Chapter 14 Inflammation Tissue Repair and Wound Healing
- Slides: 31
Chapter 14 Inflammation, Tissue Repair, and Wound Healing Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Inflammation • Intimately interwoven with the repair processes that replace damaged tissue or fill in the residue defects with fibrous scar tissue Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cardinal Signs of Inflammation • Rubor (redness) • Tumor (swelling) • Calor (heat) • Dolor (pain) • Functio laesa (loss of function) Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors Involved in Protective Responses and Bodily Repair • Inflammatory reaction • Immune response • Tissue repair and wound healing Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Causes of Inflammation • Immune response to infectious microorganisms • Trauma • Surgery • Caustic chemicals • Extremes of heat and cold • Ischemic damage to body tissues Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Inflammation 2 responses • Acute Inflammation –immediate and early response relatively short duration, few minutes to several days – 2 phases: vascular and cellular • Chronic inflammation – longer duration, days to years Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Vascular Changes that May Occur with Inflammation • An immediate transient response – Occurs with minor injury • An immediate sustained response – Occurs with more serious injury and continues for several days and damages the vessels in the area • A delayed hemodynamic response – Involves an increase in capillary permeability that occurs 4 to 24 hours after injury Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cellular Stage of Acute Inflammation • Marked by movement of phagocytic white blood cells (leukocytes) into the area of injury • Two types of leukocytes participate in the acute inflammatory response: – Granulocytes (neutrophils, eosinophils, and basophils) – Monocytes (the largest of the white blood cells) Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Inflammatory Mediators • Histamine – causes dilation of arterioles and increase permeability of venules • Arachidonic acid metabolites – Eicosanoids • Prostaglandins, Leukotrienes, Omega-3 polyunsaturated fatty acids • Platelet-activating factor (PAF) – induces platelet aggregation • Plasma proteins – interrelated systems clotting, compliment, and kinin • Cytokines – modulate the function of other cells Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
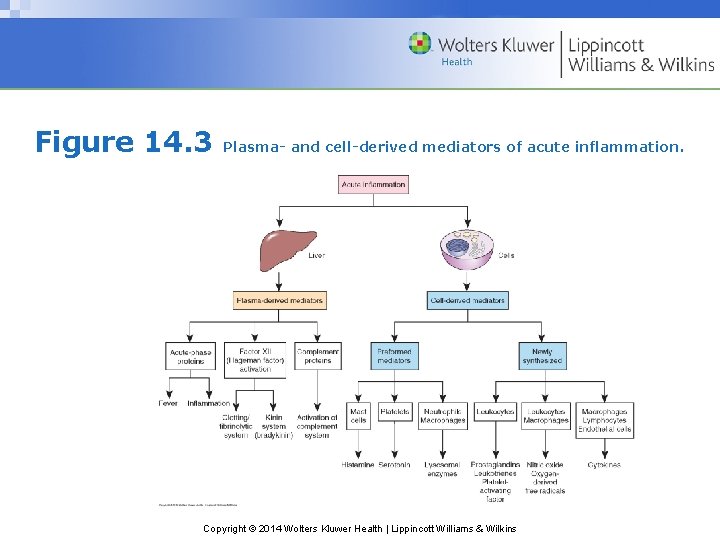
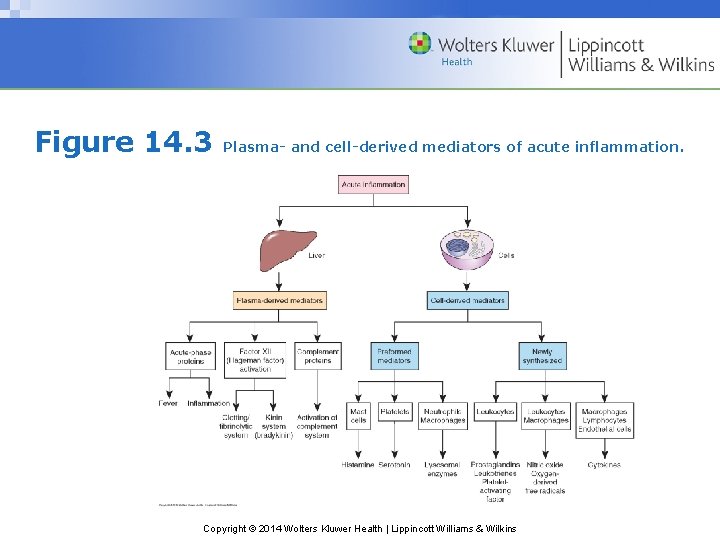
Figure 14. 3 Plasma- and cell-derived mediators of acute inflammation. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Classification of Inflammatory Mediators by Function • Those with vasoactive and smooth muscle–constricting properties • Chemotactic factors such as complement fragments and cytokines • Plasma proteases that can activate complement and components of the clotting system • Reactive molecules and cytokines liberated from leukocytes, which when released into the extracellular environment can damage the surrounding tissue Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Inflammatory Exudates • Serous Exudates – Watery fluids low in protein content – Result from plasma entering the inflammatory site • Hemorrhagic Exudates – Occur when there is severe tissue injury that causes damage to blood vessels or when there is significant leakage of red cells from the capillaries Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Inflammatory Exudates (cont. ) • Fibrinous Exudates – Contain large amounts of fibrinogen and form a thick and sticky meshwork • Membranous or Pseudomembranous Exudates – Develop on mucous membrane surfaces – Are composed of necrotic cells enmeshed in a fibropurulent exudate • Purulent or Suppurative Exudates – Contain pus; composed of degraded white blood cells, proteins, and tissue debris Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Basic Patterns of Inflammation • Acute inflammation – Of relatively short duration; nonspecific early response to injury – Aimed primarily at removing the injurious agent and limiting tissue damage • Chronic inflammation – Longer duration lasting for days to years – A recurrent or progressive acute inflammatory process or a low-grade smoldering response that fails to evoke an acute response Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Chronic Versus Acute Inflammation • Acute inflammation—self-limited and of short duration – Infiltration of neutrophils – Exudate • Chronic inflammation—self-perpetuating and may last for weeks, months, or even years – Infiltration by mononuclear cells (macrophages) and lymphocytes – Proliferation of fibroblasts Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Most Prominent Systemic Manifestations of Inflammation • Acute-phase response • Alterations in white blood cell count (leukocytosis or leukopenia) • Fever • Sepsis and septic shock (severe) Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Is the following statement true or false? • Permanent cells, once damaged, can easily be regenerated and their functions recovered. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • False • Rationale: Many cells in the body cannot be replaced once they die. Neurons and cardiac cells are such examples. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Tissue Repair: Types of Structures of Body Organs and Tissues • Parenchymal Tissues – Tissues contain the functioning cells of an organ or body part (e. g. , hepatocytes, renal tubular cells) • The Stromal Tissues – Consist of the supporting connective tissues, blood vessels, extracellular matrix, and nerve fibers Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Body Cells – according to their ability to regenerate • Labile Cells – Continue to divide and replicate throughout life, replacing cells that are continually being destroyed – Include oral cavity, skin, vagina, gastrointestinal track • Stable Cells – Normally stop dividing when growth ceases – Include liver, kidney, smooth muscle • Permanent Cells – Cannot undergo mitotic division – Include nerve, skeletal and cardiac muscle Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Fibrous Tissue Repair • Severe or persistent injury may not be repaired with regeneration alone. • Repair occurs by replacement with connective tissue that involves generation of granulation tissue and formation of scar tissue. • Granulation tissue is a glistening red, moist connective tissue that contains newly formed capillaries, proliferating fibroblasts, and residual inflammatory cells. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Steps in Development of a New Capillary Vessel • Proteolytic degradation of the parent vessel basement membrane, allowing formation of a capillary sprout • Migration of endothelial cells from the original capillary toward an angiogenic stimuli • Proliferation of the endothelial cells behind the leading edge of the migrating cells • Maturation of the endothelial cells and proliferation of pericytes (for capillaries) and smooth muscle cells (for larger vessels) Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Two Phases of Scar Formation • Emigration and proliferation of fibroblasts into the site of injury • Deposition of the ECM by these cells Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Healing by Primary or Secondary Intention • The objective of the healing process is to fill the gap created by tissue destruction and to restore the structural continuity. • Primary healing—small, clean wound • Secondary healing—great loss of tissue with contamination Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
3 Basic Components of the Extracellular Matrix (ECM) • 1. Fibrous structural proteins – Collagen and elastin fibers • 2. Water-hydrated gels that permit resilience and lubrication – Proteoglycans and hyaluronic acid • 3. Adhesive glycoproteins that connect the matrix elements to each other and to cells – Fibronectin and laminin Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
2 Basic Forms of the ECM • Basement Membrane – Surrounds epithelial, endothelial, and smooth muscle cells • Interstitial Matrix – Present in the spaces between cells the connective tissue and between the epithelium and supporting cells of blood vessels Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Stages of Wound Healing (pages 321 -322) • Mediated through cytokines and growth factors • 3 phases: – Inflammatory phase – Proliferative phase – Maturational or remodeling phase Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors Regulating the Healing Process • Action of chemical mediators and growth factors that mediate the healing process • Interactions between the extracellular and cell matrix Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Causes of Impaired Wound Healing • Malnutrition • Impaired blood flow and oxygen delivery • Impaired inflammatory and immune responses • Infection • Wound separation • Foreign bodies • Age effects Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question • Which of the following will promote wound healing? − A. Malnutrition − B. Increased blood flow and oxygen delivery − C. Infection − D. Foreign bodies Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer • B. Increased blood flow and oxygen delivery • Rationale: Increasing blood flow and oxygen delivery is one of the main objectives of the inflammatory response. This will allow for greater energy production and faster removal of dead material. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins