Ch 4 Skin and Body Membranes Epithelial Membranes
Ch. 4 Skin and Body Membranes
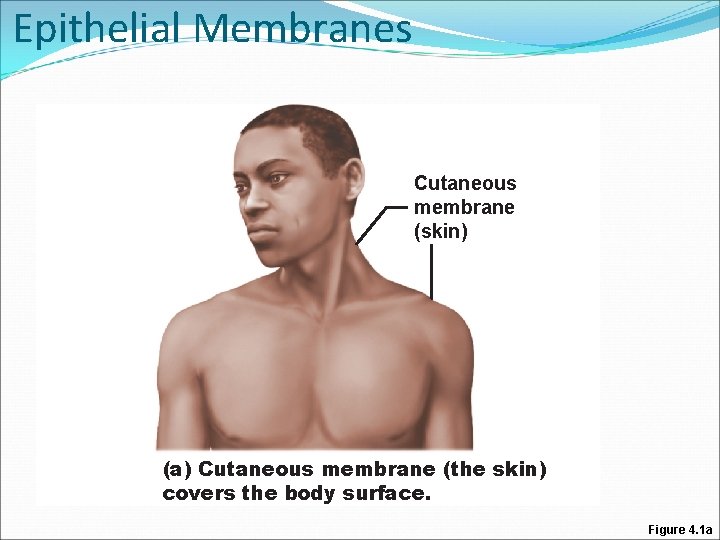
Epithelial Membranes Cutaneous membrane (skin) (a) Cutaneous membrane (the skin) covers the body surface. Figure 4. 1 a
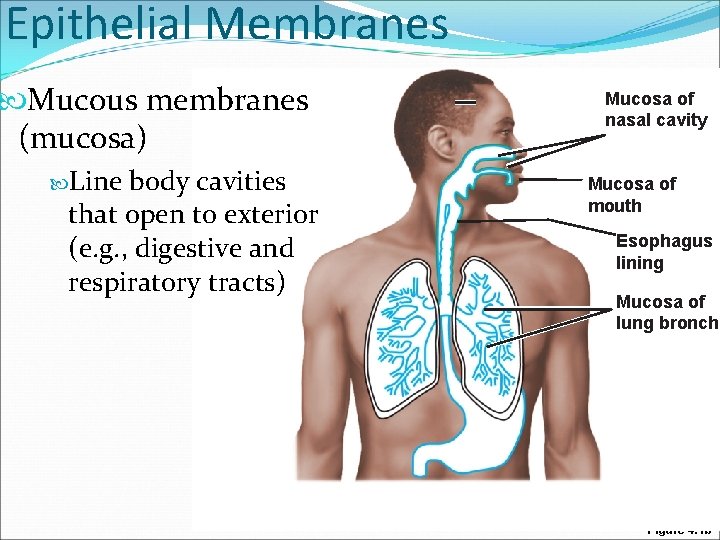
Epithelial Membranes Mucous membranes (mucosa) Line body cavities that open to exterior (e. g. , digestive and respiratory tracts) Mucosa of nasal cavity Mucosa of mouth Esophagus lining Mucosa of lung bronchi Figure 4. 1 b
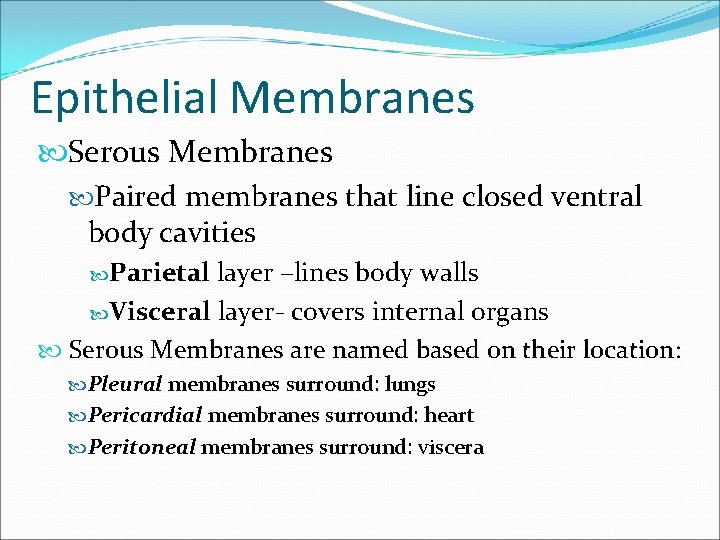
Epithelial Membranes Serous Membranes Paired membranes that line closed ventral body cavities Parietal layer –lines body walls Visceral layer- covers internal organs Serous Membranes are named based on their location: Pleural membranes surround: lungs Pericardial membranes surround: heart Peritoneal membranes surround: viscera
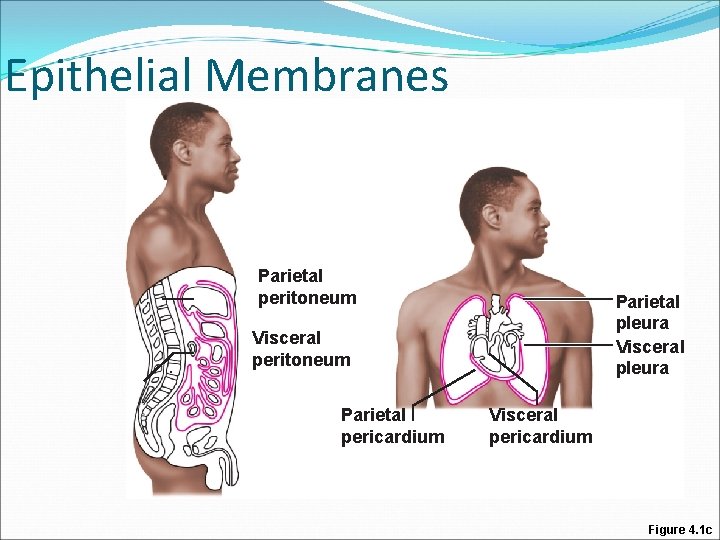
Epithelial Membranes Parietal peritoneum Parietal pleura Visceral peritoneum Parietal pericardium Visceral pericardium Figure 4. 1 c
Skin (Integument) Consists of three major regions 1. Epidermis—superficial region 2. Dermis—middle region 3. Hypodermis —deepest region Mostly adipose tissue
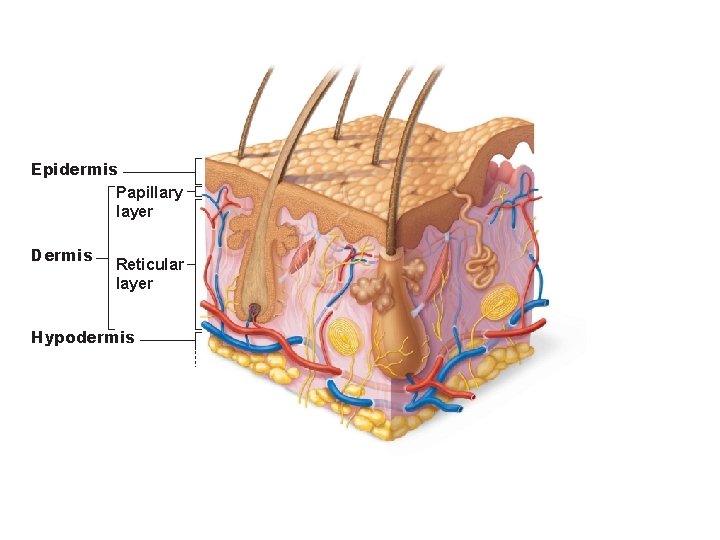
Epidermis Papillary layer Dermis Reticular layer Hypodermis
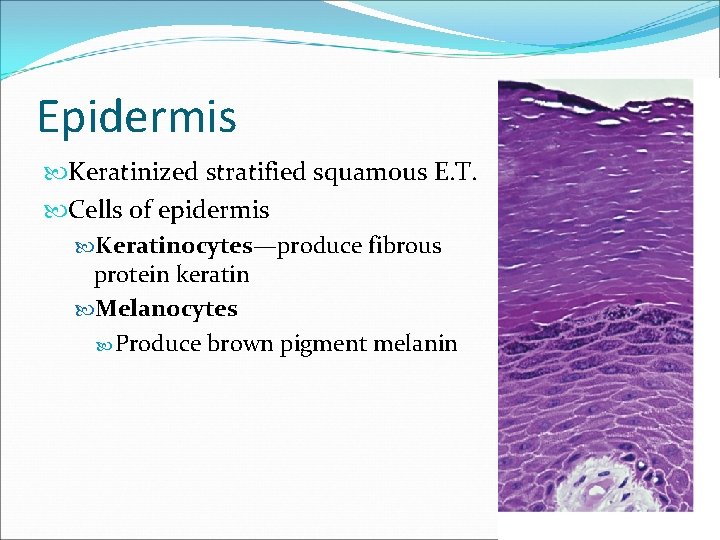
Epidermis Keratinized stratified squamous E. T. Cells of epidermis Keratinocytes—produce fibrous protein keratin Melanocytes Produce brown pigment melanin
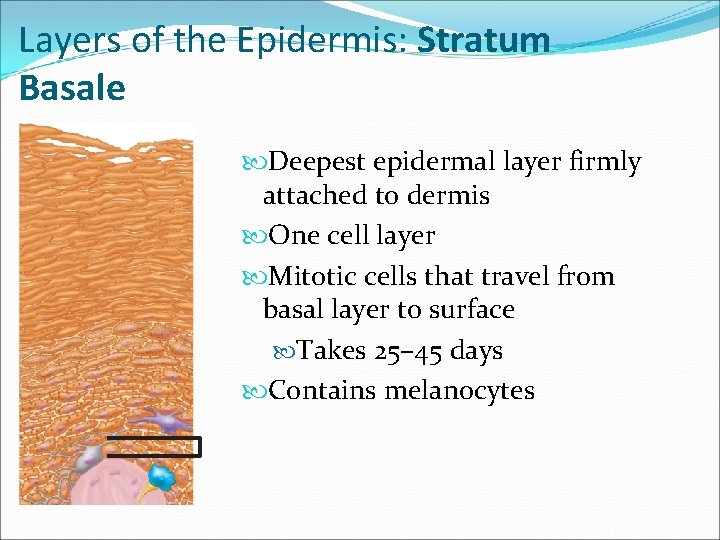
Layers of the Epidermis: Stratum Basale Deepest epidermal layer firmly attached to dermis One cell layer Mitotic cells that travel from basal layer to surface Takes 25– 45 days Contains melanocytes
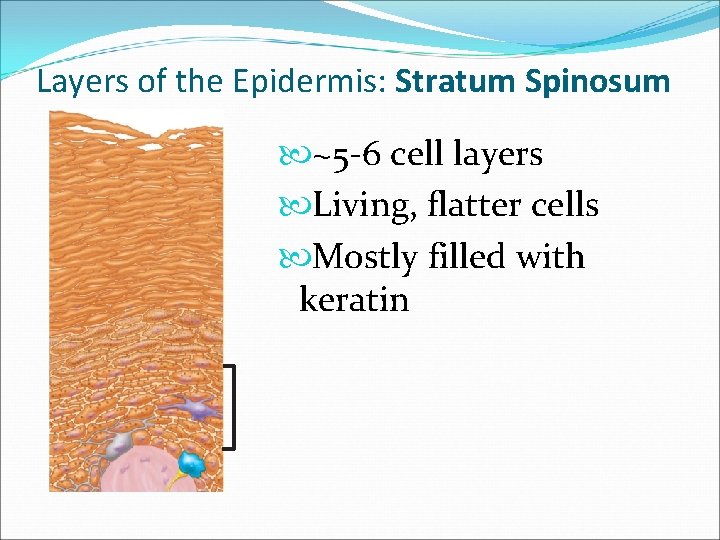
Layers of the Epidermis: Stratum Spinosum ~5 -6 cell layers Living, flatter cells Mostly filled with keratin
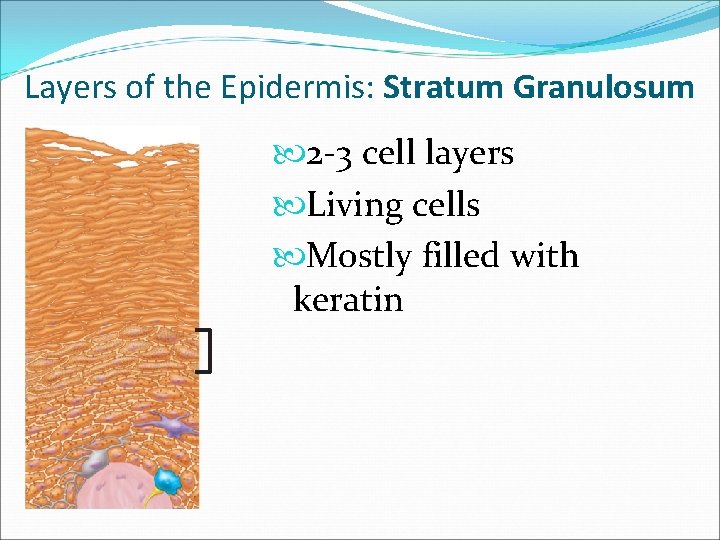
Layers of the Epidermis: Stratum Granulosum 2 -3 cell layers Living cells Mostly filled with keratin
Layers of the Epidermis: Stratum Lucidum A few rows of flat, dead keratinocytes Thin, transparent band superficial to the stratum granulosum Only in soles and palms
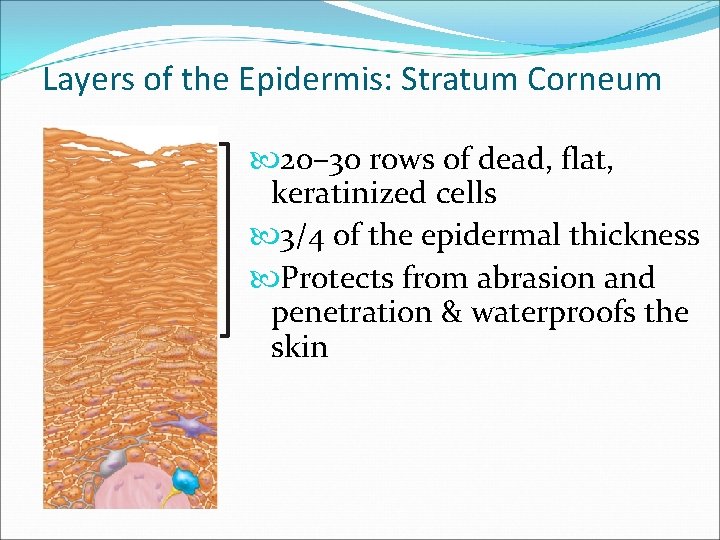
Layers of the Epidermis: Stratum Corneum 20– 30 rows of dead, flat, keratinized cells 3/4 of the epidermal thickness Protects from abrasion and penetration & waterproofs the skin
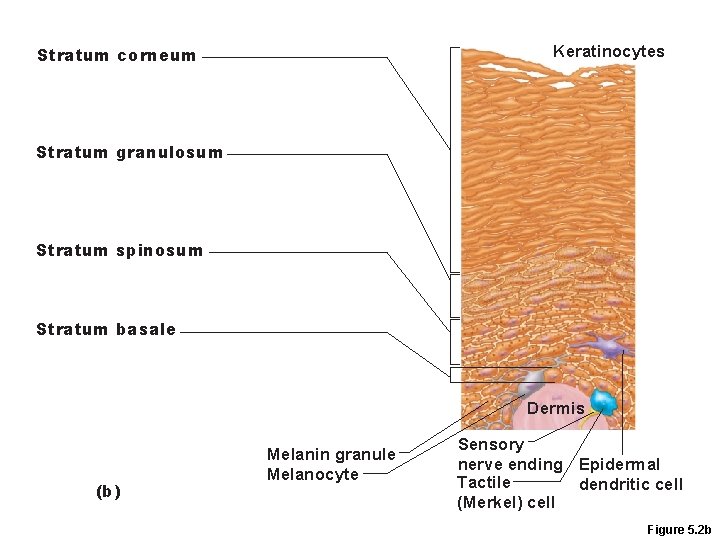
Keratinocytes Stratum corneum Stratum granulosum Stratum spinosum Stratum basale Dermis (b) Melanin granule Melanocyte Sensory nerve ending Epidermal Tactile dendritic cell (Merkel) cell Figure 5. 2 b
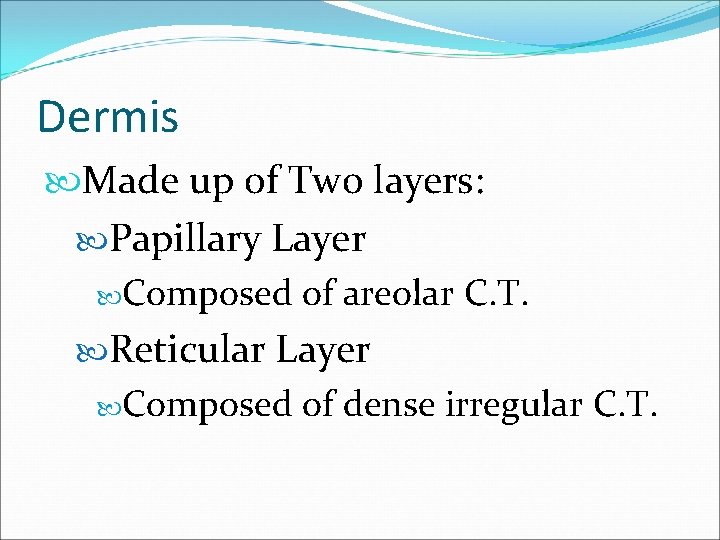
Dermis Made up of Two layers: Papillary Layer Composed of areolar C. T. Reticular Layer Composed of dense irregular C. T.
