CESAREAN SECTION When Why and How Matthew Snyder




- Slides: 33
CESAREAN SECTION When, Why and How Matthew Snyder, DO, Maj, USAF, MC Nellis AFB, NV
OVERVIEW � Indications � Instruments � Procedure � Post-operative management � Post-partum counseling
C/S INDICATIONS - FETAL � Fetal Macrosomia (over 5000 g, GDM – 4500 g) � Multiple Gestations � Fetal Intolerance to Labor � Malpresentation / Unstable Lie – Breech or Transverse presentation
C/S INDICATIONS - FETAL � Non-reassuring � Repetitive Fetal Heart Tracing Variable Decelerations � Repetitive Late Decelerations � Fetal Bradycardia � Fetal Tachycardia � Cord Prolapse
C/S INDICATIONS - MATERNAL � Elective Repeat C/S � Maternal infection (active HSV, HIV) � Cervical Cancer/Obstructive Tumor � Abdominal Cerclage � Contracted Pelvis � Congenital, � Medical Fracture Conditions � Cardiac, Pulmonary, Thrombocytopenia
C/S INDICATIONS – MATERNAL/FETAL � Abnormal Placentation � Placenta previa � Vasa previa � Placental abruption � Conjoined Twins � Perimortem � Failed Induction / Trial of Labor
