Chapter 10 Cardiovascular System Cardiovascular System CO 2












- Slides: 52
Chapter 10 Cardiovascular System
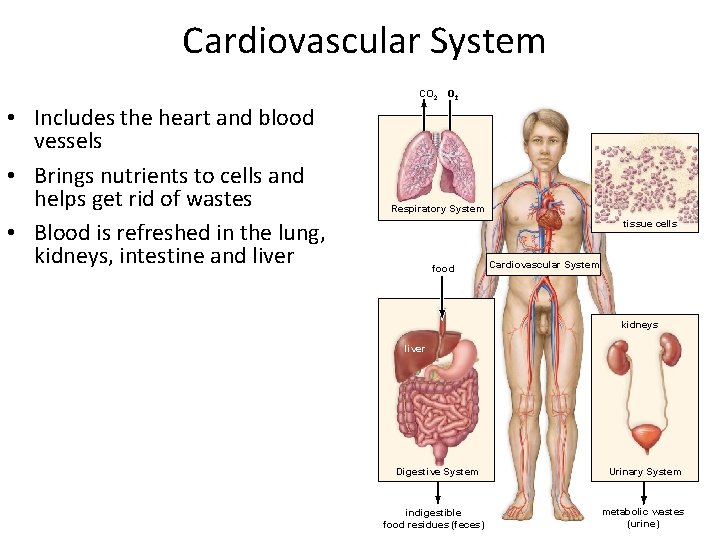
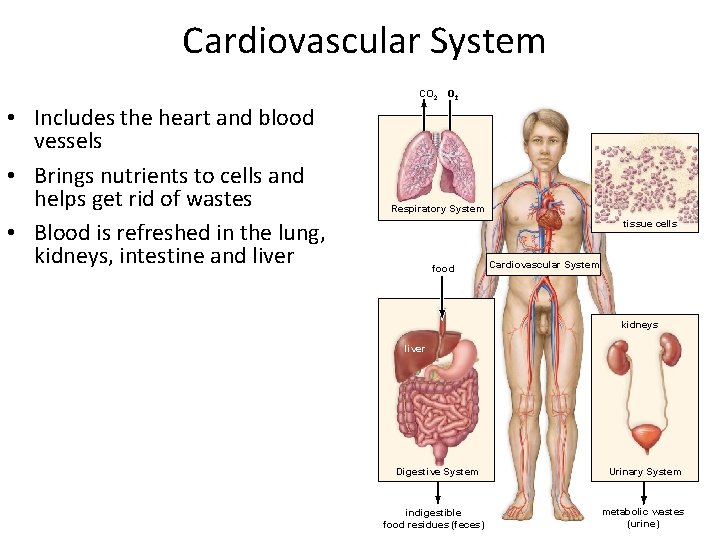
Cardiovascular System CO 2 • Includes the heart and blood vessels • Brings nutrients to cells and helps get rid of wastes • Blood is refreshed in the lung, kidneys, intestine and liver Respiratory System tissue cells food Cardiovascular System kidneys liver Digestive System indigestible food residues (feces) Urinary System metabolic wastes (urine)
Function of the Cardiovascular System 1. Generate blood pressure 2. Transport blood 3. Exchange of nutrients and wastes at the capillaries 4. Regulate blood flow as needed

Main pathway of blood in the body • Heart – arteries – arterioles – capillaries venules – veins – back to the heart…
Blood Vessels—Venous System • Arteries: – Large elastic: • Closest to the heart with walls containg elastic connective tissue • Are under a lot of pressure • They distend as: – Maintains: – Arterioles: • Small arteries with muscular walls • Regulate flow from:
Blood Vessels—Venous System • Capillaries: – Thinnest blood vessels – Deliver: – Remove:
Blood Vessels—Venous System • Veins: – Under low pressure so 3 mechanisms assist veins in returning blood to heart: 1. Contraction of skeletal muscles 2. One-way valves 3. Pressure changes associated with breathing – – Inhale: increase abdominal pressure & squeeze abdominal veins This pushes blood from abdomen toward heart (respiratory pump)
