Chapter 11 Muscle Tissue Types and Characteristics of

- Slides: 98
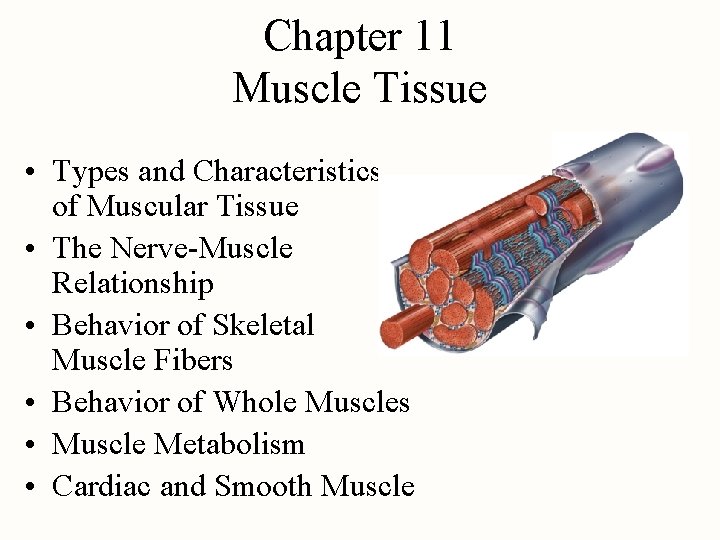
Chapter 11 Muscle Tissue • Types and Characteristics of Muscular Tissue • The Nerve-Muscle Relationship • Behavior of Skeletal Muscle Fibers • Behavior of Whole Muscles • Muscle Metabolism • Cardiac and Smooth Muscle
• Relate the form to the function of the molecular components of muscles. • Identify 3 types of muscle cells from pictures • Explain the mechanisms of contraction • Describe genetic components of muscle growth • Describe aspects of Muscular Dystrophy • Pump you up Objectives
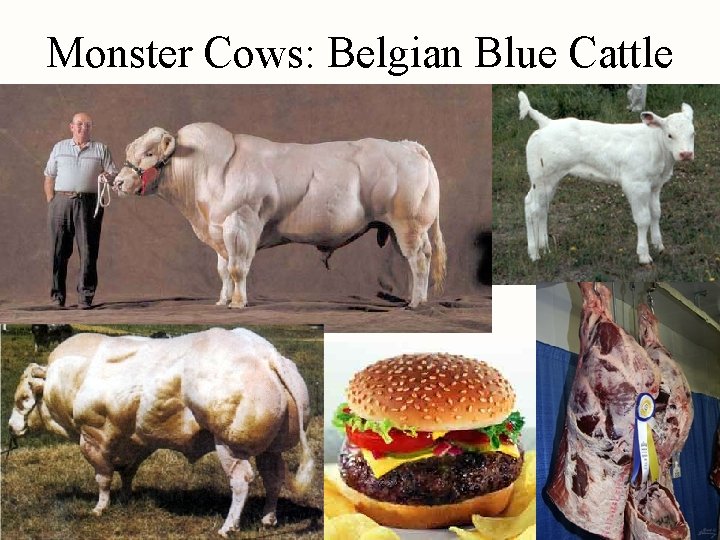
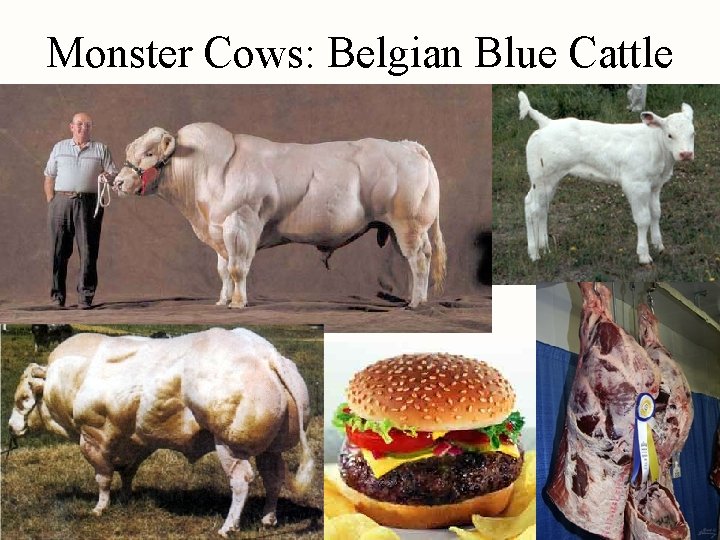
Monster Cows: Belgian Blue Cattle
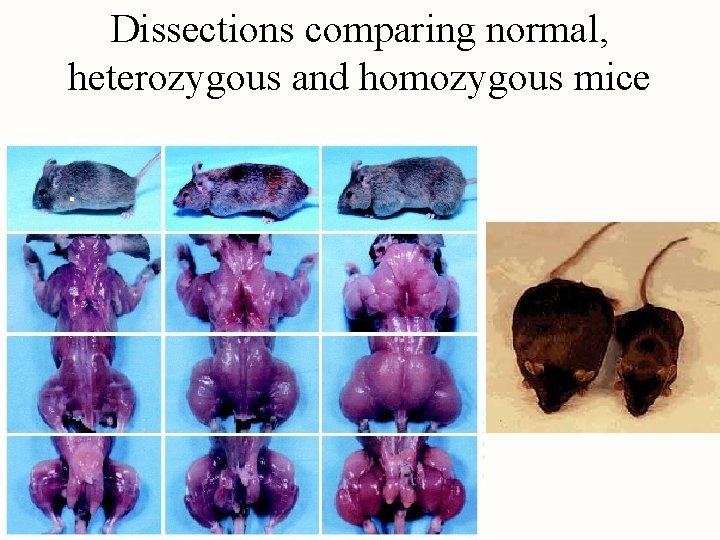
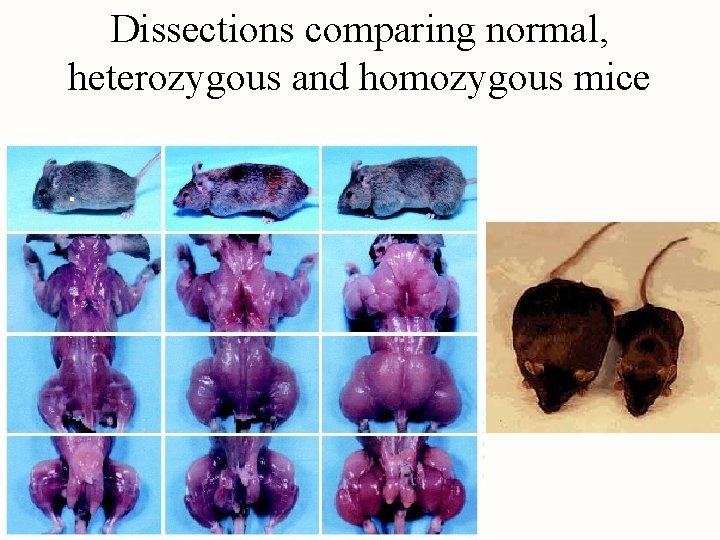
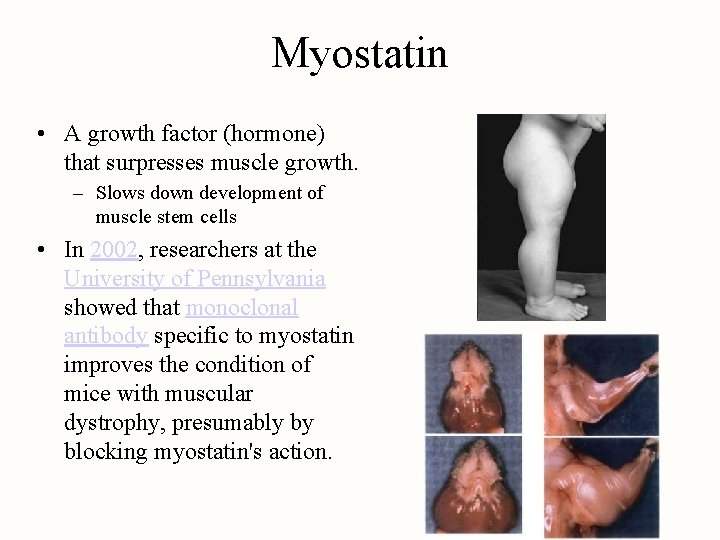
Dissections comparing normal, heterozygous and homozygous mice
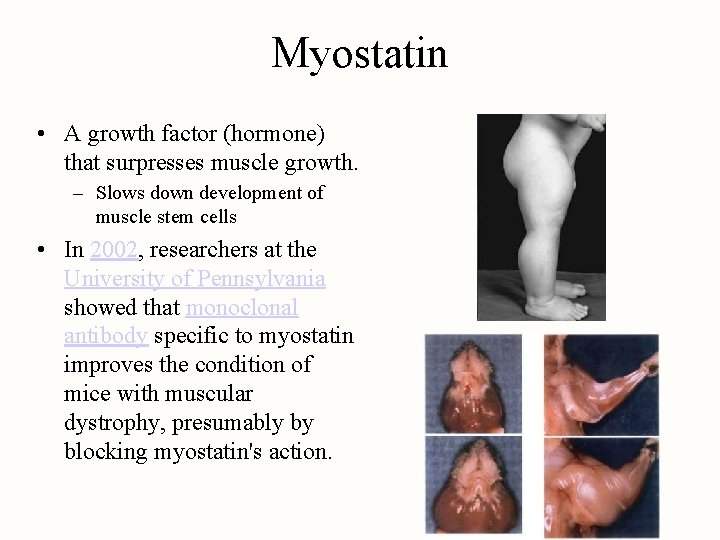
Myostatin • A growth factor (hormone) that surpresses muscle growth. – Slows down development of muscle stem cells • In 2002, researchers at the University of Pennsylvania showed that monoclonal antibody specific to myostatin improves the condition of mice with muscular dystrophy, presumably by blocking myostatin's action.
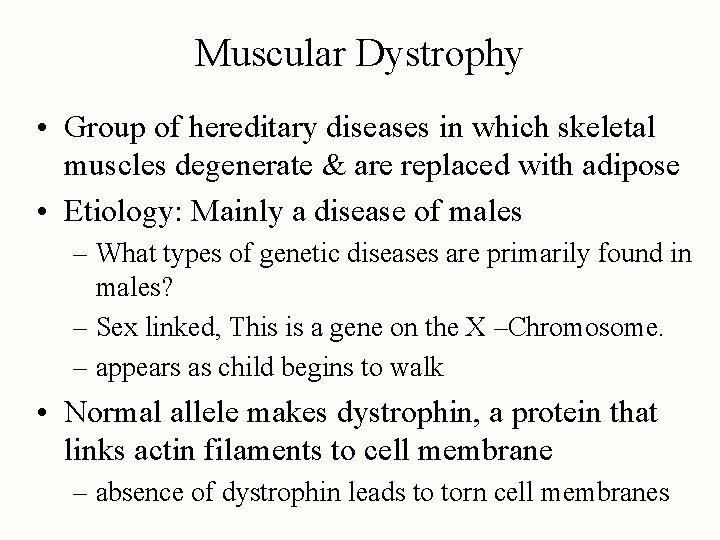
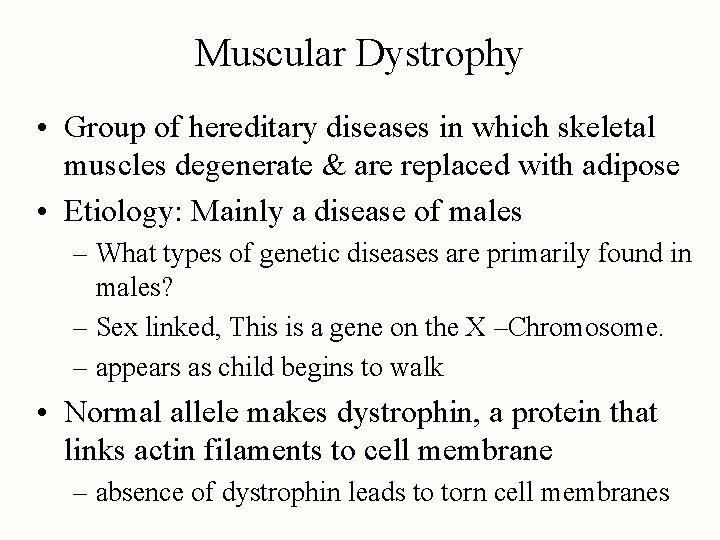
Muscular Dystrophy • Group of hereditary diseases in which skeletal muscles degenerate & are replaced with adipose • Etiology: Mainly a disease of males – What types of genetic diseases are primarily found in males? – Sex linked, This is a gene on the X –Chromosome. – appears as child begins to walk • Normal allele makes dystrophin, a protein that links actin filaments to cell membrane – absence of dystrophin leads to torn cell membranes
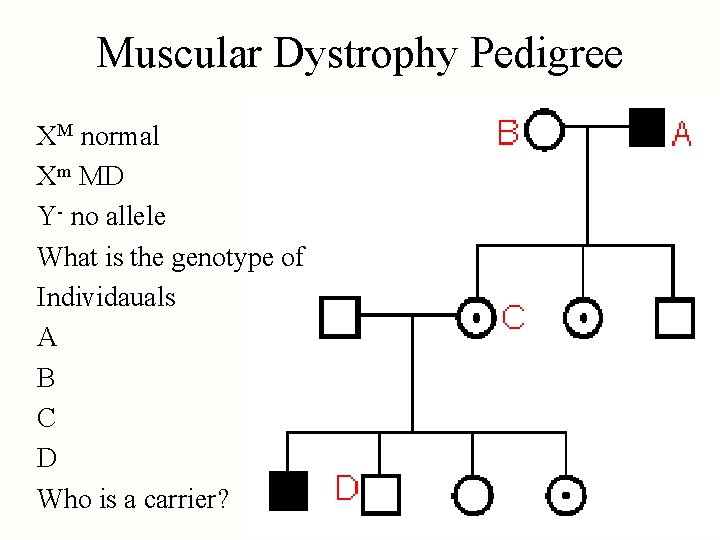
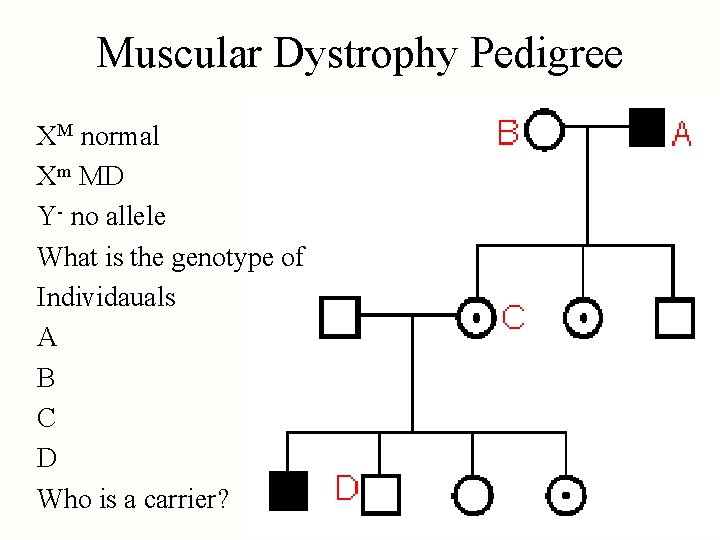
Muscular Dystrophy Pedigree XM normal Xm MD Y- no allele What is the genotype of Individauals A B C D Who is a carrier?
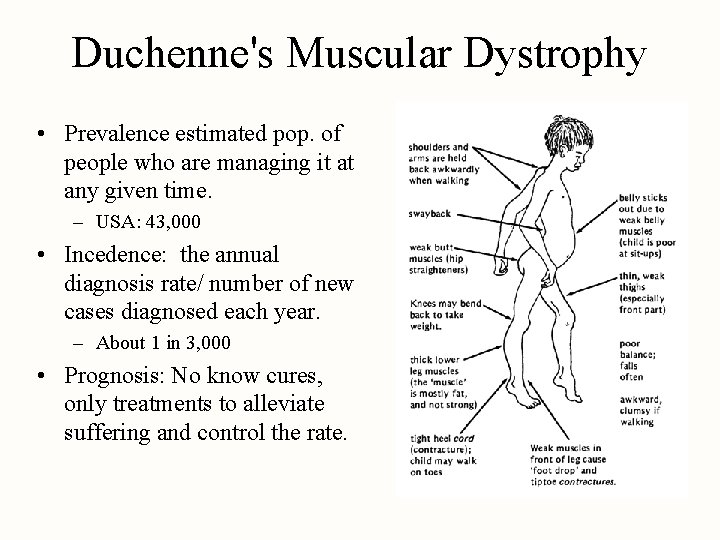
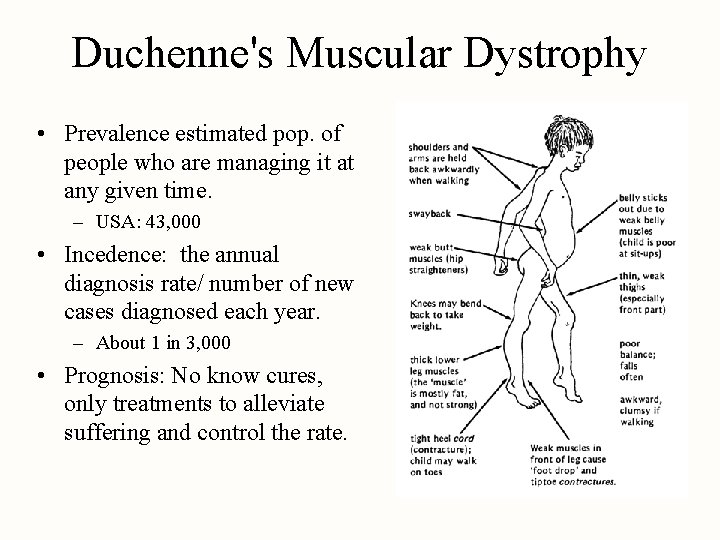
Duchenne's Muscular Dystrophy • Prevalence estimated pop. of people who are managing it at any given time. – USA: 43, 000 • Incedence: the annual diagnosis rate/ number of new cases diagnosed each year. – About 1 in 3, 000 • Prognosis: No know cures, only treatments to alleviate suffering and control the rate.
Group of kids with Muscular Dystrophy
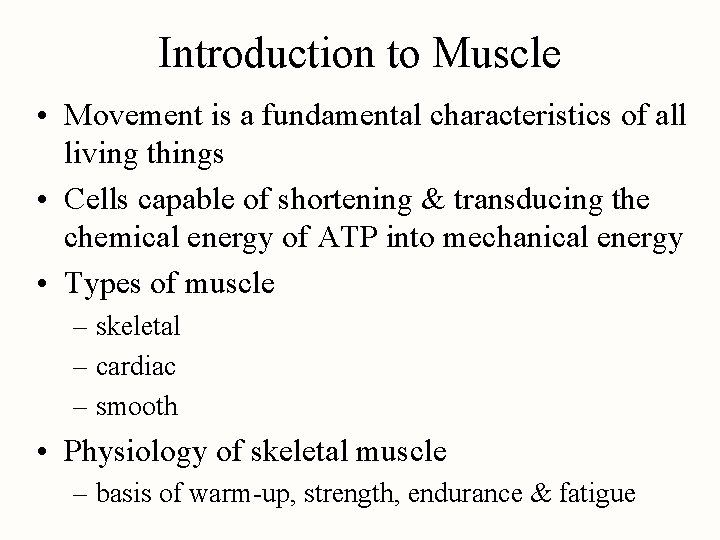
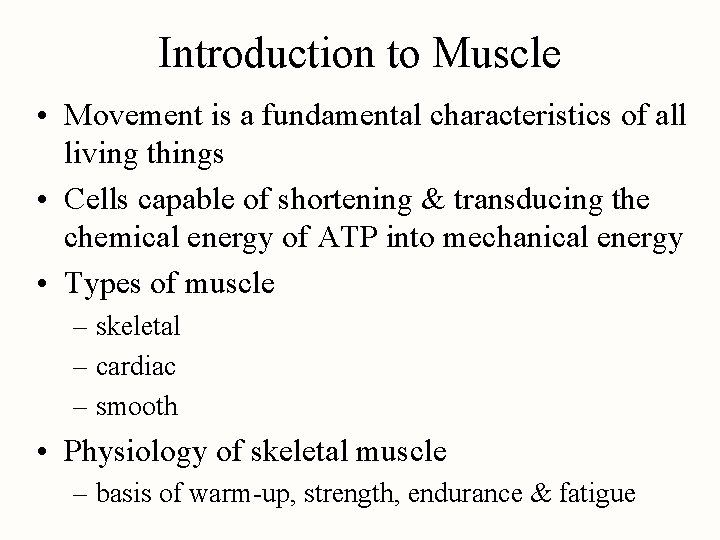
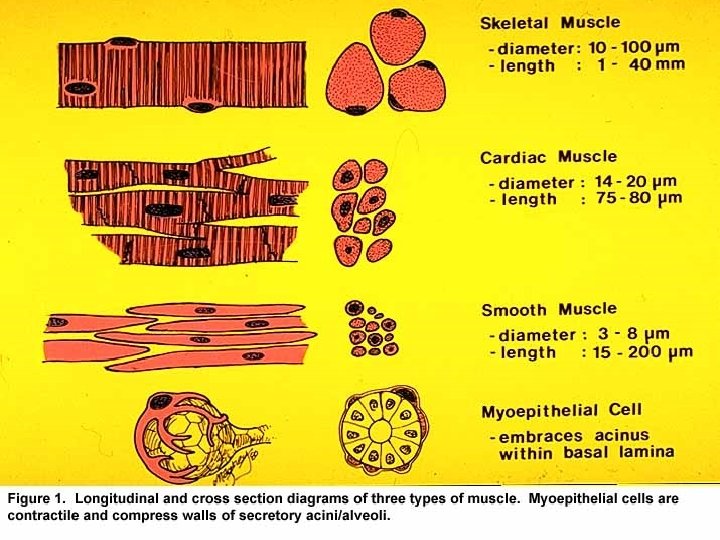
Introduction to Muscle • Movement is a fundamental characteristics of all living things • Cells capable of shortening & transducing the chemical energy of ATP into mechanical energy • Types of muscle – skeletal – cardiac – smooth • Physiology of skeletal muscle – basis of warm-up, strength, endurance & fatigue
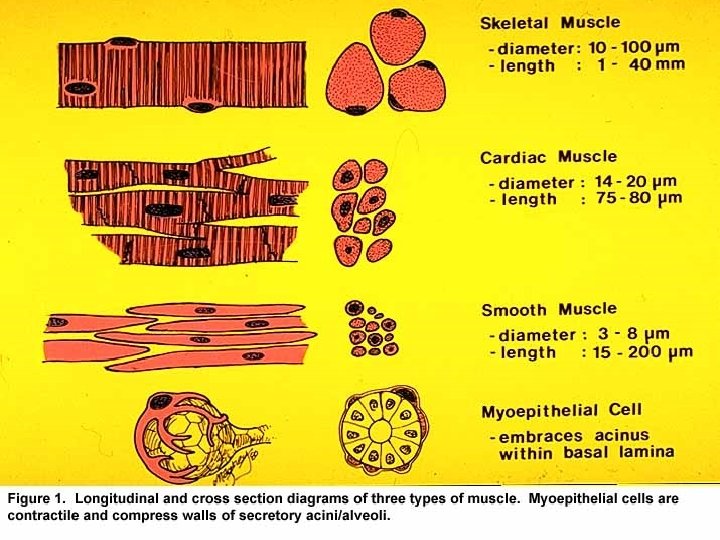
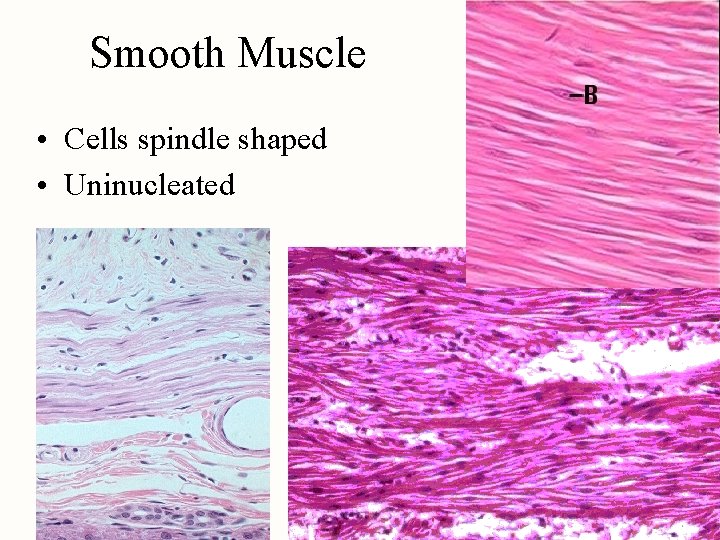
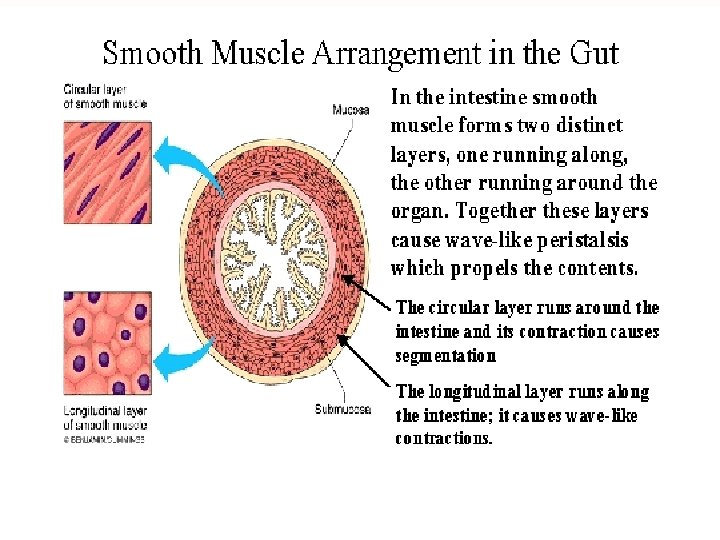
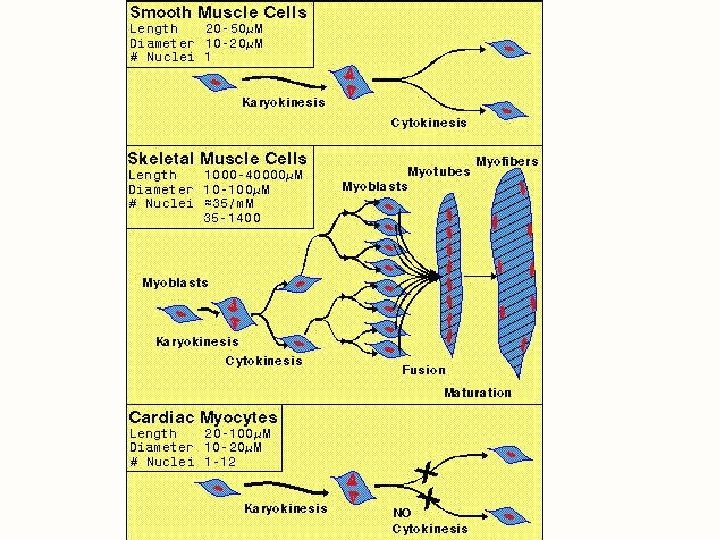
Smooth Muscle • Cells spindle shaped • Uninucleated
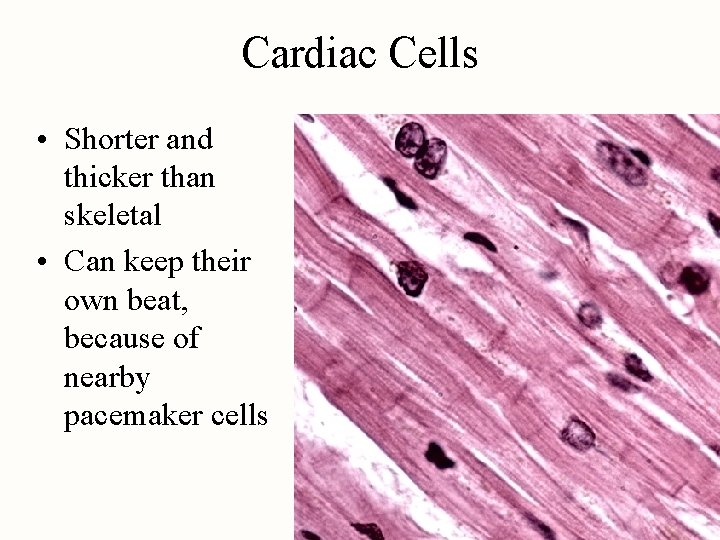
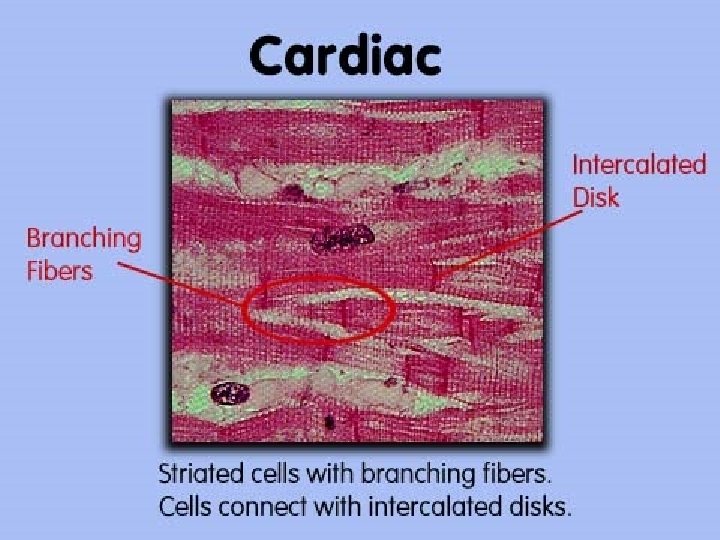
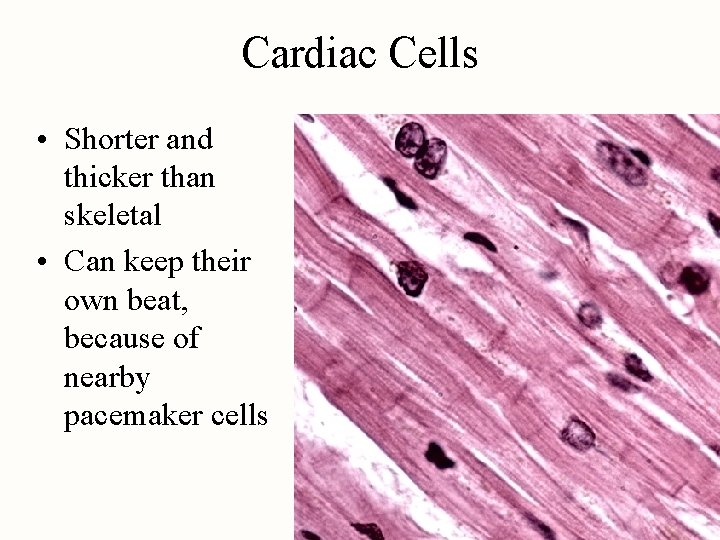
Cardiac Cells • Shorter and thicker than skeletal • Can keep their own beat, because of nearby pacemaker cells
Universal Characteristics of Muscle • Responsiveness (excitability) – capable of response to chemical signals, stretch or other signals & responding with electrical changes across the plasma membrane • Conductivity – local electrical change triggers a wave of excitation that travels along the muscle fiber • Contractility -- shortens when stimulated • Extensibility -- capable of being stretched • Elasticity -- returns to its original resting length after being stretched
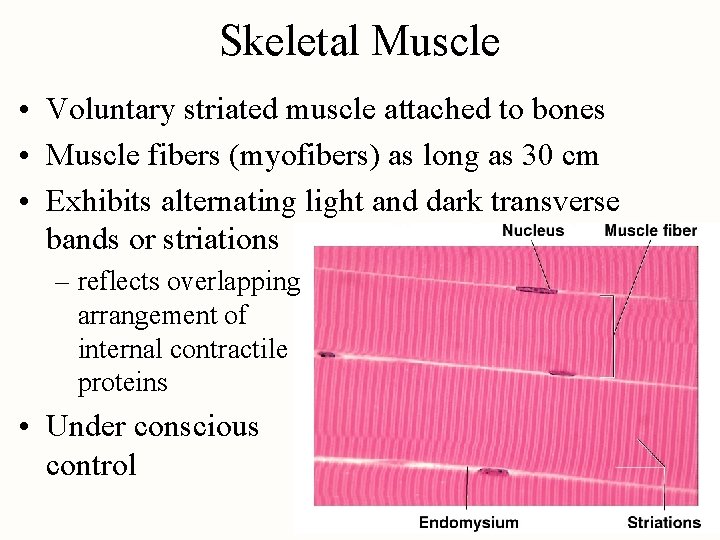
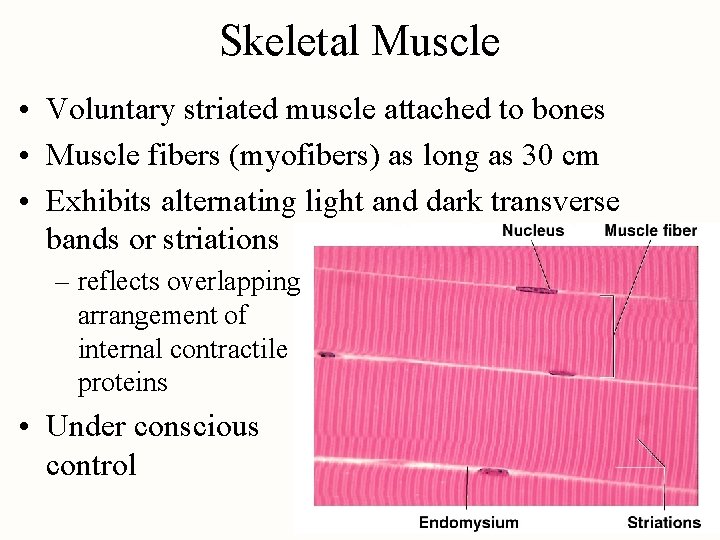
