Chapter 12 Conception and Prenatal Development Conception The


- Slides: 47
Chapter 12 Conception and Prenatal Development
Conception • The union of egg and sperm • It requires preparation in male and female
Preparation of conception in female • Oogenesis: ova production in female begins during prenatal life but it called primary oocytes (not mature) • Menstruation: necessary for: • Maturation of the primary follicles and ovulation • Endometrial preparation for implantation that occurs during menstruation
• Ovum Transportation -after ovulation the mature ovum is picked up by the fimbriated end of fallopian tube. -then the ovum is transported through the muscular action and cilia within the tube -the ovum is fertilized in the distal third of fallopian tube (Ampulla)
Preparation of conception in male • Spermatogenesis -formation of sperm, begins during puberty -the primary sperm (spermatogonia) develop during fetal life and begin multiplying during puberty • Ejaculation -With each ejaculation during intercourse about 35 -200 million sperm are deposited in upper vagina and over cervix
• Transport of Sperm -whiplike movement of tail of sperm propels them through cervix, uterus and fallopian tube -uterine contraction induced by prostaglandins in the seminal fluid also enhance sperm movement -only few hundred sperm reach the fallopian tube where the ovum wait
• Preparation of sperm for fertilization through their trip to reach ovum sperm undergo changes called - Capacitation. • Capacitation: removal of a glycoprotein coat and seminal proteins from acrosome(tip of sperm head) • Capacitation is necessary to make sperm more active and able to penetrate the ovum layers • Sperm that reach ovum release an enzyme (hyaluronidase) to digest a pathway through ovum layers
Life Span of Ovum and Sperm • The ovum may have the capacity to be fertilized no longer than 24 hours • Most sperm survive no more than 1 to 2 days although a few may remain fertile in the woman reproductive tracts up to 80 hours. Copyright © 2005 by Elsevier, Inc. All rights reserved.
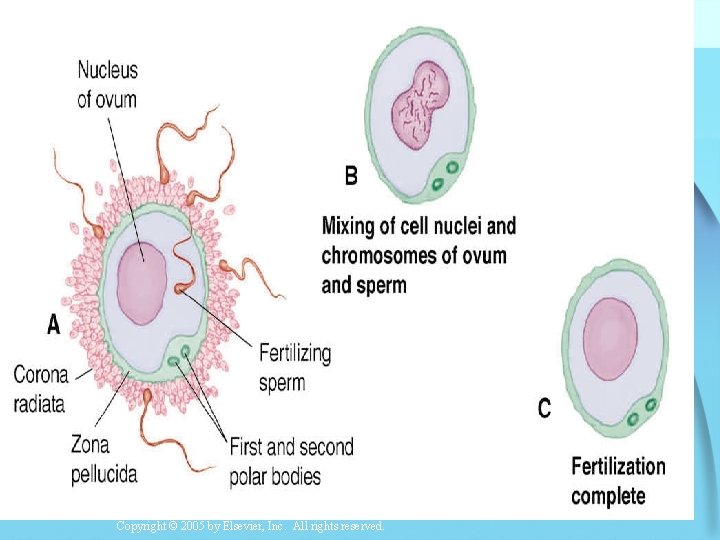
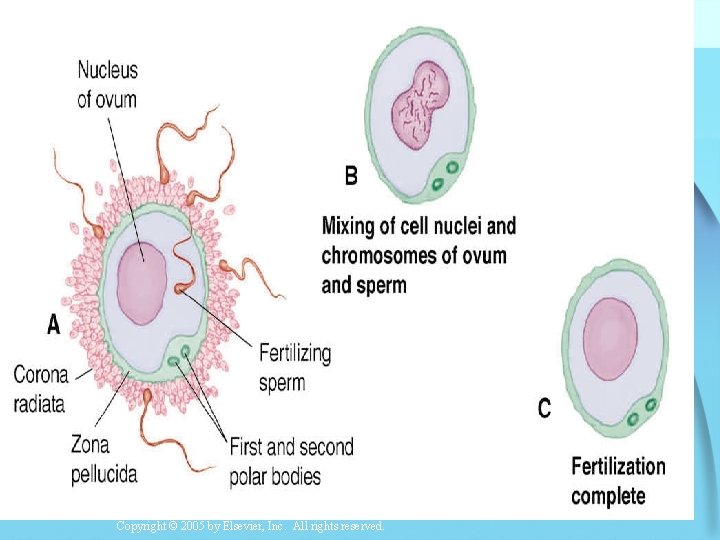
Fertilization • Occurs when one spermatozoon enters the ovum and the two nuclei containing parent’s chromosome merge. • After one sperm enter the ovum , it become impermeable for any other sperm • After fertilization the 23 chromosomes from sperm mingle with he 23 chromosomes from the ovum resulting in the diploid number of 46 chromosome (Zygote)
Copyright © 2005 by Elsevier, Inc. All rights reserved.
The Sex of the Fetus • The gametes from the male (sperm) determine the sex of the baby • If an X-bearing spermatozoon fertilizes the ovum, the sex of the new baby is female • If a Y-bearing spermatozoon fertilizes the ovum the sex of baby is male. Copyright © 2005 by Elsevier, Inc. All rights reserved.
