Chapter 22 Gynecologic Emergencies National EMS Education Standard
- Slides: 127
Chapter 22 Gynecologic Emergencies
National EMS Education Standard Competencies Medicine Integrates assessment findings with principles of epidemiology and pathophysiology to formulate a field impression and implement a comprehensive treatment disposition plan for a patient with a medical complaint.
National EMS Education Standard Competencies Gynecology Recognition and management of shock associated with − Vaginal bleeding Anatomy, physiology, assessment findings, and management of − Vaginal bleeding − Sexual assault − Infections
National EMS Education Standard Competencies Anatomy, physiology, epidemiology, pathophysiology, psychosocial impact, presentations, prognosis, and management of common or major gynecologic diseases and/or emergencies − − Vaginal bleeding Sexual assault Infections Pelvic inflammatory disease
National EMS Education Standard Competencies Anatomy, physiology, epidemiology, pathophysiology, psychosocial impact, presentations, prognosis, and management of common or major gynecologic diseases and/or emergencies (cont’d) − Ovarian cysts − Dysfunctional uterine bleeding − Vaginal foreign body
Introduction • Gynecology − Deals with diseases and routine care of female reproductive system • Obstetrics − Deals with birth • These branches of medicine are entwined.
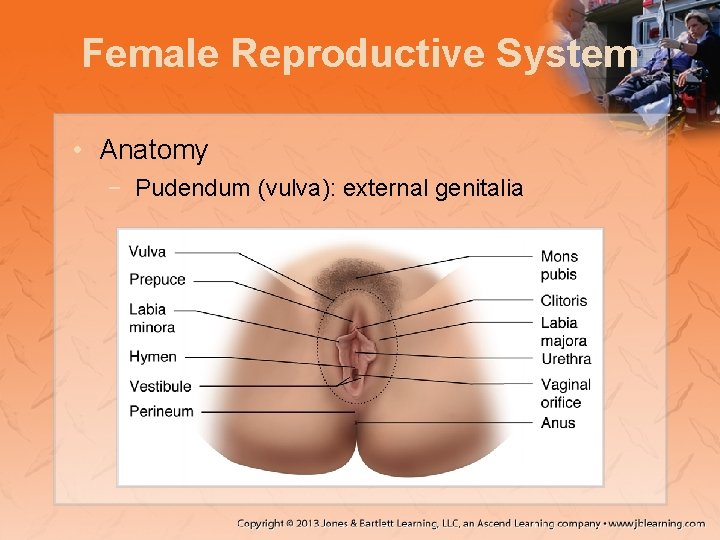
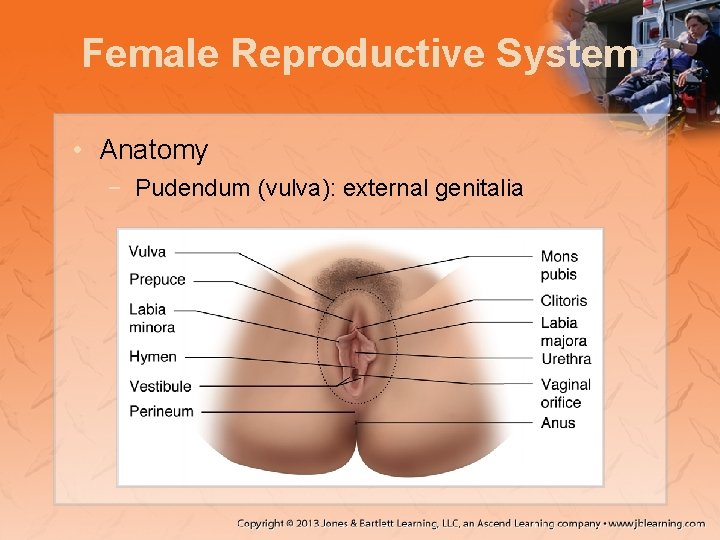
Female Reproductive System • Anatomy − Pudendum (vulva): external genitalia
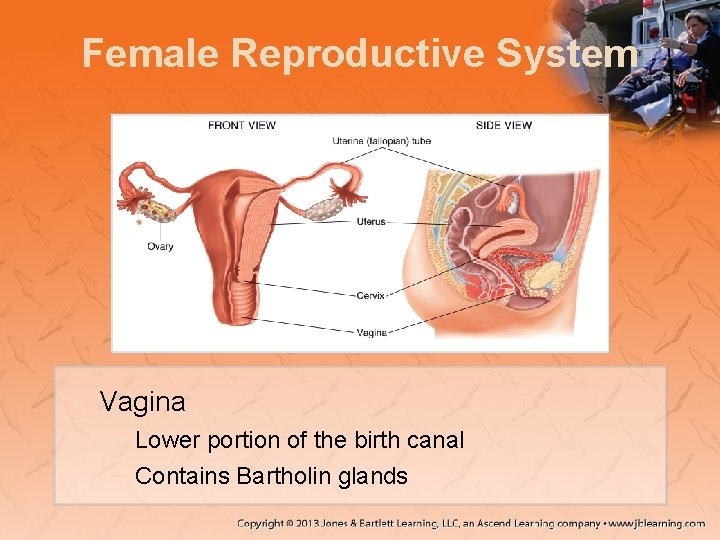
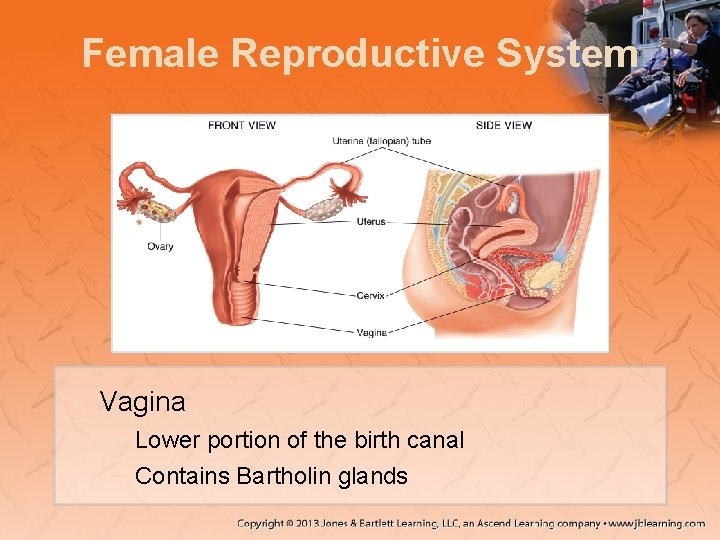
Female Reproductive System • Vagina − Lower portion of the birth canal − Contains Bartholin glands
Female Reproductive System • Hymen − Protects vaginal orifice − May break before first intercourse − When hymen breaks, pain and vaginal bleeding may occur
