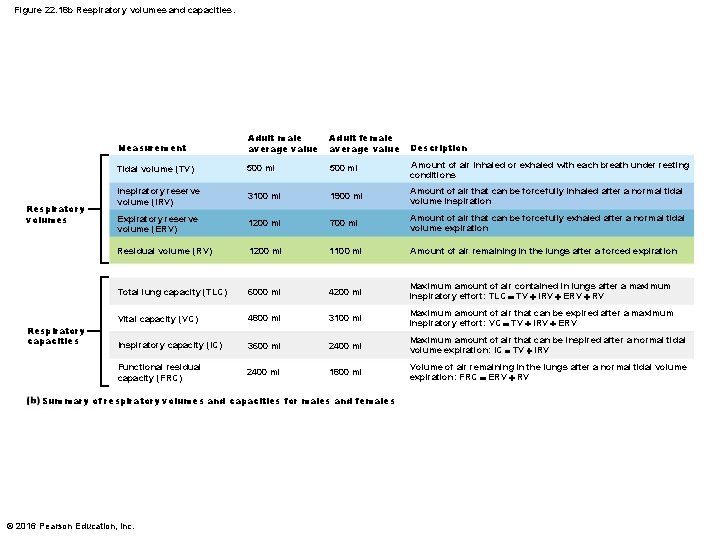
Figure 22. 18 b Respiratory volumes and capacities. Respiratory volumes Respiratory capacities Measurement Adult male average value Adult female average value Tidal volume (TV) 500 ml Amount of air inhaled or exhaled with each breath under resting conditions Inspiratory reserve volume (IRV) 3100 ml 1900 ml Amount of air that can be forcefully inhaled after a normal tidal volume inspiration Expiratory reserve volume (ERV) 1200 ml 700 ml Amount of air that can be forcefully exhaled after a normal tidal volume expiration Residual volume (RV) 1200 ml 1100 ml Amount of air remaining in the lungs after a forced expiration Total lung capacity (TLC) 6000 ml 4200 ml Maximum amount of air contained in lungs after a maximum inspiratory effort: TLC TV IRV ERV RV Vital