Chapter 13 MicrobeHuman Interactions Infection Disease and Epidemiology
Chapter 13 Microbe-Human Interactions Infection, Disease, and Epidemiology Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display.
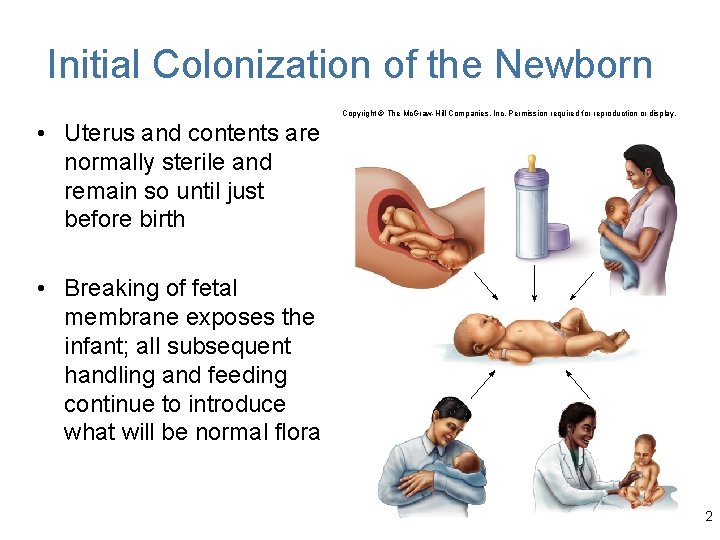
Initial Colonization of the Newborn Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. • Uterus and contents are normally sterile and remain so until just before birth • Breaking of fetal membrane exposes the infant; all subsequent handling and feeding continue to introduce what will be normal flora 2
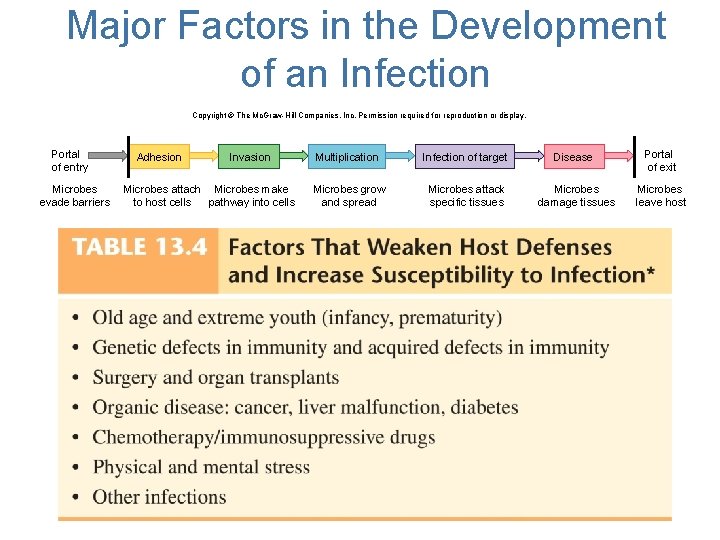
Major Factors in the Development of an Infection Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Portal of entry Microbes evade barriers Adhesion Invasion Microbes attach Microbes make to host cells pathway into cells Multiplication Infection of target Microbes grow and spread Microbes attack specific tissues Disease Microbes damage tissues Portal of exit Microbes leave host 3
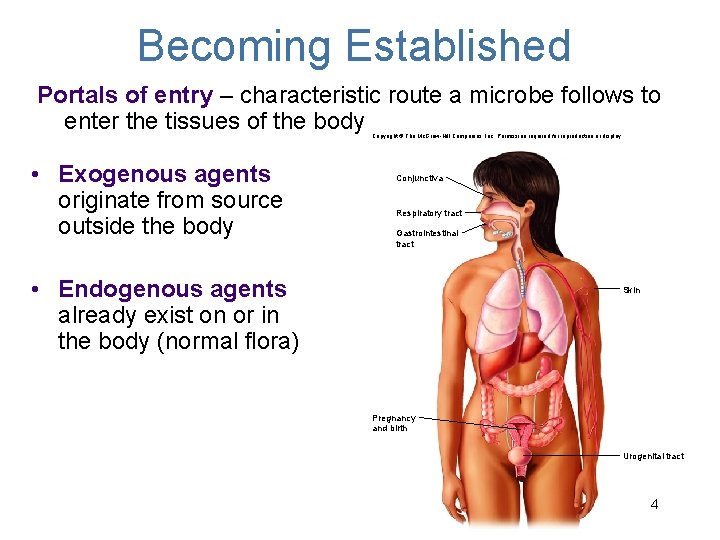
Becoming Established Portals of entry – characteristic route a microbe follows to enter the tissues of the body Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. • Exogenous agents originate from source outside the body Conjunctiva Respiratory tract Gastrointestinal tract • Endogenous agents already exist on or in the body (normal flora) Skin Pregnancy and birth Urogenital tract 4
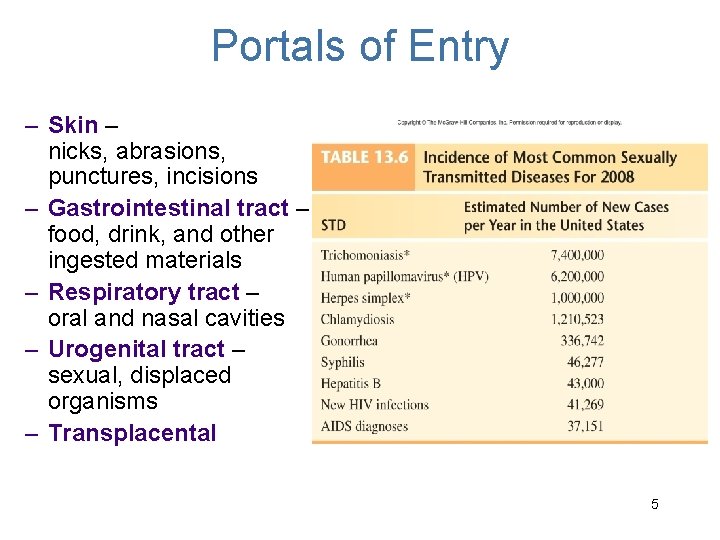
Portals of Entry – Skin – nicks, abrasions, punctures, incisions – Gastrointestinal tract – food, drink, and other ingested materials – Respiratory tract – oral and nasal cavities – Urogenital tract – sexual, displaced organisms – Transplacental 5
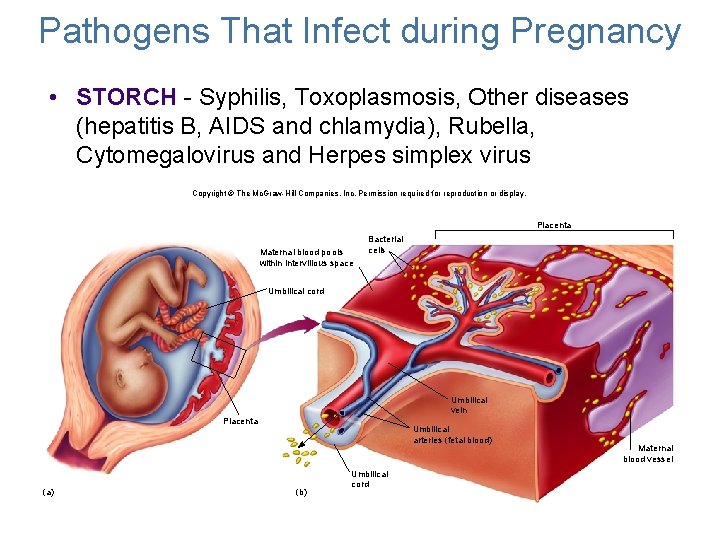
Pathogens That Infect during Pregnancy • STORCH - Syphilis, Toxoplasmosis, Other diseases (hepatitis B, AIDS and chlamydia), Rubella, Cytomegalovirus and Herpes simplex virus Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Placenta Maternal blood pools within intervillous space Bacterial cells Umbilical cord Umbilical vein Placenta (a) Umbilical arteries (fetal blood) (b) Maternal blood vessel Umbilical cord 6
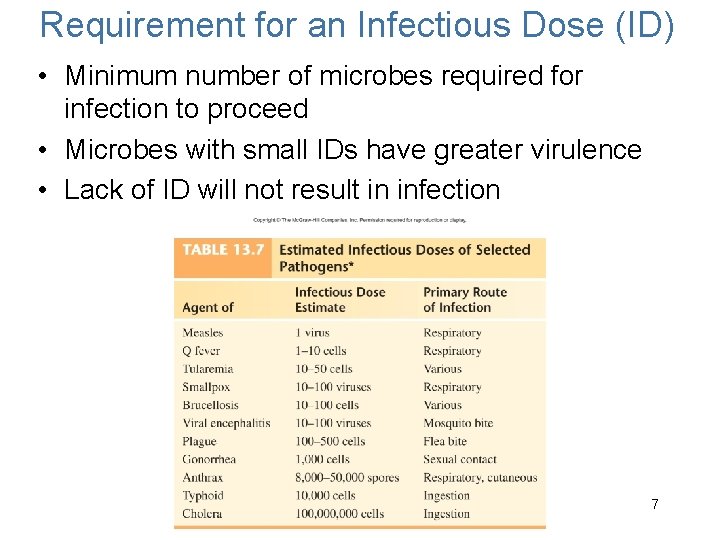
