Chapter 13 Intravenous Infusion Transfusion Section Two Intravenous
- Slides: 78
Chapter 13 Intravenous Infusion & Transfusion
Section Two Intravenous Transfusion • Definition: Intravenous transfusion is the intravenous administration of whole blood or a blood component such as plasma, packed red cells, white blood cells, or platelets.
Transfusion Blood transfusion requires the nurse to • follow a specific procedure to match the blood accurately • identify the blood for the individual and recipient correctly • monitor the patient throughout the procedure for transfusion reactions The nurse is responsible for assessment before, during, and after transfusion and for regulation of transfusion.
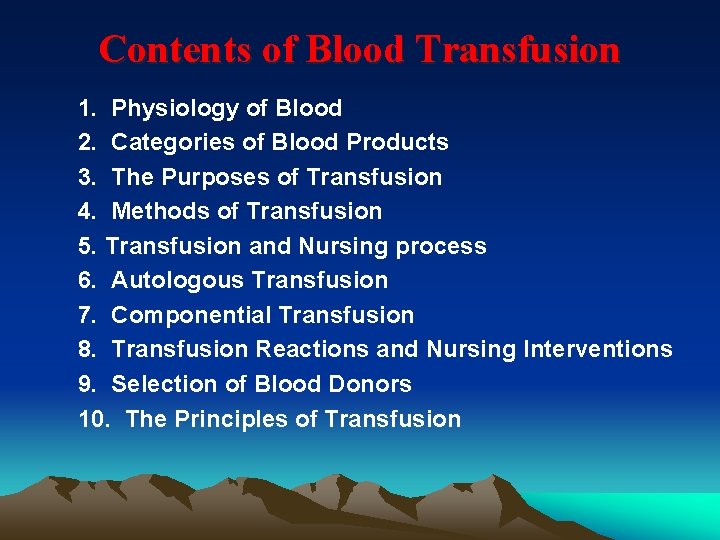
Contents of Blood Transfusion 1. Physiology of Blood 2. Categories of Blood Products 3. The Purposes of Transfusion 4. Methods of Transfusion 5. Transfusion and Nursing process 6. Autologous Transfusion 7. Componential Transfusion 8. Transfusion Reactions and Nursing Interventions 9. Selection of Blood Donors 10. The Principles of Transfusion
1. Physiology of Blood • Blood Groups and Types • Blood Typing and Cross-matching Test
Blood Groups and Types • Blood groups are named by types of the proteins as antigens on the surface of an individual’s red blood cells. Ø ABO Blood Groups System Ø Rhesus ( Rh ) Blood Group System
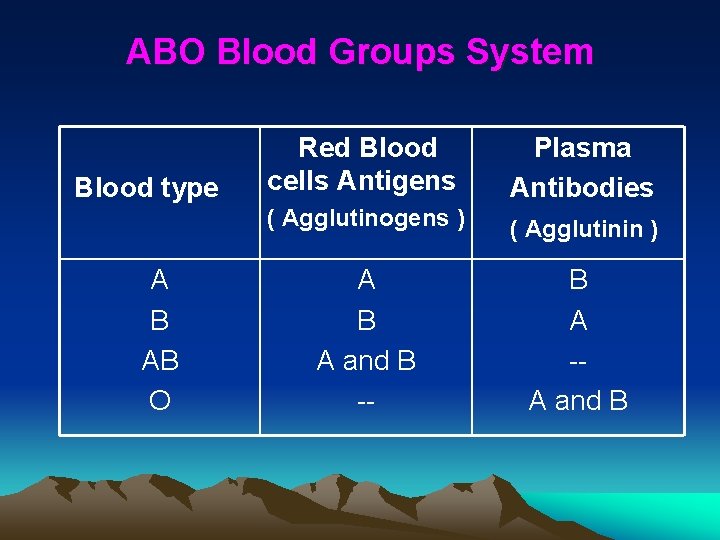
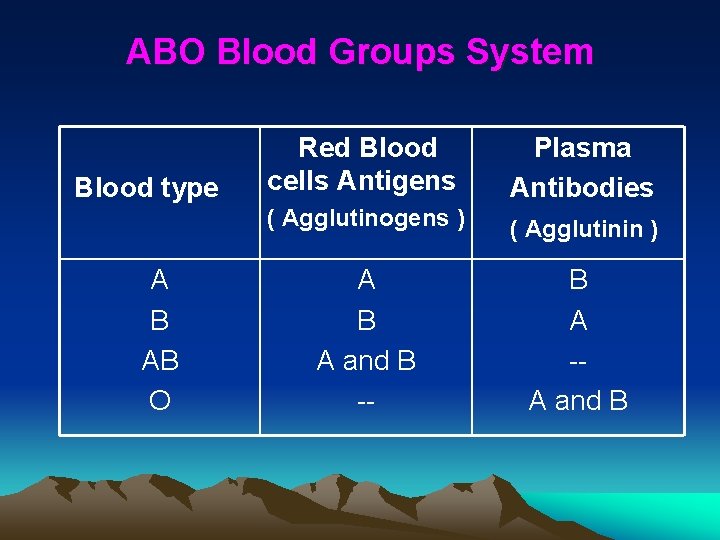
ABO Blood Groups System Blood type A B AB O Red Blood cells Antigens Plasma Antibodies ( Agglutinogens ) ( Agglutinin ) A B A and B -- B A -A and B
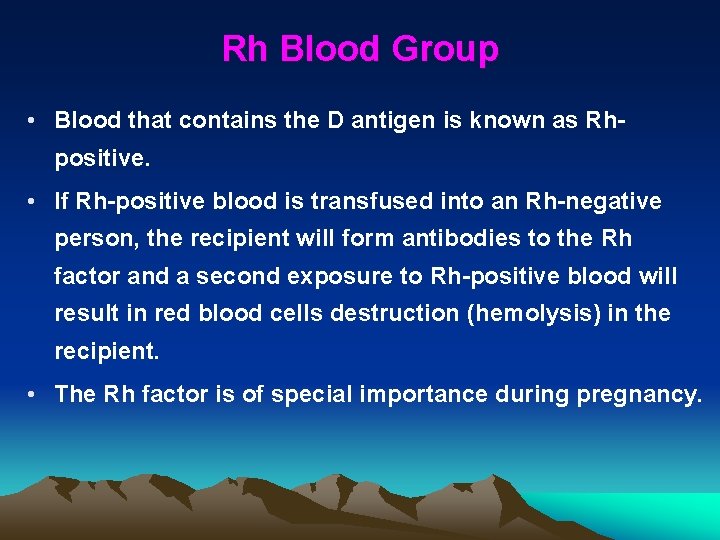
Rh Blood Group • Blood that contains the D antigen is known as Rhpositive. • If Rh-positive blood is transfused into an Rh-negative person, the recipient will form antibodies to the Rh factor and a second exposure to Rh-positive blood will result in red blood cells destruction (hemolysis) in the recipient. • The Rh factor is of special importance during pregnancy.
