Chapter 17 Drugs Used To Manage Pain pain





- Slides: 24
Chapter 17 Drugs Used To Manage Pain
�pain means to: ache, hurt or be sore �pain is subjective (you cannot see, hear, touch or smell pain, must rely on what person says) �differs from person to person, you must believe the person �pain is a warning sign from the body, means there is tissue damage �often pain causes person to seek health care
�there are different types of pain: �acute pain: �felt suddenly from injury, disease, trauma or surgery �tissue damage present �lasts a short time, usually less than 6 months �lessens with healing �chronic pain: �lasts longer than 6 months �pain is constant or off and on �no longer tissue damage �remains long after healing �common causes: arthritis, cancer
�different types of pain continued…. �radiating pain: �felt at site of tissue damage and in nearby areas �example: heart attack pain is felt in chest, jaw, shoulder �phantom pain: �felt in a body part that is no longer there �example: person with amputated leg feels leg pain

�Many factors affect reactions to pain: �past experience: severity of pain, it’s cause, how long it lasted, and if relief occurred all affect the persons current response to pain. Knowing what to expect can help or hinder how person handles pain �anxiety: pain and anxiety are related, pain cause anxiety. Anxiety increases how much pain the person feels. Reducing anxiety lessens pain. Example: Letting person know ahead of time to expect pain postsurgery, but that there will be drugs for pain relief may help reduce anxiety and therefore reduce the amount of pain felt
�factors affecting reactions to pain continued. . �rest and sleep: both restore energy, reduce body demands and the body can repair itself. Lack of rest and sleep affects thinking and coping with daily life. Sleep and rest needs increase with injury/illness. Pain seems worse when tired or restless. Also tend to focus on pain when tired �attention: the more one thinks about pain the worse it seems. Pain seems worse at night when activity is less and it is quiet. When unable to sleep the person has time to think about the pain

�factors affecting reactions to pain continued. . �personal and family duties: Pain is often ignored when there are children to care for. Some people go to work with pain. Others deny pain if serious illness is feared. Illness can interfere with jobs, school, caring for others �the value or meaning of pain: To some pain is a sign of weakness. May indicate serious illness and need for painful tests/treatments, therefore pain is ignored or denied. Sometimes pain gives pleasure. For some people pain means not having to work or assume daily routines. Pain can be used to avoid certain people or things.
�factors affecting reactions to pain continued. . �support from others: dealing with pain often easier when family and friends offer comfort/support. The use of touch by a valued person is very comforting. Dealing with pain alone can increase anxiety, person has more time to think about the pain �culture: Culture can affect pain responses, some cultures are stoic when it comes to pain (show no reaction). Other cultures show strong verbal and non-verbal reactions to pain. Non-english speaking persons may have problems describing pain. Someone
�factors affecting reactions to pain continued. . �illness: some diseases cause decreased pain sensation. CNS disorders may not allow person to feel pain, or it may not feel severe. Person at risk for undetected disease or injury. If pain is not felt person will not know to seek health care. �age: children may not understand pain, they know it feels bad but have fewer experiences with pain. They do not know what to expect or how to relieve pain. They rely on adults to help. Adults must be alert to behaviors and situations that signal pain.
