Chapter 2 Reproductive Anatomy and Physiology Copyright 2012
- Slides: 55
Chapter 2 Reproductive Anatomy and Physiology Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 1
Puberty and the Reproductive Tract Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 2
Objectives Define key terms listed. Discuss puberty in the developing male and female. Identify the female external reproductive organs. Describe the female internal reproductive organs. Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 3
Objectives (cont. ) Describe the influence of hormones on the female reproductive process. Explain the menstrual and ovarian cycles. Discuss the functions of the uterus. Identify the bones that make up the pelvis. Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 4
Human Reproduction Requires that the male and female reproductive systems work together to produce a new human life Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 5
Puberty Before onset, male and female children appear similar except for genitalia Process involves changes in the whole body and psyche Reproductive system matures and becomes capable of reproduction Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 6
Puberty (cont. ) Begins when secondary sex characteristics appear Ends when Mature sperm are formed in males Ø Regular menstrual cycles begin in females Ø Celebrated in many cultures as a rite of passage into adulthood Other cultures lack this ritual Ø Has led to confusion for some adolescents in many industrialized nations Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 7
The Male Hormonal changes begin between 10 and 16 years of age Ø Testosterone levels become constant, not cyclic Outward changes Penis and testes increase in size Ø Adolescent grows taller, more muscular Ø Secondary sex characteristics • Pubic and facial hair begin to appear • Voice deepens Ø Nocturnal emissions occur without sexual stimulation; usually do not contain sperm Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 8