Stages of Fetal Development • 1. Pre-embryonic Period: first two weeks after conception • 2. Embryonic period: from third week to eight week of conception • 3. Fetal Period from nine weeks until birth
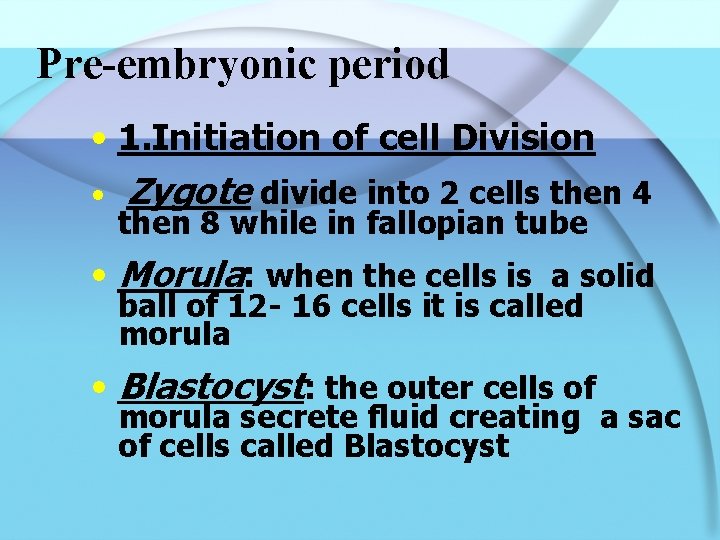
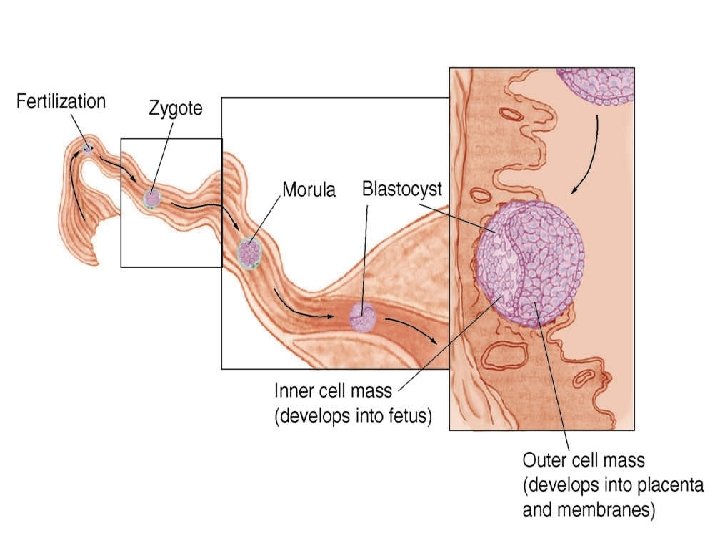
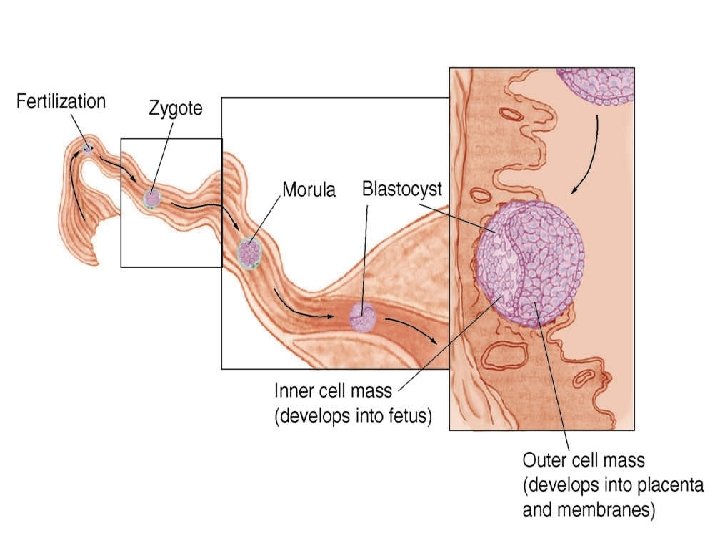
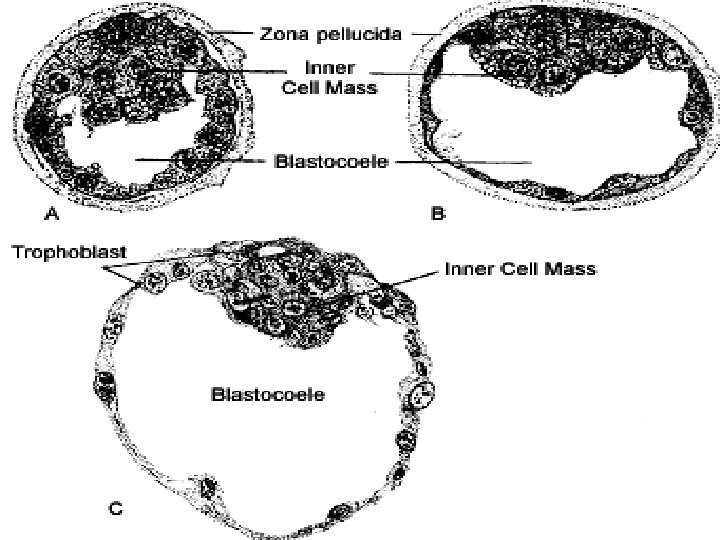
Pre-embryonic period • 1. Initiation of cell Division • Zygote divide into 2 cells then 4 then 8 while in fallopian tube • Morula: when the cells is a solid ball of 12 - 16 cells it is called morula • Blastocyst: the outer cells of morula secrete fluid creating a sac of cells called Blastocyst
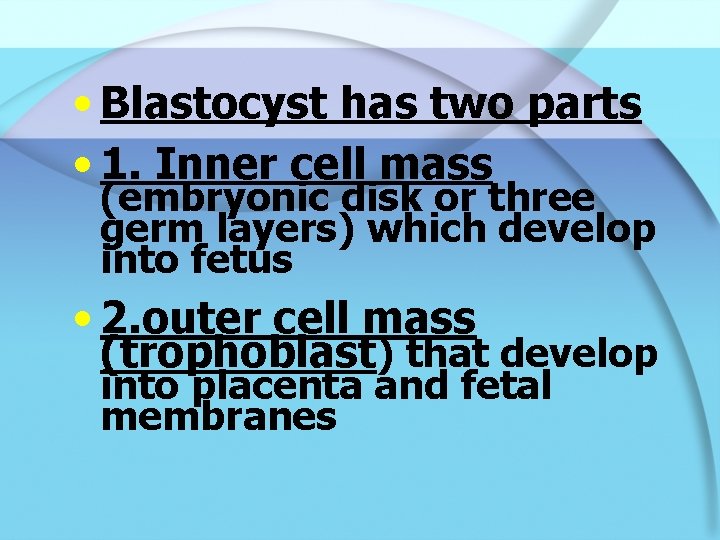
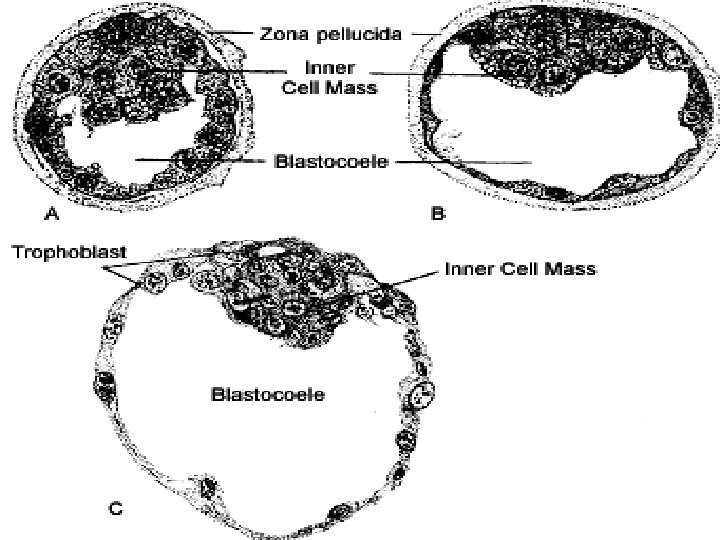
• Blastocyst has two parts • 1. Inner cell mass (embryonic disk or three germ layers) which develop into fetus • 2. outer cell mass (trophoblast) that develop into placenta and fetal membranes
Copyright © 2005 by Elsevier, Inc. All rights reserved.
Copyright © 2005 by Elsevier, Inc. All rights reserved.