Female Reproductive System • Imperforate hymen − Hymen completely covers the vaginal orifice − May lead to complications such as: • Blockage of menses • Endometriosis − Can also be caused by sexual abuse
Female Reproductive System • Ovaries − Two glands − Each ovary contains thousands of follicles. • Normally one fallopian tube associated with each ovary
Female Reproductive System • Uterus − Muscular organ where the embryo grows • The birth canal consists of the: − Cervix − Vagina
Menstruation • Menstruation − Cyclic and periodic discharge of 25 to 65 m. L of blood, epithelial cells, mucus, and tissue − Duration varies − The menstrual cycle is composed of phases.
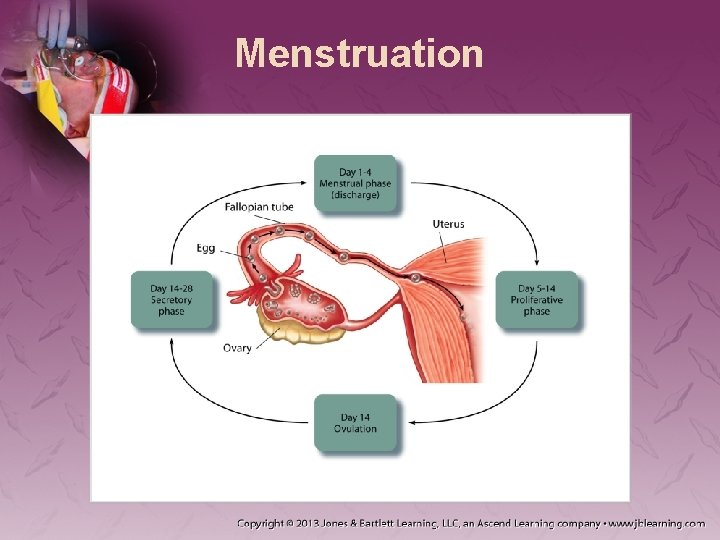
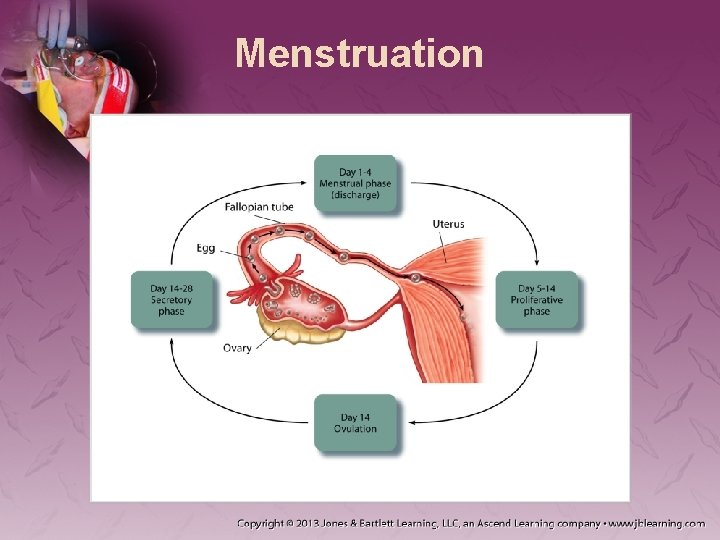
Menstruation • Ovarian cycle − Follicular phase • Days 1 to 13 • First day of menstruation until ovulation − Luteal phase • Days 14 to 28 • Time from ovulation until first day of menstruation
Menstruation • Uterine cycle − Proliferative phase • Days 5 to 14 • After menstruation to before the next ovulation − Secretory phase • Days 14 to 28 • Time after ovulation until menstruation
Menstruation
Menstruation • Women experience several changes during the menstrual cycle, including: − Weight gain due to extracellular edema − Hypertonicity − Emotional changes
Menstruation • Menarche − Onset of first menses • Menopause − Last menses − End of childbearing age • Menopause symptoms include: − − − Diaphoresis Hot flashes Dyspnea Vertigo Digestive problems
Menstruation • Due to decreased hormone production, postmenopausal women: − Are more susceptible to diseases like osteoporosis − Experience atrophy of genitourinary organs
Menstruation • PMS − Cluster of symptoms that occur during the menstrual cycle − Normally 7 to 14 days prior to menstrual flow
Menstruation • PMS (cont’d) − Symptoms may be exacerbated by many factors. − Some women may experience hypoglycemia. − Prehospital treatment is mainly supportive.
