Chapter 10 Bathing and Personal Hygiene Copyright 2016
Chapter 10 Bathing and Personal Hygiene Copyright © 2016 by Mosby, an imprint of Elsevier Inc.
Hygiene Supports physical and mental health Maintains skin integrity When performing hygiene: Ø Ø Discuss health-related concerns Ensure privacy Discuss patient concerns Perform physical assessment Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 2
Hygiene (Cont. ) Functions of intact skin Ø Ø Ø Defense against infection Sensory perception Regulation of body temperature Benefits of bathing Ø Ø Ø Cleansing the skin Stimulates circulation Promotes ROM Reduces body odors Improves self image Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 3
Patient-Centered Care Take time to talk with the patient to identify personal and cultural preferences for care. Before beginning any aspect of hygiene care, inform the patient of the procedure and acknowledge his/her preferences. Taking the person’s preferences into consideration promotes patient-centered care. When possible, ask friends/family to bring in appropriate hygiene soaps, oils, and creams not available in the health care setting. Use a calm and gentle manner, and a reassuring tone of voice. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 4
Safety Some patients lack the physical energy or functional status to perform self-care and are temporarily dependent on others to enhance the healing and recovery process. Do not leave patients unattended because there is an increased risk for falls. If the patient cannot participate, the family or significant other may want to assist. Assist the patient and family to understand that a full bath 3 times a week may be adequate for many older patients. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 5
Safety (Cont. ) Bathing is an opportunity to assess the skin for common skin problems or pressure points, which are potential risks for pressure ulcers. Be aware of other factors that contribute to pressure ulcer formation: Ø Ø Ø incontinence friction and shear immobility loss of sensory perception level of activity poor nutrition Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 6
Safety (Cont. ) Before using showers or baths in health care settings, be sure that the patient has the physical energy and functional status to use the tub or shower. Fully assess the patient’s activity tolerance and instruct the patient on how to use the emergency call device. In the home setting assess the patient’s bath/shower facilities for a safety bar, setting on hot water heaters, and the physical layout of the bathroom. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 7
Common Skin Problems Dry skin Acne Rashes Contact dermatitis Abrasion Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 8
Evidence-Based Practice Provide a daily bath for bed-bound patients to improve hygiene and promote comfort. Determine bath time based on patient preference and clinical condition Use a basin dedicated to bathing only and not for the storage of supplies. Avoid use of unfiltered tap water. Use no-rinse p. H balanced cleansers. Apply emollients after each nonprepackaged bathing product when available. Bathe patients at high risk for skin colonization and infection daily using a disposable cloth prepackaged with a 2% solution of chlorhexidine gluconate (CHG). Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 9
Skill 10 -1: Complete Bathing The type of bath, the extent of the bath, and the methods for bathing depend on the patient’s ability to participate, the condition of the patient’s skin, and in some settings, the time of day Types of Baths: Ø Ø Ø Complete bed bath Partial bed bath Sponge bath at the sink Tub bath Shower Bed bath/travel bag Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 10
Skill 10 -1: Complete Bathing (Cont. ) Assessment Assess degree of assistance needed for bathing. Assess patient’s fall risk, tolerance of activity, level of discomfort with movement, and presence of shortness of breath or chest pain with exertion. Ø Assess patient’s bathing preferences such as time of day, products used, usual frequency of bathing, and type of bath. Ø Ask if patient has noticed any problems related to skin and genitalia. Ø Identify presence of devices. Ø Assess room environment for temperature level. Ø Ø Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 11
Skill 10 -1: Complete Bathing (Cont. ) Assessment (Cont. ) Ø Assess patients at risk for skin breakdown: for patients at risk for pressure ulcers use a pressure ulcer assessment tool. • Immobilization or decreased mobility • Reduced sensation • Excessive moisture on skin, particularly on skin surfaces • • • that rub against each other Vascular insufficiencies External devices applied to or around skin Older adult patients Shear or friction (sliding down in bed) Incontinence (bowel or bladder). Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 12
Skill 10 -1: Complete Bathing (Cont. ) Planning/Expected Outcomes Delegation and Collaboration Assessment of the patient’s skin, pain level, and ROM cannot be delegated to nursing assistive personnel. The skill of bathing can be delegated. Ø The nurse instructs the NAP about: • reporting early signs of impaired skin integrity, including Ø redness or pallor; • reporting perineal drainage, discomfort, or tenderness; • proper ways to position male and female patients with musculoskeletal limitations and indwelling catheters; • reporting fatigue or report of pain during hygiene care. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 13
Skill 10 -1: Complete Bathing (Cont. ) Evaluation Unexpected Outcomes Patient’s skin on lower extremities is dry, flaky, and itchy. Ø The patient’s skin has evidence of rashes, redness, scaling, or cracking. Ø The rectum, perineum, or genital region is inflamed, is swollen, or has foul-smelling discharge. Ø Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 14