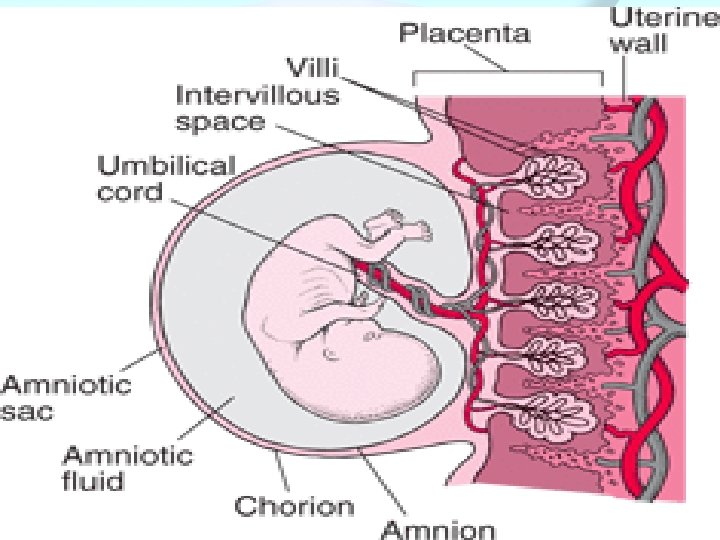
–Fetal membranes are two : • 1. Amnion: inner membrane • 2. Chorion: outer membrane Copyright © 2005 by Elsevier, Inc. All rights reserved.
Continued pre embryonic period • 2. Entry of zygote into uterus • The conceptus enters uterus about 3 to 4 days after conception when it contain 100 cells • Implantation • Occurs between 6 to 10 th days of fertilization
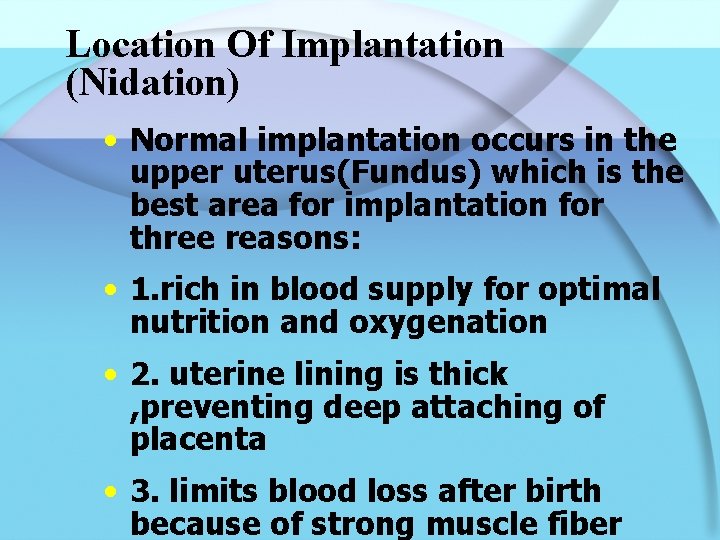
Location Of Implantation (Nidation) • Normal implantation occurs in the upper uterus(Fundus) which is the best area for implantation for three reasons: • 1. rich in blood supply for optimal nutrition and oxygenation • 2. uterine lining is thick , preventing deep attaching of placenta • 3. limits blood loss after birth because of strong muscle fiber
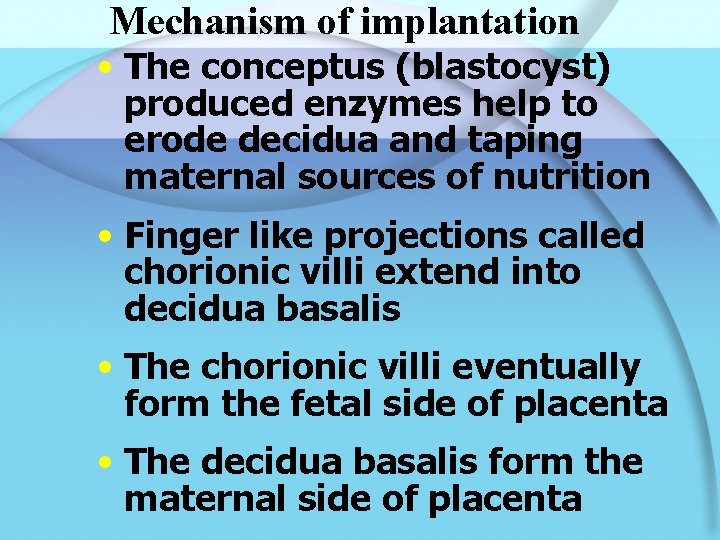
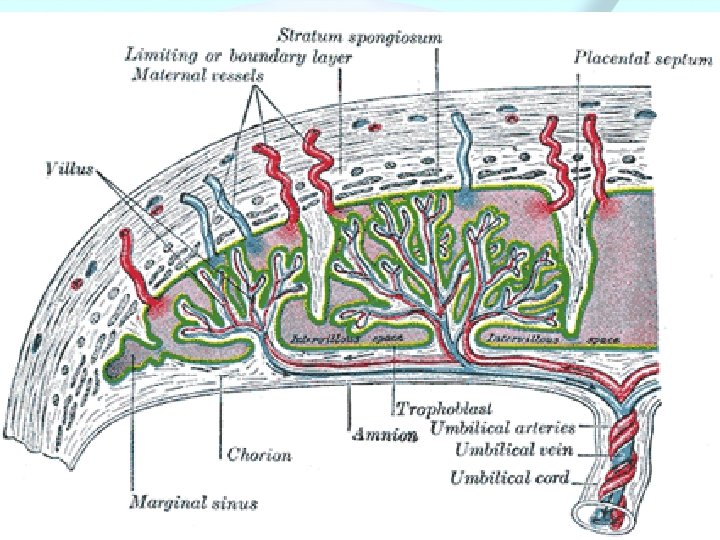
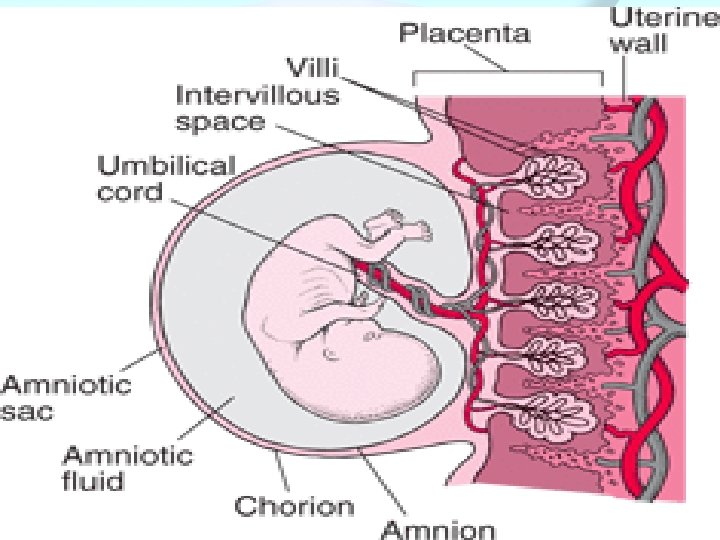
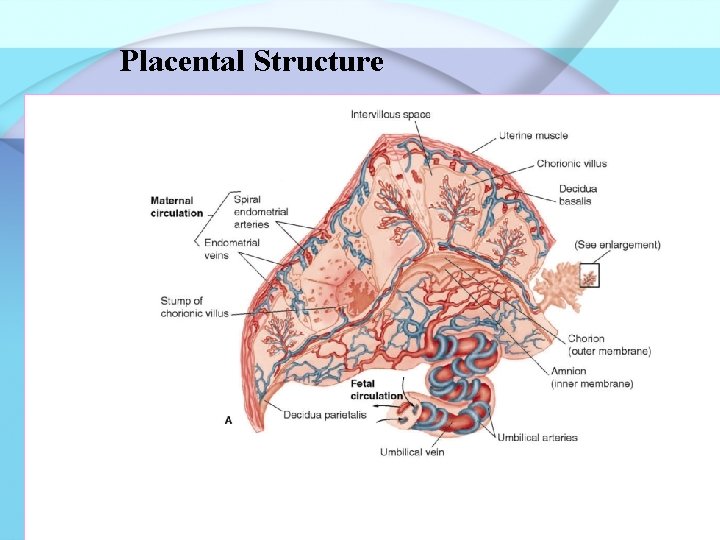
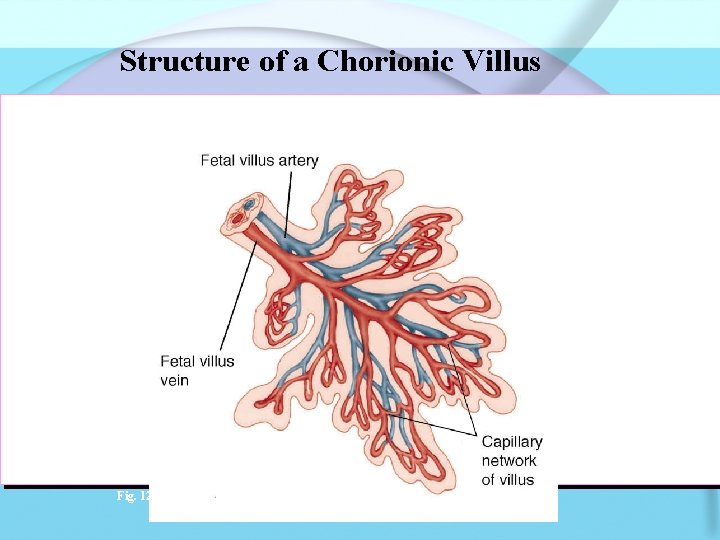
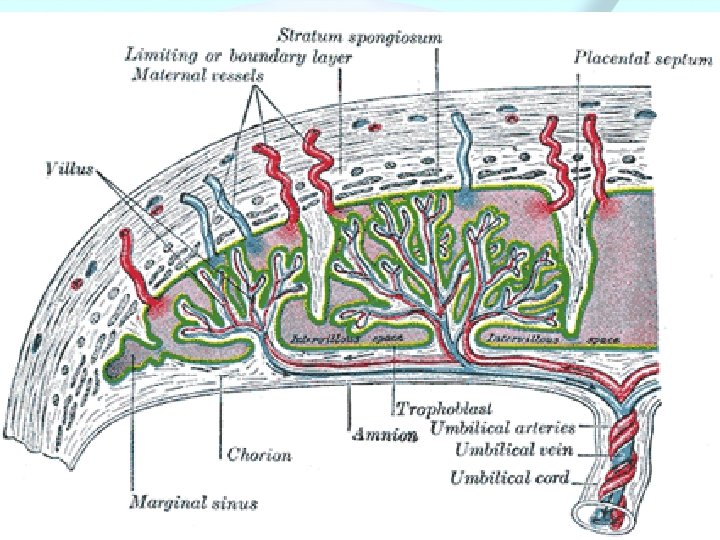