Requirement for an Infectious Dose (ID) • Minimum number of microbes required for infection to proceed • Microbes with small IDs have greater virulence • Lack of ID will not result in infection 7
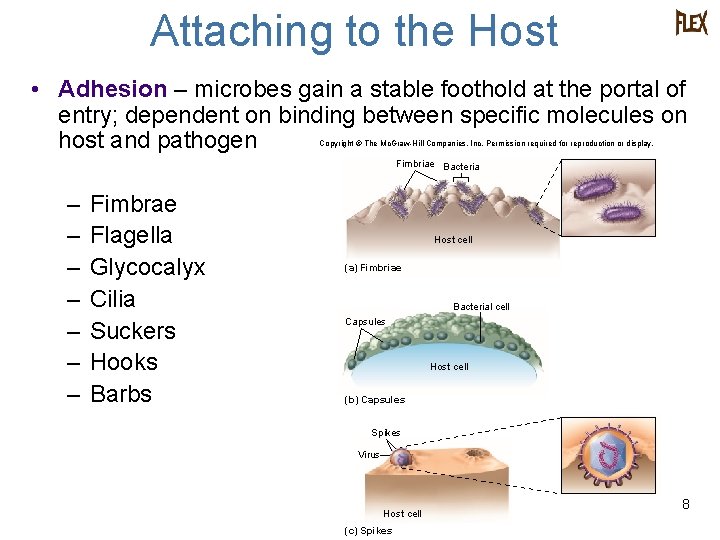
Attaching to the Host • Adhesion – microbes gain a stable foothold at the portal of entry; dependent on binding between specific molecules on host and pathogen Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Fimbriae Bacteria – – – – Fimbrae Flagella Glycocalyx Cilia Suckers Hooks Barbs Host cell (a) Fimbriae Bacterial cell Capsules Host cell (b) Capsules Spikes Virus Host cell (c) Spikes 8
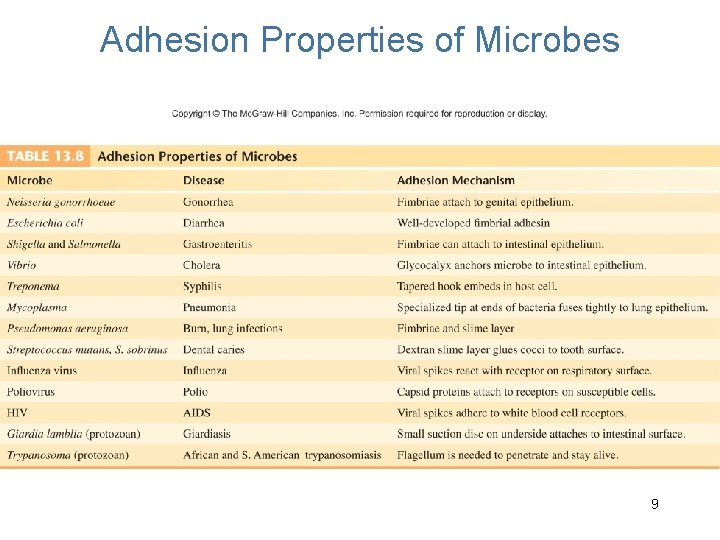
Adhesion Properties of Microbes 9
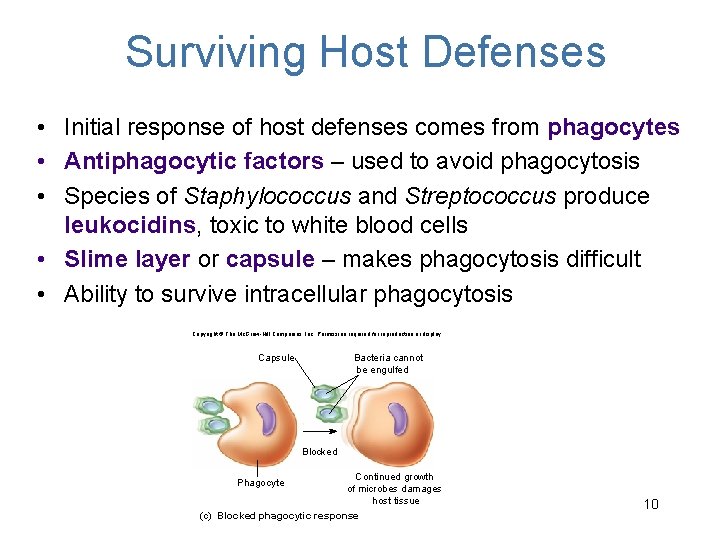
Surviving Host Defenses • Initial response of host defenses comes from phagocytes • Antiphagocytic factors – used to avoid phagocytosis • Species of Staphylococcus and Streptococcus produce leukocidins, toxic to white blood cells • Slime layer or capsule – makes phagocytosis difficult • Ability to survive intracellular phagocytosis Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Capsule Bacteria cannot be engulfed Blocked Continued growth of microbes damages host tissue (c) Blocked phagocytic response Phagocyte 10
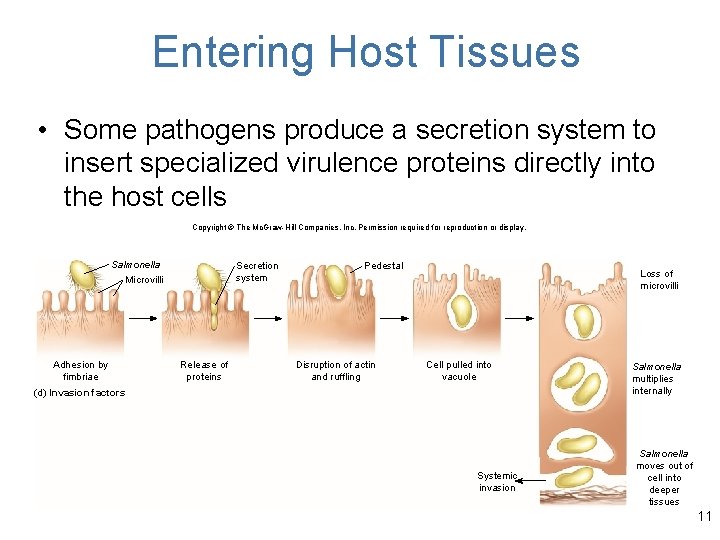
Entering Host Tissues • Some pathogens produce a secretion system to insert specialized virulence proteins directly into the host cells Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Salmonella Secretion system Microvilli Adhesion by fimbriae Release of proteins Pedestal Disruption of actin and ruffling Loss of microvilli Cell pulled into vacuole (d) Invasion factors Systemic invasion Salmonella multiplies internally Salmonella moves out of cell into deeper tissues 11
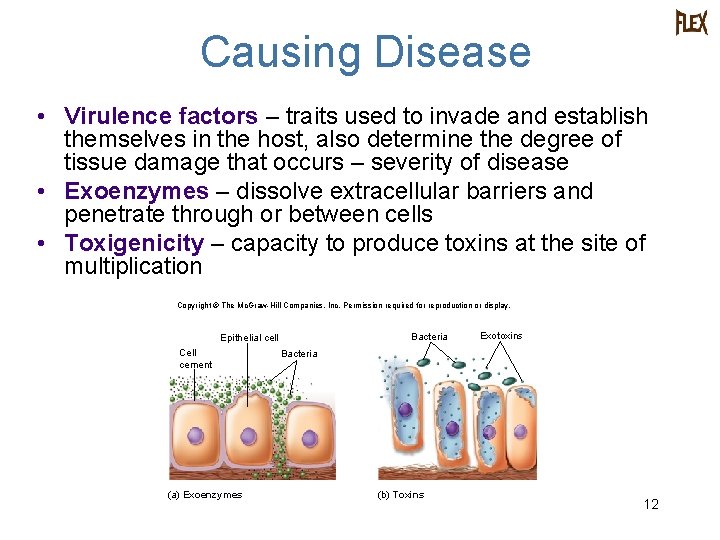
Causing Disease • Virulence factors – traits used to invade and establish themselves in the host, also determine the degree of tissue damage that occurs – severity of disease • Exoenzymes – dissolve extracellular barriers and penetrate through or between cells • Toxigenicity – capacity to produce toxins at the site of multiplication Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Bacteria Epithelial cell Cell cement (a) Exoenzymes Exotoxins Bacteria (b) Toxins 12