Skeletal Muscle • Voluntary striated muscle attached to bones • Muscle fibers (myofibers) as long as 30 cm • Exhibits alternating light and dark transverse bands or striations – reflects overlapping arrangement of internal contractile proteins • Under conscious control
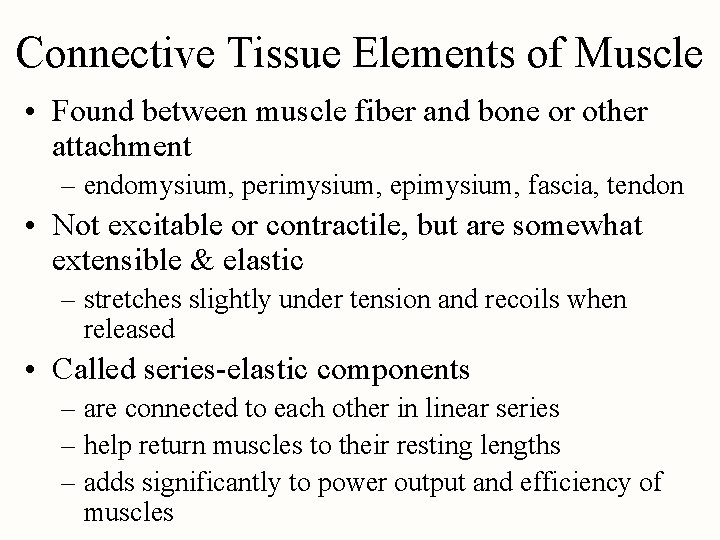
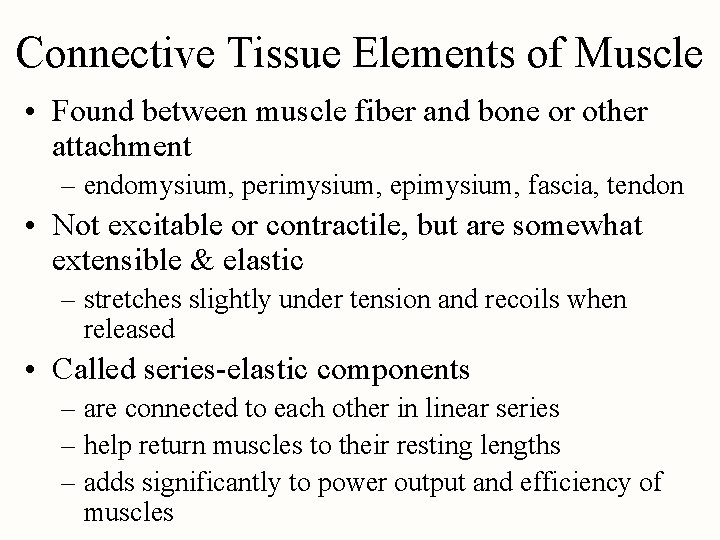
Connective Tissue Elements of Muscle • Found between muscle fiber and bone or other attachment – endomysium, perimysium, epimysium, fascia, tendon • Not excitable or contractile, but are somewhat extensible & elastic – stretches slightly under tension and recoils when released • Called series-elastic components – are connected to each other in linear series – help return muscles to their resting lengths – adds significantly to power output and efficiency of muscles
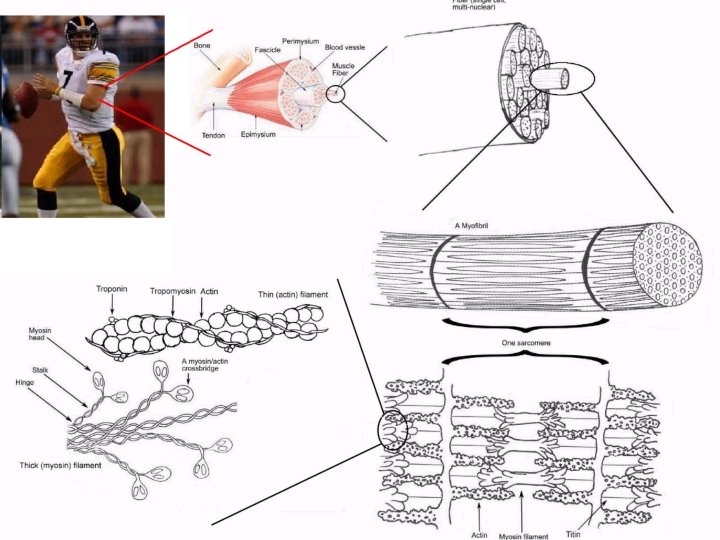
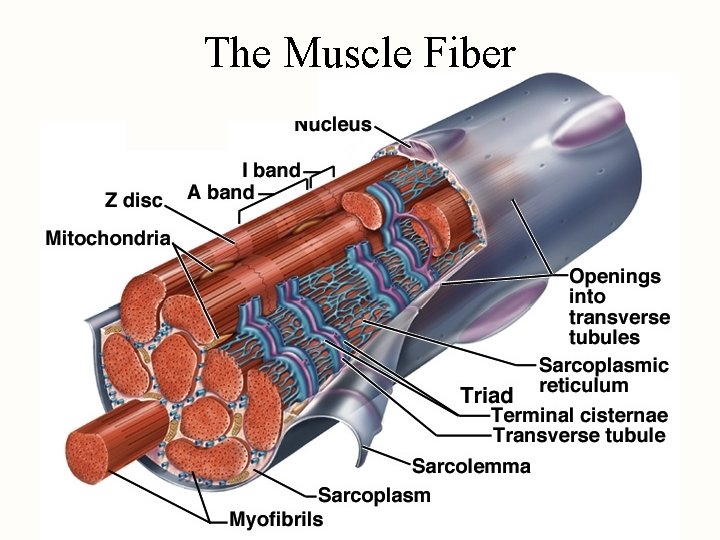
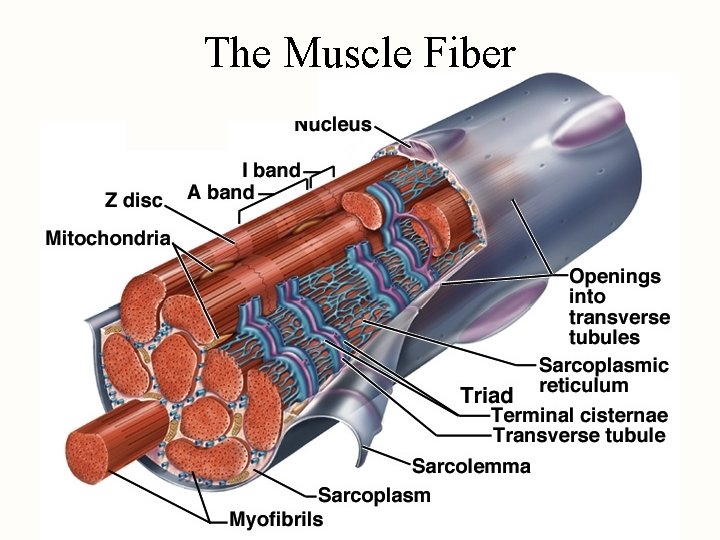
The Muscle Fiber
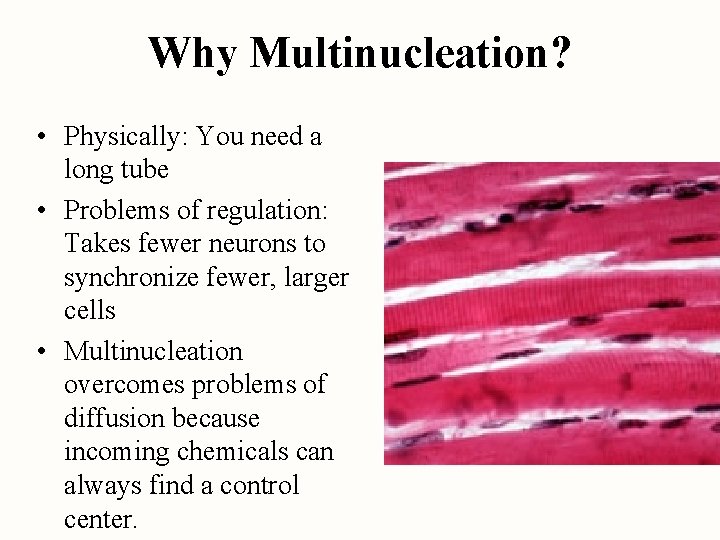
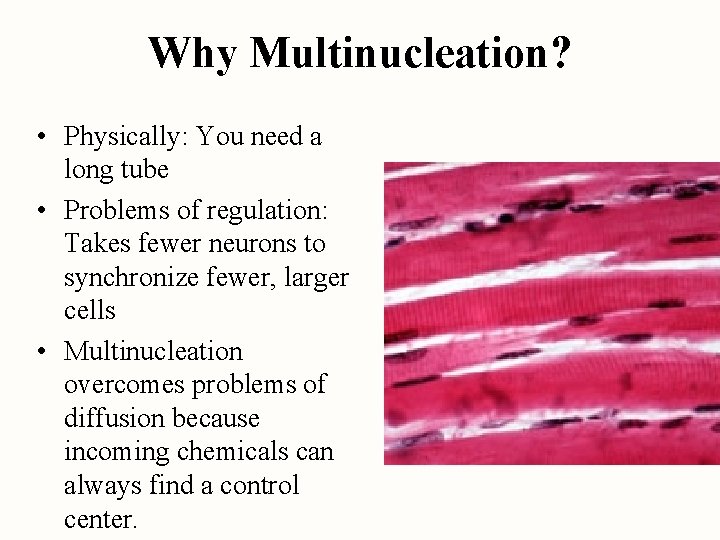
Why Multinucleation? • Physically: You need a long tube • Problems of regulation: Takes fewer neurons to synchronize fewer, larger cells • Multinucleation overcomes problems of diffusion because incoming chemicals can always find a control center.
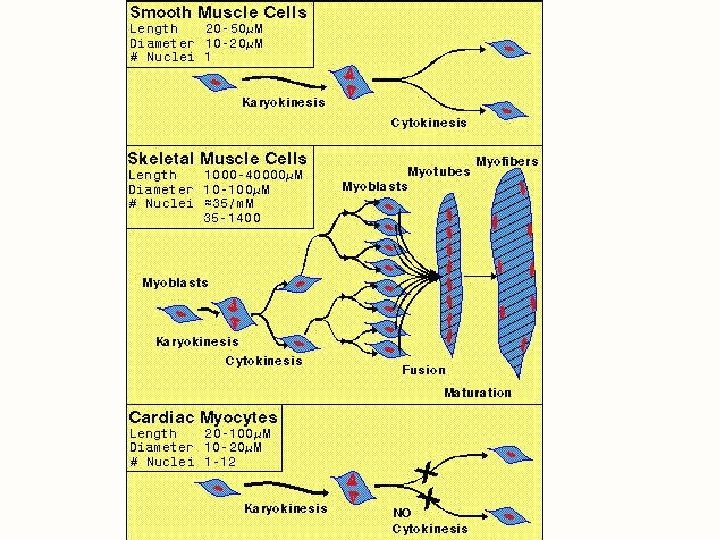
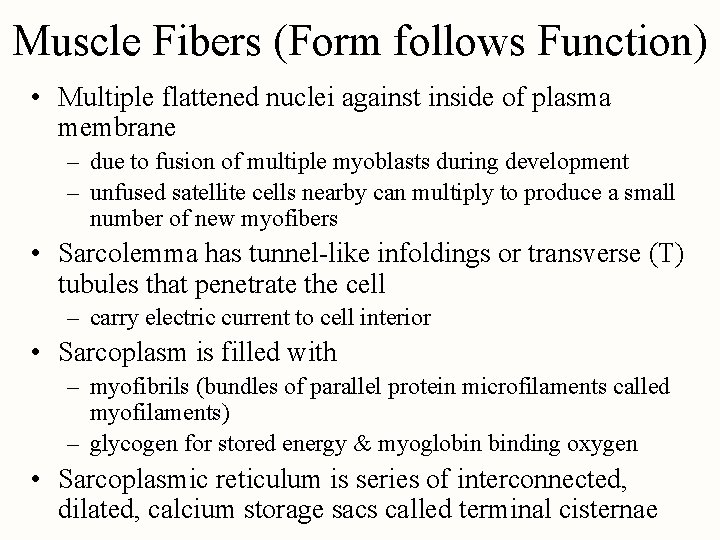
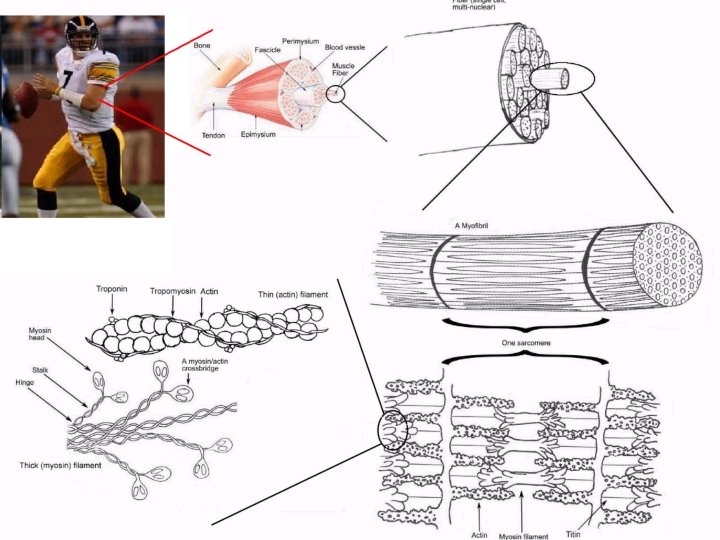
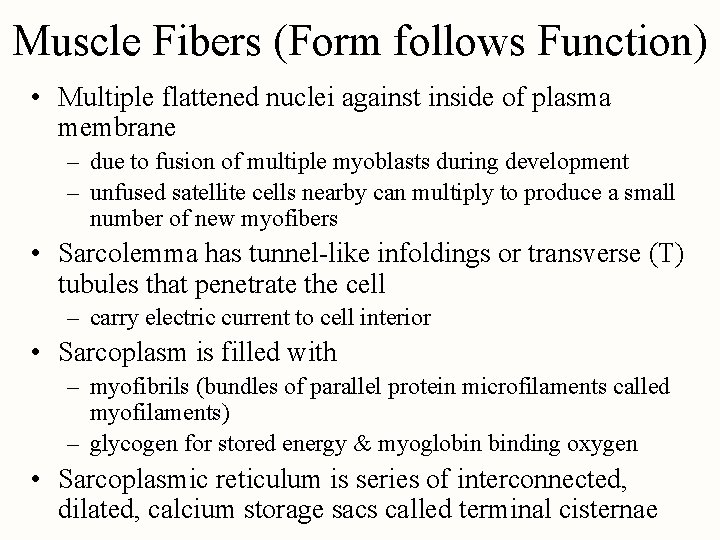
Muscle Fibers (Form follows Function) • Multiple flattened nuclei against inside of plasma membrane – due to fusion of multiple myoblasts during development – unfused satellite cells nearby can multiply to produce a small number of new myofibers • Sarcolemma has tunnel-like infoldings or transverse (T) tubules that penetrate the cell – carry electric current to cell interior • Sarcoplasm is filled with – myofibrils (bundles of parallel protein microfilaments called myofilaments) – glycogen for stored energy & myoglobin binding oxygen • Sarcoplasmic reticulum is series of interconnected, dilated, calcium storage sacs called terminal cisternae
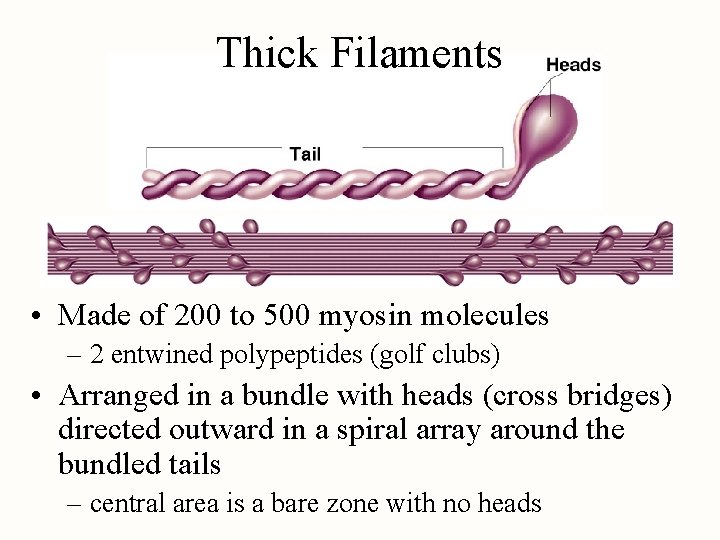
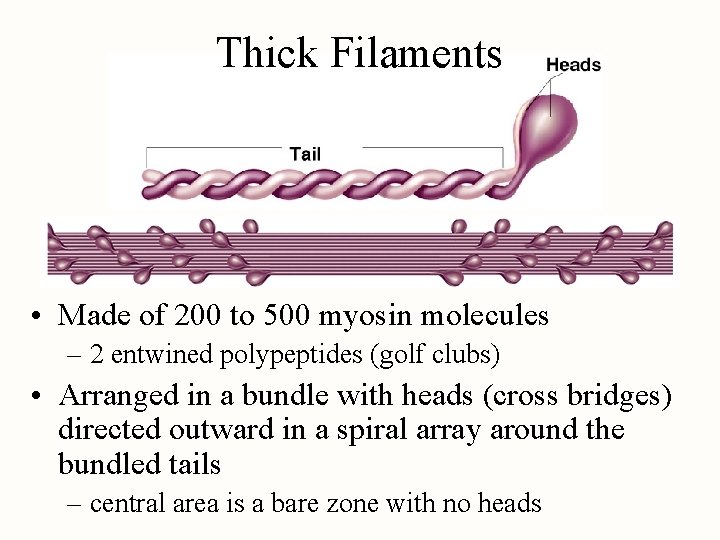
Thick Filaments • Made of 200 to 500 myosin molecules – 2 entwined polypeptides (golf clubs) • Arranged in a bundle with heads (cross bridges) directed outward in a spiral array around the bundled tails – central area is a bare zone with no heads
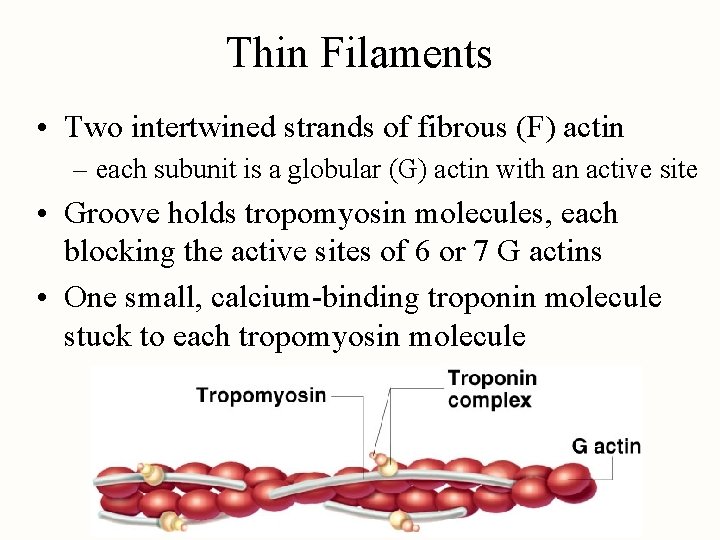
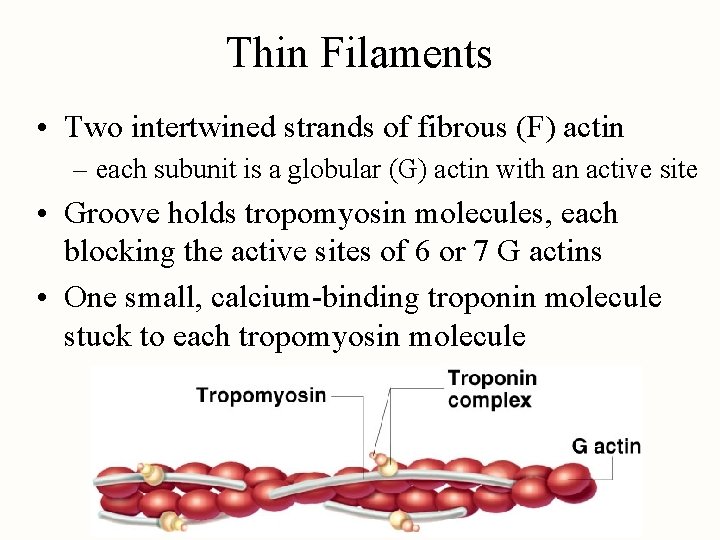
Thin Filaments • Two intertwined strands of fibrous (F) actin – each subunit is a globular (G) actin with an active site • Groove holds tropomyosin molecules, each blocking the active sites of 6 or 7 G actins • One small, calcium-binding troponin molecule stuck to each tropomyosin molecule
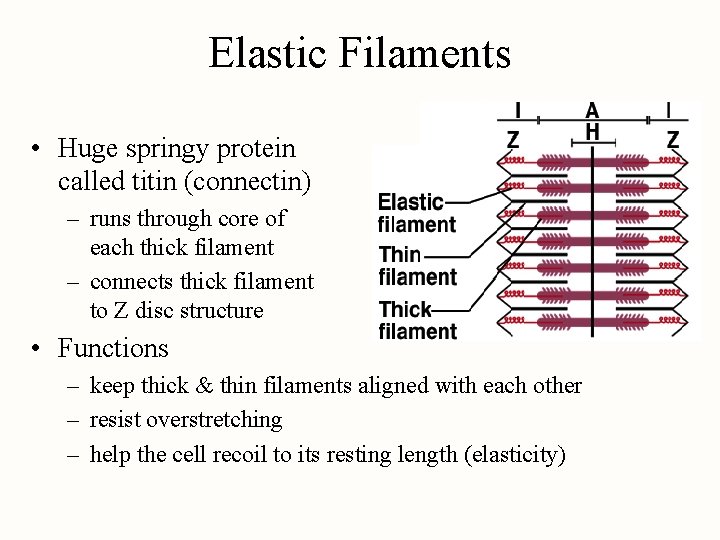
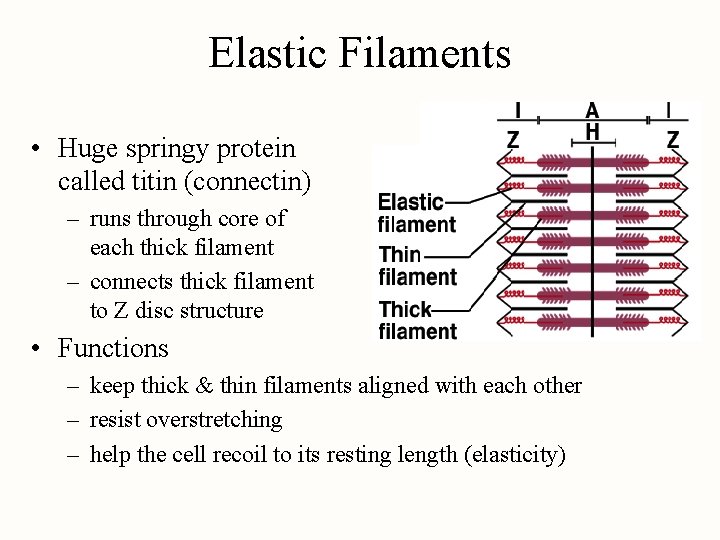
Elastic Filaments • Huge springy protein called titin (connectin) – runs through core of each thick filament – connects thick filament to Z disc structure • Functions – keep thick & thin filaments aligned with each other – resist overstretching – help the cell recoil to its resting length (elasticity)
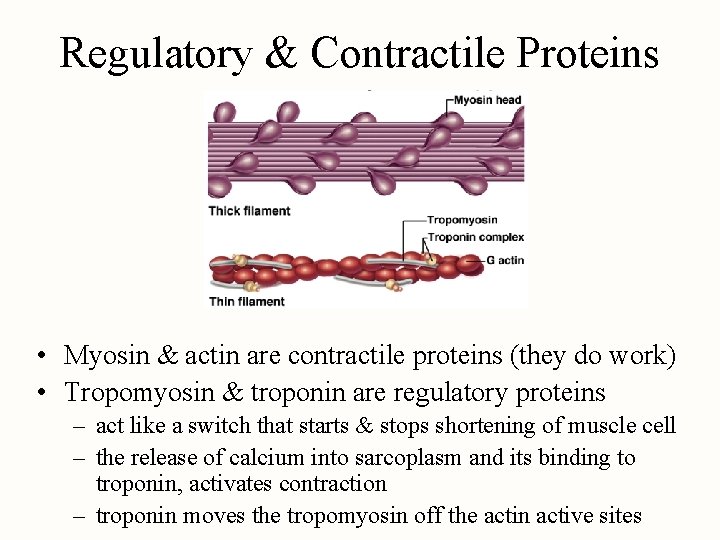
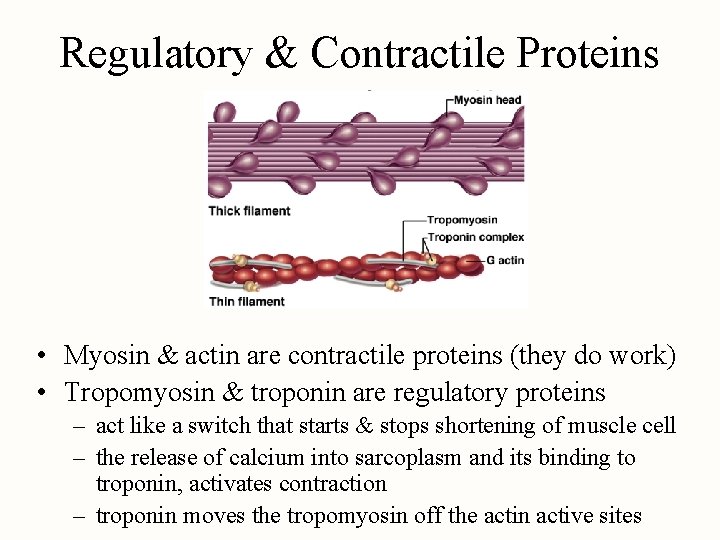
Regulatory & Contractile Proteins • Myosin & actin are contractile proteins (they do work) • Tropomyosin & troponin are regulatory proteins – act like a switch that starts & stops shortening of muscle cell – the release of calcium into sarcoplasm and its binding to troponin, activates contraction – troponin moves the tropomyosin off the actin active sites
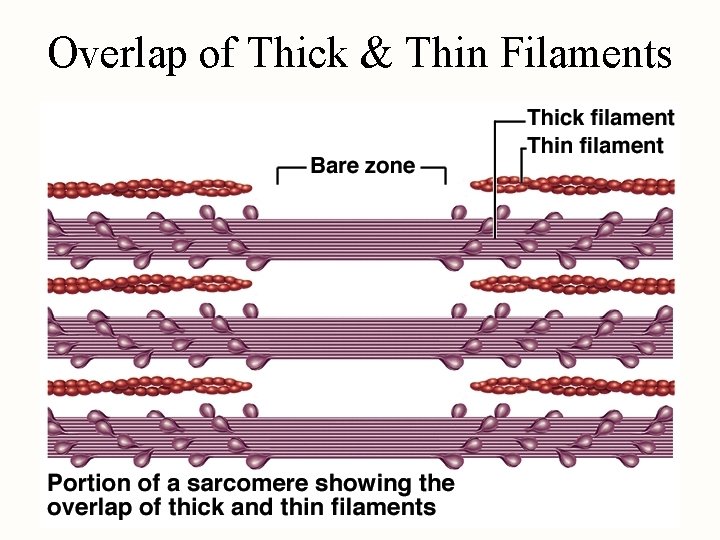
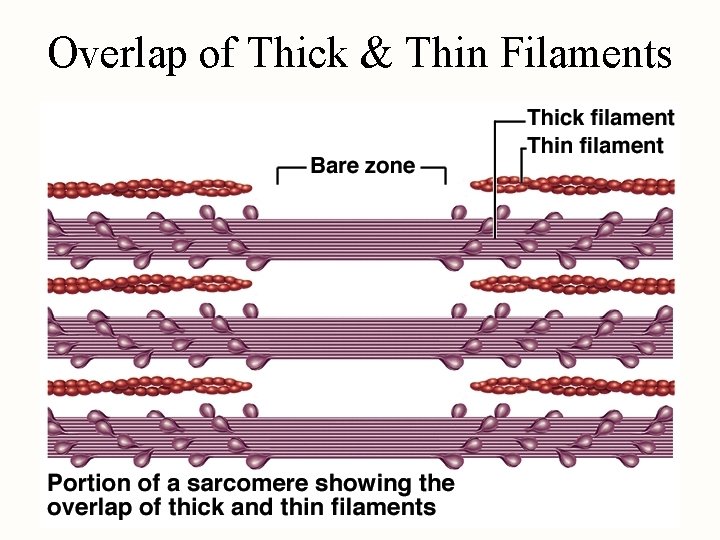
Overlap of Thick & Thin Filaments
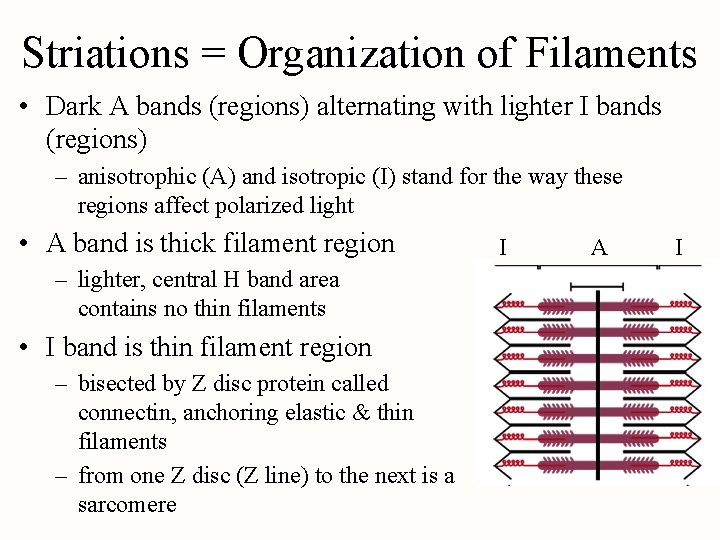
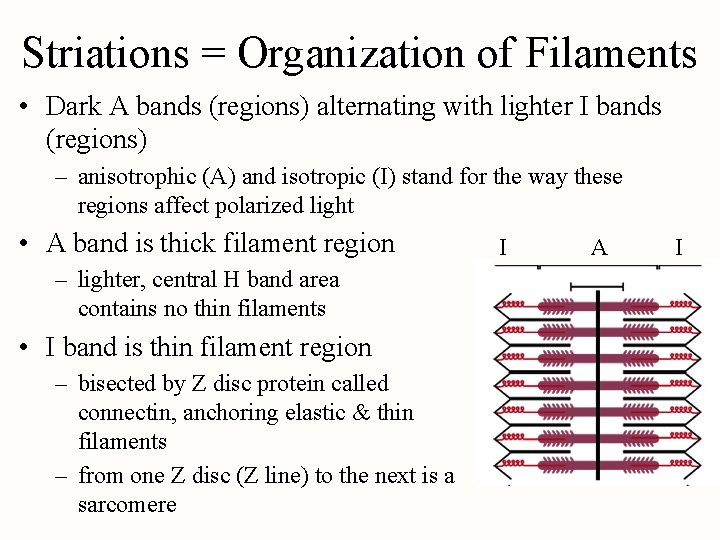
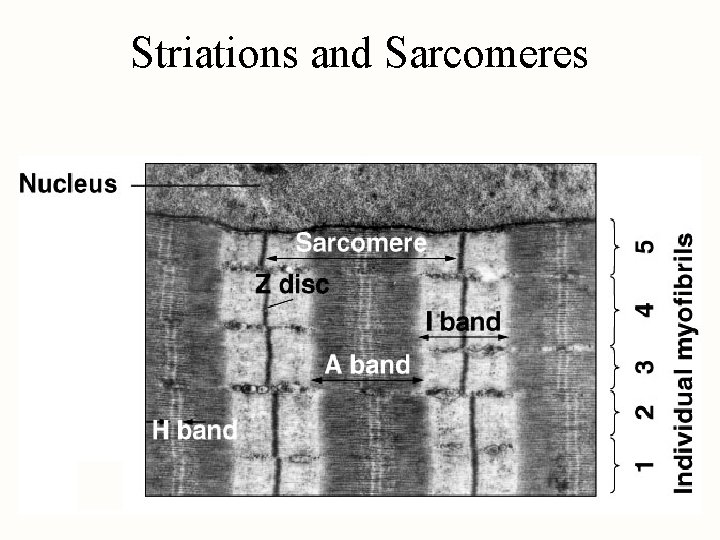
Striations = Organization of Filaments • Dark A bands (regions) alternating with lighter I bands (regions) – anisotrophic (A) and isotropic (I) stand for the way these regions affect polarized light • A band is thick filament region – lighter, central H band area contains no thin filaments • I band is thin filament region – bisected by Z disc protein called connectin, anchoring elastic & thin filaments – from one Z disc (Z line) to the next is a sarcomere I A I
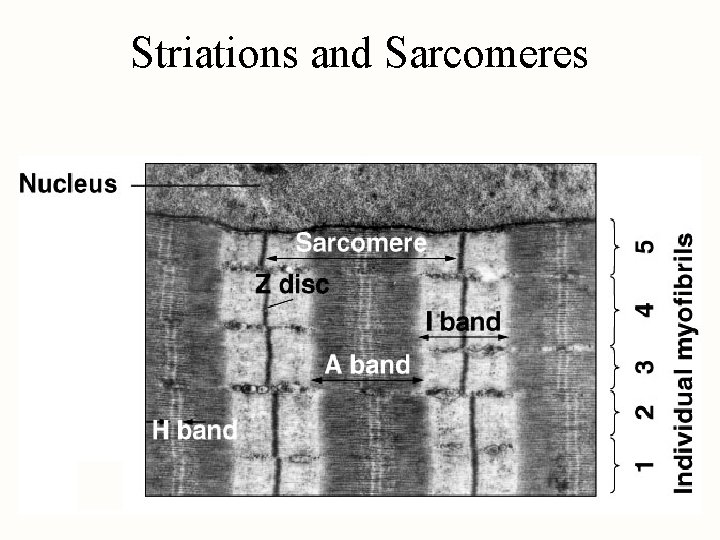
Striations and Sarcomeres
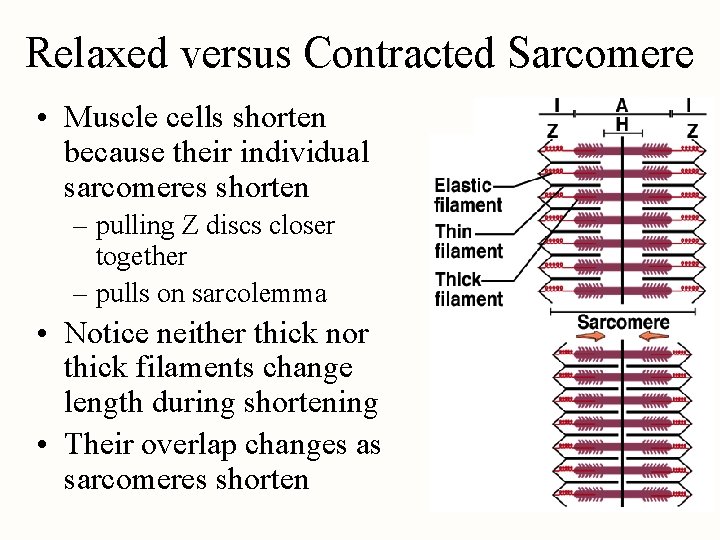
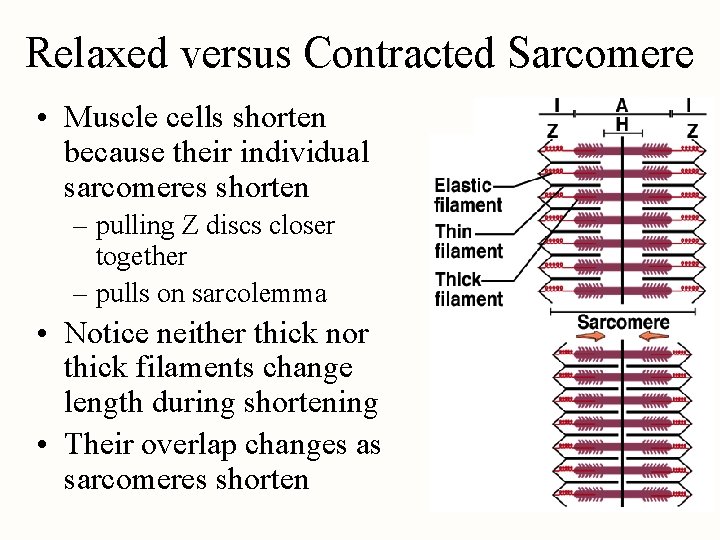
Relaxed versus Contracted Sarcomere • Muscle cells shorten because their individual sarcomeres shorten – pulling Z discs closer together – pulls on sarcolemma • Notice neither thick nor thick filaments change length during shortening • Their overlap changes as sarcomeres shorten
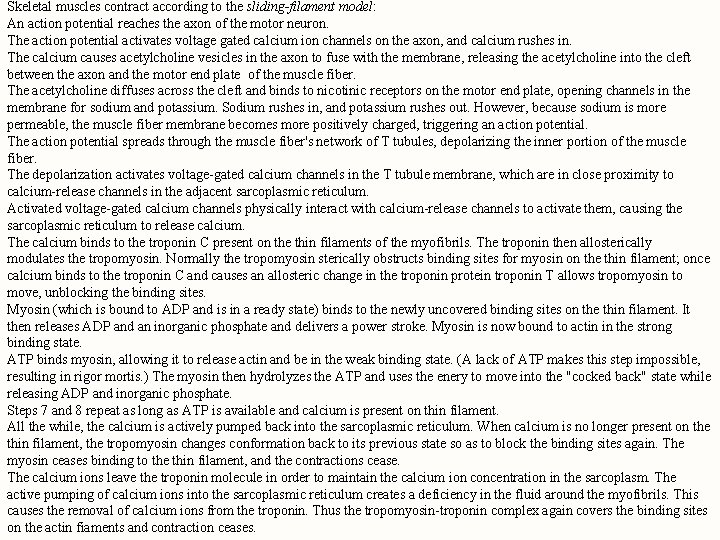
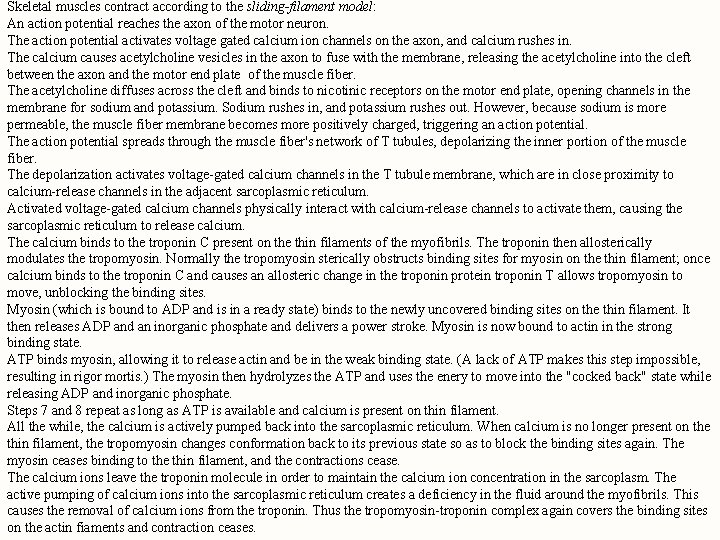
Skeletal muscles contract according to the sliding-filament model: An action potential reaches the axon of the motor neuron. The action potential activates voltage gated calcium ion channels on the axon, and calcium rushes in. The calcium causes acetylcholine vesicles in the axon to fuse with the membrane, releasing the acetylcholine into the cleft between the axon and the motor end plate of the muscle fiber. The acetylcholine diffuses across the cleft and binds to nicotinic receptors on the motor end plate, opening channels in the membrane for sodium and potassium. Sodium rushes in, and potassium rushes out. However, because sodium is more permeable, the muscle fiber membrane becomes more positively charged, triggering an action potential. The action potential spreads through the muscle fiber's network of T tubules, depolarizing the inner portion of the muscle fiber. The depolarization activates voltage-gated calcium channels in the T tubule membrane, which are in close proximity to calcium-release channels in the adjacent sarcoplasmic reticulum. Activated voltage-gated calcium channels physically interact with calcium-release channels to activate them, causing the sarcoplasmic reticulum to release calcium. The calcium binds to the troponin C present on the thin filaments of the myofibrils. The troponin then allosterically modulates the tropomyosin. Normally the tropomyosin sterically obstructs binding sites for myosin on the thin filament; once calcium binds to the troponin C and causes an allosteric change in the troponin protein troponin T allows tropomyosin to move, unblocking the binding sites. Myosin (which is bound to ADP and is in a ready state) binds to the newly uncovered binding sites on the thin filament. It then releases ADP and an inorganic phosphate and delivers a power stroke. Myosin is now bound to actin in the strong binding state. ATP binds myosin, allowing it to release actin and be in the weak binding state. (A lack of ATP makes this step impossible, resulting in rigor mortis. ) The myosin then hydrolyzes the ATP and uses the enery to move into the "cocked back" state while releasing ADP and inorganic phosphate. Steps 7 and 8 repeat as long as ATP is available and calcium is present on thin filament. All the while, the calcium is actively pumped back into the sarcoplasmic reticulum. When calcium is no longer present on the thin filament, the tropomyosin changes conformation back to its previous state so as to block the binding sites again. The myosin ceases binding to the thin filament, and the contractions cease. The calcium ions leave the troponin molecule in order to maintain the calcium ion concentration in the sarcoplasm. The active pumping of calcium ions into the sarcoplasmic reticulum creates a deficiency in the fluid around the myofibrils. This causes the removal of calcium ions from the troponin. Thus the tropomyosin-troponin complex again covers the binding sites on the actin fiaments and contraction ceases.
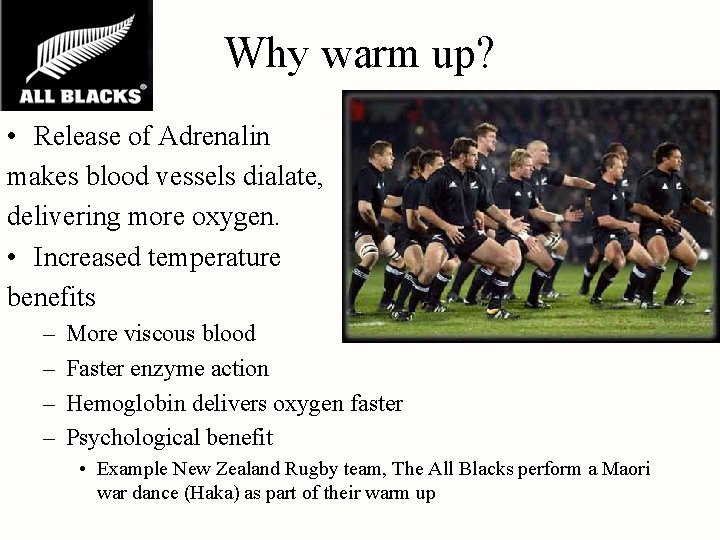
Why warm up? • Release of Adrenalin makes blood vessels dialate, delivering more oxygen. • Increased temperature benefits – – More viscous blood Faster enzyme action Hemoglobin delivers oxygen faster Psychological benefit • Example New Zealand Rugby team, The All Blacks perform a Maori war dance (Haka) as part of their warm up
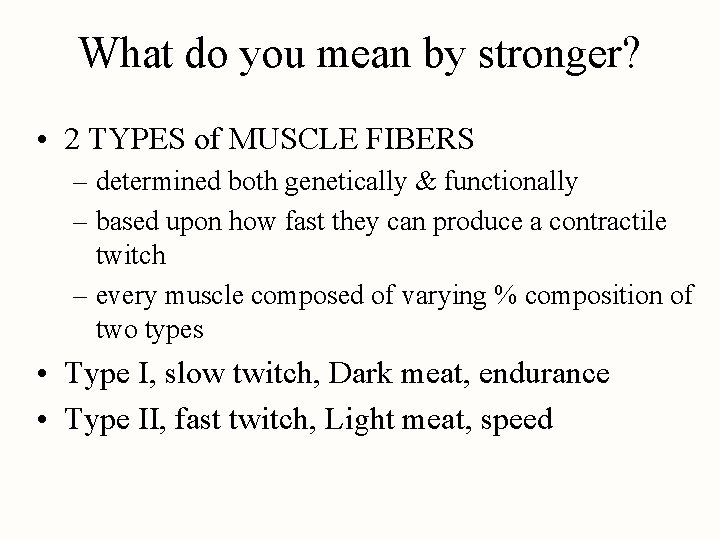
What do you mean by stronger? • 2 TYPES of MUSCLE FIBERS – determined both genetically & functionally – based upon how fast they can produce a contractile twitch – every muscle composed of varying % composition of two types • Type I, slow twitch, Dark meat, endurance • Type II, fast twitch, Light meat, speed
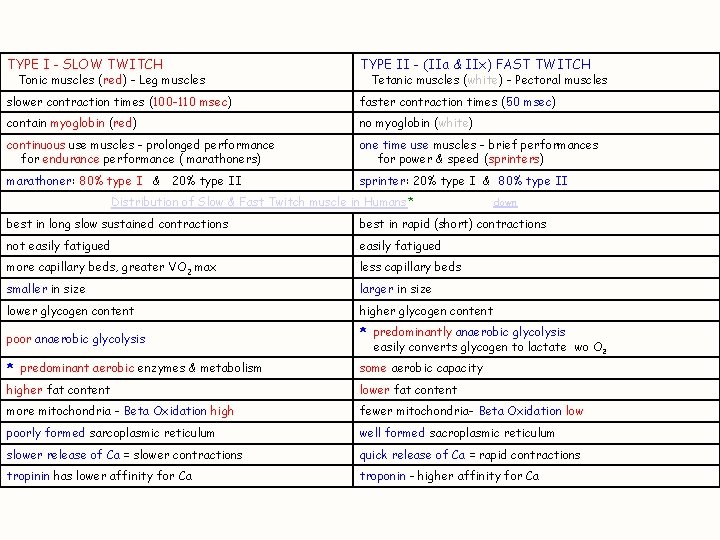
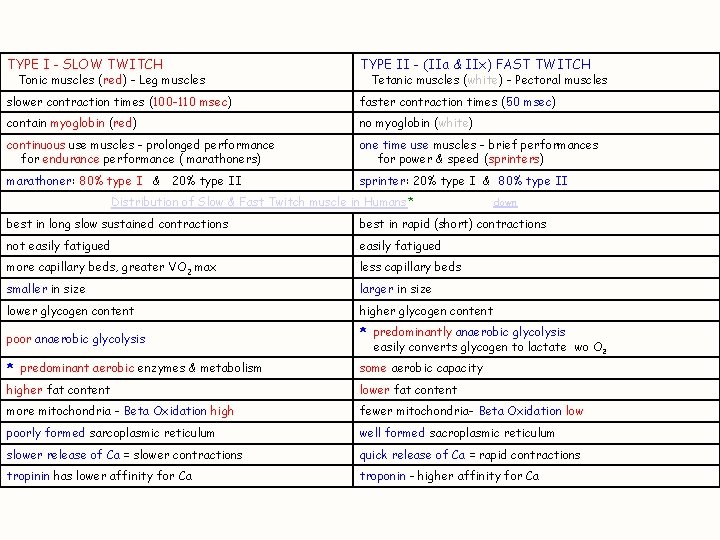
TYPE I - SLOW TWITCH TYPE II - (IIa & IIx) FAST TWITCH slower contraction times (100 -110 msec) faster contraction times (50 msec) contain myoglobin (red) no myoglobin (white) continuous use muscles - prolonged performance for endurance performance ( marathoners) one time use muscles - brief performances for power & speed (sprinters) marathoner: 80% type I & 20% type II sprinter: 20% type I & 80% type II Tonic muscles (red) - Leg muscles Tetanic muscles (white) - Pectoral muscles Distribution of Slow & Fast Twitch muscle in Humans* down best in long slow sustained contractions best in rapid (short) contractions not easily fatigued more capillary beds, greater VO 2 max less capillary beds smaller in size larger in size lower glycogen content higher glycogen content poor anaerobic glycolysis * predominantly anaerobic glycolysis easily converts glycogen to lactate wo O 2 * predominant aerobic enzymes & metabolism some aerobic capacity higher fat content lower fat content more mitochondria - Beta Oxidation high fewer mitochondria- Beta Oxidation low poorly formed sarcoplasmic reticulum well formed sacroplasmic reticulum slower release of Ca = slower contractions quick release of Ca = rapid contractions tropinin has lower affinity for Ca troponin - higher affinity for Ca
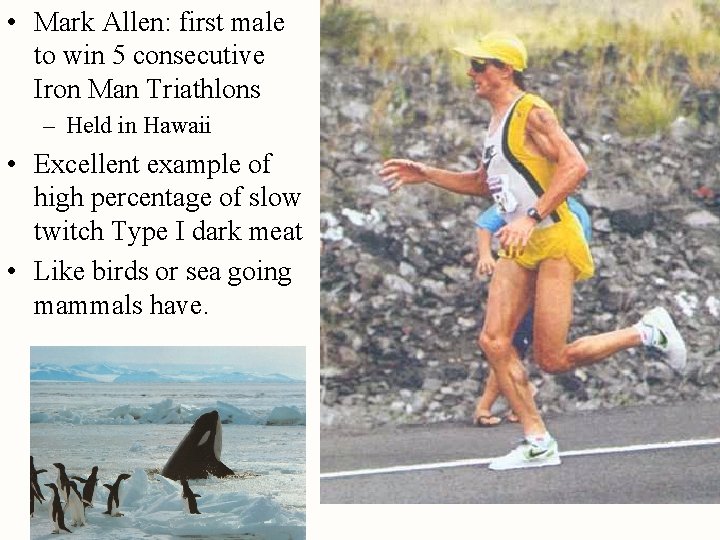
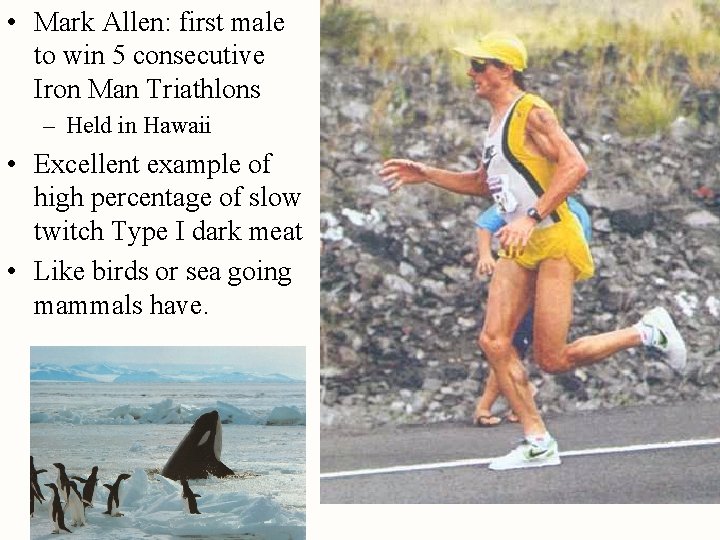
• Mark Allen: first male to win 5 consecutive Iron Man Triathlons – Held in Hawaii • Excellent example of high percentage of slow twitch Type I dark meat • Like birds or sea going mammals have.
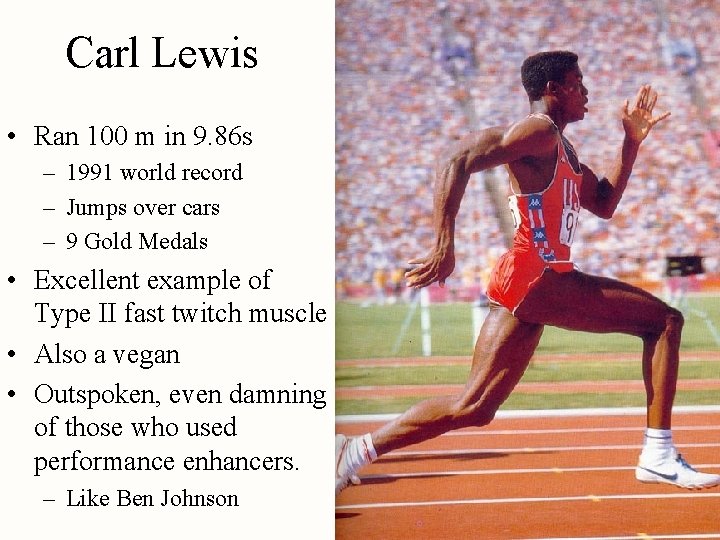
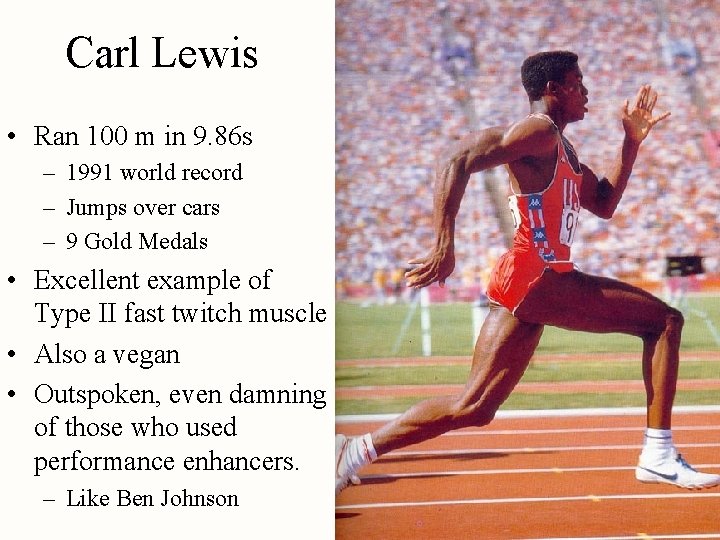
Carl Lewis • Ran 100 m in 9. 86 s – 1991 world record – Jumps over cars – 9 Gold Medals • Excellent example of Type II fast twitch muscle • Also a vegan • Outspoken, even damning of those who used performance enhancers. – Like Ben Johnson
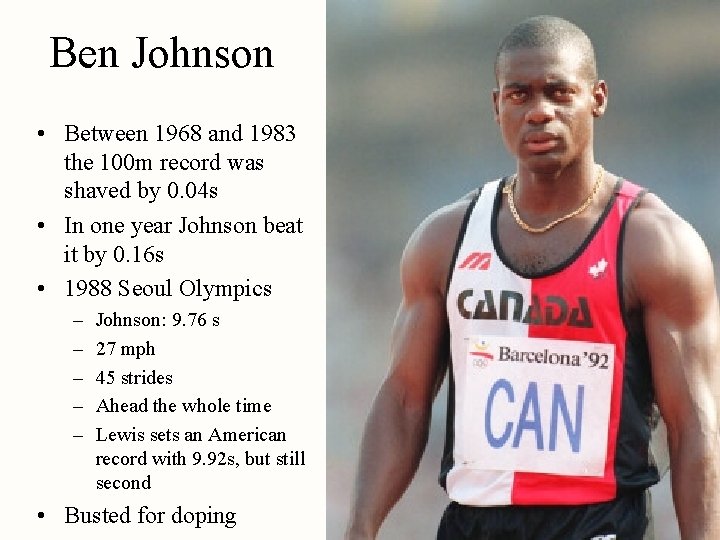
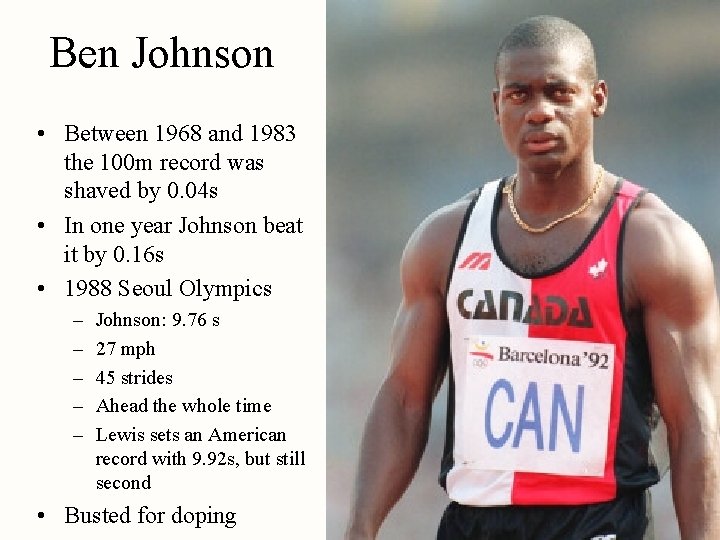
Ben Johnson • Between 1968 and 1983 the 100 m record was shaved by 0. 04 s • In one year Johnson beat it by 0. 16 s • 1988 Seoul Olympics – – – Johnson: 9. 76 s 27 mph 45 strides Ahead the whole time Lewis sets an American record with 9. 92 s, but still second • Busted for doping

Back to Carl Lewis • Johnson’s medal revoked and given to Lewis • 5 years later in 2003 Lewis admits he was busted 3 times in 1988 for banned stimulants. – He “thought they were herbal supplements” – The U. S. Olympic committee found his ingestion to be, “inadvertant” – Since it was after the 3 year statute of limitations he could keep his medals – Stimulants could have masked more serious steroids from tests • Johnson beating Lewis in ‘ 88
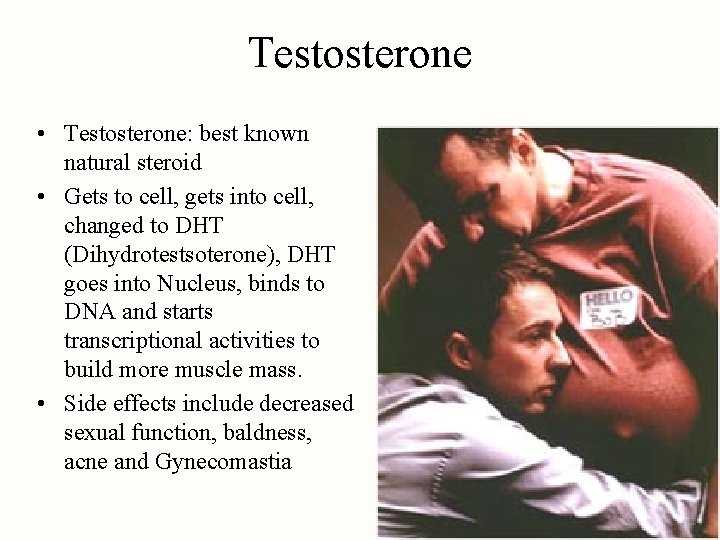
Which leads to the question how do steroids work? • Androgenic: increasing masculine traits • Anabolic: building muscles as opposed to • Catabolic: breaking down nutrients
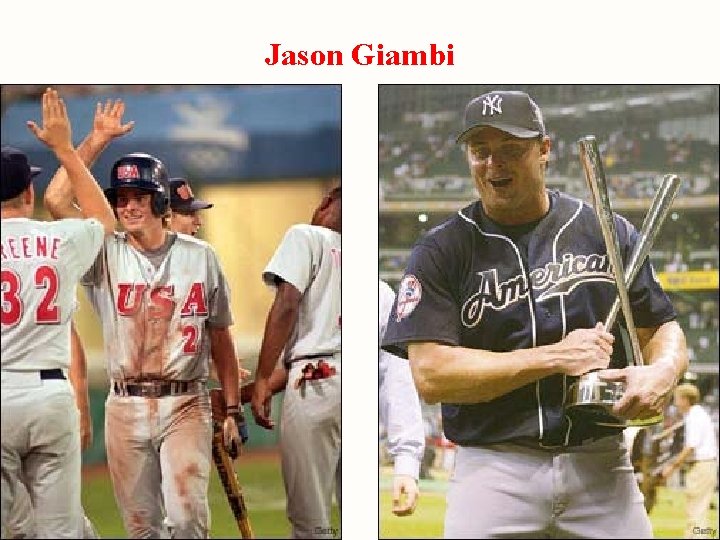
Jason Giambi
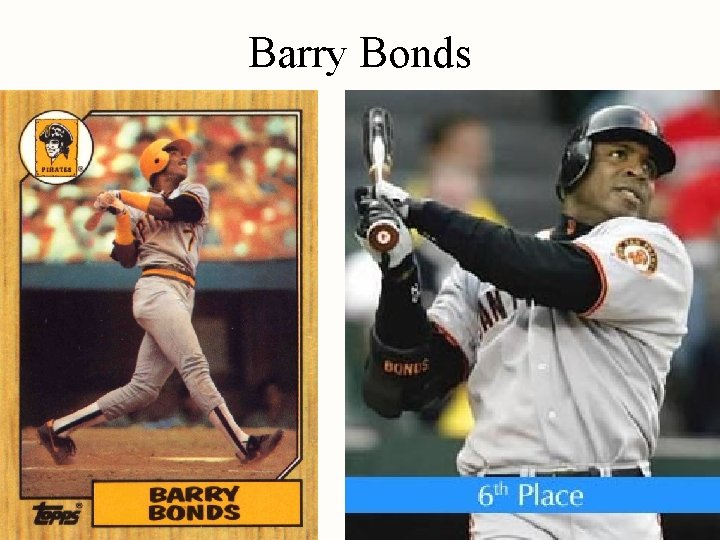
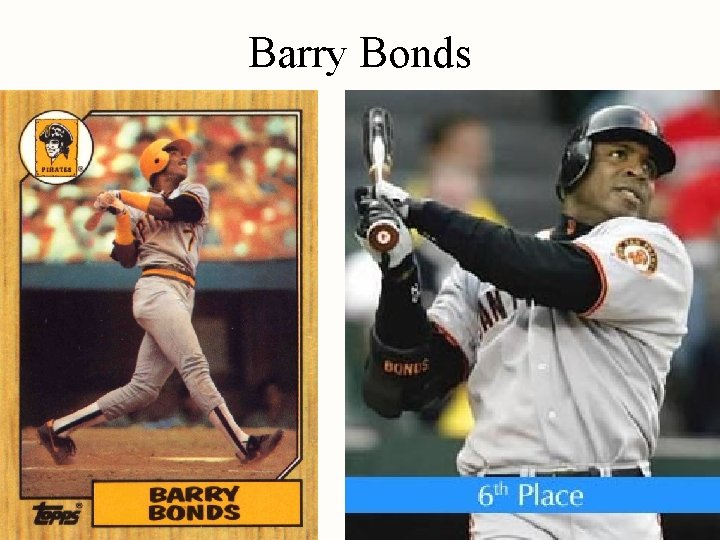
Barry Bonds
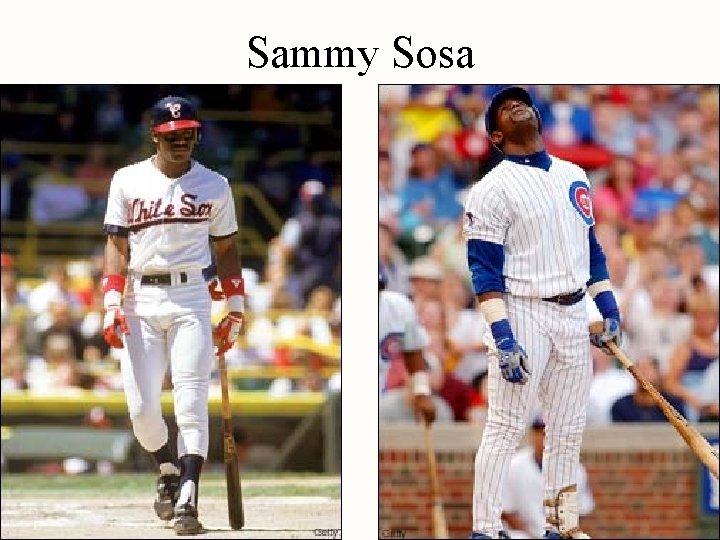
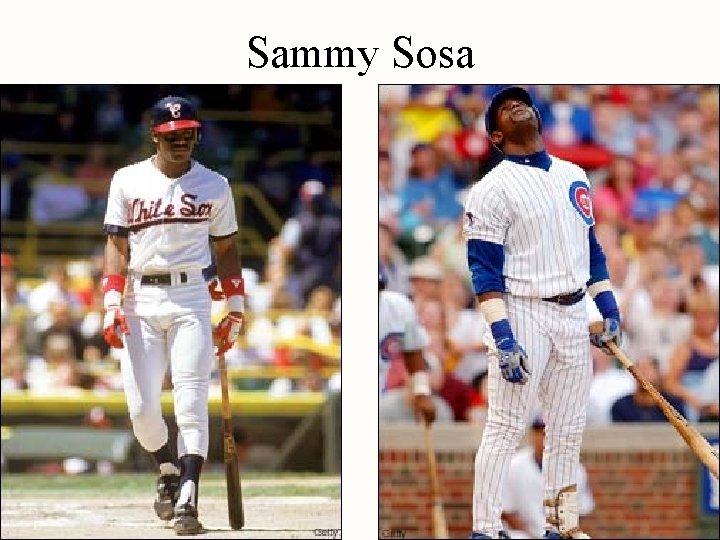
Sammy Sosa
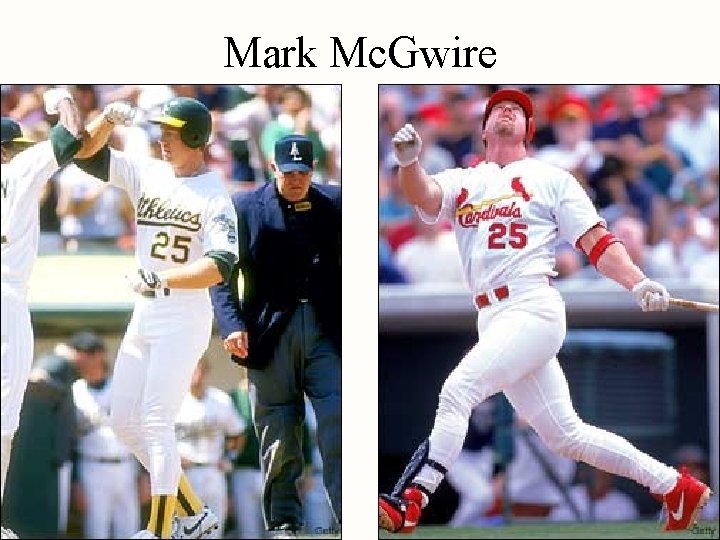
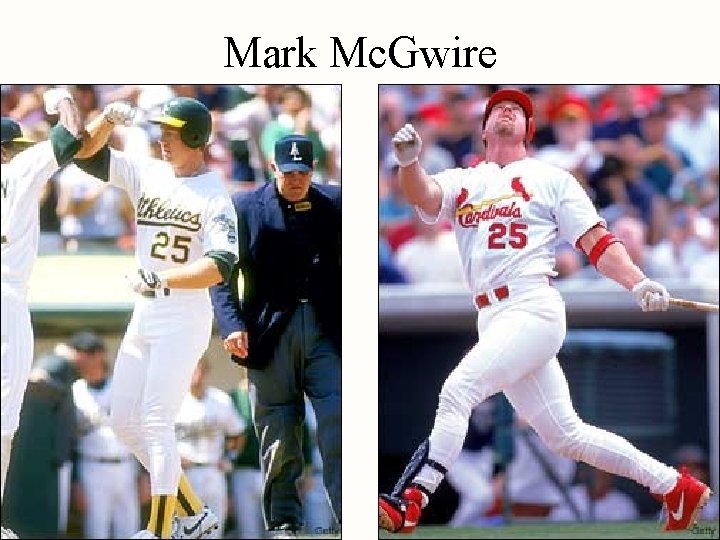
Mark Mc. Gwire
Testosterone • Testosterone: best known natural steroid • Gets to cell, gets into cell, changed to DHT (Dihydrotestsoterone), DHT goes into Nucleus, binds to DNA and starts transcriptional activities to build more muscle mass. • Side effects include decreased sexual function, baldness, acne and Gynecomastia
Warm-up Strength Endurance Fatigue
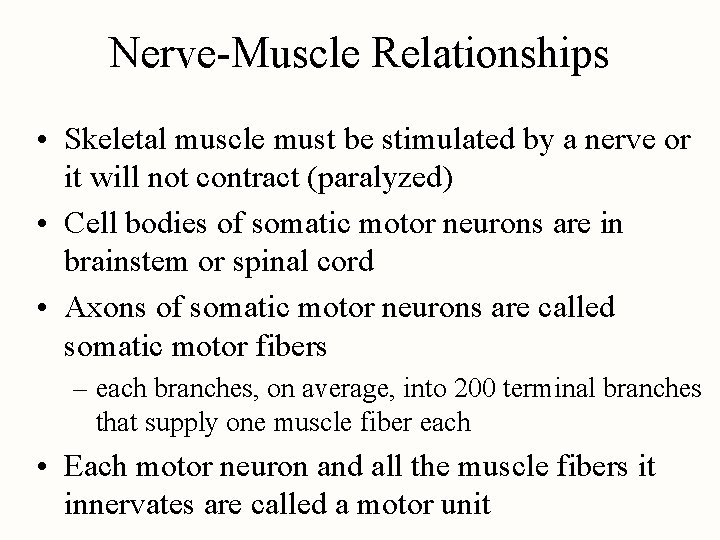
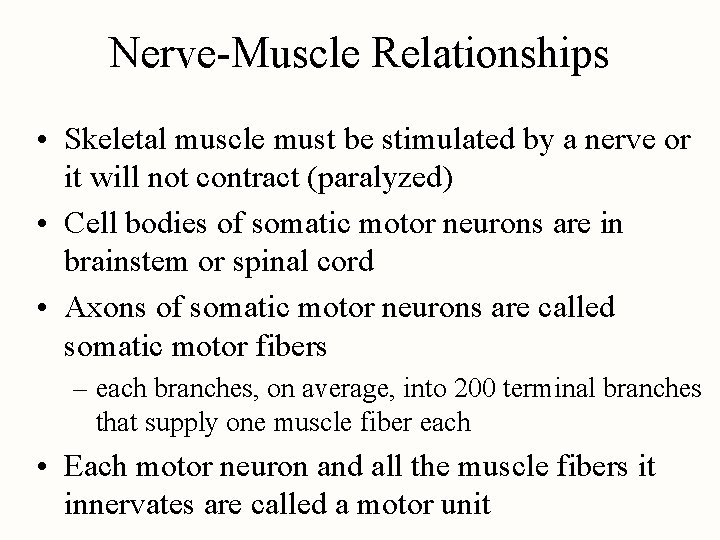
Nerve-Muscle Relationships • Skeletal muscle must be stimulated by a nerve or it will not contract (paralyzed) • Cell bodies of somatic motor neurons are in brainstem or spinal cord • Axons of somatic motor neurons are called somatic motor fibers – each branches, on average, into 200 terminal branches that supply one muscle fiber each • Each motor neuron and all the muscle fibers it innervates are called a motor unit
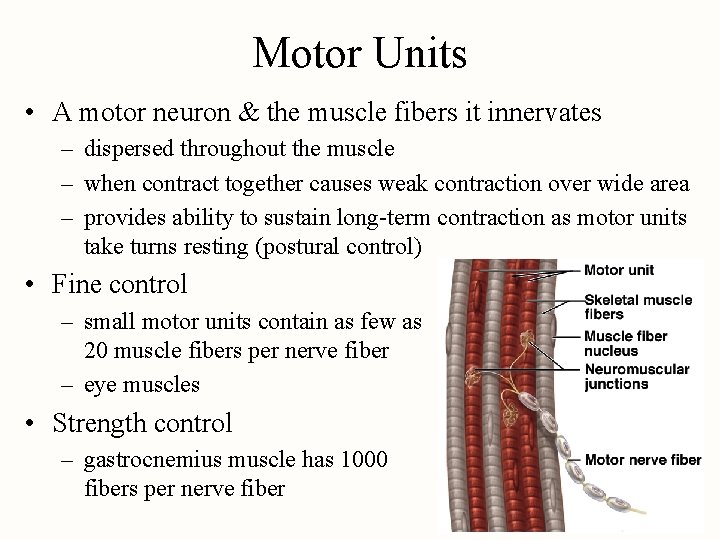
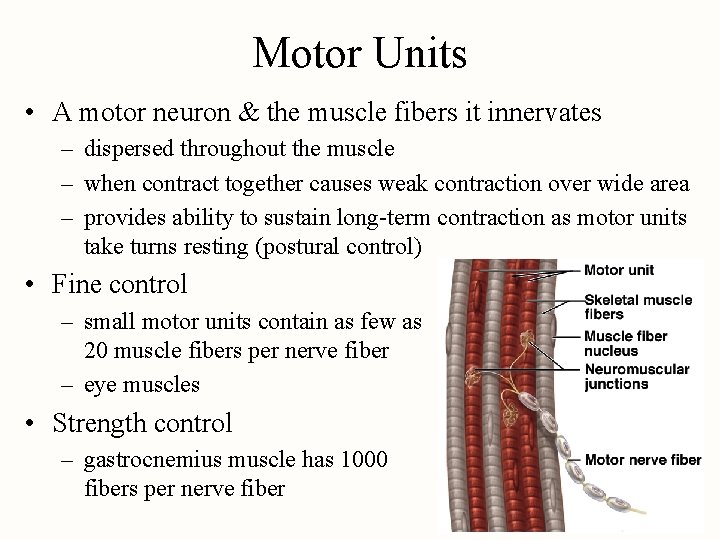
Motor Units • A motor neuron & the muscle fibers it innervates – dispersed throughout the muscle – when contract together causes weak contraction over wide area – provides ability to sustain long-term contraction as motor units take turns resting (postural control) • Fine control – small motor units contain as few as 20 muscle fibers per nerve fiber – eye muscles • Strength control – gastrocnemius muscle has 1000 fibers per nerve fiber
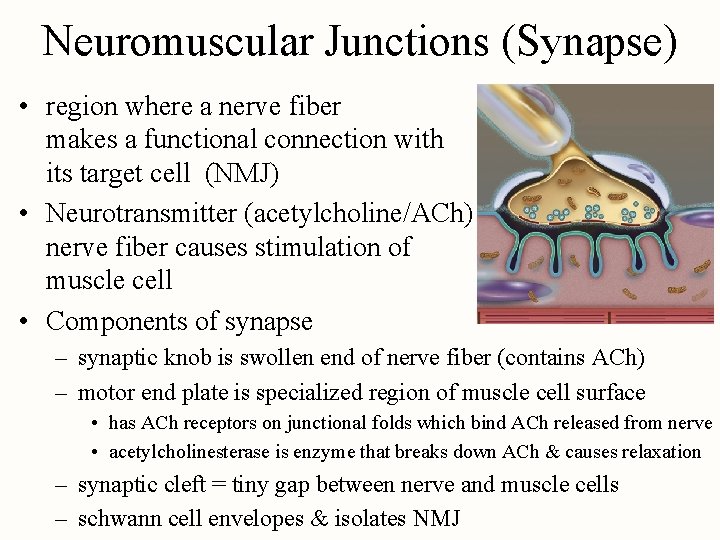
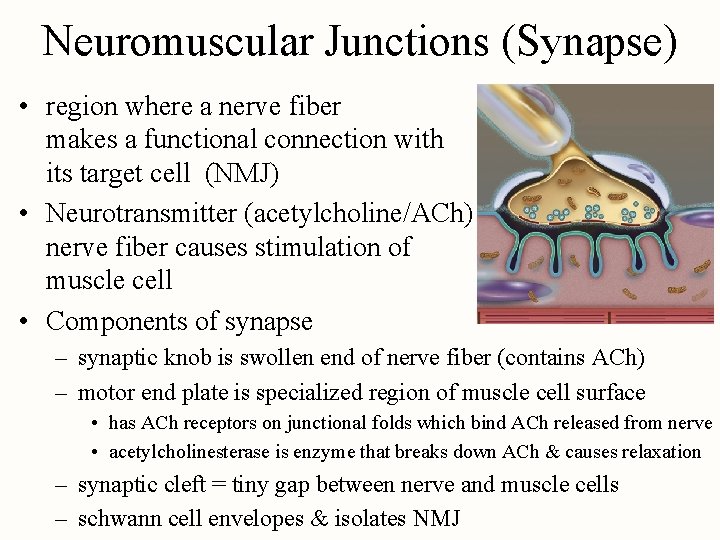
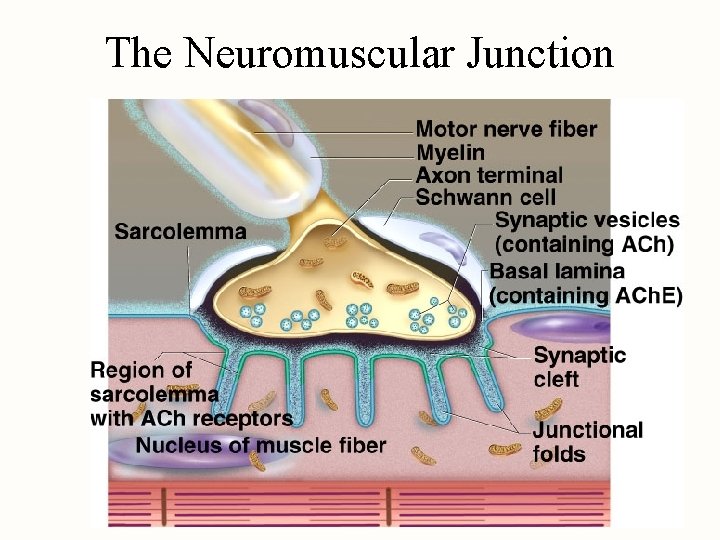
Neuromuscular Junctions (Synapse) • region where a nerve fiber makes a functional connection with its target cell (NMJ) • Neurotransmitter (acetylcholine/ACh) released from nerve fiber causes stimulation of muscle cell • Components of synapse – synaptic knob is swollen end of nerve fiber (contains ACh) – motor end plate is specialized region of muscle cell surface • has ACh receptors on junctional folds which bind ACh released from nerve • acetylcholinesterase is enzyme that breaks down ACh & causes relaxation – synaptic cleft = tiny gap between nerve and muscle cells – schwann cell envelopes & isolates NMJ
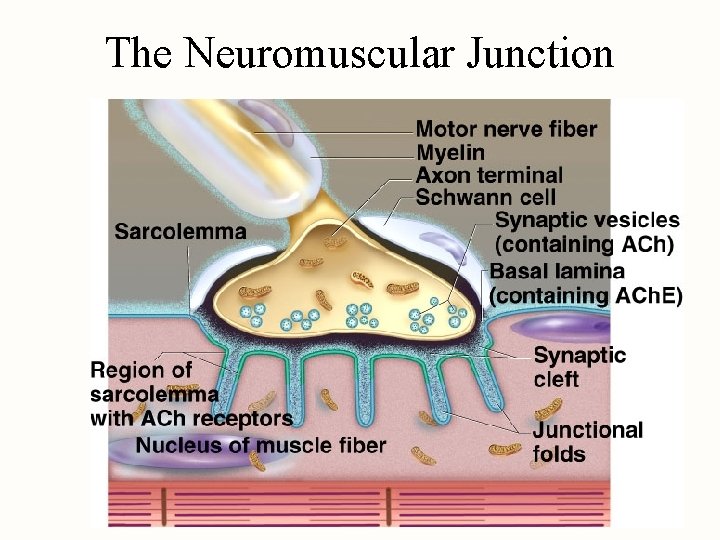
The Neuromuscular Junction
• • • Botulism Poisoning by bacteria Clostridium botulinum Gets in through spoiled food releases most potent neurotoxin known Botulin, brand name: Botox – It prevents neurons from releasing Ach – Muscles exhibit flaccid paralysis – lethal dose of about 200 -300 pg/kg, meaning that somewhat over a hundred grams could kill every human living on the earth (for perspective, the rat poison Strychnine, often described as highly toxic, has an LD 50 of 1 mg/kg, or 1 billion pg/kg). Symptoms start with double vision as eye muscles go Ronald Reagan is rumored to have been among first to receive treatment in 1960 s
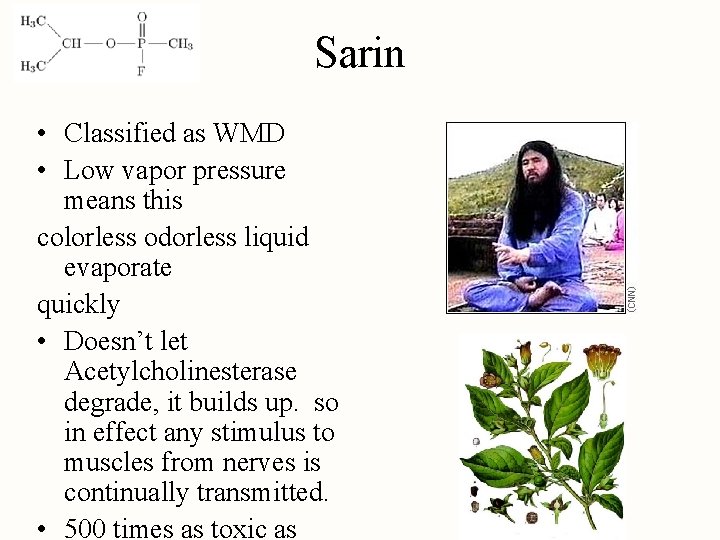
Sarin • Classified as WMD • Low vapor pressure means this colorless odorless liquid evaporate quickly • Doesn’t let Acetylcholinesterase degrade, it builds up. so in effect any stimulus to muscles from nerves is continually transmitted. • 500 times as toxic as
Atropine • Derivitive of Deadly Nightshade (Belladona • Atropos was the fate who decided your death • Competitive inhibitor for Ac. H receptors, so it fills up the plug where Ac. H would go to excite muscles • If nerve gases flood the system with Ac. H Atropine competes with the Ac. H for its receptor sites.
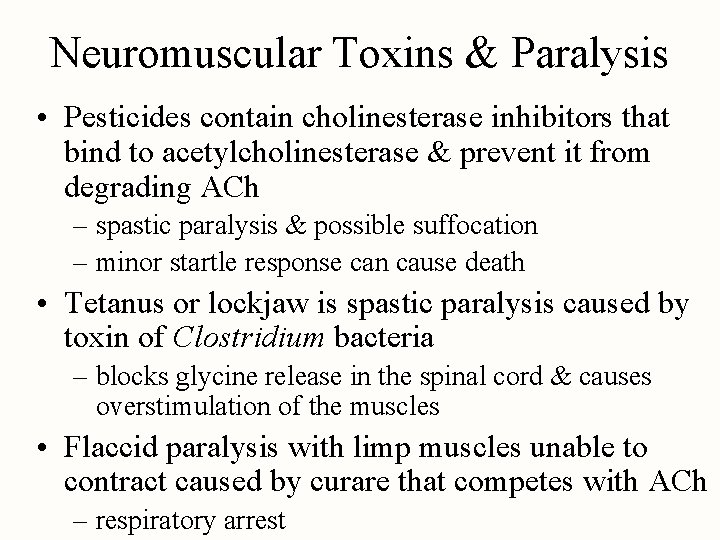
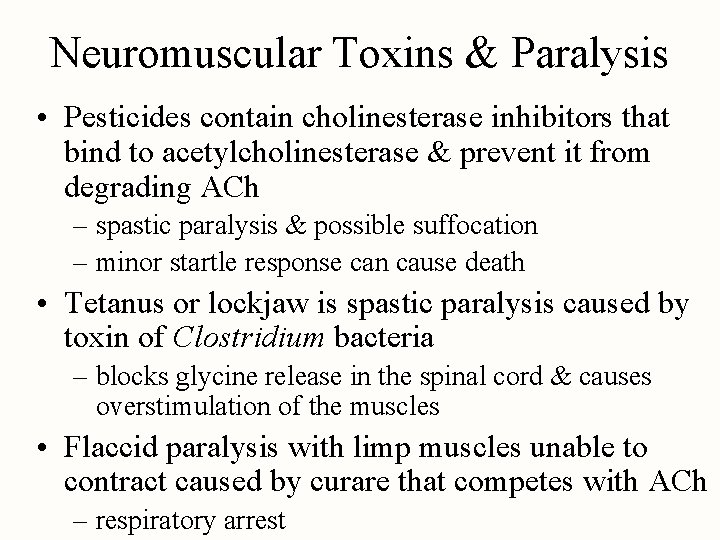
Neuromuscular Toxins & Paralysis • Pesticides contain cholinesterase inhibitors that bind to acetylcholinesterase & prevent it from degrading ACh – spastic paralysis & possible suffocation – minor startle response can cause death • Tetanus or lockjaw is spastic paralysis caused by toxin of Clostridium bacteria – blocks glycine release in the spinal cord & causes overstimulation of the muscles • Flaccid paralysis with limp muscles unable to contract caused by curare that competes with ACh – respiratory arrest
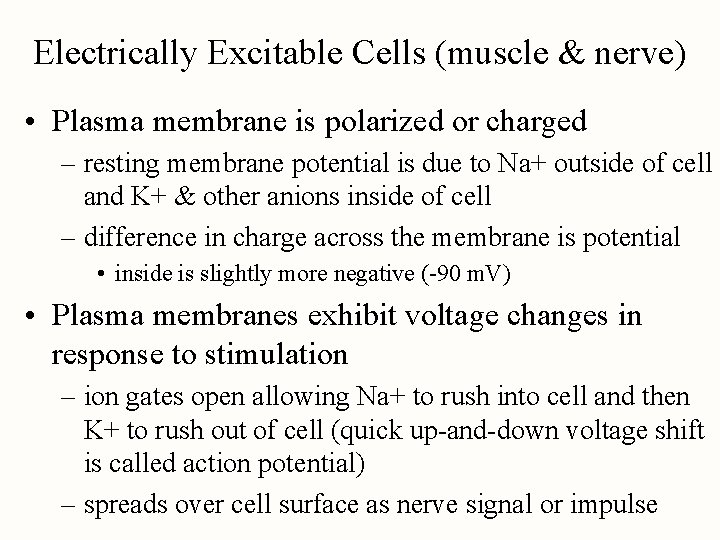
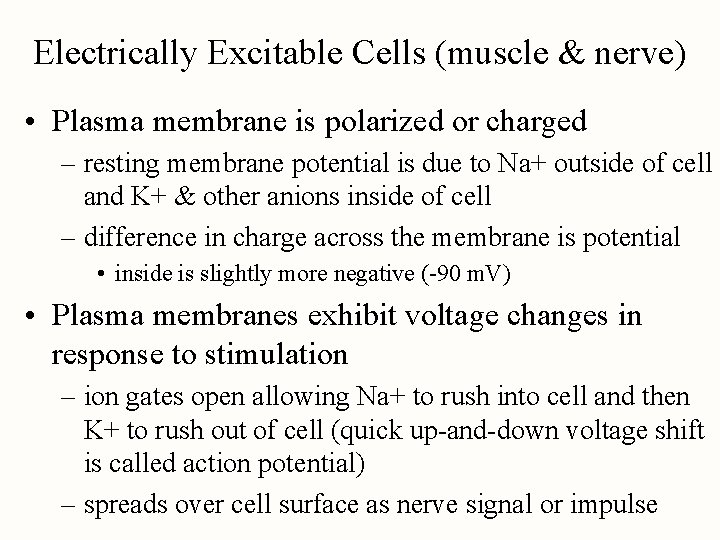
Electrically Excitable Cells (muscle & nerve) • Plasma membrane is polarized or charged – resting membrane potential is due to Na+ outside of cell and K+ & other anions inside of cell – difference in charge across the membrane is potential • inside is slightly more negative (-90 m. V) • Plasma membranes exhibit voltage changes in response to stimulation – ion gates open allowing Na+ to rush into cell and then K+ to rush out of cell (quick up-and-down voltage shift is called action potential) – spreads over cell surface as nerve signal or impulse
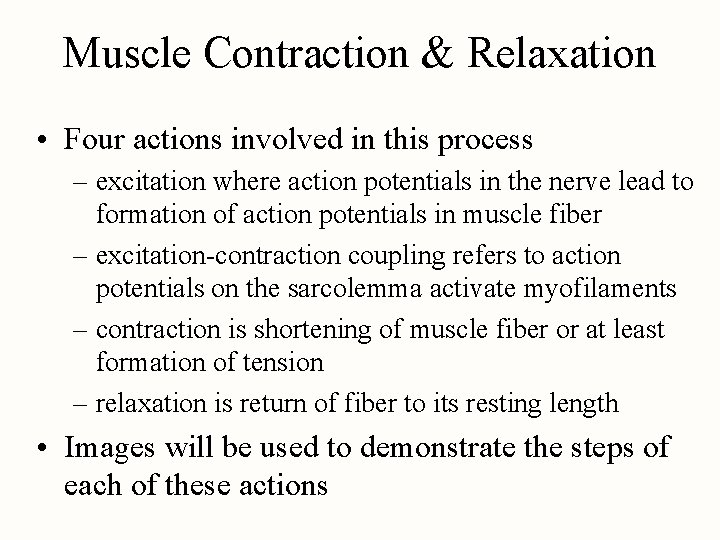
Muscle Contraction & Relaxation • Four actions involved in this process – excitation where action potentials in the nerve lead to formation of action potentials in muscle fiber – excitation-contraction coupling refers to action potentials on the sarcolemma activate myofilaments – contraction is shortening of muscle fiber or at least formation of tension – relaxation is return of fiber to its resting length • Images will be used to demonstrate the steps of each of these actions
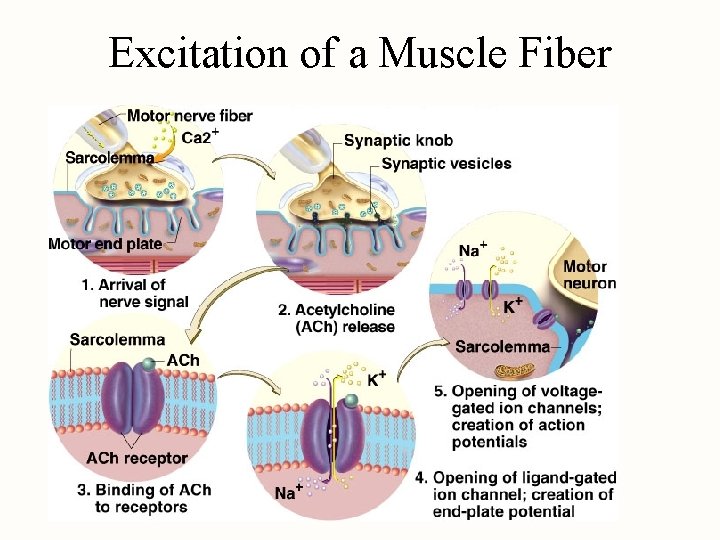
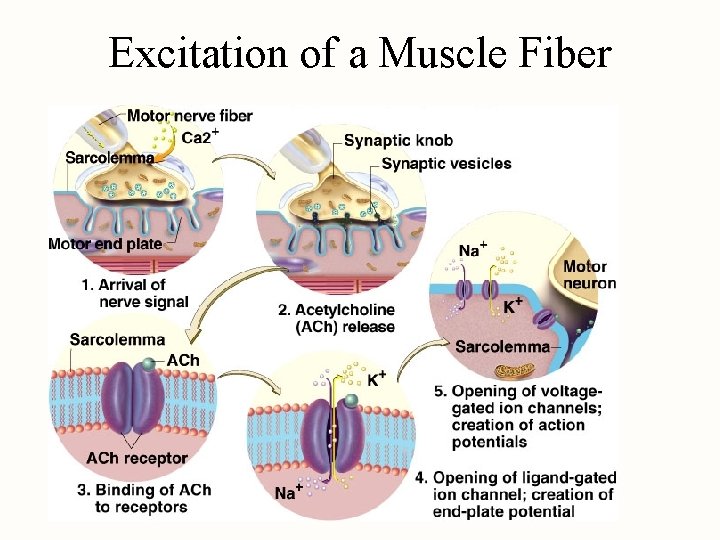
Excitation of a Muscle Fiber
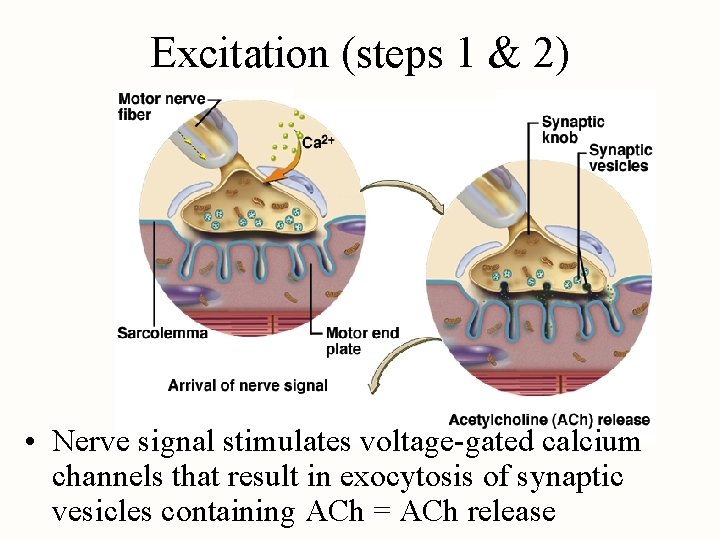
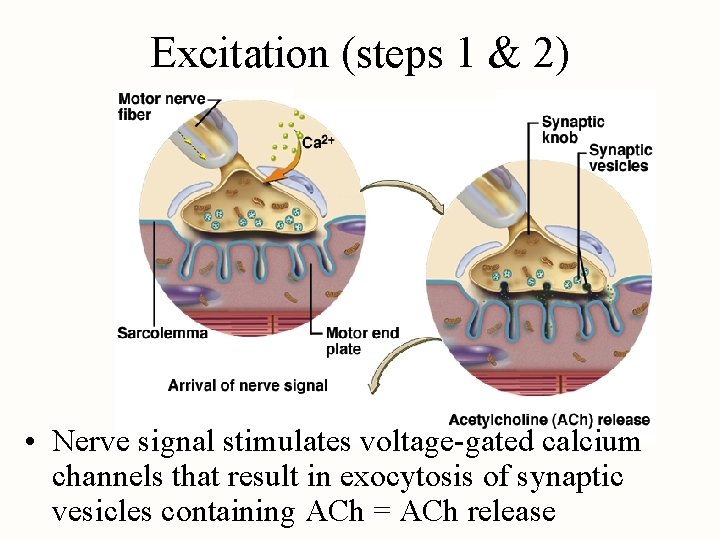
Excitation (steps 1 & 2) • Nerve signal stimulates voltage-gated calcium channels that result in exocytosis of synaptic vesicles containing ACh = ACh release
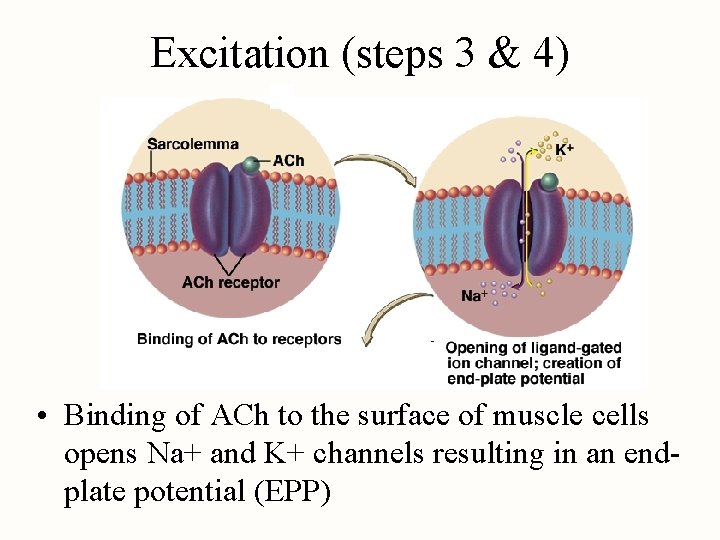
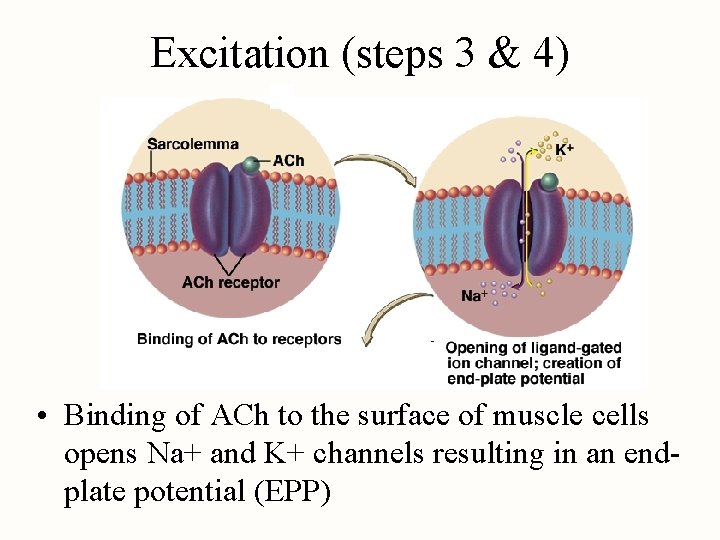
Excitation (steps 3 & 4) • Binding of ACh to the surface of muscle cells opens Na+ and K+ channels resulting in an endplate potential (EPP)
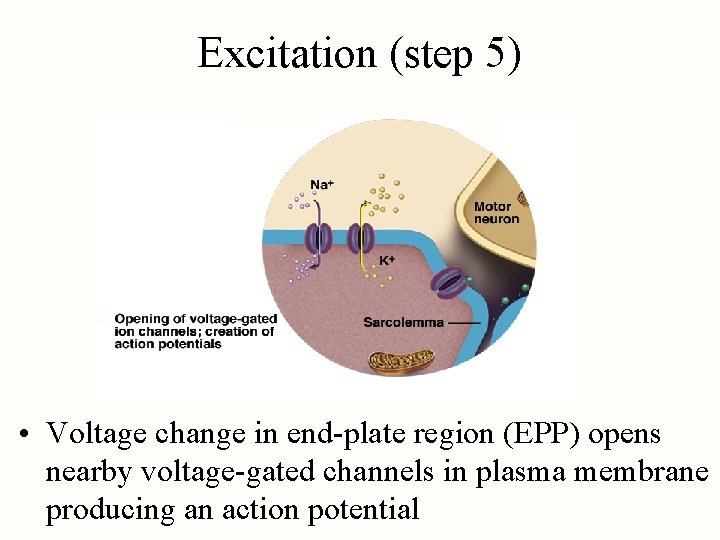
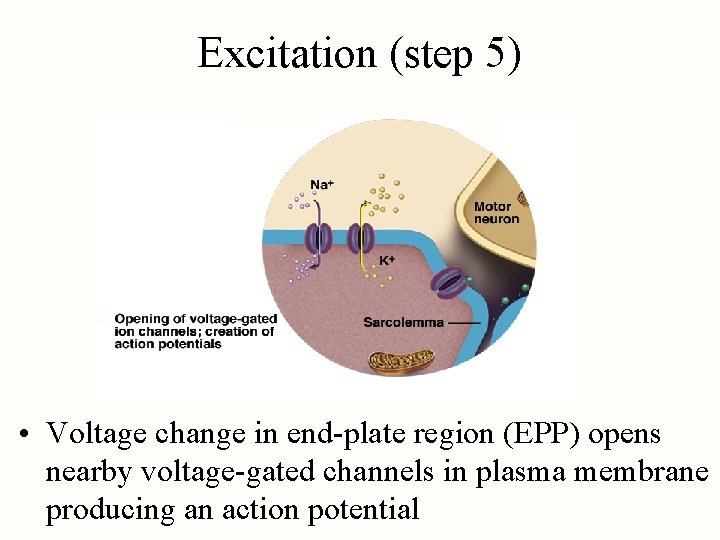
Excitation (step 5) • Voltage change in end-plate region (EPP) opens nearby voltage-gated channels in plasma membrane producing an action potential
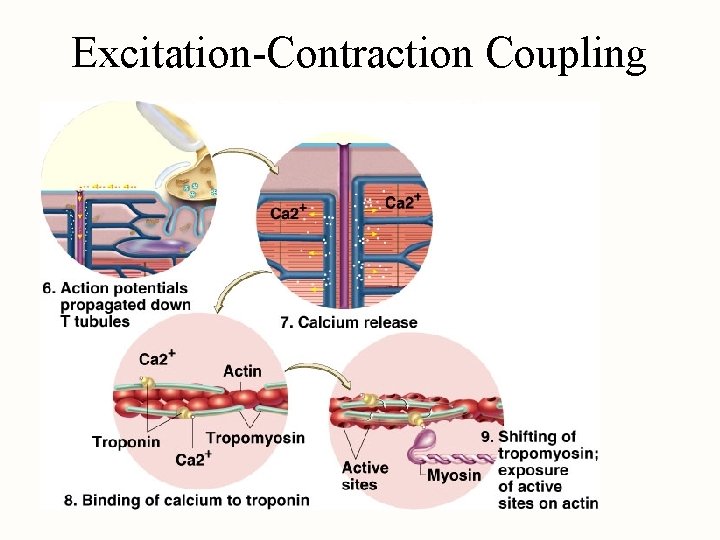
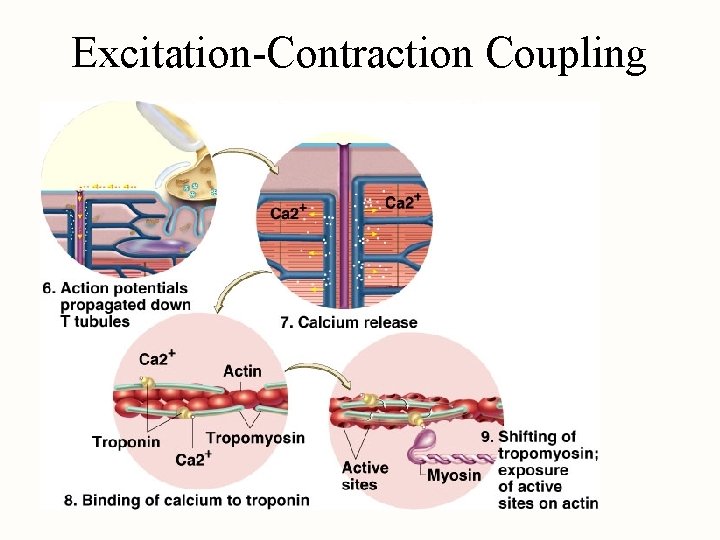
Excitation-Contraction Coupling
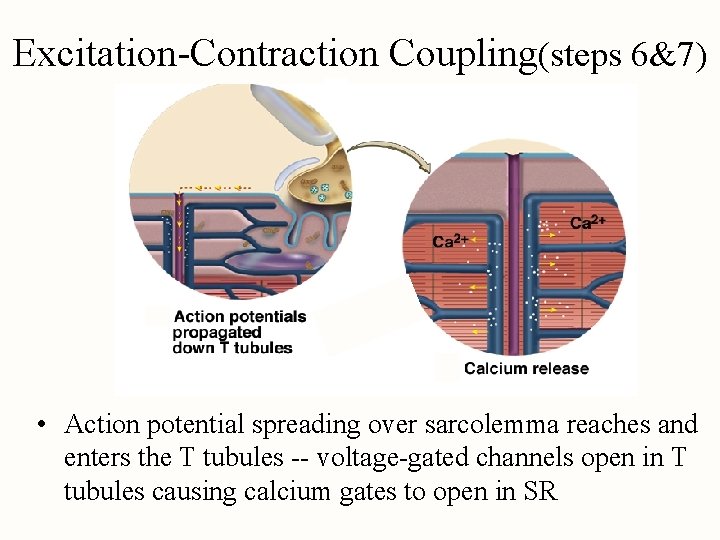
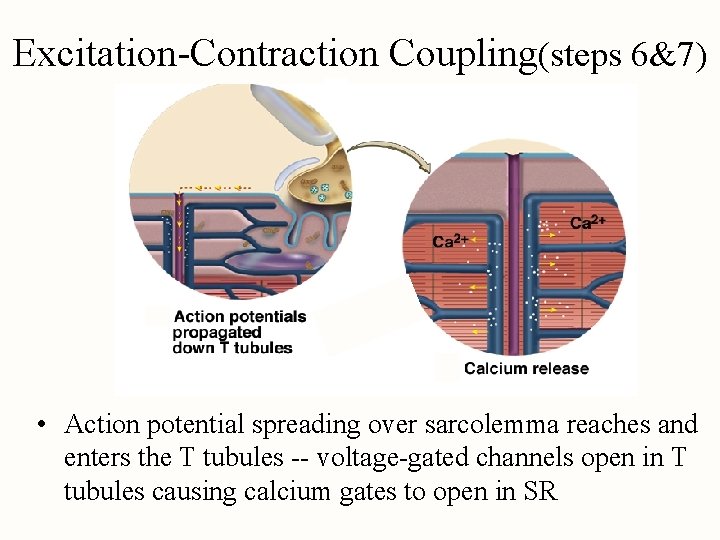
Excitation-Contraction Coupling(steps 6&7) • Action potential spreading over sarcolemma reaches and enters the T tubules -- voltage-gated channels open in T tubules causing calcium gates to open in SR
