Chapter 13 Promotion of Safety 2009 Delmar Cengage





- Slides: 40

Chapter 13 Promotion of Safety © 2009 Delmar, Cengage Learning
Oxygen • Oxygen is necessary for life • Some diseases and conditions cause the patient to be unable to take in enough oxygen • Doctors will usually order additional oxygen to be given by an oxygen delivery system © 2009 Delmar, Cengage Learning
Oxygen • • Oyxgen is: a colorless, odorless gas a medication prescribed by a doctor highly flammable and feeds a fire, which can turn a small spark into a big flame • used by many people in healthcare facilities and in the community • represented by the chemical symbol of O 2. © 2009 Delmar, Cengage Learning
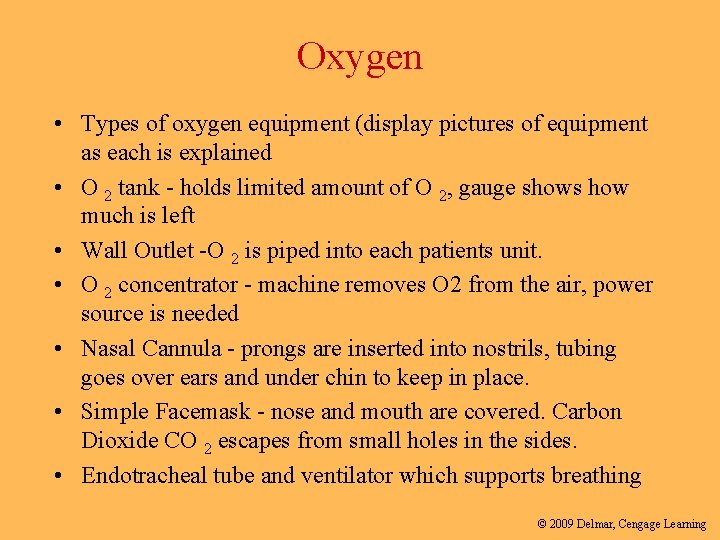
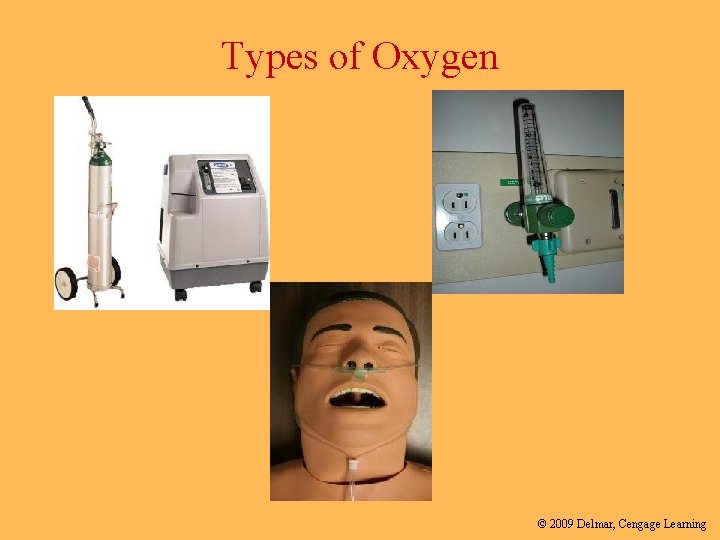
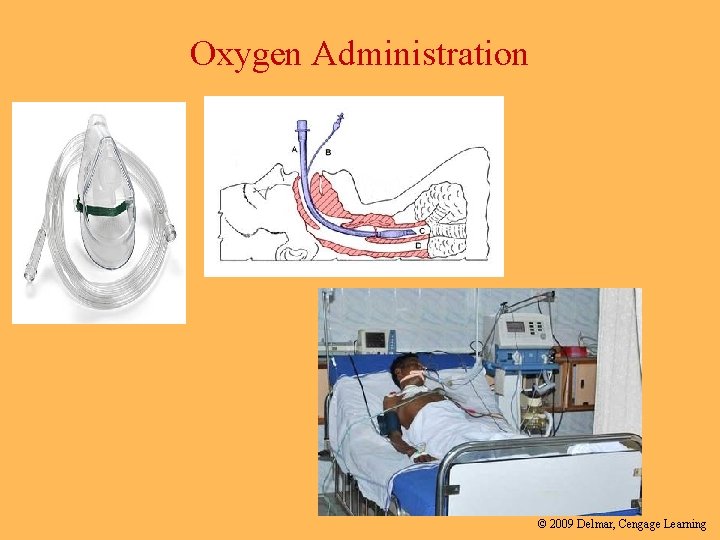
Oxygen • Types of oxygen equipment (display pictures of equipment as each is explained • O 2 tank - holds limited amount of O 2, gauge shows how much is left • Wall Outlet -O 2 is piped into each patients unit. • O 2 concentrator - machine removes O 2 from the air, power source is needed • Nasal Cannula - prongs are inserted into nostrils, tubing goes over ears and under chin to keep in place. • Simple Facemask - nose and mouth are covered. Carbon Dioxide CO 2 escapes from small holes in the sides. • Endotracheal tube and ventilator which supports breathing © 2009 Delmar, Cengage Learning
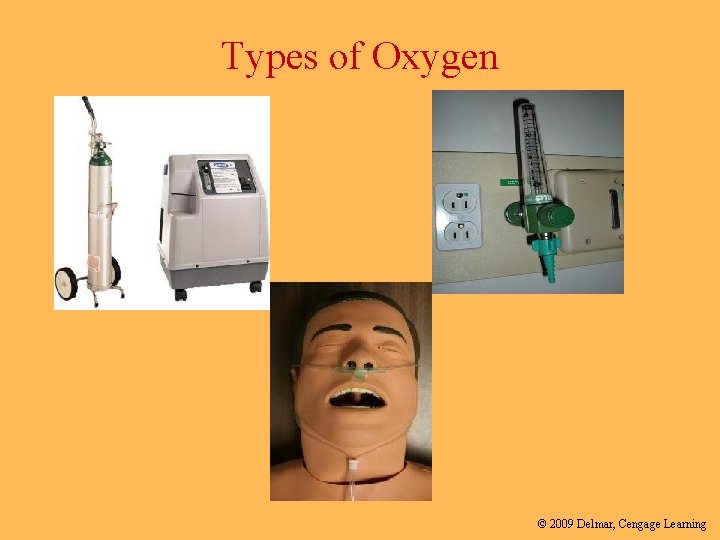
Types of Oxygen © 2009 Delmar, Cengage Learning
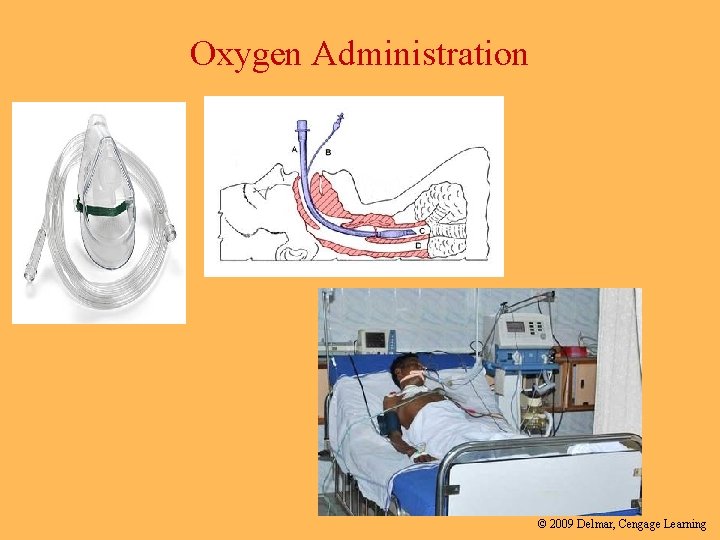
Oxygen Administration © 2009 Delmar, Cengage Learning
O 2 Precautions • • • O 2 in use sign on patient door No smoking sign O 2 tanks should always be in a carrier Be mindful of oxygen extension tubing Cotton clothing only – Avoid static electricity • No open flames © 2009 Delmar, Cengage Learning
