Changes to Breast Cancer Staging AJCC 8 th
Changes to Breast Cancer Staging, AJCC 8 th Ed Cancer Staging Manual/Challenges in Staging after Neoadjuvant Systemic Treatment David R. Byrd, MD Chair, AJCC Surgical Oncology, University of Washington/Seattle Cancer Care Alliance Seattle, WA Validating science. Improving patient care.
Disclosures • I have no financial disclosures relevant to this presentation • Member of the AJCC 8 th Ed Cancer Staging Manual editorial board • Chair, AJCC • I have a strong bias, FAVORING tumor registrars and their dedication. Copyright © 2013 AJCC All Rights Reserved

Staging – The Foundation of Cancer Care • Understanding the extent of cancer, its prognosis, and impact of therapy are central to personalized care; and to improving cancer impact on society • Staging is the common language of cancer care – Clinical care • • Define extent and prognosis of cancer Guide appropriate treatment Basis for Guidelines NCCN Guidelines all base recommendations on cancer stage – Communicate among users about groups of patients • Population impact of cancer; Changes over time • Group similar cases for clinical trials Copyright © 2013 AJCC All Rights Reserved
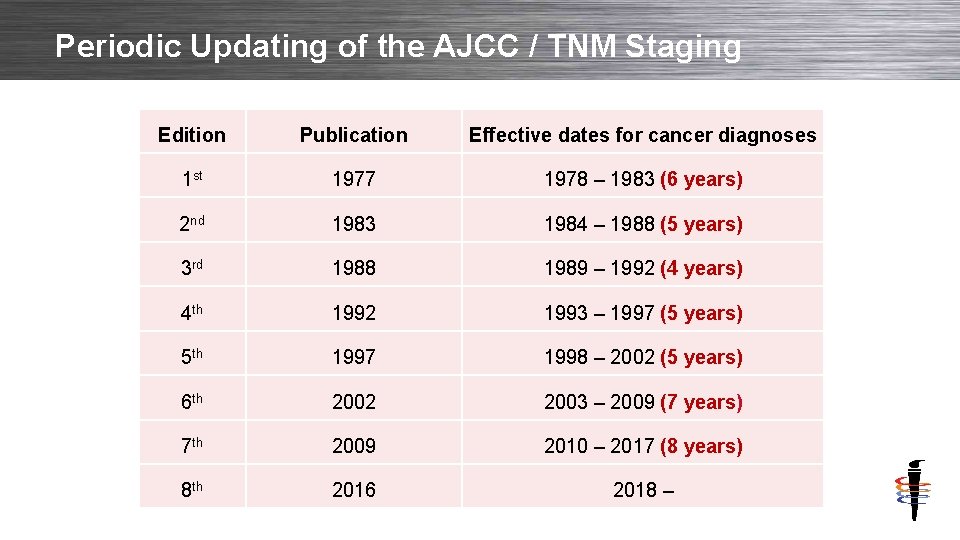
Periodic Updating of the AJCC / TNM Staging Edition Publication Effective dates for cancer diagnoses 1 st 1977 1978 – 1983 (6 years) 2 nd 1983 1984 – 1988 (5 years) 3 rd 1988 1989 – 1992 (4 years) 4 th 1992 1993 – 1997 (5 years) 5 th 1997 1998 – 2002 (5 years) 6 th 2002 2003 – 2009 (7 years) 7 th 2009 2010 – 2017 (8 years) 8 th 2016 2018 – Copyright © 2013 AJCC All Rights Reserved

Key Elements and Terminology of Staging • STAGE: The aggregate information resulting from T, N, M – Anatomic groups – Anatomy only – Prognostic stage groups – Anatomy PLUS key non-anatomic factors • Categories: The individual information on –T –N –M – There is no such thing as “T-Stage” or “N-Stage” – they are categories Copyright © 2013 AJCC All Rights Reserved

T, N, M categories: Breast Cancer Example Category Description Tx Primary tumor cannot be assessed Category Description T 0 No evidence of primary tumor NX Regional nodes cannot be assessed Tis Carcinoma in situ (DCIS) N 0 No regional node spread N 1 mi Regional node spread; <0. 2 mm T 1 mi Tumor < 0. 1 cm T 1 a Tumor >0. 1 – 0. 5 cm N 1 1 – 3 positive regional nodes T 1 b Tumor >0. 5 – 1. 0 cm N 2 4 – 9 positive regional nodes T 1 c Tumor >1. 0 – 2. 0 cm N 3 T 2 Tumor >2. 0 – 5. 0 cm T 3 Tumor >5. 0 cm T 4 Tumor invades chest wall or skin >10 positive regional node Infraclavicular nodes Supraclavicular nodes Positive axillary and internal mammary nodes Category Copyright © 2013 AJCC All Rights Reserved Description M 0 No distant metastases M 1 Distant metastases present (There is no MX category in any TNM staging

Stage: Groups Based on T, N, M • Stage Groups defined by combinations of T, N and M for patients with generally similar prognosis • Prognostic Stage Groups defined by similar groups of T, N, M + selected non-anatomic factors • In general: – – – Stage 0 Stage III Stage IV Copyright © 2013 AJCC All Rights Reserved non-invasive cancer Small cancers; node negative Larger/more extensive plus/minus positive nodes Larger/extensive; increasing extent of positive nodes Cancers with distant metastases

Staging Classifications – Time Points of Staging • Clinical – Before initiation of treatment: prefix ”c” – c. T, c. N – All information from history, physical examination and imaging – Whatever is available – advanced imaging NOT required • Pathological – Clinical information – PLUS results of surgery (if surgery initial treatment): prefix p. T, p. N • Post-therapy (post-neoadjuvant) – Clinical or pathologic information after completion of systemic or radiation therapy if this treatment precedes / replaces surgery: prefix yc. T; yc. N, prefix yp. T; yp. N if surgery then performed • Less Commonly Used: – Recurrent – Extent of disease at recurrence: prefix r. T, r. N – Autopsy – For cancer identified only at autopsy Copyright © 2013 AJCC All Rights Reserved

