Ch 27 The Reproductive System Related Issues Copyright
- Slides: 34
Ch 27 The Reproductive System & Related Issues Copyright © 2010 Pearson Education, Inc.
ASSIGNMENT MW Class: Please have this ppt filled in for Monday WF Class: Please have this ppt filled in for Wednesday Copyright © 2010 Pearson Education, Inc.
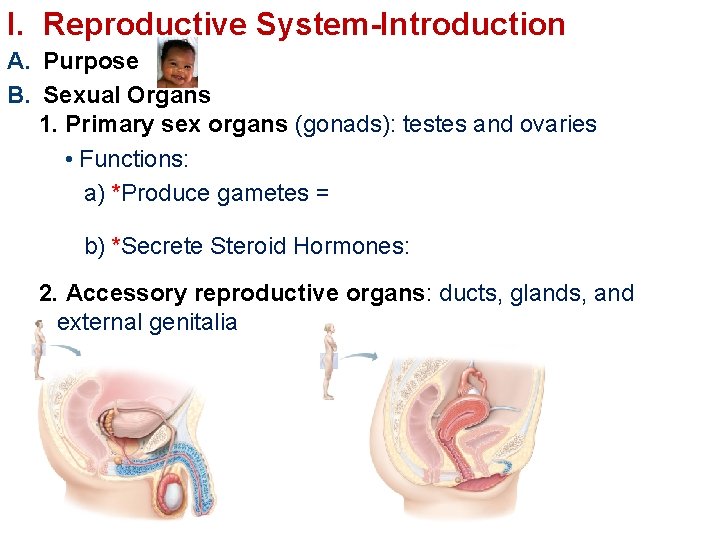
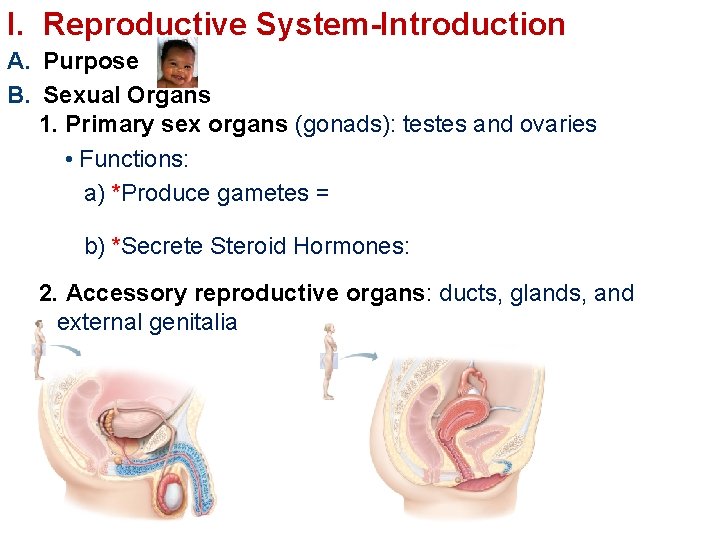
I. Reproductive System-Introduction A. Purpose B. Sexual Organs 1. Primary sex organs (gonads): testes and ovaries • Functions: a) *Produce gametes = b) *Secrete Steroid Hormones: 2. Accessory reproductive organs: ducts, glands, and external genitalia
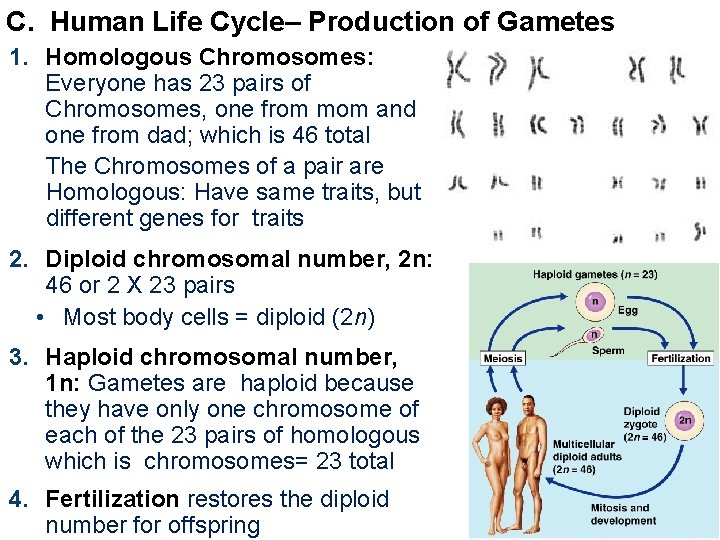
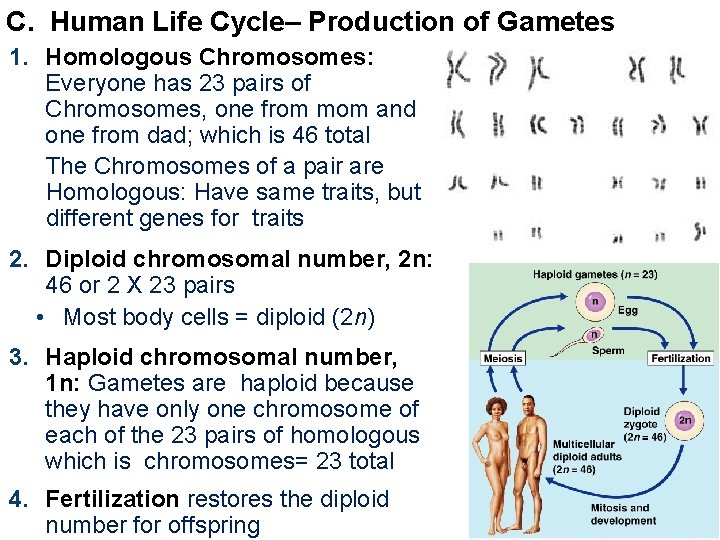
C. Human Life Cycle– Production of Gametes 1. Homologous Chromosomes: Everyone has 23 pairs of Chromosomes, one from mom and one from dad; which is 46 total The Chromosomes of a pair are Homologous: Have same traits, but different genes for traits 2. Diploid chromosomal number, 2 n: 46 or 2 X 23 pairs • Most body cells = diploid (2 n) 3. Haploid chromosomal number, 1 n: Gametes are haploid because they have only one chromosome of each of the 23 pairs of homologous which is chromosomes= 23 total 4. Fertilization restores the diploid number for offspring
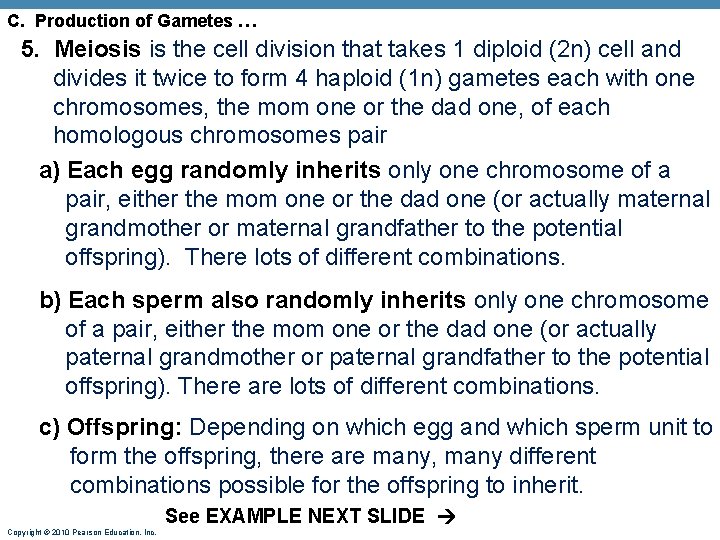
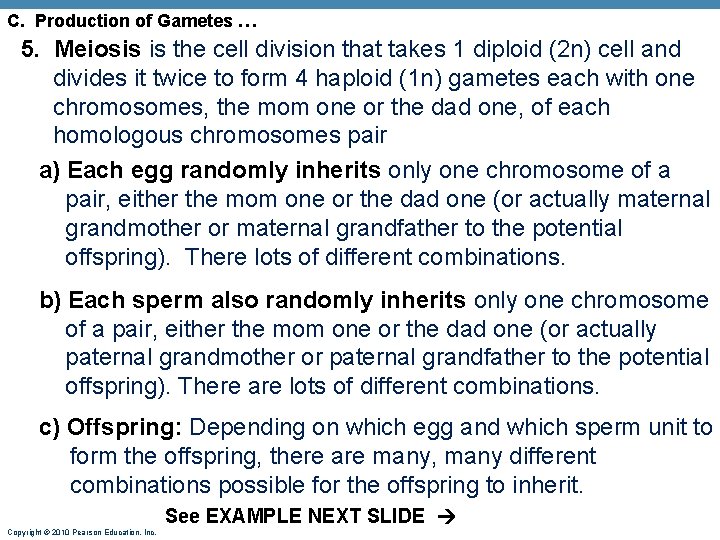
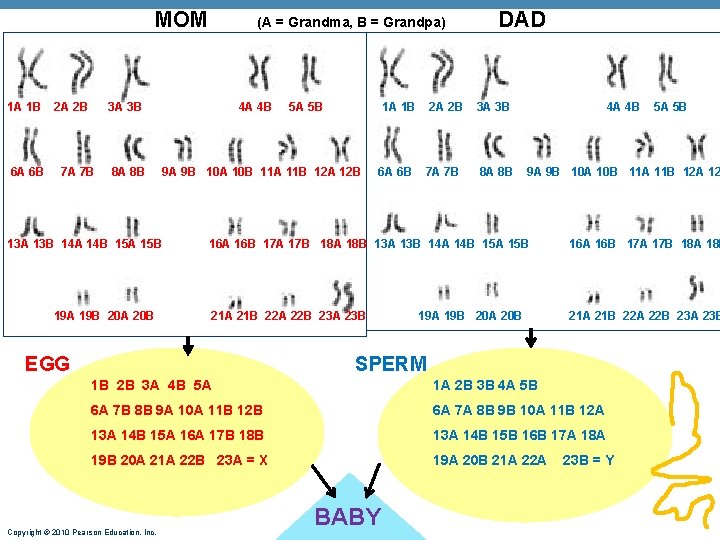
C. Production of Gametes … 5. Meiosis is the cell division that takes 1 diploid (2 n) cell and divides it twice to form 4 haploid (1 n) gametes each with one chromosomes, the mom one or the dad one, of each homologous chromosomes pair a) Each egg randomly inherits only one chromosome of a pair, either the mom one or the dad one (or actually maternal grandmother or maternal grandfather to the potential offspring). There lots of different combinations. b) Each sperm also randomly inherits only one chromosome of a pair, either the mom one