capacity (VC) 4800 ml 3100 ml Maximum amount of air that can be expired after a maximum inspiratory effort: VC TV IRV ERV Inspiratory capacity (IC) 3600 ml 2400 ml Maximum amount of air that can be inspired after a normal tidal volume expiration: IC TV IRV Functional residual capacity (FRC) 2400 ml 1800 ml Volume of air remaining in the lungs after a normal tidal volume expiration: FRC ERV RV Summary of respiratory volumes and capacities for males and females © 2016 Pearson Education, Inc. Description
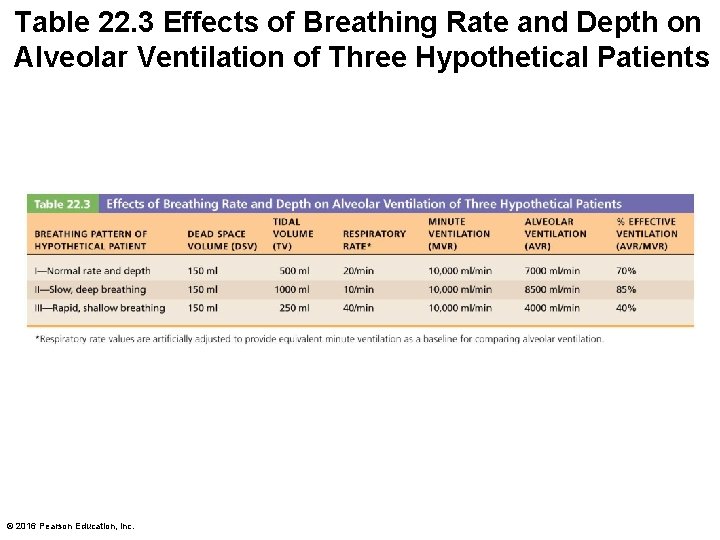
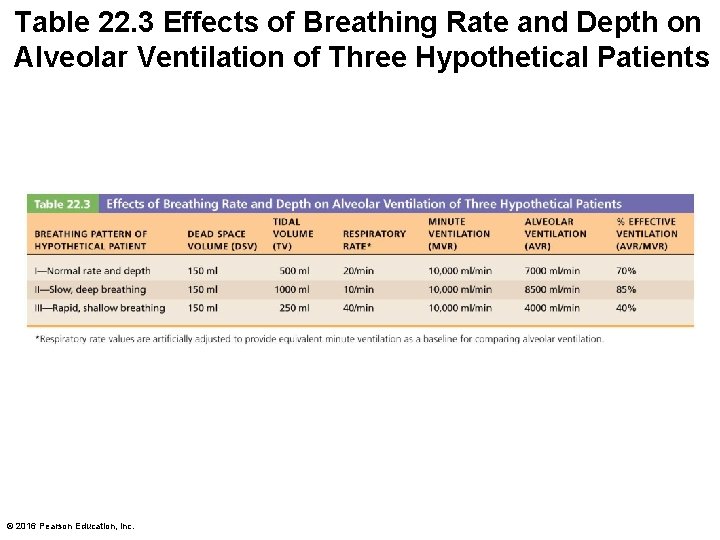
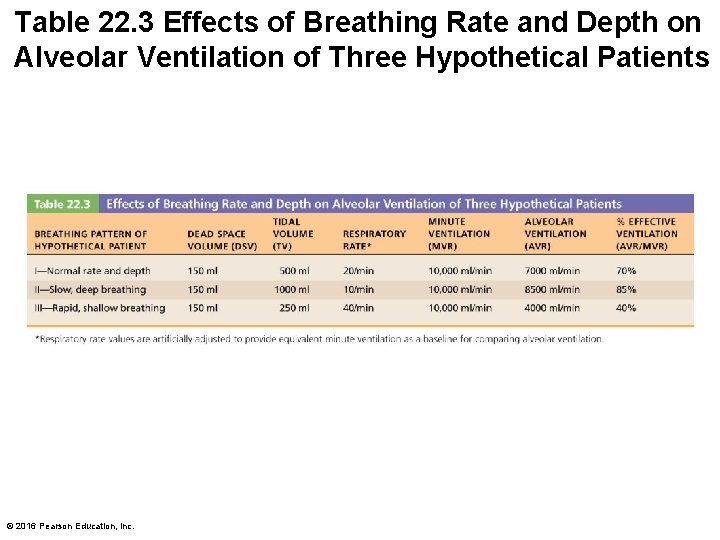
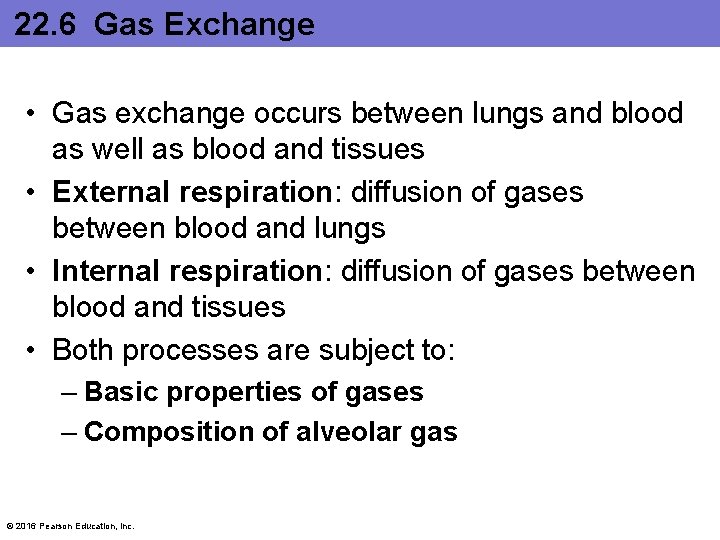
Table 22. 3 Effects of Breathing Rate and Depth on Alveolar Ventilation of Three Hypothetical Patients © 2016 Pearson Education, Inc.