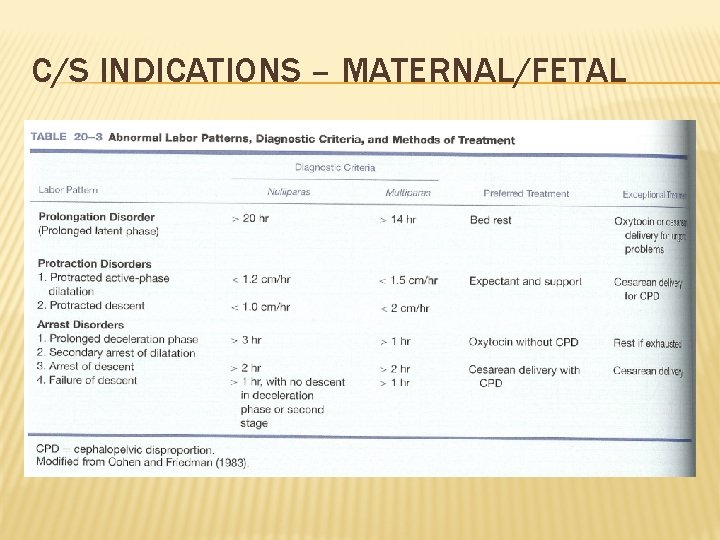
C/S INDICATIONS – MATERNAL/FETAL � Arrest Disorders � Arrest of Descent (no change in station after 2 hours, <10 cm dilated) � Arrest of Dilation (< 1. 2 cm/hr nullip; < 1. 5 cm/hr multip) � Failure of Descent (no change in station after 2 hours, fully dilated)
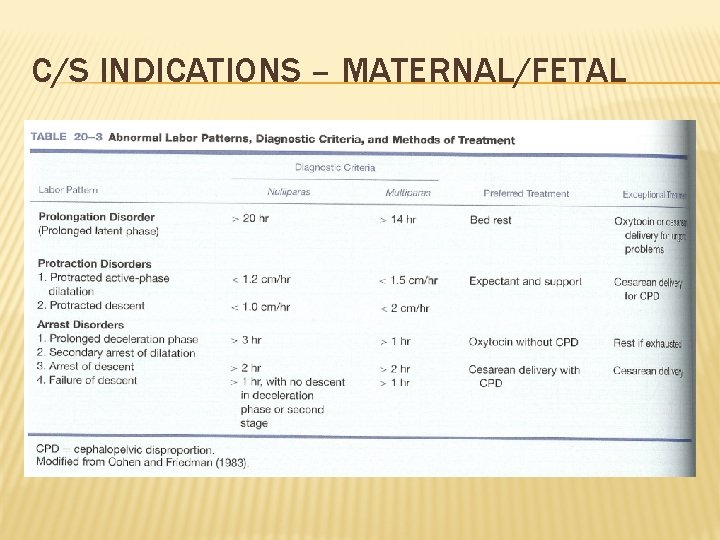
C/S INDICATIONS – MATERNAL/FETAL
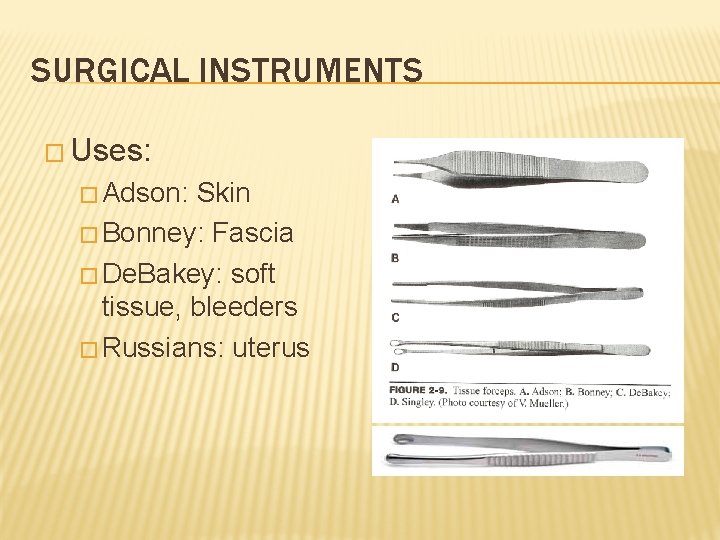
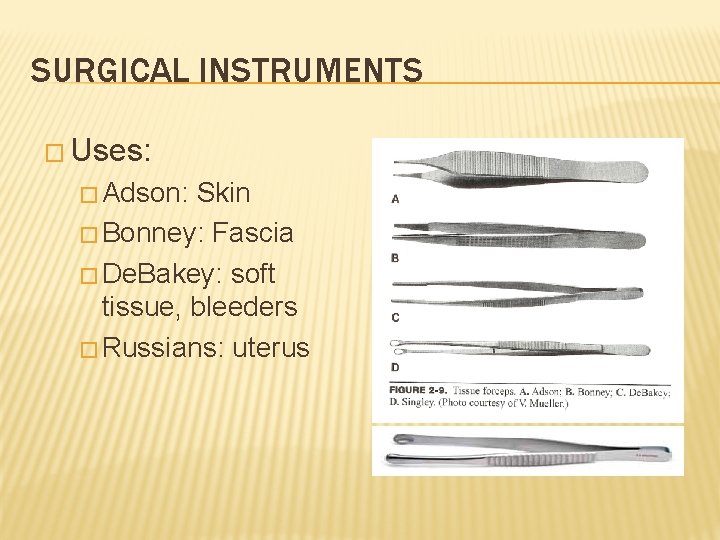
SURGICAL INSTRUMENTS � Uses: � Adson: Skin � Bonney: Fascia � De. Bakey: soft tissue, bleeders � Russians: uterus