Understanding Stage Classifications Pathological – p* Clinical - c Date of Diagnosis Clinical - c Diagnostic Workup – Hx and Phys exam, imaging, bx Surgical Treatment Pathology Report Systemic or Radiation Therapy Evaluation by imaging & physical exam Posttherapy - yc Posttherapy - yp • Includes post-surgery imaging if within 4 months of Dx; the. Reserved absence of disease progression or systemic Rx or RT Copyright © 2013 AJCCin All Rights Surgical Treatment Pathology Report

Key Important Rule in Assigning Stage: The Role of the Managing Physician • Staging requires collaborative effort for information from many professionals • Assigning stage requires synthesis of information from an array of many sources – History and Physical – Imaging; Pathology; Biopsy and diagnostic procedures – Surgical findings (beyond pathology report - e. g. status of other organs; invasion of local structures) • Managing Physician (NOT pathologist / radiologist) assigns the final cancer stage – Pathologist and radiologist provide important information to help assign stage related to T-, N -, and M- categories from the data they have available – BUT it is the managing physician who must synthesize all this information and make the final assignment of the clinical, pathological and post-therapy stage. Copyright © 2013 AJCC All Rights Reserved

Anatomic Stage is Key Predictor of Breast Cancer Outcome: The National Cancer Data Base 10‐year survey of breast carcinoma treatment at hospitals in the US Copyright © 2013 AJCC All Rights Reserved Cancer; Volume 83, Issue 6, pages 1262 -1273
Staging Needs to Be Relevant to Practice • Anatomic staging valuable but not always sufficient – Many cancer types do not have validated non-anatomic factors to modify anatomic state – Advanced cancer characterization and biomarker determination not available in many parts of the world • Providers use other information – Biomarkers / subtypes – Genomic profiling – Specific molecular targets • “Staging” must incorporate new information beyond anatomy to remain relevant and useful Copyright © 2013 AJCC All Rights Reserved

Evolution of Anatomic to AJCC “Prognostic” Staging • Non-anatomic factors in AJCC TNM sinception – Soft tissue sarcoma – grade included in 1 st Edition AJCC Manual – Bone – grade including in 2 nd Edition AJCC Manual – Thyroid – Age and histologic type included in 2 nd Edition Manual • Beginning in the 6 th and 7 th Editions of AJCC Staging, marked increase in use of non-anatomic factors incorporated to defining Stage Groups • Non-anatomic factors used primarily to modify anatomic stage • Maintain ability to derive pure anatomic stage – Comparisons over time – Allow use of stage around the world as the common language of cancer – even where it is not possible to obtain non-anatomic information Copyright © 2013 AJCC All Rights Reserved

AJCC Vision – Evolution to Prognostic Staging The Transition from Population Based to a more “Personalized” Approach Cancer Stage AJCC/UICC TNM Stage (Basic Classification) AJCC Prognostic Stage Groups Comprehensive Cancer Profile TNM (Advanced Clinical Relevance) AJCC “Personalized” (Advanced Clinical + Personalized Relevance) TNM + Prognostic Factors Population Survival Outcomes Copyright © 2013 AJCC All Rights Reserved + Risk Assement Models + Clinical Trial Stratification Personalized Survival Outcomes

The 8 th Edition Published Late 2016 Breast Updated November 2017 Effective for Cases Dx’d 1/1/2018

American Joint Committee on Cancer (AJCC) 8 th ed. Editorial Board Strategy • Maintain anatomic extent of disease - TNM foundation • Incorporate evidence-based nonanatomic factors, including molecular markers • Era of precision medicine evolution from a “population based” to a “more personalized” approach TNM - Anatomic Extent of Disease Evaluate site-specific prognostic & predictive factors Link to “AJCC Approved” Predictive/prognostic risk calculating tools • “One size fits all” model does not exist AJCC Cancer Staging Manual. 8 th Ed. New York: Springer; 2017 Copyright © 2013 AJCC All Rights Reserved Adapted from Mahul Amin
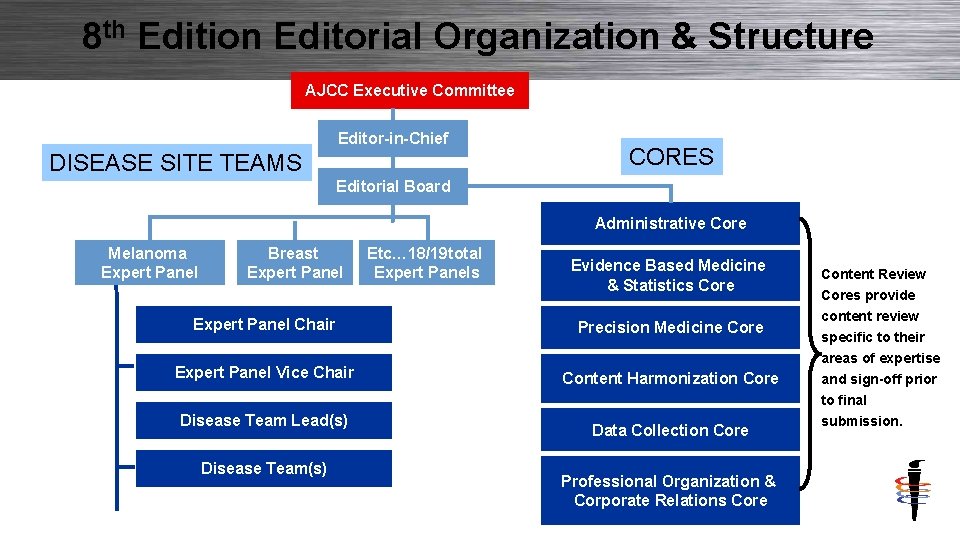
8 th Edition Editorial Organization & Structure AJCC Executive Committee Editor-in-Chief DISEASE SITE TEAMS CORES Editorial Board Administrative Core Melanoma Expert Panel Breast Expert Panel Etc… 18/19 total Expert Panels Evidence Based Medicine & Statistics Core Expert Panel Chair Precision Medicine Core Expert Panel Vice Chair Content Harmonization Core Disease Team Lead(s) Disease Team(s) Copyright © 2013 AJCC All Rights Reserved Data Collection Core Professional Organization & Corporate Relations Core Content Review Cores provide content review specific to their areas of expertise and sign-off prior to final submission.