� You must rely on what the person tells you about their pain � Promptly report any info you collect about pain � Write down exactly what the person says � Nurse needs following info to assess pain: �location: where is pain, have them point, ask if anywhere else �onset and duration: when did it start, how long has it lasted �intensity: mild, moderate, severe, ask them to rate on scale of 1 -10, or use Wong-Baker Faces Pain Rating Scale (17 -2 pg. 224). Ask person to pick the face that best describes how they feel. �factors causing pain: (precipitating factors) moving, turning, coughing, ask what person was doing before pain started and when it started �factors affecting pain: what makes pain better and worse �vital signs: take vitals, increases will often occur with acute pain, may be normal with chronic pain �description: ask them to describe the pain, if they cannot offer them some words such as: - aching - crushing -burning -cramping -dull -gnawing
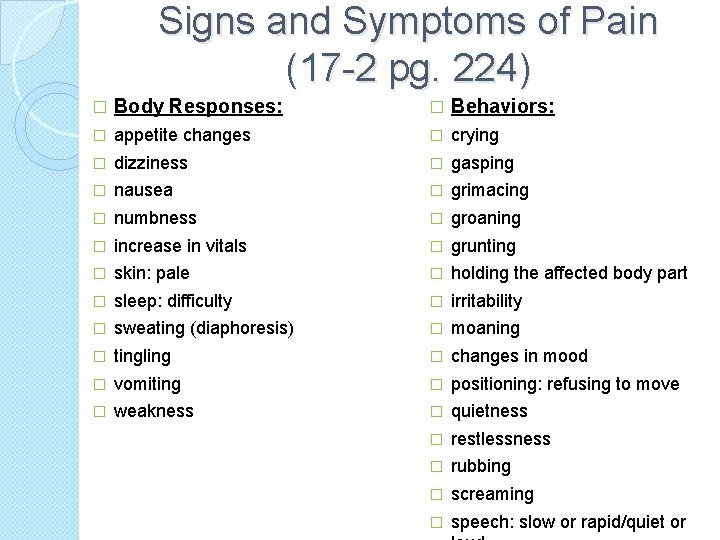
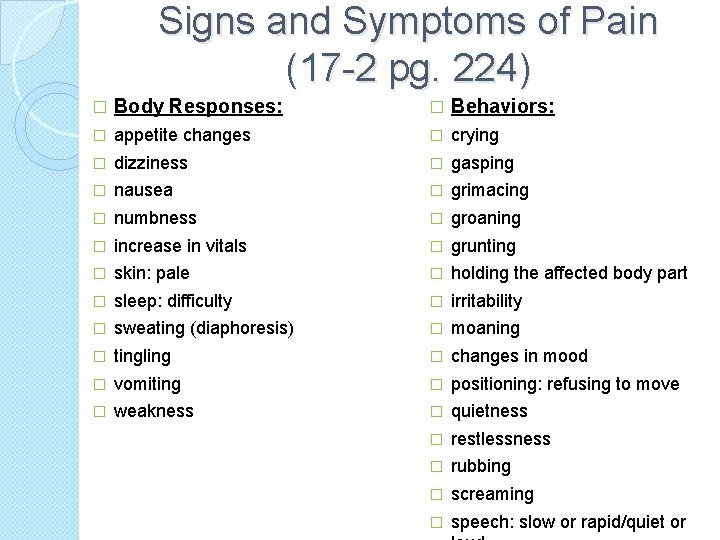
Signs and Symptoms of Pain (17 -2 pg. 224) � Body Responses: � Behaviors: � appetite changes � crying � dizziness � gasping � nausea � grimacing � numbness � groaning � increase in vitals � grunting � skin: pale � holding the affected body part � sleep: difficulty � irritability � sweating (diaphoresis) � moaning � tingling � changes in mood � vomiting � positioning: refusing to move � weakness � quietness � restlessness � rubbing � screaming � speech: slow or rapid/quiet or
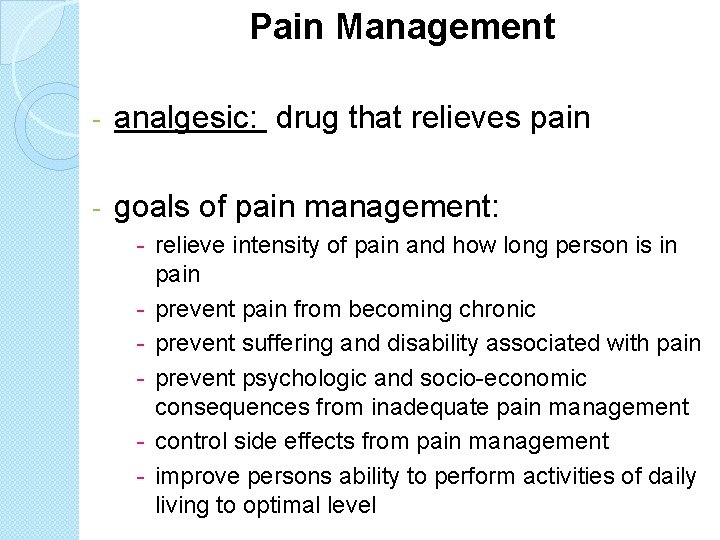
Pain Management - analgesic: drug that relieves pain - goals of pain management: - relieve intensity of pain and how long person is in pain - prevent pain from becoming chronic - prevent suffering and disability associated with pain - prevent psychologic and socio-economic consequences from inadequate pain management - control side effects from pain management - improve persons ability to perform activities of daily living to optimal level
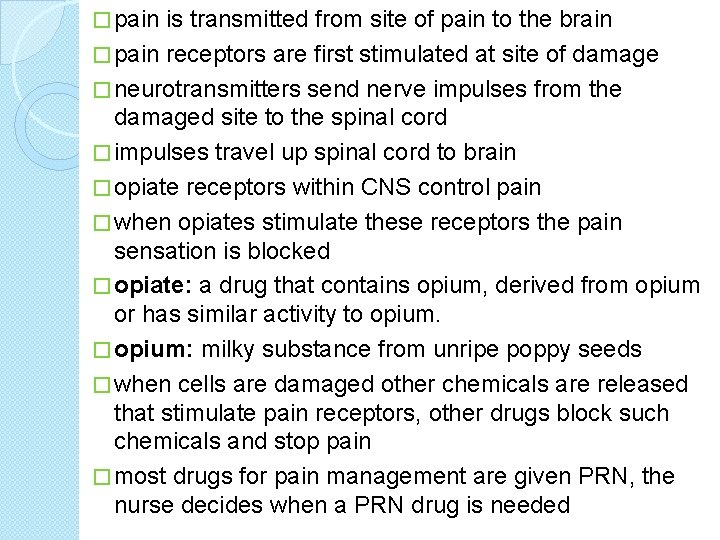
� pain is transmitted from site of pain to the brain � pain receptors are first stimulated at site of damage � neurotransmitters send nerve impulses from the damaged site to the spinal cord � impulses travel up spinal cord to brain � opiate receptors within CNS control pain � when opiates stimulate these receptors the pain sensation is blocked � opiate: a drug that contains opium, derived from opium or has similar activity to opium. � opium: milky substance from unripe poppy seeds � when cells are damaged other chemicals are released that stimulate pain receptors, other drugs block such chemicals and stop pain � most drugs for pain management are given PRN, the nurse decides when a PRN drug is needed

Opiate Agents �opiates are derived from opium and include morphine and heroine �opiate agonists: group of semi-synthetic or synthetic drugs that can relieve severe pain without loss of consciousness �synthetic: substance that is made, not naturally occurring �semi-synthetic: natural substance that has partially been altered by chemicals
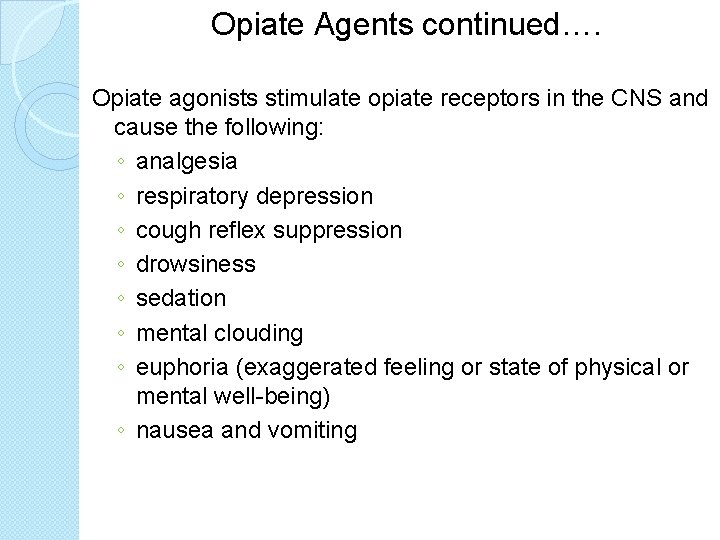