Recording and Reporting • Routine documentation may include completion of flow sheet. Record observations made during the bath, which may include type of bath given, patient’s ability to assist or cooperate, condition of patient’s skin, and any nursing interventions for improving skin integrity. • Record patient’s response to bathing and any concerns voiced by patient regarding self-care needs. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 15
Skill 10 -1: Complete Bathing (Cont. ) Geriatric Older adults may chill easily. Older adults with urinary incontinence need meticulous skin care to reduce skin irritation from urine and feces. Ø Older adults have dry skin and do not need frequent bathing. Avoid use of harsh soaps which can increase skin p. H. Ø Ø Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 16
Special Considerations Pediatric Ø Ø Ø Infants chill easily; keep body covered and work quickly. Use only mild soap for bathing infants and children. Families need to be involved in a child’s care; children feel more secure in the presence of their family. Home Care Type of bath chosen depends on assessment of the home, availability of running water, and condition of bathing facilities. Ø Adhesive strips on bottom of tub or shower, hand rails, chairs, or stools in tub or shower help protect patients from falls and injury. Ø Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 17
Quick Quiz! The nurse will administer a complete bed bath for which of the following patients? A. B. C. D. 12 -year-old boy with a long leg cast 92 -year-old woman in assisted living 25 -year-old ventilator dependent man 40 -year-old patient with Parkinson’s disease Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 18
Procedural Guideline 10 -1: Perineal Care A patient routinely receives perineal care during a complete bath. However, patients who have fecal or urinary incontinence or an indwelling Foley catheter or are recovering from rectal or genital surgery or childbirth need more frequent perineal hygiene. Perineal care may be embarrassing for both the patient and nurse. Always act in a professional and sensitive manner and provide privacy at all times. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 19
Procedural Guideline 10 -1: Perineal Care (Cont. ) Delegation and Collaboration The skill of perineal care can be delegated to nursing assistive personnel. Ø The nurse instructs the NAP about: • Any physical restriction that affects proper positioning of Ø patient • The proper ways to position male and female patients with an indwelling Foley catheter during perineal care. • Notifying the nurse of any perineal drainage, excoriation, or rash observed. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 20