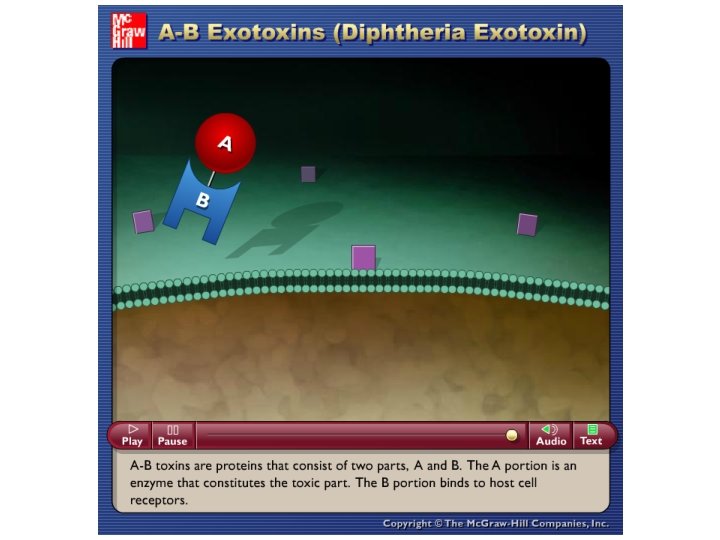
Bacterial Toxins: A Potent Source of Cellular Damage • 2 Types of Bacterial Toxins: – Endotoxin – toxin that is not secreted but is released after the cell is damaged • Composed of lipopolysaccharide (LPS), part of the outer membrane of gram-negative cell walls – Exotoxin – toxin molecule secreted by a living bacterial cell into the infected tissue • Strong specificity for a target cell • Hemolysins • A-B toxins (A-active, B-binding) 13
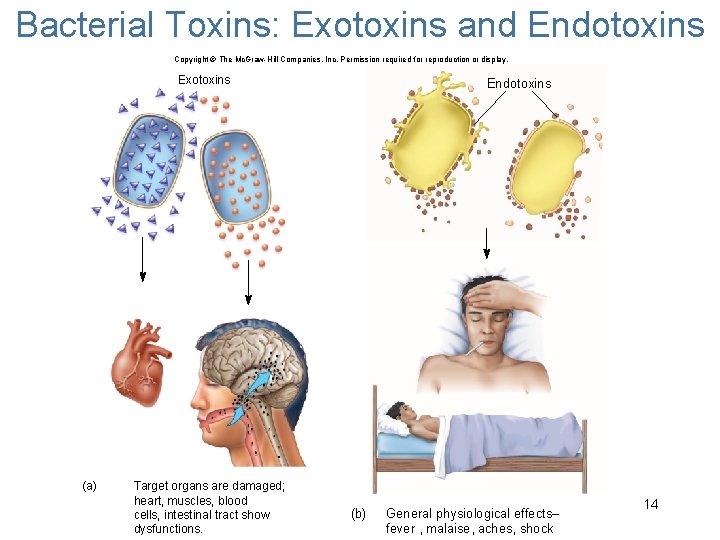
Bacterial Toxins: Exotoxins and Endotoxins Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Exotoxins (a) Target organs are damaged; heart, muscles, blood cells, intestinal tract show dysfunctions. Endotoxins (b) General physiological effects– fever , malaise, aches, shock 14
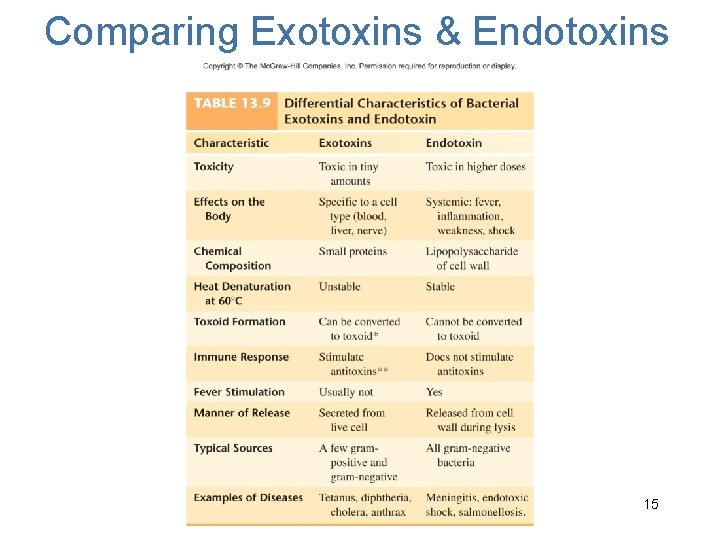
Comparing Exotoxins & Endotoxins 15
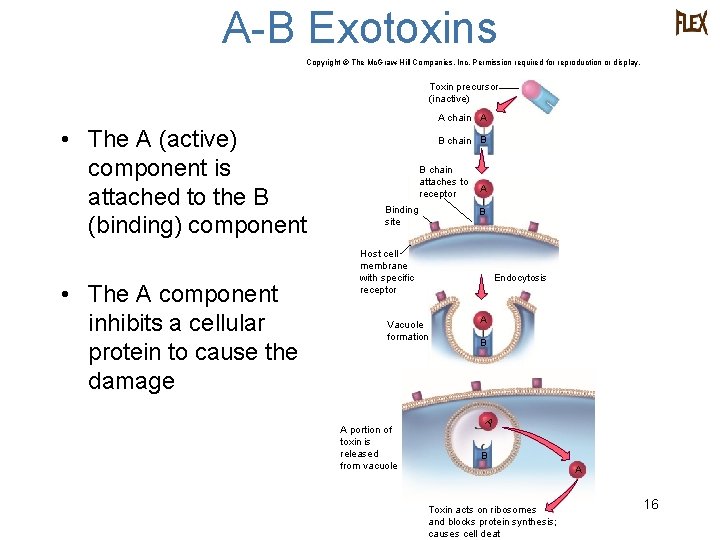
A-B Exotoxins Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Toxin precursor (inactive) A chain A • The A (active) component is attached to the B (binding) component • The A component inhibits a cellular protein to cause the damage B chain B B chain attaches to receptor Binding site A B Host cell membrane with specific receptor Endocytosis Vacuole formation A portion of toxin is released from vacuole A B A Toxin acts on ribosomes and blocks protein synthesis; causes cell deat 16
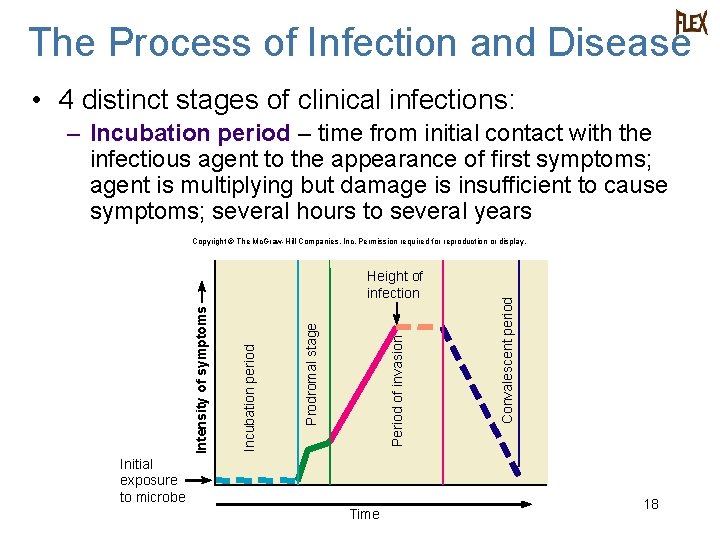
The Process of Infection and Disease • 4 distinct stages of clinical infections: – Incubation period – time from initial contact with the infectious agent to the appearance of first symptoms; agent is multiplying but damage is insufficient to cause symptoms; several hours to several years Period of invasion Prodromal stage Incubation period Intensity of symptoms Height of infection Initial exposure to microbe Time Convalescent period Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. 18
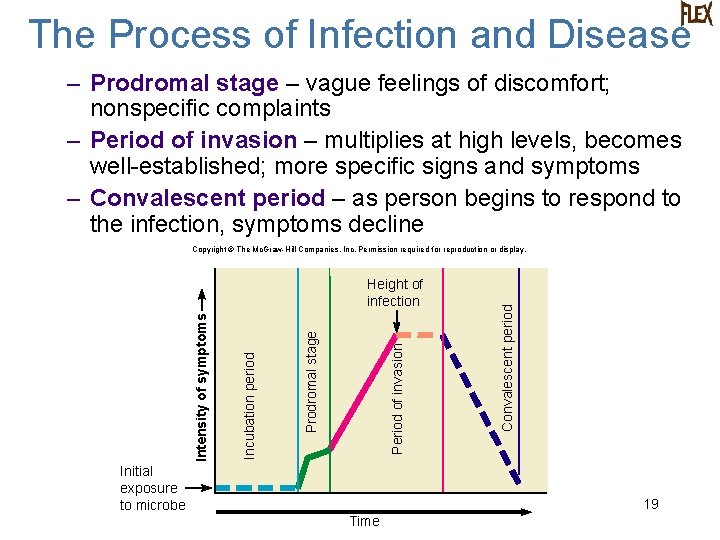
The Process of Infection and Disease – Prodromal stage – vague feelings of discomfort; nonspecific complaints – Period of invasion – multiplies at high levels, becomes well-established; more specific signs and symptoms – Convalescent period – as person begins to respond to the infection, symptoms decline Period of invasion Prodromal stage Incubation period Intensity of symptoms Height of infection Initial exposure to microbe Convalescent period Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. 19 Time

