Chapter 17 The Special Senses Special Senses Olfaction









- Slides: 62
Chapter 17 The Special Senses
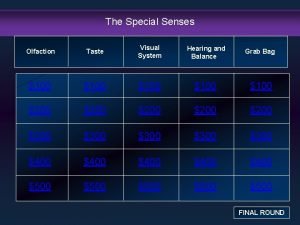
Special Senses • • Olfaction Taste Visual system Hearing and balance
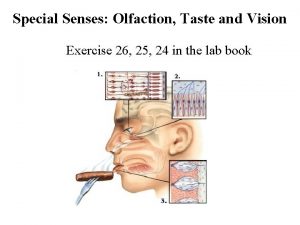
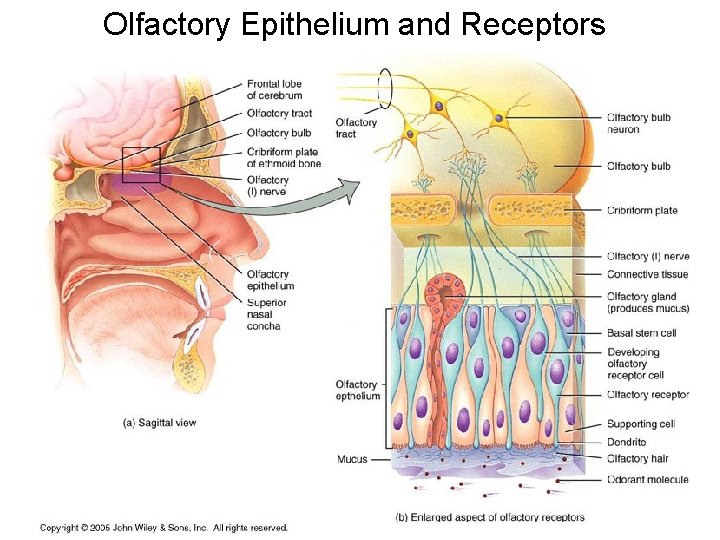
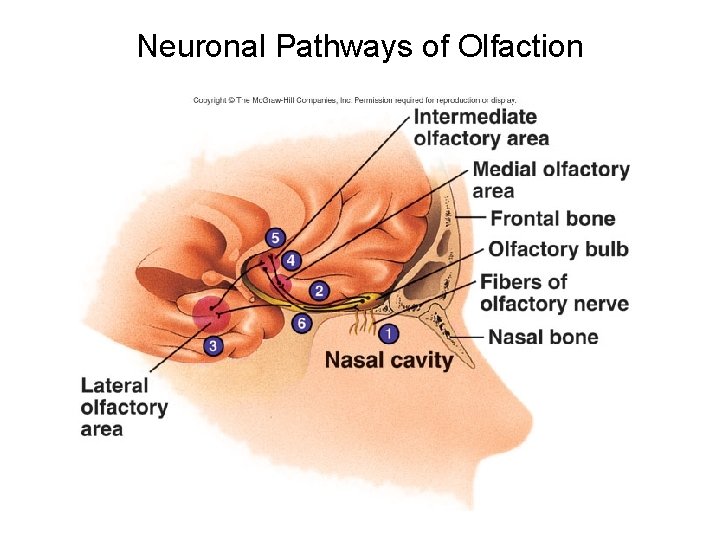
Olfactory System • Nose- olfactory epithelium-receptors, supporting cells, and basal cells • Olfactory Receptors- bipolar neuron, exposed knob shaped dendrite and axon that projects through the cribiform plate synapsing in the olfactory bulb. • Supporting cells- columnar epithelium-mucous membrane in the lining of the nose. • Basal cells- stem cells underneath the supporting cells that divide to produce new olfactory receptor cells. • Olfactory nerve (I)- olfactory receptor axons bundle and form the olfactory nerve which terminate in the olfactory bulb. Axons of olfactory bulb form the olfactory tract that projects to the primary olfactory area (inf. and med. temporal lobe), frontal lobe, limbic system, and hypothalamus.
Olfactory Physiology • Olfactory receptors respond to odors and produce a generator potential that triggers an action potential in olfactory nerves that terminate in the olfactory bulb. • Odorant--binds to a G-protein linked receptor--biochemical cascade--opening Na+ channels--depolarizing generator potential--generation of action potential. • Adaptation- Occurs rapidly in olfactory receptors. There is a component of olfactory perception that adapts more slowly and is likely in the brain.
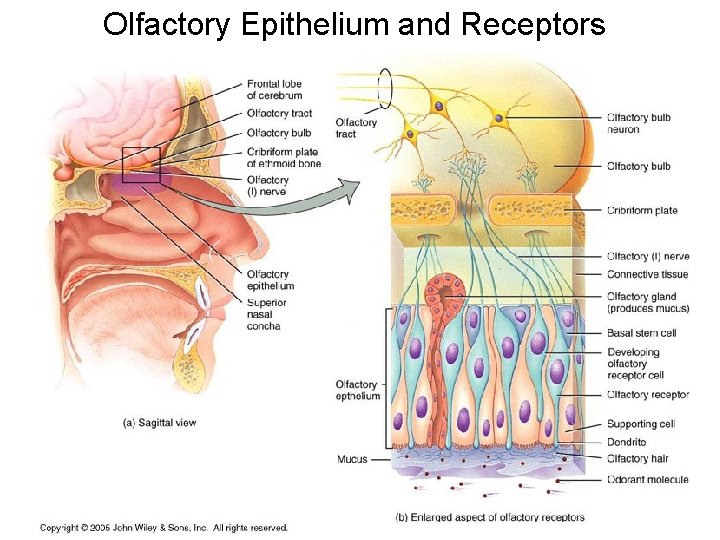
Olfactory Epithelium and Receptors
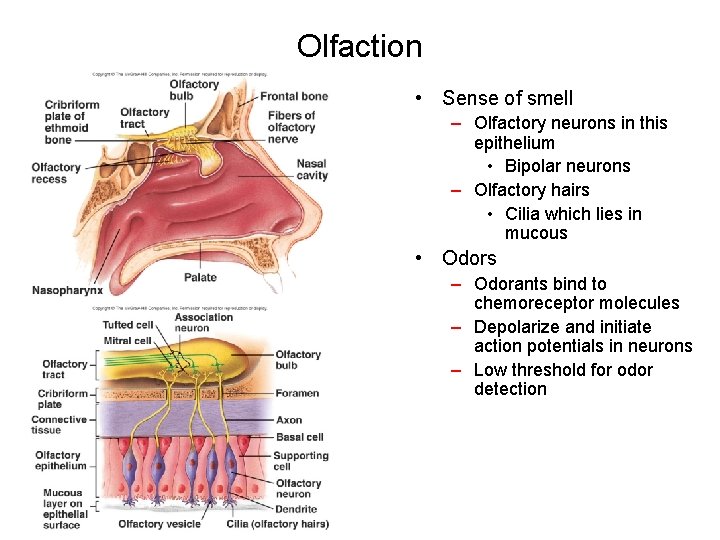
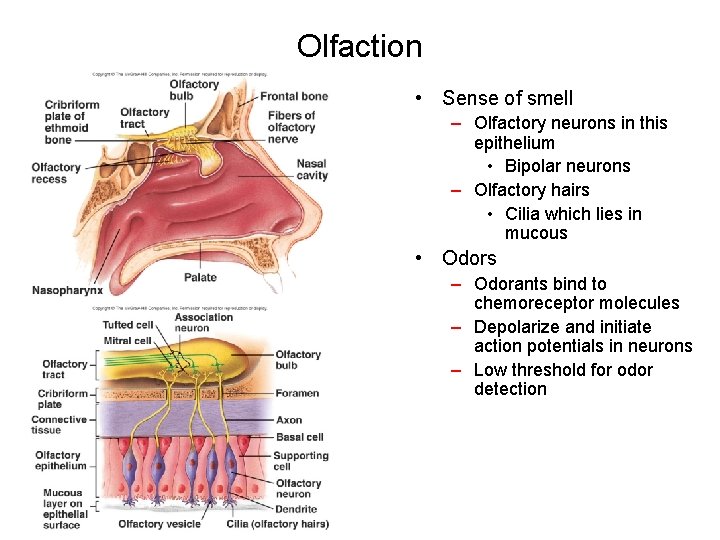
Olfaction • Sense of smell – Olfactory neurons in this epithelium • Bipolar neurons – Olfactory hairs • Cilia which lies in mucous • Odors – Odorants bind to chemoreceptor molecules – Depolarize and initiate action potentials in neurons – Low threshold for odor detection

Figure 16. 8
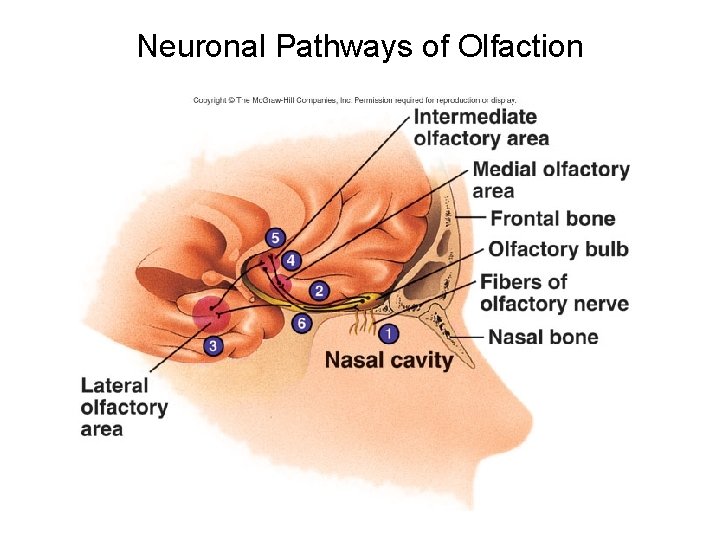
Neuronal Pathways of Olfaction
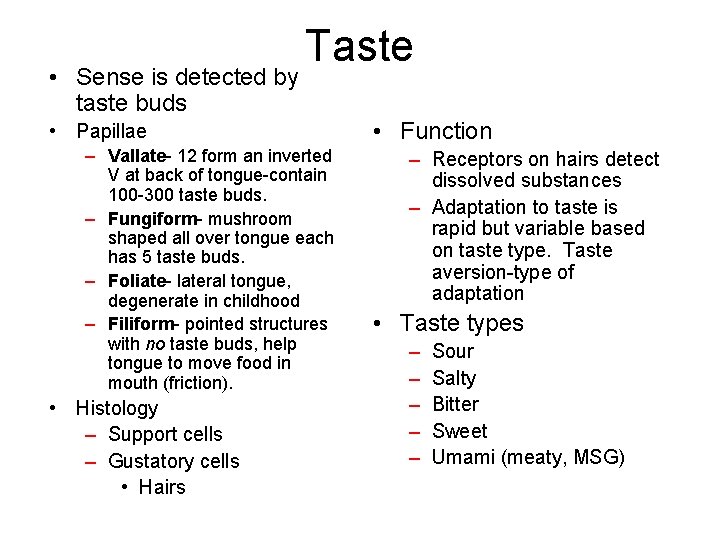
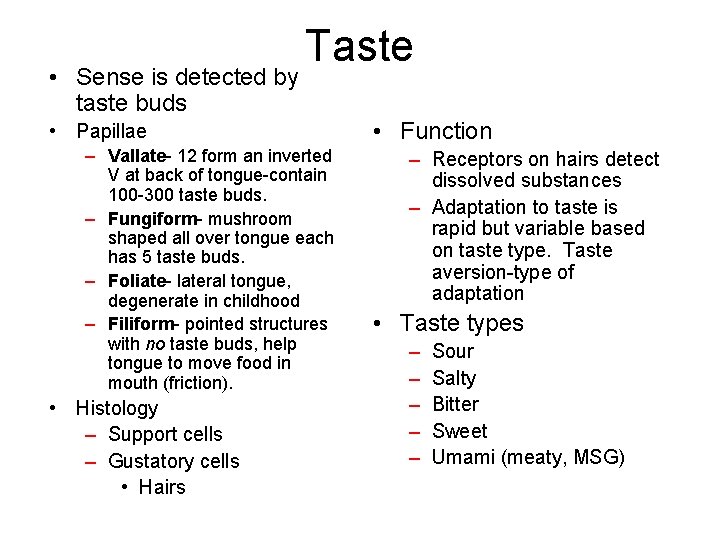
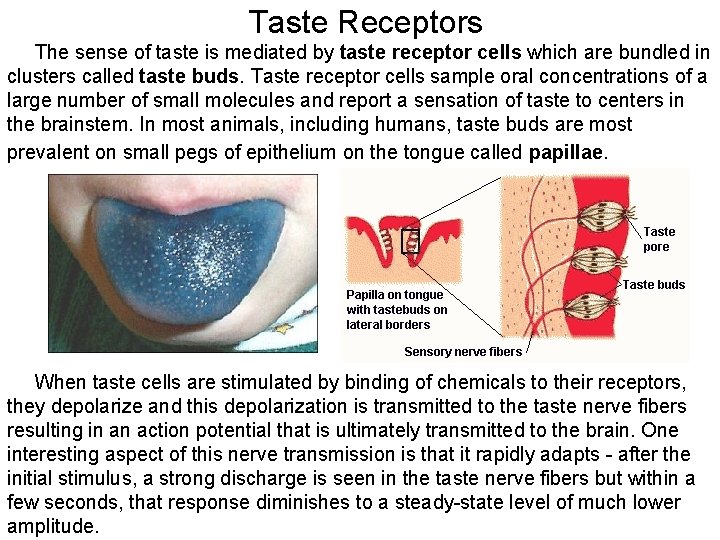
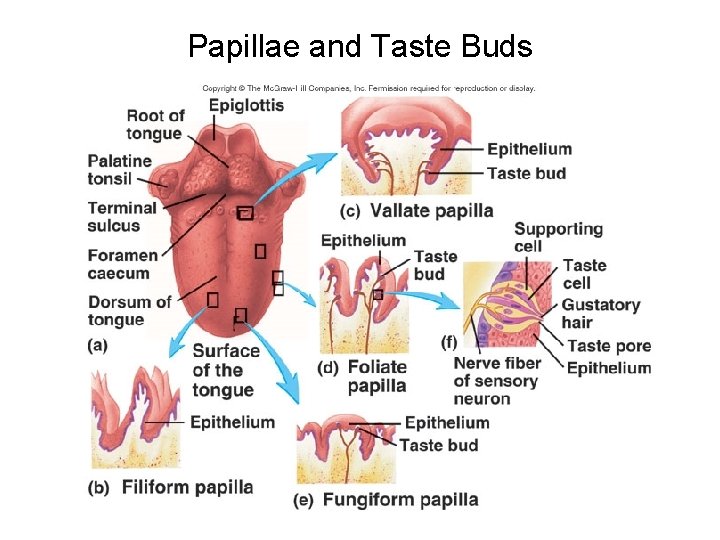
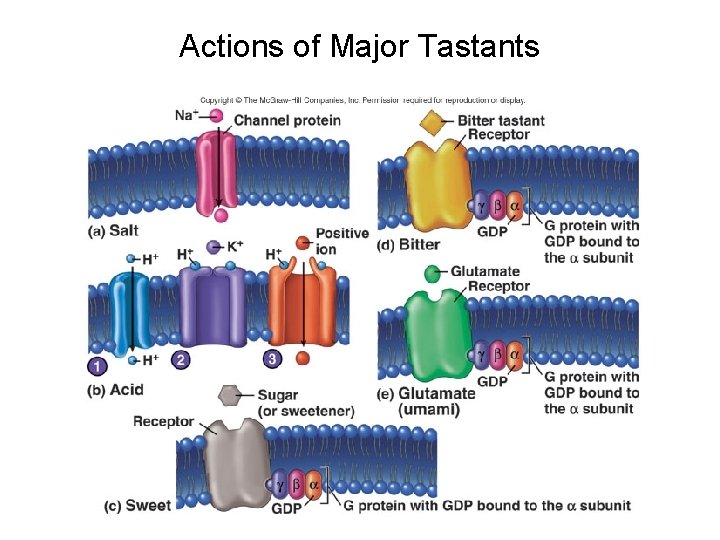
• Sense is detected by taste buds Taste • Papillae – Vallate- 12 form an inverted V at back of tongue-contain 100 -300 taste buds. – Fungiform- mushroom shaped all over tongue each has 5 taste buds. – Foliate- lateral tongue, degenerate in childhood – Filiform- pointed structures with no taste buds, help tongue to move food in mouth (friction). • Histology – Support cells – Gustatory cells • Hairs • Function – Receptors on hairs detect dissolved substances – Adaptation to taste is rapid but variable based on taste type. Taste aversion-type of adaptation • Taste types – – – Sour Salty Bitter Sweet Umami (meaty, MSG)
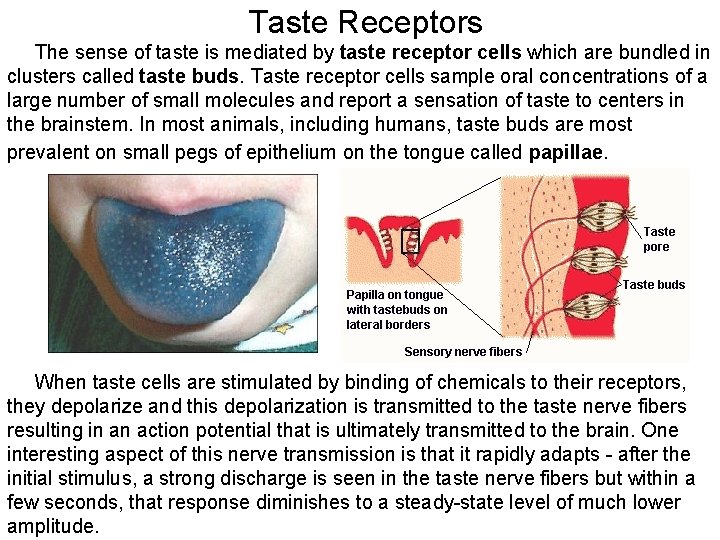
Taste Receptors The sense of taste is mediated by taste receptor cells which are bundled in clusters called taste buds. Taste receptor cells sample oral concentrations of a large number of small molecules and report a sensation of taste to centers in the brainstem. In most animals, including humans, taste buds are most prevalent on small pegs of epithelium on the tongue called papillae. When taste cells are stimulated by binding of chemicals to their receptors, they depolarize and this depolarization is transmitted to the taste nerve fibers resulting in an action potential that is ultimately transmitted to the brain. One interesting aspect of this nerve transmission is that it rapidly adapts - after the initial stimulus, a strong discharge is seen in the taste nerve fibers but within a few seconds, that response diminishes to a steady-state level of much lower amplitude.

