Chapter 18 Safetly Lifting Moving and Positioning Patients
- Slides: 49
Chapter 18 Safetly Lifting, Moving, and Positioning Patients Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lesson 18. 1 Overview of Anatomy and Body Mechanics, Movement, Alignment Theory 1) Describe the anatomy and function of the musculoskeletal system 2) Explain the importance of proper body mechanics, alignment, and position change for both patient and nurse 3) Discuss the principles of safe body movement and positioning, giving an appropriate example for each principle 4) Identify ways to maintain the patient’s correct body alignment in bed or in a chair Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Overview of the Structure and Function of the Musculoskeletal System Bones Ø Joint Ø Four types • Short, long, flat, and irregular A union of two or more bones; moves freely Bursa Ø A small fluid-filled sac that provides a cushion at friction points in the joints Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Overview of the Structure and Function of the Musculoskeletal System (cont’d) Skeletal muscle Ø Tendon Ø Fibrous tissue that connects muscle to bone Ligament Ø Striated muscles surrounded by a connective tissue sheath Connects bone to cartilage Cartilage Ø Fibrous connective tissue; acts as a cushion Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Functions of Bones Provide a scaffolding to support the body Give shape to the body and support the internal organs and skin Provide places for ligaments and tendons to attach to facilitate movement Ø Joints allow movement and flexibility of the skeleton Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Functions of Muscles Can stretch; can be stimulated to contract electrically or to extend elastically Provide movement Stabilize joints Produce heat Maintain posture Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Changes