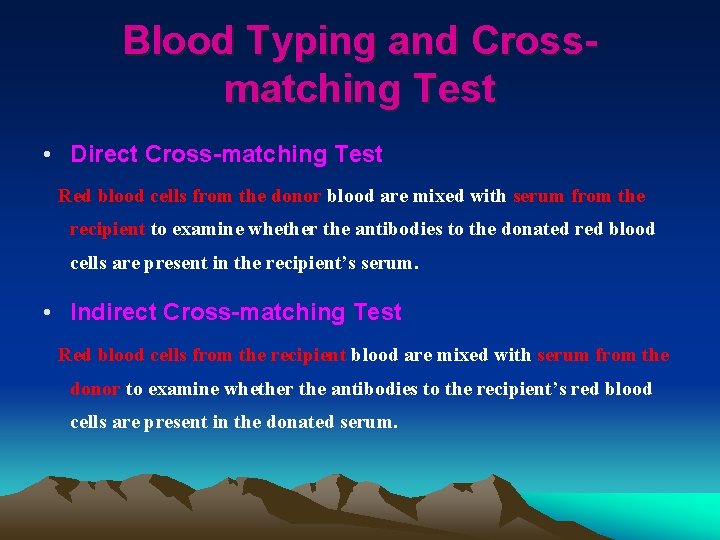
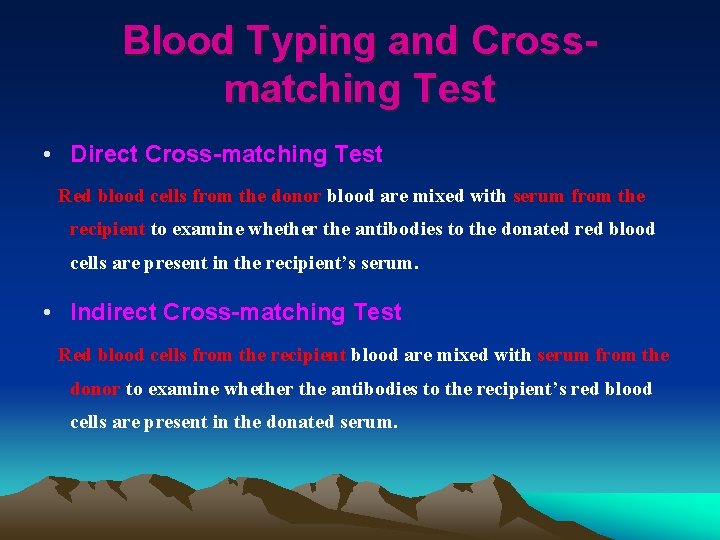
Blood Typing and Crossmatching Test • Direct Cross-matching Test Red blood cells from the donor blood are mixed with serum from the recipient to examine whether the antibodies to the donated red blood cells are present in the recipient’s serum. • Indirect Cross-matching Test Red blood cells from the recipient blood are mixed with serum from the donor to examine whether the antibodies to the recipient’s red blood cells are present in the donated serum.