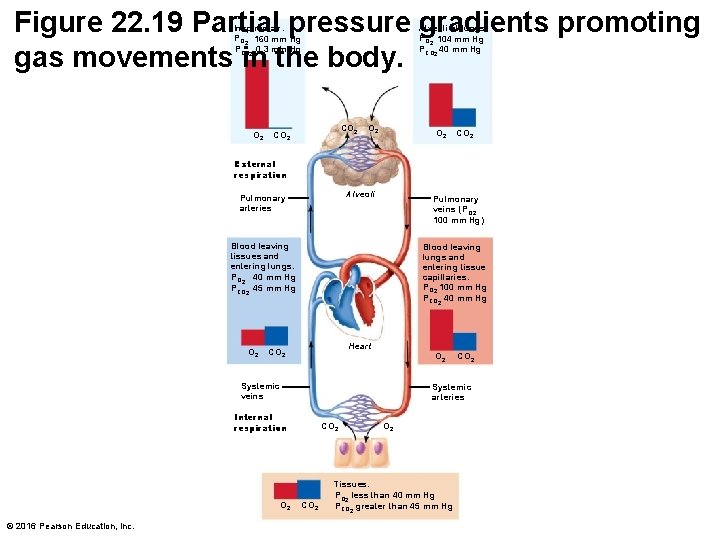
22. 6 Gas Exchange • Gas exchange occurs between lungs and blood as well as blood and tissues • External respiration: diffusion of gases between blood and lungs • Internal respiration: diffusion of gases between blood and tissues • Both processes are subject to: – Basic properties of gases – Composition of alveolar gas © 2016 Pearson Education, Inc.
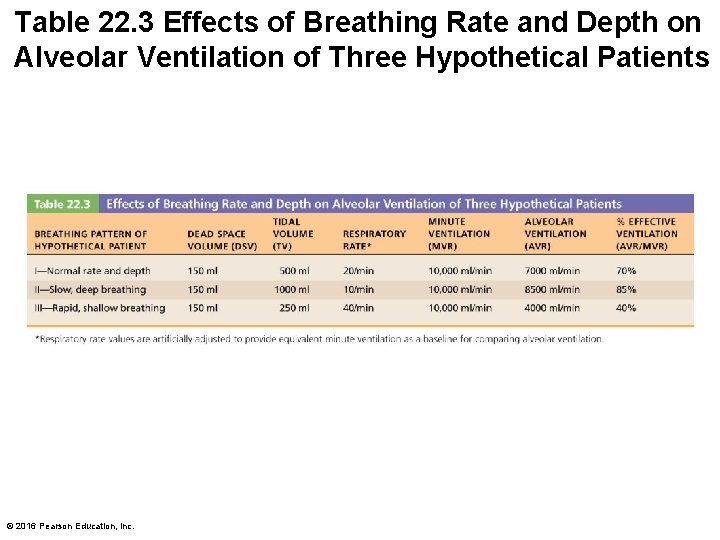
Table 22. 3 Effects of Breathing Rate and Depth on Alveolar Ventilation of Three Hypothetical Patients © 2016 Pearson Education, Inc.
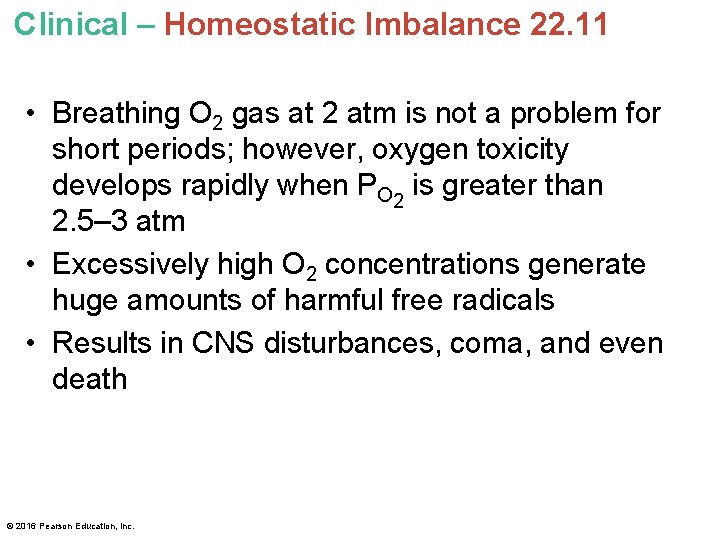
Clinical – Homeostatic Imbalance 22. 11 • Breathing O 2 gas at 2 atm is not a problem for short periods; however, oxygen toxicity develops rapidly when PO 2 is greater than 2. 5– 3 atm • Excessively high O 2 concentrations generate huge amounts of harmful free radicals • Results in CNS disturbances, coma, and even death © 2016 Pearson Education, Inc.