or the dad one (or actually paternal grandmother or paternal grandfather to the potential offspring). There are lots of different combinations. c) Offspring: Depending on which egg and which sperm unit to form the offspring, there are many, many different combinations possible for the offspring to inherit. Copyright © 2010 Pearson Education, Inc. See EXAMPLE NEXT SLIDE
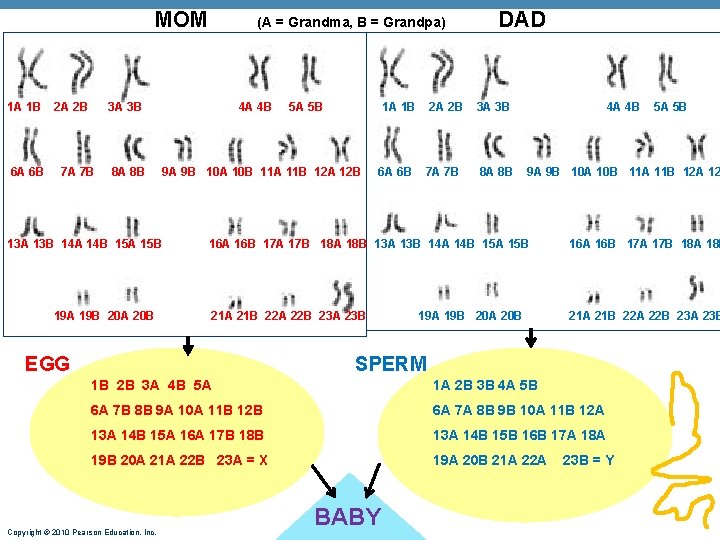
MOM 1 A 1 B 6 A 6 B 2 A 2 B (A = Grandma, B = Grandpa) 3 A 3 B 7 A 7 B 8 A 8 B 4 A 4 B 9 A 9 B 10 A 10 B 11 A 11 B 12 A 12 B 13 A 13 B 14 A 14 B 15 A 15 B 19 A 19 B 20 A 20 B 5 A 5 B DAD 1 A 1 B 2 A 2 B 3 A 3 B 4 A 4 B 6 A 6 B 7 A 7 B 8 A 8 B 9 A 9 B 10 A 10 B 11 A 11 B 12 A 12 16 A 16 B 17 A 17 B 18 A 18 B 13 A 13 B 14 A 14 B 15 A 15 B 16 A 16 B 17 A 17 B 18 A 18 B 21 A 21 B 22 A 22 B 23 A 23 B EGG 19 A 19 B 20 A 20 B SPERM 1 B 2 B 3 A 4 B 5 A 1 A 2 B 3 B 4 A 5 B 6 A 7 B 8 B 9 A 10 A 11 B 12 B 6 A 7 A 8 B 9 B 10 A 11 B 12 A 13 A 14 B 15 A 16 A 17 B 18 B 13 A 14 B 15 B 16 B 17 A 18 A 19 B 20 A 21 A 22 B 23 A = X 19 A 20 B 21 A 22 A Copyright © 2010 Pearson Education, Inc. 5 A 5 B BABY 23 B = Y
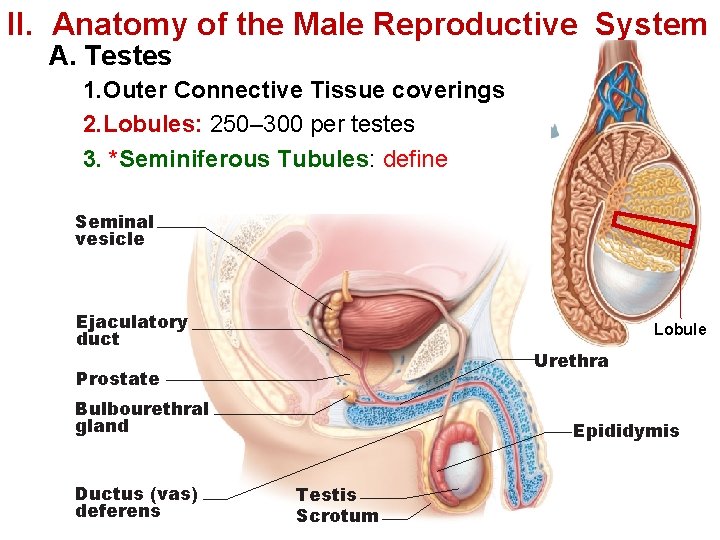
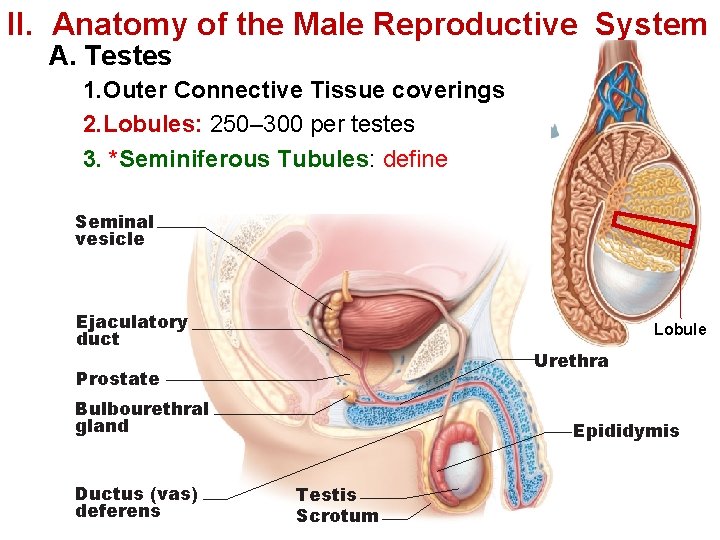
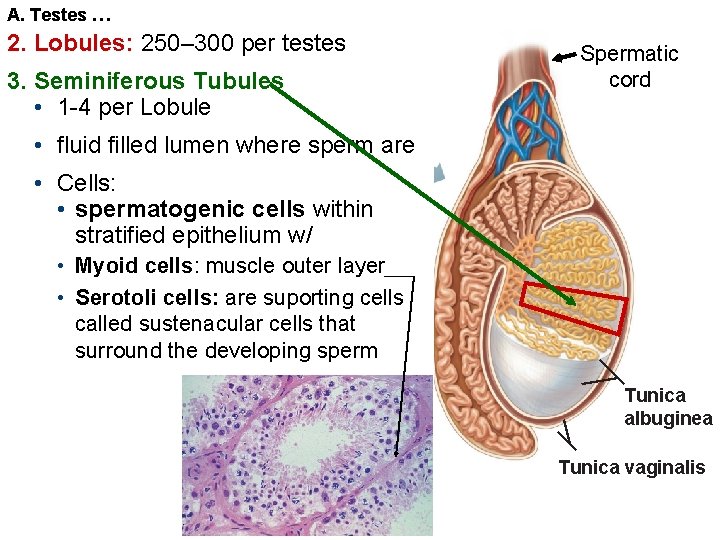
II. Anatomy of the Male Reproductive System A. Testes 1. Outer Connective Tissue coverings 2. Lobules: 250– 300 per testes 3. *Seminiferous Tubules: define Seminal vesicle Ejaculatory duct Lobule Urethra Prostate Bulbourethral gland Ductus (vas) deferens Epididymis Testis Scrotum
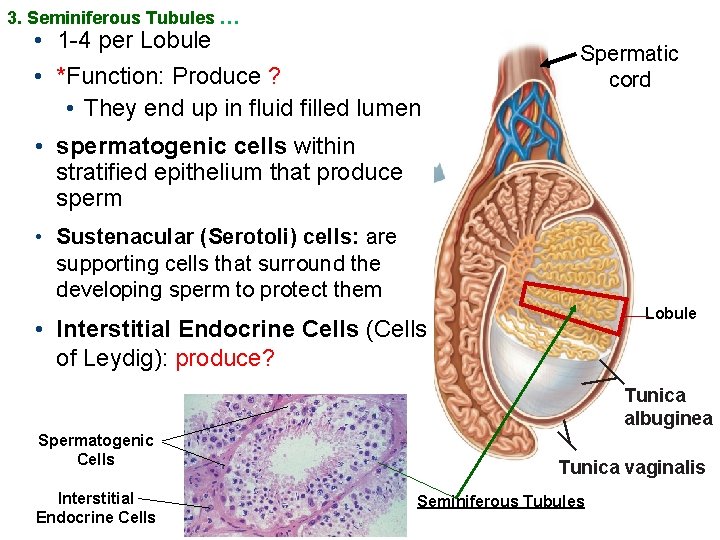
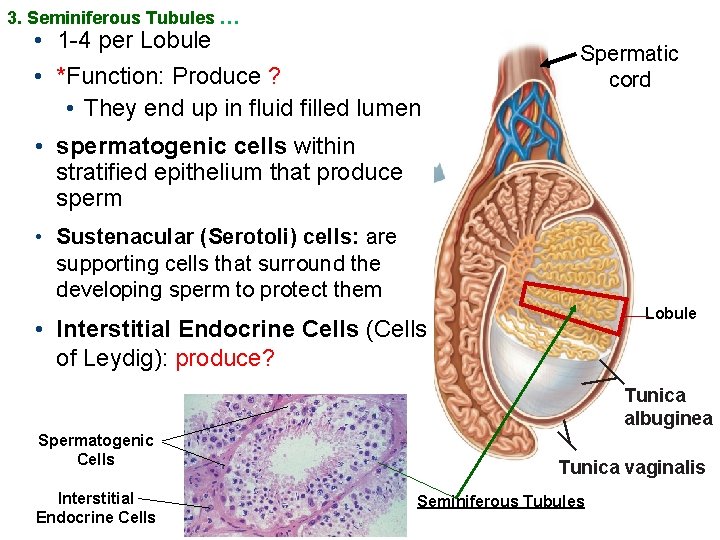
3. Seminiferous Tubules … • 1 -4 per Lobule • *Function: Produce ? • They end up in fluid filled lumen Spermatic cord • spermatogenic cells within stratified epithelium that produce sperm • Sustenacular (Serotoli) cells: are supporting cells that surround the developing sperm to protect them Lobule • Interstitial Endocrine Cells (Cells of Leydig): produce? Tunica albuginea Spermatogenic Cells Interstitial Endocrine Cells Tunica vaginalis Seminiferous Tubules
