CHAPTER 11 CARDIOVASCULAR SYSTEM The Cardiovascular System A

- Slides: 45
CHAPTER 11: CARDIOVASCULAR SYSTEM
The Cardiovascular System � A closed system of the heart/blood �The heart pumps blood �Blood vessels allow blood to circulate throughout the body �At all times, blood is contained within the vessels or heart � Function: �Deliver oxygen and nutrients and re”move” carbon dioxide and other waste products
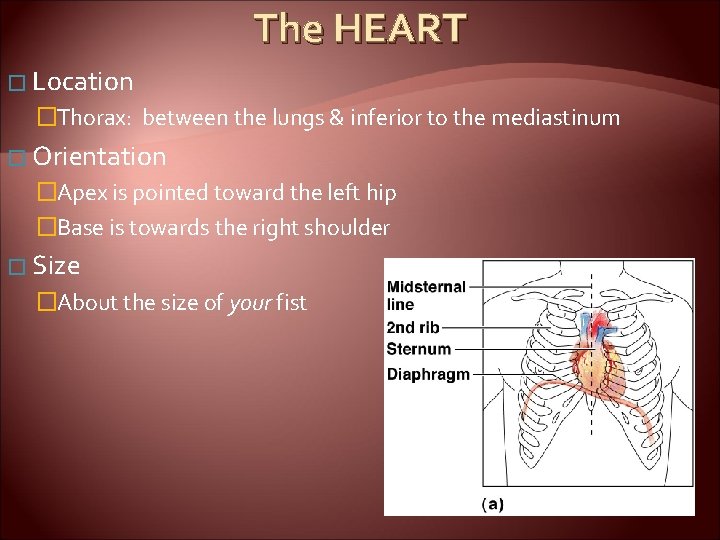
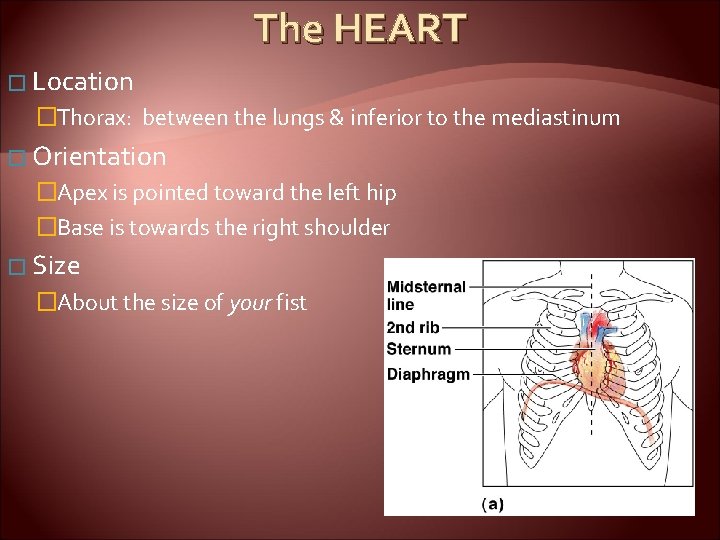
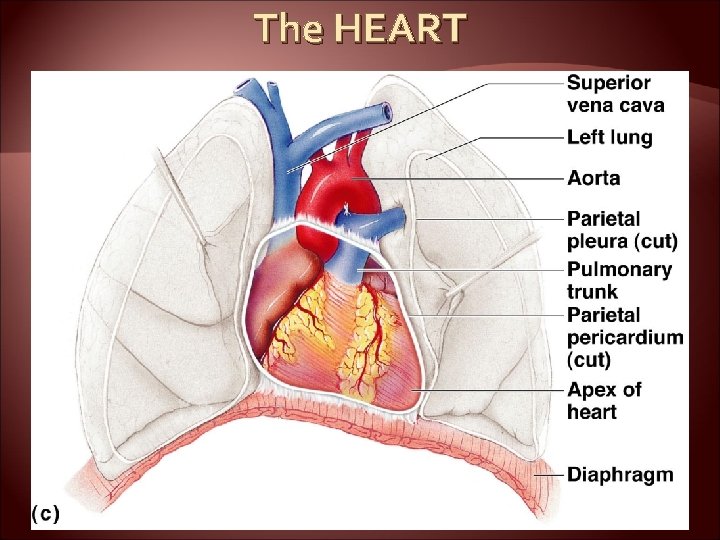
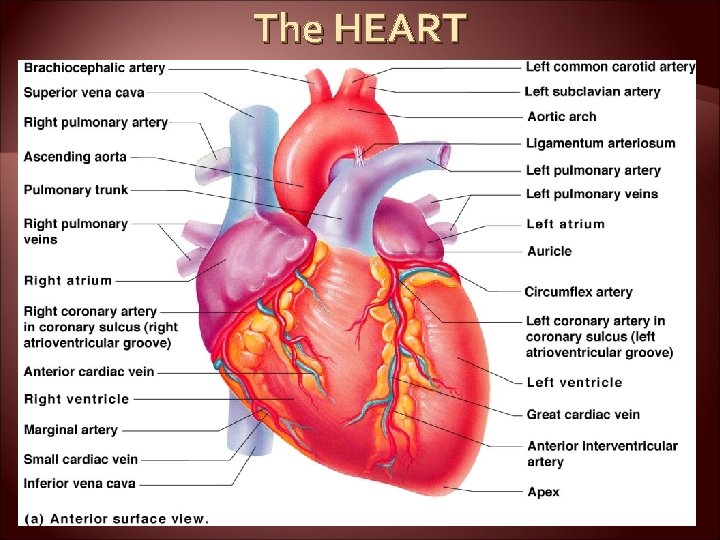
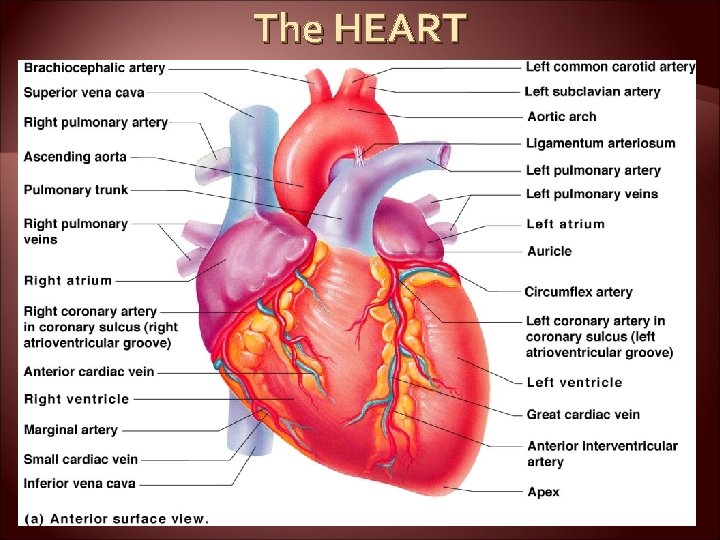
The HEART � Location �Thorax: between the lungs & inferior to the mediastinum � Orientation �Apex is pointed toward the left hip �Base is towards the right shoulder � Size �About the size of your fist
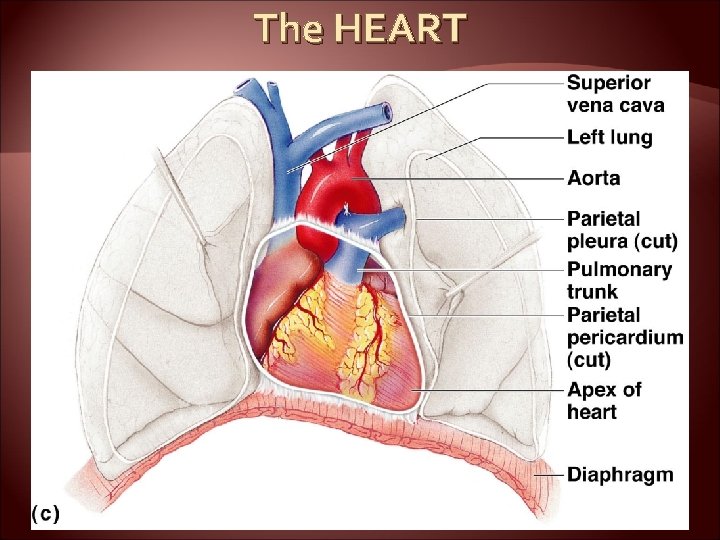
The HEART
The HEART
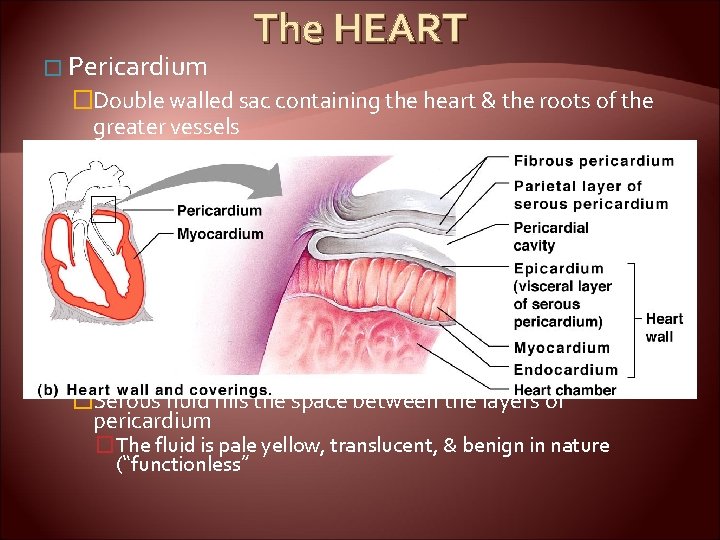
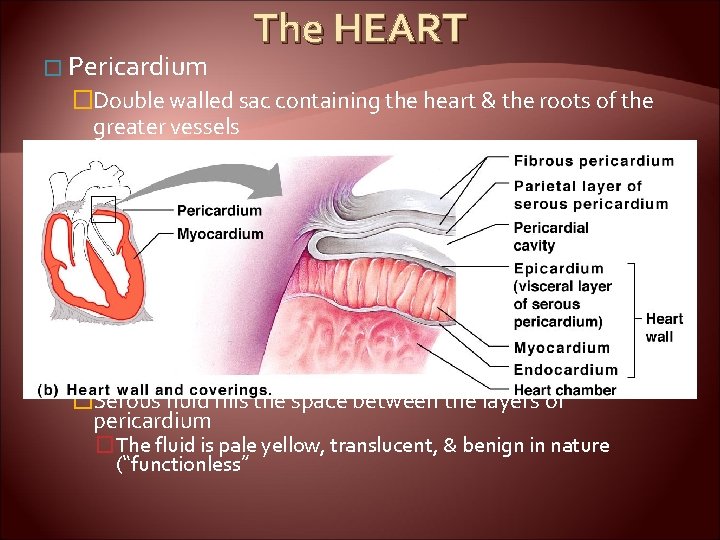
� Pericardium The HEART �Double walled sac containing the heart & the roots of the greater vessels �Two walls: fibrous pericardium & serous pericardium �Functions to protect the heart & lubricate the heart � Fibrous pericardium is loose and superficial �Serous membrane is deep to the fibrous pericardium and composed of two layers �Visceral pericardium �Next to heart; also known as the epicardium �Parietal pericardium �Outside layer that lines the inner surface of the fibrous pericardium �Serous fluid fills the space between the layers of pericardium �The fluid is pale yellow, translucent, & benign in nature (“functionless”
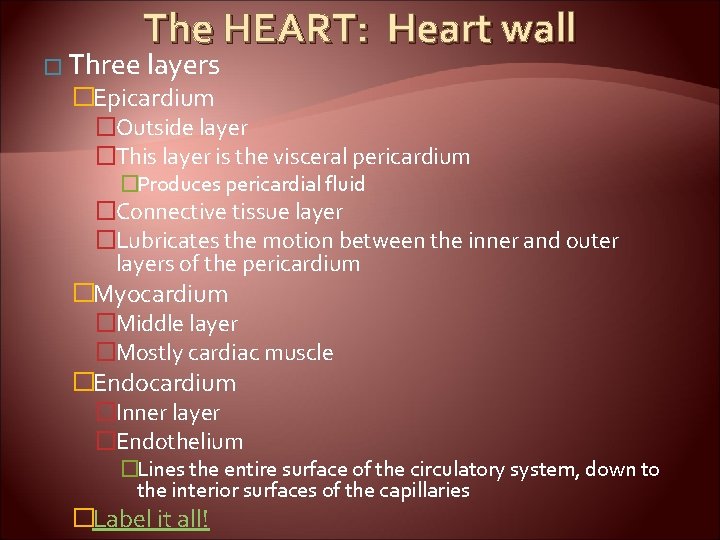
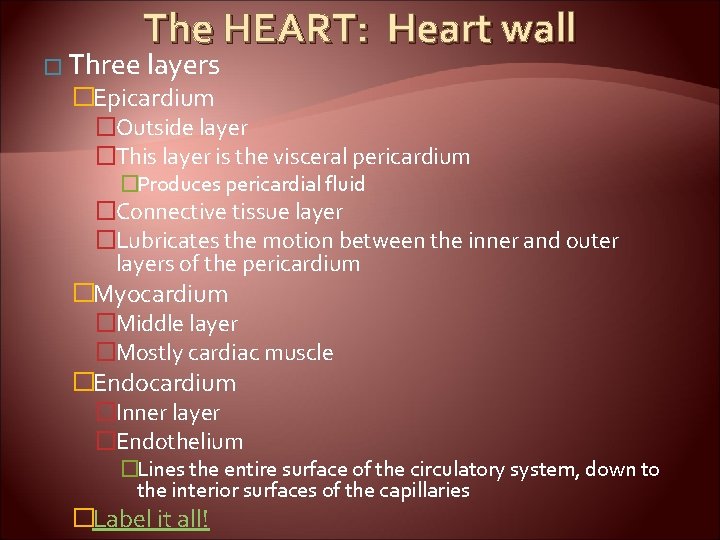
The HEART: Heart wall � Three layers �Epicardium �Outside layer �This layer is the visceral pericardium �Produces pericardial fluid �Connective tissue layer �Lubricates the motion between the inner and outer layers of the pericardium �Myocardium �Middle layer �Mostly cardiac muscle �Endocardium �Inner layer �Endothelium �Lines the entire surface of the circulatory system, down to the interior surfaces of the capillaries �Label it all!
