Chapter 15 Urinary Incontinence Learning Objectives Describe the
Chapter 15: Urinary Incontinence
Learning Objectives • Describe the prevalence of urinary incontinence among older adults in community, acute care, and long-term care settings. • Identify the negative social, psychological, physical, and economic implications of urinary incontinence. • Understand that urinary incontinence is not a normal part of aging.
Learning Objectives (cont’d) • Collect the appropriate data related to patients’ urine control and plan evidence-based nursing care accordingly. • Initiate evidence-based behavioral interventions to treat urinary incontinence and promote continence for those at risk for urinary incontinence.
Prevalence • Estimates vary widely due to differences in definition, population studied, sampling approaches, and data collection methods – Total population with UI: 10% – Long-term care residents: up to 70% • Older women: 30% - 50% • Older men: 9% - 28% • Not normal consequence of aging but some physiological changes of aging increase risk of UI and some conditions that predispose UI occur more in older persons
Implications of Urinary Incontinence • Physical – Incontinence is associated with an increased risk of falls, fractures, skin breakdown, UTIs, disrupted sleep • Psychological (Figure 15 -1, p. 548) – Depression and anxiety both cause and consequence – Feelings of loss of control, dependency, shame and guilt, impaired self esteem – Majority of UI people do not seek help because they consider it a normal part of aging
Implications of Urinary Incontinence (cont’d) • Social – Social isolation, avoidance of activities • Economic – Costs not covered by insurance – Direct costs of UI: $16 billion/year – Costs to nursing homes: $5. 2 billion/year • Estimated 3% - 8% of nursing home costs and 1 hr labor per day go to incontinence care • Plus costs of medical effects like falls, fractures, pressure ulcers
Assessment • Transient Urinary Incontinence – caused by onset of an acute problem and should resolve once problem is successfully treated (P. 551, Table 15 -2). • Established Urinary Incontinence – Stress UI – Urge UI – Overflow UI – Functional UI – Mixed UI
• Stress incontinence: involuntary loss of urine during activities that increase intra-abdominal pressure (Triggered by laughing, sneezing, coughing or straining of abdominal muscles) – Absence of bladder contraction or overdistention. – Related to pregnancy, obesity, surgery, exercise, medications – Small amounts urine lost – Occasional or continual episodes of incontinence – Treatment: biofeedback, Kegel exercise.
• Urge incontinence: a strong, abrupt desire to void and the inability to inhibit leakage in time to reach a toilet. – Related to birth defects, spine or nerve damage, immobility, prostate problems or cancer – Moderate to large amounts of urine lost – Occasional or situational episodes of incontinence – Increase risk of falls – Treatment: Kegels
• Overflow incontinence: overdistention of the bladder due to abnormal emptying. – Related to birth defects, spine or nerve damage, MS, loss of bladder muscle tone, surgery, medications – No warning prior to incontinent episode – Small to moderate amount of urine lost – Frequent or continual incontinence – Treatment: treat cause, intermittent cath, bladder scans for post-void residuals
• Functional incontinence: refers to problems from factors external to the lower urinary tract such as cognitive impairments, obesity, clutter, immobility, or environmental barriers. – Related to inability to get to bathroom facilities due to functional reasons – May be associated with urge incontinence (mixed incontinence) – Treatment: modify environment; modify lifestyle

• Mixed incontinence: • Clinically, patients may exhibit symptoms of more than one type of incontinence. • Pure stress and pure urge incontinence were uncommon in a urodynamic evaluation of people age 65 years or older.
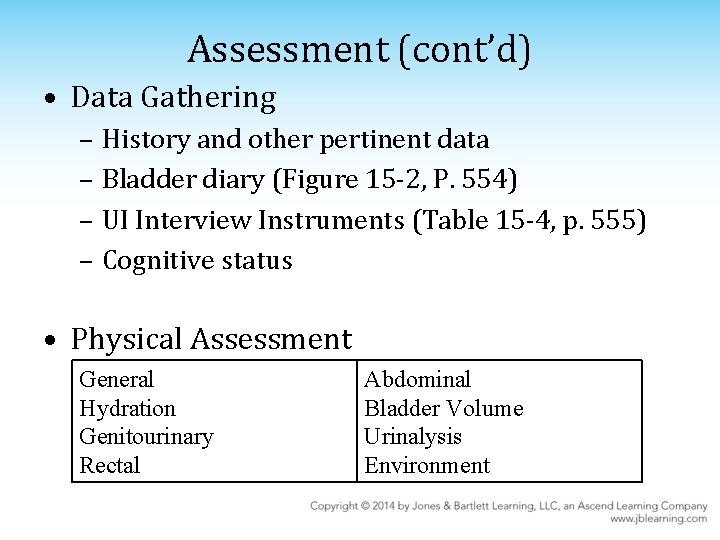
Assessment (cont’d) • Data Gathering – History and other pertinent data – Bladder diary (Figure 15 -2, P. 554) – UI Interview Instruments (Table 15 -4, p. 555) – Cognitive status • Physical Assessment General Hydration Genitourinary Rectal Abdominal Bladder Volume Urinalysis Environment

Interventions and Care Strategies • Patient-Centered Urinary Incontinence Treatment Goals – Understanding the patient’s expectations for treatment outcomes will provide direction for intervention – Patient goals are multidimensional; don't necessarily require total continence for patient satisfaction and improved healthrelated quality of life
Interventions and Care Strategies • Behavioral Management – Prompted voiding (Table 15 -7, p. 565): for the physically & cognitively impaired people. – Bladder training (Table 15 -8, p. 566): for the physically & cognitively independent, community dwelling people. – Pelvic muscle rehabilitation: “draw in” and “lift up” the rectal/anal sphincter muscles. Lift up the perivaginal muscles and avoid contracting the abdominal muscles. 10 repetitions 2~3 x /day (P. 568)
Interventions and Care Strategies (cont’d) • Pharmacological Management (Table 15 -9): Oxybutynin, Imipramine, Tamsulosin… – Can add to the effectiveness of behavioral strategies in frail older persons with urge UI – Potential for adverse reactions – Added cost • Devices and products – Continence garments – Toileting equipment and collection devices
Interventions and Care Strategies (cont’d) • Skin care – Preventing skin breakdown is very important – Moisture barriers & no-rinse incontinence cleansers are recommended over soap and water alone in preventing skin breakdown. – Incontinence-associated dermatitis (IAD) • Increases risk of pressure ulcers
Interventions and Care Strategies (cont’d) • Environmental Intervention – Modifying environment to allow rapid access to the toilet • Indwelling urinary catheters – No longer primary means of managing UI – Centers for Medicare and Medicaid Services (CMS) developed regulations for guidance of long-term indwelling catheter use. (Table 1510, p. 574)
Summary • Urinary incontinence – is a serious, potentially disabling condition with negative social, physical, psychological, and economic impacts – is a common condition in the older population, but is not a part of the normal aging process – can be successfully treated for improved health-related quality of life
- Slides: 19