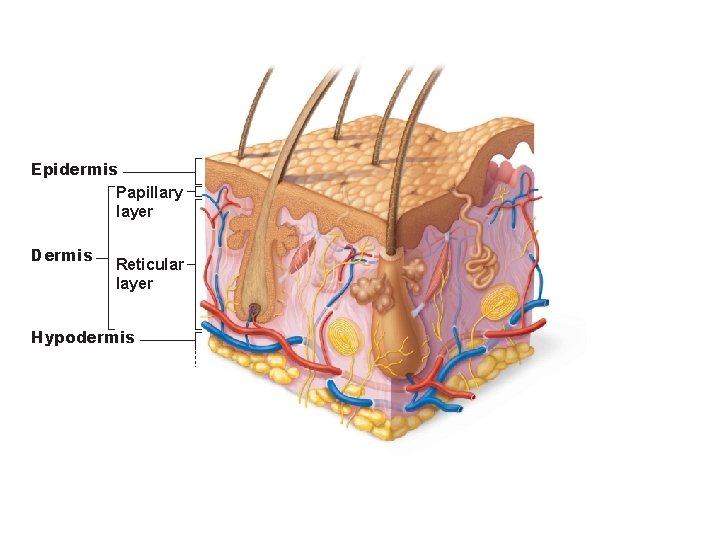
Epidermis Papillary layer Dermis Reticular layer Hypodermis
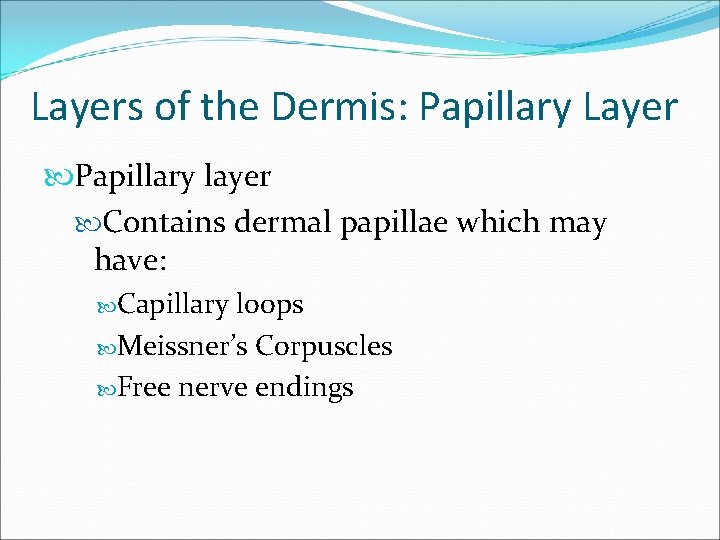
Layers of the Dermis: Papillary Layer Papillary layer Contains dermal papillae which may have: Capillary loops Meissner’s Corpuscles Free nerve endings
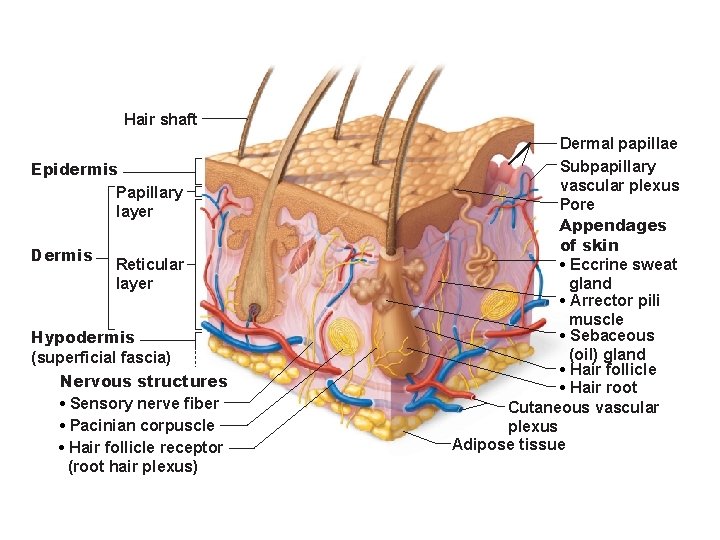
Hair shaft Epidermis Papillary layer Dermis Reticular layer Hypodermis (superficial fascia) Nervous structures • Sensory nerve fiber • Pacinian corpuscle • Hair follicle receptor (root hair plexus) Dermal papillae Subpapillary vascular plexus Pore Appendages of skin • Eccrine sweat gland • Arrector pili muscle • Sebaceous (oil) gland • Hair follicle • Hair root Cutaneous vascular plexus Adipose tissue
Layers of the Dermis: Reticular Layer Reticular layer Most glands, hair follicles, emerge from the dermis
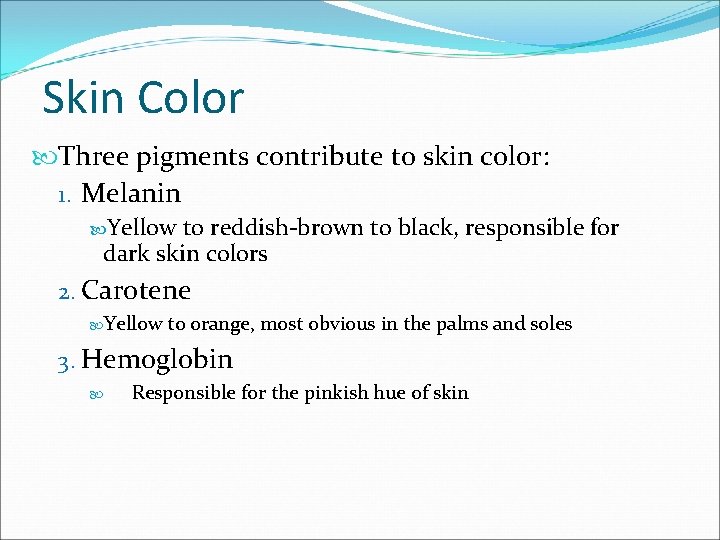
Skin Color Three pigments contribute to skin color: 1. Melanin Yellow to reddish-brown to black, responsible for dark skin colors 2. Carotene Yellow to orange, most obvious in the palms and soles 3. Hemoglobin Responsible for the pinkish hue of skin