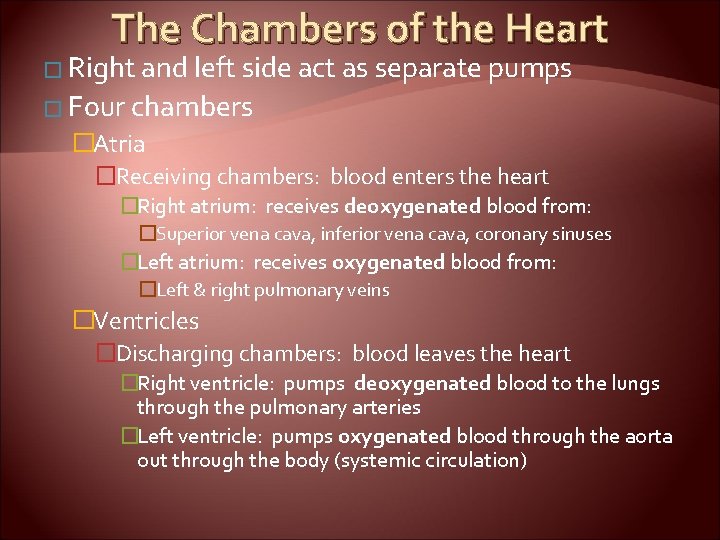
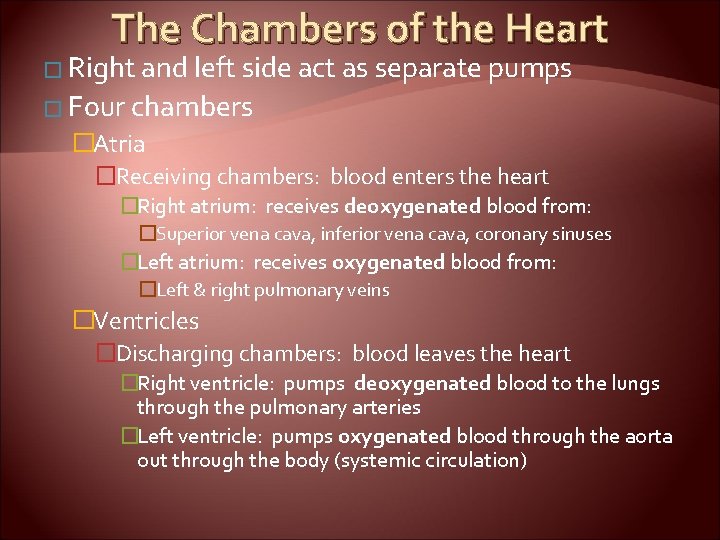
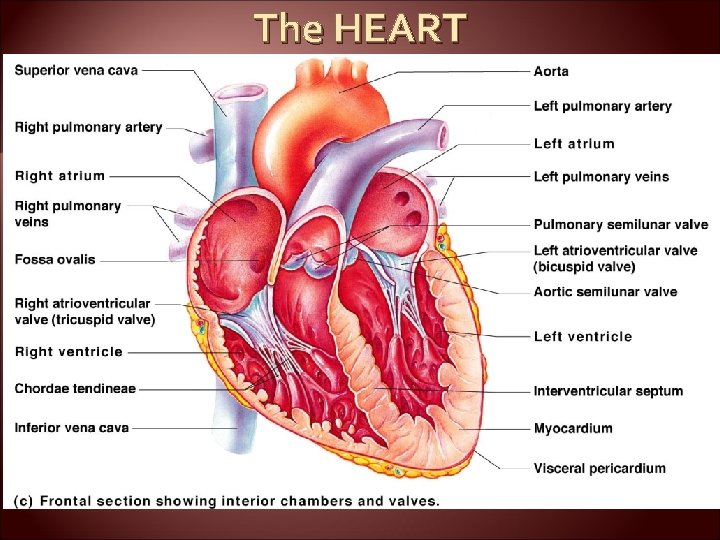
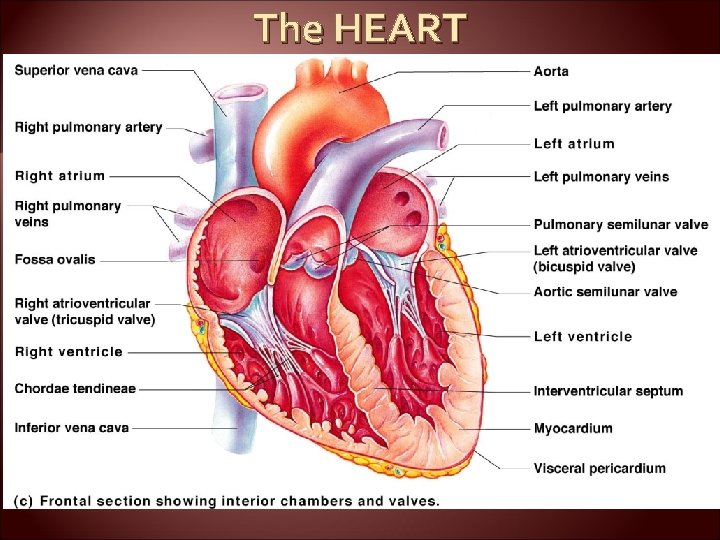
The Chambers of the Heart � Right and left side act as separate pumps � Four chambers �Atria �Receiving chambers: blood enters the heart �Right atrium: receives deoxygenated blood from: �Superior vena cava, inferior vena cava, coronary sinuses �Left atrium: receives oxygenated blood from: �Left & right pulmonary veins �Ventricles �Discharging chambers: blood leaves the heart �Right ventricle: pumps deoxygenated blood to the lungs through the pulmonary arteries �Left ventricle: pumps oxygenated blood through the aorta out through the body (systemic circulation)
The HEART

The Heart: Septa � Interventricular septum �Separates the two ventricles � Interatrial septum �Separates the two atria
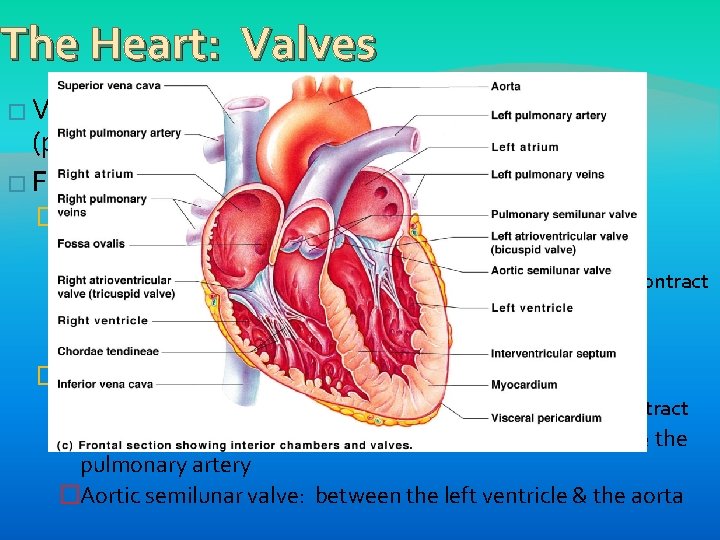
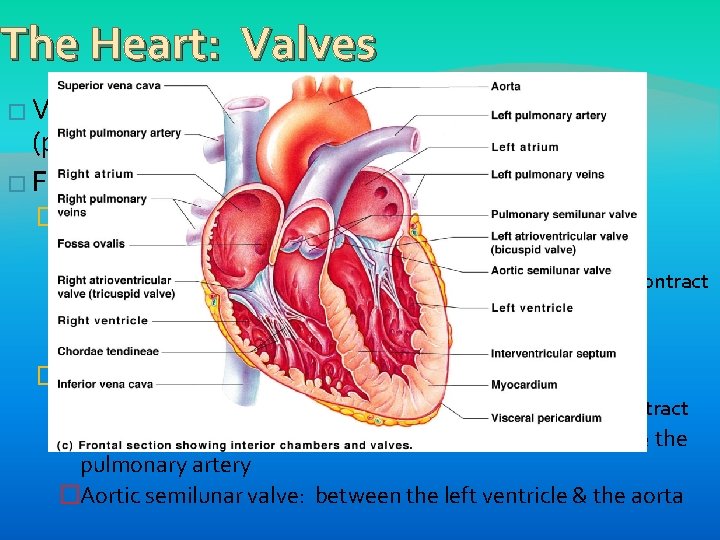
The Heart: Valves � Valves allow blood to only flow in (prevent backflow) � Four valves: one direction �Between the atria & ventricles: AV valves �Anchored in place by chordae tendinae: “heart strings” �Open during heart relaxation and closed during ventricular contract �Bicuspid (mitral): left side of the heart �Tricuspid: right side of the heart �Between ventricles & an artery: semilunar valves �Closed during heart relaxation & open during ventricular contract �Pulmonary semilunar valve: between the right ventricle & the pulmonary artery �Aortic semilunar valve: between the left ventricle & the aorta
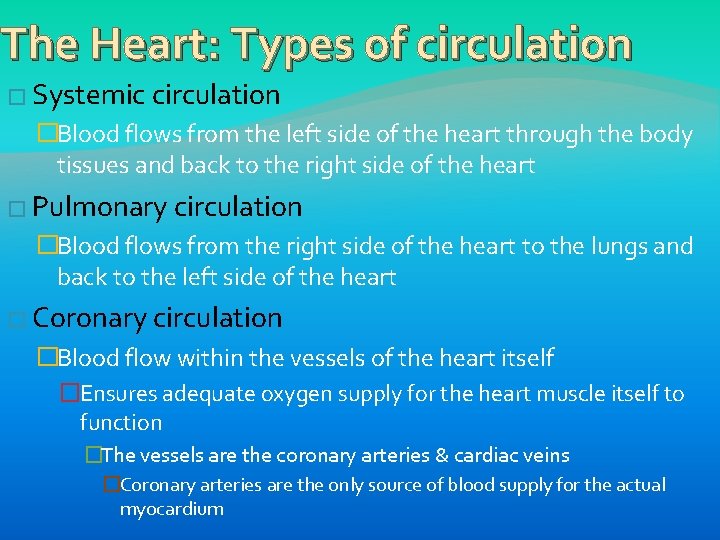
The Heart: Types of circulation � Systemic circulation �Blood flows from the left side of the heart through the body tissues and back to the right side of the heart � Pulmonary circulation �Blood flows from the right side of the heart to the lungs and back to the left side of the heart � Coronary circulation �Blood flow within the vessels of the heart itself �Ensures adequate oxygen supply for the heart muscle itself to function �The vessels are the coronary arteries & cardiac veins �Coronary arteries are the only source of blood supply for the actual myocardium
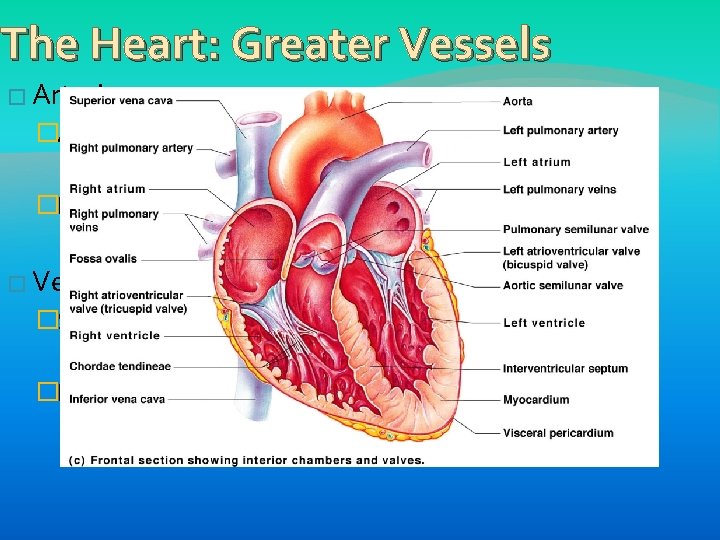
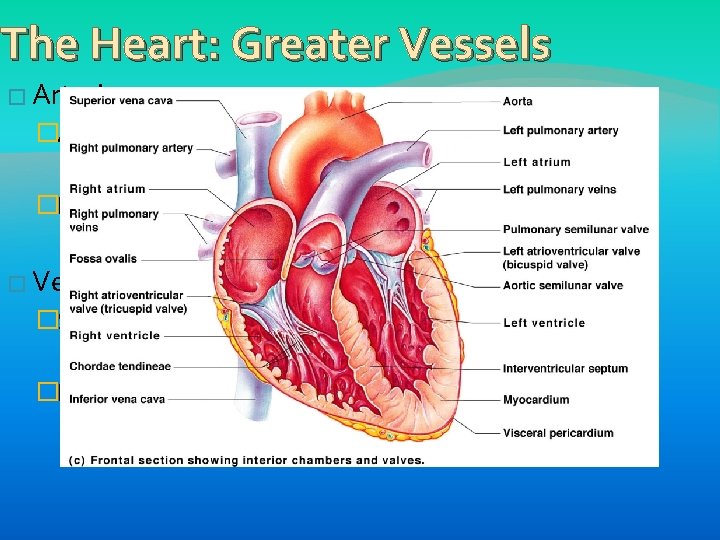
