CH 19 FOODDRUG INTERACTIONS Fooddrug interactions can Alter








- Slides: 30

CH 19 FOOD-DRUG INTERACTIONS Food-drug interactions can - Alter the intended response to the medication - Cause drug toxicity - Alter the normal nutritional status.
I. Pharmacologic Aspects of Food-Drug Interactions Two types: 1. Pharmacodynamic interactions - affect the pharmacologic action of the drug 2. Pharmacokinetic interactions - affect the movement of the drug into, around, or out of the body
1. Pharmacodynamics: - Studying the biochemical and physiologic effects of a drug - Mechanism of action of a drug: binding of the drug mol. to receptor, enzyme, or ion channel→ physiologic response. *Agonist: Enhance normal metabolism and physiologic function *Antagonist: Attenuate normal metabolism and physiologic function
2. Pharmacokinetics – the study of the time course of a drug in the body, including absorption , distribution, metabolism (biotransformation), excretion. (1) Absorption – from the adm. Site to blood stream a. route of administration iv: intravenous im: intramuscular ip: intraperitoneal Sc: subcutaneous b. the chemistry of the drug and its ability to cross biologic membranes c. the rate of gastric emptying and GI movement d. the quality of the product formulation.
(2) Distribution – drug leaves the systemic circulation and travels to various regions of the body, - the drug’s chemistry and ability to cross biologic membranes. - the rate and extent of blood flow - bound form or unbound fraction

(3) Biotransformation (metabolism) of drugs: major in the liver. - cytochrome P-450 enzyme system (Fig 12 -2, p 311), substances ↑or↓ this enzyme system may change the rate or extent of drug metabolism.
(4) Excretion: - Renal excretion: Glomerular filtration or tubular secretion Ex. Urinary p. H – affect tubular reabsorption - Bile or other body fluid, lesser extent.
II. Risk factors for Drug-Nutrient Interactions 1. Drug-induced malnutrition – most commonly during long-term treatment for chronic disease 2. Existing malnutrition places people at risk for drug-nutrient interactions 3. Specific nutrient deficiencies can affect drug metabolism by influencing the MFOS 4. Body composition - drug response
Pharmacogenomics – Genetically determined variations that are revealed solely by the effects of drugs. Ex. (1) Slow acetylators: lower levels of the hepatic enzyme acetyl transferase → (a) INH (isoniazid) user: ↑risk of pyridoxine def. (b) phenelzine (MAO inhibitor) user: ↑risk of HTN if ingest foods high in tyramine (Box 19 -2) (2) G 6 PD deficiency: X-chromosome-linked def. of G 6 PD in RBC - Fava beans or pollen cause acute hemolysis

III. EFFECT OF FOOD ON DRUG THERAPY 1. Effect on Drug Absorption: The presence of food and nutrients in the stomach or GI lumen →↓drug abs. Ex. : abs. of Fe may be ↓ 50% when taken with food

- Mechanisms (1) Rate of the gastric empty (2) Chelation – drugs and divalent or trivalent cations (3) Adsorption (4) GI p. H