The Heart • Pumps in order to move blood • Layers of the heart wall: – Epicardium: outermost layer of epithelium & connective tissue – myocardium: thick middle layer of cardiac muscle – Endocardium: thin endothelial layer • 4 Chambers: – No direct communication between: right & left side • “Right heart” sends blood: • “Left heart” sends blood:
The Heart • Cardiac valves – Permit flow of blood in: • Atrioventricular (AV) valves: – Prevent: – Tricuspid valve: » directs blood flow from: » prevents backflow to: – Bicuspid (mitral) valve: » directs blood flow from: » prevents backflow to:

The Heart • Cardiac valves – Permit flow of blood in: • 2 semilunar valves: – Prevent: – Pulmonary valve: » directs blood flow from: » prevents backflow to: – Aortic valve: » directs blood flow from: » prevents backflow to:

The Heart Aorta Superior vena cava Left pulmonary artery Right pulmonary artery Pulmonary trunk Left pulmonary veins Pulmonary semilunar valve Right atrium Right AV valve Right ventricle Inferior vena cava Left atrium Aortic semilunar valve Left AV valve Left ventricle Chordae tendineae Papillary muscles Septum

Pulmonary Circuit—Oxygenation of Blood Pathway – Deoxygenated blood from the body into heart 1. Through the vena cava to the right 2. 3. – atrium Through the right atrioventricular valve to the right ventricle Through the pulmonary semilunar valve to the pulmonary trunk and the lungs Oxygenated blood from lungs to heart 1. Through the pulmonary veins to 2. the left atrium Through the left atrioventricular valve to the left ventricle

Systemic Circuit—Delivery of Oxygenated Blood to Tissues • Pathway – Oxygenated blood from the heart to tissues 1. Through the aortic semilunar valve to the aorta 2. Through branching arteries and arterioles to tissues 3. Through the arterioles to capillaries
Systemic Circuit: Return of Blood to the Heart • Pathway – Deoxygenated blood returns to heart 1. From capillaries into venules and veins 2. To the vena cava and into the right atrium
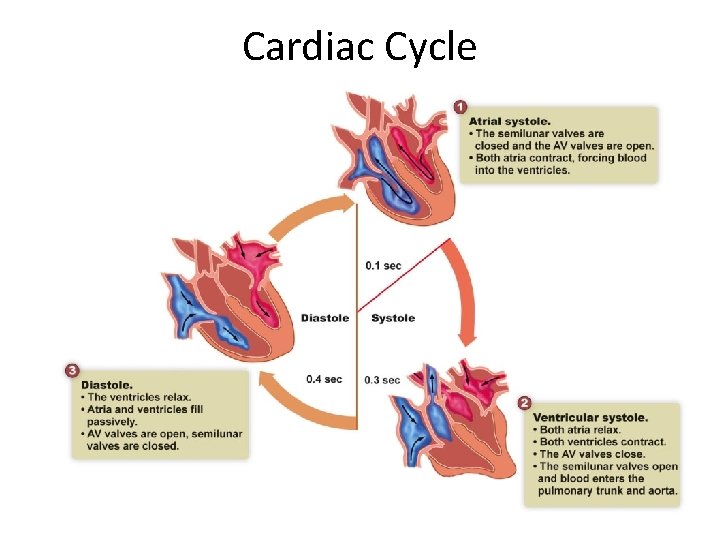
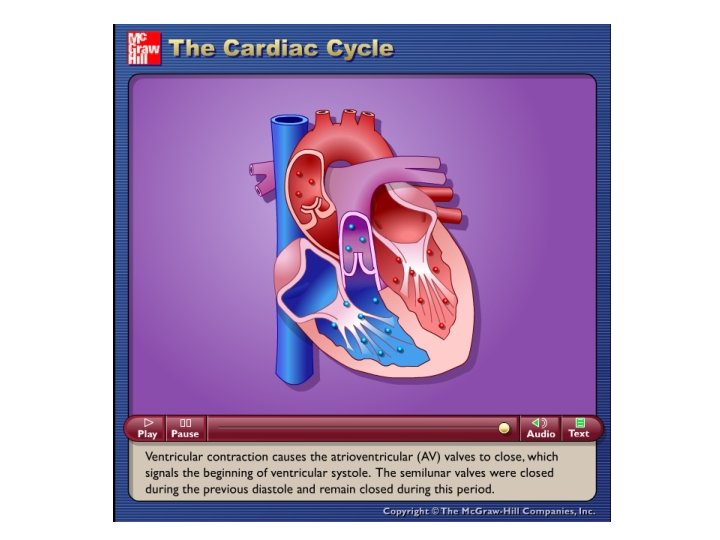
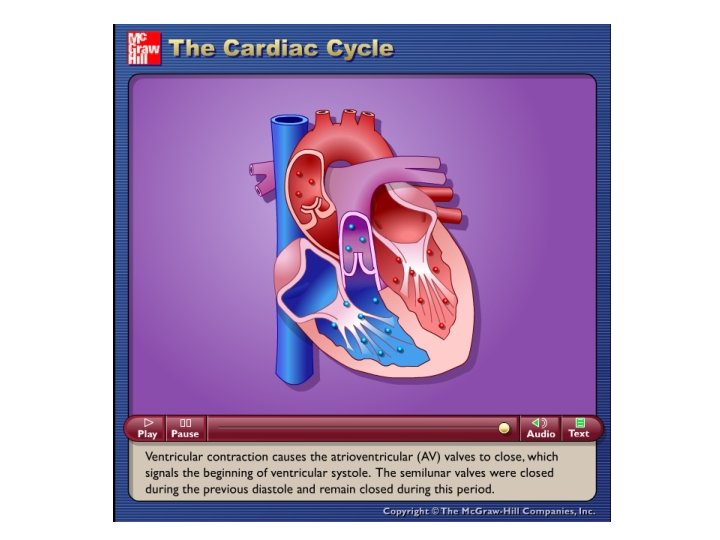
Cardiac Cycle • Beating of the heart is pulsatile – – – The sequence of events that occurs during a single contraction & relaxation of the heart Systole: Diastole:
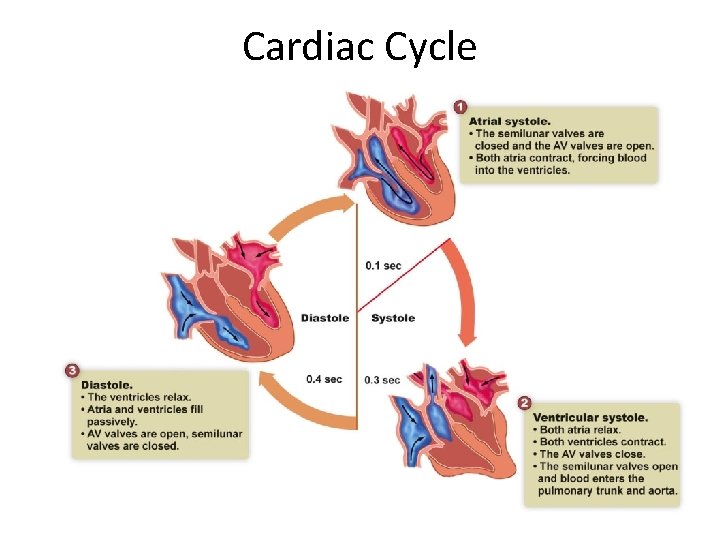
Cardiac Cycle
Please note that due to differing operating systems, some animations will not appear until the presentation is viewed in Presentation Mode (Slide Show view). You may see blank slides in the “Normal” or “Slide Sorter” views. All animations will appear after viewing in Presentation Mode and playing each animation. Most animations will require the latest version of the Flash Player, which is available at http: //get. adobe. com/flashplayer.

Heart Sounds and Heart Valves • Lub-dub – These sound occur due to vibrations caused by the closing of valves • Lub: closure of the 2 AV valves during ventricular systole • Dub: closure of aortic & pulmonary semilunar valves close during ventricular diastole
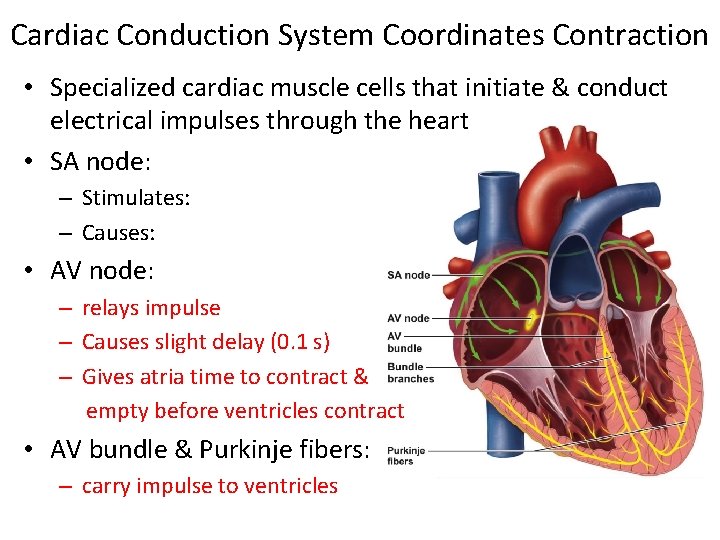
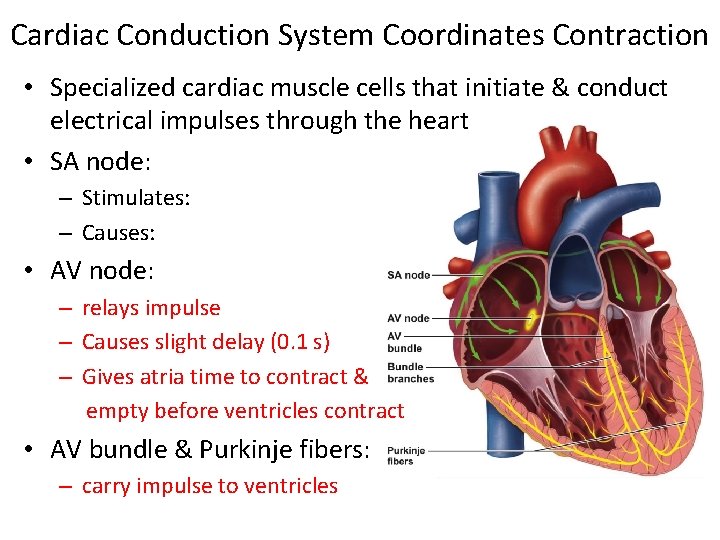
Cardiac Conduction System Coordinates Contraction • Specialized cardiac muscle cells that initiate & conduct electrical impulses through the heart • SA node: – Stimulates: – Causes: • AV node: – relays impulse – Causes slight delay (0. 1 s) – Gives atria time to contract & empty before ventricles contract • AV bundle & Purkinje fibers: – carry impulse to ventricles
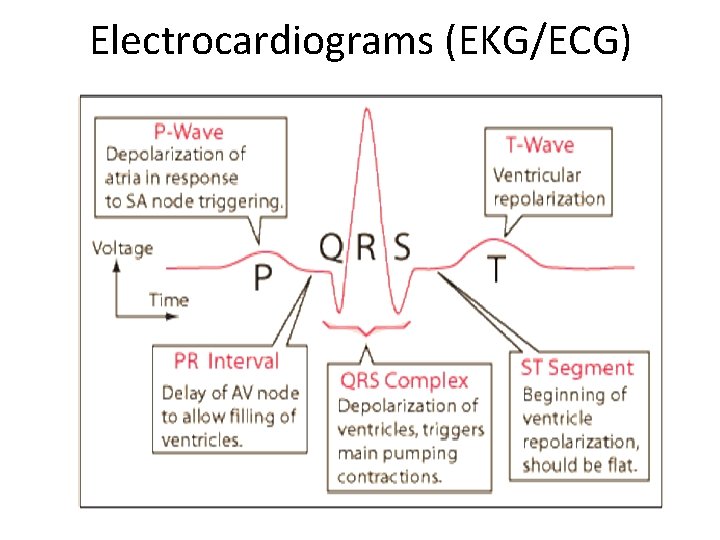
Electrocardiograms (EKG/ECG) • Measures: • Three formations – P wave: – QRS complex: – T wave:
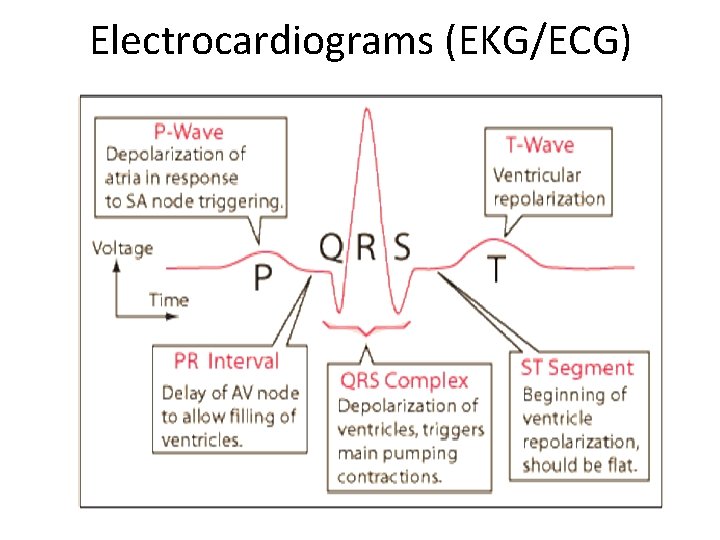
Electrocardiograms (EKG/ECG)
Blood Pressure • The force that blood exerts on the wall of a blood vessel as the heart beats • Definitions – Systolic pressure: – Diastolic pressure: • Measurement – Sphygmomanometer
