Chapter 20 The Heart 2015 Pearson Education Inc
- Slides: 58
Chapter 20: The Heart © 2015 Pearson Education, Inc.
Homeostasis • Heart contributes to homeostasis by pumping blood throughout the body to deliver O 2 & nutrients & remove wastes © 2015 Pearson Education, Inc.
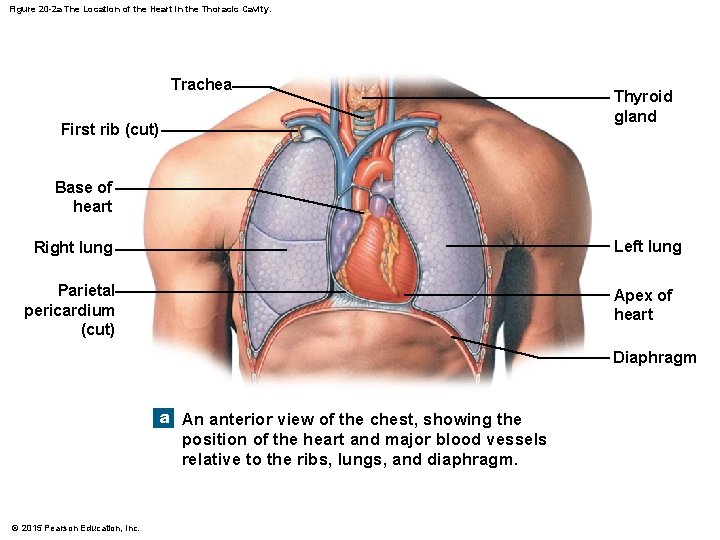
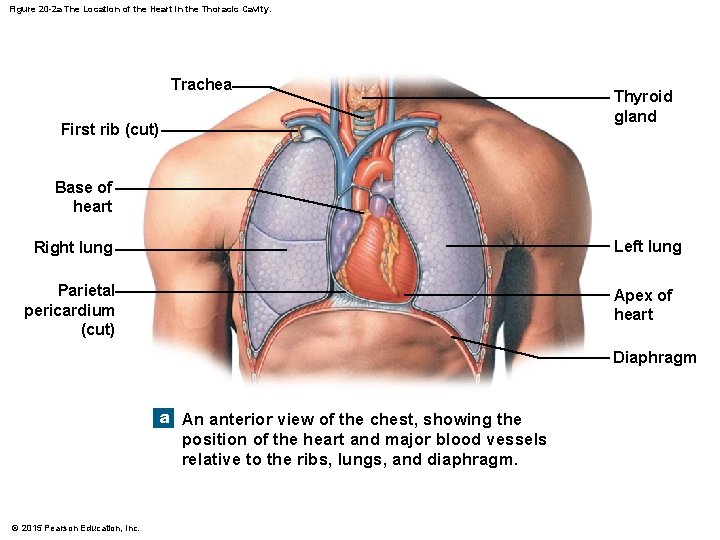
Figure 20 -2 a The Location of the Heart in the Thoracic Cavity. Trachea First rib (cut) Thyroid gland Base of heart Right lung Left lung Parietal pericardium (cut) Apex of heart Diaphragm a An anterior view of the chest, showing the position of the heart and major blood vessels relative to the ribs, lungs, and diaphragm. © 2015 Pearson Education, Inc.
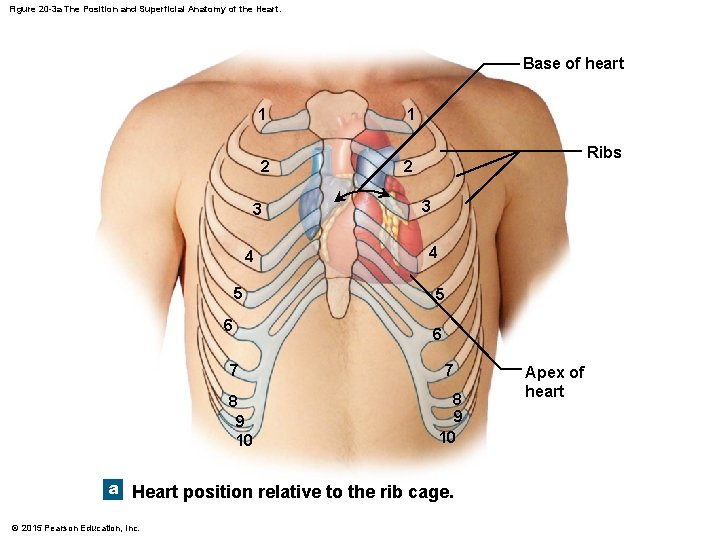
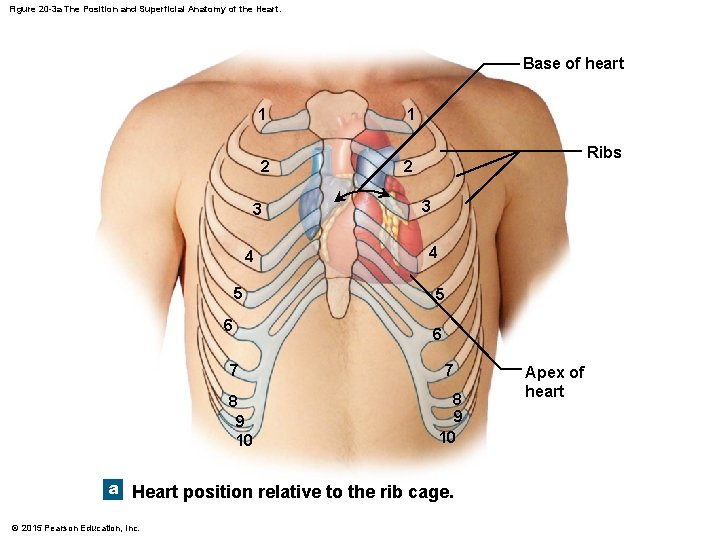
Figure 20 -3 a The Position and Superficial Anatomy of the Heart. Base of heart 1 2 3 4 5 6 7 8 9 10 1 Ribs 2 3 4 5 6 7 8 9 10 a Heart position relative to the rib cage. © 2015 Pearson Education, Inc. Apex of heart
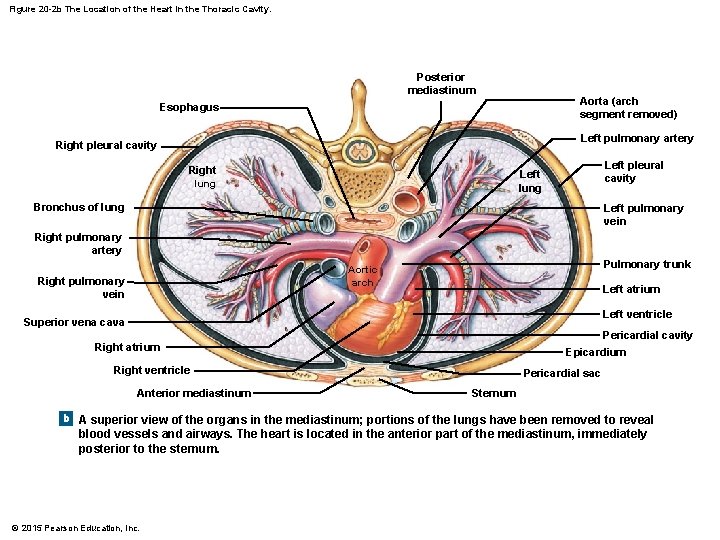
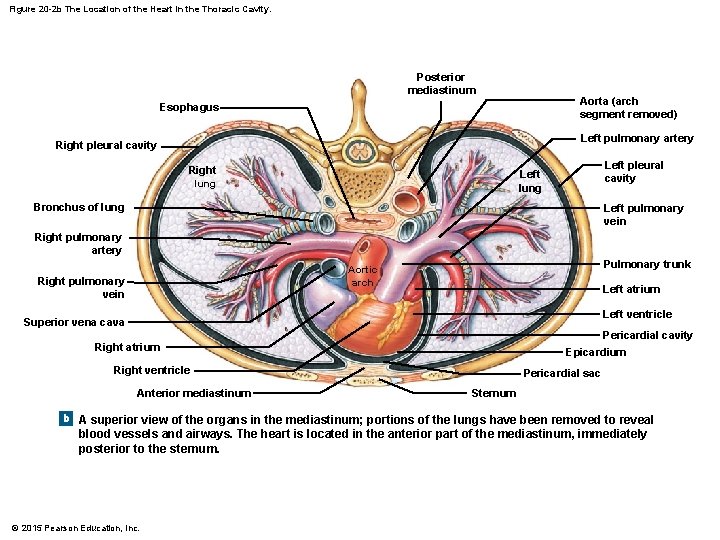
Figure 20 -2 b The Location of the Heart in the Thoracic Cavity. Posterior mediastinum Aorta (arch segment removed) Esophagus Left pulmonary artery Right pleural cavity Right lung Left pleural cavity Left lung Bronchus of lung Left pulmonary vein Right pulmonary artery Pulmonary trunk Aortic arch Right pulmonary vein Left atrium Left ventricle Superior vena cava Pericardial cavity Right atrium Epicardium Right ventricle Anterior mediastinum Pericardial sac Sternum b A superior view of the organs in the mediastinum; portions of the lungs have been removed to reveal blood vessels and airways. The heart is located in the anterior part of the mediastinum, immediately posterior to the sternum. © 2015 Pearson Education, Inc.
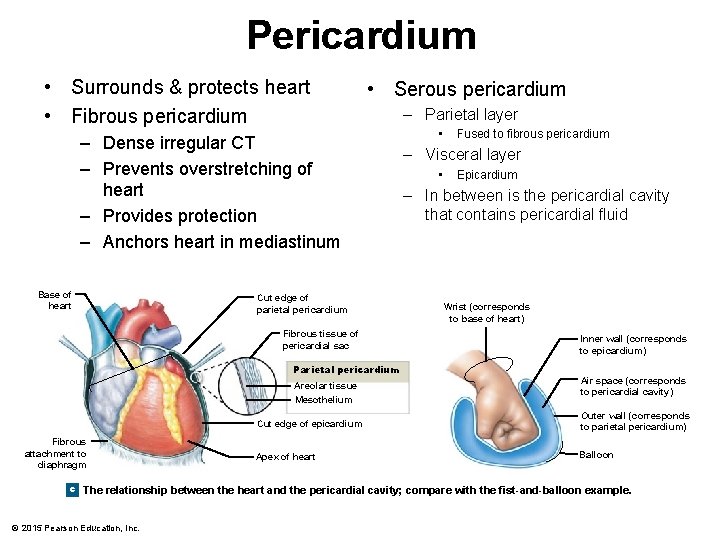
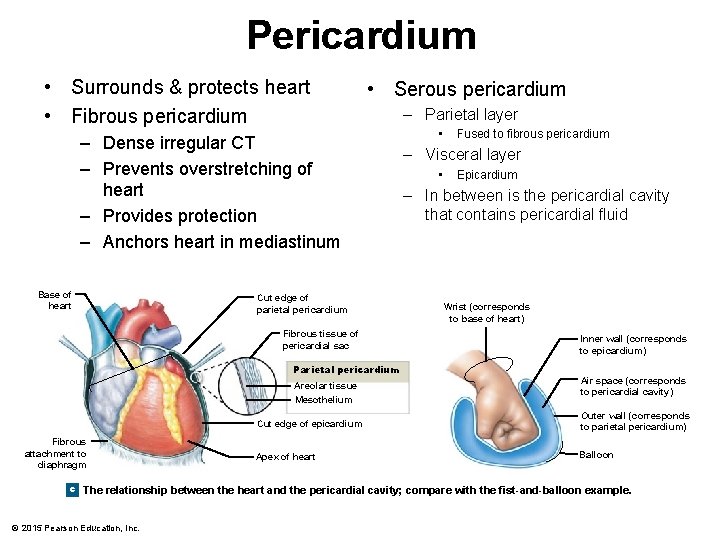
Pericardium • Surrounds & protects heart • Fibrous pericardium • Serous pericardium – Dense irregular CT – Prevents overstretching of heart – Provides protection – Anchors heart in mediastinum Base of heart Cut edge of parietal pericardium Fibrous tissue of pericardial sac Parietal pericardium Areolar tissue Mesothelium Fibrous attachment to diaphragm – Parietal layer • Fused to fibrous pericardium – Visceral layer • Epicardium – In between is the pericardial cavity that contains pericardial fluid Wrist (corresponds to base of heart) Inner wall (corresponds to epicardium) Air space (corresponds to pericardial cavity) Cut edge of epicardium Outer wall (corresponds to parietal pericardium) Apex of heart Balloon c The relationship between the heart and the pericardial cavity; compare with the fist-and-balloon example. © 2015 Pearson Education, Inc.
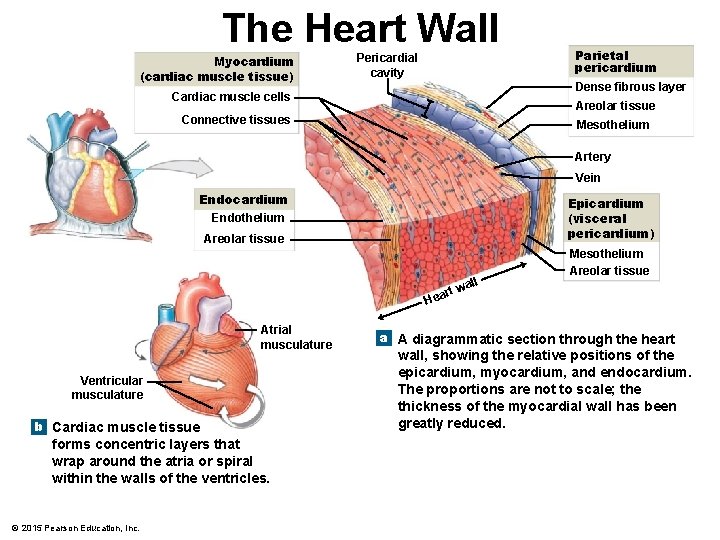
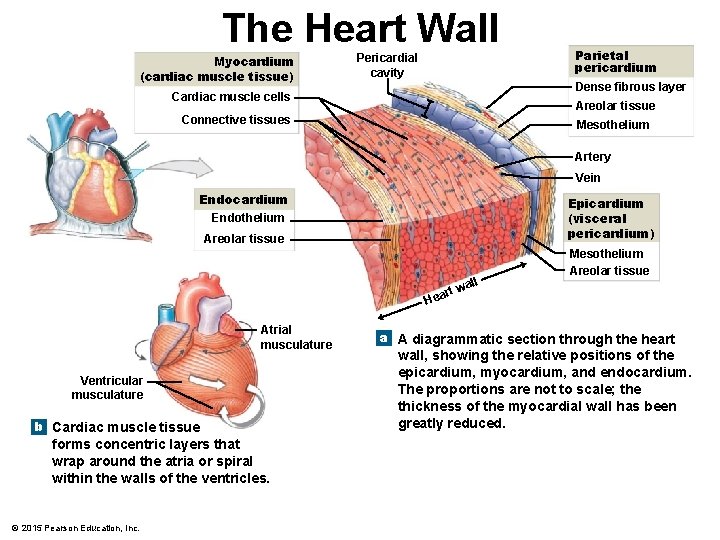
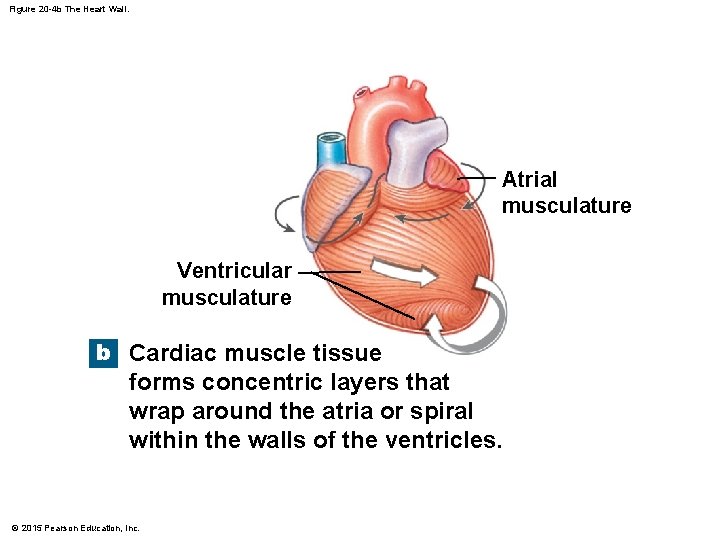
The Heart Wall Myocardium (cardiac muscle tissue) Pericardial cavity Parietal pericardium Dense fibrous layer Cardiac muscle cells Areolar tissue Connective tissues Mesothelium Artery Vein Endocardium Endothelium Epicardium (visceral pericardium) Areolar tissue all Mesothelium Areolar tissue rt w Hea Atrial musculature Ventricular musculature b Cardiac muscle tissue forms concentric layers that wrap around the atria or spiral within the walls of the ventricles. © 2015 Pearson Education, Inc. a A diagrammatic section through the heart wall, showing the relative positions of the epicardium, myocardium, and endocardium. The proportions are not to scale; the thickness of the myocardial wall has been greatly reduced.
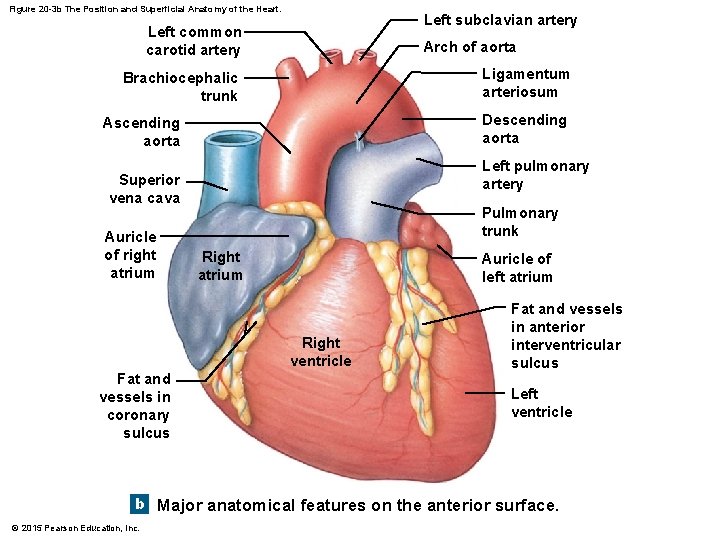
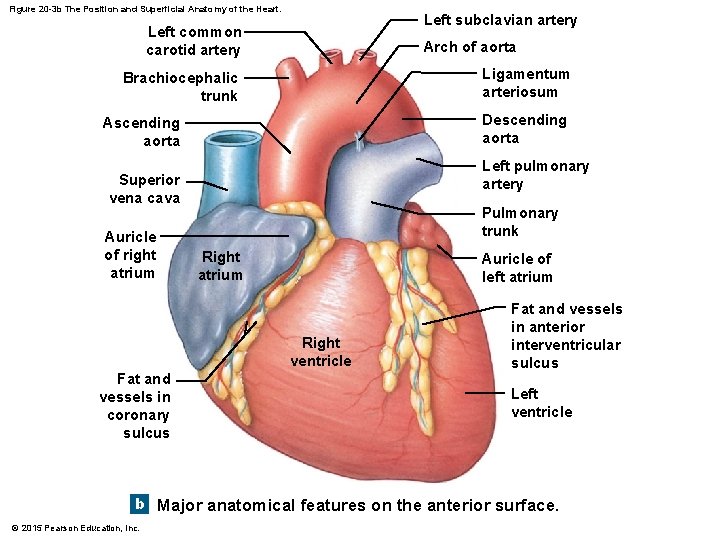
Figure 20 -3 b The Position and Superficial Anatomy of the Heart. Left subclavian artery Left common carotid artery Arch of aorta Ligamentum arteriosum Brachiocephalic trunk Descending aorta Ascending aorta Left pulmonary artery Superior vena cava Auricle of right atrium Pulmonary trunk Right atrium Auricle of left atrium Right ventricle Fat and vessels in coronary sulcus Fat and vessels in anterior interventricular sulcus Left ventricle b Major anatomical features on the anterior surface. © 2015 Pearson Education, Inc.
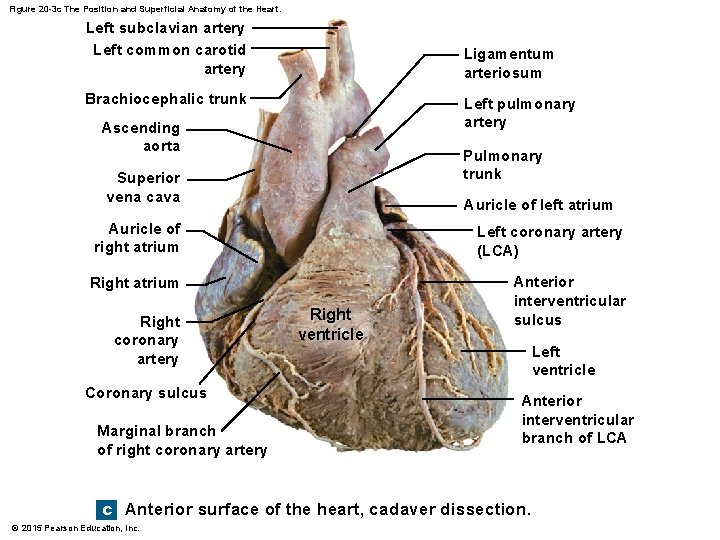
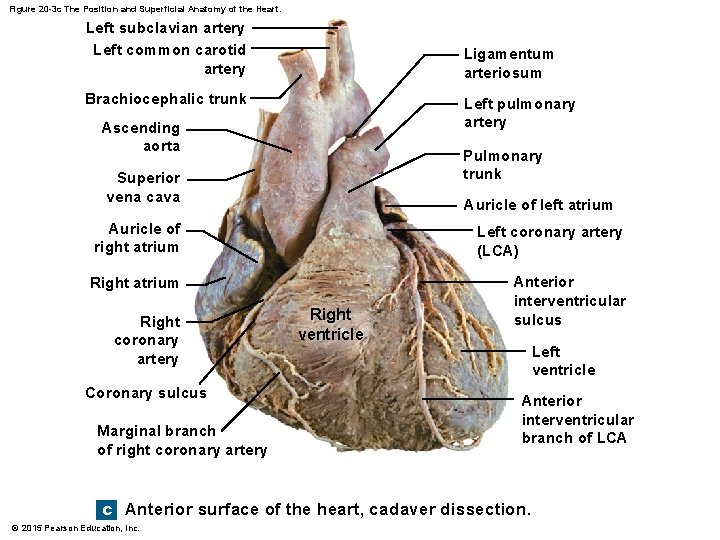
Figure 20 -3 c The Position and Superficial Anatomy of the Heart. Left subclavian artery Left common carotid artery Ligamentum arteriosum Brachiocephalic trunk Left pulmonary artery Ascending aorta Pulmonary trunk Superior vena cava Auricle of left atrium Auricle of right atrium Left coronary artery (LCA) Right atrium Anterior interventricular sulcus Right coronary artery Coronary sulcus Marginal branch of right coronary artery Right ventricle Left ventricle Anterior interventricular branch of LCA c Anterior surface of the heart, cadaver dissection. © 2015 Pearson Education, Inc.
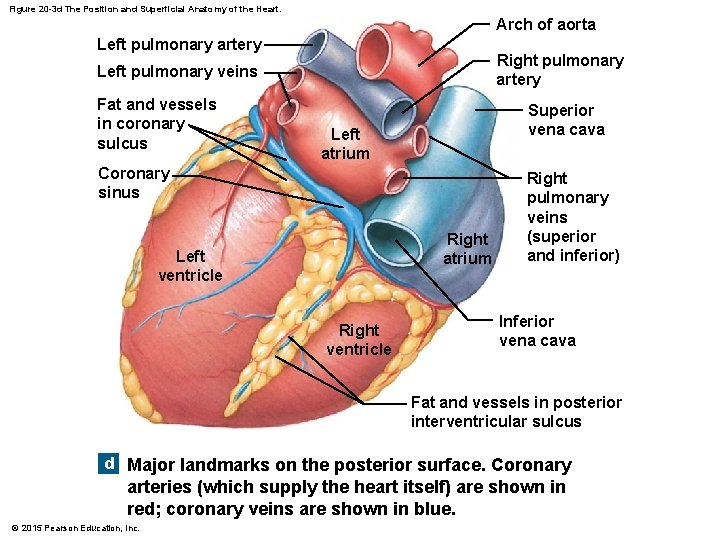
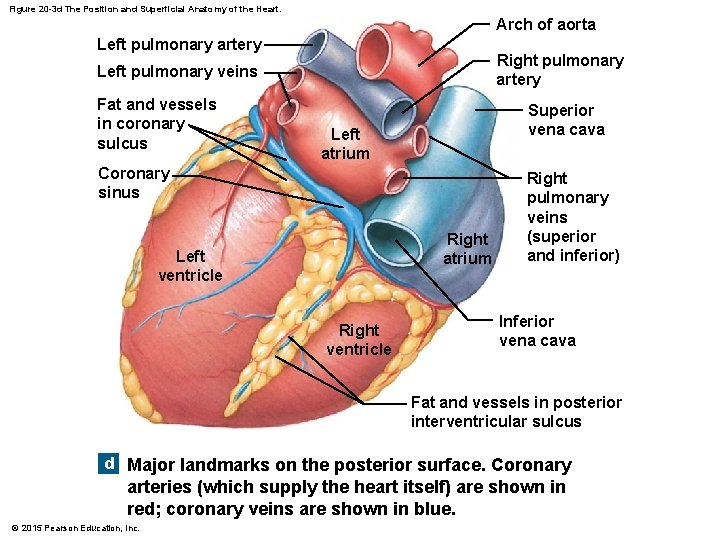
Figure 20 -3 d The Position and Superficial Anatomy of the Heart. Arch of aorta Left pulmonary artery Right pulmonary artery Left pulmonary veins Fat and vessels in coronary sulcus Superior vena cava Left atrium Coronary sinus Right atrium Left ventricle Right pulmonary veins (superior and inferior) Inferior vena cava Fat and vessels in posterior interventricular sulcus d Major landmarks on the posterior surface. Coronary arteries (which supply the heart itself) are shown in red; coronary veins are shown in blue. © 2015 Pearson Education, Inc.
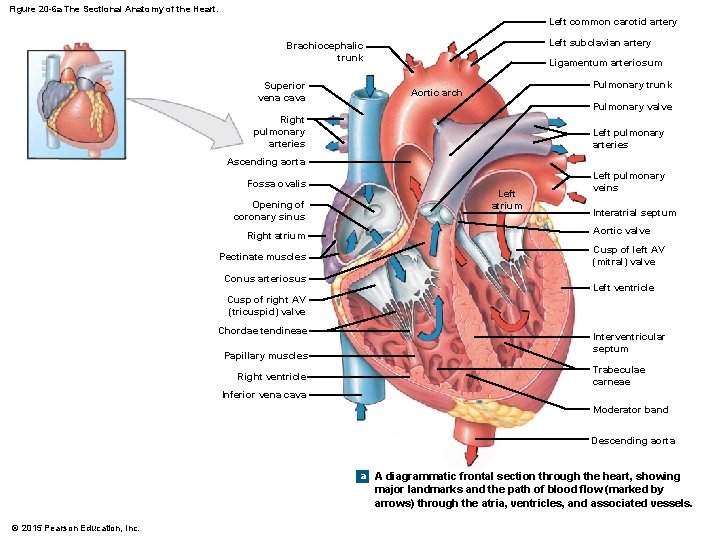
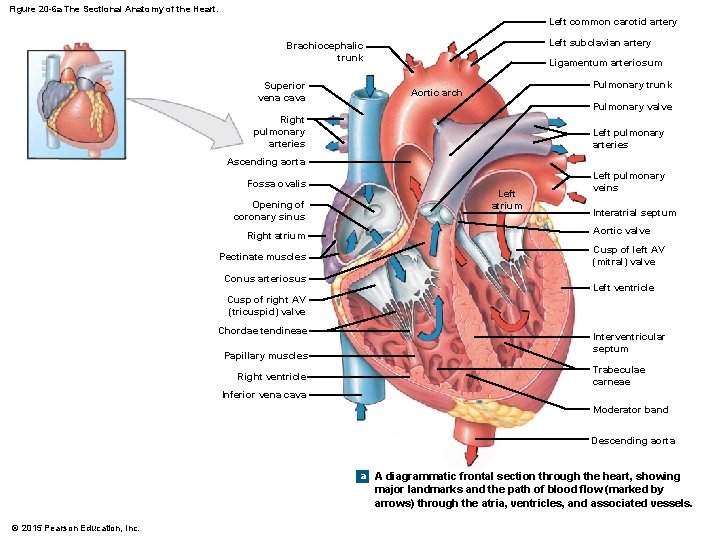
Figure 20 -6 a The Sectional Anatomy of the Heart. Left common carotid artery Left subclavian artery Brachiocephalic trunk Superior vena cava Ligamentum arteriosum Pulmonary trunk Aortic arch Pulmonary valve Right pulmonary arteries Left pulmonary arteries Ascending aorta Fossa ovalis Opening of coronary sinus Right atrium Pectinate muscles Conus arteriosus Left atrium Left pulmonary veins Interatrial septum Aortic valve Cusp of left AV (mitral) valve Left ventricle Cusp of right AV (tricuspid) valve Chordae tendineae Papillary muscles Right ventricle Interventricular septum Trabeculae carneae Inferior vena cava Moderator band Descending aorta a A diagrammatic frontal section through the heart, showing major landmarks and the path of blood flow (marked by arrows) through the atria, ventricles, and associated vessels. © 2015 Pearson Education, Inc.
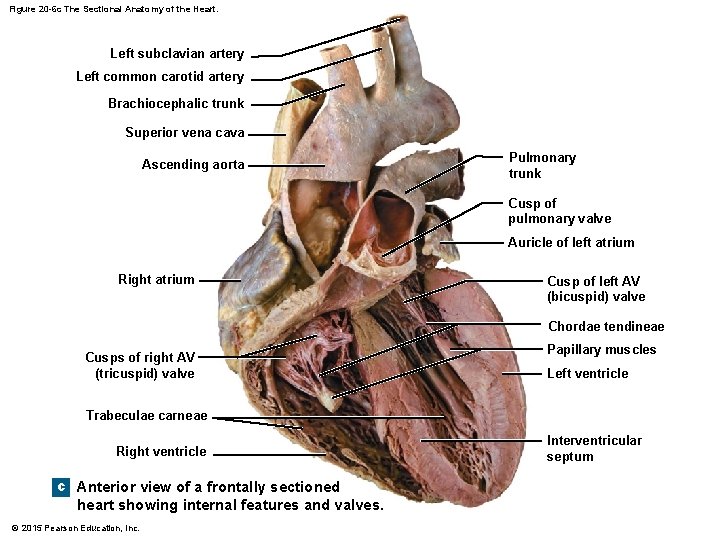
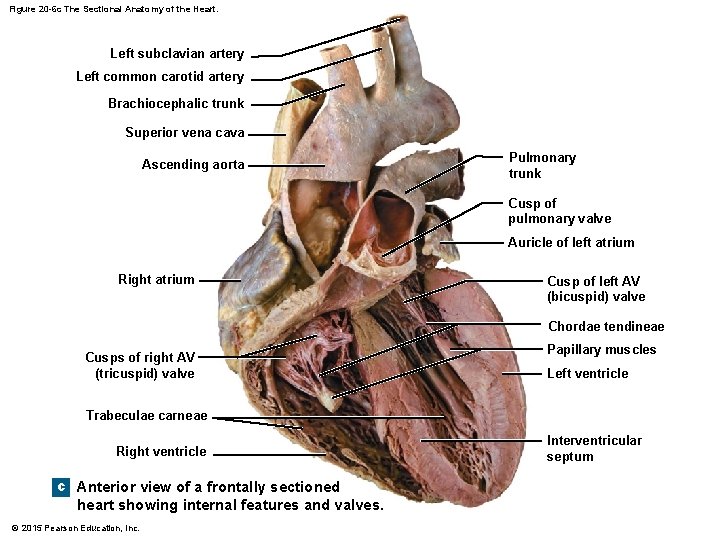
Figure 20 -6 c The Sectional Anatomy of the Heart. Left subclavian artery Left common carotid artery Brachiocephalic trunk Superior vena cava Ascending aorta Pulmonary trunk Cusp of pulmonary valve Auricle of left atrium Right atrium Cusp of left AV (bicuspid) valve Chordae tendineae Cusps of right AV (tricuspid) valve Papillary muscles Left ventricle Trabeculae carneae Right ventricle c Anterior view of a frontally sectioned heart showing internal features and valves. © 2015 Pearson Education, Inc. Interventricular septum
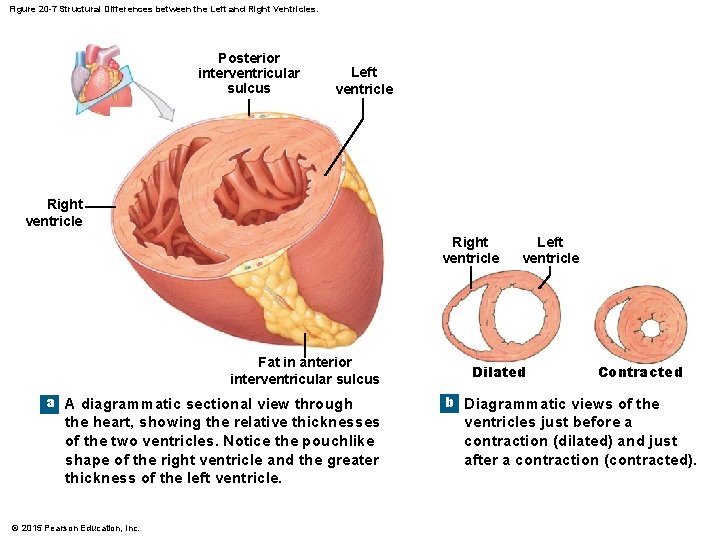
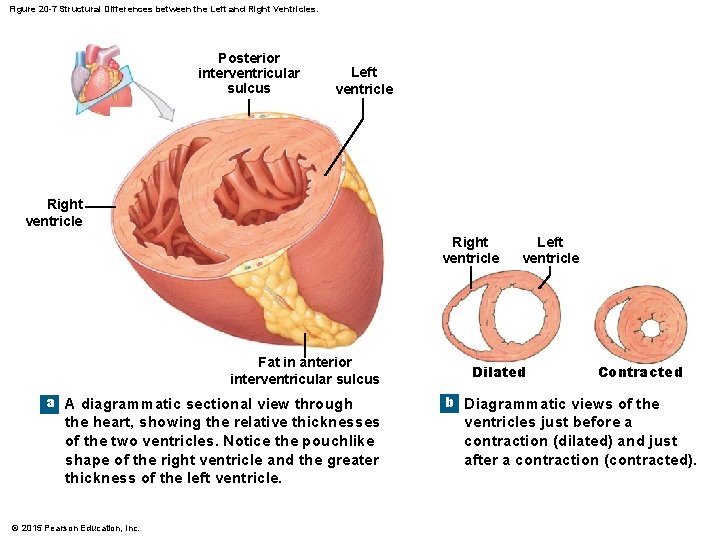
Figure 20 -7 Structural Differences between the Left and Right Ventricles. Posterior interventricular sulcus Left ventricle Right ventricle Fat in anterior interventricular sulcus a A diagrammatic sectional view through the heart, showing the relative thicknesses of the two ventricles. Notice the pouchlike shape of the right ventricle and the greater thickness of the left ventricle. © 2015 Pearson Education, Inc. Left ventricle Dilated Contracted b Diagrammatic views of the ventricles just before a contraction (dilated) and just after a contraction (contracted).