Regulatory Agencies • The Joint Commission • OSHA- Occupational Safety and Health Administration • WHO- World Health Organization © 2009 Delmar, Cengage Learning

The Joint Commission (TJC) • The Joint Commission (TJC), formerly the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) • An independent, not-for-profit organization • Certifies more than 20, 000 health care organizations • Certification is recognized nationwide as a symbol of quality that reflects an organization’s commitment to meeting certain performance standards. © 2009 Delmar, Cengage Learning
The Joint Commission • Annual National Patient Safety Goals- to improve patient safety in identified problematic areas – Patient falls – Patient identification – Improve communication – Medication safety – Health care associated infections – Reconcile medications – Reduce flu and pneumococcal disease – Surgical fires – Pressure ulcers – Risk assessment – Changes in patient condition – Universal/standard precautions © 2009 Delmar, Cengage Learning
13: 2 Preventing Accidents and Injuries • Occupational Safety and Health Administration (OSHA) – Division of the Department of Labor – Establishes and enforces safety standards in the workplace – Two main standards that affect health care: • The Occupational Exposure to Hazardous Chemicals Standard • The Bloodborne Pathogen Standard (continues) © 2009 Delmar, Cengage Learning
1. Occupational Exposure to Hazardous Chemicals • The Standard requires employers to inform employees of all chemicals and hazards in workplace • All manufacturers must provide Material Safety Data Sheet (MSDS) with any hazardous product they sell • Specific information has to be provided on the MSDS • See MSDS on page 337 on DHO • Training for employees © 2009 Delmar, Cengage Learning
