Chapter 10 Rapid Response Teams and Code Management
- Slides: 82
Chapter 10 Rapid Response Teams and Code Management Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc.
Cardiopulmonary Arrest Most codes filled with panic and pandemonium Best options Prevent Ø Plan Ø Practice Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 2
Rapid Response Teams “Failure to rescue” is important concept to address RRT established to address concerns Call BEFORE the cardiac/respiratory arrest Recommended by The Joint Commission and Institute for Healthcare Improvement to implement systems to request assistance for worsening conditions Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 3
RRTs (continued) Call any time a staff member is concerned about changes in a patient’s condition including: Heart rate, systolic blood pressure Ø Respiratory rate, oxygen saturation Ø Mental status Ø Urinary output Ø Laboratory values Ø Some institutions empower family members to activate the RRT Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 4
RRT Effectiveness RRT reduces: Cardiac arrests Ø Critical care unit length of stay Ø Incidence of acute illness, such as respiratory failure, stroke, severe sepsis, and acute kidney injury Ø Recent review of literature and meta-analysis of 1. 3 million patients Ø RRT was not associated with lower hospital mortality rates in hospitalized adults Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 5
Codes Code, code blue, code 99, Dr. Heart Cardiac and/or respiratory arrest Lifesaving resuscitation and intervention needed BLS/AED Ø ACLS Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 6
Code Team Notification system Members vary within setting Better patient management Care according to ACLS protocols Other healthcare workers manage other patients Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 7
Team Members Leader usually MD skilled in ACLS Nurses (usually ICU or ER) Primary nurse knows patient Ø Second nurse gives medications and gets equipment from crash cart Ø Another nurse records events Ø Nursing supervisor provides traffic control and secures ICU bed (if needed) Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 8
Team Members (continued) Anesthesiologist/anesthetist intubation Respiratory therapist manages airway, sometimes intubates Pharmacist prepares medications in some settings Chaplain ECG technician Other personnel to run errands Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 9
Critical Thinking Challenge Who has observed resuscitation efforts? What observations were made? What perceptions of care were noted? Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 10