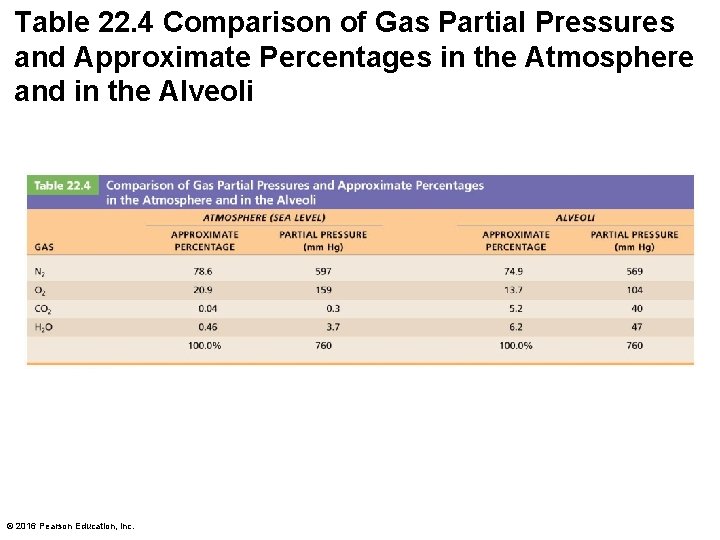
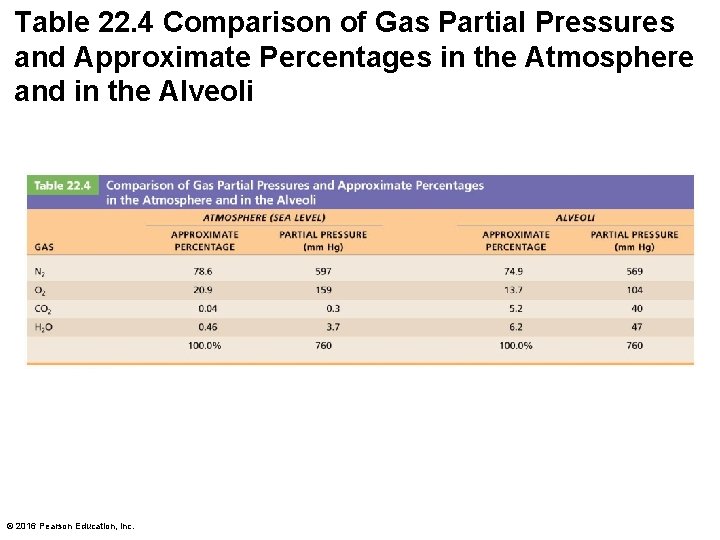
Table 22. 4 Comparison of Gas Partial Pressures and Approximate Percentages in the Atmosphere and in the Alveoli © 2016 Pearson Education, Inc.