Appendages of the Skin Appendages are derived from the epidermis Sweat glands Oil glands Hairs and hair follicles Nails
Sweat Glands Two main types of sweat glands 1. Eccrine sweat glands—abundant on palms, soles, and forehead Sweat: 99% water, Na. Cl, vitamin C, antibodies, metabolic wastes Ducts connect to pores Thermoregulatory function
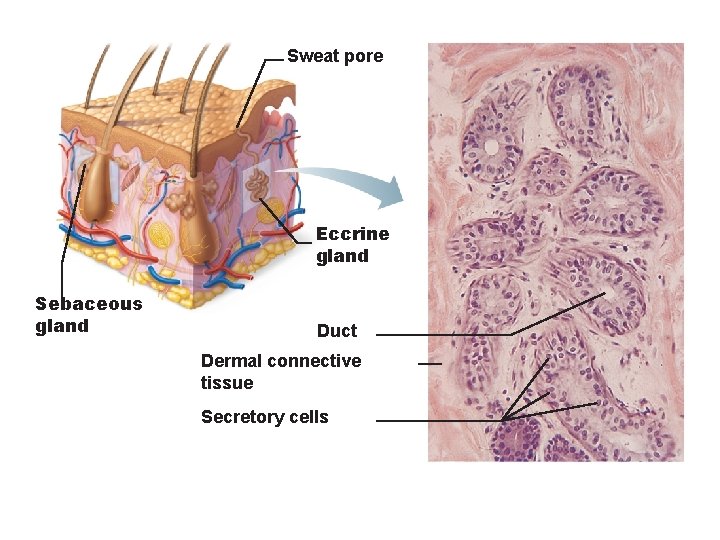
Sweat pore Eccrine gland Sebaceous gland Duct Dermal connective tissue Secretory cells
Sweat Glands 2. Apocrine sweat glands—confined to axillary and anogenital areas Sebum: sweat + fatty substances and proteins Ducts connect to hair follicles Functional from puberty onward
Sebaceous (Oil) Glands Most develop from hair follicles Secrete Sebum: Oily secretion Bactericidal Softens hair and skin
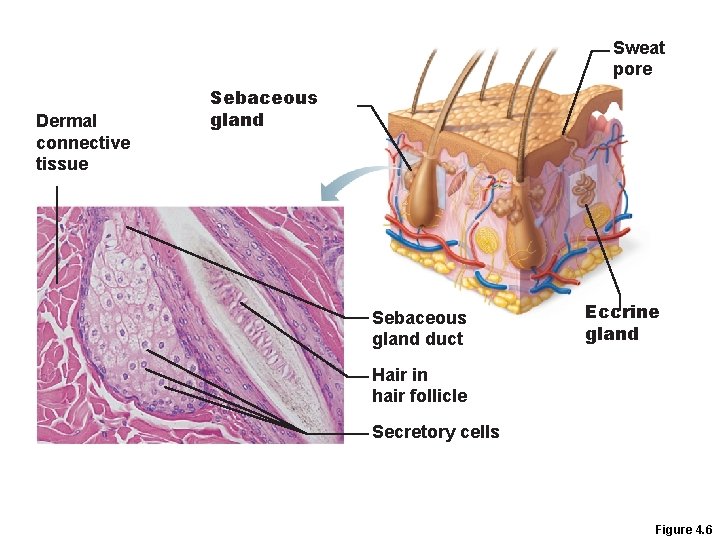
Sweat pore Dermal connective tissue Sebaceous gland duct Eccrine gland Hair in hair follicle Secretory cells Figure 4. 6
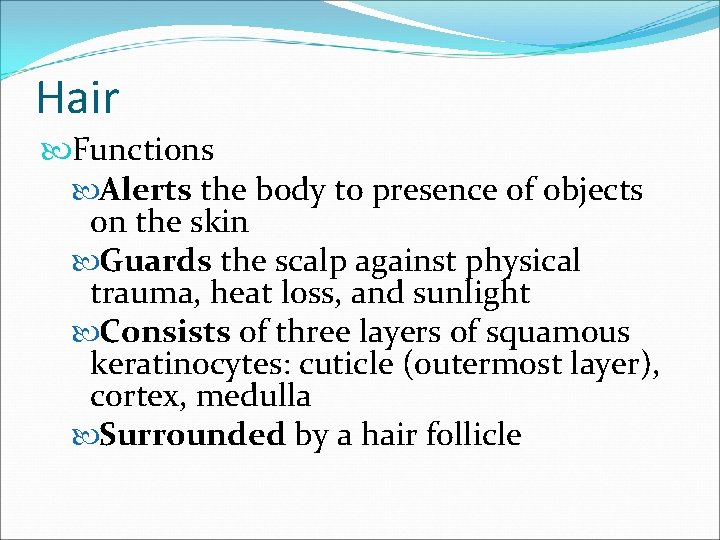
Hair Functions Alerts the body to presence of objects on the skin Guards the scalp against physical trauma, heat loss, and sunlight Consists of three layers of squamous keratinocytes: cuticle (outermost layer), cortex, medulla Surrounded by a hair follicle
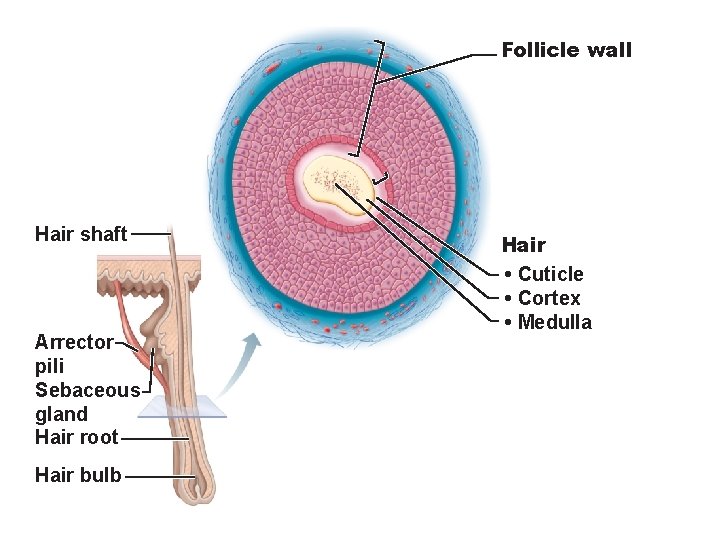
Follicle wall Hair shaft Arrector pili Sebaceous gland Hair root Hair bulb Hair • Cuticle • Cortex • Medulla
Hair Follicle Two layered wall consisting of CT and ET Hair bulb: expanded deep end Hair follicle receptor (root hair plexus): Sensory nerve endings around each hair bulb
Hair Follicle Arrector pili Smooth muscle attached to follicle Contraction of these muscles causes the hairs to stand on end (forming “goose bumps”)
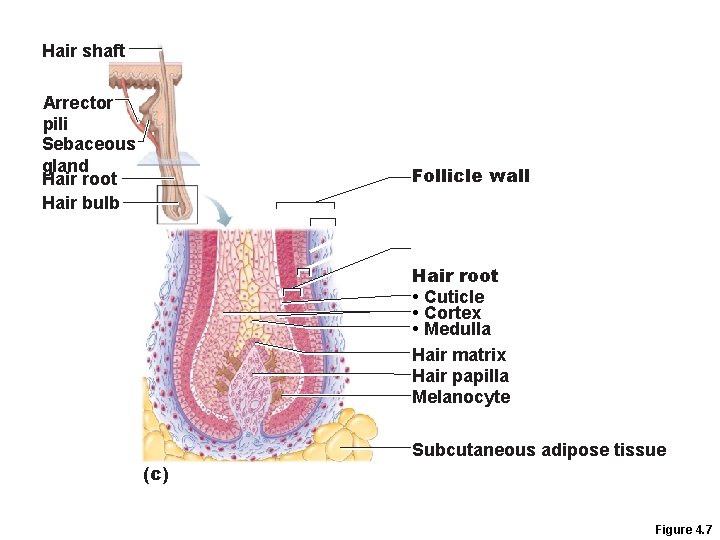
Hair shaft Arrector pili Sebaceous gland Hair root Hair bulb Follicle wall Hair root • Cuticle • Cortex • Medulla Hair matrix Hair papilla Melanocyte Subcutaneous adipose tissue (c) Figure 4. 7
Structure of a Nail Scalelike modification of the epidermis Structures of the nail: Free edge, body, nail matrix, nail bed, hyponichium, eponichium,
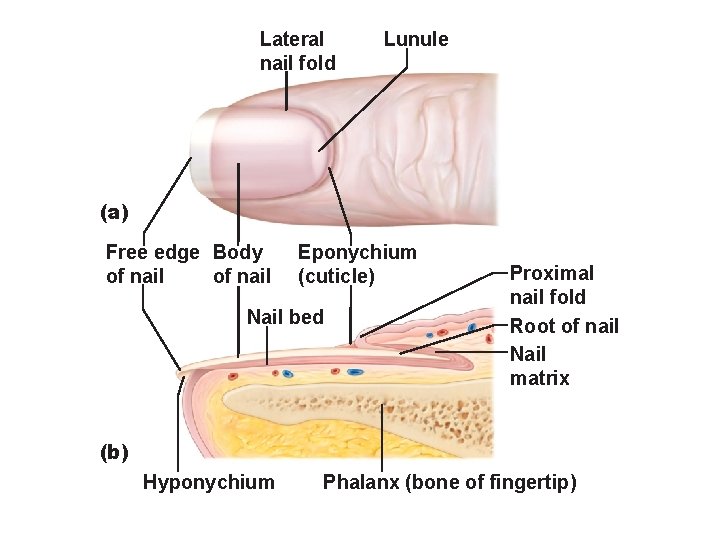
Lateral nail fold Lunule (a) Free edge Body of nail Eponychium (cuticle) Nail bed Proximal nail fold Root of nail Nail matrix (b) Hyponychium Phalanx (bone of fingertip)
Functions of the Integumentary System 1. Protection Chemical Low p. H secretions retard bacterial activity Physical/mechanical barriers Keratin and glycolipids block most water and water- soluble substances Biological barriers Macrophages
Functions of the Integumentary System 2. Body temperature regulation At elevated temperature, dilation of dermal vessels and increased sweat gland activity cool the body 3. Cutaneous sensations Temperature, touch, and pain
Functions of the Integumentary System 4. Metabolic functions Synthesis of vitamin D precursor 5. Blood reservoir—up to 5% of body’s blood volume 6. Excretion—nitrogenous wastes and salt in sweat
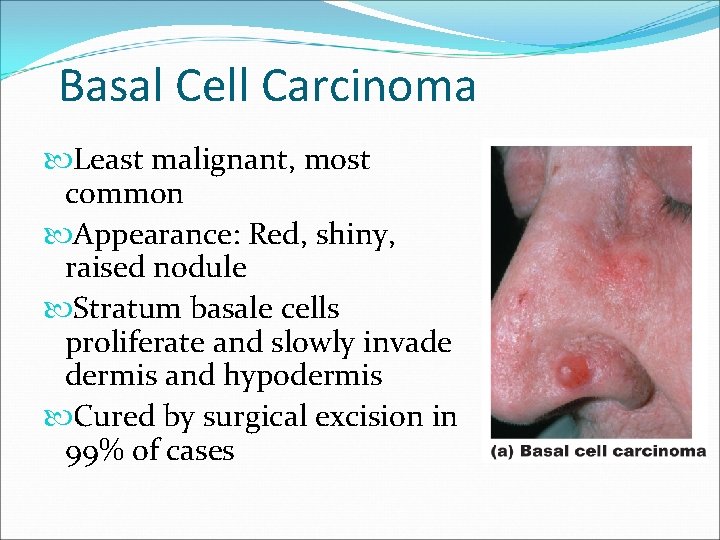
Basal Cell Carcinoma Least malignant, most common Appearance: Red, shiny, raised nodule Stratum basale cells proliferate and slowly invade dermis and hypodermis Cured by surgical excision in 99% of cases
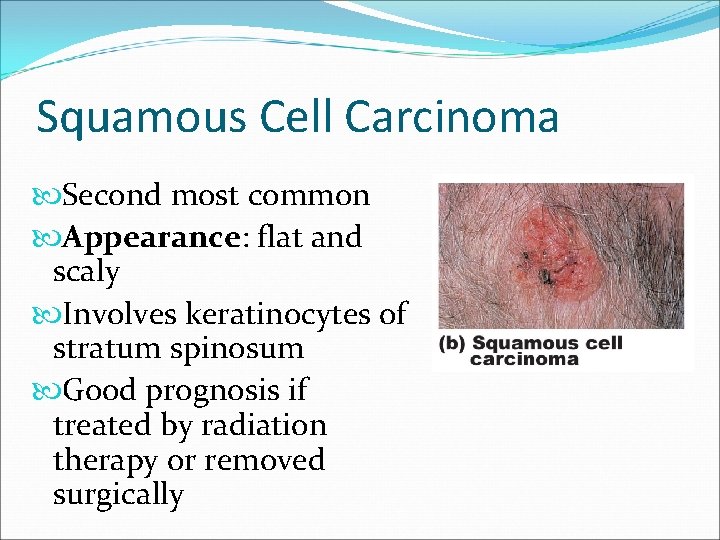
Squamous Cell Carcinoma Second most common Appearance: flat and scaly Involves keratinocytes of stratum spinosum Good prognosis if treated by radiation therapy or removed surgically
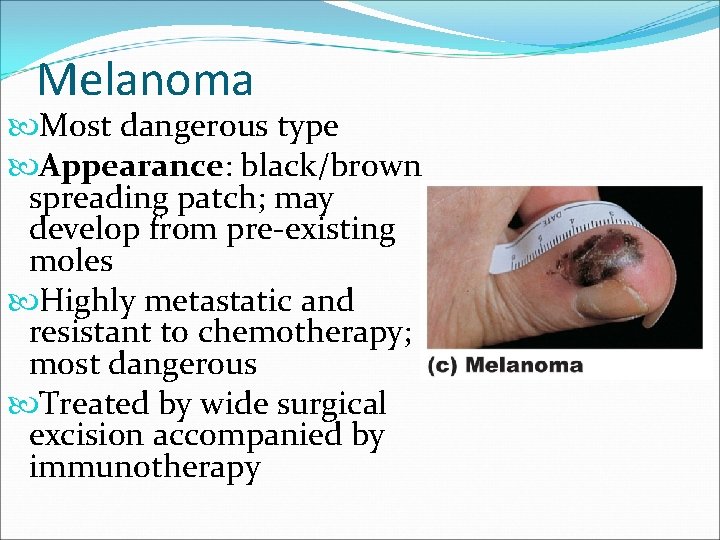
Melanoma Most dangerous type Appearance: black/brown spreading patch; may develop from pre-existing moles Highly metastatic and resistant to chemotherapy; most dangerous Treated by wide surgical excision accompanied by immunotherapy
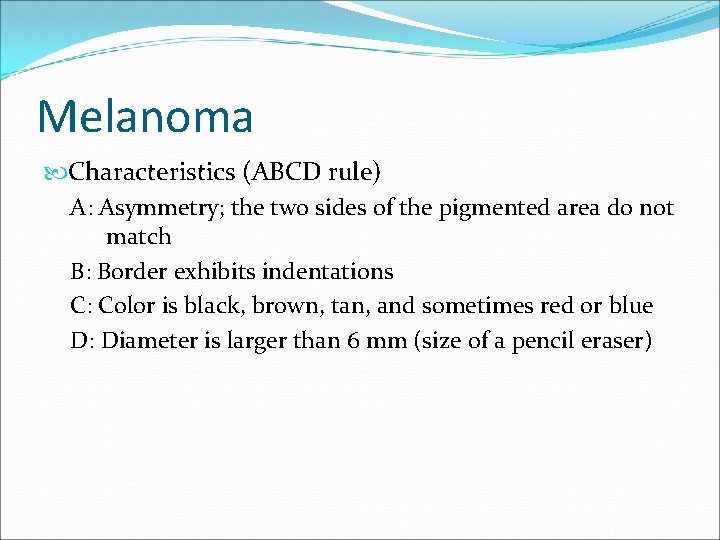
Melanoma Characteristics (ABCD rule) A: Asymmetry; the two sides of the pigmented area do not match B: Border exhibits indentations C: Color is black, brown, tan, and sometimes red or blue D: Diameter is larger than 6 mm (size of a pencil eraser)
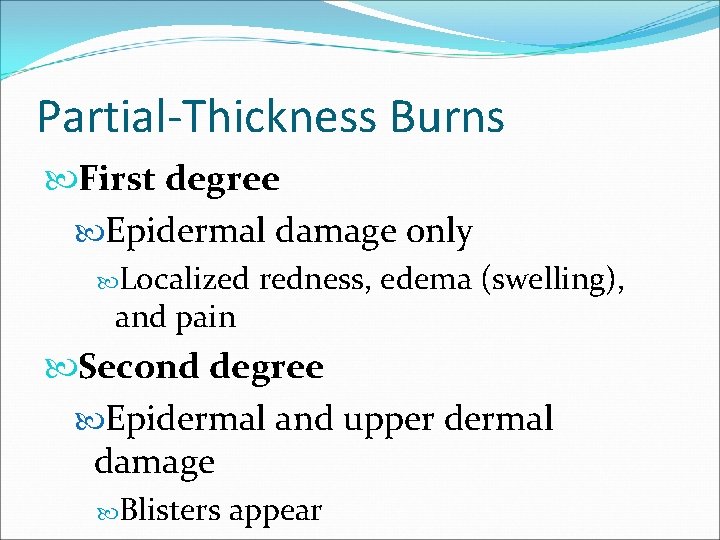
Partial-Thickness Burns First degree Epidermal damage only Localized and pain redness, edema (swelling), Second degree Epidermal and upper dermal damage Blisters appear
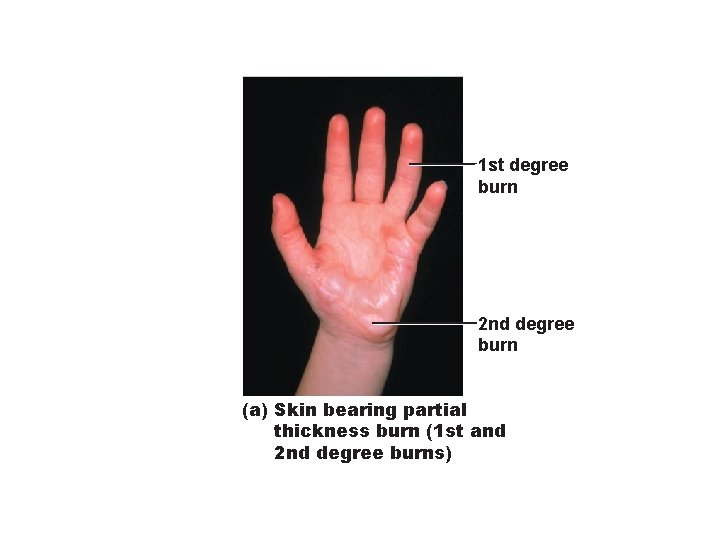
1 st degree burn 2 nd degree burn (a) Skin bearing partial thickness burn (1 st and 2 nd degree burns)
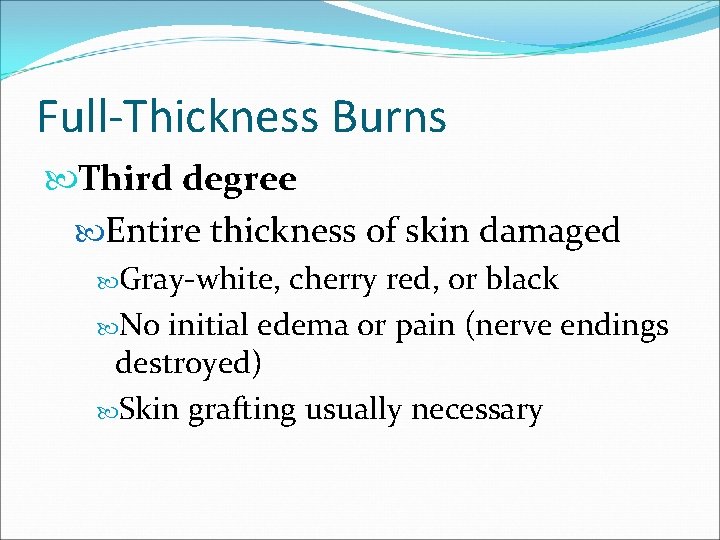
Full-Thickness Burns Third degree Entire thickness of skin damaged Gray-white, cherry red, or black No initial edema or pain (nerve endings destroyed) Skin grafting usually necessary
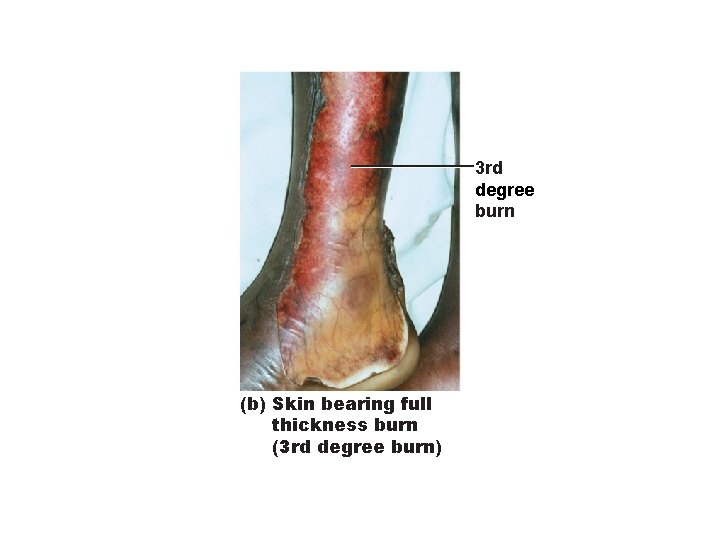
3 rd degree burn (b) Skin bearing full thickness burn (3 rd degree burn)
- Slides: 44