Menstruation • Mittelschmerz − Abdominal pain and cramping − May start any time during ovulation − Affects approximately 20 percent of women − Pain is usually not severe. • Amenorrhea − Absence of menses − Most common cause is pregnancy − Can also be due to: • Exercise • Drop of body fat • Stress • Anorexia nervosa
Patient Assessment • Obtaining an accurate and detailed patient assessment is very important. − Consider a gynecologic cause in a woman who complains of abdominal pain.
Scene Size-Up • Ask these questions: − − − − Is the scene safe? Is assistance necessary? What is the type of call? How many patients are there? Have standard precautions been taken? What is the MOI or NOI? Where is the patient found?
Primary Assessment • Ask these questions (cont’d): − − − − What is the overall presentation of the patient? Are there any obvious life threats? Is she conscious? Does she have breathing difficulty or injury? What is her appearance? What is her emotional state? In what position did you find her?
Primary Assessment • Protect the patient’s modesty. − Limit the crowd. • Form a general impression. − Assess consciousness.
Primary Assessment • Evaluate the airway and breathing. − Identify and treat life threats. • Assess circulation. − Palpate pulse. − Evaluate skin.
Primary Assessment • Transport decision − Rapid transport is warranted if signs of shock exist because of bleeding. • Perform the remainder of the assessment en route.
History Taking • Determine the patient’s chief complaint. − If excessive bleeding, obtain the gynecologic history. − If abdominal pain, find out more about the pain.
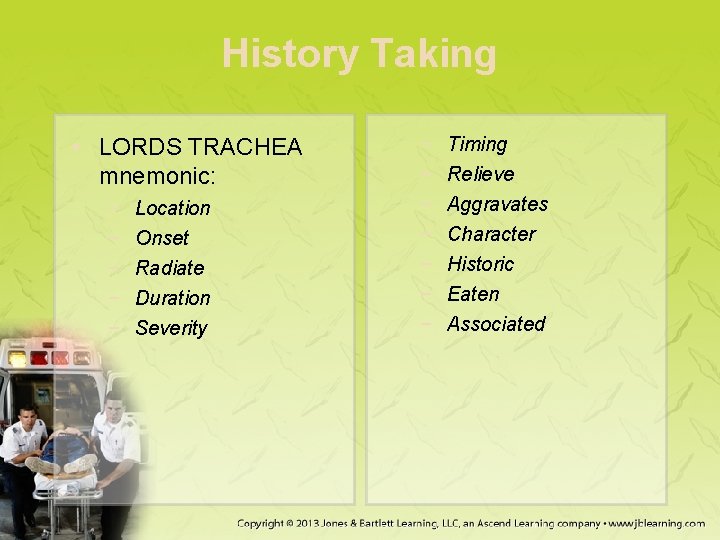
History Taking • LORDS TRACHEA mnemonic: − − − Location Onset Radiate Duration Severity − − − − Timing Relieve Aggravates Character Historic Eaten Associated
History Taking • Gynecologic history − − − LMP? Possibility of pregnancy? Contraception use? Spermicides, condoms, or a diaphragm? Implanted devise or an IUD?
History Taking • Gynecologic history (cont’d) − Vaginal bleeding? • If signs of shock are present, a fluid bolus of 100 to 200 m. L should improve the status. − Vaginal discharge? − STD?
History Taking • Determine obstetric history with G (gravida), P (para), and A (abortive history). − Gravida: number of times pregnant − Para: number of times delivering a newborn − Abortive history: number of elective abortions
History Taking • Additional questions: − − − How many times has she been pregnant? How many live births has she had? Any complications? Vaginal or cesarean deliveries? How much time between pregnancies?
History Taking • Additional questions (cont’d): − Any miscarriages or abortions? − Any gynecologic problems? − Any known medical conditions?
History Taking • Gynecologic emergencies often have the same signs and symptoms as other abdominal emergencies. − Use the SAMPLE mnemonic.
Secondary Assessment • Chief concern is to identify signs of shock − General presentation? − Condition of skin and mucous membranes?
Secondary Assessment • Examine the patient’s abdomen for: − − − Bruising Surgical scarring or stretch marks Needle tracks A positive Cullen sign or Grey-Turner sign A swollen and distended abdomen
Secondary Assessment • Examine the patient’s abdomen for (cont’d): − − − A flat and flaccid abdomen Guarding of the abdomen Rashes or lesions A symmetrical abdomen An enlarged liver or spleen
Secondary Assessment • Palpate the abdomen. − Start at the quadrant farthest from the pain. • • • Rigid abdomen? Point tenderness? Does the palpation elicit more pain? Rebound tenderness? Masses?