The Female Development of breasts occurs first First menstrual period (menarche) occurs approximately 2 to 2½ years later (around 11 to 15 years of age) Growth spurt ends earlier than the male’s Hips broaden as pelvis assumes wide basin shape Pubic and axillary hair appear Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 9
Female Reproductive System Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 10
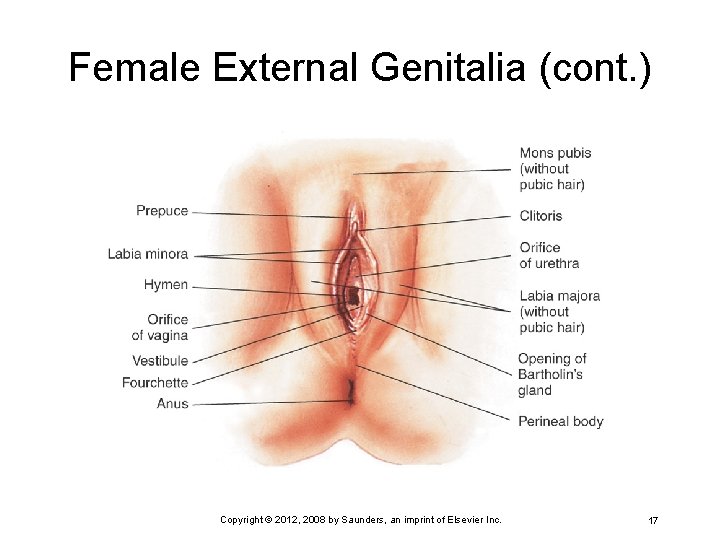
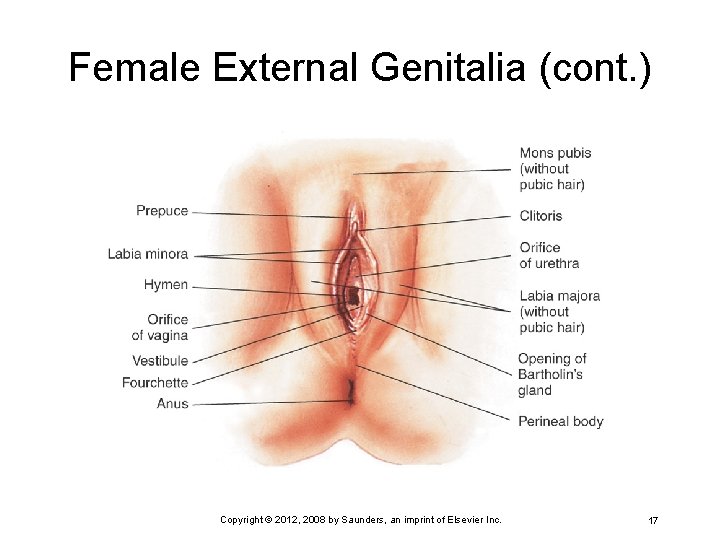
Female External Genitalia Collectively called the vulva Ø Includes mons pubis, labia majora, labia minora, clitoris, vaginal vestibule, fourchette, and perineum Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 11
Female External Genitalia (cont. ) Mons pubis Upper margins of symphysis pubis Ø Shaped like an inverted triangle Ø Pad of fatty tissue covered by coarse skin and pubic hair Ø Protects symphysis pubis Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 12
Female External Genitalia (cont. ) Labia majora Two folds of fatty tissue on each side of vaginal vestibule Ø Covered with pubic hair on outer aspect Ø Smooth and moist on inner aspect Ø Many small glands in this area Ø Labia minora Ø Two thin, soft folds of erectile tissue • Secretions from sebaceous glands Bactericidal secretions Lubricate and protect the skin of the vulva Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 13
Female External Genitalia (cont. ) Fourchette Fold of tissue just below vagina Ø Known as obstetrical perineum Ø Clitoris Erectile body Ø Most sensitive part of female genitalia, produces smegma (a cheeselike secretion of sebaceous glands in the area) Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 14