Mechanism of implantation • The conceptus (blastocyst) produced enzymes help to erode decidua and taping maternal sources of nutrition • Finger like projections called chorionic villi extend into decidua basalis • The chorionic villi eventually form the fetal side of placenta • The decidua basalis form the maternal side of placenta

Decidua • Endomterium after implantation is called Decidua • Classified as: • 1. Decidua basalis: underlies the developing embryo and form maternal side of placenta • 2. Decidua Capsularis: overlies embryo • 3. Decidua Parietalis: lines the rest of uterine cavity, about 22 GW decidua capsularis fuses with parietalis
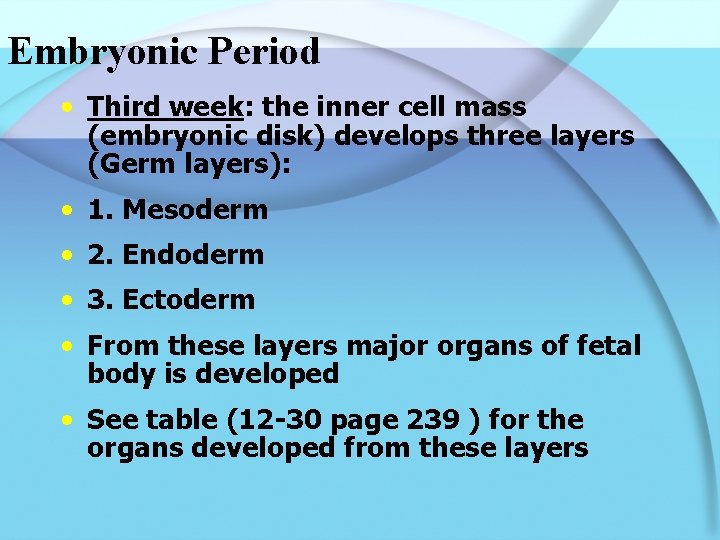
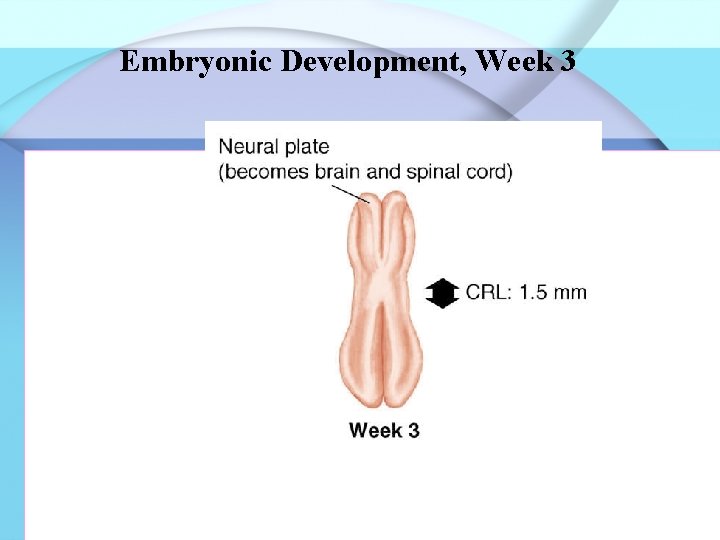
Embryonic Period • Third week: the inner cell mass (embryonic disk) develops three layers (Germ layers): • 1. Mesoderm • 2. Endoderm • 3. Ectoderm • From these layers major organs of fetal body is developed • See table (12 -30 page 239 ) for the organs developed from these layers
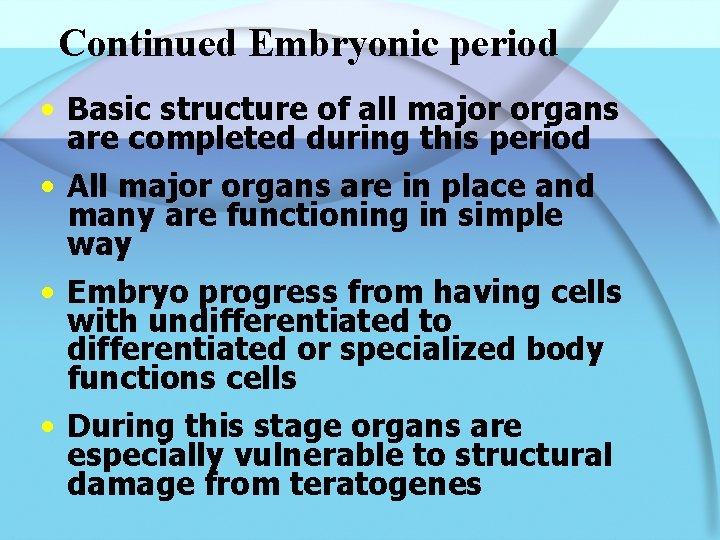
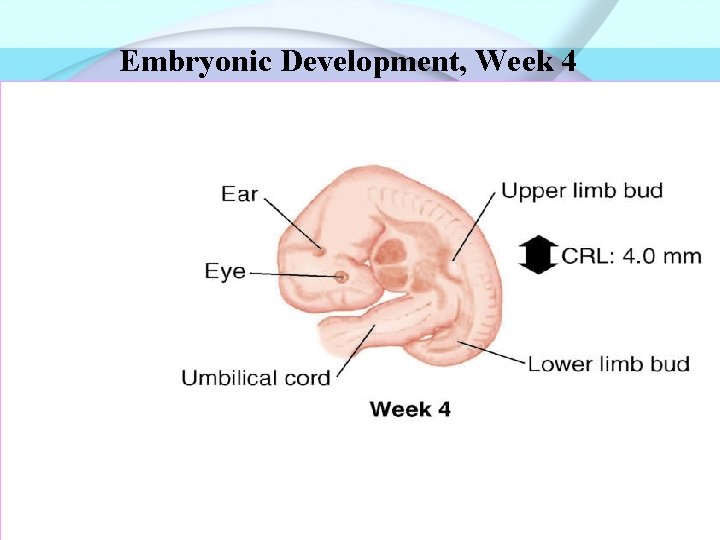
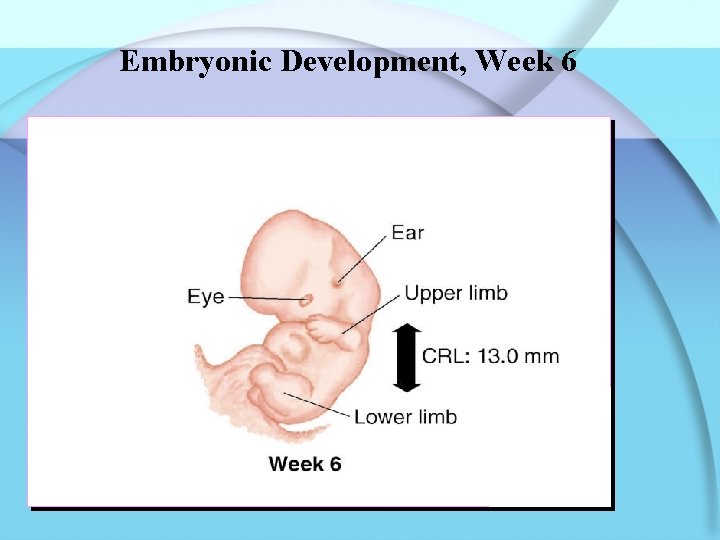
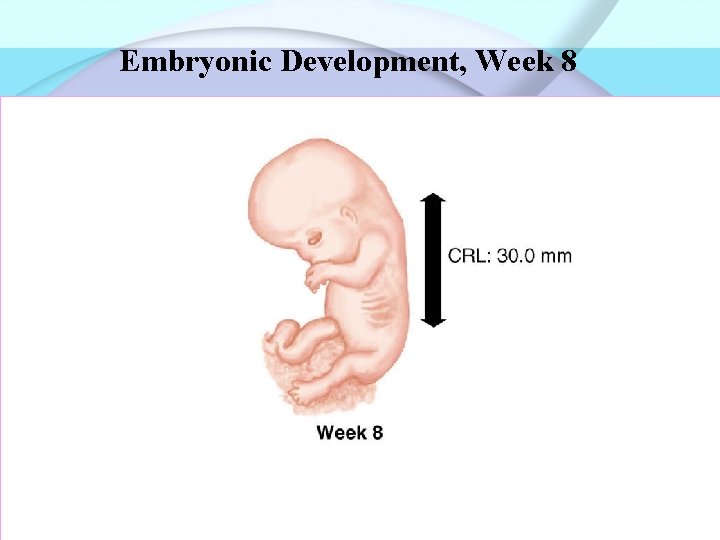
Continued Embryonic period • Basic structure of all major organs are completed during this period • All major organs are in place and many are functioning in simple way • Embryo progress from having cells with undifferentiated to differentiated or specialized body functions cells • During this stage organs are especially vulnerable to structural damage from teratogenes
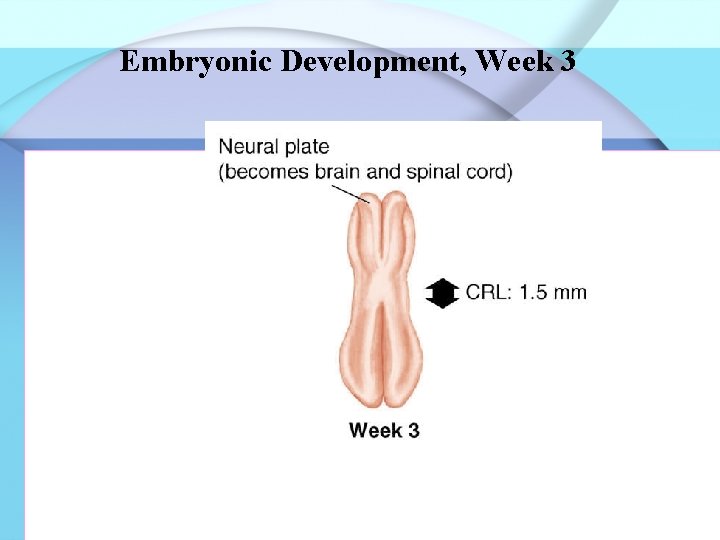
Embryonic Development, Week 3 Fig. 12 -5 a
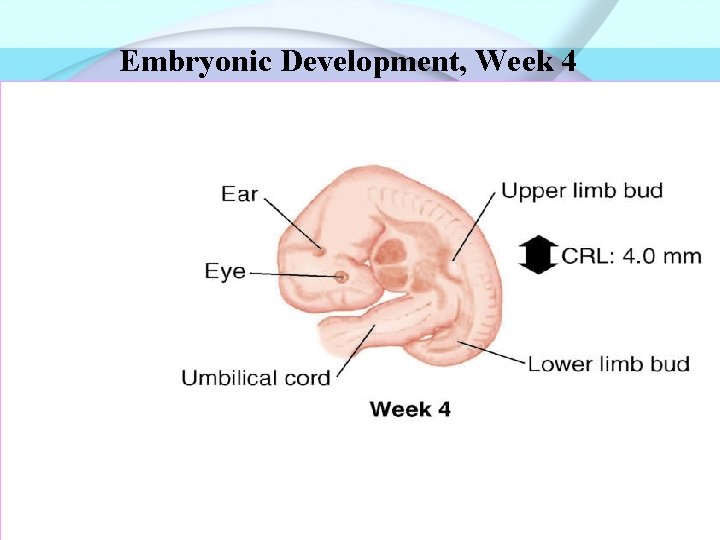
Embryonic Development, Week 4 Fig. 12 -5 b
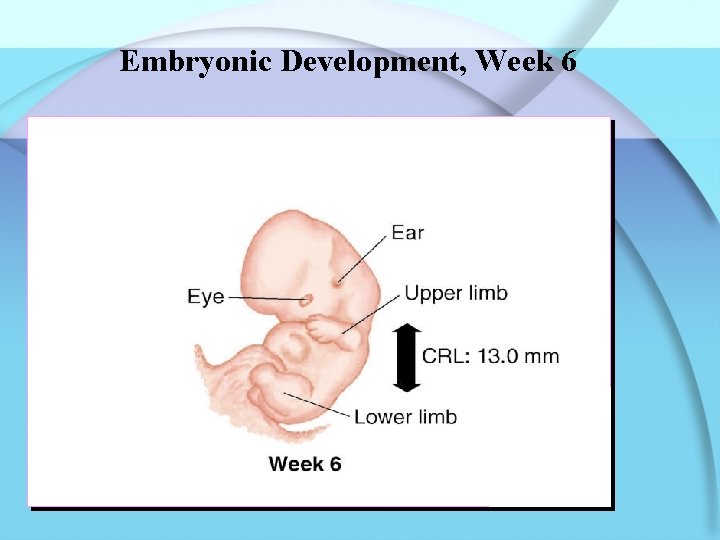
Embryonic Development, Week 6 Fig. 12 -5 c
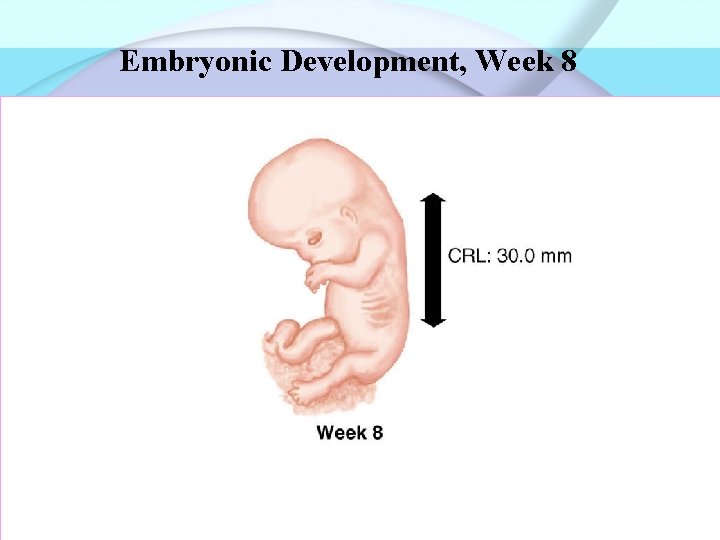
Embryonic Development, Week 8 Fig. 12 -5 d
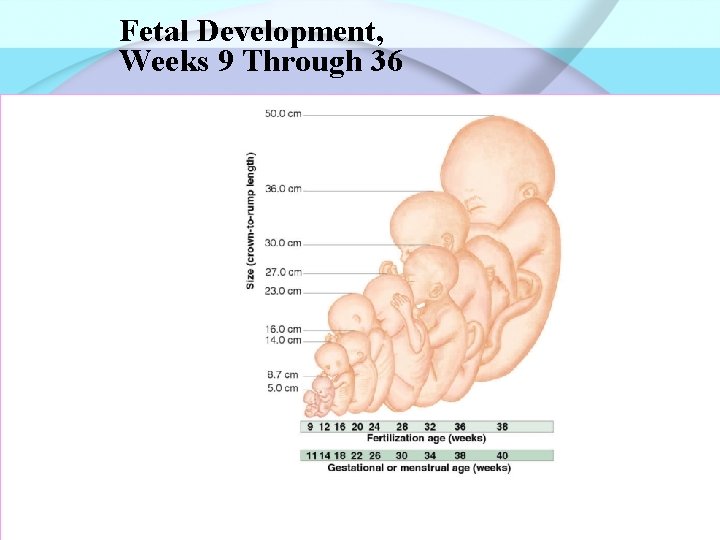
Fetal period • See details of fetal period from table in book
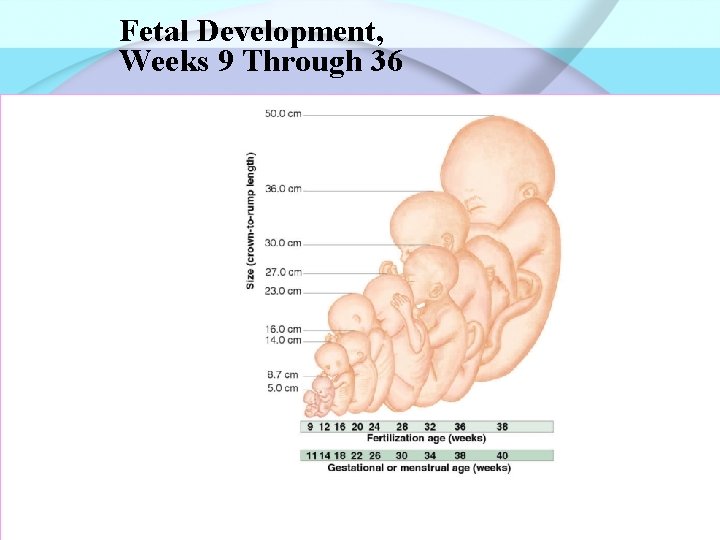
Fetal Development, Weeks 9 Through 36 Fig. 12 -6