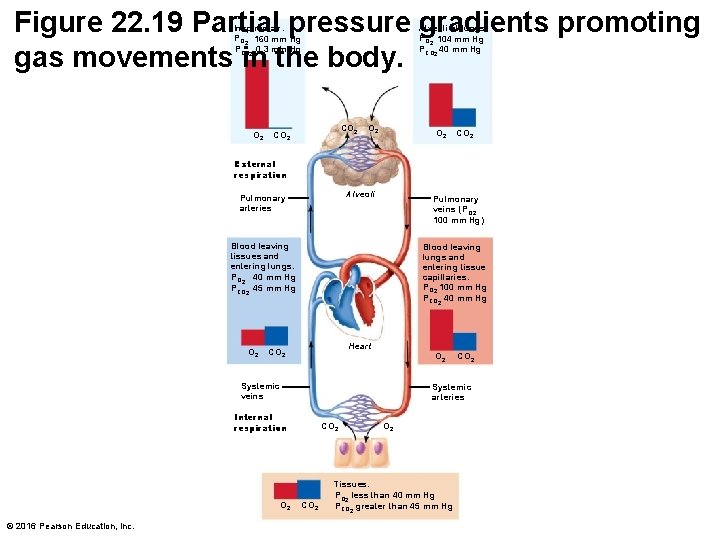
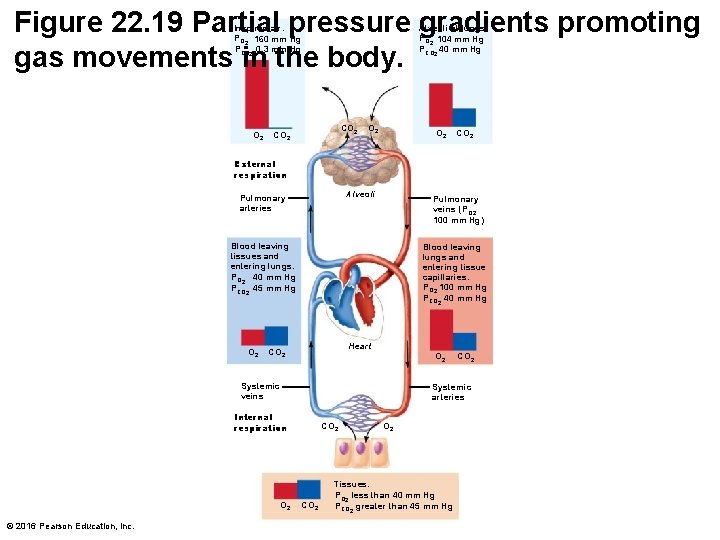
Figure 22. 19 Partial pressure gradients promoting gas movements in the body. Inspired air: PO 2 160 mm Hg PCO 2 0. 3 mm Hg O 2 Alveoli of lungs: PO 2 104 mm Hg PCO 2 40 mm Hg CO 2 O 2 CO 2 External respiration Alveoli Pulmonary arteries Pulmonary veins (P O 2 100 mm Hg) Blood leaving tissues and entering lungs: PO 2 40 mm Hg PCO 2 45 mm Hg O 2 Blood leaving lungs and entering tissue capillaries: PO 2 100 mm Hg PCO 2 40 mm Hg Heart CO 2 Systemic veins Systemic arteries Internal respiration O 2 © 2016 Pearson Education, Inc. CO 2 Tissues: PO 2 less than 40 mm Hg PCO 2 greater than 45 mm Hg
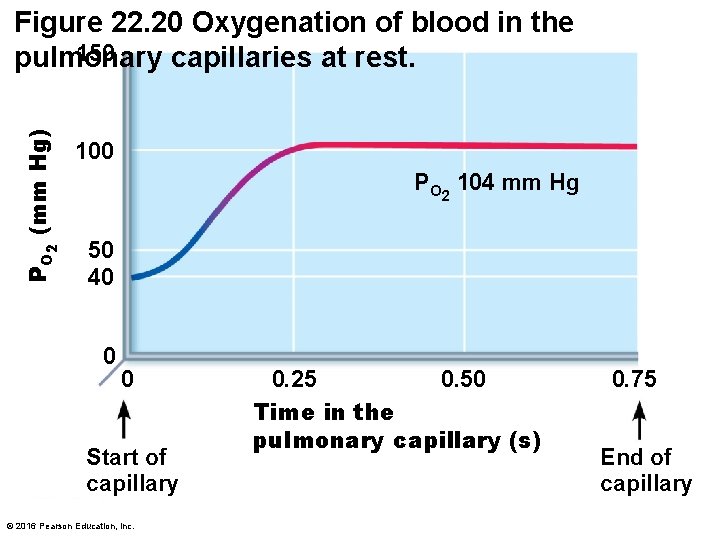
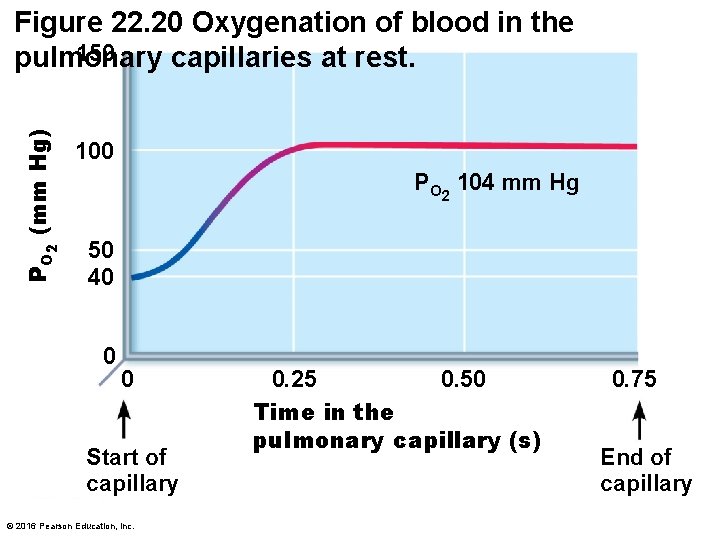
PO 2 (mm Hg) Figure 22. 20 Oxygenation of blood in the 150 pulmonary capillaries at rest. 100 PO 2 104 mm Hg 50 40 0 0 Start of capillary © 2016 Pearson Education, Inc. 0. 25 0. 50 Time in the pulmonary capillary (s) 0. 75 End of capillary