Limitations of Anatomic Staging • Anatomic stage alone does not meet the needs of patients • Rapid evolution in understanding cancer biology has made other factors beyond anatomy as or MORE important in defining prognosis; and in defining optimal therapy Copyright © 2013 AJCC All Rights Reserved
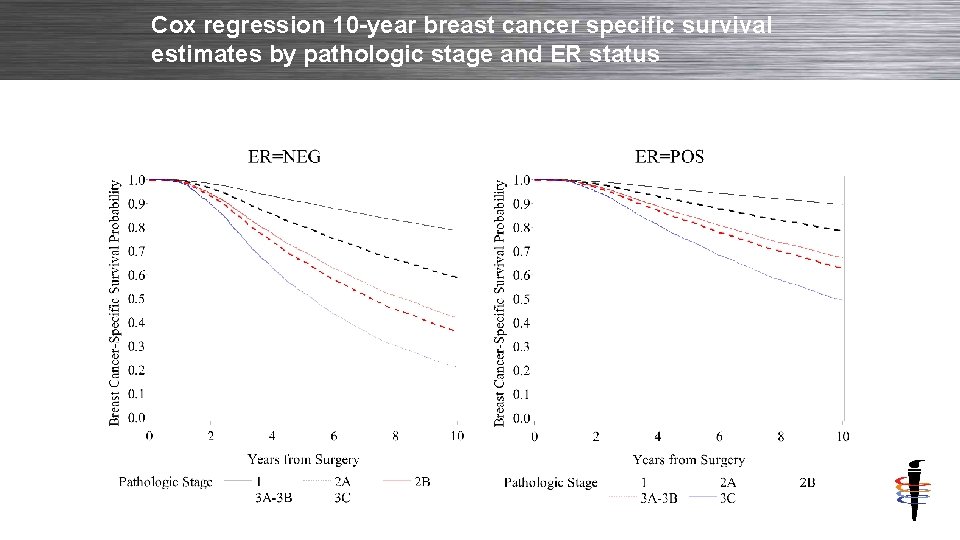
Cox regression 10 -year breast cancer specific survival estimates by pathologic stage and ER status Copyright © 2013 AJCC All Rights Reserved
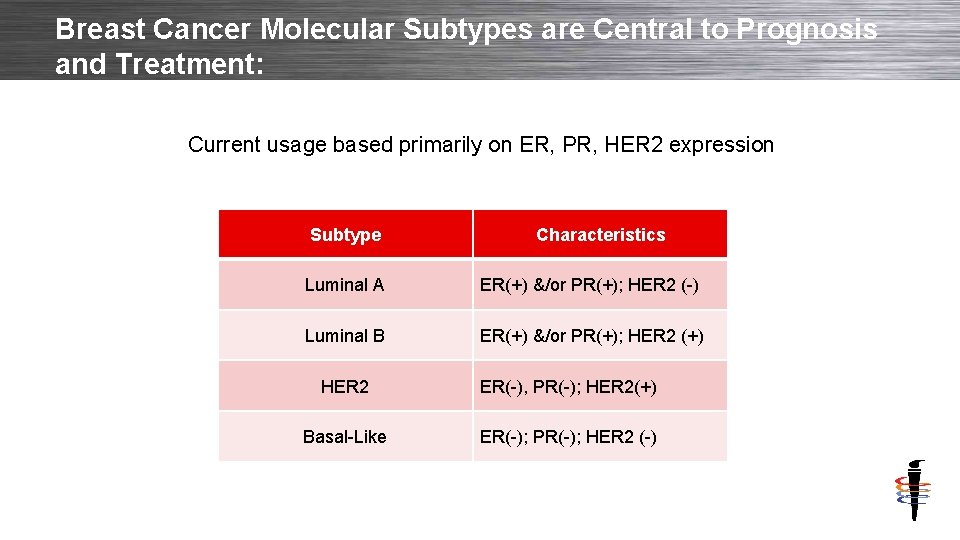
Breast Cancer Molecular Subtypes are Central to Prognosis and Treatment: Current usage based primarily on ER, PR, HER 2 expression Subtype Copyright © 2013 AJCC All Rights Reserved Characteristics Luminal A ER(+) &/or PR(+); HER 2 (-) Luminal B ER(+) &/or PR(+); HER 2 (+) HER 2 ER(-), PR(-); HER 2(+) Basal-Like ER(-); PR(-); HER 2 (-)