Preventing Accidents and Injuries (continued) • Two standards that affect health care workers: 1. The Occupational Exposure to Hazardous Chemicals Standard 2. The Bloodborne Pathogen Standard © 2009 Delmar, Cengage Learning

Bloodborne Pathogen Standard • Contains mandates to protect health care providers from diseases caused by exposure to body fluids • Diseases that can be contracted by exposure to body fluids include hepatitis B, hepatitis C, and HIV/AIDS © 2009 Delmar, Cengage Learning
Ergonomics © 2009 Delmar, Cengage Learning
Ergonomics • Applied science to promote the safety and well-being of a person by adapting the environment and using techniques to prevent injuries © 2009 Delmar, Cengage Learning
Components of Ergonomics • Correct placement of furniture and equipment • Training in muscle movements • Efforts to avoid repetitive motions • An awareness of the environment to prevent injuries (continues) © 2009 Delmar, Cengage Learning
Components of Ergonomics (continued) • Prevention of accident and injury • Centers around people and the immediate environment • Health care worker must follow safety regulations • Remember, health care workers have a legal responsibility to protect the patient from harm and injury © 2009 Delmar, Cengage Learning
Equipment and Solutions Regulations • Do not operate or use any equipment until you have been trained on how to use it • Read and follow operating instructions • Report any damaged or malfunctioning equipment immediately • Do not use frayed or damaged electrical cords (continues) © 2009 Delmar, Cengage Learning
Equipment and Solutions Regulations (continued) • Observe all safety rules • Read MSDSs • Never use solutions that are from unlabeled bottles • Read labels at least three times • Do not mix solutions together unless instructed to do so © 2009 Delmar, Cengage Learning