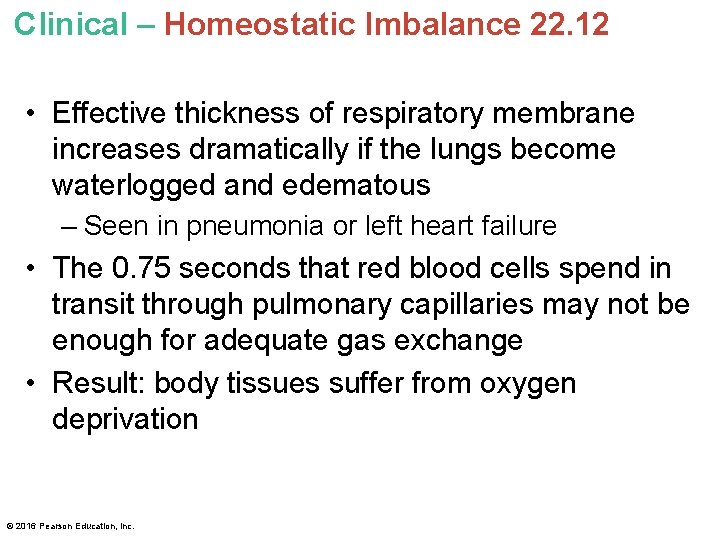
Clinical – Homeostatic Imbalance 22. 12 • Effective thickness of respiratory membrane increases dramatically if the lungs become waterlogged and edematous – Seen in pneumonia or left heart failure • The 0. 75 seconds that red blood cells spend in transit through pulmonary capillaries may not be enough for adequate gas exchange • Result: body tissues suffer from oxygen deprivation © 2016 Pearson Education, Inc.
Clinical – Homeostatic Imbalance 22. 13 • Certain pulmonary diseases drastically reduce alveolar surface area • Example: in emphysema, walls of adjacent alveoli break down, and alveolar chambers enlarge • Tumors, mucus, or inflammatory material also can reduce surface area by blocking gas flow into alveoli © 2016 Pearson Education, Inc.