Opiate Agents continued…. Opiate agonists stimulate opiate receptors in the CNS and cause the following: ◦ analgesia ◦ respiratory depression ◦ cough reflex suppression ◦ drowsiness ◦ sedation ◦ mental clouding ◦ euphoria (exaggerated feeling or state of physical or mental well-being) ◦ nausea and vomiting
Opiate Agents continued…. opiate agents are used: �relieve acute or chronic moderate to severe pain �pain from acute injury, surgery, renal or biliary colic, MI and cancer �pre-operative sedation �supplement anesthesia �reduce anxiety in persons with acute pulmonary edema

Opiate Agents continued…. - most opiate agonists can produce addiction (after 3 -6 weeks of continuous use) - considered a controlled substance - Signs and Symptoms of opiate withdrawals: �restlessness �perspiration �goose-flesh �tears �runny nose �dilated pupils �muscle spasms �pain �cramps (muscle/abdominal) flashes: hot and cold � insomnia � nausea � vomiting � diarrhea � severe sneezing � vital signs: increased temp, heart rate, respiratory rate, blood pressure �
Opiate Agents continued…. Assisting With the Nursing Process -Opiate agonists are given PRN for pain relief -Some uses they may be ordered STAT (at once) ie: MI for pulmonary edema -Could also be a one-time order ie: pre-op sedation Assessment: observe the persons speech pattern, degree of alertness and orientation to person, time and place. Measure vital signs, if respirations are below 12/minute tell nurse immediately. Ask person to rate pain. Check medication administration record (MAR) for when person last received analgesic Planning: available for subcutaneous, intramuscular or IV injection. You do NOT give drugs by these routes Implementation: see table 17 -1 (p. 225 -226) for “Initial Adult Dose” Evaluation: report and record: - lightheadedness, dizziness, sedation, nausea, vomiting, sweating: tend to occur with first dose, supine position helps to reduce these symptoms, provide for safety - confusion, disorientation: observe person’s alertness and orientation to person time and place. Provide for safety - orthostatic hypotension: provide for safety, measure BP, do not allow person to sit up - constipation: may occur from continued use, follow care plan re: food/liquids, give stool softeners or laxative as ordered -respiratory depression: if respirations are below 12/minute tell nurse immediately, also observe depth of respirations, if shallow breathing tell nurse immediately
� Salicylates: most commonly used analgesics for slightmoderate pain. ◦ Drugs inhibit prostaglandin(PG) production. ◦ PGs are fatty acids that cause various responses: �Analgesic effect: Salicylates inhibit formation of PGs affecting pain receptors �Anti-inflammatory effect: salicylates inhibit PGs that produce signs/symptoms of inflammation (redness, swelling, and warmth) �Anti-pyretic effect: given to reduce fever See table 17 -2 (pg. 227) for salicylates