Equipment Crash cart Backboard Monitor/defibrillator/p acemaker AED Ø Transcutaneous pacemaker Ø Bag-valve-mask device Airway supplies/suction Medications IV supplies Nasogastric tube BP cuff Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 11
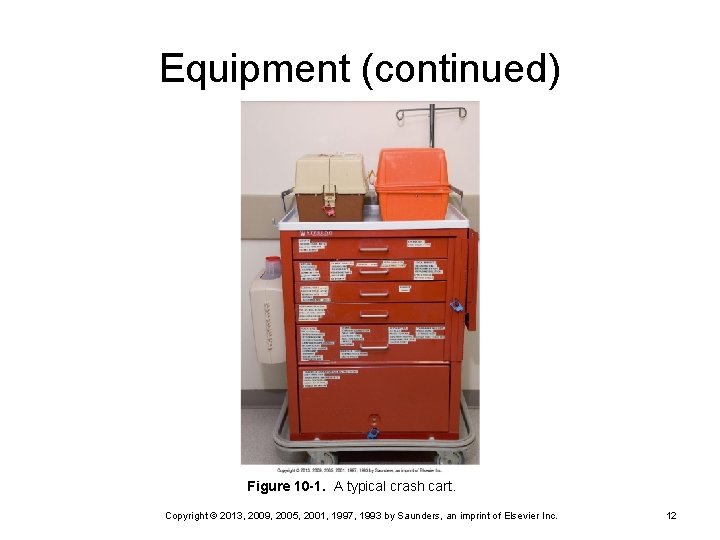
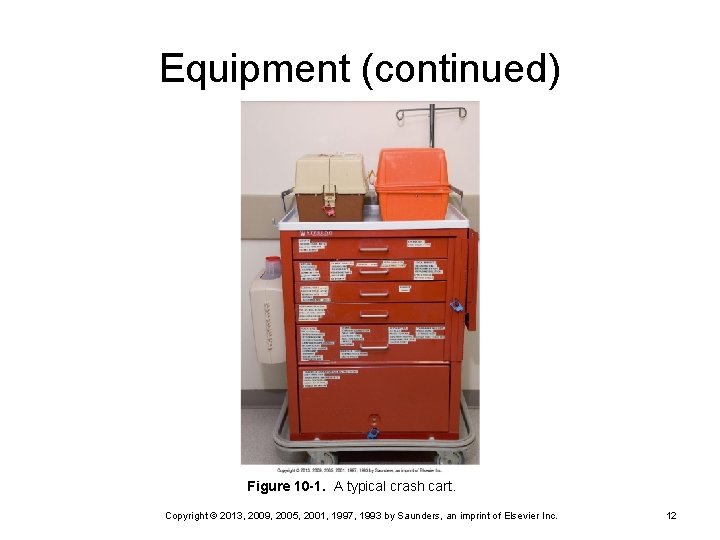
Equipment (continued) Figure 10 -1. A typical crash cart. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 12
Things to Know Your cart Where it is located? Ø How do you unlock it? Ø How do you check it per unit protocol? Ø Your equipment O 2 and suction Ø Is child-sized equipment available if needed (e. g. , ED)? Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 13
Sequence of Events: BLS Advance directives or living wills Airway open Breathing Mouth to mask Ø Bag-valve-mask device Ø Circulation: chest compressions Ø May do open chest compression in trauma patients or after cardiac surgery Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 14
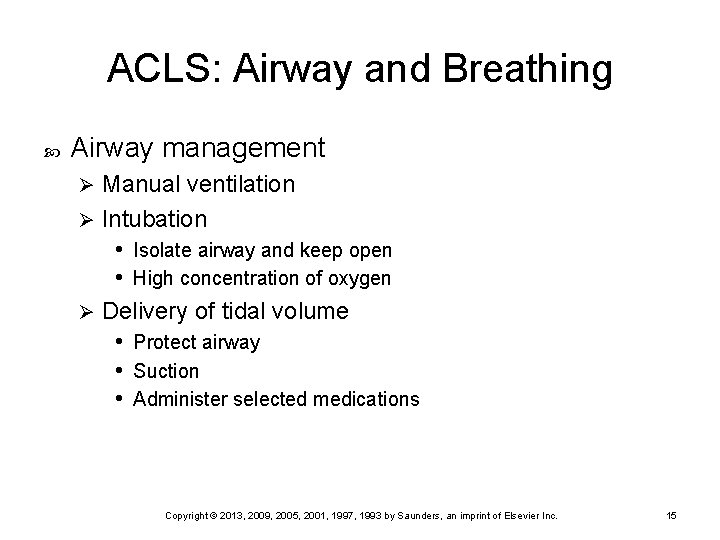
ACLS: Airway and Breathing Airway management Manual ventilation Ø Intubation • Isolate airway and keep open • High concentration of oxygen Ø Delivery of tidal volume • Protect airway • Suction • Administer selected medications Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 15
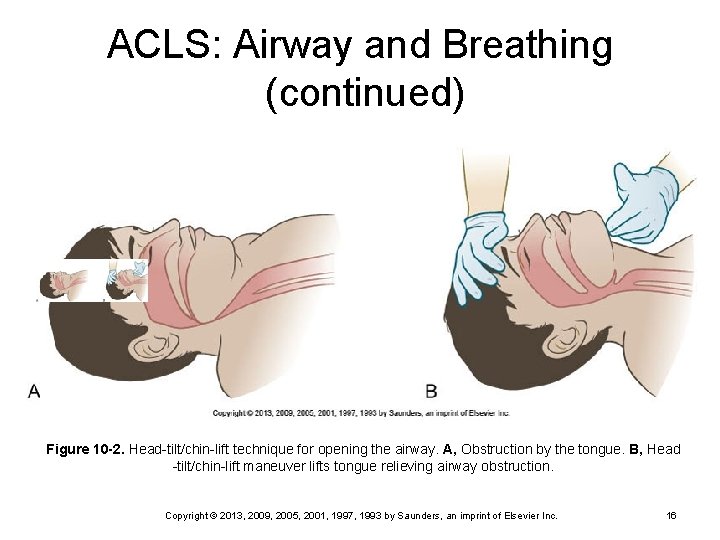
ACLS: Airway and Breathing (continued) Figure 10 -2. Head-tilt/chin-lift technique for opening the airway. A, Obstruction by the tongue. B, Head -tilt/chin-lift maneuver lifts tongue relieving airway obstruction. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 16
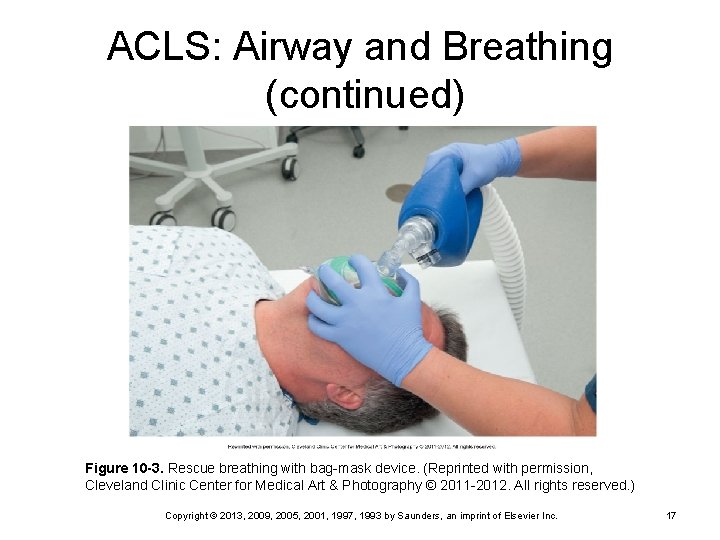
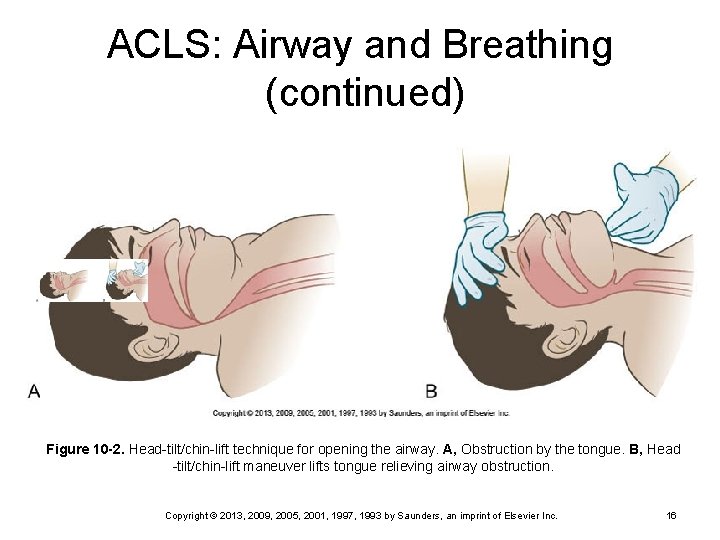
ACLS: Airway and Breathing (continued) Figure 10 -3. Rescue breathing with bag-mask device. (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2011 -2012. All rights reserved. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 17
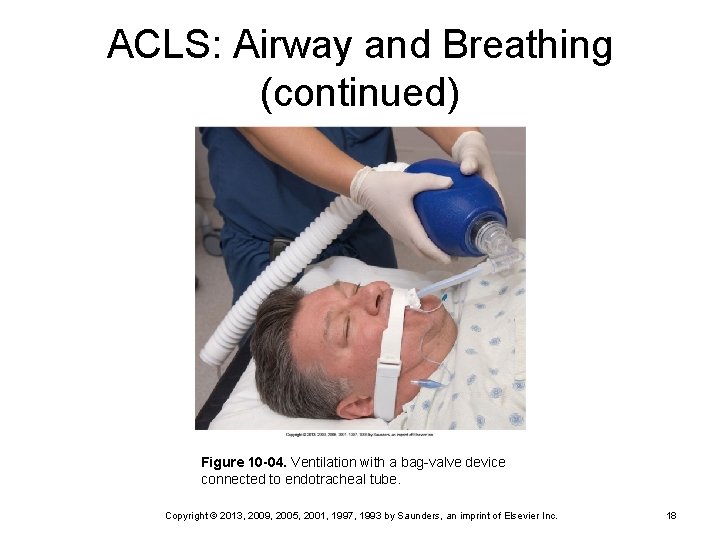
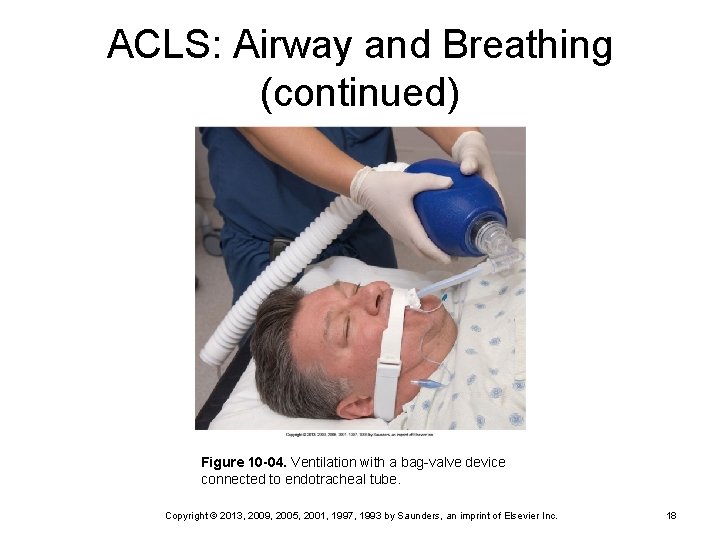
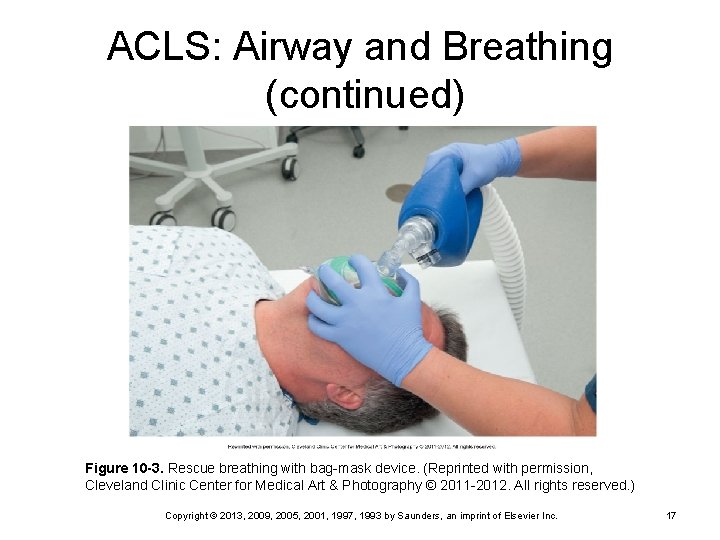
ACLS: Airway and Breathing (continued) Figure 10 -04. Ventilation with a bag-valve device connected to endotracheal tube. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 18
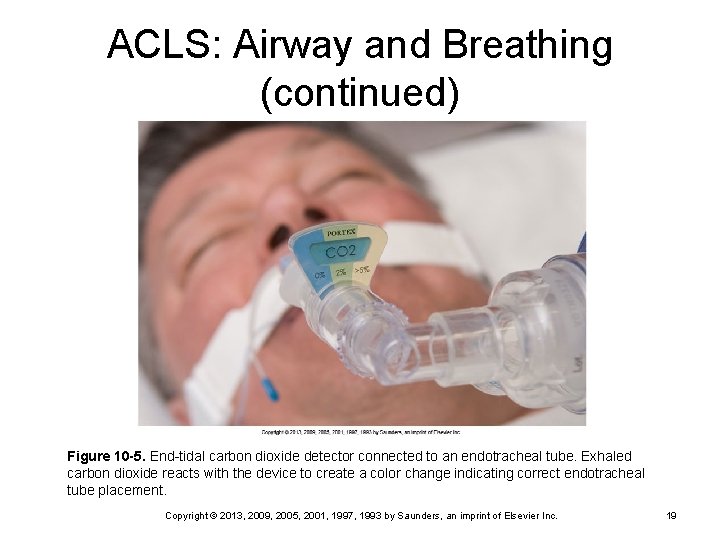
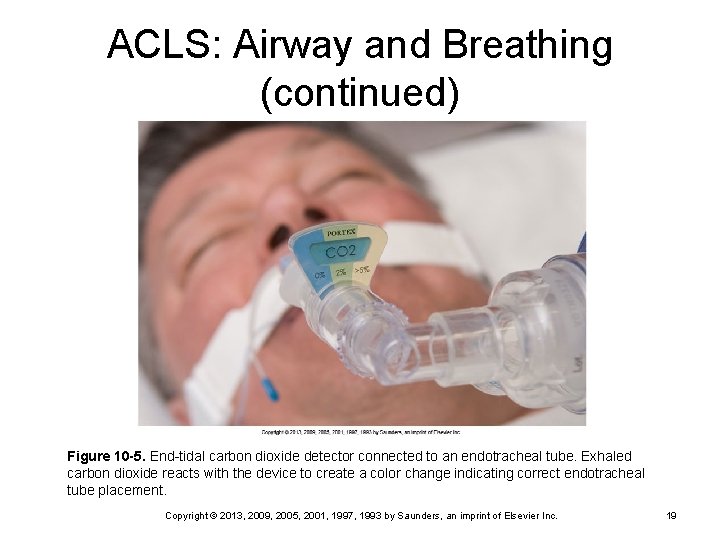
ACLS: Airway and Breathing (continued) Figure 10 -5. End-tidal carbon dioxide detector connected to an endotracheal tube. Exhaled carbon dioxide reacts with the device to create a color change indicating correct endotracheal tube placement. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 19