Breast Cancer Survival by Subtype Copyright © 2013 AJCC All Rights Reserved Knutsvik G, Stefansson IM, Aziz S, Arnes J, Eide J, Collett K, Akslen LA - PLo. S ONE (2014)
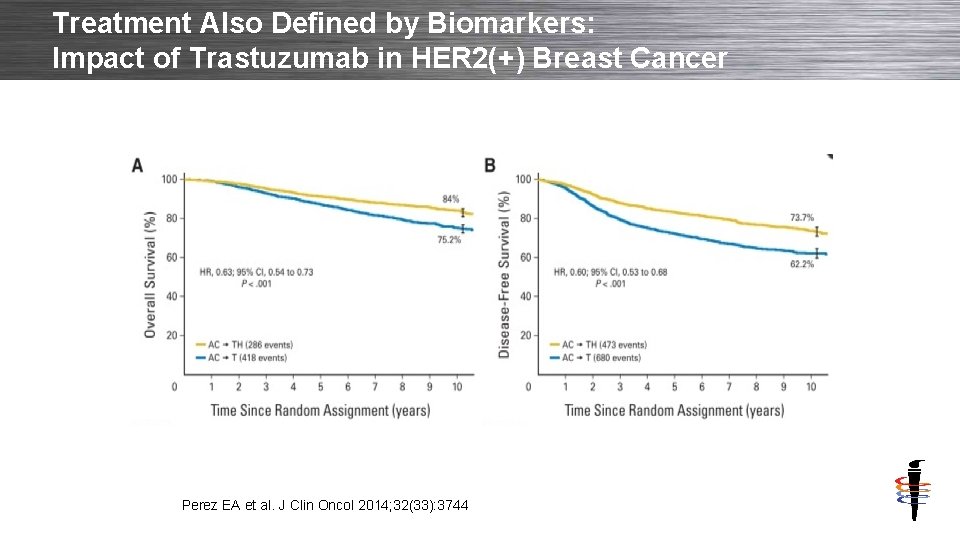
Treatment Also Defined by Biomarkers: Impact of Trastuzumab in HER 2(+) Breast Cancer Perez EA et al. J Clin Oncol 2014; 32(33): 3744 Copyright © 2013 AJCC All Rights Reserved
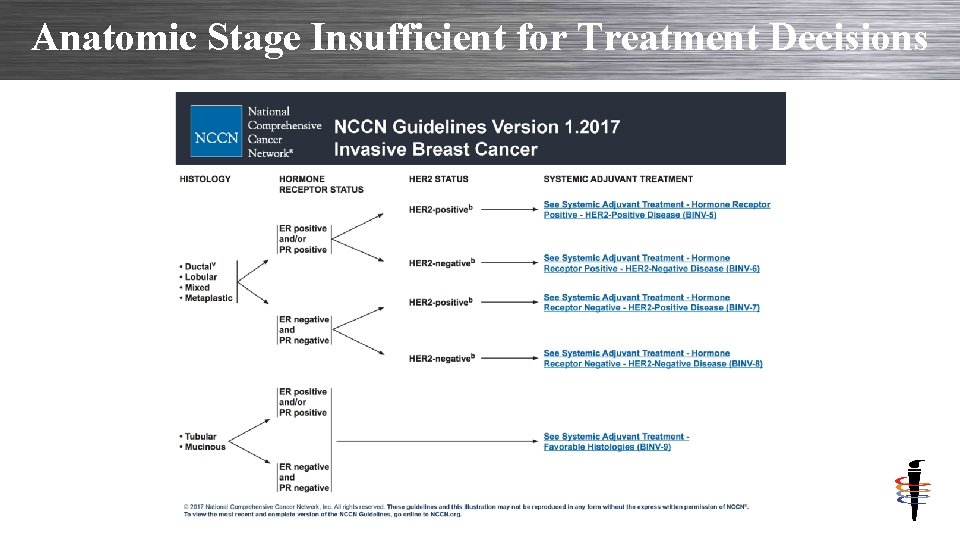
Anatomic Stage Insufficient for Treatment Decisions Copyright © 2013 AJCC All Rights Reserved
Major Changes in Breast Cancer Staging with 8 th Edition • Lobular carcinoma in situ (LCIS) no longer included in AJCC Staging – LCIS is a “benign” entity and not cancer – Should not be in a cancer staging system – Issue with “pleomorphic” LCIS – but insufficient data available • Prognostic Staging – Incorporation of Grade, HER 2, ER, PR • Incorporation of genomic profiling to assign pathological prognostic stage group Copyright © 2013 AJCC All Rights Reserved