Salicylates: � Aspirin: - inhibits platelet activity, platelets needed for blood clotting. - aspirin is used to: reduce risk of transient, ischemic attacks or stroke in men reduce risk of MI in person with previous MI or unstable angina Assisting With Nursing Process: Assessment: observe the persons speech pattern, degree of alertness and orientation to person, time and place. Measure vital signs. Ask person to rate pain. Check (MAR) for when person last received ordered drug Planning: see 17 -2 for “Dose Forms” Implementation: see table 17 -2 (p. 227) for “Uses and Adult Dosages” and for “Maximum Daily Dose” Evaluation: report and record: - stomach irritation: give with food or milk or with large amounts of water, if antacids are ordered they are give 1 hour later - GI bleeding: vomitus that looks like coffee grounds, red vomitus and black or tarry stools are signs of GI bleeding. Test stools for occult blood as directed by nurse/care plan - tinnitus (ringing of ears), impaired hearing, dimmed vision, sweating, fever, lethargy, dizziness, confusion, nausea, vomiting: signal salicylate toxicity
Non-steroidal Anti-inflammatory Drugs (NSAIDs) - known as aspirin-like drugs - prostaglandin inhibitors - used to reduce pain, inflammation, fever - tend to have less side effects that salicylates, there is a risk however of MI, stroke, GI bleeds from NSAIDs Assisting With Nursing Process: Assessment: observe the persons speech pattern, degree of alertness and orientation to person, time and place. Measure vital signs. Ask person to rate pain. Planning: see 17 -3 (p. 229 -230) for “Dose Forms” Implementation: see table 17 -3 (p. 229 -230) for “Uses and Adult Dosages” and for “Maximum Daily Dose” Evaluation: report and record: - stomach irritation: give with food or milk - constipation: follow care plan for fluid intake and diet, give stool softeners or laxatives as ordered - dizziness or drowsiness: provide for safety - GI bleeding: vomitus that looks like coffee grounds, red vomitus and black or tarry stools are signs of GI bleeding. Test stools for occult blood as directed by nurse/care plan - confusion: observe persons alertness and orientation to person, place and time. Provide for safety - rash, hives, itching: may signal an allergic reaction, tell nurse at once - decreased urine output, red or smoky-colored urine: signal kidney problems - anorexia, nausea, vomiting, jaundice: may signal liver toxicity - sore throat, fever, jaundice, weakness: may signal changes in red/white blood cells
Other analgesic agents: acetaminophen (Tylenol, Datril, Tempra): - synthetic non-opiate analgesic - anti-pyretic - no anti-inflammatory activity Assisting With the Nursing Process Assessment: Measure vital signs. Ask person to rate pain. Check MAR for when person last received ordered drug Planning: see pg. 232 for “Dose Forms” Implementation: see p. 232 for “Uses and Adult Dosages” and for “Maximum Daily Dose” Evaluation: report and record: - stomach irritation: give with food or milk, or large amounts of water - anorexia, nausea, vomiting, low blood pressure, drowsiness, confusion, abdominal pain, jaundice: signal liver toxicity