Female External Genitalia (cont. ) Vaginal vestibule Urethral meatus: exit for urine Ø Skene’s ducts: lubricate urethra and vaginal orifice Ø Ducts of Bartholin’s glands: secrete yellow mucus that lubricates introitus during sexual arousal; not normally visible Ø Vaginal introitus: divides external and internal genitalia Ø Hymen: thin elastic membrane that closes vagina from vestibule Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 15
Female External Genitalia (cont. ) Perineum Strong muscular area between vaginal opening and anus Ø Allows stretching for birth Ø Site of episiotomy during the delivery of a fetus Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 16
Female External Genitalia (cont. ) Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 17
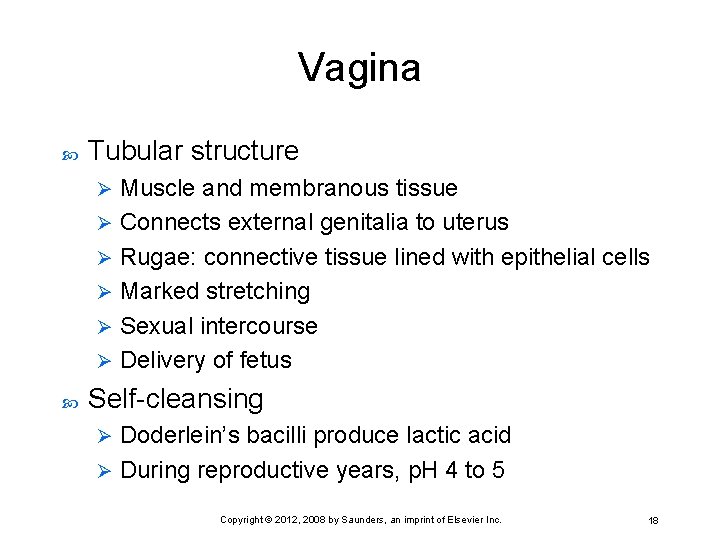
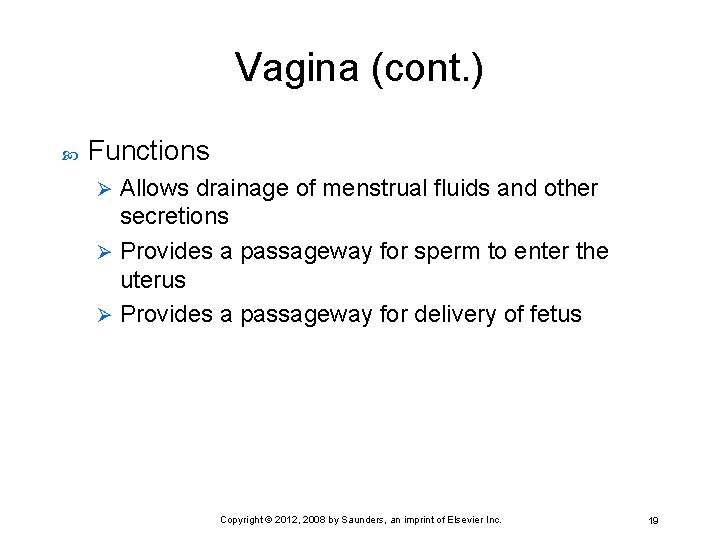
Vagina Tubular structure Muscle and membranous tissue Ø Connects external genitalia to uterus Ø Rugae: connective tissue lined with epithelial cells Ø Marked stretching Ø Sexual intercourse Ø Delivery of fetus Ø Self-cleansing Doderlein’s bacilli produce lactic acid Ø During reproductive years, p. H 4 to 5 Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 18
Vagina (cont. ) Functions Allows drainage of menstrual fluids and other secretions Ø Provides a passageway for sperm to enter the uterus Ø Provides a passageway for delivery of fetus Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 19
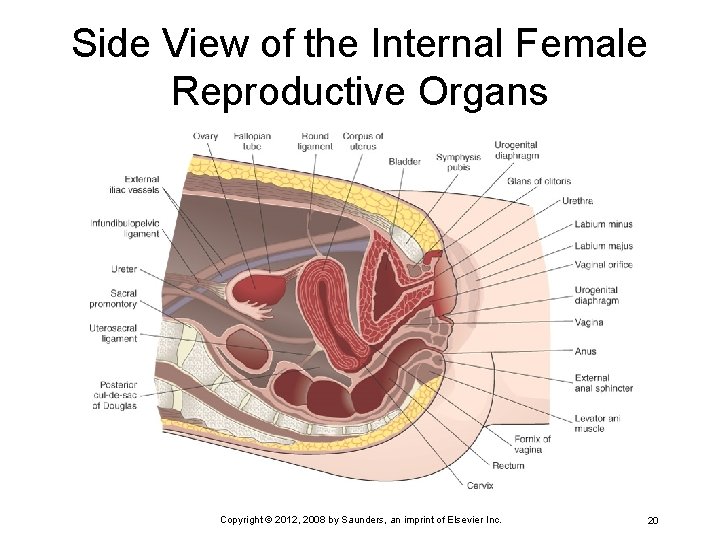
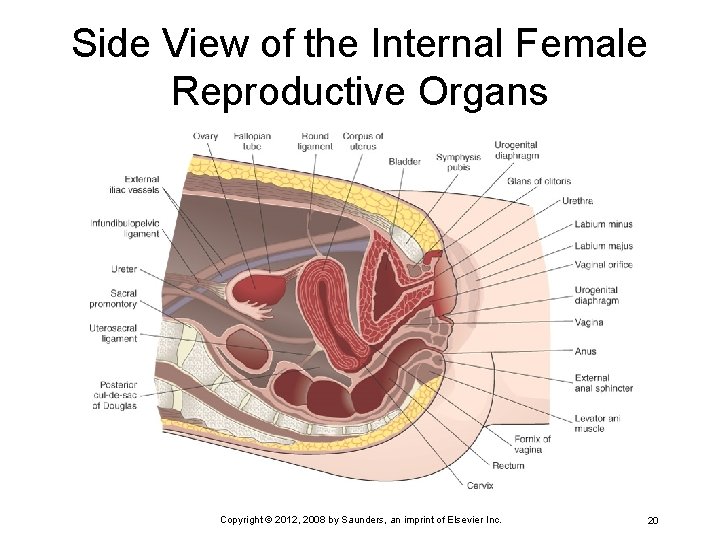
Side View of the Internal Female Reproductive Organs Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 20
Uterus Hollow muscular organ Implanted fertilized ovum develops into an embryo Ø Fetus develops Ø Lies between urinary bladder and rectum, above vagina Supported by the following ligaments Broad Ø Round Ø Cardinal Ø Uterosacral Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 21
Uterus (cont. ) Autonomic nerve supply (not under voluntary or conscious control Divided into three parts Fundus Ø Corpus Ø Cervix Ø Fundus and corpus Both governed by cyclic hormonal changes Ø Three distinct layers: perimetrium, myometrium, endometrium Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 22