Patient/Resident Safety Regulations • Do not perform any procedures on patients unless instructed and properly authorized • Provide privacy for all patients • Identify your patient • Explain the procedure (continues) © 2009 Delmar, Cengage Learning
Personal Safety Regulations • Responsible to protect yourself and others from injury • Use correct body mechanics • Wear the required uniform • Walk; do not run • Report any injury or accident • Unsafe situations need to be reported (continues) © 2009 Delmar, Cengage Learning
Personal Safety Regulations (continued) • Keep all areas neat and clean • Wash hands frequently • Dry hands thoroughly before handling electrical equipment • Wear safety glasses when appropriate • Observe all safety precautions (continues) © 2009 Delmar, Cengage Learning
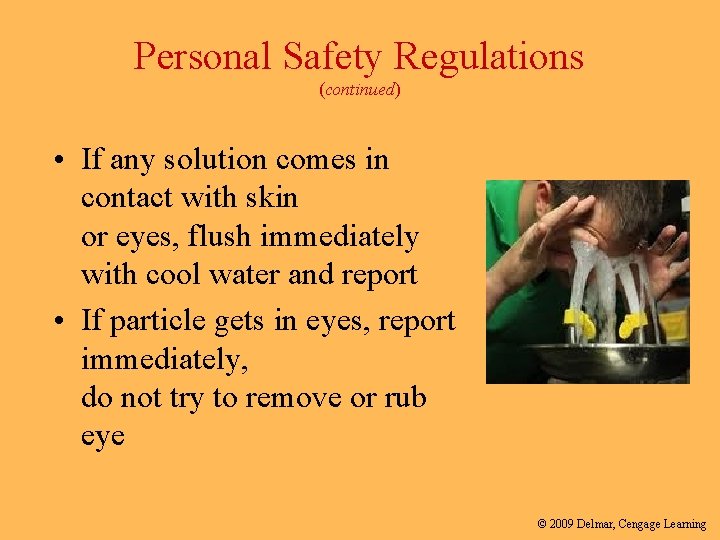
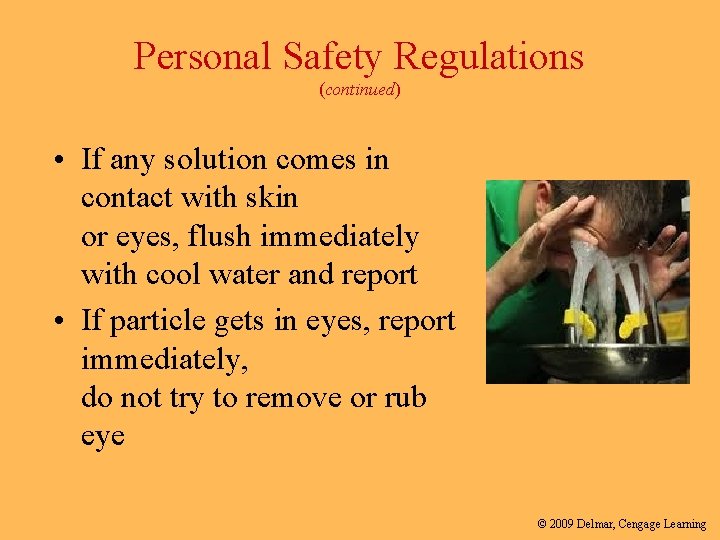
Personal Safety Regulations (continued) • If any solution comes in contact with skin or eyes, flush immediately with cool water and report • If particle gets in eyes, report immediately, do not try to remove or rub eye © 2009 Delmar, Cengage Learning
Occurrence/ Incident Reports • Records details of an accident or unusual event of patient, visitor or employee within 24 hours of event • This report documents exact details of the occurrence • Useful when dealing with possible liability issues in the future • It never becomes a part of the patient medical record © 2009 Delmar, Cengage Learning
Hospital Safety Informational Video • Hospital Workers Safety Video © 2009 Delmar, Cengage Learning
Summary • Health care workers are legally responsible for familiarizing themselves with disaster policies • Preventing fires is everyone’s concern • Be alert to causes of fires and take measures to prevent them • Know policies to follow in case of fire © 2009 Delmar, Cengage Learning

