Chapter 12 Administering Medication Contents 2 Basic Knowledge
Chapter 12 Administering Medication

Contents 2 Basic Knowledge about Medication Administration Oral Administration 3 Parenteral Administration 4 Inhalation Administration 5 Medication Anaphylaxis Test 6 Topical Administration 1
Section 1 Basic Knowledge about Medication Administration
Contents n n n Drug Forms, Distribution System and Medication Storage Principles of Administering Medications Routes of Administration Times and Time of Administration Contributing Factors of Drug Actions

Drug Forms n n n n n Aerosol spray Aqueous solution Aqueous suspension Capsule Enteric-coated tablet Extended/ sustained release Extract Glycerite Liniment Lotion n n Ointment Paste Pill Powder/granule Suppository Syrup Tablet Tincture Transdermal disk patch Troche (lozenge) or

Four kinds n n oral medications external medications for injection new preparations
Distribution System n n n Stock Supply System Unit-dose System Computer-controlled Dispensing System
Store medication n Cabinet n n bright and ventilative, avoiding direct shine and keep clean, tidy and dry. Placement of medications n n n Store separately according to their different routes (oral, injection, or topical), toxicity or untoxicity Expensive drugs, narcotics and virulent toxicants must be taken charge of by a special nurse who should lock the cabinet and have the key always with her. On every shift
n Label the container of medications clearly n n n blue strip labels oral medications, Red strip labels external medications, and black strip labels virulent toxicants. Label the container with name, concentration and dose of drugs If the labels are soiled or illegible, discontinue using the medications
n n Check the medications carefully Store the medications properly according to their different nature. n Medications which tend to volatilize, deliquesce, or effloresce should be kept in airtight bottles, e. g. , ethanol, iodine, sugar-coat tablets.
n Medications that will be oxidized if exposed to air and be denatured if exposed to light should be kept in airtight colored bottles. Cover the container with shade paper box if necessary and store it in the shady and cool area, e. g. , Vitamine C 氨茶碱 � 酸 � 上腺素
n Biologic products and antibiotics that will be destroyed and decomposed if exposed to heat should be kept in the dry, and shady and cool area (about 20℃) or in refrigerator (about 2~ 10℃) according to their natures and requirements of storage, e. g. , an antitoxic serum, vaccine, placental globin, penicillin skin test solution.
Medications should be used designedly according to valid periods in case of invalidation, e. g. , antibiotics and insulin. n Store the inflammable and explosive medications in airtight bottle and place in the shady and cool area separately and keep them away from fire and electric appliances. n
Principles of Administering Medications n n Correct Transcription and Communication of Orders Use the Guidelines of Three Checks and Seven Rights to Ensure Safe Drug Administration Administer medication safely and accurately Observe the client’s response to the medication after administration
Three Checks n n n the check before operation the check during operation the check after operation
Seven Rights n n n n the right name of the client right bed number of the client right name of the medication right concentration right dose right route right time. Quality valid
Routes of Administration n Oral Routes n n Parenteral Routes n n n Oral administration Sublingual Administration the intrathecal or intraspinal, Buccal Administration Intradermal (ID) Subcutaneous (SQ) Intramuscular(IM) Intravenous( IV) intraosseous, intrapleural, intraarterial, intraarticular, and intracardiac, routes Skin and Mucous Membrane Route Inhalation Route Topical administration
Skin and Mucous Membrane Route n n n 1. Direct application of liquid or ointment (e. g. , eye drops, gargling, swabbing the throat) 2. Insertion of drug into a body cavity (e. g. , placing a suppository in rectum or vagina or inserting medicated packing into vagina) 3. Instillation of fluid into body cavity (e. g. , ear drops, nose drops, or bladder and rectal instillation [fluid is retained]) 4. Irrigation of body cavity (e. g. , flushing eye, ear, vagina, bladder, or rectum with medicated fluid [fluid is not retained]) 5. Spraying (e. g. , instillation into nose and throat)
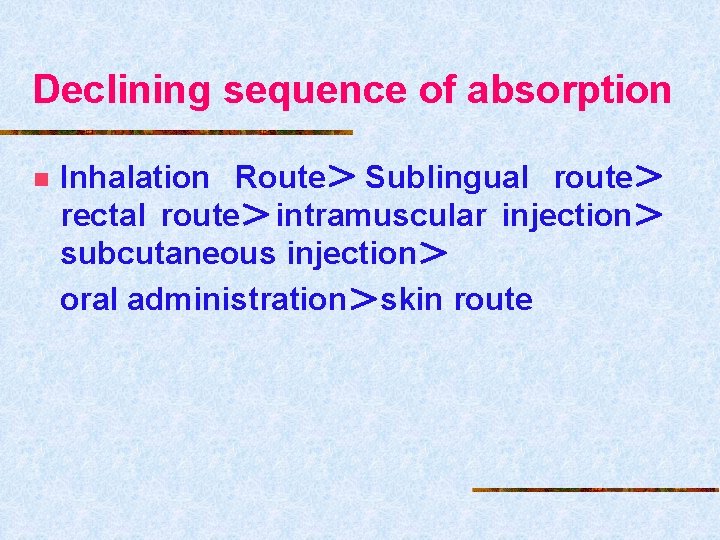
Declining sequence of absorption n Inhalation Route> Sublingual route> rectal route>intramuscular injection> subcutaneous injection> oral administration>skin route
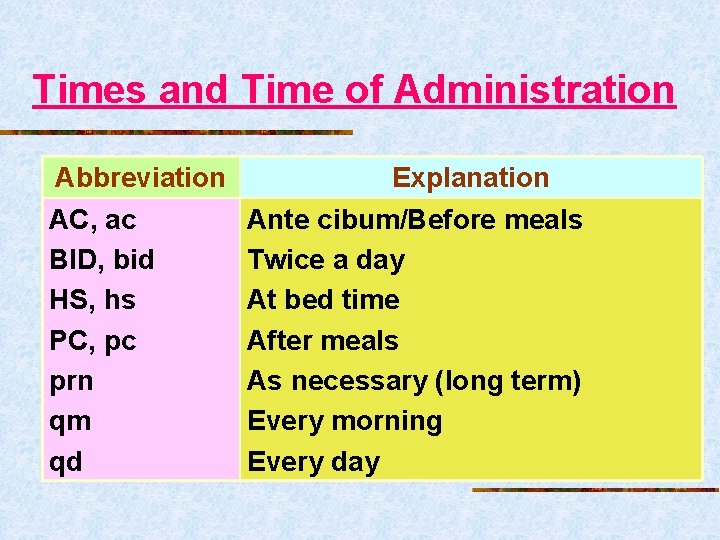
Times and Time of Administration Abbreviation AC, ac BID, bid HS, hs PC, pc prn qm qd Explanation Ante cibum/Before meals Twice a day At bed time After meals As necessary (long term) Every morning Every day

Abbreviation qod qh q 2 h q 4 h q 6 h qid SOS St tid DC Explanation Every other day Every 1 hour Every 2 hour Every 4 hour Every 6 hour 4 times a day As needed (only one time within 12 hours) Immediately 3 times a day discontinue
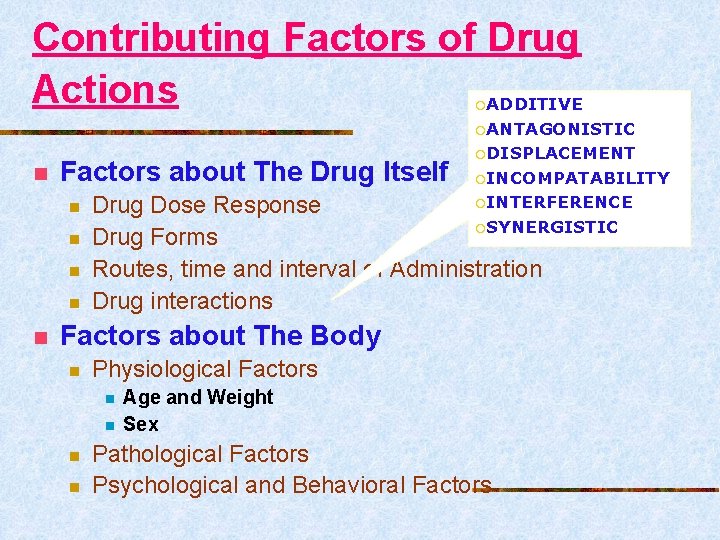
Contributing Factors of Drug Actions ADDITIVE ¡ ¡ANTAGONISTIC n Factors about The Drug Itself n n n ¡DISPLACEMENT ¡INCOMPATABILITY ¡INTERFERENCE Drug Dose Response ¡SYNERGISTIC Drug Forms Routes, time and interval of Administration Drug interactions Factors about The Body n Physiological Factors n n Age and Weight Sex Pathological Factors Psychological and Behavioral Factors
Section 2 Oral Administration
ORAL MEDICATIONS n n n Most common route Convenient Least expensive Most meds available in this form Easy to counteract overdose or toxicity
Indications n Clients who are able to swallow solid and liquid
Contraindications n n n n 1. Clients with impaired swallowing function 2. Unconscious clients 3. clients who refuse to take medications orally 4. clients with vomiting or/and nausea 5. clients with gastric or intestinal suction 6. clients with bowel inflammation or reduced peristalsis 7. clients with recent GI surgery
DIFFERENT FORMS n n n n Capsules Tablets Elixirs Emulsions Lozenges Suspensions Syrups
NASOGASTRIC ADMINISTRATION n n n For patients who cannot swallow NG tubes Similar to oral administration
Skills _Equipment n n n Medication cards, sheets, or records Medication cart or tray Medication cups, measuring cup, drop tube Drinking straws Pill-crushing or pillating device(研钵) Kettle with warm water Paper towels See disk
Procedure Medication preparation 1. Wash hands, wear mouth mask and assemble the equipment 2.Follow the three checks and seven rights principle. 3. Prepare medications with appropriate method based on different forms of medication. Fetching meds from bottles.
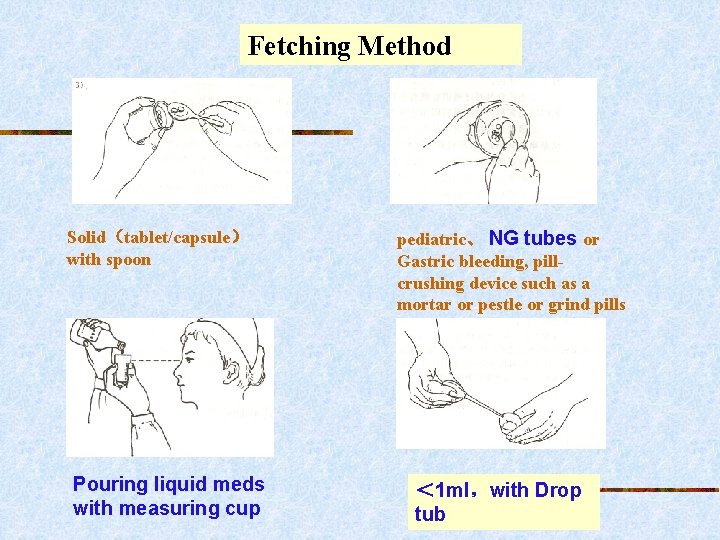
Fetching Method Solid(tablet/capsule) with spoon Pouring liquid meds with measuring cup pediatric、 NG tubes or Gastric bleeding, pillcrushing device such as a mortar or pestle or grind pills < 1 ml,with Drop tub
Administering medication 1.Wash hands. Take Medication cards, sheets, or records Medication cart or tray to bedside. 2.Offer medications and warm water 3. Assist clients with critical illness or pediatric clients. For NG, grind meds. 4.Teach clients the effects and cautions of meds 4.Clean the cup See disk
Guidelines followed when administering oral medications n n n 1. Always administer a drug with warm boiled water of 40~60℃ instead of with tea. 2. Medications that erode teeth such as acid and chalybeate should be sucked with a sucker and then rinse to protect teeth. 3. Never chew, crush or break sustained release tablets, enteric-coated tablets and capsules
n n 4. Place lozenges under the tongue or between buccal membrane and teeth dissolved slowly rather than allow clients to chew or swallow. 5. Generally, stomachic medications are appropriately taken before meal, while those irritating gastric membrane taken after meal. Hypnotics is properly taken before sleep and parasiticides taken in limosis or half limosis.
n n 6. Antibiotics and sulfonamide should be taken at certain interval to ensure effective drug blood concentration. 7. Avoid giving fluids immediately after a client swallows medication such as syrup that exerts local medicating effects on the oral mucosa
n n 8. Allow the client to drink more water after sulfonamide is taken to prevent the crystal which the drug produces when excreted through kidney with the less urine volume to block the nephridium. 9. Observe the heart rate and rhythm closely when cardiotonic is taken. If the heart rate is lower than 60 times per minute or arrhythmia occurs, discontinue to use the drug and inform the physicist.