2. Medication and Enteral Nutrition Interactions - Liquid medication mixed with enteral feeding formulas (1) cause granulation and gel formation (2) Emulsion breakage
3. Drug Distribution low serum Alb. →↑unbound fraction drug →↑risk for adverse effects from highly proteinbound drugs Ex. : Anticoagulant - warfarin, anticonvulsant - phenytoin
4. Effect on Drug Metabolism - Enzymes in GI & liver – account for a large portion of the drug meta. (1) Hi-protein, Lo-CHO diet →↑the hepatic metabolism of theophylline (antiasthma drug) (2) Substance found in grapefruit can inhibit the intestinal metabolism of drugs →↑drug in the circulation →↑toxicity. (3) Competition between food and drugs with hepatic enzymes →↑drug in the circulation →↑toxicity
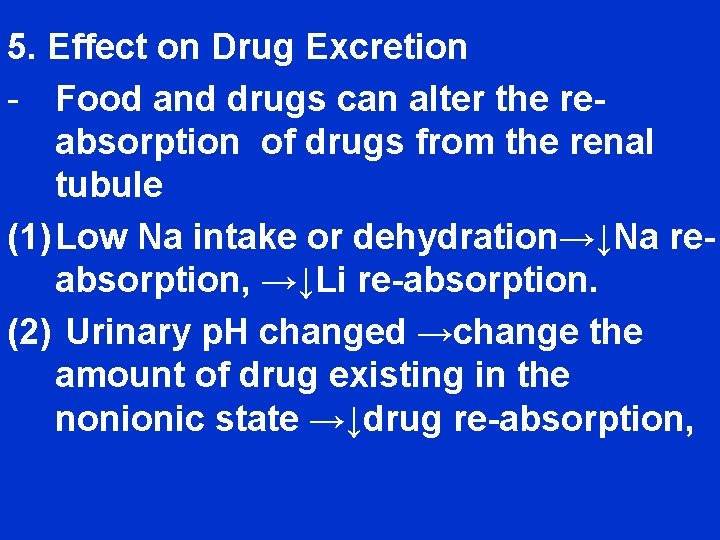
5. Effect on Drug Excretion - Food and drugs can alter the reabsorption of drugs from the renal tubule (1) Low Na intake or dehydration→↓Na reabsorption, →↓Li re-absorption. (2) Urinary p. H changed →change the amount of drug existing in the nonionic state →↓drug re-absorption,
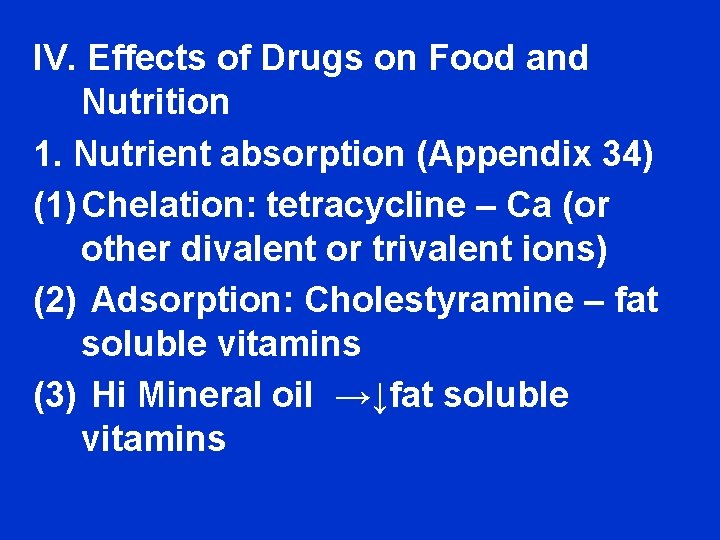
IV. Effects of Drugs on Food and Nutrition 1. Nutrient absorption (Appendix 34) (1) Chelation: tetracycline – Ca (or other divalent or trivalent ions) (2) Adsorption: Cholestyramine – fat soluble vitamins (3) Hi Mineral oil →↓fat soluble vitamins
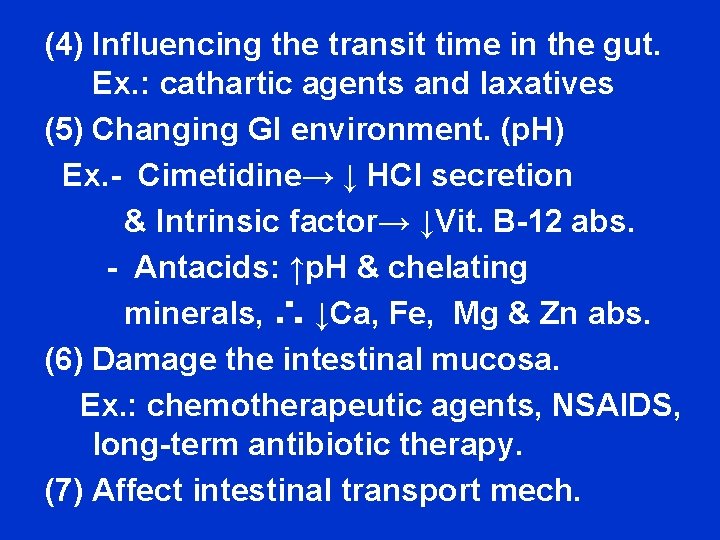
(4) Influencing the transit time in the gut. Ex. : cathartic agents and laxatives (5) Changing GI environment. (p. H) Ex. - Cimetidine→ ↓ HCl secretion & Intrinsic factor→ ↓Vit. B-12 abs. - Antacids: ↑p. H & chelating minerals, ∴ ↓Ca, Fe, Mg & Zn abs. (6) Damage the intestinal mucosa. Ex. : chemotherapeutic agents, NSAIDS, long-term antibiotic therapy. (7) Affect intestinal transport mech.