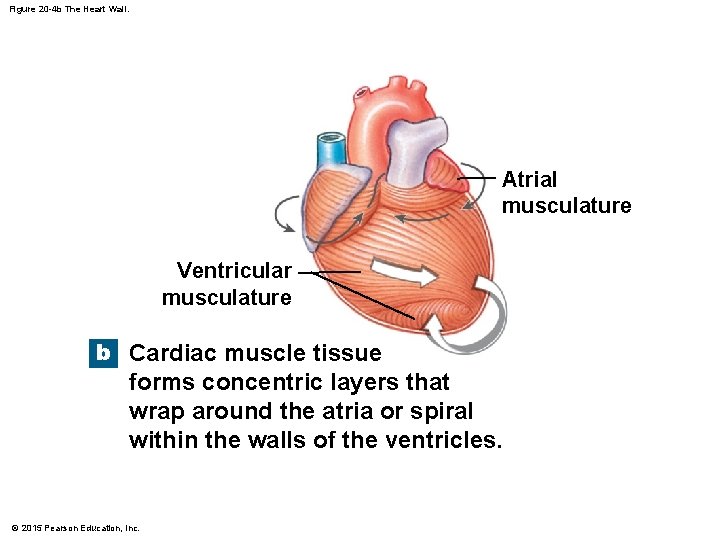
Figure 20 -4 b The Heart Wall. Atrial musculature Ventricular musculature b Cardiac muscle tissue forms concentric layers that wrap around the atria or spiral within the walls of the ventricles. © 2015 Pearson Education, Inc.
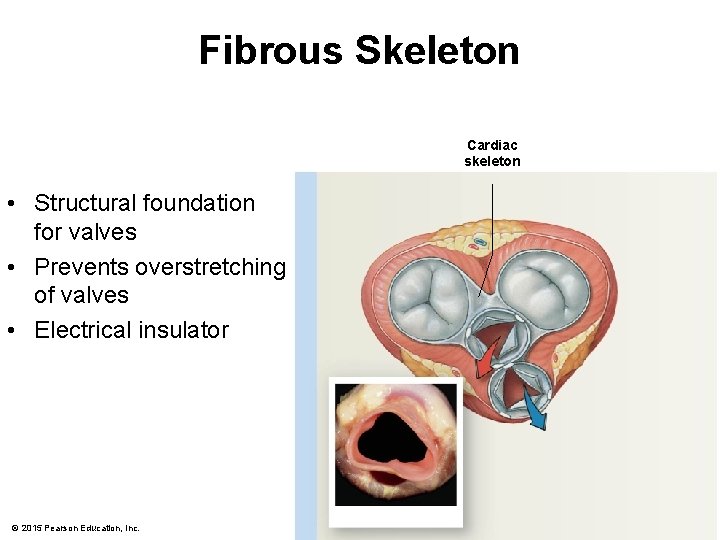
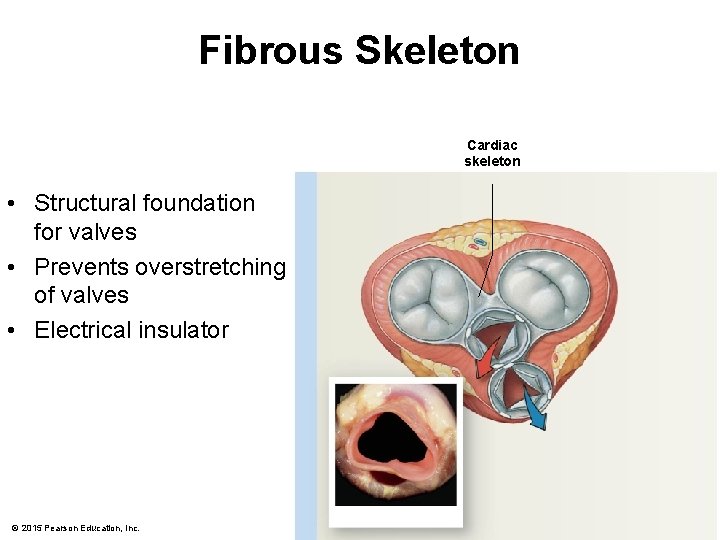
Fibrous Skeleton Cardiac skeleton • Structural foundation for valves • Prevents overstretching of valves • Electrical insulator © 2015 Pearson Education, Inc.
Valves • Ensure one-way flow of blood so that it does not backflow • Open & close in response to pressure changes as heart contracts & relaxes © 2015 Pearson Education, Inc.
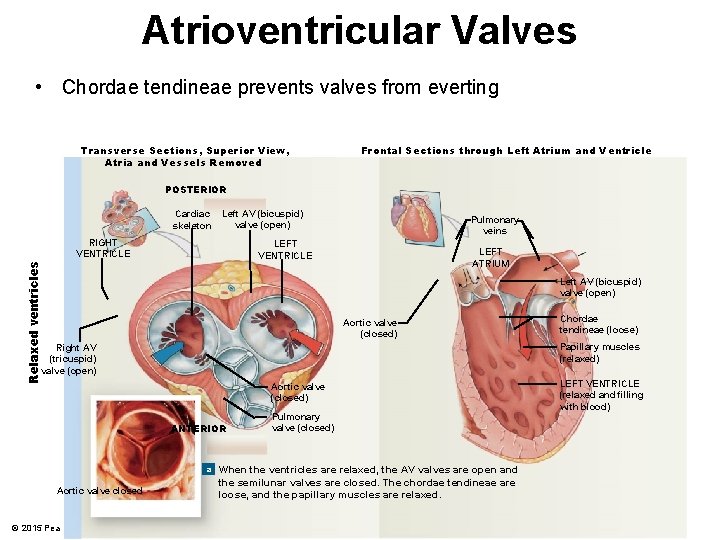
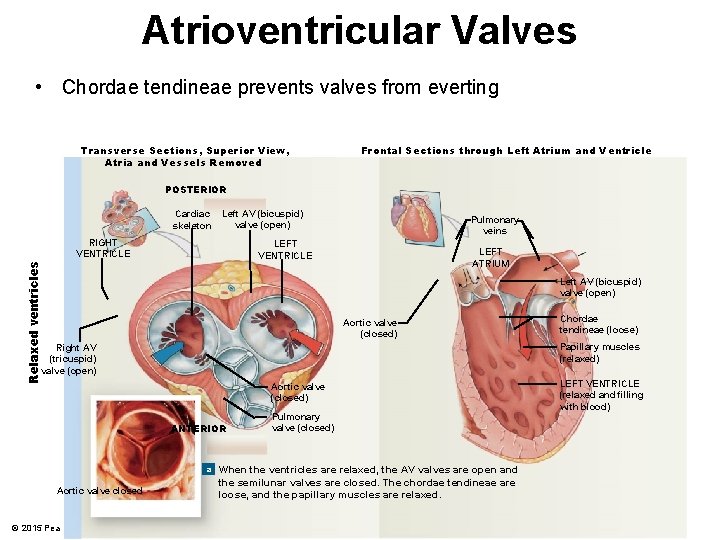
Atrioventricular Valves • Chordae tendineae prevents valves from everting Transverse Sections, Superior View, Atria and Vessels Removed Frontal Sections through Left Atrium and Ventricle POSTERIOR Cardiac skeleton Left AV (bicuspid) valve (open) RIGHT VENTRICLE Pulmonary veins Relaxed ventricles LEFT VENTRICLE LEFT ATRIUM Left AV (bicuspid) valve (open) Aortic valve (closed) Papillary muscles (relaxed) Right AV (tricuspid) valve (open) Aortic valve (closed) ANTERIOR Pulmonary valve (closed) a When the ventricles are relaxed, the AV valves are open and Aortic valve closed © 2015 Pearson Education, Inc. Chordae tendineae (loose) the semilunar valves are closed. The chordae tendineae are loose, and the papillary muscles are relaxed. LEFT VENTRICLE (relaxed and filling with blood)
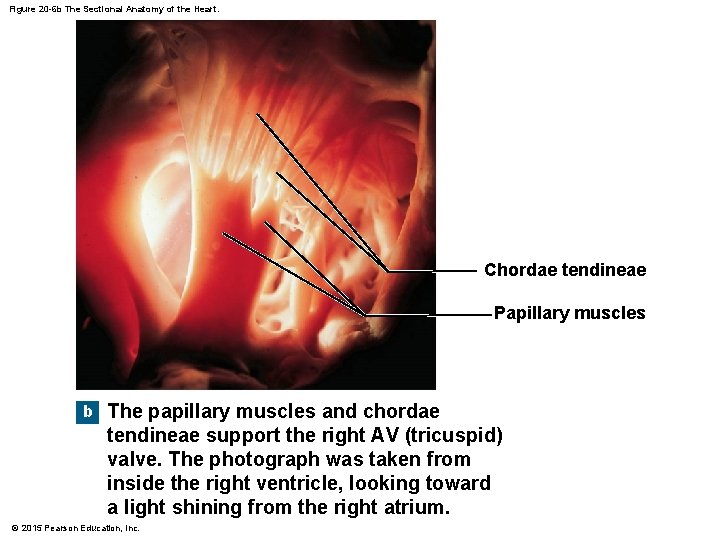
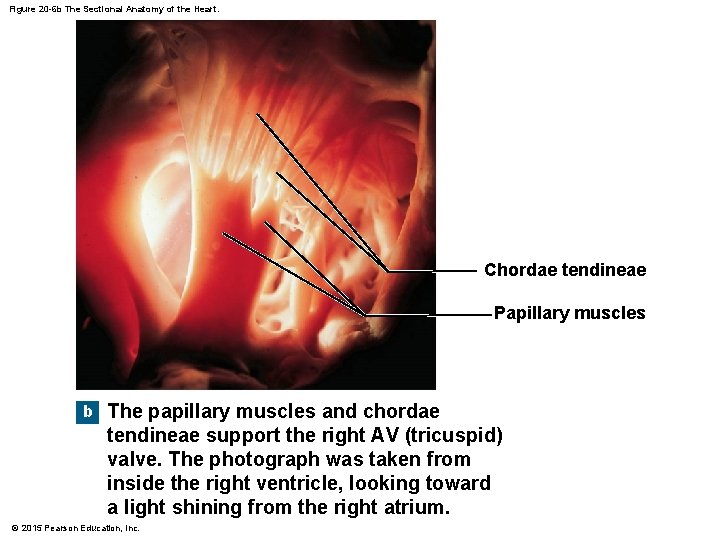
Figure 20 -6 b The Sectional Anatomy of the Heart. Chordae tendineae Papillary muscles b The papillary muscles and chordae tendineae support the right AV (tricuspid) valve. The photograph was taken from inside the right ventricle, looking toward a light shining from the right atrium. © 2015 Pearson Education, Inc.