Secondary Assessment • Determine vital signs. − Pulse variations − Blood pressure − Orthostatic changes • General management is mostly supportive.
Reassessment • Recheck your interventions en route to the hospital. − Note improvement or decline. − Obtain serial vitals. • Complete paperwork after delivery.
Emergency Medical Care • Management is directed at: − Mitigating life threats − Being compassionate − Protecting the patient’s modesty
Management of Gynecologic Trauma • The female genital area is highly vascular. − Bleeding may be profuse. • Applying external pressure is usually sufficient. − Exsanguinating vaginal hemorrhage must be treated as any exsanguinating hemorrhage.
Management of Gynecologic Trauma • Assessment of trauma will focus on: − − Symptoms? Mechanism of injury? Is she using sanitary pads or tampons? Normal blood color?
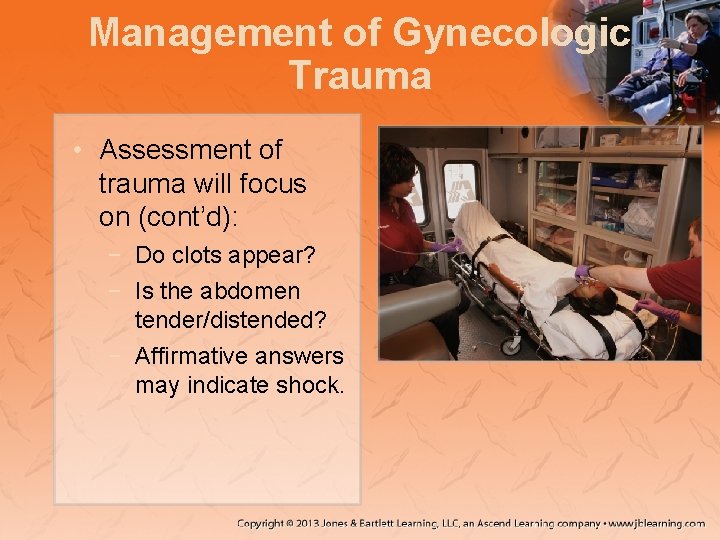
Management of Gynecologic Trauma • Assessment of trauma will focus on (cont’d): − Do clots appear? − Is the abdomen tender/distended? − Affirmative answers may indicate shock.
Specific Emergencies • Life-threatening gynecologic emergencies include: − Ectopic pregnancy − Ruptured ovarian cyst − Tubo-ovarian abscess
Vaginal Bleeding • Pathophysiology − Dysmenorrhea: painful menses • Primary dysmenorrhea occurs with the start of the menstrual flow, lasting 1 to 2 days. • Secondary dysmenorrhea is present before, during, and after the menstrual flow.
Vaginal Bleeding • Pathophysiology (cont’d) − Vaginal bleeding is one of the most frequent reasons that women consult a gynecologist. − Hypermenorrhea: flow lasts longer than normal or is excessive.
Vaginal Bleeding • Pathophysiology (cont’d) − Polymenorrhea: flow occurs more often than a 24 -day interval. − Metrorrhagia: flow or intermittent spotting occurring irregularly but frequently
Vaginal Bleeding • Assessment − Depends largely on mechanism of injury − Assess for hypovolemic shock. • Management − Prehospital treatment is largely supportive.
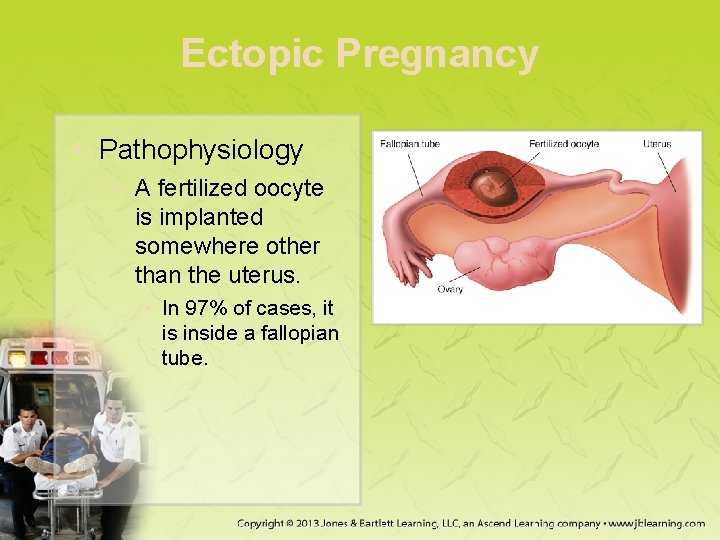
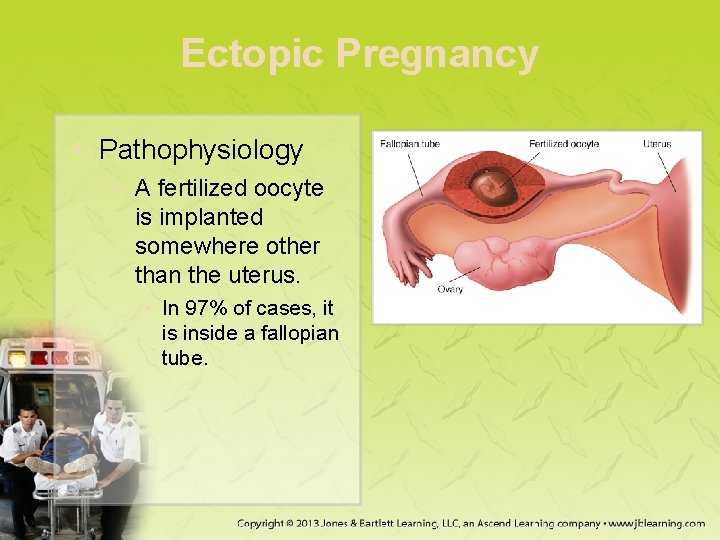
Ectopic Pregnancy • Pathophysiology − A fertilized oocyte is implanted somewhere other than the uterus. • In 97% of cases, it is inside a fallopian tube.