Occurring with Aging Bone mass loss may lead to osteoporosis (more severe in women) Loss of bone density predisposes the elderly to fractures Muscle cells are lost and replaced by fat cells Elasticity of muscle fibers is decreased, limiting flexibility Joint motion may decrease, limiting motion and mobility Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
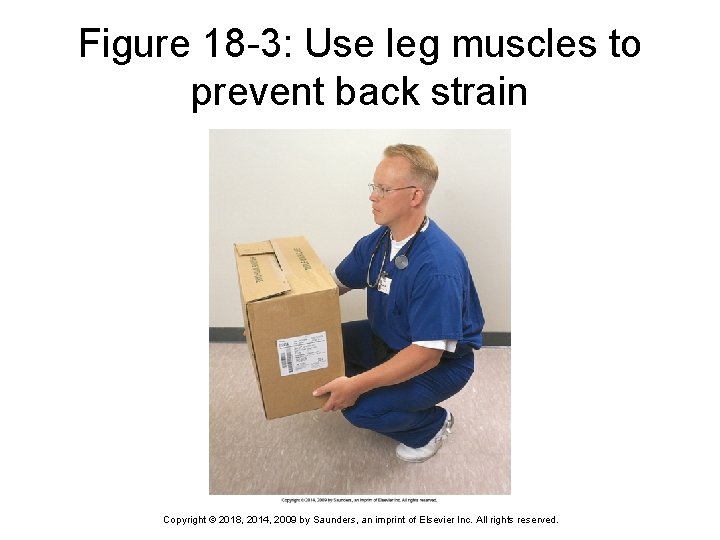
Principles of Body Movement for Nurses One of the most common injuries in health care workers is lower back strain Get help whenever possible; ask patient to help if able Ø Encourage patient to assist when transferring and moving if possible Use thigh, arm, or leg muscles rather than back muscles, and use a wide base of support Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Principles of Body Movement for Nurses (cont’d) Provide stability for movement Keep feet approximately shoulder-width apart Ø Use the greatest number of muscles possible Ø Use smooth, coordinated movements Keep loads close to the body Keep loads near the center of gravity Pull and pivot, using smooth, coordinated movements; avoid jerking or sudden pulling movements Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
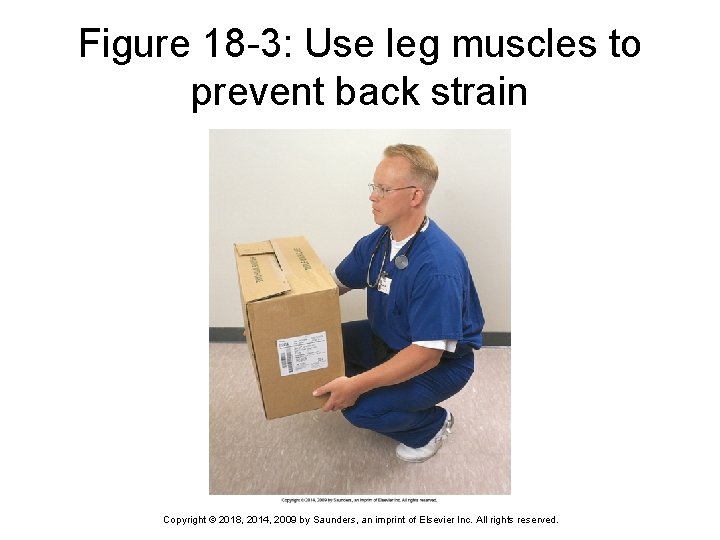
Figure 18 -3: Use leg muscles to prevent back strain Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Moving and Lifting Patients Keep elbows close and work close to your body; work at same level or height as the object to be moved; keep the load near your center of gravity Pulling actions require less effort than pushing or lifting; face the direction of the movement Use arms as levers when pulling patient toward you; lock elbows and rock back on your heels, using weight of your body to move the patient Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Principles of Body Movement for Patients Two basic principles Maintain correct anatomic position Ø Change position frequently Ø Hazards of improper alignment and positioning Interference with circulation, which may lead to pressure ulcers Ø Muscle cramps and possible contractures Ø Fluid collection in the lungs Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