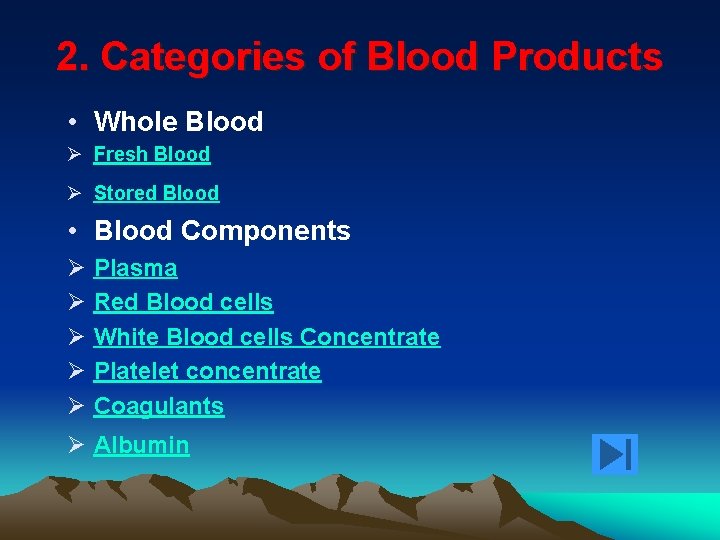
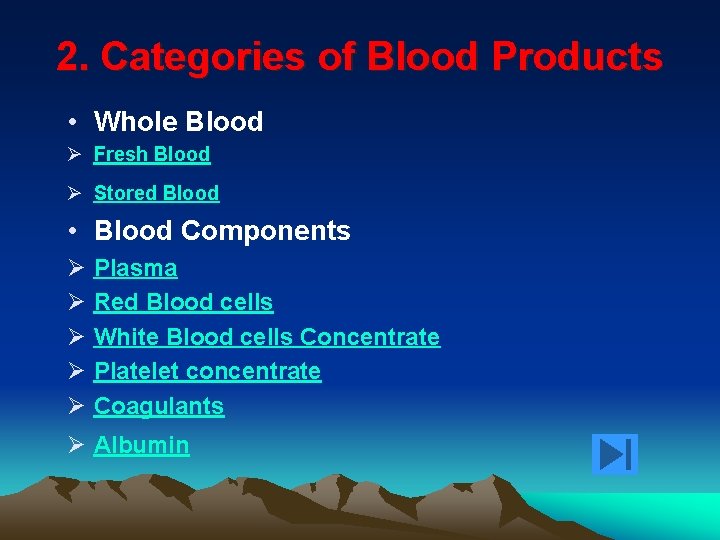
2. Categories of Blood Products • Whole Blood Ø Fresh Blood Ø Stored Blood • Blood Components Ø Ø Ø Plasma Red Blood cells White Blood cells Concentrate Platelet concentrate Coagulants Ø Albumin
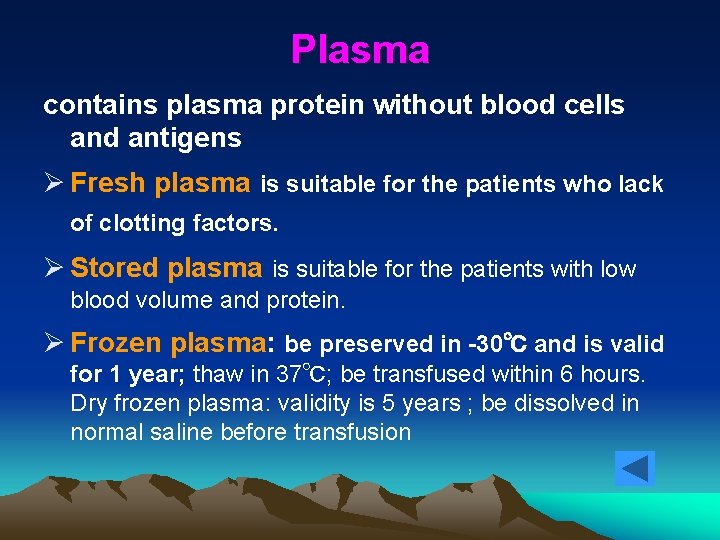
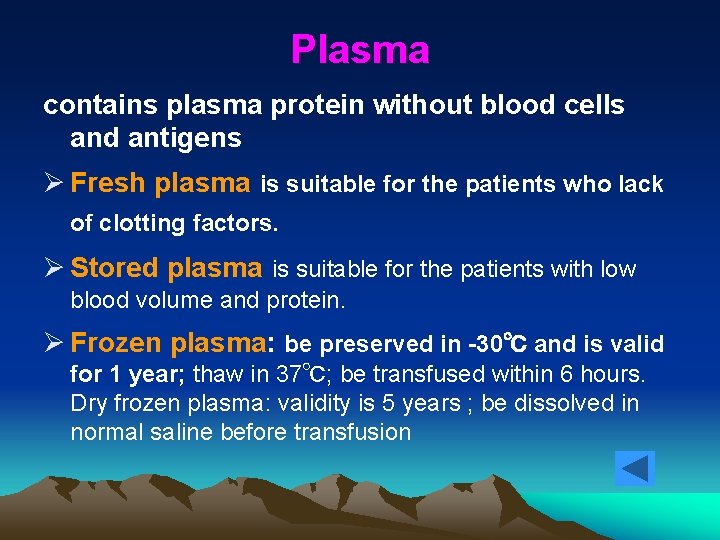
Plasma contains plasma protein without blood cells and antigens Ø Fresh plasma is suitable for the patients who lack of clotting factors. Ø Stored plasma is suitable for the patients with low blood volume and protein. Ø Frozen plasma: be preserved in -30℃ and is valid for 1 year; thaw in 37℃; be transfused within 6 hours. Dry frozen plasma: validity is 5 years ; be dissolved in normal saline before transfusion
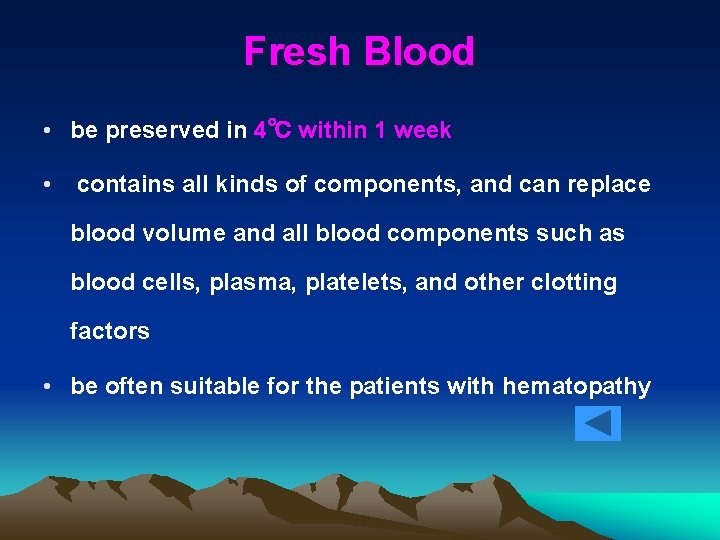
Fresh Blood • be preserved in 4℃ within 1 week • contains all kinds of components, and can replace blood volume and all blood components such as blood cells, plasma, platelets, and other clotting factors • be often suitable for the patients with hematopathy
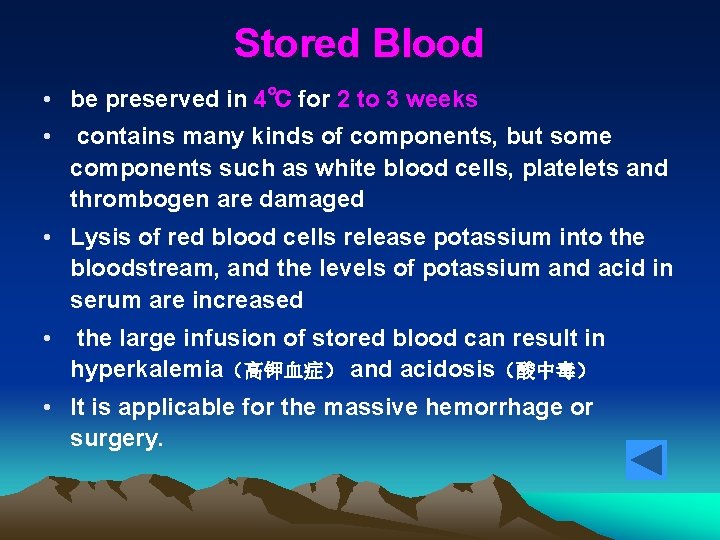
Stored Blood • be preserved in 4℃ for 2 to 3 weeks • contains many kinds of components, but some components such as white blood cells, platelets and thrombogen are damaged • Lysis of red blood cells release potassium into the bloodstream, and the levels of potassium and acid in serum are increased • the large infusion of stored blood can result in hyperkalemia(高钾血症) and acidosis(酸中毒) • It is applicable for the massive hemorrhage or surgery.