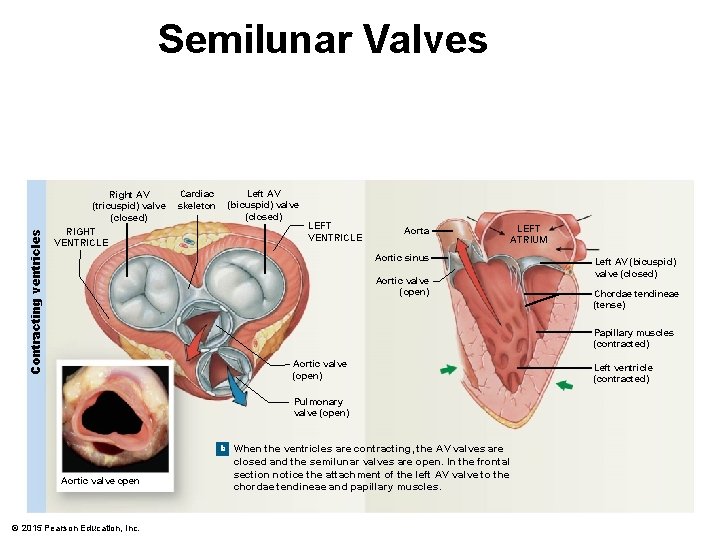
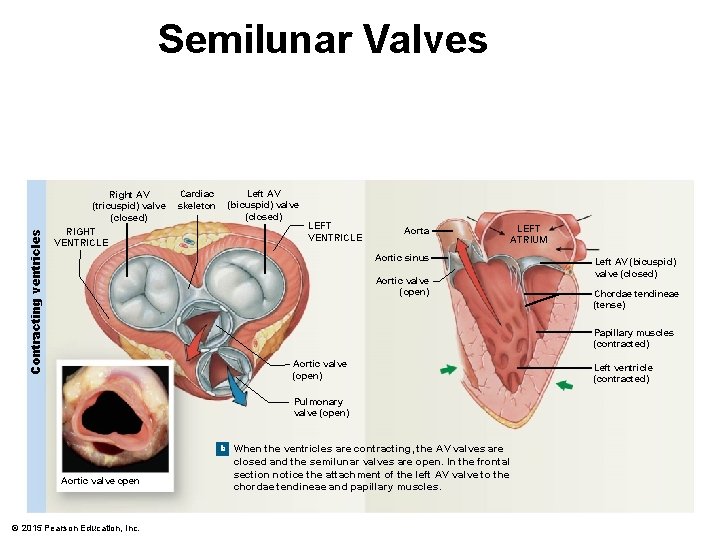
Contracting ventricles Semilunar Valves Right AV (tricuspid) valve (closed) RIGHT VENTRICLE Cardiac skeleton Left AV (bicuspid) valve (closed) LEFT VENTRICLE Aorta LEFT ATRIUM Aortic sinus Aortic valve (open) Left AV (bicuspid) valve (closed) Chordae tendineae (tense) Papillary muscles (contracted) Aortic valve (open) Pulmonary valve (open) b When the ventricles are contracting, the AV valves are Aortic valve open © 2015 Pearson Education, Inc. closed and the semilunar valves are open. In the frontal section notice the attachment of the left AV valve to the chordae tendineae and papillary muscles. Left ventricle (contracted)
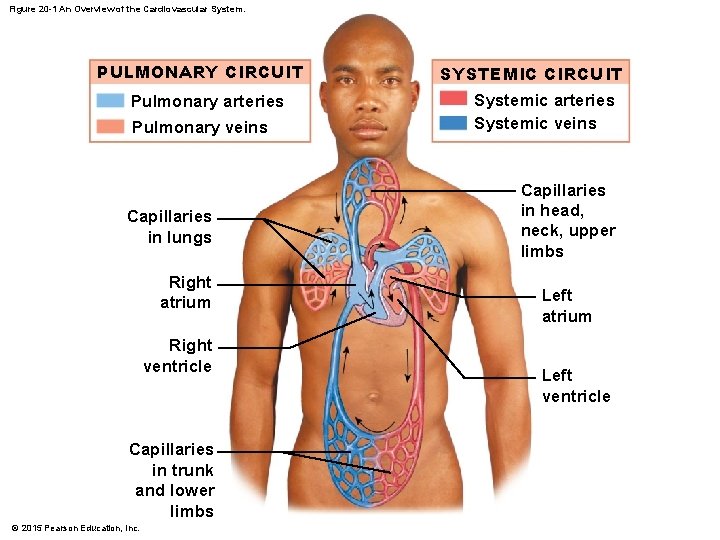
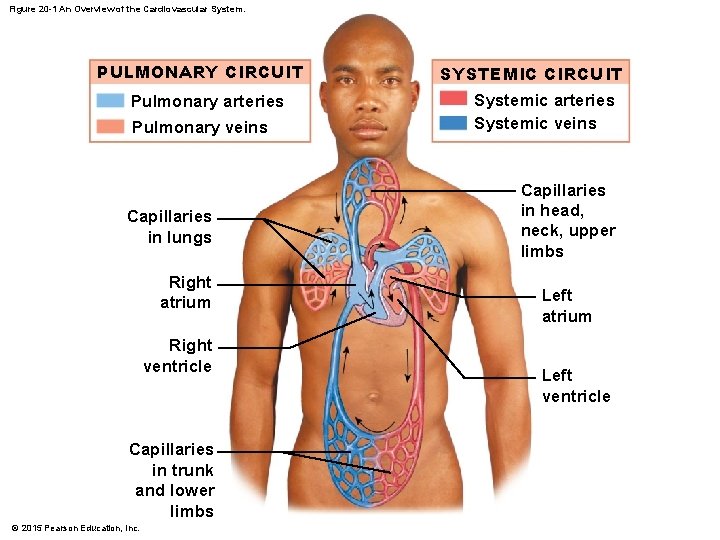
Figure 20 -1 An Overview of the Cardiovascular System. PULMONARY CIRCUIT Pulmonary arteries Pulmonary veins Capillaries in lungs Right atrium Right ventricle Capillaries in trunk and lower limbs © 2015 Pearson Education, Inc. SYSTEMIC CIRCUIT Systemic arteries Systemic veins Capillaries in head, neck, upper limbs Left atrium Left ventricle
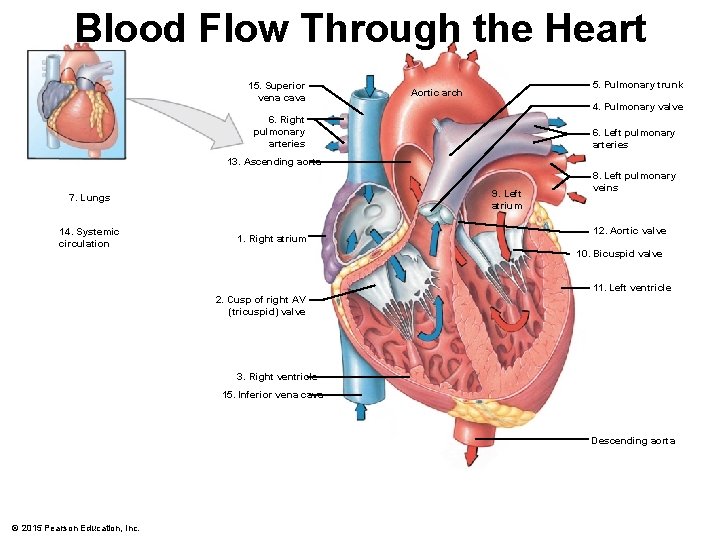
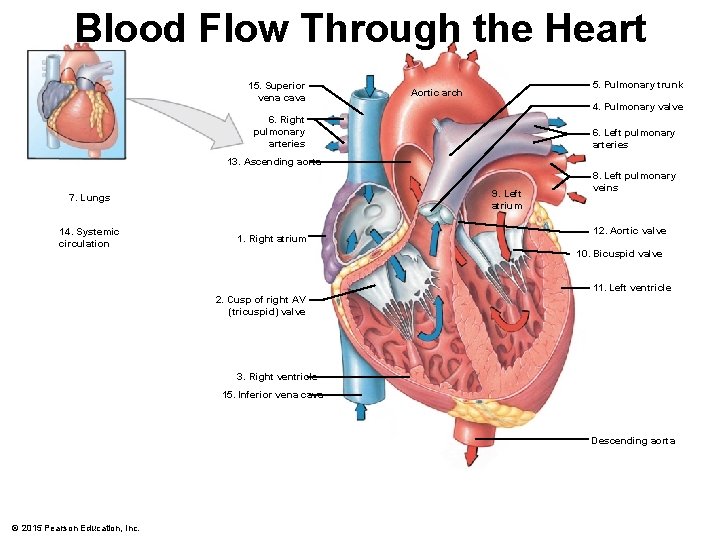
Blood Flow Through the Heart 15. Superior vena cava 5. Pulmonary trunk Aortic arch 4. Pulmonary valve 6. Right pulmonary arteries 6. Left pulmonary arteries 13. Ascending aorta 9. Left atrium 7. Lungs 14. Systemic circulation 1. Right atrium 8. Left pulmonary veins 12. Aortic valve 10. Bicuspid valve 11. Left ventricle 2. Cusp of right AV (tricuspid) valve 3. Right ventricle 15. Inferior vena cava Descending aorta © 2015 Pearson Education, Inc.
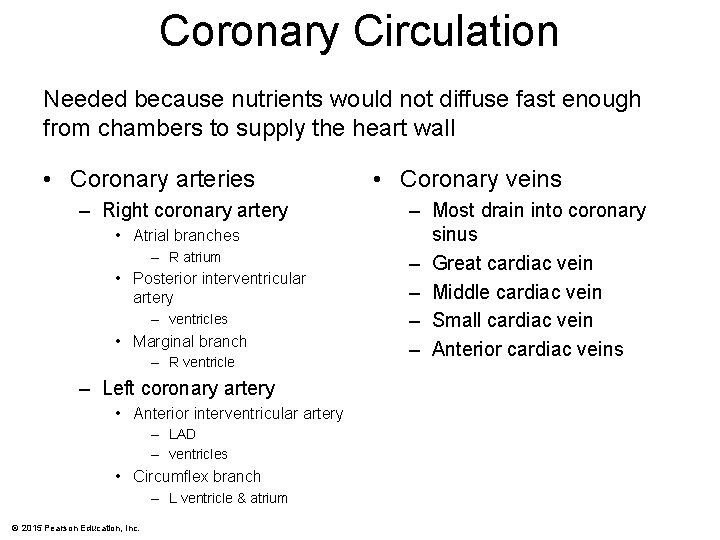
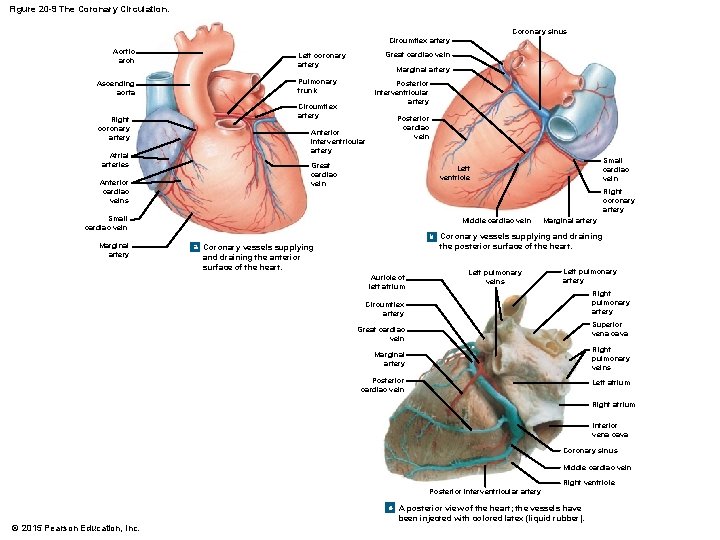
Coronary Circulation Needed because nutrients would not diffuse fast enough from chambers to supply the heart wall • Coronary arteries – Right coronary artery • Atrial branches – R atrium • Posterior interventricular artery – ventricles • Marginal branch – R ventricle – Left coronary artery • Anterior interventricular artery – LAD – ventricles • Circumflex branch – L ventricle & atrium © 2015 Pearson Education, Inc. • Coronary veins – Most drain into coronary sinus – Great cardiac vein – Middle cardiac vein – Small cardiac vein – Anterior cardiac veins
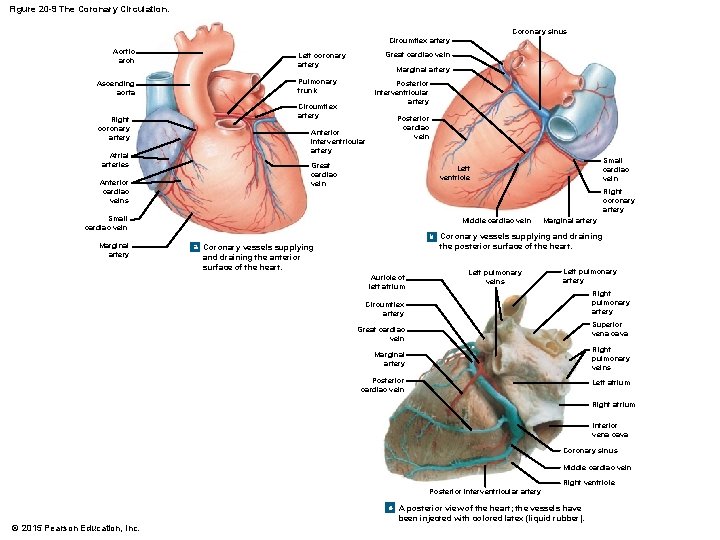
Figure 20 -9 The Coronary Circulation. Coronary sinus Circumflex artery Aortic arch Ascending aorta Right coronary artery Great cardiac vein Left coronary artery Marginal artery Pulmonary trunk Posterior interventricular artery Circumflex artery Anterior interventricular artery Atrial arteries Posterior cardiac vein Great cardiac vein Anterior cardiac veins Right coronary artery Small cardiac vein Marginal artery Small cardiac vein Left ventricle Middle cardiac vein Marginal artery b Coronary vessels supplying and draining a Coronary vessels supplying the posterior surface of the heart. and draining the anterior surface of the heart. Auricle of left atrium Left pulmonary veins Left pulmonary artery Right pulmonary artery Circumflex artery Superior vena cava Great cardiac vein Marginal artery Right pulmonary veins Posterior cardiac vein Left atrium Right atrium Inferior vena cava Coronary sinus Middle cardiac vein Right ventricle Posterior interventricular artery c A posterior view of the heart; the vessels have © 2015 Pearson Education, Inc. been injected with colored latex (liquid rubber).
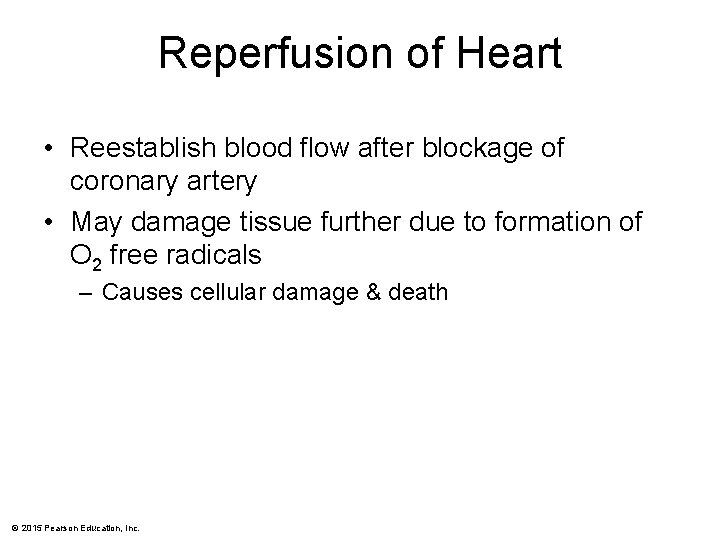
Reperfusion of Heart • Reestablish blood flow after blockage of coronary artery • May damage tissue further due to formation of O 2 free radicals – Causes cellular damage & death © 2015 Pearson Education, Inc.
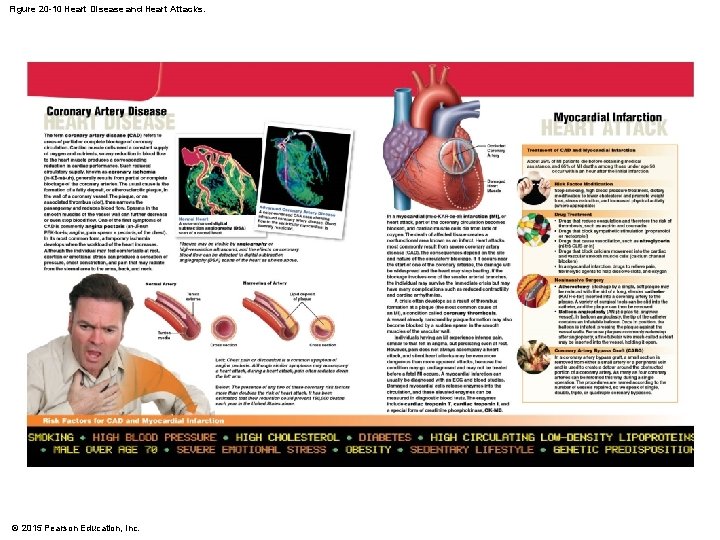
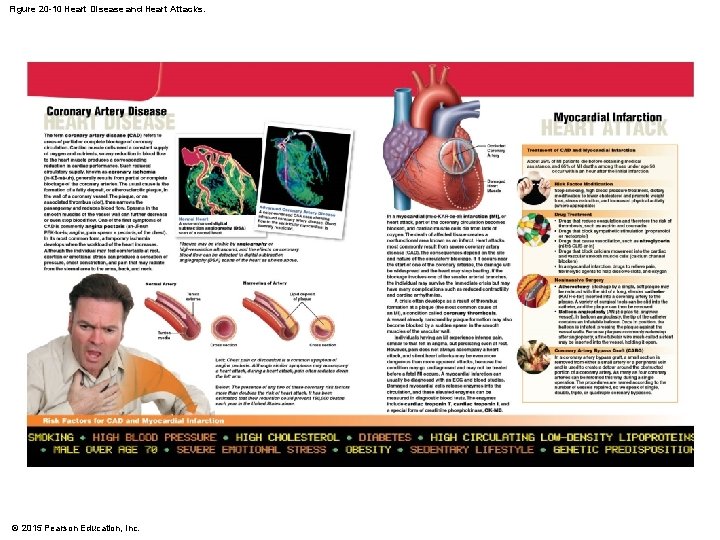
Figure 20 -10 Heart Disease and Heart Attacks. © 2015 Pearson Education, Inc.