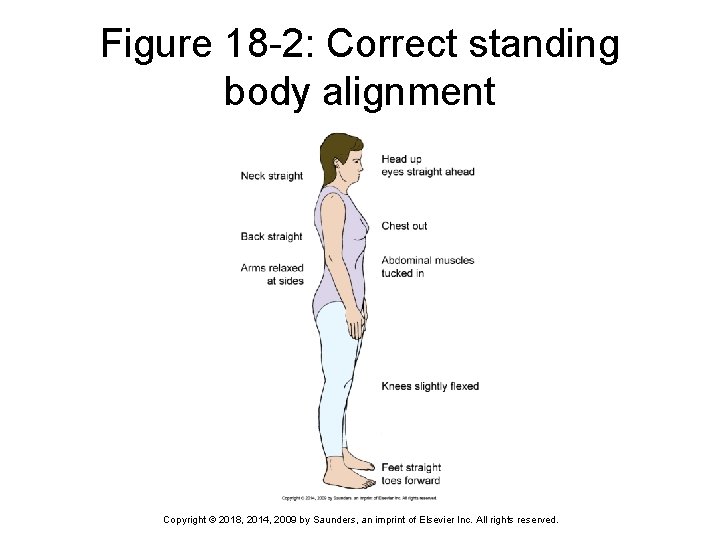
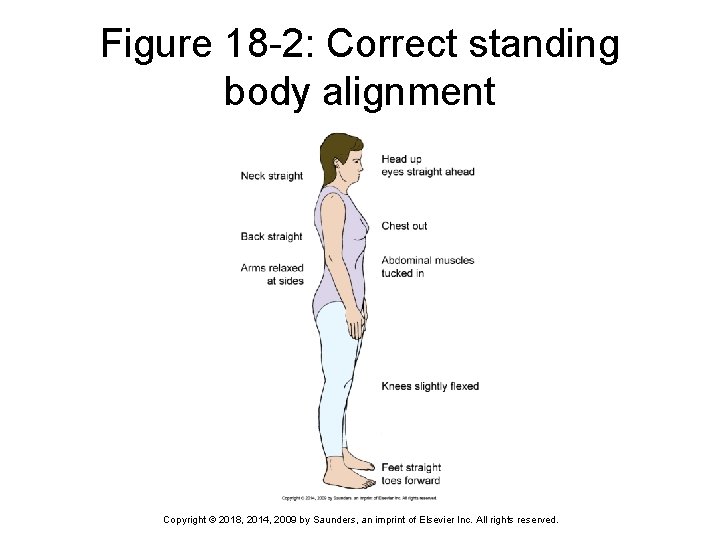
Figure 18 -2: Correct standing body alignment Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
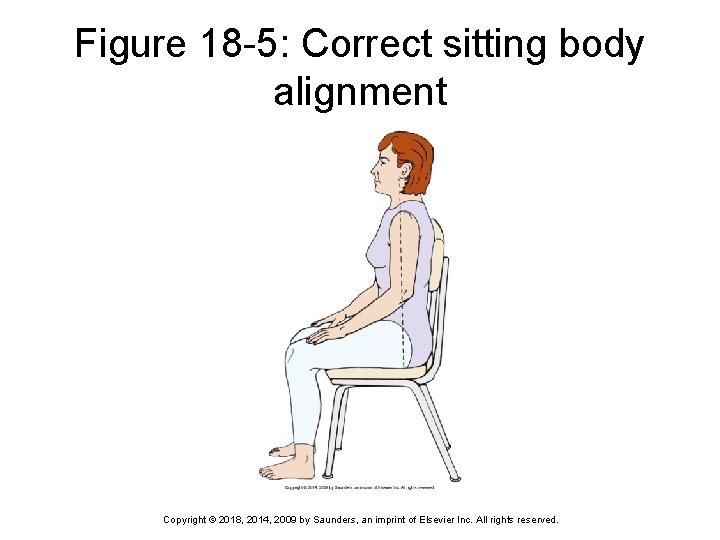
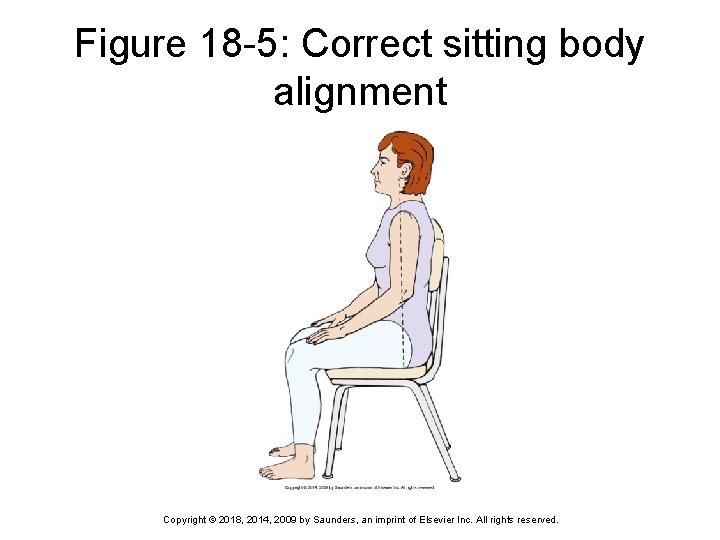
Figure 18 -5: Correct sitting body alignment Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Pressure Ulcers Also known as decubitus ulcers, or bedsores Occur when pressure on the skin causes an area of local tissue necrosis Occur most often between a bony prominence and an external surface May be caused by shearing as force is applied downward and forward on tissue beneath the skin (as when a patient slides down in a chair) Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Application of the Nursing Process: Assessment (Data Collection) When assessing the patient’s standing body alignment, start by noting the head position in relation to the rest of the body When assessing the sitting patient, observe for symmetry When assessing the lying patient, assess carefully for alignment and correct position Assess the patient’s ability to ambulate (walk) and to change position independently Observe the patient walking Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Application of the Nursing Process: Nursing Diagnosis Commonly used nursing diagnoses Risk for injury Ø Impaired physical mobility Ø Risk for impaired skin integrity Ø Impaired walking Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Application of the Nursing Process: Planning Decide how to change the patient’s position and whether you can delegate this task to assistive personnel The home setting must also be considered when planning care for the patient Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Expected Outcomes of Planning Patient will experience no musculoskeletal injury Former level of mobility will be reattained within 6 months Skin integrity will remain intact while patient is on bed rest Patient will not experience injury while ambulating Patient should have full range-of-motion exercise actively or passively performed several times a day Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 1 When moving a patient, it is important to use proper body mechanics. Which of the following is not a proper body mechanic? 1) 2) 3) 4) Using your leg muscles Keeping your feet together to provide stability for movement Using smooth, coordinated movements instead of jerking or sudden movements Keeping loads as well as your elbows close to the body Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 2 Leann is teaching her patient’s husband how to lift his wife safely. Which of the following is true regarding lifting the elderly? 1) 2) 3) 4) As the body ages, there is no change in posture. There is usually an increase in muscle mass as we age. Whatever items that could be lifted in your youth should be lifted in later years. Joint motion may decrease, limiting mobility. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lesson 18. 2 Lifting, Moving, and Positioning Patients Theory 5) Describe the proper method for transferring a patient between wheelchair and bed Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lesson 18. 2 Lifting, Moving, and Positioning Patients Clinical Practice 1) Correctly position a patient in the following positions: supine, prone, Fowler, and Sims 2) Assist patients to sit up in bed 3) Demonstrate complete passive range-of-motion (ROM) exercises for a patient 4) Correctly transfer a patient from