Patterns of Infection • Localized infection – microbes enter the body and remains confined to a specific tissue • Systemic infection – infection spreads to several sites and tissue fluids usually in the bloodstream • Focal infection – when infectious agent breaks loose from a local infection and is carried to other tissues Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Localized infection (boil) Systemic infection (influenza) (c) Focal infection 20 (a) (b)
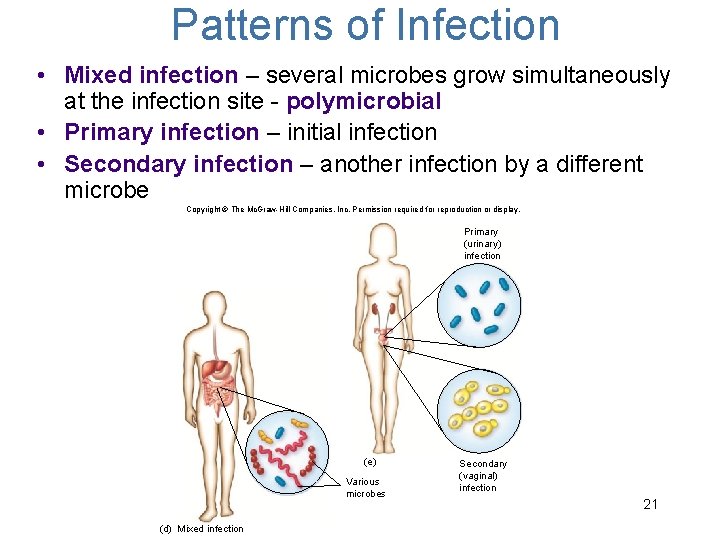
Patterns of Infection • Mixed infection – several microbes grow simultaneously at the infection site - polymicrobial • Primary infection – initial infection • Secondary infection – another infection by a different microbe Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Primary (urinary) infection (e) Various microbes (d) Mixed infection Secondary (vaginal) infection 21
Patterns of Infection • Acute infection – comes on rapidly, with severe but short-lived effects – Common cold- most commonly caused by a rhinovirus • Symptoms begin 2 -3 days after contact • Resolve by ~ 10 days without therapy • http: //www. mayoclinic. com/health/commoncold/DS 00056/DSECTION=symptoms • Chronic infections – progress and persist over a long period of time – Cold sores- Herpes simplex virus- type 2 • Periods of infection and latency • http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0001631 22
Signs and Symptoms of Inflammation • Earliest symptoms of disease as a result of the activation of the body defenses – Fever, pain, soreness, swelling • Signs of inflammation: – Edema – accumulation of fluid – Granulomas and abscesses – walled-off collections of inflammatory cells and microbes – Lymphadenitis – swollen lymph nodes 23

Signs of Infection in the Blood • Changes in the number of circulating white blood cells – Leukocytosis – increase in white blood cells – Leukopenia – decrease in white blood cells – Septicemia – microorganisms are multiplying in the blood and present in large numbers • Bacteremia – small numbers of bacteria present in blood not necessarily multiplying • Viremia – small number of viruses present not necessarily multiplying 24