Red Blood cells • to increase the oxygen carrying capacity of blood in the patients with anemia, less surgical bleeding or disorders with less bleeding and replenish red blood cells in cardiovascular failure for avoiding cardiovascular overload • one unit is 100 ml of red blood cells, and can raise hematocrit by approximately 4%
Red Blood cells • Red Blood cells Concentrate: to increase the oxygen carrying capacity of blood in the patients with anemia and normal blood volume • Washed Red Blood cells: for the patients after organ transplantation or the patients with immunological haemolytic anemia • Red Blood cells suspension: for battleground first aid; middle or small operations
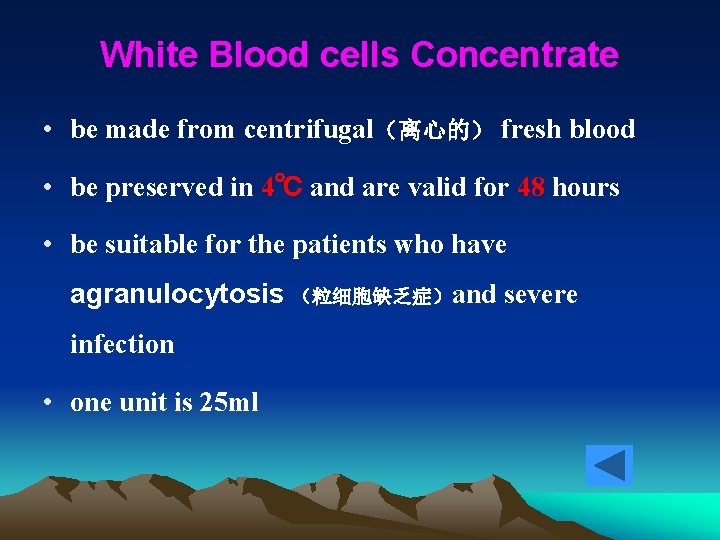
White Blood cells Concentrate • be made from centrifugal(离心的) fresh blood • be preserved in 4℃ and are valid for 48 hours • be suitable for the patients who have agranulocytosis (粒细胞缺乏症)and severe infection • one unit is 25 ml
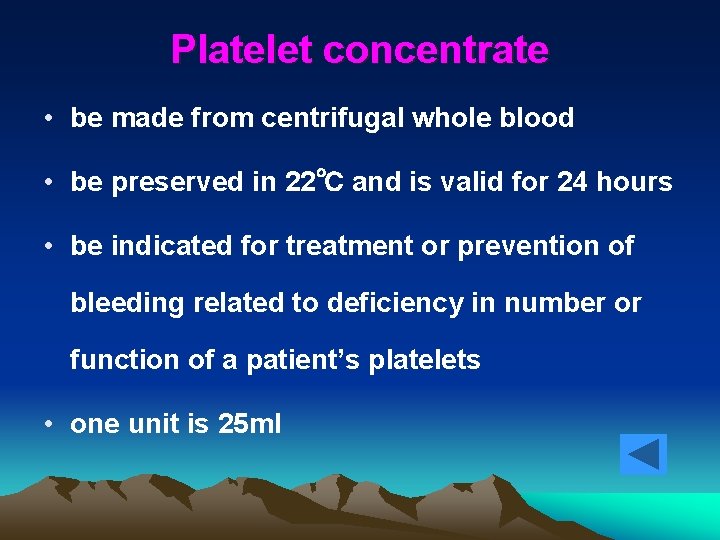
Platelet concentrate • be made from centrifugal whole blood • be preserved in 22℃ and is valid for 24 hours • be indicated for treatment or prevention of bleeding related to deficiency in number or function of a patient’s platelets • one unit is 25 ml
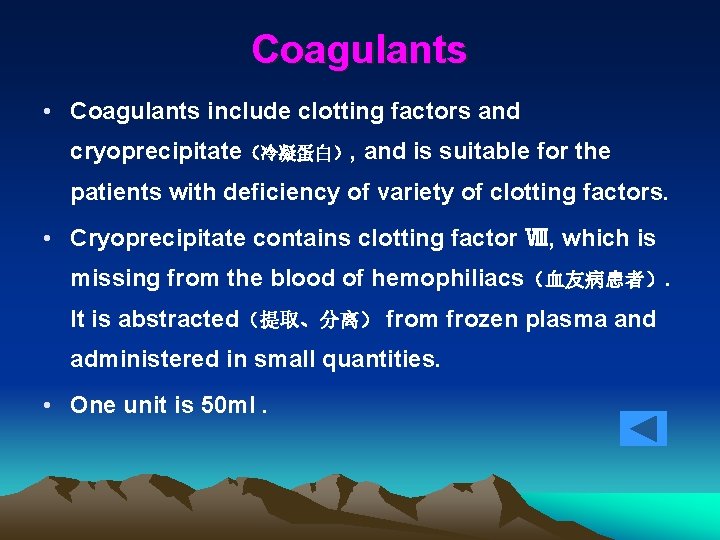
Coagulants • Coagulants include clotting factors and cryoprecipitate(冷凝蛋白), and is suitable for the patients with deficiency of variety of clotting factors. • Cryoprecipitate contains clotting factor Ⅷ, which is missing from the blood of hemophiliacs(血友病患者). It is abstracted(提取、分离) from frozen plasma and administered in small quantities. • One unit is 50 ml.