a wheelchair to a bed 5) Transfer a patient from a bed to a stretcher 6) Demonstrate the correct techniques for ambulating a patient and for breaking a fall while ambulating Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Application of the Nursing Process: Implementation: Positioning Accomplishes four objectives Positioning provides comfort Ø Positioning relieves pressure on bony prominences and other parts, decreasing the patient’s risk of developing bedsores Ø Positioning prevents contractures, deformities, and respiratory problems Ø Positioning improves circulation Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
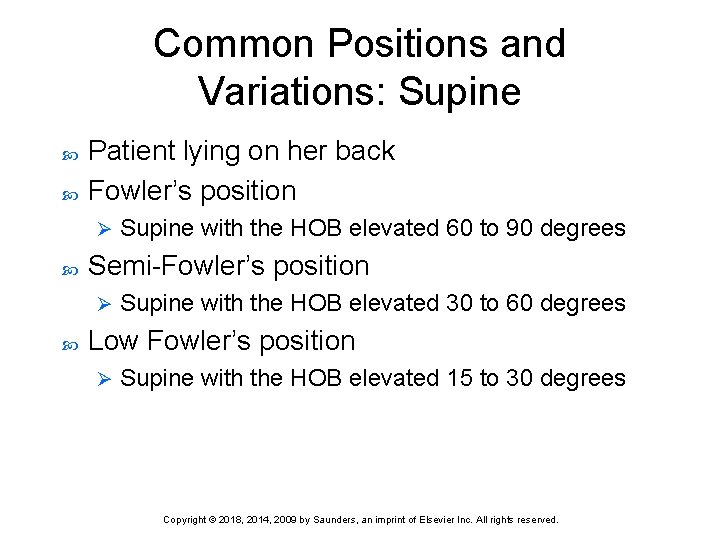
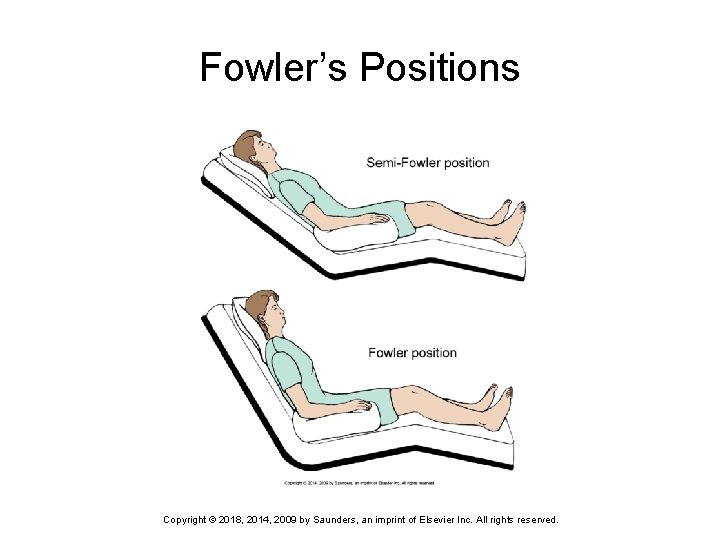
Common Positions and Variations: Supine Patient lying on her back Fowler’s position Ø Semi-Fowler’s position Ø Supine with the HOB elevated 60 to 90 degrees Supine with the HOB elevated 30 to 60 degrees Low Fowler’s position Ø Supine with the HOB elevated 15 to 30 degrees Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
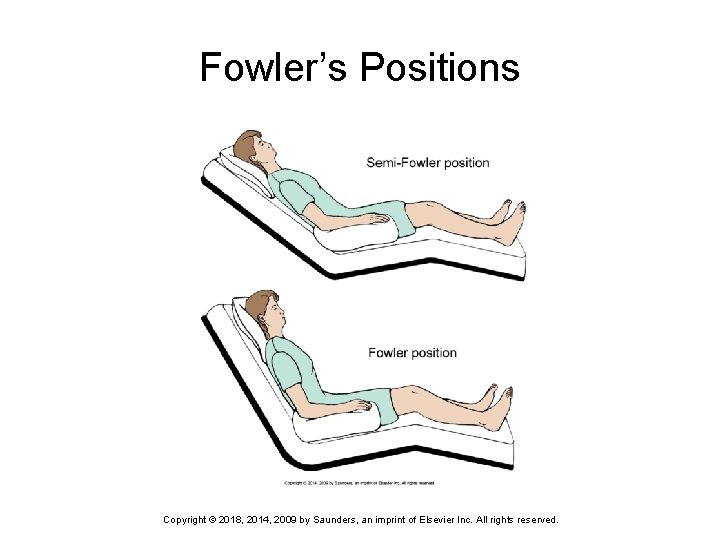
Fowler’s Positions Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
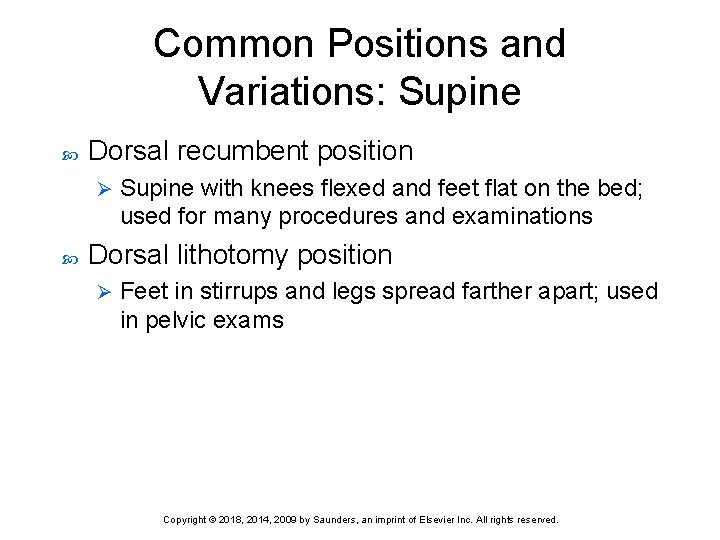
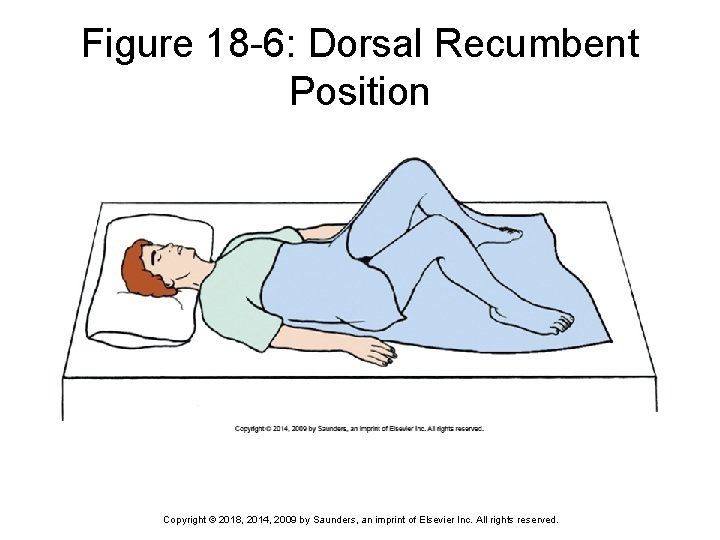
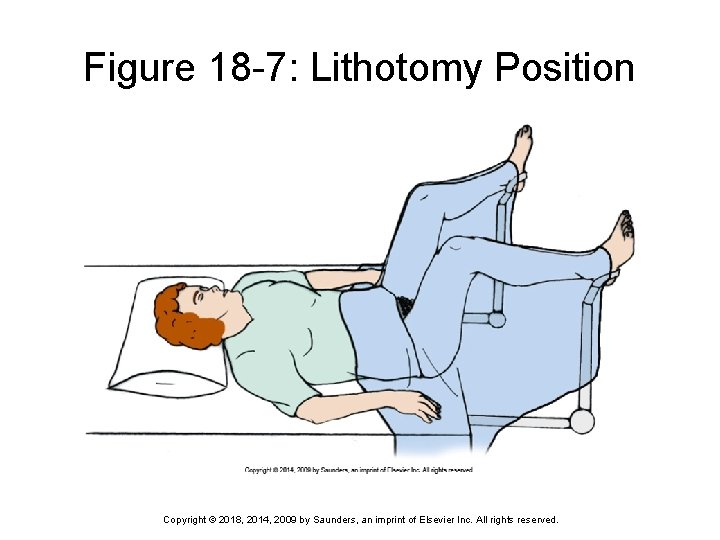
Common Positions and Variations: Supine Dorsal recumbent position Ø Supine with knees flexed and feet flat on the bed; used for many procedures and examinations Dorsal lithotomy position Ø Feet in stirrups and legs spread farther apart; used in pelvic exams Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
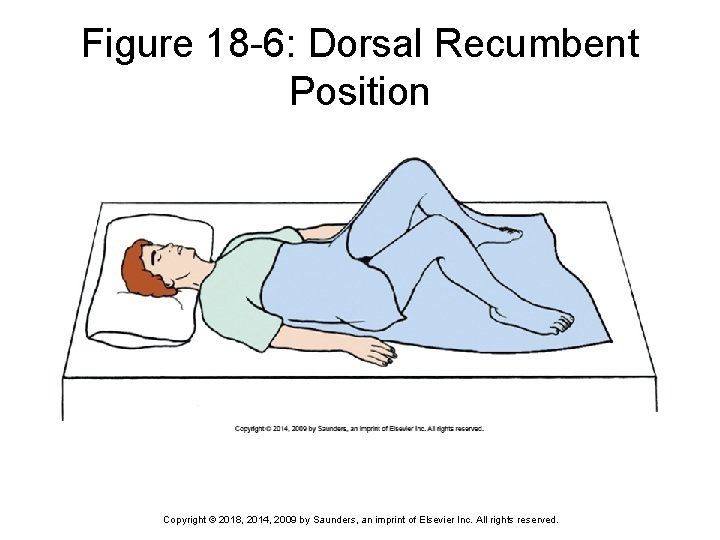
Figure 18 -6: Dorsal Recumbent Position Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
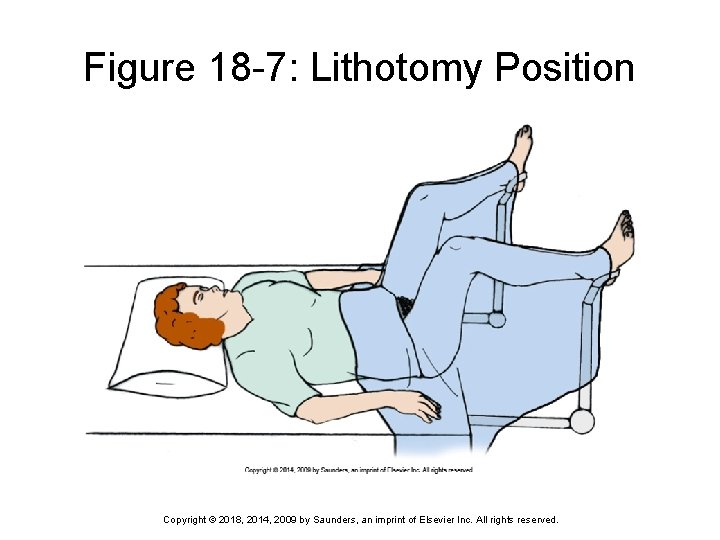
Figure 18 -7: Lithotomy Position Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
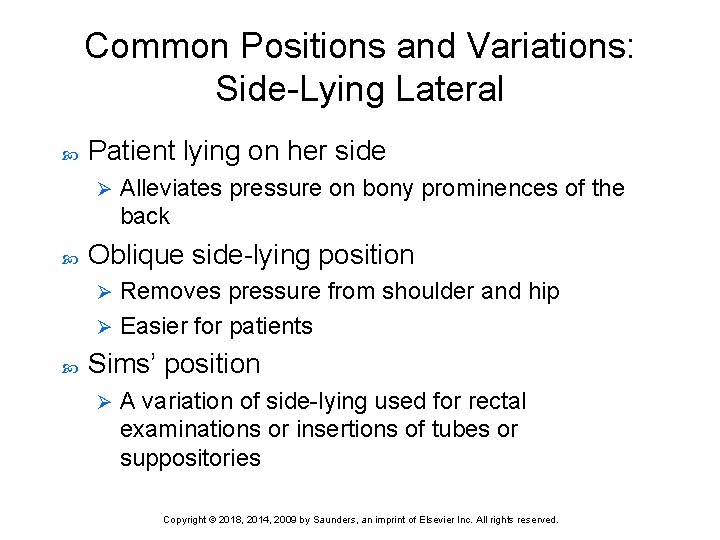