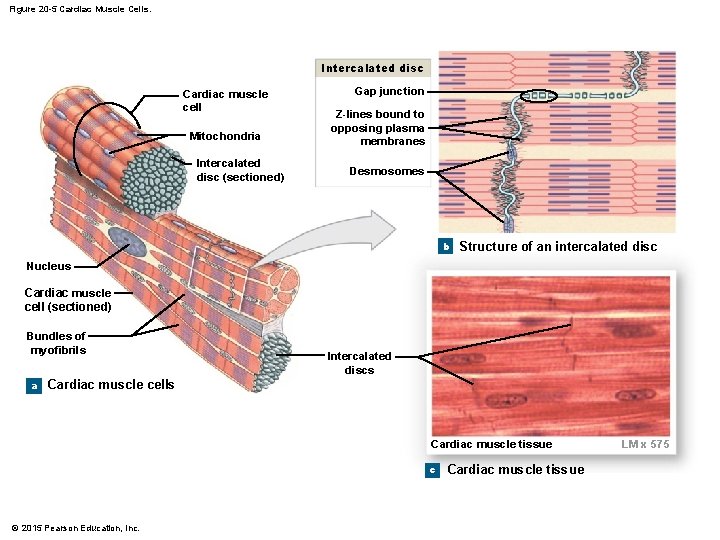
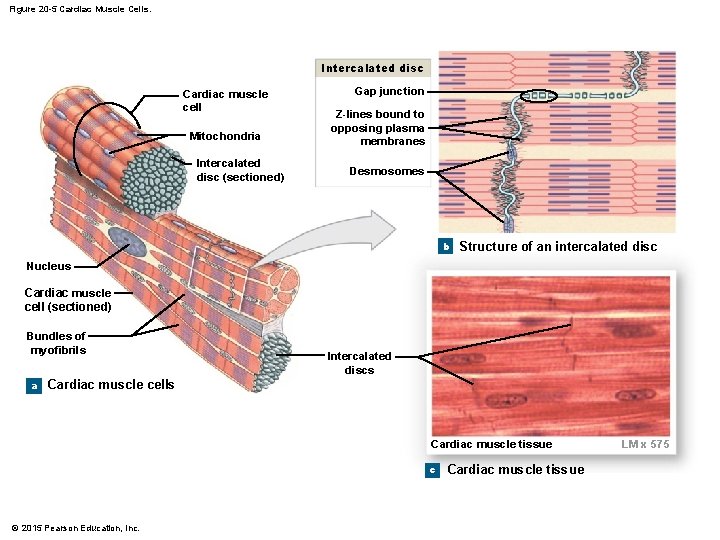
Figure 20 -5 Cardiac Muscle Cells. Intercalated disc Cardiac muscle cell Mitochondria Intercalated disc (sectioned) Gap junction Z-lines bound to opposing plasma membranes Desmosomes b Structure of an intercalated disc Nucleus Cardiac muscle cell (sectioned) Bundles of myofibrils a Intercalated discs Cardiac muscle cells Cardiac muscle tissue c © 2015 Pearson Education, Inc. Cardiac muscle tissue LM x 575
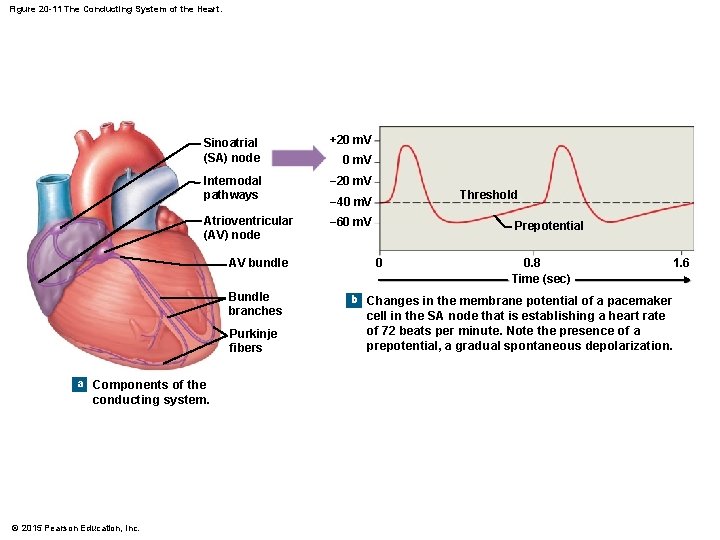
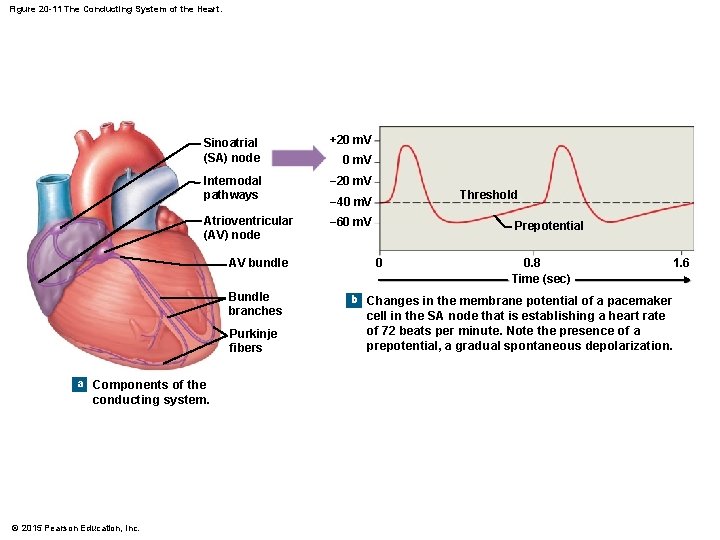
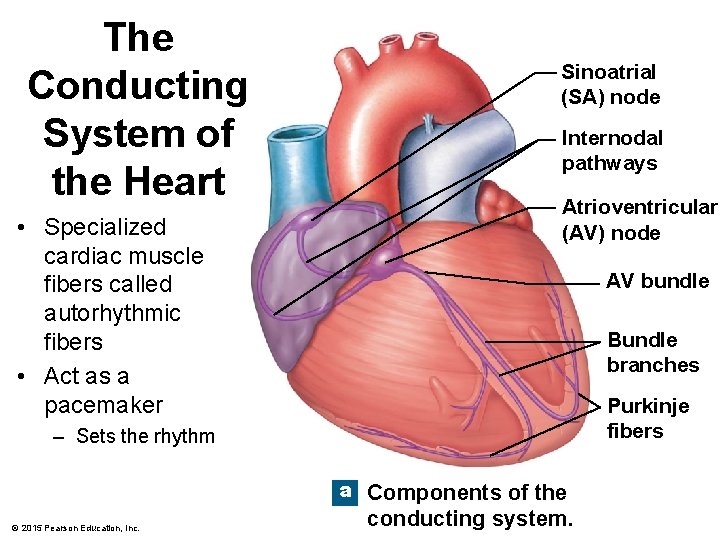
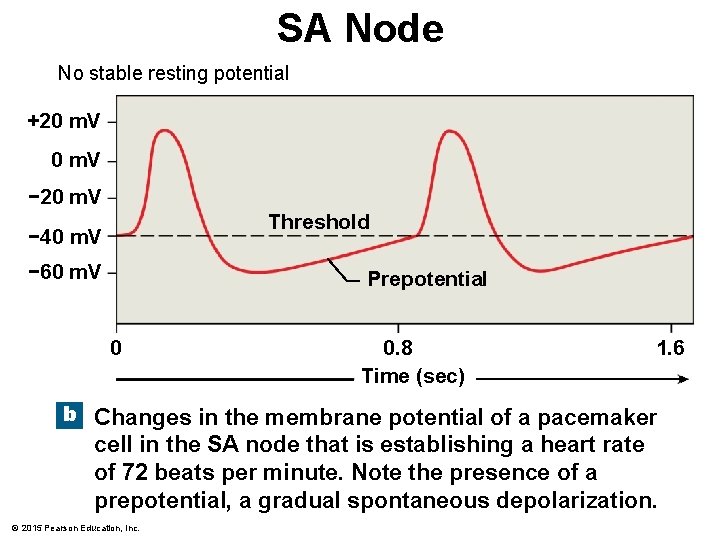
Figure 20 -11 The Conducting System of the Heart. Sinoatrial (SA) node +20 m. V Internodal pathways − 20 m. V Atrioventricular (AV) node − 60 m. V AV bundle Bundle branches Purkinje fibers a Components of the conducting system. © 2015 Pearson Education, Inc. 0 m. V Threshold − 40 m. V Prepotential 0 0. 8 Time (sec) 1. 6 b Changes in the membrane potential of a pacemaker cell in the SA node that is establishing a heart rate of 72 beats per minute. Note the presence of a prepotential, a gradual spontaneous depolarization.
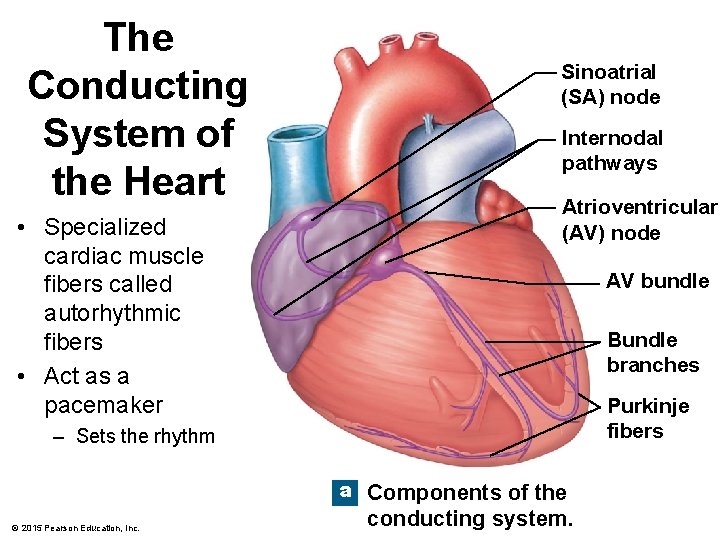
The Conducting System of the Heart • Specialized cardiac muscle fibers called autorhythmic fibers • Act as a pacemaker Sinoatrial (SA) node Internodal pathways Atrioventricular (AV) node AV bundle Bundle branches Purkinje fibers – Sets the rhythm a Components of the © 2015 Pearson Education, Inc. conducting system.
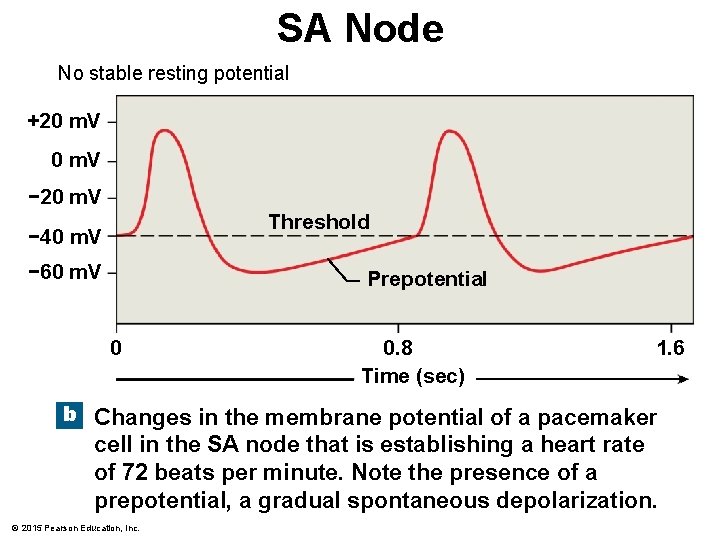
SA Node No stable resting potential +20 m. V − 20 m. V Threshold − 40 m. V − 60 m. V Prepotential 0 0. 8 Time (sec) 1. 6 b Changes in the membrane potential of a pacemaker cell in the SA node that is establishing a heart rate of 72 beats per minute. Note the presence of a prepotential, a gradual spontaneous depolarization. © 2015 Pearson Education, Inc.
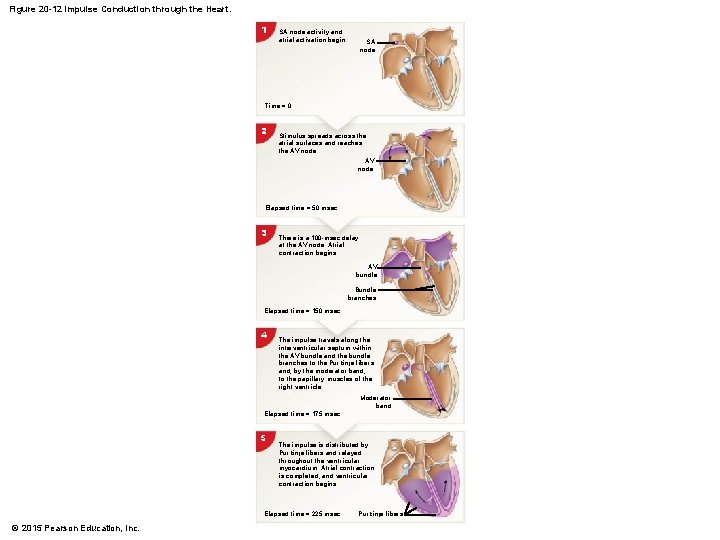
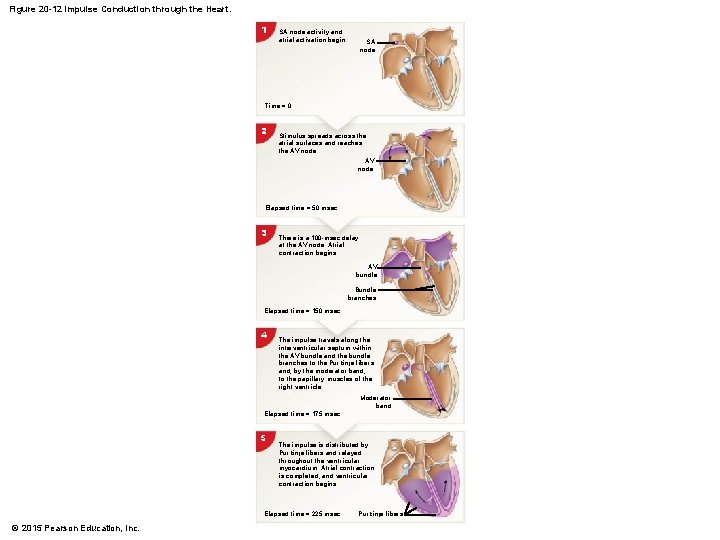
Figure 20 -12 Impulse Conduction through the Heart. 1 SA node activity and atrial activation begin. SA node Time = 0 2 Stimulus spreads across the atrial surfaces and reaches the AV node Elapsed time = 50 msec 3 There is a 100 -msec delay at the AV node. Atrial contraction begins. AV bundle Bundle branches Elapsed time = 150 msec 4 The impulse travels along the interventricular septum within the AV bundle and the bundle branches to the Purkinje fibers and, by the moderator band, to the papillary muscles of the right ventricle. Moderator band Elapsed time = 175 msec 5 The impulse is distributed by Purkinje fibers and relayed throughout the ventricular myocardium. Atrial contraction is completed, and ventricular contraction begins. Elapsed time = 225 msec © 2015 Pearson Education, Inc. Purkinje fibers
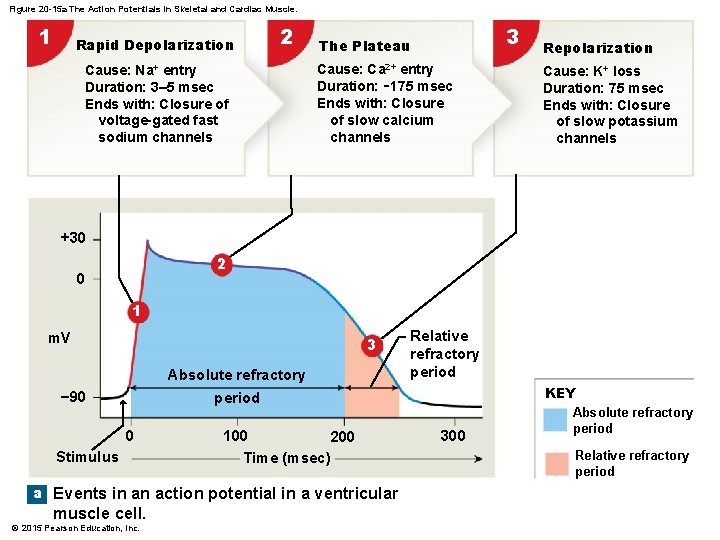
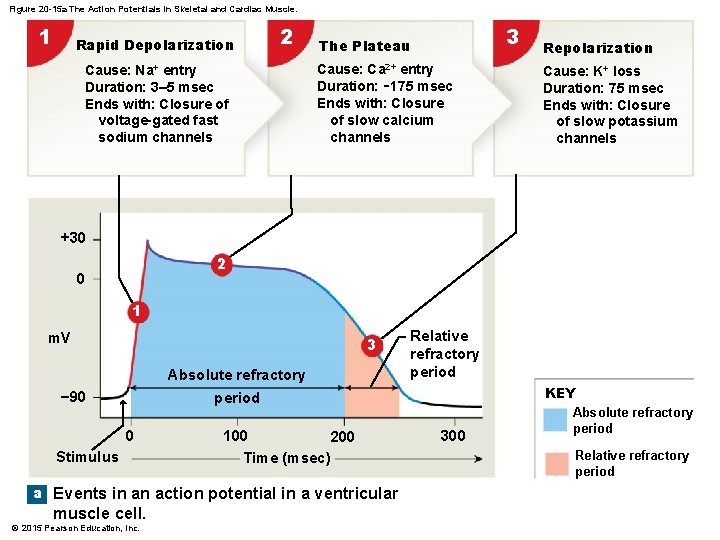
Figure 20 -15 a The Action Potentials in Skeletal and Cardiac Muscle. 1 Rapid Depolarization 2 Cause: Na+ entry Duration: 3– 5 msec Ends with: Closure of voltage-gated fast sodium channels 3 The Plateau Cause: Ca 2+ entry Duration: ∼ 175 msec Ends with: Closure of slow calcium channels Repolarization Cause: K+ loss Duration: 75 msec Ends with: Closure of slow potassium channels +30 2 0 1 m. V 3 Absolute refractory − 90 Relative refractory period KEY period 0 Stimulus 100 200 Time (msec) a Events in an action potential in a ventricular muscle cell. © 2015 Pearson Education, Inc. 300 Absolute refractory period Relative refractory period
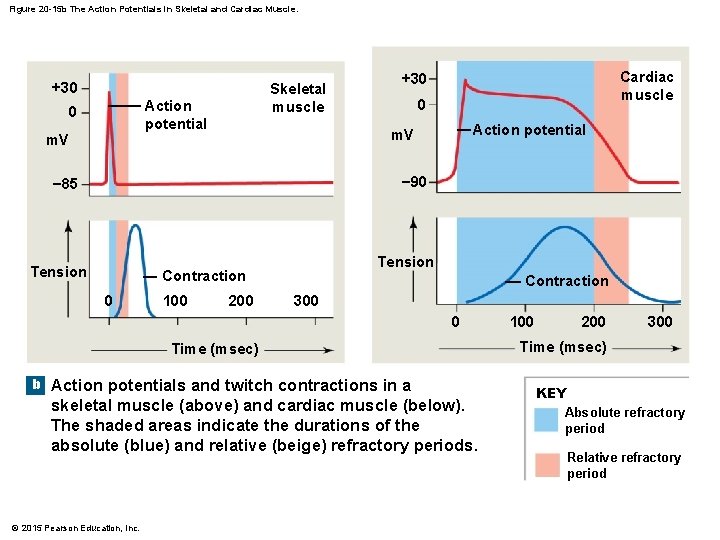
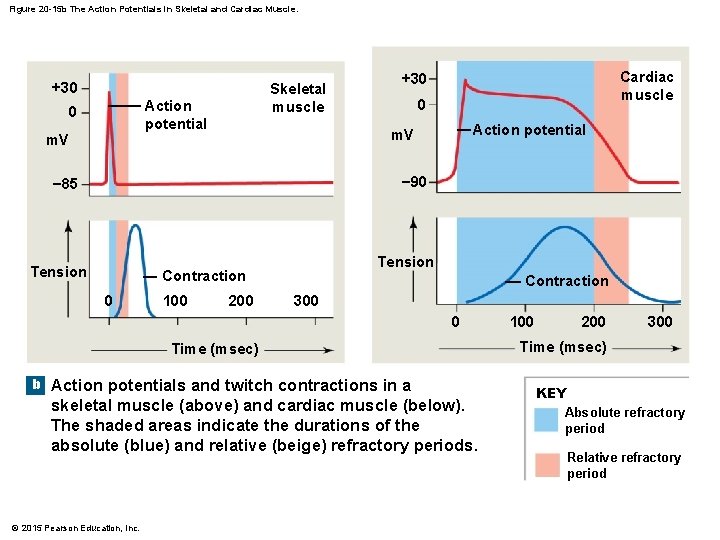