The Heart: Greater Vessels � Arteries: �Aorta: leaves the left ventricle �Brings oxygenated blood out to the body �Pulmonary artery: leaves the right ventricle �Brings deoxygenated blood to the lungs � Veins �Superior & inferior vena cava: enters the right atrium �Brings deoxygenated blood into the heart �Pulmonary veins (there are four): enters the left atrium �Brings oxygenated blood into the heart
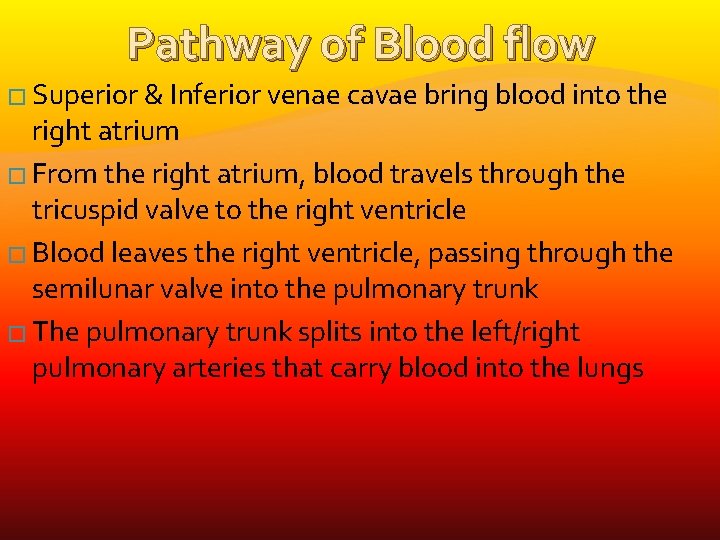
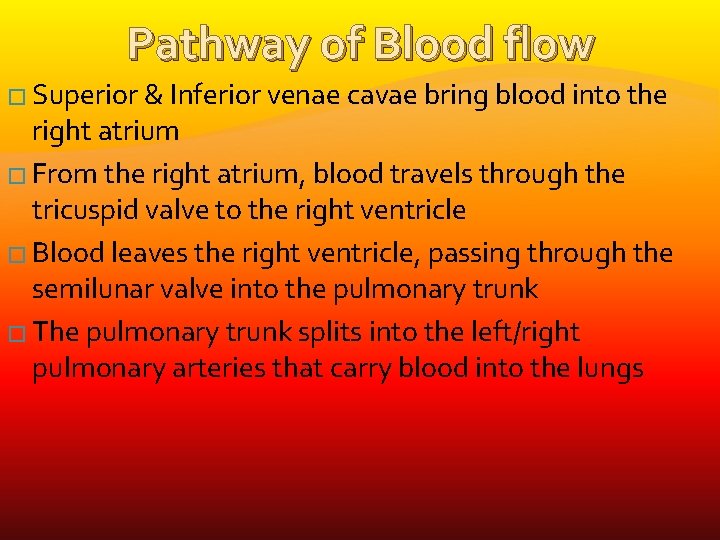
Pathway of Blood flow � Superior & Inferior venae cavae bring blood into the right atrium � From the right atrium, blood travels through the tricuspid valve to the right ventricle � Blood leaves the right ventricle, passing through the semilunar valve into the pulmonary trunk � The pulmonary trunk splits into the left/right pulmonary arteries that carry blood into the lungs
Pathway of Blood flow � Oxygen is picked up and carbon dioxide is dropped off � Oxygen rich blood travels back to the heart through the four pulmonary veins � Blood enters the left atrium, travels through the bicuspid valve into the left ventricle � From the left ventricle, blood leaves the heart via the aortic semilunar valve and ultimately the aorta – allowing the blood to travel through the body. � Simple, no?
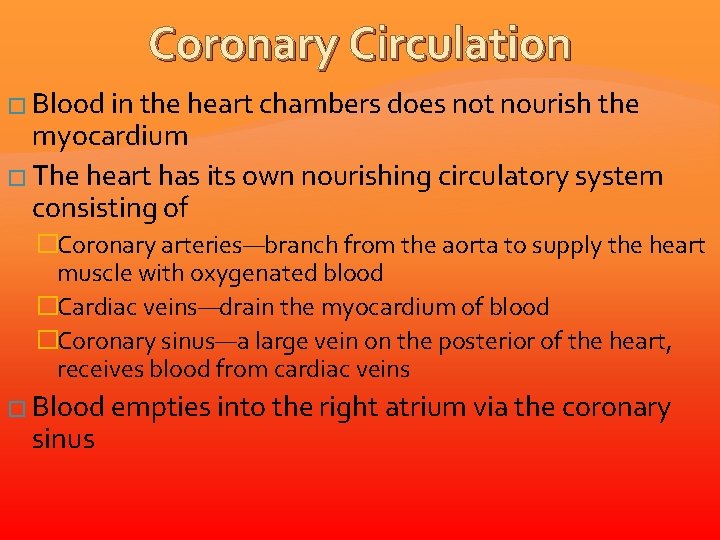
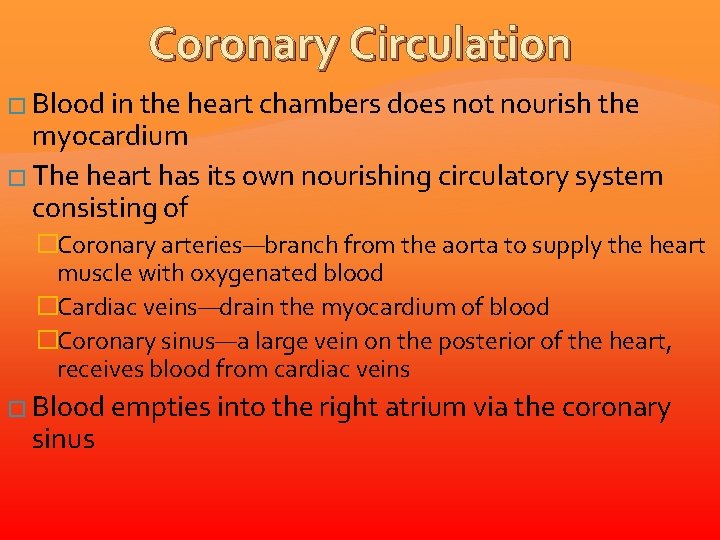
Coronary Circulation � Blood in the heart chambers does not nourish the myocardium � The heart has its own nourishing circulatory system consisting of �Coronary arteries—branch from the aorta to supply the heart muscle with oxygenated blood �Cardiac veins—drain the myocardium of blood �Coronary sinus—a large vein on the posterior of the heart, receives blood from cardiac veins � Blood empties into the right atrium via the coronary sinus
Electrical Conduction of the Heart
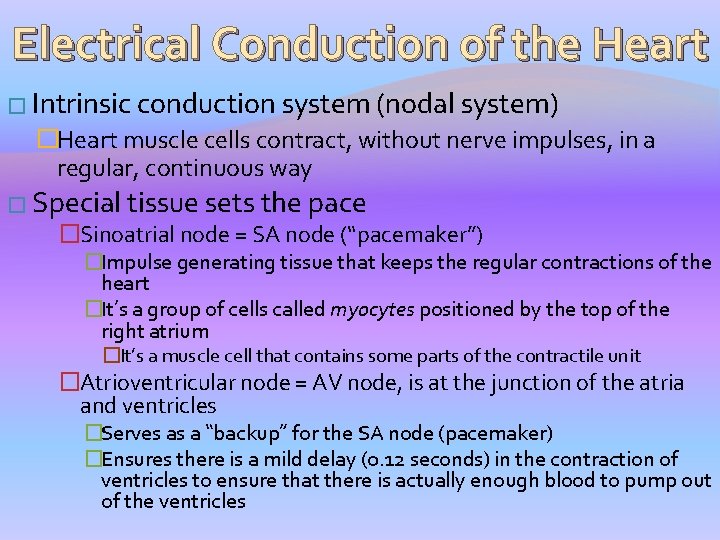
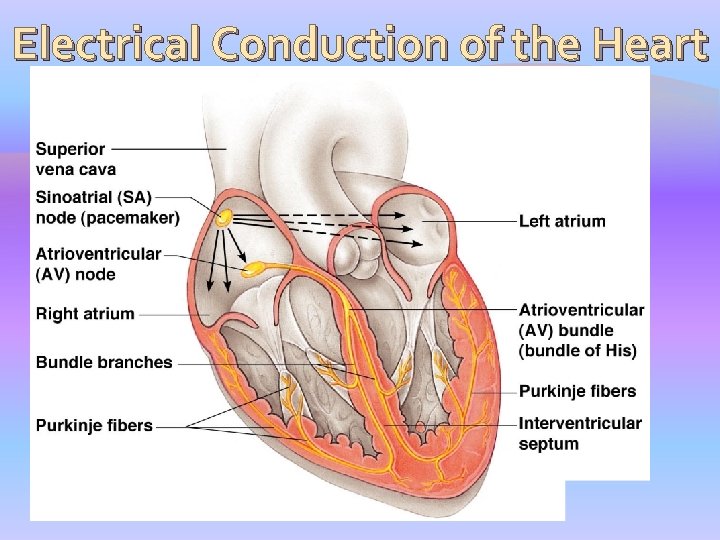
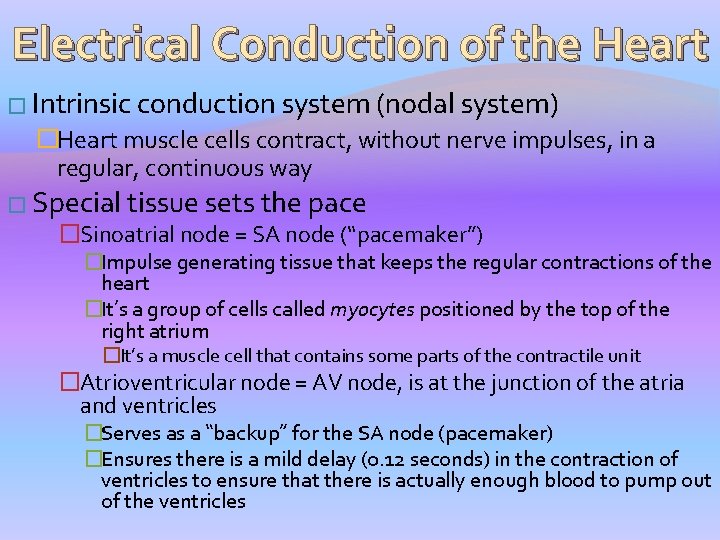
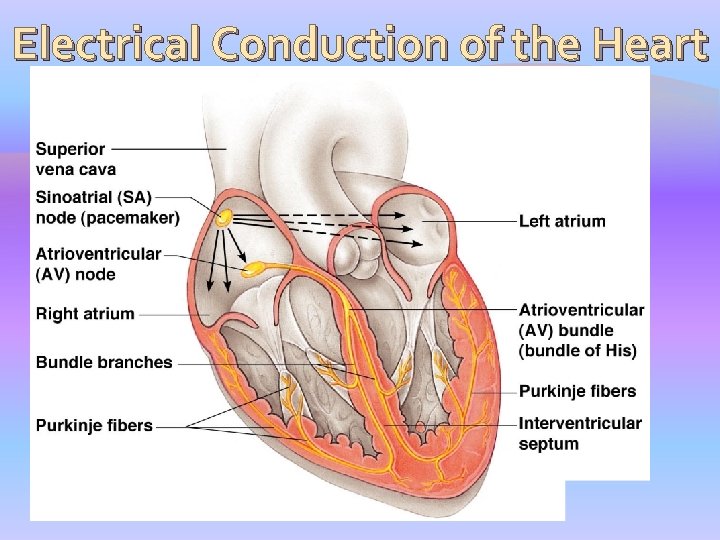
Electrical Conduction of the Heart � Intrinsic conduction system (nodal system) �Heart muscle cells contract, without nerve impulses, in a regular, continuous way � Special tissue sets the pace �Sinoatrial node = SA node (“pacemaker”) �Impulse generating tissue that keeps the regular contractions of the heart �It’s a group of cells called myocytes positioned by the top of the right atrium �It’s a muscle cell that contains some parts of the contractile unit �Atrioventricular node = AV node, is at the junction of the atria and ventricles �Serves as a “backup” for the SA node (pacemaker) �Ensures there is a mild delay (0. 12 seconds) in the contraction of ventricles to ensure that there is actually enough blood to pump out of the ventricles