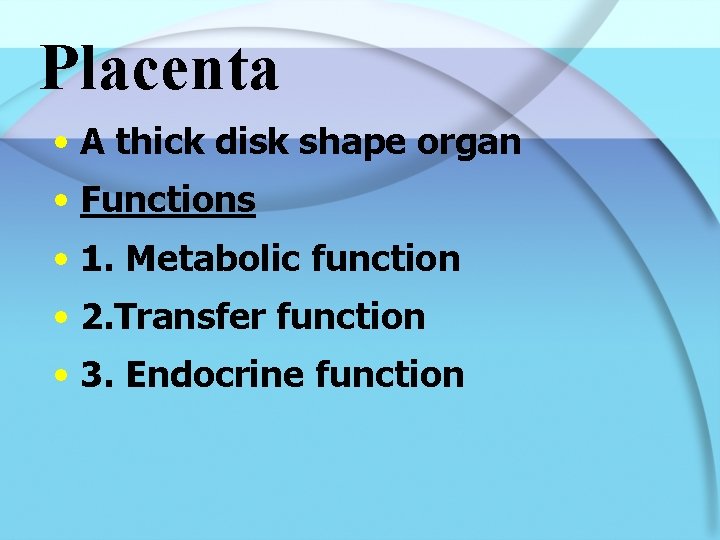
Placenta • A thick disk shape organ • Functions • 1. Metabolic function • 2. Transfer function • 3. Endocrine function
Metabolic function • Placenta produces some nutrients needed for embryo and for its own function such as glycogen, fatty acids and cholesterol
Transfer Function • Exchange of oxygene, nutrients and waste product across chorionic villi
Endocrine Functions • Produces many hormones necessary for normal pregnancy, the most important are: • 1. HCG: Human Chorionic Gonadotropin causes the corpus luteum to persist and secrete estrogen and progesterone for the first 6 to 8 GW • 2. Human placental lactogene: promotes normal nutrition and growth of fetus and maternal breast development for lactation
• 3. Estrogen: enhance uterine activity and playing a role as labor begins • 4. Progesterone: prepare endometrium for implantation and reduce uterine contraction and help in growth of breast •
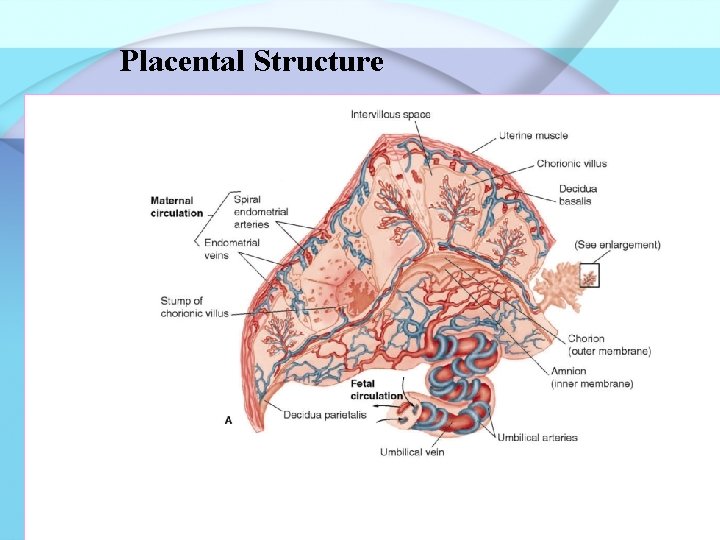
Placental Structure Fig. 12 -7