Ectopic Pregnancy • Pathophysiology (cont’d) − Tubal pregnancy • Fertilized oocyte implants in the fallopian tube. • Embryo runs out of room to grow. • The tube is likely to rupture.
Ectopic Pregnancy • Assessment − Chief complaint of abdominal pain • Generally localized to one side • Crampy and intermittent in early stages − Vaginal bleeding usually begins after pain.
Ectopic Pregnancy • Assessment (cont’d) − To gauge extent of internal bleeding, look for: • • A positive Cullen sign A positive Grey-Turner sign Signs of shock Abdominal distention and tenderness
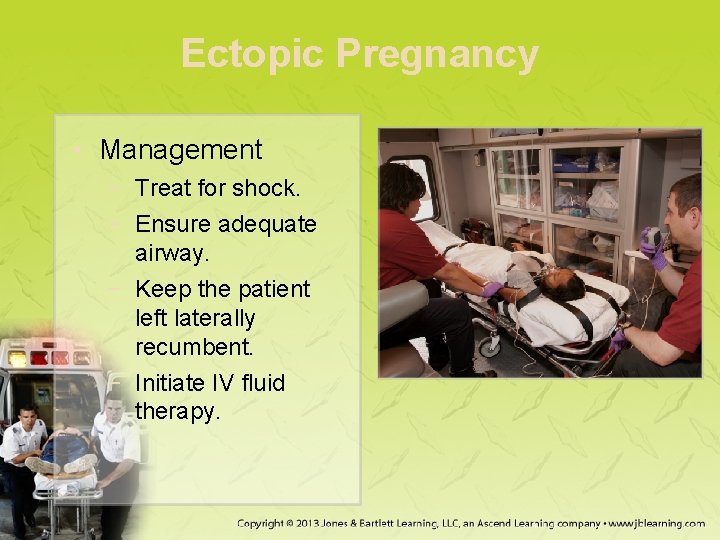
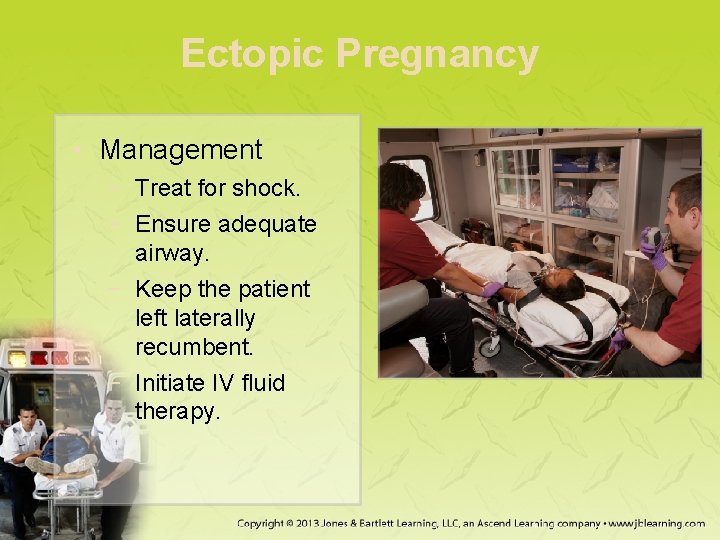
Ectopic Pregnancy • Management − Treat for shock. − Ensure adequate airway. − Keep the patient left laterally recumbent. − Initiate IV fluid therapy.
Ectopic Pregnancy • Management (cont’d) − − − Give nothing by mouth. Consider urethral catheterization. Anticipate vomiting. Keep the patient warm. Monitor the patient's ECG. Transport.
Endometritis • Pathophysiology − Inflammation or irritation of the endometrium • More likely after a baby or miscarriage • Most likely caused by an infection
Endometritis • Assessment − Symptoms may include: • • Malaise Vaginal bleeding or discharge Abdominal or pelvic pain Decreased bowel sounds
Endometritis • Management − Treat with antibiotics. − Provide reassurance. − Transport in a comfortable position.
Endometriosis • Pathophysiology − Endometrial tissue grows outside the uterus. • Organs of the pelvic cavity are the most common locations for growths. − One of the leading causes of infertility
Endometriosis • Assessment − Symptoms include: • • Pain Dysuria Very heavy menstrual periods Bleeding between periods
Endometriosis • Management − Prehospital care is based on signs/symptoms. − If the patient reports severe pain: • Provide pain relief. • Use dressing or towels as needed.