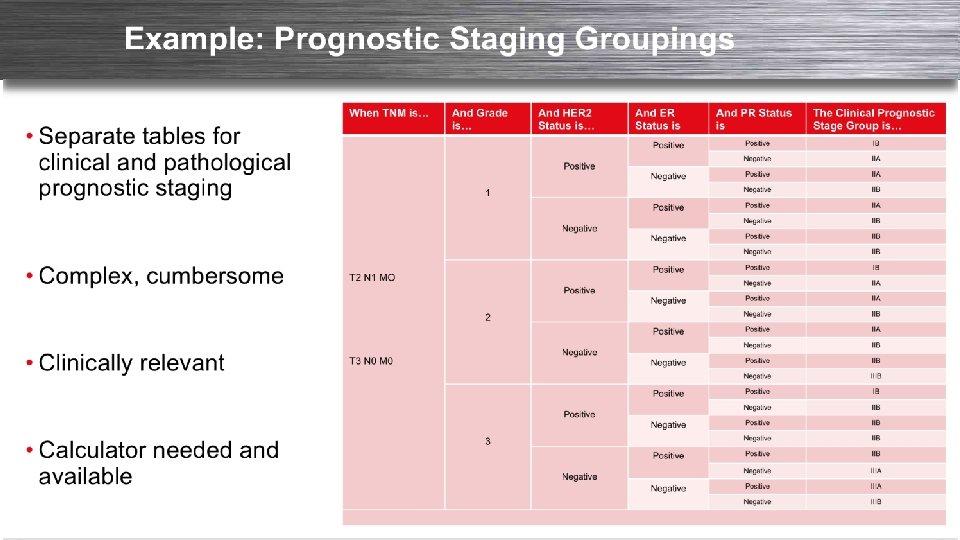
Evolution to Prognostic Staging: Breast Cancer • The AJCC 8 th Edition Breast Staging incorporates key prognostic factors into the primary staging – Anatomic stage groups still maintained • Clinical Stage • When biomarkers not available. • “Prognostic Stage” will the primary stage recorded in cancer registries in the United States • Requires: – T; N; M – Grade; HER 2; Estrogen Receptor; Progesterone Receptor – Genomic profiles (Oncotype. Dx™) as appropriate Copyright © 2013 AJCC All Rights Reserved
Evolution to Prognostic Staging: Breast Cancer • The AJCC 8 th Edition Breast Staging incorporates key prognostic factors into the primary staging – Anatomic stage groups still maintained for use in areas of world where biomarkers are not available. • “Prognostic Stage” will the primary stage recorded in cancer registries in the United States – Decision made on 2 separate studies • E Mittendorf – Using MDACC dat • DJ Winchester – Using NCDB – Final changes based on NCDB analysis • Requires: – T; N; M – Grade; HER 2; Estrogen Receptor; Progesterone Receptor Copyright © 2013 AJCC All Rights Reserved
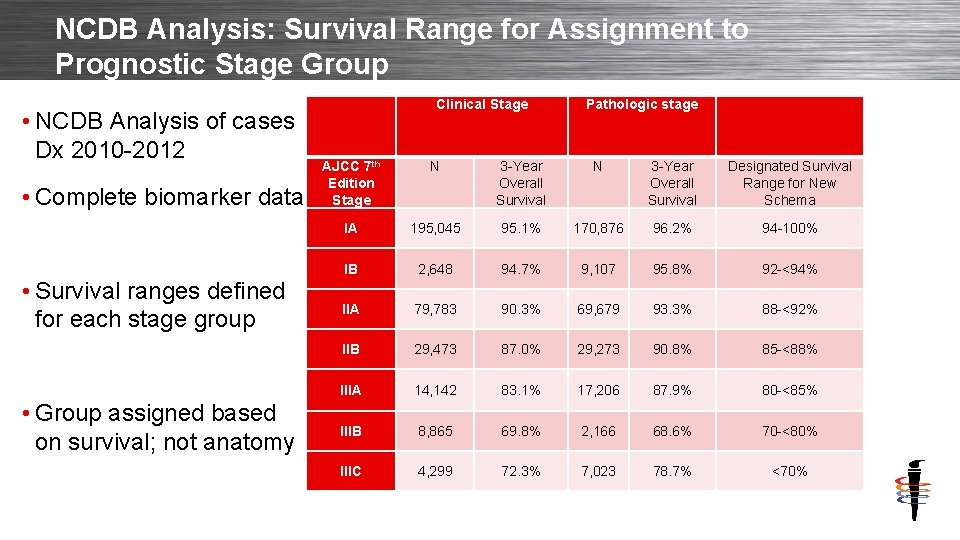
NCDB Analysis: Survival Range for Assignment to Prognostic Stage Group • NCDB Analysis of cases Dx 2010 -2012 • Complete biomarker data • Survival ranges defined for each stage group • Group assigned based on survival; not anatomy Copyright © 2013 AJCC All Rights Reserved Clinical Stage Pathologic stage AJCC 7 th Edition Stage N 3 -Year Overall Survival Designated Survival Range for New Schema IA 195, 045 95. 1% 170, 876 96. 2% 94 -100% IB 2, 648 94. 7% 9, 107 95. 8% 92 -<94% IIA 79, 783 90. 3% 69, 679 93. 3% 88 -<92% IIB 29, 473 87. 0% 29, 273 90. 8% 85 -<88% IIIA 14, 142 83. 1% 17, 206 87. 9% 80 -<85% IIIB 8, 865 69. 8% 2, 166 68. 6% 70 -<80% IIIC 4, 299 72. 3% 7, 023 78. 7% <70%