ACLS Primary survey ABCD (early defibrillation) Ø Use of automatic external defibrillator (AED) Ø Secondary survey Advanced skills Ø Differential diagnosis Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 20
ACLS: Circulation Large-bore IVs Biggest veins May insert central line or intraosseous cannula if IV access is difficult Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 21
ACLS (continued) Administer medications via ETT if needed Lidocaine Ø Epinephrine Ø Vasopressin Ø Defibrillation Differential diagnosis Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 22
Logical Flow of Events BLS ACLS/AED Ongoing assessment Pulse oximetry Ø ETCO 2 Ø Pulse checks Ø ABGs Ø Lab work Ø Crowd control Notification of family and communication Family presence in code If successful code, transfer to ICU Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 23
ACLS Summary Treat patient, not monitor CPR throughout Early defibrillation essential Use ETT as needed for medication administration Provide treatment according to algorithms Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 24
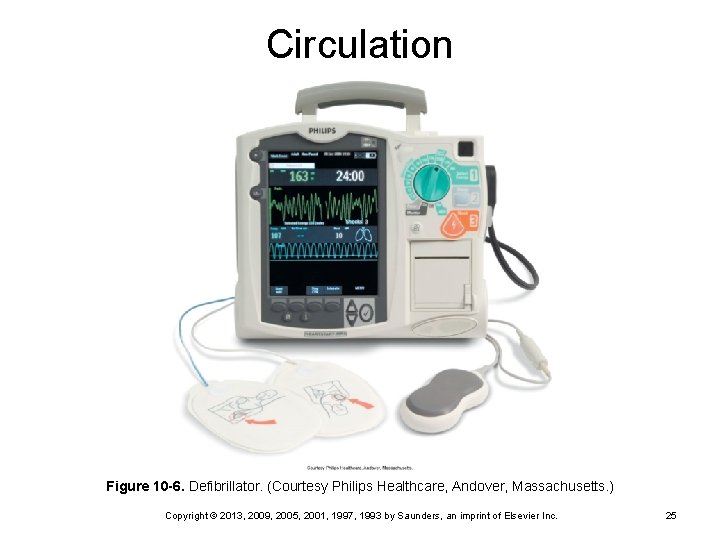
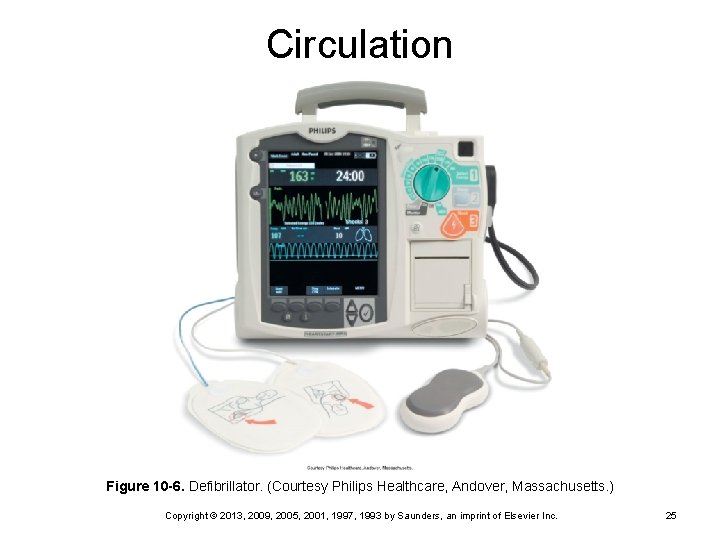
Circulation Figure 10 -6. Defibrillator. (Courtesy Philips Healthcare, Andover, Massachusetts. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 25
Dysrhythmia Management Algorithms Early defibrillation Public access defibrillation encouraged Ø AED used in field Ø AED may be used during in-hospital codes; newer defibrillators have built-in AED Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 26
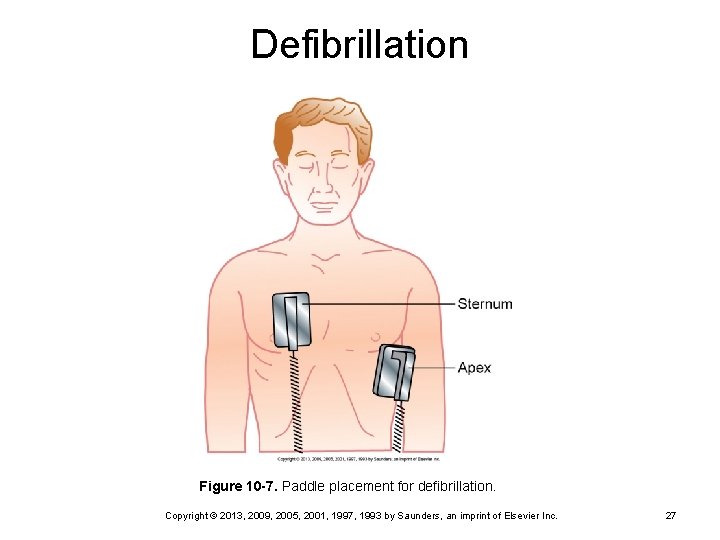
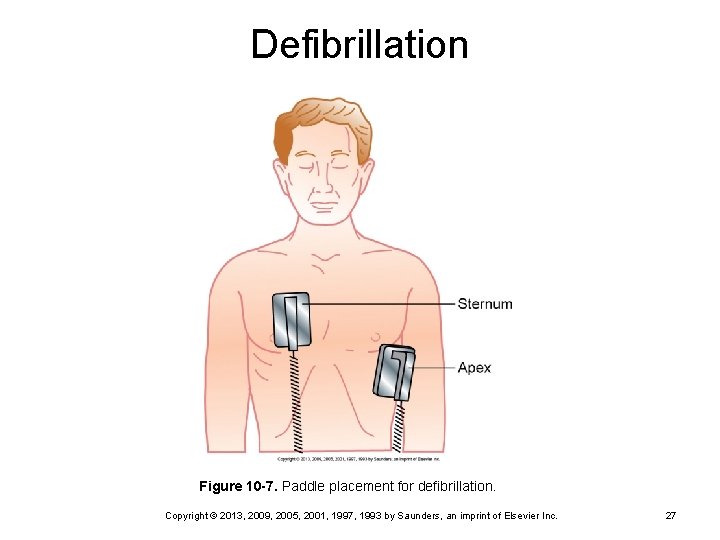
Defibrillation Figure 10 -7. Paddle placement for defibrillation. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 27
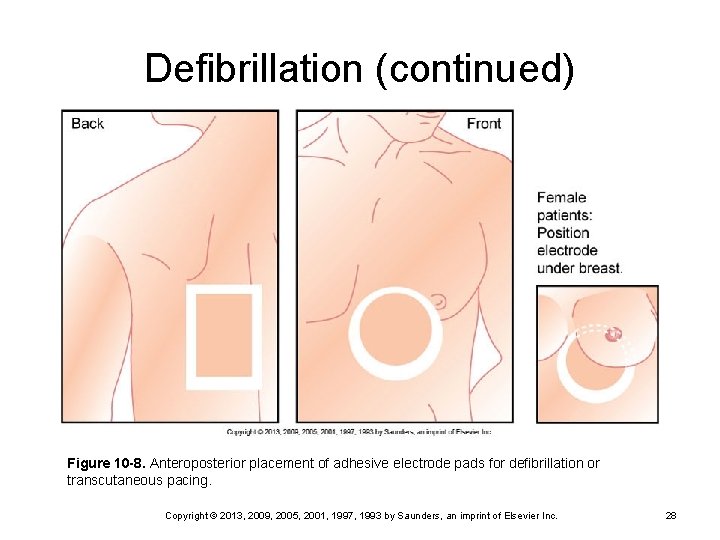
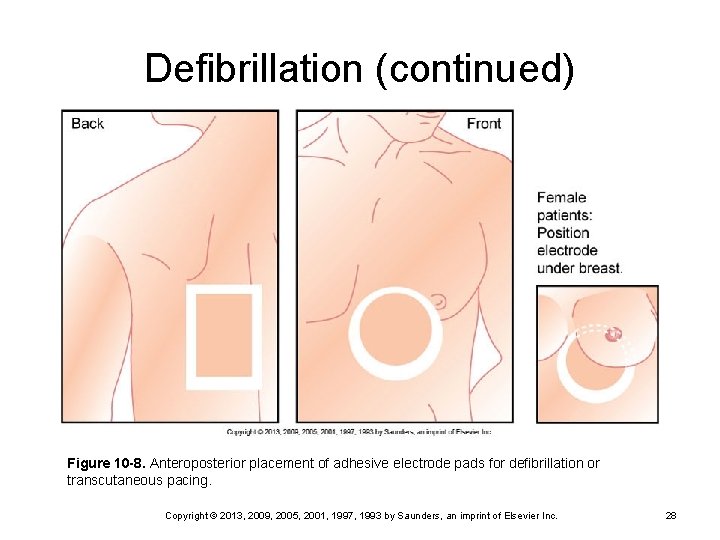
Defibrillation (continued) Figure 10 -8. Anteroposterior placement of adhesive electrode pads for defibrillation or transcutaneous pacing. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 28
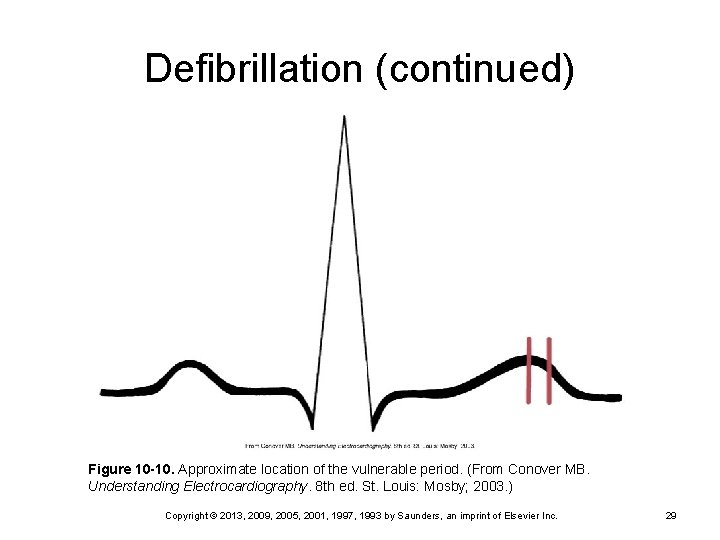
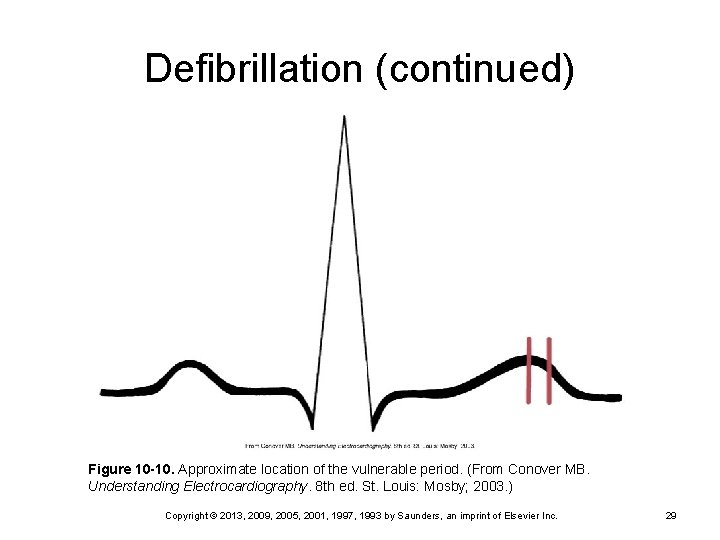
Defibrillation (continued) Figure 10 -10. Approximate location of the vulnerable period. (From Conover MB. Understanding Electrocardiography. 8 th ed. St. Louis: Mosby; 2003. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 29
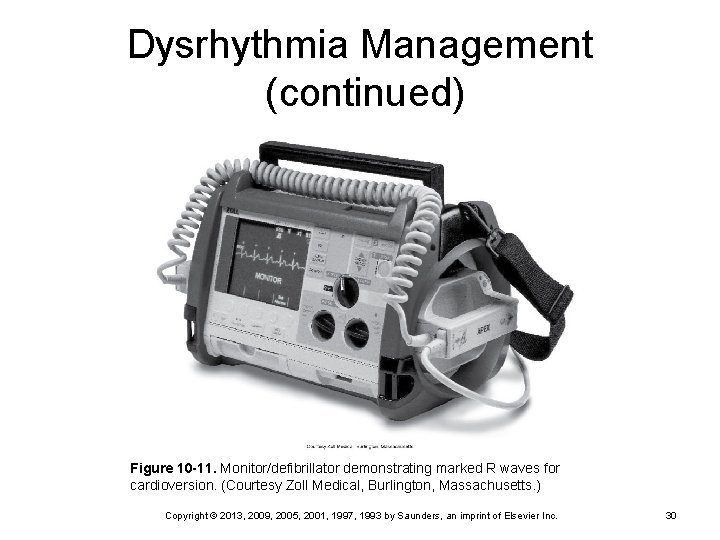
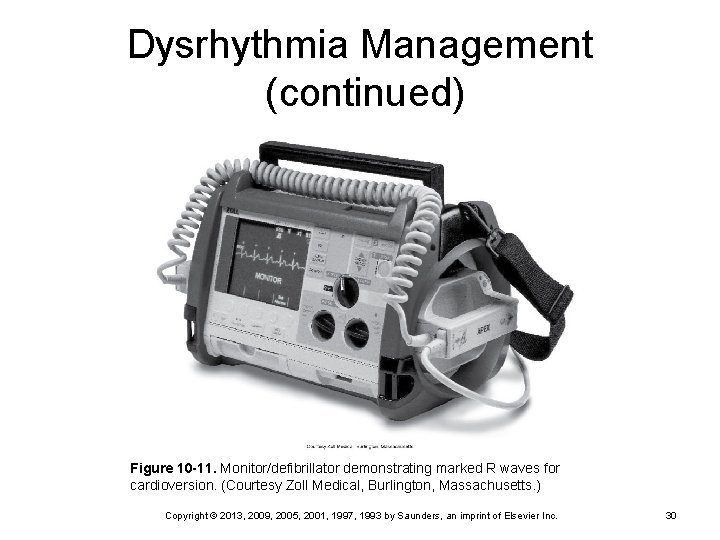
Dysrhythmia Management (continued) Figure 10 -11. Monitor/defibrillator demonstrating marked R waves for cardioversion. (Courtesy Zoll Medical, Burlington, Massachusetts. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 30
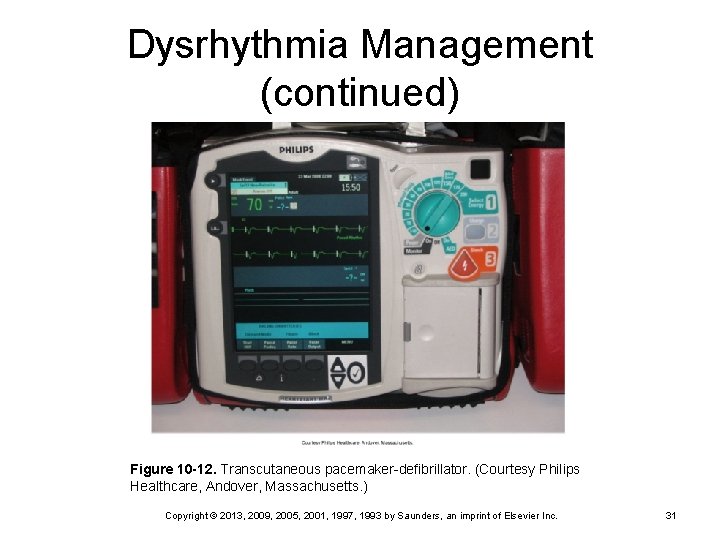