Cardiac Arrhythmias • Disturbances in heart rate or rhythm – 3 types: • Atrial fibrillation • Ventricular fibrillation • Heart block
Cardiac Arrhythmias • Atrial fibrillation: – Abnormal cardiac rhythms in which: – Caused when: – Effects: • Heart beats so fast that: – Treatment:
Cardiac Arrhythmias • Ventricular fibrillation: – Unlike a-fib ventricular fibrillation is: – Ventricles are unable to contract normally causing: – If recognized early its possible to stop by: • Heart block: – A delay or complete interruption of impulse transmission from atria to ventricles – Complete heart block requires:
Valvular Heart Disease • Rheumatic heart disease – A complication of rheumatic fever • Review rheumatic fever discussed in Ch 4 – Caused by : • Primarily affects: • Leads to : – Prevention • Treat strep infection promptly

Valvular Heart Disease • Mitral Valve Prolapse – Common but only few develop problems – Valve leaflets: – Prolapsing leaflets may not fit together tightly: • blood leaks back into left atrium: – On auscultation: • Murmur caused by:
Coronary Heart Disease • Results from: – Narrowing of arteries due to: • Lipids are deposited in an area where: • The collection of fatty material & debris is called: – This type of arteriosclerosis is called:
Coronary Heart Disease • Atherosclerosis: – Early stage of atherosclerosis: • Newly formed plaques may break loose into blood & are called: – Late stage of atherosclerosis: • Cholesterol becomes crystallized & fibrous scar tissue forms – Risk factors:
Coronary Heart Disease • Atherosclerosis plaque causes narrowing of the lumen: – Narrowing by 50% or more may decrease blood flow • At rest: • With exertion: – Myocardial ischemia: • Leads to pain called:
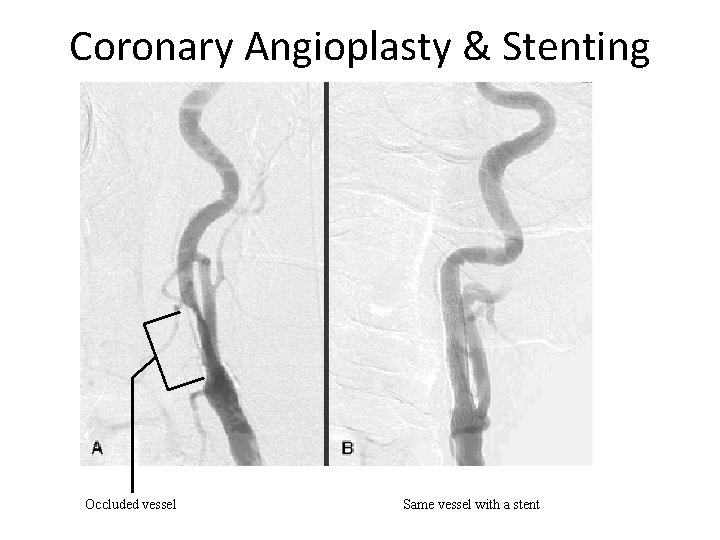
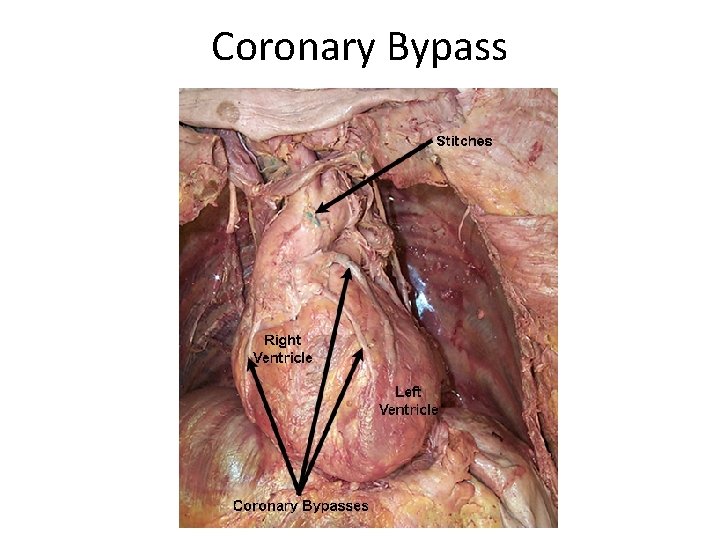
Coronary Heart Disease • Diagnosed with a procedure called: – Performed by passing: • Helps determine: • Treatment: – Medicine: – Lifestyle changes: – Angioplasty & stenting: – Bypass surgery:

Coronary Angioplasty & Stenting
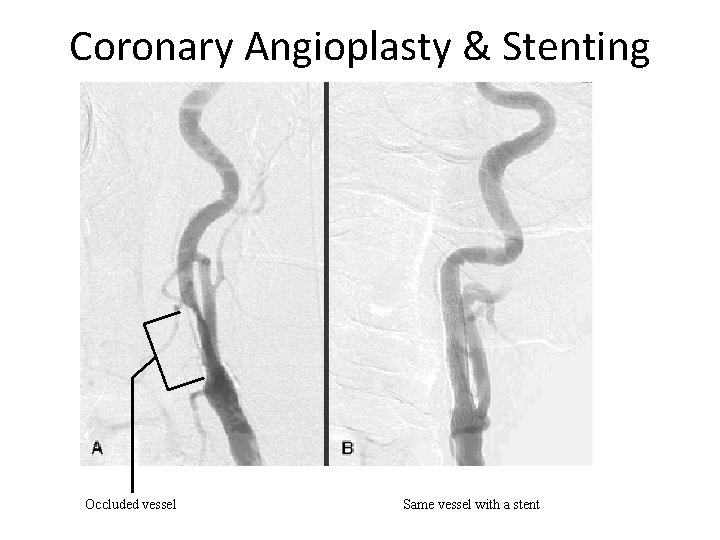
Coronary Angioplasty & Stenting Occluded vessel Same vessel with a stent
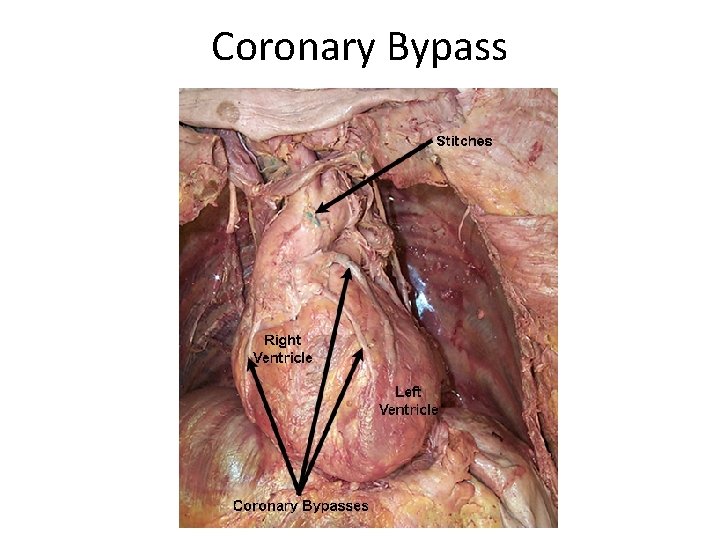
Coronary Bypass
Coronary Heart Disease • Severe & prolonged myocardial ischemia may lead to a “heart attack” – The term “heart attack” can actually refer to two different events: • Cardiac arrest • Myocardial infarction

Cardiac Arrest • Occurs when: – Myocardial ischemia causes cardiac arrhythmias which are: – Most common arrhythmia that leads to cardiac arrest is: • Rapidly fatal because: • If recognized early its possible to stop by:
Myocardial Infarction • Occurs when: – Myocardial ischemia decreases blood flow to the heart muscle • Leads to: • Usually only involves: – Complications: • Arrhythmias • Heart failure • Intracardial thrombi • Cardiac rupture