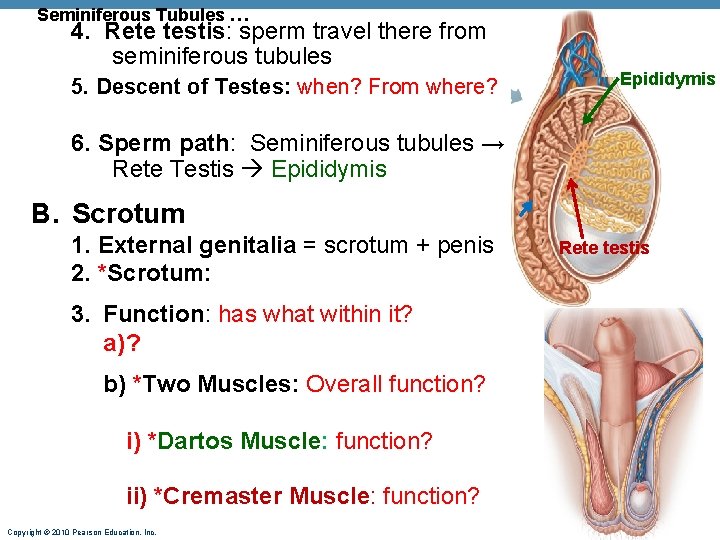
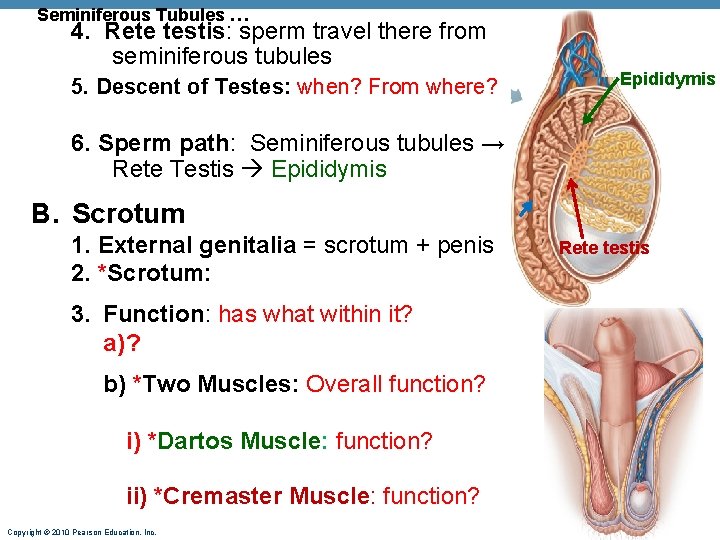
Seminiferous Tubules … 4. Rete testis: sperm travel there from seminiferous tubules 5. Descent of Testes: when? From where? Epididymis 6. Sperm path: Seminiferous tubules → Rete Testis Epididymis B. Scrotum 1. External genitalia = scrotum + penis 2. *Scrotum: 3. Function: has what within it? a) ? b) *Two Muscles: Overall function? i) *Dartos Muscle: function? ii) *Cremaster Muscle: function? Copyright © 2010 Pearson Education, Inc. Rete testis
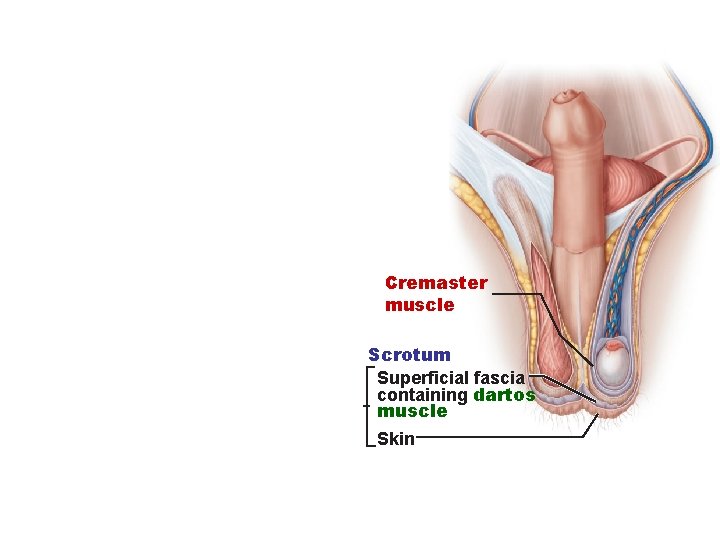
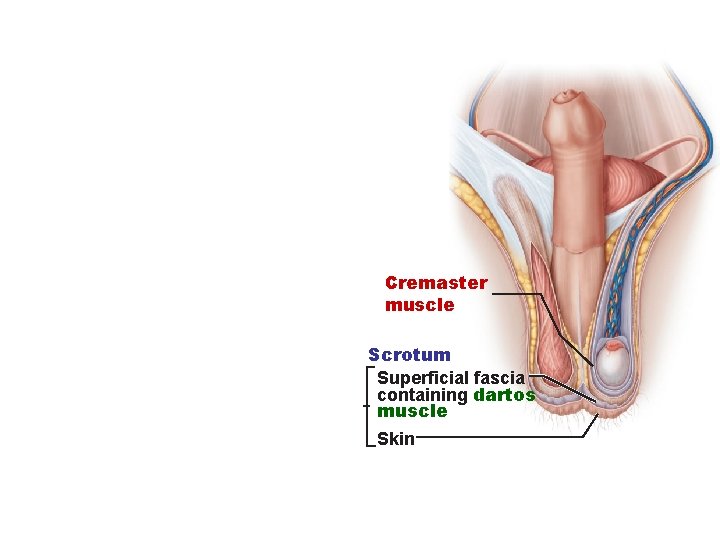
Cremaster muscle Scrotum Superficial fascia containing dartos muscle Skin
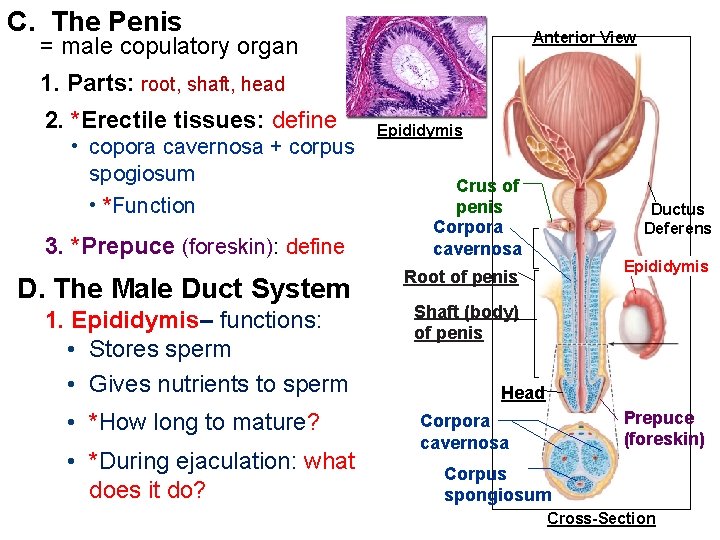
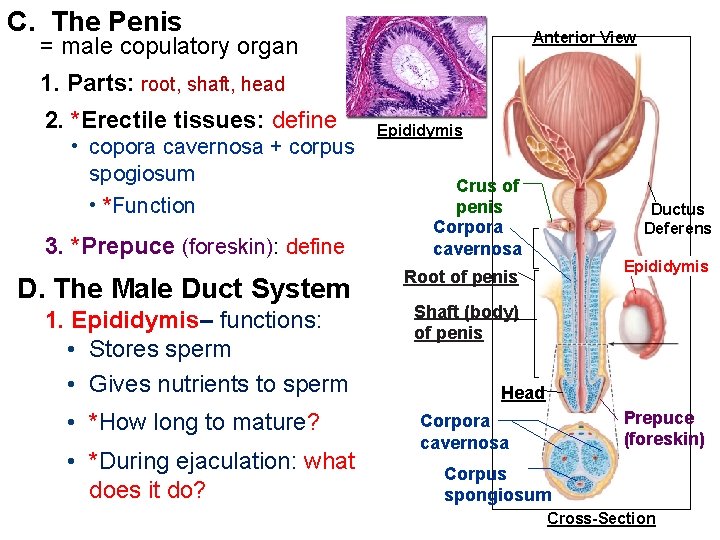
C. The Penis Anterior View = male copulatory organ 1. Parts: root, shaft, head 2. *Erectile tissues: define • copora cavernosa + corpus spogiosum • *Function 3. *Prepuce (foreskin): define D. The Male Duct System Epididymis Crus of penis Corpora cavernosa Epididymis Root of penis 1. Epididymis– functions: • Stores sperm • Gives nutrients to sperm Shaft (body) of penis • *How long to mature? Corpora cavernosa • *During ejaculation: what does it do? Ductus Deferens Head Prepuce (foreskin) Corpus spongiosum Cross-Section
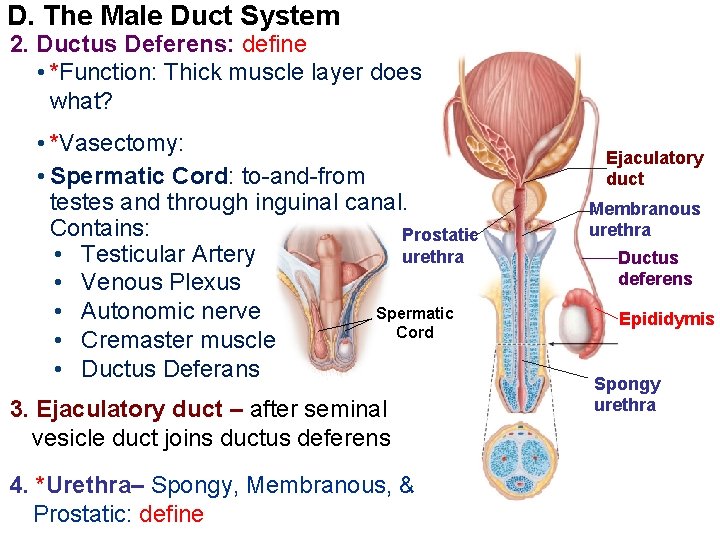
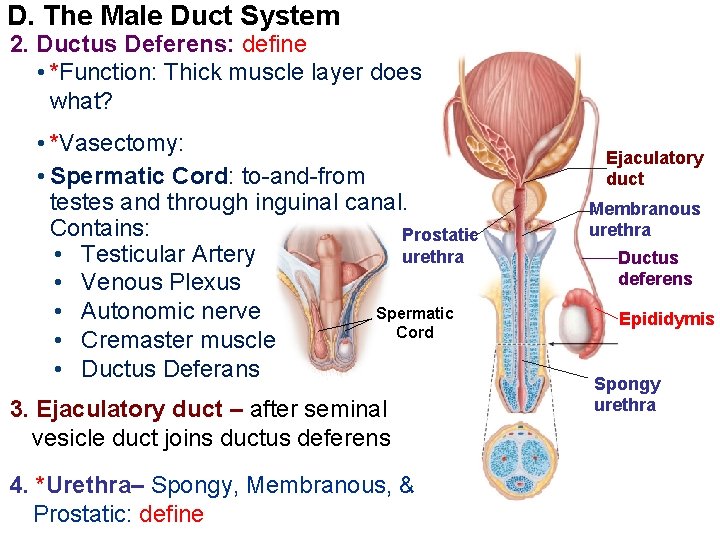
D. The Male Duct System 2. Ductus Deferens: define • *Function: Thick muscle layer does what? • *Vasectomy: • Spermatic Cord: to-and-from testes and through inguinal canal. Contains: Prostatic • Testicular Artery urethra • Venous Plexus Spermatic • Autonomic nerve Cord • Cremaster muscle • Ductus Deferans 3. Ejaculatory duct – after seminal vesicle duct joins ductus deferens 4. *Urethra– Spongy, Membranous, & Prostatic: define Ejaculatory duct Membranous urethra Ductus deferens Epididymis Spongy urethra
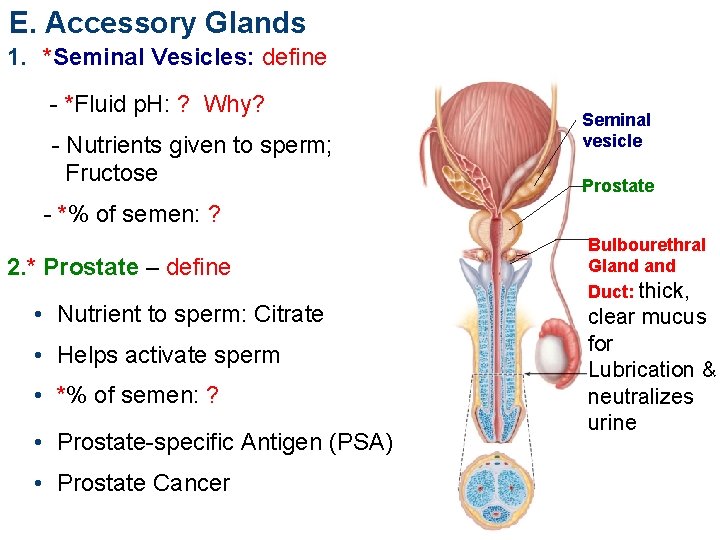
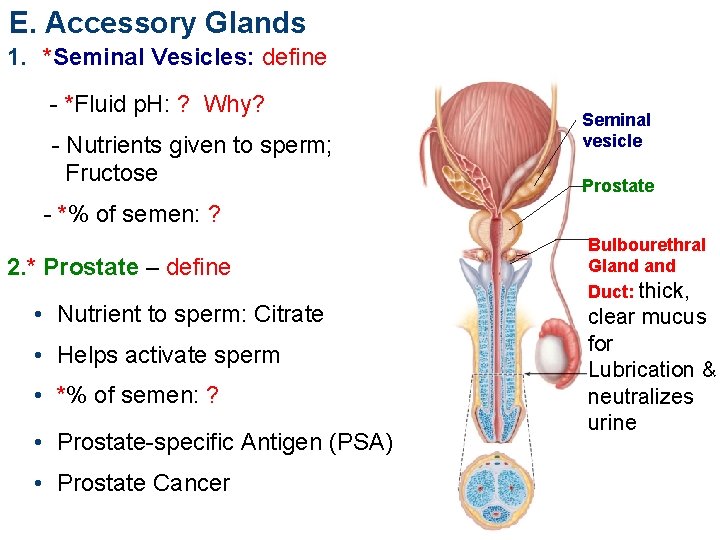
E. Accessory Glands 1. *Seminal Vesicles: define - *Fluid p. H: ? Why? - Nutrients given to sperm; Fructose Seminal vesicle Prostate - *% of semen: ? 2. * Prostate – define • Nutrient to sperm: Citrate • Helps activate sperm • *% of semen: ? • Prostate-specific Antigen (PSA) • Prostate Cancer Bulbourethral Gland Duct: thick, clear mucus for Lubrication & neutralizes urine
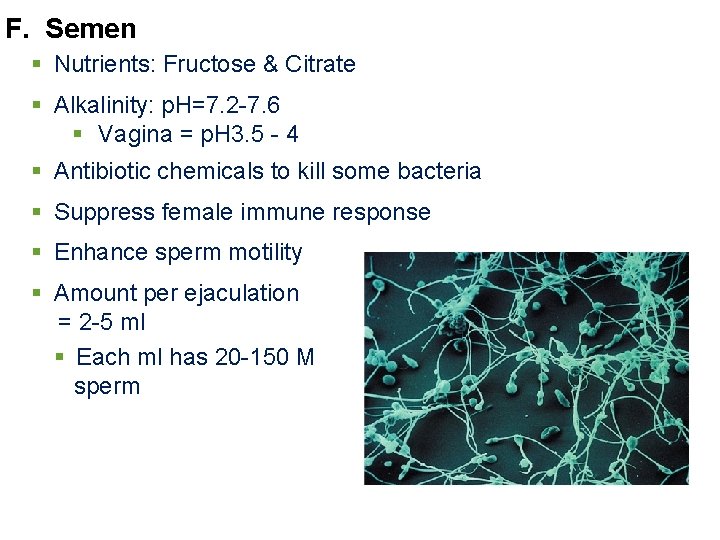
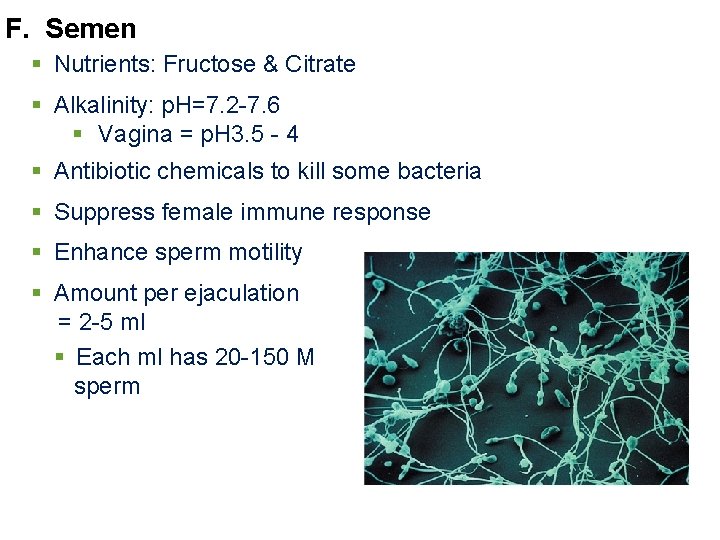
F. Semen § Nutrients: Fructose & Citrate § Alkalinity: p. H=7. 2 -7. 6 § Vagina = p. H 3. 5 - 4 § Antibiotic chemicals to kill some bacteria § Suppress female immune response § Enhance sperm motility § Amount per ejaculation = 2 -5 ml § Each ml has 20 -150 M sperm
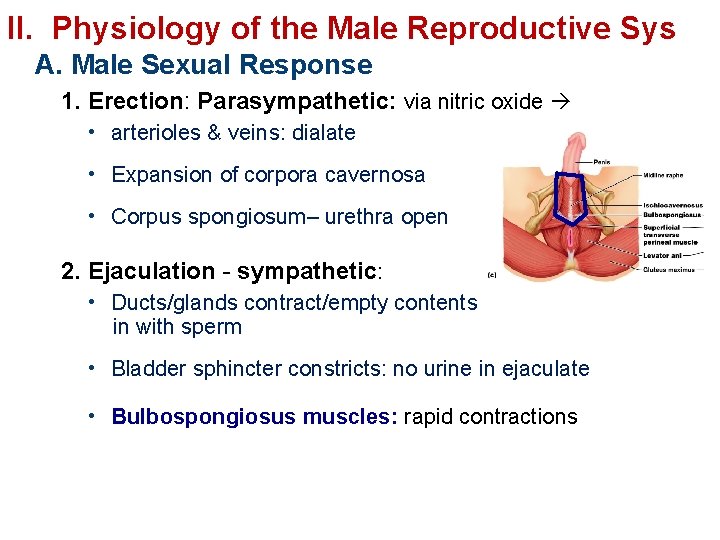
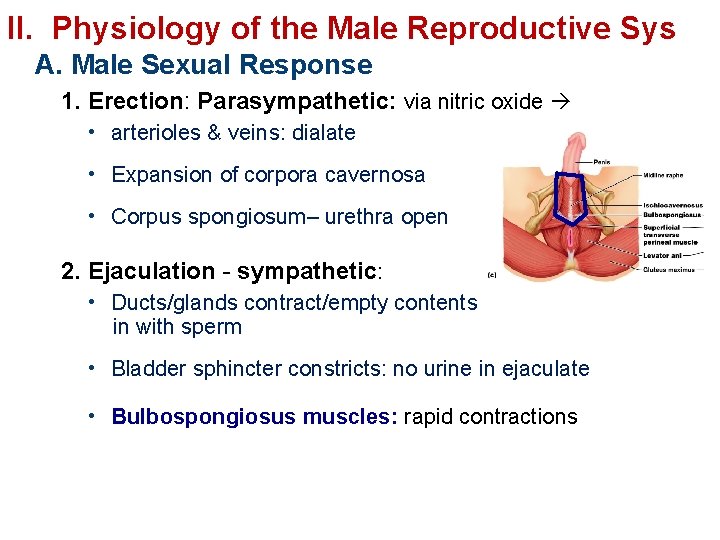
II. Physiology of the Male Reproductive Sys A. Male Sexual Response 1. Erection: Parasympathetic: via nitric oxide • arterioles & veins: dialate • Expansion of corpora cavernosa • Corpus spongiosum– urethra open 2. Ejaculation - sympathetic: • Ducts/glands contract/empty contents in with sperm • Bladder sphincter constricts: no urine in ejaculate • Bulbospongiosus muscles: rapid contractions
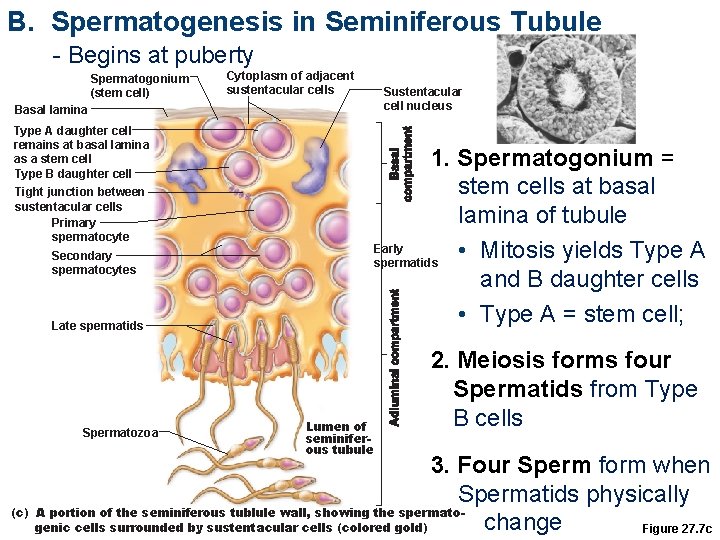
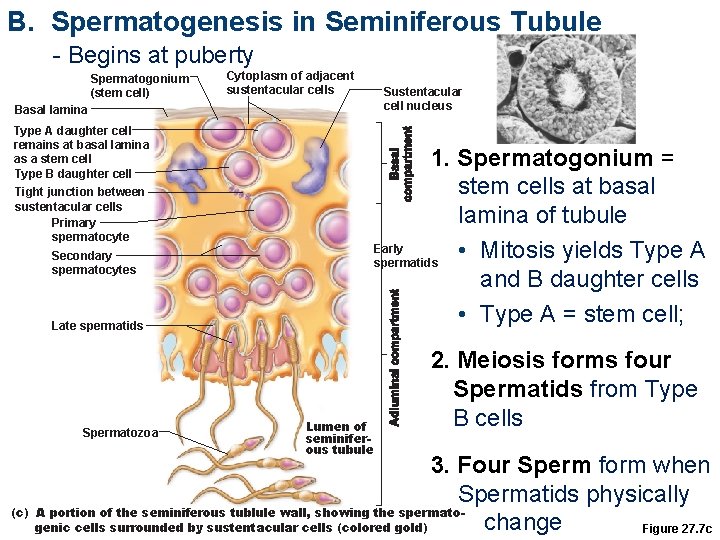
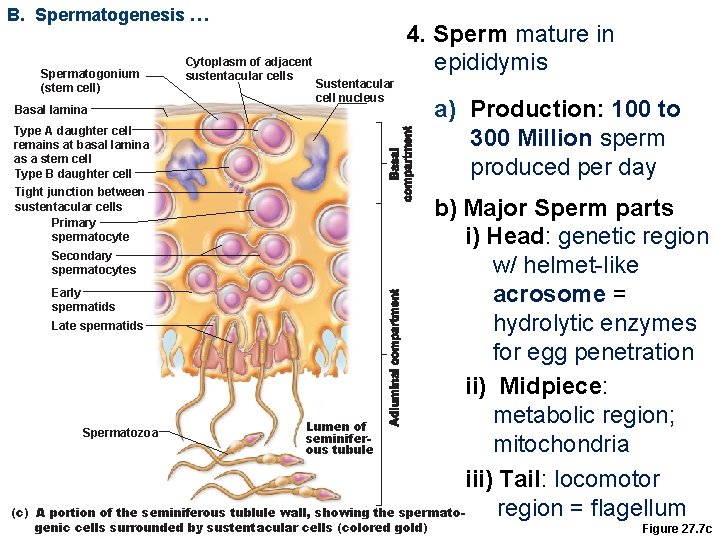
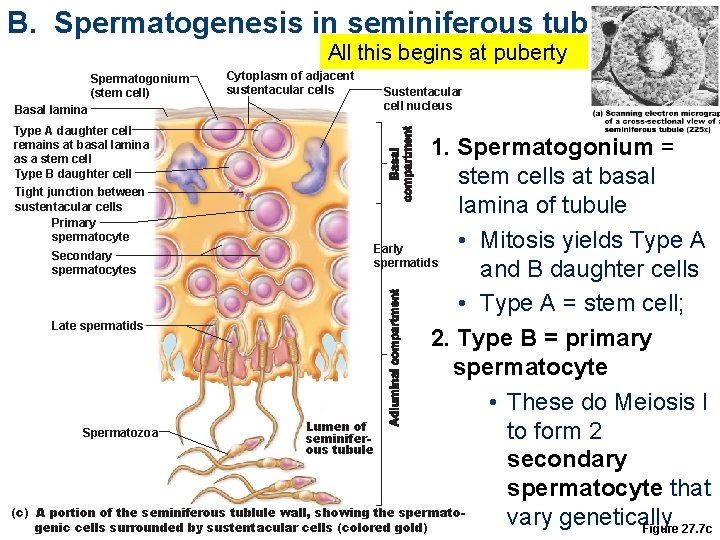
B. Spermatogenesis in Seminiferous Tubule - Begins at puberty Spermatogonium (stem cell) Cytoplasm of adjacent sustentacular cells Basal lamina Type A daughter cell remains at basal lamina as a stem cell Type B daughter cell Tight junction between sustentacular cells Primary spermatocyte 1. Spermatogonium = stem cells at basal lamina of tubule Early • Mitosis yields Type A spermatids and B daughter cells • Type A = stem cell; Secondary spermatocytes Late spermatids