Copyright © 2013 AJCC All Rights Reserved
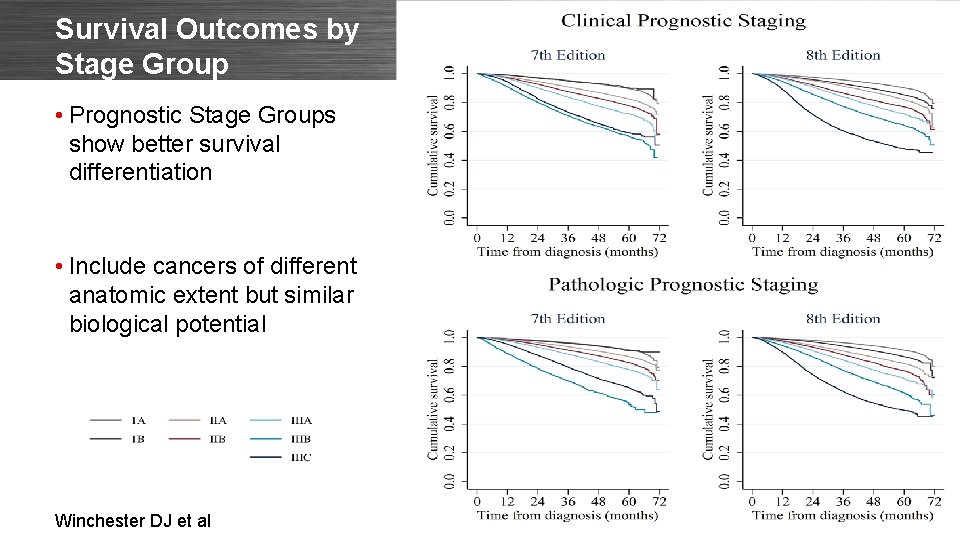
Survival Outcomes by Stage Group • Prognostic Stage Groups show better survival differentiation • Include cancers of different anatomic extent but similar biological potential Winchester DJ et al Copyright © 2013 AJCC All Rights Reserved
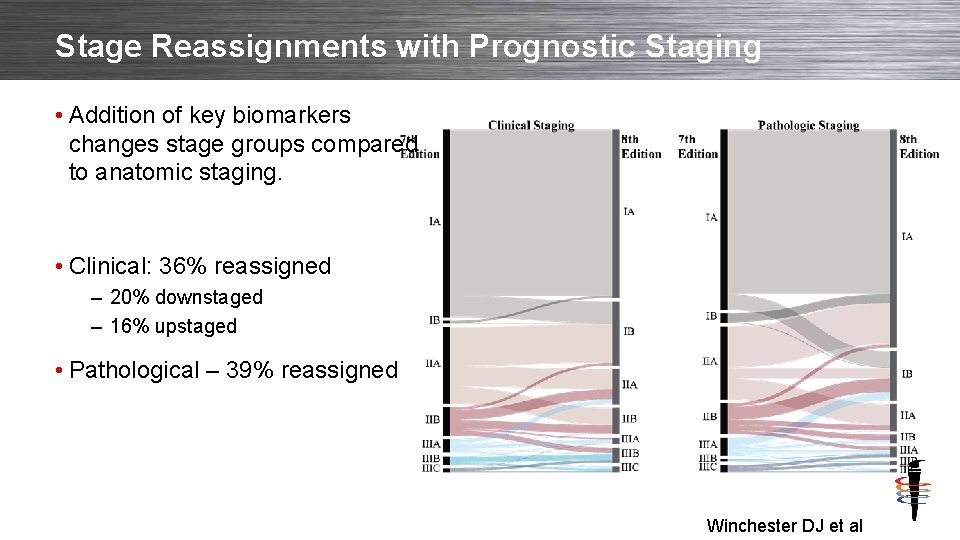
Stage Reassignments with Prognostic Staging • Addition of key biomarkers changes stage groups compared to anatomic staging. • Clinical: 36% reassigned – 20% downstaged – 16% upstaged • Pathological – 39% reassigned Copyright © 2013 AJCC All Rights Reserved Winchester DJ et al
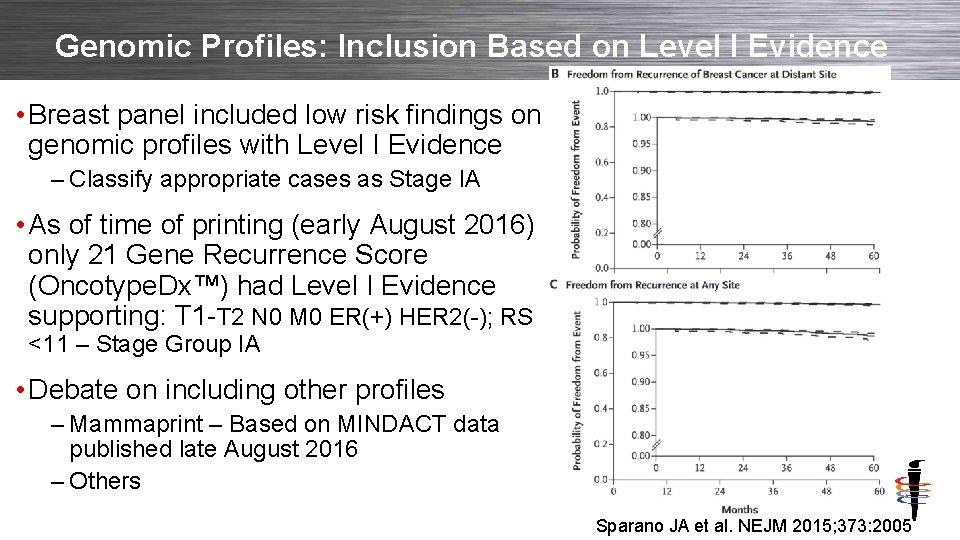
Genomic Profiles: Inclusion Based on Level I Evidence • Breast panel included low risk findings on genomic profiles with Level I Evidence – Classify appropriate cases as Stage IA • As of time of printing (early August 2016) only 21 Gene Recurrence Score (Oncotype. Dx™) had Level I Evidence supporting: T 1 -T 2 N 0 M 0 ER(+) HER 2(-); RS <11 – Stage Group IA • Debate on including other profiles – Mammaprint – Based on MINDACT data published late August 2016 – Others Copyright © 2013 AJCC All Rights Reserved Sparano JA et al. NEJM 2015; 373: 2005
Selection of Genomic Profiles for Use in Clinical Care The AJCC determined to include Oncotype. Dx in assigned Stage IA to T 1 -2 N 0 ER+ HER 2 - RS<11; but recognizes that other profiles may be useful in clinical management. The AJCC Manual is NOT a practice guideline and the Expert Panel is NOT a guideline developer. Physicians are to use the best information available at the time to plan treatment, including the determination to use (one or several) genomic panels, and which genomic panel to select. Copyright © 2013 AJCC All Rights Reserved