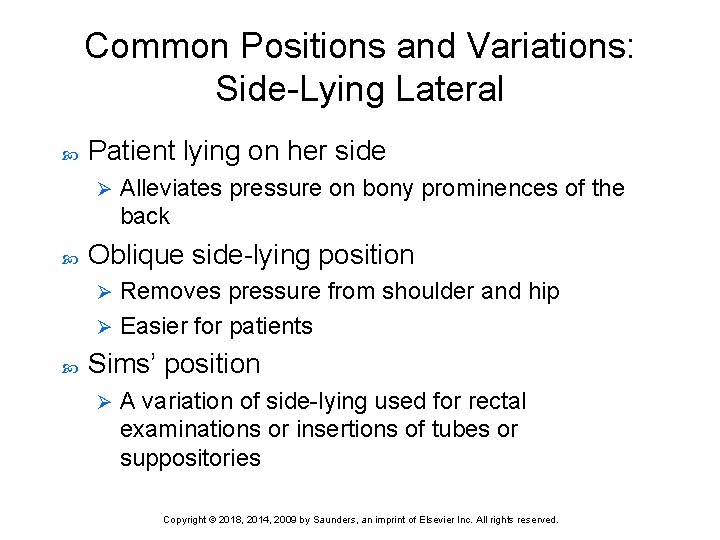
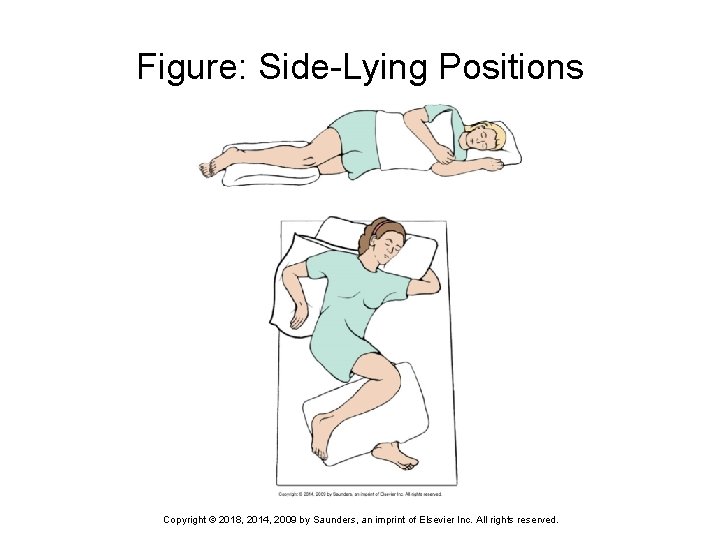
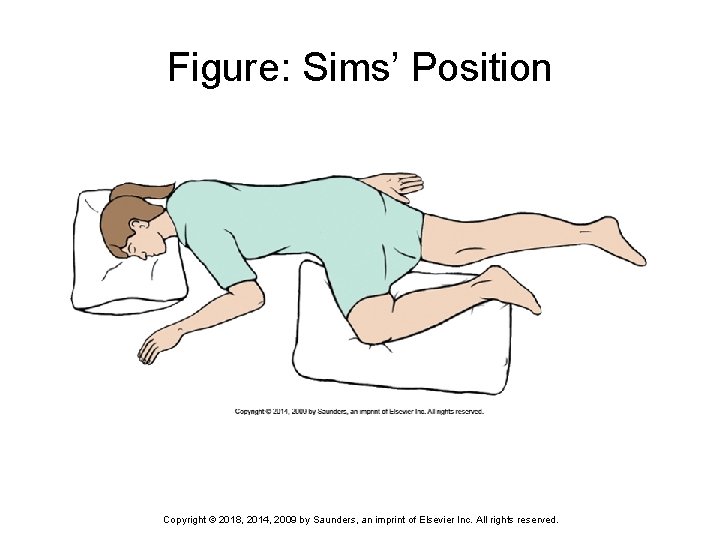
Common Positions and Variations: Side-Lying Lateral Patient lying on her side Ø Alleviates pressure on bony prominences of the back Oblique side-lying position Removes pressure from shoulder and hip Ø Easier for patients Ø Sims’ position Ø A variation of side-lying used for rectal examinations or insertions of tubes or suppositories Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
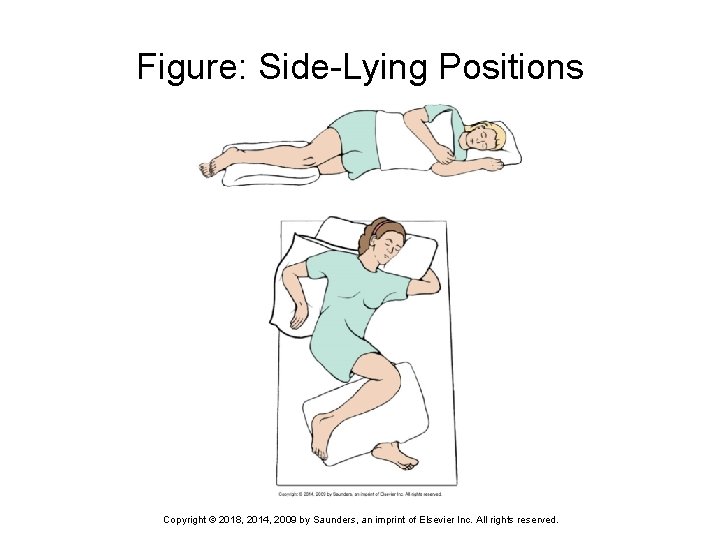
Figure: Side-Lying Positions Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
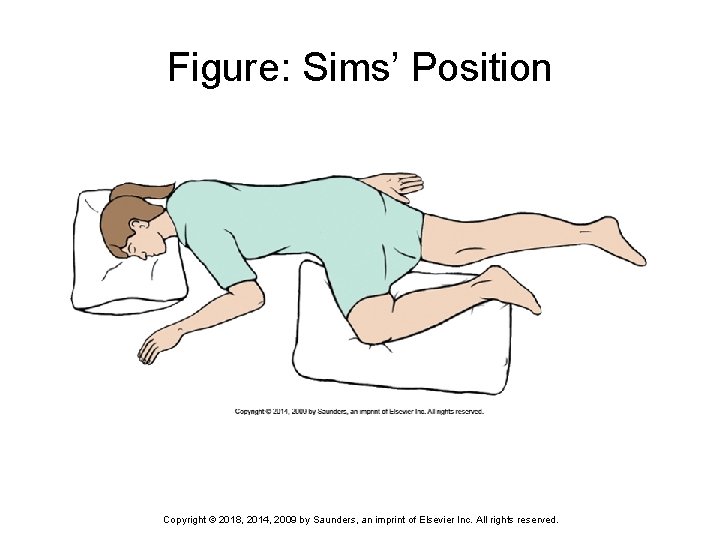
Figure: Sims’ Position Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
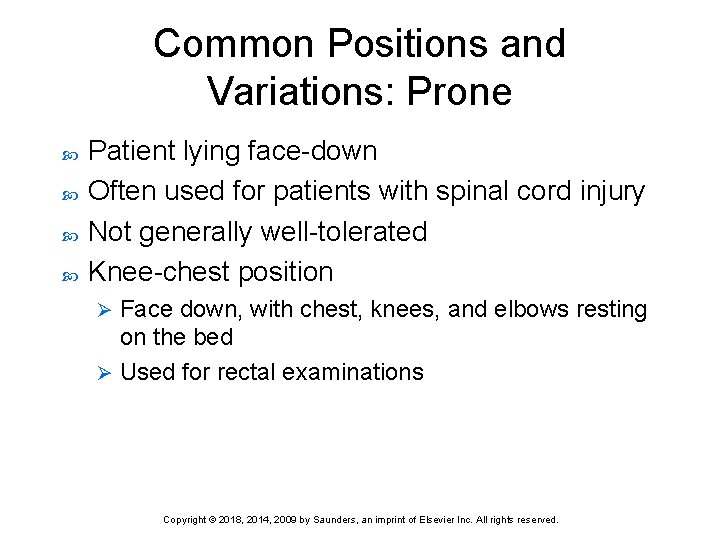
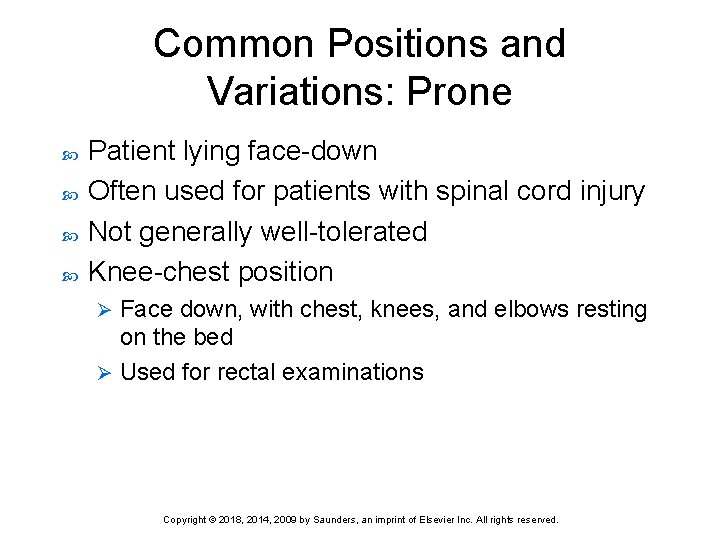
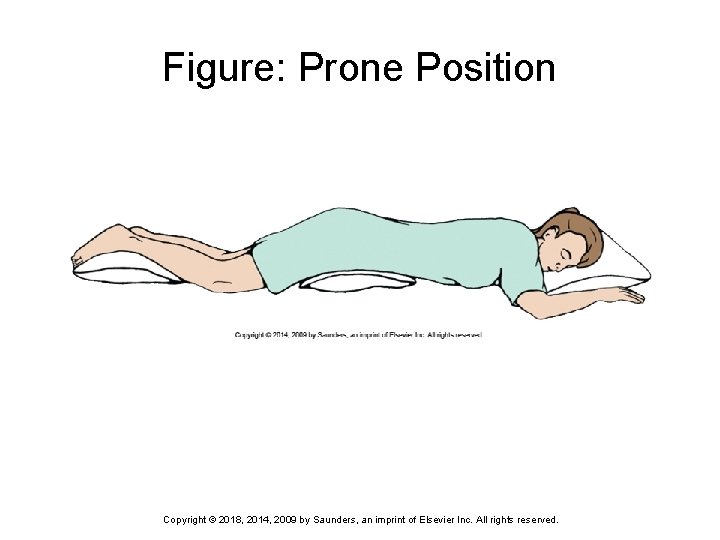
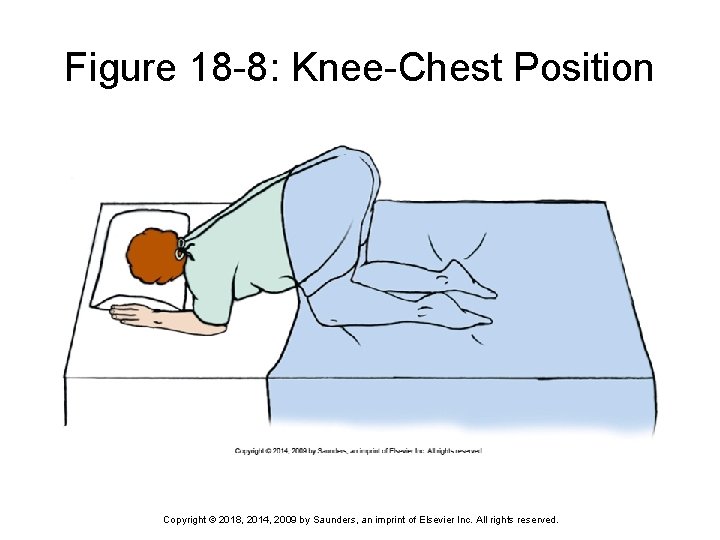
Common Positions and Variations: Prone Patient lying face-down Often used for patients with spinal cord injury Not generally well-tolerated Knee-chest position Face down, with chest, knees, and elbows resting on the bed Ø Used for rectal examinations Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
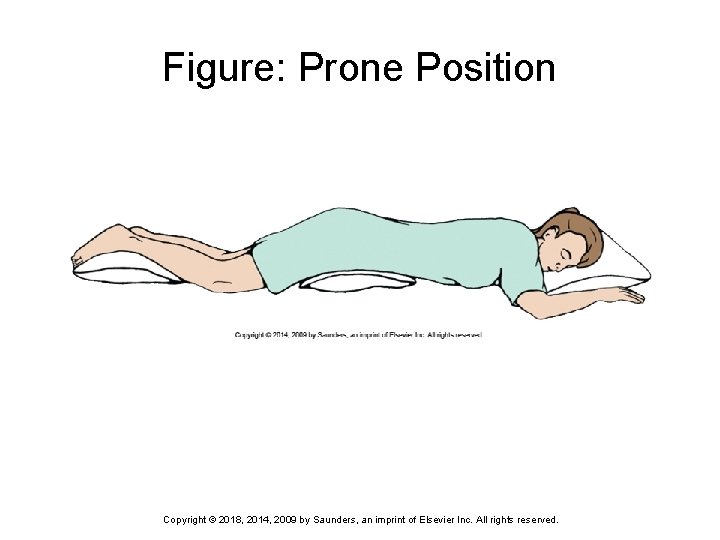
Figure: Prone Position Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
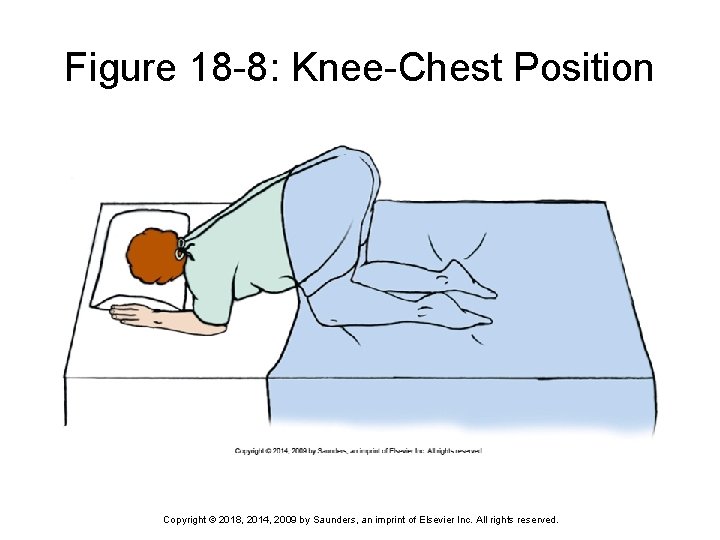
Figure 18 -8: Knee-Chest Position Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
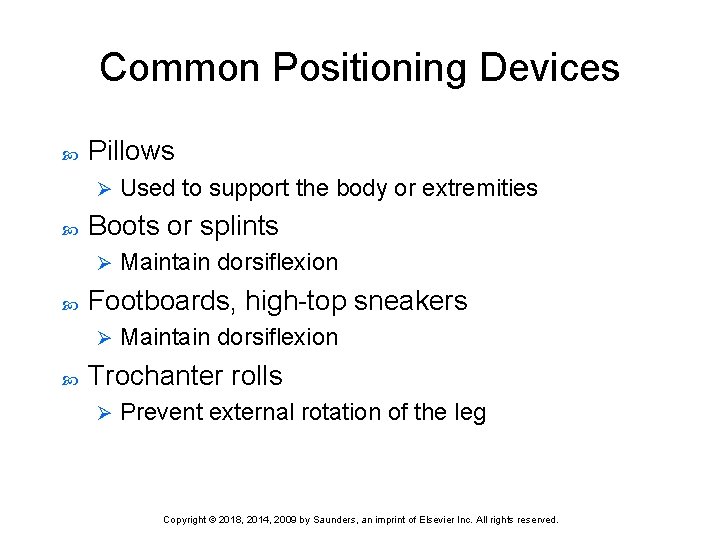
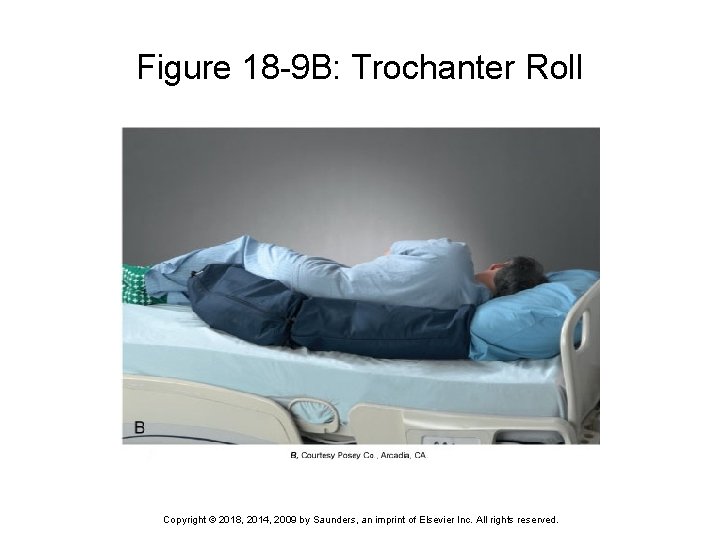
Common Positioning Devices Pillows Ø Boots or splints Ø Maintain dorsiflexion Footboards, high-top sneakers Ø Used to support the body or extremities Maintain dorsiflexion Trochanter rolls Ø Prevent external rotation of the leg Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
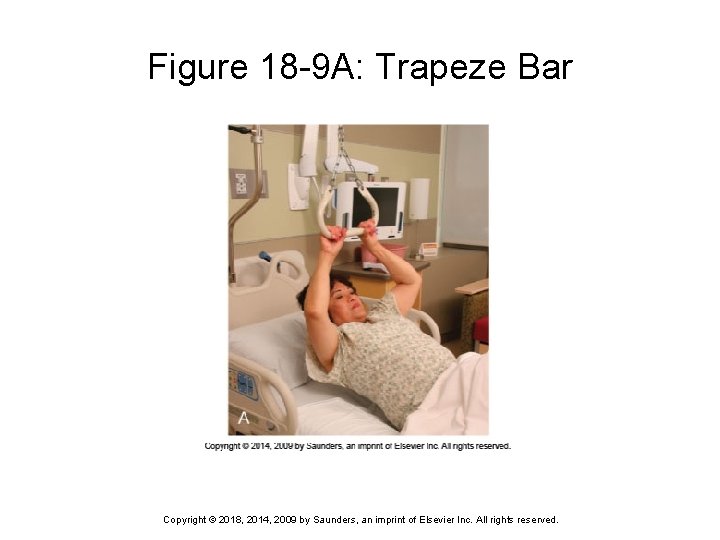