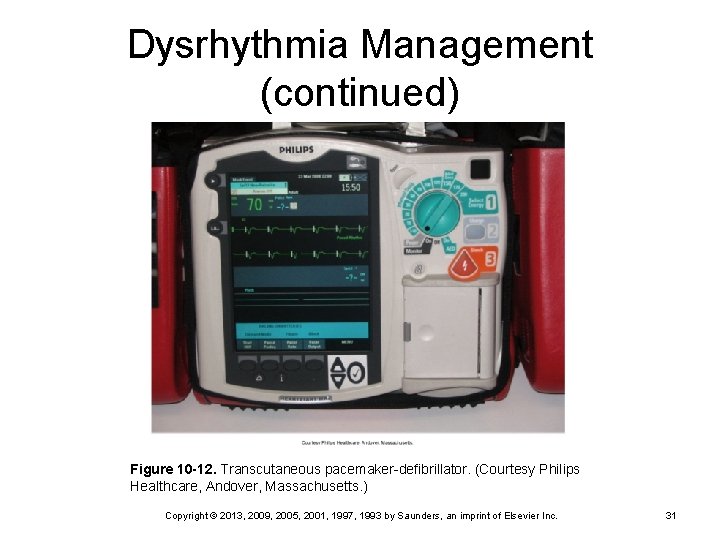
Dysrhythmia Management (continued) Figure 10 -12. Transcutaneous pacemaker-defibrillator. (Courtesy Philips Healthcare, Andover, Massachusetts. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 31
VF and Pulseless VT ABCD, initiate CPR Shock, CPR, shock Ø IV access Ø 200 (biphasic), 360 (monophasic) joules Epinephrine or vasopressin Intubate if unable to effectively manage airway and ventilate patient Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 32
VF and Pulseless VT (continued) Drug-shock continues Epinephrine repeated as needed; vasopressin is given only once Ø Consider antidysrhythmic drugs • Amiodarone (drug of choice) • Lidocaine • Procainamide Ø Magnesium if level is low or torsades is present Ø Sodium bicarbonate (only if severely acidotic) Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 33
Pulseless Electrical Activity (PEA) Rhythm without pulse Airway, oxygen, intubate, IV access ABCD with CPR Treat cause Epinephrine Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 34
Pulseless Electrical Activity (continued) Hypoxia Hypovolemia Hypothermia H+ ions (acidosis) Hypokalemia or hyperkalemia Tablets (overdose) Tamponade (cardiac) Tension pneumothorax Thrombosis (coronary) Thrombosis (pulmonary) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 35
Asystole ABCD with CPR Airway, oxygen, intubate, IV access Confirm in two leads Treat cause (see PEA) Transcutaneous pacemaker Epinephrine Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 36
Quick Quiz! The patient is in asystole with a blood p. H of 6. 95 and has lost the IV access. The nurse knows to administer which drug via the ET tube first? Atropine B. Epinephrine C. Vasopressin D. Sodium bicarbonate A. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 37
Symptomatic Bradycardia ABCD with CPR Airway, oxygen, IV access Atropine Consider cause Transcutaneous pacing Ø May need sedation/analgesia Dopamine or epinephrine No lidocaine Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 38
Unstable Tachycardia ABCD Airway, oxygen, IV access Identify the unstable tachycardia Sedation Cardioversion Reassess patient and rhythm Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 39
Defibrillation Primary treatment for VF and pulseless VT Monophasic waveform Electrical current 200 to 360 joules Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 40
Defibrillation (continued) Completely depolarize the heart Allow for the resumption of rhythm Safety is essential Complications Skin burns Ø Damage to heart muscle Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 41