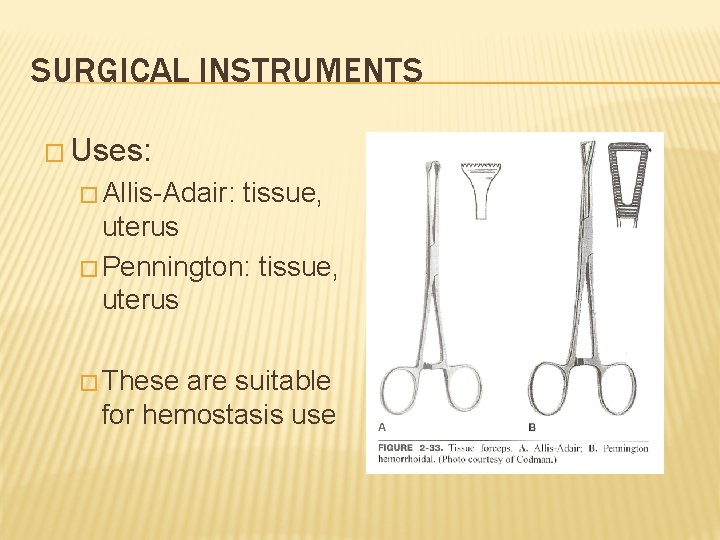
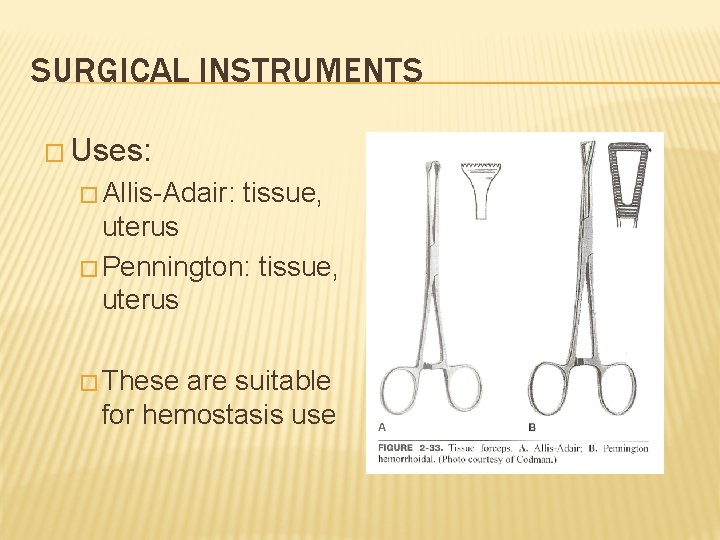
SURGICAL INSTRUMENTS � Uses: � Allis-Adair: tissue, uterus � Pennington: tissue, uterus � These are suitable for hemostasis use
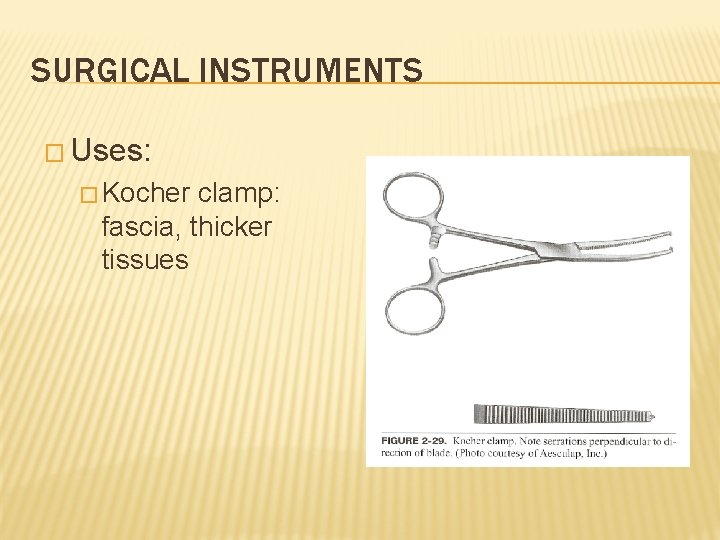
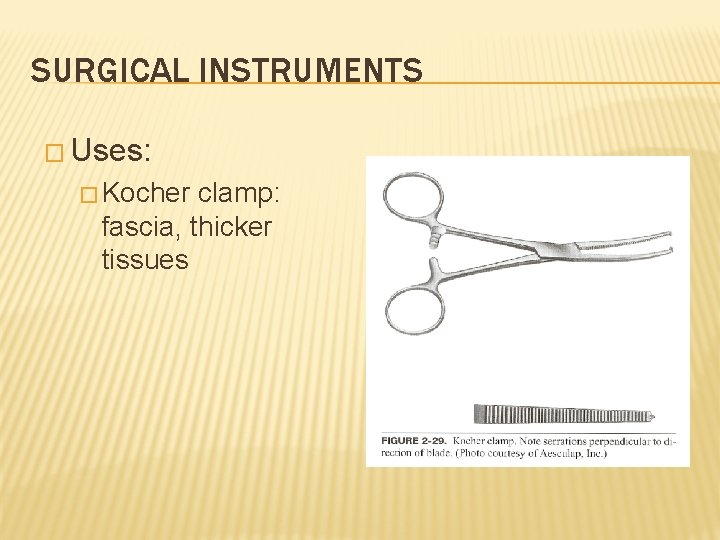
SURGICAL INSTRUMENTS � Uses: � Kocher clamp: fascia, thicker tissues
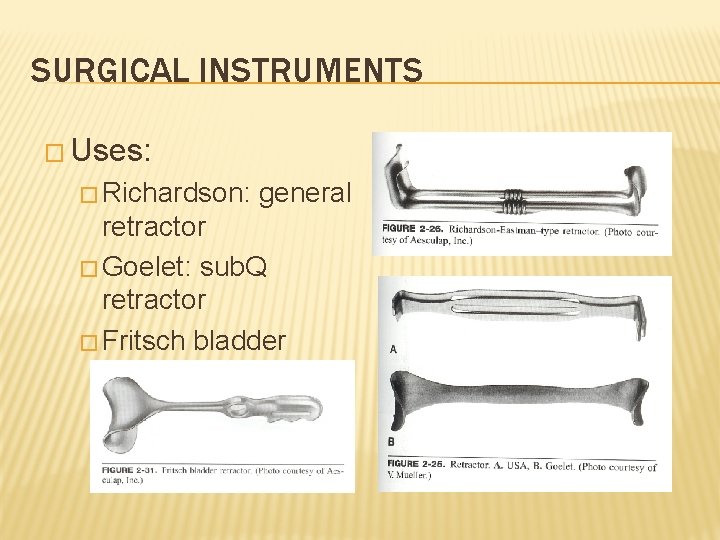
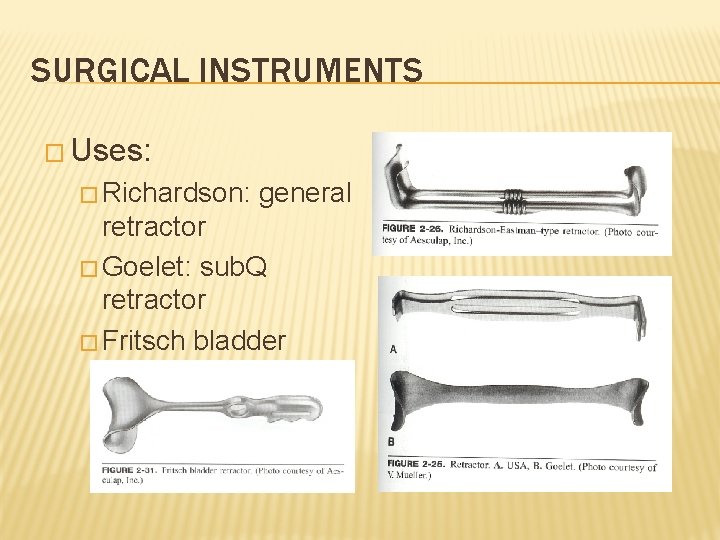