Gustatory (taste) Receptors
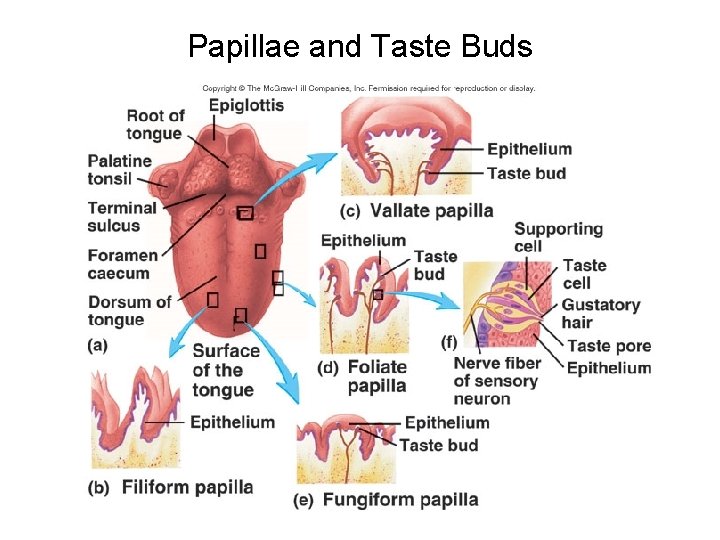
Papillae and Taste Buds
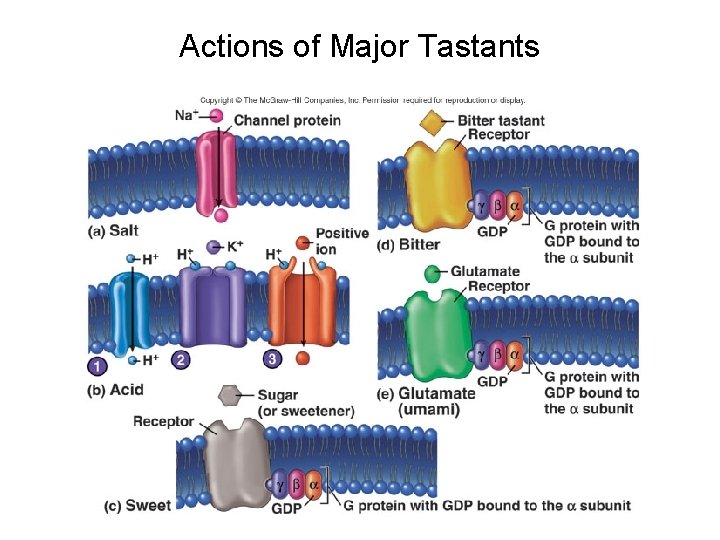
Actions of Major Tastants
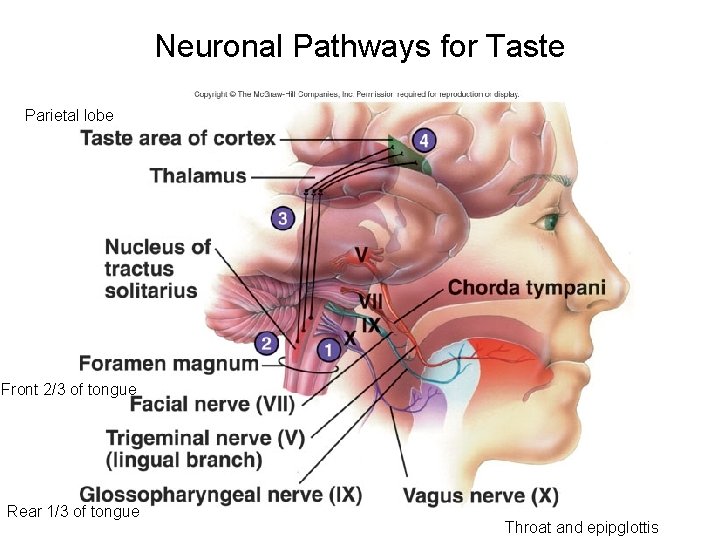
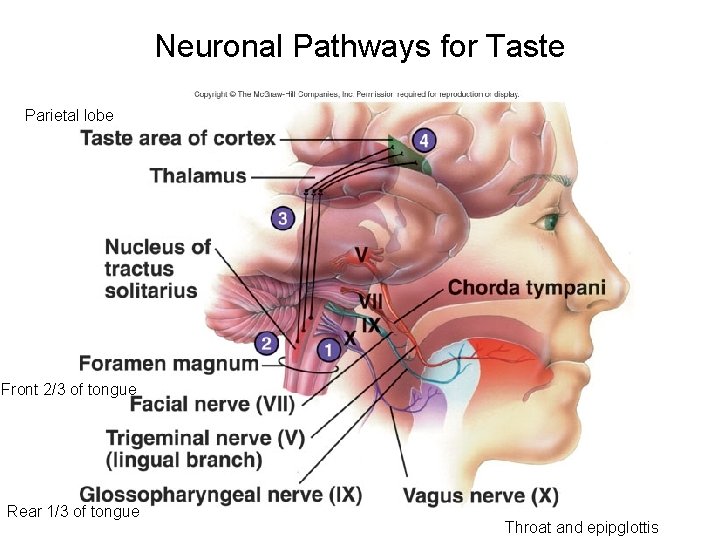
Neuronal Pathways for Taste Parietal lobe Front 2/3 of tongue Rear 1/3 of tongue Throat and epipglottis
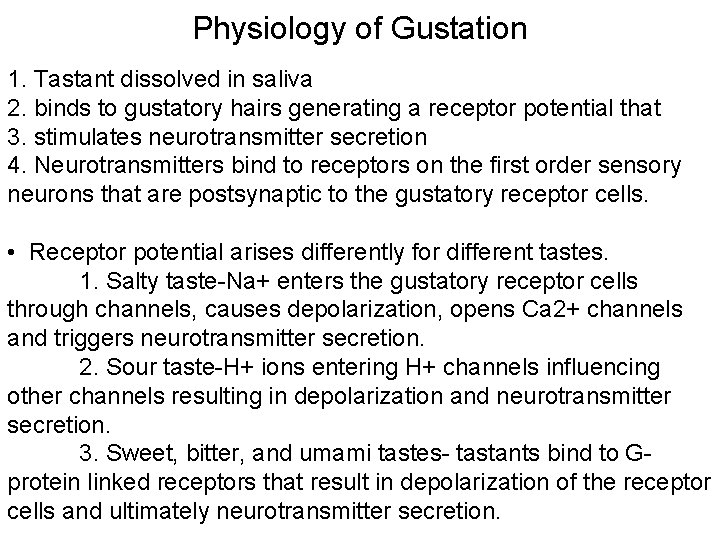
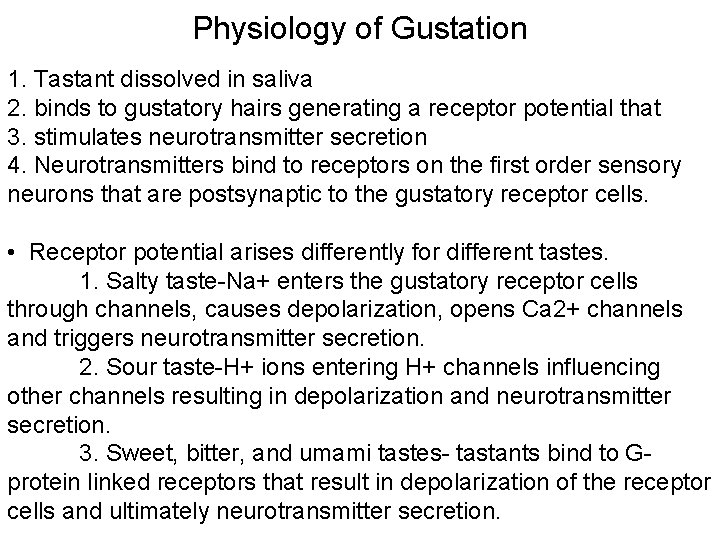
Physiology of Gustation 1. Tastant dissolved in saliva 2. binds to gustatory hairs generating a receptor potential that 3. stimulates neurotransmitter secretion 4. Neurotransmitters bind to receptors on the first order sensory neurons that are postsynaptic to the gustatory receptor cells. • Receptor potential arises differently for different tastes. 1. Salty taste-Na+ enters the gustatory receptor cells through channels, causes depolarization, opens Ca 2+ channels and triggers neurotransmitter secretion. 2. Sour taste-H+ ions entering H+ channels influencing other channels resulting in depolarization and neurotransmitter secretion. 3. Sweet, bitter, and umami tastes- tastants bind to Gprotein linked receptors that result in depolarization of the receptor cells and ultimately neurotransmitter secretion.
Visual System • Eye • Accessory structures – Eyebrows, eyelids, eyelashes, tear glands – Protect eyes from sunlight and damaging particles • Optic nerve (II) – Tracts – Pathways • Eyes respond to light and initiate afferent action potentials
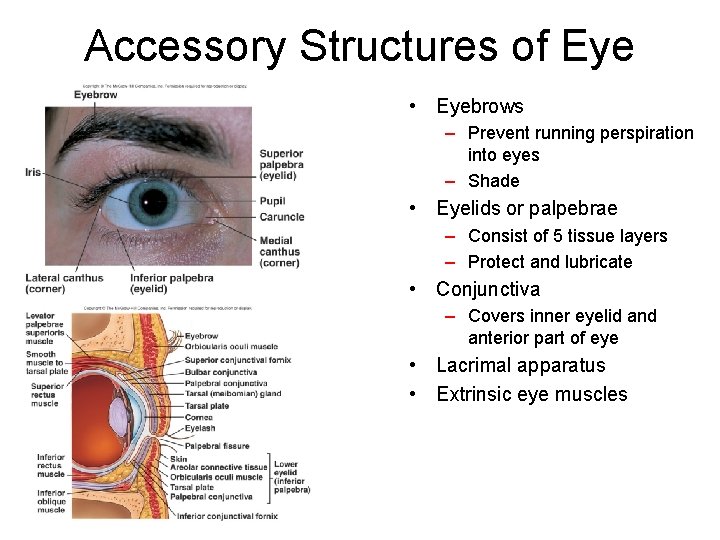
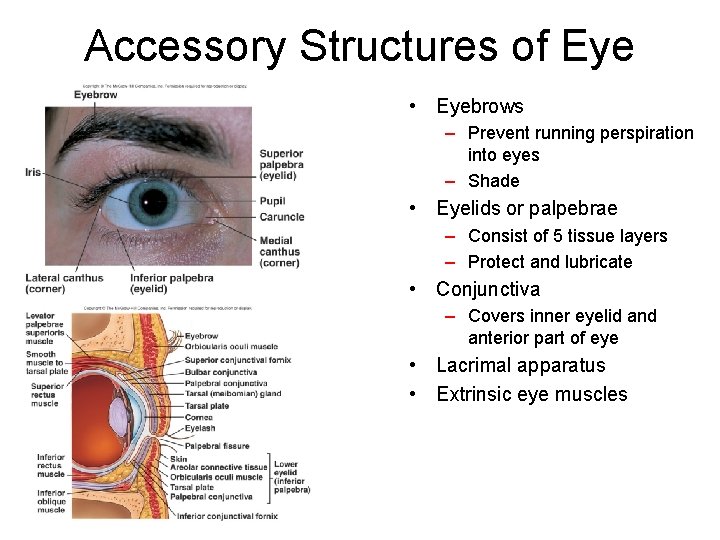
Accessory Structures of Eye • Eyebrows – Prevent running perspiration into eyes – Shade • Eyelids or palpebrae – Consist of 5 tissue layers – Protect and lubricate • Conjunctiva – Covers inner eyelid anterior part of eye • Lacrimal apparatus • Extrinsic eye muscles
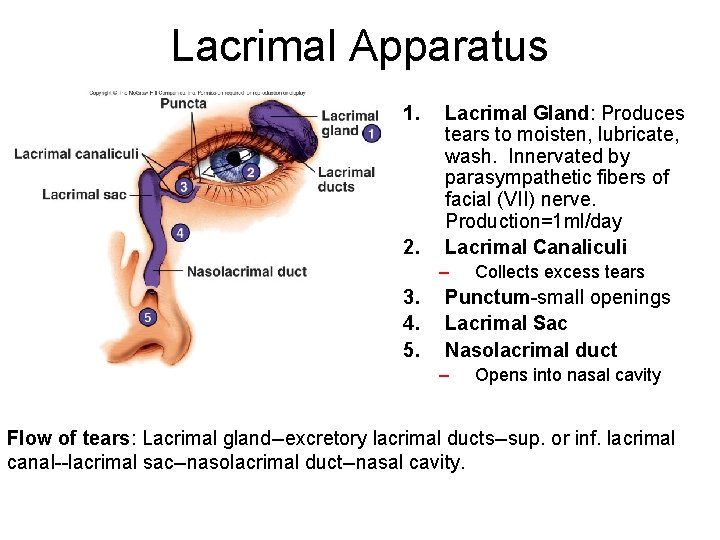
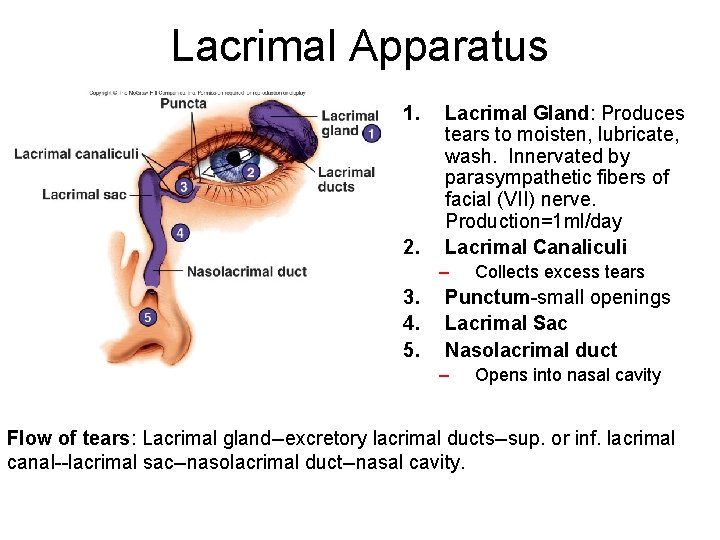
Lacrimal Apparatus 1. 2. Lacrimal Gland: Produces tears to moisten, lubricate, wash. Innervated by parasympathetic fibers of facial (VII) nerve. Production=1 ml/day Lacrimal Canaliculi – 3. 4. 5. Collects excess tears Punctum-small openings Lacrimal Sac Nasolacrimal duct – Opens into nasal cavity Flow of tears: Lacrimal gland--excretory lacrimal ducts--sup. or inf. lacrimal canal--lacrimal sac--nasolacrimal duct--nasal cavity.