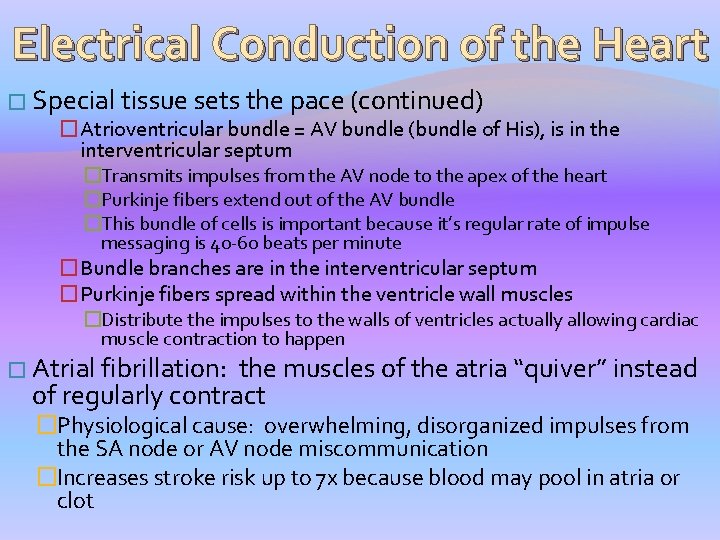
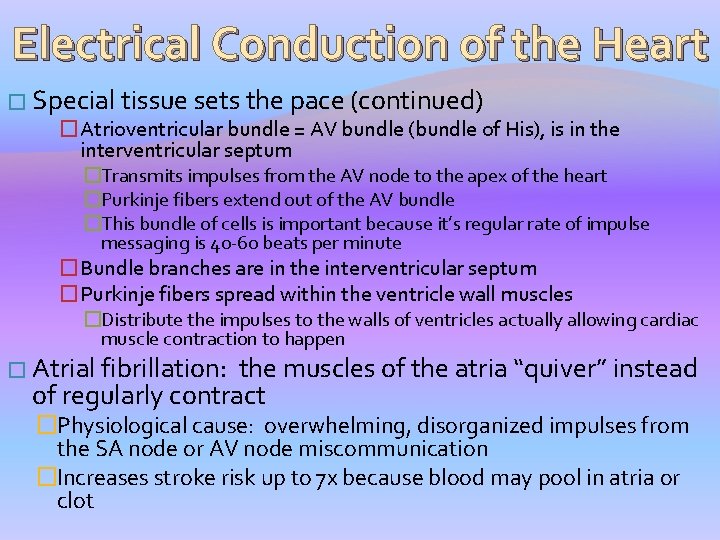
Electrical Conduction of the Heart � Special tissue sets the pace (continued) �Atrioventricular bundle = AV bundle (bundle of His), is in the interventricular septum �Transmits impulses from the AV node to the apex of the heart �Purkinje fibers extend out of the AV bundle �This bundle of cells is important because it’s regular rate of impulse messaging is 40 -60 beats per minute �Bundle branches are in the interventricular septum �Purkinje fibers spread within the ventricle wall muscles �Distribute the impulses to the walls of ventricles actually allowing cardiac muscle contraction to happen � Atrial fibrillation: the muscles of the atria “quiver” instead of regularly contract �Physiological cause: overwhelming, disorganized impulses from the SA node or AV node miscommunication �Increases stroke risk up to 7 x because blood may pool in atria or clot
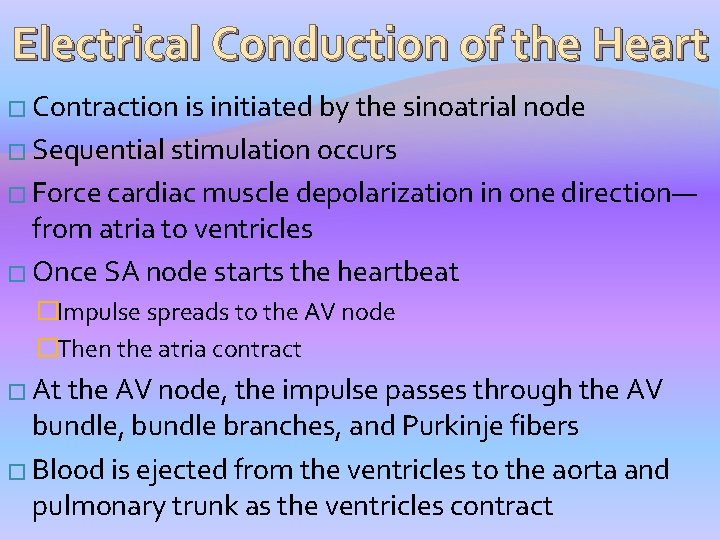
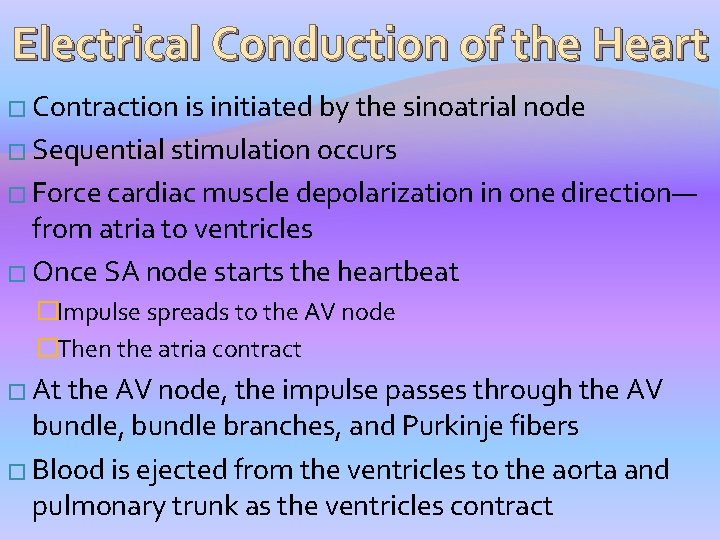
Electrical Conduction of the Heart � Contraction is initiated by the sinoatrial node � Sequential stimulation occurs � Force cardiac muscle depolarization in one direction— from atria to ventricles � Once SA node starts the heartbeat �Impulse spreads to the AV node �Then the atria contract � At the AV node, the impulse passes through the AV bundle, bundle branches, and Purkinje fibers � Blood is ejected from the ventricles to the aorta and pulmonary trunk as the ventricles contract
Heart Contraction �Tachycardia—rapid heart rate Tachycardia over 100 beats per minute �Bradycardia—slow heart rate less than 60 beats per minutes
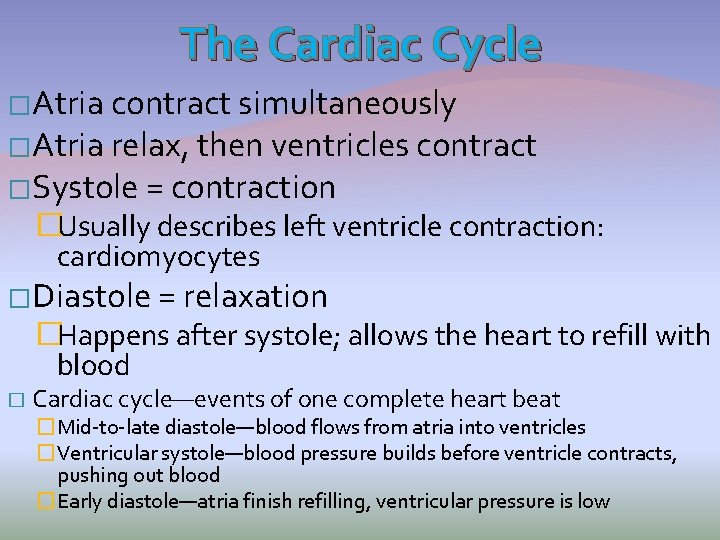
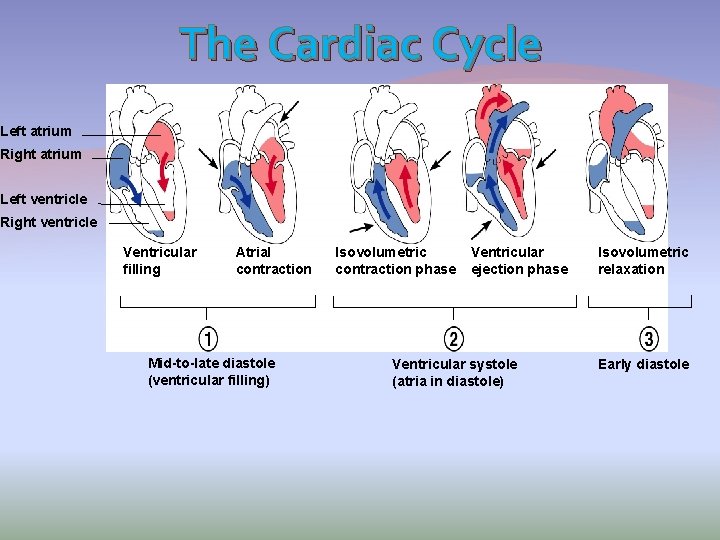
The Cardiac Cycle �Atria contract simultaneously �Atria relax, then ventricles contract �Systole = contraction �Usually describes left ventricle contraction: cardiomyocytes �Diastole = relaxation �Happens after systole; allows the heart to refill with blood � Cardiac cycle—events of one complete heart beat �Mid-to-late diastole—blood flows from atria into ventricles �Ventricular systole—blood pressure builds before ventricle contracts, pushing out blood �Early diastole—atria finish refilling, ventricular pressure is low