SURGICAL INSTRUMENTS � Uses: � Richardson: general retractor � Goelet: sub. Q retractor � Fritsch bladder blade
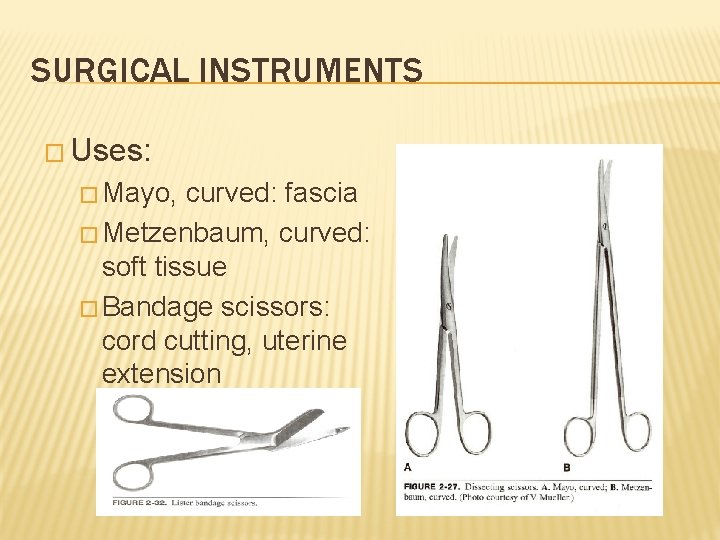
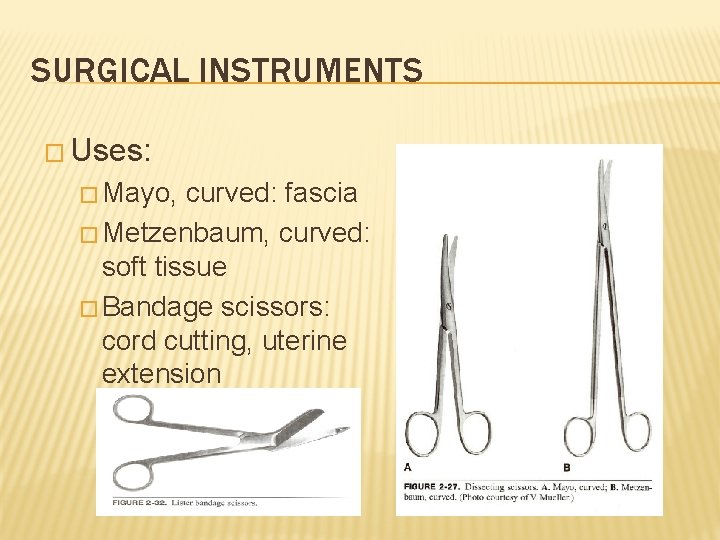
SURGICAL INSTRUMENTS � Uses: � Mayo, curved: fascia � Metzenbaum, curved: soft tissue � Bandage scissors: cord cutting, uterine extension
CESAREAN SECTION: INCISION TO UTERUS � Preparation: � Ensure SCDs applied � Setup bovie and suction � Test pt by pinching on either side of incision and around navel with Allis clamp � Lap sponge in other hand