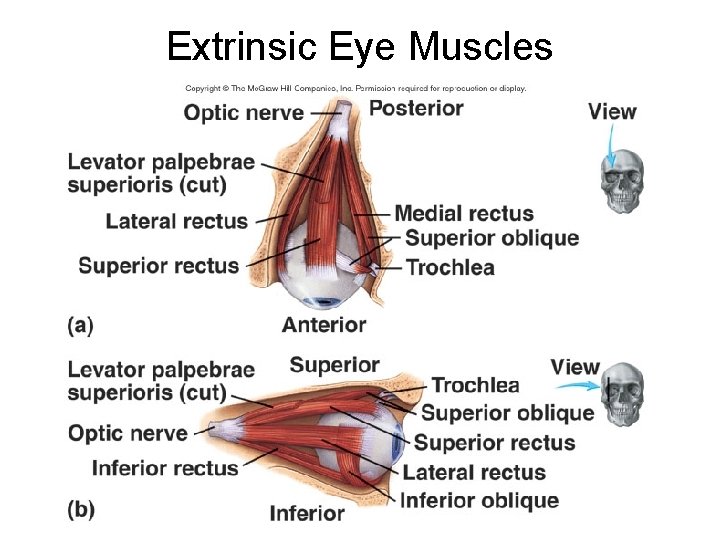
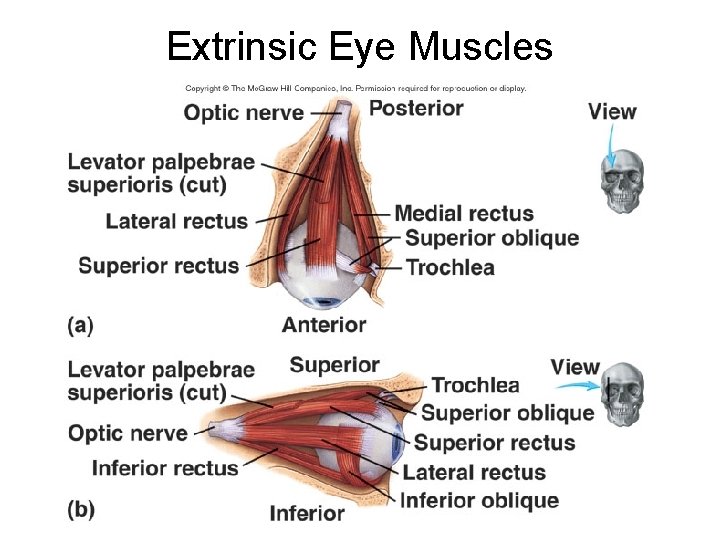
Extrinsic Eye Muscles
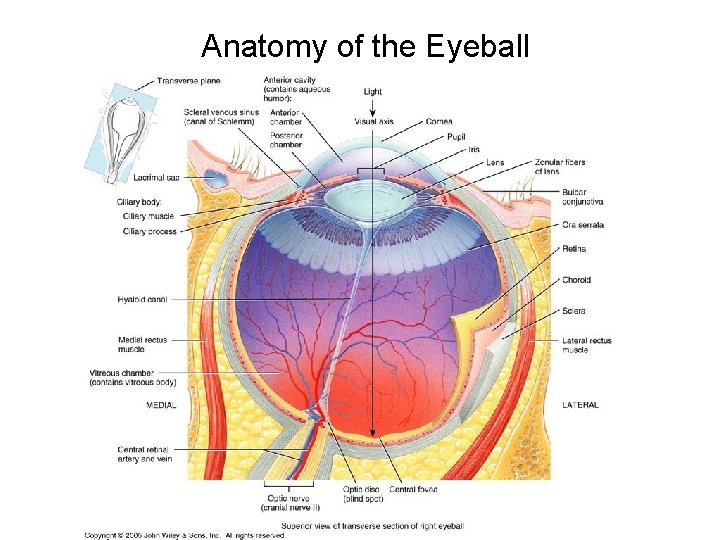
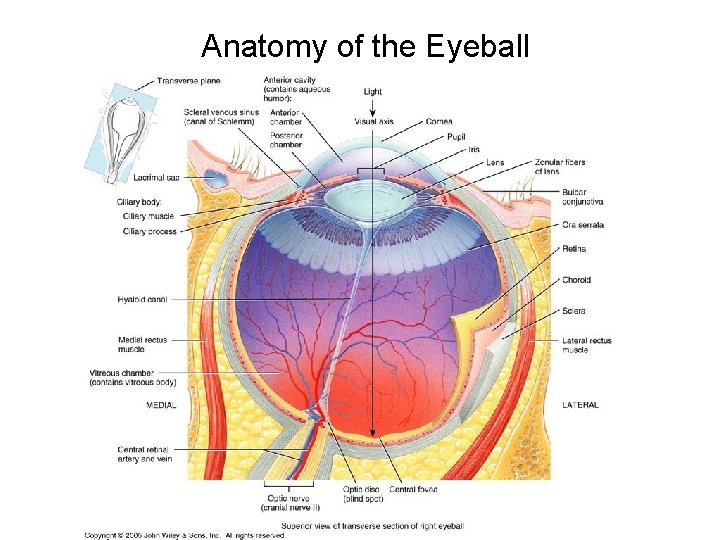
Anatomy of the Eyeball
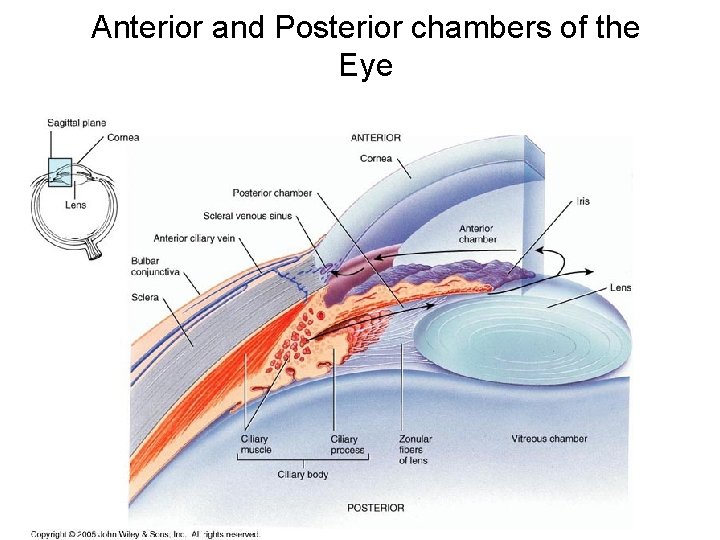
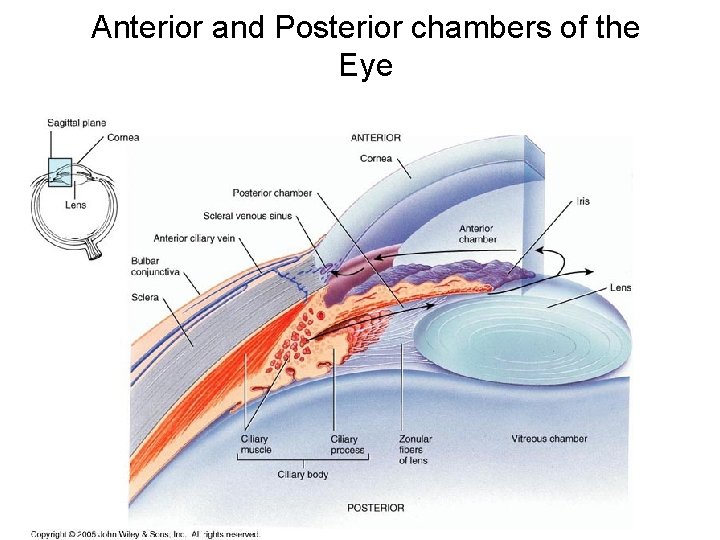
Anterior and Posterior chambers of the Eye
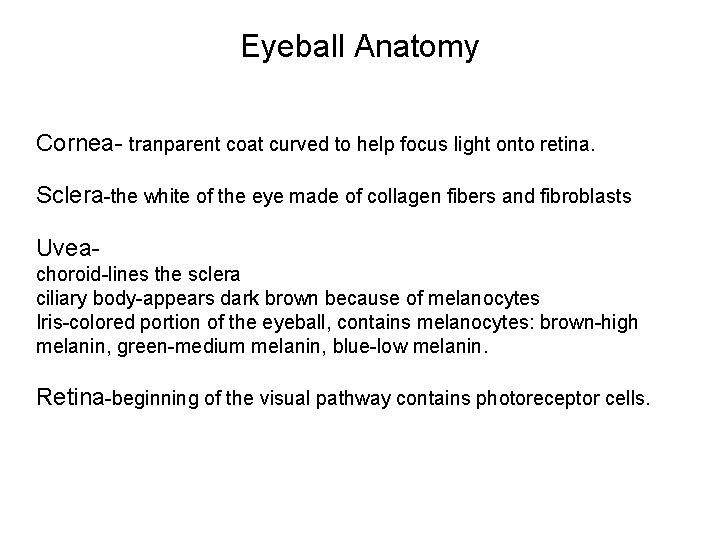
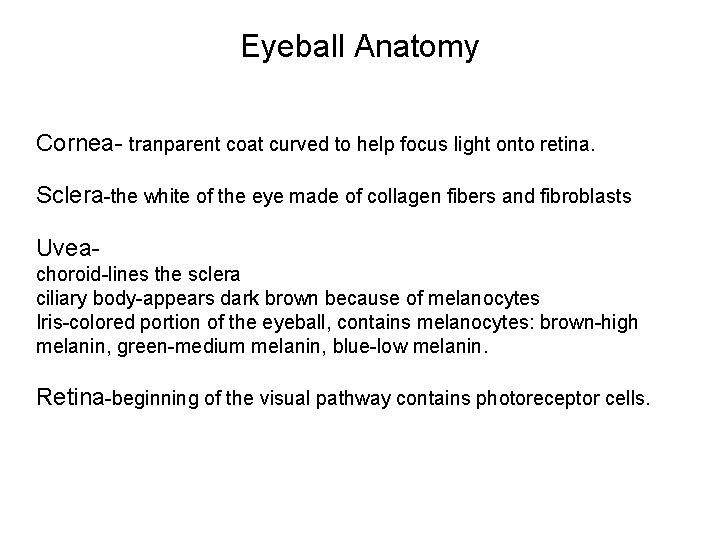
Eyeball Anatomy Cornea- tranparent coat curved to help focus light onto retina. Sclera-the white of the eye made of collagen fibers and fibroblasts Uveachoroid-lines the sclera ciliary body-appears dark brown because of melanocytes Iris-colored portion of the eyeball, contains melanocytes: brown-high melanin, green-medium melanin, blue-low melanin. Retina-beginning of the visual pathway contains photoreceptor cells.
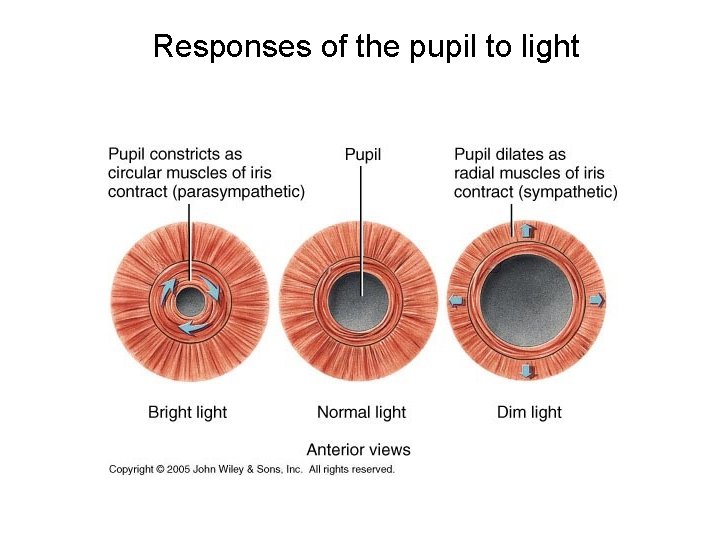
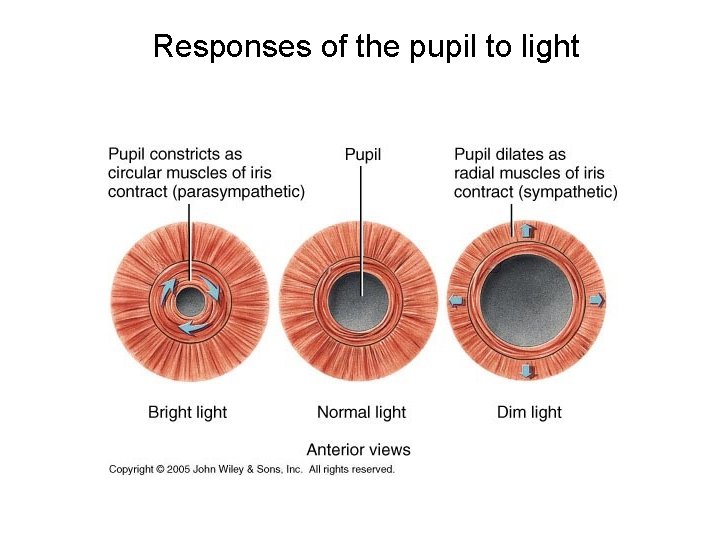
Responses of the pupil to light
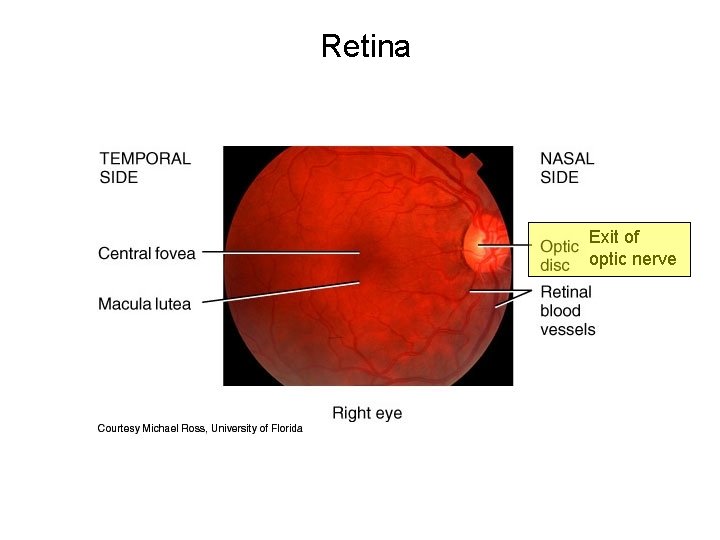
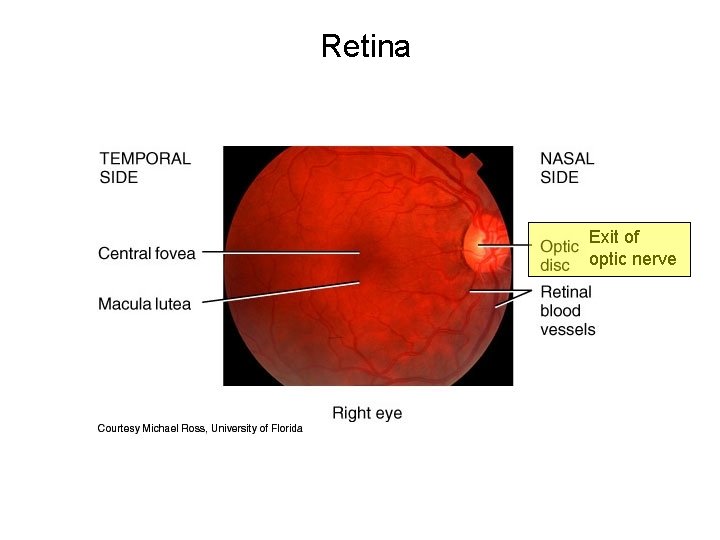
Retina Exit of optic nerve

The Retina Four kinds of light-sensitive receptors are found in the retina: ・rods ・three kinds of cones, each "tuned" to absorb light from a portion of the spectrum of visible light ・cones that absorb long-wavelength light (red) ・cones that absorb middle-wavelength light (green) ・cones that absorb short-wavelength light (blue) Each type of receptor has its own special pigment for absorbing light. Each consists of: ・ a transmembrane protein called opsin coupled to・the prosthetic group retinal. Retinal is a derivative of vitamin A (which explains why night blindness is one sign of vitamin A deficiency) and is used by all four types of receptors. The retina also contains a complex array of interneurons: ・bipolar cells and ganglion cells that together form a path from the rods and cones to the brain・a complex array of other interneurons that form synapses with the bipolar and ganglion cells and modify their activity. Ganglion cells are always active. Even in the dark they generate trains of action potentials and conduct them back to the brain along the optic nerve. Vision is based on the modulation of these nerve impulses. There is not the direct relationship between visual stimulus and an action potential that is found in the senses of hearing, taste, and smell. In fact, action potentials are not even generated in the rods and cones.