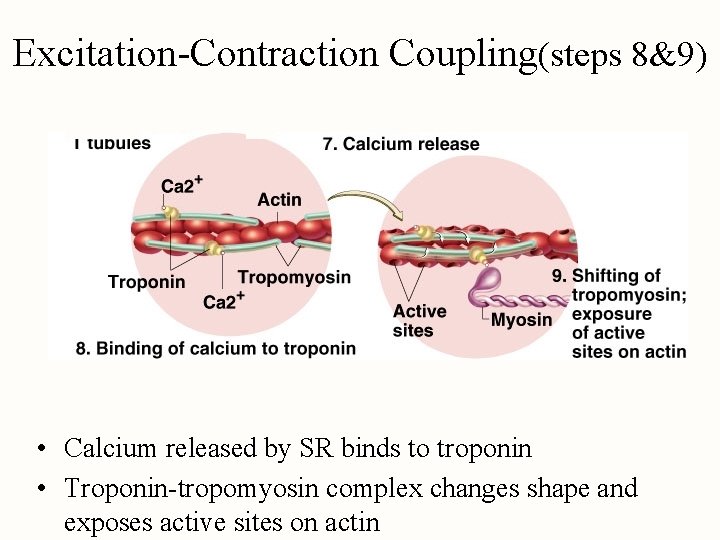
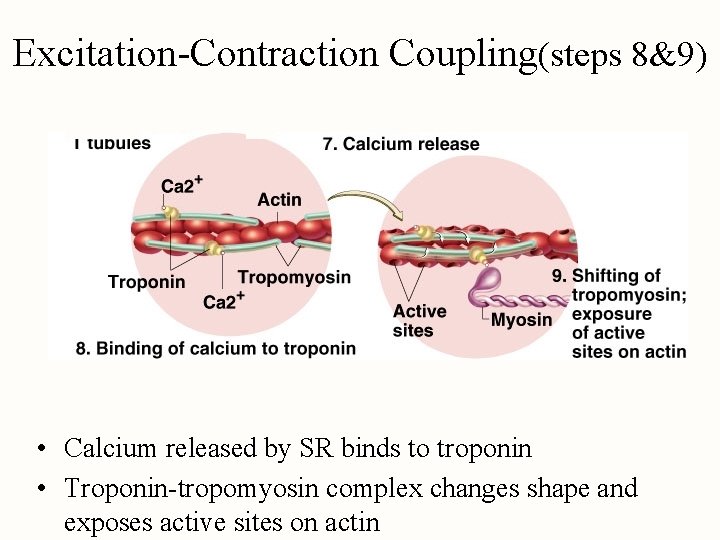
Excitation-Contraction Coupling(steps 8&9) • Calcium released by SR binds to troponin • Troponin-tropomyosin complex changes shape and exposes active sites on actin
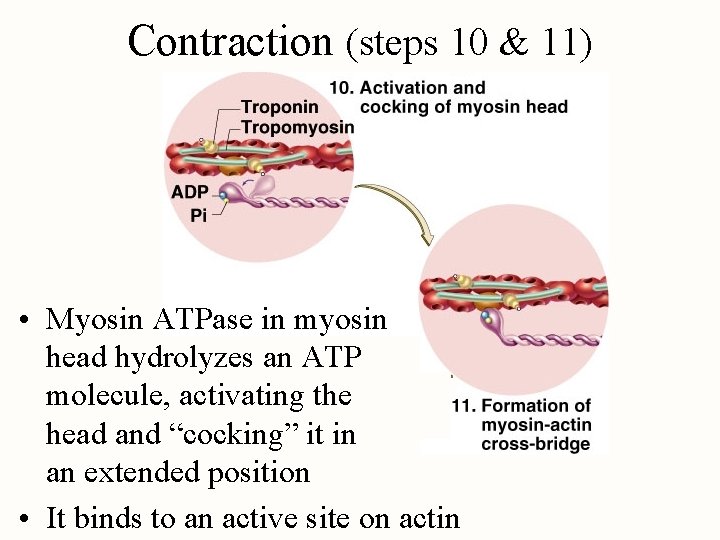
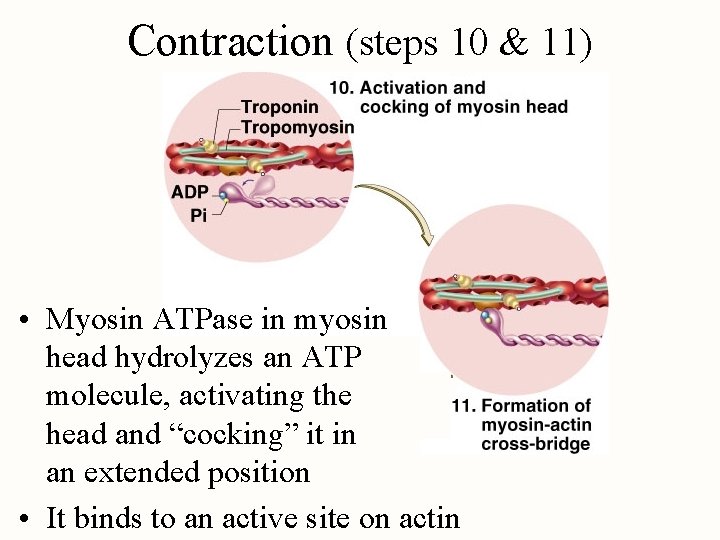
Contraction (steps 10 & 11) • Myosin ATPase in myosin head hydrolyzes an ATP molecule, activating the head and “cocking” it in an extended position • It binds to an active site on actin
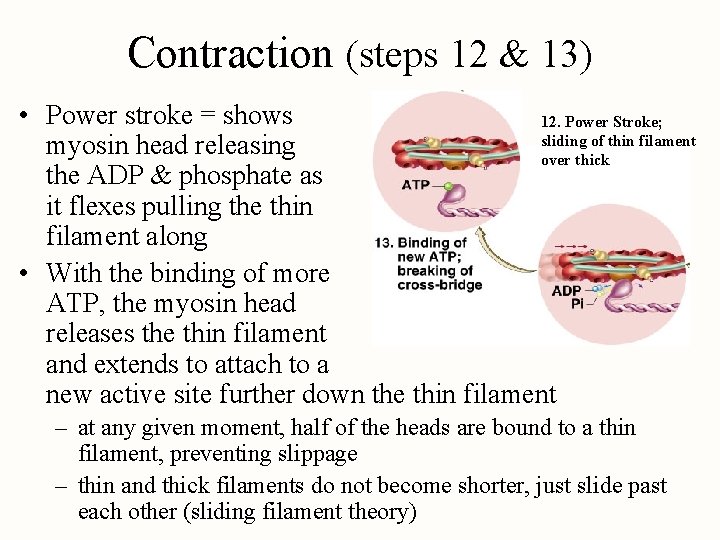
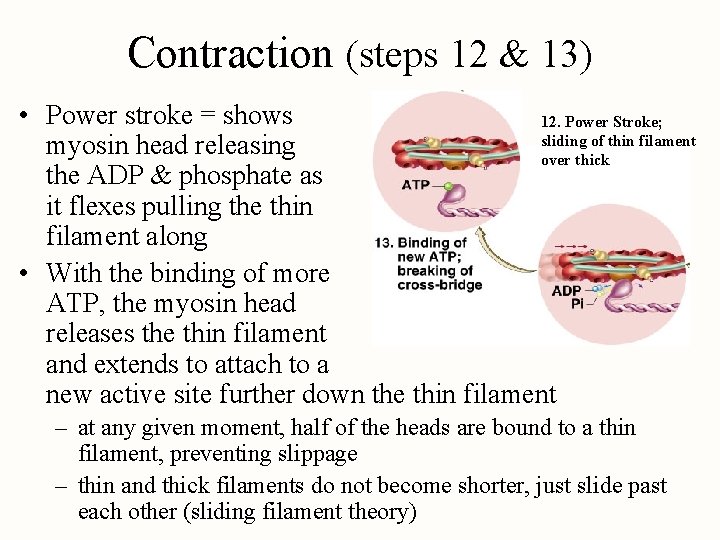
Contraction (steps 12 & 13) • Power stroke = shows 12. Power Stroke; sliding of thin filament myosin head releasing over thick the ADP & phosphate as it flexes pulling the thin filament along • With the binding of more ATP, the myosin head releases the thin filament and extends to attach to a new active site further down the thin filament – at any given moment, half of the heads are bound to a thin filament, preventing slippage – thin and thick filaments do not become shorter, just slide past each other (sliding filament theory)
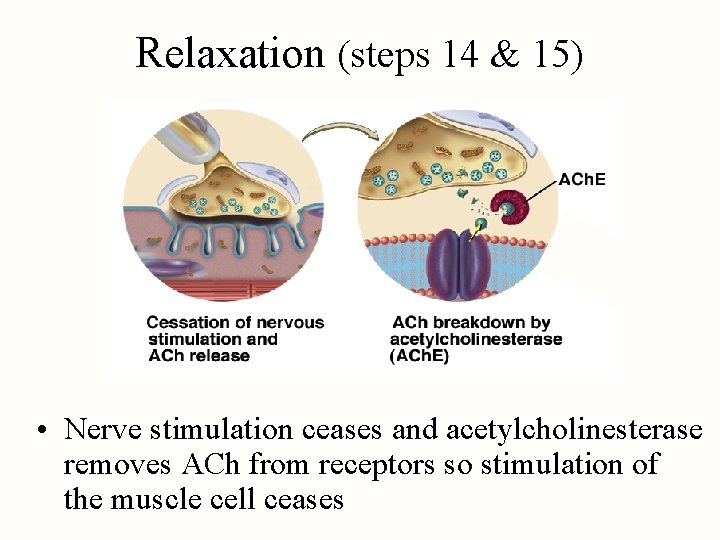
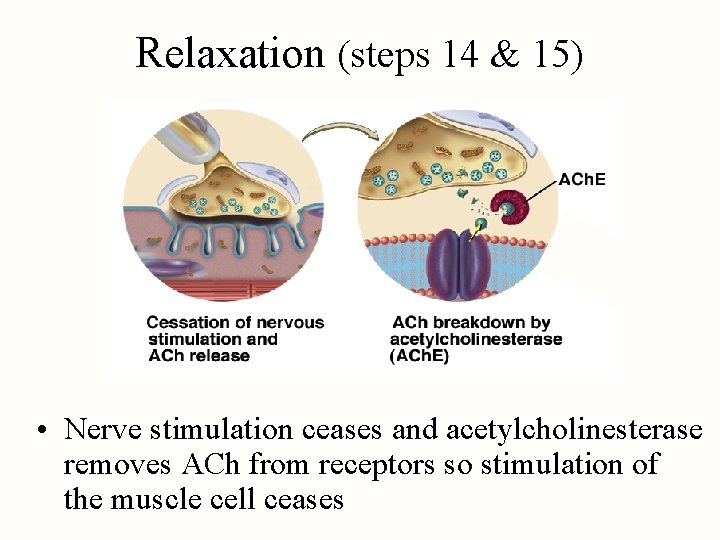
Relaxation (steps 14 & 15) • Nerve stimulation ceases and acetylcholinesterase removes ACh from receptors so stimulation of the muscle cell ceases
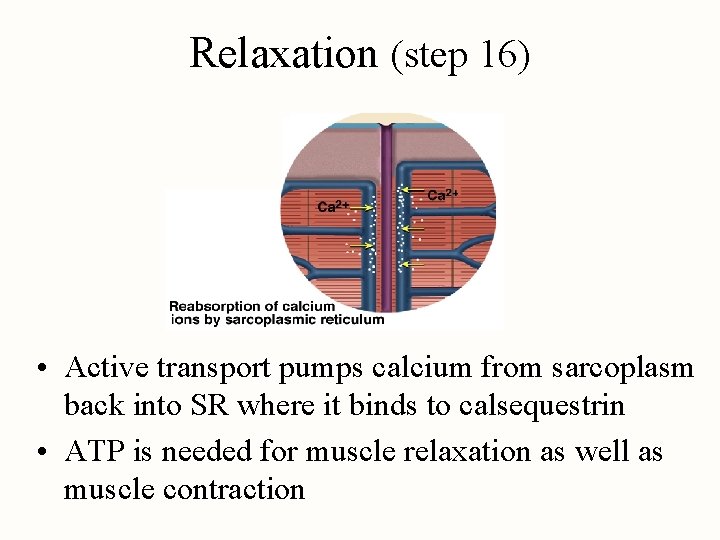
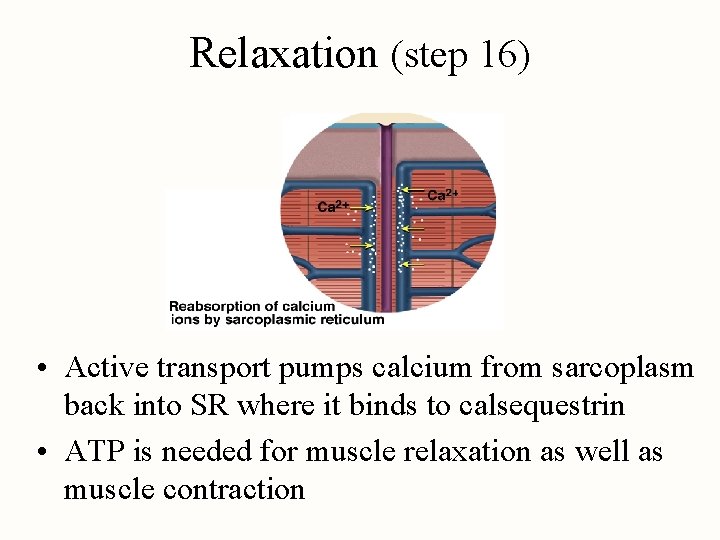
Relaxation (step 16) • Active transport pumps calcium from sarcoplasm back into SR where it binds to calsequestrin • ATP is needed for muscle relaxation as well as muscle contraction
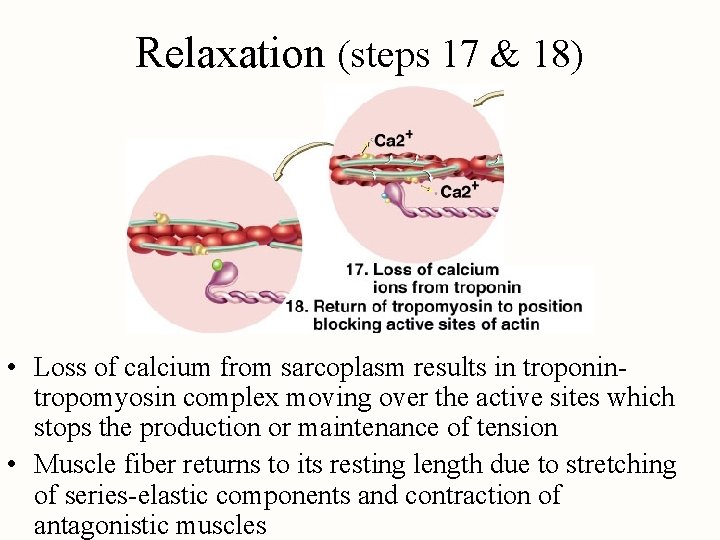
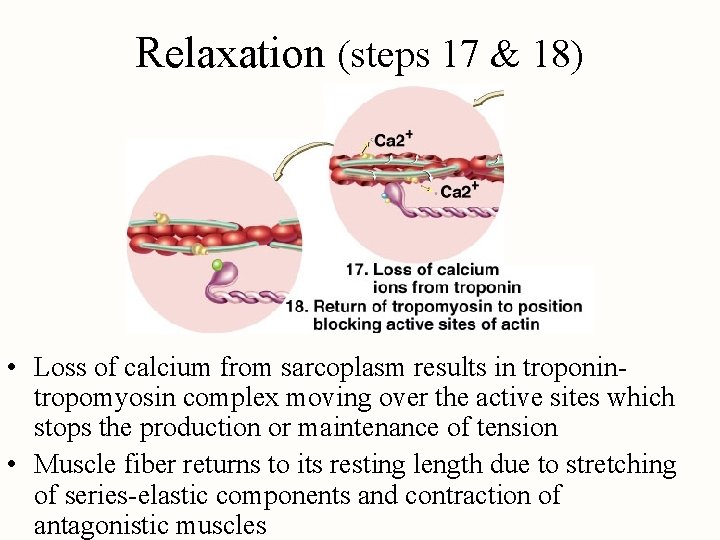
Relaxation (steps 17 & 18) • Loss of calcium from sarcoplasm results in troponintropomyosin complex moving over the active sites which stops the production or maintenance of tension • Muscle fiber returns to its resting length due to stretching of series-elastic components and contraction of antagonistic muscles
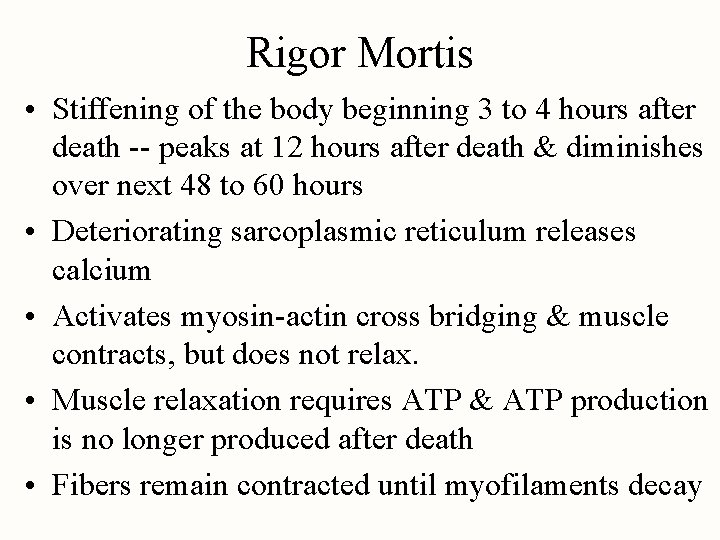
Rigor Mortis • Stiffening of the body beginning 3 to 4 hours after death -- peaks at 12 hours after death & diminishes over next 48 to 60 hours • Deteriorating sarcoplasmic reticulum releases calcium • Activates myosin-actin cross bridging & muscle contracts, but does not relax. • Muscle relaxation requires ATP & ATP production is no longer produced after death • Fibers remain contracted until myofilaments decay
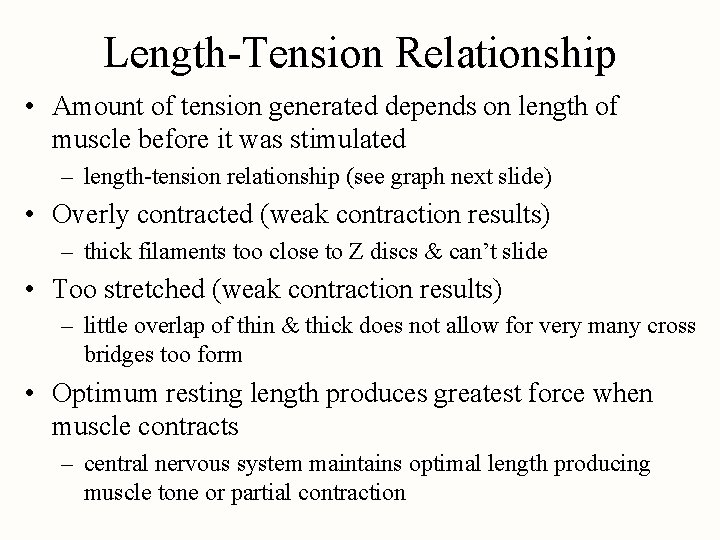
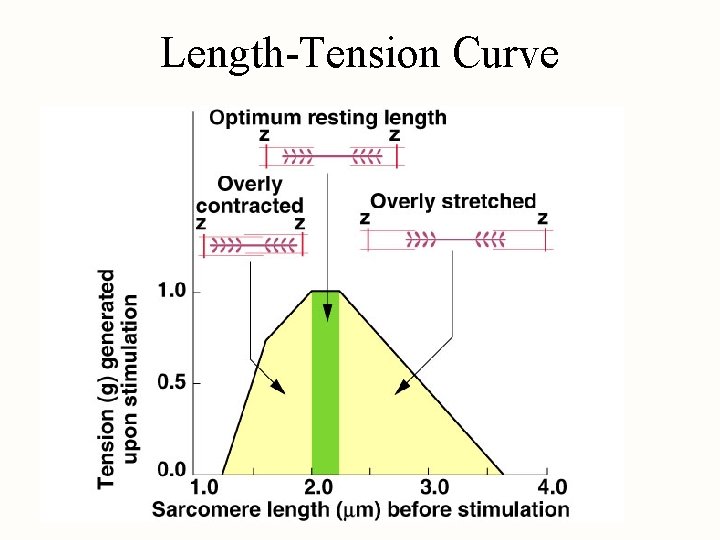
Length-Tension Relationship • Amount of tension generated depends on length of muscle before it was stimulated – length-tension relationship (see graph next slide) • Overly contracted (weak contraction results) – thick filaments too close to Z discs & can’t slide • Too stretched (weak contraction results) – little overlap of thin & thick does not allow for very many cross bridges too form • Optimum resting length produces greatest force when muscle contracts – central nervous system maintains optimal length producing muscle tone or partial contraction
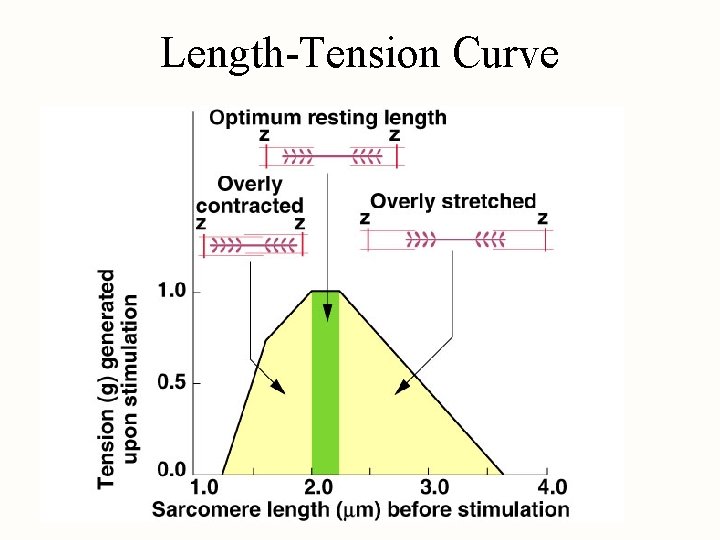
Length-Tension Curve
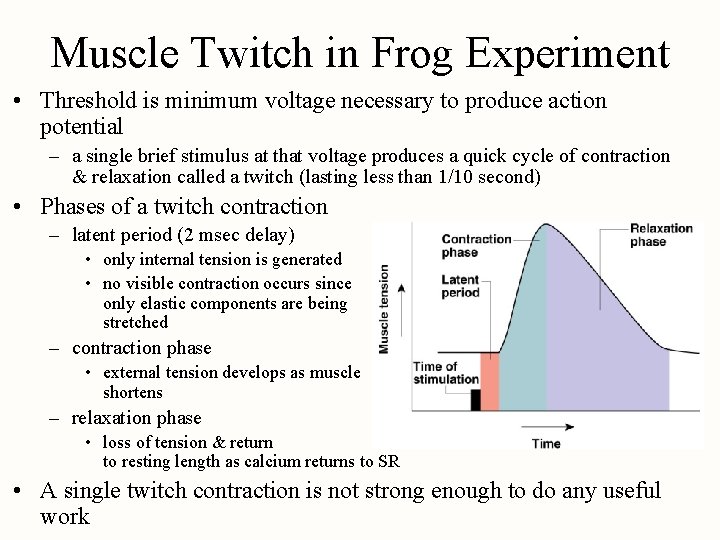
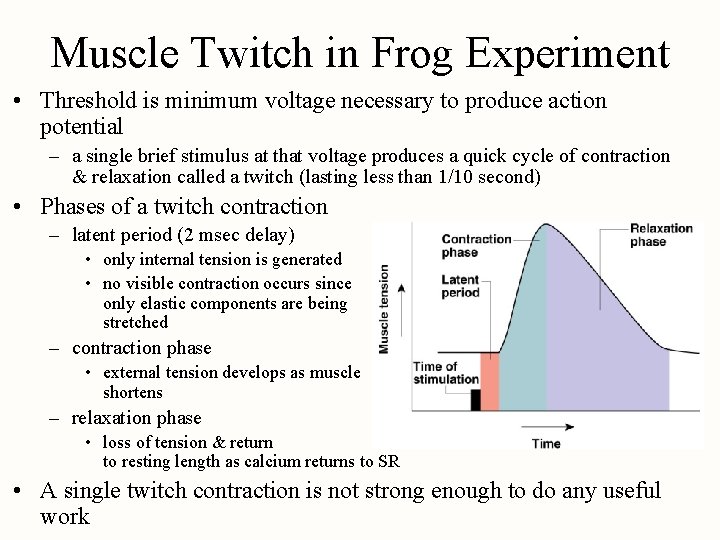
Muscle Twitch in Frog Experiment • Threshold is minimum voltage necessary to produce action potential – a single brief stimulus at that voltage produces a quick cycle of contraction & relaxation called a twitch (lasting less than 1/10 second) • Phases of a twitch contraction – latent period (2 msec delay) • only internal tension is generated • no visible contraction occurs since only elastic components are being stretched – contraction phase • external tension develops as muscle shortens – relaxation phase • loss of tension & return to resting length as calcium returns to SR • A single twitch contraction is not strong enough to do any useful work
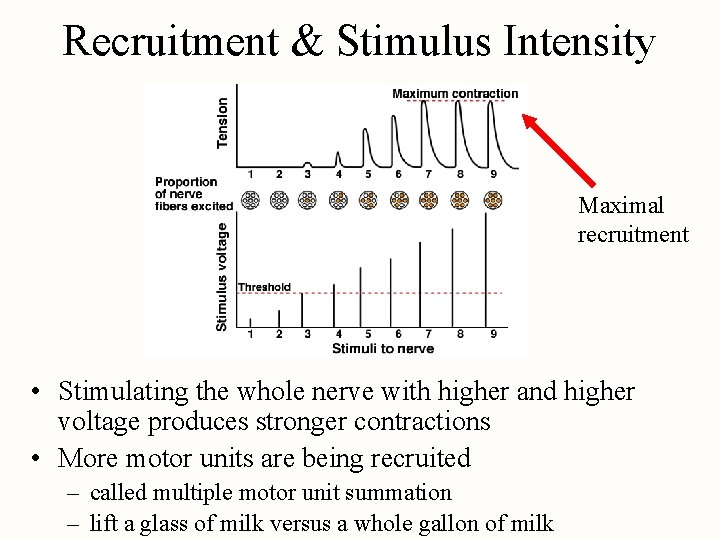
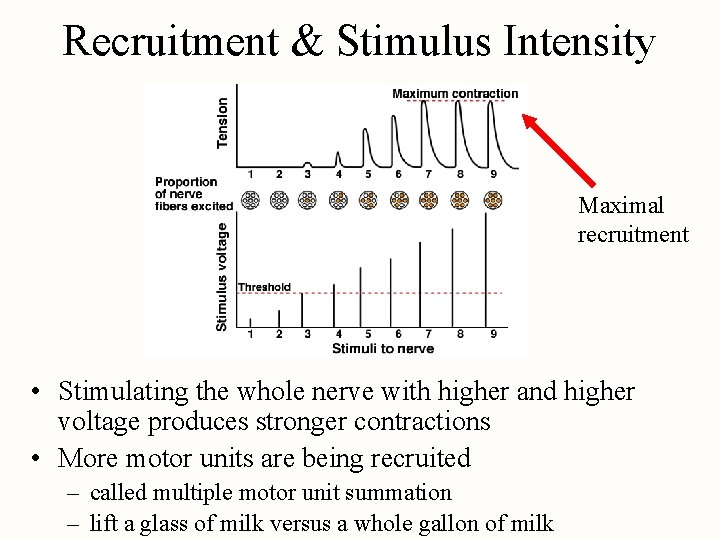
Recruitment & Stimulus Intensity Maximal recruitment • Stimulating the whole nerve with higher and higher voltage produces stronger contractions • More motor units are being recruited – called multiple motor unit summation – lift a glass of milk versus a whole gallon of milk
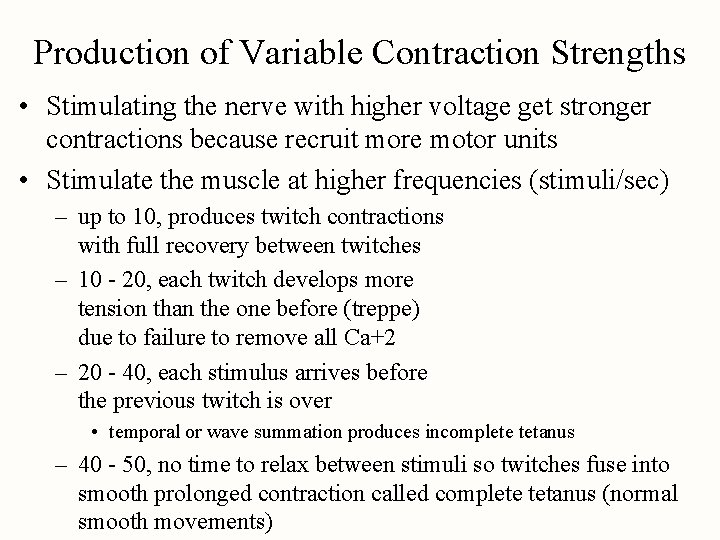
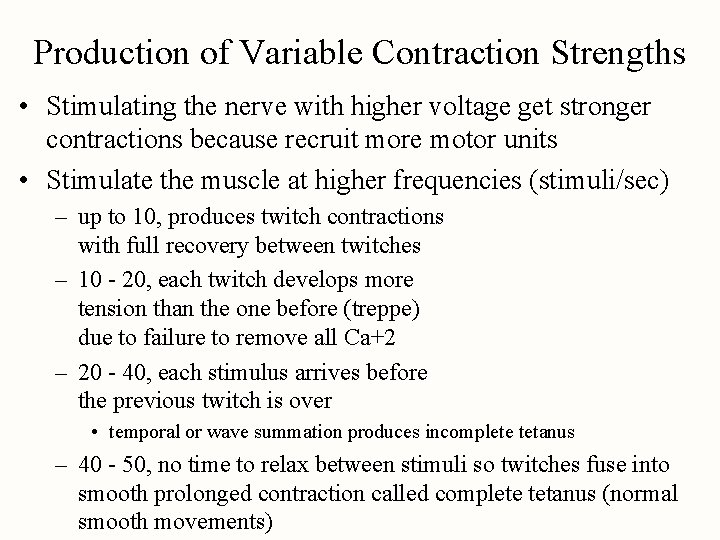
Production of Variable Contraction Strengths • Stimulating the nerve with higher voltage get stronger contractions because recruit more motor units • Stimulate the muscle at higher frequencies (stimuli/sec) – up to 10, produces twitch contractions with full recovery between twitches – 10 - 20, each twitch develops more tension than the one before (treppe) due to failure to remove all Ca+2 – 20 - 40, each stimulus arrives before the previous twitch is over • temporal or wave summation produces incomplete tetanus – 40 - 50, no time to relax between stimuli so twitches fuse into smooth prolonged contraction called complete tetanus (normal smooth movements)
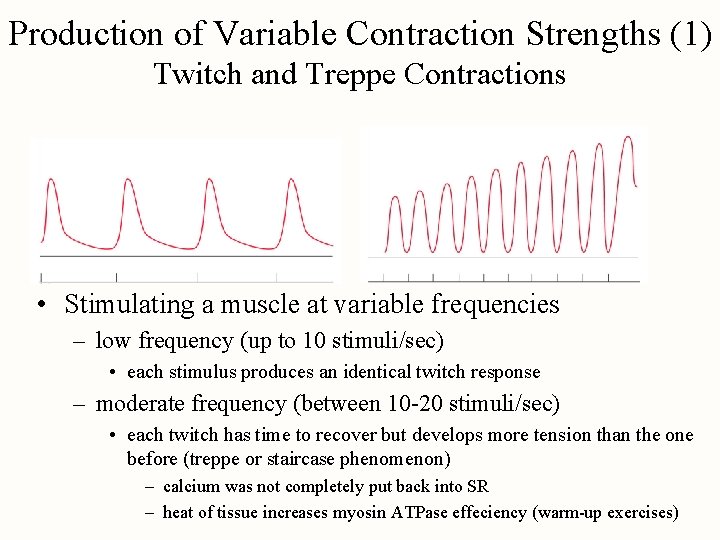
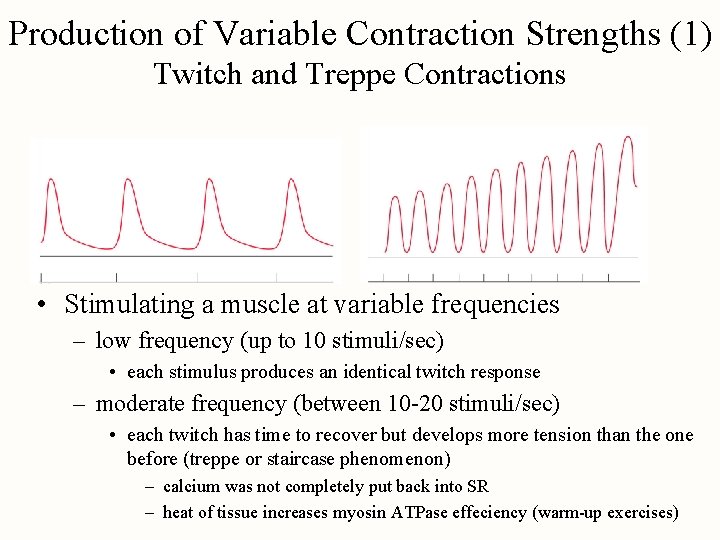
Production of Variable Contraction Strengths (1) Twitch and Treppe Contractions • Stimulating a muscle at variable frequencies – low frequency (up to 10 stimuli/sec) • each stimulus produces an identical twitch response – moderate frequency (between 10 -20 stimuli/sec) • each twitch has time to recover but develops more tension than the one before (treppe or staircase phenomenon) – calcium was not completely put back into SR – heat of tissue increases myosin ATPase effeciency (warm-up exercises)
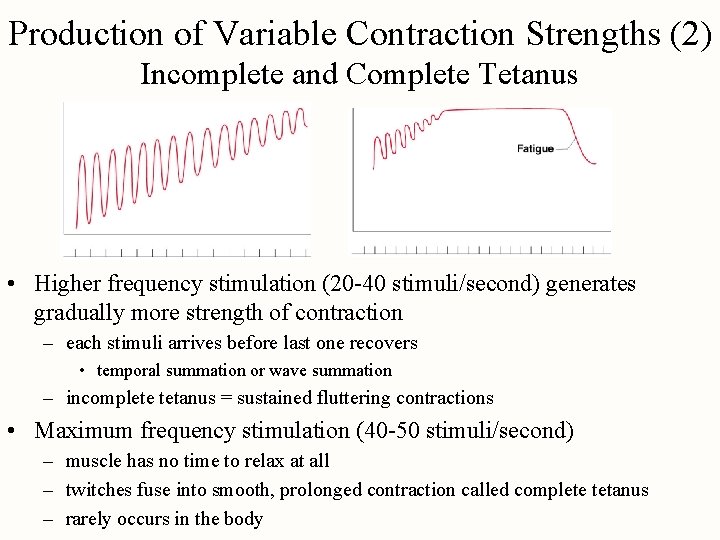
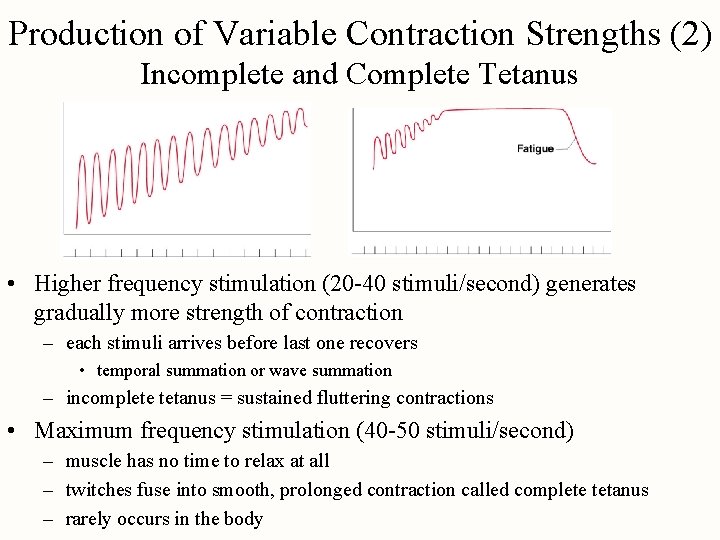
Production of Variable Contraction Strengths (2) Incomplete and Complete Tetanus • Higher frequency stimulation (20 -40 stimuli/second) generates gradually more strength of contraction – each stimuli arrives before last one recovers • temporal summation or wave summation – incomplete tetanus = sustained fluttering contractions • Maximum frequency stimulation (40 -50 stimuli/second) – muscle has no time to relax at all – twitches fuse into smooth, prolonged contraction called complete tetanus – rarely occurs in the body
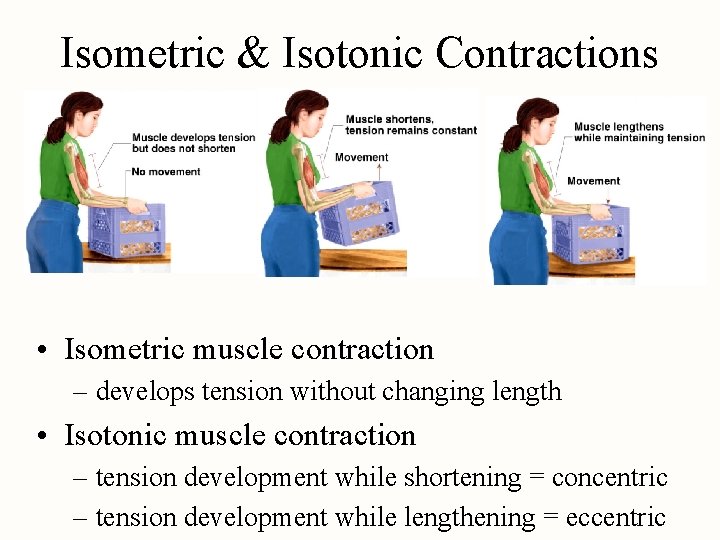
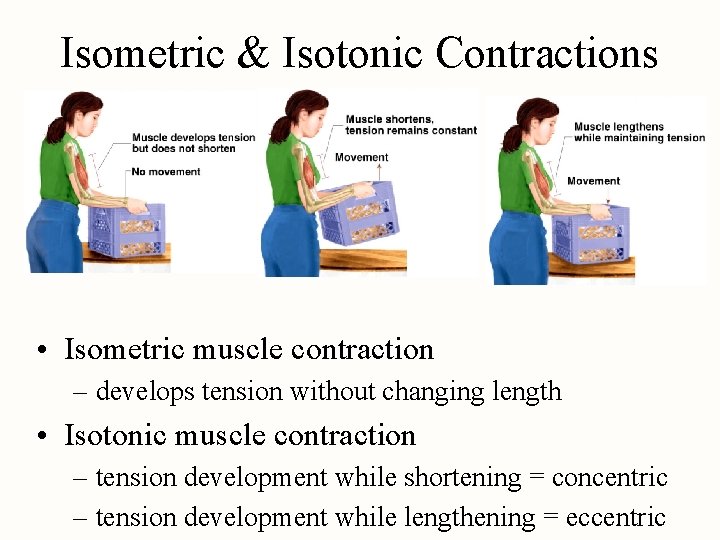
Isometric & Isotonic Contractions • Isometric muscle contraction – develops tension without changing length • Isotonic muscle contraction – tension development while shortening = concentric – tension development while lengthening = eccentric
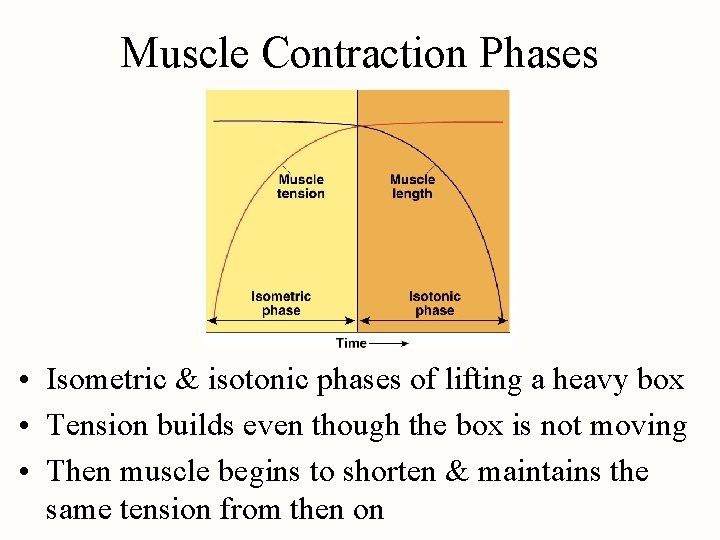
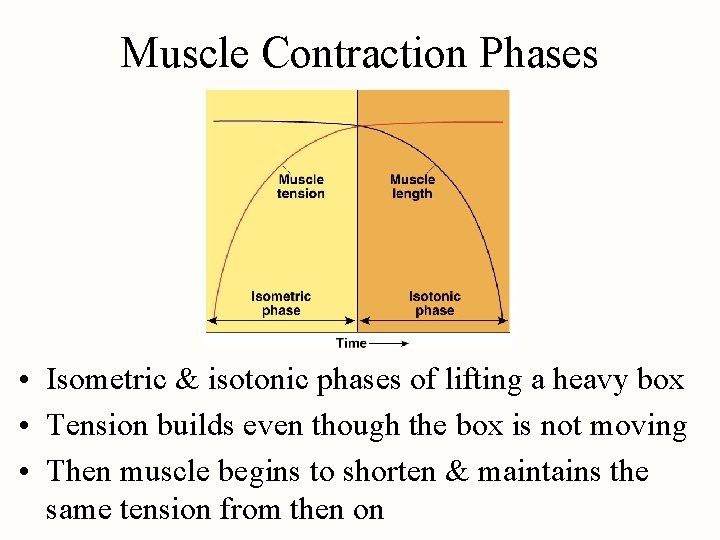
Muscle Contraction Phases • Isometric & isotonic phases of lifting a heavy box • Tension builds even though the box is not moving • Then muscle begins to shorten & maintains the same tension from then on
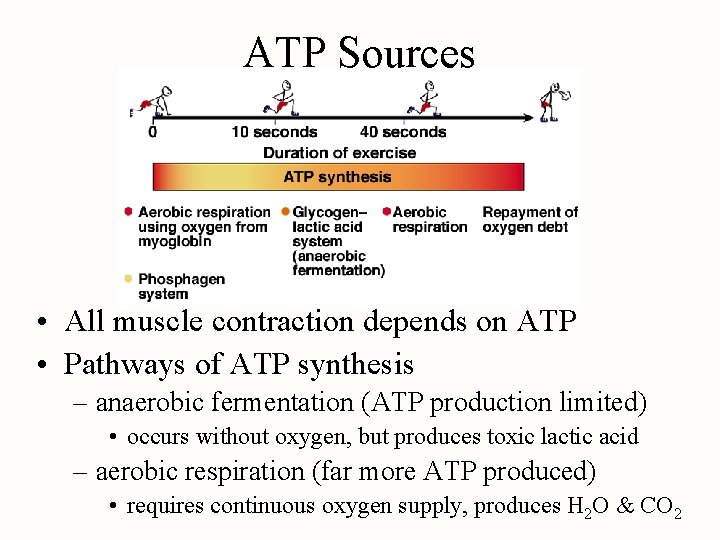
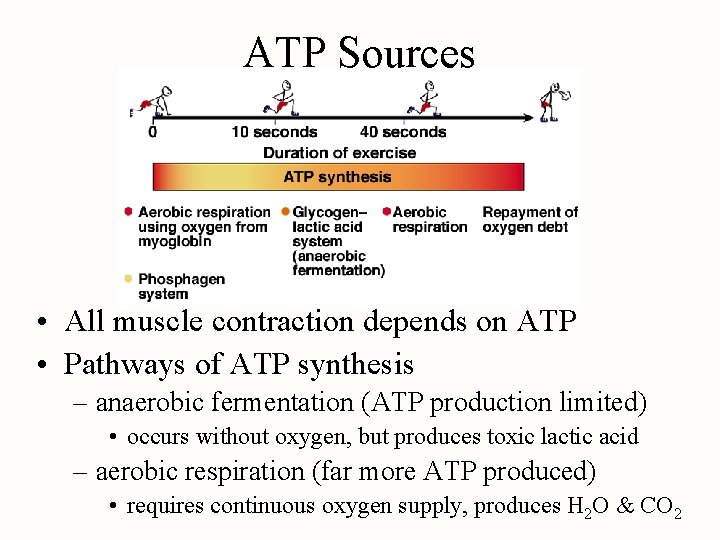
ATP Sources • All muscle contraction depends on ATP • Pathways of ATP synthesis – anaerobic fermentation (ATP production limited) • occurs without oxygen, but produces toxic lactic acid – aerobic respiration (far more ATP produced) • requires continuous oxygen supply, produces H 2 O & CO 2
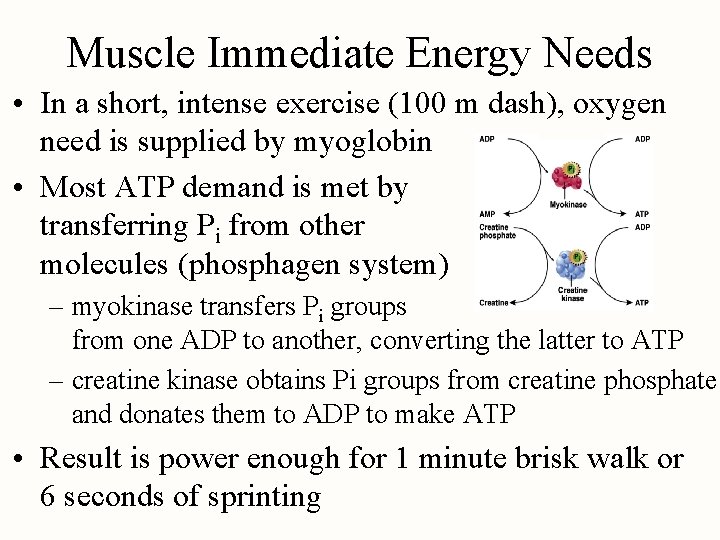
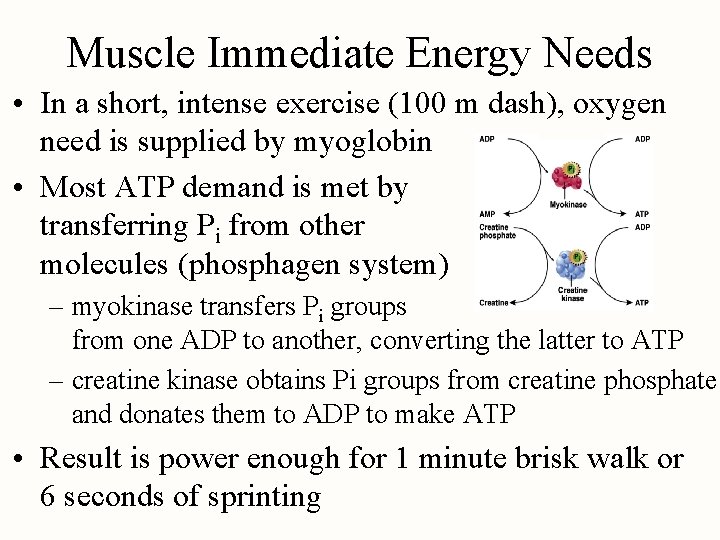
Muscle Immediate Energy Needs • In a short, intense exercise (100 m dash), oxygen need is supplied by myoglobin • Most ATP demand is met by transferring Pi from other molecules (phosphagen system) – myokinase transfers Pi groups from one ADP to another, converting the latter to ATP – creatine kinase obtains Pi groups from creatine phosphate and donates them to ADP to make ATP • Result is power enough for 1 minute brisk walk or 6 seconds of sprinting
Muscle Short-Term Energy Needs • Once phosphagen system is exhausted, glycogenlactic acid system (anaerobic fermentation) takes over – produces ATP for 30 -40 seconds of maximum activity – muscles obtain glucose from blood & stored glycogen – while playing basketball or running around baseball diamonds
Muscle Long-Term Energy Needs • After 40 seconds of exercise, respiratory & cardiovascular systems “catch up” and begin to deliver enough oxygen for aerobic respiration – oxygen consumption rate increases for first 3 -4 minutes & then levels off to a steady state – ATP production keeps pace with demand • Limits are set by depletion of glycogen & blood glucose, loss of fluid and electrolytes through sweating – little lactic acid buildup occurs
Fatigue • Fatigue is progressive weakness & loss of contractility from prolonged use • Causes – ATP synthesis declines as glycogen is consumed – ATP shortage causes sodium-potassium pumps to fail to maintain membrane potential & excitability – lactic acid lowers p. H of sarcoplasm inhibiting enzyme function – accumulation of extracellular K+ lowers the membrane potential & excitability – motor nerve fibers use up their acetylcholine
Endurance • Ability to maintain high-intensity exercise is determined by maximum oxygen uptake and nutrient availability – VO 2 max is proportional to body size, peaks at age 20, is larger in trained athlete & males – depends on the supply of organic nutrients • fatty acids, amino acids & glucose • carbohydrate loading is used by some athletes – dietary strategy used to pack glycogen into muscle cells – may add water at same time (2. 7 g water with each gram/glycogen) – side effects include “heaviness” feeling
Oxygen Debt • Need to breathe heavily after strenuous exercise – known as excess postexercise oxygen consumption (EPOC) – typically about 11 liters extra is consumed • Purposes for extra oxygen – replace oxygen reserves (myoglobin, blood hemoglobin, in air in the lungs & dissolved in plasma) – replenishing the phosphagen system – reconverting lactic acid to glucose in kidneys and liver – serving the elevated metabolic rate that occurs as long as the body temperature remains elevated by exercise
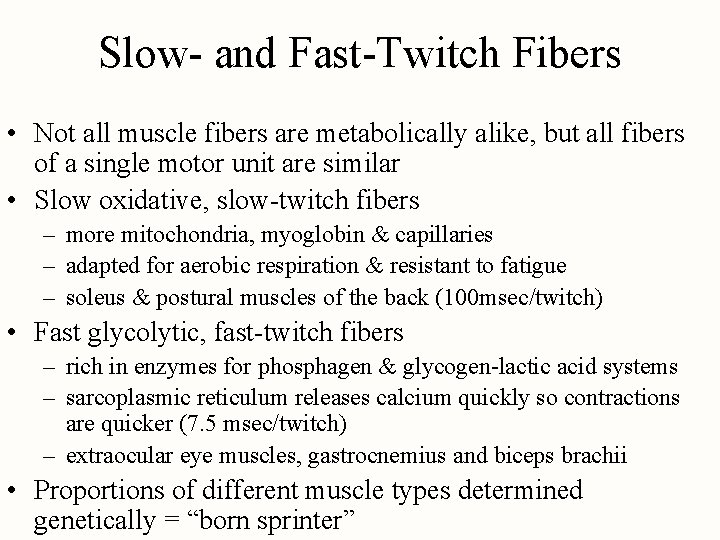
Slow- and Fast-Twitch Fibers • Not all muscle fibers are metabolically alike, but all fibers of a single motor unit are similar • Slow oxidative, slow-twitch fibers – more mitochondria, myoglobin & capillaries – adapted for aerobic respiration & resistant to fatigue – soleus & postural muscles of the back (100 msec/twitch) • Fast glycolytic, fast-twitch fibers – rich in enzymes for phosphagen & glycogen-lactic acid systems – sarcoplasmic reticulum releases calcium quickly so contractions are quicker (7. 5 msec/twitch) – extraocular eye muscles, gastrocnemius and biceps brachii • Proportions of different muscle types determined genetically = “born sprinter”
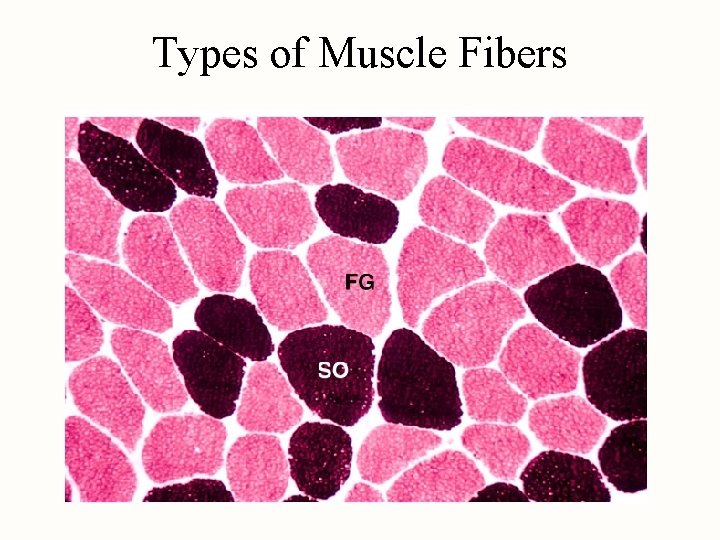
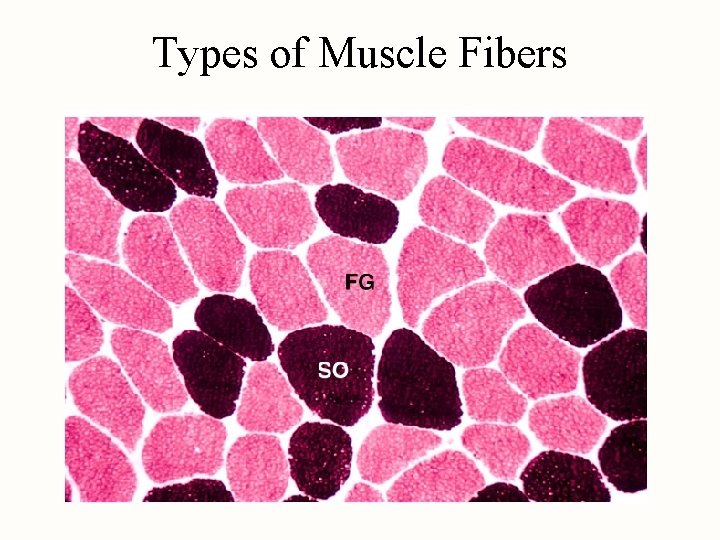
Types of Muscle Fibers
Strength and Conditioning • Factors that increase strength of contraction – muscle size and fascicle arrangement – size of motor units and motor unit recruitment – frequency of stimulations, length of muscle at start of contraction and fatigue • Resistance training (weight lifting) – stimulates cell enlargement due to synthesis of more myofilaments -- some cell splitting may occur • Endurance training (aerobic exercise) – produces an increase in mitochondria, glycogen & density of capillaries
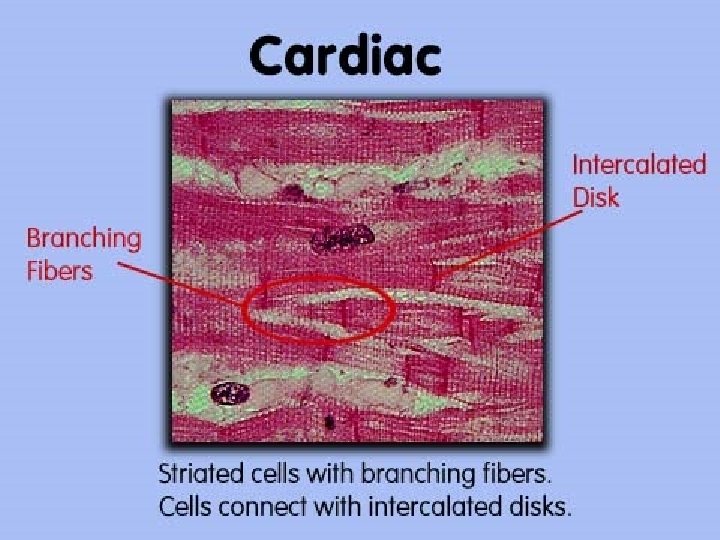
Cardiac Muscle • Cells are shorter, thicker, branched and linked to each other at intercalated discs – electrical gap junctions allow cells to stimulate their neighbors & mechanical junctions keep the cells from pulling apart – sarcoplasmic reticulum is less developed but T tubules are larger to admit Ca+2 from extracellular fluid – damaged cells repaired by fibrosis, not mitosis • Autorhythmic due to pacemaker cells • Uses aerobic respiration almost exclusively – large mitochondria make it resistant to fatigue – very vulnerable to interruptions in oxygen supply
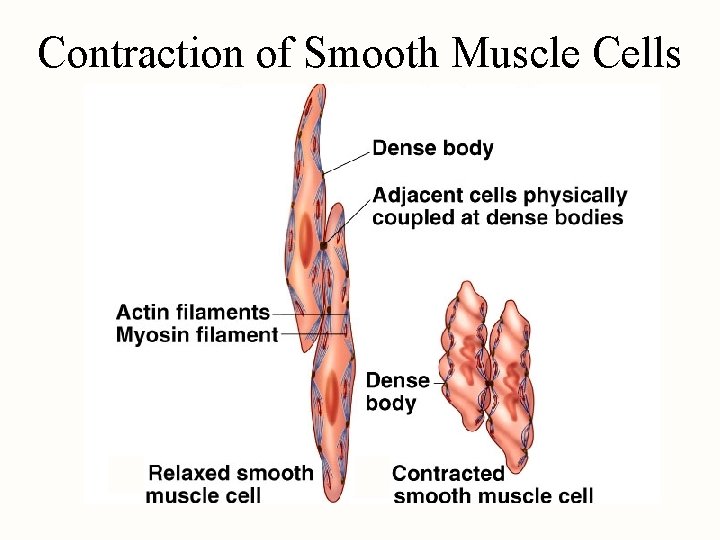
Smooth Muscle • Fusiform cells with one nucleus – 30 to 200 microns long & 5 to 10 microns wide – no visible striations, sarcomeres or Z discs – thin filaments attach to dense bodies scattered throughout sarcoplasm & on sarcolemma – SR is scanty & has no T tubules • calcium for contraction comes from extracellular fluid • If present, nerve supply is autonomic – releases either ACh or norepinephrine – different effects in different locations
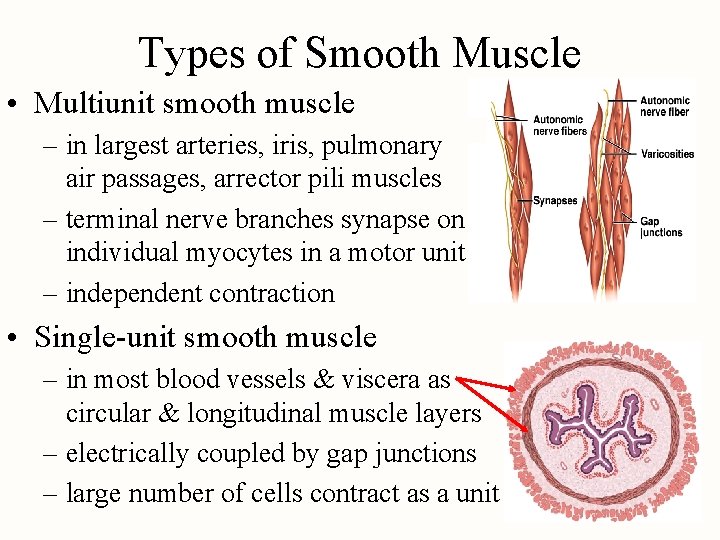
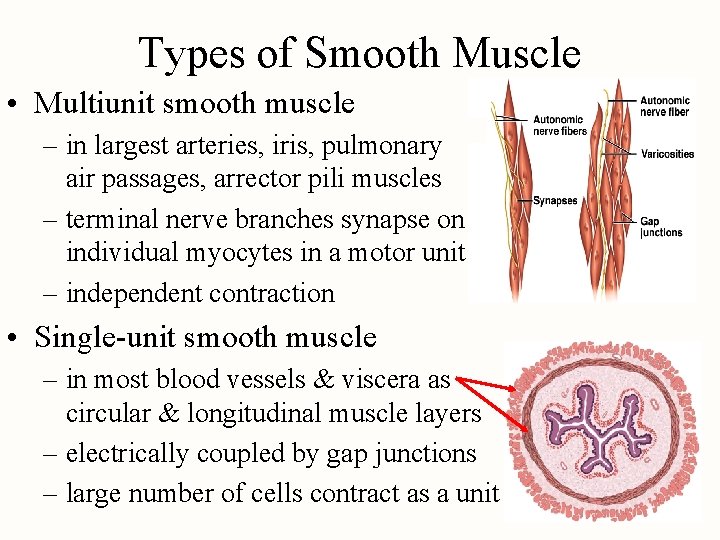
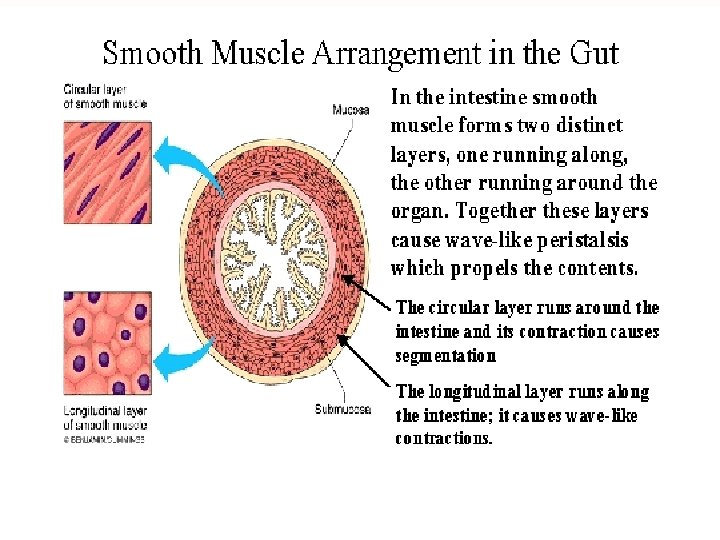
Types of Smooth Muscle • Multiunit smooth muscle – in largest arteries, iris, pulmonary air passages, arrector pili muscles – terminal nerve branches synapse on individual myocytes in a motor unit – independent contraction • Single-unit smooth muscle – in most blood vessels & viscera as circular & longitudinal muscle layers – electrically coupled by gap junctions – large number of cells contract as a unit
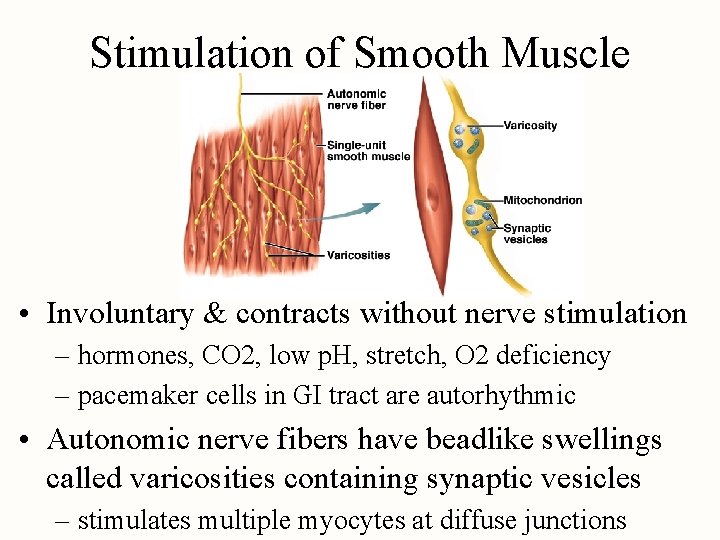
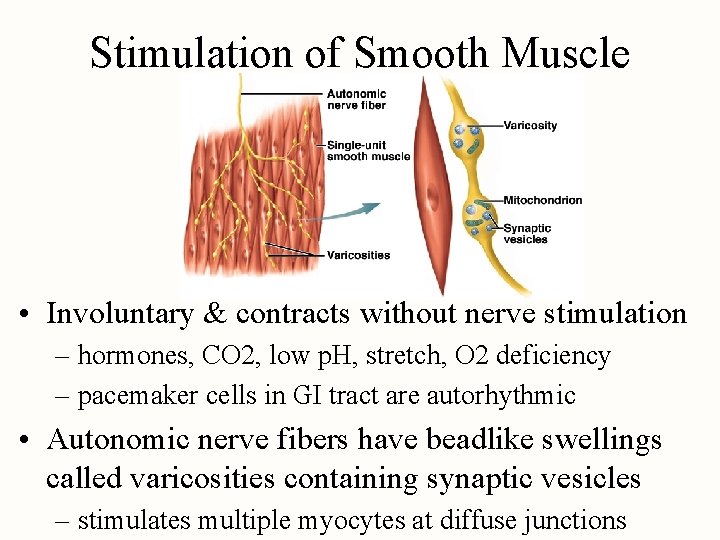
Stimulation of Smooth Muscle • Involuntary & contracts without nerve stimulation – hormones, CO 2, low p. H, stretch, O 2 deficiency – pacemaker cells in GI tract are autorhythmic • Autonomic nerve fibers have beadlike swellings called varicosities containing synaptic vesicles – stimulates multiple myocytes at diffuse junctions
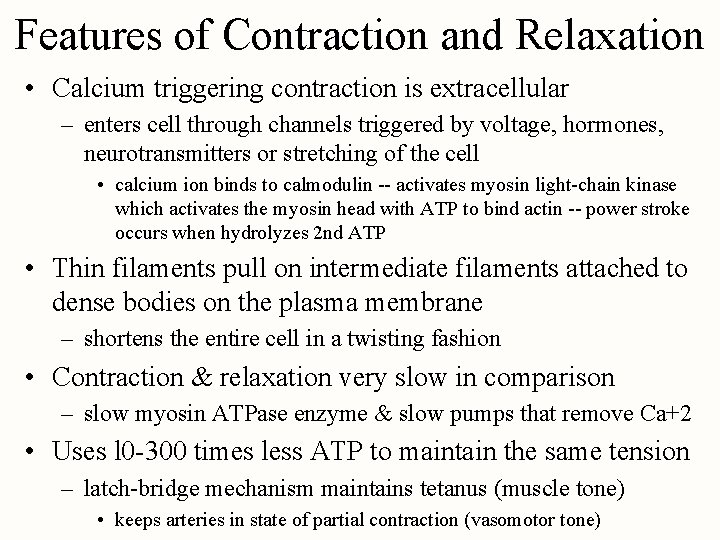
Features of Contraction and Relaxation • Calcium triggering contraction is extracellular – enters cell through channels triggered by voltage, hormones, neurotransmitters or stretching of the cell • calcium ion binds to calmodulin -- activates myosin light-chain kinase which activates the myosin head with ATP to bind actin -- power stroke occurs when hydrolyzes 2 nd ATP • Thin filaments pull on intermediate filaments attached to dense bodies on the plasma membrane – shortens the entire cell in a twisting fashion • Contraction & relaxation very slow in comparison – slow myosin ATPase enzyme & slow pumps that remove Ca+2 • Uses l 0 -300 times less ATP to maintain the same tension – latch-bridge mechanism maintains tetanus (muscle tone) • keeps arteries in state of partial contraction (vasomotor tone)
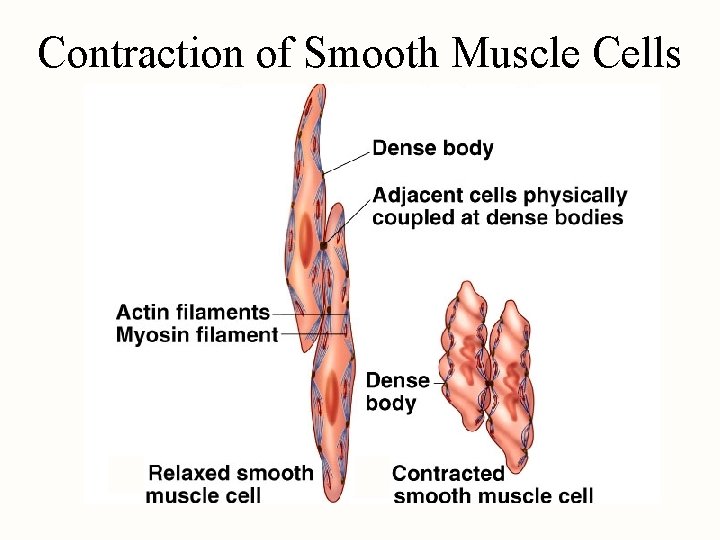
Contraction of Smooth Muscle Cells
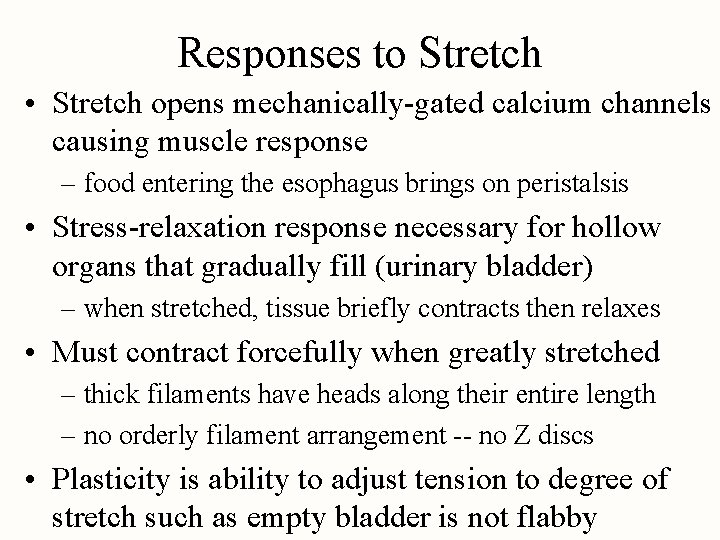
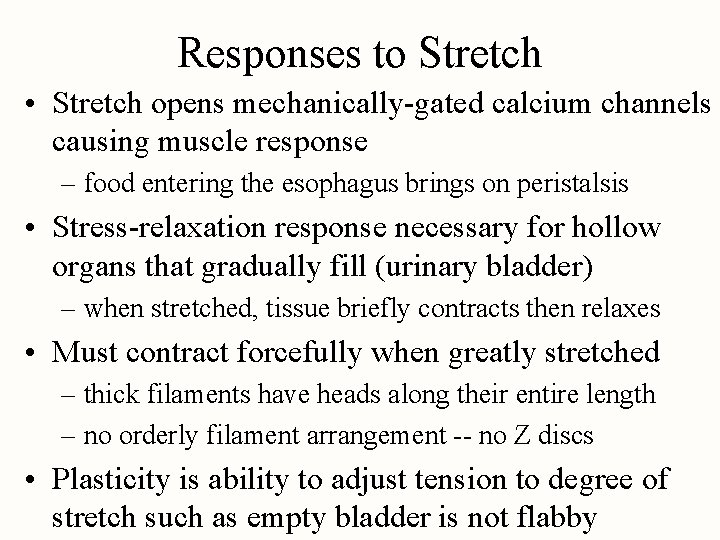
Responses to Stretch • Stretch opens mechanically-gated calcium channels causing muscle response – food entering the esophagus brings on peristalsis • Stress-relaxation response necessary for hollow organs that gradually fill (urinary bladder) – when stretched, tissue briefly contracts then relaxes • Must contract forcefully when greatly stretched – thick filaments have heads along their entire length – no orderly filament arrangement -- no Z discs • Plasticity is ability to adjust tension to degree of stretch such as empty bladder is not flabby
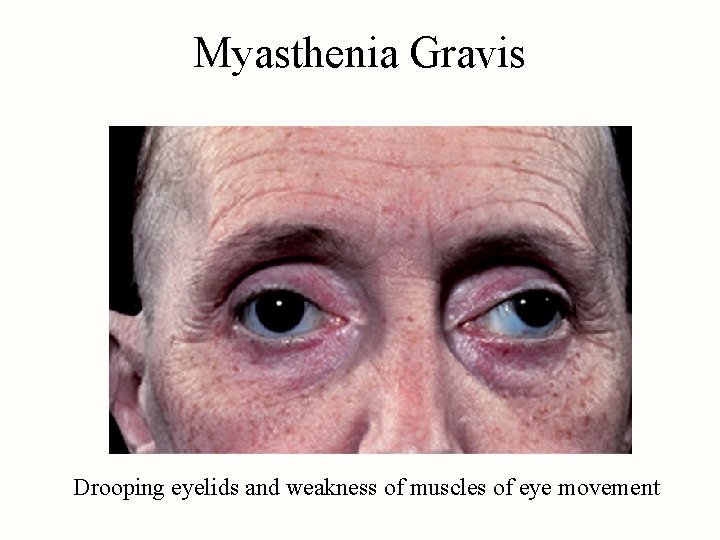
Myasthenia Gravis • Autoimmune disease where antibodies attack NMJ and bind ACh receptors together in clusters – fibers remove the receptors – less and less sensitive to ACh • • drooping eyelids and double vision difficulty swallowing weakness of the limbs respiratory failure • Disease of women between ages of 20 and 40 • Treated with cholinesterase inhibitors, thymus removal or immunosuppressive agents
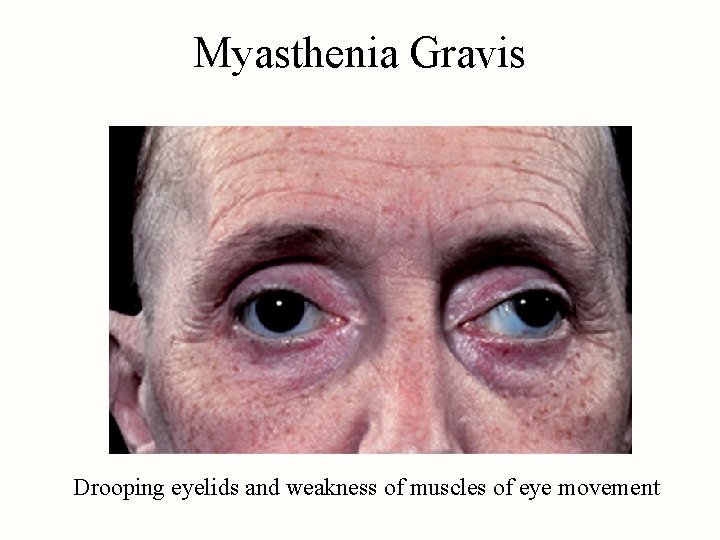
Myasthenia Gravis Drooping eyelids and weakness of muscles of eye movement