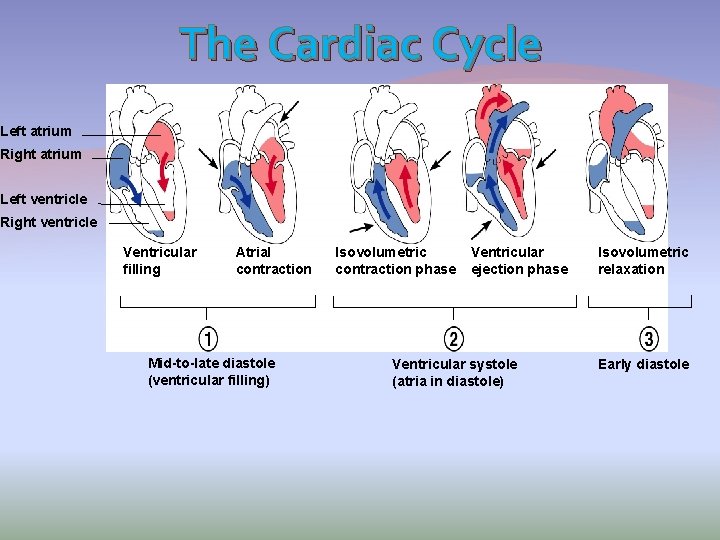
The Cardiac Cycle Left atrium Right atrium Left ventricle Right ventricle Ventricular filling Atrial contraction Mid-to-late diastole (ventricular filling) Isovolumetric contraction phase Ventricular ejection phase Ventricular systole (atria in diastole) Isovolumetric relaxation Early diastole
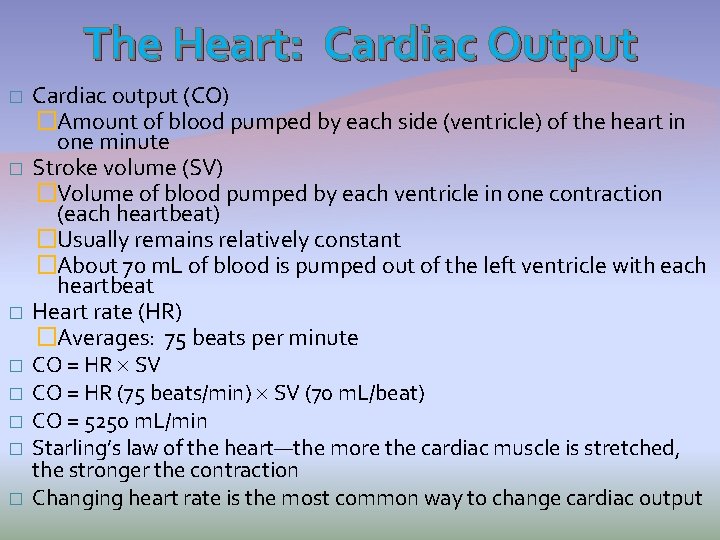
The Heart: Cardiac Output � � � � Cardiac output (CO) �Amount of blood pumped by each side (ventricle) of the heart in one minute Stroke volume (SV) �Volume of blood pumped by each ventricle in one contraction (each heartbeat) �Usually remains relatively constant �About 70 m. L of blood is pumped out of the left ventricle with each heartbeat Heart rate (HR) �Averages: 75 beats per minute CO = HR SV CO = HR (75 beats/min) SV (70 m. L/beat) CO = 5250 m. L/min Starling’s law of the heart—the more the cardiac muscle is stretched, the stronger the contraction Changing heart rate is the most common way to change cardiac output
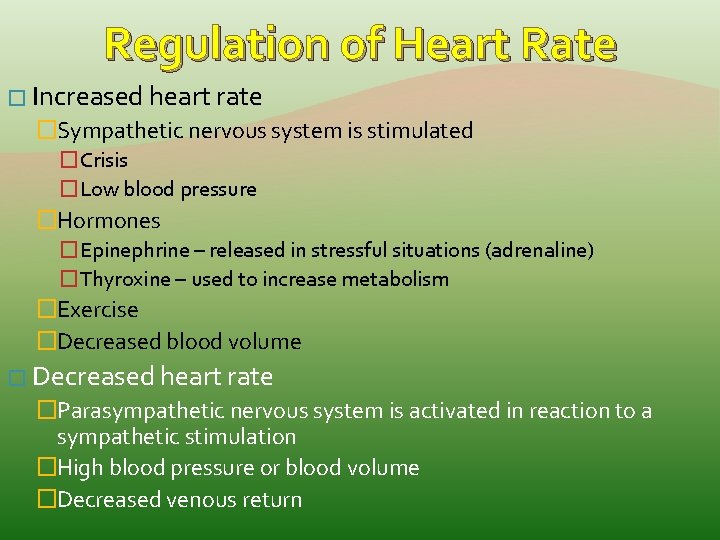
Regulation of Heart Rate � Increased heart rate �Sympathetic nervous system is stimulated �Crisis �Low blood pressure �Hormones �Epinephrine – released in stressful situations (adrenaline) �Thyroxine – used to increase metabolism �Exercise �Decreased blood volume � Decreased heart rate �Parasympathetic nervous system is activated in reaction to a sympathetic stimulation �High blood pressure or blood volume �Decreased venous return
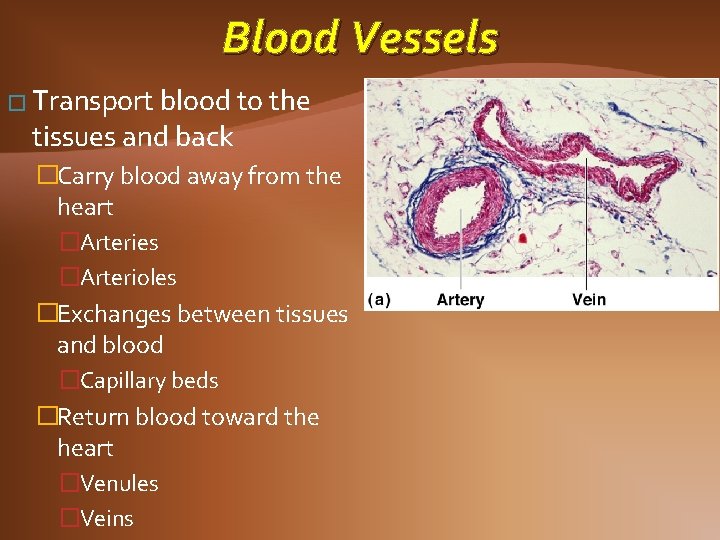
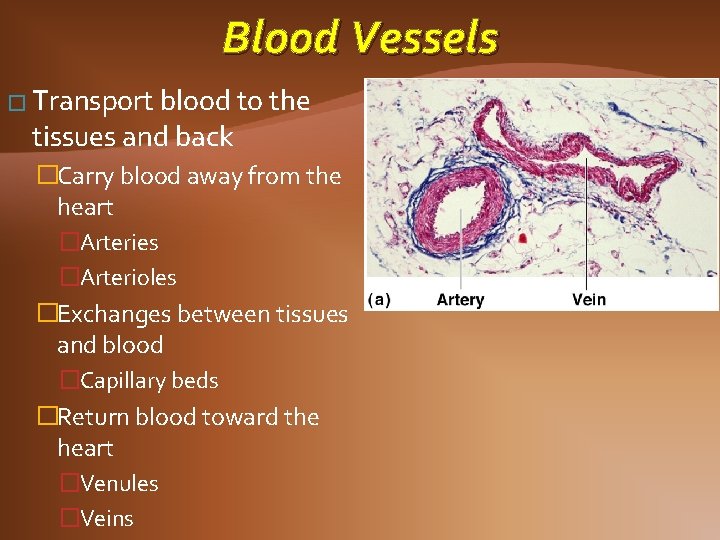
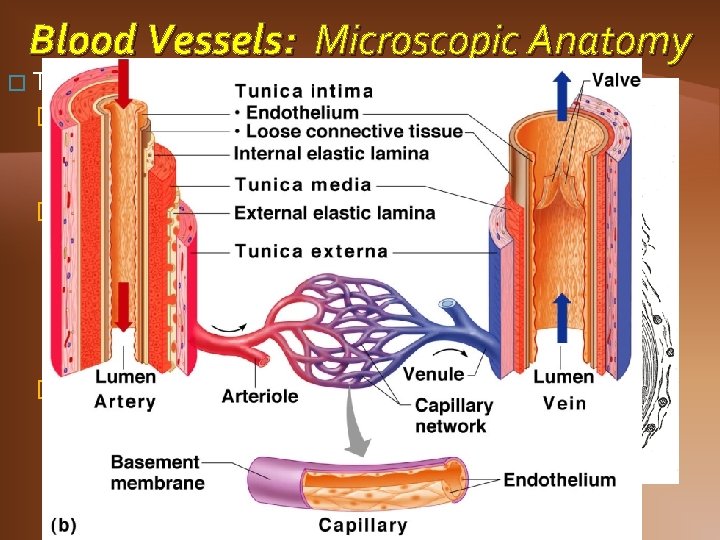
Blood Vessels � Transport blood to the tissues and back �Carry blood away from the heart �Arteries �Arterioles �Exchanges between tissues and blood �Capillary beds �Return blood toward the heart �Venules �Veins
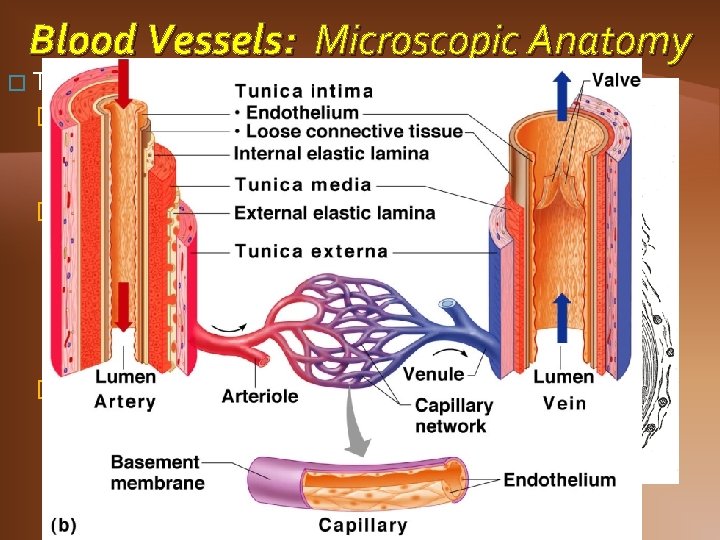
Blood Vessels: Microscopic Anatomy � Three layers (tunics) �Tunica intima �Endothelium – one layer of cells �Have direct contact with blood �Tunica media �Smooth muscle �In larger arteries, there may be elastic tissue �Controlled by sympathetic nervous system �Tunica externa �Mostly fibrous connective tissue (collagen) �Anchors blood vessels to body organs
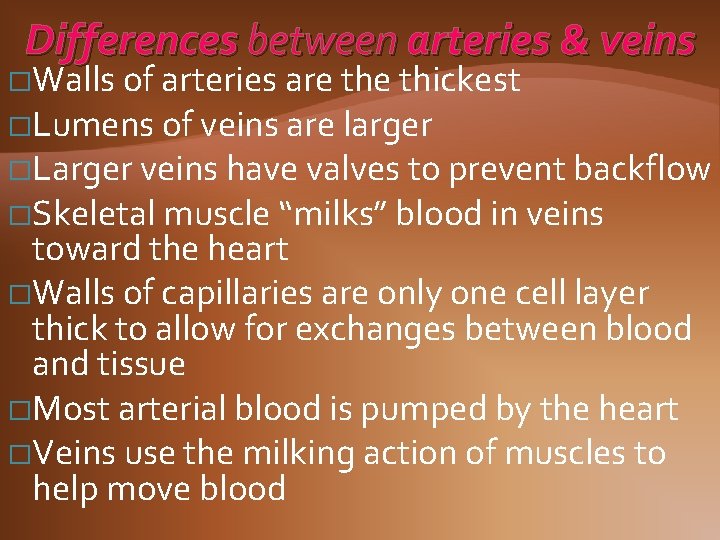
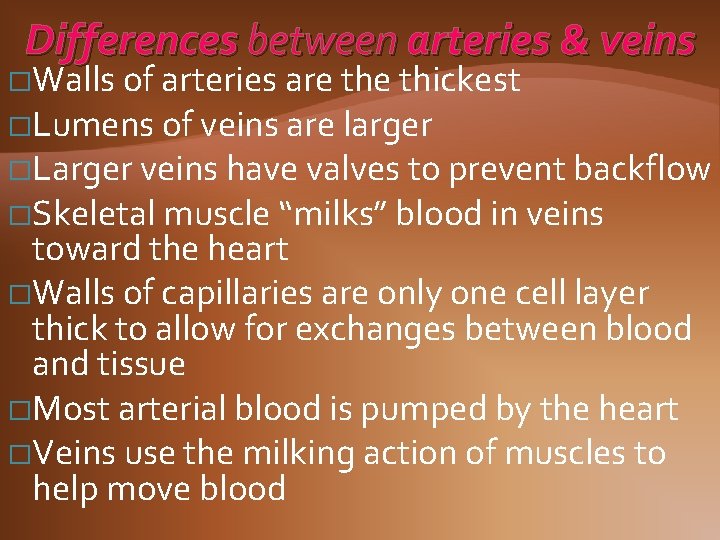