Amniotic Fluid • Sources: • Fetal urine • Fluid transported from maternal blood • Volume: • 500 -1000 ml • Less than 500 ml called oligohydraminios, associated with poor fetal lung or kidney development
Continued aminotic fluid • More than 2000 ml called hydramnios or polyhydramnios, associated with CNS Or GIS malformation • Functions of amniotic Fluid • 1. Protect fetus by • cushioning against an impact to maternal abdomen • providing stable temperature
• 2. Promote normal development by: • allowing symmetric development of fetus • keeping membranes from adhering to fetal parts • providing room for fetal movement • constant intrauterine temperature • provide a cushion to distribute pressure within uterus
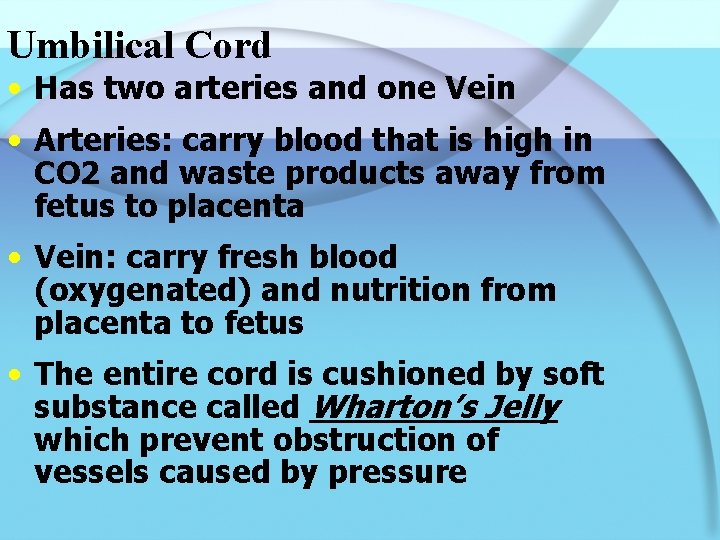
Umbilical Cord • Has two arteries and one Vein • Arteries: carry blood that is high in CO 2 and waste products away from fetus to placenta • Vein: carry fresh blood (oxygenated) and nutrition from placenta to fetus • The entire cord is cushioned by soft substance called Wharton’s Jelly which prevent obstruction of vessels caused by pressure
