CHAPTER 16 First Aid 16 1 Providing First














- Slides: 160
CHAPTER 16 First Aid
16: 1 Providing First Aid • Immediate care given to the victim of an accident or illness to minimize the effect of injury or illness until experts can take over • Reasons for providing correct first aid
Basic Principles of Providing First Aid • Remain calm and avoid panic • Evaluate situation thoroughly • Have a reason for anything you do • Treatment you provide will vary depending on type of injury or illness, environment, others present, equipment or supplies on hand, and availability of medical help
First Steps • Recognize that an emergency exists • Use all senses to detect problems • Sometimes signs of emergency are obvious and at other times they are less obvious
Next Steps • Check the scene and make sure it is safe to approach • What to observe • If not safe, call for medical help • If safe, approach the victim • Call emergency medical services (EMS) as soon as possible (continues)
Next Steps (continued) • If possible, obtain the victim’s permission before providing any care • Triage if necessary • Check for other injuries • Obtain as much information as possible before you proceed
General Principles • Obtain qualified help • Avoid any unnecessary movement of the victim • Reassure the victim • Use a confident, calm attitude to help relieve victim’s anxiety • Avoid giving the victim anything to eat or drink (continues)
General Principles (continued) • Protect the victim from cold or chilling, but avoid overheating • Work quickly in an organized and efficient manner • Do not make a diagnosis or discuss condition with observers at scene (continues)
General Principles (continued) • Maintain confidentiality and protect the victim’s right to privacy while providing treatment • Make every attempt to avoid further injury or harm • Provide only the treatment you are qualified to provide
CPR
16: 2 Performing CPR • Cardiopulmonary resuscitation (CPR): • Cardio: the heart • Pulmonary: the lungs • Resuscitation: to remove from apparent death or unconsciousness • When performing CPR, you breathe for the patient and circulate blood (continues)
Performing CPR (continued) • Purpose: keep oxygenated blood flowing to the brain and other vital body organs • Performed until the heart and lungs start working again or until medical help is available • Clinical versus biological death (continues)
Performing CPR (continued) • ABCDs of CPR • A stands for airway • B stands for breathing • C stands for circulation • D stands for defibrillation (continues)
Performing CPR (continued) • Evaluate victim’s condition before starting CPR: • Check if patient is conscious • If unconscious, check for breathing • If not breathing, place victim on back • Open the airway by using the head-tilt/chin lift or jaw-thrust maneuver (continues)
Performing CPR (continued) • Look for chest movement • Listen for breathing • Feel for movement of air from the nose or mouth • If not breathing, give two breaths • Make sure breaths are effective • Then check the carotid pulse (continues)
Performing CPR (continued) • Correct hand placement is needed before performing chest compressions • Various methods of CPR used • One-person adult rescue for adult • 30 compressions followed by 2 ventilations (30: 2 ratio) (continues)
Performing CPR (continued) • Two-person adult rescue for adult • 30 compressions by one rescuer followed with 2 ventilations by the second rescuer (30: 2 ratio) • CPR for infants (birth to one year) • 30 compressions followed by 2 ventilations for one rescuer (30: 2 ratio) • 15 compressions followed by 2 ventilations for two rescuers (15: 2 ratio) (continues)
Performing CPR (continued) • CPR for children (1 year to puberty) • 30 compressions followed by 2 ventilations for one rescuer (30: 2 ratio) • 15 compressions followed by 2 ventilations for two rescuers (15: 2 ratio) • CPR for choking victims • Reasons for stopping CPR
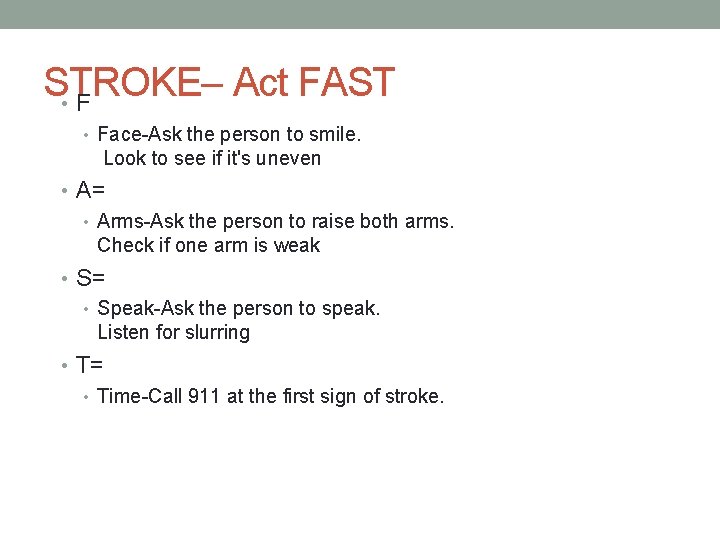
STROKE– Act FAST • Face-Ask the person to smile. Look to see if it's uneven • A= • Arms-Ask the person to raise both arms. Check if one arm is weak • S= • Speak-Ask the person to speak. Listen for slurring • T= • Time-Call 911 at the first sign of stroke.
Providing First Aid for Bleeding and Wound
16: 3 Providing First Aid for Bleeding and Wounds • Wound is an injury to soft tissues • Open: break in skin or mucous membranes • Closed: no break in skin or mucous membranes, but injury occurs to underlying tissues • Wounds can result in bleeding, infection, and/or tetanus
Classifications of Open Wounds • Abrasion • Skin is scraped off • Incision • Cut caused by a sharp object- knife, razor , blade
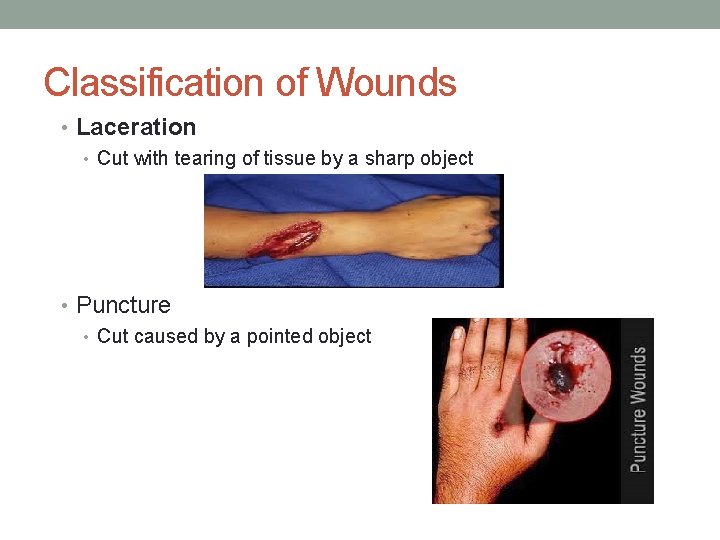
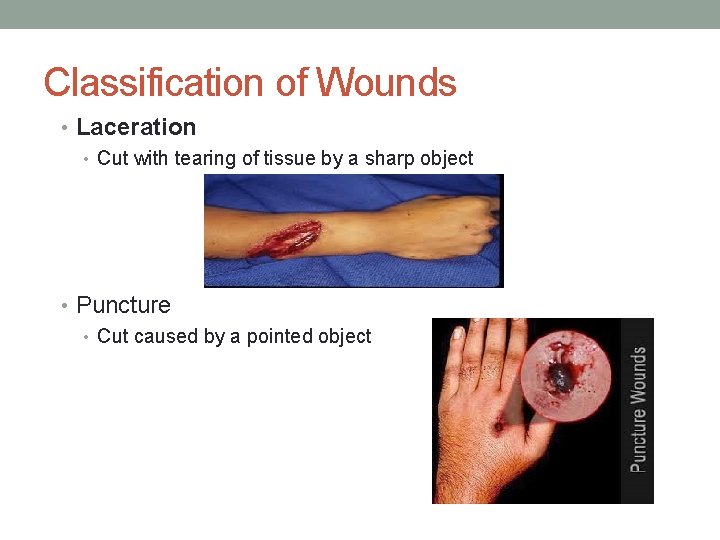
Classification of Wounds • Laceration • Cut with tearing of tissue by a sharp object • Puncture • Cut caused by a pointed object
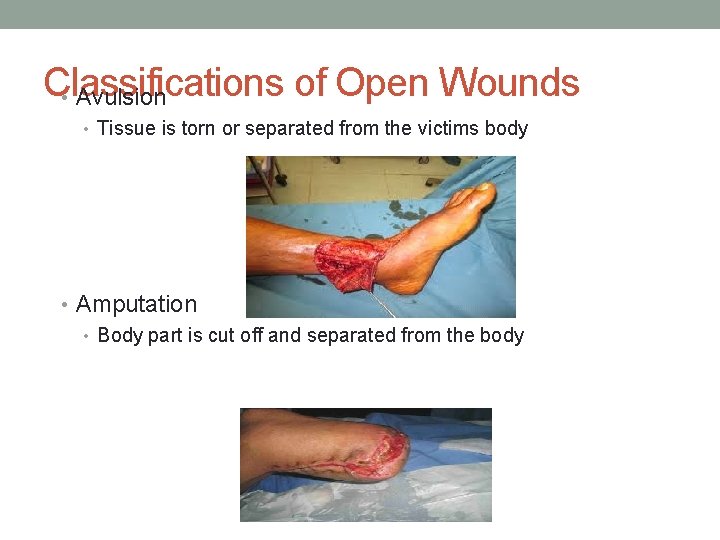
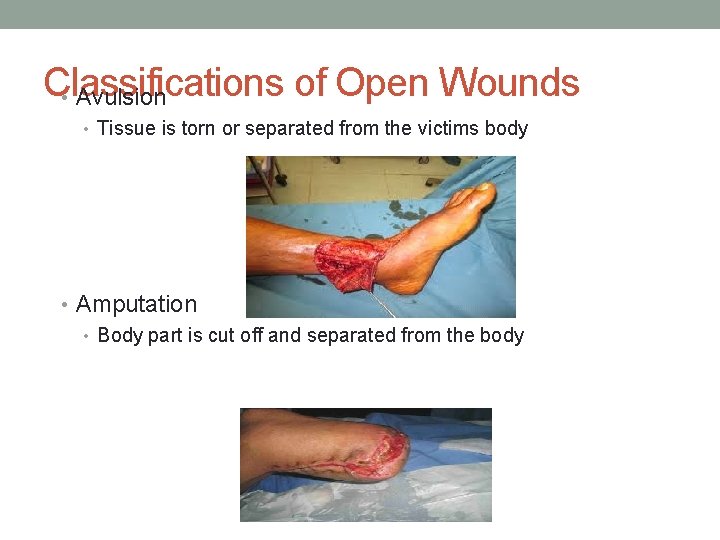
Classifications of Open Wounds • Avulsion • Tissue is torn or separated from the victims body • Amputation • Body part is cut off and separated from the body
Controlling Bleeding • First priority because victim can bleed to death quickly • Bleeding can come from arteries, veins, or capillaries • Observe standard precautions (continues)
Controlling Bleeding (continued) • Direct pressure • Pressure applied with gauze- use a clean cloth if sterile gauze not available • Elevation • Above the level of the heart- gravity helps to stop bleeding • Pressure bandages • Direct pressure and elevation are used • Pressure on pressure points • Main blood supply to the affected area helps minimize blood loss

Controlling Bleeding • Do not disturb clots • Clots are a natural defense in the bodies attempt to stop bleeding • Do not remove dressings • May result in additional bleeding • Do not clean wound • May also lead to further bleeding
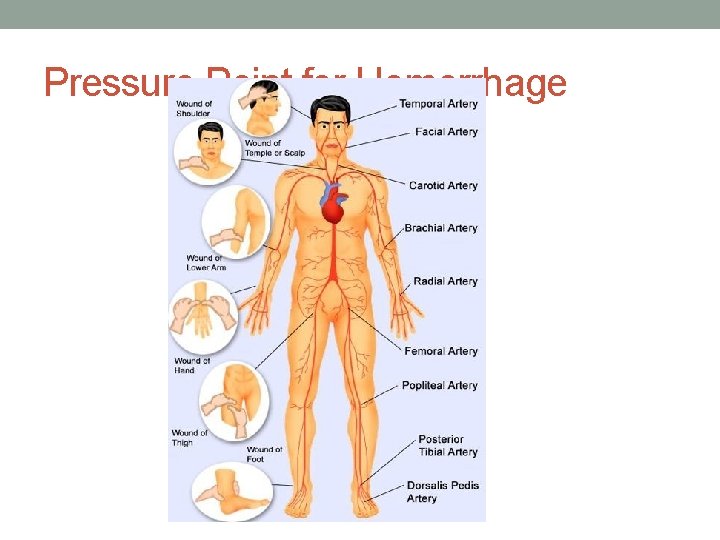
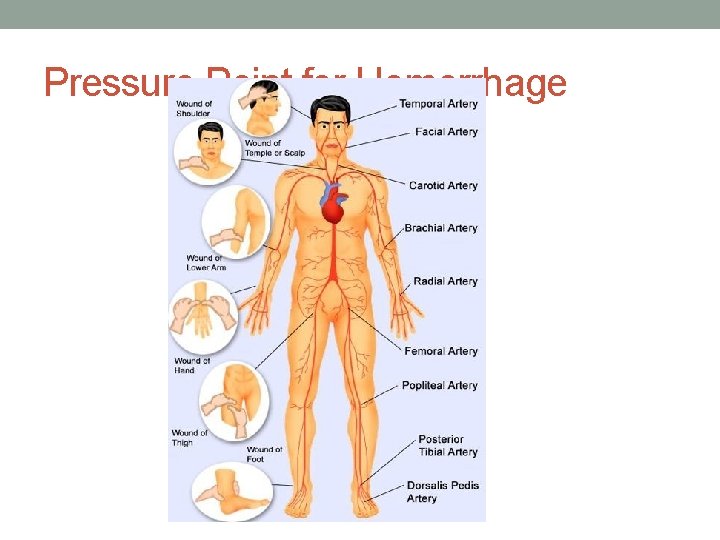
Pressure Point for Hemorrhage
Minor Wounds • First priority— • prevention of infection • Wash your hands thoroughly before caring for wound • Put on gloves • Wash the wound with soap and water • Rinse the wound • Use sterile supplies
Signs of Infection • Swelling • Heat • Redness • Pain • Fever • Pus • Red streaks • Seek prompt medical care if any of the above occur
Tetanus • Tetanus bacteria can easily enter an open wound • Tetanus is a serious illness caused by Clostridium bacteria • The infection causes painful tightening of the muscles, usually all over the body. It can lead to "locking" of the jaw. This makes it impossible to open your mouth or swallow. Tetanus is a medical emergency. You need to get treatment in a hospital • Most common in puncture wounds • Assess for last tetanus shot • Serious illness • Get tetanus shot or booster as needed
Objects Embedded in Wound • Examples such as splinters, pieces of glass, or small stones • If superficial, gently remove • Objects embedded in tissues should be left and removed by physician
Closed Wounds • Can occur anywhere on body • If bruise, apply cold application to reduce swelling • Observe for signs of internal bleeding • Get medical help • Check breathing and treat for shock • Avoid unnecessary movement • No food or fluids
What should you do? • You are slicing carrots and cut off the end of your finger--- What should you do? ? ?
What Should You Do? • You are watching TV with your parents. Suddenly your father c/o • Severe chest pain radiating down his left arm • Shortness of breath • Lips are cyanotic • Skin is diaphoretic • What should you do?
SHOCK STATES
Inflammatory Response • INJURY (bacteria, physical trauma, heat) – injured cells release chemicals (like histamine, kinins) – blood vessels dilate and capillaries become leaky- injury attracts WBC’s and phagocytes- dilation of blood vessels causes increased blood flow to area ( ie. redness)- swelling caused by fluid leaking out of capillaries WHY DOES OUR BODY RESPOND THIS WAY? - Prevents spread of damaging agents to nearby tissues - Disposes of pathogens/debris - Clotting proteins/ fibrin wall off damaged area and prevent spread of pathogen
16: 4 Providing First Aid for Shock • Also called hypoperfusion • Can exist with any injury or illness • Shock: clinical set of signs and symptoms that are associated with an inadequate supply of blood to body organs, especially brain and heart • Just 4 -6 minutes of hyoperfusion cause brain damage • Causes of shock • Can you name some? ? ?
Types of Shock • See Table 16 -1 in text • Anaphylactic • Allergic reactions causing histamine release = massive vasodilatation (hives, wheezing, coughing, chest tightness)= give epinephrine • Cardiogenic • Heart can not pump • Hemorrhagic • Excessive blood loss • Respiratory • Gas exchange is altered (continues)
Types of Shock • Psychogenic • Severe emotional distress- anger, fear, grief cause dilation of blood vessels (fainting) • Septic • Infections or poisoning causing severe vasodilatation • Metabolic • Causing changes in normal balance or homeostasis of the body • Loss of fluids from extreme vomiting, diarrhea, and heat • Neurogenic • Sympathetic nervous system can’t control the size of blood vessels • Injury and/or trauma to the spinal cord, general anesthesia,
Signs and Symptoms of Shock • Skin is pale or bluish-gray and cool or cold to the touch • Diaphoresis • Rapid and weak pulse • Respirations rapid, shallow, and may be irregular • Blood pressure very low or unobtainable (late sign of shock) (continues)
Signs and Symptoms of Shock (continued) • General weakness • Anxiety and extreme restlessness • Excessive thirst • Nausea and/or vomiting • Blurred vision or changes in appearance of eyes
Treatment for Shock • Goals of treatment- Shock states are life threatening • SEEK MEDICAL ATTENTION STAT • Improve circulation—especially – to the heart and brain • Provide oxygen • Maintain body temperature • *****Reduce effects of or eliminate the cause
Shock • Positioning of victim • Best position is supine with legs elevated 12 inches • DO NOT move Pt if neck or spine injuries are suspected unless pt in danger • Put on side if mouth bleeding or vomiting • Raise head and shoulders if respiratory problems • Maintain body temperature • cover the victim with blankets to prevent chilling and exposure to cold– avoid overheating the victim • Avoid food or drink • DO NOT GIVE anything by mouth
First Aid for Shock • Other principles of care • Standard precautions if available! • Check the scene • Move victim only if absolutely necessary • CALL 911 • Provide care to the victim • Control bleeding • Observe for signs of shock
First Aid for Shock • Try to reduce or eliminate the cause • Control bleeding by applying pressure to sites • Provide O 2 if possible • Attempt to ease the pain through position changes and comfort measures • Give emotional support
Poisoning
16: 5 Providing First Aid for Poisoning • Poison: any substance that causes a harmful reaction to the outside or inside of the body • Immediate action is needed • First aid varies depending on type of poison, injury involved, and the method of contact • Are they breathing? Are they breathing but unconscious?
Ways Poisoning Occurs • Ingesting various substances • Inhaling poisonous gases • Injecting substances • Contacting the skin with poison
First Aid for Poisoning • If poison has been swallowed • Immediate attention before what occurs? ? • Call poison control center (PCC), 911, or go to ER immediately • Save the label or container to give to PCC or MD • How much was ingested? • Save a sample of vomitus if patient happens to vomit • Methods to induce vomiting- caution– must be told to do so • DO NOT INDUCE VOMITING on a unconscious victim!! • Some instructions by PCC may be to tickle back of throat, give warm saltwater to drink, syrup of ipecac/water (can be kept in first aid kit), activated charcoal

First Aid for Poisoning Victim • If poisoning by inhalation of gases • If entering area- take deep breath- try to hold breath while rescuing patient • Remove victim from the area • Check for adequate breathing • Provide artificial respiration if necessary • Call for help--- 911
First Aid for Poisoning Victim • If poisoning by contact with skin • Wash area with large amounts of water 15 -20 min • Will help to dilute the substance • Remove any contaminated clothing • Call Dr. or seek medical attention ASAP or PCC
First Aid for Poisoning Victim • Contact with poisonous plants • Wash well with water and soap • If rash develops– apply Calamine or Caladryl lotion as directed
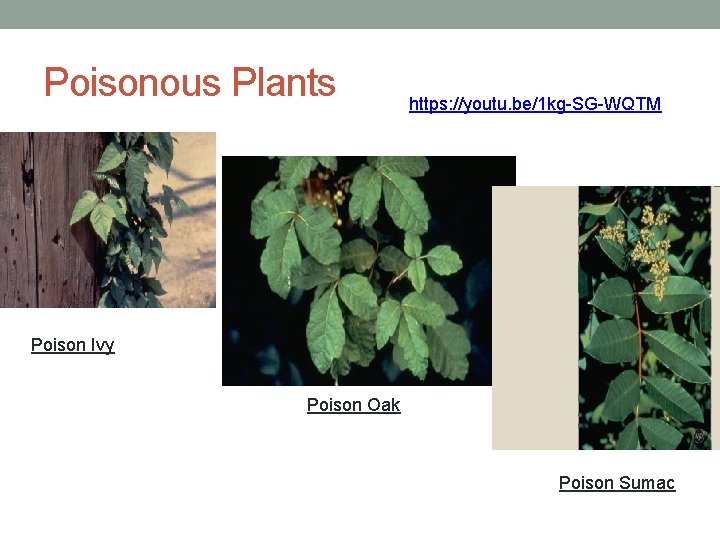
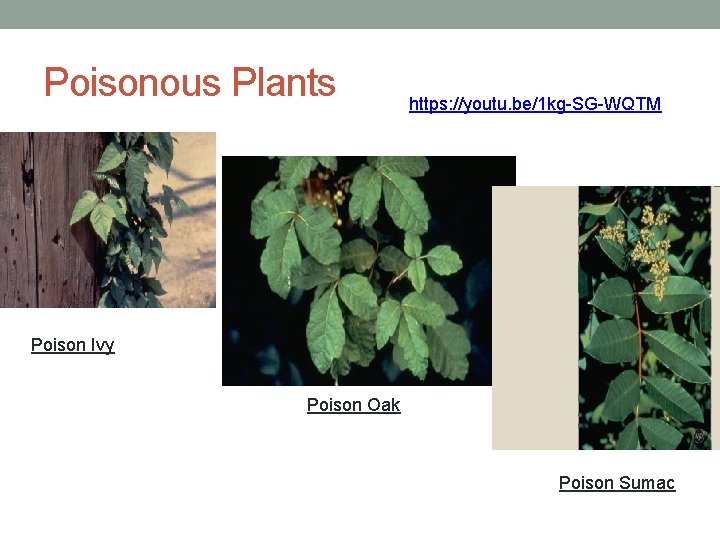
Poisonous Plants https: //youtu. be/1 kg-SG-WQTM Poison Ivy Poison Oak Poison Sumac

Poison Ivy Rash
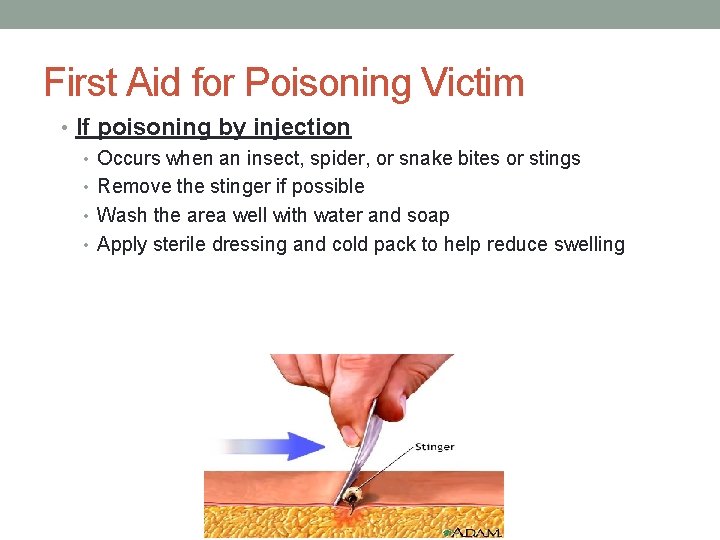
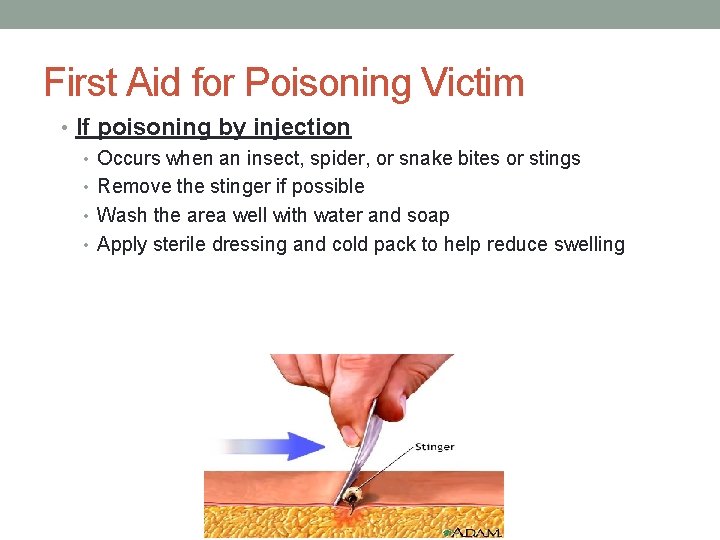
First Aid for Poisoning Victim • If poisoning by injection • Occurs when an insect, spider, or snake bites or stings • Remove the stinger if possible • Wash the area well with water and soap • Apply sterile dressing and cold pack to help reduce swelling
First Aid for Poisoning Victim • Ticks • Wash area with water and soap • Apply antiseptic • Monitor for signs of infection • Seek medical attention
First Aid for Poisoning Victim • Restrict movement –keep affected area below heart level reduce the flow of venom • Wash wound • Remove rings or constricting items • Monitor pulse, rate of breathing, and blood pressure -- if possible. Signs of shock , lay the person flat, raise the feet about a foot, and cover the person with a blanket • Get medical help right away. • Do not waste time hunting for the snake • Call MD, seek medical advise to
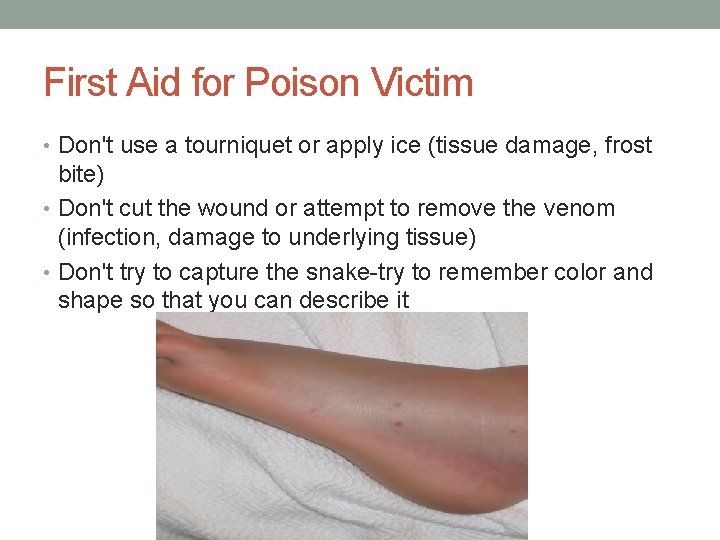
First Aid for Poison Victim • Don't use a tourniquet or apply ice (tissue damage, frost bite) • Don't cut the wound or attempt to remove the venom (infection, damage to underlying tissue) • Don't try to capture the snake-try to remember color and shape so that you can describe it
First Aid for Poisoning Victim • For any type of injection poisoning-- • Watch for allergic reactions and or anaphylactic shock • Monitor airway • Call for medical assistance ASAP • Reassure patient throughout • REVIEW- What are the signs of an allergic/anaphylaxis reaction?
Watch for : • Redness at site • Swelling or edema at site • Itch • Hives • Pain • Swelling of throat • Dyspnea • Dizziness • Changes in LOC • hypotension
Burns
16: 6 Providing First Aid for Burns • Injury caused by fire, heat, chemical agents, radiation, and/or electricity • Classifications of burns • Superficial – first degree burn • least severe type of burn • Involves only the top layer of skin • Skin is red or discolored, mild swelling or pain • Most common cause of sunburn • brief contact with steam or hot object
Classifications of Burns • Partial-thickness -- second degree burn • Involves injury to the top layers of skin • Blister will form • Skin is red with mottled appearance, painful, may take 3 -4 weeks to heal • Common causes—excessive sub exposure, sunlamp, radiation, contact with hot or boiling liquids, fire • Full-thickness– third degree burn • Most severe burn • Injury to all layers and underlying tissue • White and or charred appearance, very painful or painless if nerves damaged • Can be life threatening—if infection, shock develops
Treatment Objectives • Remove source of heat • Cool the skin • Do not use ice– may cool skin excessively • Cover the burn • Relieve pain • Observe for and treat shock • Prevent infections
Treatment • Medical treatment--Usually not required for superficial and mild partial-thickness burns • Rules for when to treat • If more than 15 % of the body is burned (adult) or 10% of a • • child’s body Rule of Nines– see figure 16: 26 p. 490 Seek Dr if burns affect face or respiratory tract Burns cover more than one body part Less than 5 or greater than 60 years old (continues)
Treatment • All full-thickness burns require medical treatment • How to treat superficial and mild partial-thickness burns • Cool area with large amounts of cool water • dry with sterile gauze • Apply sterile dressing • Use non-adhering dressing to area
Treatment • How to treat severe partial- or full-thickness burns • Call for help immediately • Cover with a sterile dressing • Elevate affected areas • Do no allow victim to walk • Do not remove any clothing that may be attached to the burn • Watch for sign of shock/ respiratory distress until medical help arrives • How to treat when chemicals splashed on skin • How to treat eyes burned by chemicals or irritating gases
Chemical Burns • How to treat when chemicals splashed on skin • Use large amounts of water to flush the area– 15 -30 minutes • Remove any clothing or jewelry that may still have chemical • Watch for signs of shock/respiratory distress until help arrives

Eyes • How to treat eyes burned by chemicals or irritating gases • Flush the eyes with large amounts of water 15 -30 minutes • Caution not to drain water into the unaffected eye if only one is affected • Flush from the inner to outer eye • Watch for signs of shock/ respiratory distress until medical help arrives
Summary • Loss of body fluids can occur very quickly with severe burns • Shock is common in burn victims • Be alert and know the signs of shock • remain calm- reassure patient • Call for help ASAP
Heat Stroke
16: 7 Providing First Aid for Heat Exposure • Overexposure to heat may cause a chemical imbalance in the body • Occurs when water and salt are lost through perspiration • Also occurs when body cannot eliminate excess heat
Heat Cramps • Muscle pains and spasms • As a result of water and sodium loss • Caused by exposure to heat • Loss of water and salt • Through perspiration • Apply firm pressure on cramped muscle to provide relief • Provide rest and move to cooler area • Small sips of water or electrolyte solution (e. g. , sports drink)
Heat Exhaustion • Occurs when exposed to heat with loss of fluids through sweating • Excessive exposure to heat or high external temperature • Heat exhaustion can quickly become heat stroke • Signs and symptoms • Pale and clammy skin • Excessive sweating • Headache • Muscle cramps • Nausea and cramps • Fainting and or dizziness
First Aid for Heat Exhaustion • First Aid Care • Move to a cooler area • Loosen clothing • Apply cool- wet cloths • Lay the patient down and elevate feet 12 inches • Give sips of cool water or a sports drink • Watch for shock/ respiratory distress and call for help if condition worsens
Heat Stroke • Prolonged exposure to higher than normal temperatures • Temperature greater that 105 F or 40. 6 C • Medical emergency—needs immediate care and attention • Body unable to eliminate excess heat • Normal body defenses are not working • Signs and symptoms • First aid care
First Aid for Heat Stroke • Signs and symptoms • High temperature • Red, hot, flushed skin • Rapid pulse • May lose consciousness • First aid care • Geared at cooling the body • High temp will lead to convulsions • Cool sponge bath • Ice or cold packs to groin, armpits • Call for medical help ASAP
Cold Exposure
16: 8 Providing First Aid for Cold Exposure • Exposure to cold temperatures can cause body tissues to freeze and body processes to slow down • Needs immediate attention • Degree of injury affected by wind velocity, amount of humidity, and length of exposure to cold
Hypothermia • When body temperature is less than 95ºF (35ºC) • Caused by prolonged exposure to cold • Signs and symptoms • Shivering • Numbness • Weakness or drowsiness • Confusion • LOC

• Death can occur if body processes become too slowed down • First aid care • Warm up the victim---slowly • Remove any wet clothing • Warm beverage if patient is conscious and able to swallow • Bair hugger devices
Frostbite • Freezing of tissue fluids with damage to the skin and underlying tissues • Caused by exposure to freezing or below-freezing temperatures • Early signs and symptoms • Redness • Tingling • Other signs and symptoms as frostbite progresses • • • Pale, glossy skin Blisters White- grayish color Pain LOC and death (continues)
Frostbite • Objectives of first aid • Directed at maintaining respirations • Treating shock • Warming body • Preventing further injury • Common sites: fingers, toes, ears, nose, cheeks • First aid care • Assess for signs and symptoms of shock and treat as needed
Bone and Joint Injuries
Anatomy Review • Bones provide framework for muscles and tendons • Bone is living tissue containing nerves and blood supply • Red marrow---sternum, ribs, vertebrae humerus, femur---- RBC’s, Plts, some WBC’S • Muscle is directly attached to bone by tendons (tough, fibrous connective- tissue cords)--- move bone • Ligaments fibrous connective tissue connect bones to hold structures together and provide stability

16: 9 Providing First Aid for Bone and Joint Injuries • Frequently occur during accidents or falls with variety of injuries • Examples: fractures, dislocations, sprains, and strains • May have more than one type of injury to bones and joints at the same time
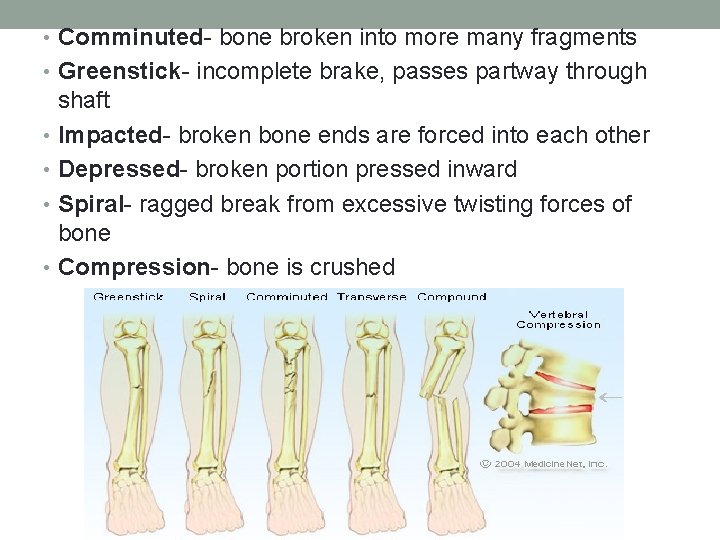
Fracture • Break in the bone • Closed or simple fracture • A bone break that is not accompanied by an external or open wound of the skin • Open or compound fracture • Broken bone ends penetrate through skin Examples= comminuted, compression, depressed, impacted, spiral, greenstick
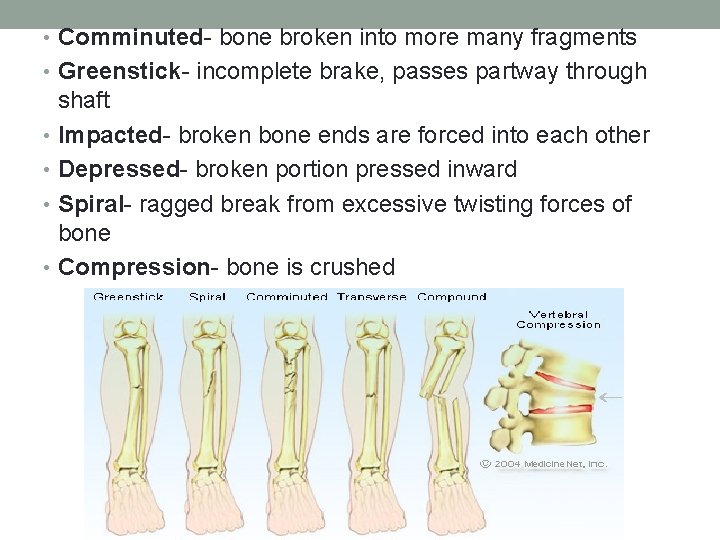
• Comminuted- bone broken into more many fragments • Greenstick- incomplete brake, passes partway through shaft • Impacted- broken bone ends are forced into each other • Depressed- broken portion pressed inward • Spiral- ragged break from excessive twisting forces of bone • Compression- bone is crushed
Sign & Symptoms • Signs and symptoms • Deformity (compare to uninjured limb; shortening, rotation, angulation) • Limited motion or loss of (guarding but not always with minimal tissue damage) • Free Movement • Pain & tenderness at the site (point tenderness) • Swelling , bleeding & discoloration (can mask break) • Protrusion of bone ends through the skin • Hearing a “snap” • Crepitus (grating or grinding sensation sometimes even heard) • Abnormal movement of the area • Objectives of first aid • Seek a doctor whenever a fracture is suspected
Dislocation • The end of the bone is displaced from a joint or moved out of its normal position within a joint • Tearing or stretching of ligaments, muscles, and other soft tissues also frequently occurs • Fingers, shoulder, elbow, knee • Signs and symptoms • Deformity • Limited or abnormal movement • Swelling & discoloration • Pain & tenderness • numbness • First aid care • Seek medical attention, sometimes reduces on its own • Immobilize affected part in place it was found (sling, splint)
Sprain • Injury to tissues surrounding a joint • Occurs when the joint is twisted or stretched beyond its normal ROM • Ligaments stretched or torn • Common sites: ankles, knee, and wrists • Signs and symptoms • Swelling, ecchymosis • Pain & discoloration (point tenderness) • Impaired motion may also occur • Sprains frequently resemble fractures or dislocations— treat as fracture if any doubt
First Aid for Sprain • Apply cold pack to reduce swelling • Elevate the affect area • Encourage rest of joint • Apply elastic bandage for support • Seek medical evaluation if the patient has sever swelling, pain or a fracture is suspected
Strain • Overstretching of a muscle • Caused by overexertion or by lifting • Frequent site: back • Signs and symptoms • Sudden pain • Swelling • bruising • First aid treatment • Rest • Cold pack application • Warm pack after cold reduces swelling • Seek medical evaluation
Assessment • Perfusion, motion, sensation? • Distal pulse, Cap refill, temp • Many important blood vessels and nerves are close to bone= injury can cause blood vessel or nerve injury • Manipulation of bone fragments can to press against or impale a nerve or vessel
Splints • Devices to immobilize injured parts • Many types of splints are available • Pneumatic or air splints • Padded boards • Traction splints • Splints can also be made from cardboard, newspapers, pillows, boards, etc. (continues)

Splints (continued) • Need to be long enough to immobilize the joint above and below the injured area to prevent movement • Should be padded • Tied in place • Apply as not to create pressure on affected area • If open wound, control bleeding before applying splint (continues)
Splints (continued) • Never attempt to reposition bone • Do not move the victim • Must splint before moving victim • Observe precautions when using pneumatic splints • Traction splints • Special devices that provide pulling or traction effect on the injured bone • Commonly used for fx of femur
Circulation Check After Splint • Verify that the splints are not too tight • Check skin temperature • Check color • Note swelling or edema • Numbness or tingling • Check pulse • If circulation impaired, immediately loosen the ties
Slings • Commercial slings • Triangular bandages • Use: support arm, hand, forearm, and shoulder • Positioning of sling • Hand should be slightly higher than that elbow • Helps with circulation, pain and edema (continues)
Slings (continued) • Check circulation • Check for skin color, temp, edema, pain numbness or tingling • Nail bed check • Limit movement of limb • If using knots • Placement • Padding • Considerations for shoulder injury • Keep arm close to the body • Additional strap can be placed to keep arm against the body • https: //youtu. be/Ot 7 c 3 sy. Ptr 4

Neck & Spine Injuries
Neck or Spine Injury • Most dangerous types of injuries involving bones and joints • Movement can result in permanent injury resulting in paralysis • Avoid any movement of victim if at all possible • Wait for backboard, cervical collar, and adequate help to arrive for transfer
Neck & Spine • Injuries to these areas involve a great deal of: • Pain • Anxiety • Discomfort • First Aid • Check for LOC– assess airway, breathing & circuation • Call EMS • Move only if NECESSARY • Reassure patient that help is on the way

First Aid for Specific Injuries
16: 10 Providing First Aid for Specific Injuries • For the most part— • Treatment for burns, bleeding, wounds, poisoning, and fractures is basically the same • Injuries to specific body parts require special care • Examples: eyes, ears, nose, brain, chest, abdomen, and genital organs
Eye Injuries • Always involves danger of vision loss • Best to avoid giving major treatment • Obtain help of a specialist • Foreign objects in the eye • dirt, dust small particles can easily enter the eye • Will cause irritation, and can scratch the eye
Signs & Symptoms of FBE • Redness • Burning sensation • Watering or tearful eyes • Presence of a floating object in the eye • TREATMENT • Wash the eye with lots of water • Pull the upper lid over the lower lid to stimulate tearing and wiping action • Raise eyelid, pt look down, flush, or remove with sterile gauze • Remove the FB when possible • DO NOT ATTEMPT TO REMOVE if it is embedded or you are not able to see it
Eye -- continued • Blows to the eye • Caused by fist, accidents or explosions • May cause contusions, and other internal bleeding • May lead to loss of vision • Penetrating injuries that cut eye tissue • Are very dangerous!! • Do not attempt to remove the object • Loosely apply dressing if possible and get to an ER ASAP • Paper cup with hole to stabilize impaled object • Lie flat if possible • Both injuries require the evaluation of a medical professional!!!!

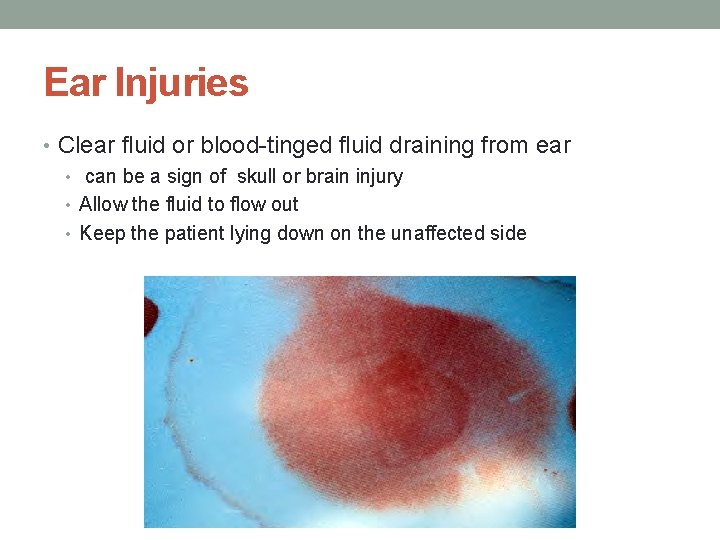
Ear Injuries • Can result in rupture or perforation of eardrum • Torn or detached tissue • apply sterile dressing and apply light pressure to control any bleeding • Ruptured or perforated eardrum • Place sterile gauze in the outer ear canal • Do not put any liquids in the ear • Clear fluid or blood-tinged fluid draining from ear

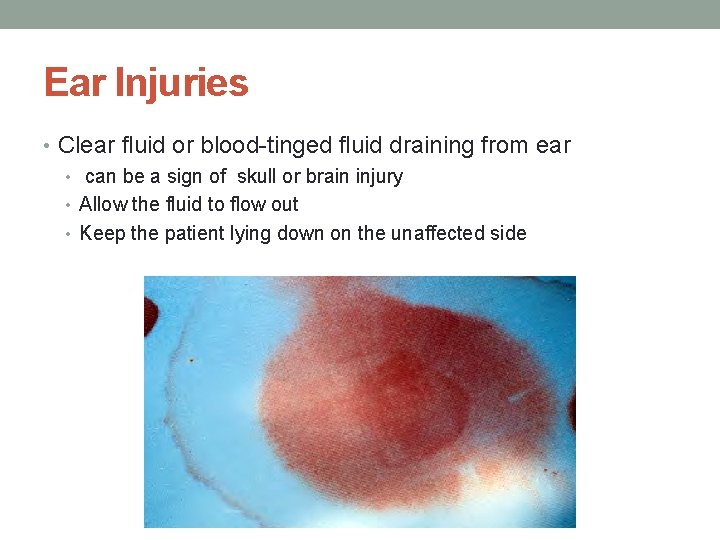
Ear Injuries • Clear fluid or blood-tinged fluid draining from ear • can be a sign of skull or brain injury • Allow the fluid to flow out • Keep the patient lying down on the unaffected side
Brain Injuries
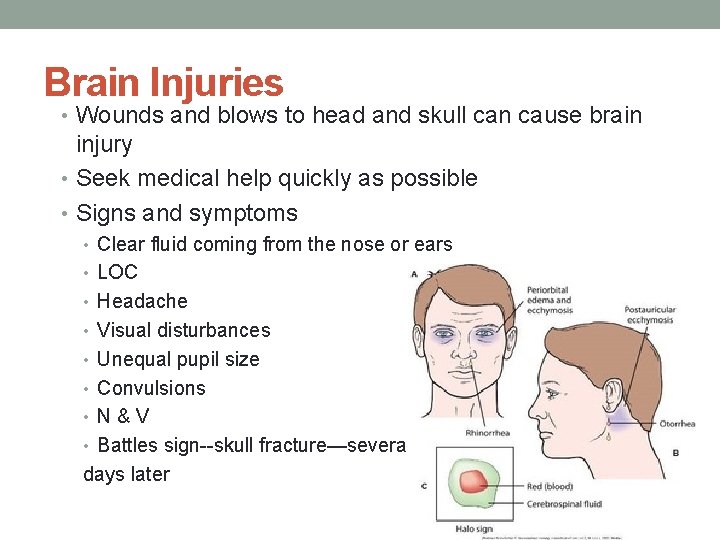
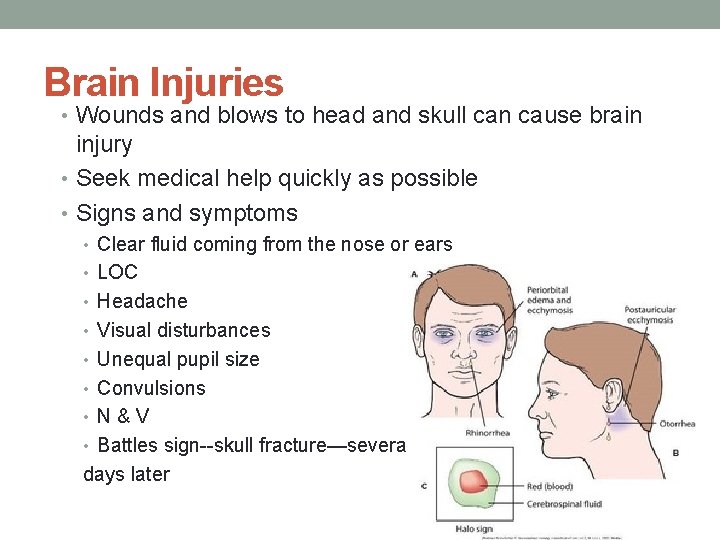
Brain Injuries • Wounds and blows to head and skull can cause brain injury • Seek medical help quickly as possible • Signs and symptoms • Clear fluid coming from the nose or ears • LOC • Headache • Visual disturbances • Unequal pupil size • Convulsions • N&V • Battles sign--skull fracture—several days later
First Aid for Head or Skull Injuries • Keep patient lying down and watch for shock • If no neck injury – you may slightly elevate the head • Watch for signs of respiratory distress • Do not give anything by mouth • Continue to watch for changes in LOC and report all findings to the EMS team
Nose Injuries
Nose Injuries • Epistaxis is the medical word for nosebleeds • Nosebleeds are usually more frightening than serious • Causes of nosebleeds • changes in altitude • Strenuous activity • HBP • Rupture of small vessels after a cold • First aid care
First Aid for Epistaxis • Treatment • Keep patient calm • Keep in a sitting position– with head slightly forward • Apply pressure toward the midline • If pressure does not stop the bleeding– you may insert a gauze into the affected nostril • Cold compresses to the bridge of the nose are helpful • Seek medical evaluation if bleeding persists or if a fx is suspected
Chest Injuries
Chest Injuries • Usually medical emergencies • Involve heart, lungs, and major vessels • Sucking chest wound • A deep open chest wound allowing air flow in and out with breathing • The partial vacuum present in the pleura is destroyed and the lung will collapse • Place an air tight dressing to the site and immediate medical evaluation is needed
Chest Injuries • Penetrating injuries to the chest • Can result in sucking chest wounds • If an object is the cause– do not remove it!!! • Place the victim in a comfortable position • Assess ABC’s and call 9111 • Crushing injuries to the chest • caused by car accidents or by heavy objects • May cause damage to ribs, lungs and heart • Elevate head and shoulders if no spine injury • Assess ABC’s • Call 911 immediately • https: //youtu. be/EHSe. Fm 89 Eo. M
Abdominal Injuries

Abdominal Injuries • Can cause damage to internal organs and bleeding in major blood vessels • Intestines and other abdominal organs may protrude from open wound • Medical emergency • Bleeding, shock, and damage to organs can be fatal
Signs & Symptoms of Abdominal Injuries • Severe abdominal pain • Protruding organs • Open wounds • Nausea and vomiting • Muscle rigidity • Shock symptom
First Aid of Abdominal Wounds • Position patient on his/her back– supine • Elevate head & shoulders • Place a rolled blanket or pillow under knees • Place moistened gauze over the wound– preferably with normal saline or sterile water • Warm tap water maybe used if sterile supplies are not available • cover with towel and maintain area warm
Genital Organs
Injuries to Genital Organs • Result of falls, blows, or explosions • Can cause severe pain, bleeding, and shock • First aid care is indicated to: • Contain bleeding • Control pain • Assess and treat for shock as indicated
First Aid Points for Genital Injuries • Assess and treat for shock • Do not remove any penetrating objects • Cover affect areas with moist dressings as you would with abdominal injuries • Collect and save any torn tissue (on ice) to the medical facility for evaluation and possible reattachment
Sudden Illness • Topics for discussion: • Heart attack • Syncope • Convulsions • Diabetic reactions
16: 11 Providing First Aid for Sudden Illness • Can be difficult to determine exact illness being experienced • Base care on signs and symptoms • Information from victim if possible • Look for medical alert bracelets or necklaces or medical cards
Heart Attack • Known by other names as coronary thrombosis, coronary occlusion, or myocardial infarction • Occurs when there is blockage in one or more coronary arteries • If heart stops, start CPR • Signs and symptoms • First aid care
Heart Attack Signs & Symptoms • Signs and symptoms • Pain – can be radiating to arms , neck, jaw can shoulders • Intense shortness of breath • Pallor of skin– especially the lips, nail beds • Weakness • Nausea and/ or vomiting • Diaphoresis • Eventual LOC
First Aid for a Heart Attack Victim • Place in comfortable position • Call for help-- 911 • Assess for breathing and for symptoms of shock • Reassure victim that help is on the way • *** it is recommended by the AHA the patients are given an aspirin to prevent platelet aggregation
Cerebral Vascular Accident. CVA / Stroke
Cerebrovascular Accident • Also called stroke, apoplexy, or cerebral thrombosis • Causes of stroke • Clots or a bleed in the brain • Signs and symptoms • Numbness • Paralysis • Unequal pupils • Confusion • Slurred speech • N &V
First Aid for Stroke • Call for help 911 • Aimed at monitoring respirations • Position- supine • Elevate head slightly and turn head to allow for drainage of secretions • Reassure patient • Treatment in an ER with interventions in less than 3 hours from the onset of symptoms can prevent extensive brain damage and recovery
Syncope
Syncope/Fainting • Temporary reduction in supply of blood to brain • Early signs and treatment • dizziness • Pallor • N&V • Diaphoresis • Numbness & tingling • If victim loses consciousness, try to prevent injury • Obtain medical help if recovery not prompt, there are other injuries, or fainting reoccurs
First Aid for Fainting • Postion– supine with legs elevated • Assess for breathing • Loosen clothing • Moisten face with cool cloths • Assess for other injuries • Allow for complete recovery before allowing patient to stand • Transition positions slowly
Convulsions/ Seizures
Convulsions • Type of seizure—strong involuntary contraction of muscles • Causes • Hyperthermia • Head injury • Brain diseases- tumors • epilepsy
Convulsions • Signs and symptoms • Body muscles become rigid • Jerky movements • May stop breathing • Loss of bladder and bowel control • Cyanosis of skin • Confusion and disorientation • headache
First Aid for Convulsions • Directed at preventing injury • Do not place anything in mouth • Do not force or stop movements • Assess for saliva/vomit– postion head to the side • Can for help if convulsion last more than a few minutes or for repeated seizure activity
Diabetic Reactions
Diabetes Mellitus • Body’s ability to metabolize glucose is impaired • Glucose is one of the basic sugars in the body and is the primary fuel for cell metabolism • Brain needs constant supply or cells can die • PROBLEM=lack of or ineffective action of insulin • Cells “starve” because insulin is needed to allow glucose to enter and nourish cells (like a key to let glucose into cell) • Glucose will remain in blood and continue to rise (hyperglycemia)
Type 1 diabetes- most people don’t produce insulin at all (IDDM), usually in children, need synthetic insulin injections Type 11 diabetes- appear later in life, make inadequate amounts of insulin, or resistant (NIDD)—oral meds stimulate pancreas to make more insulin, diet, exercise • Glucometer, test strips
Diabetic Ketoacidosis • When BG reaches 200 mg/dl (double normal level) or more, excess glucose is excreted by kidneys (spills into the urine) • Large amounts of fluid are lost due to osmotic dieresis. Glucose molecules “pull” fluid into blood vessels---- large amount urine output CAUSES the THREE “P’s” Polyuria- frequent large amount of urine Polydipsia- excessive thirst Polyphagia-excessive eating because of “cellular” hunger

• Body will turn to other food sources-----FAT-------Ketones and fatty acids are byproducts of the breakdown of fat • Increased ketones in blood can cause acidosis (PH 7. 357. 45) ACIDOSIS will prevent certain cells from functioning • SIGNS AND SYMPTOMS • vomiting, • Abdominal pain • Kussmaul respiration • Dehydration • Sweet fruity breath • Tachycardia • Low BP • Decreased LOC • Left untreated= unconsciousness, coma, death
Why does DKA happen? - Not under medical care - Not taking insulin or not enough insulin, overeating - Infection, illness - Overexertion - Fatigue
Diabetic Coma State of unconsciousness resulting from----- • Causes • Hyperglycemia • Ketoacidosis • Dehydration • Signs & Symptoms • Confusion • Weakness- dizziness • Nausea and/or vomiting • Rapid – deep respirations • Flushed skin • “fruity or sweet” breath • Low bp • Tachycardia • BLOOD GLUCOSE 400 - >800
Treatment • Aimed at restoring normal glucose levels for that patient • Call for help 911 • IVF • Insulin administration intravenously • Frequent blood glucose monitoring- every hour • Frequent electrolyte monitoring- every 4 hours • Potassium moves back into cells when glucose is moved back into cells • WATCH for decreased blood potassium levels— 3. 5 -4. 5 normal • LOW potassium can cause cardiac arrhythmias
Insulin Shock or Hypoglycemia • Caused by an excess amount of insulin/ not enough glucose in blood • Causes • Failure to eat • Infection • Vomiting after eating • Excessive insulin administration • Excessive exercise • Signs & Symptoms • Confusion, weakness, ANXIETY • Diaphoresis • Pallor • Hunger • Palpitations • Dizzy, HA • Tachycardia

Treatment for Hypoglycemic or Insulin Shock • Aim is to restore normal insulin levels in that patient • Activate 911 • Administer a source of glucose if conscious- juice, sugar gel between cheek and gum • Glucagon injection maybe indicated if pt is not conscious
16: 12 Applying Dressings and Bandages • Dressings used as sterile covering and to control bleeding • Materials used in dressings • Dressings can be held in place with tape or a bandage • Bandages used to hold dressings in place, to secure splints, and to support and protect body parts (continues)
Applying Dressings and Bandages (continued) • Apply bandages snugly to control bleeding and prevent movement of dressing, but not to interfere with circulation • Types of bandages consist of: • Roller gauze • Triangular • Elastic
Methods to Wrap Bandages • Depends on the body part • Spiral • Figure-eight for joints • Recurrent or finger wrap
Checkpoints for Circulation • Check circulation after application • Signs of poor or impaired circulation: • Swelling or edema • Pale or cyanotic color • Coldness to touch • Numbness or tingling • Poor or slow capillary refill • Loosen bandage immediately
Summary • Proper first aid can save a life • Provide only care you are qualified to provide • Always reassure victim and avoid unnecessary stress and movement • Obtain medical help as needed