Infections That Go Unnoticed • Asymptomatic (subclinical) infections – although infected, the host doesn’t show any signs of disease • Inapparent infection, so person doesn’t seek medical attention 25
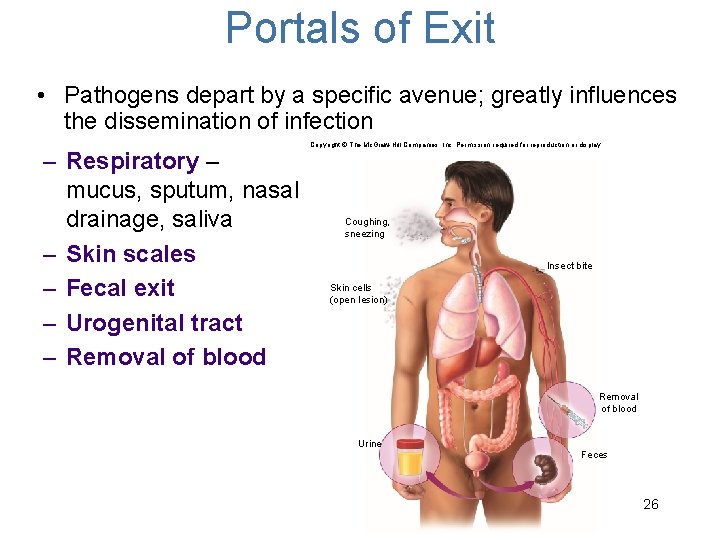
Portals of Exit • Pathogens depart by a specific avenue; greatly influences the dissemination of infection – Respiratory – mucus, sputum, nasal drainage, saliva – Skin scales – Fecal exit – Urogenital tract – Removal of blood Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Coughing, sneezing Insect bite Skin cells (open lesion) Removal of blood Urine Feces 26
Persistence of Microbes and Pathologic Conditions • Apparent recovery of host does not always mean the microbe has been removed • Latency – after the initial symptoms in certain chronic diseases, the microbe can periodically become active and produce a recurrent disease; person may or may not shed it during the latent stage • Chronic carrier – person with a latent infection who sheds the infectious agent • Sequelae – long-term or permanent damage to tissues or organs 27

Sources and Transmission of Microbes • Reservoir – primary habitat of pathogen in the natural world – Human or animal carrier, soil, water, plants • Ex: Influenza virus, the reservoir is birds since they can harbor the virus without showing signs of infection • Source – individual or object from which an infection is actually acquired • Ex: Door knob, roommate, two year old daughter etc. 28

Living Reservoirs • Carrier – an individual who inconspicuously shelters a pathogen and spreads it to others; may or may not have experienced disease due to the microbe • Asymptomatic carrier – shows no symptoms • Passive carrier – contaminated healthcare provider picks up pathogens and transfers them to other patients – Carries the pathogen on their skin or a fomite an inanimate object that can transport a pathogen. Ex: ties, mops, blankets, clothing, stethoscope. Passive (c) Infectious agent Transfer of infectious agent through contact 29
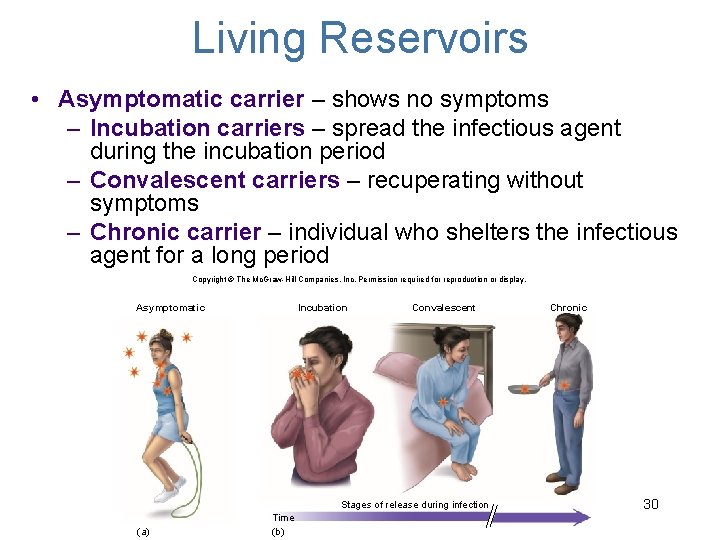