Common Positioning Devices (cont’d) Sandbags Ø Hand rolls Ø Used to immobilize an extremity, provide support, and maintain body alignment Help prevent contractures and prevent dorsiflexion of the wrist Trapeze bars, side rails, bed boards Ø Enhance patient mobility, provide patient safety, and support patient’s back Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Moving Patients Up in Bed Using a lift sheet Requires at least two people standing on opposite sides of the bed Ø Both face the bed and use the sheet to move the patient up in the bed Ø Moving the patient is performed as a coordinated effort Ø Patient is lifted and moved, not dragged Ø Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
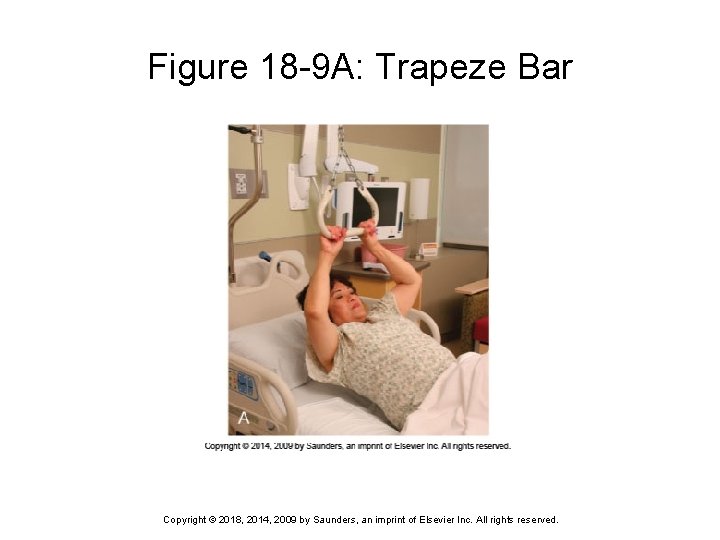
Figure 18 -9 A: Trapeze Bar Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
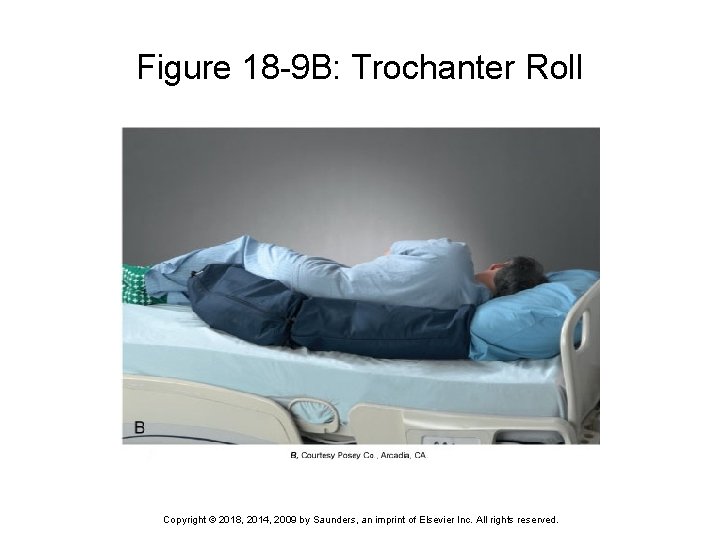
Figure 18 -9 B: Trochanter Roll Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
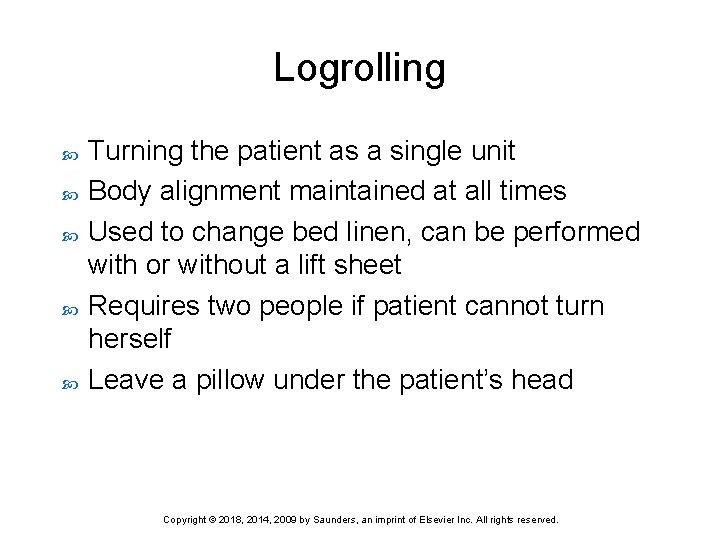
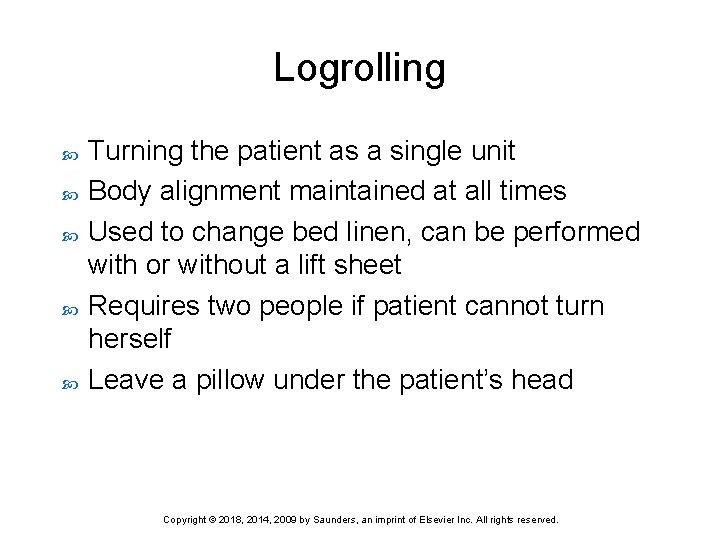
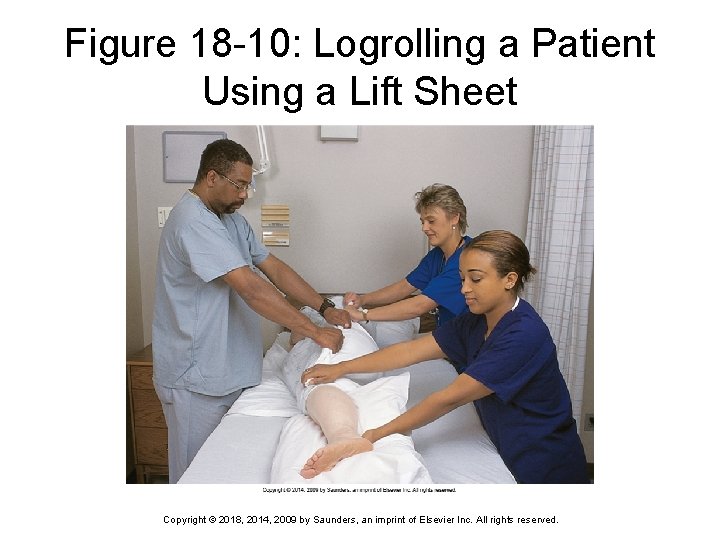
Logrolling Turning the patient as a single unit Body alignment maintained at all times Used to change bed linen, can be performed with or without a lift sheet Requires two people if patient cannot turn herself Leave a pillow under the patient’s head Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
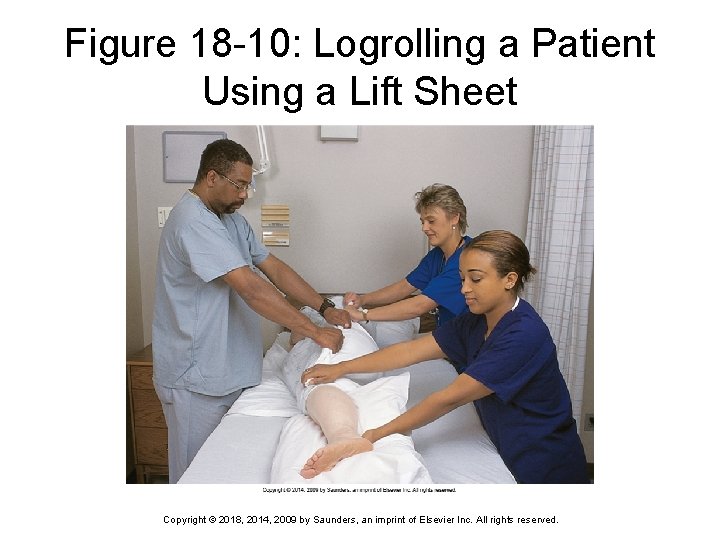
Figure 18 -10: Logrolling a Patient Using a Lift Sheet Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
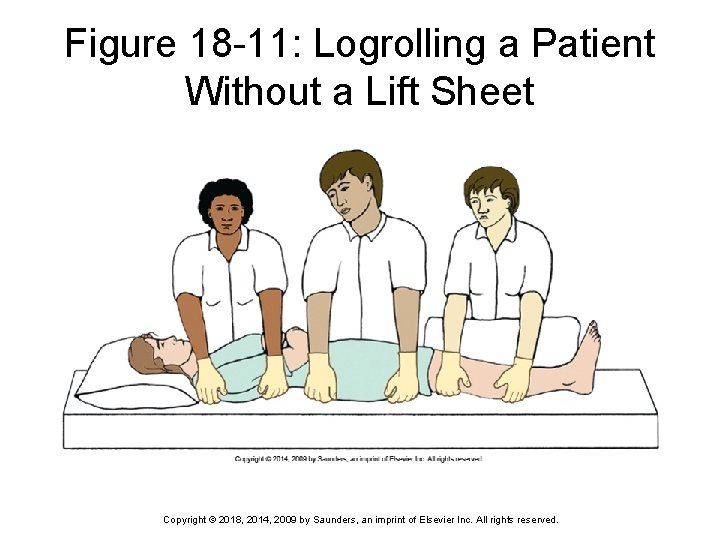
Figure 18 -11: Logrolling a Patient Without a Lift Sheet Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
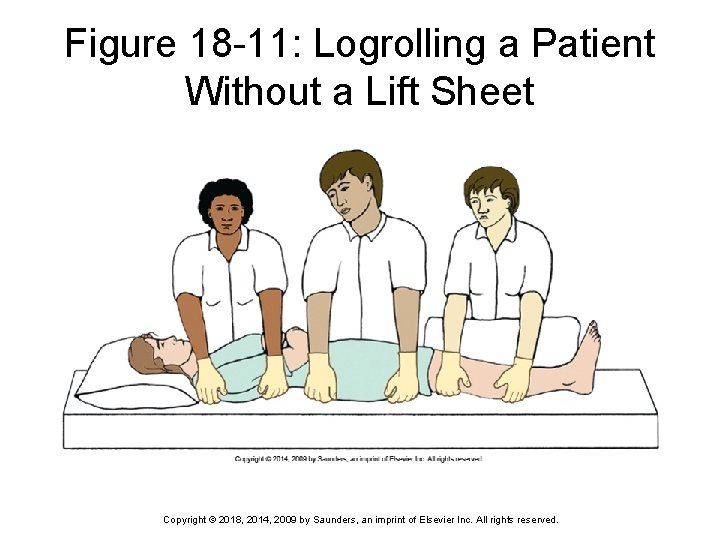
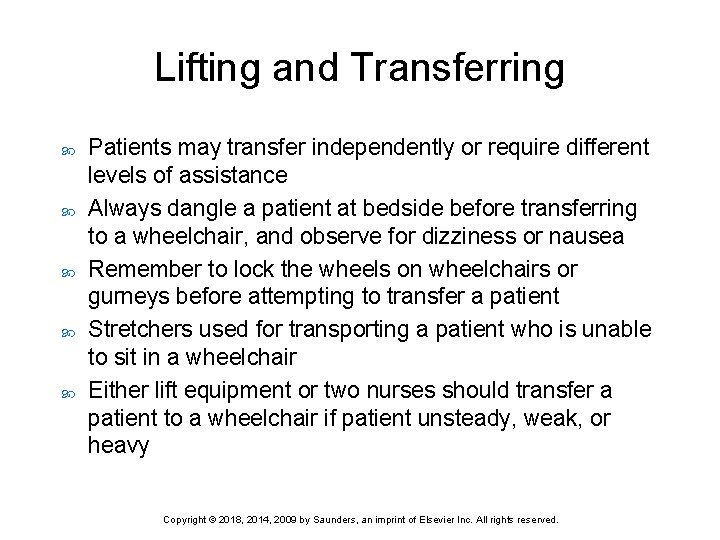