Figure 20 -15 b The Action Potentials in Skeletal and Cardiac Muscle. +30 Skeletal muscle Action potential 0 m. V Cardiac muscle +30 0 Action potential m. V − 90 − 85 Tension Contraction 0 100 200 Contraction 300 0 Time (msec) b Action potentials and twitch contractions in a skeletal muscle (above) and cardiac muscle (below). The shaded areas indicate the durations of the absolute (blue) and relative (beige) refractory periods. © 2015 Pearson Education, Inc. 100 200 300 Time (msec) KEY Absolute refractory period Relative refractory period
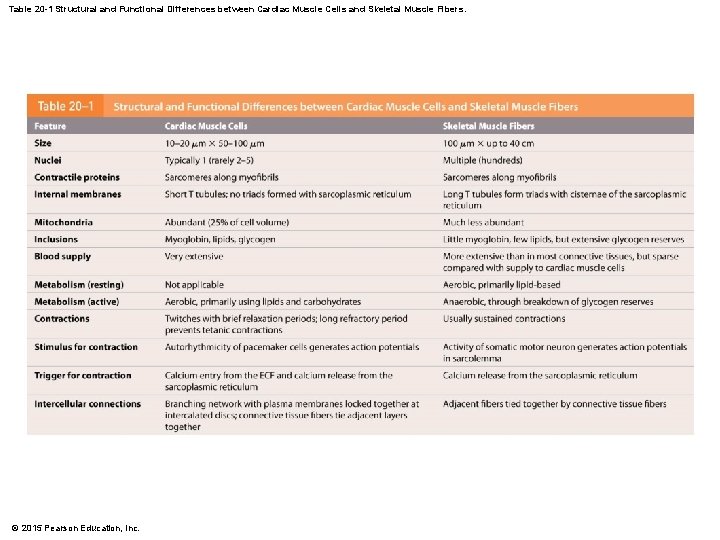
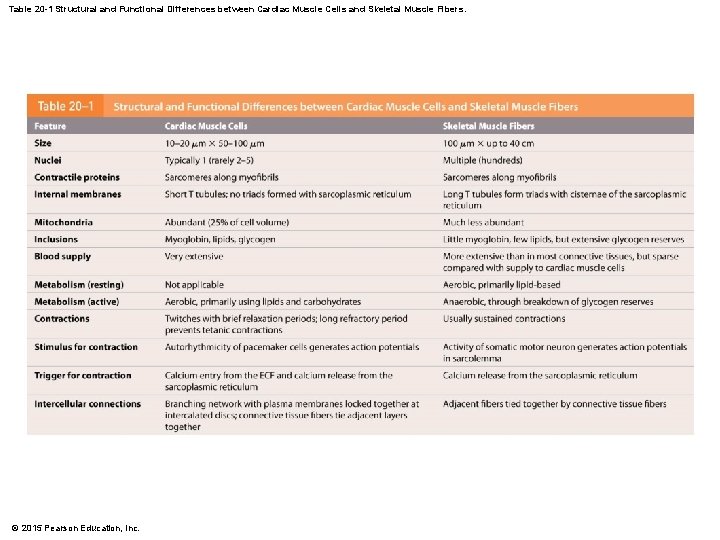
Table 20 -1 Structural and Functional Differences between Cardiac Muscle Cells and Skeletal Muscle Fibers. © 2015 Pearson Education, Inc.
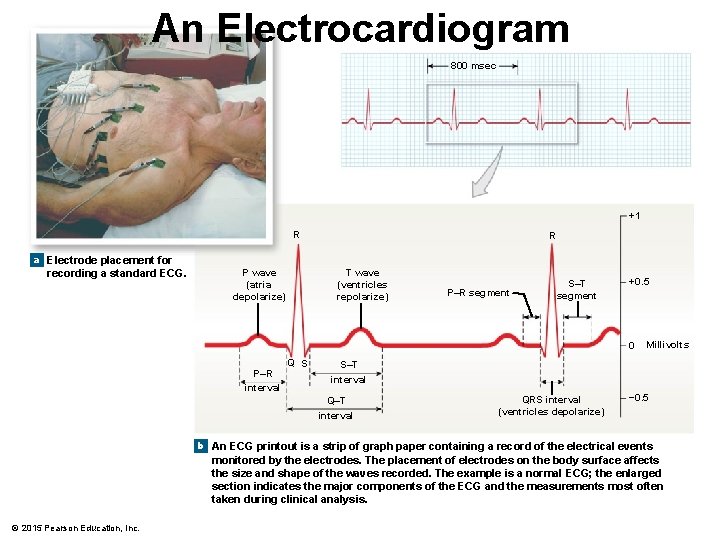
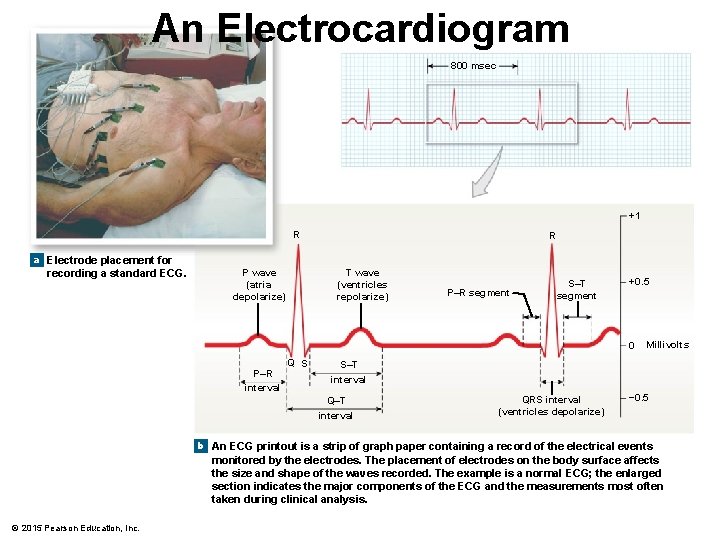
An Electrocardiogram 800 msec +1 R R a Electrode placement for recording a standard ECG. P wave (atria depolarize) T wave (ventricles repolarize) P–R segment S–T segment +0. 5 0 P–R interval Q S Millivolts S–T interval QRS interval (ventricles depolarize) − 0. 5 b An ECG printout is a strip of graph paper containing a record of the electrical events monitored by the electrodes. The placement of electrodes on the body surface affects the size and shape of the waves recorded. The example is a normal ECG; the enlarged section indicates the major components of the ECG and the measurements most often taken during clinical analysis. © 2015 Pearson Education, Inc.
ECG • Compare with normal readings & can determine – If conducting pathway is abnormal – If heart is enlarged – If certain regions of heart are damaged – Cause of chest pain © 2015 Pearson Education, Inc.
ECG Abnormalities • Larger P waves – Enlargement of atrium • Enlarged Q wave – May indicate MI • Enlarged R wave – Indicates enlarged ventricles • Flat T wave – Insufficient O 2 • Elevated T wave – hyperkalemia © 2015 Pearson Education, Inc.
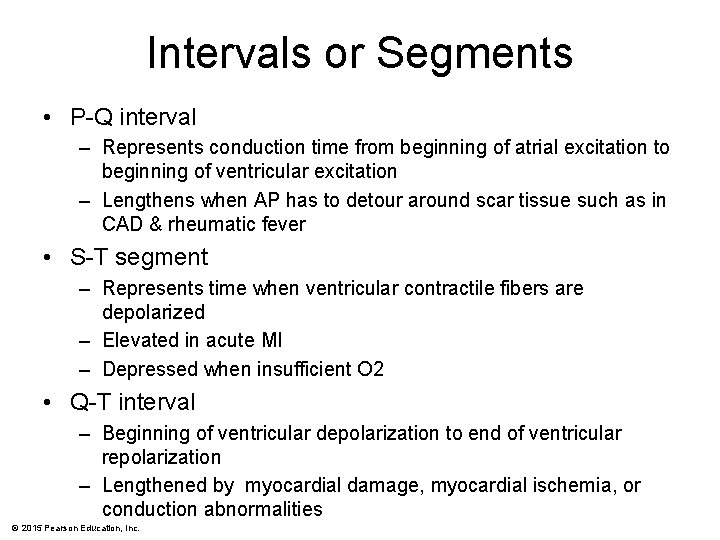
Intervals or Segments • P-Q interval – Represents conduction time from beginning of atrial excitation to beginning of ventricular excitation – Lengthens when AP has to detour around scar tissue such as in CAD & rheumatic fever • S-T segment – Represents time when ventricular contractile fibers are depolarized – Elevated in acute MI – Depressed when insufficient O 2 • Q-T interval – Beginning of ventricular depolarization to end of ventricular repolarization – Lengthened by myocardial damage, myocardial ischemia, or conduction abnormalities © 2015 Pearson Education, Inc.
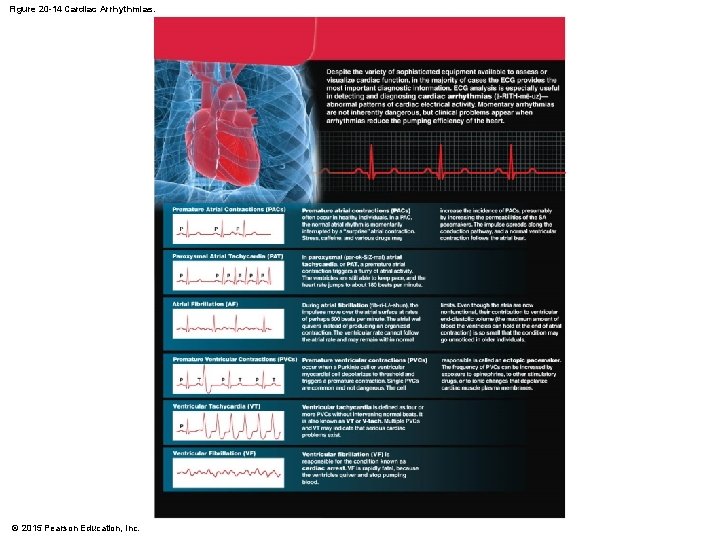
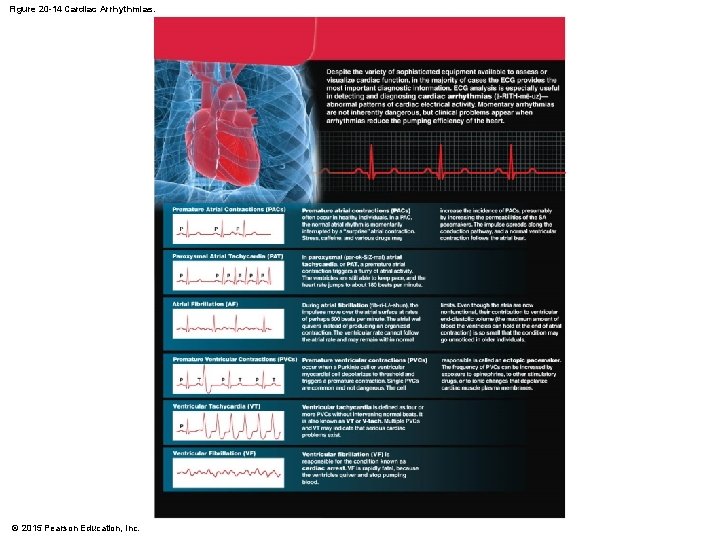
Figure 20 -14 Cardiac Arrhythmias. © 2015 Pearson Education, Inc.
• Systole – Phase of contraction • Diastole – Phase of relaxation © 2015 Pearson Education, Inc.
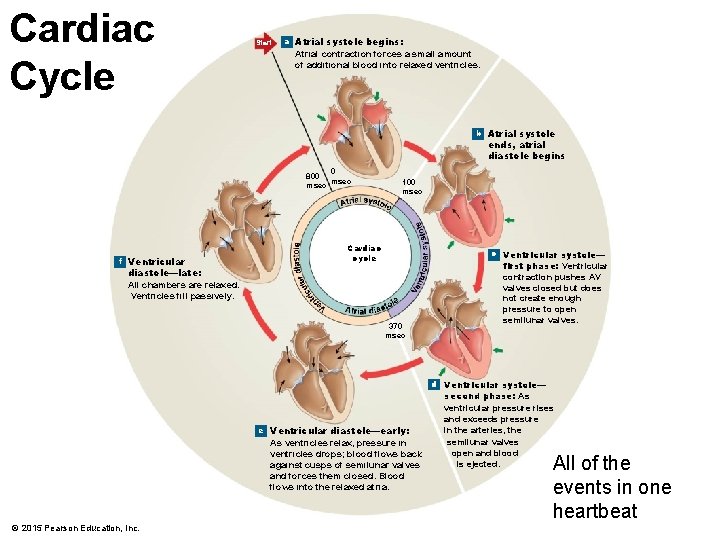
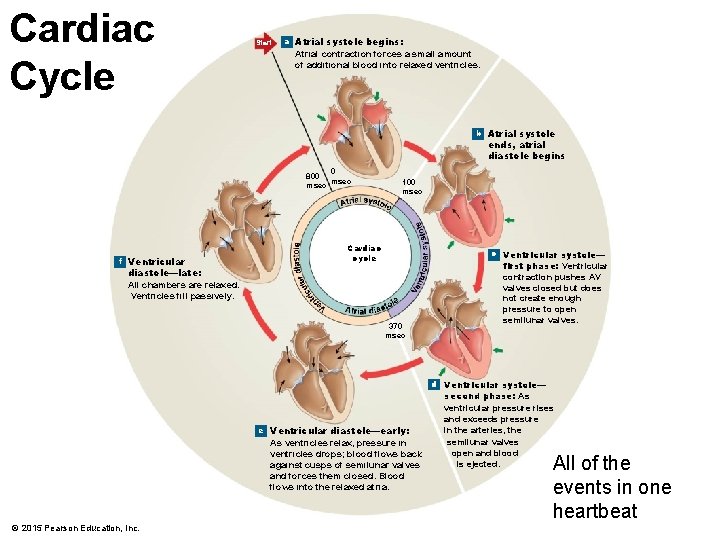
Cardiac Cycle Start a Atrial systole begins: Atrial contraction forces a small amount of additional blood into relaxed ventricles. b Atrial systole ends, atrial diastole begins 0 800 msec f Ventricular 100 msec Cardiac cycle c Ventricular systole— diastole—late: All chambers are relaxed. Ventricles fill passively. 370 msec first phase: Ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves. d Ventricular systole— e Ventricular diastole—early: As ventricles relax, pressure in ventricles drops; blood flows back against cusps of semilunar valves and forces them closed. Blood flows into the relaxed atria. © 2015 Pearson Education, Inc. second phase: As ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected. All of the events in one heartbeat
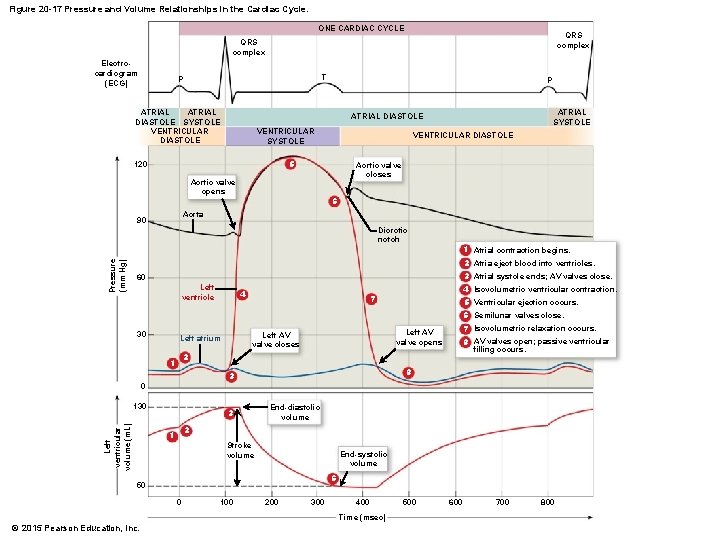
Atrial Systole • Atria are contracting while ventricles are relaxed • Atrial depolarization (P wave) causes atril contraction • Pressure inside increases on blood forcing blood through AV valves • End of atrial systole is also end of ventricular diastole – Volume of blood in ventricles at this time known as end-diastolic volume (EDV) © 2015 Pearson Education, Inc.