Other analgesic agents: propoxyphene (Darvon) - synthetic opiate agonist, used to relieve mild to moderate pain from muscle cramps, pre-menstrual cramps, minor surgery and trauma, and headache Assisting With the Nursing Process Assessment: Observe person’s speech pattern, degree of alertness and orientation to person, time and place. Measure vital signs. Measure intake/output. Ask person to rate pain. Planning: see pg. 233 for “Dose Forms” Implementation: usual adult dose 65 mg capsules or 100 mg tablets, every 4 hours, PRN Evaluation: report and record: - stomach irritation: give with food or milk - sedation or dizziness: sedation is usually mild, tends to resolve, provide for safety - excess use or abuse: always report complaints of pain or drug requests to the nurse at once - rash: may signal allergic reaction, tell nurse at once. Do not give next dose unless approved by nurse
Other analgesic agents: pentazocine (Talwin) - opiate partial agonist - if person has not received opiate agonists this is an effective analgesic - effect is similar to morphine when used within first few weeks of therapy - tolerance can develop with prolonged use - used for short-term relief (up to 3 weeks) of moderate to severe pain Assisting With the Nursing Process Assessment: Observe person’s speech pattern, degree of alertness and orientation to person, time and place. Measure vital signs. Ask person to rate pain. Planning: oral dose form 50 mg tablets Implementation: usual adult oral dose is 50 -100 mg every 3 -4 hours Evaluation: report and record: - clamminess, dizziness, sedation, nausea, vomiting, dry-mouth, sweating: tend to occur with first dose, supine position helps these symptoms, provide for safety - constipation: may occur with continued use, follow care plan - confusion, disorientation, hallucinations: provide for safety - respiratory depression: tell nurse if respiratory rate is 12 per minute or less, also tell nurse if person has shallow breathing - excess use or abuse: always report complaints of pain or drug requests to
 Res pain management
Res pain management Mad pain and martian pain
Mad pain and martian pain Breast tenderness early pregnancy
Breast tenderness early pregnancy Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps 7 tray in labour room
7 tray in labour room Drugs used in pregnancy
Drugs used in pregnancy Chapter 8 learning to manage
Chapter 8 learning to manage Drug glencoe
Drug glencoe Inhibitions drivers ed
Inhibitions drivers ed Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Chapter 22 lesson 1 the health risks of drug use
Chapter 22 lesson 1 the health risks of drug use Chapter 22 illegal drugs
Chapter 22 illegal drugs Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Chapter 44 antiinflammatory and antigout drugs
Chapter 44 antiinflammatory and antigout drugs Chapter 11 medications and drugs
Chapter 11 medications and drugs Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Chapter 6 drinking drugs and health
Chapter 6 drinking drugs and health Rpkbun
Rpkbun Stakeholders mapping
Stakeholders mapping Stakeholder matrix
Stakeholder matrix Direct and manage project execution
Direct and manage project execution Kata manajemen berasal dari bahasa
Kata manajemen berasal dari bahasa Manage men tactfully
Manage men tactfully Bsbpmg508a manage project risk
Bsbpmg508a manage project risk Blackberry devices working on january
Blackberry devices working on january