Chapter 18 The GramPositive and GramNegative Diplococci of


- Slides: 27
Chapter 18 The Gram-Positive and Gram-Negative Diplococci of Medical Importance

Meet the Blood Agar Plate (BAP) • • Non-selective, differential growth medium Used to distinguish clinically significant bacteria from throat and sputum cultures. BAP contains 5% sheep blood… aka red blood cells Certain bacteria produce exotoxins called hemolysins, which act on the red blood cells to lyse, or break them down. 2
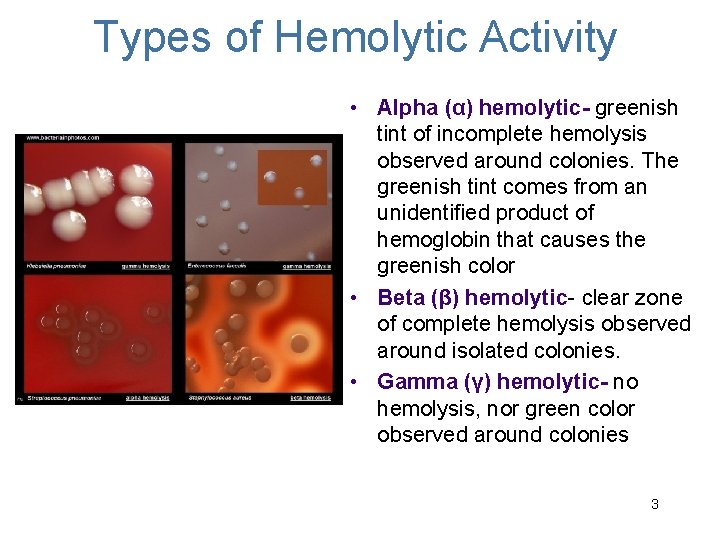
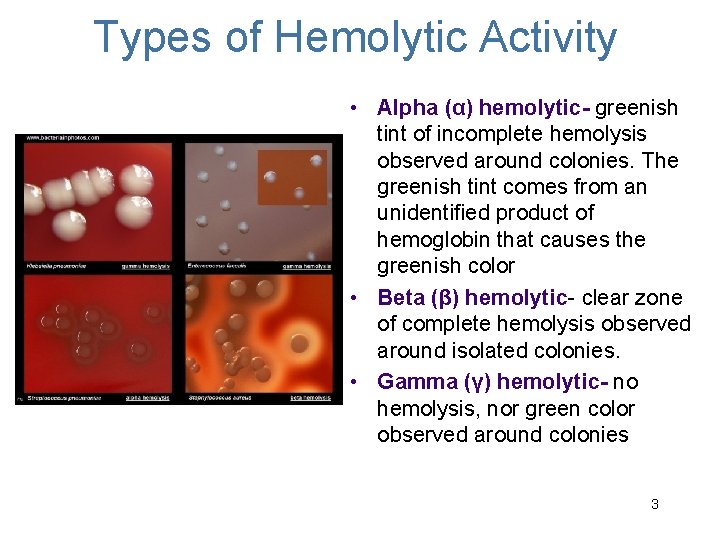
Types of Hemolytic Activity • Alpha (α) hemolytic- greenish tint of incomplete hemolysis observed around colonies. The greenish tint comes from an unidentified product of hemoglobin that causes the greenish color • Beta (β) hemolytic- clear zone of complete hemolysis observed around isolated colonies. • Gamma (γ) hemolytic- no hemolysis, nor green color observed around colonies 3
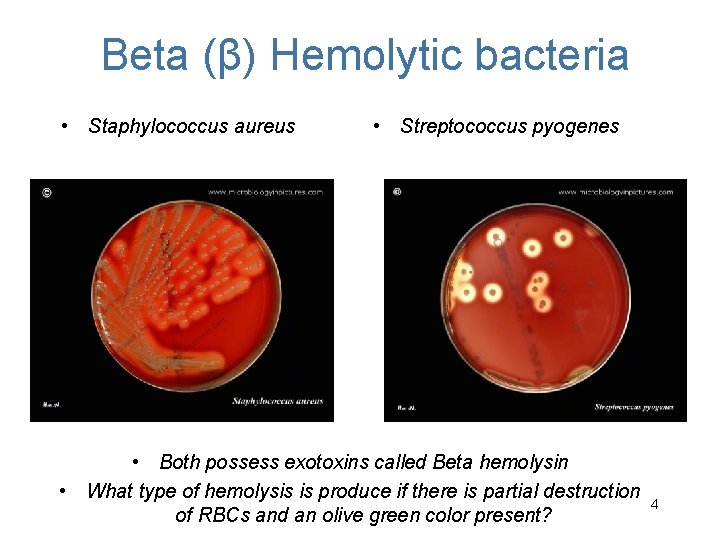
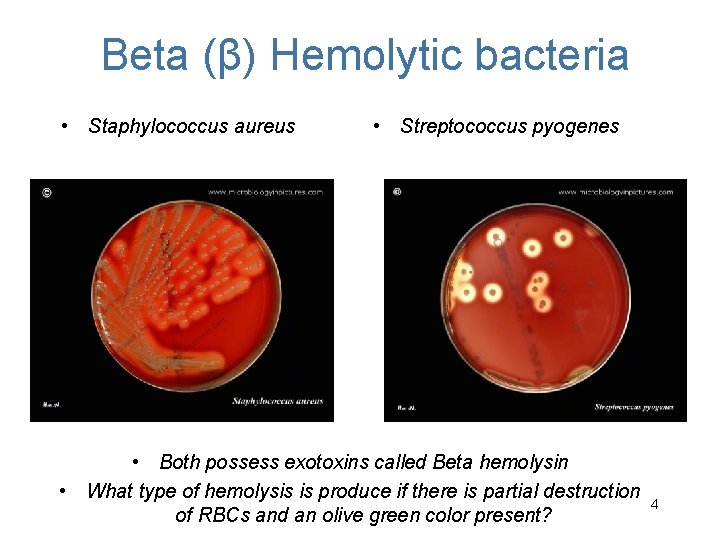
Beta (β) Hemolytic bacteria • Staphylococcus aureus • Streptococcus pyogenes • Both possess exotoxins called Beta hemolysin • What type of hemolysis is produce if there is partial destruction of RBCs and an olive green color present? 4

VRSA 5
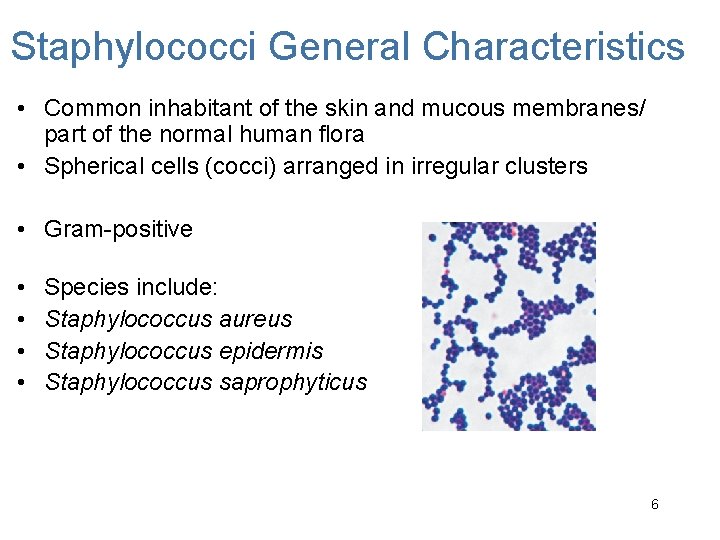
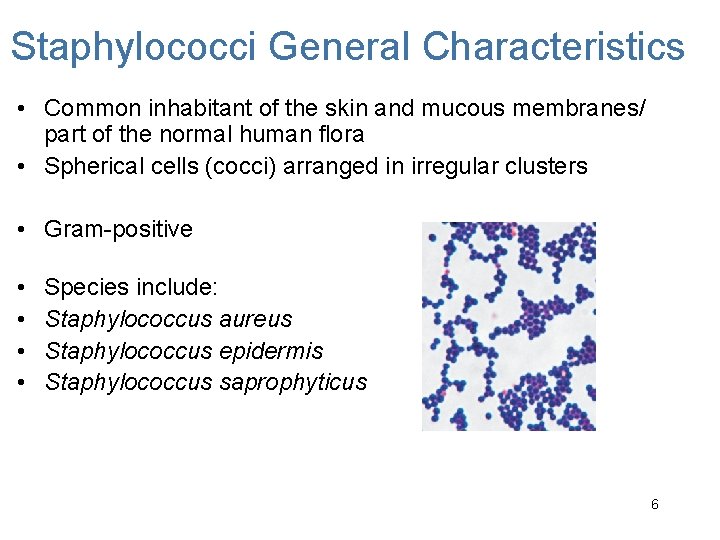
Staphylococci General Characteristics • Common inhabitant of the skin and mucous membranes/ part of the normal human flora • Spherical cells (cocci) arranged in irregular clusters • Gram-positive • • Species include: Staphylococcus aureus Staphylococcus epidermis Staphylococcus saprophyticus 6
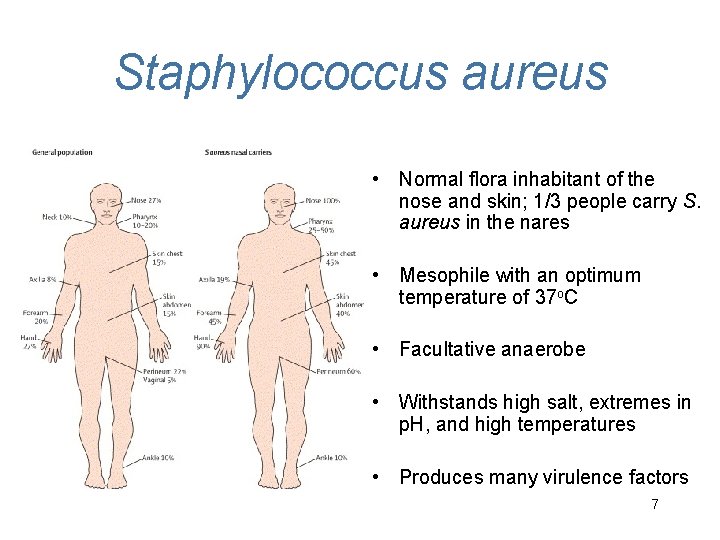
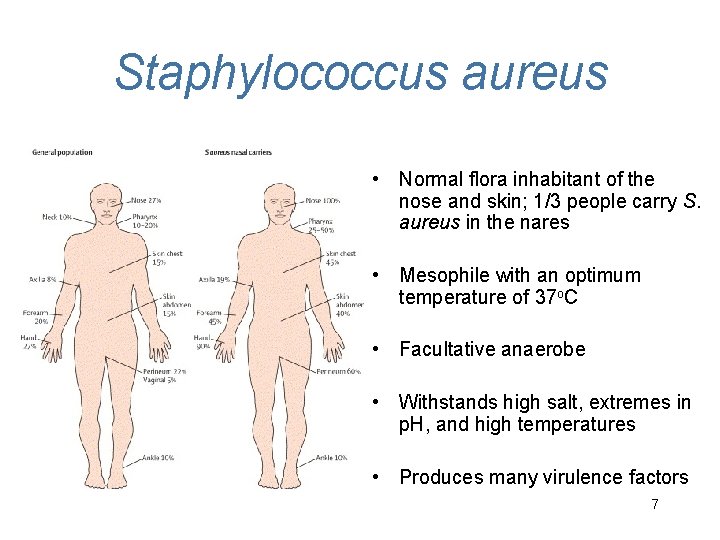
Staphylococcus aureus • Normal flora inhabitant of the nose and skin; 1/3 people carry S. aureus in the nares • Mesophile with an optimum temperature of 37 o. C • Facultative anaerobe • Withstands high salt, extremes in p. H, and high temperatures • Produces many virulence factors 7
Virulence factors of S. aureus Enzymes: • Coagulase – coagulates plasma and blood; produced by 97% of human isolates; labs test for coagulase to diagnose patients with Staphylococcus aureus infections • DNase – digests DNA • Penicillinase – inactivates penicillin Toxins: • Hemolysins (α, β, γ, δ) – lyse red blood cells • Leukocidin – lyses neutrophils and macrophages • Enterotoxin – induce gastrointestinal distress • Toxic shock syndrome toxin (TSST) – induces fever, vomiting, shock, systemic organ damage • Exfoliatin toxin – causes separation within the epidermis 8
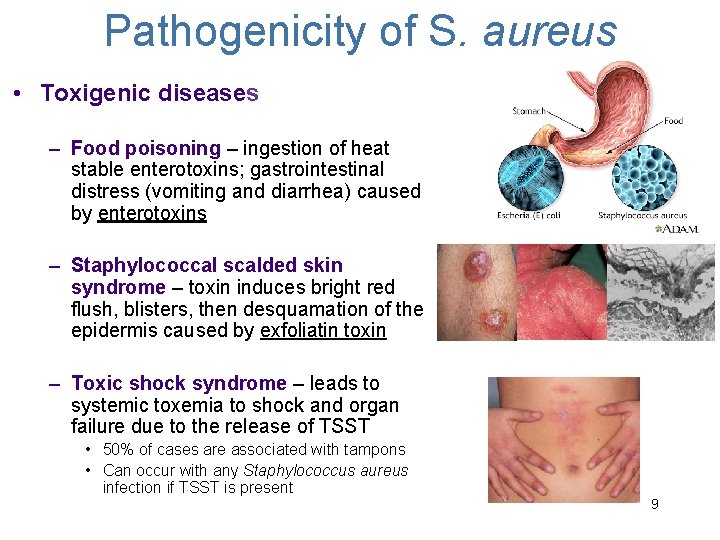
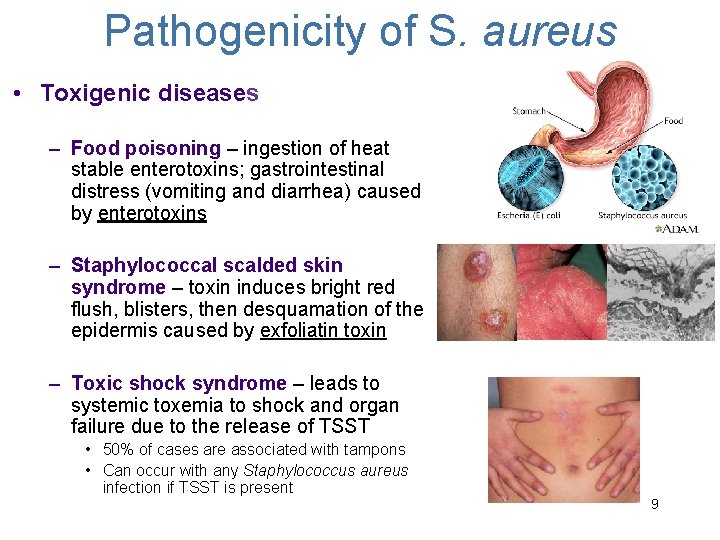
Pathogenicity of S. aureus • Toxigenic diseases – Food poisoning – ingestion of heat stable enterotoxins; gastrointestinal distress (vomiting and diarrhea) caused by enterotoxins – Staphylococcal scalded skin syndrome – toxin induces bright red flush, blisters, then desquamation of the epidermis caused by exfoliatin toxin – Toxic shock syndrome – leads to systemic toxemia to shock and organ failure due to the release of TSST • 50% of cases are associated with tampons • Can occur with any Staphylococcus aureus infection if TSST is present 9
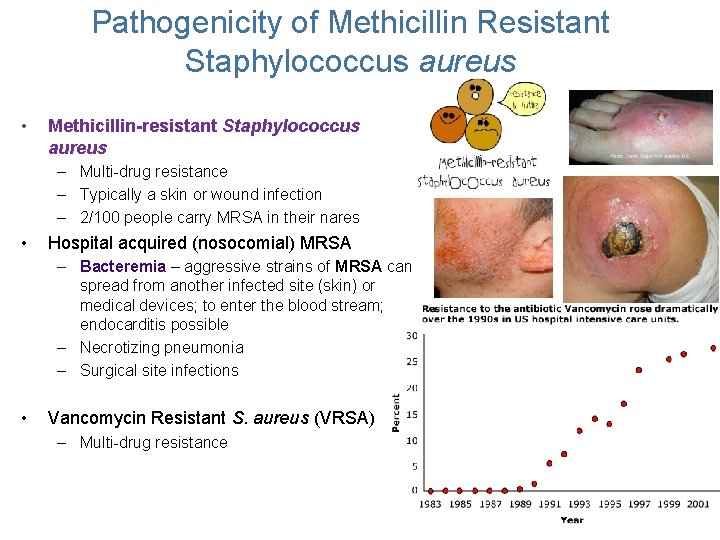
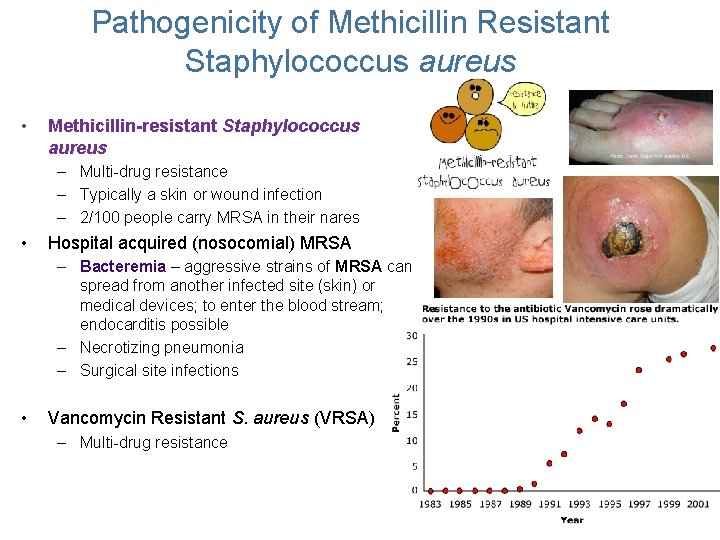
Pathogenicity of Methicillin Resistant Staphylococcus aureus • Methicillin-resistant Staphylococcus aureus – Multi-drug resistance – Typically a skin or wound infection – 2/100 people carry MRSA in their nares • Hospital acquired (nosocomial) MRSA – Bacteremia – aggressive strains of MRSA can spread from another infected site (skin) or medical devices; to enter the blood stream; endocarditis possible – Necrotizing pneumonia – Surgical site infections • Vancomycin Resistant S. aureus (VRSA) – Multi-drug resistance 10
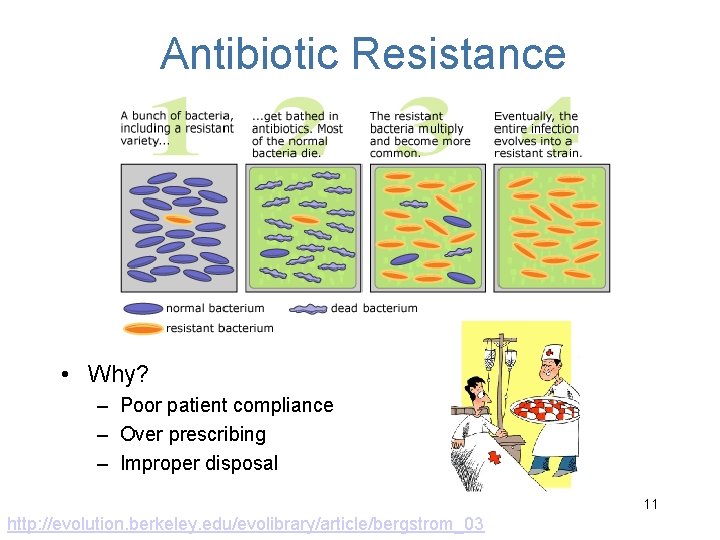
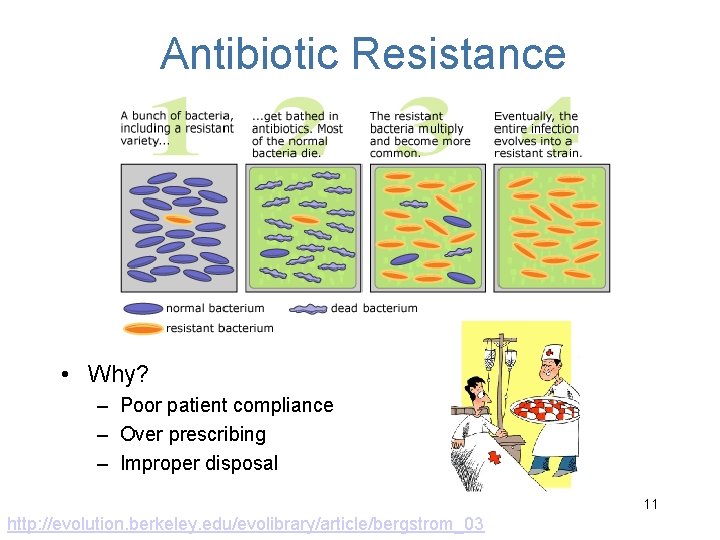
Antibiotic Resistance • Why? – Poor patient compliance – Over prescribing – Improper disposal 11 http: //evolution. berkeley. edu/evolibrary/article/bergstrom_03
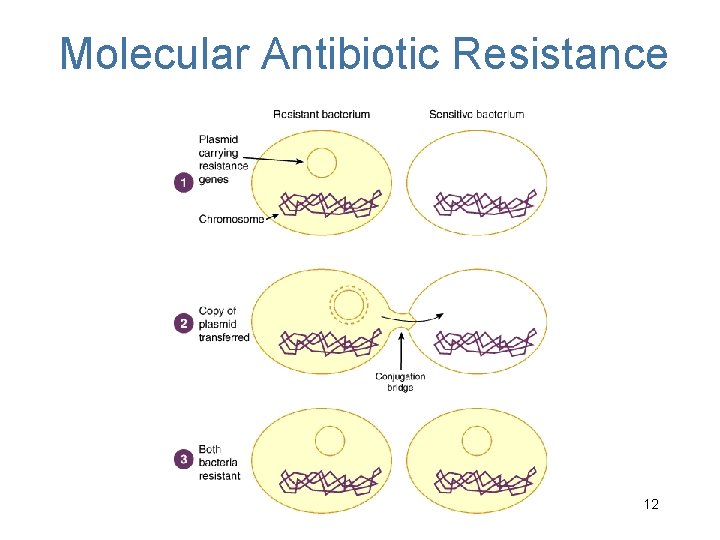
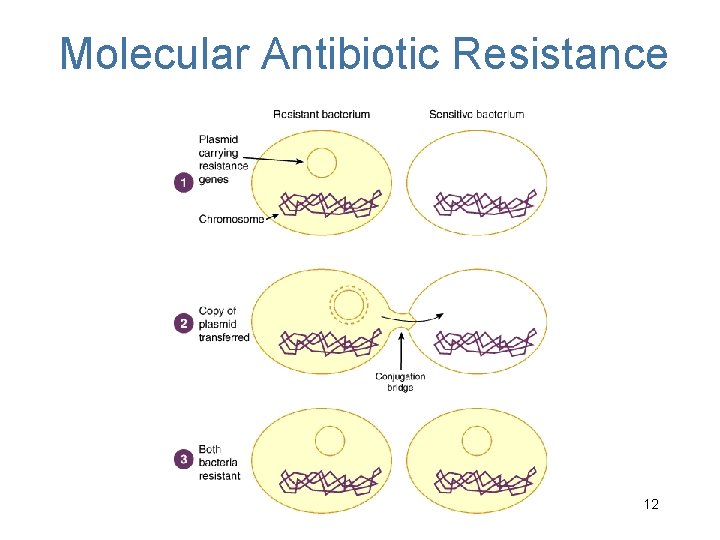
Molecular Antibiotic Resistance 12
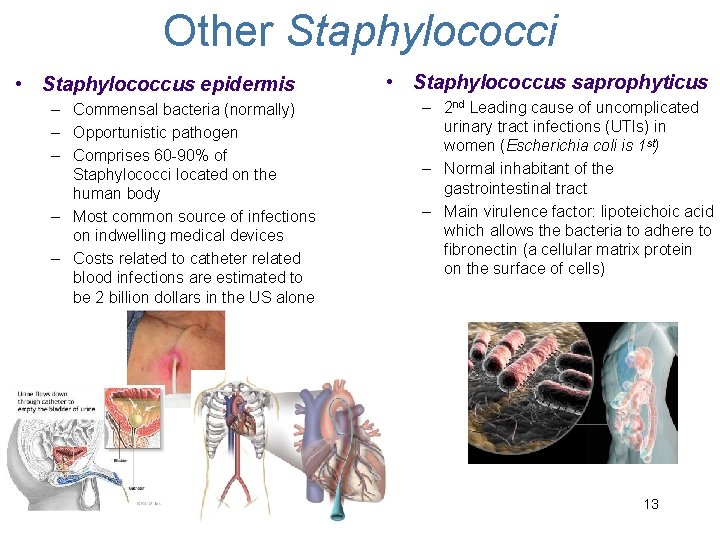
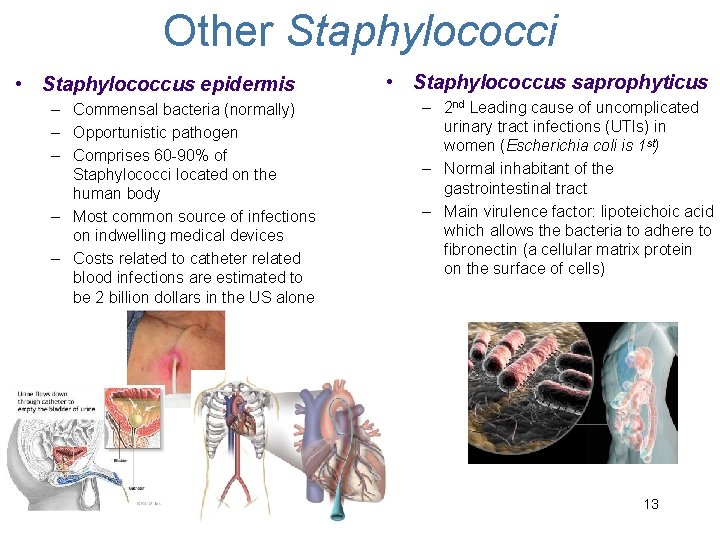
Other Staphylococci • Staphylococcus epidermis – Commensal bacteria (normally) – Opportunistic pathogen – Comprises 60 -90% of Staphylococci located on the human body – Most common source of infections on indwelling medical devices – Costs related to catheter related blood infections are estimated to be 2 billion dollars in the US alone • Staphylococcus saprophyticus – 2 nd Leading cause of uncomplicated urinary tract infections (UTIs) in women (Escherichia coli is 1 st) – Normal inhabitant of the gastrointestinal tract – Main virulence factor: lipoteichoic acid which allows the bacteria to adhere to fibronectin (a cellular matrix protein on the surface of cells) 13
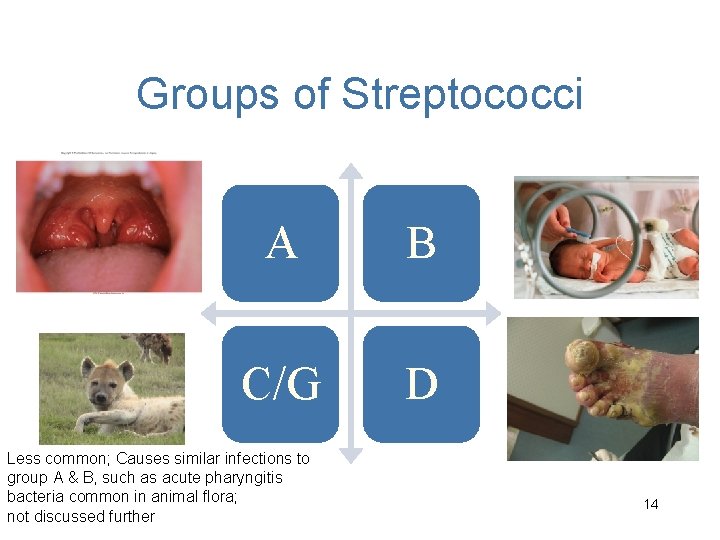
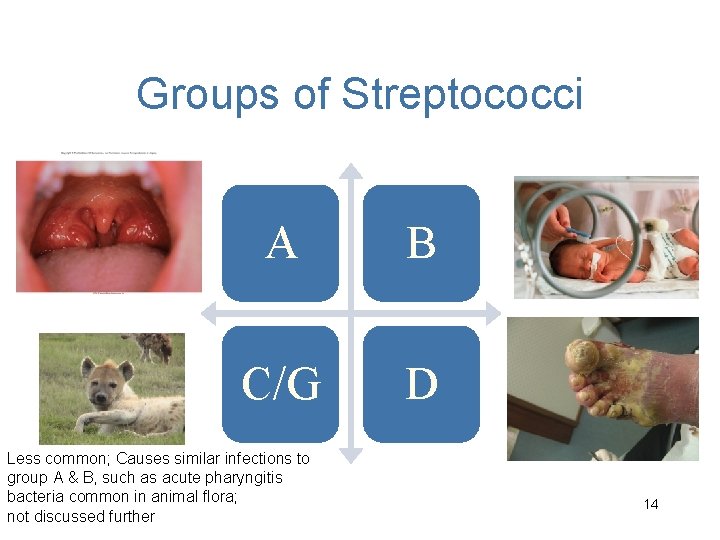
Groups of Streptococci A B C/G D Less common; Causes similar infections to group A & B, such as acute pharyngitis bacteria common in animal flora; not discussed further 14
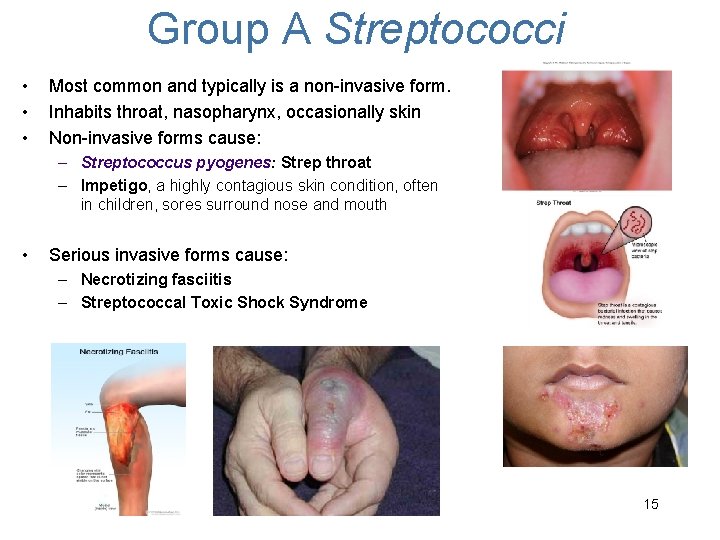
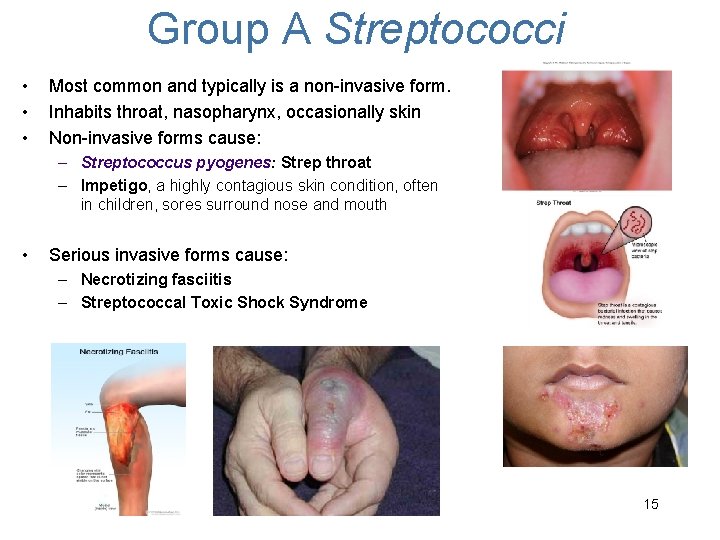
Group A Streptococci • • • Most common and typically is a non-invasive form. Inhabits throat, nasopharynx, occasionally skin Non-invasive forms cause: – Streptococcus pyogenes: Strep throat – Impetigo, a highly contagious skin condition, often in children, sores surround nose and mouth • Serious invasive forms cause: – Necrotizing fasciitis – Streptococcal Toxic Shock Syndrome 15
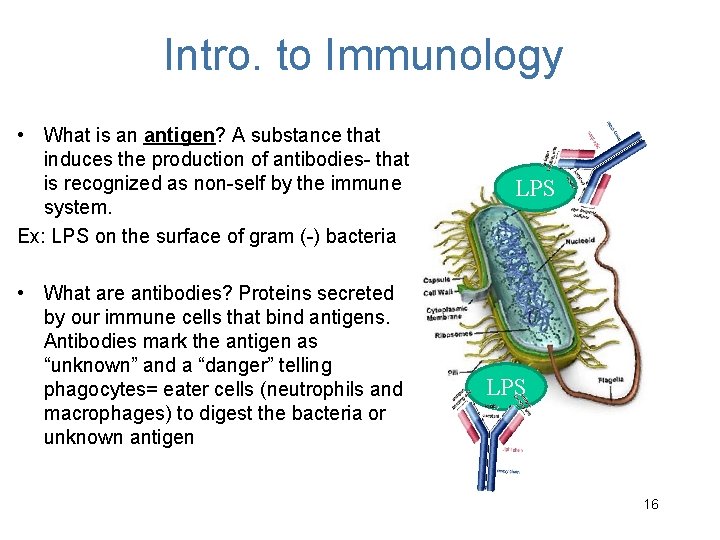
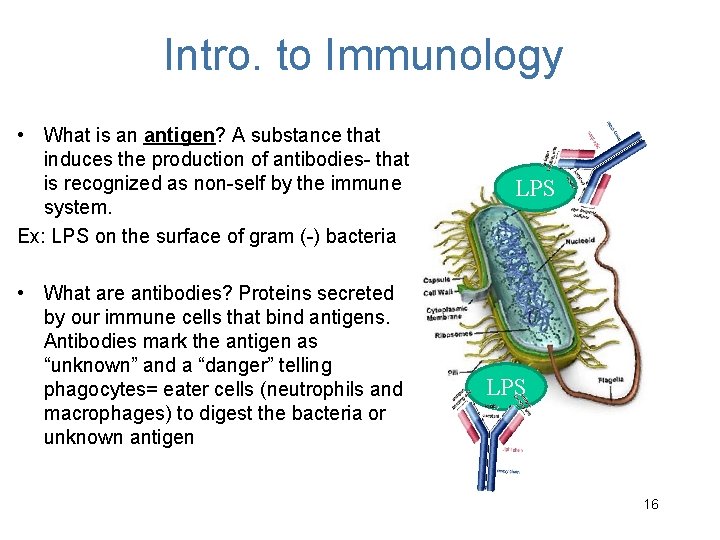
Intro. to Immunology • What is an antigen? A substance that induces the production of antibodies- that is recognized as non-self by the immune system. Ex: LPS on the surface of gram (-) bacteria • What are antibodies? Proteins secreted by our immune cells that bind antigens. Antibodies mark the antigen as “unknown” and a “danger” telling phagocytes= eater cells (neutrophils and macrophages) to digest the bacteria or unknown antigen LPS 16
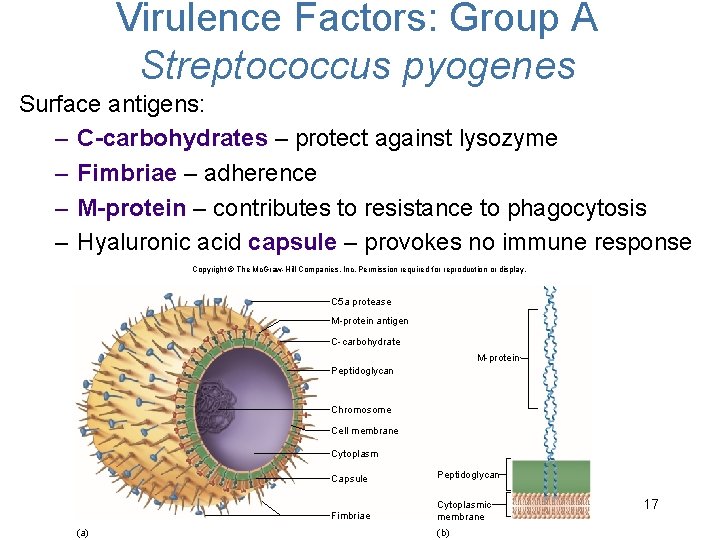
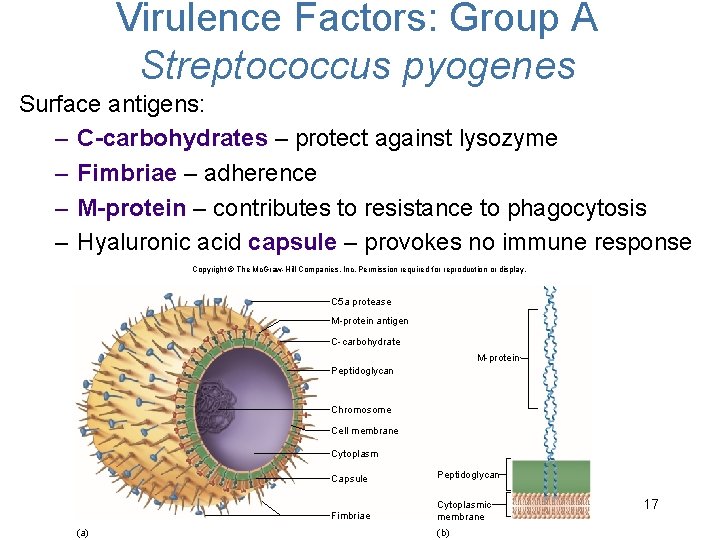
Virulence Factors: Group A Streptococcus pyogenes Surface antigens: – C-carbohydrates – protect against lysozyme – Fimbriae – adherence – M-protein – contributes to resistance to phagocytosis – Hyaluronic acid capsule – provokes no immune response Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. C 5 a protease M-protein antigen C-carbohydrate M-protein Peptidoglycan Chromosome Cell membrane Cytoplasm (a) Capsule Peptidoglycan Fimbriae Cytoplasmic membrane (b) 17
Virulence Factors of Group A S. pyogenes Extracellular toxins: Streptolysins – hemolysins; cause cell and tissue injury Erythrogenic toxin (pyrogenic) – induces fever and typical red rash Superantigens – strong monocyte and lymphocyte stimulants; cause the release of tissue necrotic factor 18
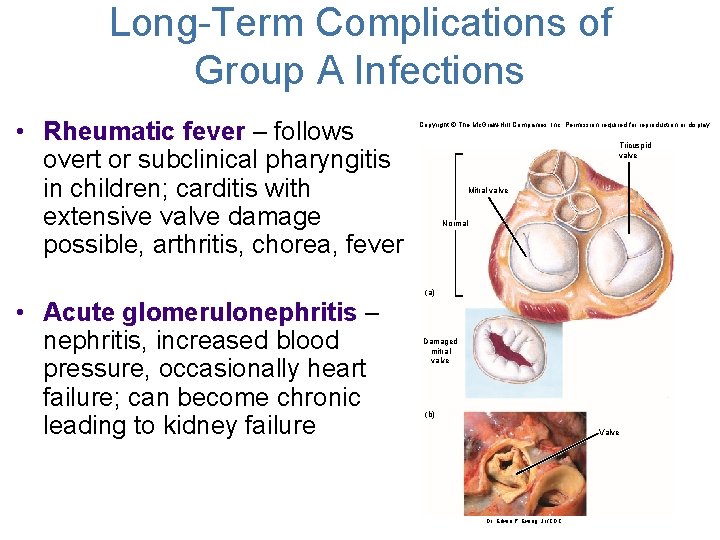
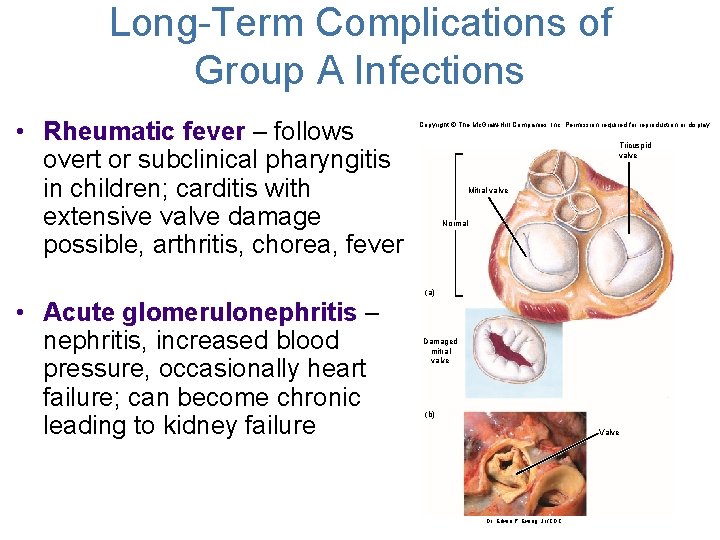
Long-Term Complications of Group A Infections • Rheumatic fever – follows overt or subclinical pharyngitis in children; carditis with extensive valve damage possible, arthritis, chorea, fever Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Tricuspid valve Mitral valve Normal (a) • Acute glomerulonephritis – nephritis, increased blood pressure, occasionally heart failure; can become chronic leading to kidney failure Damaged mitral valve (b) Valve 19 Dr. Edwin P. Ewing, Jr. /CDC
Group B Streptococci • Regularly resides in human vagina, pharynx, and large intestine • Newborn’s 1 st week of life Group B Strep is the leading cause of: – Neonatal pneumonia, – Sepsis (infection of the blood), – meningitis (infection of the fluid and lining around the brain) • Illness is predominately in newborns and non-pregnant adults over 60 years
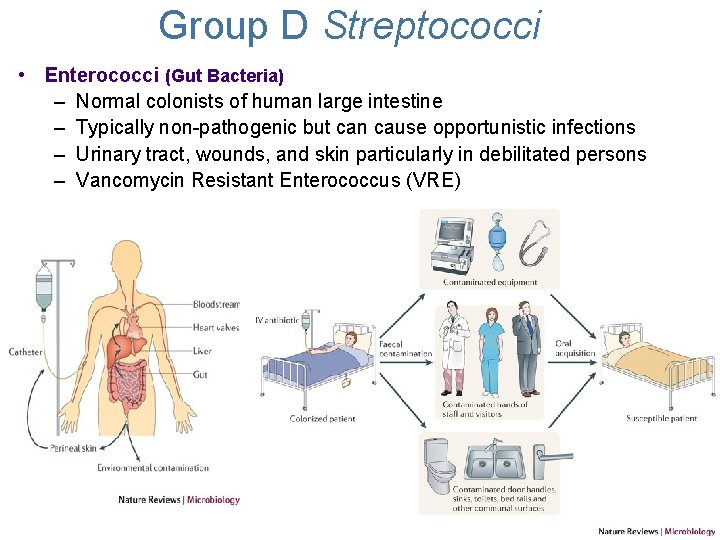
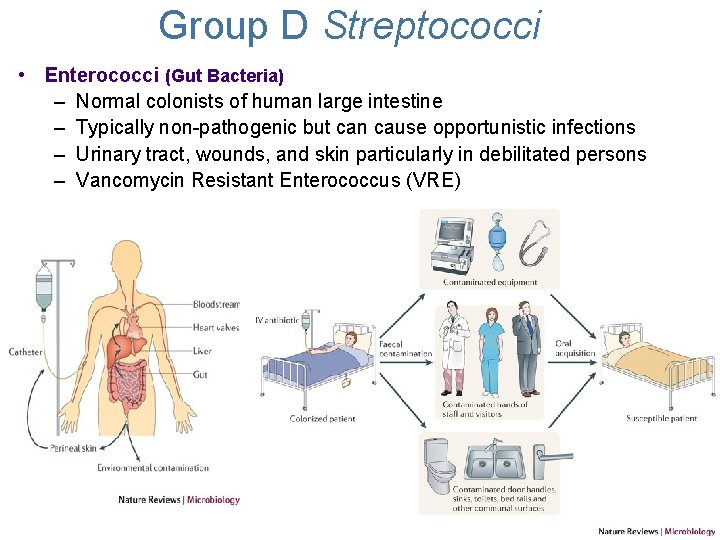
Group D Streptococci • Enterococci (Gut Bacteria) – Normal colonists of human large intestine – Typically non-pathogenic but can cause opportunistic infections – Urinary tract, wounds, and skin particularly in debilitated persons – Vancomycin Resistant Enterococcus (VRE)
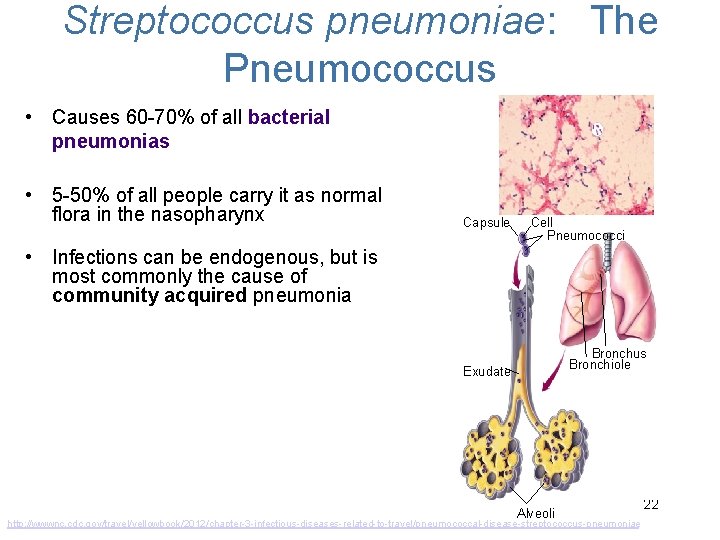
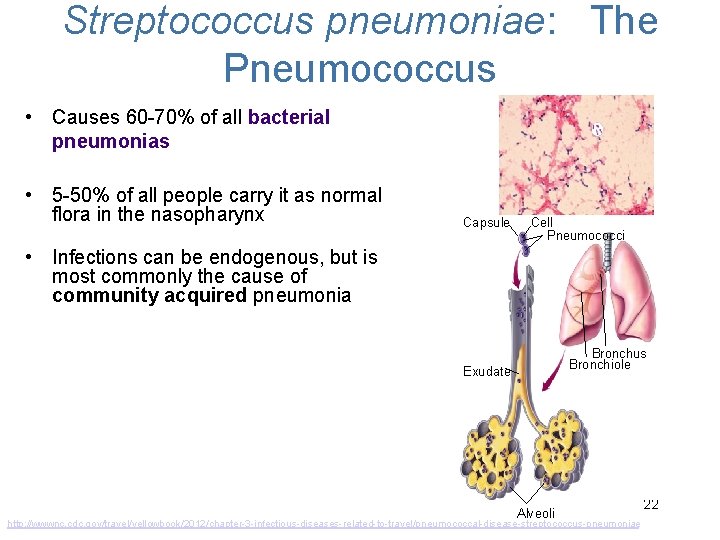
Streptococcus pneumoniae: The Pneumococcus • Causes 60 -70% of all bacterial pneumonias • 5 -50% of all people carry it as normal flora in the nasopharynx Capsule Cell Pneumococci • Infections can be endogenous, but is most commonly the cause of community acquired pneumonia Bronchus Bronchiole Exudate Alveoli http: //wwwnc. cdc. gov/travel/yellowbook/2012/chapter-3 -infectious-diseases-related-to-travel/pneumococcal-disease-streptococcus-pneumoniae 22
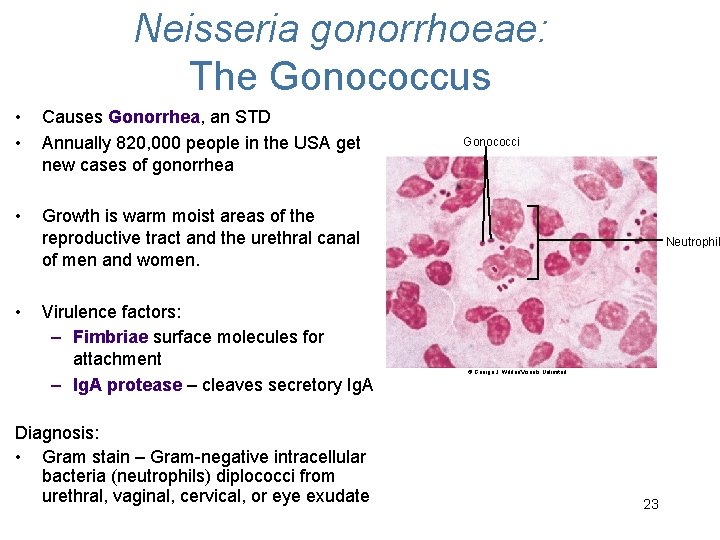
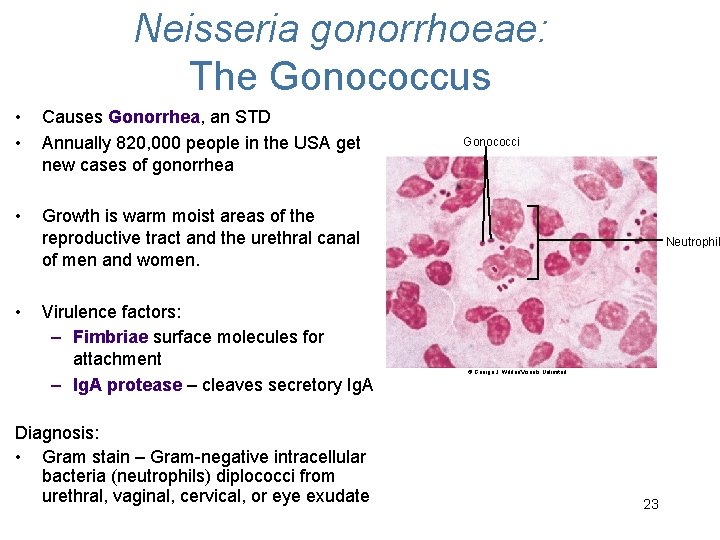
Neisseria gonorrhoeae: The Gonococcus • • Causes Gonorrhea, an STD Annually 820, 000 people in the USA get new cases of gonorrhea • Growth is warm moist areas of the reproductive tract and the urethral canal of men and women. • Virulence factors: – Fimbriae surface molecules for attachment – Ig. A protease – cleaves secretory Ig. A Diagnosis: • Gram stain – Gram-negative intracellular bacteria (neutrophils) diplococci from urethral, vaginal, cervical, or eye exudate Gonococci Neutrophil © George J. Wilder/Visuals Unlimited 23
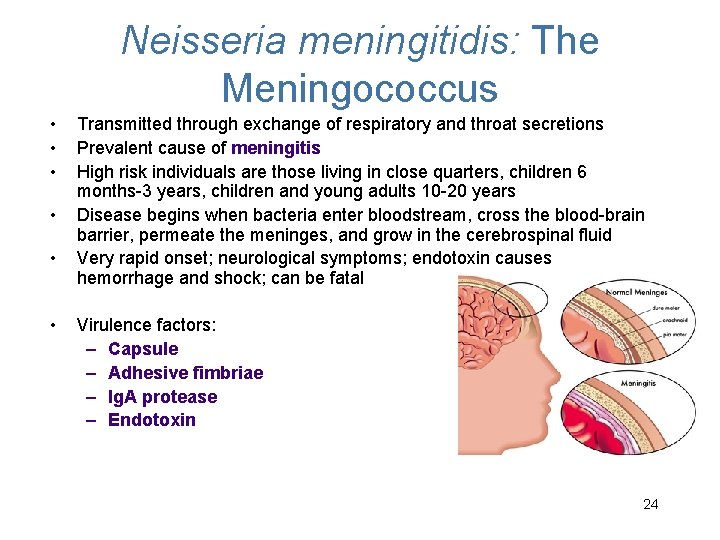
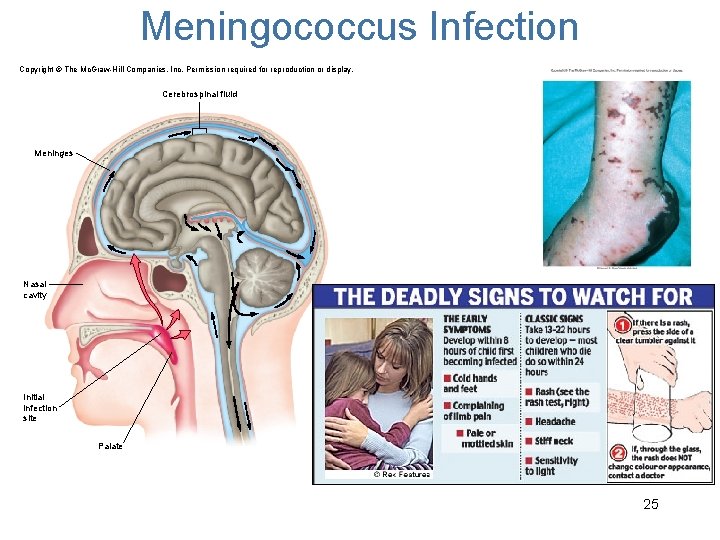
Neisseria meningitidis: The Meningococcus • • • Transmitted through exchange of respiratory and throat secretions Prevalent cause of meningitis High risk individuals are those living in close quarters, children 6 months-3 years, children and young adults 10 -20 years Disease begins when bacteria enter bloodstream, cross the blood-brain barrier, permeate the meninges, and grow in the cerebrospinal fluid Very rapid onset; neurological symptoms; endotoxin causes hemorrhage and shock; can be fatal Virulence factors: – Capsule – Adhesive fimbriae – Ig. A protease – Endotoxin 24
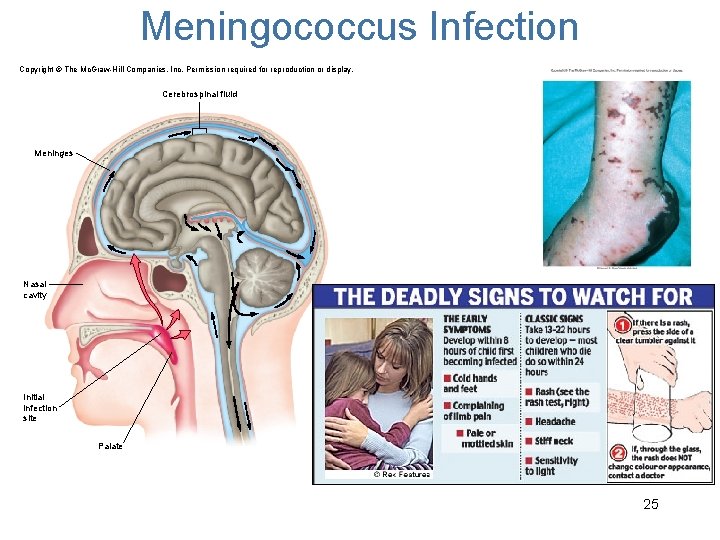
Meningococcus Infection Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Cerebrospinal fluid Meninges Nasal cavity Initial infection site Palate 25
Infection Prevention • Good hygiene • Hand washing • Personal Protection Equipment (PPE) • Sterile technique 26
Concept Check: A common cause of meningitis in young adults is found in the genus A. Streptococcus B. Staphylococcus C. Neisseria D. Branhamella