Section 3 Parenteral Administration
Parenteral Administration n Concept n n the process that injects a certain volume of sterile solution and/or biological products into human body by using sterile syringe Purpose n to prevent, diagnose and cure disease.
n Characteristics n n Appropriate for clients unable to take meds orally Rapid absorption Difficult to Counteract Adverse Reaction Invasive procedure, be performed using aseptic techniques
Contents n n Principles of Injections Equipment Draw medication Common Injection Methods
Principles of Injections n Apply Sterile Technique Strictly Carry out Check Principles Strictly Perform Disinfection and Seclusion Policy Appropriate Syringe and Needle Appropriate Injection Site Prepare and Administer Temporarily Eject Air thoroughly Note Blood Return Insert Needle at Appropriate Angle and Depth n Give No-Pain Injection n n n n
Apply Sterile Technique Strictly n n n Preparation of nurses Sterilize the local skin over injection site as required Maintain sterility of equipment
Carrying out Check Principles Strictly n n three checks and seven rights inspect the package of medication and sterile equipment
Perform Disinfection and Seclusion Policy n n every client individually uses one series of equipment All of used equipments are disposed according to the disinfection and seclusion policy
Appropriate Syringe and Needle n n Consider route of injection Other factors n n n dosage, viscosity, irritation of medication, and the age, height, and weight of the client, the site of injection check the package and the expiration date check whether the needle is sharp, without crooks, and is tightly connected with tip of syringe
Appropriate Injection Site n n away from nerves, bones, and blood vessels free of inflammation, bruises, itches, edema, nodules and scars change the site for each injection When intravenously injecting, a distal site first, proximal site later.
Prepare and Administer Temporarily n n The medication solution is prepared and dispensed when administered To prevent from the lower effect or contamination
Eject Air thoroughly n If not, arouse air embolism
Note Blood Return n n administering by SQ(皮下),ID, or IM, no blood return appears By IV or IA, blood return appears
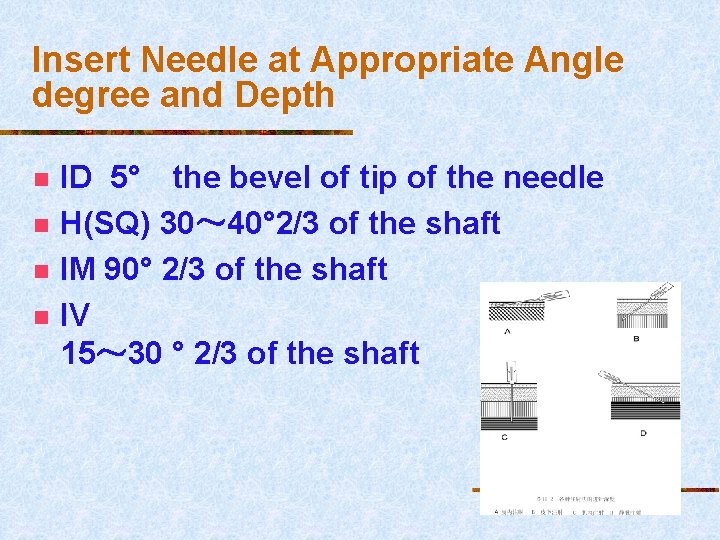
Insert Needle at Appropriate Angle degree and Depth n n ID 5° the bevel of tip of the needle H(SQ) 30~ 40° 2/3 of the shaft IM 90° 2/3 of the shaft IV 15~ 30 ° 2/3 of the shaft
Give No-Pain Injection n n Explain the procedure and comfort the client Assist the client to take a comfortable position Divert the client’s attention Make skin taut when inserting the needle two quicks and one slow n n quick insertion and withdrawal of needles slow injection of medication except pediartic clients
n n inject less irritating medication first, then more irritating medications in deep muscle tissues with a sharpbeveled, long shaft needle Follow sterile and Seclusion techniques strictly
PARENTERAL MEDICATIONS n n n Intradermal Subcutaneous Intramuscular Intravenous Intraarterial
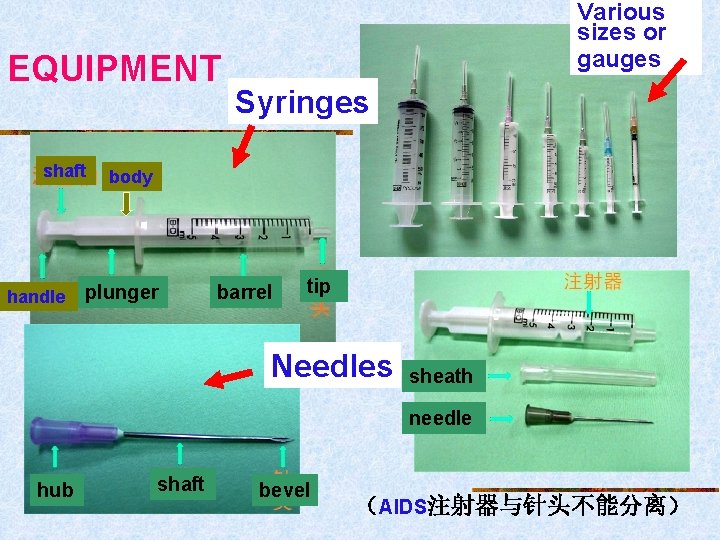
EQUIPMENT shaft handle Various sizes or gauges Syringes body plunger barrel tip Needles sheath needle hub shaft bevel (AIDS注射器与针头不能分离)
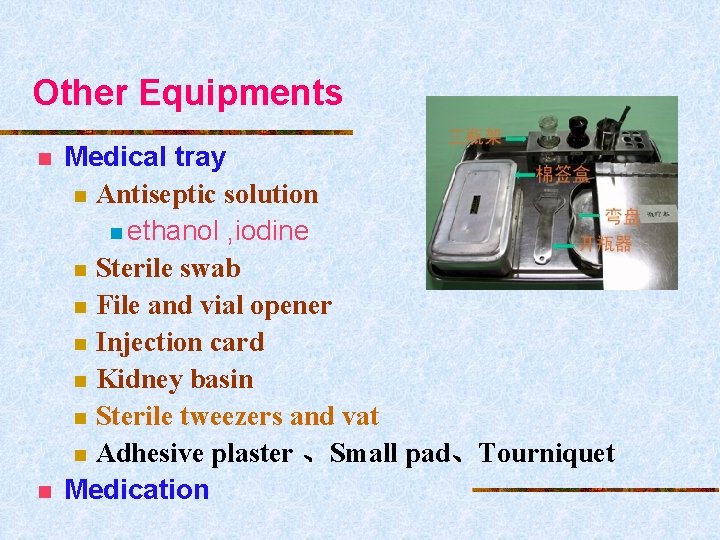
Other Equipments n n Medical tray n Antiseptic solution n ethanol , iodine n Sterile swab n File and vial opener n Injection card n Kidney basin n Sterile tweezers and vat n Adhesive plaster 、Small pad、Tourniquet Medication
MEDICATION FORMS n n Vials Ampules n n Check medications Prefilled tubes 扫描上图P 679
Draw medication n n Preparing an Injection from an Ampule Preparing an Injection from a Vial See disk
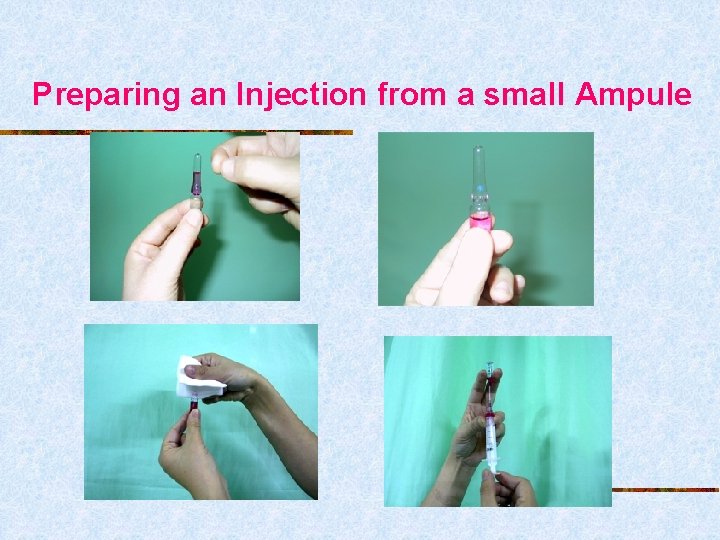
Preparing an Injection from a small Ampule
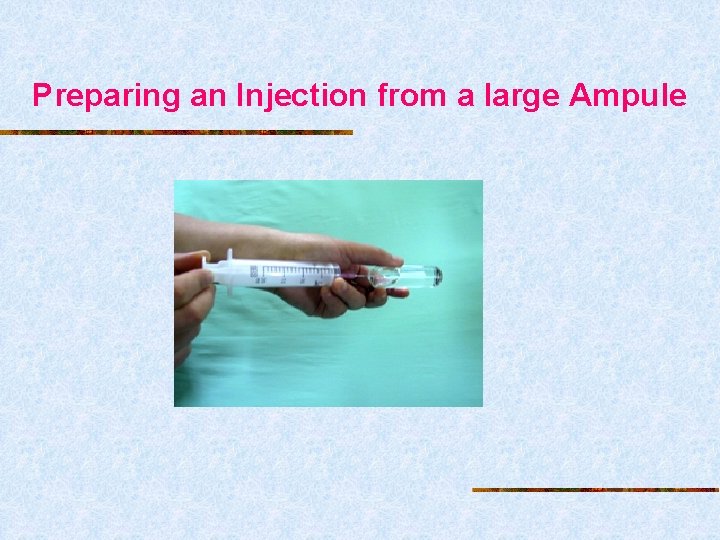
Preparing an Injection from a large Ampule
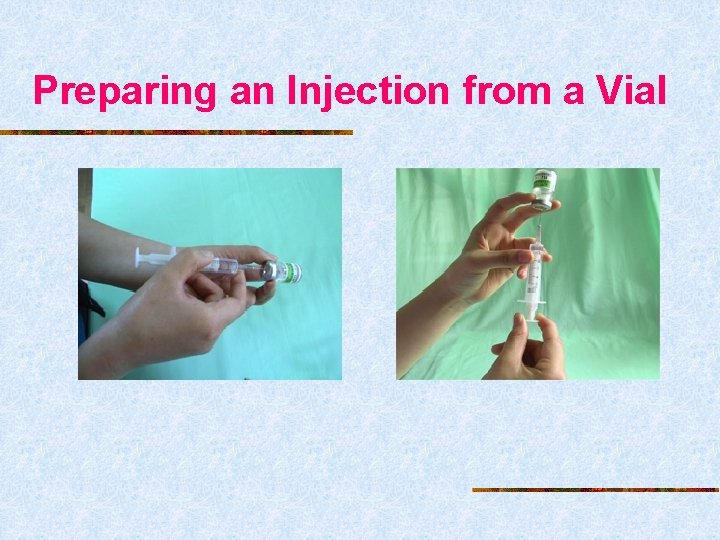
Preparing an Injection from a Vial
Common Injection Methods n n n Intradermal Subcutaneous or Hypodermic : SQ or H Intramuscular Intravenous intraarterial
Intradermal Injection(ID) n Definition n n Intradermal injections involve placing drugs into the tissue between the epidermis and dermis where blood supply is reduced and drug absorption occurs slowly. Purpose n n n Skin test Vaccine inoculation A prior step to local anesthesia