Ventricular Systole • Ventricles are contracting while atria are relaxing • As ventricles begin to contract, pressure rises causing AV valves to shut • Isovolumetric contraction – all 4 valves briefly closed • Pressure rises sharply causing semilunar valves to open • Ventricular ejection – Volume remaining in ventricle after ejection is endsystolic volume (ESV) – Stroke volume is volume ejected & is equal to EDV ESV © 2015 Pearson Education, Inc.
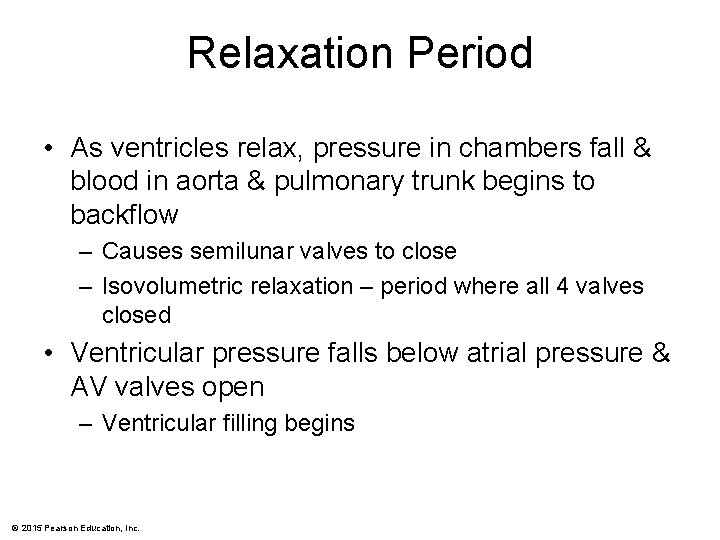
Relaxation Period • As ventricles relax, pressure in chambers fall & blood in aorta & pulmonary trunk begins to backflow – Causes semilunar valves to close – Isovolumetric relaxation – period where all 4 valves closed • Ventricular pressure falls below atrial pressure & AV valves open – Ventricular filling begins © 2015 Pearson Education, Inc.
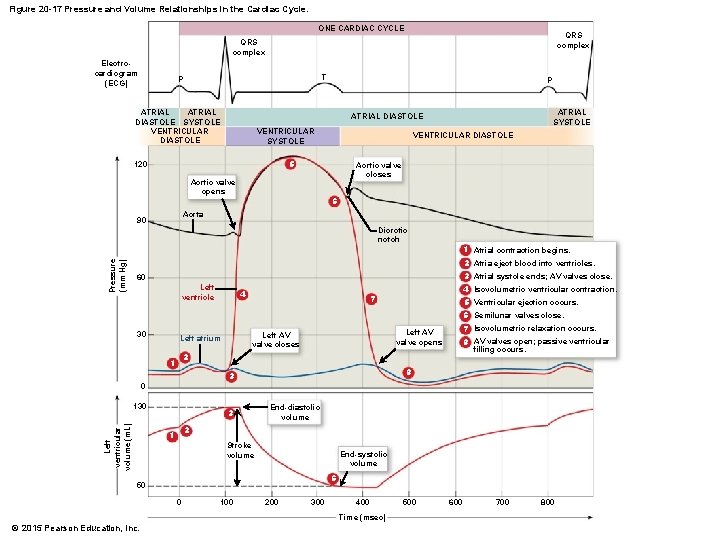
Figure 20 -17 Pressure and Volume Relationships in the Cardiac Cycle. ONE CARDIAC CYCLE QRS complex Electrocardiogram (ECG) T P ATRIAL DIASTOLE SYSTOLE VENTRICULAR DIASTOLE P ATRIAL SYSTOLE ATRIAL DIASTOLE VENTRICULAR SYSTOLE VENTRICULAR DIASTOLE 5 120 Aortic valve closes Aortic valve opens 6 Aorta 90 Pressure (mm Hg) Dicrotic notch 1 Atrial contraction begins. 2 Atria eject blood into ventricles. 3 Atrial systole ends; AV valves close. 60 Left ventricle 4 4 Isovolumetric ventricular contraction. 7 5 Ventricular ejection occurs. 6 Semilunar valves close. 30 7 Isovolumetric relaxation occurs. 8 AV valves open; passive ventricular filling occurs. Left AV valve opens Left AV valve closes Left atrium 2 1 8 3 0 Left ventricular volume (m. L) 130 3 End-diastolic volume 2 1 Stroke volume End-systolic volume 6 50 0 100 200 300 400 Time (msec) © 2015 Pearson Education, Inc. 500 600 700 800
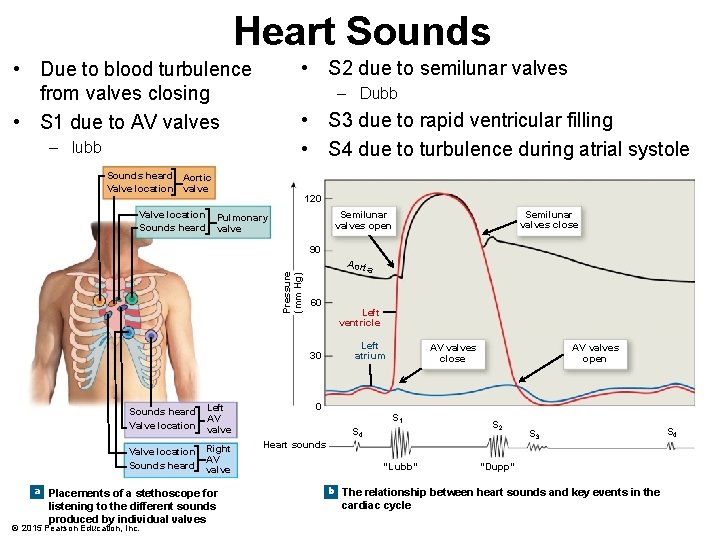
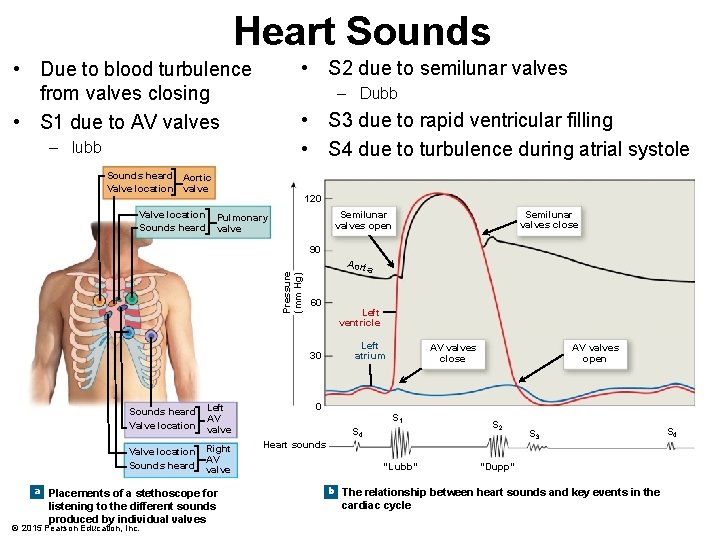
Heart Sounds • S 2 due to semilunar valves • Due to blood turbulence from valves closing • S 1 due to AV valves – Dubb • S 3 due to rapid ventricular filling • S 4 due to turbulence during atrial systole – lubb Sounds heard Aortic Valve location valve Valve location Sounds heard 120 Semilunar valves close Semilunar valves open Pulmonary valve Pressure (mm Hg) 90 Aorta 60 30 Sounds heard Valve location Left AV valve Valve location Sounds heard Right AV valve a Placements of a stethoscope for listening to the different sounds produced by individual valves © 2015 Pearson Education, Inc. Left ventricle Left atrium AV valves close AV valves open 0 S 1 S 4 S 2 Heart sounds “Lubb” S 3 “Dupp” b The relationship between heart sounds and key events in the cardiac cycle S 4
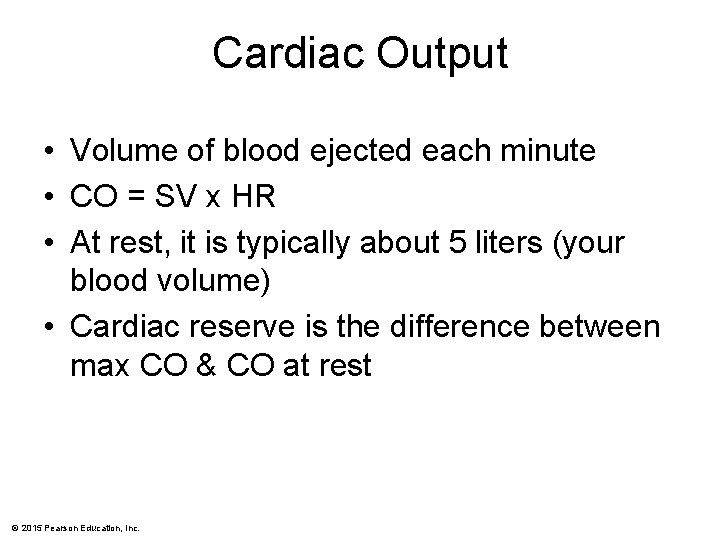
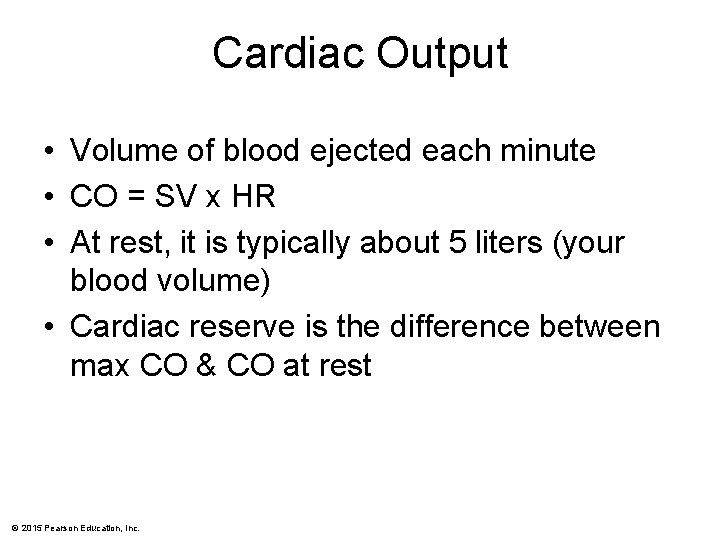
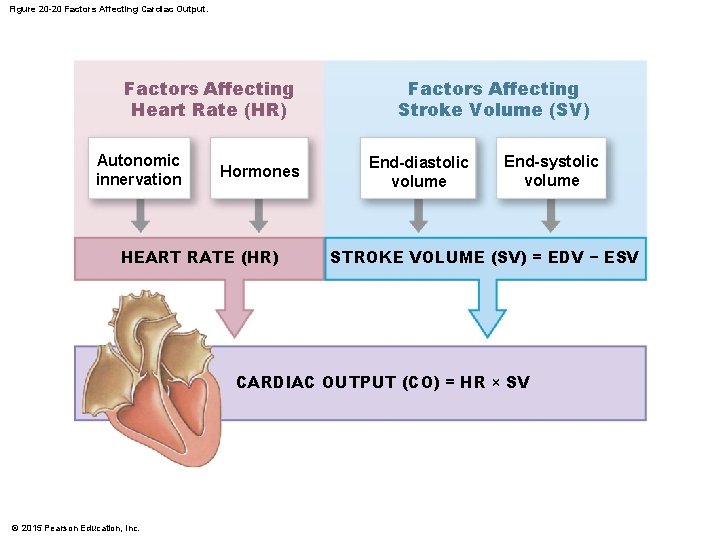
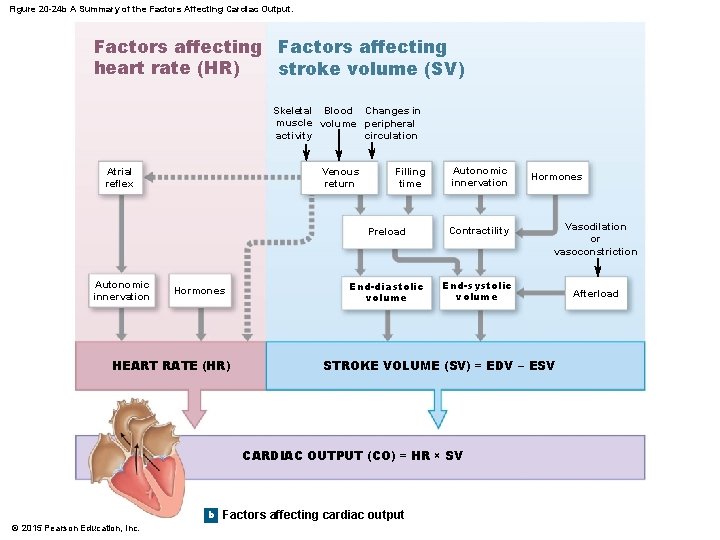
Cardiac Output • Volume of blood ejected each minute • CO = SV x HR • At rest, it is typically about 5 liters (your blood volume) • Cardiac reserve is the difference between max CO & CO at rest © 2015 Pearson Education, Inc.
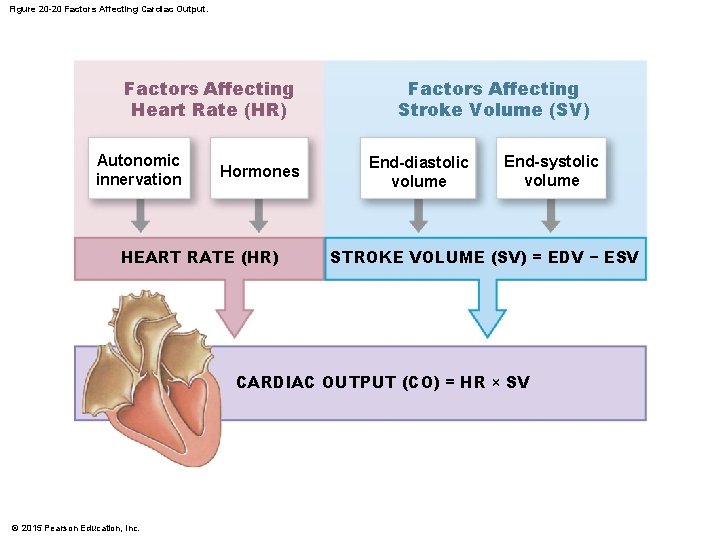
Figure 20 -20 Factors Affecting Cardiac Output. Factors Affecting Heart Rate (HR) Autonomic innervation Hormones HEART RATE (HR) Factors Affecting Stroke Volume (SV) End-diastolic volume End-systolic volume STROKE VOLUME (SV) = EDV − ESV CARDIAC OUTPUT (CO) = HR × SV © 2015 Pearson Education, Inc.