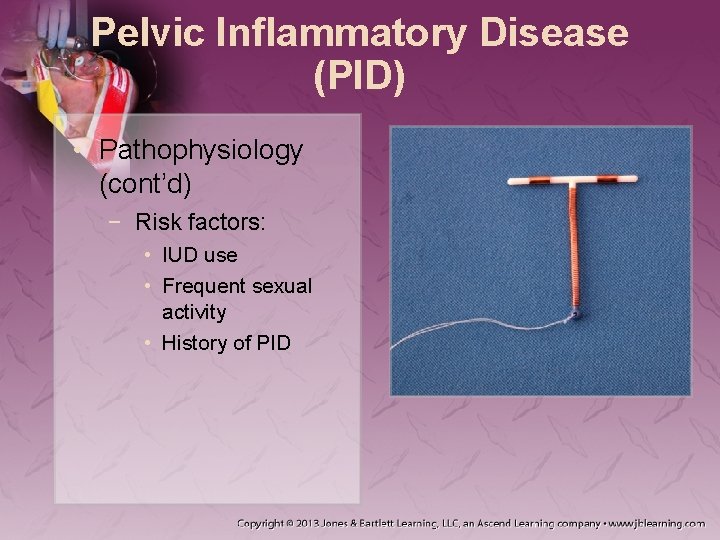
Pelvic Inflammatory Disease • Pathophysiology − Infection of the female upper organs − Affects sexually active women most often • Organisms enter the vagina and migrate into the uterine cavity.
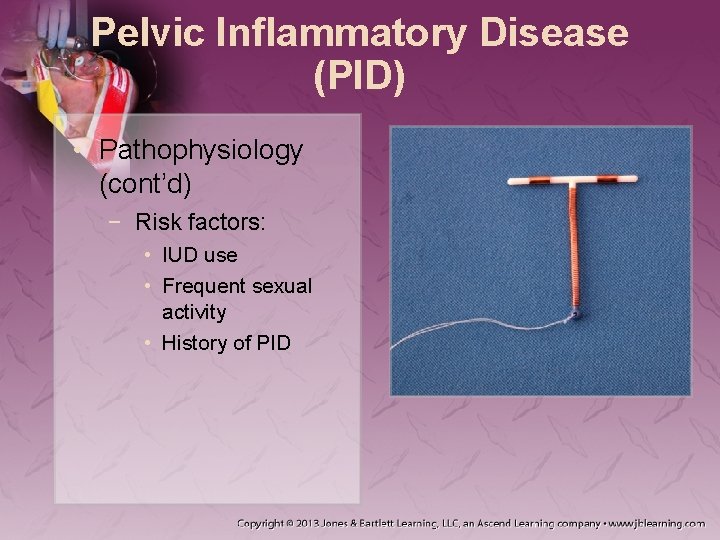
Pelvic Inflammatory Disease (PID) • Pathophysiology (cont’d) − Risk factors: • IUD use • Frequent sexual activity • History of PID
Pelvic Inflammatory Disease (PID) • Assessment − Abdominal pain will be present. • During or after normal menstruation • Typically diffuse − Be alert for signs of peritoneal irritation.
Pelvic Inflammatory Disease (PID) • Management − − Cannot be treated in the field Obtain a thorough history. Make the patient comfortable. Transport with a gentle ride.
Vaginitis • Pathophysiology − Inflammation of the vagina caused by infection − Vaginal yeast infections • Yeast population may increase if the vagina becomes less acidic.
Vaginitis • Pathophysiology (cont’d) − Vulvovaginitis: inflammation of the external vulva • Patients should be evaluated by a physician.
Vaginitis • Assessment − Symptoms of yeast infections: • Itching/burning • Soreness • Vulvar swelling • Thick, white vaginal discharge • Pain during intercourse − Symptoms of vulvovaginitis: • Redness • Pain • Swelling • Discharge • Burning • Itching
Vaginitis • Management − If not treated, vaginitis can lead to: • Infertility or preterm birth • Endometritis • PID − Antibiotics are required for definitive treatment.
Bartholin Abscess • Pathophysiology − Two small ducts just inside the lower vagina • Lead to the Bartholin glands • Bacterial infections may cause the openings to become abscessed and cystic.
Bartholin Abscess • Assessment − Patients may report: • Painful lump and/or irritation • Painful intercourse • Fever • Management − May need surgical removal
Gardnerella Vaginitis • Pathophysiology − Caused by too many Gardnerella bacterium in the genital area • Mainly affects young, sexually active women • Recent use of antibiotics can increase risk. • Can cause complications in pregnant women
Gardnerella Vaginitis • Assessment − Signs and symptoms: • “Fishy” odor • Itching and/or irritation • Smooth, thin, sticky, white or gray discharge • Management − Patients should see a physician.
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Pathophysiology − Ovarian cyst • Fluid-filled sac on or within an ovary • Functional cyst is the most common • Corpus luteum cyst develops if the sac seals itself after release of the oocyte.
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Pathophysiology (cont’d) − If the cycle of forming sacs is repeated excessively, polycystic ovaries may develop. • Lack of progesterone and high levels of androgens
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Pathophysiology (cont’d) − Ovarian torsion occurs when a cyst does not self-resolve and grows to a significant size. • Sudden onset of severe lower abdominal pain • Nausea and vomiting
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Pathophysiology (cont’d) − Tubo-ovarian abscess is encountered secondary to a primary infectious agent. • Fallopian tubes or ovaries become blocked by an infectious mass.