Survival for Locally Advanced Cancer: Anatomic vs. 8 th Edition Prognostic - SEER • Cases of LABC defined by AJCC 7 • 10, 053 cases • 74% changed stage • Survival by – AJCC 7 – Prognostic AJCC 8 Wang M et al. The Breast 2018; 37: 56 -63 Copyright © 2013 AJCC All Rights Reserved Anatomic – AJCC 7 Prognostic – AJCC 8

Post Neoadjuvant Therapy Classification
AJCC 8 th Edition Staging: 1 -Page Guide POST NEOADJUVANT THERAPY STAGING CLASSIFICATION RULES • yc Clinical – Includes physical exam and imaging assessment – After neoadjuvant systemic/radiation therapy • yp Pathological – Includes all information from yc staging, – Surgeon’s operative findings and – Pathology report from resected specimen Copyright © 2013 AJCC All Rights Reserved
Post Neoadjuvant Therapy Staging • Assigned after neoadjuvant therapy and surgical resection • yp. T category – Largest focus of residual tumor – Treatment-related fibrosis near invasive tumor NOT used – Multiple foci of residual tumor, use (m) • yp. N category – Largest focus of residual tumor in nodes – Treatment-related fibrosis near nodal tumor deposits NOT used • M category – If M 1 prior to therapy, remains M 1 following neoadjuvant therapy – Regardless of observed response to therapy • Assign degree of response to therapy Copyright © 2013 AJCC All Rights Reserved
Stage Groups • Stage groups assigned using available tables in chapter • If no label on stage group table, use for – Clinical (c) – Pathological (p) or posttherapy (yp) • If stage group table is labeled, use as follows – Clinical group table used for c and yc – Pathological group table used for p and yp – IF posttherapy group table available • Use for yp and yc • Do NOT use p table Copyright © 2013 AJCC All Rights Reserved
Stage Group Exceptions Breast – Clinical stage group table – Pathological stage group table – NO stage group assignment for posttherapy (yp) • Must record yp. T yp. N c. M Grade Copyright © 2013 AJCC All Rights Reserved
Neoadjuvant Response • c. T 2 c. N 1 c. M 0 invasive ductal breast cancer. Neoadjuvant chemo 6 cycles followed by MRM w/axillary dissection. Pathology report is no residual tumor, nodes negative. • Neoadjuvant therapy destroyed all tumor, complete pathological response • yp. T 0 yp. N 0 c. M 0 stage 99 • Entered into new data item for posttherapy staging • Reminder - must meet criteria for neoadjuvant Copyright © 2013 AJCC All Rights Reserved
Neoadjuvant No Response • 4. 1 cm breast tumor c. T 2 c. N 0. Neoadjuvant chemo 6 months. Post chemo imaging 6. 5 cm yc. T 3, no response. Surgical resection path 7. 7 cm, yp. T 3 yp. N 0. • Assign posttherapy yp staging yp. T 3 yp. N 0 c. M 0 • Some patients do not respond to neoadjuvant therapy • Analysis on response – – If no data on cases not responding to neoadjuvant therapy Data would only show cases that responded Result in skewed analysis Would not know effectiveness of neoadjuvant therapy & risk Copyright © 2013 AJCC All Rights Reserved
Posttherapy Classification Assignment • Posttherapy classification assigned regardless of response • Always assign yp. T yp. N c. M – Does NOT depend on response to treatment – Even if pt responds completely, no evidence of tumor – Even if pt has partial response, tumor or nodes shrink – Even if pt did not respond, tumor/nodes stayed the same – Even if pt did not respond, tumor/nodes grew while on treatment • Not considered progression that stops staging • Not considered progression that makes surgery subsequent treatment Copyright © 2013 AJCC All Rights Reserved

Colorectal Staging Tables – 8 th Ed AJCC Cancer Staging Manual. 8 th Ed. New York: Springer; 2017 Copyright © 2013 AJCC All Rights Reserved
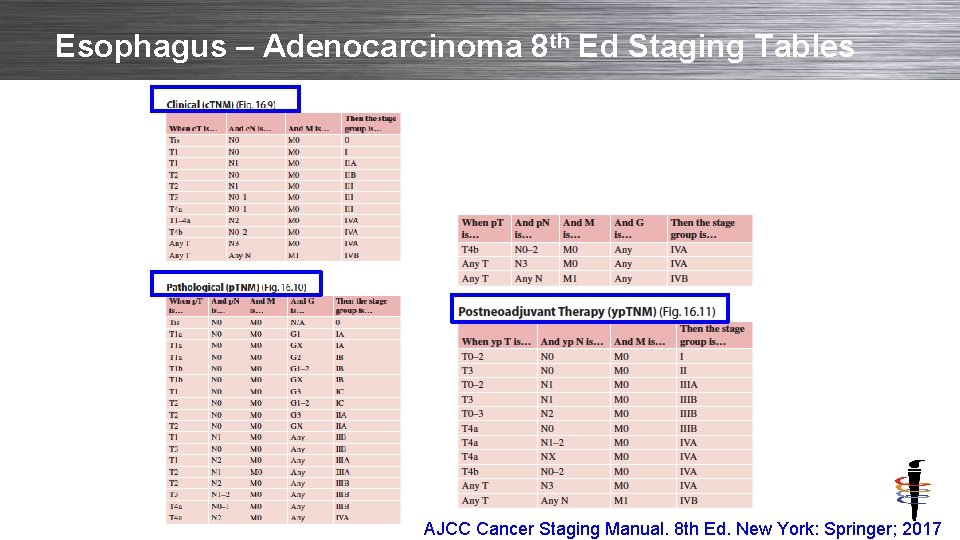
Esophagus – Adenocarcinoma 8 th Ed Staging Tables Copyright © 2013 AJCC All Rights Reserved AJCC Cancer Staging Manual. 8 th Ed. New York: Springer; 2017