Defibrillation (continued) External paddles (traditional) External “hands-off” defibrillation with multipurpose pads (ECG, pace, defib) Paddle/pad placement Transverse/anterior Ø Anterior-posterior Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 42
Defibrillation (continued) Internal paddles “Spoons” • Cardiac surgery • Open-chest CPR Ø Lower joules Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 43
Defibrillation (continued) Automatic implantable cardioverter-defibrillator (AICD) Recognizes ectopy Ø Delivers countershock Ø Prevents episodes of sudden death Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 44
Procedure for Defibrillation Paddle or defibrillation pad placement Good contact with skin (protect from burns) Ø Conductive medium with paddles Charge defibrillator to desired setting “I’m clear, you’re clear, everyone clear, oxygen clear” Adequate pressure with paddles Shock Continue CPR 2 minutes, then assess rhythm Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 45
Automated External Defibrillation (AED) External defibrillator with rhythm analysis capabilities For cardiac arrest Procedure Place two adhesive pads Ø Analysis by AED Ø Shock advisory Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 46
Cardioversion Electrical current Lower joules (e. g. , 50) Synchronized delivery on R wave (prevents “shock on T”) Disrupts ectopic foci Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 47
Defibrillation Versus Cardioversion No pulse—defibrillation Symptomatic tachycardia—cardioversion (can also do overdrive pacing) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 48
Transcutaneous Pacemaker Symptomatic bradycardia External pads/anterior-posterior placement Demand mode Adjust m. As to initiate a paced rhythm Assess rhythm for proper functioning Sedation and analgesia as needed Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 49
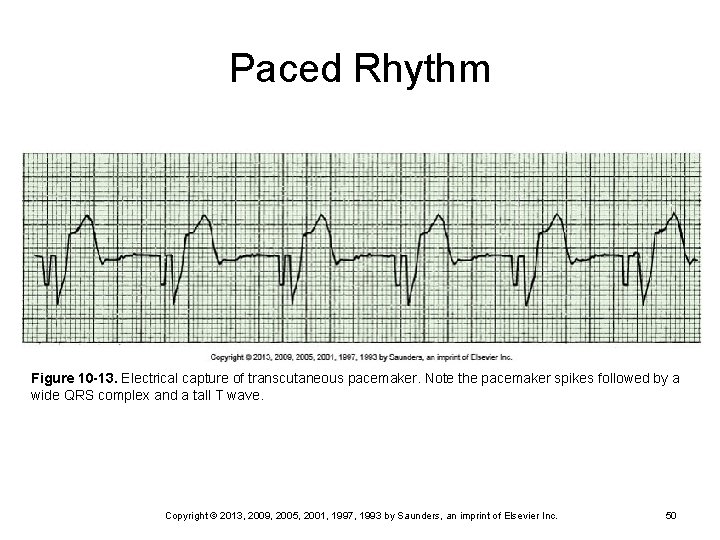
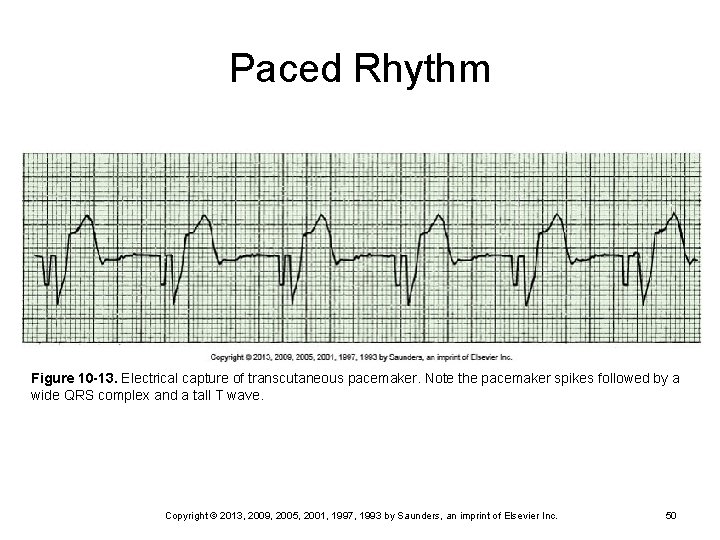
Paced Rhythm Figure 10 -13. Electrical capture of transcutaneous pacemaker. Note the pacemaker spikes followed by a wide QRS complex and a tall T wave. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 50
Overview of Medications Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 51
Oxygen Treat hypoxemia Improve tissue oxygenation Delivered via mouth to mask or bag-valve device (BVD) to mask or ETT During a cardiopulmonary arrest 100% oxygen (15 L/min via BVD) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 52
Epinephrine Potent vasoconstrictor Alpha- and beta-adrenergic effects Ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), asystole, and PEA 1 mg IV push every 3 to 5 minutes Can be given via ETT Infusion if needed Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 53