Albumin • It is transfused to increase blood volume and provide plasma proteins for the patients with low blood proteins.
3. The Purposes of Blood Transfusion • To supply and restore the blood volume. • To correct anemia, maintain hemoglobin level and the oxygen carrying capacity of red blood cells. • To supply plasma protein to increase the plasma protein and maintain the colloid osmotic pressure. • To supply clotting factors and platelets to prevent or treat hemorrhagic disease. • To supply antibodies and alexin(补体) to resist the infection. • To remove deleterious substances from blood.
The Indications of Blood Transfusion • Hemorrhage • Anemia or hypoproteinemia(低蛋白血症) • Serious infection • Disturbances of blood coagulation
The Contraindications of Blood Transfusion • Acute pulmonary edema • Congestive heart failure • Pulmonary embolism • Malignant hypertension • Hypercythemia(红细胞过多症) • Serious renal failure • Serious allergy to blood transfusion
4. Methods of Blood Transfusion • Direct Venous Blood Transfusion: The blood which is collected from a donors is infused into the recipient immediately. • Indirect Venous Blood Transfusion: The collected blood is infused into the patient as well as the method of intravenous infusion. • Arterial Blood Transfusion: be appropriate for the patients with serious hemorrhagic shock or first aid resuscitation.
5. Preparations for Transfusion • Prepare the Blood: specimen; fill in the blank of the transfusion form ; send them to the blood bank. —for blood type examination and cross-matching test • Obtaining the Blood Ø Three checks include: The expiry date of the blood is not beyond. The pack is intact and without any leaking. The quality of the blood. Ø Eight rights include: the patient’s name, the bed number, inpatient number, the number of the blood bag label, the ABO groups and Rh type on the blood bag label, the result of cross-matching, the category and the amount of the blood.
Preparations for Transfusion • After Obtaining the Blood Ø The blood should not be shaken to avoid red blood cells being damaged Ø make sure that the stored blood is kept in room temperature for 15 to 20 minutes before transfusion Ø The blood must not be warmed to avoid the reactions caused by solidified and denatured plasma albumin.
Preparations for Transfusion • Recheck the Blood: check the blood and the laboratory report with another nurse, validate the collect blood, and inspect blood for clots before starting blood transfusion. • Check Consent Form: The patient should understand agree to receive the blood transfusion, and be asked to sign consent form before blood transfusion.
5 -1. Indirect Venous Blood Transfusion • Preparation before Implementation • Procedure • Cautions
Preparation • Assessment • Preparation of the patient • Preparation of the nurse • Equipment preparation • Environment preparation
Assessment • History: clinical condition, treatment and transfusion history ; gender of the patient, medical diagnosis, place and reason for the blood transfusion, the amount and type of the blood or blood components required, the history of the transfusion reactions • Physical Examination: temperature, pulse, respiration and blood pressure; skin and blood vessels for the paracentesis • Psychological status and the knowledge about transfusion
Preparation of the patient • Education: The patient can tell the knowledge related to transfusion, and identify the reactions related to transfusion. • Sign Consent Form. • Ask the patient to void. Position the patient for comfort and optimal visibility for skill performance.
Preparation of the nurse Wear working clothes prune nails wash hands wear mask.
Equipment preparation Medical tray: transfusion sheet transfusion set antiseptic solution Sterile swabs tourniquet infusion pad adhesive tape 250 ml normal saline blood unit ( packed blood ) Kidney-shaped tray
Environment preparation • cleanness; • commodiousness ; • brightness
Procedures and key points 1. Wash hands, wear a mask, and carry the equipment to bedside 2. Recheck the physician’s order for number and type of transfusion unit and the patient’s name and bed number. 3. Explain procedures to the patient, instruct the patient to identify transfusion reactions.
4. Perform venipuncture on a suitable vein use transfusion set connecting with 0. 9% normal saline. 5. Gently agitate and suspend blood bag. 6. Complete the transfusion, infuse NS to clear the tubing, then remove the needle. 7. Wash hands. 8. Record administration of transfusion.
Cautions 1. Comply with the principles of surgical asepsis and transfusion procedure;check the blood with another registered nurse and make sure it correct before transfusion 2. perform the intravenous infusion before transfusion, and choose the sterile blood administration set with in-line filter, and prime it with 0. 9% normal saline 3. Drugs such as ( hyperosmolar or hypoosmolar solutions, medications or other additives ) must not be added to blood under any circumstances.