Cervix Consists of a cervical canal with an internal opening near uterine corpus (internal os) Ø Opening into vagina (external os) Ø Mucosal lining has four functions Lubricates vagina Ø Acts as a bacteriostatic agent Ø Provides alkaline environment to shelter deposited sperm from acidic environment Ø Produces a mucous plug in cervical canal during pregnancy Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 23
Function of the Uterus Menstruation Ø Sloughs off endometrium Pregnancy Supports fetus Ø Allows for fetal growth Ø Labor and birth Ø Muscles contact, cervix dilates to expel fetus Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 24
Fallopian Tubes Four sections Interstitial Ø Isthmus Ø Ampulla Ø Infundibulum Ø Fingerlike projections called fimbriae capture the ovum (egg) as it is released from the ovary Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 25
Fallopian Tubes (cont. ) Four functions Passageway for sperm to meet the ovum Ø Site of fertilization Ø Safe, nourishing environment for the ovum or zygote (fertilized ovum) Ø Means of transporting ovum or zygote to the corpus of the uterus Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 26
Ovaries Almond-shaped Size of a walnut Held in place by ovarian and uterine ligaments At birth, every female has all the ova that she will have throughout her reproductive years (around 2 million) By adulthood, only a few thousand remain About 400 mature enough to be fertilized Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 27
Ovaries (cont. ) Estrogen Secreted by the ovary Ø Stimulates development of secondary sex characteristics Ø Progesterone Ø Prepares and maintains the uterine lining for implantation of the ovum Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 28