Procedural Guideline 10 -2: Oral Hygiene Oral hygiene maintains the comfort and integrity of oral cavity mucosa and helps control plaque-associated oral diseases. Oral hygiene promotes comfort, prevents infection, and aids in nutrition. Adequate daily oral hygiene includes brushing, flossing, and rinsing. Encouraging dependent or chronically ill patients to attend to their own oral hygiene creates a general sense of comfort and improves appetite. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 21
Procedural Guideline 10 -2: Oral Hygiene (Cont. ) Factors Influencing Oral Hygiene Ø Ø Ø Ø Ø Upper-extremity strength or dexterity Willingness and ability to perform hygiene Diabetes Tendency to dehydration Radiation therapy Chronic inflammatory disease Chemotherapy or other chemical injury Mucositis Trauma Mouth breathing Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 22
Procedural Guideline 10 -2: Oral Hygiene (Cont. ) Oral hygiene may be required as often as every 1 to 2 hours. For unconscious patients, first assess the patient’s gag reflex and determine the type of suction apparatus needed to prevent aspiration. Ø Many patients have no gag reflex. Ø Critically ill patients with endotracheal tubes and who are on mechanical ventilation are at risk for ventilatorassociated pneumonia (VAP) if the saliva is aspirated. Ø Mechanical cleansing and oral hygiene reduce plaque and oropharyngeal colonization associated with VAP. Ø Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 23
Procedural Guideline 10 -2: Oral Hygiene (Cont. ) Delegation and Collaboration The skill of providing oral hygiene can be delegated to nursing assistive personnel. However, the nurse is responsible for the assessment of the patient’s gag reflex to determine if the patient is at risk for aspiration. Ø The nurse instructs the NAP about: • The patient’s level of consciousness, presence or absence Ø of gag reflex, proper positioning, and whether oral suction apparatus is needed for clearing oral secretions • Reporting any changes in oral mucosa to the nurse • Reporting excessive coughing or choking during or after oral care Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 24
Procedural Guideline 10 -3: Care of Dentures Loose dentures can cause discomfort and make it difficult for patients to chew food and speak clearly. Dentures can be easily lost or broken. Store them in an enclosed, labeled cup and soak when not worn (e. g. , at night, during surgery or a diagnostic procedure). Reinsert them as soon as possible. The change in appearance when they are not worn may be of major concern to the patient. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 25
Procedural Guideline 10 -3: Care of Dentures (Cont. ) Delegation and Collaboration The skill of denture can be delegated to nursing assistive personnel. Ø The nurse instructs the NAP to: • not to use hot or excessively cold water when caring for Ø dentures • inform the nurse if there are cracks in the dentures • inform the nurse if the patient complains of any oral discomfort Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 26
Quick Quiz! Which of the following issues can contribute to malnutrition for an elderly man? A. B. C. D. Loose-fitting dentures Moist mucous membranes Visible layer of tooth enamel Clear colored saliva Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 27
Procedural Guideline 10 -4: Hair Care—Combing, Shampooing, and Shaving Having the hair groomed makes a person feel more comfortable. Fever, malnutrition, some medications, emotional stress, and depression affect the condition of hair. Diaphoresis leaves hair oily and unmanageable. Dry hair requires less frequent shampooing than oily hair. Hospitalized patients who have excess perspiration or treatments that leave blood or solutions in the hair may need a shampoo. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 28
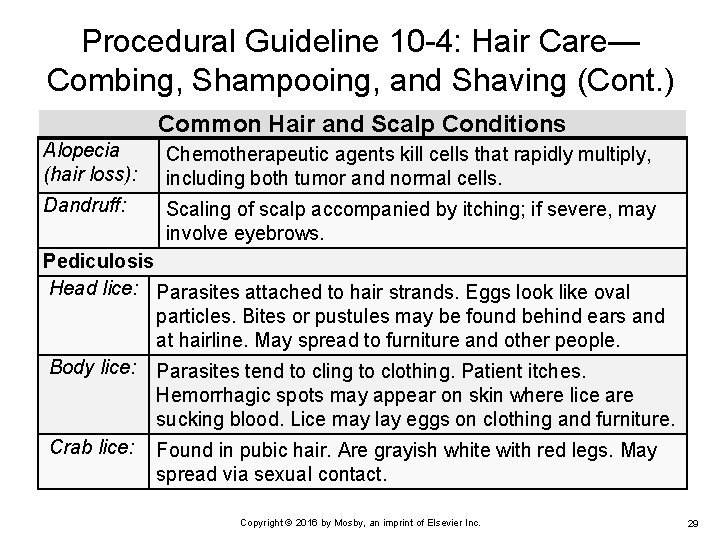
Procedural Guideline 10 -4: Hair Care— Combing, Shampooing, and Shaving (Cont. ) Common Hair and Scalp Conditions Alopecia (hair loss): Chemotherapeutic agents kill cells that rapidly multiply, including both tumor and normal cells. Dandruff: Scaling of scalp accompanied by itching; if severe, may involve eyebrows. Pediculosis Head lice: Parasites attached to hair strands. Eggs look like oval particles. Bites or pustules may be found behind ears and at hairline. May spread to furniture and other people. Body lice: Parasites tend to cling to clothing. Patient itches. Hemorrhagic spots may appear on skin where lice are sucking blood. Lice may lay eggs on clothing and furniture. Crab lice: Found in pubic hair. Are grayish white with red legs. May spread via sexual contact. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 29
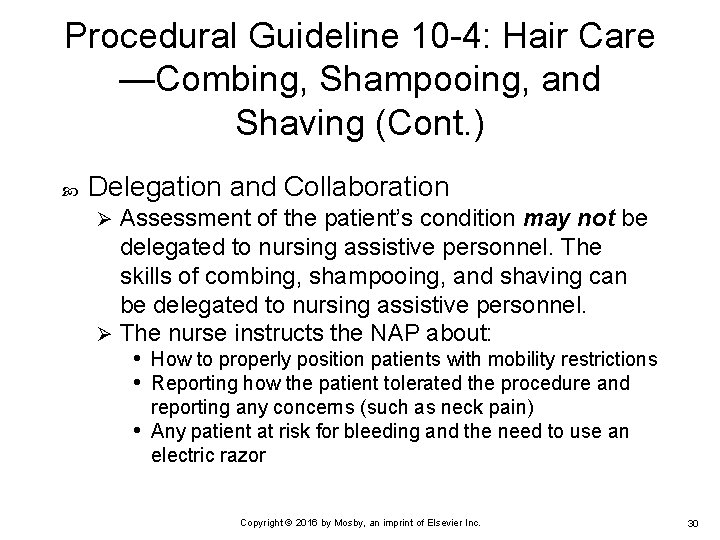
Procedural Guideline 10 -4: Hair Care —Combing, Shampooing, and Shaving (Cont. ) Delegation and Collaboration Assessment of the patient’s condition may not be delegated to nursing assistive personnel. The skills of combing, shampooing, and shaving can be delegated to nursing assistive personnel. Ø The nurse instructs the NAP about: • How to properly position patients with mobility restrictions • Reporting how the patient tolerated the procedure and Ø reporting any concerns (such as neck pain) • Any patient at risk for bleeding and the need to use an electric razor Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 30
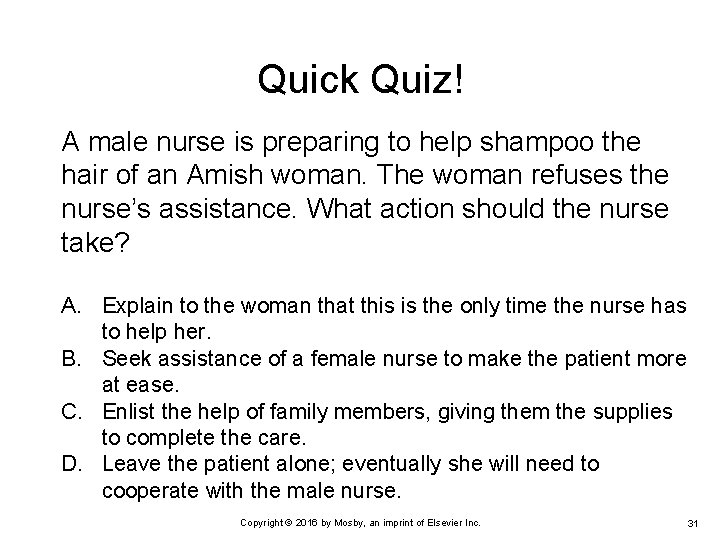
Quick Quiz! A male nurse is preparing to help shampoo the hair of an Amish woman. The woman refuses the nurse’s assistance. What action should the nurse take? A. Explain to the woman that this is the only time the nurse has to help her. B. Seek assistance of a female nurse to make the patient more at ease. C. Enlist the help of family members, giving them the supplies to complete the care. D. Leave the patient alone; eventually she will need to cooperate with the male nurse. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 31
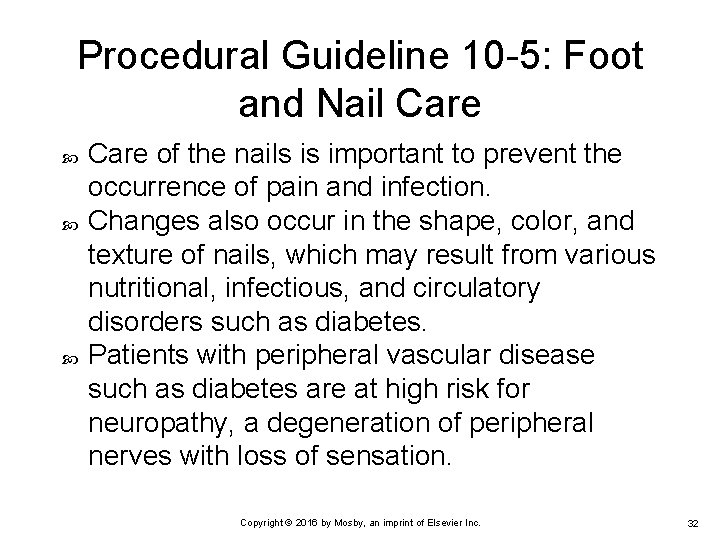
