CHALLENGES FOR MEDICAL MODELS OF ADDICTION 1 3
- Slides: 1
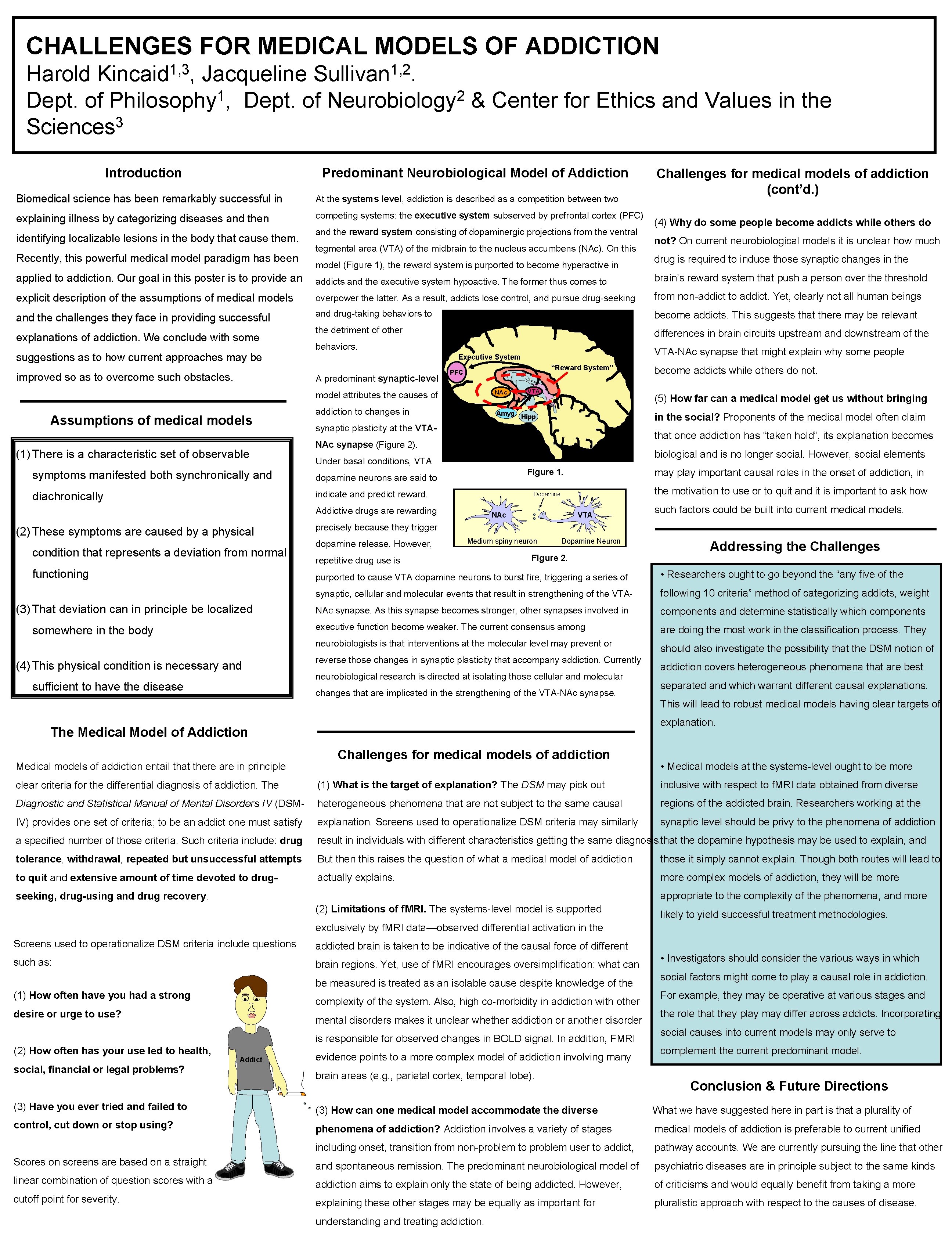
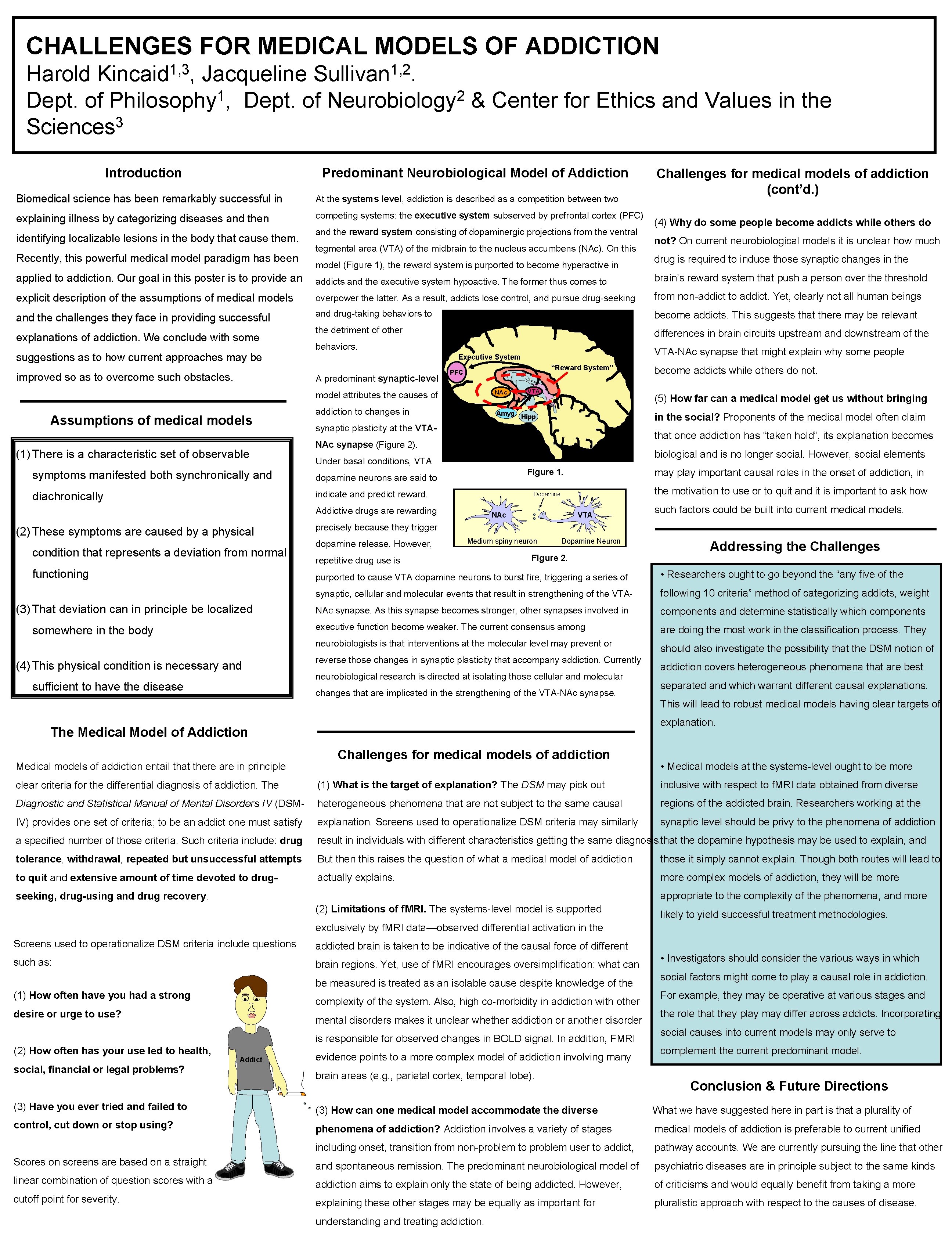
CHALLENGES FOR MEDICAL MODELS OF ADDICTION 1, 3 Kincaid , 1, 2 Sullivan. Harold Jacqueline 1 2 Dept. of Philosophy , Dept. of Neurobiology & Center for Ethics and Values in the 3 Sciences Introduction Predominant Neurobiological Model of Addiction Biomedical science has been remarkably successful in At the systems level, addiction is described as a competition between two explaining illness by categorizing diseases and then competing systems: the executive system subserved by prefrontal cortex (PFC) identifying localizable lesions in the body that cause them. Recently, this powerful medical model paradigm has been and the reward system consisting of dopaminergic projections from the ventral tegmental area (VTA) of the midbrain to the nucleus accumbens (NAc). On this model (Figure 1), the reward system is purported to become hyperactive in Challenges for medical models of addiction (cont’d. ) (4) Why do some people become addicts while others do not? On current neurobiological models it is unclear how much drug is required to induce those synaptic changes in the applied to addiction. Our goal in this poster is to provide an addicts and the executive system hypoactive. The former thus comes to brain’s reward system that push a person over the threshold explicit description of the assumptions of medical models overpower the latter. As a result, addicts lose control, and pursue drug-seeking from non-addict to addict. Yet, clearly not all human beings and the challenges they face in providing successful and drug-taking behaviors to become addicts. This suggests that there may be relevant the detriment of other differences in brain circuits upstream and downstream of the explanations of addiction. We conclude with some suggestions as to how current approaches may be improved so as to overcome such obstacles. behaviors. A predominant synaptic-level “Reward System” PFC NAc model attributes the causes of Assumptions of medical models (1) There is a characteristic set of observable addiction to changes in Amyg. Hipp diachronically that once addiction has “taken hold”, its explanation becomes biological and is no longer social. However, social elements (3) That deviation can in principle be localized somewhere in the body may play important causal roles in the onset of addiction, in Figure 1. the motivation to use or to quit and it is important to ask how Dopamine Addictive drugs are rewarding functioning in the social? Proponents of the medical model often claim Under basal conditions, VTA indicate and predict reward. NAc VTA sufficient to have the disease such factors could be built into current medical models. precisely because they trigger dopamine release. However, Medium spiny neuron repetitive drug use is Dopamine Neuron Figure 2. Addressing the Challenges purported to cause VTA dopamine neurons to burst fire, triggering a series of • Researchers ought to go beyond the “any five of the synaptic, cellular and molecular events that result in strengthening of the VTA- following 10 criteria” method of categorizing addicts, weight NAc synapse. As this synapse becomes stronger, other synapses involved in components and determine statistically which components executive function become weaker. The current consensus among are doing the most work in the classification process. They neurobiologists is that interventions at the molecular level may prevent or (4) This physical condition is necessary and become addicts while others do not. (5) How far can a medical model get us without bringing NAc synapse (Figure 2). dopamine neurons are said to condition that represents a deviation from normal VTA synaptic plasticity at the VTA- symptoms manifested both synchronically and (2) These symptoms are caused by a physical VTA-NAc synapse that might explain why some people Executive System reverse those changes in synaptic plasticity that accompany addiction. Currently neurobiological research is directed at isolating those cellular and molecular changes that are implicated in the strengthening of the VTA-NAc synapse. should also investigate the possibility that the DSM notion of addiction covers heterogeneous phenomena that are best separated and which warrant different causal explanations. This will lead to robust medical models having clear targets of explanation. The Medical Model of Addiction Medical models of addiction entail that there are in principle Challenges for medical models of addiction • Medical models at the systems-level ought to be more clear criteria for the differential diagnosis of addiction. The (1) What is the target of explanation? The DSM may pick out inclusive with respect to f. MRI data obtained from diverse Diagnostic and Statistical Manual of Mental Disorders IV (DSM- heterogeneous phenomena that are not subject to the same causal regions of the addicted brain. Researchers working at the IV) provides one set of criteria; to be an addict one must satisfy explanation. Screens used to operationalize DSM criteria may similarly synaptic level should be privy to the phenomena of addiction a specified number of those criteria. Such criteria include: drug result in individuals with different characteristics getting the same diagnosis. that the dopamine hypothesis may be used to explain, and tolerance, withdrawal, repeated but unsuccessful attempts But then this raises the question of what a medical model of addiction those it simply cannot explain. Though both routes will lead to to quit and extensive amount of time devoted to drug- actually explains. more complex models of addiction, they will be more appropriate to the complexity of the phenomena, and more seeking, drug-using and drug recovery. (2) Limitations of f. MRI. The systems-level model is supported likely to yield successful treatment methodologies. exclusively by f. MRI data—observed differential activation in the Screens used to operationalize DSM criteria include questions such as: addicted brain is taken to be indicative of the causal force of different brain regions. Yet, use of f. MRI encourages oversimplification: what can be measured is treated as an isolable cause despite knowledge of the (1) How often have you had a strong complexity of the system. Also, high co-morbidity in addiction with other desire or urge to use? mental disorders makes it unclear whether addiction or another disorder is responsible for observed changes in BOLD signal. In addition, FMRI (2) How often has your use led to health, social, financial or legal problems? Addict evidence points to a more complex model of addiction involving many brain areas (e. g. , parietal cortex, temporal lobe). • Investigators should consider the various ways in which social factors might come to play a causal role in addiction. For example, they may be operative at various stages and the role that they play may differ across addicts. Incorporating social causes into current models may only serve to complement the current predominant model. Conclusion & Future Directions (3) Have you ever tried and failed to (3) How can one medical model accommodate the diverse What we have suggested here in part is that a plurality of control, cut down or stop using? phenomena of addiction? Addiction involves a variety of stages medical models of addiction is preferable to current unified including onset, transition from non-problem to problem user to addict, pathway accounts. We are currently pursuing the line that other Scores on screens are based on a straight and spontaneous remission. The predominant neurobiological model of psychiatric diseases are in principle subject to the same kinds linear combination of question scores with a addiction aims to explain only the state of being addicted. However, of criticisms and would equally benefit from taking a more cutoff point for severity. explaining these other stages may be equally as important for pluralistic approach with respect to the causes of disease. understanding and treating addiction.