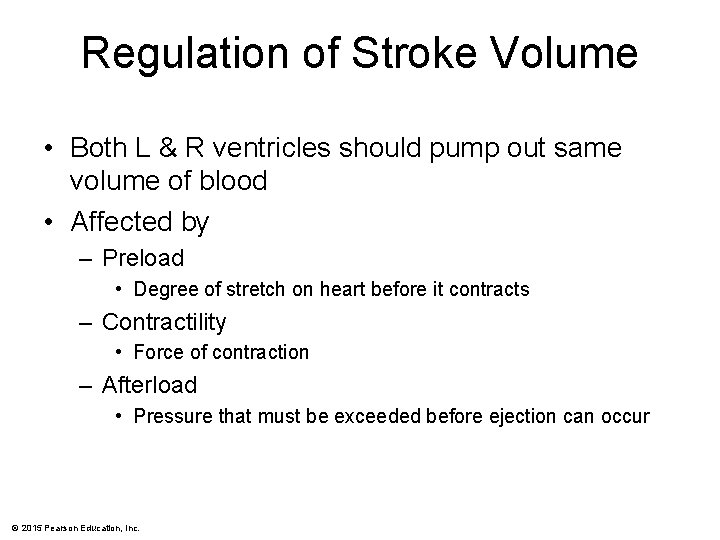
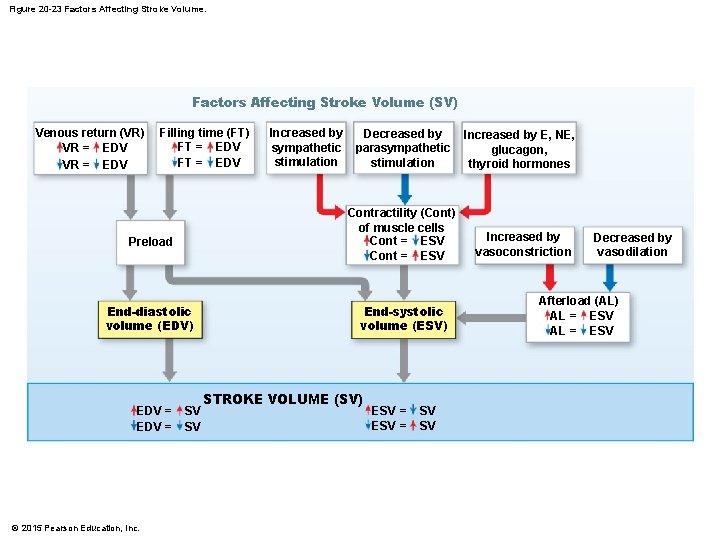
Regulation of Stroke Volume • Both L & R ventricles should pump out same volume of blood • Affected by – Preload • Degree of stretch on heart before it contracts – Contractility • Force of contraction – Afterload • Pressure that must be exceeded before ejection can occur © 2015 Pearson Education, Inc.
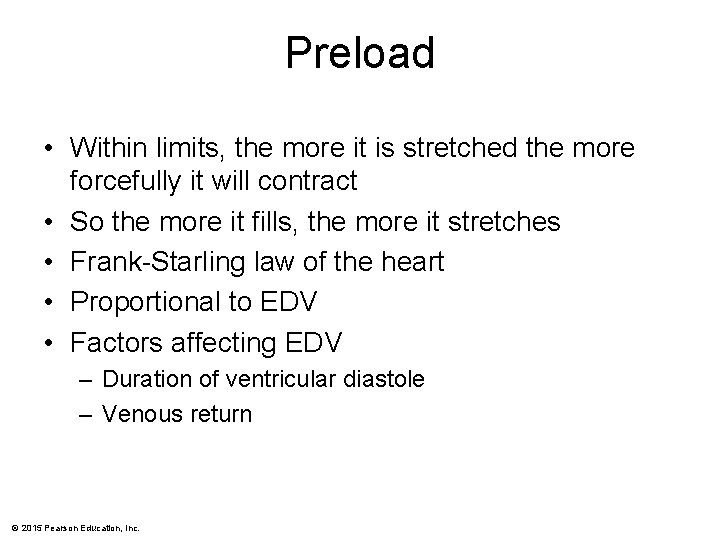
Preload • Within limits, the more it is stretched the more forcefully it will contract • So the more it fills, the more it stretches • Frank-Starling law of the heart • Proportional to EDV • Factors affecting EDV – Duration of ventricular diastole – Venous return © 2015 Pearson Education, Inc.
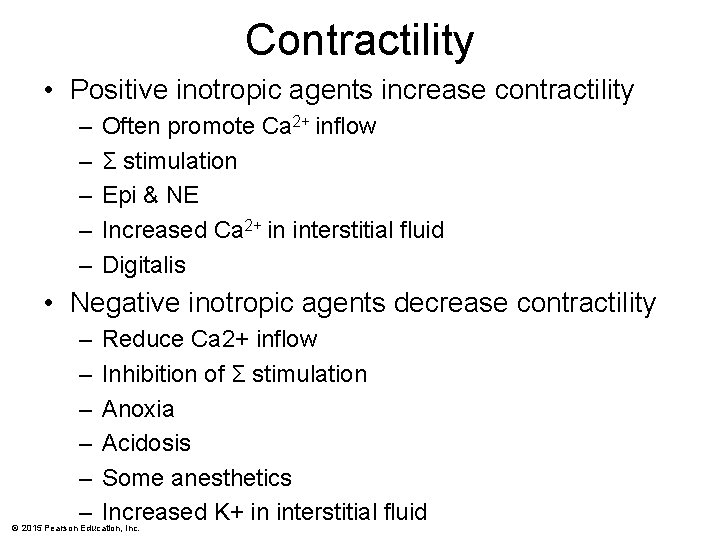
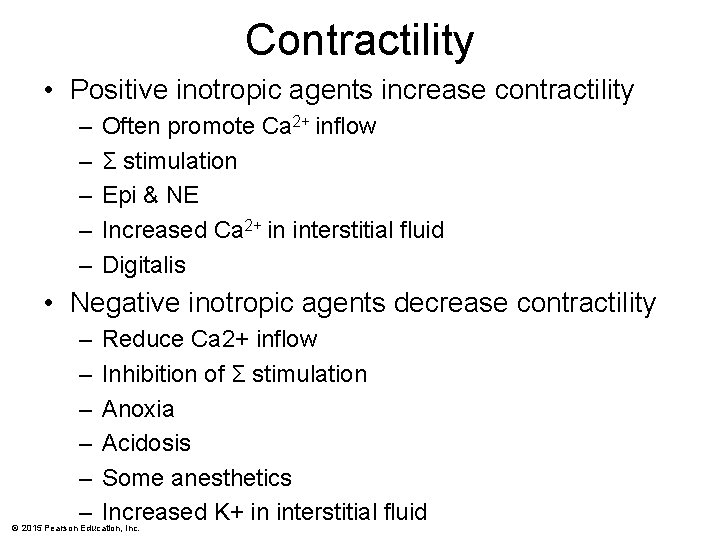
Contractility • Positive inotropic agents increase contractility – – – Often promote Ca 2+ inflow Σ stimulation Epi & NE Increased Ca 2+ in interstitial fluid Digitalis • Negative inotropic agents decrease contractility – – – Reduce Ca 2+ inflow Inhibition of Σ stimulation Anoxia Acidosis Some anesthetics Increased K+ in interstitial fluid © 2015 Pearson Education, Inc.
Afterload • Increased afterload causes SV to decrease • Increased by – HTN – Narrowing of arteries by atherosclerosis © 2015 Pearson Education, Inc.
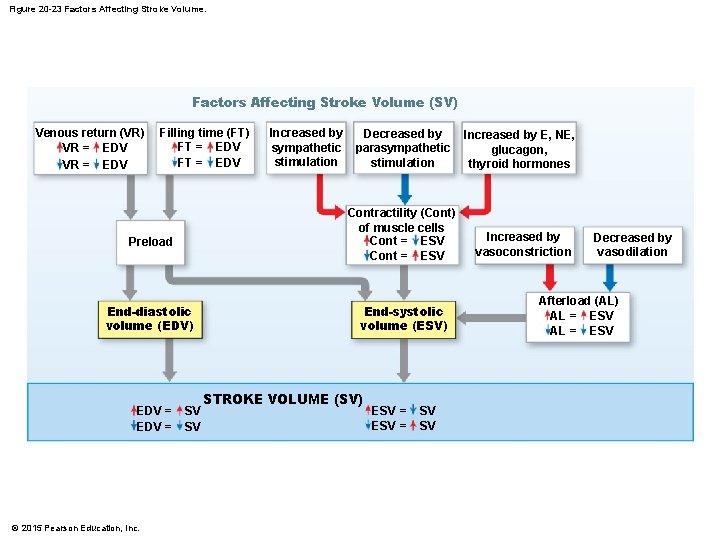
Figure 20 -23 Factors Affecting Stroke Volume (SV) Venous return (VR) VR = EDV Filling time (FT) FT = EDV End-diastolic volume (EDV) © 2015 Pearson Education, Inc. Decreased by parasympathetic stimulation Contractility (Cont) of muscle cells Cont = ESV Preload EDV = Increased by sympathetic stimulation SV SV End-systolic volume (ESV) STROKE VOLUME (SV) ESV = SV SV Increased by E, NE, glucagon, thyroid hormones Increased by vasoconstriction Decreased by vasodilation Afterload (AL) AL = ESV
Regulation of Heart Rate • ANS • Hormones © 2015 Pearson Education, Inc.
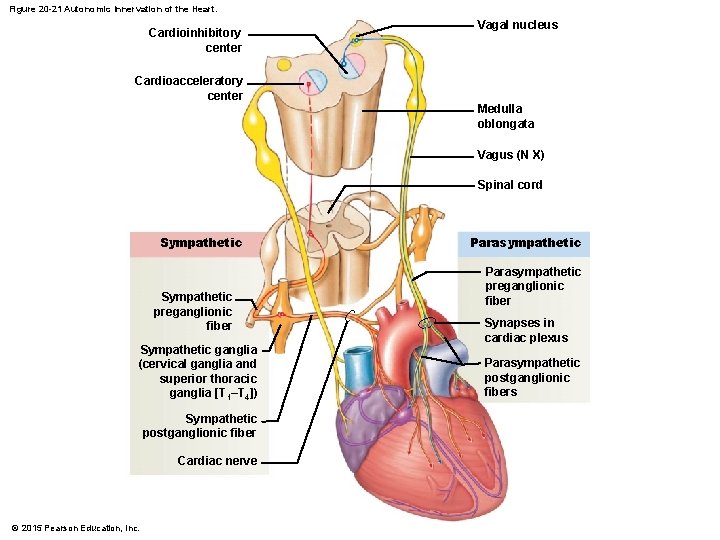
ANS • Originates in cardiovascular center • Input provided by proprioceptors, chemoreceptors, & baroreceptors • Σ increases HR & force of contraction • PΣ decreases HR © 2015 Pearson Education, Inc.
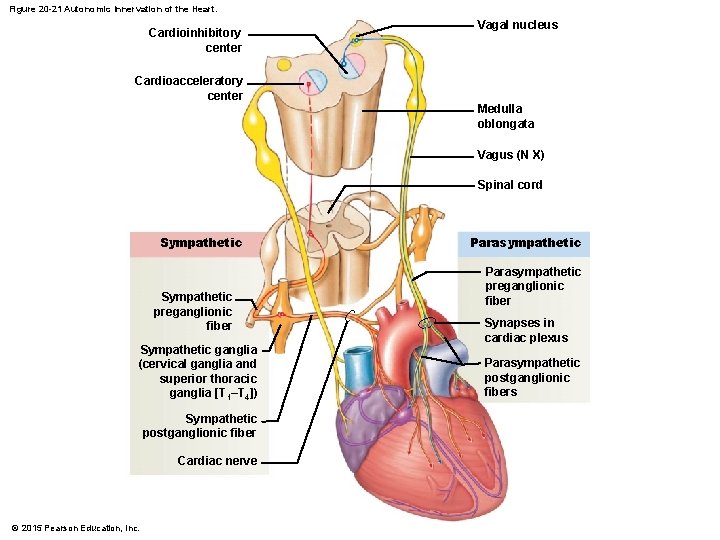
Figure 20 -21 Autonomic Innervation of the Heart. Cardioinhibitory center Vagal nucleus Cardioacceleratory center Medulla oblongata Vagus (N X) Spinal cord Sympathetic preganglionic fiber Sympathetic ganglia (cervical ganglia and superior thoracic ganglia [T 1–T 4]) Sympathetic postganglionic fiber Cardiac nerve © 2015 Pearson Education, Inc. Parasympathetic preganglionic fiber Synapses in cardiac plexus Parasympathetic postganglionic fibers
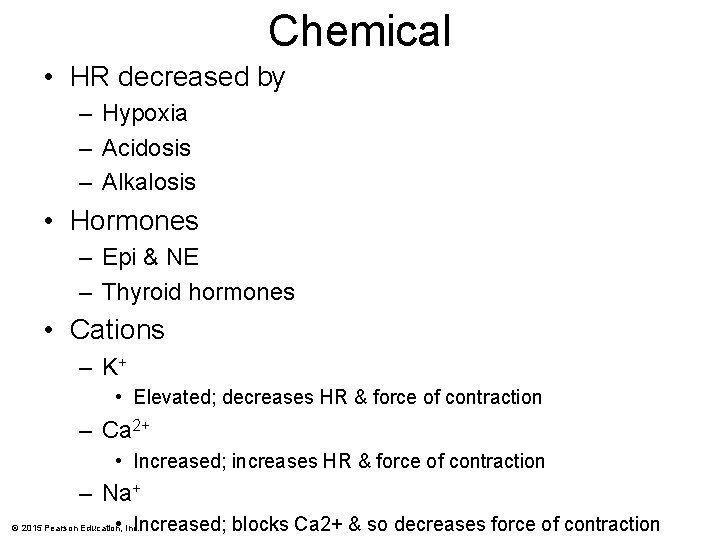
Chemical • HR decreased by – Hypoxia – Acidosis – Alkalosis • Hormones – Epi & NE – Thyroid hormones • Cations – K+ • Elevated; decreases HR & force of contraction – Ca 2+ • Increased; increases HR & force of contraction – Na+ • Increased; blocks Ca 2+ & so decreases force of contraction © 2015 Pearson Education, Inc.
Others • Also influenced by – Age • Newborn higher – Gender • Females higher – Physical fitness • lowers – Body temp • increases © 2015 Pearson Education, Inc.
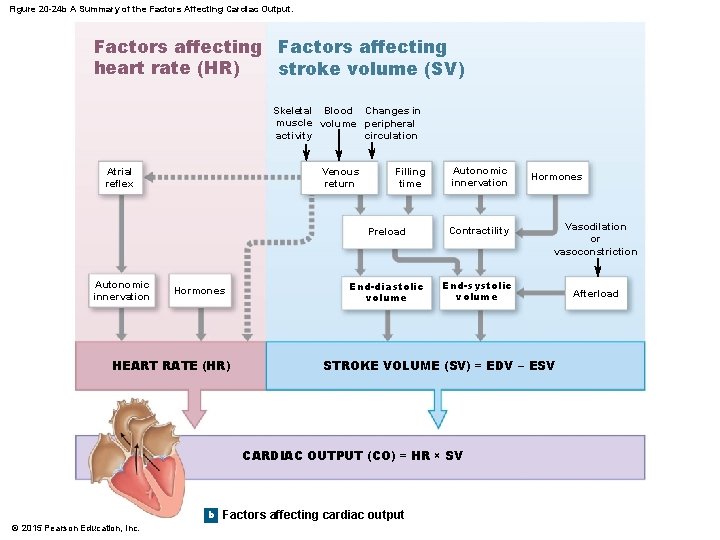
Figure 20 -24 b A Summary of the Factors Affecting Cardiac Output. Factors affecting heart rate (HR) stroke volume (SV) Skeletal Blood Changes in muscle volume peripheral activity circulation Atrial reflex Autonomic innervation Venous return Hormones HEART RATE (HR) Filling time Autonomic innervation Preload Contractility End-diastolic volume End-systolic volume b Vasodilation or vasoconstriction STROKE VOLUME (SV) = EDV − ESV CARDIAC OUTPUT (CO) = HR × SV © 2015 Pearson Education, Inc. Hormones Factors affecting cardiac output Afterload