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Assessment − A patient with an ovarian cyst may report: • • • Dull, achy pain in the lower back and thighs Abdominal pain or pressure Nausea and vomiting Breast tenderness Abnormal bleeding and painful menstruation
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Assessment (cont’d) − A ruptured ovarian cyst usually presents: • • • Lower abdominal pain (sharp) Abdominal distention and tenderness Dizziness Weakness Syncopal episode
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Assessment (cont’d) − A tubo-ovarian abscess may present with: • • • Severe abdominal pain Guarding and rebound tenderness Nausea and vomiting Abdominal distention Fever
Ruptured Ovarian Cyst, Ovarian Torsion, and Tubo-ovarian Abscess • Management − Treat a ruptured ovarian cyst or tubo-ovarian abscess the same as an ectopic pregnancy. − For patients with ovarian torsion: • Start an IV for pain medications and dehydration. • Administer antiemetics.
Prolapsed Uterus • Pathophysiology − Uterus drops from its normal position − Many women who have been through childbirth experience this condition. − Varying degrees of prolapse
Prolapsed Uterus • Assessment − Patients report may include: • • Vaginal and pelvic pain or low back pain Dysuria Incontinence Discharge − Assess for any signs of shock.
Prolapsed Uterus • Management − Prehospital treatment is limited to: • Pain management • Treatment for shock • Care for any tissue or the uterus itself − Do not replace any tissue.
Toxic Shock Syndrome • Pathophysiology − A form of septic shock caused by Streptococcus pyogenes or Staphylococcus aureus − Can include several body systems − Can progress from minor infections − Particularly affects menstruating women
Toxic Shock Syndrome • Assessment − Initial symptoms may include: • • Syncope Myalgia Diarrhea and/or vomiting Sore throat
Toxic Shock Syndrome • Management − Rapid transport is indicated. − Provide: • • High-flow supplemental oxygen IV therapy Pressors Cardiac monitoring
Sexually Transmitted Diseases • PID is typically secondary to an STD. − If indicated: • • Apply oxygen. Control bleeding. Start an IV line. Administer analgesics and antiemetics.
Sexually Transmitted Diseases • Bacterial vaginosis − Normal bacteria in the vagina are replaced by other bacterial forms. − Symptoms may include: • Itching, burning, pain • A “fishy, ” foul-smelling discharge
Sexually Transmitted Diseases • Bacterial vaginosis (cont’d) − Left untreated, can lead to: • Premature birth or low birthweight • Increased susceptibility to infections • PID − Treat with metronidazole.
Sexually Transmitted Diseases • Chancroid − Caused by infection with Haemophilus ducreyi − May cause painful sores or lymph glands or may be asymptomatic − Prehospital treatment is supportive.
Sexually Transmitted Diseases • Chlamydia − Caused by the Chlamydia trachomatis − Symptoms may include: • Lower abdominal or back pain • Pain during intercourse • Bleeding between menstrual periods
Sexually Transmitted Diseases • Cytomegalovirus (CMV) − Member of the herpes family − No known cure − Symptoms may include: • Prolonged high fever • Malaise • Enlarged spleen
Sexually Transmitted Diseases • Cytomegalovirus (CMV) (cont’d) − People with an increased risk include: • Those with immune disorders • People receiving chemotherapy • Pregnant women − Newborns may acquire CMV.
Sexually Transmitted Diseases • Genital herpes − Infection of the genitals, buttocks, or anal area caused by herpes simplex virus • Type I: infects the mouth and lips • Type II: primary cause of genital herpes
Sexually Transmitted Diseases • Genital herpes (cont’d) − In an outbreak, symptoms can last several weeks and may include: • Tingling or sores where the virus entered the body • Small red bumps that develop into small blisters and painful sores
Sexually Transmitted Diseases • Gonorrhea − Caused by Neisseria gonorrhoeae − Can grow and multiply in warm, moist areas − Symptoms may include: • Dysuria • Burning or itching • A yellowish or bloody vaginal discharge
Sexually Transmitted Diseases • Gonorrhea (cont’d) − Severe infections may progress to PID. − Gonococcal pharyngitis: infection of the throat − If not treated, may enter the bloodstream and other parts of the body • Disseminated gonococcemia
Sexually Transmitted Diseases • Genital warts − Caused by HPV • Causative agent in cervical, vulvar, and anal cancers − In pregnant women, warts may impede urination or obstruct the birth canal. − Some infected people have no symptoms.
Sexually Transmitted Diseases • Syphilis − − Caused by Treponema pallidum Signs and symptoms mimic other diseases. Manifests in three stages Transmission occurs through direct contact.
Sexually Transmitted Diseases • Syphilis (cont’d) − Primary stage: appearance of a single sore − Secondary stage: development of mucous membrane lesions and a skin rash − Late stage: internal damage
Sexually Transmitted Diseases • Syphilis (cont’d) − Pregnant women with syphilis may have: • • Stillborn babies Babies who are born blind Developmentally delayed babies Babies who die shortly after birth
Sexually Transmitted Diseases • Trichomoniasis − Caused by Trichomonas vaginalis − Symptoms may include: • A frothy, yellow-green vaginal discharge • Irritation and itching • Discomfort during intercourse
Sexual Assault • Pathophysiology − Rape is the most common form. − Police involvement should be expected. − Victim may “shut down. ” • If possible, a female paramedic should be optional.