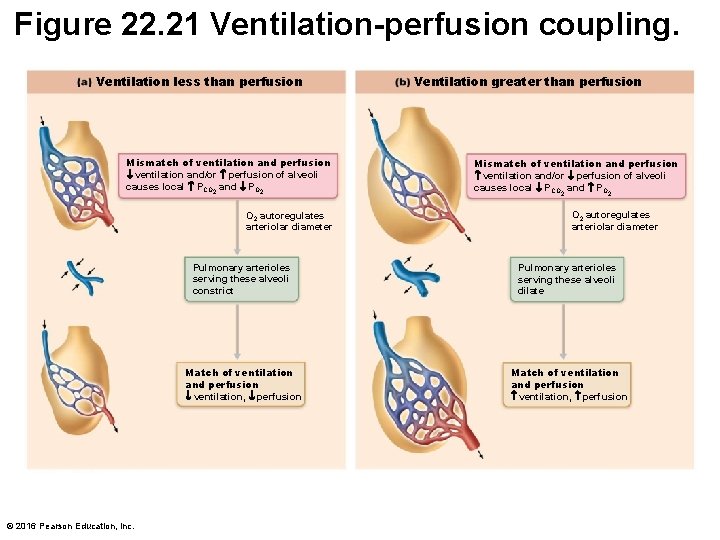
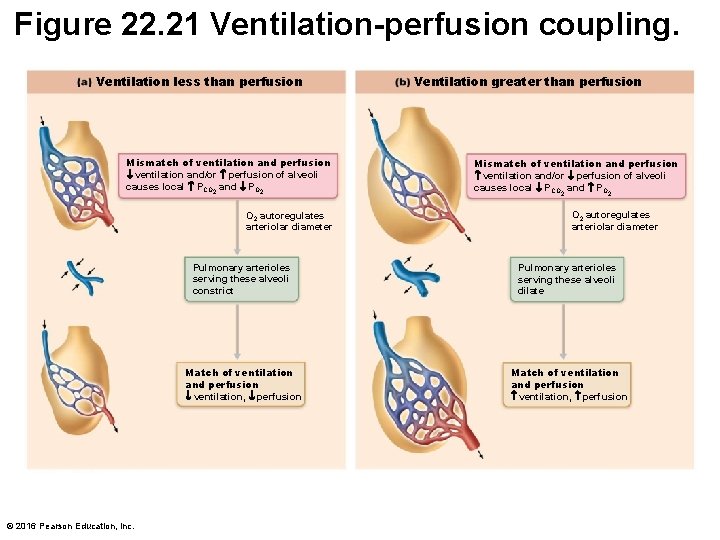
Figure 22. 21 Ventilation-perfusion coupling. Ventilation less than perfusion Mismatch of ventilation and perfusion ventilation and/or perfusion of alveoli causes local PCO 2 and PO 2 autoregulates arteriolar diameter © 2016 Pearson Education, Inc. Ventilation greater than perfusion Mismatch of ventilation and perfusion ventilation and/or perfusion of alveoli causes local PCO 2 and PO 2 autoregulates arteriolar diameter Pulmonary arterioles serving these alveoli constrict Pulmonary arterioles serving these alveoli dilate Match of ventilation and perfusion ventilation, perfusion
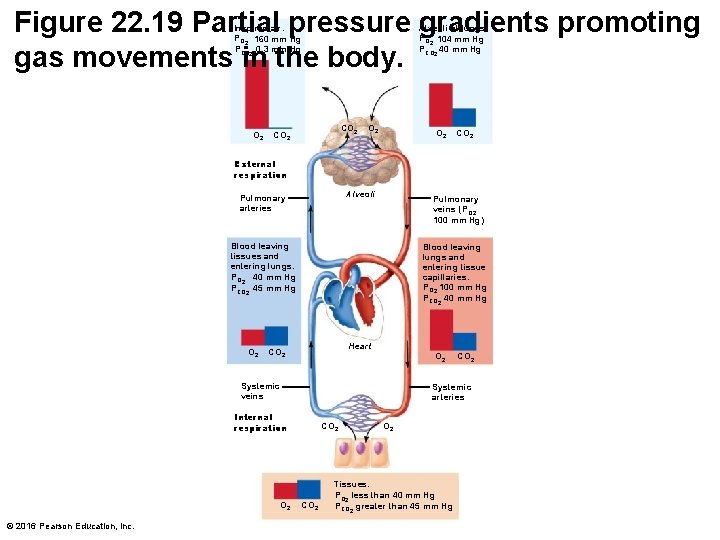
Figure 22. 19 Partial pressure gradients promoting gas movements in the body. Inspired air: PO 2 160 mm Hg PCO 2 0. 3 mm Hg O 2 Alveoli of lungs: PO 2 104 mm Hg PCO 2 40 mm Hg CO 2 O 2 CO 2 External respiration Alveoli Pulmonary arteries Pulmonary veins (P O 2 100 mm Hg) Blood leaving tissues and entering lungs: PO 2 40 mm Hg PCO 2 45 mm Hg O 2 Blood leaving lungs and entering tissue capillaries: PO 2 100 mm Hg PCO 2 40 mm Hg Heart CO 2 Systemic veins Systemic arteries Internal respiration O 2 © 2016 Pearson Education, Inc. CO 2 Tissues: PO 2 less than 40 mm Hg PCO 2 greater than 45 mm Hg