Selecting Stage Group
Selecting Appropriate Stage Group Table: Anatomic Groups Not Used If Biomarker available • Anatomic Stage Groups • Appropriate for regions of world where biomarkers cannot be routinely obtained – Based solely on anatomic extent of cancer – Defined only by T, N, and M categories • Not appropriate where biomarkers are used for patient care Copyright © 2013 AJCC All Rights Reserved
Selecting Appropriate Stage Group Table – Prognostic Staging for all Patients where Biomarker available • Clinical and Pathological Prognostic Stage Groups – Based on populations of breast cancer patients offered and mostly treated with endocrine and/or chemotherapy and/or anti-HER 2 therapy – Includes T, N, M, tumor grade, HER 2, ER, PR – Includes multi-gene panels – Can be based on clinical or pathological findings • Necessary for patient care • Must be used for reporting of all cancer patients in U. S. Copyright © 2013 AJCC All Rights Reserved
Implementing Prognostic Stage in Practice Cannot memorize tables!!
8 th Edition API • License and deliver content professional organizations that need to update their products based on AJCC content – – – UICC: TNM + Stage groups for TNM manual CAP: cancer protocols NCCN: clinical practice guidelines ASCO: Cancer. Lin. Q American Cancer Society: patient education Standard setters and registry software developers • Content being made available to vendors through API (currently being validated by registry vendors) Copyright © 2013 AJCC All Rights Reserved
Incorporation into Daily Work Flow • Staging must be incorporated into EHR’s • Electronic data capture of key elements to present to managing physician to define final stage assignment • Integrate with oncology care pathways to define therapy • Include biologic / genomic data for individual cases • Incorporate into tools to assist patients with understanding and assisting with treatment decisions Copyright © 2013 AJCC All Rights Reserved
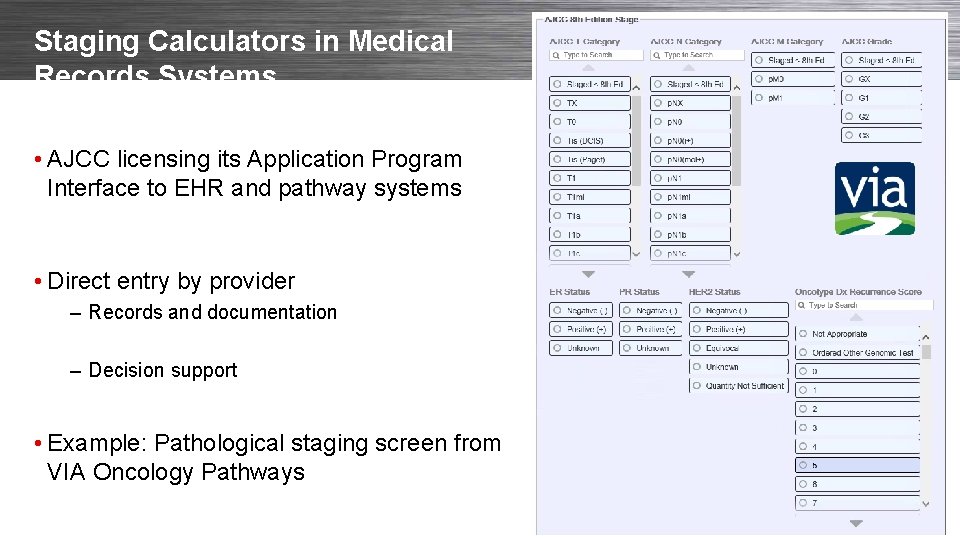
Staging Calculators in Medical Records Systems • AJCC licensing its Application Program Interface to EHR and pathway systems • Direct entry by provider – Records and documentation – Decision support • Example: Pathological staging screen from VIA Oncology Pathways Copyright © 2013 AJCC All Rights Reserved

Two Staging Calculators – Available at App Store * I am not endorsing nor have any interest in any software tool TNM 8 Breast Cancer Calculator Copyright © 2013 AJCC All Rights Reserved Breast cancer Staging TNM 8 Integrated Cancer Research Ltd
Implications for Future for Staging? • Today: Must rapidly develop better tools for clinicians and patients; • Staging as we see it now will change dramatically – Biology – Diversity of cancer – Ultimately with individualization of prognosis and therapy • We will still need these tools to maintain robust data systems for patient care and counseling, population study and clinical research Copyright © 2013 AJCC All Rights Reserved
Electronic Updates • Rolling Updates (based on literature review and continuous engagement of panels) – Prognostic factors for clinical use – Emerging Factors for Clinical Care – Risk Assessment Models for additional cancers Copyright © 2013 AJCC All Rights Reserved
Conclusions • Major change to include biomarkers in AJCC Staging • Clearly necessary; improves value to patients and providers • Complex – requires calculator tools to apply in practice • Stage concepts and tools must evolve in the era of personalized medicine • AJCC committee to ongoing improvement and to supporting patient and providers Copyright © 2013 AJCC All Rights Reserved
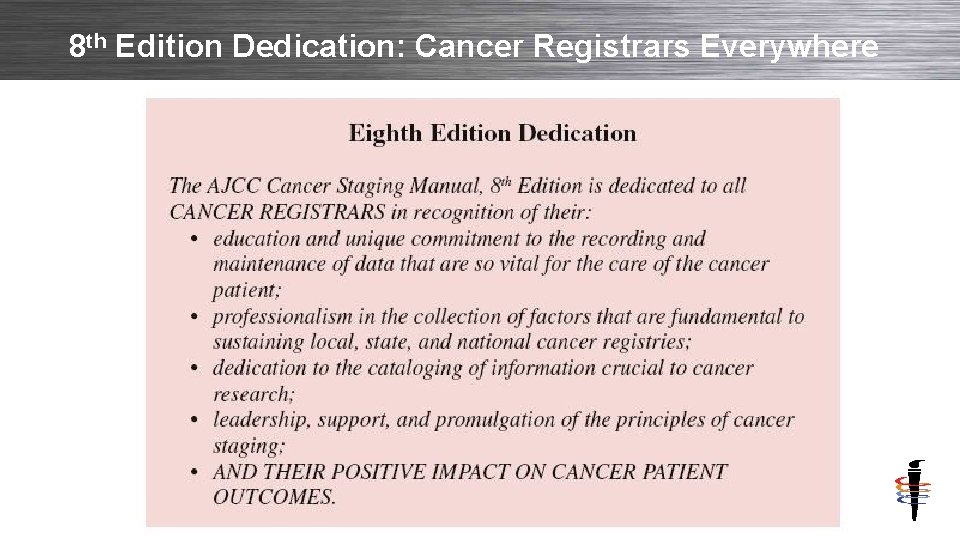
8 th Edition Dedication: Cancer Registrars Everywhere Copyright © 2013 AJCC All Rights Reserved
- Slides: 55