Sexual Assault • Assessment − Ask if patient would be more comfortable with a female or male paramedic. − Limit examination to a brief survey. − Protect the patient's privacy.
Sexual Assault • Management − You have a responsibility to preserve evidence. − Discourage the patient from doing anything that will possibly corrupt any evidence. − Offer to call the local rape crisis center.
Sexual Assault • Management (cont’d) − The patient care report is a legal document. − Record the following observations: • The patient's emotional state • The condition of her clothing • Any obvious injuries
Sexual Assault • Drugs used to facilitate rape − Alcohol − Club drugs • • GHB Ketamine Ecstasy Rohypnol
Sexual Practices and Vaginal Foreign Bodies • Pathophysiology − Foreign objects stuck in the vagina or anus • • Keep the patient calm. Protect his or her dignity. Do not attempt to remove any foreign object. Do not let the patient walk.
Sexual Practices and Vaginal Foreign Bodies • Pathophysiology (cont’d) − Fisting • Organ rupture is likely. − Insertion of live animals into the vagina
Sexual Practices and Vaginal Foreign Bodies • Assessment − Maintain your patient's privacy. − Inspection of the genital area may be necessary. − Conduct a thorough patient assessment.
Sexual Practices and Vaginal Foreign Bodies • Management − Treat as you would with any foreign object. • Remain nonjudgmental • Transport. • Do not attempt to retrieve the object. − Transport with knees-flexed, legs-together.
Summary • Gynecology is the study of and care for diseases of the female reproductive system. • External female genitalia is sometimes referred to as the pudendum and has many different parts. • The vagina, Bartholin glands, cervix, uterus, fallopian tubes, and ovaries make up the internal female genitalia.
Summary • Menstruation is the vaginal discharge of primarily blood, which usually occurs monthly. • A woman can experience many physical changes during the menstrual cycle. • The last menses is called menopause. • When assessing a patient with a gynecologic emergency, begin by focusing on the ABCs.
Summary • Protect the patient’s modesty at all times. • If the chief complaint is abdominal pain, investigate the pain by following the mnemonic LORDS TRACHEA. • Determine when the patient had her LMP, if it was unusual in any way, whether she could be pregnant, and whether she uses contraception.
Summary • Vaginal bleeding that does not occur during the course of regular menstruation is cause for concern. • Obtain the patient’s obstetric history, including any previous pregnancies, miscarriages, or abortions and a description of any vaginal discharge.
Summary • General management for gynecologic emergencies includes addressing life threats, being supportive, and protecting a patient’s modesty. • Ectopic pregnancy, ruptured ovarian cyst, and tubo-ovarian abscess are lifethreatening gynecologic emergencies.
Summary • Mittelschmerz is abdominal pain and cramping that occur about 2 weeks before menstruation. Dysmenorrhea is painful menstruation. • Amenorrhea is the absence or cessations of menses usually from pregnancy. • Endometritis is inflammation of the endometrium. • Endometriosis is the growth of endometrial tissue outside of the uterus.
Summary • Endometriosis is the growth of endometrial tissue outside of the uterus. • PID is a common infection of the female upper reproductive organs that causes abdominal pain in women. • Patients with PID will present with abdominal pain starting during or after menstruation.
Summary • Vaginitis and vulvovaginitis are inflammations of the vaginal tissues and external vulva caused by an infection. • A Bartholin abscess will cause a painful lump, irritation, painful intercourse, and possibly fever. The abscess may need to be drained by a physician. • In ectopic pregnancy, a fertilized oocyte implants somewhere other than the uterus.
Summary • Ruptured ovarian cyst, tubo-ovarian abscess, and ovarian torsion are other gynecologic conditions that can become an emergency. • A prolapsed uterus is when the uterus drops into the vagina. • TSS is a form of septic shock that can result from an infection in the body.
Summary • STDs include bacterial vaginosis, chancroid, chlamydia, cytomegalovirus, genital herpes, gonorrhea, syphilis, and trichomoniasis. • There are many different symptoms associated with STDs. • Sexual assault is a category of crime that includes molestation and rape.
Summary • It may be difficult to obtain a history from a victim of rape. Have a same-sex paramedic treat the patient when possible. • Limit physical examinations to lifethreatening injuries in sexually assaulted victims, and ask only medical questions.
Summary • Preserve evidence when possible. • Document cases of sexual assault properly and professionally. • Drugs are often used to facilitate rape. • Sexual emergencies may involve foreign objects stuck in the vagina or anus.
Credits • Chapter opener: © Jones & Bartlett Learning. Courtesy of MIEMSS. • Backgrounds: Orange—© Keith Brofsky/Photodisc/Getty Images; Green—Jones & Bartlett Learning; Purple— Courtesy of Rhonda Beck; Lime—© Photodisc. • Unless otherwise indicated, all photographs and illustrations are under copyright of Jones & Bartlett Learning, courtesy of Maryland Institute for Emergency Medical Services Systems, or have been provided by the American Academy of Orthopaedic Surgeons.