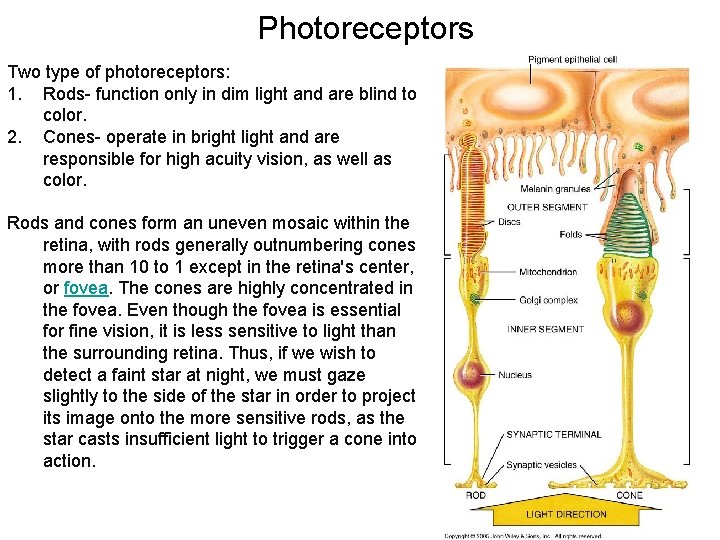
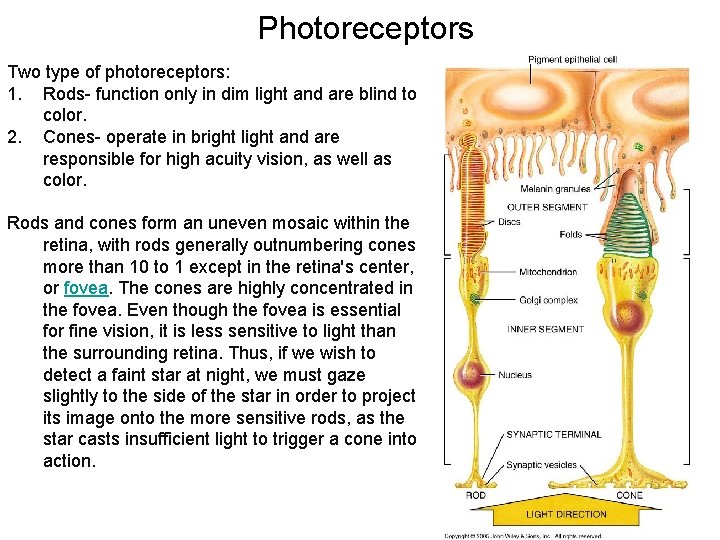
Photoreceptors Two type of photoreceptors: 1. Rods- function only in dim light and are blind to color. 2. Cones- operate in bright light and are responsible for high acuity vision, as well as color. Rods and cones form an uneven mosaic within the retina, with rods generally outnumbering cones more than 10 to 1 except in the retina's center, or fovea. The cones are highly concentrated in the fovea. Even though the fovea is essential for fine vision, it is less sensitive to light than the surrounding retina. Thus, if we wish to detect a faint star at night, we must gaze slightly to the side of the star in order to project its image onto the more sensitive rods, as the star casts insufficient light to trigger a cone into action.
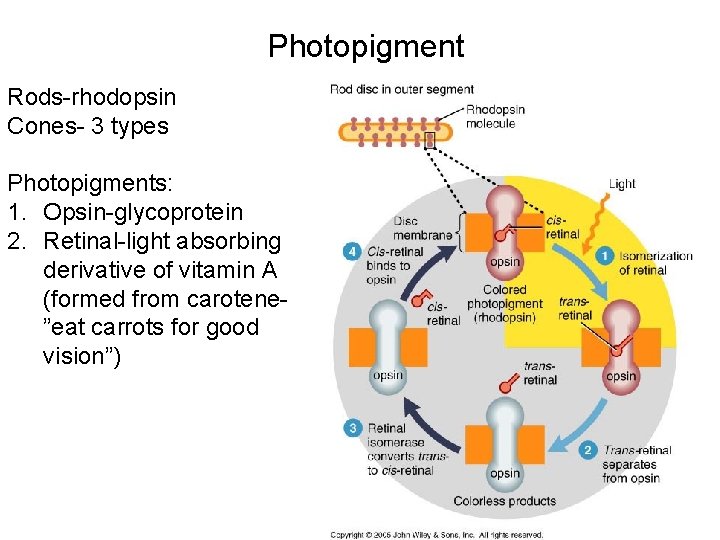
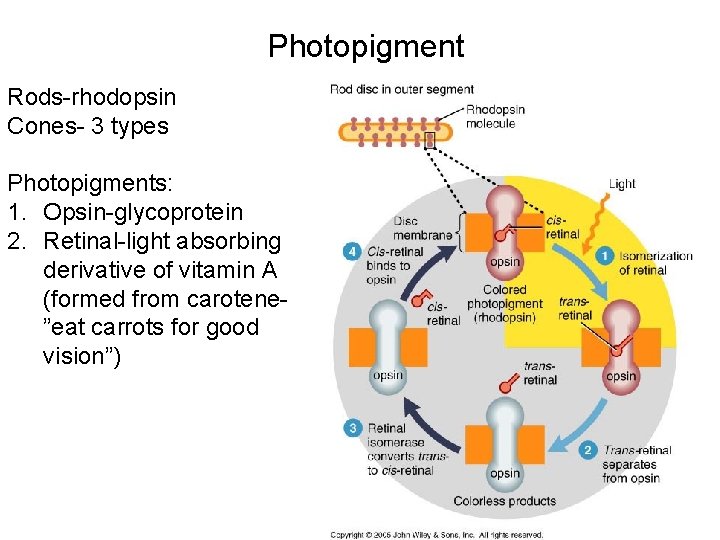
Photopigment Rods-rhodopsin Cones- 3 types Photopigments: 1. Opsin-glycoprotein 2. Retinal-light absorbing derivative of vitamin A (formed from carotene”eat carrots for good vision”)
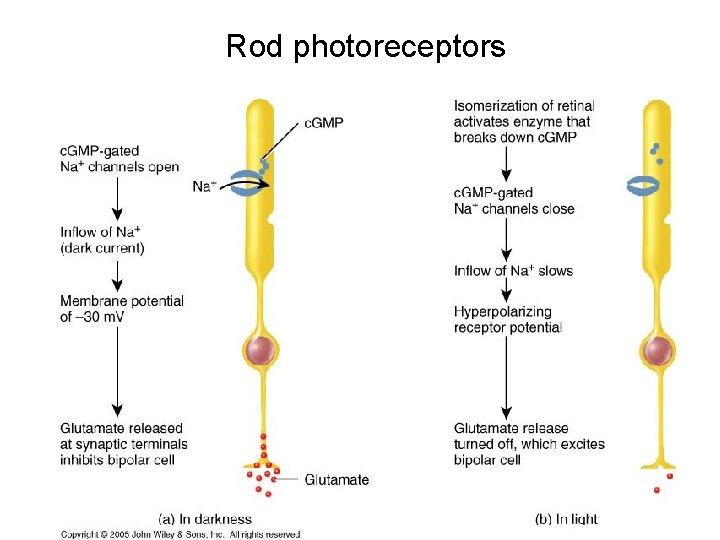
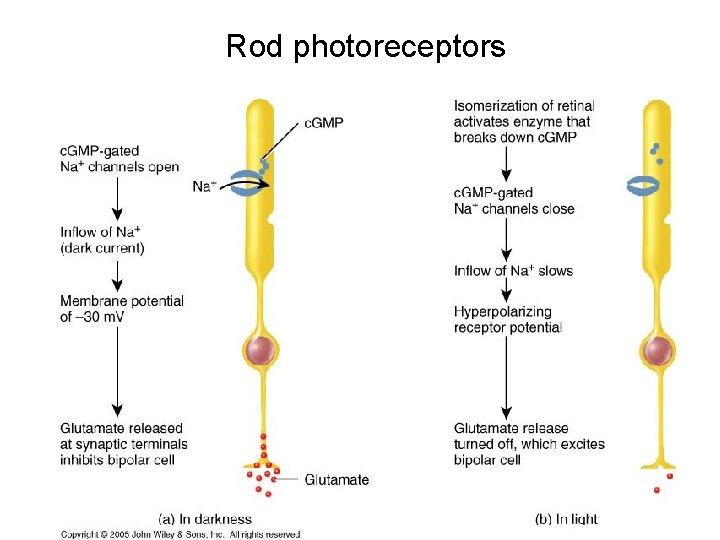
Rod photoreceptors
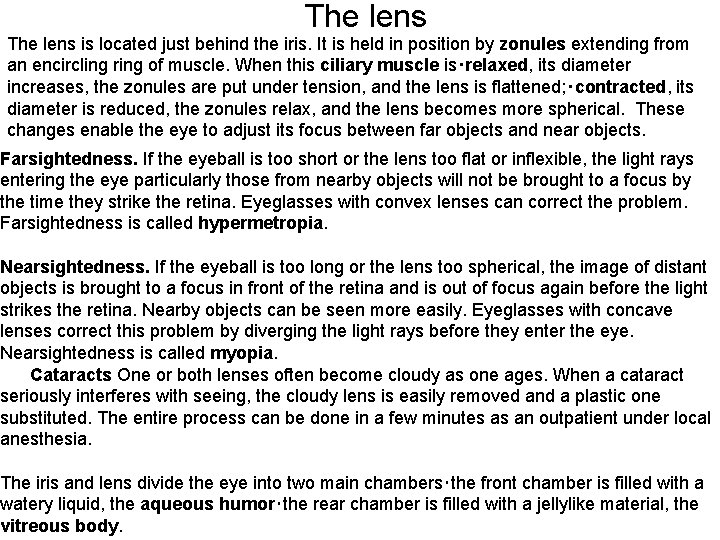
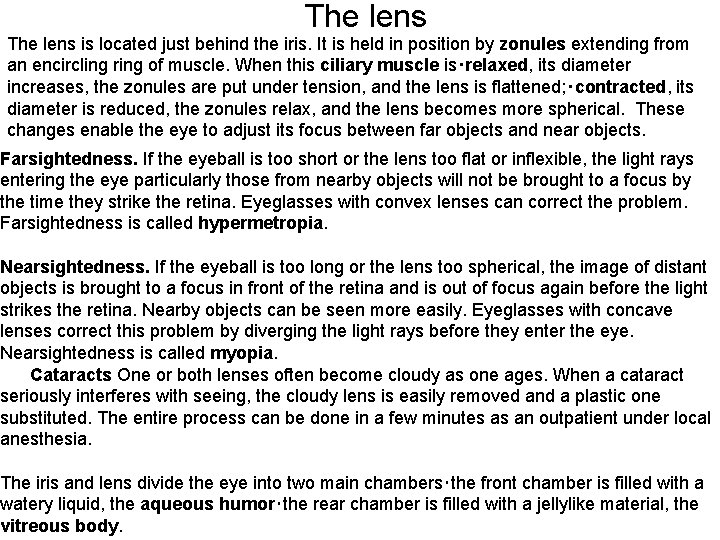
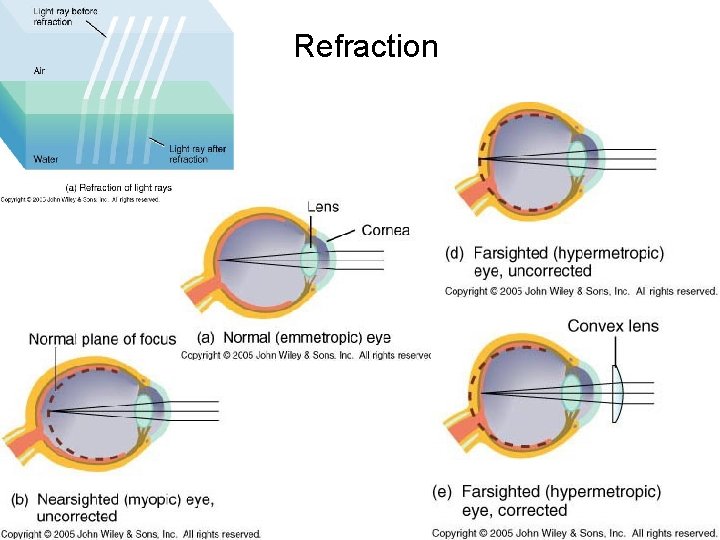
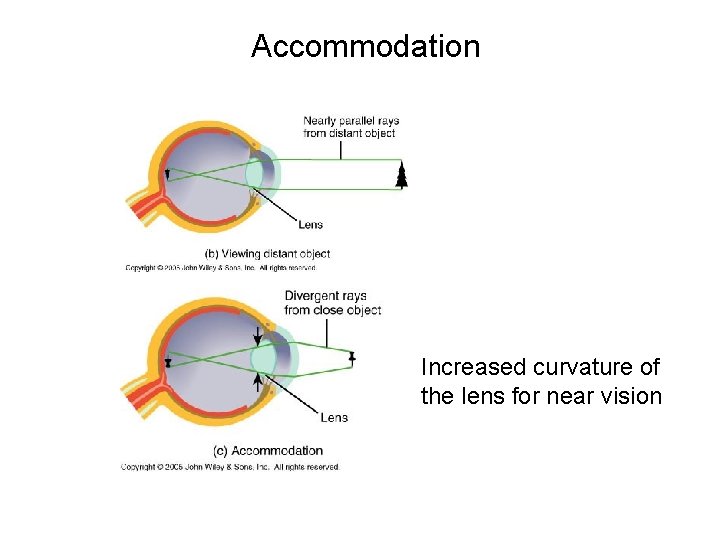
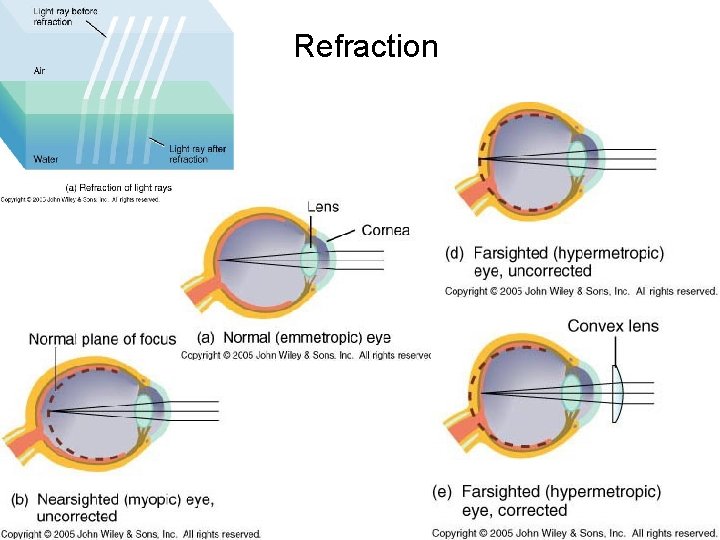
The lens is located just behind the iris. It is held in position by zonules extending from an encircling ring of muscle. When this ciliary muscle is・relaxed, its diameter increases, the zonules are put under tension, and the lens is flattened; ・contracted, its diameter is reduced, the zonules relax, and the lens becomes more spherical. These changes enable the eye to adjust its focus between far objects and near objects. Farsightedness. If the eyeball is too short or the lens too flat or inflexible, the light rays entering the eye particularly those from nearby objects will not be brought to a focus by the time they strike the retina. Eyeglasses with convex lenses can correct the problem. Farsightedness is called hypermetropia. Nearsightedness. If the eyeball is too long or the lens too spherical, the image of distant objects is brought to a focus in front of the retina and is out of focus again before the light strikes the retina. Nearby objects can be seen more easily. Eyeglasses with concave lenses correct this problem by diverging the light rays before they enter the eye. Nearsightedness is called myopia. Cataracts One or both lenses often become cloudy as one ages. When a cataract seriously interferes with seeing, the cloudy lens is easily removed and a plastic one substituted. The entire process can be done in a few minutes as an outpatient under local anesthesia. The iris and lens divide the eye into two main chambers・the front chamber is filled with a watery liquid, the aqueous humor・the rear chamber is filled with a jellylike material, the vitreous body.