Spermatozoa Sustentacular cell nucleus Lumen of seminiferous tubule 2. Meiosis forms four Spermatids from Type B cells 3. Four Sperm form when Spermatids physically (c) A portion of the seminiferous tublule wall, showing the spermatochange genic cells surrounded by sustentacular cells (colored gold) Figure 27. 7 c
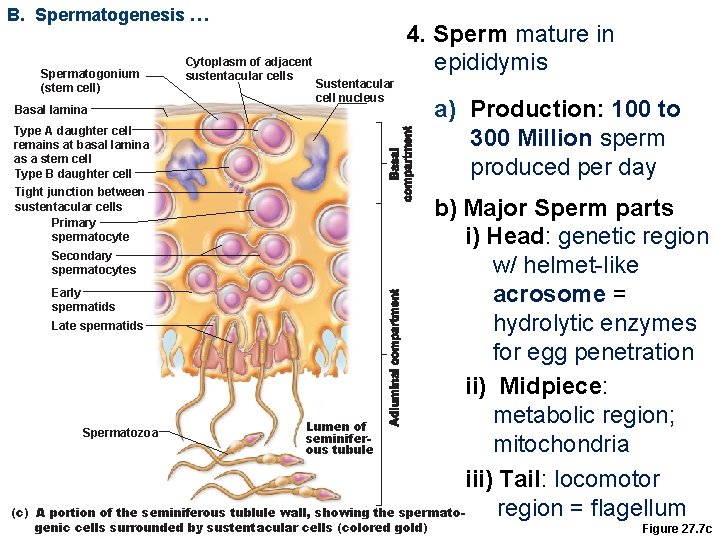
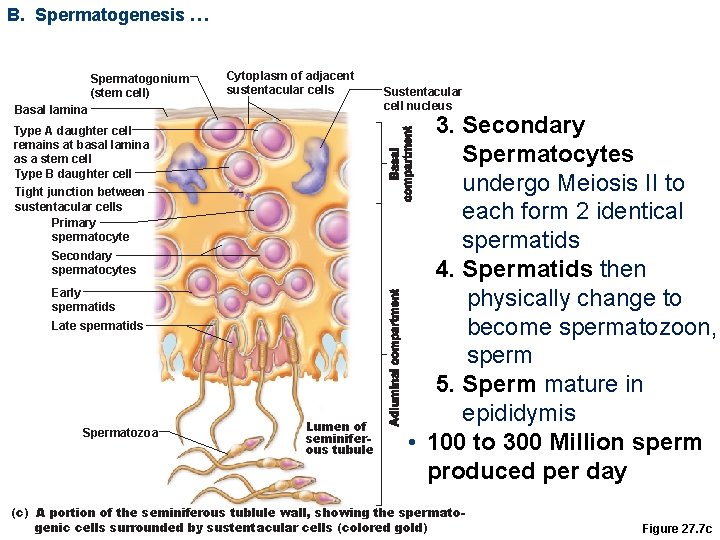
B. Spermatogenesis … Spermatogonium (stem cell) Basal lamina Cytoplasm of adjacent sustentacular cells 4. Sperm mature in epididymis Sustentacular cell nucleus Type A daughter cell remains at basal lamina as a stem cell Type B daughter cell Tight junction between sustentacular cells Primary spermatocyte (c) a) Production: 100 to 300 Million sperm produced per day b) Major Sperm parts i) Head: genetic region Secondary w/ helmet-like spermatocytes Early acrosome = spermatids Late spermatids hydrolytic enzymes for egg penetration ii) Midpiece: metabolic region; Lumen of Spermatozoa seminifermitochondria ous tubule iii) Tail: locomotor region = flagellum A portion of the seminiferous tublule wall, showing the spermato- genic cells surrounded by sustentacular cells (colored gold) Figure 27. 7 c
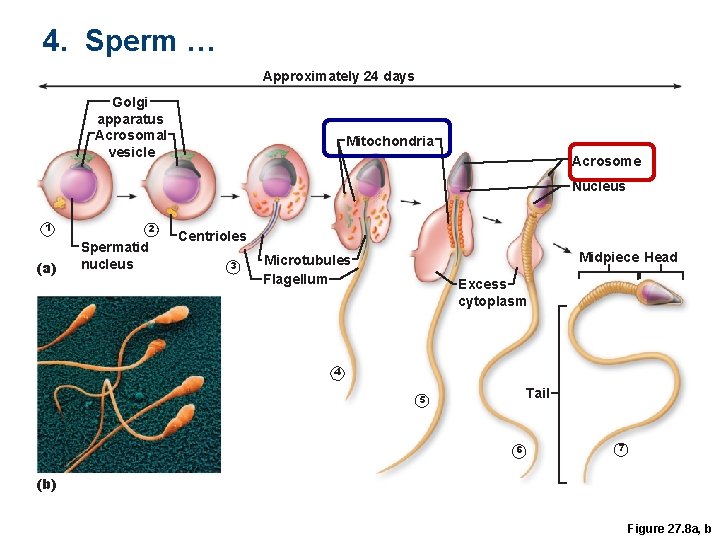
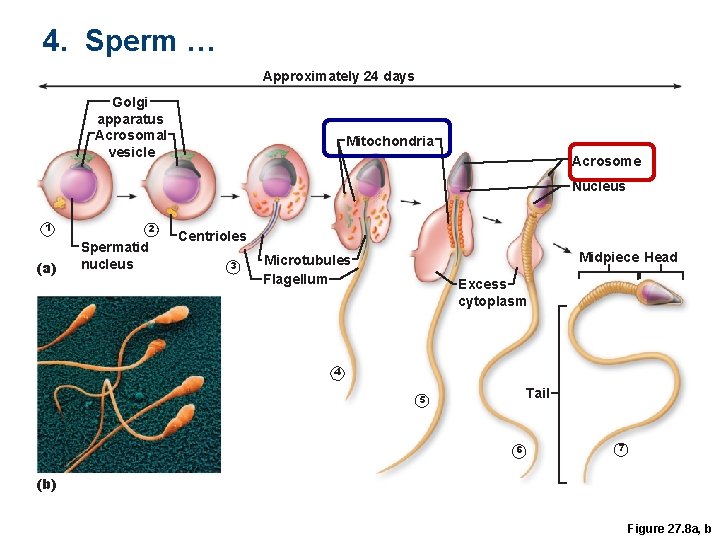
4. Sperm … Approximately 24 days Golgi apparatus Acrosomal vesicle Mitochondria Acrosome Nucleus 1 (a) 2 Spermatid nucleus Centrioles 3 Midpiece Head Microtubules Flagellum Excess cytoplasm 4 Tail 5 6 7 (b) Figure 27. 8 a, b
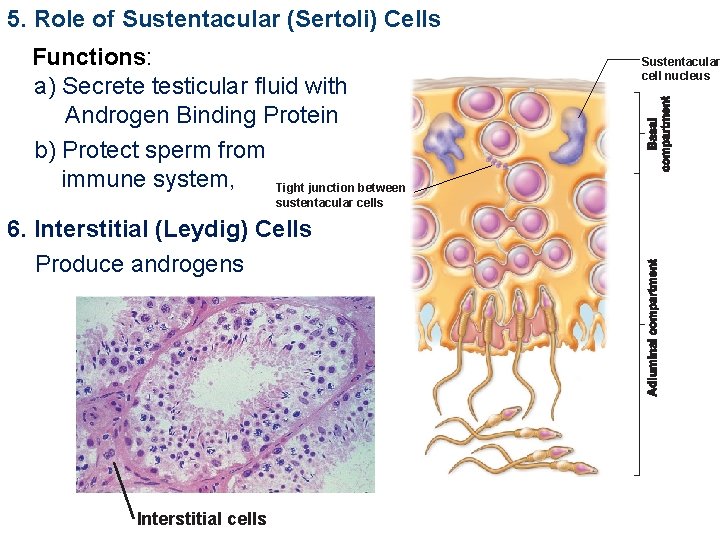
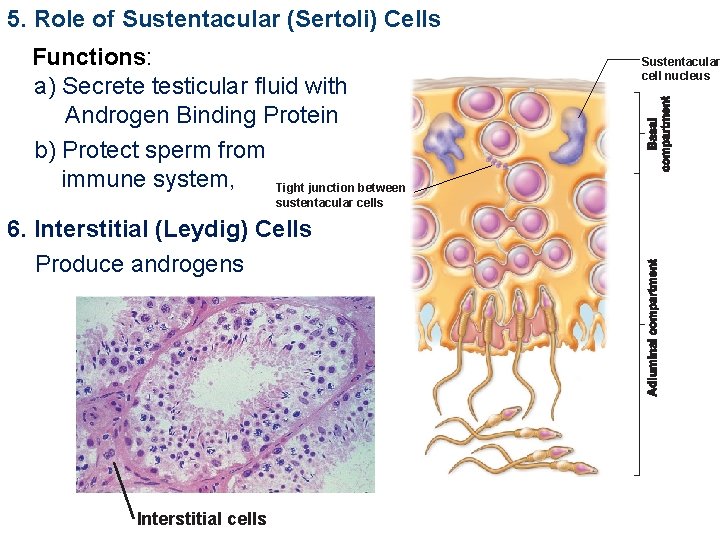
5. Role of Sustentacular (Sertoli) Cells Functions: a) Secrete testicular fluid with Androgen Binding Protein b) Protect sperm from immune system, Tight junction between sustentacular cells 6. Interstitial (Leydig) Cells Produce androgens Interstitial cells Sustentacular cell nucleus
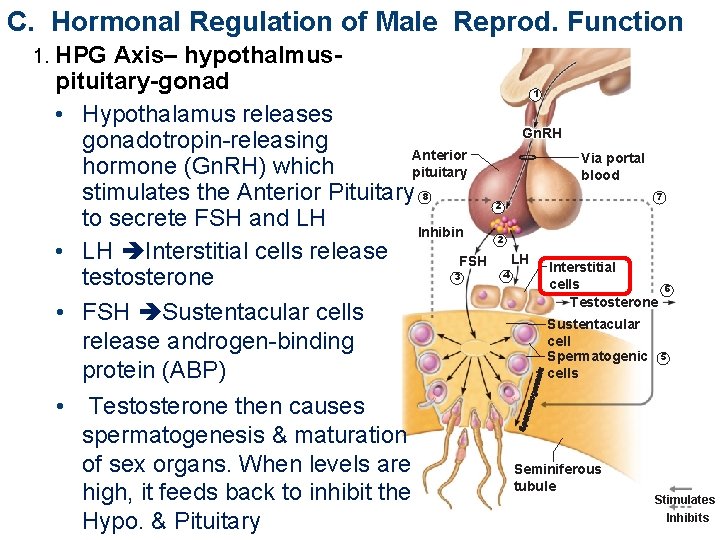
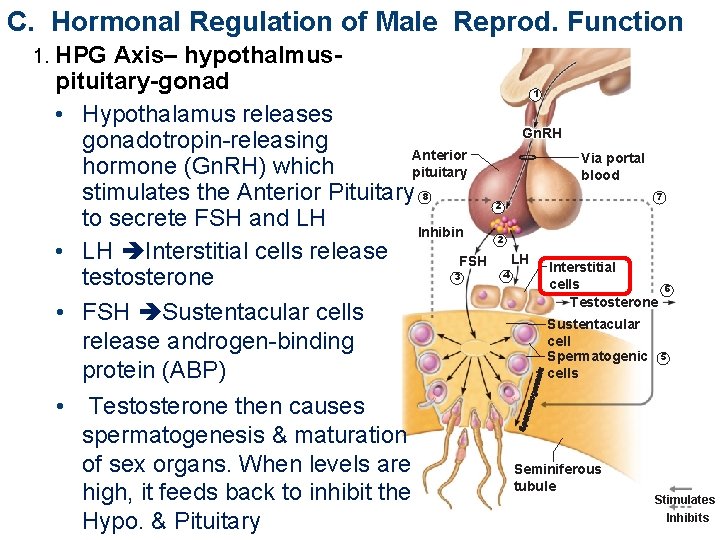