2. Nutrient Metabolism – - Drugs →↓or ↑nutrient metabolism Ex. : (1) phenobarbital and phenytoin (anticonvulsants) → ↑Vit. D, K and folic acid meta. (2) INH (anti-tuberculosis): blocks the conversion of pyridoxine → PLP (3) MTX: a folic acid antagonist →↓folate to be active form →megaloblastic anemia
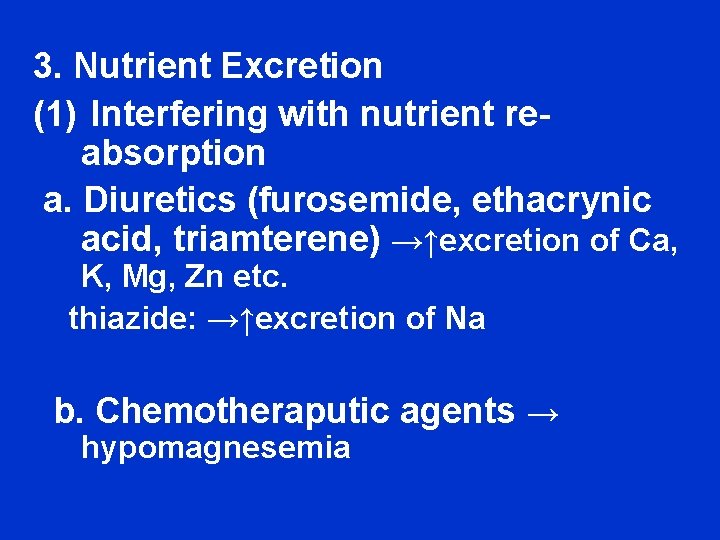
3. Nutrient Excretion (1) Interfering with nutrient reabsorption a. Diuretics (furosemide, ethacrynic acid, triamterene) →↑excretion of Ca, K, Mg, Zn etc. thiazide: →↑excretion of Na b. Chemotheraputic agents → hypomagnesemia
V. MODIFICATION OF DRUG ACTION BY FOOD AND NUTRIENTS 1. Substances enhance drug effects (1) MAOI and pressor agents (Box 19 -2) * Biologically active amines a. the psychoactive amines (neuotransmitters) – norepinephrine and dopamine b. the vasoactive amines – tyramine, serotonin & histamine monoamine & diamine oxidase Amines→ → → → deamination

Presence of the unoxidized pressor amines causes constriction of blood vessels and HTN→ Symptoms (2) Caffeine - ↑the adverse effects of stimulant drugs (3) Warfarin ( an oral anticoagulant) → ↓hepatic production of 4 vit. Kdependent clotting factors. *Dong Quai- contains coumarin-like substance *Ginseng - contains a platelet inhibitor.
2. Alcohol (1) ethanol combined with CNSdepressant→ excessive drowsiness, incoordination and other signs of CNS depression (2) Mucosal irritant – with aspirin or other NSAIDs→↑risk of GI ulceration (3) →↑risk of hepatic toxicity (4) Inhibit gluconeogenesis, →↑prolong a hypoglycemic episode (5) ethanol+disulfiram →↑risk of lifethreatening reaction
VI. Effects of drugs on Nutritional Status Drugs 1. Oral, Taste, and Smell (Box 19 -3) - ↓Food intake (1) alteration in taste sensation (dysgeusia) (2) ↓taste sensation (hypogeusia) (3) an unpleasant aftertaste * Mechanisms? - alter the turnover of taste cells - interfere with transduction mech. - Alter neurotransmitters in the CNS
(4) Inflammation of the mucous membranes (mucositis) - Stomatitis (mouth inflammation) - glossitis (tongue inflammation) - Cheilitis (lip inflammation and cracking) (5)↓secretions → dry mouth→ dental caries and loss of teeth, gum disease, stomatitis and glossitis.