4. During transfusion the patient is at risk for a reaction, particularly during the first 15 minutes. --observe the vital signs and skin color--detect the early warning symptom and signs of reactions, and provide the intervention. 5. Most adults can tolerate receiving one unit of blood in 1. 5 to 2 hours. Transfusion rate should be slow properly for elders, serious anemia patients, and heart function failure patients. 6. The empty blood bag should be preserved for 24 hours after transfusion in order to analyse the transfusion reaction reasons when it occurs.
5 -2. Direct Venous Blood Transfusion Equipment Medical Tray: 50 ml syringes 3. 8% sodium citrate solution sphygmomanometer antiseptic solution sterile swabs adhesive tape sterile dressing
Procedures and key points 1. Explain the procedures to the donor and recipient ----making the patient and the donor understand the procedure and cooperate with it 2. Wash hands and wear mask, put anticoagulant in the syringes ----adding 5 ml of 3. 8% sodium citrate solution into 50 ml of blood 3. The donor and patient lie on bed and show one arm respectively 4. Check the name, the result of blood typing and crossmatching between the donor and the recipient ----preventing the mistake
5. The sphygmomanometer is tangled on the arm and pressured by air. The nurse should choose the large vena, clear the skin over insertion site with antiseptic swabs, perform venipuncture to collect the blood, and infuse blood to the recipient by intravenous injection ----the pressure is maintained 100 mm. Hg 6. Cooperate with three nurses, the first nurse is responsible for collecting the blood, the second nurse is for transferring and the third nurse is for infusion
7. When transfusion is completed, remove the needle and press the venipuncture site 8. Disinfect and clean the equipment, and record administration of blood transfusion ----record the time and amount of blood transfusion and reaction
6. Autologous Transfusion Definition: Autologous transfusion also be called autotransfusion, is the collection and reinfusion of a patient’s own blood. Advantages: be safer for the patient ---- decrease the risk of complications such as mismatched blood exposure to blood-borne infectious agents save time---needn’t to type and cross-match the blood
6. Autologous Transfusion There are three approaches of autologous blood: Ø Preoperative autologous Blood Storage Ø Perioperative Hemodilution Ø Intraoperative Lost Blood
Preoperative autologous Blood Storage • 1 to 5 units of patient’s own blood be prestored before operation depending on the type of surgery and the ability of the patient to maintain an acceptable hematocrit • blood be drew from a patient usually starting 3 to 5 weeks before an elective surgical procedure • The blood should be collected once a week or two weeks until 3 days before surgery. • It is helpful for the patient to withstand the blood loss that occurs with the collection, and return to normal level of plasma albumin.
Perioperative Hemodilution • Blood is collected at the date of surgery ( most often prior to surgery ). The fluid volume lost is replaced with intravenous crystal solution or colloid solution. • Blood loss in surgery thus occurs at a lower hematocrit -- the amount of red blood cells and other blood components lost during the entire procedure may be reduced. • Finally, collected blood is returned to the patient after the surgical procedure.
Intraoperative Lost Blood • The lost blood is salvaged from the surgical field for reinfusion during or after the surgical procedure. • For the patients with rupture of spleen or fallopian-tube, if the bleeding in abdominal cavity is not contaminated and coagulated within 6 hours, the blood can usually be collected. • Then, the filtered blood is returned to the patient after anticoagulation is added in.
7. Componential Transfusion Advantages: Ø Economic: allows several patients to benefit from one unit of donated whole blood, appropriate component is usually transfused for the patients who are lack of the component in blood Ø be helpful to reduce the blood transfusion reaction
7. Componential Transfusion • principles 1. During the transfusion of blood components, the patients may receive the blood components from several donors, so it is necessary to administer medication ( antihistamines 抗组胺药 ) as ordered to prevent the anaphylactic reactions. 2. It is necessary for the patient to be tested blood typing and cross-matching before red blood cells is transfused.
7. Componential Transfusion 3. Some of blood component, such as white blood cells, platelet concentrate, are living for a short time, so it is necessary to transfuse blood components completely within term of validity by special blood administration set. 4. Blood components should be first transfused to provide the fresh components if the patients need both whole blood and blood components.
8. Transfusion Reactions and Nursing Interventions • Fever Reaction • Anaphylactic Transfusion Reactions • Hemolytic Reaction • The reaction Related to Large Volume of Blood Transfusion • Other Reactions
Fever Reaction • Causes Ø The blood, blood bag or blood administration set is contaminated by bacteria. Ø The principles of surgical asepsis are violated during blood transfusion. Ø Antibodies in recipient’s blood react to antigens on donor’s white blood cells, platelets, or plasma proteins, especially with multiple transfusions.
Fever Reaction • Clinical Manifestations Ø After first 30 minutes to 6 hours after the transfusion, the patient may have chills and fever suddenly ( the temperature can range from 38℃ to 40℃ ), flushing, headache, anxiety, nausea, vomiting, muscle pain. Ø The mild reaction may be relieved within 1 to 2 hours, and the temperature drops to the normal level gradually.
Fever Reaction • Preventing Intervention Ø remove the factors causing fever Ø follow the principles of surgical asepsis during blood transfusion Ø choose disposable blood administration set
Fever Reaction • Nursing Intervention Ø Transfusion should be administered slowly if mild reaction occurs. Ø Stop transfusion immediately and send the blood bag and blood administration set to the laboratory if severe reaction occurs. Ø Monitor the vital signs. Ø Provide cold therapy if the patient has hyperthermia. Ø Administer antipyretics as ordered.
Anaphylactic Transfusion Reactions • Causes Ø The patient has anaphylactic predisposition(过敏体质). Ø There are substances causing anaphylaxis in donor’s blood. Ø After the patient received several blood transfusion, the allergic antibody is produced in patient’s plasma. When blood transfusion is performed again, the antibody-antigen reaction cause anaphylaxis. Ø The allergic antibodies(变应性抗体) in donor’s blood is infused into the patient. The anaphylaxis may occur if the antibody reacts to corresponding antigen.
Anaphylactic Transfusion Reactions • Clinical Manifestations Ø In mild anaphylaxis After blood transfusion, the patient may feel skin itching, and covered with urticaria. (荨麻疹) Ø In middle anaphylaxis The patient may have vascular and neuropathic edema, normally appear in face. The patient may have palpebra(眼睑), or lip edema. The laryngeal edema also may occur. The patient may have dyspnea, bronchial spasm(支气管痉挛), or chest pain. The wheezing sounds(哮鸣音) are found when lungs auscultated. Ø In serious anaphylaxis The patient may suffer from anaphylaxis shock.
Anaphylactic Transfusion Reactions • Preventing Intervention Ø Administer blood or blood products correctly. Ø Choose blood donor without allergy history. Ø Blood donor should be fasting for 4 hours before blood donation. Ø The patient having history of allergy should be given antihistamines(抗组胺药) as ordered before transfusion.
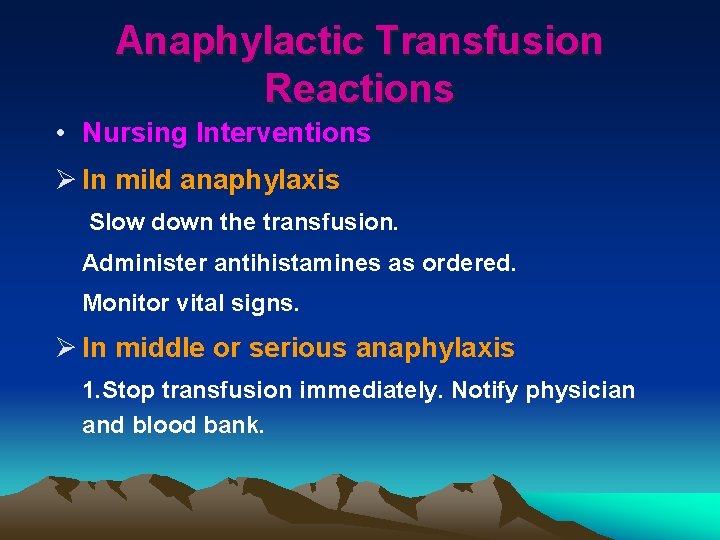
Anaphylactic Transfusion Reactions • Nursing Interventions Ø In mild anaphylaxis Slow down the transfusion. Administer antihistamines as ordered. Monitor vital signs. Ø In middle or serious anaphylaxis 1. Stop transfusion immediately. Notify physician and blood bank.
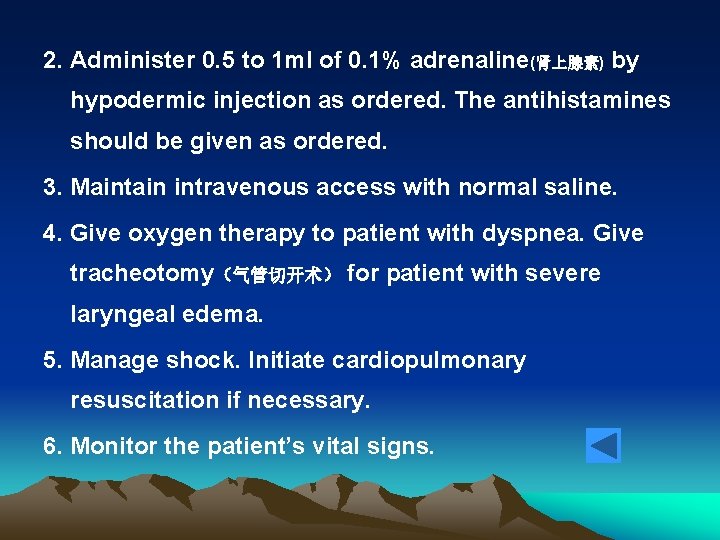
2. Administer 0. 5 to 1 ml of 0. 1% adrenaline(肾上腺素) by hypodermic injection as ordered. The antihistamines should be given as ordered. 3. Maintain intravenous access with normal saline. 4. Give oxygen therapy to patient with dyspnea. Give tracheotomy(气管切开术) for patient with severe laryngeal edema. 5. Manage shock. Initiate cardiopulmonary resuscitation if necessary. 6. Monitor the patient’s vital signs.
Haemolytic Reaction • Intravascular Haemolytic reaction • Extravascular Haemolytic Reaction
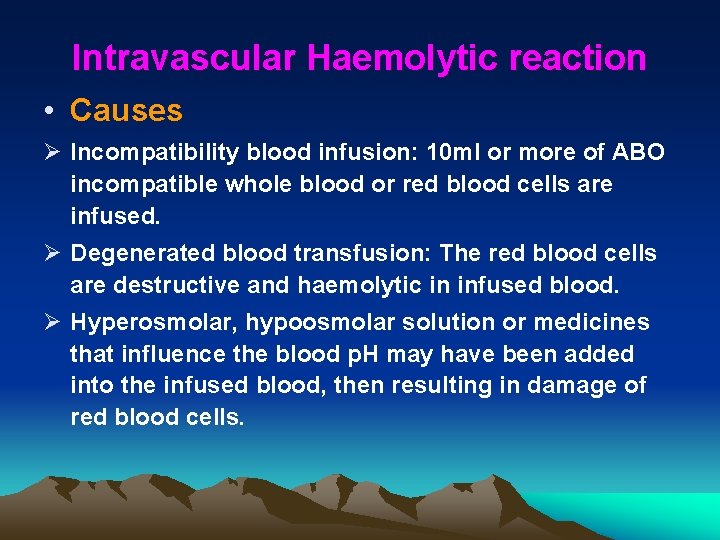
Intravascular Haemolytic reaction • Causes Ø Incompatibility blood infusion: 10 ml or more of ABO incompatible whole blood or red blood cells are infused. Ø Degenerated blood transfusion: The red blood cells are destructive and haemolytic in infused blood. Ø Hyperosmolar, hypoosmolar solution or medicines that influence the blood p. H may have been added into the infused blood, then resulting in damage of red blood cells.
Intravascular Haemolytic reaction • Clinical Manifestations (3 stages) Ø In the first stage: headache, nausea, vomiting, chest pain, limbs numbness, and increased pain in kidney region Ø In the second stage: hemoglobinuria(血红蛋白尿), jaundice(黄疸), chills, fever, dyspnea, cyanosis, and hypotension Ø In the third stage: oliguria(少尿), anuria(无尿), even acute renal failure or death
Intravascular Haemolytic reaction • Preventing Intervention Ø The nurse should meticulously verify and document patient identification from sample collection to component infusion to prevent the haemolytic reaction, and make sure the compatibility of blood typing and cross-matching.
Intravascular Haemolytic reaction • Nursing Interventions 1. Stop transfusion immediately, remove blood any blood-filled tubing, and replace with saline bag and new tubing to keep line open, notify the physician and blood bank immediately. 2. Provide oxygen therapy, maintain intavenous access, administer medications as ordered.
Intravascular Haemolytic reaction • Nursing Interventions 3. Return blood bag and tubing to blood bank. Obtain blood and urine samples of the patient and send to the laboratory. 4. Local blocking in both renal regions; heat therapy on the back should be provided to reduce the spasm of renal blood vessels.
Intravascular Haemolytic reaction • Nursing Interventions 5. Infuse sodium bicarbonate by intravenous injection to make urine alkaline to promote hemoglobin dissolved to reduce the obstruction of renal tubule. 6. Monitor vital signs every 15 minutes; monitor and record urine output hourly by inserting indwelling catheter. Peritoneal dialysis(腹透) or haemodialysis( 血透) may be required if renal failure occurs. 7. Treating shock as prescribed, if present. 8. Give mental support.
Extravascular Haemolytic Reaction • caused by D, C, and E antibodies in Rh system. • is present after one week or more of blood transfusion. • the signs of reaction are mild: mild fever, anemia , feel tired. The bilirubin(胆红素) in blood is increasing. • These kinds of patients should avoid transfusion again as far as possible.
The reaction Related to Large Volume of Blood Transfusion • Circulatory Overload • Hemorrhage • Sodium Citrate Poisoning Reaction
Circulatory Overload • Causes: pulmonary edema • Clinical Manifestations: occur at anytime during or immediately after completion of the transfusion; chest pressed,shortness of breath, dyspnea, cough, frothy or pinkish sputum,facial paleness,diaphoresis, anxiety, headache, tachycardia, tachypnea(气促), orthopnea(端坐呼吸), increased venous pressure, neck veins tension, rales in lungs
Circulatory Overload • Nursing Interventions Ø slow or stop the transfusion immediately,notify the physician Ø assume a Folower’s position with the feet dangling at the bedside if the patient’s condition is allowed Ø apply oxygen inhale with higher flow rate, put 20% to 30% ethanol solution into humidifying bottle Ø administer the sedative,vasodilators,antiasthma(平喘), digitalis,and diuretics to the patient according to the physician’s order Ø apply tourniquet to limbs of the patient in alternation in order to reduce the venous return if necessary
Hemorrhage • Causes Ø Platelets and thrombogen(凝血酶原) are damaged in stored blood. Ø Too much sodium citrate is infused, and may cause the disturbances of blood coagulation. • Clinical Manifestations wound bleeding, skin bleeding, gingival(牙龈) bleeding, bleeding in venipuncture site, or hematuria(血尿)
Hemorrhage • Nursing Interventions Ø Monitor the symptoms and signs of hemorrhage. Ø One unit of fresh blood is infused after 3 units of stored blood. Ø The patient should be provided the blood components according to the lack of clotting factors.
Sodium Citrate Poisoning Reaction • Causes sodium citrate and serum calcium are combined -- hypocalcemia (低血钙症) • Clinical Manifestations tetany(抽搐), hypotension, Q—T interval is prolonged in EKG, cardiac arrest may occur if the condition is serious • Nursing Intervention 1000 ml of blood--10 ml of 10% calcium gluconate IV
Other Reactions • air embolism • Sepsis(败血症) • hypothermia • blood transmitted disease (hepatitis, malaria, AIDS ) • hyperkalemia (stored blood ) • Acidosis (stored blood )
9. Selection of Blood Donors • The Contraindications for Blood donors Ø The person who have the history of allergies, hepatitis and malaria, HIV infection Ø The person with risk factors for HIV infection, heart disease, cancers, severe asthma(哮喘), bleeding disorders, convulsions(惊厥), hypertension or hypotension Ø The patient who undergo the operation, pregnancy women, or the persons who take certain medicines Ø The person who have high-risk behaviors such as having unsafe sex relationships, IV drug abuse
10. The Principles of Blood Transfusion • Need physician’s order; blood typing and crossmatching should be tested before transfusion • Cross-matching test should be did again if the patient need another transfusion to examine antibodies produced in the serum
10. The Principles of Blood Transfusion • In general, whole blood is administered ABO identical. In emergency situations, when time does not allow ABO determination, group O blood may be given, group AB blood can accept group A and B blood with direct cross-matching test negative, transfusion rate must be slowly, and the amount of blood should not overrun 400 ml.