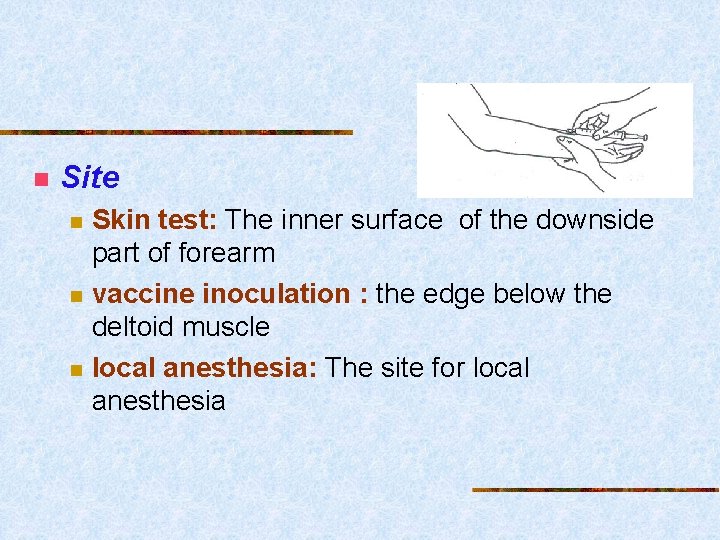
n Site n n n Skin test: The inner surface of the downside part of forearm vaccine inoculation : the edge below the deltoid muscle local anesthesia: The site for local anesthesia

Equipment
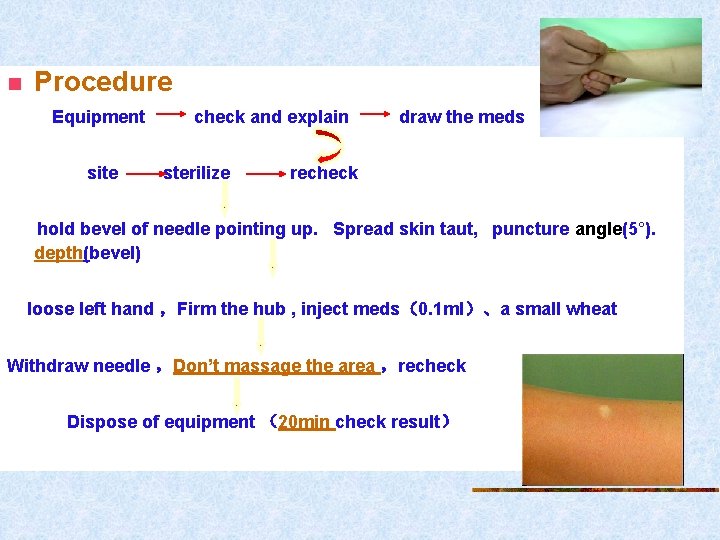
n Procedure Equipment site check and explain sterilize draw the meds recheck hold bevel of needle pointing up. Spread skin taut, puncture angle(5°). depth(bevel) loose left hand ,Firm the hub , inject meds(0. 1 ml)、a small wheat Withdraw needle ,Don’t massage the area ,recheck Dispose of equipment (20 min check result)

Cautions! n n n Follow the three checks and seven rights policy and sterile technique principles strictly Ban sterilizing the skin with tincture of iodine Ban embrocating time and again when sterilizing the skin Ban massaging the injection site after withdrawing the needle Don’t leave the ward until the test result is checked
Subcutaneous or Hypodermic : SQ or H n n Definition n involve placing drugs into the loose connective tissue under the dermis. Purpose n To inject medications that need to produce effect within given time but cannot be administered orally n To inject vaccine n To give local anesthesia
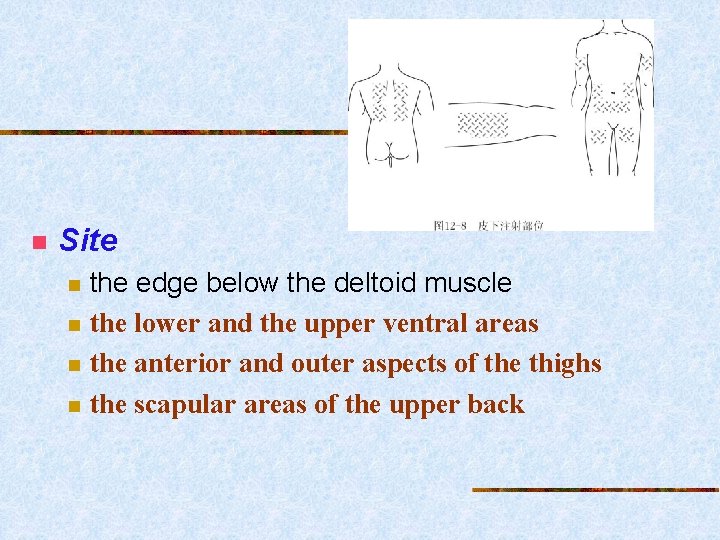
n Site n n the edge below the deltoid muscle the lower and the upper ventral areas the anterior and outer aspects of the thighs the scapular areas of the upper back
n Common medications n n vaccines, preoperative medications, narcotics, insulin, and heparin < 2 ml
n Equipment and procedure
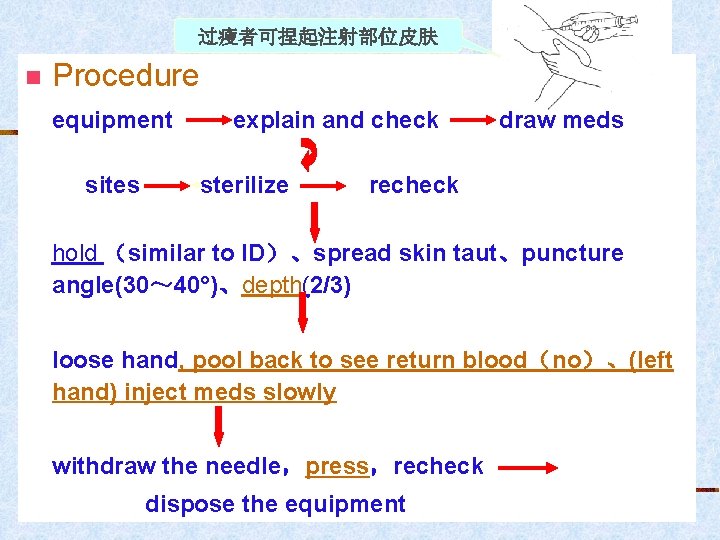
过瘦者可捏起注射部位皮肤 n Procedure equipment sites explain and check sterilize draw meds recheck hold (similar to ID)、spread skin taut、puncture angle(30~ 40°)、depth(2/3) loose hand, pool back to see return blood(no)、(left hand) inject meds slowly withdraw the needle,press,recheck dispose the equipment
Cautions! n n n Follow the checks policy and sterile principle strictly Irritating solutions and large volumes of drugs are inappropriately taken by SQ Rotate injection sites frequently Insertion angle is less than 45° Use 1 ml syringe when injecting medications lower 1 ml
Intramuscular Injections n Definition n n the method to inject certain medication solutions into muscles faster drug absorption than subcutaneous less danger of causing tissue damage Purpose n n n Inject medications inappropriately taken by mouth Inject medications inappropriately administered by subcutaneous injection Inject irritating medications
• site n n n Generally, the site should have well developed muscles, being away from large nerves, bones, and with no blood vessels under the location, and away from infection, necrosis, bruising, or abrasions in the surface Dorsogluteal muscle Ventrogluteal muscle site Vastus lateralis muscle site Deltoid muscle site
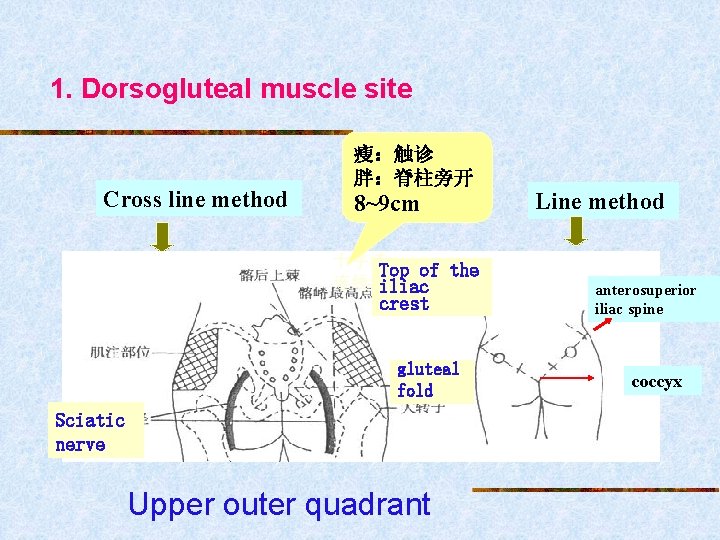
1. Dorsogluteal muscle site Cross line method 瘦:触诊 胖:脊柱旁开 8~9 cm 十字法 Top of the 连线法iliac crest gluteal fold Sciatic nerve Upper outer quadrant Line method anterosuperior iliac spine coccyx
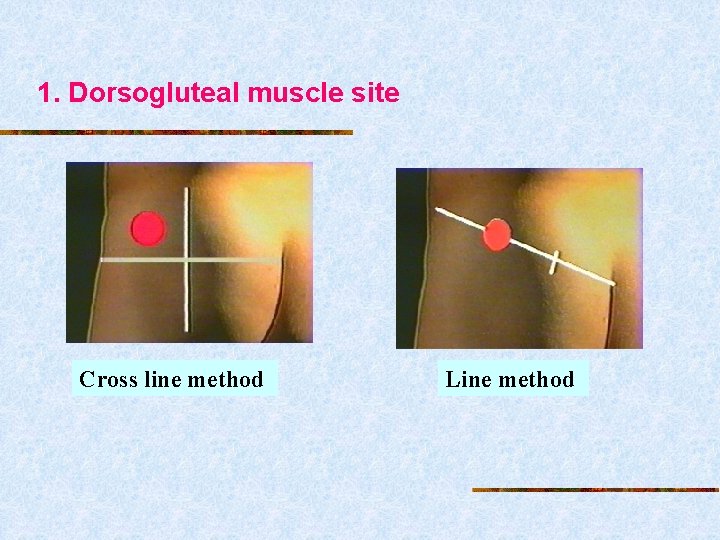
1. Dorsogluteal muscle site Cross line method Line method
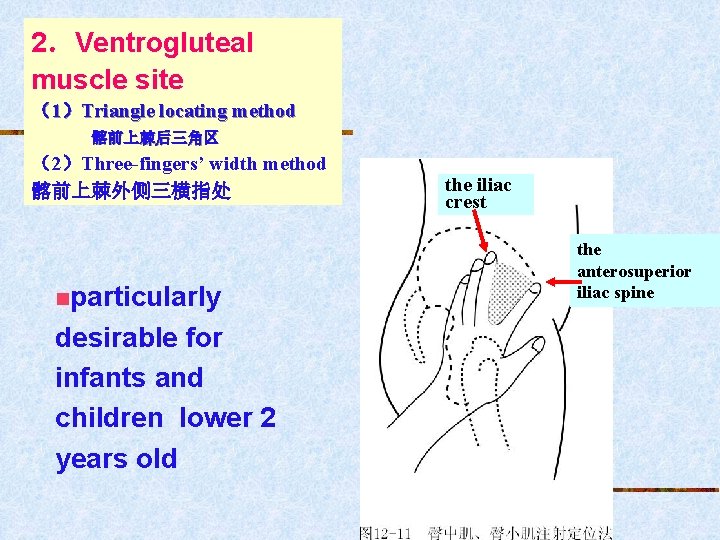
2.Ventrogluteal muscle site (1)Triangle locating method 髂前上棘后三角区 (2)Three-fingers’ width method 髂前上棘外侧三横指处 nparticularly desirable for infants and children lower 2 years old the iliac crest the anterosuperior iliac spine

2.Ventrogluteal muscle site
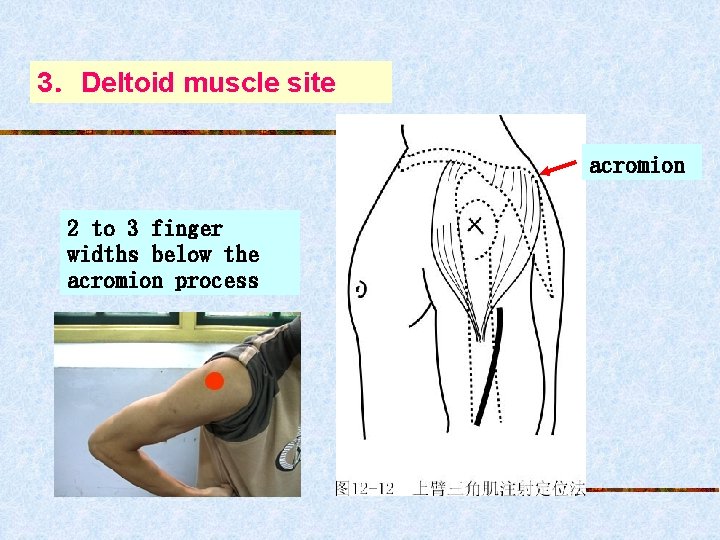
3.Deltoid muscle site acromion 2 to 3 finger widths below the acromion process
4.Vastus lateralis muscle site n on the anterior lateral aspect of the thighs n n From the site 10 cm below coxa joint to Knee joint particularly desirable for infants and children lower 2 years old
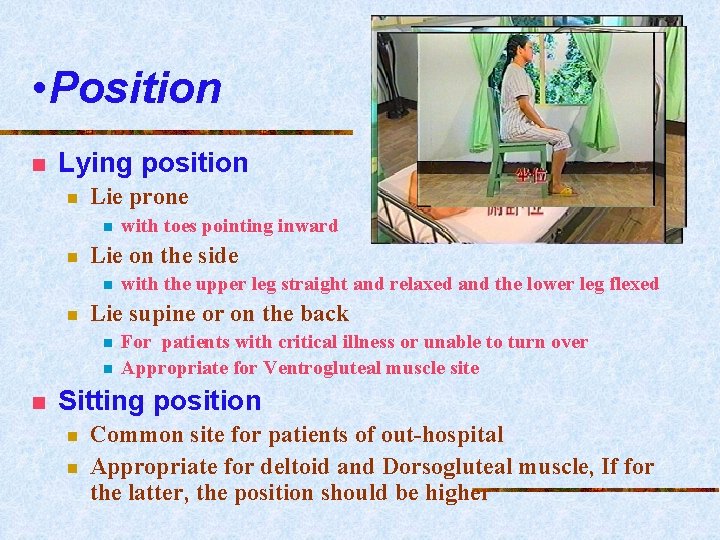
• Position n Lying position n Lie prone n n Lie on the side n n with the upper leg straight and relaxed and the lower leg flexed Lie supine or on the back n n n with toes pointing inward For patients with critical illness or unable to turn over Appropriate for Ventrogluteal muscle site Sitting position n n Common site for patients of out-hospital Appropriate for deltoid and Dorsogluteal muscle, If for the latter, the position should be higher