Ovaries (cont. ) By climacteric (menopause), the ovaries no longer respond to hormonal stimulation to mature Two functions Development, maturation, and later expulsion of an ovum during each reproductive cycle Ø Production of hormones • Mainly estrogen and progesterone Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 29
The Female Pelvis Supports and protects pelvic contents Supports and distributes body weight Forms the birth passageway Made up of four bones Two innominate (hip bones) Ø Sacrum Ø Coccyx Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 30
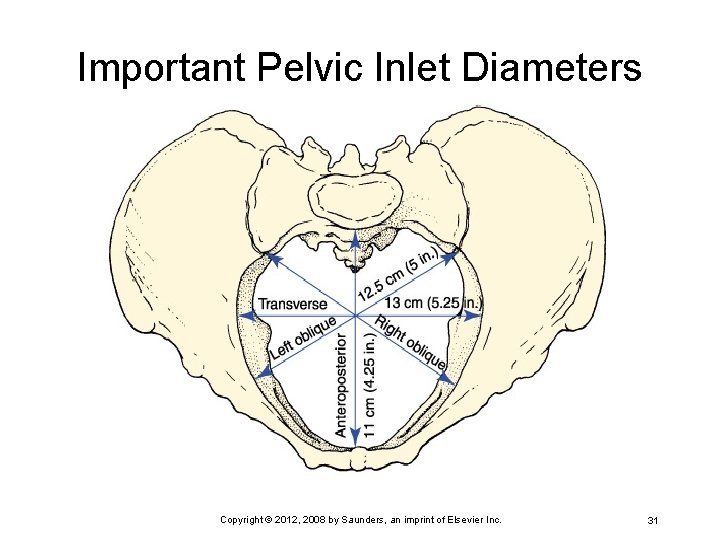
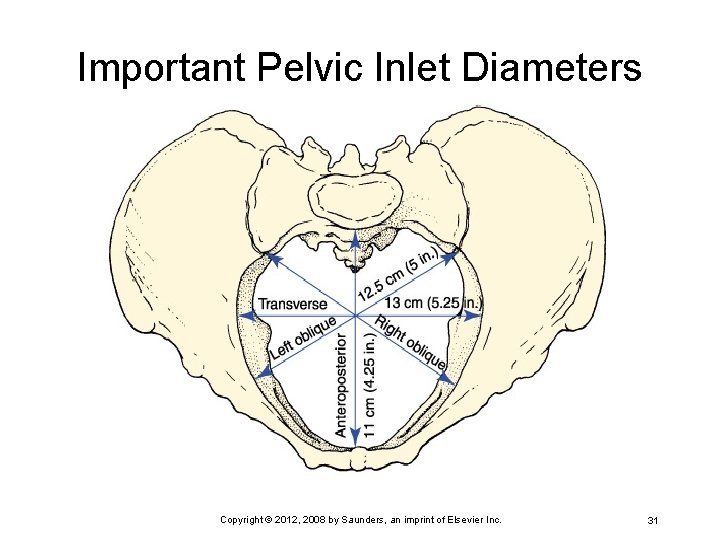
Important Pelvic Inlet Diameters Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 31
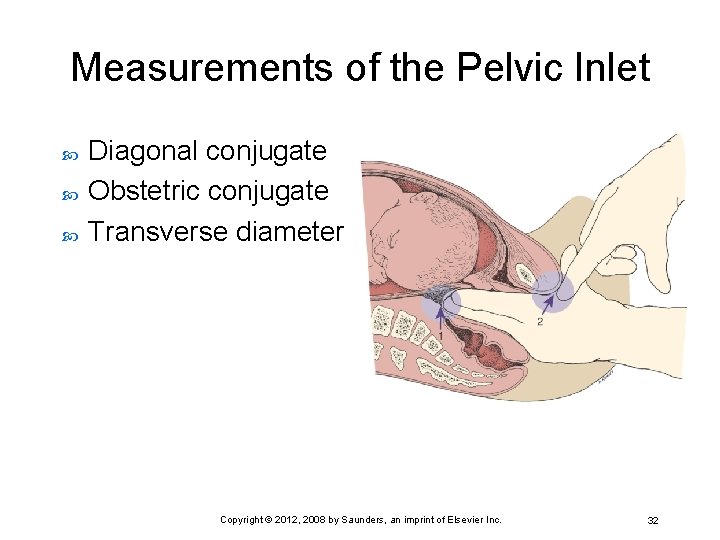
Measurements of the Pelvic Inlet Diagonal conjugate Obstetric conjugate Transverse diameter Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 32
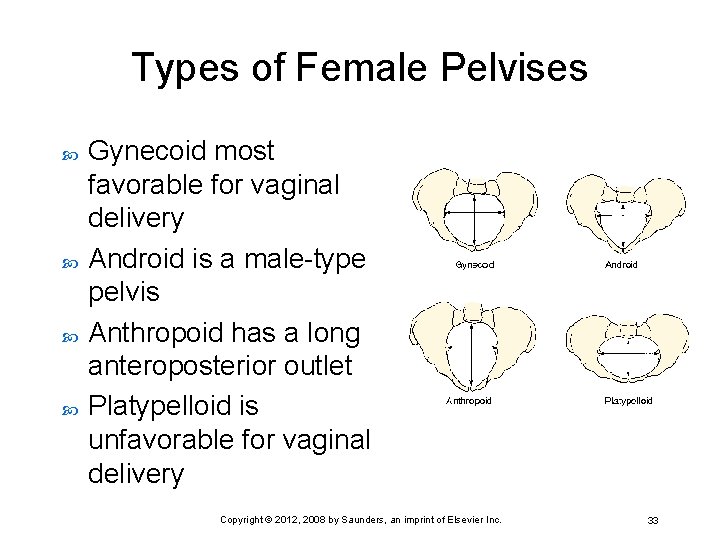
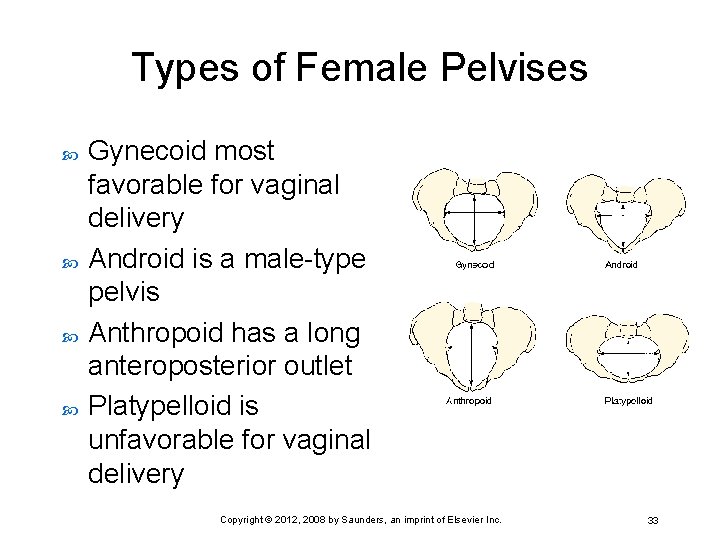
Types of Female Pelvises Gynecoid most favorable for vaginal delivery Android is a male-type pelvis Anthropoid has a long anteroposterior outlet Platypelloid is unfavorable for vaginal delivery Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 33
Endocrine System and Female Reproduction Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 34
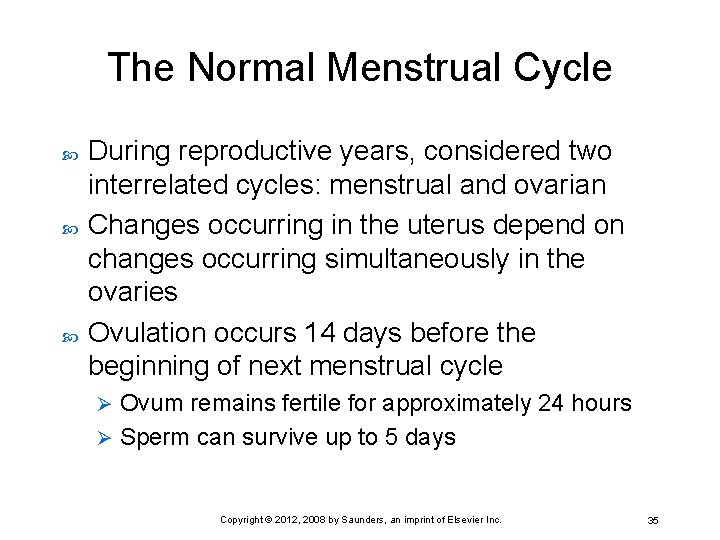
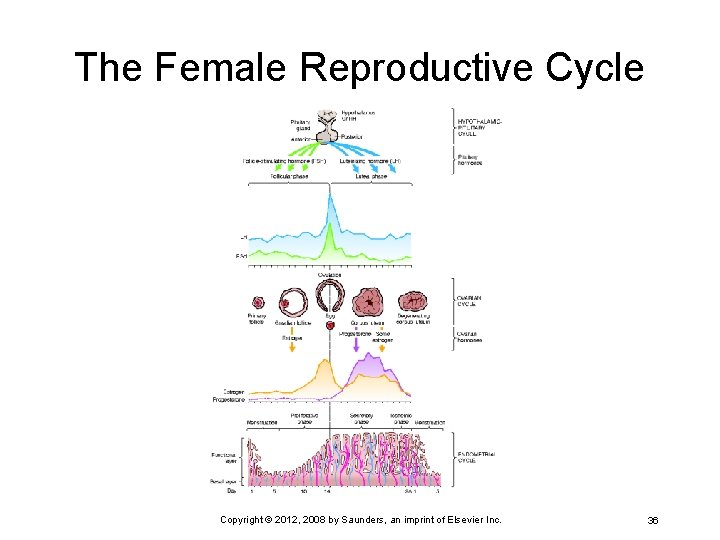
The Normal Menstrual Cycle During reproductive years, considered two interrelated cycles: menstrual and ovarian Changes occurring in the uterus depend on changes occurring simultaneously in the ovaries Ovulation occurs 14 days before the beginning of next menstrual cycle Ovum remains fertile for approximately 24 hours Ø Sperm can survive up to 5 days Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 35
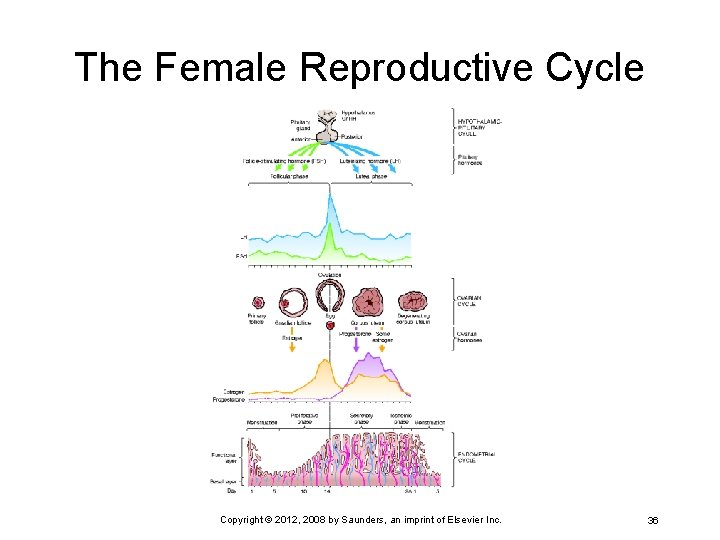
The Female Reproductive Cycle Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 36