Hypertension • Arterial blood pressure higher than: • Ideal “normal” blood pressure: • Two types: – Primary hypertension – Secondary hypertension
Hypertension • Primary hypertension: – Cause is not well understood • Excessive vasoconstriction of small arterioles occurs resulting in: – Increased peripheral resistance – Increased diastolic blood pressure – Increased force of ventricular contraction – Compensatory increase in systolic pressure – Treatment: • Drugs that:
Hypertension • Primary hypertension: – Effects on the body if left untreated: • Cardiac effects: increased peripheral resistance → higher workload → heart enlarges → • Vascular effects: increased pressure → premature wearing out of vessels; accelerates atherosclerosis; injury to arterioles → • Renal effects: narrowed renal arterioles → decreased blood supply to kidneys → injury and degenerative changes in glomeruli and tubules →
Hypertension • Secondary hypertension: – Caused by a know disease • Ex. chronic kidney disease, pituitary or adrenal tumor, & hyperthyroidism – Treatment:
Heart Failure • Heart fails to pump adequate blood supply to tissues • Cause: • Two types: – Acute heart failure: – Chronic heart failure: – This is why this type of heart failure is also called:
Heart Failure • Treatment: – Decrease workload – Diuretics – Salt and fluid restrictions – Medications to strengthen and slow heart • E. g. , digitalis

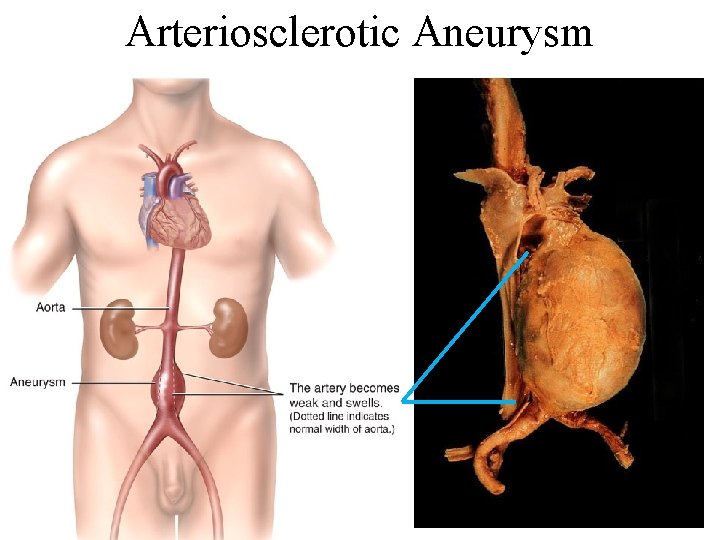
Aneurysm • Aneurysm – Dilatation or outpouching of the wall of an artery • Most common cause: – Two types: • Arteriosclerotic aneurysm • Dissecting aneurysm of the aorta
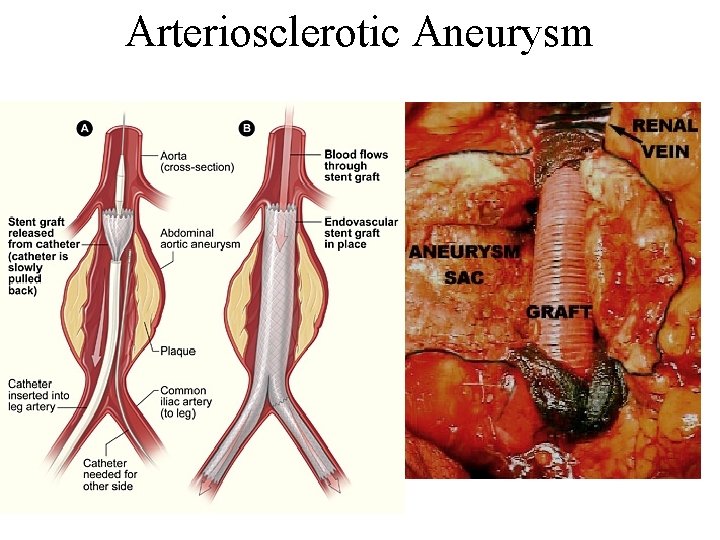
Aneurysm • Arteriosclerotic aneurysm – Caused by: • Leads to: • Most commonly seen in the aortic wall which: – Usually develops: • If aorta ruptures results in: – Treatment involves:
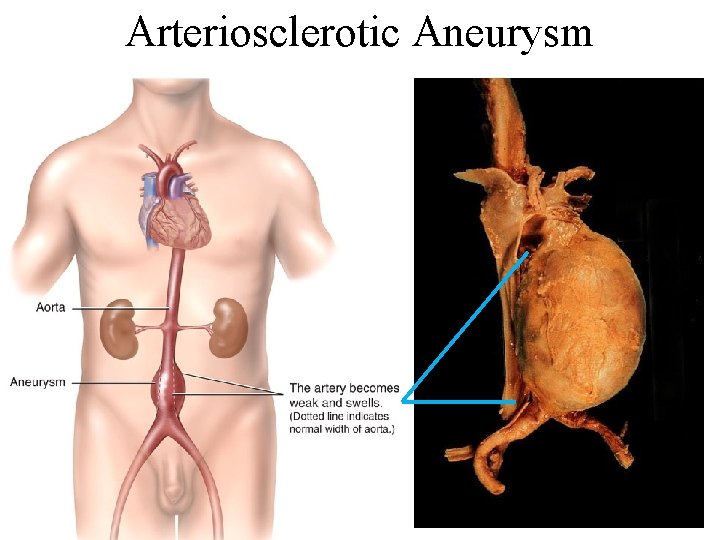
Arteriosclerotic Aneurysm
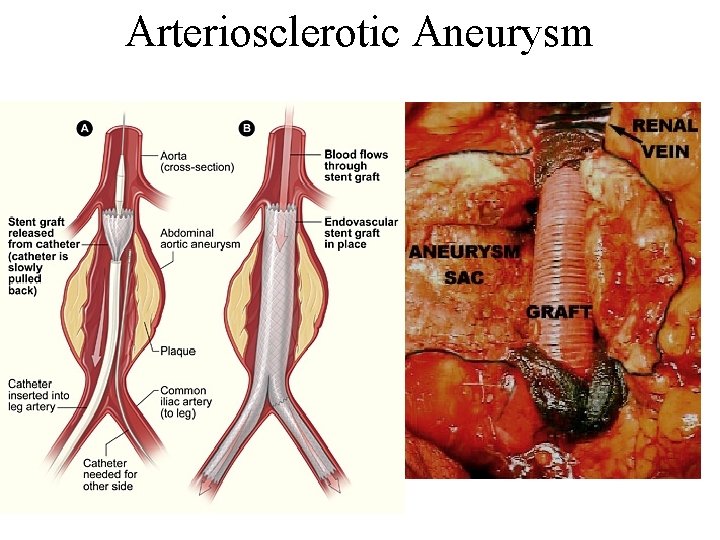
Arteriosclerotic Aneurysm
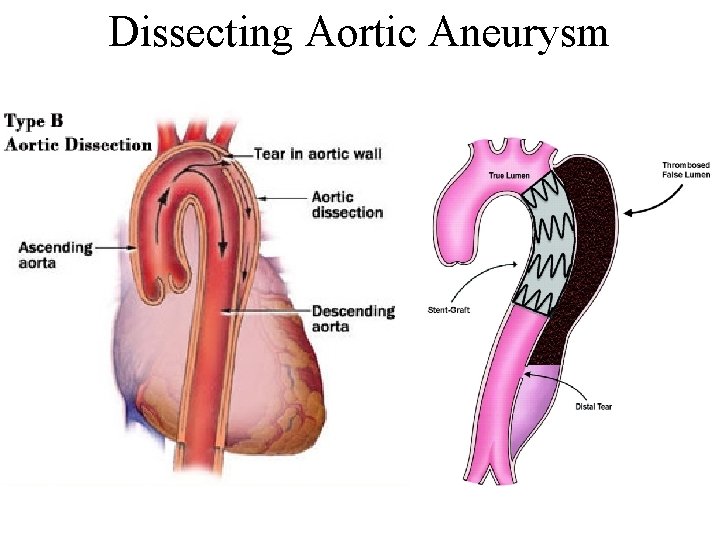
Aneurysm • Dissecting aneurysm of the aorta – Caused by: • Leads to: • Most commonly seen in people with: – Symptoms often include: • If aorta ruptures results in: – Treatment involves:
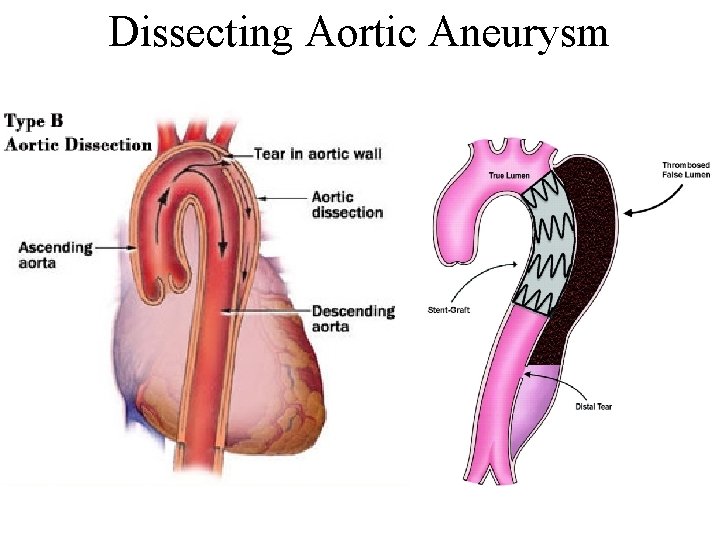
Dissecting Aortic Aneurysm

Diseases of the Veins • Varicose veins – Dilated, tortuous, and elongated veins • Commonly occur in: • Due to: • Causes: • Most likely a congenital weakness • Any activity blood flow back to heart & increases pressure

Diseases of the Veins • Varicose veins – Treatment: • • Elevate legs Walk Use support or elastic stockings Strip vein
? ? QUESTIONS? ? 52