n procedures equipment sites explain and check sterilize aspirate meds recheck Hold as dart、tighten skin、puncture angle (90°)、 depth(2/3 of needle) loose left hand、pool back to see return blood(no)、 (left hand) inject meds slowly withdraw the needle,press,recheck dispose the equipment
Cautions! n n n Once broken, the nurse should ask the client keep the position, steady the local tissue, take out the needle by using sterile forceps or ask a surgical doctor for help Ban piercing all the shaft into the tissue, avoiding the needle is broken Rotate sites for patients with long term injection, and select thin and long needle Ban selecting dorsogluteal muscle site for children lower 2 years old because they don’t well developed
Intravenous Injections n Definition n the method to administer medications into vein directly the most rapid and complete absorption of medication cause an immediate and critical response
n Purpose n n To inject medication which are not suitable for other routes , such as irritating medications To inject drugs or dyestuffs to diagnose diseases. To get desired effect rapidly, especially for the client with critical illness To get blood sampling
• sites n n n peripheral superficial veins of the limbs Scalp veins of pediatric clients femoral vein
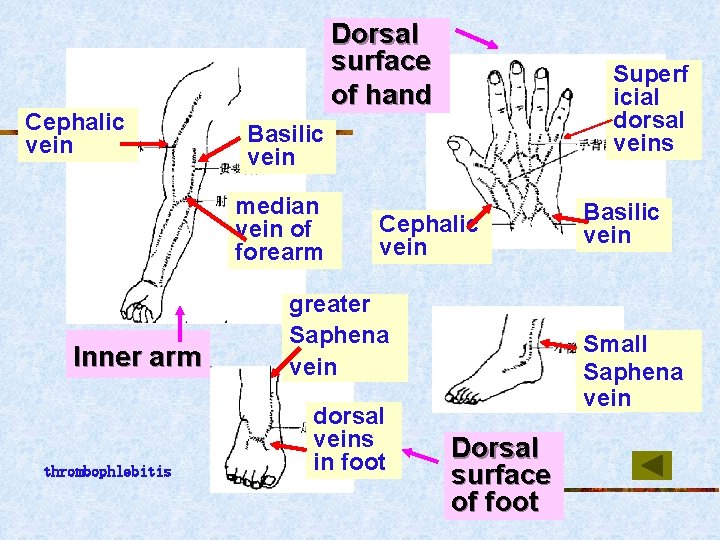
Cephalic vein Dorsal surface of hand Basilic vein median vein of forearm Inner arm thrombophlebitis Superf icial dorsal veins Cephalic vein greater Saphena vein dorsal veins in foot Basilic vein Small Saphena vein Dorsal surface of foot
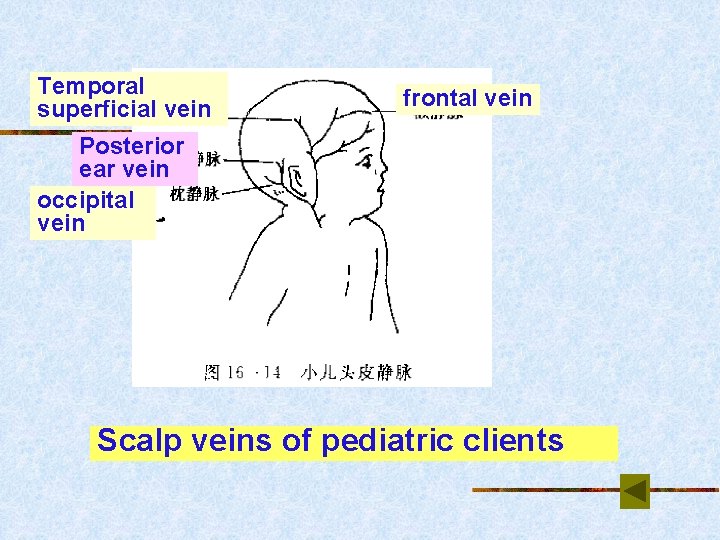
Temporal superficial vein frontal vein Posterior ear vein occipital vein Scalp veins of pediatric clients
• Procedures: equipment explain and check aspirate meds sites Tourniquet clench the hand sterilize recheck Hold syringe、tighten skin,anchor vein、puncture angle(15~30°)、 depth(blood return),Lower the needle until it is nearly parallel to the skin , advance needle Two loose(Release the tourniquet and unclench the hand ), one anchor needle、 (left hand)inject meds slowly observe response withdraw needle,press or flex elbow, recheck dispose equipment Vein in limbs injection
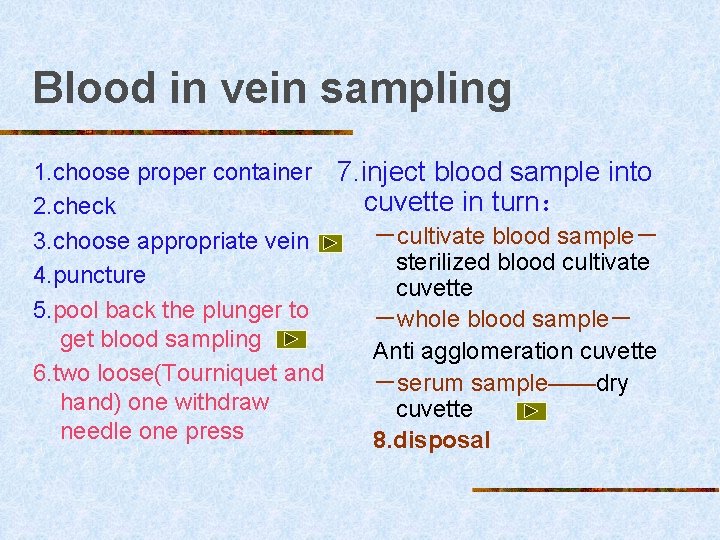
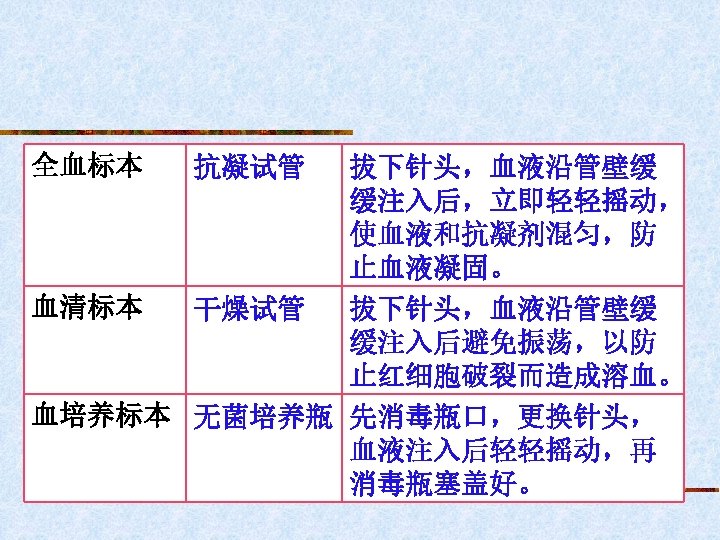
Blood in vein sampling 1. choose proper container 7. inject blood sample into cuvette in turn: 2. check -cultivate blood sample- 3. choose appropriate vein sterilized blood cultivate 4. puncture cuvette 5. pool back the plunger to -whole blood sample- get blood sampling Anti agglomeration cuvette 6. two loose(Tourniquet and -serum sample——dry hand) one withdraw cuvette needle one press 8. disposal
choose appropriate vein n Ban fetching the blood sample from the veins where intravenous transfusion or blood transfusion is.
Volume of sample n general cultivate sample 5 ml n n Sub-acute infectional endocarditis 10~ 15 ml Whole blood and serum: general 2 ml
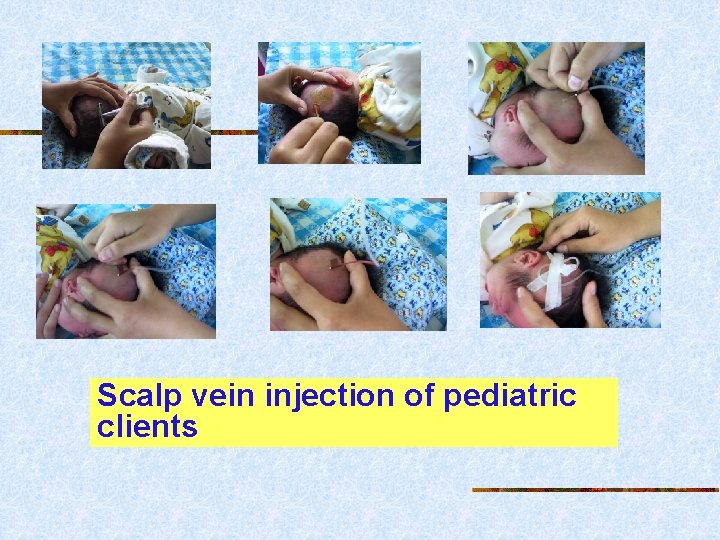
Scalp vein injection of pediatric clients
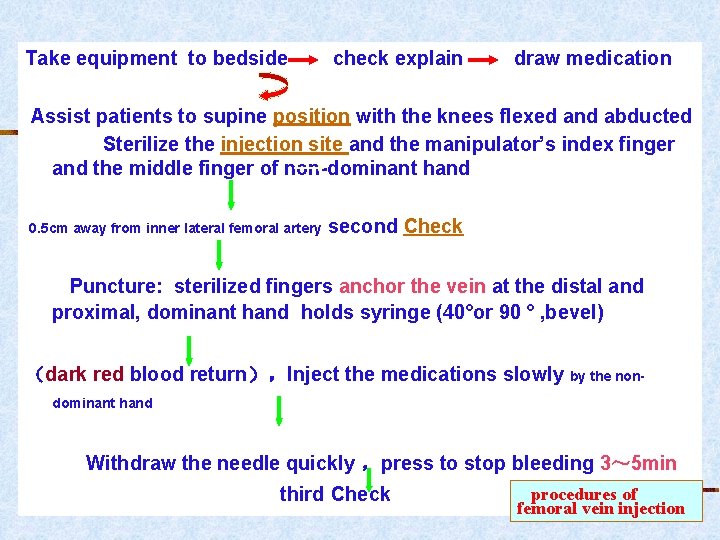
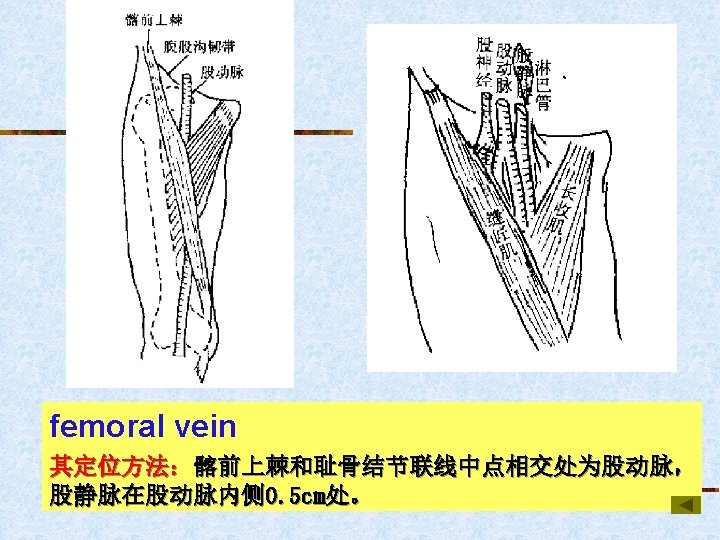
Take equipment to bedside check explain draw medication Assist patients to supine position with the knees flexed and abducted Sterilize the injection site and the manipulator’s index finger and the middle finger of non-dominant hand 0. 5 cm away from inner lateral femoral artery second Check Puncture: sterilized fingers anchor the vein at the distal and proximal, dominant hand holds syringe (40°or 90 ° , bevel) (dark red blood return),Inject the medications slowly by the nondominant hand Withdraw the needle quickly ,press to stop bleeding 3~ 5 min third Check procedures of femoral vein injection
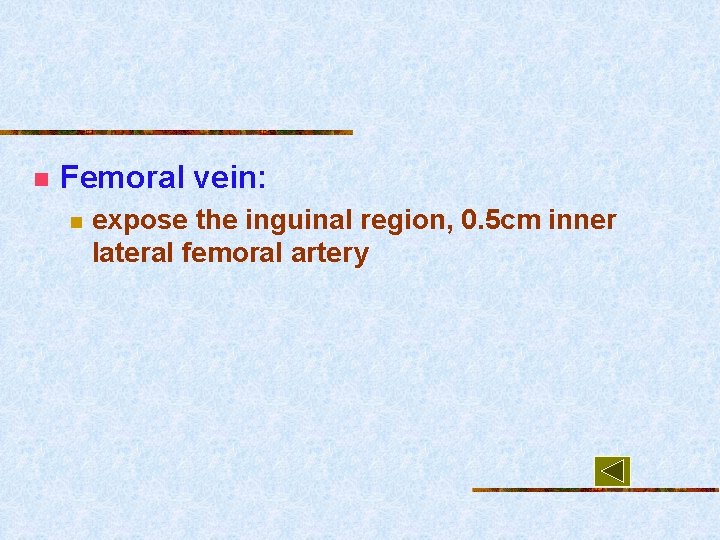
n Femoral vein: n expose the inguinal region, 0. 5 cm inner lateral femoral artery
Cautions! 1.Follow the three checks and seven rights policy and sterile technique principles strictly 2.Clinical guidelines for. Irritating vein selection drugs is injected slowly 3. Control the speed of injection according to age of client and nature of medication 4. Bis injectional method
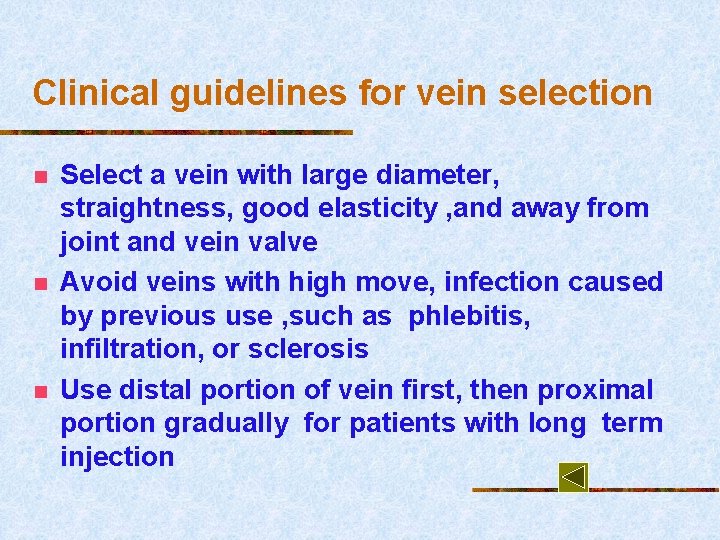