Differences between arteries & veins �Walls of arteries are thickest �Lumens of veins are larger �Larger veins have valves to prevent backflow �Skeletal muscle “milks” blood in veins toward the heart �Walls of capillaries are only one cell layer thick to allow for exchanges between blood and tissue �Most arterial blood is pumped by the heart �Veins use the milking action of muscles to help move blood
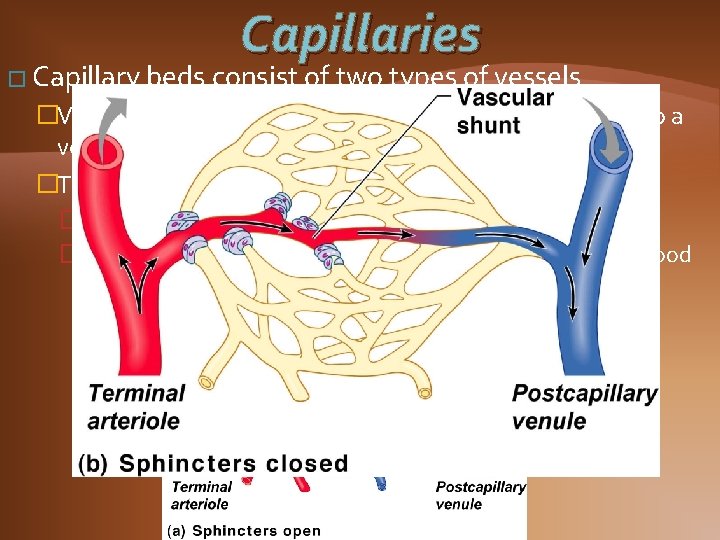
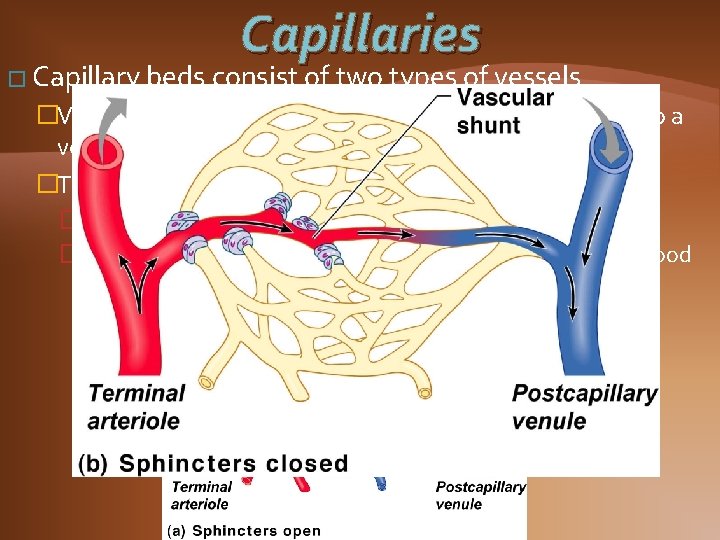
Capillaries � Capillary beds consist of two types of vessels �Vascular shunt—vessel directly connecting an arteriole to a venule �True capillaries—exchange vessels �Oxygen and nutrients cross to cells �Carbon dioxide and metabolic waste products cross into blood
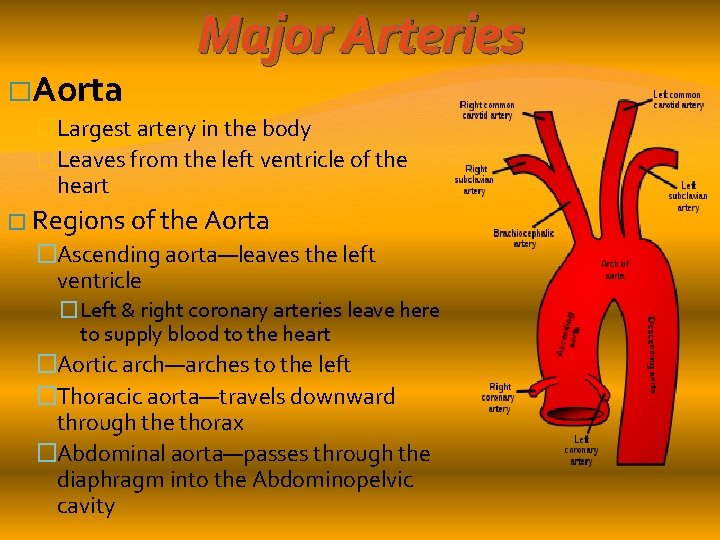
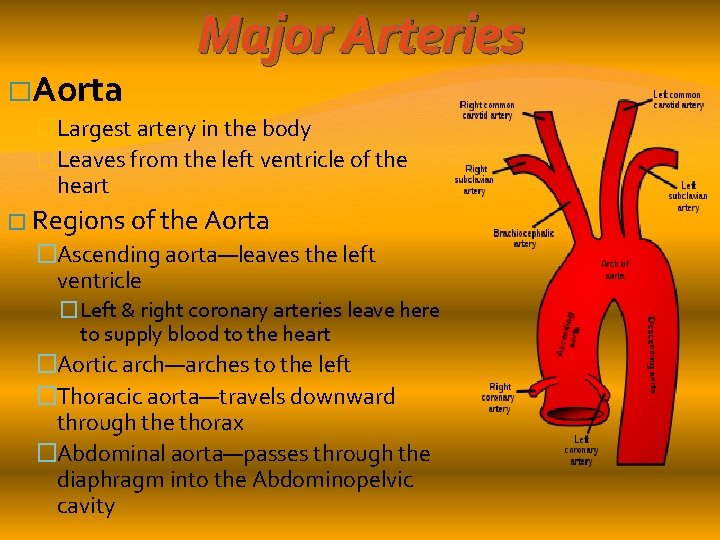
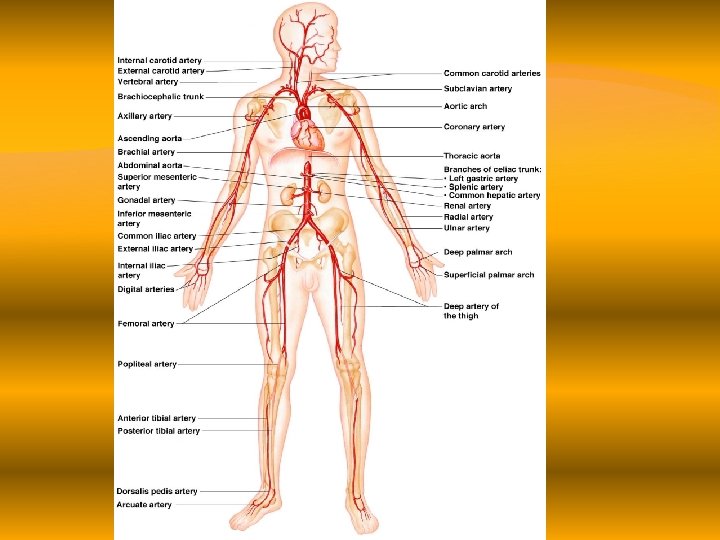
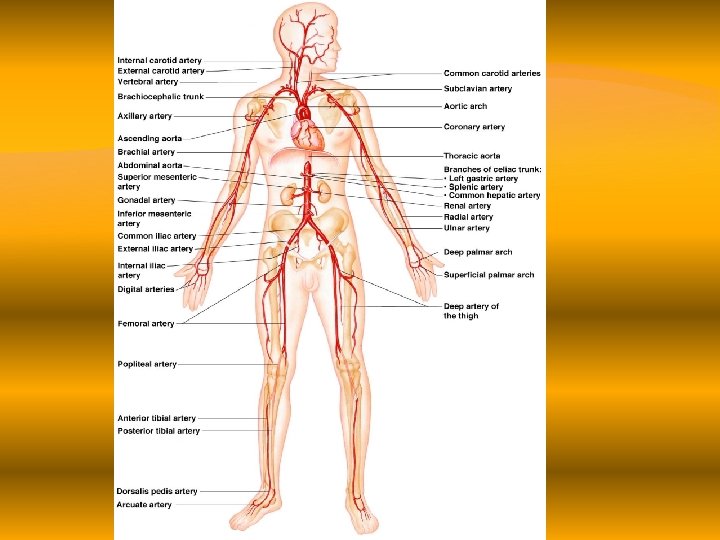
�Aorta Major Arteries �Largest artery in the body �Leaves from the left ventricle of the heart � Regions of the Aorta �Ascending aorta—leaves the left ventricle �Left & right coronary arteries leave here to supply blood to the heart �Aortic arch—arches to the left �Thoracic aorta—travels downward through the thorax �Abdominal aorta—passes through the diaphragm into the Abdominopelvic cavity
Major Arteries �Arterial branches of the aortic arch (BCS) �Brachiocephalic trunk splits into the �Right common carotid artery �Right subclavian artery �Left common carotid artery splits into the �Left internal and external carotid arteries �Left subclavian artery branches into the �Vertebral artery �In the axilla, the subclavian artery becomes the axillary artery brachial artery radial and ulnar arteries
Major Arteries �Arterial branches of the thoracic aorta �Intercostal arteries supply the muscles of the thorax wall �Other branches of the thoracic aorta supply the �Lungs (bronchial arteries) �Esophagus (esophageal arteries) �Diaphragm (phrenic arteries)
Major Arteries � Arterial branches of the abdominal aorta �Celiac trunk is the first branch of the abdominal aorta. Three branches are �Left gastric artery (stomach) �Splenic artery (spleen) �Common hepatic artery (liver) �Superior mesenteric artery supplies most of the small intestine and first half of the large intestine �Left and right renal arteries (kidney) �Left and right gonadal arteries �Ovarian arteries in females serve the ovaries �Testicular arteries in males serve the testes �Lumbar arteries serve muscles of the abdomen and trunk