Refraction
Accommodation Increased curvature of the lens for near vision
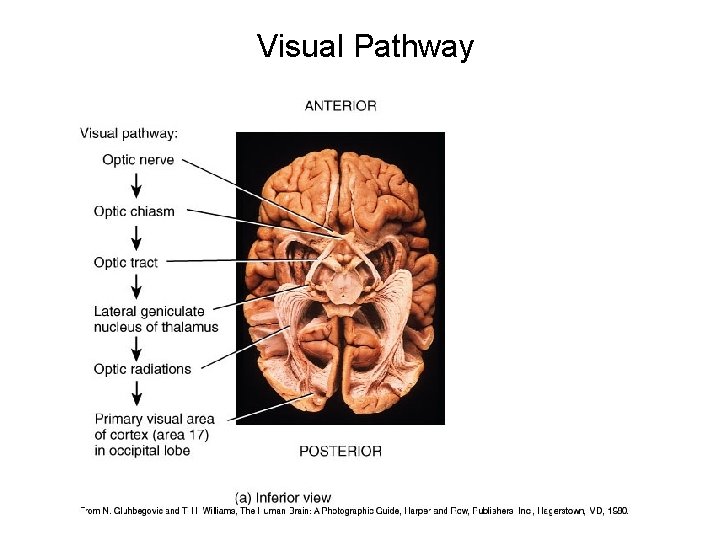
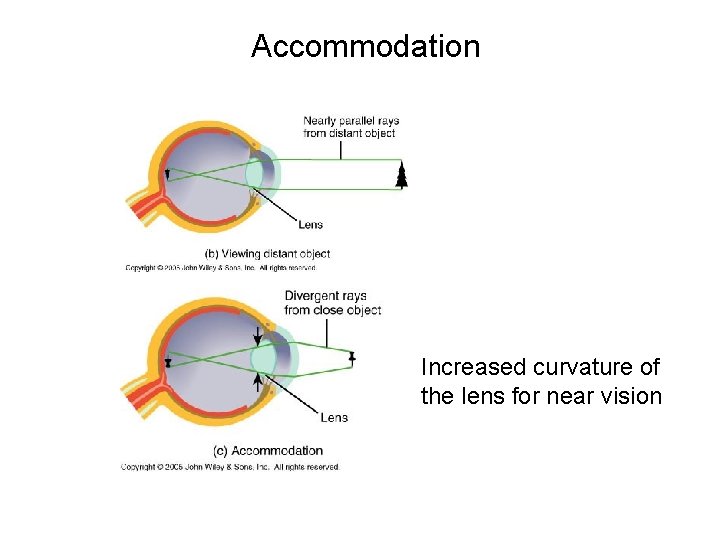
Visual Pathway
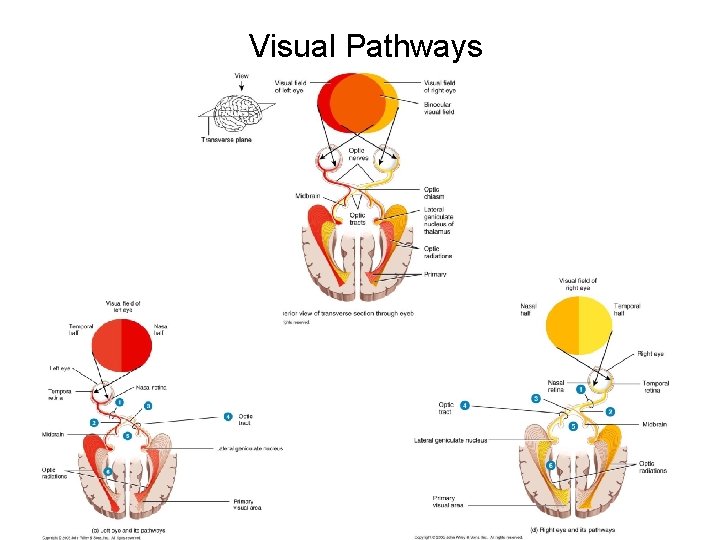
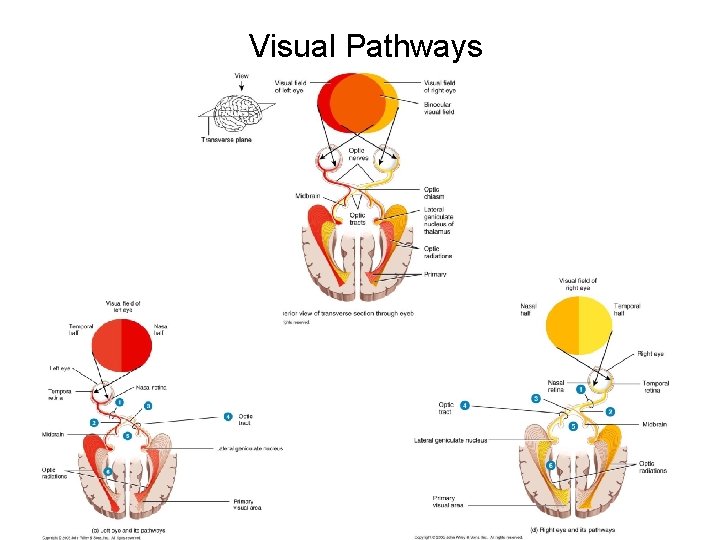
Visual Pathways

Figure 16. 10
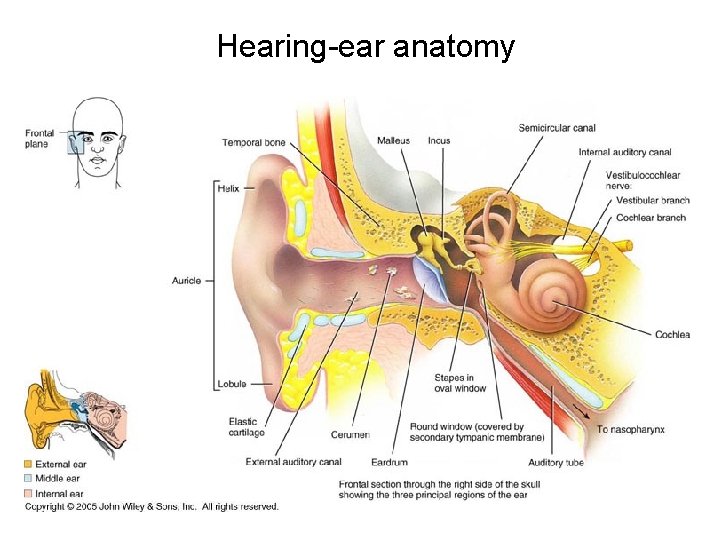
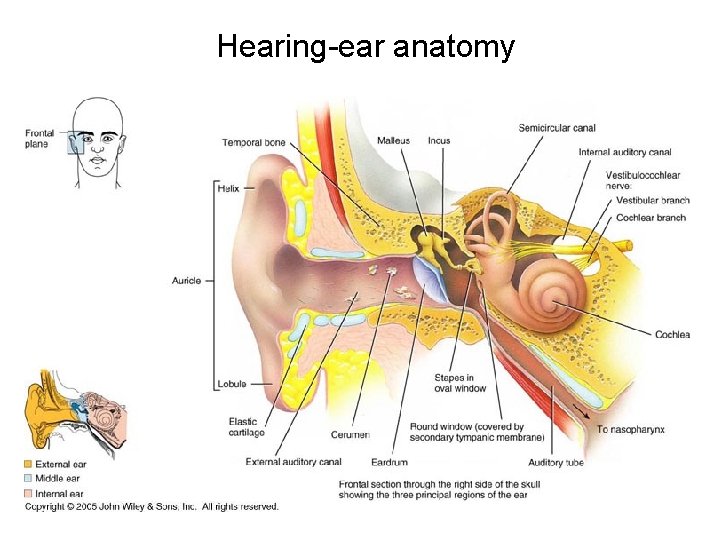
Hearing-ear anatomy
Properties of Sound Pitch-perception of different sound frequencies Frequency-cycles per second of sound waves (20 -20, 000 Hz Loudness-sound wave intensity Intensity-sound waves have greater amplitude resulting in stimulation of more fibers and louder perception of sound.

External Ear The external ear includes the auricle (pinna) and external auditory canal. The auricle is composed of elastic fibrocartilage covered by perichondrium and skin. The skin over the lateral aspect of the ear is tightly adherent to the perichondrium whereas on the medial surface, it is more loosely attached. The auricle is attached to the tympanic portion of the temporal bone on the lateral aspect of the skull by extension of the auricular cartilage into the cartilaginous external canal, by three ligaments (anterior, superior, posterior), by six poorly developed muscles and by its skin and subcutaneous tissue. The auricle receives sensory innervation from branches of cranial nerves V (auriculotemporal nerve), VII (auricular branch), X (auricular branch) and by the greater auricular nerve from the cervical plexus. The external auditory canal extends from the conchal cartilage of the auricle to the tympanic membrane. It is approximately 25 mm long in the adult. It courses slightly anteriorly and inferiorly in the adult. The lateral one half of the canal is cartilagenous, has thicker skin with subcutaneous tissue and ceruminous glands. The medial one half is osseous with only epidermis lying on the periosteum of the bony external canal.
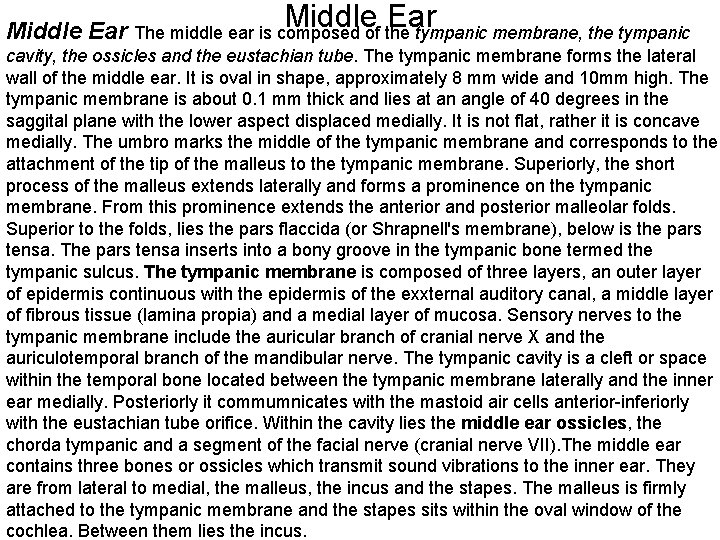
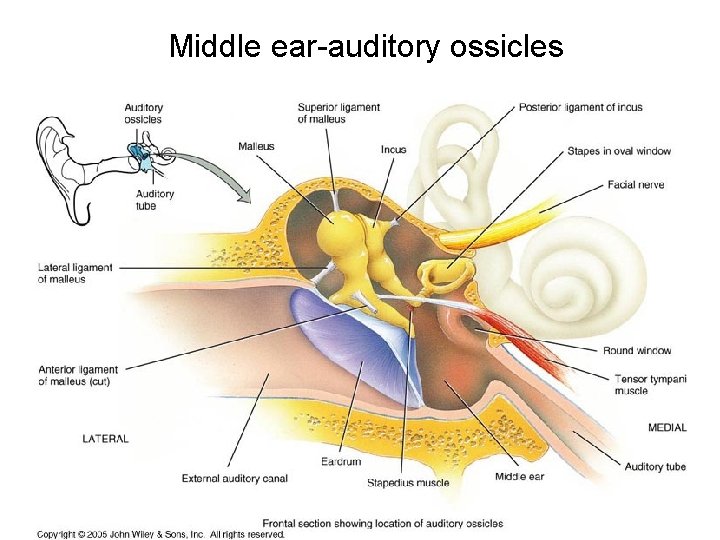
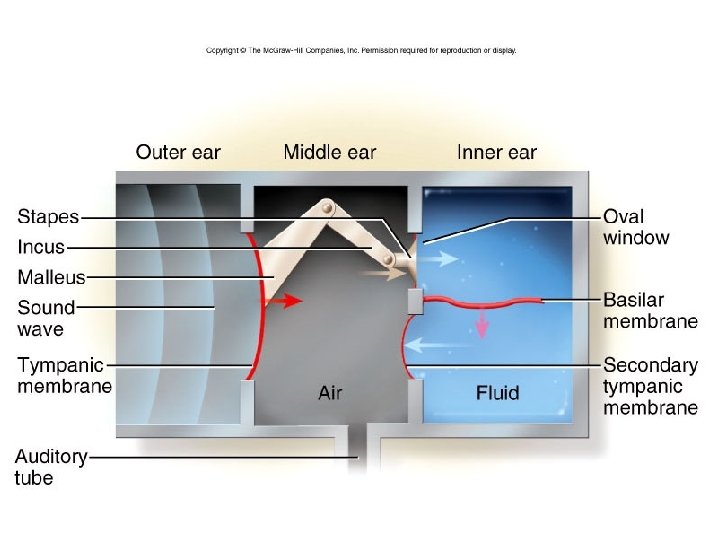
Middle Ear The middle ear is composed of the tympanic membrane, the tympanic cavity, the ossicles and the eustachian tube. The tympanic membrane forms the lateral wall of the middle ear. It is oval in shape, approximately 8 mm wide and 10 mm high. The tympanic membrane is about 0. 1 mm thick and lies at an angle of 40 degrees in the saggital plane with the lower aspect displaced medially. It is not flat, rather it is concave medially. The umbro marks the middle of the tympanic membrane and corresponds to the attachment of the tip of the malleus to the tympanic membrane. Superiorly, the short process of the malleus extends laterally and forms a prominence on the tympanic membrane. From this prominence extends the anterior and posterior malleolar folds. Superior to the folds, lies the pars flaccida (or Shrapnell's membrane), below is the pars tensa. The pars tensa inserts into a bony groove in the tympanic bone termed the tympanic sulcus. The tympanic membrane is composed of three layers, an outer layer of epidermis continuous with the epidermis of the exxternal auditory canal, a middle layer of fibrous tissue (lamina propia) and a medial layer of mucosa. Sensory nerves to the tympanic membrane include the auricular branch of cranial nerve X and the auriculotemporal branch of the mandibular nerve. The tympanic cavity is a cleft or space within the temporal bone located between the tympanic membrane laterally and the inner ear medially. Posteriorly it commumnicates with the mastoid air cells anterior-inferiorly with the eustachian tube orifice. Within the cavity lies the middle ear ossicles, the chorda tympanic and a segment of the facial nerve (cranial nerve VII). The middle ear contains three bones or ossicles which transmit sound vibrations to the inner ear. They are from lateral to medial, the malleus, the incus and the stapes. The malleus is firmly attached to the tympanic membrane and the stapes sits within the oval window of the cochlea. Between them lies the incus.