Procedural Guideline 10 -5: Foot and Nail Care of the nails is important to prevent the occurrence of pain and infection. Changes also occur in the shape, color, and texture of nails, which may result from various nutritional, infectious, and circulatory disorders such as diabetes. Patients with peripheral vascular disease such as diabetes are at high risk for neuropathy, a degeneration of peripheral nerves with loss of sensation. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 32
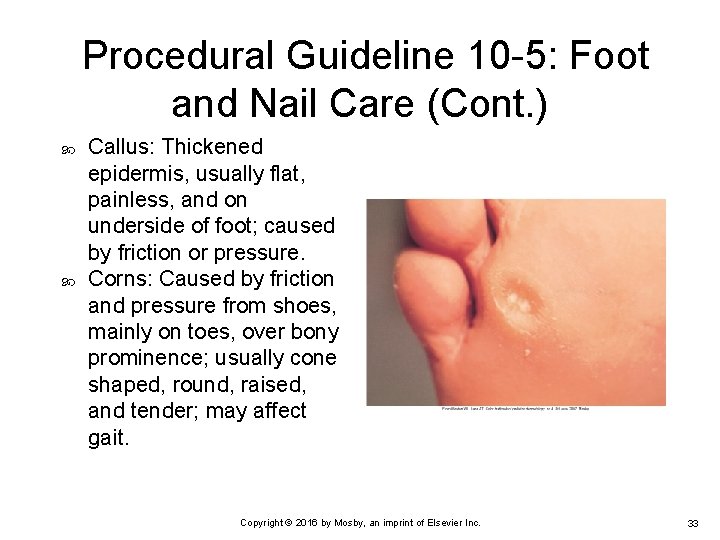
Procedural Guideline 10 -5: Foot and Nail Care (Cont. ) Callus: Thickened epidermis, usually flat, painless, and on underside of foot; caused by friction or pressure. Corns: Caused by friction and pressure from shoes, mainly on toes, over bony prominence; usually cone shaped, round, raised, and tender; may affect gait. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 33
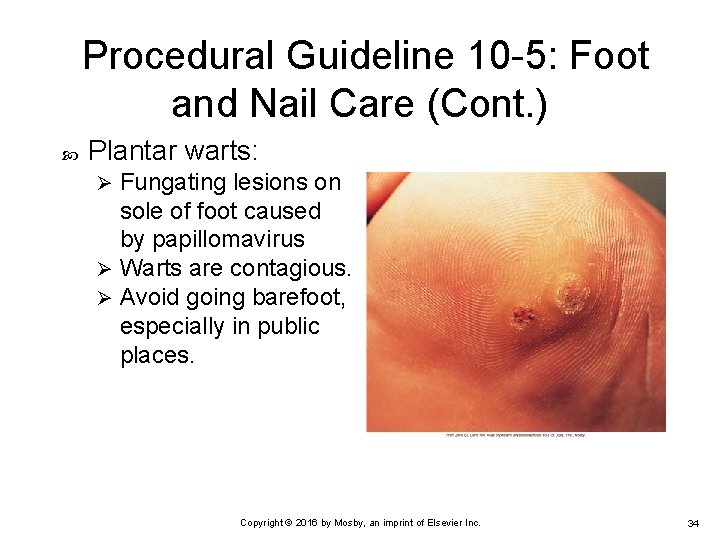
Procedural Guideline 10 -5: Foot and Nail Care (Cont. ) Plantar warts: Fungating lesions on sole of foot caused by papillomavirus Ø Warts are contagious. Ø Avoid going barefoot, especially in public places. Ø Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 34
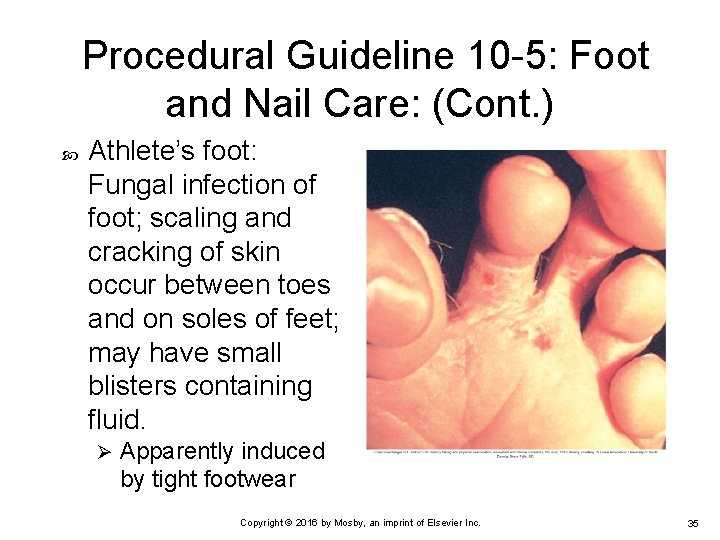
Procedural Guideline 10 -5: Foot and Nail Care: (Cont. ) Athlete’s foot: Fungal infection of foot; scaling and cracking of skin occur between toes and on soles of feet; may have small blisters containing fluid. Ø Apparently induced by tight footwear Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 35
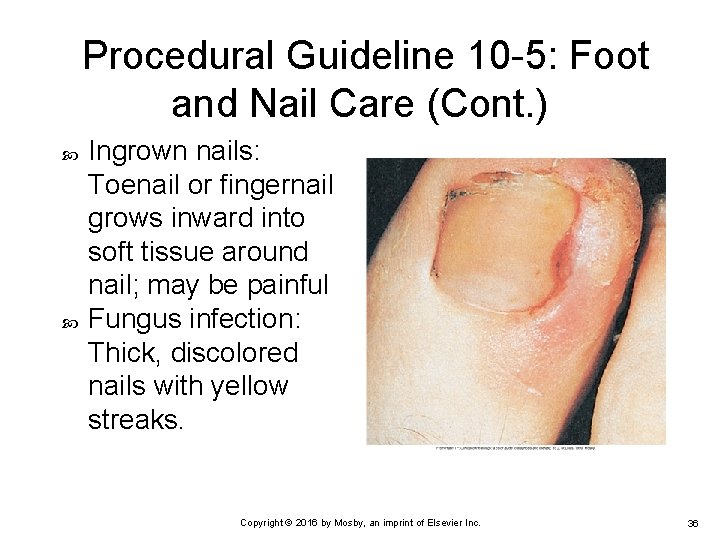
Procedural Guideline 10 -5: Foot and Nail Care (Cont. ) Ingrown nails: Toenail or fingernail grows inward into soft tissue around nail; may be painful Fungus infection: Thick, discolored nails with yellow streaks. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 36
Procedural Guideline 10 -5: Foot and Nail Care (Cont. ) Delegation and Collaboration The skill of foot and nail care may be delegated to nursing assistive personnel, except for patients with diabetes or patients with peripheral vascular disease or circulatory compromise. Ø The nurse instructs the NAP about: • Reporting any breaks in skin, redness, numbness, Ø swelling, or pain • Not trimming patient’s nails Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 37
Procedural Guideline 10 -6: Making an Occupied Bed The typical hospital bed consists of a firm mattress on a metal frame that you can raise or lower horizontally. The frame of the bed is divided into three sections so the operator can raise and lower the head and foot of the bed separately, in addition to inclining the entire bed with the head up or down. Each bed sits on four rollers or casters, which allows you to move the bed easily. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 38
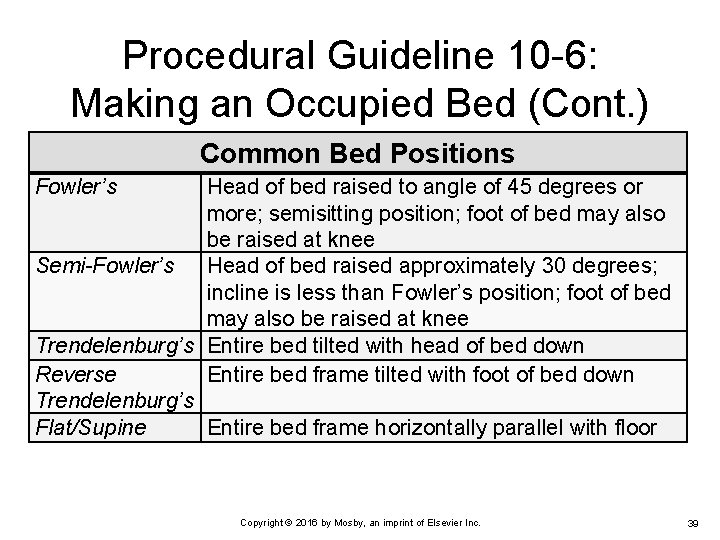
Procedural Guideline 10 -6: Making an Occupied Bed (Cont. ) Common Bed Positions Fowler’s Head of bed raised to angle of 45 degrees or more; semisitting position; foot of bed may also be raised at knee Semi-Fowler’s Head of bed raised approximately 30 degrees; incline is less than Fowler’s position; foot of bed may also be raised at knee Trendelenburg’s Entire bed tilted with head of bed down Reverse Entire bed frame tilted with foot of bed down Trendelenburg’s Flat/Supine Entire bed frame horizontally parallel with floor Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 39
Procedural Guideline 10 -6: Making an Occupied Bed (Cont. ) Bedmaking may be done with the patient out of the bed (unoccupied) or in the bed (occupied). Occupied bedmaking is limited to patients who cannot tolerate being out of bed. Ø Some patients have activity or positioning restrictions ordered by their health care provider; thus it is important to understand which position the patient can assume while the bed linens are changed. Ø Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 40
Procedural Guideline 10 -6: Making an Occupied Bed (Cont. ) If a patient experiences severe pain with movement, an analgesic administered 30 to 60 minutes before the procedure is helpful in controlling pain and maintaining comfort. Even though the patient is unable to get out of bed, encourage self-help if possible, which helps maintain the patient’s strength and mobility. Ø For example, depending on restrictions, the patient can turn, assist in moving up in bed, or hold top sheets while linen is applied. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 41

Procedural Guideline 10 -6: Making an Occupied Bed (Cont. ) Delegation and Collaboration The skill of bedmaking is delegated to nursing assistive personnel. Ø The nurse instructs the NAP about: • The patient’s activity or position restrictions • What to do if the patient becomes fatigued or short of Ø breath • Immediately reporting any unexpected concerns (e. g. , excess wound drainage, dislodged IV tubing) Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 42
Procedural Guideline 10 -7: Making an Unoccupied Bed An unoccupied bed is one left open with the top sheets fanfolded down. A postoperative surgical bed is prepared for patients returning from the operating room or procedural area. Ø The bed is left with the top sheets fanfolded lengthwise and not tucked in to facilitate the patient’s transfer from a stretcher. Ø A closed bed, which is made with the top sheets pulled up to the head of the bed, is used after a patient is discharged and housekeeping cleans the unit. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 43
Procedural Guideline 10 -7: Making an Unoccupied Bed (Cont. ) Delegation and Collaboration The skill of making an unoccupied bed can be delegated to nursing assistive personnel. Ø The nurse instructs the NAP about: • Use of special linen instructions if the patient is on an Ø airflow or specialty mattress. Copyright © 2016 by Mosby, an imprint of Elsevier Inc. 44
- Slides: 44