Clinical guidelines for vein selection n Select a vein with large diameter, straightness, good elasticity , and away from joint and vein valve Avoid veins with high move, infection caused by previous use , such as phlebitis, infiltration, or sclerosis Use distal portion of vein first, then proximal portion gradually for patients with long term injection
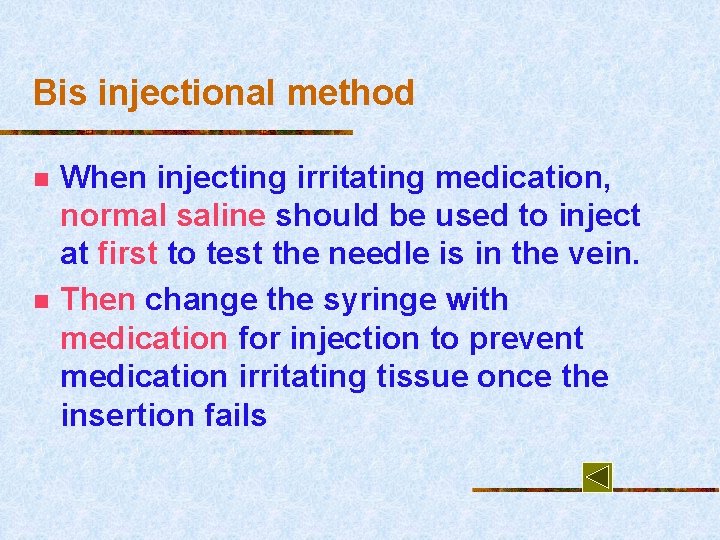
Bis injectional method n n When injecting irritating medication, normal saline should be used to inject at first to test the needle is in the vein. Then change the syringe with medication for injection to prevent medication irritating tissue once the insertion fails
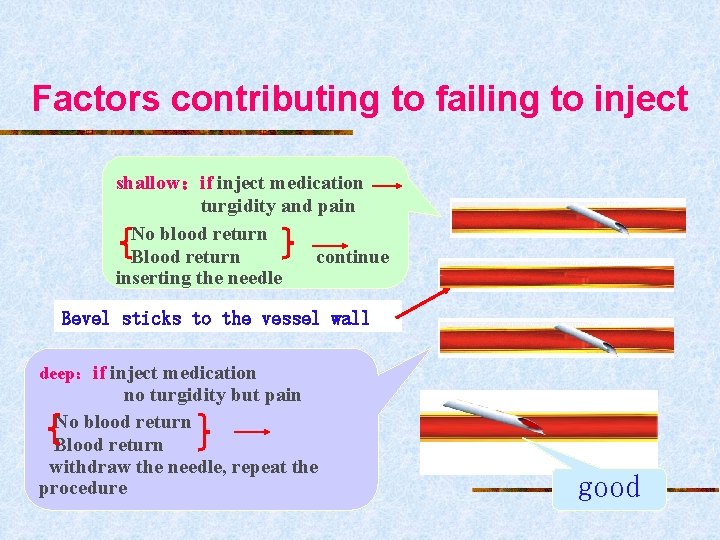
Factors contributing to failing to inject shallow:if inject medication turgidity and pain No blood return Blood return continue inserting the needle Bevel sticks to the vessel wall deep:if inject medication no turgidity but pain No blood return Blood return withdraw the needle, repeat the procedure good
The key to venipuncture for special clients n n 1.Obese patients n Vein is deep but stable n palate the vein clearly, sterilize the index finger of nondominant hand, increase angle degree of venipuncture( 30°~ 40°),insert the needle from the site above the vein 2.Aged patients n vein is superficial and fragile but unstable(easily moved) n so it is essential to anchor the vein from the distal and proximal portions before venipuncture
n 3. Severely dehydrated patients n n n Vein may collapse Applying warm compresses and light tapping and massage over the vein may foster venous dilation well 4. Patients with edema n n Vein may be seen unclearly Massage skin above tended vein may expose the vein
Arterial Injection and blood sampling n n n n Definition the nursing skill to inject medications into artery and collect arterial blood as specimen. Common sites common carotid artery: illness in head and face humerus artery( 肱 动 脉 ) and subclavian artery : illness in superior limb and chest femoral artery: illness in inferior limb and abdomen Radial artery(桡动脉)
• Purposes n n 1. To get arterial blood sample, Arterial Blood Gases (ABGs) 2. To prepare for some special test, for example, cerebral angiography 3. To give some medications for local chemotherapy 4. To make arterial blood transfusion with high tension,in order to rescue patients with shock
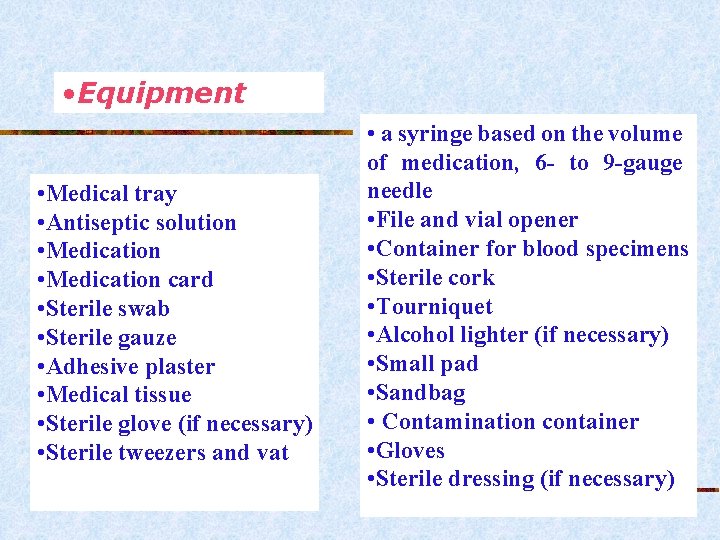
• Equipment • Medical tray • Antiseptic solution • Medication card • Sterile swab • Sterile gauze • Adhesive plaster • Medical tissue • Sterile glove (if necessary) • Sterile tweezers and vat • a syringe based on the volume of medication, 6 - to 9 -gauge needle • File and vial opener • Container for blood specimens • Sterile cork • Tourniquet • Alcohol lighter (if necessary) • Small pad • Sandbag • Contamination container • Gloves • Sterile dressing (if necessary)
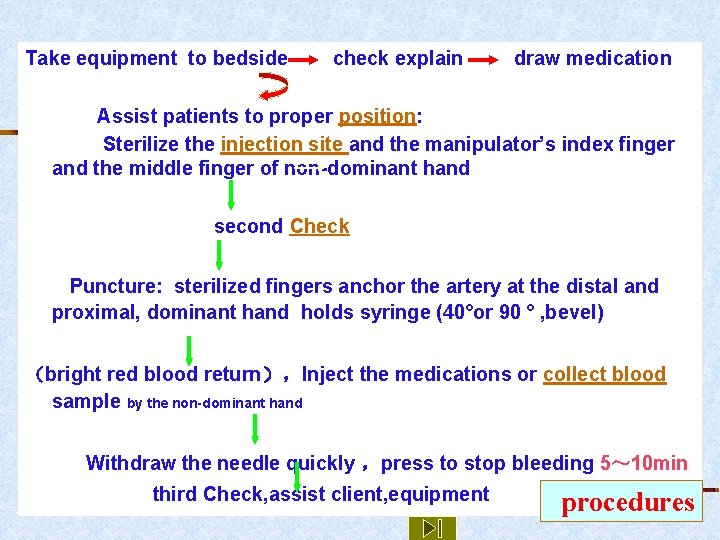
Take equipment to bedside check explain draw medication Assist patients to proper position: Sterilize the injection site and the manipulator’s index finger and the middle finger of non-dominant hand second Check Puncture: sterilized fingers anchor the artery at the distal and proximal, dominant hand holds syringe (40°or 90 ° , bevel) (bright red blood return),Inject the medications or collect blood sample by the non-dominant hand Withdraw the needle quickly ,press to stop bleeding 5~ 10 min third Check, assist client, equipment procedures
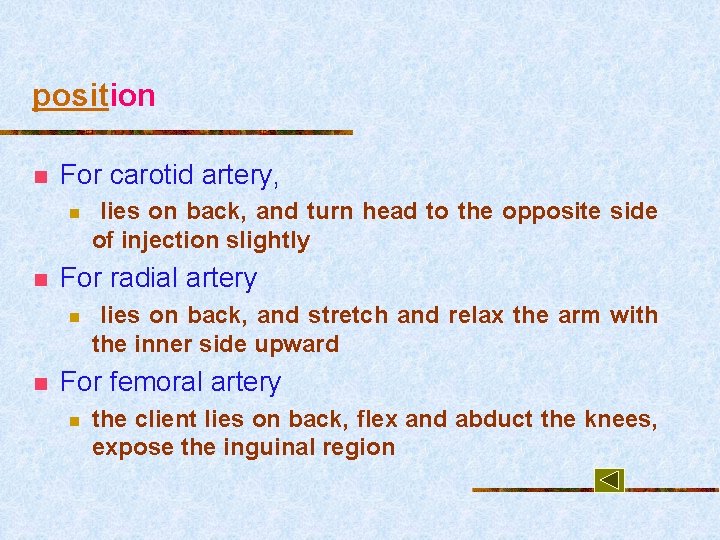
position n For carotid artery, n n For radial artery n n lies on back, and turn head to the opposite side of injection slightly lies on back, and stretch and relax the arm with the inner side upward For femoral artery n the client lies on back, flex and abduct the knees, expose the inguinal region
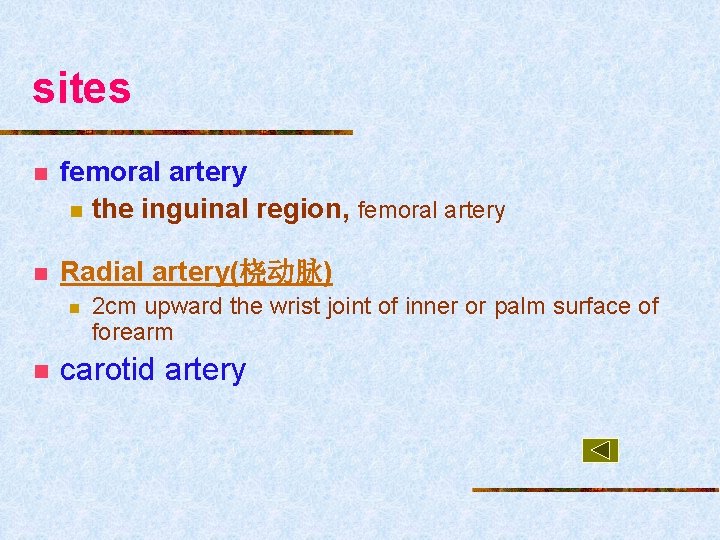
sites n femoral artery n the inguinal region, femoral artery n Radial artery(桡动脉) n n 2 cm upward the wrist joint of inner or palm surface of forearm carotid artery
Check_equipment n Before collecting blood sample, the nurse should aspirate 0. 5 ml of heparin (1: 500), and spread it evenly on the inside wall of barrel, then eject residual solution, to prevent blood agglutination
collect blood sample n n Blood volume: 0. 1~1 ml If blood sample is used for Arterial Blood Gases (ABGs), as soon as the needle is withdrawn, it should be inserted into a cork immediately. Roll the syringe in palms.
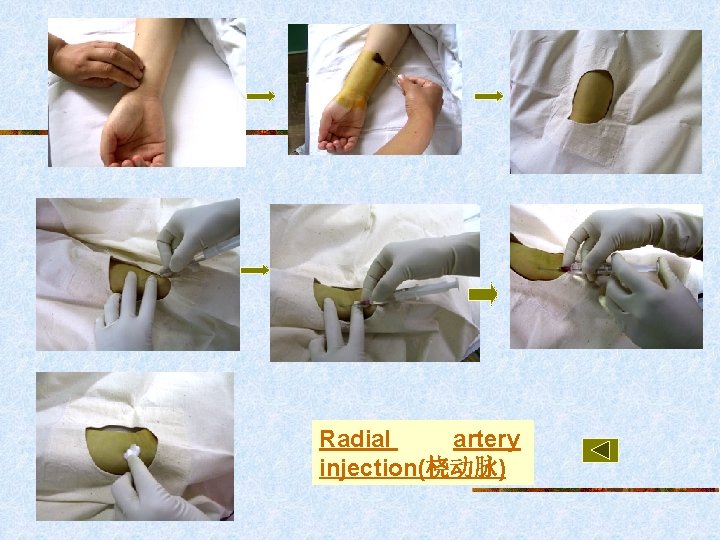
Radial artery injection(桡动脉)
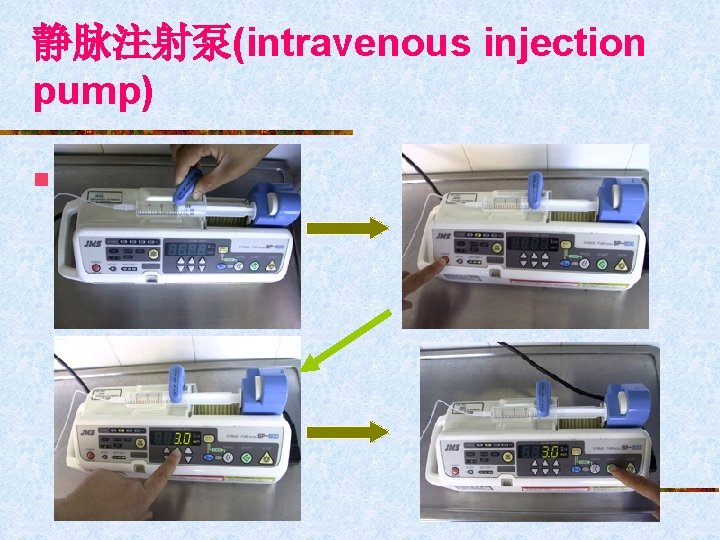
静脉注射泵(intravenous injection pump) n 图片CAI课件
Section 4 Inhalation Administration
Inhalation Administration n Concept n n the process that medications administered with inhalers are dispersed into an aerosol spray or mist that penetrates lung airways by nose or mouth Characteristics n n Local and systemic effects Rapid absorption, small dose, light adverse effects
Common medications n bronchodilators(支气管扩张剂) n n Eliminate bronchospasm:氨茶碱,沙丁胺醇 expectorants(祛痰剂): α-糜蛋白酶 decongestants (解除充血剂):Dex Antibiotics :庆大霉素、卡那霉素
Purpose n n To moisturize the airway To prevent and treat infection of respiratory system n n n bronchitis (支气管炎), Bronchiectasis(支气管 扩张),pneumonia, pulmonary empyema(肺 脓肿), pulmonary tuberculosis To relieve airway obstruction bronchial asthma (哮喘), or bronchitis (支气 管炎)
Common types n n ultrasonic nebulization oxygen nebulization handheld nebulization, Compressed nebulization
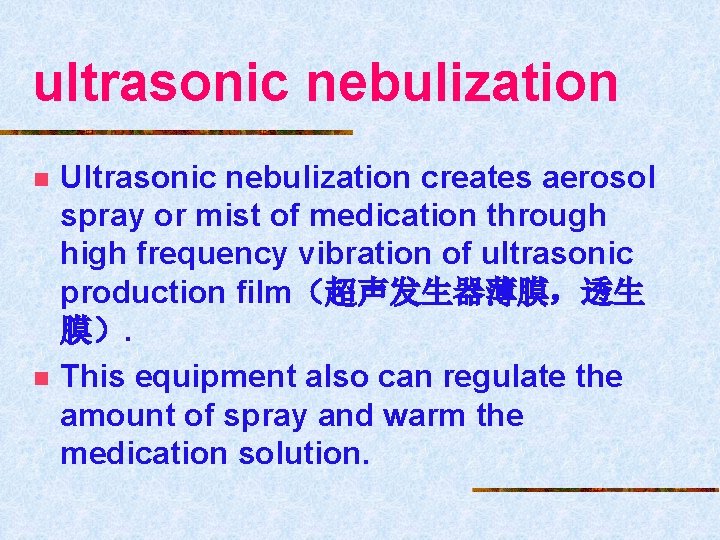
ultrasonic nebulization n n Ultrasonic nebulization creates aerosol spray or mist of medication through high frequency vibration of ultrasonic production film(超声发生器薄膜,透生 膜). This equipment also can regulate the amount of spray and warm the medication solution.
Equipment Ultrasonic nebulizers medications
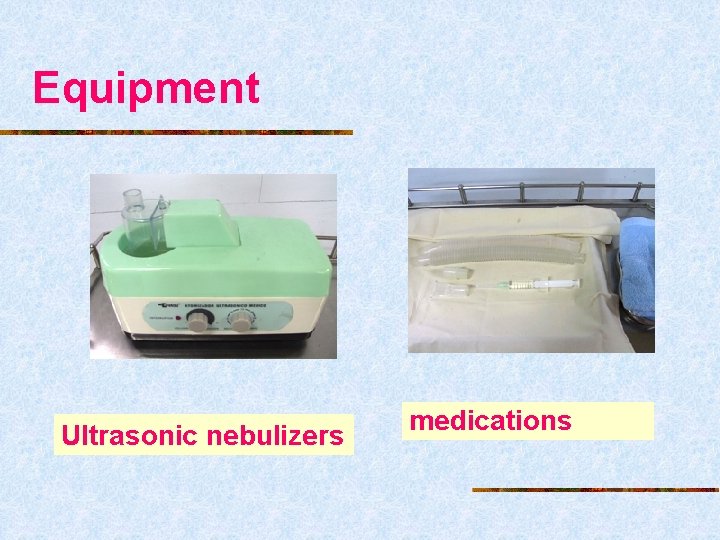
Atomization tank, entrant sound membrane Screwed pipe and mouthpiece Indicator light Power and volume switch timer Ultrasonic generator Water flume, crystal transducer An ultrasonic nebulizer
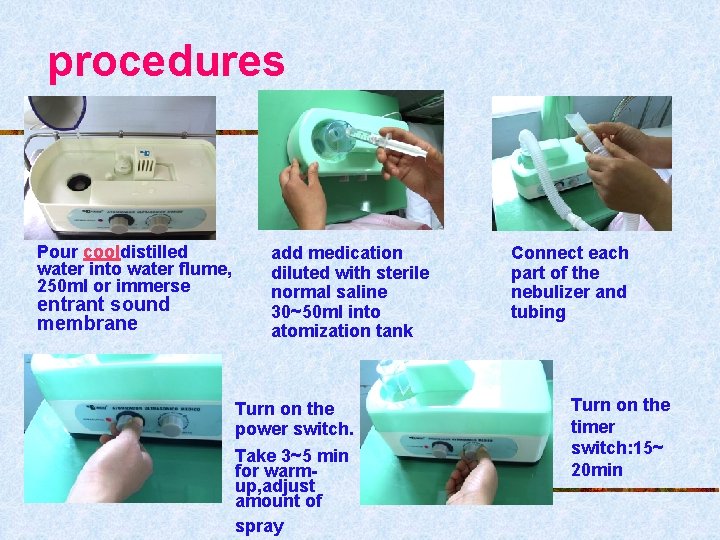
procedures Pour cooldistilled water into water flume, 250 ml or immerse entrant sound membrane add medication diluted with sterile normal saline 30~50 ml into atomization tank Turn on the power switch. Take 3~5 min for warmup, adjust amount of spray Connect each part of the nebulizer and tubing Turn on the timer switch: 15~ 20 min
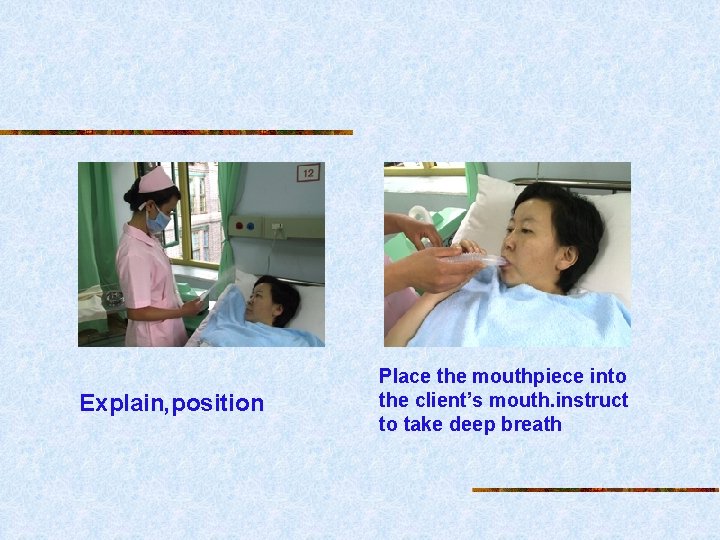
Explain, position Place the mouthpiece into the client’s mouth. instruct to take deep breath
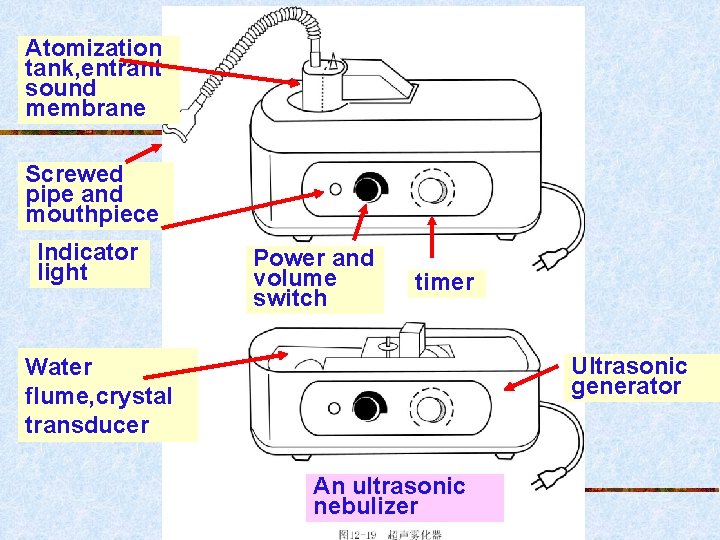
oxygen nebulization n Oxygen nebulization is accomplished by using the force of an oxygen stream or compressed air passed through the fluid in a nebulizer or an atomizer (喷雾 器).
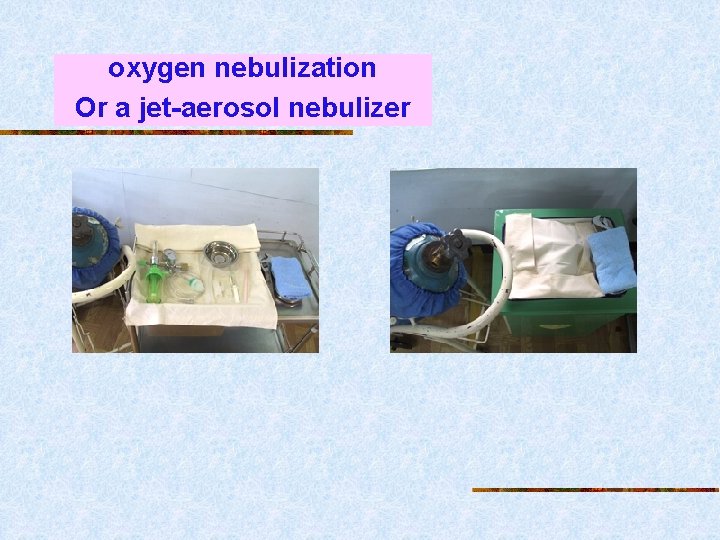
oxygen nebulization Or a jet-aerosol nebulizer
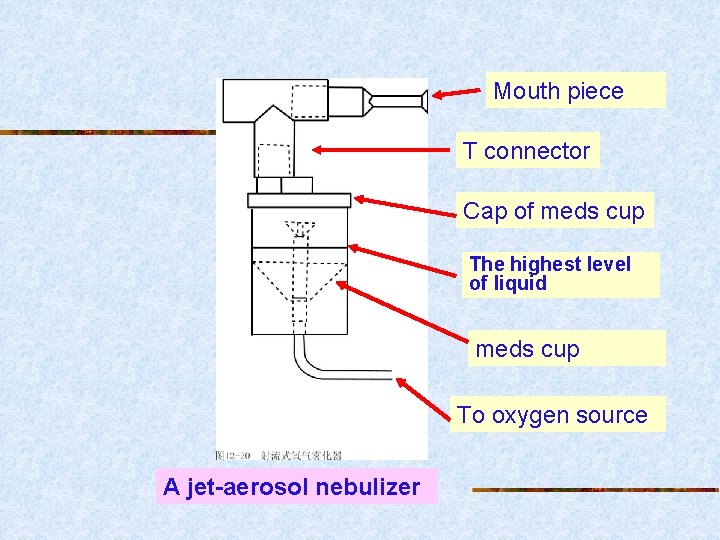
Mouth piece T connector Cap of meds cup The highest level of liquid meds cup To oxygen source A jet-aerosol nebulizer
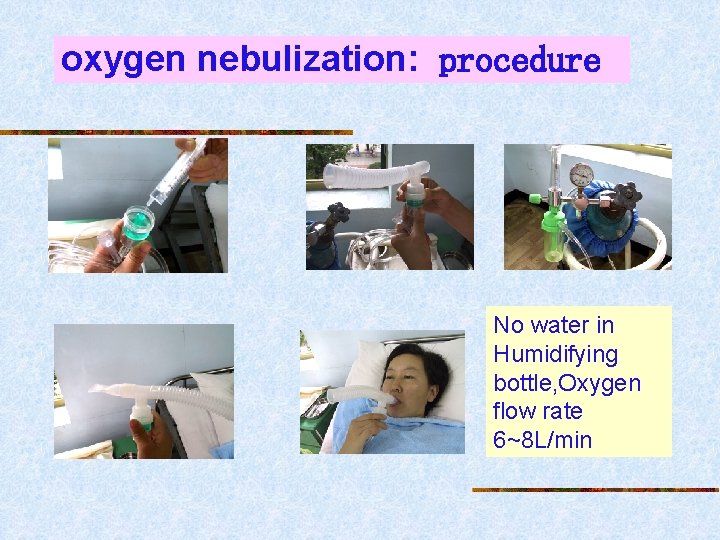
oxygen nebulization: procedure No water in Humidifying bottle, Oxygen flow rate 6~8 L/min
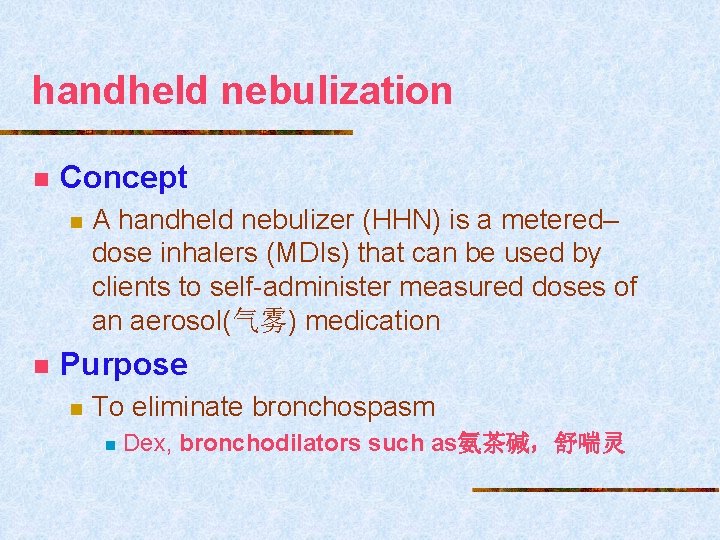
handheld nebulization n Concept n n A handheld nebulizer (HHN) is a metered– dose inhalers (MDIs) that can be used by clients to self-administer measured doses of an aerosol(气雾) medication Purpose n To eliminate bronchospasm n Dex, bronchodilators such as氨茶碱,舒喘灵

handheld nebulization _With Areochamber Metered-Dose Inhalers See disk Inspire spray Hold breath 10 s expire 1~ 2 spray/次
Section 6 Topical Administration

Contents n n n Nasal Instillations Eye Instillations Ear Instillations Vaginal Instillations Rectal Instillations Skin Application
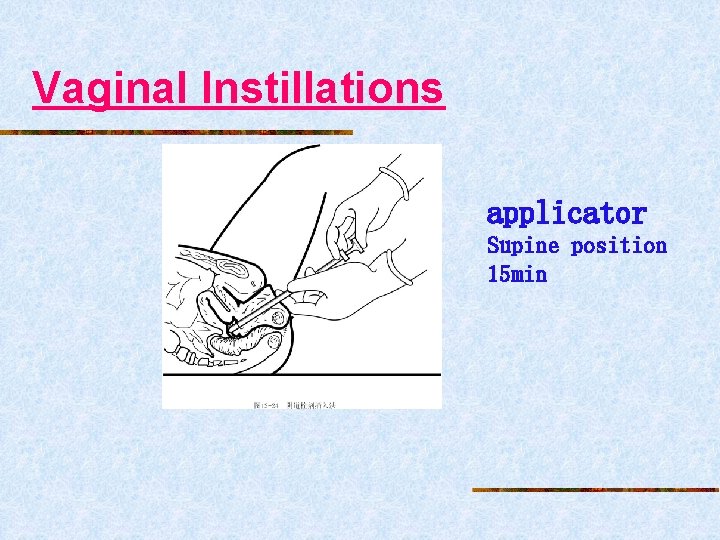
Vaginal Instillations applicator Supine position 15 min
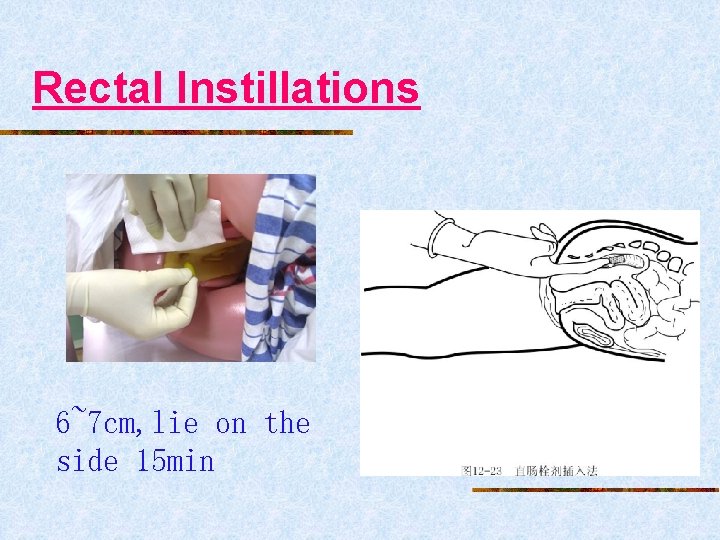
Rectal Instillations 6~7 cm, lie on the side 15 min
Skin Application Ointment or cream
tincture powder
Sublingual
Section 5 Medication anaphylaxis test
过敏反应(anaphylactic reaction/anaphylaxis) 过敏性休克(allergic/anaphylactic shock) medication history allergic history family allergic history (用药史、过敏史、家族史) 过敏试验(allergic/anaphylactic test) skin test (皮试) intradermal test(皮内注射试验)
What is anaphylactic reaction to medication? What is anaphylactic test of medication?
Characteristics of Anaphylactic Reaction to Medication allergy üAn pathological immune reaction üAnaphylaxis does not usually happen to patients who take the medication for the first time,but not absolutely. Øsensitized course Ønon typical exposure、cross reaction(隐性致敏、交叉反应)
Characteristics üAnaphylaxis only happens to a few persons with allergic habitus, with no relation to dosage. üThe different medications with similar chemical structure may lead to full or part cross reactions.
Medications prone to provoke anaphylaxis: n n Antibiotics : penicillin streptomycin cephalothin Biological products : TAT Narcotics: procaine Contrast medium: Iodide
Safely and correctly administering meds • Inquire • medication history • Allergic history • Family allergic history (用药史、过敏史、家族史) • Anaphylactic test before administeri ng meds
Anaphylactic test? • It is a clinical method to monitor whether the patients get immediate or delayed anaphylaxis after the small dosage medication came into the body through some approaches. • skin test: intradermal injection scratch test(划痕试验) • conjunctiva method(眼结膜试验法) • intravenous injection
üSkin test can detect the anaphylaxis, but sometimes the result is false negative. Why: Øinsufficient dosage ØHave taken anti-allergic medication before the test. (皮试。假阴性:计量小或服用抗过敏药)
contents 1. How to dispense the allergic reagent of penicillin and other common medications 2. To learn test method and determination of the test result 3. How to treat the anaphylactic reaction, especially allergic shock
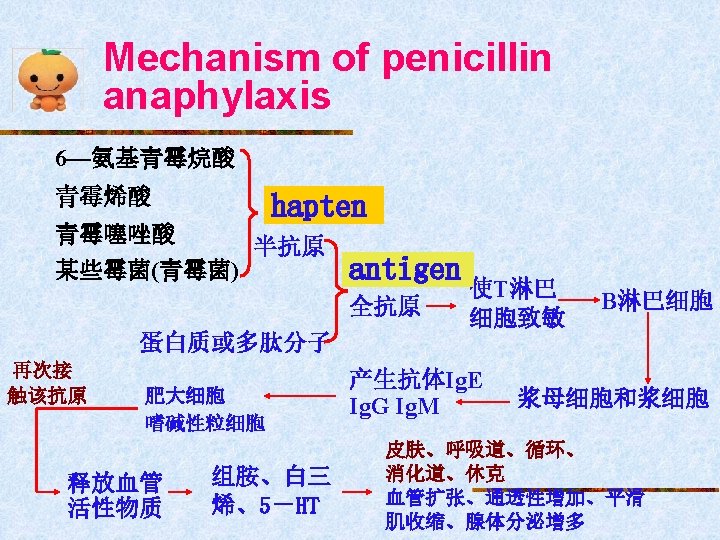
Part 1 Penicillin Anaphylactic Test n n Mechanism of penicillin anaphylaxis The clinical manifestations of penicillin anaphylaxis The treatment of penicillin allergic shock The method of penicillin anaphylactic test
The clinical manifestations of penicillin anaphylaxis n Anaphylactic shock n n n Respiratory failure symptoms Cardiovascular failure symptoms Central nervous system symptoms Cutaneous allergic symptoms Serum sickness reaction Anaphylaxis of organ and tissue n n n Cutaneous anaphylaxis Respiratory anaphylaxis digestive system anaphylaxis
The treatment of penicillin allergic shock • Emergency treatment on site • Stop medication immediately • Lie on the back, keep warm • Administering epinephrine immediately • 0. 1% epinephrine 1 ml H, every 0. 5 h repeatedly H or iv 0. 5 ml
treatment • Correct Hypoxia and improving respiration • Oxygen administration • If depressed respiration: • mouth-to-mouth artificial breathing • respiratory stimulants: nikethamide/lobeline • If laryngeal edema: • incision of trachea or intubation of trachea
treatment • Treating allergic shock • Dexamethasone 5~10 mg 25% glucose IV or • Hydrocortisone 200~400 mg 5%~10% glucose ivdrip • Anti-histamine medications: 异丙嗪 25~50 mg im、苯海拉明40 mg im
treatment • Improve cardiovascular function( correct shock): • Increase peripheral blood capacity • 10%GS, balanced solution ivdrip • dopamine or metaraminol • Cardiac arrest • cardiac compression • Observe the patient intensively and record information: • vital signs urine volume consciousness
The method of penicillin anaphylactic test Test objects: • First take medication (首次用药者) • Stop penicillin three days ago and reuse (停药 3天以上再用者) • The batch of the medication is changed (更换批号)
The method of penicillin anaphylactic test • The anaphylactic test reagent and its dispensing method • Method of anaphylactic test • Result determination
The anaphylactic test reagent Reagent: 200~ 500 u P/ml NS 0. 1 ml ID
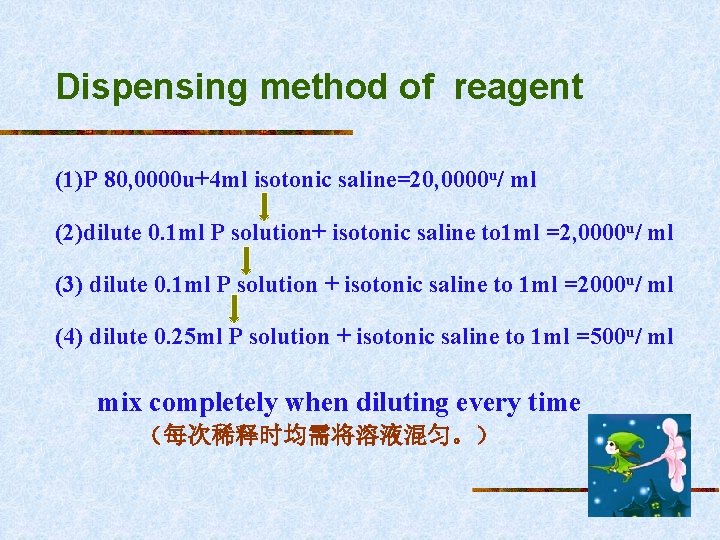
Dispensing method of reagent (1)P 80, 0000 u+4 ml isotonic saline=20, 0000 u/ ml (2)dilute 0. 1 ml P solution+ isotonic saline to 1 ml =2, 0000 u/ ml (3) dilute 0. 1 ml P solution + isotonic saline to 1 ml =2000 u/ ml (4) dilute 0. 25 ml P solution + isotonic saline to 1 ml =500 u/ ml mix completely when diluting every time (每次稀释时均需将溶液混匀。)
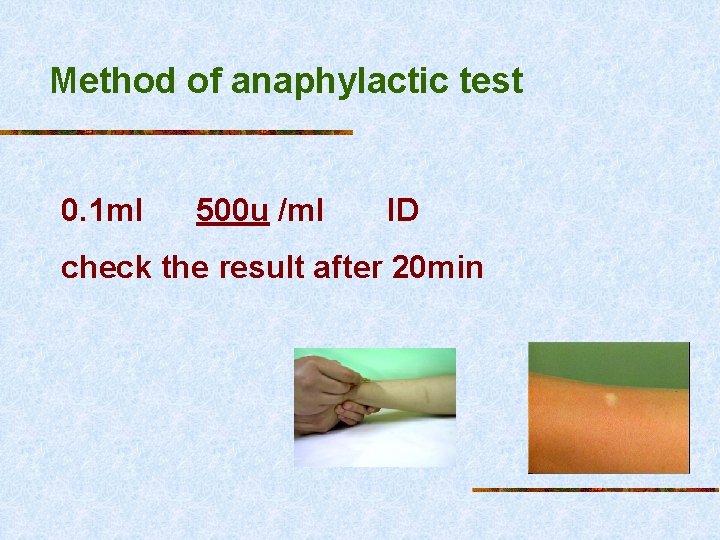
Method of anaphylactic test 0. 1 ml 500 u /ml ID check the result after 20 min
Result determination Negative result: There is no skin redness, swelling, blush and the patient has no uncomfortable feeling. (阴性:皮丘无改变,周围不红肿,无红晕, 病人无自觉症状。)
Positive result: • The wheal becomes large. • There is skin redness and swelling. • The diameter of the wheal is more than 1 cm, or there is pseudopodium. • The patient has pruritus feeling. • Dizziness, fluster, nausea may occur in severe cases, even anaphylactic shock. (阳性:局部皮丘隆起增大,出现红晕,直径大于1 cm,或周 围出现伪足、有痒感。严重时病人可出现头晕、心慌、恶心, 甚至过敏性休克。)
Cautions of penicillin administration n Inquire the patient’s medication history, allergic history and family allergic history before test. (皮试前应询问用药史、过敏史家族过敏史。) n Normal/isotonic saline is always used as menstruum to dissolve and dilute penicillin. (配制试验液的溶媒多采用生理盐水, 不用注射用水。) n Menstruum, syringe and needle used in dilute penicillin is banned to use in other medications. (配制试验液的溶媒、注射器、针头不宜交叉使用。)
Dispense allergic test reagent when used. The dosage and concentration of reagent is accurate. (试验液的浓度、剂量应准确,且应现用现配。) n Anti-histamine medications is banned in 24 h before test in case of false negative. (皮试前24 h禁用抗组织胺类药物,以免影响皮试反应结果) n Be ready for aids before, and keep epinephrine on hand. n (过敏试验前应准备好抢救物品,以备急救。)
n Keep close watch on the patient. (在进行皮内试验时应严密观察过敏反应,首次注射青霉素 者需观察 30 min后再离开。) n If positive, penicillin should be banned, and the nurse should report to the doctor. Record penicillin positive result on the doctor’s order sheet, medical record, injection card and bedside card, and inform the patient and his family of the result. (阳性结果者不用青霉素,并及时告诉医生,将阳性结果标 识在医嘱单、病历、注射卡、床头卡上。并告知病人及家 属。)
n If you doubt false positive,control experiment is made to exclude allergy induced by disinfector. (疑假阳性反应做对照试验,以排除消毒剂的影响)
Part II streptomycin anaphylactic test n Clinical n Twitch manifestation: because of deficient calcium (低钙抽搐) n Be similar to penicillin n Treatment 10%葡萄糖酸钙、5%氯化钙 n 其他同 penicillin n
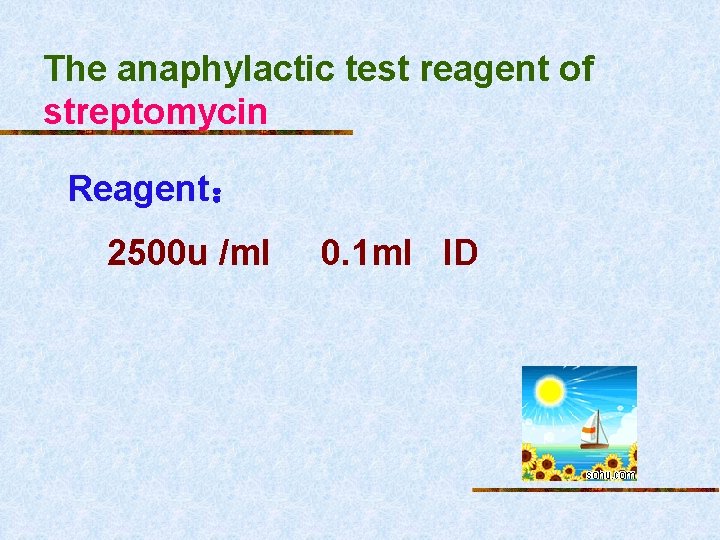
The anaphylactic test reagent of streptomycin Reagent: 2500 u /ml 0. 1 ml ID
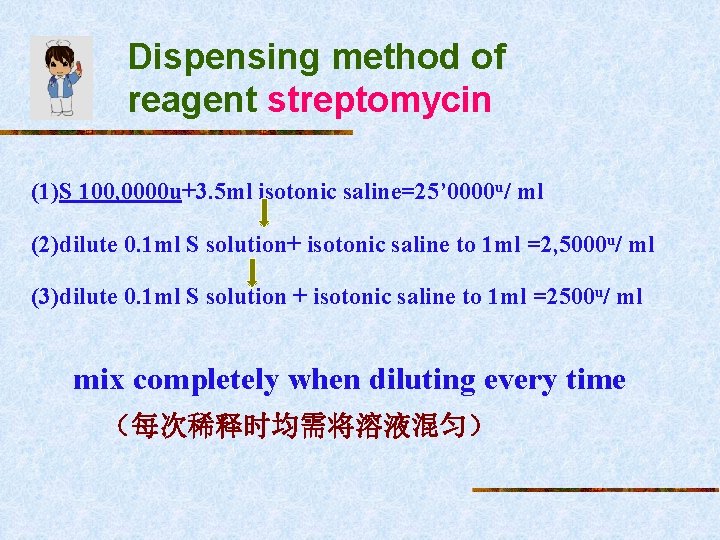
Dispensing method of reagent streptomycin (1)S 100, 0000 u+3. 5 ml isotonic saline=25’ 0000 u/ ml (2)dilute 0. 1 ml S solution+ isotonic saline to 1 ml =2, 5000 u/ ml (3)dilute 0. 1 ml S solution + isotonic saline to 1 ml =2500 u/ ml mix completely when diluting every time (每次稀释时均需将溶液混匀)
Method of anaphylactic test 0. 1 ml 2500 u/ ml ID check the result after 20 min
Result determination Be similar to penicillin
TAT(tetanus antitoxin) anaphylactic test n n n The cause of anaphylaxis The method of TAT anaphylactic test TAT desensitized injection
The cause of anaphylaxis n The immune serum of equine(马) n n n Neutralise tetanus toxin:prevent and cure Heterogeneous protein The clinical manifestation of anaphylaxis n n Fever, immediate or delayed serum sickness Allergic shock occasionally
The method of TAT anaphylactic test Test objects: • First take TAT (首次用药) • Stop therapy with TAT more than 1 week ago (停药 1周以上)
The method of TAT anaphylactic test • The anaphylactic test reagent and its dispensing method • Method of anaphylactic test • Result determination
The anaphylactic test reagent TAT Reagent: 150 u TAT/ml isotonic saline 0. 1 ml ID
Dispensing method of reagent TAT 1500 u(original solution) 0. 1 ml TAT 1500 u + isotonic saline to 1 ml =150 u/ml
Method of anaphylactic test 0. 1 ml 150 u/ml TAT ID check the result after 20 minute
Result determination of TAT Negative result: No local skin redness and swelling. No abnormal systemic reaction. (阴性: 局部皮丘无红肿,病人无全身异常反应)。
Determination criterion Positive result: • The wheal is red and swelling. • Induration with diameter larger than 1. 5 cm, • blushing with diameter larger than 4 cm, • Sometimes there is pseudopodium • The patient has pruritus feeling. • The systemic reaction is similar to that of penicillin and serum sickness is the most common. (阳性: 局部皮丘红肿,硬结直径大于1. 5 cm,红晕范围直径 大于4 cm,有时出现伪足或有痒感。全身过敏性反应表现与青 霉素过敏反应相似,以血清病型反应多见。)
TAT desensitized injection n Mechanism of desensitized injection n Object:Positive result and no substitute Concept:Divide the dosage into several smaller dosages and inject them separately and continuously in a short period time Mechanism:Neutralise and consume Ig. E gradually ,up to totally. n temporary desensitization n Desensitized injection method
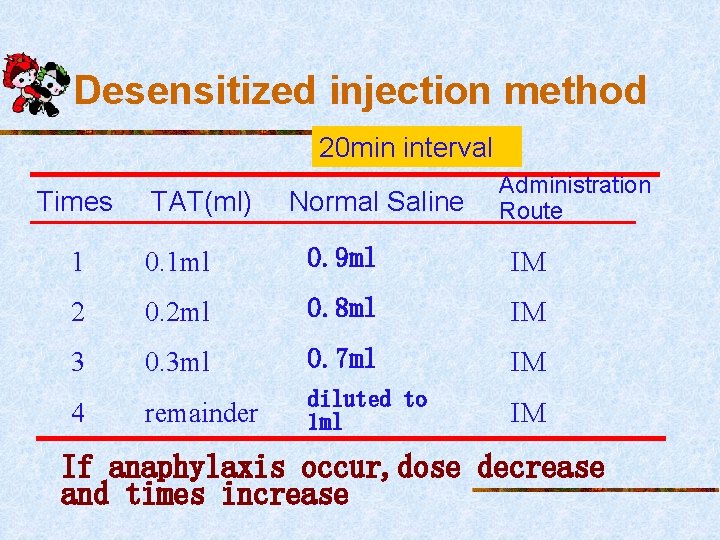
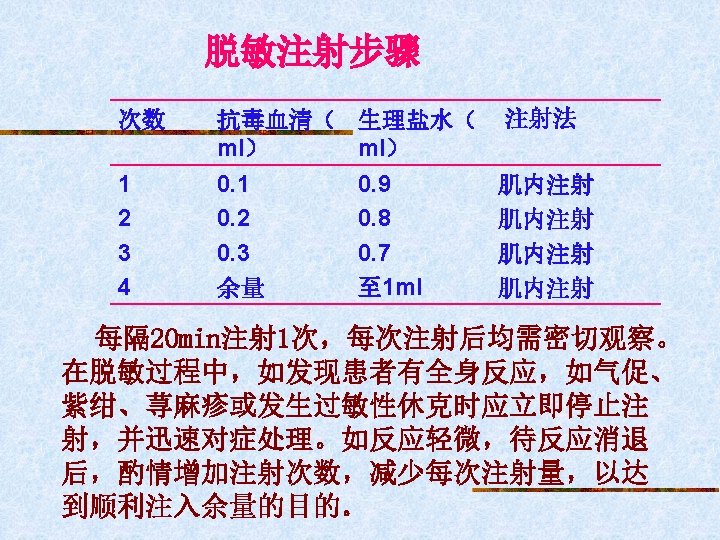
Desensitized injection method 20 min interval Times TAT(ml) Normal Saline Administration Route 1 0. 1 ml 0. 9 ml IM 2 0. 2 ml 0. 8 ml IM 3 0. 3 ml 0. 7 ml IM remainder diluted to 1 ml IM 4 If anaphylaxis occur, dose decrease and times increase
Part 4 Procaine(novocaine) anaphylactic test Test method: • First use procaine(首次用药者) • 0. 25% procaine solution 0. 1 ml ID • Check the result after 20 min • Result determination is similar to penicillin
Iodic Preparation Anaphylactic. Test n Test objects n n So if it is the first time to use them, anaphylactic test should be done 1 or 2 days before graphs with iodode. Method of Anaphylactic Test n n n Oral Administration Intradermal Injection Intravenous Injection
Determination criterion n Oral Administration n n If the symptoms of paralysis of mouth, dizziness, palpitation, nausea, and vomiting, or/and urticaria are present, the result is positive. Intradermal Injection n If local skin becomes red and swelling or sclerosis appears, with the diameter more than 1 cm, the result is positive.
n Intravenous Injection n If the blood pressure, pulse, respiration and face color of the client have changed, if the client has palpitation, mucous edema, nausea and vomiting, uritcaria and other discomforts, the result is positive.
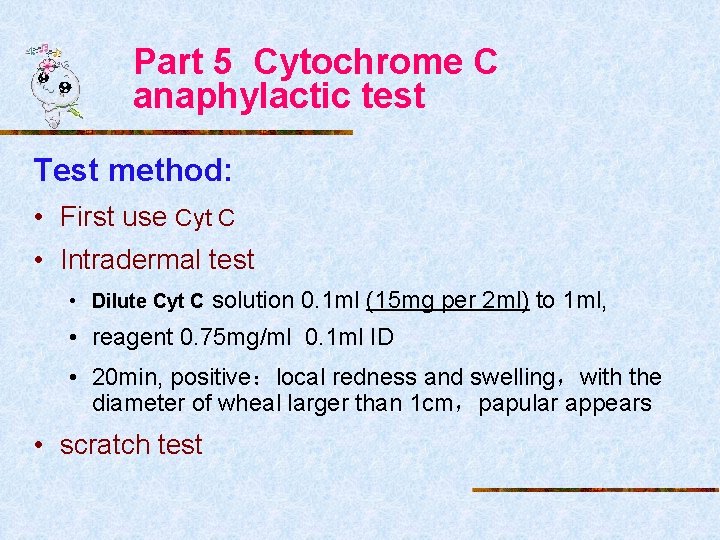
Part 5 Cytochrome C anaphylactic test Test method: • First use Cyt C • Intradermal test • Dilute Cyt C solution 0. 1 ml (15 mg per 2 ml) to 1 ml, • reagent 0. 75 mg/ml 0. 1 ml ID • 20 min, positive:local redness and swelling,with the diameter of wheal larger than 1 cm,papular appears • scratch test
Cytochrome C • scratch test • Put one drip of original Cyt C solution on the forearm • Make two scratches 0. 5 cm long and little bleeding deep with a sterile needle • 20 min, result determination is similar to ID
Part 6 Cephalosporin anaphylactic test n n Part cross-reaction between Cephalosporin and penicillin n The mechanism is similar to penicillin n They have the sameβ-lactam structure Test method : cephalothin(先锋霉素)
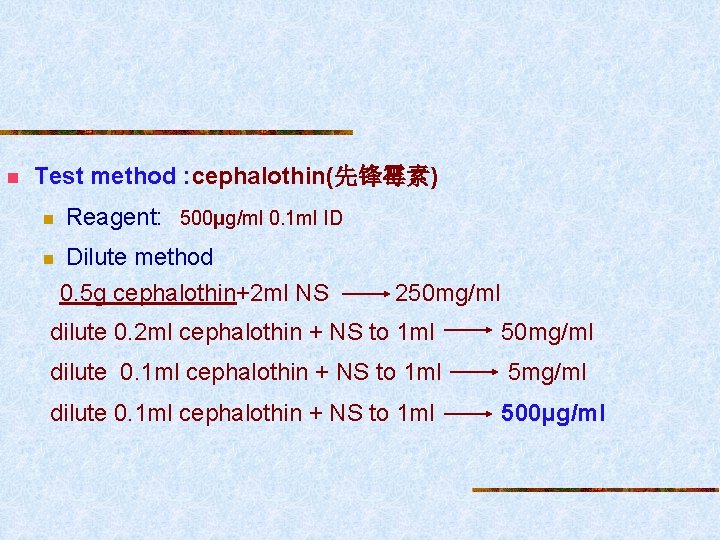
n Test method : cephalothin(先锋霉素) n n Reagent: 500μg/ml 0. 1 ml ID Dilute method 0. 5 g cephalothin+2 ml NS 250 mg/ml dilute 0. 2 ml cephalothin + NS to 1 ml 50 mg/ml dilute 0. 1 ml cephalothin + NS to 1 ml 500μg/ml

- Slides: 194