Living Reservoirs • Asymptomatic carrier – shows no symptoms – Incubation carriers – spread the infectious agent during the incubation period – Convalescent carriers – recuperating without symptoms – Chronic carrier – individual who shelters the infectious agent for a long period Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Asymptomatic Incubation Convalescent Stages of release during infection (a) Time (b) Chronic 30
Concept Check: If a nurse transfers a pathogen between patients without becoming infected herself, the nurse as acted as the A. Chronic Carrier B. Convalescent Carrier C. Incubation Carrier D. Asymptomatic Carrier E. Passive Carrier
Acquisition and Transmission of Infectious Agents • Communicable disease – when an infected host can transmit the infectious agent to another host and establish infection in that host • Highly communicable disease is contagious • Non-communicable infectious disease does not arise through transmission from host to host – Occurs primarily when a compromised person is invaded by his or her own normal microflora – Contact with organism in natural, non-living reservoir 32
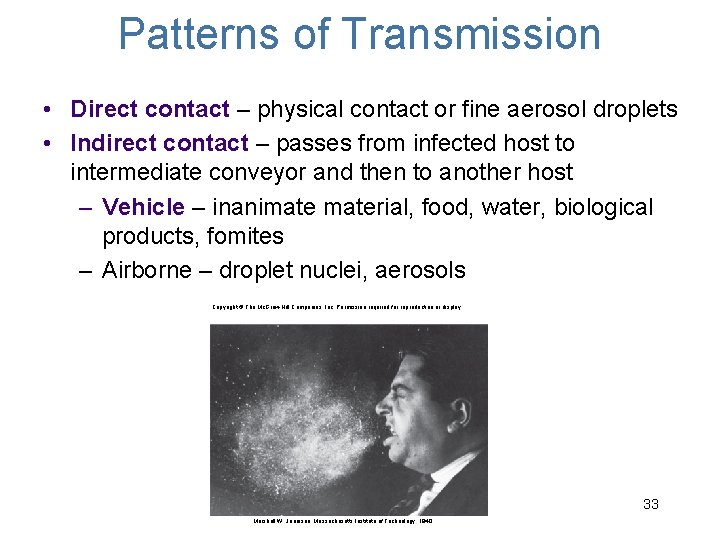
Patterns of Transmission • Direct contact – physical contact or fine aerosol droplets • Indirect contact – passes from infected host to intermediate conveyor and then to another host – Vehicle – inanimaterial, food, water, biological products, fomites – Airborne – droplet nuclei, aerosols Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. 33 Marshall W. Jennison, Massachusetts Institute of Technology, 1940
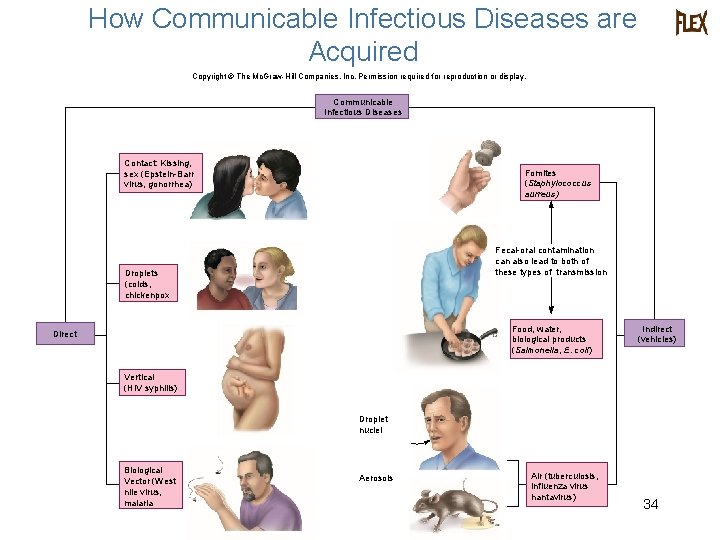
How Communicable Infectious Diseases are Acquired Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Communicable Infectious Diseases Contact: Kissing, sex (Epstein-Barr virus, gonorrhea) Fomites (Staphylococcus aurreus) Fecal-oral contamination can also lead to both of these types of transmission Droplets (colds, chickenpox Food, water, biological products (Salmonella, E. coli) Direct Indirect (vehicles) Vertical (HIV syphilis) Droplet nuclei Biological Vector (West nile virus, malaria Aerosols Air (tuberculosis, influenza virus hantavirus) 34