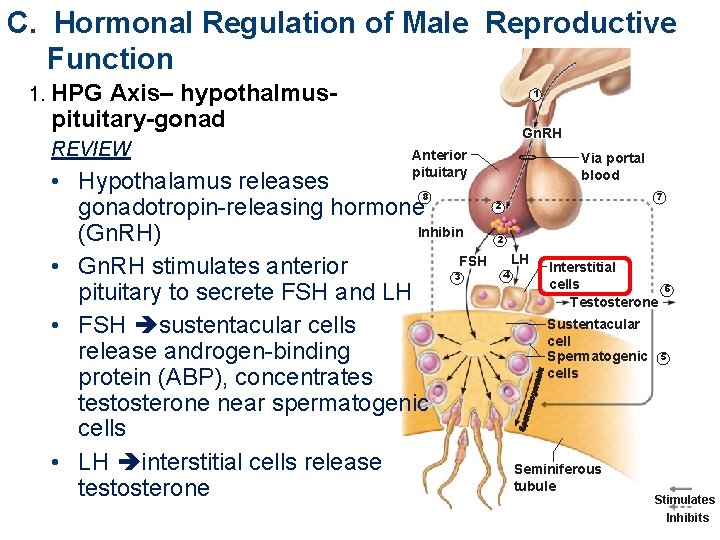
C. Hormonal Regulation of Male Reprod. Function 1. HPG Axis– hypothalmuspituitary-gonad • Hypothalamus releases gonadotropin-releasing Anterior hormone (Gn. RH) which pituitary stimulates the Anterior Pituitary 8 to secrete FSH and LH Inhibin • LH Interstitial cells release FSH 3 testosterone • FSH Sustentacular cells release androgen-binding protein (ABP) • Testosterone then causes spermatogenesis & maturation of sex organs. When levels are high, it feeds back to inhibit the Hypo. & Pituitary 1 Gn. RH Via portal blood 7 2 2 4 LH Interstitial cells Testosterone Sustentacular cell Spermatogenic cells Seminiferous tubule 6 5 Stimulates Inhibits
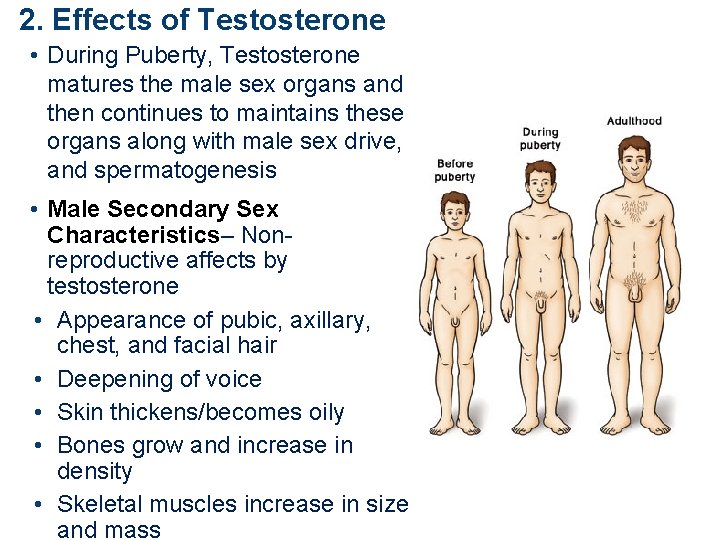
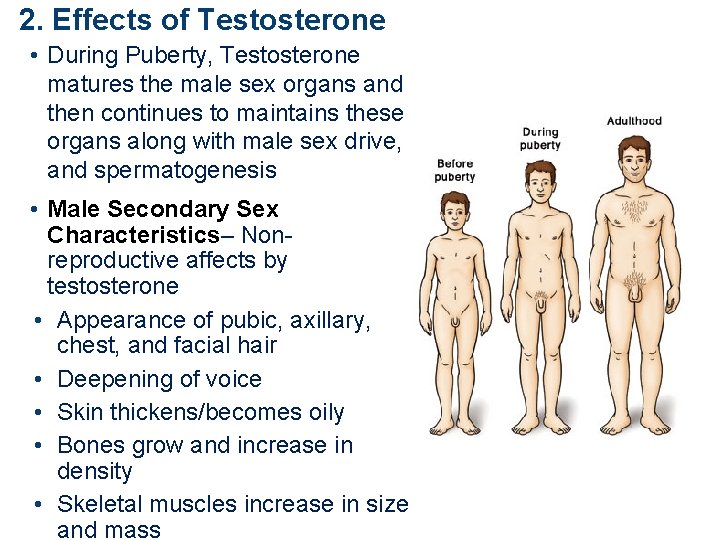
2. Effects of Testosterone • During Puberty, Testosterone matures the male sex organs and then continues to maintains these organs along with male sex drive, and spermatogenesis • Male Secondary Sex Characteristics– Nonreproductive affects by testosterone • Appearance of pubic, axillary, chest, and facial hair • Deepening of voice • Skin thickens/becomes oily • Bones grow and increase in density • Skeletal muscles increase in size and mass
Next ppt part-b Copyright © 2010 Pearson Education, Inc.
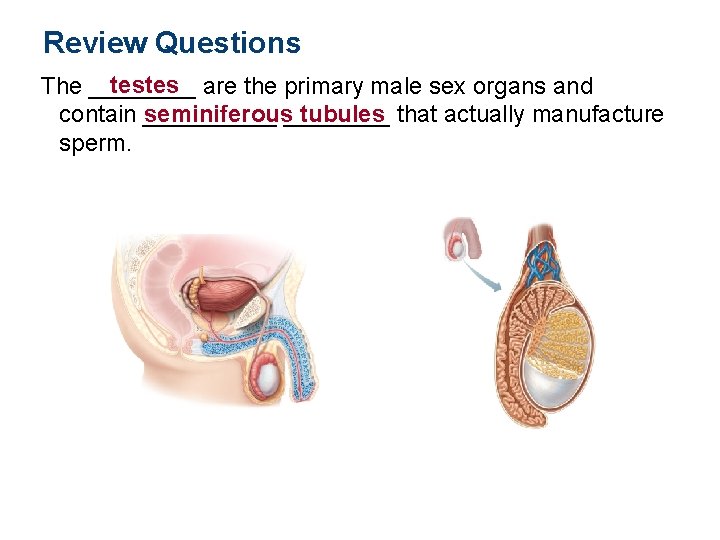
Review Questions testes are the primary male sex organs and The ____ contain _____ seminiferous____ tubules that actually manufacture sperm.
Review Questions Gametes are generated through a cell division meiosis process called _____ 4 which creates up to ___ haploid cells, each with 23 chromosomes in _____ humans.
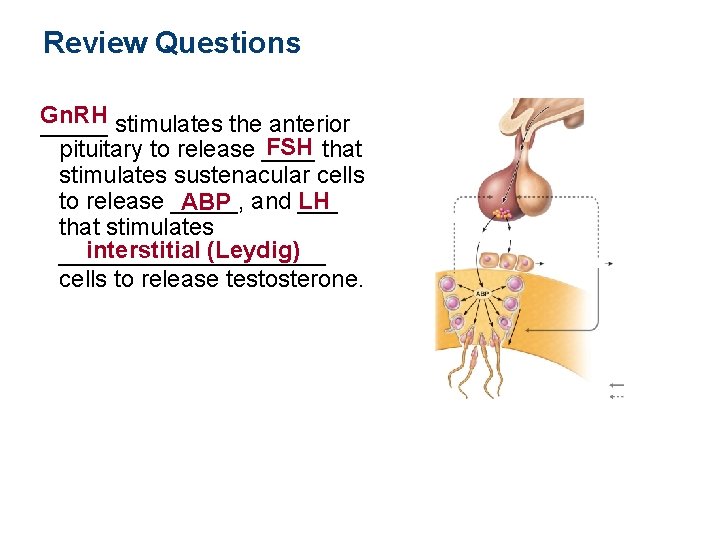
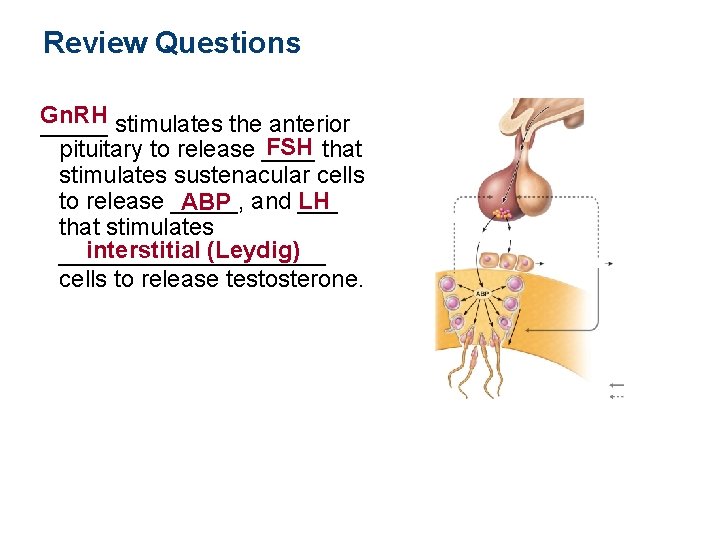
Review Questions Gn. RH _____ stimulates the anterior FSH that pituitary to release ____ stimulates sustenacular cells to release _____, ___ ABP and LH that stimulates interstitial (Leydig) __________ cells to release testosterone.
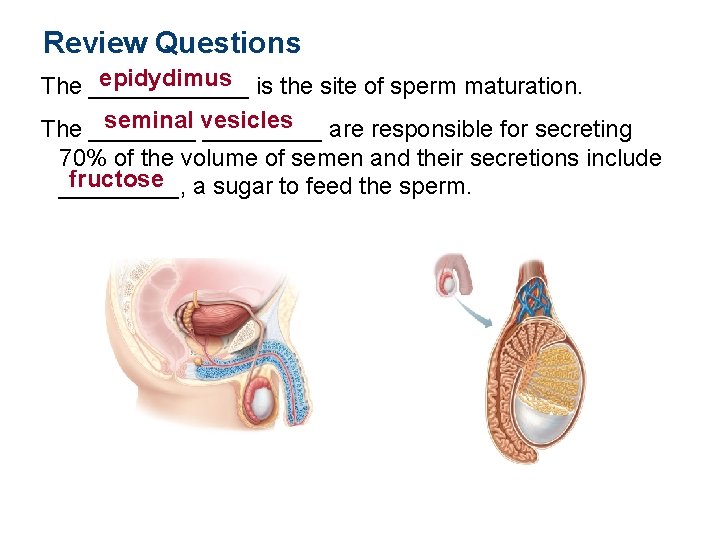
Review Questions epidydimus is the site of sperm maturation. The ______ seminal vesicles The _________ are responsible for secreting 70% of the volume of semen and their secretions include fructose a sugar to feed the sperm. _____,
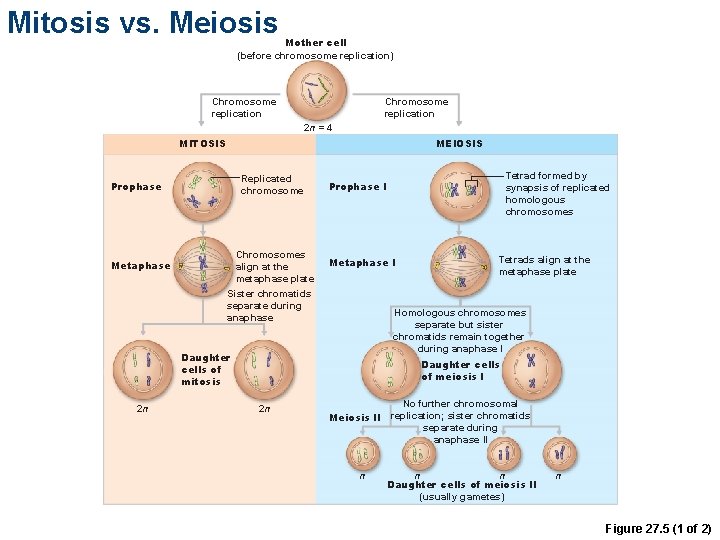
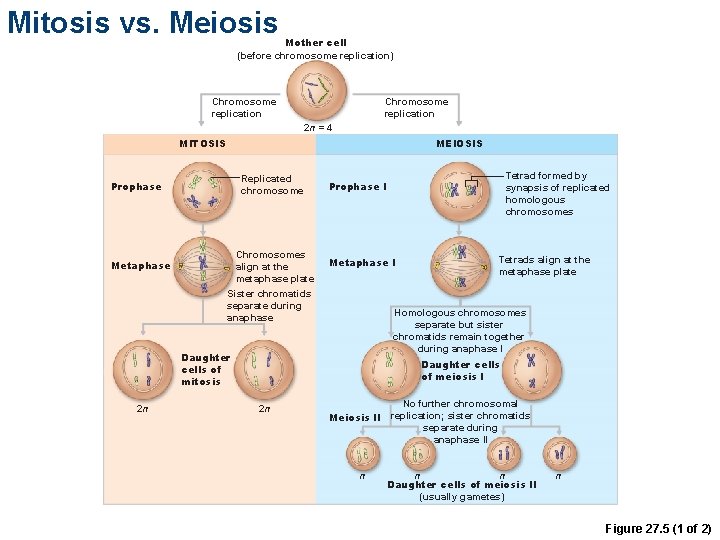
Mitosis vs. Meiosis Mother cell (before chromosome replication) Chromosome replication 2 n = 4 MITOSIS MEIOSIS Replicated chromosome Prophase Metaphase Chromosomes align at the metaphase plate Sister chromatids separate during anaphase Metaphase I Tetrads align at the metaphase plate Homologous chromosomes separate but sister chromatids remain together during anaphase I Daughter cells of mitosis 2 n Tetrad formed by synapsis of replicated homologous chromosomes Prophase I Daughter cells of meiosis I 2 n No further chromosomal replication; sister chromatids Meiosis II separate during anaphase II n n n Daughter cells of meiosis II (usually gametes) n Figure 27. 5 (1 of 2)
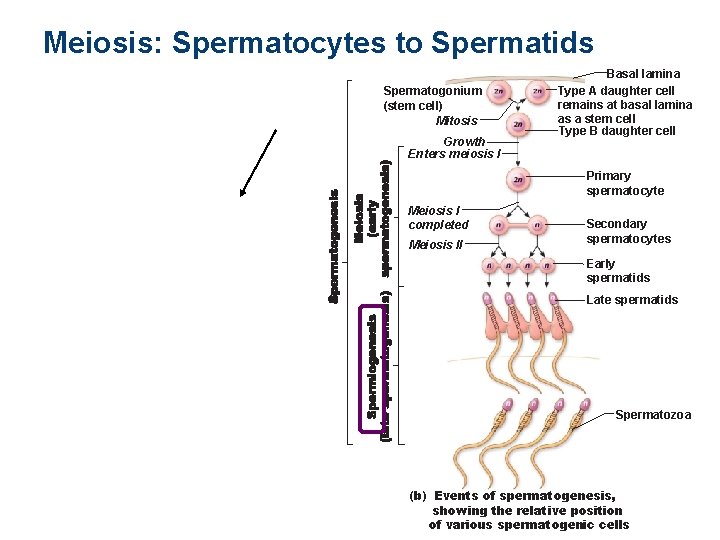
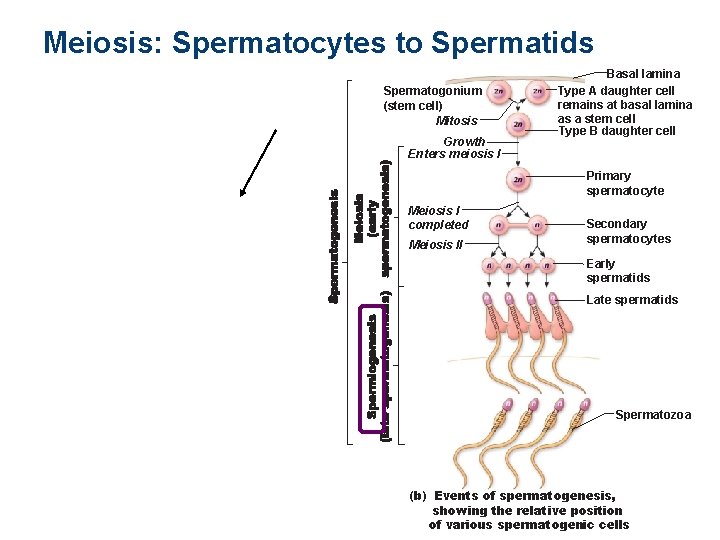
Meiosis: Spermatocytes to Spermatids Spermatogonium (stem cell) Mitosis Growth Enters meiosis I Basal lamina Type A daughter cell remains at basal lamina as a stem cell Type B daughter cell Primary spermatocyte Meiosis I completed Meiosis II Secondary spermatocytes Early spermatids Late spermatids Spermatozoa (b) Events of spermatogenesis, showing the relative position of various spermatogenic cells
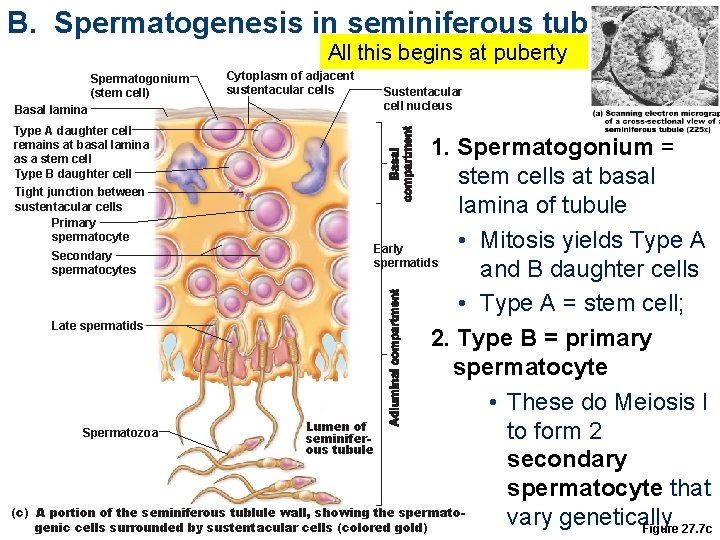
B. Spermatogenesis in seminiferous tubule All this begins at puberty Spermatogonium (stem cell) Basal lamina Type A daughter cell remains at basal lamina as a stem cell Type B daughter cell Tight junction between sustentacular cells Primary spermatocyte Cytoplasm of adjacent sustentacular cells Sustentacular cell nucleus 1. Spermatogonium = stem cells at basal lamina of tubule • Mitosis yields Type A Early Secondary spermatids spermatocytes and B daughter cells • Type A = stem cell; Late spermatids 2. Type B = primary spermatocyte • These do Meiosis I Lumen of Spermatozoa to form 2 seminiferous tubule secondary spermatocyte that (c) A portion of the seminiferous tublule wall, showing the spermatovary genetically genic cells surrounded by sustentacular cells (colored gold) Figure 27. 7 c
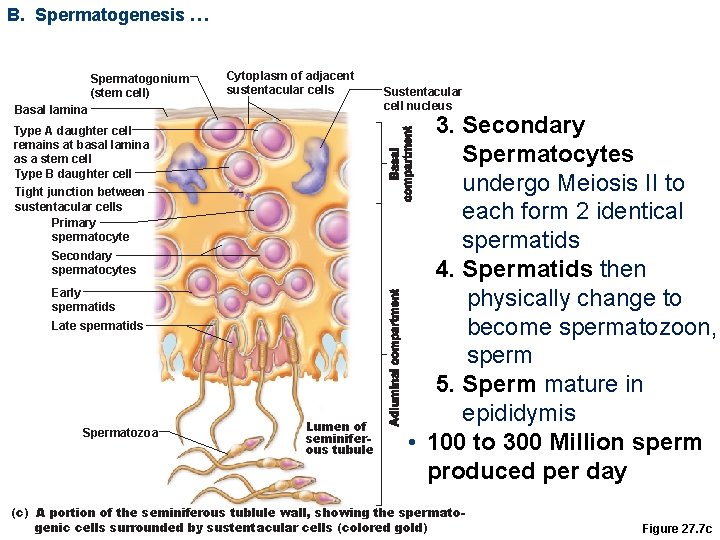
B. Spermatogenesis … Spermatogonium (stem cell) Cytoplasm of adjacent sustentacular cells Basal lamina Type A daughter cell remains at basal lamina as a stem cell Type B daughter cell Tight junction between sustentacular cells Primary spermatocyte Secondary spermatocytes Early spermatids Late spermatids Spermatozoa Lumen of seminiferous tubule Sustentacular cell nucleus 3. Secondary Spermatocytes undergo Meiosis II to each form 2 identical spermatids 4. Spermatids then physically change to become spermatozoon, sperm 5. Sperm mature in epididymis • 100 to 300 Million sperm produced per day (c) A portion of the seminiferous tublule wall, showing the spermatogenic cells surrounded by sustentacular cells (colored gold) Figure 27. 7 c
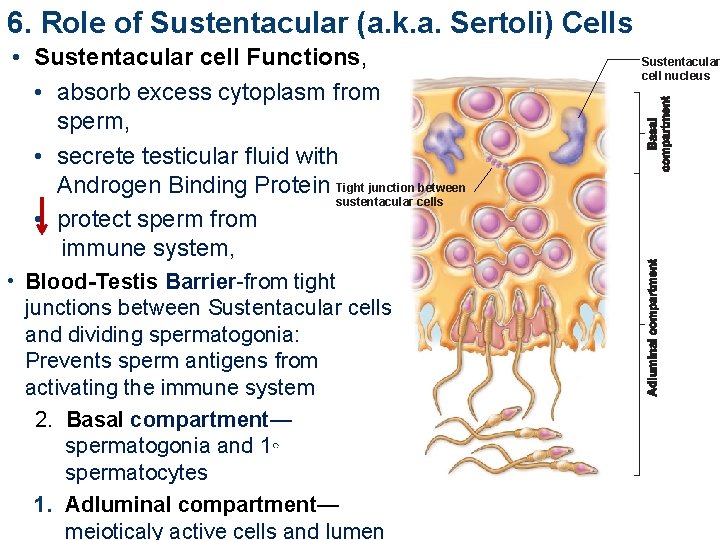
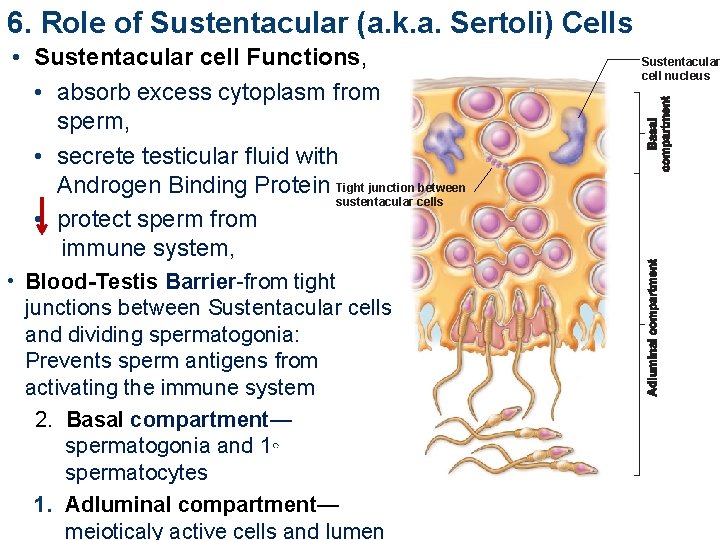
6. Role of Sustentacular (a. k. a. Sertoli) Cells • Sustentacular cell Functions, • absorb excess cytoplasm from sperm, • secrete testicular fluid with Androgen Binding Protein Tight junction between sustentacular cells • protect sperm from immune system, • Blood-Testis Barrier-from tight junctions between Sustentacular cells and dividing spermatogonia: Prevents sperm antigens from activating the immune system 2. Basal compartment— spermatogonia and 1◦ spermatocytes 1. Adluminal compartment— meioticaly active cells and lumen Sustentacular cell nucleus
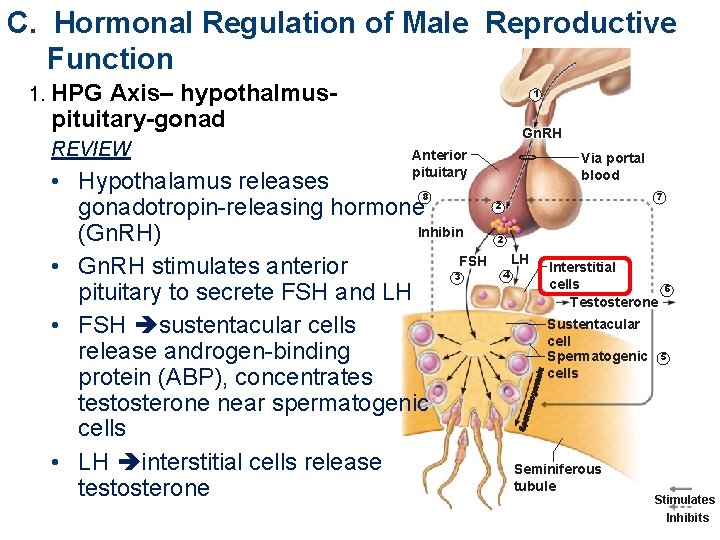
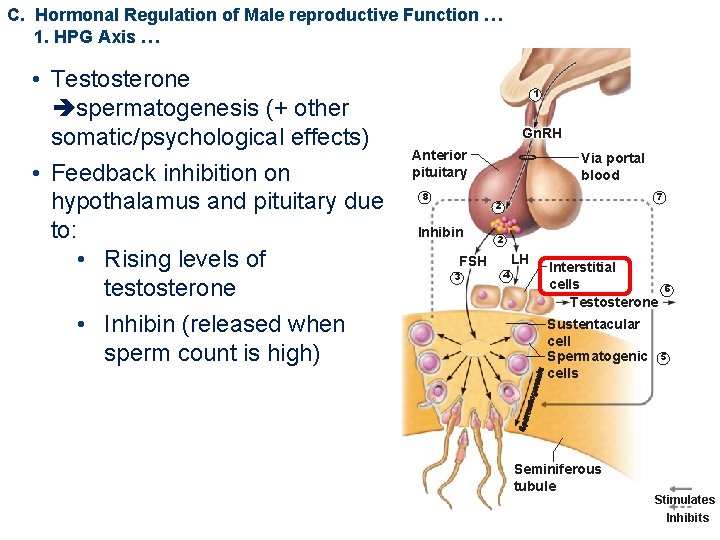
C. Hormonal Regulation of Male Reproductive Function 1. HPG Axis– hypothalmuspituitary-gonad REVIEW 1 Gn. RH Anterior pituitary • Hypothalamus releases 8 gonadotropin-releasing hormone Inhibin (Gn. RH) FSH • Gn. RH stimulates anterior 3 pituitary to secrete FSH and LH • FSH sustentacular cells release androgen-binding protein (ABP), concentrates testosterone near spermatogenic cells • LH interstitial cells release testosterone Via portal blood 7 2 2 4 LH Interstitial cells Testosterone Sustentacular cell Spermatogenic cells Seminiferous tubule 6 5 Stimulates Inhibits
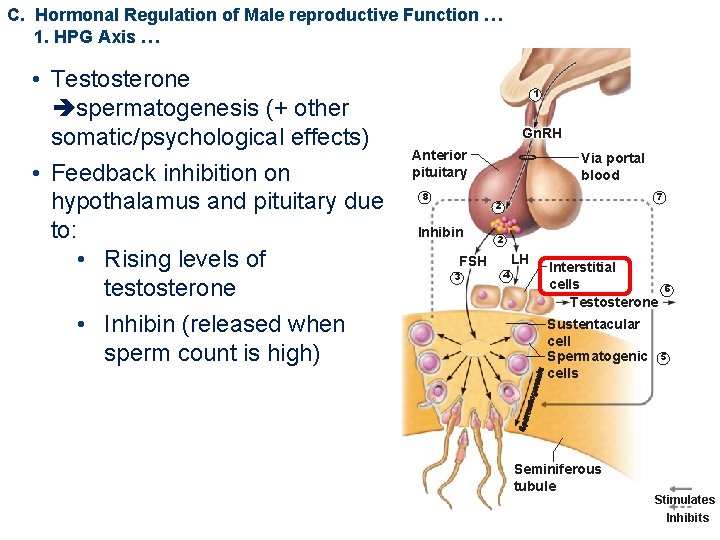
C. Hormonal Regulation of Male reproductive Function … 1. HPG Axis … • Testosterone spermatogenesis (+ other somatic/psychological effects) • Feedback inhibition on hypothalamus and pituitary due to: • Rising levels of testosterone • Inhibin (released when sperm count is high) 1 Gn. RH Anterior pituitary 8 Via portal blood 7 2 Inhibin FSH 3 2 4 LH Interstitial cells Testosterone Sustentacular cell Spermatogenic cells Seminiferous tubule 6 5 Stimulates Inhibits
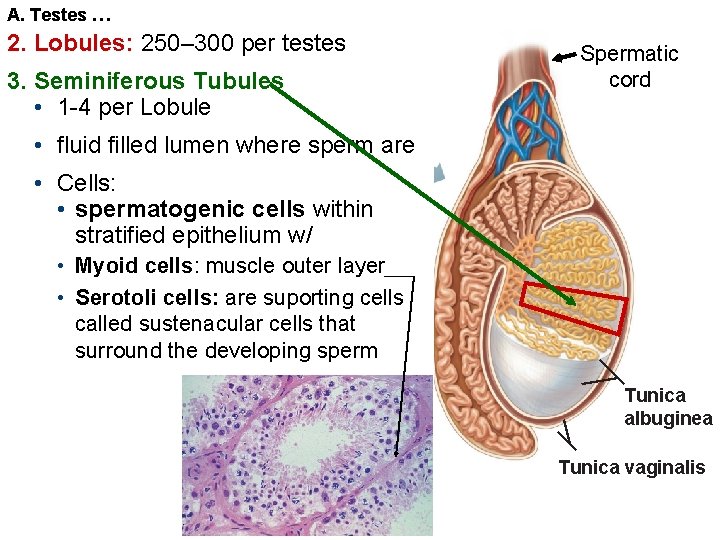
A. Testes … 2. Lobules: 250– 300 per testes 3. Seminiferous Tubules • 1 -4 per Lobule Spermatic cord • fluid filled lumen where sperm are • Cells: • spermatogenic cells within stratified epithelium w/ • Myoid cells: muscle outer layer • Serotoli cells: are suporting cells called sustenacular cells that surround the developing sperm Tunica albuginea Tunica vaginalis