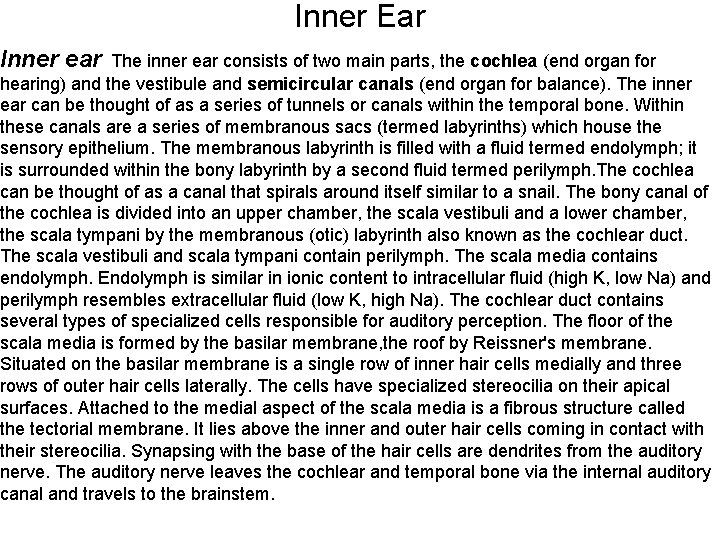
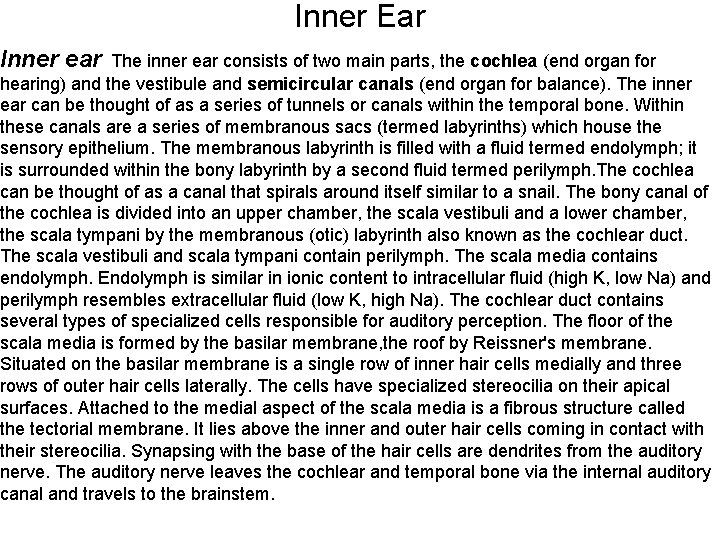
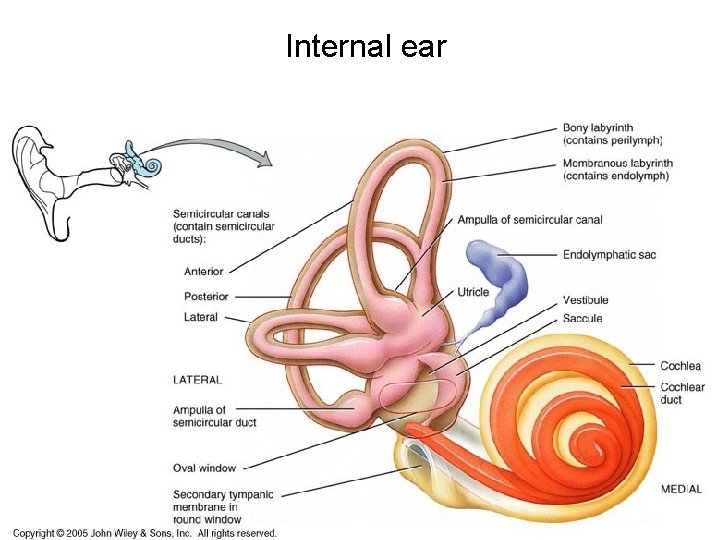
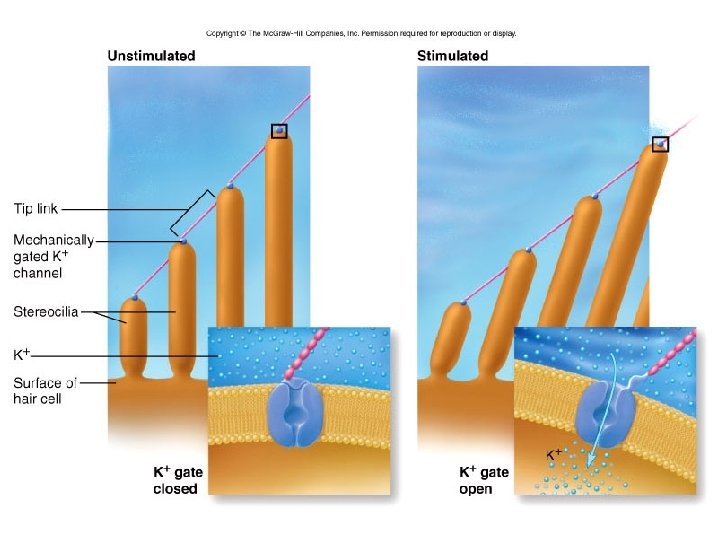
Inner ear Inner Ear The inner ear consists of two main parts, the cochlea (end organ for hearing) and the vestibule and semicircular canals (end organ for balance). The inner ear can be thought of as a series of tunnels or canals within the temporal bone. Within these canals are a series of membranous sacs (termed labyrinths) which house the sensory epithelium. The membranous labyrinth is filled with a fluid termed endolymph; it is surrounded within the bony labyrinth by a second fluid termed perilymph. The cochlea can be thought of as a canal that spirals around itself similar to a snail. The bony canal of the cochlea is divided into an upper chamber, the scala vestibuli and a lower chamber, the scala tympani by the membranous (otic) labyrinth also known as the cochlear duct. The scala vestibuli and scala tympani contain perilymph. The scala media contains endolymph. Endolymph is similar in ionic content to intracellular fluid (high K, low Na) and perilymph resembles extracellular fluid (low K, high Na). The cochlear duct contains several types of specialized cells responsible for auditory perception. The floor of the scala media is formed by the basilar membrane, the roof by Reissner's membrane. Situated on the basilar membrane is a single row of inner hair cells medially and three rows of outer hair cells laterally. The cells have specialized stereocilia on their apical surfaces. Attached to the medial aspect of the scala media is a fibrous structure called the tectorial membrane. It lies above the inner and outer hair cells coming in contact with their stereocilia. Synapsing with the base of the hair cells are dendrites from the auditory nerve. The auditory nerve leaves the cochlear and temporal bone via the internal auditory canal and travels to the brainstem.
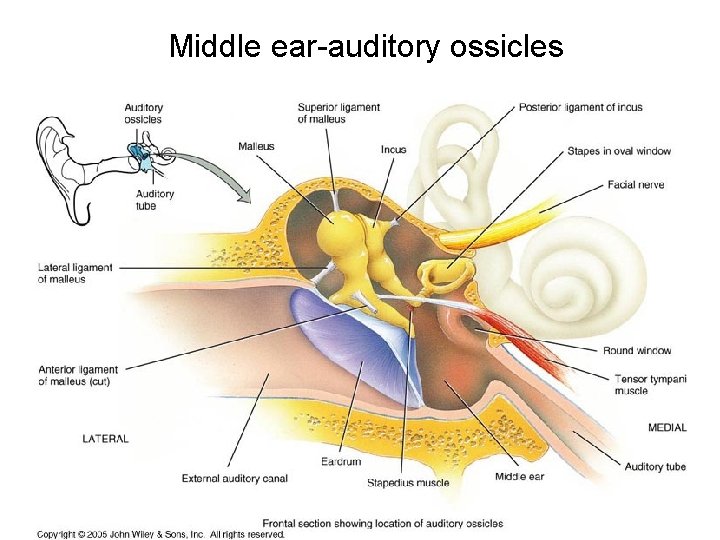
Middle ear-auditory ossicles
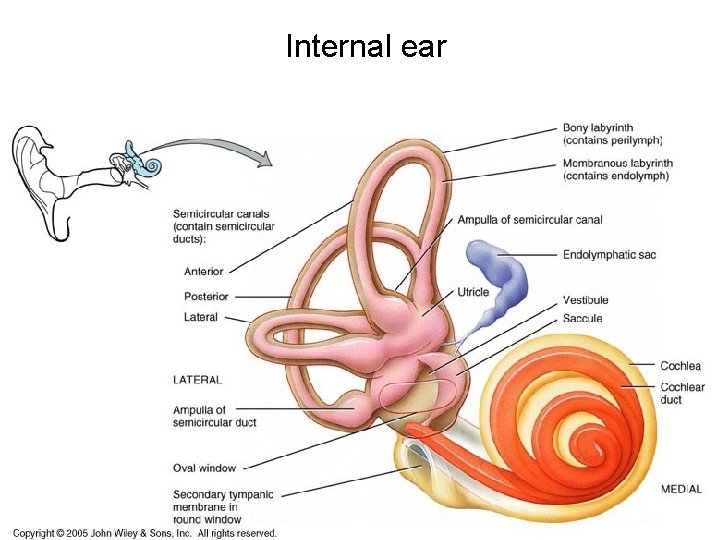
Internal ear
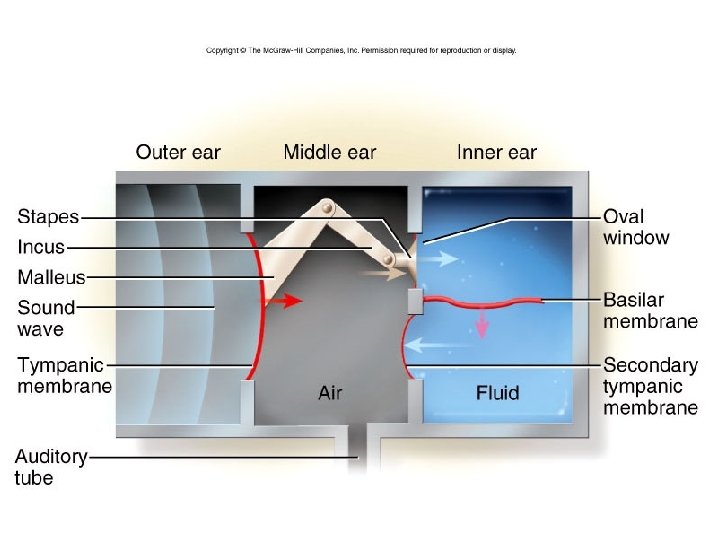
Figure 16. 15
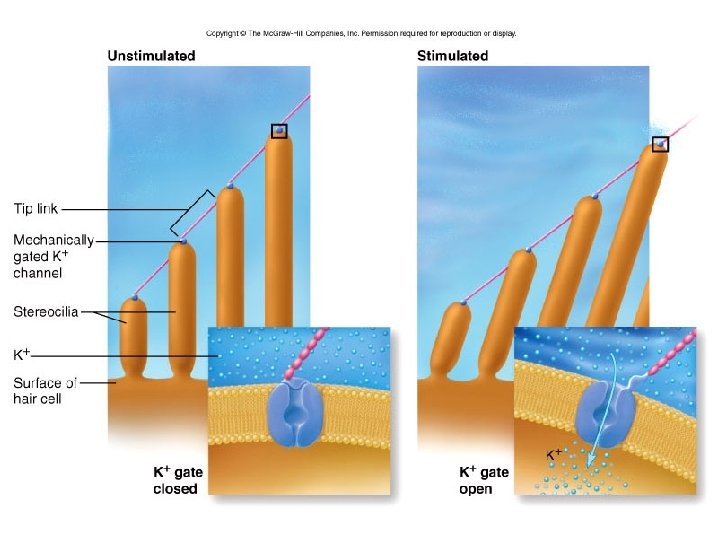
Figure 16. 16

Figure 16. 17

Figure 16. 18
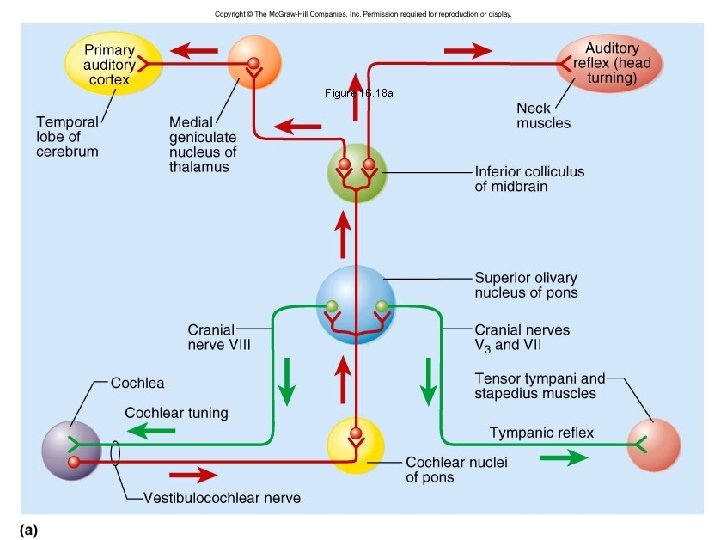
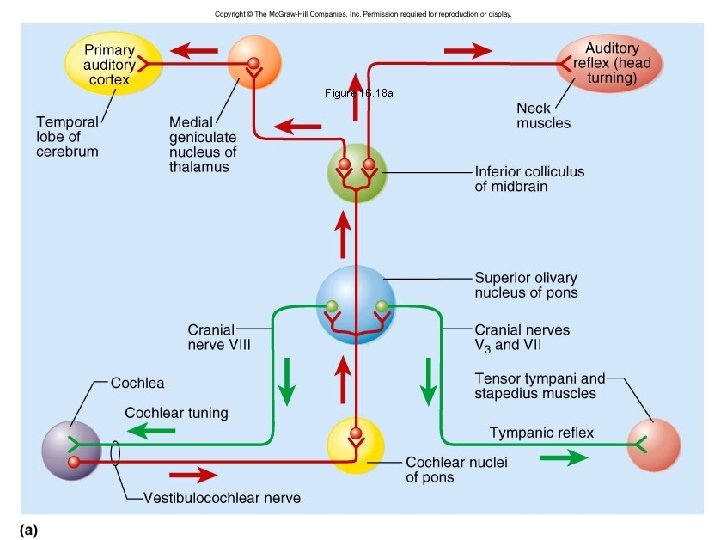
Figure 16. 18 a
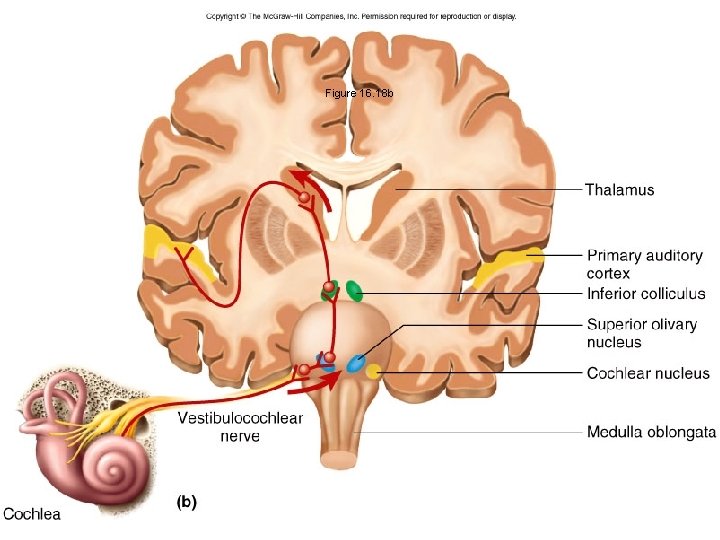
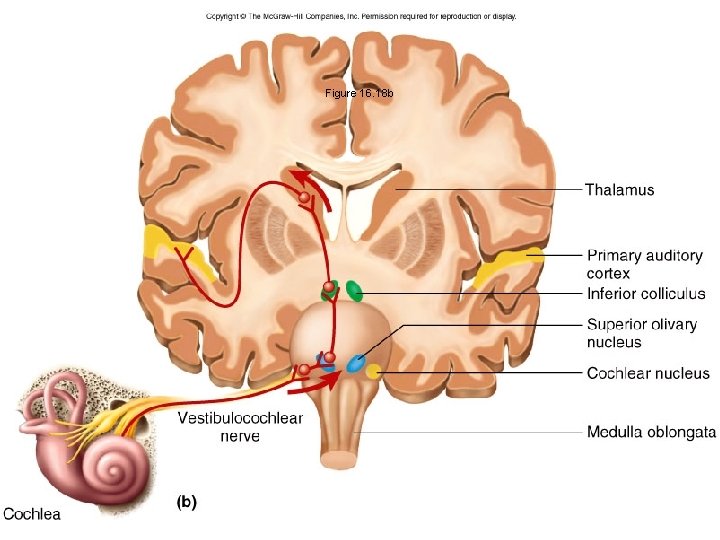
Figure 16. 18 b
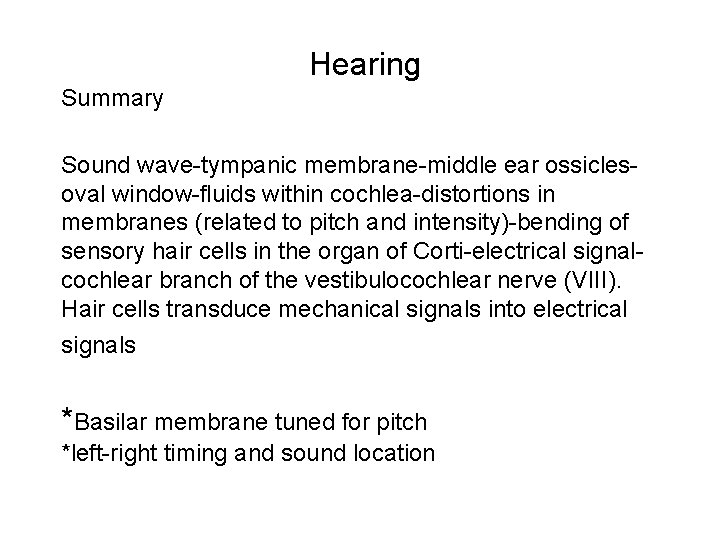
Hearing Summary Sound wave-tympanic membrane-middle ear ossiclesoval window-fluids within cochlea-distortions in membranes (related to pitch and intensity)-bending of sensory hair cells in the organ of Corti-electrical signalcochlear branch of the vestibulocochlear nerve (VIII). Hair cells transduce mechanical signals into electrical signals *Basilar membrane tuned for pitch *left-right timing and sound location
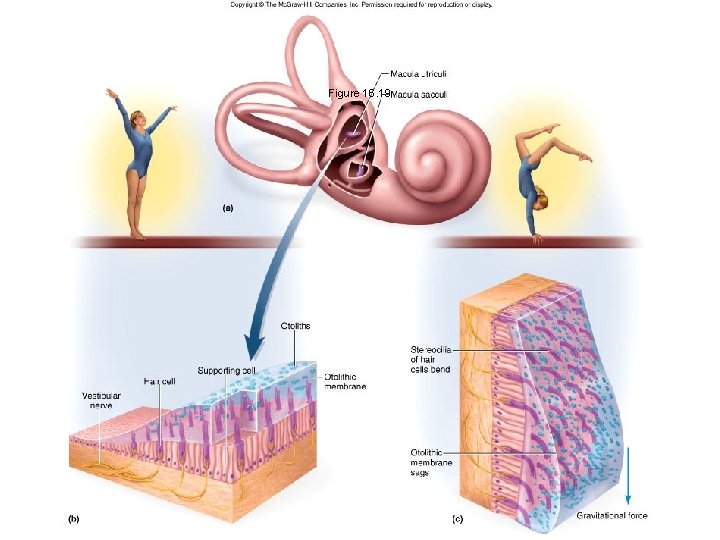
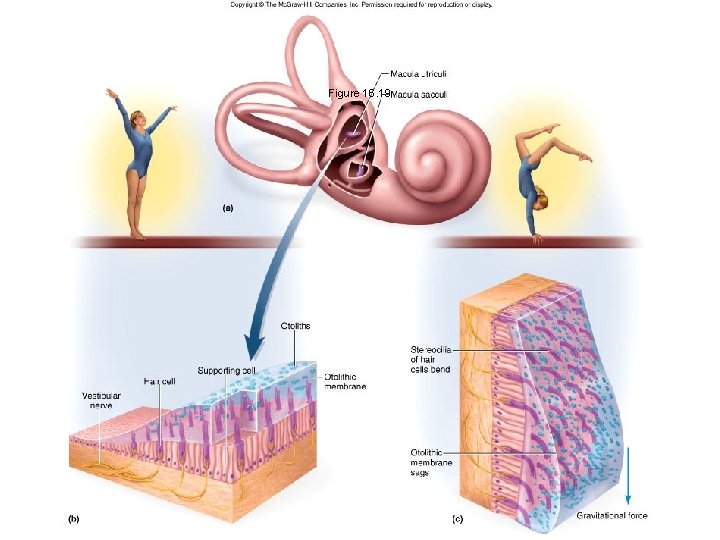
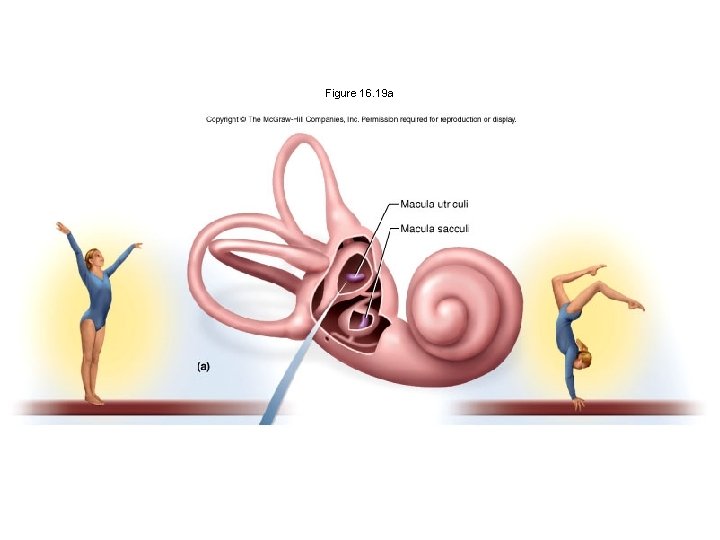
Figure 16. 19
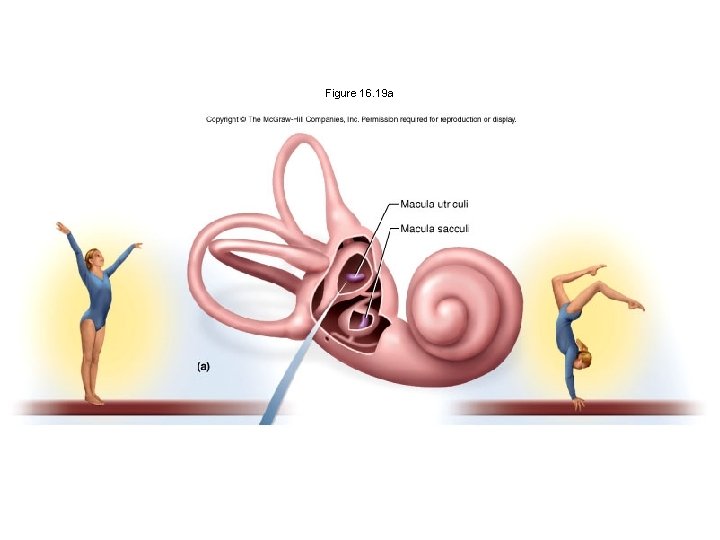
Figure 16. 19 a
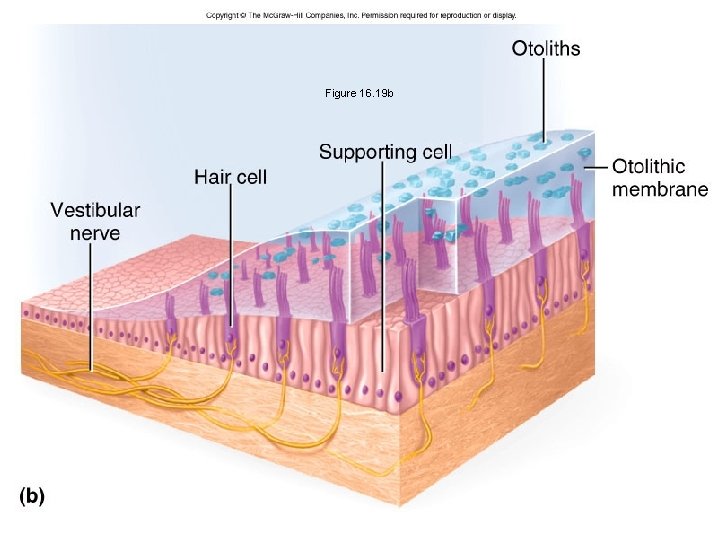
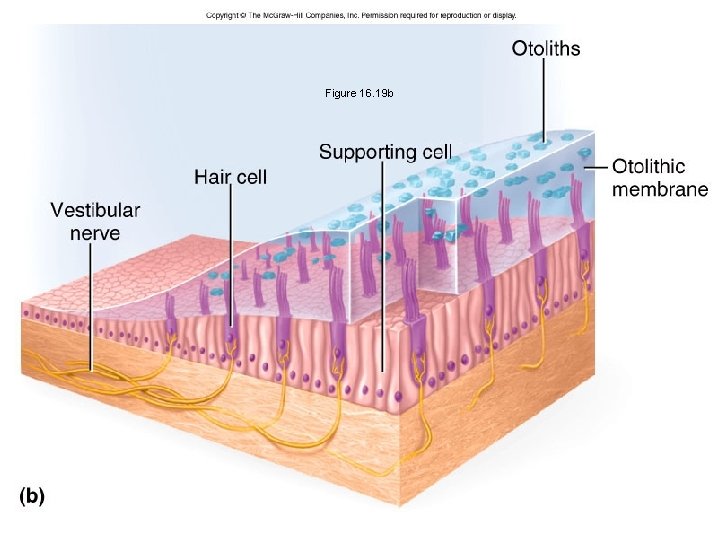
Figure 16. 19 b

Figure 16. 19 c
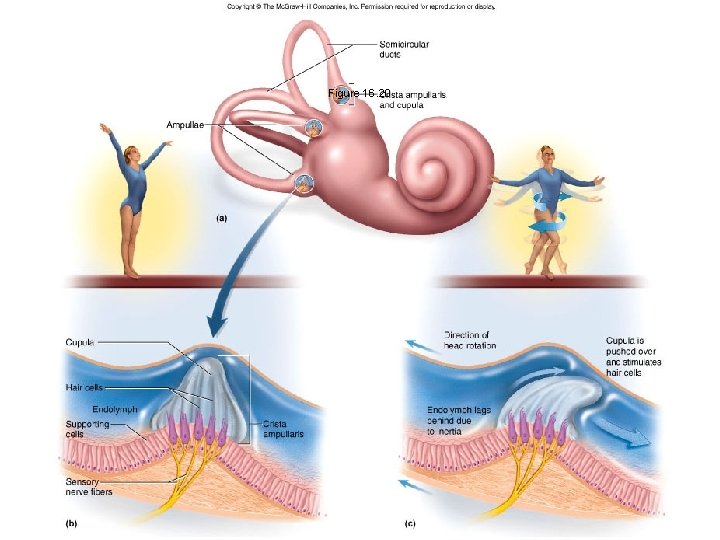
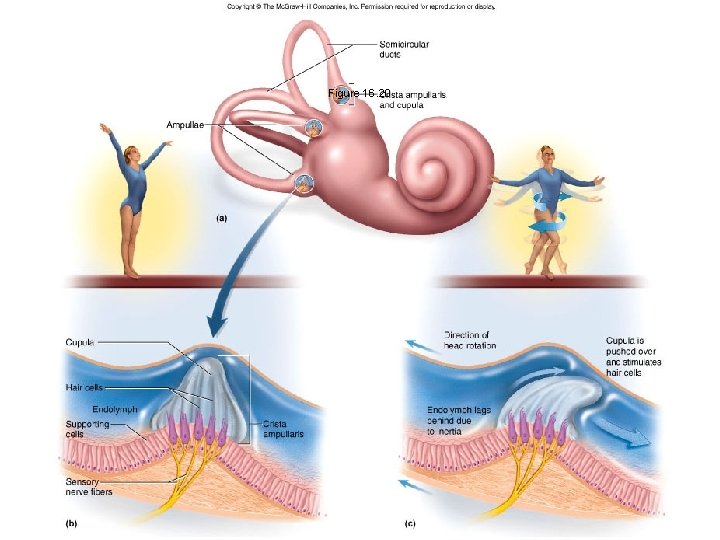
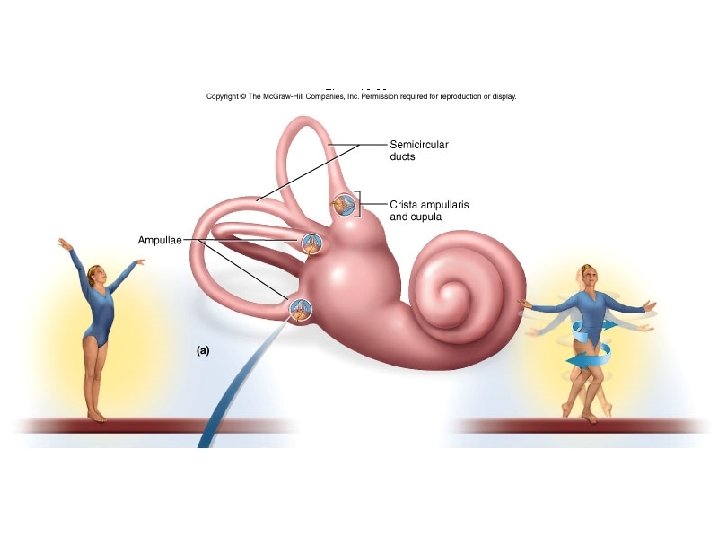
Figure 16. 20
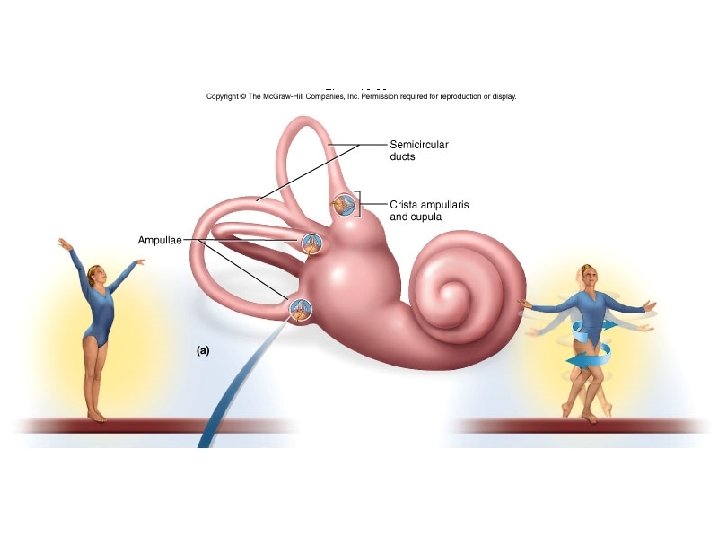
Figure 16. 20 a
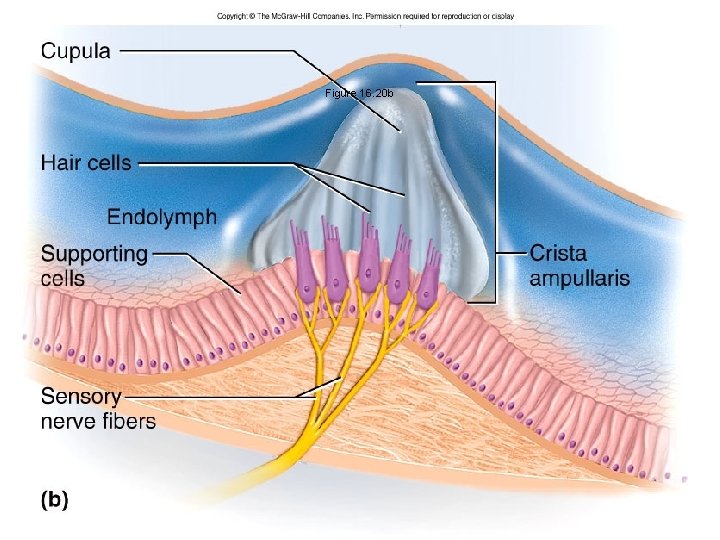
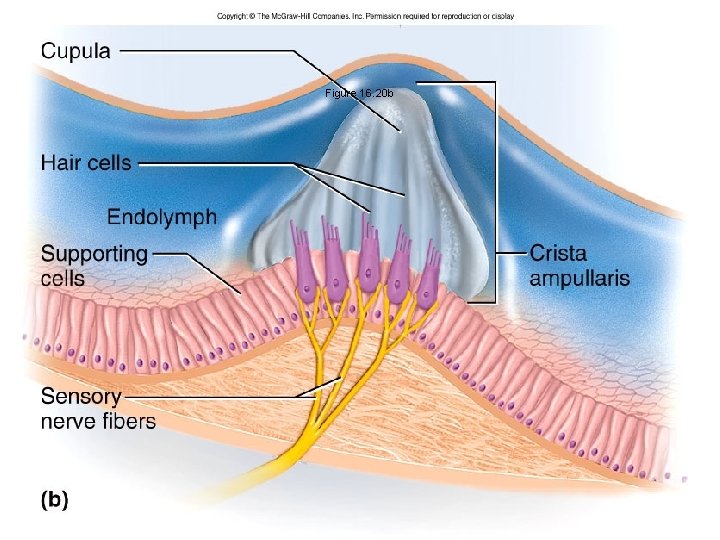
Figure 16. 20 b
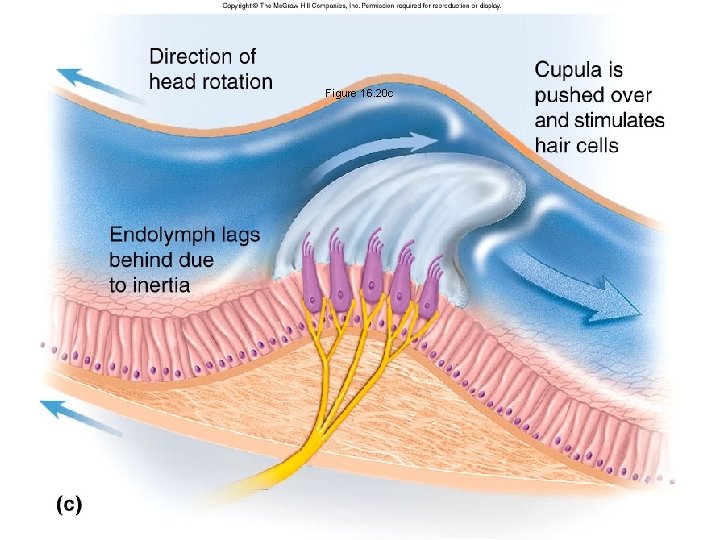
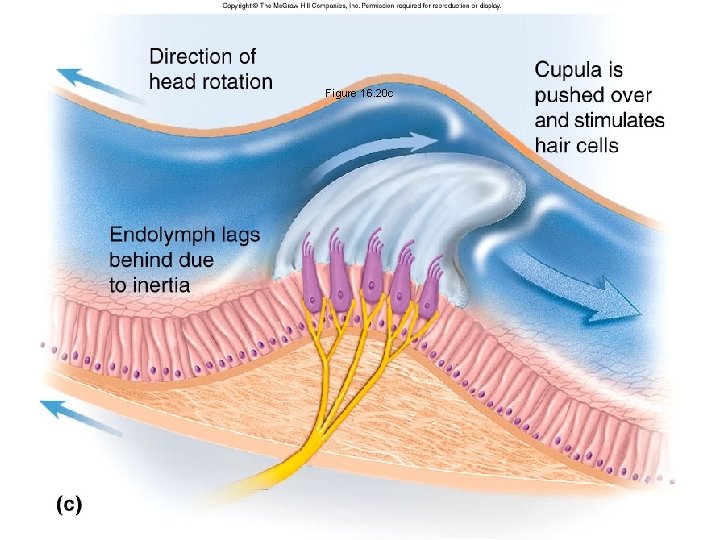
Figure 16. 20 c
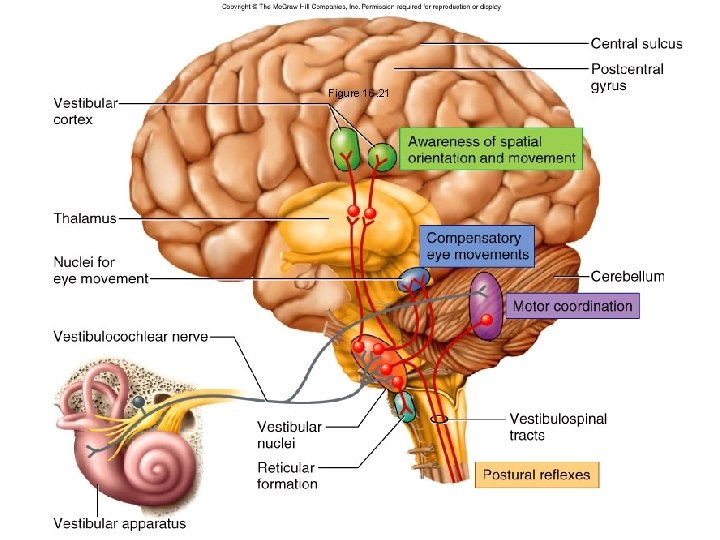
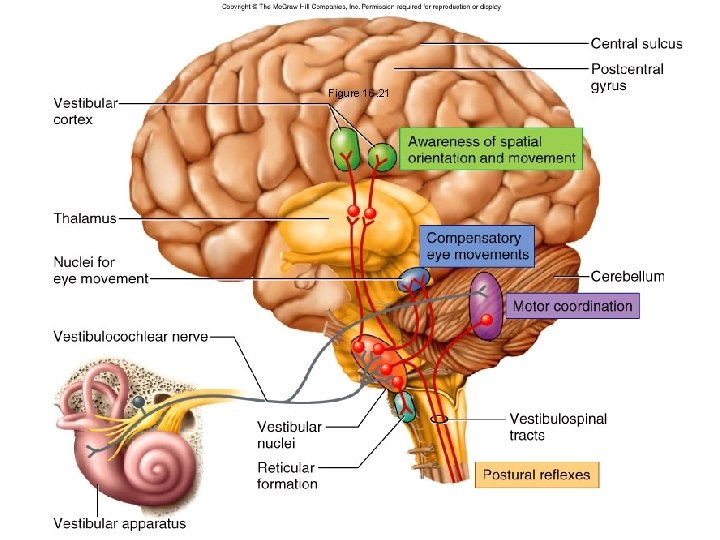
Figure 16. 21
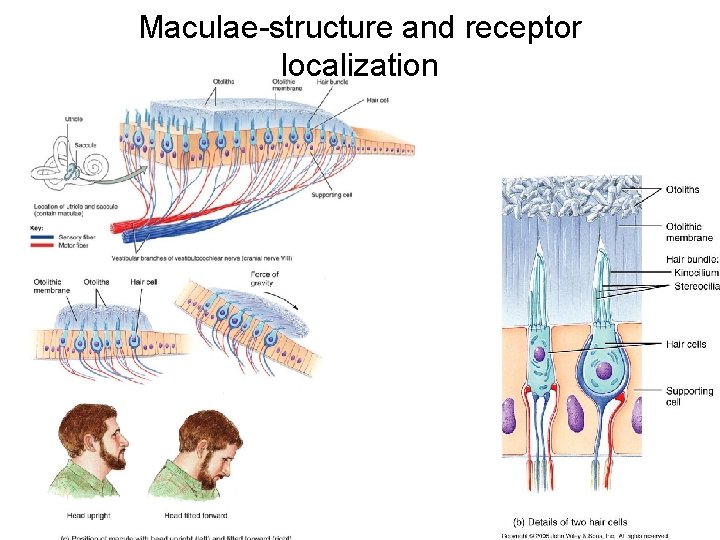
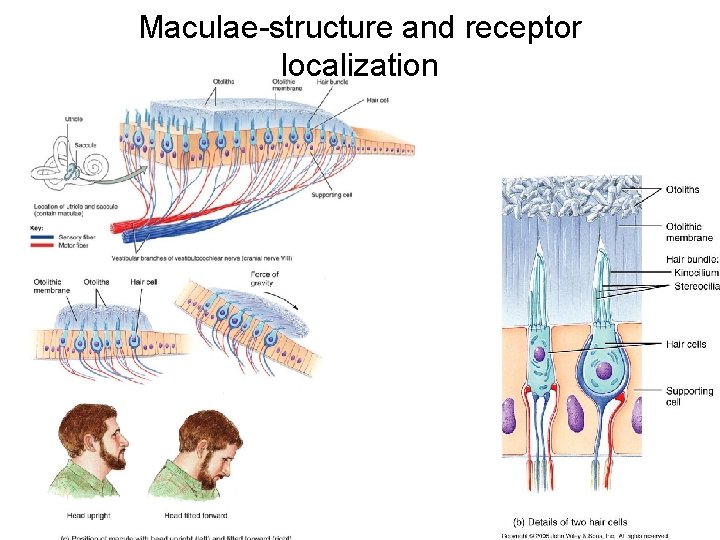
Maculae-structure and receptor localization