Vasopressin Nonadrenergic vasopressor Intense vasoconstriction at high doses May be as effective as epinephrine One-time dose of 40 units IV for VF/pulseless VT Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 54
Atropine Decreases vagal tone Symptomatic bradycardia 0. 5 mg to 1. 0 mg every 3 to 5 min IV push Ø Maximum of 0. 03 to 0. 04 mg/kg Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 55
Atropine (continued) Can be given via ETT; 2 to 3 mg in 10 m. L normal saline External pacemaker on standby Atropine is no longer given in PEA or asystole Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 56
Amiodarone (Cordarone) Reduces membrane excitability Prolongs the action potential and retards the refractory period; thus facilitates the termination of VT and VF Alpha-adrenergic and beta-adrenergic blocking properties Does not have the same prodysrhythmic properties of other antidysrhythmics Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 57
Lidocaine Antidysrhythmic Suppresses ventricular ectopy Bolus 1 to 1. 5 mg/kg; additional bolus 0. 5 to 0. 75 mg/kg every 5 to 10 minutes up to 3 mg/kg Follow with infusion at 2 to 4 mg/min (250 m. L 5% dextrose in water with 1 g) Ø Concentration: 1 mg/min = 15 m. L/hr Assess for lidocaine toxicity Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 58
Adenosine Slows conduction through AV node Primary use for paroxysmal supraventricular tachycardia Rapid IV push through port nearest insertion site of IV Expect short pause in rhythm after administration Half-life 10 seconds; duration 1 to 2 minutes Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 59
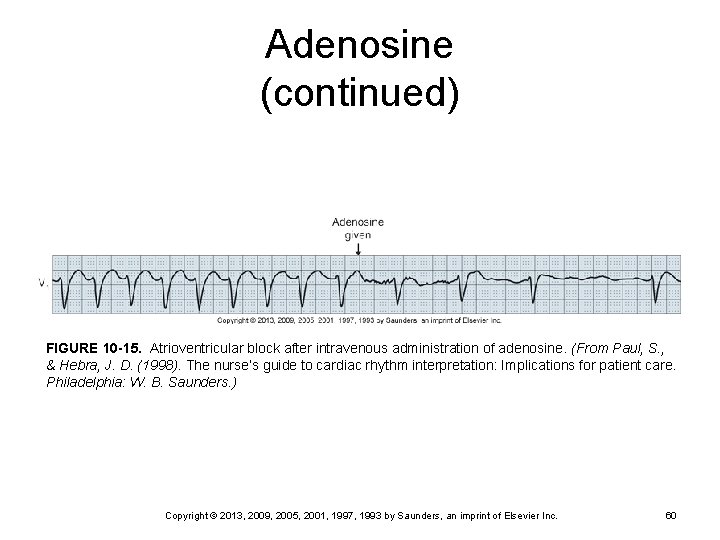
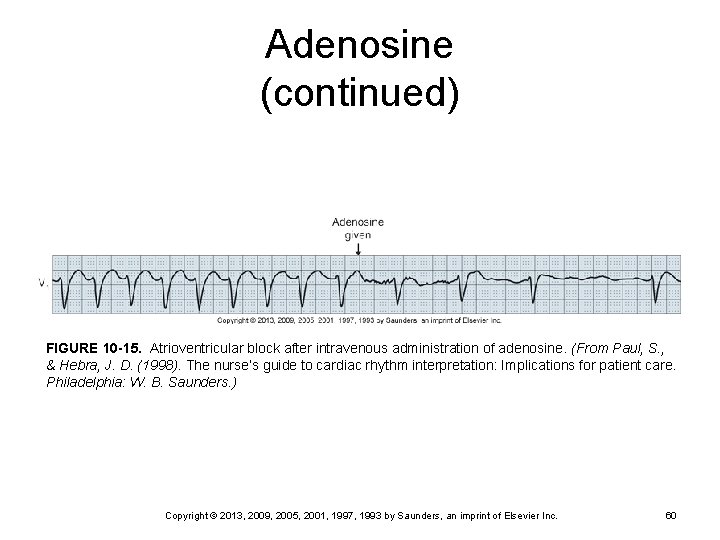
Adenosine (continued) FIGURE 10 -15. Atrioventricular block after intravenous administration of adenosine. (From Paul, S. , & Hebra, J. D. (1998). The nurse’s guide to cardiac rhythm interpretation: Implications for patient care. Philadelphia: W. B. Saunders. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 60
Magnesium Refractory VF Torsades de pointes (type of VT) Known deficiency IV bolus followed by infusion titrated by magnesium levels Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 61
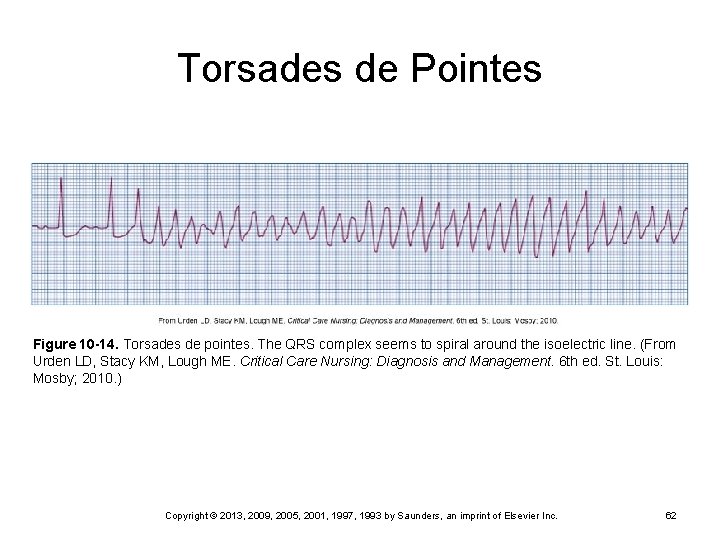
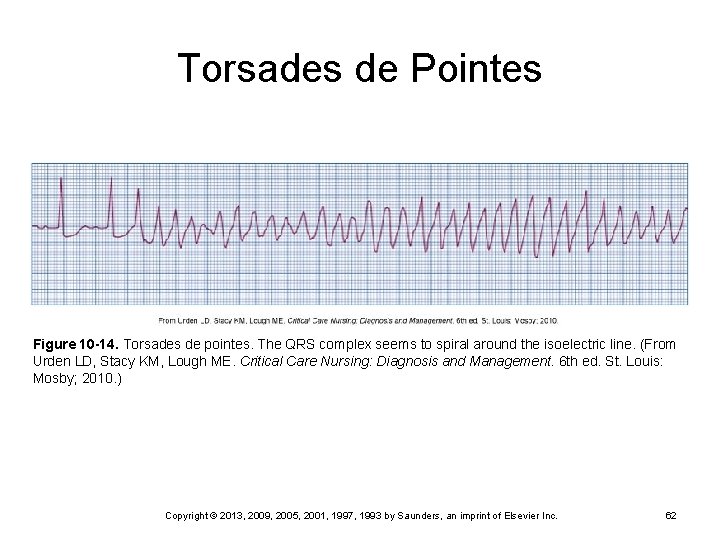
Torsades de Pointes Figure 10 -14. Torsades de pointes. The QRS complex seems to spiral around the isoelectric line. (From Urden LD, Stacy KM, Lough ME. Critical Care Nursing: Diagnosis and Management. 6 th ed. St. Louis: Mosby; 2010. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 62
Sodium Bicarbonate According to ABGs Treatment of metabolic acidosis Rarely given Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 63
Dopamine Vasoactive (vasoconstrictor) to increase BP Continuous drip 2 to 20 mcg/kg/min (learn calculations) Ø Up to 50 mcg/kg/min can be given Ø Effects dose related Moderate doses = cardiac doses Ø Higher doses = vasopressor doses Ø Consider need for fluids versus dopamine Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 64
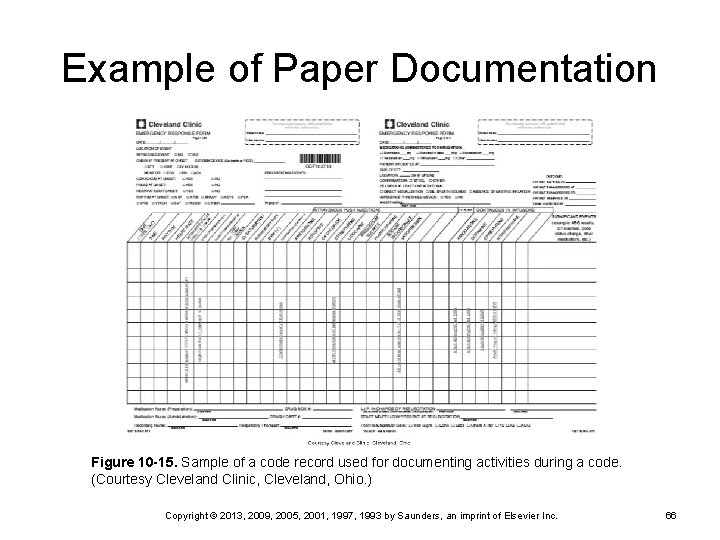
Documentation of Events Assign someone to document during code and record rhythm strips Time started Ø Actions taken and patient’s response • Defibrillation • Medications • Procedures • Pacemakers Ø Intubation and airway management Ø Vital signs Ø Team members present Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 65
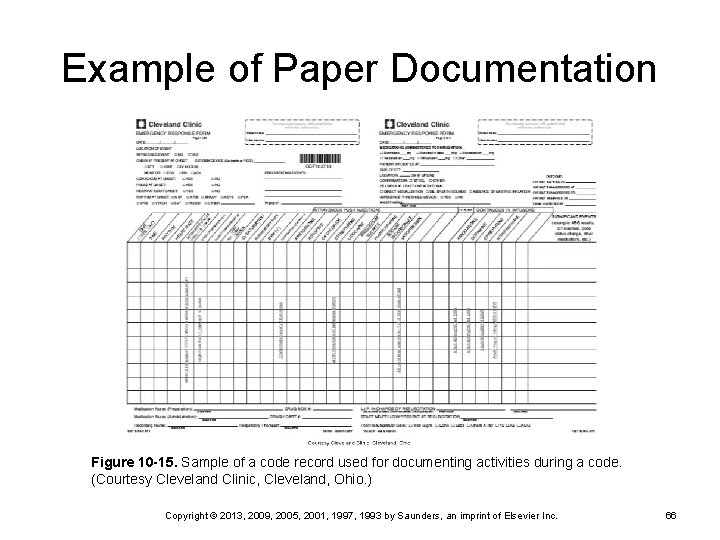
Example of Paper Documentation Figure 10 -15. Sample of a code record used for documenting activities during a code. (Courtesy Cleveland Clinic, Cleveland, Ohio. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 66
Post-Resuscitation Goals Optimize cardiopulmonary function Ø Transport to critical care unit Ø Determine cause of arrest to prevent Ø Management of patient care continues Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 67
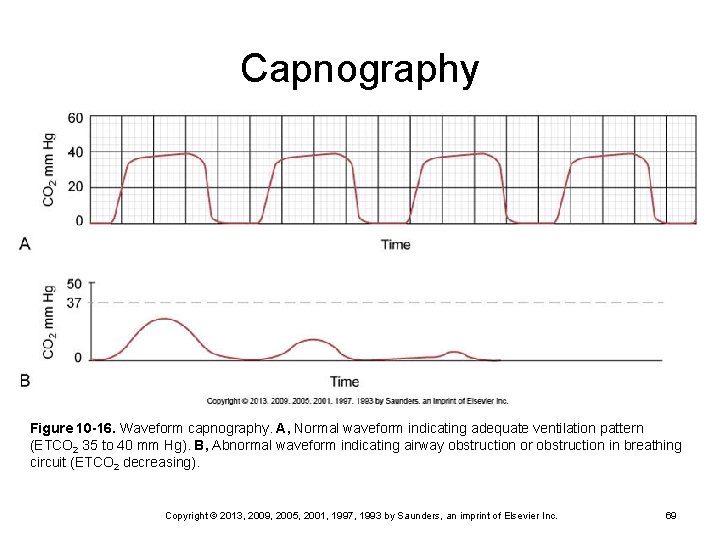
Post-Resuscitation (continued) Airway placement Maintenance of blood pressure and oxygenation Control of dysrhythmias Advanced neurological monitoring Capnography Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 68
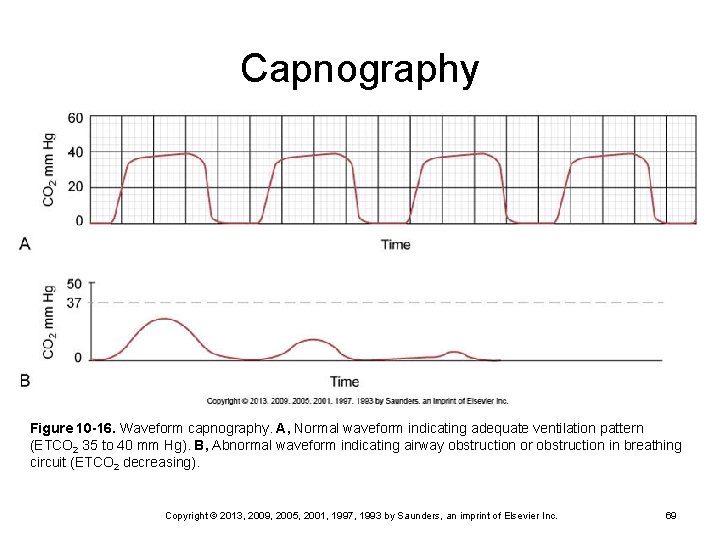
Capnography Figure 10 -16. Waveform capnography. A, Normal waveform indicating adequate ventilation pattern (ETCO 2 35 to 40 mm Hg). B, Abnormal waveform indicating airway obstruction or obstruction in breathing circuit (ETCO 2 decreasing). Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 69
Post-CPR Interventions 12 -lead ECG Arterial line Pulmonary artery catheter Indwelling urinary catheter for hourly output NG tube if bowel sounds are absent or if patient is mechanically ventilated Serial neurological exams Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 70
Post-CPR Care Palliative comfort care Pain management Ø Sedation Ø Anxiety management Ø Head CT scan and EEG if comatose Blood glucose levels (may be hyperglycemic) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 71
Supporting the Family Should they be present during a code? Providing information Ø Active communication Ø Visitation after a code Ø Support from chaplain and nursing staff Ø Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 72
Supporting Other Patients Remove from the situation Talk with them Assess their feelings Continue their care Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 73
Therapeutic Hypothermia Fever from brain injury increases the level of neurological damage post-CPR Ø Increased length of stay Lower body temperature is associated with better recovery Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 74
Hypothermia Optimal temperature is not known Firm guidelines have not been developed Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 75
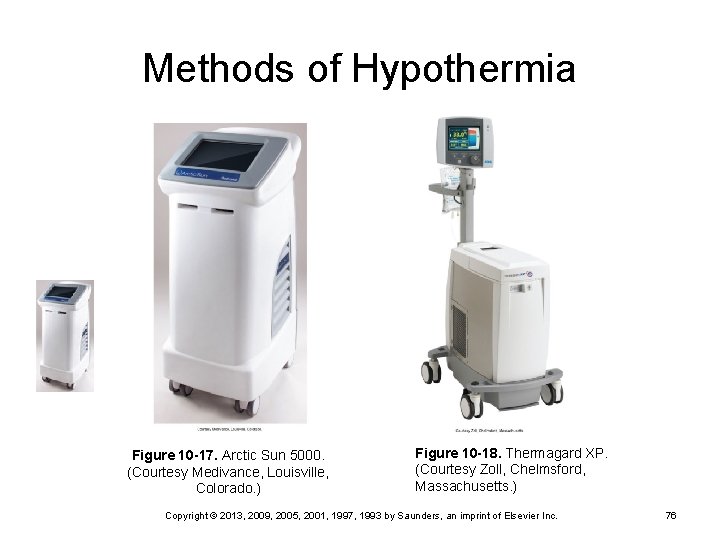
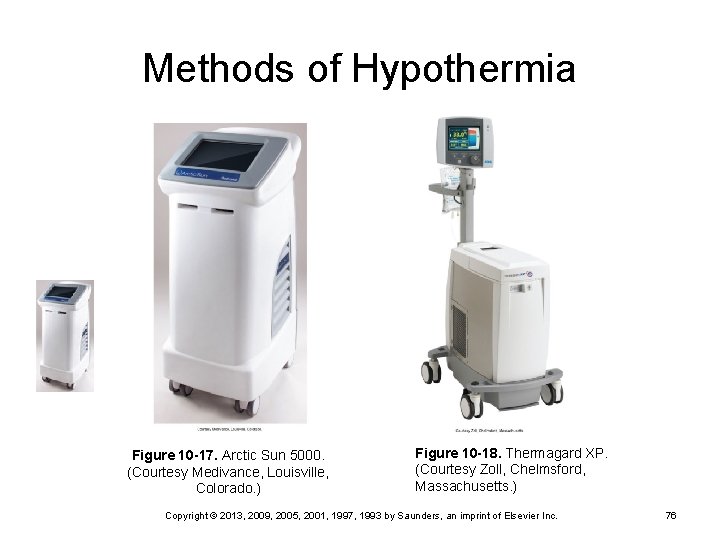
Methods of Hypothermia Figure 10 -17. Arctic Sun 5000. (Courtesy Medivance, Louisville, Colorado. ) Figure 10 -18. Thermagard XP. (Courtesy Zoll, Chelmsford, Massachusetts. ) Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 76
Nursing Care During Hypothermia Monitor core body temperature Bladder catheter with a temperature probe Ø Esophageal thermometer Ø Pulmonary artery catheter Ø Axillary, tympanic, and oral probes do not measure core body temperature and should not be used Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 77
Monitoring with Hypothermia Shivering Increase oxygen consumption Ø Increases body temperature Ø Controlled with IV sedatives Ø Analgesics Ø Neuromuscular blockade medications Ø Drugs can mask seizure activity Ø Continuous EEG monitoring Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 78
Complications Bleeding Infection Metabolic and electrolyte disturbances Hyperglycemia Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 79
Nursing Care Infection prevention Handwashing Ø VAP prevention Ø Hyperglycemic management Ø IV insulin Monitor electrolytes During cooling, K+, Mg+, phosphate, and Ca+ may decrease Ø During rewarming, K+, Mg+, phosphate, and Ca+ may increase Ø Rewarm after 24 hours very slowly Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 80
Quick Quiz! The nurse is caring for a patient being treated with therapeutic hypothermia post-CPR. Which order should the nurse question? Draw serum electrolytes stat B. Measure blood glucose every 2 hours C. Continuously monitor EEG and ECG D. Record tympanic temperature every hour A. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 81
Quick Quiz! A 56 -year-old female patient reports feeling fatigued with sudden nausea and lightheadedness. The nurse immediately chooses to take which action? Call the charge nurse B. Get the patient an antiemetic C. Call the attending physician D. Notify the rapid response team A. Copyright © 2013, 2009, 2005, 2001, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 82