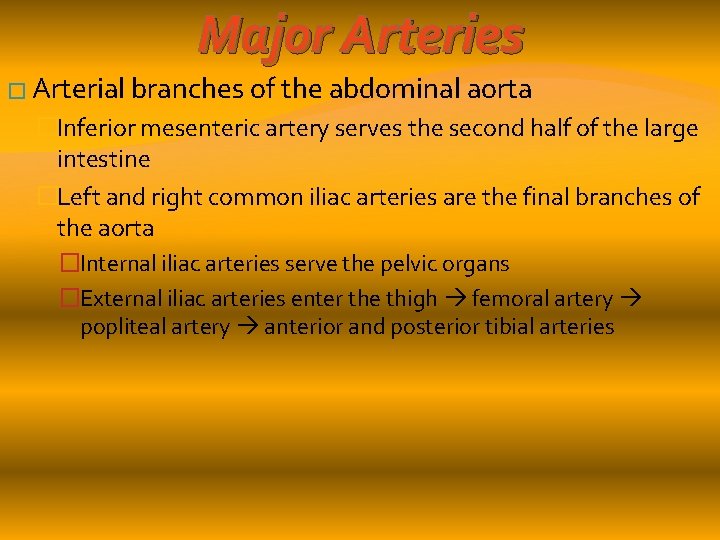
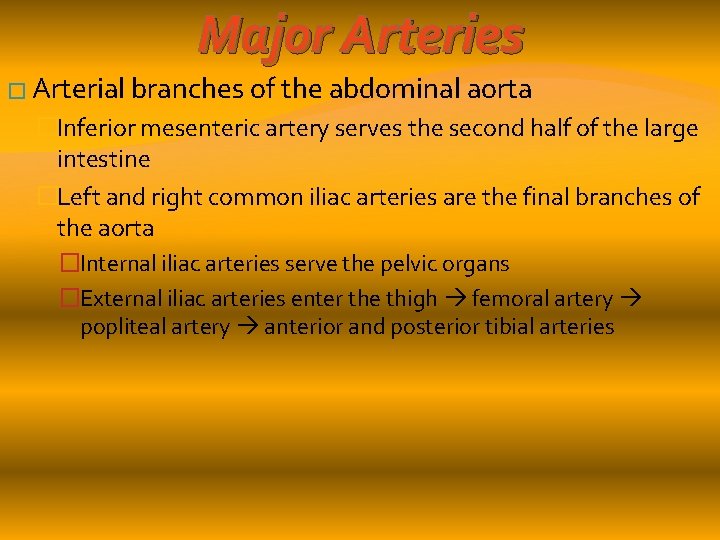
Major Arteries � Arterial branches of the abdominal aorta �Inferior mesenteric artery serves the second half of the large intestine �Left and right common iliac arteries are the final branches of the aorta �Internal iliac arteries serve the pelvic organs �External iliac arteries enter the thigh femoral artery popliteal artery anterior and posterior tibial arteries
Major Arteries
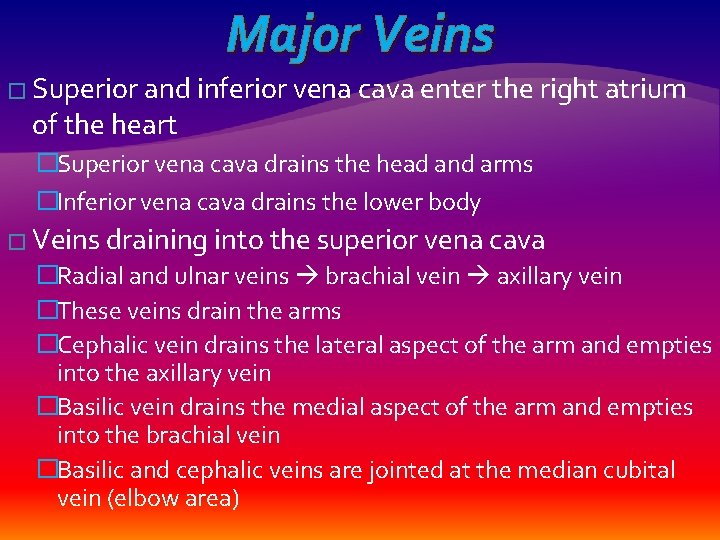
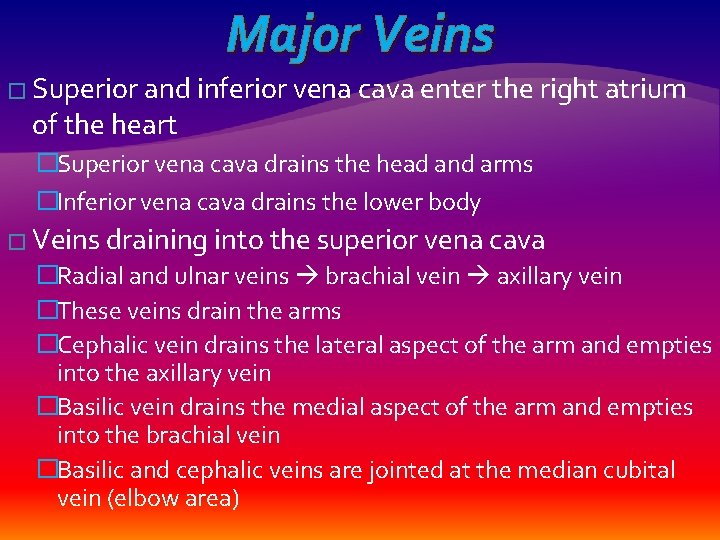
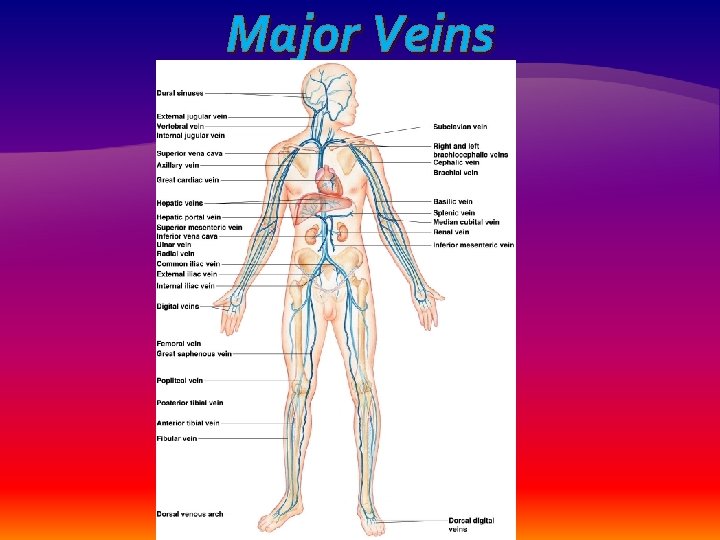
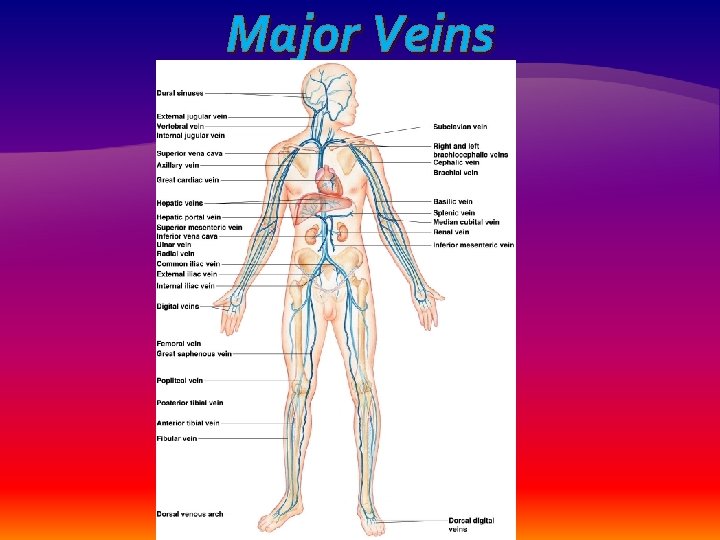
Major Veins � Superior and inferior vena cava enter the right atrium of the heart �Superior vena cava drains the head and arms �Inferior vena cava drains the lower body � Veins draining into the superior vena cava �Radial and ulnar veins brachial vein axillary vein �These veins drain the arms �Cephalic vein drains the lateral aspect of the arm and empties into the axillary vein �Basilic vein drains the medial aspect of the arm and empties into the brachial vein �Basilic and cephalic veins are jointed at the median cubital vein (elbow area)
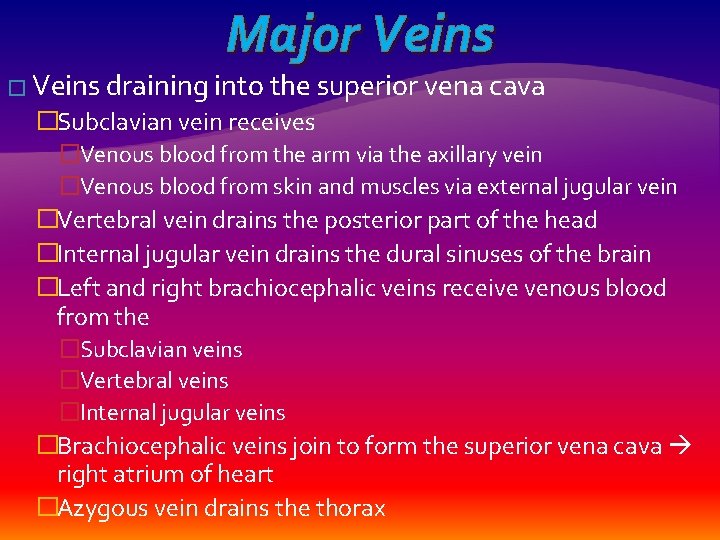
Major Veins � Veins draining into the superior vena cava �Subclavian vein receives �Venous blood from the arm via the axillary vein �Venous blood from skin and muscles via external jugular vein �Vertebral vein drains the posterior part of the head �Internal jugular vein drains the dural sinuses of the brain �Left and right brachiocephalic veins receive venous blood from the �Subclavian veins �Vertebral veins �Internal jugular veins �Brachiocephalic veins join to form the superior vena cava right atrium of heart �Azygous vein drains the thorax
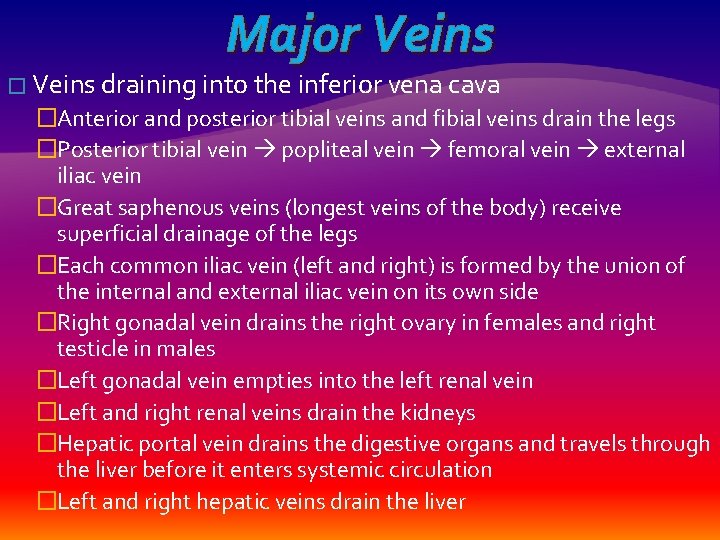
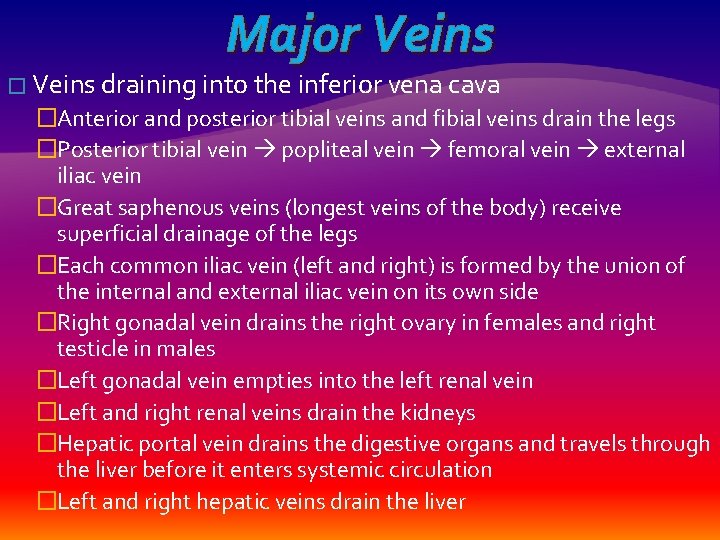
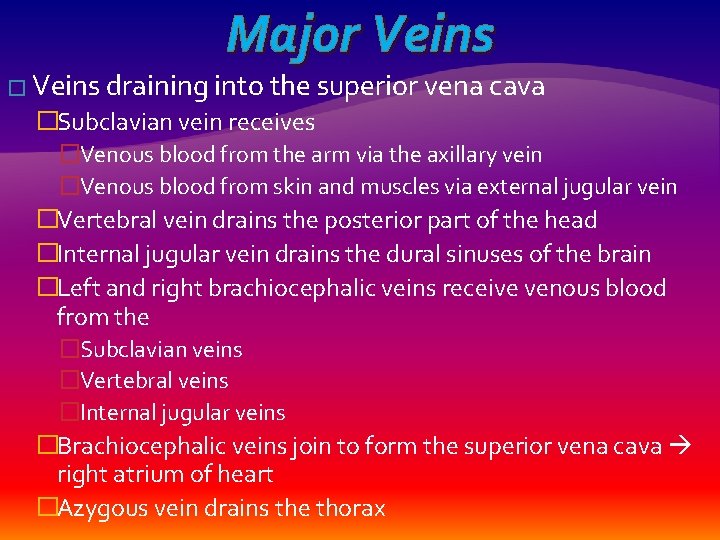
Major Veins � Veins draining into the inferior vena cava �Anterior and posterior tibial veins and fibial veins drain the legs �Posterior tibial vein popliteal vein femoral vein external iliac vein �Great saphenous veins (longest veins of the body) receive superficial drainage of the legs �Each common iliac vein (left and right) is formed by the union of the internal and external iliac vein on its own side �Right gonadal vein drains the right ovary in females and right testicle in males �Left gonadal vein empties into the left renal vein �Left and right renal veins drain the kidneys �Hepatic portal vein drains the digestive organs and travels through the liver before it enters systemic circulation �Left and right hepatic veins drain the liver
Major Veins
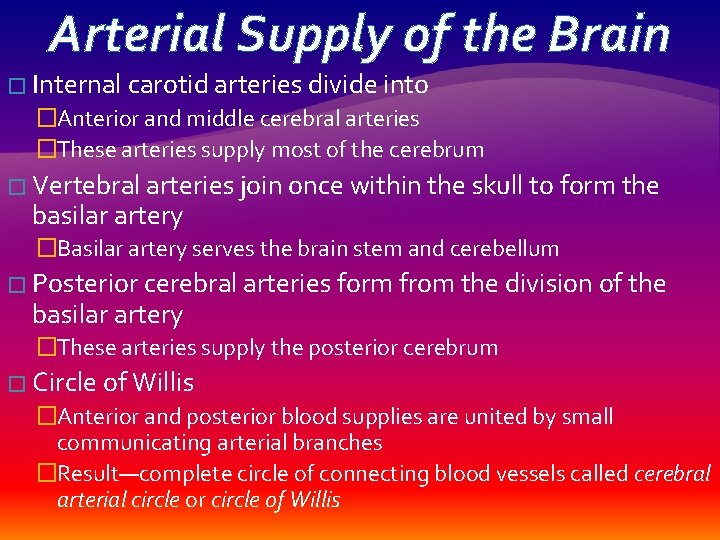
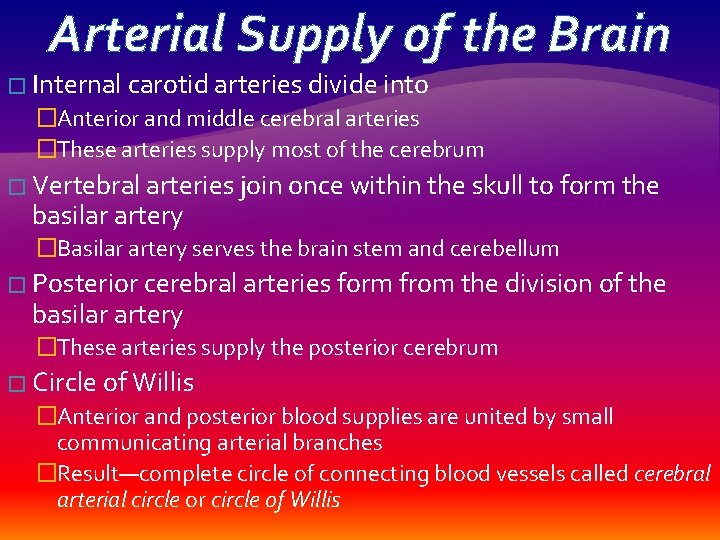
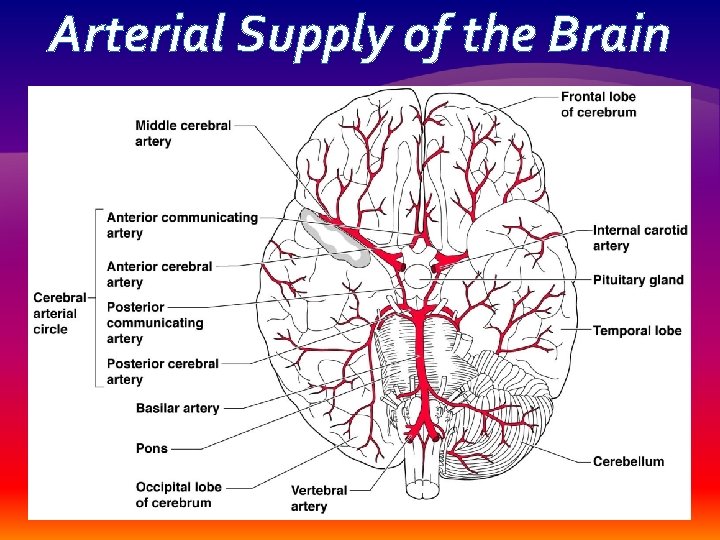
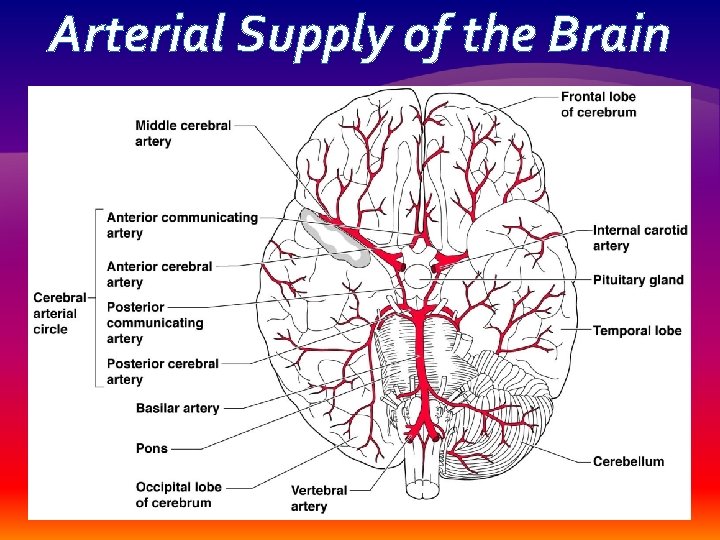
Arterial Supply of the Brain � Internal carotid arteries divide into �Anterior and middle cerebral arteries �These arteries supply most of the cerebrum � Vertebral arteries join once within the skull to form the basilar artery �Basilar artery serves the brain stem and cerebellum � Posterior cerebral arteries form from the division of the basilar artery �These arteries supply the posterior cerebrum � Circle of Willis �Anterior and posterior blood supplies are united by small communicating arterial branches �Result—complete circle of connecting blood vessels called cerebral arterial circle or circle of Willis
Arterial Supply of the Brain
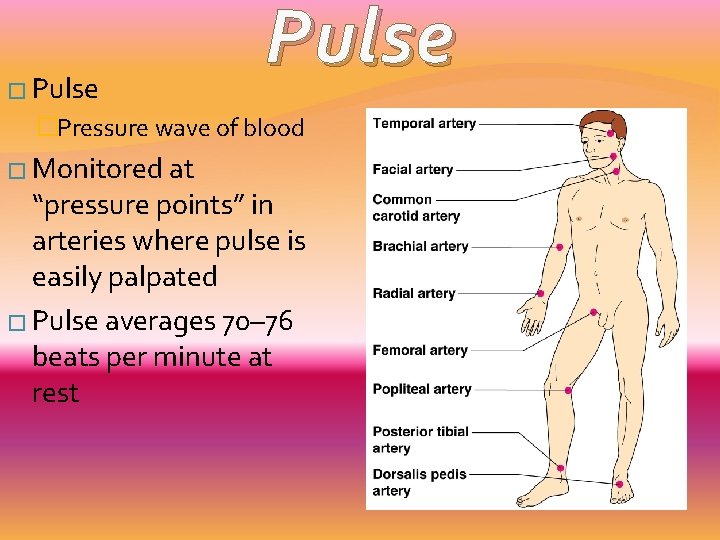
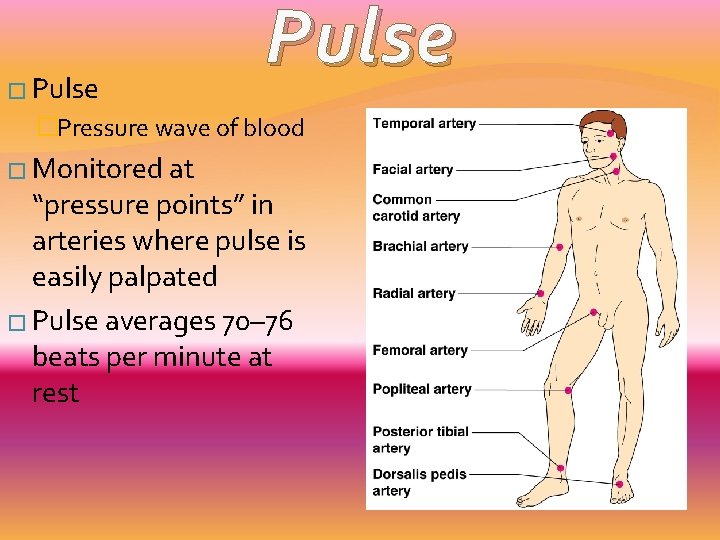
� Pulse �Pressure wave of blood � Monitored at “pressure points” in arteries where pulse is easily palpated � Pulse averages 70– 76 beats per minute at rest
Variations in Blood Pressure � Normal human range is variable �Normal � 140– 110 mm Hg systolic � 80– 75 mm Hg diastolic �Hypotension �Low systolic (below 110 mm HG) �Often associated with illness �Hypertension �High systolic (above 140 mm HG) �Can be dangerous if it is chronic
Factors that affect blood pressure � BP is blood pressure �BP is affected by age, weight, time of day, exercise, body position, emotional state � CO is the amount of blood pumped out of the left ventricle per minute � PR is peripheral resistance, or the amount of friction blood encounters as it flows through vessels �Narrowing of blood vessels and increased blood volume increases PR � BP = CO PR
Factors that affect blood pressure � Neural factors �Autonomic nervous system adjustments (sympathetic division) � Renal factors �Regulation by altering blood volume �Renin—hormonal control � Temperature �Heat has a vasodilating effect �Cold has a vasoconstricting effect � Chemicals �Various substances can cause increases or decreases � Diet