2. Gastrointestinal Effects (1) GI irritation and ulceration – NSAIDs (2) Severe nausea and vomiting – Antineoplastic drugs → nausea nd vomiting (3) Changes in bowel function → constipation or diarrhea (↓peristalsis) (4) Destruction of intestinal bacteria (Box 19 -6) (5) Inhibit intestinal enzymes – DM drugs →undigested CHO →diarrhea, flatulence, cramping etc.
3. Appetite Changes • Suppress appetite (Box 19 -7)→wt. changes, nutritional imbalance, and growth retardation in kids. - Side effects of stimulant drugs a. HTN b. interfere with the ability or desire to eat (2) Stimulate appetite (Box 19 -8) )→wt. gains
4. Organ System Toxicity - hepatotoxicity, nephrotoxicity, pulmonary toxicity, neurotoxicity, ototoxicity, ocular toxicity, pancreatitis, cardiotoxicity etc. Ex. Hepatotoxicity→ hepatitis, jaudice, hepatomegaly, liver failure etc.
5. Glucose levels - Hypoglycemia or hyperglycemia (Box 19 -9)
VII. EXCIPIENTS AND FOOD-DRUG INTERACTIONS - An excipients ( inactive ingredients) is added to drug formulations for its action as a buffer, binder, filler, diluent, disintegrate, glidant, flavoring, dye, preservative, suspending agent, or coating.
VIII. MEDICAL NUTRITION THERAPY (MNT) 1. Prospective – All MNT offered when the pt. first starts a drug 2. Retrospective – evaluation of symptoms to determine whether medical problems might be the result of food-drug interactions.
 Alter mann ist kein d-zug
Alter mann ist kein d-zug Why does the inner party alter the past
Why does the inner party alter the past Dr. christa preissing
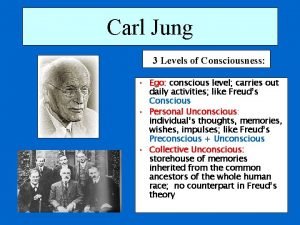
Dr. christa preissing 3 levels of consciousness
3 levels of consciousness Alter database add supplemental log data
Alter database add supplemental log data Palmendieb öffnet kokosnuss
Palmendieb öffnet kokosnuss Alter system set optimizer_features_enable
Alter system set optimizer_features_enable Afshaan alter
Afshaan alter Alter nrg
Alter nrg Avoid alter accept adapt
Avoid alter accept adapt Heinz erhardt pommes fritz
Heinz erhardt pommes fritz Alter ego trust
Alter ego trust Abu markub
Abu markub Humans alter the sulfur cycle by
Humans alter the sulfur cycle by Altered cast technique impression
Altered cast technique impression Versorgung im alter
Versorgung im alter Don homero y doña hermelinda significado
Don homero y doña hermelinda significado Ddl create alter drop
Ddl create alter drop Greg alter
Greg alter Vier dimensionen der lebensqualität nach lawton
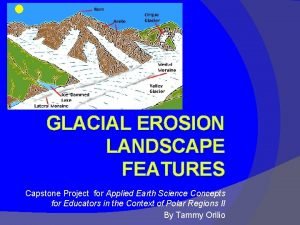
Vier dimensionen der lebensqualität nach lawton Erosion occurs when natural forces alter the landscape
Erosion occurs when natural forces alter the landscape Madonna dob
Madonna dob Ich komme jetzt langsam in das alter
Ich komme jetzt langsam in das alter Drug that alters moods, thoughts, and sense perceptions
Drug that alters moods, thoughts, and sense perceptions Paige naimann
Paige naimann Eva alter
Eva alter Alter intro template
Alter intro template Brazen alter
Brazen alter Ldd que es
Ldd que es Notitiam primosque gradus vicinia fecit
Notitiam primosque gradus vicinia fecit Steppenwolf maria
Steppenwolf maria