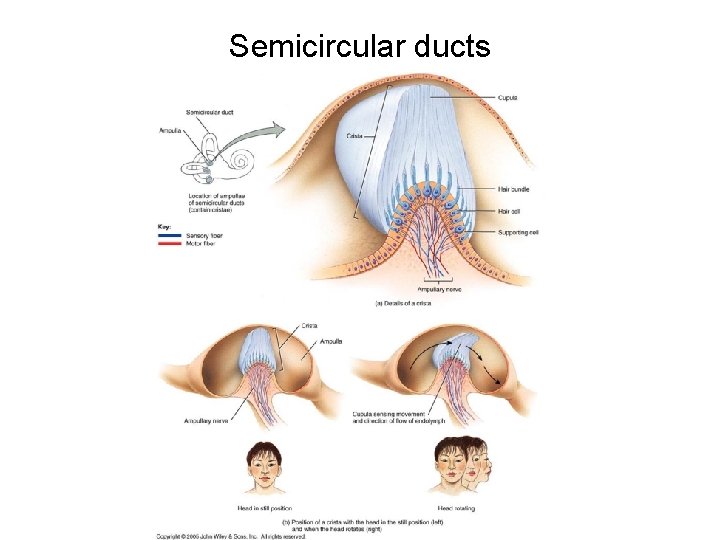
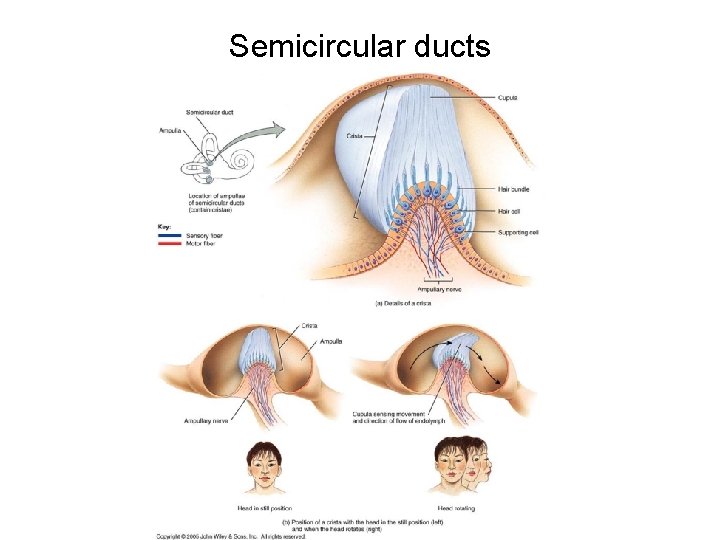
Semicircular ducts
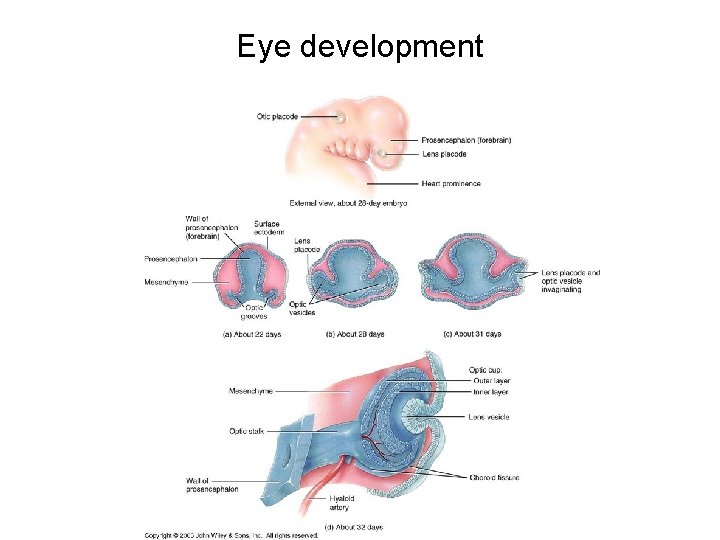
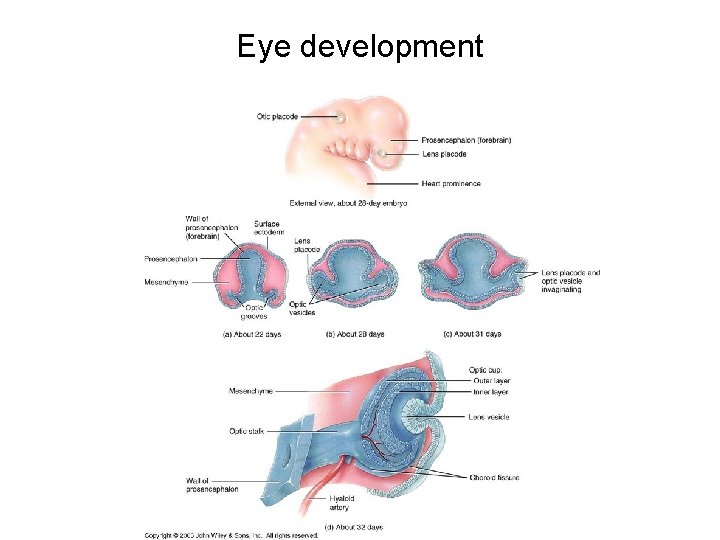
Eye development

Ear Development
Chapter 17 END
 What is the difference between somatic and special senses
What is the difference between somatic and special senses Special vs general senses
Special vs general senses Gustatory system
Gustatory system Gustation and olfaction
Gustation and olfaction Olfaction
Olfaction Chemoreceptor example
Chemoreceptor example Thermoreceptors
Thermoreceptors Chapter 17 special senses answer key
Chapter 17 special senses answer key Chapter 11 labeling exercises
Chapter 11 labeling exercises Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 8 special senses
Chapter 8 special senses Chapter 10 special senses
Chapter 10 special senses The general and special senses chapter 9
The general and special senses chapter 9 Olfactory receptor cells
Olfactory receptor cells Chapter 15 special senses
Chapter 15 special senses Bio 137
Bio 137 Five special senses
Five special senses The cones of the retina are coursera quiz answers
The cones of the retina are coursera quiz answers Pneumonic for cranial nerves
Pneumonic for cranial nerves Special senses quiz
Special senses quiz Special senses
Special senses Conclusion of special senses
Conclusion of special senses Building vocabulary activity: the special senses
Building vocabulary activity: the special senses Building vocabulary activity: the special senses
Building vocabulary activity: the special senses Special senses anatomy
Special senses anatomy The general senses
The general senses Somatic senses
Somatic senses Special senses the eyes and ears
Special senses the eyes and ears Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Số.nguyên tố
Số.nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates