Challenges to Device Innovation Atrial Appendage Closure Devices





- Slides: 14

Challenges to Device Innovation: Atrial Appendage Closure Devices Patient Selection - FDA View Andrew Farb, MD Division of Cardiovascular Devices Center for Devices and Radiological Health (CDRH) andrew. farb@fda. hhs. gov FDA Town Hall II CRT 2012 Washington, DC February 7, 2012
Andrew Farb, MD I have no real or apparent conflicts of interest to report.
Non-Valvular Atrial Fibrillation Significant public health problem Most common cardiac arrhythmia requiring medical intervention Increasing in prevalence, particularly with advancing age of population Independently associated with mortality in numerous observational studies Important cause of ischemic stroke and peripheral thromboembolism

AFib and Stroke Risk of stroke determined by risk factors CHADS 2 score, CHA 2 DS 2 -VASc score and ACC/AHA/ESC Practice guidelines useful to identify patients at incresead risk of stroke and for whom oral anticoagulation therapy is indicated Warfarin, dabigatran, rivaroxaban Based on available data on the location of thrombus in AFib patients with stroke, occlusion of the LAA orifice represents a plausible intervention to prevent stroke
Study Design Considerations for LAA Occlusion Devices Patient populations Subjects indicated for oral anticoagulation (OAC) therapy and suitable for long-term treatment Subjects for whom OAC therapy indicated but unsuitable for long-term treatment
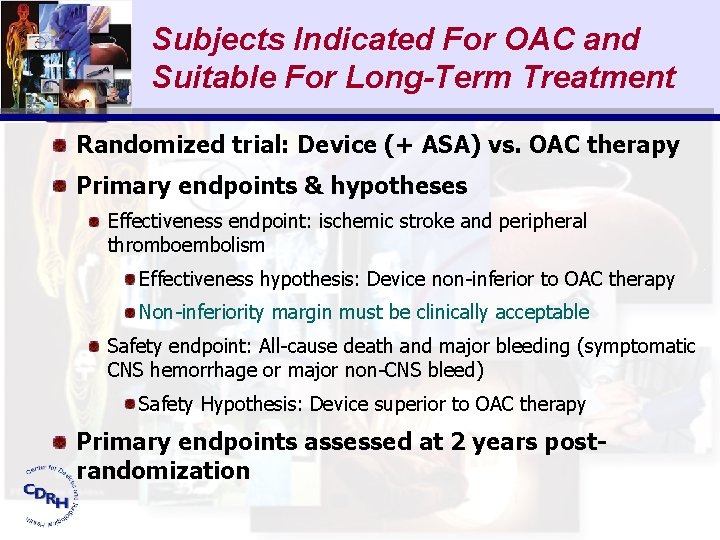
Subjects Indicated For OAC and Suitable For Long-Term Treatment Randomized trial: Device (+ ASA) vs. OAC therapy Primary endpoints & hypotheses Effectiveness endpoint: ischemic stroke and peripheral thromboembolism Effectiveness hypothesis: Device non-inferior to OAC therapy Non-inferiority margin must be clinically acceptable Safety endpoint: All-cause death and major bleeding (symptomatic CNS hemorrhage or major non-CNS bleed) Safety Hypothesis: Device superior to OAC therapy Primary endpoints assessed at 2 years postrandomization

Major Secondary Endpoint Procedural or device-related major adverse events Procedure-related death Pericardial effusion requiring treatment Device embolization Major access site hemorrhage Damage to cardiac or major non-cardiac cardiovascular structures Hypothesis: Event rate < performance goal based on a literature review of procedures with similar types of complications

Device Arm Success Secondary Endpoints In-hospital success: Successful device placement without in-hospital device or procedure-related major adverse events Day 45 clinical success: In-hospital procedure success, closure of LAA at Day 45 TEE, no ischemic stroke or peripheral thromboembolism, and discontinuation of OAC Long-term clinical success: Same as Day 45 (without temporary OAC re-start) evaluated at last available followup. Composite clinical success: Long-term clinical success and the absence device or procedure-related major adverse events
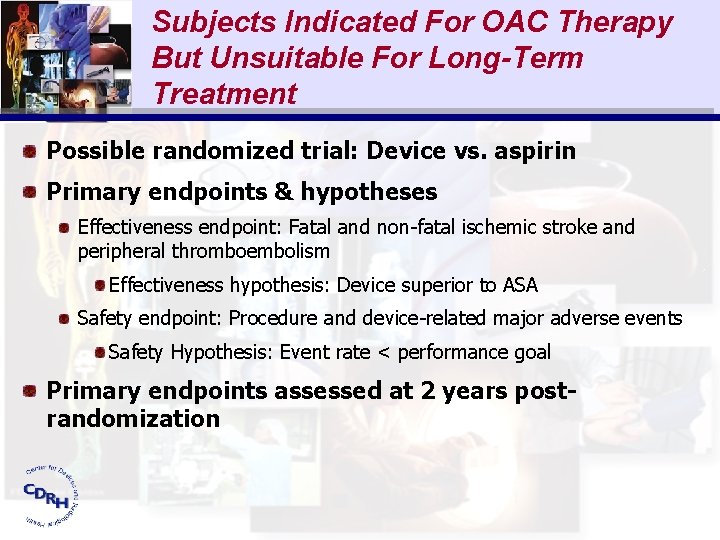
Subjects Indicated For OAC Therapy But Unsuitable For Long-Term Treatment Possible randomized trial: Device vs. aspirin Primary endpoints & hypotheses Effectiveness endpoint: Fatal and non-fatal ischemic stroke and peripheral thromboembolism Effectiveness hypothesis: Device superior to ASA Safety endpoint: Procedure and device-related major adverse events Safety Hypothesis: Event rate < performance goal Primary endpoints assessed at 2 years postrandomization
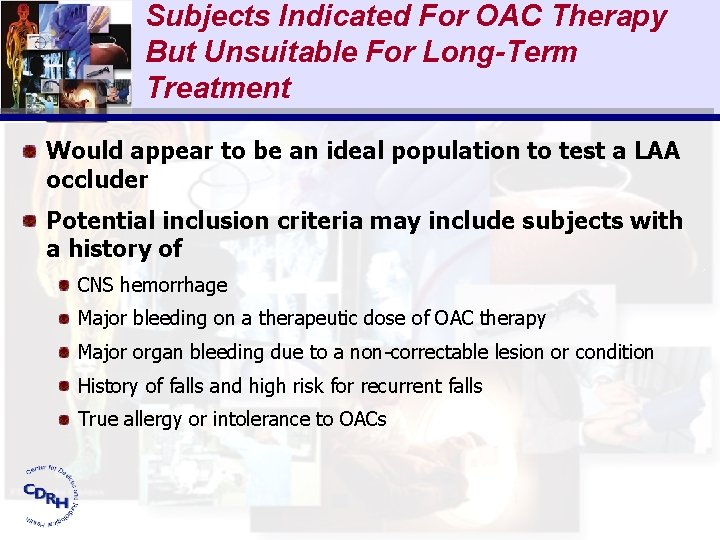
Subjects Indicated For OAC Therapy But Unsuitable For Long-Term Treatment Would appear to be an ideal population to test a LAA occluder Potential inclusion criteria may include subjects with a history of CNS hemorrhage Major bleeding on a therapeutic dose of OAC therapy Major organ bleeding due to a non-correctable lesion or condition History of falls and high risk for recurrent falls True allergy or intolerance to OACs
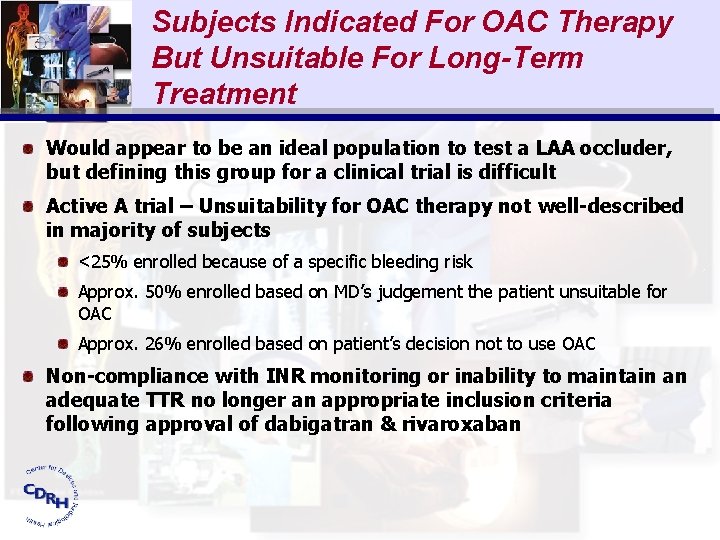
Subjects Indicated For OAC Therapy But Unsuitable For Long-Term Treatment Would appear to be an ideal population to test a LAA occluder, but defining this group for a clinical trial is difficult Active A trial – Unsuitability for OAC therapy not well-described in majority of subjects <25% enrolled because of a specific bleeding risk Approx. 50% enrolled based on MD’s judgement the patient unsuitable for OAC Approx. 26% enrolled based on patient’s decision not to use OAC Non-compliance with INR monitoring or inability to maintain an adequate TTR no longer an appropriate inclusion criteria following approval of dabigatran & rivaroxaban
Subjects Indicated For OAC Therapy But Unsuitable For Long-Term Treatment Further challenges in defining this subject group for a clinical trial The primary analysis population must be a coherent group to properly interpret study results Subjects who elect not to use OAC therapy likely represent a different population compared with those who are truly unsuitable candidates due to bleeding risks May be difficult to show benefit of LAA occlusion in subjects with multiple or advanced co-morbidities (e. g. , ESRD, hepatic disease) Bleeding risk scores (e. g. , HAS-BLED) offer some guidance but await validation
Subjects Indicated For OAC Therapy But Unsuitable For Long-Term Treatment Study subjects must be deemed acceptable candidates to receive the necessary peri- and post-procedural anticoagulants and antiplatelet agents If short-term OAC therapy or a P 2 Y 12 antagonist needed, the bleeding risk in these subjects will need to be considered Some otherwise eligible subjects may not be able to use even ASA alone due to bleeding risks Of particular importance in the elderly No role for the long-term use of clopidogrel in addition to ASA based on ACTIVE trials The benefit/risk analysis should consider the risk of stroke if closure of the LAA is unsuccessful and the subject is unsuitable for OAC therapy

Conclusion FDA is looking forward to the completion of trials of LAA occluder devices as potential safe and effective alternatives to long-term OAC therapy. Subjects indicated for OAC therapy but unsuitable for long-term treatment represent a reasonable population to test an LAA occluder, but defining this group for a clinical trial requires further work. Opportunity for discussion among FDA, industry, and clinical investigators in the pre-competitive space