Nosocomial Infections Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. • Diseases that are acquired or developed during a hospital stay • From surgical procedures, equipment, personnel, and exposure to drugresistant microorganisms • 2 to 4 million cases/year in U. S. with approximately 90, 000 deaths Enterococci Enterobacter spp. Coagulase-negative staphylococci Pseudomonas aeruginosa Staphylococcus aureus S. aureus Coagulase-negative staphylococci E. coli Candida spp. Blood 6% Candida spp. Enterobacter spp. Skin 8% P. aeruginosa Enterococci E. coli P. aeruginosa Other 12% Coagulase-negative staphylococci Enterobacter spp. Urinary tract 39% Surgical wounds 17% Lower respiratory tract 18% Enterococci E. coli P. aeruginosa S. aureus Acinetobacter spp. S. aureus P. aeruginosa Enterobacter spp. Klebsiella pneumoniae 35
Frequency of Cases • Prevalence – total number of existing cases with respect to the entire population usually represented by a percentage of the population • Incidence – measures the number of new cases over a certain time period, as compared with the general healthy population • Mortality rate – the total number of deaths in a population due to a certain disease • Morbidity rate – number of people afflicted with a certain disease 36
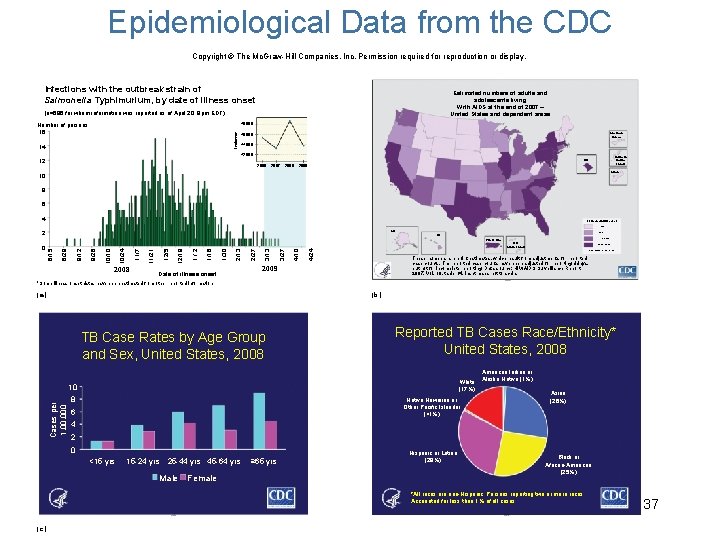
Epidemiological Data from the CDC Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Infections with the outbreak strain of Salmonella Typhimurium, by date of illness onset Estimated numbers of adults and adolescents living With AIDS at the end of 2007 – United States and dependent areas (n=696 for whom information was reported as of April 20, 9 pm EDT) Number of persons 16 Incidence 48, 000 14 Illness that began during this time may not yet be reported 46, 000 44, 000 American Samoa 42, 000 12 Northern Marina Islands DC 2006 2007 2008 2009 Guam 10 8 6 4 Estimated AIDS cases 1 - 1207 AK 2 1208 - 3333 HI 2008 Date of illness onset 4/24 4/10 3/27 3/13 2/27 2/13 1/30 1/2 1/16 12/19 12/5 11/21 11/7 10/24 10/10 9/26 9/12 8/29 0 8/15 Puerto Rico 3334 - 8855 U. S. Virgin Islands 8856 - 75146 Data classed using quartiles These numbers are point estimates, which result from adjustments for reported case counts. The reported case counts have been adjusted for reporting delays, but not for incomplete reporting. Data source: HIV/AIDS Surveillance Report, 2007. Vol. 19, table 14. Inset maps not to scale. 