Lifting and Transferring Patients may transfer independently or require different levels of assistance Always dangle a patient at bedside before transferring to a wheelchair, and observe for dizziness or nausea Remember to lock the wheels on wheelchairs or gurneys before attempting to transfer a patient Stretchers used for transporting a patient who is unable to sit in a wheelchair Either lift equipment or two nurses should transfer a patient to a wheelchair if patient unsteady, weak, or heavy Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lifting and Transferring (cont’d) Determine how much help you will need to move or transfer the patient Get help whenever possible Make sure wheels on beds, wheelchairs, and gurneys are locked Use a transfer device when possible Dangle the patient before ambulating Use a gait belt when ambulating patients Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Transferring Devices Pull or lift sheets Mechanical lifts Roller boards Slide boards Transfer or gait belts Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 3 Dr. Tingle called the unit and asked the nurse to put his patient in Fowler’s position. Which of the following correctly describes Fowler’s position? 1) 2) 3) 4) Place the patient on her back and elevate the head of the bed 30 to 60 degrees. Place the patient on her back and elevate the head of the bed 60 to 90 degrees. Place the patient on her back and place the feet in stirrups. Place the patient in a side-lying position. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 4 Dr. Tingle is now requesting you place his patient in the prone position. Which position best describes the prone position? 1) 2) 3) 4) Place the patient on her back with knees bent. Place the patient on her abdomen with knees tucked in and elbows at a 90 -degree angle on the bed. Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Question 5 Which of the following is not a position device? 1) 2) 3) 4) Pillows Boots Footboards Blankets Copyright © 2018, 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.