Breasts Mammary glands Accessory organs of reproduction because of milk production, called lactation Montgomery’s glands secrete a substance that lubricates and protects the breast during lactation Breast size does not determine amount of milk production Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 37
Audience Response System Question 1 What hormone is responsible for preparing and maintaining the lining of the uterus for implantation of the ovum? A. Estrogen B. Estradiol C. Progesterone D. Progestin Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 38
Reproduction and the Sex Act Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 39
Objectives Identify the male organs of reproduction. Review the functions of the male hormone testosterone. Explain the physiology of the sex act in the male and female. Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 40
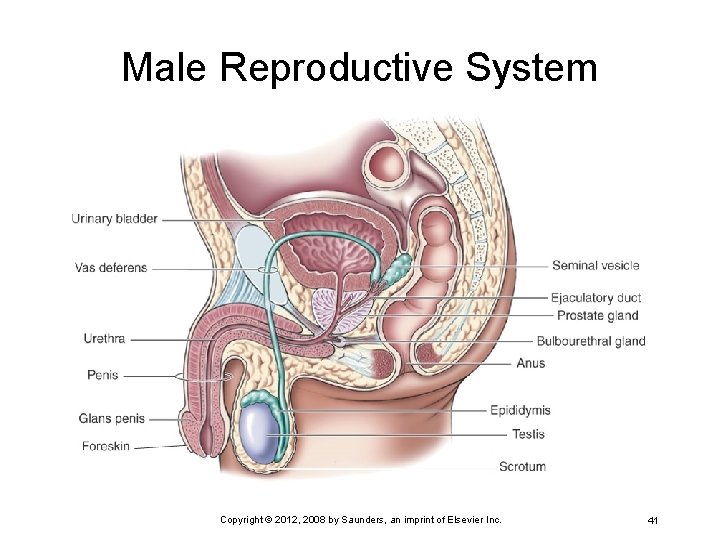
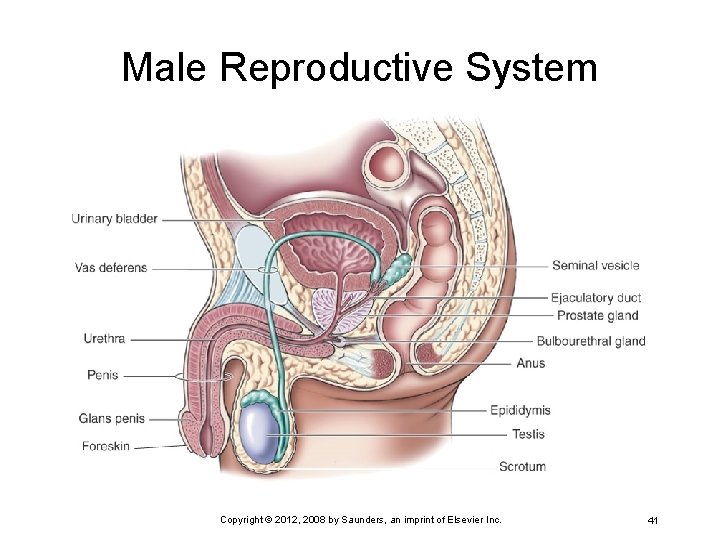
Male Reproductive System Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 41
Male External Genitalia Penis Expels urine from bladder Ø Organ of copulation Ø Deposits sperm into female’s vagina Ø Glans is covered by loosely fitting skin called the prepuce, or foreskin Contains erectile tissue that becomes erect during sexual stimulation Ø Blood is trapped within the spongy erectile tissue Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 42
Scrotum Wrinkled, pigmented pouch of skin, muscle, and fascia Each sac contains a testis (testicle), the epididymis, and a portion of spermatic cord Ø Suspended from the perineum Hangs outside the body and helps keep testes cooler than the rest of the body Ø Necessary for spermatogenesis Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 43