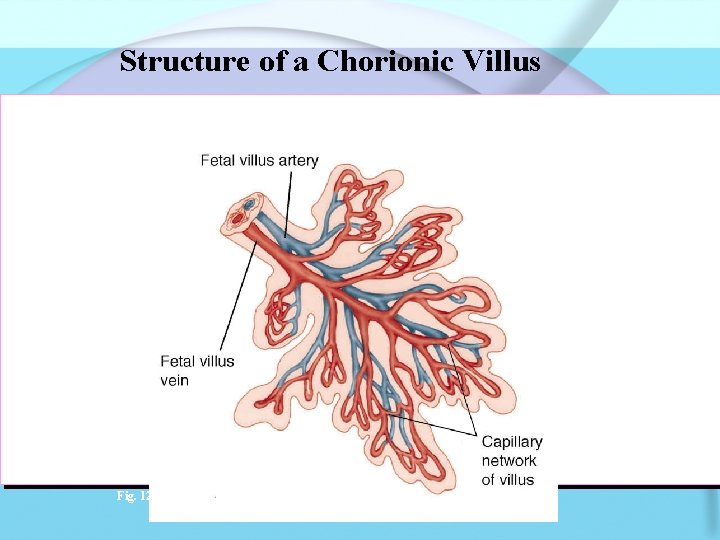
Structure of a Chorionic Villus Fig. 12 -7
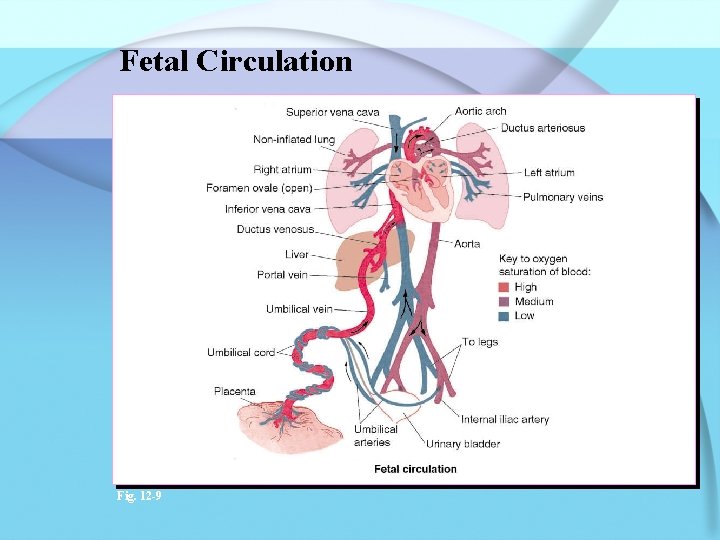
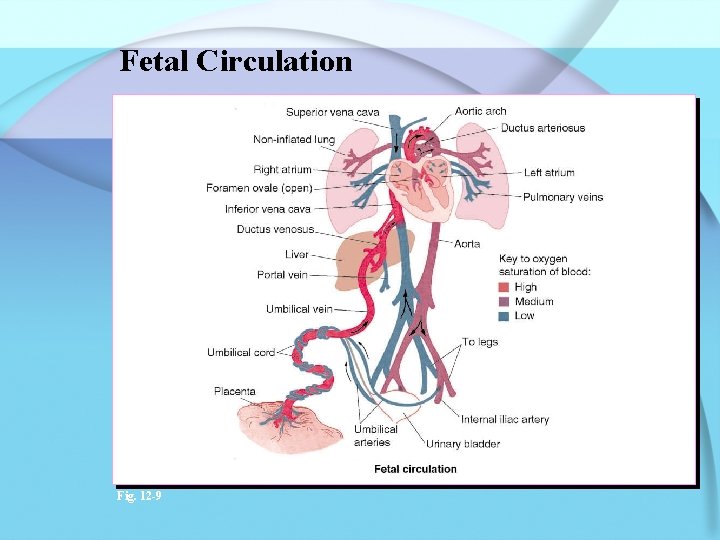
Fetal Circulation Fig. 12 -9
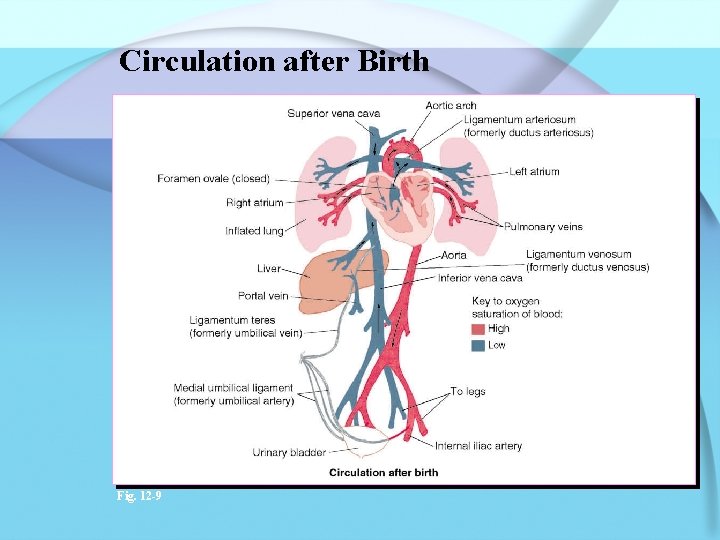
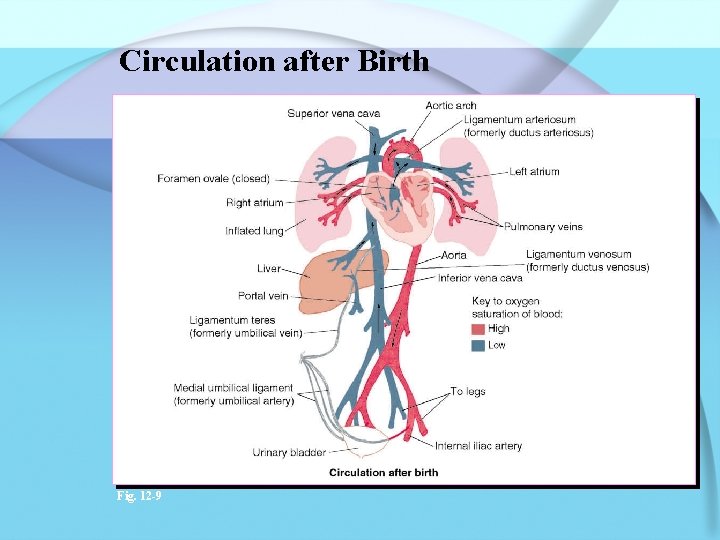
Circulation after Birth Fig. 12 -9
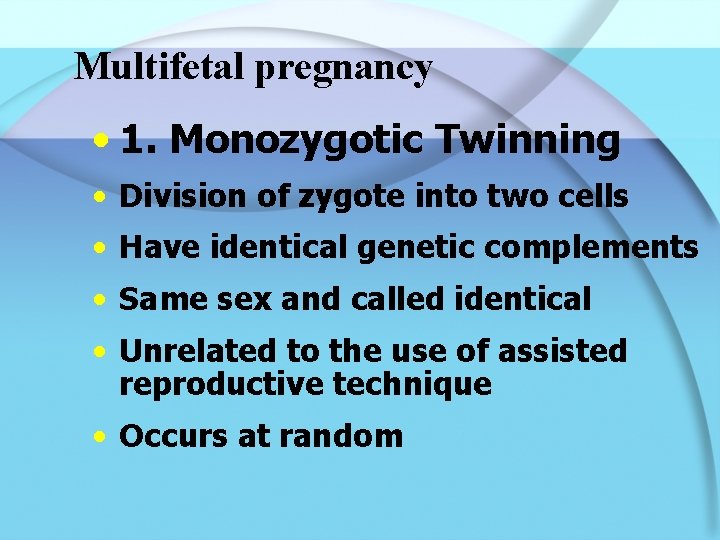
Multifetal pregnancy • 1. Monozygotic Twinning • Division of zygote into two cells • Have identical genetic complements • Same sex and called identical • Unrelated to the use of assisted reproductive technique • Occurs at random
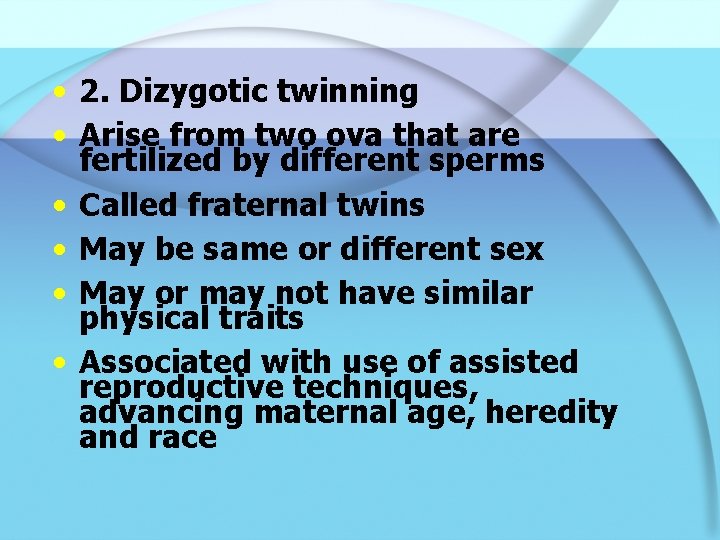
• 2. Dizygotic twinning • Arise from two ova that are fertilized by different sperms • Called fraternal twins • May be same or different sex • May or may not have similar physical traits • Associated with use of assisted reproductive techniques, advancing maternal age, heredity and race
Copyright © 2005 by Elsevier, Inc. All rights reserved.