Chapter 17 Digestive System Disorders Copyright 2019 by
Chapter 17 Digestive System Disorders Copyright © 2019 by Elsevier Inc. All rights reserved.
Structures and Their Functions Upper Gastrointestinal Tract Liver Pancreas Lower Gastrointestinal Tract Copyright © 2019 by Elsevier Inc. All rights reserved. 2
Functions Processes ingested food and fluids Breaks them down into their units Ø Controlled by enzymes Ø Absorbs necessary components Membrane transport mechanisms Ø Mostly in small intestine Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 3
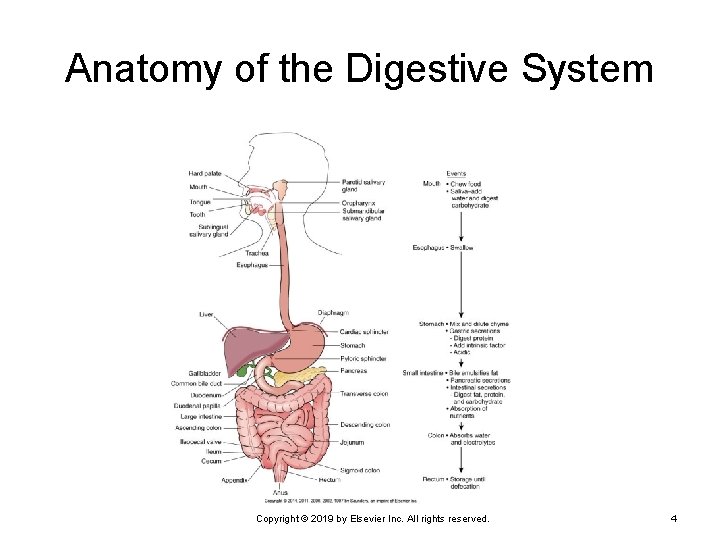
Anatomy of the Digestive System Copyright © 2019 by Elsevier Inc. All rights reserved. 4
Structures Gut wall Mucosa • Epithelium, including mucus-producing cells Ø Submucosa • Connective tissue—including blood vessels, nerves, Ø lymphatics, secretory glands Circular smooth muscle layer Ø Longitudinal smooth muscle layer Ø Serosa • Visceral peritoneum Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 5
Upper Gastrointestinal Tract Oral Cavity Esophagus Stomach Copyright © 2019 by Elsevier Inc. All rights reserved. 6
Oral Cavity Oral cavity Initial phase of mechanical breakdown of food • Mastication by teeth Ø Initial chemical digestion • Salivary amylase—starts chemical breakdown of Ø carbohydrates Ø Formation of bolus Pharynx Ø Swallowing (deglutition) Copyright © 2019 by Elsevier Inc. All rights reserved. 7
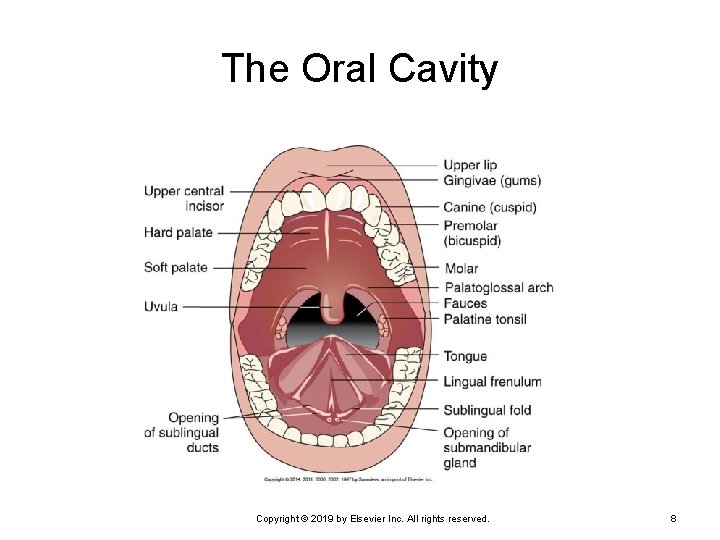
The Oral Cavity Copyright © 2019 by Elsevier Inc. All rights reserved. 8
Esophagus Closed except during swallowing, skeletal muscle at superior end—followed by smooth muscle Swallowing Ø Ø Ø The soft palate is pulled upward. The vocal cords are approximated. The epiglottis covers the larynx. Respiration ceases. The bolus is seized by the constricted pharynx. Bolus of food moves into the esophagus. Copyright © 2019 by Elsevier Inc. All rights reserved. 9
Stomach Expansible muscular sac—acts as reservoir food and fluid Three smooth muscle layers Constant mixing and churning of food Initial digestion of proteins Ø Production of intrinsic factor Ø By pepsin • Formed by combination of pepsinogen and HCl Essential for absorption of vitamin B 12 in the ileum Formation of chyme Absorption of small and lipid-soluble molecules Copyright © 2019 by Elsevier Inc. All rights reserved. 10
Liver “Metabolic factory” of the body Receives blood from hepatic portal vein Ø Hepatocytes store nutrients. Ø Transport of nutrients from intestine to liver Play role in carbohydrate, protein, fat metabolism Production of plasma proteins and clotting factors Breakdown of old and damaged erythrocytes Bile production Copyright © 2019 by Elsevier Inc. All rights reserved. 11
Pancreas Exocrine pancreas arranged in lobules Secretes digestive enzymes, electrolytes Trypsin Ø Chymotrypsin Ø Carboxypeptidase Ø Ribonuclease Ø Pancreatic amylase Ø Bicarbonate ions Ø Pancreatic duct joins bile duct to enter duodenum. Copyright © 2019 by Elsevier Inc. All rights reserved. 12
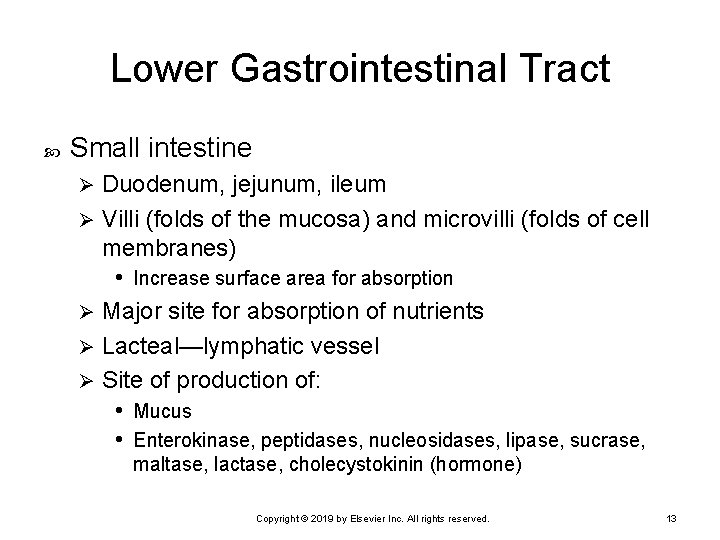
Lower Gastrointestinal Tract Small intestine Duodenum, jejunum, ileum Ø Villi (folds of the mucosa) and microvilli (folds of cell membranes) • Increase surface area for absorption Ø Major site for absorption of nutrients Ø Lacteal—lymphatic vessel Ø Site of production of: • Mucus • Enterokinase, peptidases, nucleosidases, lipase, sucrase, Ø maltase, lactase, cholecystokinin (hormone) Copyright © 2019 by Elsevier Inc. All rights reserved. 13
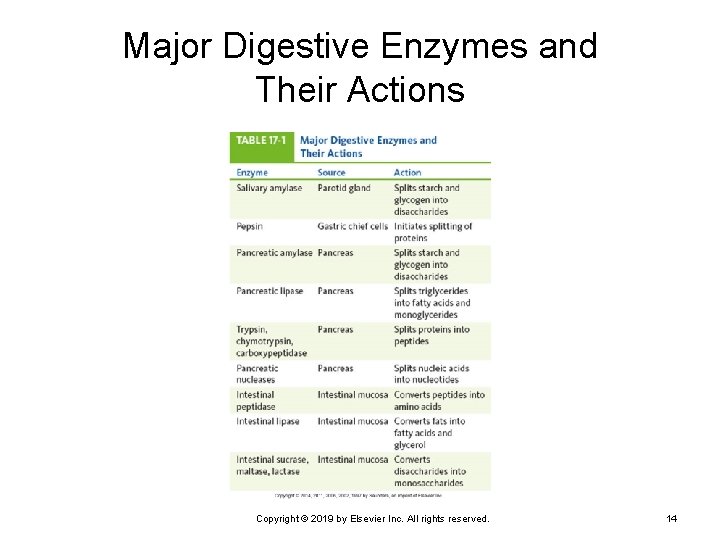
Major Digestive Enzymes and Their Actions Copyright © 2019 by Elsevier Inc. All rights reserved. 14
Lower Gastrointestinal Tract (Cont. ) Large intestine Peyer patches (lymphatic tissue) Ø Resident normal flora • Breakdown of certain food materials • Vitamin K synthesis by bacteria Ø Fluid and electrolyte reabsorption Ø Formation of solid feces • Mass movements Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 15
Neural and Hormonal Controls Parasympathetic nervous system (PNS) Primarily through vagus nerve (cranial nerve [CN] X) • Increased motility • Increased secretions Ø Sympathetic nervous system (SNS) Stimulated by factors such as fear, anger Ø Inhibits gastrointestinal activity Ø Causes vasoconstriction Ø Reduced secretions and regeneration of epithelial cells Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 16
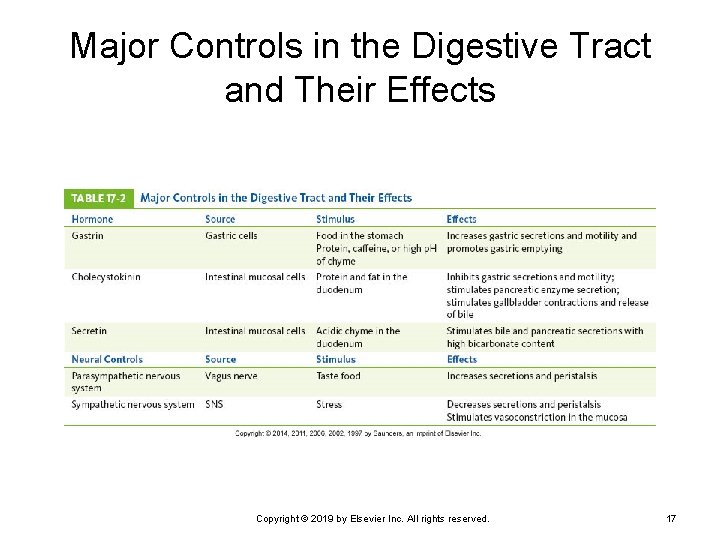
Major Controls in the Digestive Tract and Their Effects Copyright © 2019 by Elsevier Inc. All rights reserved. 17
Neural and Hormonal Controls (Cont. ) Facial (CN VII) and glossopharyngeal (CN IX) nerves Ø Maintain continuous flow of saliva in mouth Distention and stretching of stomach PNS activation Ø ↑ Peristalsis and gastric secretions Ø Stomach empties within 2 to 6 hours after meal. Food in intestine Stimulation of intestinal activity • Enterogastric reflex Ø Inhibition of gastric emptying Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 18
Hormonal Controls Gastrin Ø Secreted by mucosal cells (stomach) in response to distention of stomach or partially digested substances • Increases gastric motility, relaxes pyloric and ileocecal sphincters— promotes stomach emptying Histamine Ø Secretin Ø Increased secretion of hydrochloric acid Decreases gastric secretions Cholecystokinin Ø Inhibits gastric emptying; stimulates contraction of gallbladder Copyright © 2019 by Elsevier Inc. All rights reserved. 19
Digestion and Absorption Carbohydrates Digestion starts in mouth. Ø Followed by digestion in the small intestine Ø Proteins Ø Digestion starts in stomach, continues in small intestine. Lipids Emulsified by bile prior to chemical breakdown Ø Action of enzymes form monoglycerides and free fatty acids Ø Formation of chylomicrons Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 20
Digestion and Absorption (Cont. ) Fat-soluble vitamins Ø Water-soluble vitamins Ø Vitamins B and C—diffuse into blood Electrolytes Ø Vitamins A, D, E, K • Absorbed with fats Absorbed by active transport or diffusion Drugs are primarily absorbed in the intestine. Various transport mechanisms Ø Some (e. g. , aspirin) absorbed in the stomach Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 21
Digestion and Absorption (Cont. ) Water Absorbed primarily by osmosis Ø About 700 m. L of water is secreted into the digestive tract each day. Ø About 2300 m. L is ingested in food and fluids. Ø Only 50 to 200 m. L leaves the body in feces. Ø Severe vomiting or diarrhea will interrupt this recycling mechanism. • Affects fluid and electrolyte balance of body Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 22
Common Manifestations of Digestive System Disorders Anorexia, Nausea, Vomiting, and Bulimia Diarrhea Constipation Fluid and Electrolyte Imbalances Pain Malnutrition Copyright © 2019 by Elsevier Inc. All rights reserved. 23
Anorexia, Nausea, Vomiting, and Bulimia May be signs of digestive disorder or other condition elsewhere in the body Systemic infection Ø Uremia Ø Emotional responses Ø Motion sickness Ø Pressure in the brain Ø Overindulgence of food, drugs Ø Pain Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 24
Anorexia, Nausea, Vomiting, and Bulimia (Cont. ) Anorexia and vomiting Ø Anorexia Ø Can cause serious complications • Dehydration, acidosis, malnutrition Often precedes nausea and vomiting Nausea Unpleasant subjective feeling Ø Simulated by distention, irritation, inflammation of digestive tract Ø Also stimulated by smells, visual images, pain, and chemical toxins and/or drugs Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 25
Anorexia, Nausea, Vomiting, and Bulimia (Cont. ) Vomiting (emesis) Vomiting center located in the medulla • Coordinates activities involved in vomiting • Protects airway during vomiting Ø Forceful expulsion of chyme from stomach • Sometimes includes bile from intestine Ø Bulimia—eating disorder Ø Damage to structures of the GI tract caused by recurrent vomiting • Oral mucosa • Teeth • Esophagus Copyright © 2019 by Elsevier Inc. All rights reserved. 26
Vomiting Center Activation Distention or irritation in digestive tract Stimuli from various parts of the brain Ø Pain or stress Vestibular apparatus of inner ear (motion) Increased intracranial pressure Ø Response to unpleasant sights or smells, ischemia Sudden projectile vomiting without previous nausea Stimulation of chemoreceptor trigger zone Ø By drugs, toxins, chemicals Copyright © 2019 by Elsevier Inc. All rights reserved. 27
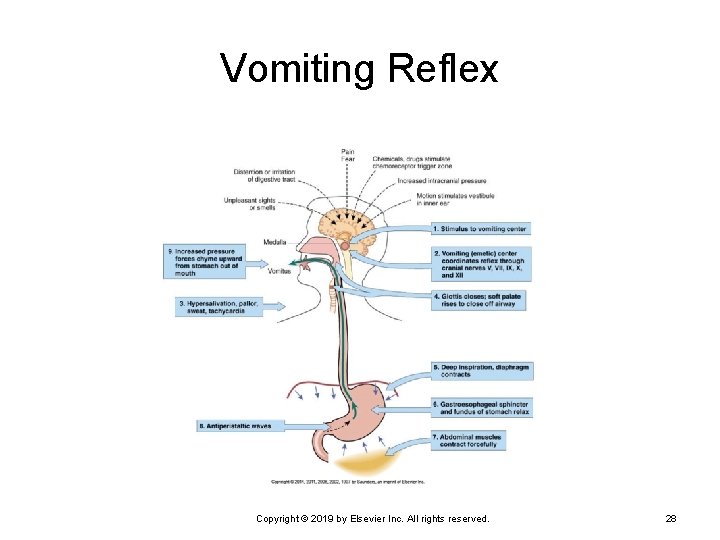
Vomiting Reflex Copyright © 2019 by Elsevier Inc. All rights reserved. 28
Vomiting Reflex Activities Deep inspiration Closing the glottis, raising the soft palate Ceasing respiration Ø Relaxing the gastroesophageal sphincter Contracting the abdominal muscles Ø Minimizes risk of aspiration of vomitus into lungs Forces gastric contents upward Reversing peristaltic waves Ø Promotes expulsion of stomach contents Copyright © 2019 by Elsevier Inc. All rights reserved. 29
Characteristics of Vomitus Presence of blood—hematemesis Coffee ground vomitus—brown granular material indicates action of HCl on hemoglobin Ø Hemorrhage—red blood may be in vomitus Ø Yellow- or green-stained vomitus Ø Deeper brown color Ø Bile from the duodenum May indicate content from lower intestine Recurrent vomiting of undigested food Ø Problem with gastric emptying or infection Copyright © 2019 by Elsevier Inc. All rights reserved. 30
Diarrhea Excessive frequency of stools Ø Usually of loose or watery consistency May be acute or chronic Frequently with nausea and vomiting when infection or inflammation develops May be accompanied by cramping pain Prolonged diarrhea may lead to dehydration, electrolyte imbalance, acidosis, malnutrition. Copyright © 2019 by Elsevier Inc. All rights reserved. 31
Common Types of Diarrhea Large-volume diarrhea (secretory or osmotic) Watery stool resulting from increased secretions into intestine from the plasma Ø Often related to infection Ø Limited reabsorption because of reversal of normal carriers for sodium and/or glucose Ø Small-volume diarrhea Often caused by inflammatory bowel disease Ø Stool may contain blood, mucus, pus. Ø May be accompanied by abdominal cramps and tenesmus Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 32
Common Types of Diarrhea (Cont. ) Steatorrhea—“fatty diarrhea” Frequent bulky, greasy, loose stools Ø Foul odor Ø Characteristic of malabsorption syndromes • Celiac disease, cystic fibrosis Ø Fat usually the first dietary component affected • Presence interferes with digestion of other nutrients. Ø Abdomen often distended Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 33
Blood in Stool Blood may occur in normal stools with diarrhea, constipation, tumors, or an inflammatory condition. Frank blood • Red blood—usually from lesions in rectum or anal canal Ø Occult blood • Small hidden amounts, detectable with stool test • May be caused by small bleeding ulcers Ø Melena • Dark-colored, tarry stool • May result from significant bleeding in upper digestive tract Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 34
Gas From swallowed air, such as drinking from a straw Bacterial action on food Foods or alterations in motility Excessive gas causes: Eructation Ø Borborygmus Ø Abdominal distention and pain Ø Flatus Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 35
Constipation Less frequent bowel movements than normal Small hard stools Acute or chronic problem May be caused by decreased peristalsis Ø Increased time for reabsorption of fluid Periods of constipation may alter with periods of diarrhea. Chronic constipation may cause hemorrhoids, anal fissures, or diverticulitis. Copyright © 2019 by Elsevier Inc. All rights reserved. 36
Causes of Constipation Weakness of smooth muscle because of age or illness Inadequate dietary fiber Inadequate fluid intake Failure to respond to defecation reflex Immobility Neurological disorders Drugs (i. e. , opiates) Some antacids, iron medications Obstructions caused by tumors or strictures Copyright © 2019 by Elsevier Inc. All rights reserved. 37

Fluid and Electrolyte Imbalances Dehydration and hypovolemia are common complications of digestive tract disorders. Electrolytes Ø Lost in vomiting and diarrhea Acid-base imbalances Metabolic alkalosis • Results from loss of hydrochloric acid with vomiting Ø Metabolic acidosis • Severe vomiting causes a change to metabolic acidosis Ø because of the loss of bicarbonate of duodenal secretions. • Diarrhea causes loss of bicarbonate. Copyright © 2019 by Elsevier Inc. All rights reserved. 38
Pain: Visceral Pain Burning sensation Ø Dull, aching pain Ø Typical result of stretching of liver capsule Cramping or diffuse pain Ø Inflammation and ulceration in upper digestive tract Inflammation, distention, stretching of intestines Colicky, often severe pain Ø Recurrent smooth muscle spasms or contraction • Response to severe inflammation or obstruction Copyright © 2019 by Elsevier Inc. All rights reserved. 39
Pain: Somatic Pain Somatic pain receptors directly linked to spinal nerves Ø May cause reflex spasm of overlying abdominal muscles Steady, intense, often well-localized abdominal pain Involvement or inflammation of parietal peritoneum Rebound tenderness—identified over area of inflammation when pressure is released Copyright © 2019 by Elsevier Inc. All rights reserved. 40
Pain: Referred Pain Common phenomenon Pain is perceived at a site different from origin. Results when visceral and somatic nerves converge at one spinal cord level Source of visceral pain is perceived as the same as that of the somatic nerve. May assist or delay diagnosis, depending on problem Copyright © 2019 by Elsevier Inc. All rights reserved. 41
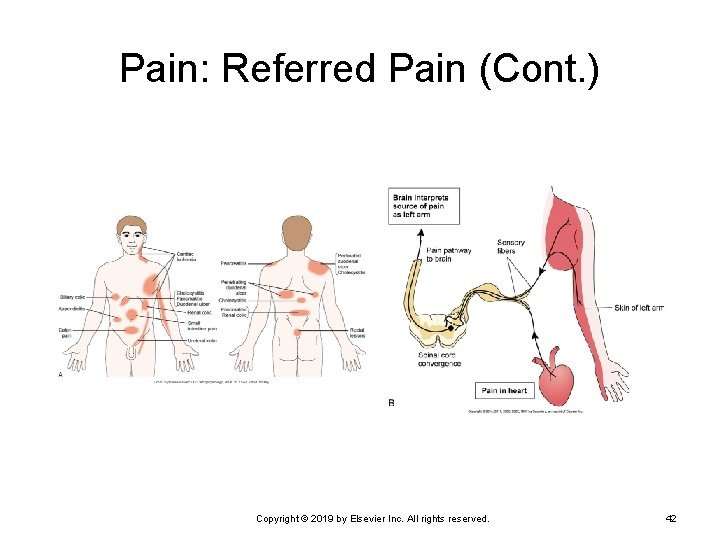
Pain: Referred Pain (Cont. ) Copyright © 2019 by Elsevier Inc. All rights reserved. 42
Malnutrition May be limited to a specific nutrient or general Causes of limited malnutrition—specific problem Vitamin B 12 deficiency Ø Iron deficiency Ø Causes of generalized malnutrition Chronic anorexia, vomiting, diarrhea Ø Other systemic causes • Chronic inflammatory bowel disorders • Cancer treatments • Wasting syndrome • Lack of available nutrients Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 43
Basic Diagnostic Tests Radiography Ø Ultrasound Ø Contrast medium may be used. May show unusual masses Computed tomography (CT) Magnetic resonance imaging (MRI) CT and MRI may use radioactive tracers. Ø Can be used for liver and pancreatic abnormalities Copyright © 2019 by Elsevier Inc. All rights reserved. 44
Basic Diagnostic Tests (Cont. ) Fiberoptic endoscopy used in upper GI tract Ø Sigmoidoscopy and colonoscopy Ø Biopsy and removal of polyps may be done. Laboratory analysis of stool specimens Ø Biopsy may be done during procedures. Check for infection, parasites and ova, bleeding, tumors, malabsorption Blood tests Ø Liver function, pancreatic function, cancer markers Copyright © 2019 by Elsevier Inc. All rights reserved. 45
Common Therapies and Prevention Dietary modifications Example—gluten-free diet (celiac disease) Ø Reduced intake of alcohol and coffee Ø Increased fiber and fluid intake Ø Stress reduction techniques Ø Stress impairs immune function and tissue healing. Drugs Ø A variety of medications are available. Copyright © 2019 by Elsevier Inc. All rights reserved. 46
Drugs Used in Digestive System Disorders Antacids Ø Antiemetics Ø To relieve vomiting Laxatives or enemas Ø To relieve pyrosis Treatment of acute constipation Antidiarrheals Reduction of peristalsis Ø Relieve cramps Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 47
Drugs Used in Digestive System Disorders (Cont. ) Sulfasalazine Antiinflammatory and antibacterial Ø Used for acute episodes of inflammatory bowel disease Ø Clarithromycin or azithromycin Ø Effective against Helicobacter pylori infection • Usually combined with a proton pump inhibitor Sucralfate Coating agent Ø Enhance gastric mucosal barrier against irritants such as nonsteroidal antiinflammatory drugs (NSAIDs) Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 48
Drugs Used in Digestive System Disorders (Cont. ) Anticholinergic drugs Reduce PNS activity Ø Reduce secretions and motility Ø Histamine 2 antagonists Ø Useful for gastric reflux Proton pump inhibitors Ø Reduce gastric secretion Copyright © 2019 by Elsevier Inc. All rights reserved. 49
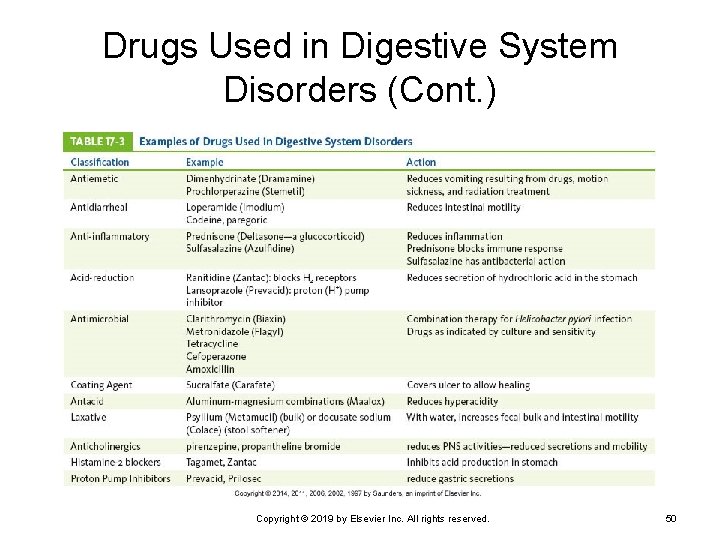
Drugs Used in Digestive System Disorders (Cont. ) Copyright © 2019 by Elsevier Inc. All rights reserved. 50
Upper Gastrointestinal Tract Disorders Disorders of the oral cavity Dysphagia Esophageal cancer Hiatal hernia Gastroesophageal reflux disease Gastritis Peptic ulcer Gastric cancer Dumping syndrome Pyloric stenosis Copyright © 2019 by Elsevier Inc. All rights reserved. 51
Disorders of the Oral Cavity Congenital abnormalities Cleft lip and cleft palate Ø Arise in sixth to seventh week of gestation Ø Most likely of multifactorial origin Ø Feeding problems of the infant • High risk of aspirating fluid into respiratory passages Ø Speech development impaired Ø Surgical repair done as soon as possible Ø Therapy with speech-language pathologist and orthodontist Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 52
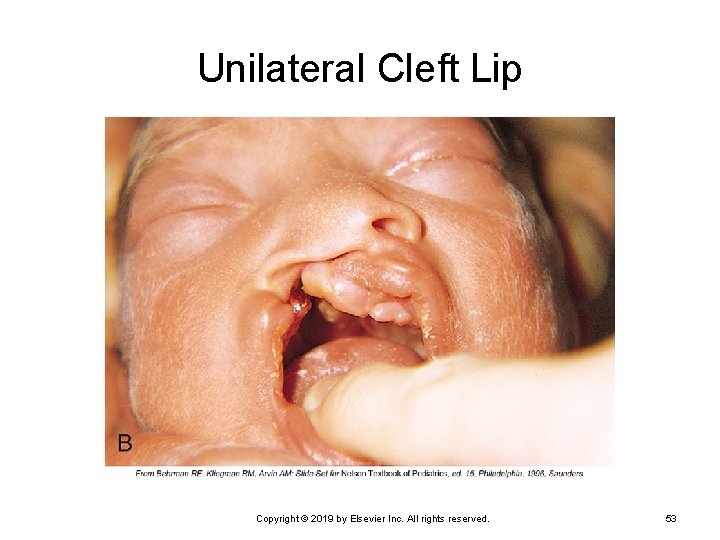
Unilateral Cleft Lip Copyright © 2019 by Elsevier Inc. All rights reserved. 53
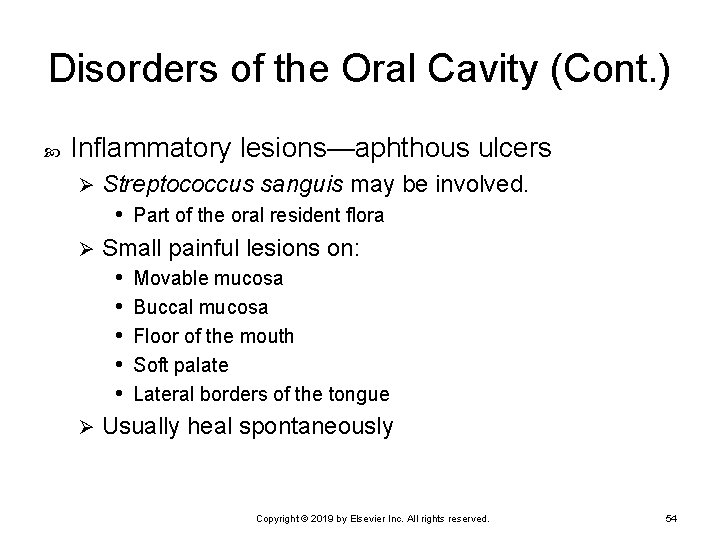
Disorders of the Oral Cavity (Cont. ) Inflammatory lesions—aphthous ulcers Streptococcus sanguis may be involved. • Part of the oral resident flora Ø Small painful lesions on: • Movable mucosa • Buccal mucosa • Floor of the mouth • Soft palate • Lateral borders of the tongue Ø Usually heal spontaneously Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 54
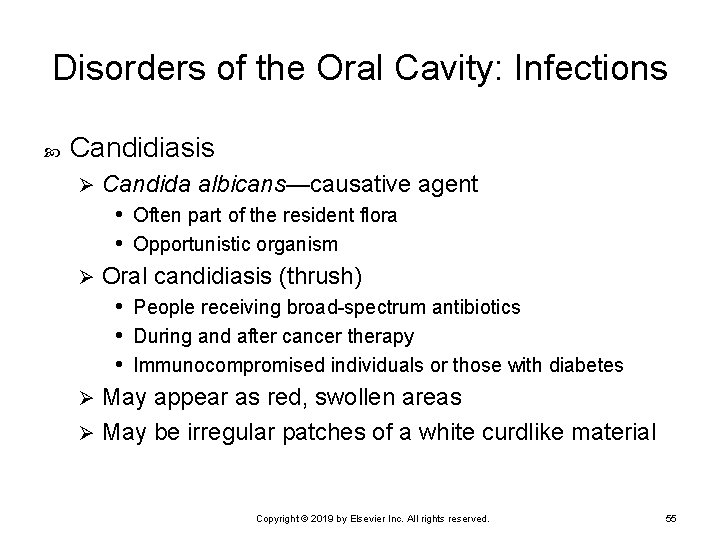
Disorders of the Oral Cavity: Infections Candidiasis Candida albicans—causative agent • Often part of the resident flora • Opportunistic organism Ø Oral candidiasis (thrush) • People receiving broad-spectrum antibiotics • During and after cancer therapy • Immunocompromised individuals or those with diabetes Ø May appear as red, swollen areas Ø May be irregular patches of a white curdlike material Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 55
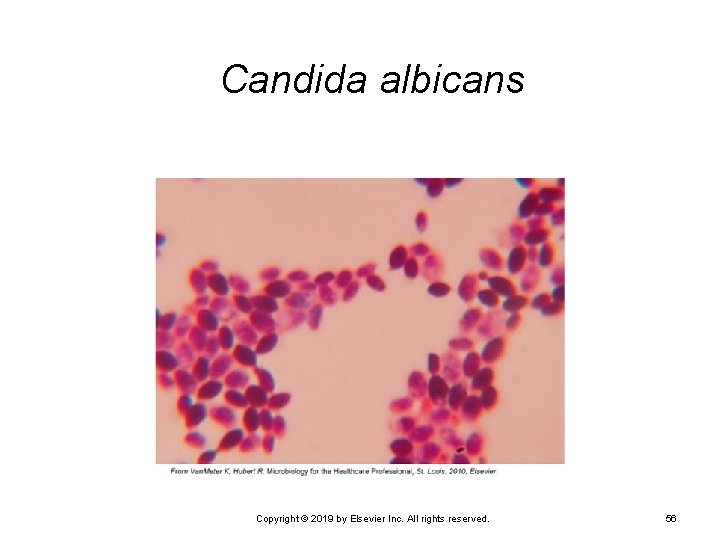
Candida albicans Copyright © 2019 by Elsevier Inc. All rights reserved. 56
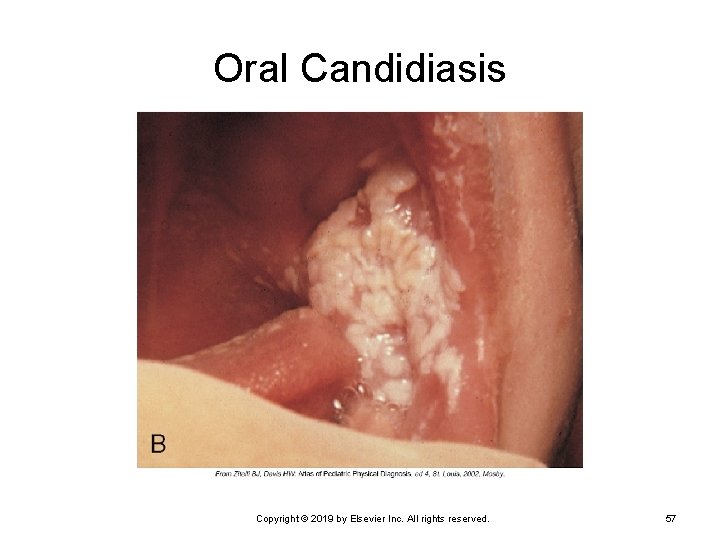
Oral Candidiasis Copyright © 2019 by Elsevier Inc. All rights reserved. 57
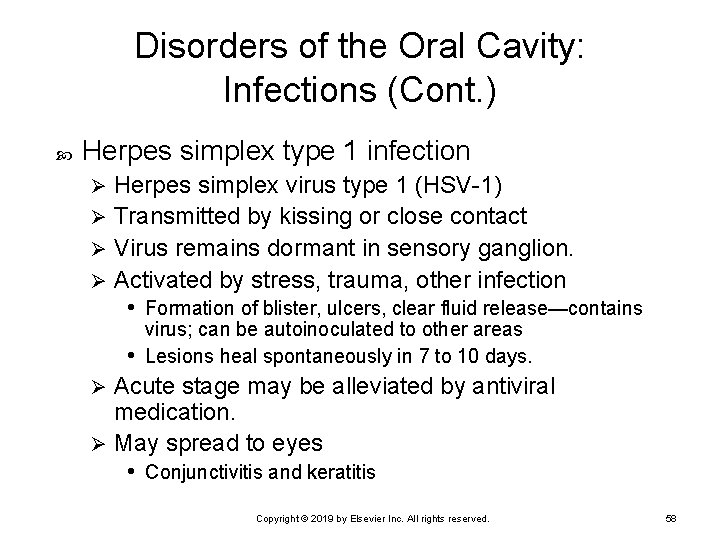
Disorders of the Oral Cavity: Infections (Cont. ) Herpes simplex type 1 infection Herpes simplex virus type 1 (HSV-1) Ø Transmitted by kissing or close contact Ø Virus remains dormant in sensory ganglion. Ø Activated by stress, trauma, other infection • Formation of blister, ulcers, clear fluid release—contains Ø virus; can be autoinoculated to other areas • Lesions heal spontaneously in 7 to 10 days. Acute stage may be alleviated by antiviral medication. Ø May spread to eyes • Conjunctivitis and keratitis Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 58
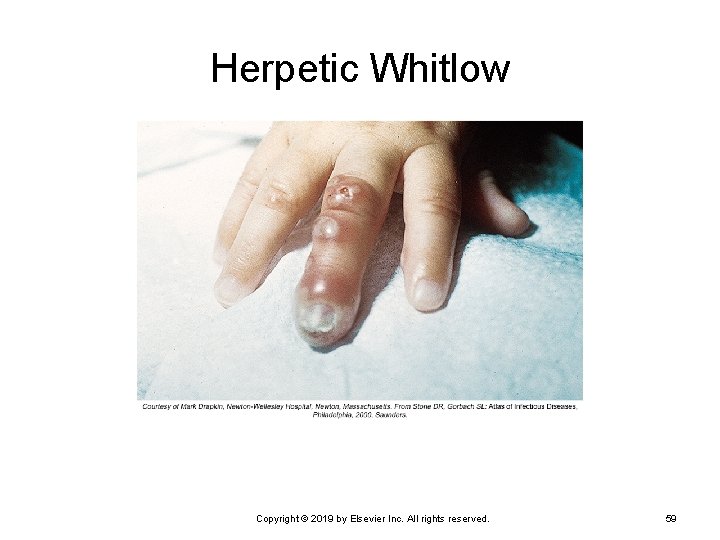
Herpetic Whitlow Copyright © 2019 by Elsevier Inc. All rights reserved. 59
Disorders of the Oral Cavity: Infections (Cont. ) Syphilis Caused by Treponema pallidum Ø May cause oral lesions Ø Highly contagious during first and second stages Ø Primary stage • Chancre, a painless ulcer on tongue, lip, palate • Heals spontaneously (1 or 2 weeks) Ø Secondary stage • Red macules or papules on palate—highly infectious • Heals spontaneously Ø Both stages treated with long-acting penicillin Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 60
Disorders of the Oral Cavity: Dental Problems Caries Streptococcus mutans—initiating microbe Ø Lactobacillus follows in large numbers. Ø Bacteria break down sugars and produce large quantities of lactic acid. Ø Lactic acid dissolves mineral in tooth enamel. Ø Tooth erosion and caries formation Ø Caries is promoted by frequent intake of sugars and acids. Ø Fluoride—anticaries treatment Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 61
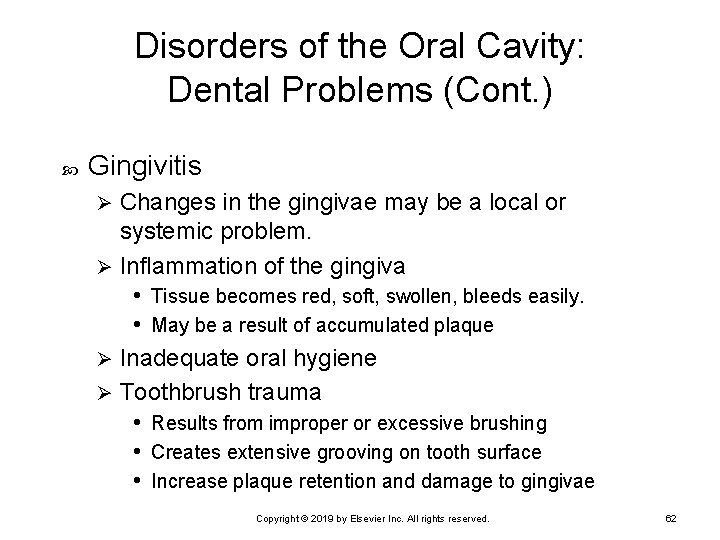
Disorders of the Oral Cavity: Dental Problems (Cont. ) Gingivitis Changes in the gingivae may be a local or systemic problem. Ø Inflammation of the gingiva • Tissue becomes red, soft, swollen, bleeds easily. • May be a result of accumulated plaque Ø Inadequate oral hygiene Ø Toothbrush trauma • Results from improper or excessive brushing • Creates extensive grooving on tooth surface • Increase plaque retention and damage to gingivae Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 62
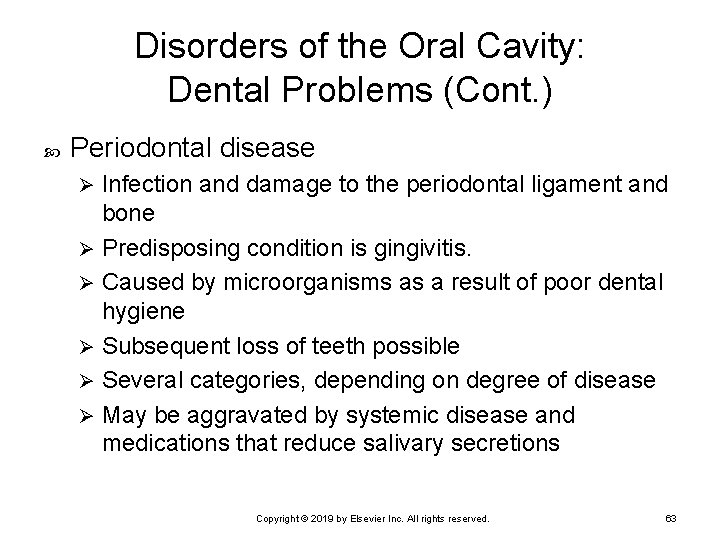
Disorders of the Oral Cavity: Dental Problems (Cont. ) Periodontal disease Infection and damage to the periodontal ligament and bone Ø Predisposing condition is gingivitis. Ø Caused by microorganisms as a result of poor dental hygiene Ø Subsequent loss of teeth possible Ø Several categories, depending on degree of disease Ø May be aggravated by systemic disease and medications that reduce salivary secretions Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 63
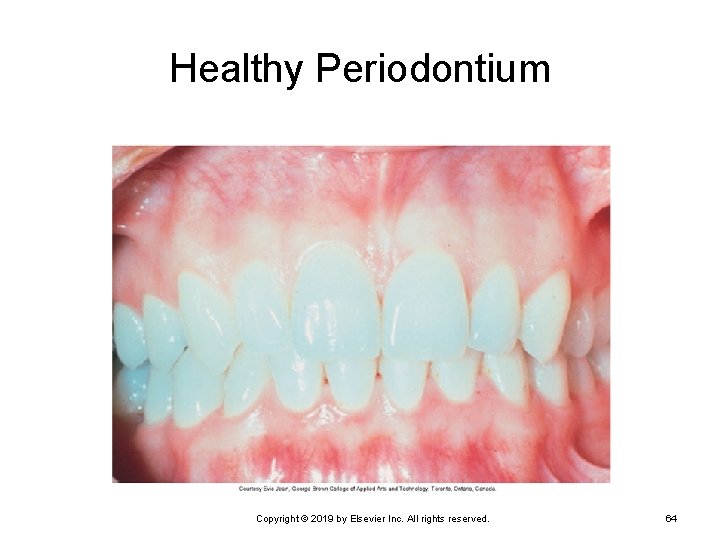
Healthy Periodontium Copyright © 2019 by Elsevier Inc. All rights reserved. 64
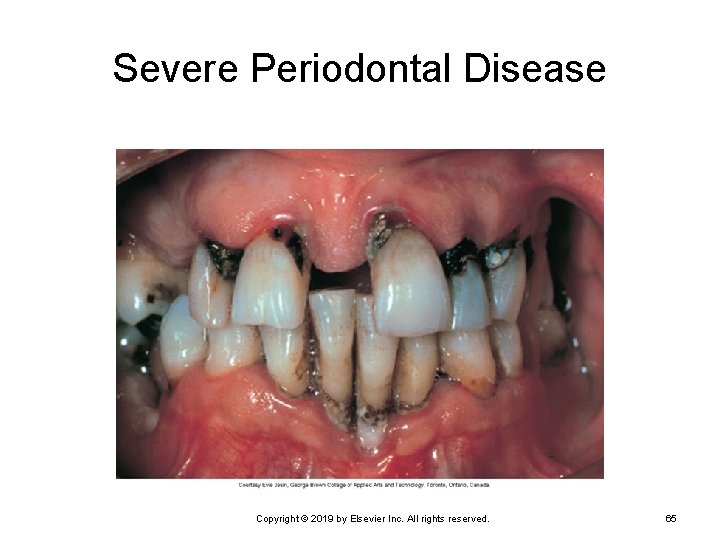
Severe Periodontal Disease Copyright © 2019 by Elsevier Inc. All rights reserved. 65
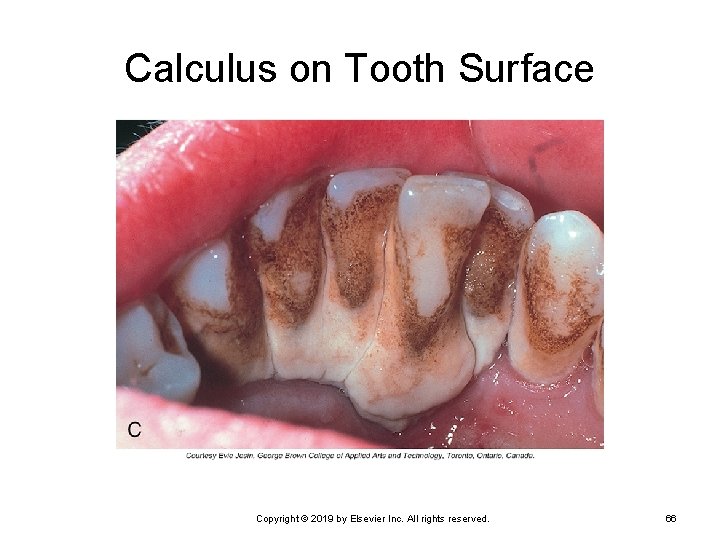
Calculus on Tooth Surface Copyright © 2019 by Elsevier Inc. All rights reserved. 66
Disorders of the Oral Cavity: Dental Problems (Cont. ) Periodontitis occurs when organisms enter the gingival blood vessels and travel to the connective tissues and bone of the dental arch. Resorption of bone and loss of ligament fibers result in weakened attachment of teeth. May result in total loss of tooth from socket Treated by antimicrobials, local surgery of gingiva, and improved dental hygiene Copyright © 2019 by Elsevier Inc. All rights reserved. 67
Disorders of the Oral Cavity: Dental Problems (Cont. ) Hyperkeratosis Leukoplakia (example) Ø Whitish plaque or epidermal thickening of mucosa Ø Occurs on buccal mucosa, palate, lower lip Ø May be related to smoking or chronic irritation Ø Lesions require monitoring. • Epithelial dysplasia beneath plaque may develop into Ø squamous cell carcinoma. Copyright © 2019 by Elsevier Inc. All rights reserved. 68
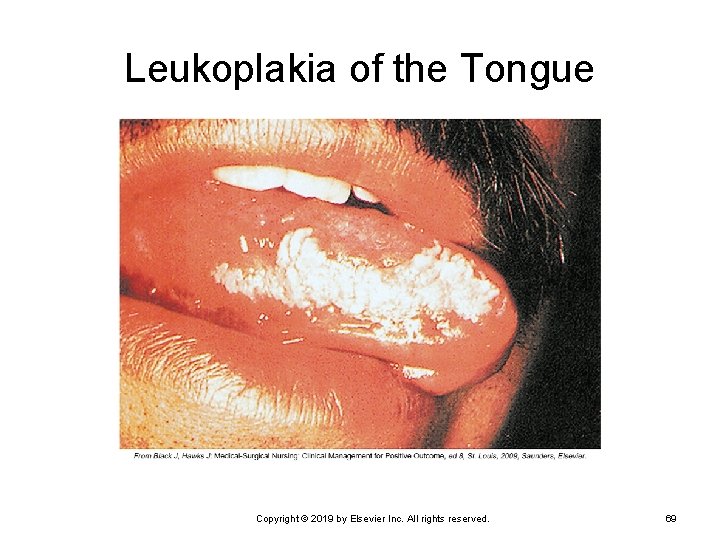
Leukoplakia of the Tongue Copyright © 2019 by Elsevier Inc. All rights reserved. 69
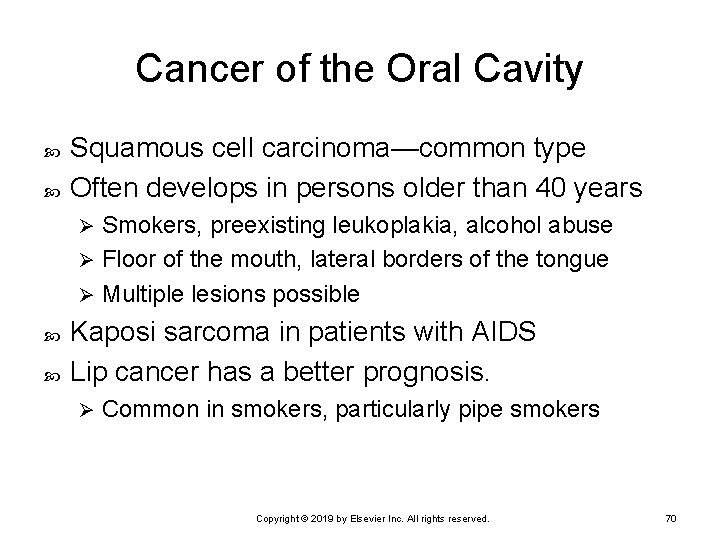
Cancer of the Oral Cavity Squamous cell carcinoma—common type Often develops in persons older than 40 years Smokers, preexisting leukoplakia, alcohol abuse Ø Floor of the mouth, lateral borders of the tongue Ø Multiple lesions possible Ø Kaposi sarcoma in patients with AIDS Lip cancer has a better prognosis. Ø Common in smokers, particularly pipe smokers Copyright © 2019 by Elsevier Inc. All rights reserved. 70
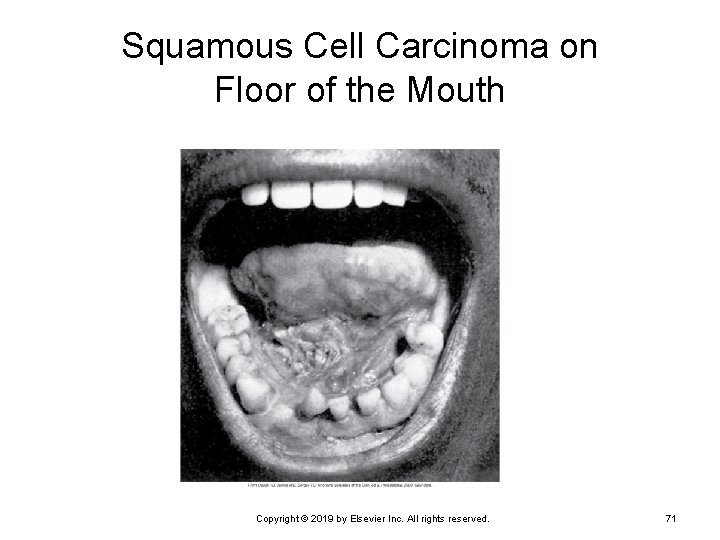
Squamous Cell Carcinoma on Floor of the Mouth Copyright © 2019 by Elsevier Inc. All rights reserved. 71
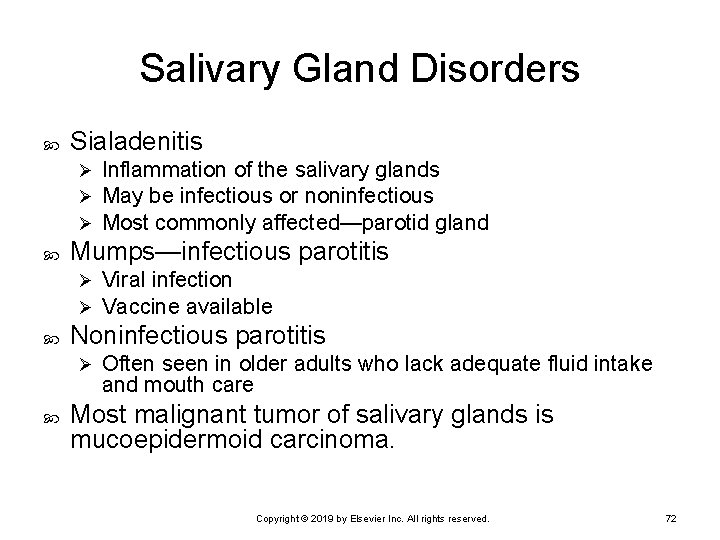
Salivary Gland Disorders Sialadenitis Ø Ø Ø Mumps—infectious parotitis Ø Ø Viral infection Vaccine available Noninfectious parotitis Ø Inflammation of the salivary glands May be infectious or noninfectious Most commonly affected—parotid gland Often seen in older adults who lack adequate fluid intake and mouth care Most malignant tumor of salivary glands is mucoepidermoid carcinoma. Copyright © 2019 by Elsevier Inc. All rights reserved. 72
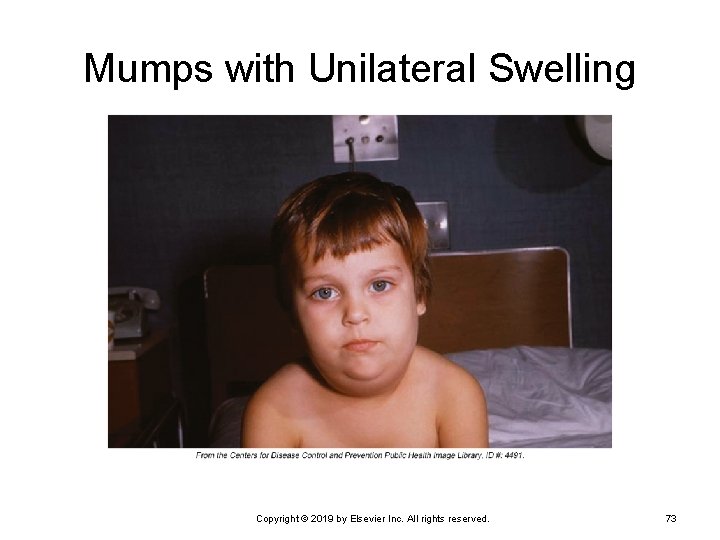
Mumps with Unilateral Swelling Copyright © 2019 by Elsevier Inc. All rights reserved. 73
Dysphagia Difficulty swallowing Causes Neurologic deficit Ø Muscular disorder Ø Mechanical obstruction Ø Results and presentation Pain with swallowing Ø Inability to swallow larger pieces of solid material Ø Difficulty swallowing liquids Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 74
Dysphagia (Cont. ) Neurological deficit Infection Ø Stroke Ø Brain damage Ø Achalasia • Failure of the lower esophageal sphincter to relax because of Ø lack of innervation Muscular disorder Ø Impairment from muscular dystrophy Copyright © 2019 by Elsevier Inc. All rights reserved. 75
Dysphagia (Cont. ) Mechanical obstruction Congenital atresia • Developmental anomaly • Upper and lower esophageal segments are separated. Ø Stenosis • Narrowing of the esophagus • May be developmental or acquired • May be secondary to fibrosis, chronic inflammation, Ø ulceration, radiation therapy • Stenosis or stricture may also result from scar tissue. • May require treatment with repeated mechanical dilation Copyright © 2019 by Elsevier Inc. All rights reserved. 76
Dysphagia (Cont. ) Mechanical obstruction (cont. ) Ø Esophageal diverticula • Outpouchings of the esophageal wall • Congenital or acquired following inflammation • Causes irritation, inflammation, scar tissue • Signs include dysphagia, foul breath, chronic cough, hoarseness Ø Tumors • May be internal or external Copyright © 2019 by Elsevier Inc. All rights reserved. 77
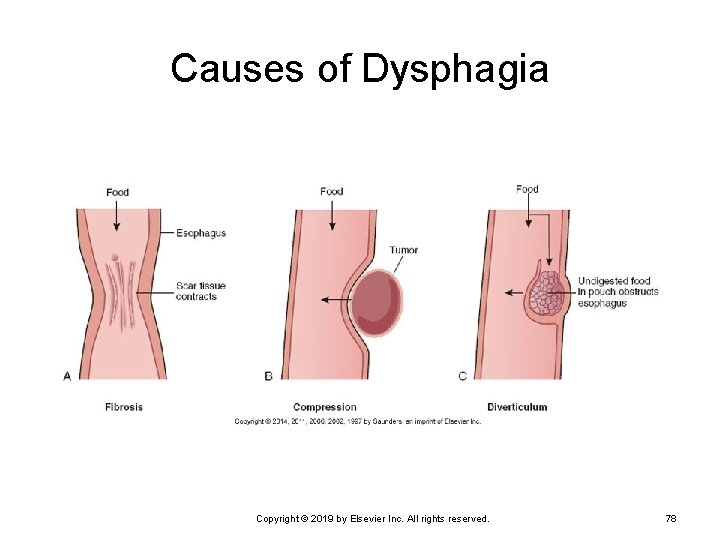
Causes of Dysphagia Copyright © 2019 by Elsevier Inc. All rights reserved. 78
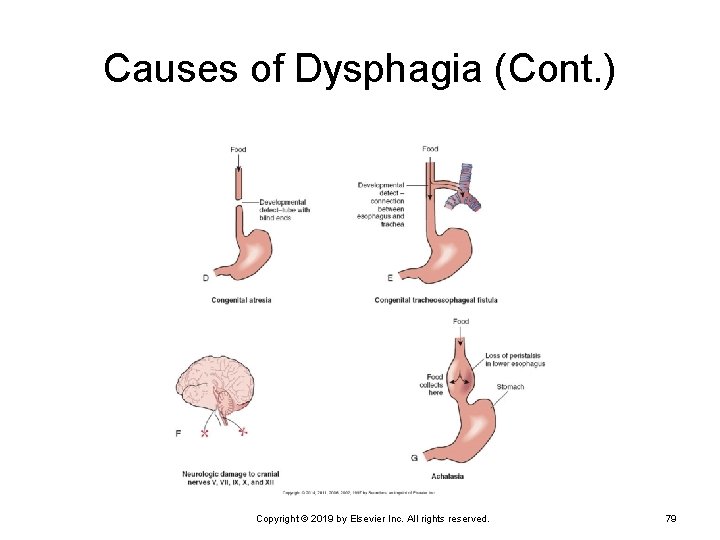
Causes of Dysphagia (Cont. ) Copyright © 2019 by Elsevier Inc. All rights reserved. 79
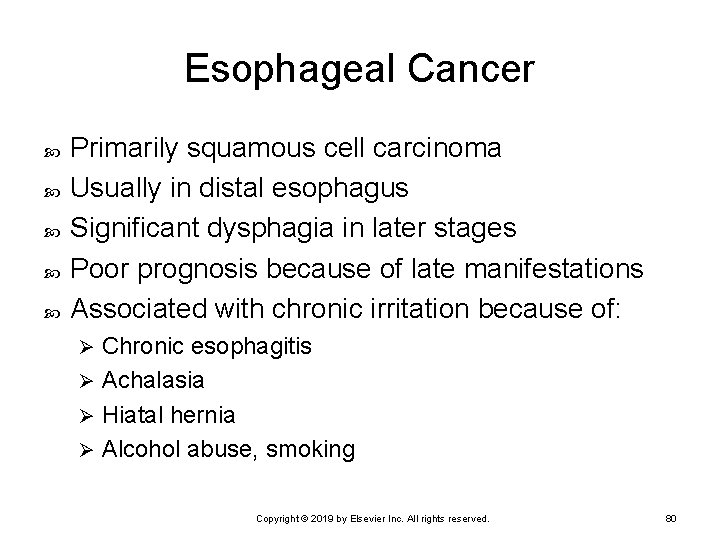
Esophageal Cancer Primarily squamous cell carcinoma Usually in distal esophagus Significant dysphagia in later stages Poor prognosis because of late manifestations Associated with chronic irritation because of: Chronic esophagitis Ø Achalasia Ø Hiatal hernia Ø Alcohol abuse, smoking Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 80
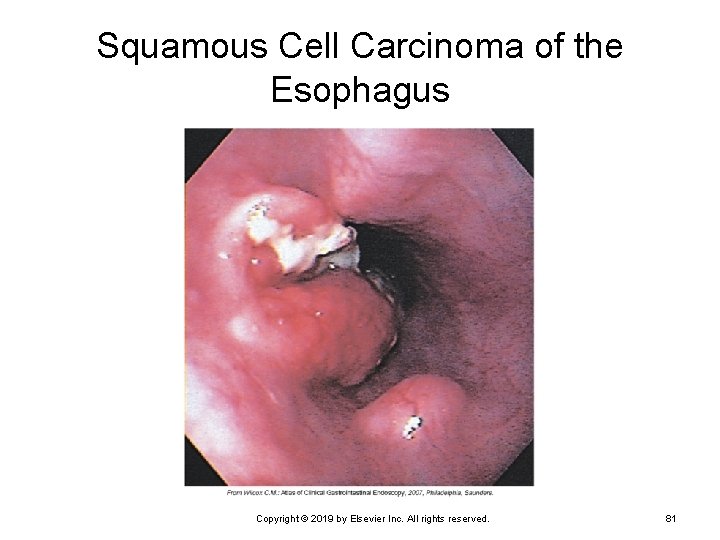
Squamous Cell Carcinoma of the Esophagus Copyright © 2019 by Elsevier Inc. All rights reserved. 81
Hiatal Hernia Part of the stomach protrudes into the thoracic cavity. Sliding hernia More common type Ø Portions of the stomach and gastroesophageal junction slide up above the diaphragm. Ø Rolling or paraesophageal hernia Ø Part of the fundus of the stomach moves up through an enlarged or weak hiatus in the diaphragm and may become trapped. Copyright © 2019 by Elsevier Inc. All rights reserved. 82
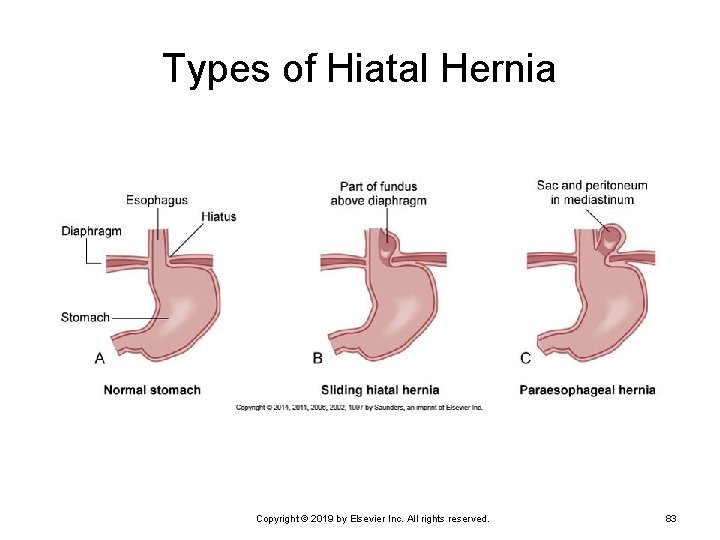
Types of Hiatal Hernia Copyright © 2019 by Elsevier Inc. All rights reserved. 83
Hiatal Hernia (Cont. ) Food may lodge in pouch of the hernia Causes inflammation of the mucosa Ø Reflux of food up the esophagus Ø May cause chronic esophagitis Ø Signs Heartburn or pyrosis Ø Frequent belching Ø Increased discomfort when laying down Ø Substernal pain that may radiate to shoulder and jaw Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 84
Gastroesophageal Reflux Disease Periodic reflux of gastric contents into distal esophagus causes erosion and inflammation. Often seen in conjunction with hiatal hernia Severity depends on competence of the lower esophageal sphincter. Delayed gastric emptying may be a factor. Avoidance of: Ø Caffeine, fatty and spicy foods, alcohol, smoking, certain drugs Use of medication may reduce reflux and inflammation. Copyright © 2019 by Elsevier Inc. All rights reserved. 85

Gastritis: Acute Gastritis Gastric mucosa is inflamed. May be ulcerated and bleeding May result from Infection by microorganisms Ø Allergies to foods Ø Spicy or irritating foods Ø Excessive alcohol intake Ø Ingestion of aspirin or other NSAIDs Ø Ingestion of corrosive or toxic substances Ø Radiation or chemotherapy Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 86
Gastritis: Acute Gastritis (Cont. ) Basic signs of gastrointestinal irritation Anorexia, nausea, vomiting may develop Ø Hematemesis caused by bleeding Ø Epigastric pain, cramps or general discomfort Ø With infection, diarrhea may develop. Ø Acute gastritis is usually self-limiting. Complete regeneration of gastric mucosa Ø Supportive treatment with prolonged vomiting Ø May require treatment with antimicrobial drugs Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 87
Gastritis: Chronic Gastritis Characterized by atrophy of stomach mucosa Loss of secretory glands Ø Reduced production of intrinsic factor Ø Helicobacter pylori infection is often present. Signs may be vague. Ø Mild epigastric discomfort, anorexia, intolerance for certain foods Increased risk of peptic ulcers and gastric carcinoma Certain autoimmune disorders are associated with one type of chronic gastric atrophy. Copyright © 2019 by Elsevier Inc. All rights reserved. 88
Gastritis: Gastroenteritis Inflammation of stomach and intestine Usually caused by infection May also be caused by allergic reactions to food or drugs Microbes can be transmitted by fecally contaminated food, soil, and/or water. Most infections are self-limiting. Ø Serious illness may result in compromised host or virulent organisms. Ø May cause epidemic outbreaks in refugee or disaster settings Ø Safe sanitation essential for prevention Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 89
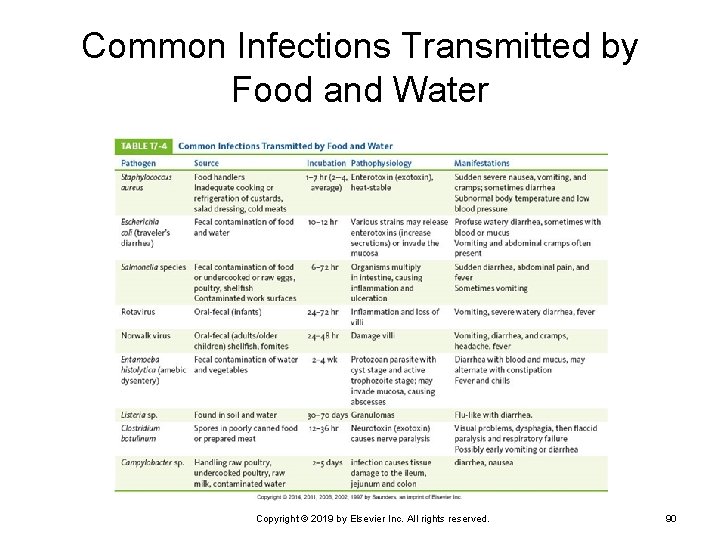
Common Infections Transmitted by Food and Water Copyright © 2019 by Elsevier Inc. All rights reserved. 90
Escherichia coli Infection Although E. coli is usually harmless as a resident in the human intestine, infective strains can cause significant problems. Infective strains Enterotoxigenic E. coli Ø Enteroinvasive E. coli Ø Enteropathogenic E. coli Ø Enteroaggregative E. coli Ø Enterohemorrhagic E. coli Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 91
Peptic Ulcer: Gastric and Duodenal Ulcers Most caused by H. pylori infection Usually occur in the proximal duodenum (duodenal ulcers) Also found in the antrum of the stomach (gastric ulcers) Development begins with breakdown of mucosal barrier. Decreased mucosal defense Ø More common in gastric ulcer development Ø Increased acid secretion predominant factor in duodenal ulcers Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 92
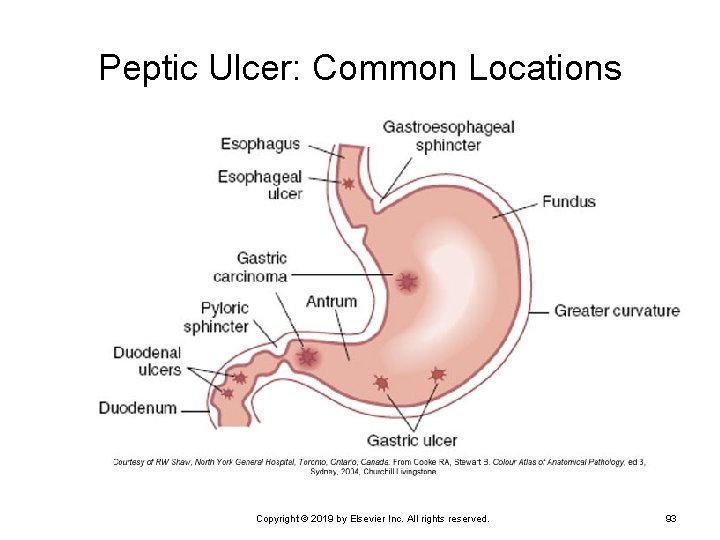
Peptic Ulcer: Common Locations Copyright © 2019 by Elsevier Inc. All rights reserved. 93
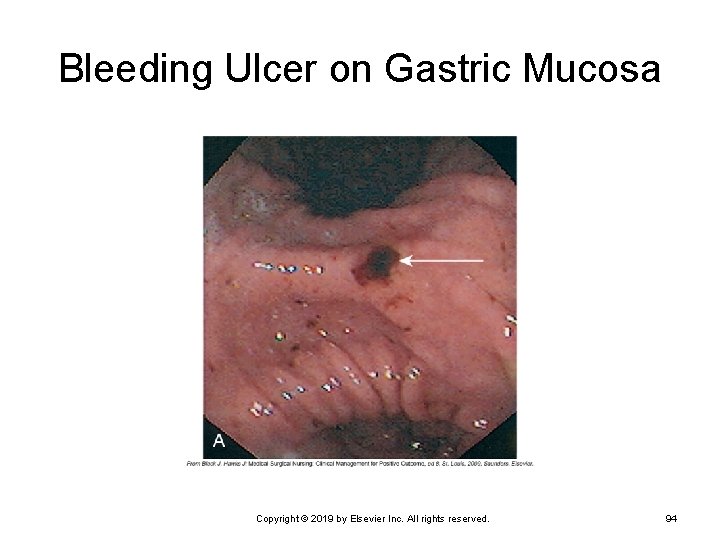
Bleeding Ulcer on Gastric Mucosa Copyright © 2019 by Elsevier Inc. All rights reserved. 94
Peptic Ulcer: Gastric and Duodenal Ulcers (Cont. ) Damage to mucosal barrier predisposes to development of ulcers and is associated with: Ø Inadequate blood supply • Caused by vasoconstriction (e. g. , by stress, smoking, shock, circulatory impairment in older adults, scar tissue, anemia) • Interferes with rapid regeneration of epithelium Excessive glucocorticoid secretion or medication Ø Ulcerogenic substances break down mucous layer. • Aspirin, NSAIDs, alcohol Ø Atrophy of gastric mucosa • Chronic gastritis Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 95
Peptic Ulcer: Gastric and Duodenal Ulcers (Cont. ) Increased acid pepsin secretions Increased gastrin secretion Ø Increased vagal stimulation Ø Increased sensitivity to vagal stimuli Ø Increased number of acid pepsin secretory cells in the stomach (genetic anomaly) Ø Increased stimulation of acid pepsin secretion • Alcohol, caffeine, certain foods Ø Interference with normal feedback mechanisms Ø Rapid gastric emptying Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 96
Peptic Ulcer: Gastric and Duodenal Ulcers (Cont. ) Complications of peptic ulcer Hemorrhage • Caused by erosion of blood vessels • Common complication • May be the first sign of a peptic ulcer Ø Perforation • Ulcer erodes completely through the wall. • Chyme can enter the peritoneal cavity. • Results in chemical peritonitis Ø Obstruction • May result later because of the formation of scar tissue Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 97
Peptic Ulcer: Gastric and Duodenal Ulcers (Cont. ) Signs and symptoms Ø Epigastric burning or localized pain, usually following stomach emptying Diagnostic tests Fiberoptic endoscopy Ø Barium x-ray Ø Endoscopic biopsy Ø Treatment Combination of antimicrobial and proton pump inhibitor to eliminate H. pylori Ø Reduction of exacerbating factors Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 98
Stress Ulcers Associated with severe trauma or systemic problems Burns, head injury Ø Hemorrhage or sepsis Ø Rapid onset Multiple ulcers (usually gastric) may form within hours of precipitating event. Ø First indicator—hemorrhage and severe pain Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 99
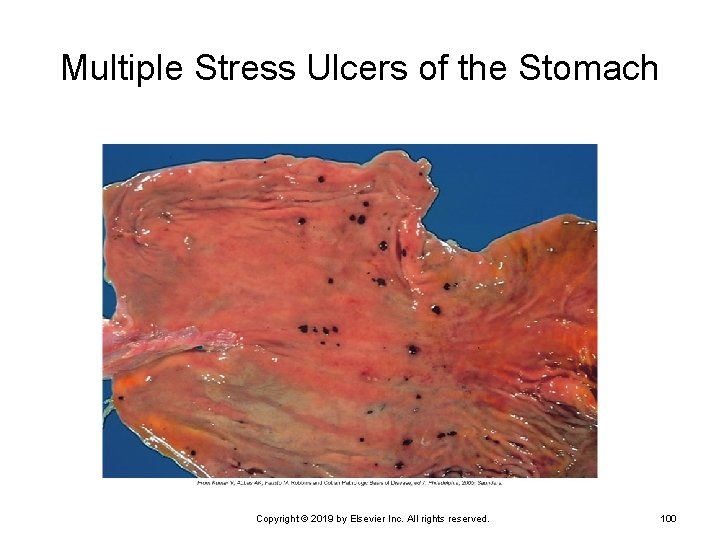
Multiple Stress Ulcers of the Stomach Copyright © 2019 by Elsevier Inc. All rights reserved. 100
Gastric Cancer Arises primarily in mucous glands Mostly in the antrum or pyloric area Early carcinoma Ø Confined to mucosa and submucosa Later stages Involves muscularis Ø Eventually invades serosa and spreads to lymph nodes Ø Asymptomatic in the early stages Ø Often, prognosis is poor on diagnosis. Copyright © 2019 by Elsevier Inc. All rights reserved. 101
Gastric Cancer (Cont. ) Diet seems to be a key factor, particularly smoked foods, nitrites, and nitrates. Genetic influences also play a role. Symptoms vague until cancer is advanced. Reason for late diagnosis Ø Surgery together with chemotherapy and radiation may relieve symptoms. Ø Survival rate less than 20% Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 102
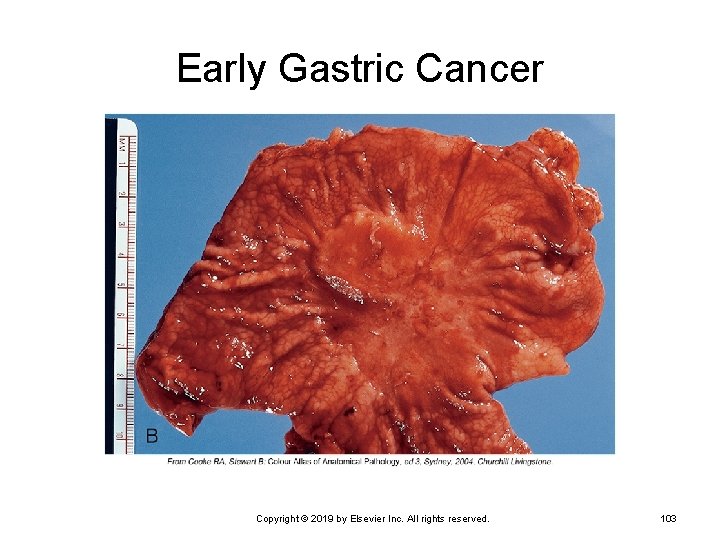
Early Gastric Cancer Copyright © 2019 by Elsevier Inc. All rights reserved. 103
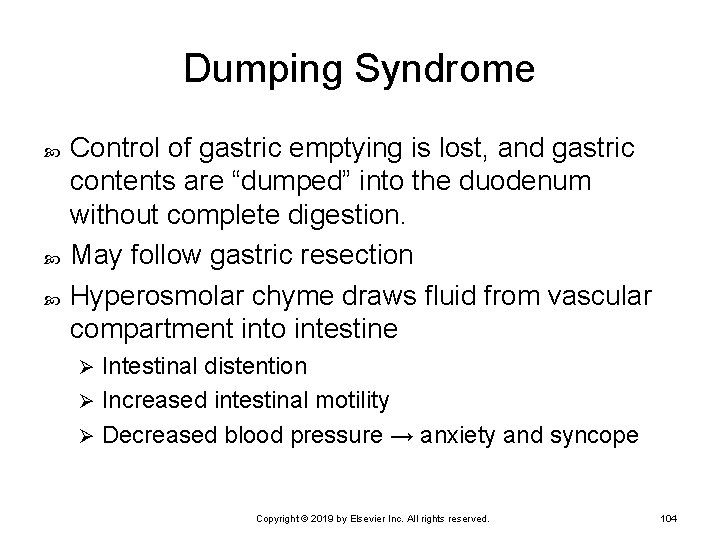
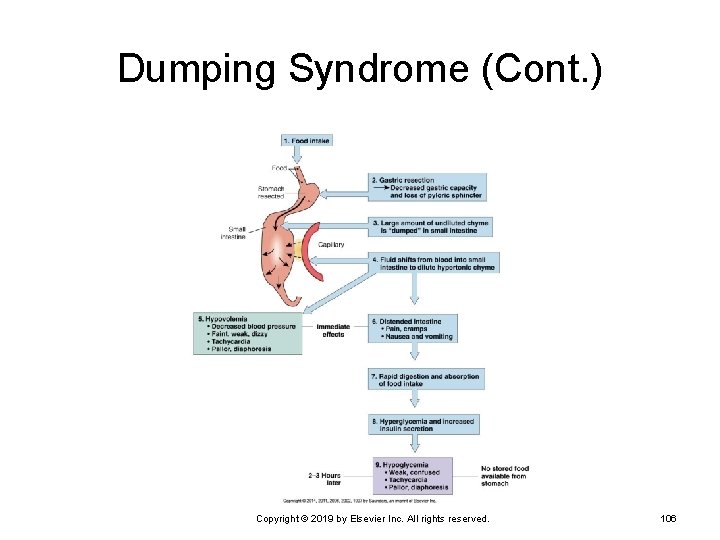
Dumping Syndrome Control of gastric emptying is lost, and gastric contents are “dumped” into the duodenum without complete digestion. May follow gastric resection Hyperosmolar chyme draws fluid from vascular compartment into intestine Intestinal distention Ø Increased intestinal motility Ø Decreased blood pressure → anxiety and syncope Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 104
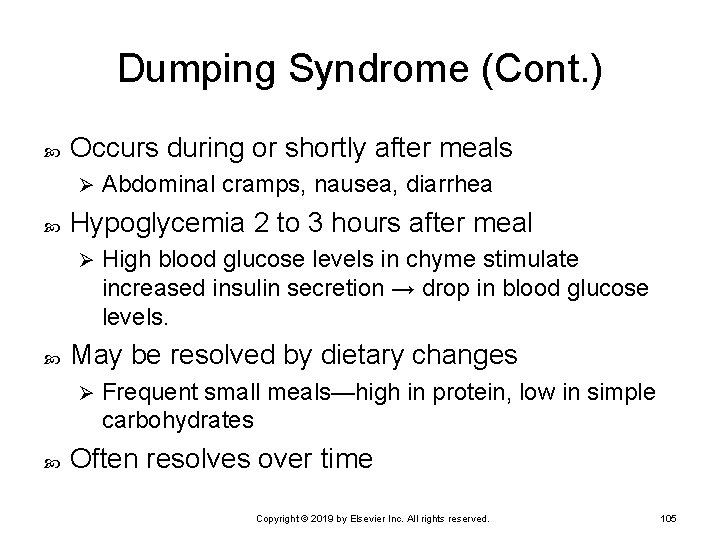
Dumping Syndrome (Cont. ) Occurs during or shortly after meals Ø Hypoglycemia 2 to 3 hours after meal Ø High blood glucose levels in chyme stimulate increased insulin secretion → drop in blood glucose levels. May be resolved by dietary changes Ø Abdominal cramps, nausea, diarrhea Frequent small meals—high in protein, low in simple carbohydrates Often resolves over time Copyright © 2019 by Elsevier Inc. All rights reserved. 105
Dumping Syndrome (Cont. ) Copyright © 2019 by Elsevier Inc. All rights reserved. 106
Pyloric Stenosis Narrowing and obstruction of pyloric sphincter May be developmental anomaly Signs appear within several weeks after birth. Projectile vomiting immediately after feeding Ø Firm mass can be palpated at pylorus. Ø Infant fails to gain weight, dehydration, persistent hunger Ø Surgery required to remove obstruction. May be acquired later in life Persistent feeling of fullness Ø Increased incidence of vomiting Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 107
Disorders of the Liver and Pancreas Copyright © 2019 by Elsevier Inc. All rights reserved. 108
Gallbladder Disorders Cholelithiasis Formation of gallstones Ø Solid material (calculi) that form in bile Ø Cholecystitis Ø Cholangitis Ø Inflammation of gallbladder and cystic duct Inflammation usually related to infection of bile ducts Choledocholithiasis Ø Obstruction of the biliary tract by gallstones Copyright © 2019 by Elsevier Inc. All rights reserved. 109
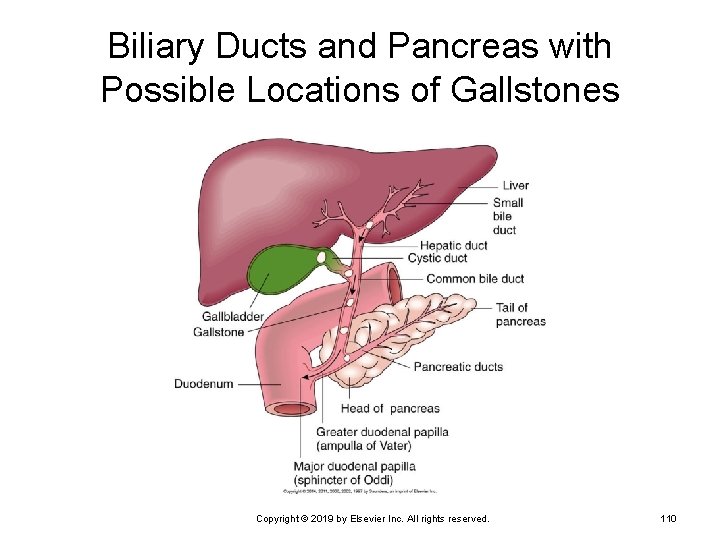
Biliary Ducts and Pancreas with Possible Locations of Gallstones Copyright © 2019 by Elsevier Inc. All rights reserved. 110
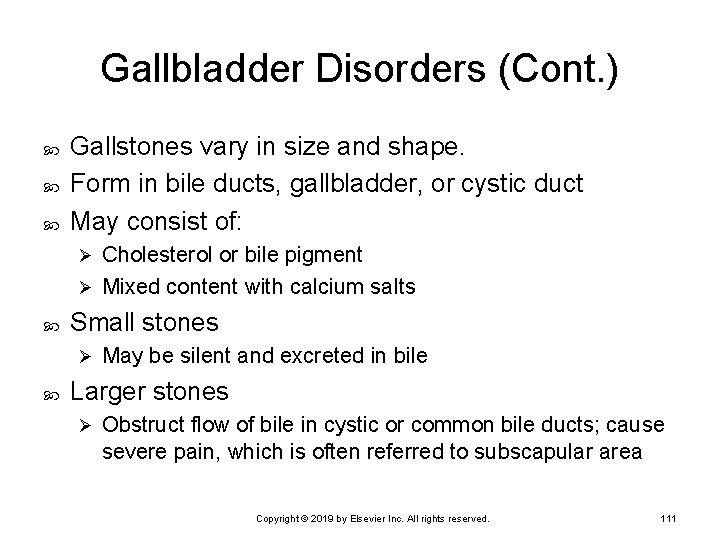
Gallbladder Disorders (Cont. ) Gallstones vary in size and shape. Form in bile ducts, gallbladder, or cystic duct May consist of: Cholesterol or bile pigment Ø Mixed content with calcium salts Ø Small stones Ø May be silent and excreted in bile Larger stones Ø Obstruct flow of bile in cystic or common bile ducts; cause severe pain, which is often referred to subscapular area Copyright © 2019 by Elsevier Inc. All rights reserved. 111
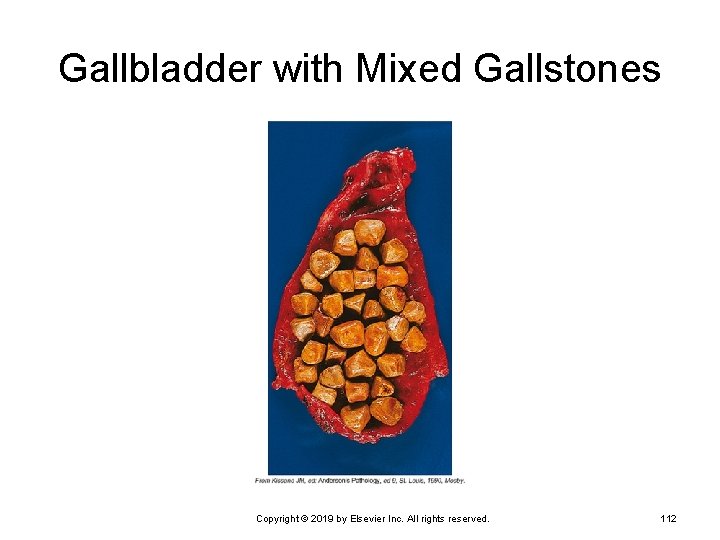
Gallbladder with Mixed Gallstones Copyright © 2019 by Elsevier Inc. All rights reserved. 112
Gallbladder Disorders (Cont. ) Risk factors for gallstones Women twice as likely to develop stones Ø High cholesterol in bile Ø High cholesterol intake Ø Obesity Ø Multiparity Ø Use of oral contraceptives or estrogen supplements Ø Hemolytic anemia Ø Alcoholic cirrhosis Ø Biliary tract infection Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 113
Gallbladder Disorders (Cont. ) Obstruction of a duct by a large calculi Sudden severe waves of pain • Radiating pain Ø Nausea and vomiting usually present Ø Pain continues, and jaundice develops. • Bile backs up into the liver and blood. • Risk of ruptured gallbladder if obstruction persists • Pain decreases if stone moves into duodenum. Ø Surgical intervention may be necessary. • May be removed using laparoscopic surgery • Low-fat diet necessary following surgery Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 114
Jaundice Prehepatic jaundice Ø Intrahepatic jaundice Ø Result of excessive destruction of red blood cells • Characteristic of hemolytic anemias or transfusion reactions Occurs with disease or damage to hepatocytes • Hepatitis or cirrhosis Posthepatic jaundice Ø Caused by obstruction of bile flow into gallbladder or duodenum • Tumor, cholelithiasis Copyright © 2019 by Elsevier Inc. All rights reserved. 115
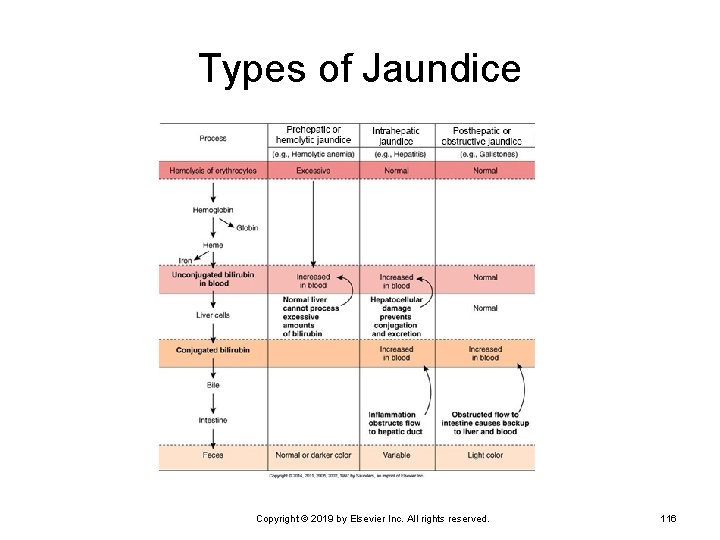
Types of Jaundice Copyright © 2019 by Elsevier Inc. All rights reserved. 116
Bilirubin Measurement in Jaundice Direct or conjugated bilirubin can be measured in the blood. Total bilirubin is measured in blood. Total bilirubin minus direct bilirubin = indirect or unconjugated bilirubin. Copyright © 2019 by Elsevier Inc. All rights reserved. 117
Jaundice Type of jaundice indicated by increase in serum bilirubin level and changes in stools Prehepatic jaundice Ø Intrahepatic jaundice Ø Unconjugated bilirubin level elevated Both unconjugated and conjugated bilirubin levels may be elevated. Posthepatic jaundice Increased conjugated bilirubin level Ø Light-colored stool caused by absence of bile Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 118
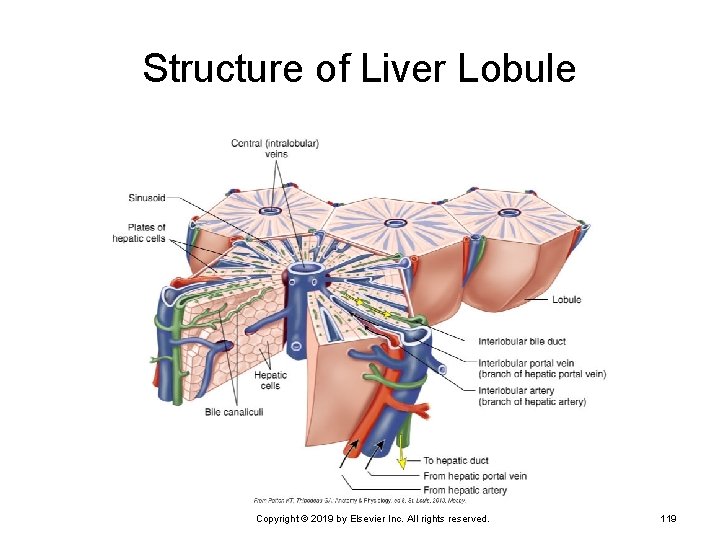
Structure of Liver Lobule Copyright © 2019 by Elsevier Inc. All rights reserved. 119
Hepatitis Inflammation of the liver Alcoholic Ø Idiopathic Ø Local infection Infection elsewhere in body Ø Fatty liver Viral hepatitis Ø Fatty liver Examples—infectious mononucleosis or amebiasis Chemical or drug toxicity Copyright © 2019 by Elsevier Inc. All rights reserved. 120
Viral Hepatitis Cell injury results in inflammation and necrosis in the liver. Ø Degrees of inflammation and damage vary. Liver is edematous and tender. Causative viruses Hepatitis A virus (HAV) Ø Hepatitis B virus (HBV) Ø Hepatitis C virus (HCV) Ø Hepatitis D virus (HDV) Ø Hepatitis E virus (HEV) Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 121
Viral Hepatitis (Cont. ) Hepatitis A (HAV) Ø Ø Ø Ø Small RNA virus Infectious hepatitis Transmitted by fecal-oral route in areas of inadequate sanitation or hygiene • Often from contaminated water or shellfish Sexual transmission has occurred during anal intercourse. Acute but self-limiting infection No carrier or chronic state Fecal shedding of virus before onset of signs Vaccine available for travelers, food care workers, and health care workers Copyright © 2019 by Elsevier Inc. All rights reserved. 122
Viral Hepatitis (Cont. ) Hepatitis B (HBV) Partially double-stranded DNA virus Ø Over 50% of HIV-positive patients are positive for HBV. Ø 50% of patients are asymptomatic but contagious because of carrier state. Ø Chronic inflammation can occur. Ø Transmission primarily by infected blood Ø Sexual transmission has been noted. Ø Tattooing and body piercing may transmit the virus. Ø Vaccine available, routinely given to children Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 123
Viral Hepatitis (Cont. ) Hepatitis C (HCV) Single-stranded RNA virus Ø Most common type transmitted by blood transfusion Ø May exist in a carrier state Ø About 50% of patients enter the chronic state. Ø Increases risk of hepatocellular carcinoma Ø Treated with interferon injections Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 124
Viral Hepatitis (Cont. ) Hepatitis D (HDV) Also called delta virus Ø Incomplete RNA virus • Requires HBV to replicate and produce active infection Ø HDV infection increases severity of HBV infection. Ø Transmitted by blood Ø Hepatitis E (HEV) Single-stranded RNA virus Ø Transmitted by oral-fecal route Ø No chronic or carrier state Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 125
Signs and Symptoms Preicteric stage Fatigue and malaise Ø Anorexia and nausea Ø General muscle aching Ø Icteric stage Onset of jaundice Ø Stools light in color, urine becomes darker Ø Liver tender and enlarged, mild aching pain Ø Posticteric stage—recovery stage Reductions in signs Ø Weakness persists for weeks Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 126
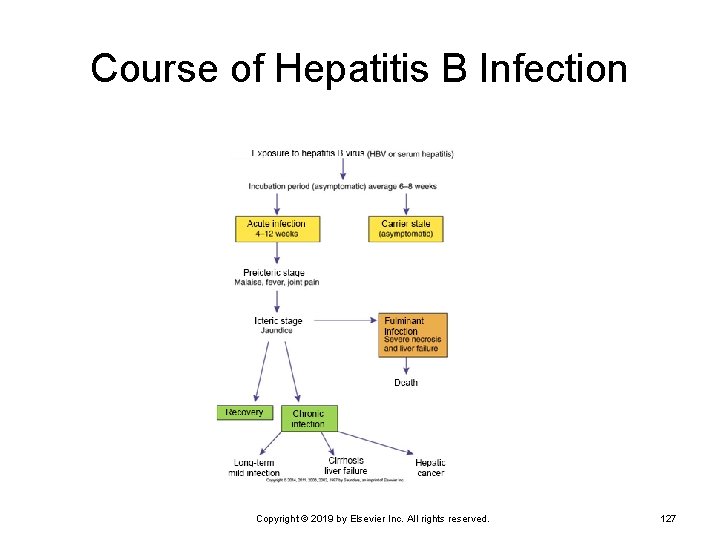
Course of Hepatitis B Infection Copyright © 2019 by Elsevier Inc. All rights reserved. 127
Viral Hepatitis (Cont. ) Only body defense is formation of antibodies via vaccination. Supportive measures Ø Rest, diet high in protein, carbohydrate, and vitamins Chronic hepatitis can be treated with interferon. Decreases viral replication Ø Effective in only 30% to 40% of individuals Ø Drug combination (slow-acting interferon plus antiviral drug) more effective Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 128
Toxic or Nonviral Hepatitis Variety of hepatotoxins can cause inflammation and necrosis of the liver. Drugs include: • Acetaminophen, halothane, phenothiazines, tetracycline Ø Chemicals include: • Carbon tetrachloride (not used currently), toluene, ethanol Ø Direct effect of toxins May result from sudden exposure to large amounts or from lower dose and long-term exposure Copyright © 2019 by Elsevier Inc. All rights reserved. 129
Cirrhosis Progressive destruction of the liver Causes Alcoholic liver disease Ø Biliary cirrhosis • Associated with immune disorders Ø Postnecrotic cirrhosis • Linked with chronic hepatitis or long-term exposure to toxic Ø materials Ø Metabolic • Usually caused by genetic metabolic storage disorders Copyright © 2019 by Elsevier Inc. All rights reserved. 130
Cirrhosis (Cont. ) Extensive diffuse fibrosis Interferes with blood supply Ø Bile may back up. Ø Loss of lobular organization Degenerative changes may be asymptomatic until disease is well advanced. Liver biopsy and serologic test to determine cause and extent of damage Copyright © 2019 by Elsevier Inc. All rights reserved. 131
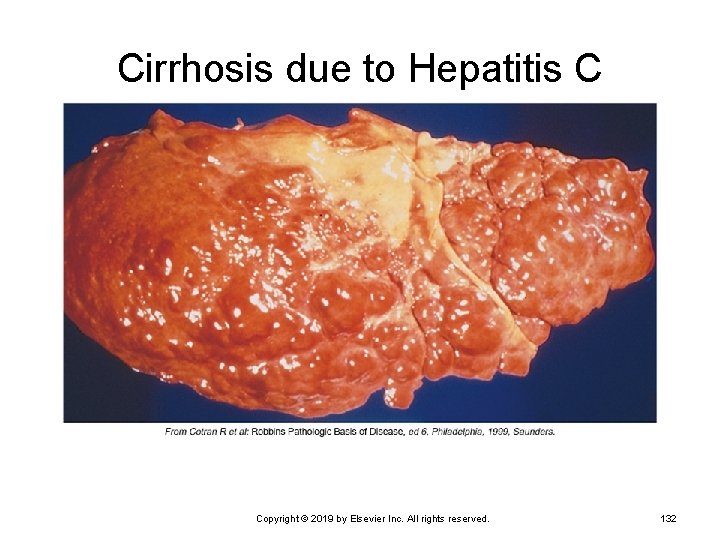
Cirrhosis due to Hepatitis C Copyright © 2019 by Elsevier Inc. All rights reserved. 132
Cirrhosis: Alcoholic Liver Disease Initial stage—fatty liver Enlargement of the liver Ø Asymptomatic and reversible with reduced alcohol intake Ø Second stage—alcoholic hepatitis Inflammation and cell necrosis Ø Fibrous tissue formation—irreversible change Ø Third stage—end-stage cirrhosis Fibrotic tissue replaces normal tissue. Ø Little normal function remains. Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 133
Functional Losses with Cirrhosis Decreased removal and conjugation of bilirubin Decreased production of bile Impaired digestion and absorption of nutrients Decreased production of blood-clotting factors Impaired glucose and glycogen metabolism Impaired conversion of ammonia to urea Copyright © 2019 by Elsevier Inc. All rights reserved. 134
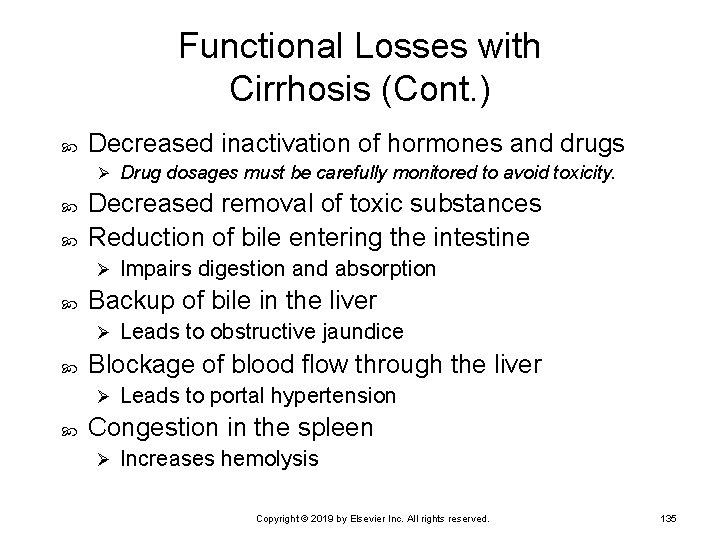
Functional Losses with Cirrhosis (Cont. ) Decreased inactivation of hormones and drugs Ø Decreased removal of toxic substances Reduction of bile entering the intestine Ø Leads to obstructive jaundice Blockage of blood flow through the liver Ø Impairs digestion and absorption Backup of bile in the liver Ø Drug dosages must be carefully monitored to avoid toxicity. Leads to portal hypertension Congestion in the spleen Ø Increases hemolysis Copyright © 2019 by Elsevier Inc. All rights reserved. 135
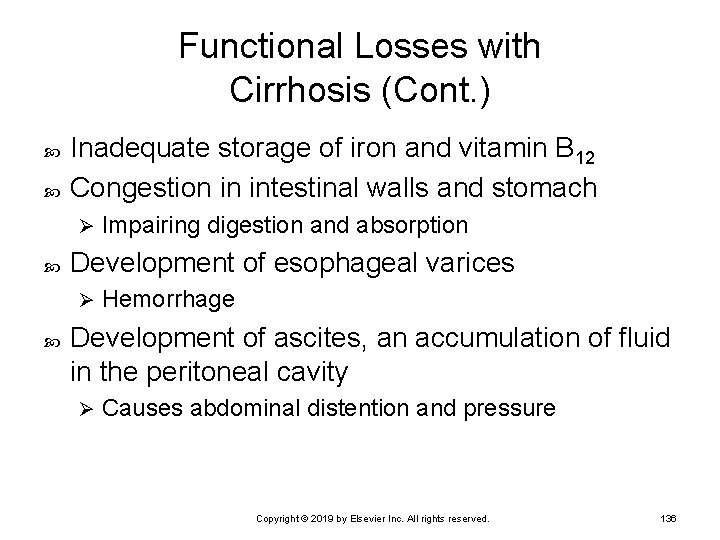
Functional Losses with Cirrhosis (Cont. ) Inadequate storage of iron and vitamin B 12 Congestion in intestinal walls and stomach Ø Development of esophageal varices Ø Impairing digestion and absorption Hemorrhage Development of ascites, an accumulation of fluid in the peritoneal cavity Ø Causes abdominal distention and pressure Copyright © 2019 by Elsevier Inc. All rights reserved. 136
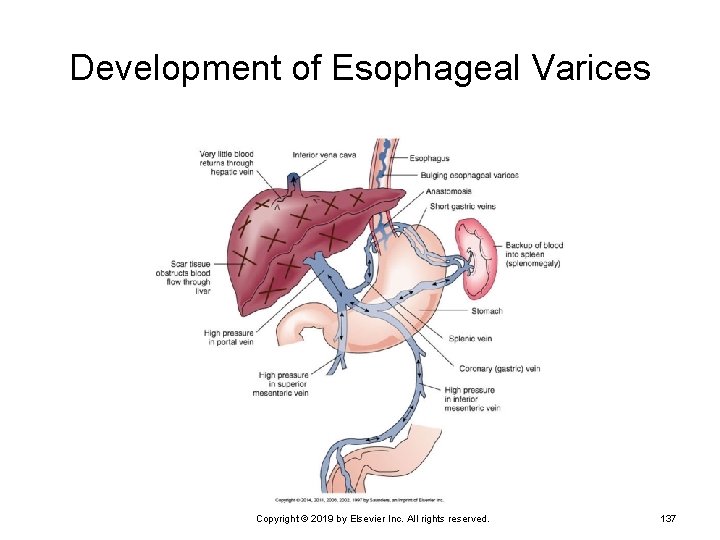
Development of Esophageal Varices Copyright © 2019 by Elsevier Inc. All rights reserved. 137
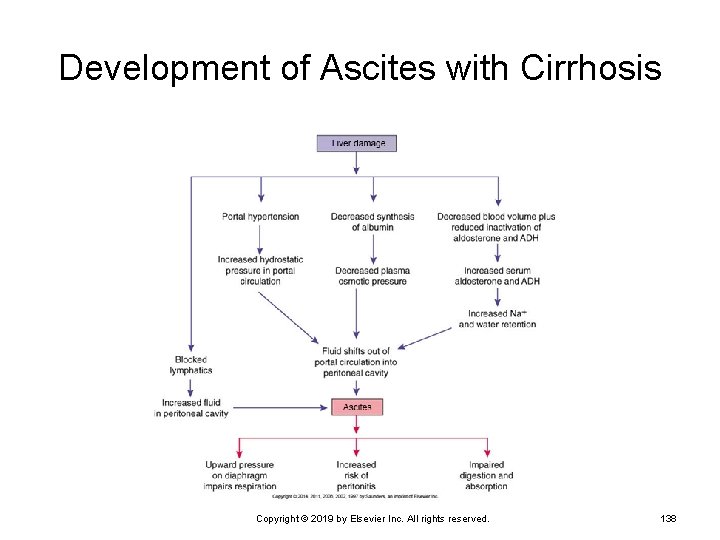
Development of Ascites with Cirrhosis Copyright © 2019 by Elsevier Inc. All rights reserved. 138
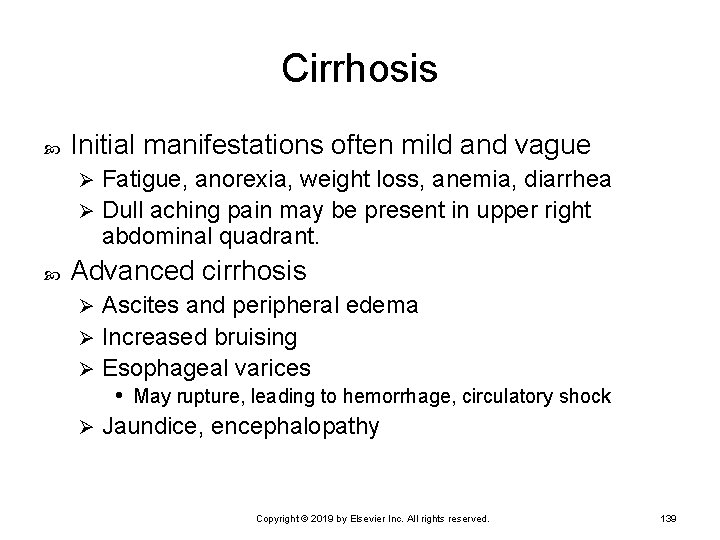
Cirrhosis Initial manifestations often mild and vague Fatigue, anorexia, weight loss, anemia, diarrhea Ø Dull aching pain may be present in upper right abdominal quadrant. Ø Advanced cirrhosis Ascites and peripheral edema Ø Increased bruising Ø Esophageal varices • May rupture, leading to hemorrhage, circulatory shock Ø Jaundice, encephalopathy Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 139
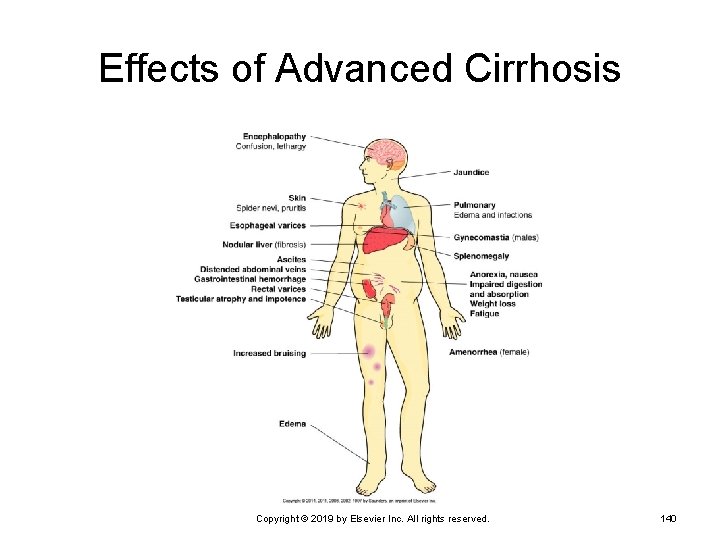
Effects of Advanced Cirrhosis Copyright © 2019 by Elsevier Inc. All rights reserved. 140
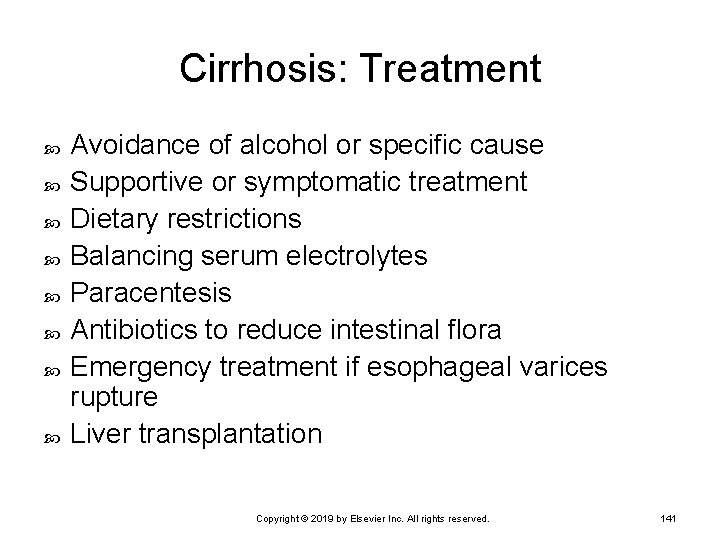
Cirrhosis: Treatment Avoidance of alcohol or specific cause Supportive or symptomatic treatment Dietary restrictions Balancing serum electrolytes Paracentesis Antibiotics to reduce intestinal flora Emergency treatment if esophageal varices rupture Liver transplantation Copyright © 2019 by Elsevier Inc. All rights reserved. 141
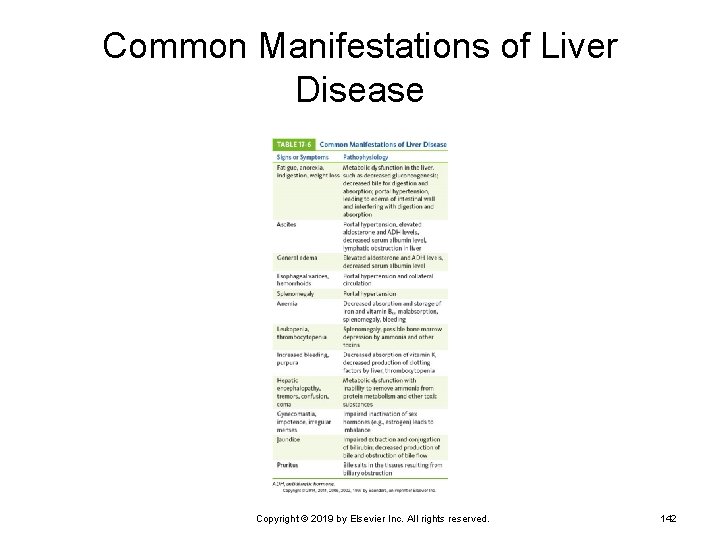
Common Manifestations of Liver Disease Copyright © 2019 by Elsevier Inc. All rights reserved. 142
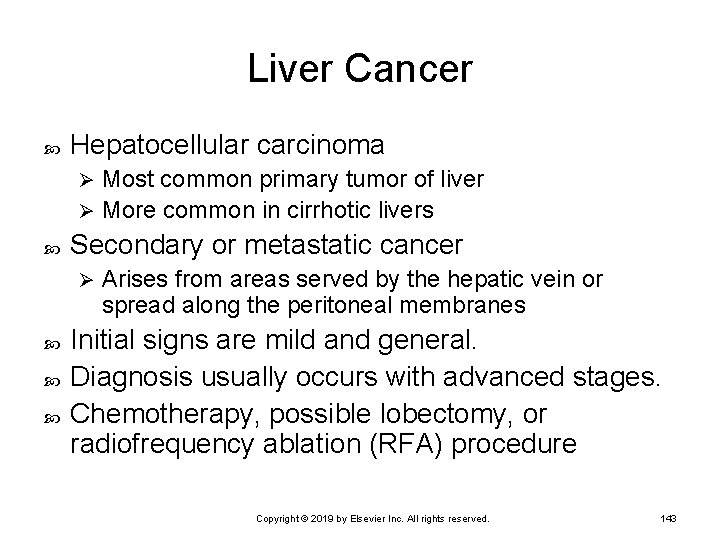
Liver Cancer Hepatocellular carcinoma Most common primary tumor of liver Ø More common in cirrhotic livers Ø Secondary or metastatic cancer Ø Arises from areas served by the hepatic vein or spread along the peritoneal membranes Initial signs are mild and general. Diagnosis usually occurs with advanced stages. Chemotherapy, possible lobectomy, or radiofrequency ablation (RFA) procedure Copyright © 2019 by Elsevier Inc. All rights reserved. 143
Acute Pancreatitis Inflammation of the pancreas Ø May be acute or chronic Ø Results in autodigestion of the tissue Acute form considered a medical emergency Pancreas lacks a fibrous capsule. Destruction may progress into tissue surrounding the pancreas. Ø Substances released by necrotic tissue lead to widespread inflammation. • Hypovolemia and circulatory collapse may follow. Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 144
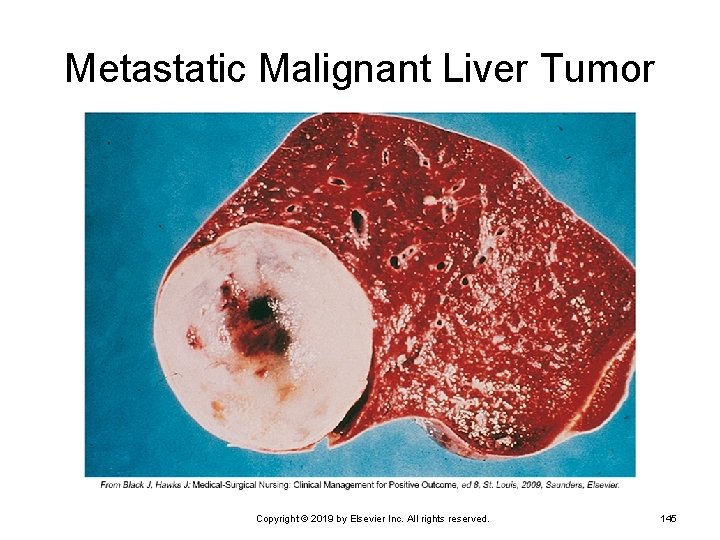
Metastatic Malignant Liver Tumor Copyright © 2019 by Elsevier Inc. All rights reserved. 145
Acute Pancreatitis (Cont. ) Chemical peritonitis results in bacterial peritonitis. Septicemia may result. Ø Adult respiratory distress syndrome and acute renal failure are possible complications. Ø Causes Gallstones Ø Alcohol abuse Ø Sudden onset may follow intake of large meal or large amount of alcohol. Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 146
Signs and Symptoms Severe epigastric or abdominal pain radiating to the back—primary symptoms Signs of shock Ø Low-grade fever until infection develops Ø Caused by o hypovolemia Body temperature may then rise significantly. Abdominal distention and decreased bowel sounds Ø Decreased peristalsis and paralytic ileus Copyright © 2019 by Elsevier Inc. All rights reserved. 147
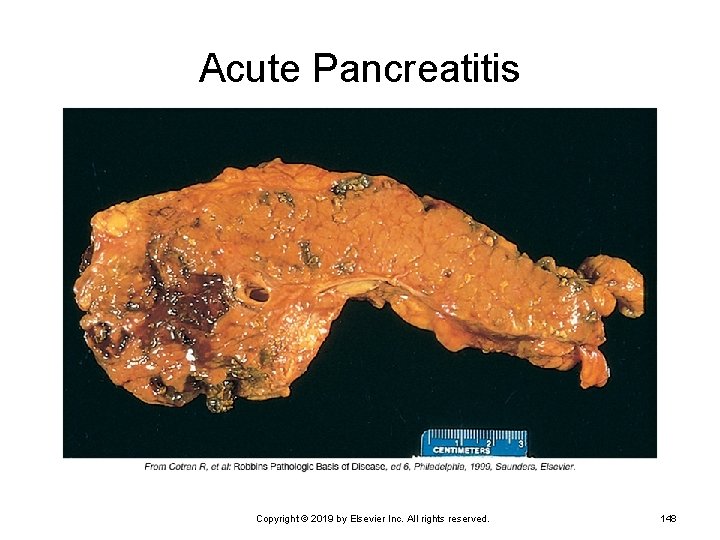
Acute Pancreatitis Copyright © 2019 by Elsevier Inc. All rights reserved. 148
Acute Pancreatitis (Cont. ) Diagnostic tests Serum amylase levels—first rise, then fall after 48 hours Ø Serum lipid levels are elevated. Ø Hypocalcemia Ø Leukocytosis Ø Treatment Oral intake is stopped. Ø Treatment of shock and electrolyte imbalances Ø Analgesics for pain relief Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 149
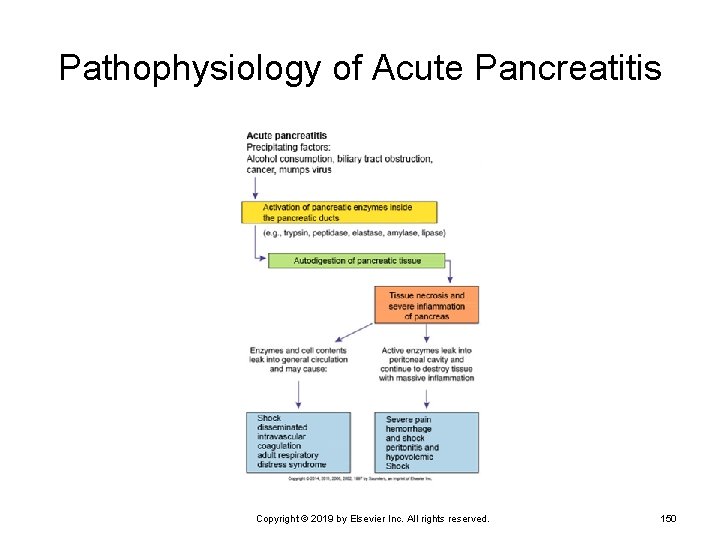
Pathophysiology of Acute Pancreatitis Copyright © 2019 by Elsevier Inc. All rights reserved. 150
Pancreatic Cancer Risk factors Smoking Ø Pancreatitis and dietary factors Ø Adenocarcinoma—most common form Ø Arises from the epithelial cells in the ducts Weight loss and jaundice are early manifestations. Frequently asymptomatic until well advanced Metastases occur early. Ø Mortality is close to 95%. Copyright © 2019 by Elsevier Inc. All rights reserved. 151
Lower Gastrointestinal Tract Disorders Celiac Disease Chronic Inflammatory Bowel Disease Irritable Bowel Syndrome Appendicitis Diverticular Disease Colorectal Cancer Intestinal Obstruction Peritonitis Copyright © 2019 by Elsevier Inc. All rights reserved. 152
Celiac Disease Malabsorption syndrome Primarily a childhood disorder Ø May occur in adults in middle age Appears to have genetic link Defect in intestinal enzyme Prevents further digestion of gliadin (breakdown product of gluten) Ø Toxic effect on intestinal villi—atrophy of villi • Malabsorption and malnutrition result. Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 153
Celiac Disease (Cont. ) First signs appear when cereals are added. Ø At about 4 to 6 months of age Manifestation Steatorrhea, muscle wasting, failure to gain weight Ø Irritability and malaise common Ø Diagnosed by a series of blood tests Gluten-free diet for treatment Ø Intestinal mucosa returns to normal after a few weeks without gluten intake. Copyright © 2019 by Elsevier Inc. All rights reserved. 154
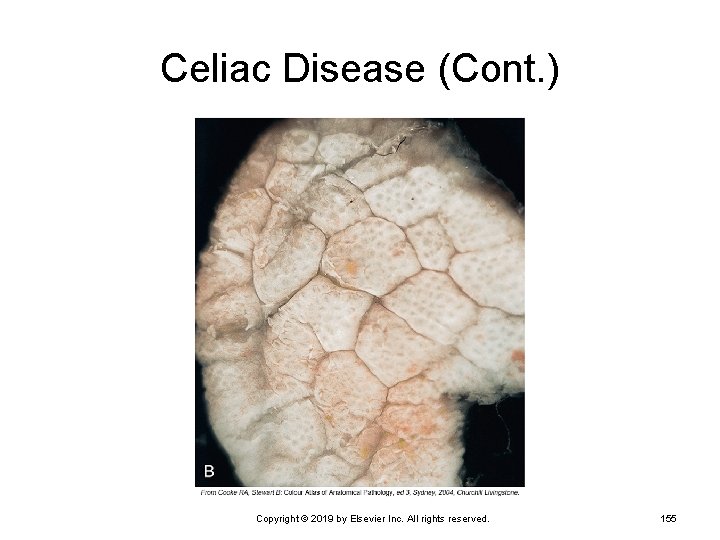
Celiac Disease (Cont. ) Copyright © 2019 by Elsevier Inc. All rights reserved. 155
Chronic Inflammatory Bowel Disease Crohn disease and ulcerative colitis are chronic inflammatory bowel diseases (IBDs). Causes unknown Genetic factor appears to be involved. Crohn disease—often during adolescence Ulcerative colitis—second or third decade Many similarities between Crohn disease and ulcerative colitis Copyright © 2019 by Elsevier Inc. All rights reserved. 156
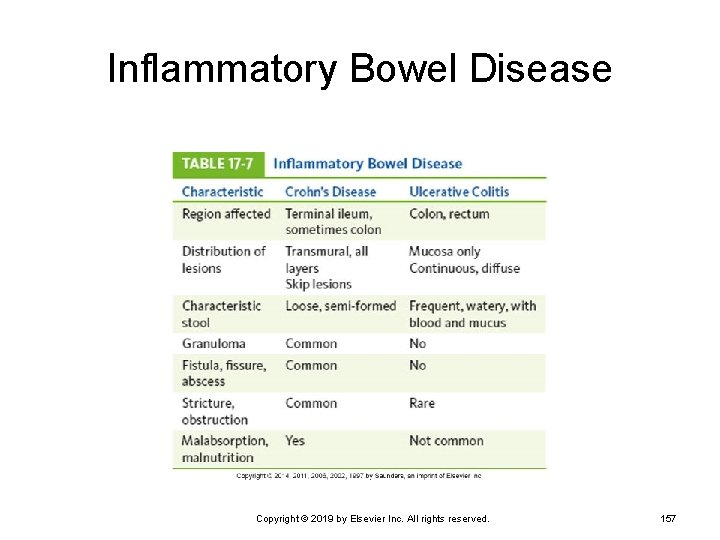
Inflammatory Bowel Disease Copyright © 2019 by Elsevier Inc. All rights reserved. 157
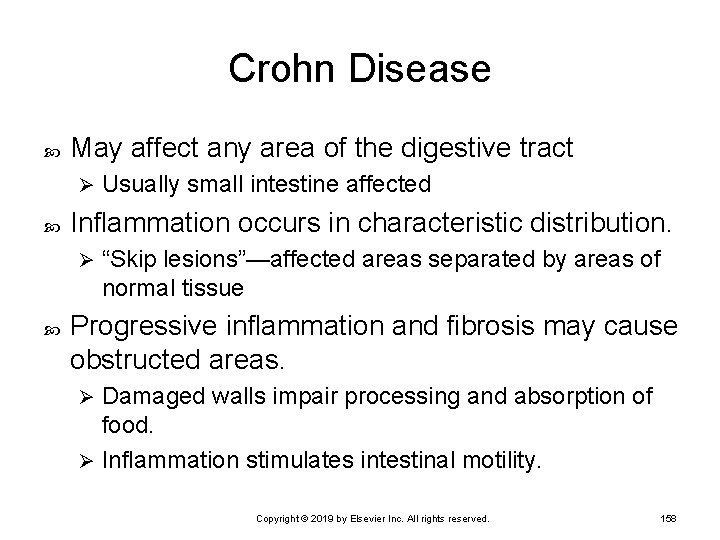
Crohn Disease May affect any area of the digestive tract Ø Inflammation occurs in characteristic distribution. Ø Usually small intestine affected “Skip lesions”—affected areas separated by areas of normal tissue Progressive inflammation and fibrosis may cause obstructed areas. Damaged walls impair processing and absorption of food. Ø Inflammation stimulates intestinal motility. Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 158
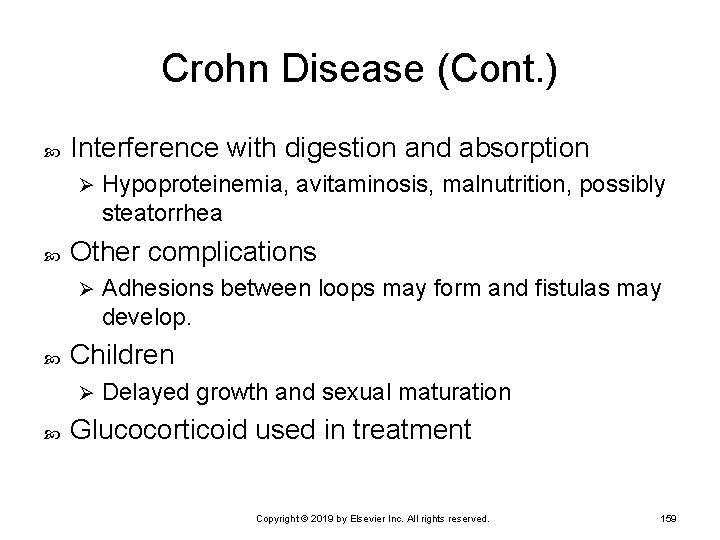
Crohn Disease (Cont. ) Interference with digestion and absorption Ø Other complications Ø Adhesions between loops may form and fistulas may develop. Children Ø Hypoproteinemia, avitaminosis, malnutrition, possibly steatorrhea Delayed growth and sexual maturation Glucocorticoid used in treatment Copyright © 2019 by Elsevier Inc. All rights reserved. 159
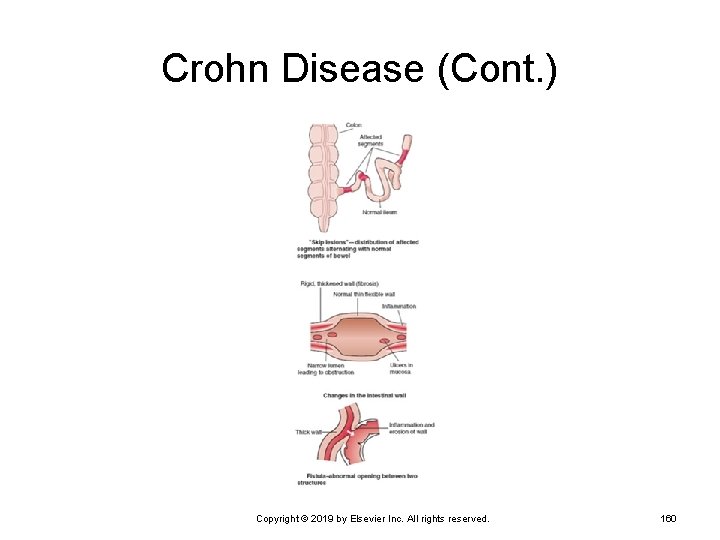
Crohn Disease (Cont. ) Copyright © 2019 by Elsevier Inc. All rights reserved. 160
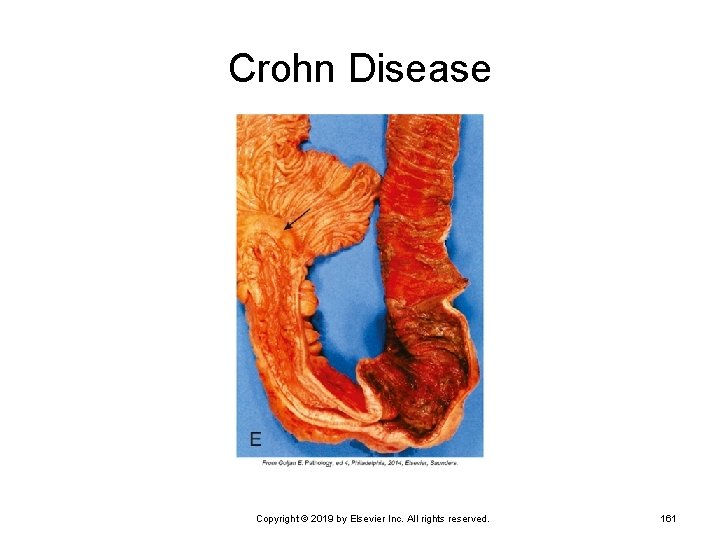
Crohn Disease Copyright © 2019 by Elsevier Inc. All rights reserved. 161
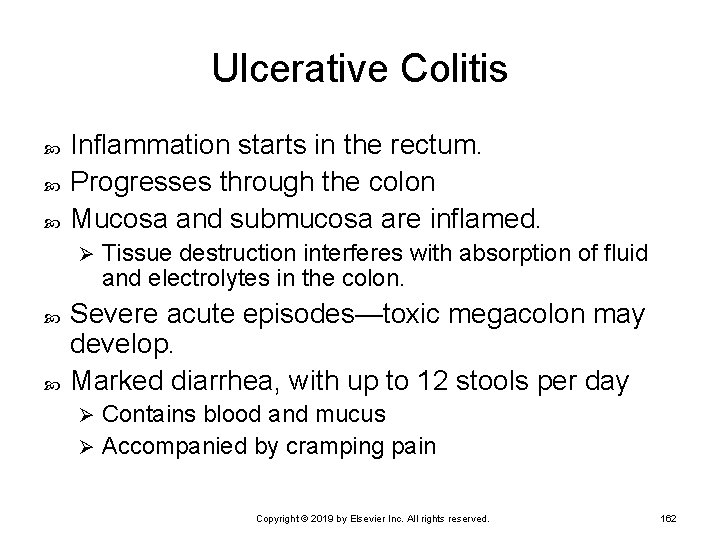
Ulcerative Colitis Inflammation starts in the rectum. Progresses through the colon Mucosa and submucosa are inflamed. Ø Tissue destruction interferes with absorption of fluid and electrolytes in the colon. Severe acute episodes—toxic megacolon may develop. Marked diarrhea, with up to 12 stools per day Contains blood and mucus Ø Accompanied by cramping pain Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 162
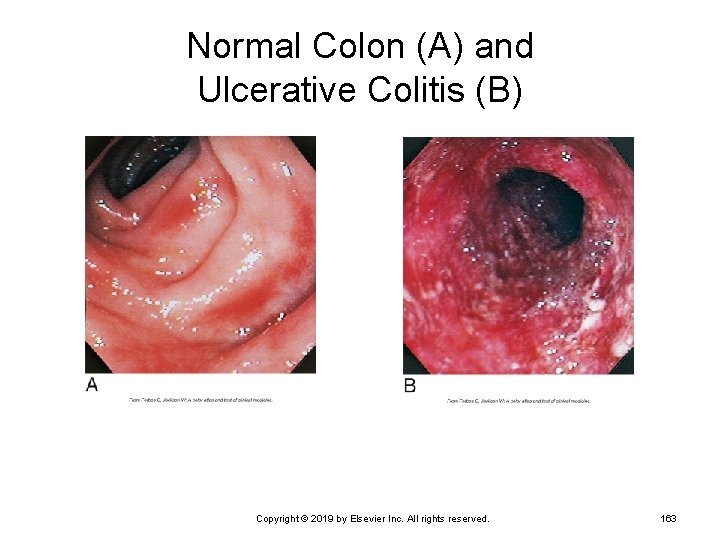
Normal Colon (A) and Ulcerative Colitis (B) Copyright © 2019 by Elsevier Inc. All rights reserved. 163
Irritable Bowel Syndrome Types Abnormal gastrointestinal mobility and secretion Ø Visceral hypersensitivity Ø Postinfectious IBS Ø Overgrowth of flora Ø Food allergy or intolerance Ø Psychosocial factors Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 164
Manifestations and Diagnosis Manifestations Lower abdominal pain Ø Diarrhea Ø Constipation, alternating with diarrhea Ø Bloating, nausea Ø Diagnosis Based on signs and symptoms Ø Testing for food allergies Ø Testing for bacterial or parasitic infections Ø No single cure for IBS Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 165
Treatment of IBS Team approach Antiinflammatory medications Sulfasalazine Ø Glucocorticoids Ø Antimotility agents Nutritional supplements Antimicrobials Immunotherapeutic agents Surgical resection Ø Usually ileostomy or colostomy Copyright © 2019 by Elsevier Inc. All rights reserved. 166
Appendicitis: Development Obstruction of the appendiceal lumen Ø Fluid builds up inside the appendix. Ø By a fecalith, gallstone, or foreign material Microorganisms proliferate. Appendiceal wall becomes inflamed. Purulent exudate forms. Ø Appendix is swollen. Ø Ischemia and necrosis of the wall Ø Results in increased permeability Copyright © 2019 by Elsevier Inc. All rights reserved. 167
Appendicitis: Development (Cont. ) Bacteria and toxins escape into surroundings. Ø Abscess may develop when inflamed area is walled off. Ø Leads to abscess formation or localized bacterial peritonitis Inflammation and pain may temporarily subside. Localized infection or peritonitis develops around the appendix. Ø May spread along the peritoneal membranes Copyright © 2019 by Elsevier Inc. All rights reserved. 168
Appendicitis: Development (Cont. ) Increased necrosis and gangrene in the wall Ø Caused by increasing pressure in the appendix Appendix ruptures or perforates Release of contents into peritoneal cavity Ø Generalized peritonitis • May be life-threatening Ø Treatment Ø Surgical removal of appendix and antimicrobial drugs Copyright © 2019 by Elsevier Inc. All rights reserved. 169
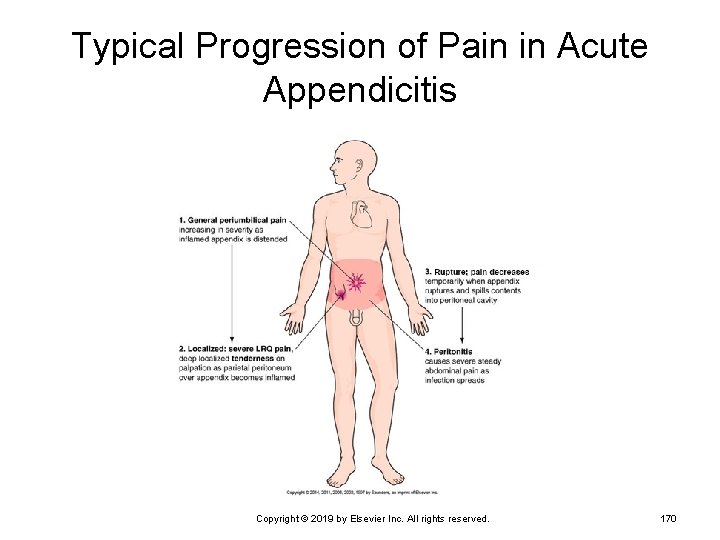
Typical Progression of Pain in Acute Appendicitis Copyright © 2019 by Elsevier Inc. All rights reserved. 170
Appendicitis: Signs and Symptoms General periumbilical pain Ø Related to the inflammation Nausea and vomiting common Pain becomes severe and localized in lower right quadrant (LRQ). LRQ rebound tenderness develops. Ø Involvement of parietal peritoneum over appendix Copyright © 2019 by Elsevier Inc. All rights reserved. 171
Appendicitis: Signs and Symptoms (Cont. ) After rupture Ø Pain recurs—severe, generalized abdominal pain and guarding Low-grade fever and leukocytosis Ø Pain subsides temporarily. Development of inflammation Boardlike abdomen, tachycardia, hypotension As peritonitis develops, abdominal wall muscles spasm. Ø Toxins lead to reduced blood pressure. Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 172
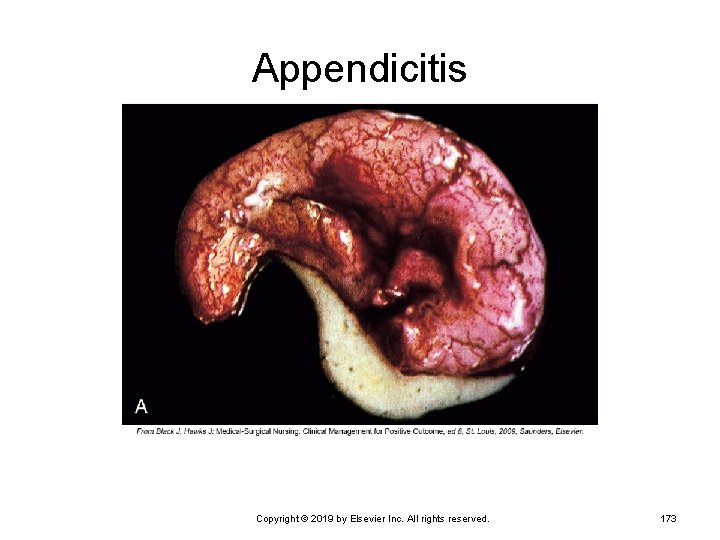
Appendicitis Copyright © 2019 by Elsevier Inc. All rights reserved. 173
Diverticular Disease Development of diverticula Diverticulum Ø Diverticulosis Ø Outpouching (herniation) of the mucosa through the muscular layer of the colon Asymptomatic diverticular disease Diverticulitis Ø Inflammation of the diverticula Copyright © 2019 by Elsevier Inc. All rights reserved. 174
Diverticular Disease (Cont. ) Form at gaps between muscle layers Congenital weakness of wall may be a factor. Weaker areas bulge when pressure increases. Many cases are asymptomatic. Diverticulitis stasis of material in diverticula leads to inflammation and infection. Cramping, tenderness, nausea, vomiting Ø Slight fever and elevated white blood cell count Ø Treatment of diverticulitis Antimicrobial drugs Ø Dietary modifications to prevent stasis Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 175
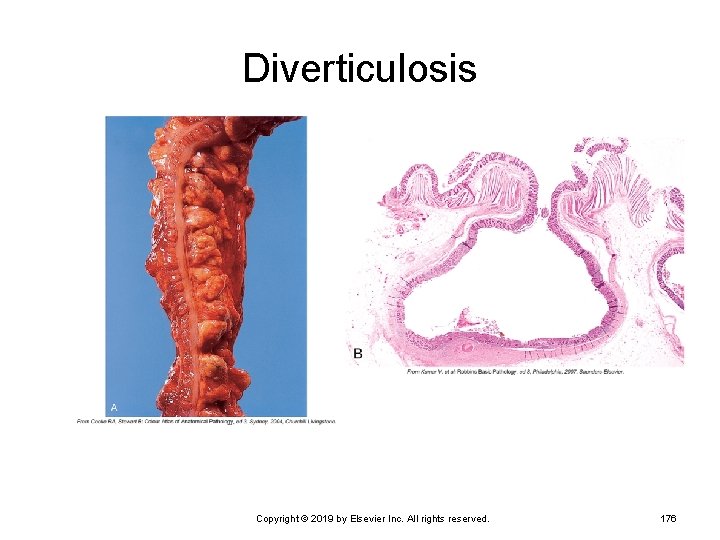
Diverticulosis Copyright © 2019 by Elsevier Inc. All rights reserved. 176
Colorectal Cancer Most malignancies develop from adenomatous polyps. Early diagnosis is essential. Cancer occurs primarily in persons older than 50 years. Risk factors Familial multiple polyposis Ø Long-term ulcerative colitis Ø Genetic factors Ø Environmental factors • Diet low in fiber Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 177
Colorectal Cancer (Cont. ) Initial signs depend largely on the location of the growth. General signs Change in bowel habits • Alternating diarrhea and constipation Ø Bleeding Ø Fatigue, weight loss, anemia Ø Treatment Ø Surgical removal with radiation and/or chemotherapy Copyright © 2019 by Elsevier Inc. All rights reserved. 178
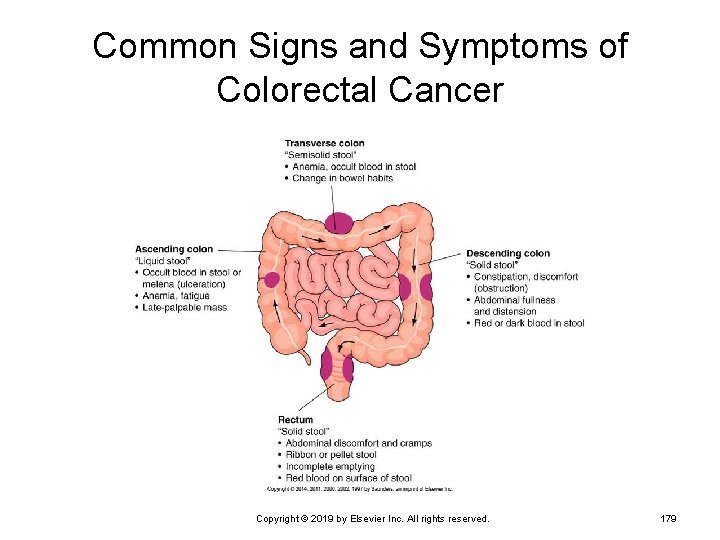
Common Signs and Symptoms of Colorectal Cancer Copyright © 2019 by Elsevier Inc. All rights reserved. 179
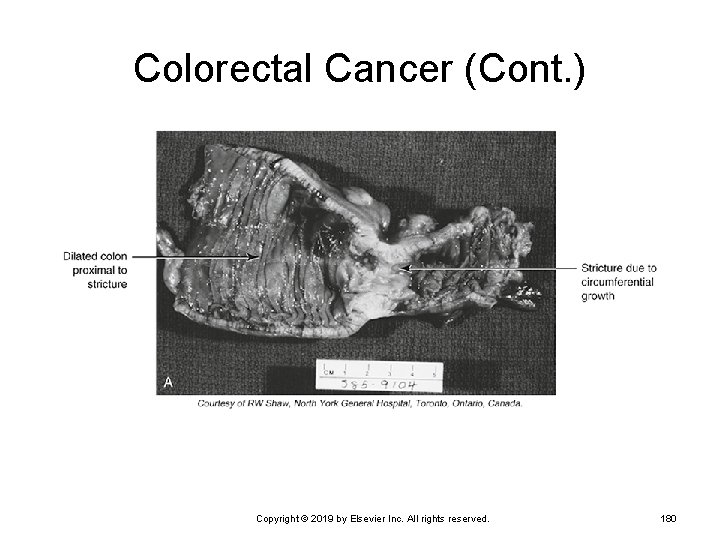
Colorectal Cancer (Cont. ) Copyright © 2019 by Elsevier Inc. All rights reserved. 180
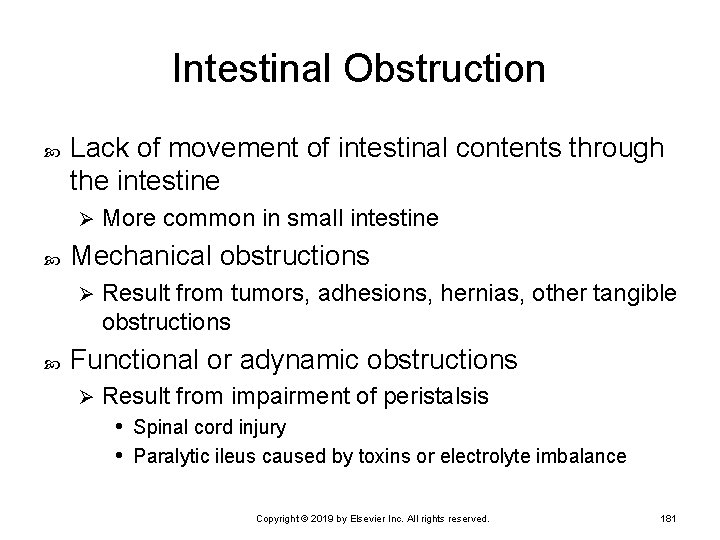
Intestinal Obstruction Lack of movement of intestinal contents through the intestine Ø Mechanical obstructions Ø More common in small intestine Result from tumors, adhesions, hernias, other tangible obstructions Functional or adynamic obstructions Ø Result from impairment of peristalsis • Spinal cord injury • Paralytic ileus caused by toxins or electrolyte imbalance Copyright © 2019 by Elsevier Inc. All rights reserved. 181
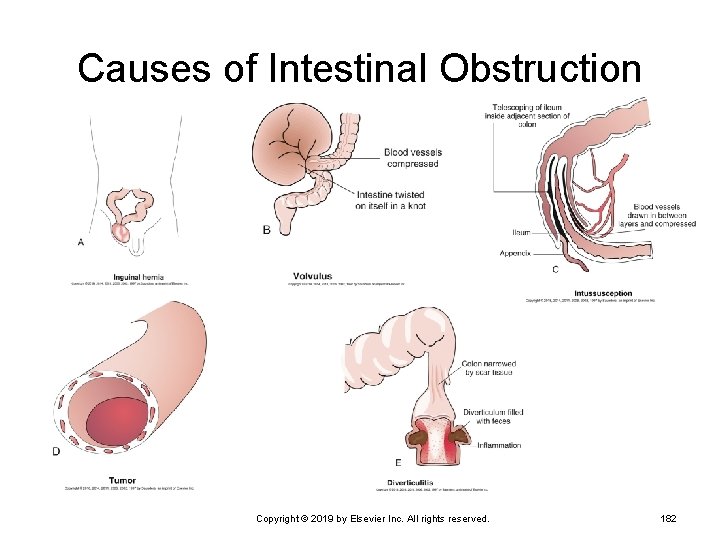
Causes of Intestinal Obstruction Copyright © 2019 by Elsevier Inc. All rights reserved. 182
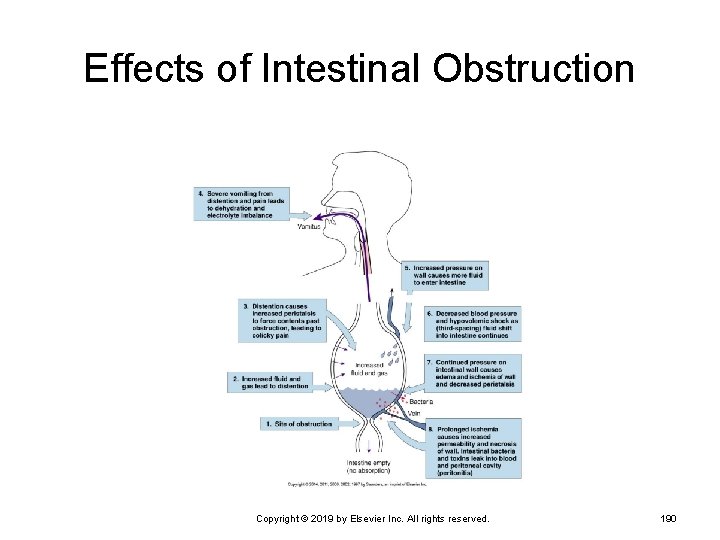
Intestinal Obstruction (Cont. ) Gases and fluids accumulate proximal to the blockage, distending the intestine. Increasingly strong contractions of proximal intestine Ø Effort to move contents along Pressure increases in lumen. More secretions enter the intestine. Ø Compression of veins in wall • Intestinal wall becomes edematous. • Prevention of absorption Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 183
Intestinal Obstruction (Cont. ) Intestinal distention leads to persistent vomiting. Additional loss of fluid and electrolytes Ø Hypovolemia can result. Ø Intestinal wall becomes ischemic and necrotic. Ø If obstruction is not removed, gangrene ensues. Ischemia and necrosis → decreased innervation and cessation of peristalsis Paralytic ileus occurs if it is not a cause to begin with. Copyright © 2019 by Elsevier Inc. All rights reserved. 184
Intestinal Obstruction (Cont. ) Obstruction promotes rapid reproduction of intestinal bacteria. Some produce endotoxins. Ø Affected wall becomes necrotic and more permeable. Ø Bacteria and toxins leak into peritoneal cavity (peritonitis) or into blood (bacteremia and septicemia). Ø Perforation of the necrotic segment may occur. Ø Generalized peritonitis and septic shock Copyright © 2019 by Elsevier Inc. All rights reserved. 185
Intestinal Obstruction (Cont. ) Functional obstructions or paralytic ileus from: Abdominal surgery (follows surgery) Ø Spinal shock following spinal cord injuries Ø Inflammation related to severe ischemia Ø Pancreatitis, peritonitis, infection in the abdominal cavity Ø Hypokalemia Ø Mesenteric thrombosis Ø Toxemia Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 186
Intestinal Obstruction (Cont. ) Mechanical obstruction from: Adhesions that twist or constrict intestine Ø Hernias Ø Strictures caused by scar tissue Ø Masses—tumors or foreign bodies Ø Intussusception Ø Volvulus Ø Hirschsprung disease Ø Gradual obstruction from chronic inflammatory conditions Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 187
Intestinal Obstruction (Cont. ) Mechanical obstruction of small intestine Severe colicky abdominal pain Ø Intermittent bowel sounds can be heard. Ø Paralytic ileus Pain is steady. Ø Bowel sounds decrease or are absent. Ø Vomiting and abdominal distention Occurs quickly with obstruction of small intestine Ø Vomiting is recurrent, eventually with bile-stained content. Ø Obstruction of the small intestine is a medical emergency! Copyright © 2019 by Elsevier Inc. All rights reserved. 188
Intestinal Obstruction (Cont. ) Obstruction of large intestine Develops slowly, with mild signs Ø Constipation Ø Mild abdominal pain, followed by abdominal distention Ø Anorexia, vomiting, more severe pain Ø Treatment of underlying cause Ø Fluid and electrolyte replacement Ø Surgery and antimicrobial therapy Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 189
Effects of Intestinal Obstruction Copyright © 2019 by Elsevier Inc. All rights reserved. 190
Peritonitis Inflammation of the peritoneal membranes Chemical peritonitis may result from: Enzymes released with pancreatitis Ø Urine leaking form a ruptured bladder Ø Chyme spilled from a perforated ulcer Ø Bile escaping from the ruptured gallbladder Ø Blood Ø Any other foreign material in the cavity Ø Copyright © 2019 by Elsevier Inc. All rights reserved. 191
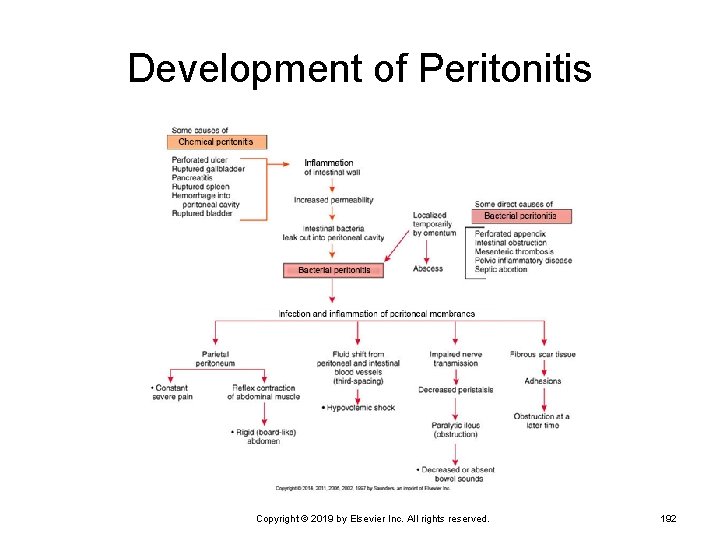
Development of Peritonitis Copyright © 2019 by Elsevier Inc. All rights reserved. 192
Peritonitis (Cont. ) Bacterial peritonitis caused by: Direct trauma affecting the intestine Ø Ruptured appendix Ø Intestinal obstruction and gangrene Ø Any abdominal surgery Ø If foreign material is left or infection develops Pelvic inflammatory disease in women Ø When infection reaches the cavity through fallopian tubes Copyright © 2019 by Elsevier Inc. All rights reserved. 193
Signs and Symptoms Signs and symptoms Sudden, severe, generalized abdominal pain Localized tenderness at site of underlying problem Vomiting common, abdominal distention Dehydration, hypovolemia, low blood pressure Decreased blood pressure, tachycardia, fever, leukocytosis Copyright © 2019 by Elsevier Inc. All rights reserved. 194
Treatment Depends on primary cause Surgery might be required Massive antimicrobial drugs—specific to causative organism Copyright © 2019 by Elsevier Inc. All rights reserved. 195
- Slides: 195