Internal Male Structures Testes Specialized tissue arranged in coiled tubes called seminiferous tubules Ø Sperm produced here Ø Some seminal fluid (semen) is produced here too Ø Leydig’s cells produce male hormone, testosterone Ø Two main functions of testes Manufacture sperm Ø Secrete male hormones (androgens) Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 44
Epididymis If fully stretched, measures more than 20 feet Becomes the vas deferens Excretory duct of each testis Provides a reservoir for sperm Sperm can be maintained here for up to 3 weeks as they mature and become motile Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 45
Vas Deferens A tube measuring around 45 cm (18 inches) Continuation of epididymis Ends by joining duct of seminal vesicles to form ejaculatory duct Carries sperm from each testis to urethra Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 46
Accessory Glands Produce secretions to Nourish sperm Ø Protect sperm from acidic environment in woman’s vagina Ø Enhance movement (motility) of sperm Ø Seminal vesicles Two saclike structures at base of urinary bladder Ø Produce thick, milky secretion that forms much of the ejaculated semen Ø Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 47
Accessory Glands (cont. ) Prostate gland During ejaculation, contracts along with vas deferens and seminal vesicles Ø Adds thin, milky, alkaline fluid to semen Ø This fluid contributes to fertilization of ovum Ø Enhances sperm motility and lifespan Ø Bulbourethral glands (or Cowper’s glands) Ø Provide a lubricant and alkaline fluid to the semen Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 48
Endocrine System and Male Reproduction Around age 15 years, boys are able to produce and ejaculate sperm Follicle-stimulating hormone (FSH) Ø Helps produce spermatozoa Luteinizing hormone (LH) Ø Acts on interstitial Leydig’s cell to release androgens, most importantly testosterone Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 49
Testosterone Develops penis, scrotum, prostate gland, and seminal vesicles Develops secondary sex characteristics Helps bones and muscles increase in mass and strength Promotes growth of long bones Increases basal metabolic rate (BMR) Enhances production of red blood cells Produces enlargement of vocal cords Affects distribution of body hair Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 50
Physiology of the Male Sex Act Psyche can initiate or inhibit sexual response Sexual stimulation causes parasympathetic and sympathetic nerve fibers to relax penile arteries, leading to erection Spinal nerves lead to contraction of the vas deferens and cause expulsion of sperm into the urethra (emission) Nerves in sacral region aid in the expulsion of semen from urethra (ejaculation) Emission and ejaculation are the male orgasm Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 51
Physiology of the Female Sex Act Stimulation by massage of the breasts, vulva, vagina, and perineum can create sexual sensations Parasympathetic nerves signal the vaginal introitus to dilate and fill the arteries; results in a tightening of the vagina around the penis Perineal and other muscles contract; oxytocin is secreted, which leads to contraction of the uterus and dilation of the cervical canal Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 52
Physiology of the Female Sex Act (cont. ) These contractions are called orgasm and are believed to aid in the transport of sperm to the fallopian tubes Ovum (egg) lives only 24 hours; therefore, sperm must be available during that time for fertilization to occur Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 53
Audience Response System Question 2 Testosterone is responsible for all of the following except: A. Developing penis and seminal vesicles B. Developing secondary sex characteristics in males C. Enhancing production of red blood cells D. Enhancing production of Leydig’s cells Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 54
Review Key Points Copyright © 2012, 2008 by Saunders, an imprint of Elsevier Inc. 55