2009 *Some illness onset dates have been estimated from other reported information (a) (b) TB Case Rates by Age Group and Sex, United States, 2008 Reported TB Cases Race/Ethnicity* United States, 2008 White (17%) Cases per 1, 000 10 8 Native Hawaiian or Other Pacific Islander (<1%) 6 American Indian or Alaska Native (1%) Asian (26%) 4 2 0 <15 yrs 15 -24 yrs 25 -44 yrs 45 -64 yrs Male Female ≥ 65 yrs Hispanic or Latino (29%) Black or African-American (25%) *All races are non-Hispanic. Persons reporting two or more races Accounted for less than 1% of all cases (c) 37

Patterns of Infectious Disease Occurrence Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Outbreaks • Endemic – disease that exhibits a relatively steady frequency over a long period of time in a particular geographic locale (a) Endemic Occurrence (Valley fever) • Sporadic – when occasional cases are reported at irregular intervals 38 (b) Sporadic Occurrence (Measles)

Patterns of Infectious Disease Occurrence Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. • Epidemic – when prevalence of a disease is increasing beyond what is expected (c) Epidemic Occurrence (Syphilis) • Pandemic – epidemic across continents (d) Pandemic Occurrence (AIDS) 39
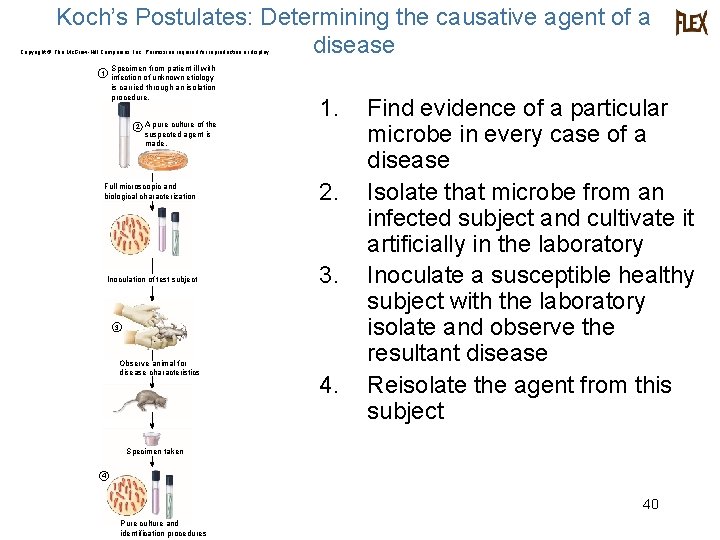
Koch’s Postulates: Determining the causative agent of a disease Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. 1 Specimen from patient ill with infection of unknown etiology is carried through an isolation procedure. 2 A pure culture of the 1. suspected agent is made. Full microscopic and biological characterization Inoculation of test subject 2. 3. 3 Observe animal for disease characteristics 4. Find evidence of a particular microbe in every case of a disease Isolate that microbe from an infected subject and cultivate it artificially in the laboratory Inoculate a susceptible healthy subject with the laboratory isolate and observe the resultant disease Reisolate the agent from this subject Specimen taken 4 40 Pure culture and identification procedures
Concept Check: The occurrence of Lyme disease mainly in areas where certain species of ticks live would define it as a/an ____ disease. A. Epidemic B. Endemic C. Sporadic D. Pandemic
- Slides: 41