© 2009 Delmar, Cengage Learning
Sentinel Event © 2009 Delmar, Cengage Learning
Sentinel Event • A sentinel event is an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes loss of limb or function. © 2009 Delmar, Cengage Learning
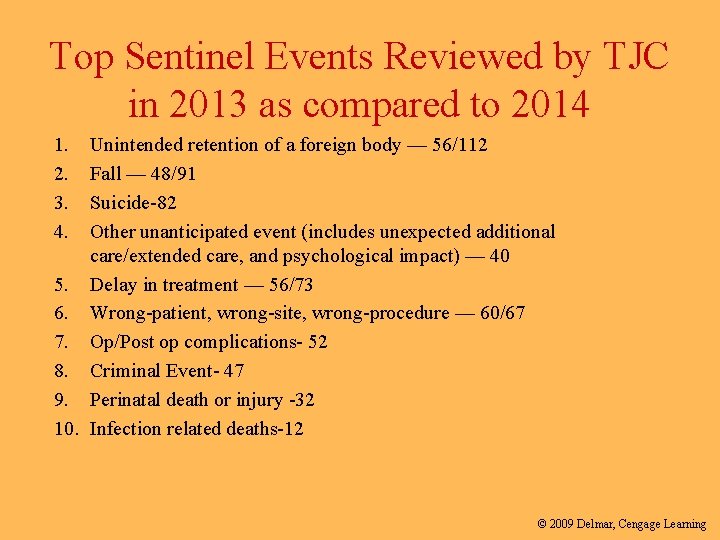
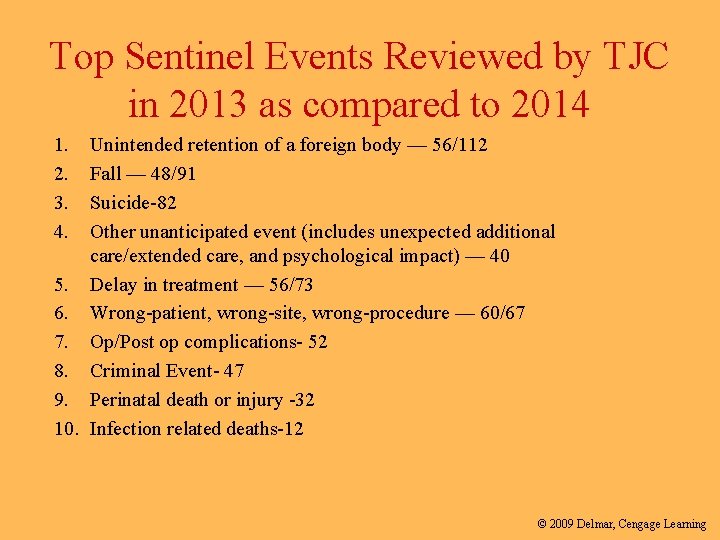
Top Sentinel Events Reviewed by TJC in 2013 as compared to 2014 1. 2. 3. 4. Unintended retention of a foreign body — 56/112 Fall — 48/91 Suicide-82 Other unanticipated event (includes unexpected additional care/extended care, and psychological impact) — 40 5. Delay in treatment — 56/73 6. Wrong-patient, wrong-site, wrong-procedure — 60/67 7. Op/Post op complications- 52 8. Criminal Event- 47 9. Perinatal death or injury -32 10. Infection related deaths-12 © 2009 Delmar, Cengage Learning
National Patient Safety Goals • Refer to handout • NPSG’s • You are expected to know all 7 NPSG’s © 2009 Delmar, Cengage Learning
Groups • In your groups– – Research specific examples of interventions ( at least 2) which currently exist to help improve patient safety as outlined by the NPSG’s © 2009 Delmar, Cengage Learning
What is your reaction? © 2009 Delmar, Cengage Learning
Statistic • ***It is estimated that between 44, 000 and 98, 000 patients die each year as a result of medical errors in the USA • That is the equivalent of at least 4 jet liners crash landing every week for one year without any survivors!! © 2009 Delmar, Cengage Learning
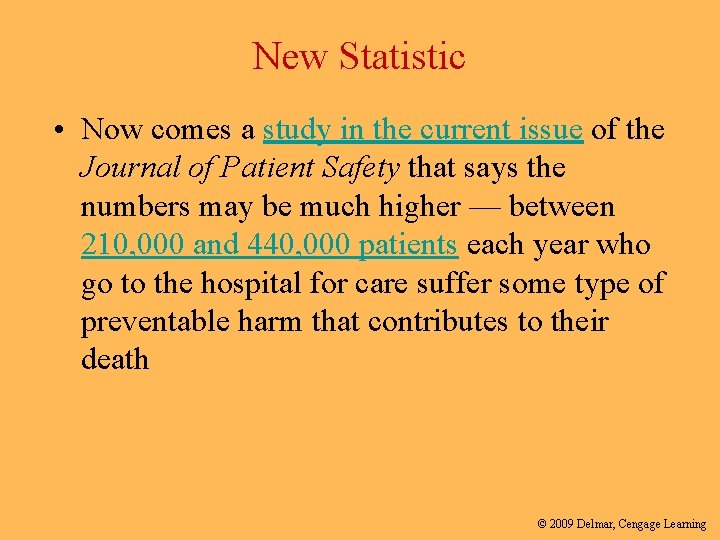
New Statistic • Now comes a study in the current issue of the Journal of Patient Safety that says the numbers may be much higher — between 210, 000 and 440, 000 patients each year who go to the hospital for care suffer some type of preventable harm that contributes to their death © 2009 Delmar, Cengage Learning
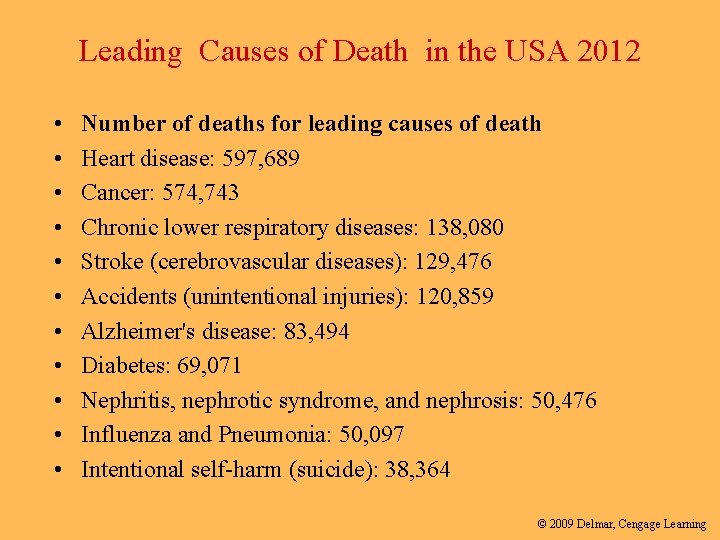
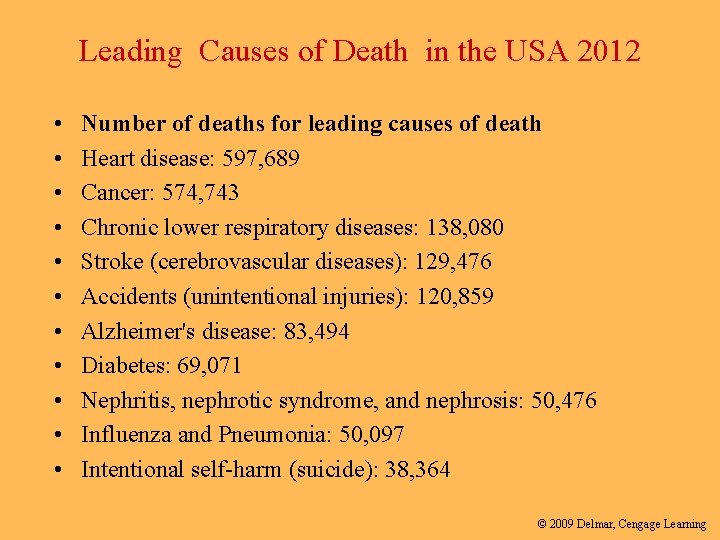
Leading Causes of Death in the USA 2012 • • • Number of deaths for leading causes of death Heart disease: 597, 689 Cancer: 574, 743 Chronic lower respiratory diseases: 138, 080 Stroke (cerebrovascular diseases): 129, 476 Accidents (unintentional injuries): 120, 859 Alzheimer's disease: 83, 494 Diabetes: 69, 071 Nephritis, nephrotic syndrome, and nephrosis: 50, 476 Influenza and Pneumonia: 50, 097 Intentional self-harm (suicide): 38, 364 © 2009 Delmar, Cengage Learning

The Josie King Story © 2009 Delmar, Cengage Learning
Josie King Story • Josie King © 2009 Delmar, Cengage Learning
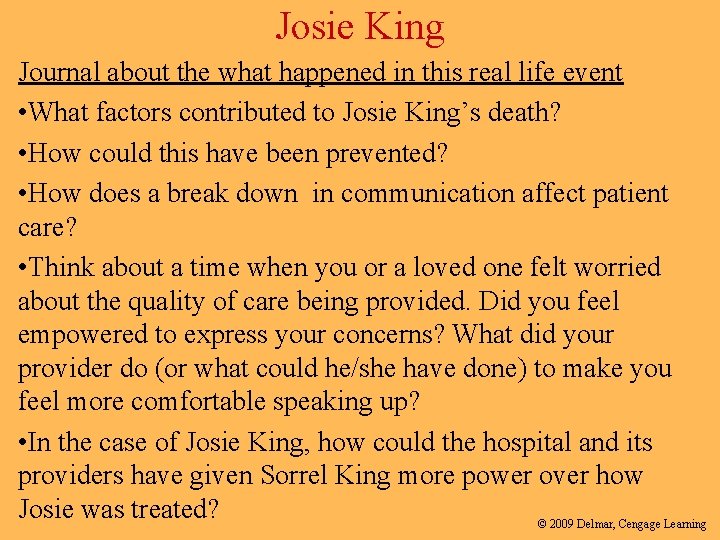
Josie King Journal about the what happened in this real life event • What factors contributed to Josie King’s death? • How could this have been prevented? • How does a break down in communication affect patient care? • Think about a time when you or a loved one felt worried about the quality of care being provided. Did you feel empowered to express your concerns? What did your provider do (or what could he/she have done) to make you feel more comfortable speaking up? • In the case of Josie King, how could the hospital and its providers have given Sorrel King more power over how Josie was treated? © 2009 Delmar, Cengage Learning
 Chapter 6:2 interpreting word parts
Chapter 6:2 interpreting word parts 2009 delmar cengage learning
2009 delmar cengage learning Chapter 1 introduction to medical terminology answer key
Chapter 1 introduction to medical terminology answer key 2009 delmar cengage learning
2009 delmar cengage learning Chapter 6 skeletal system
Chapter 6 skeletal system Chapter 13 medical math assignment sheet cengage learning
Chapter 13 medical math assignment sheet cengage learning Chapter 10 cultural diversity
Chapter 10 cultural diversity Delmar cengage learning instructor resources
Delmar cengage learning instructor resources Chapter 14 promotion of safety
Chapter 14 promotion of safety Delmar isotonic
Delmar isotonic Delmar tsi
Delmar tsi Delmar custom broker
Delmar custom broker Thomson delmar learning
Thomson delmar learning Delmar larsen
Delmar larsen Chapter 7 cengage
Chapter 7 cengage Cengage chapter 7
Cengage chapter 7 Chapter 13 accounting
Chapter 13 accounting Cengage chapter 7
Cengage chapter 7 Chapter 5 the cardiovascular system labeling exercises
Chapter 5 the cardiovascular system labeling exercises Cengage chapter 8 answers
Cengage chapter 8 answers Alges root word
Alges root word Chapter 4 the muscular system
Chapter 4 the muscular system Cengage medical terminology chapter 1
Cengage medical terminology chapter 1 Safety promotion sms
Safety promotion sms Cengage differential equations
Cengage differential equations Bank reconciliation cengage
Bank reconciliation cengage Separation of variables differential equations
Separation of variables differential equations Cengage learning heart diagram
Cengage learning heart diagram Cengage
Cengage Cengage
Cengage Cengage
Cengage South-western cengage learning
South-western cengage learning Cengage
Cengage Cengage
Cengage Artist
Artist Cengage learning heart diagram
Cengage learning heart diagram Cengage learning australia
Cengage learning australia Whille
Whille Cengage learning
Cengage learning Module 5 computer concepts exam answers
Module 5 computer concepts exam answers Halpert's dimensions of charisma
Halpert's dimensions of charisma