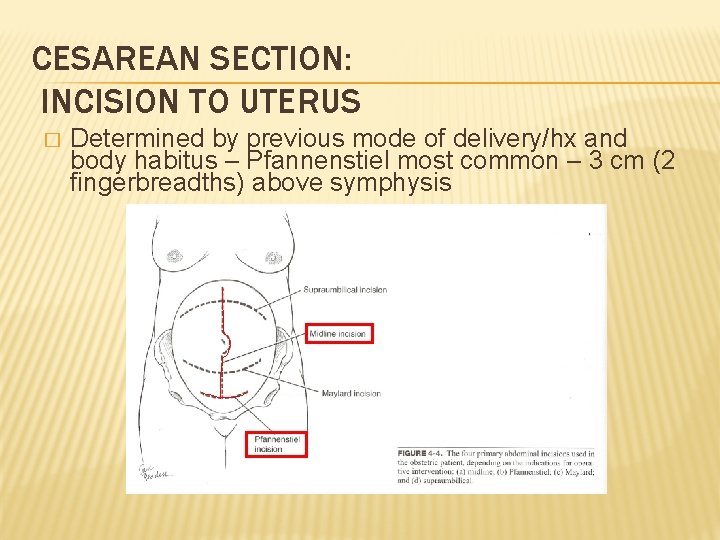
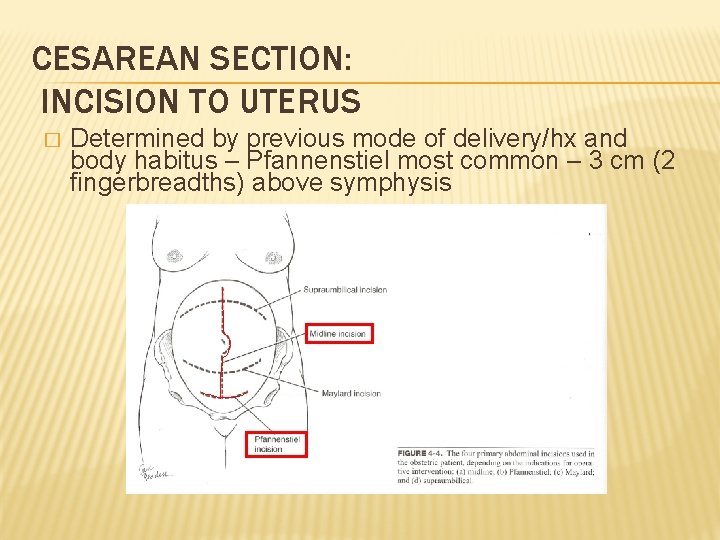
CESAREAN SECTION: INCISION TO UTERUS � Determined by previous mode of delivery/hx and body habitus – Pfannenstiel most common – 3 cm (2 fingerbreadths) above symphysis
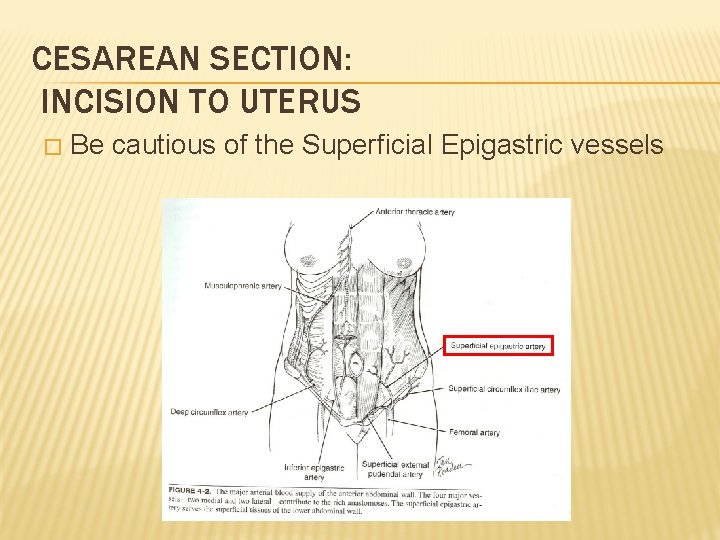
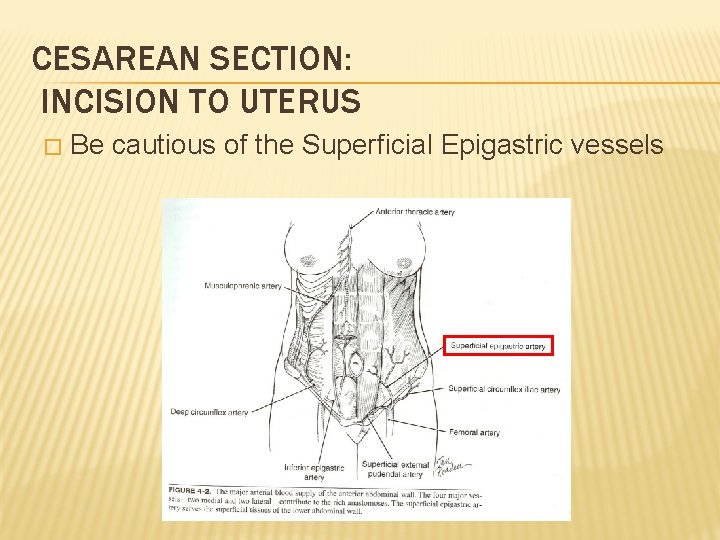
CESAREAN SECTION: INCISION TO UTERUS � Be cautious of the Superficial Epigastric vessels
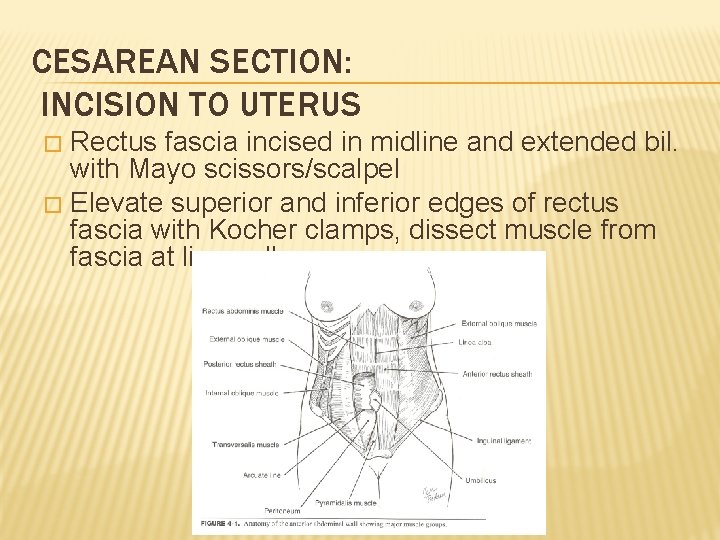
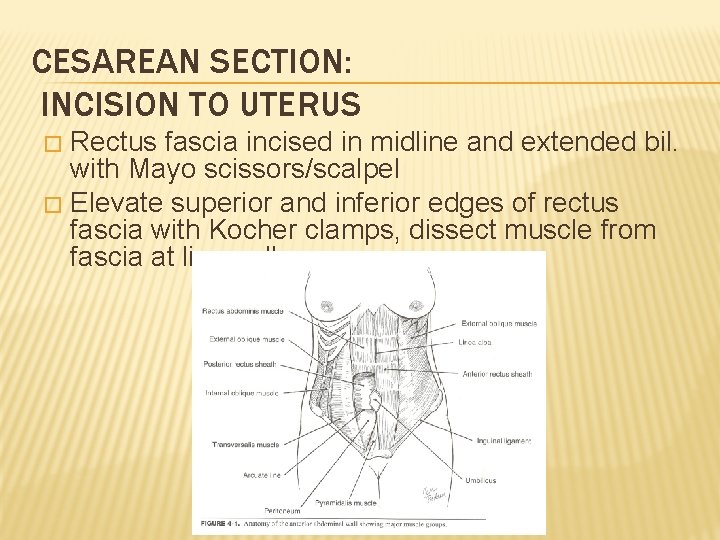
CESAREAN SECTION: INCISION TO UTERUS Rectus fascia incised in midline and extended bil. with Mayo scissors/scalpel � Elevate superior and inferior edges of rectus fascia with Kocher clamps, dissect muscle from fascia at linea alba. �
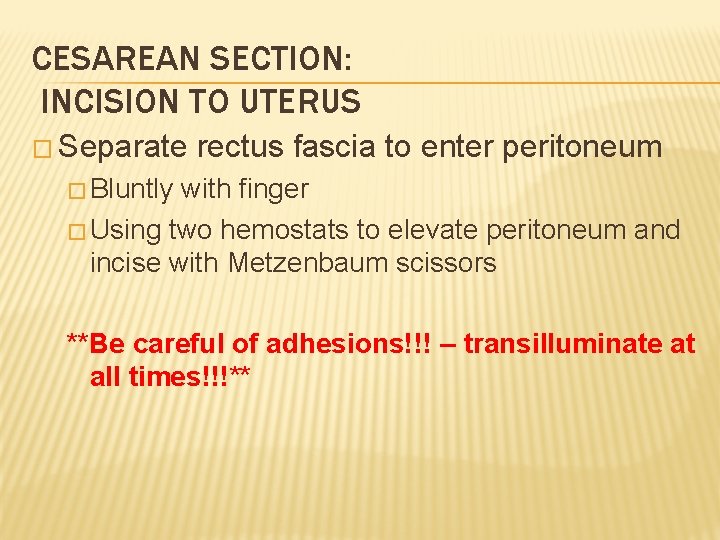
CESAREAN SECTION: INCISION TO UTERUS � Separate rectus fascia to enter peritoneum � Bluntly with finger � Using two hemostats to elevate peritoneum and incise with Metzenbaum scissors **Be careful of adhesions!!! – transilluminate at all times!!!**
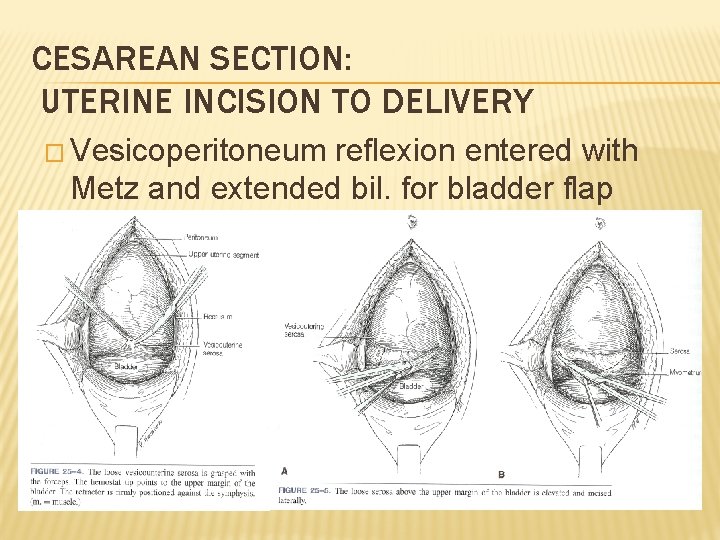
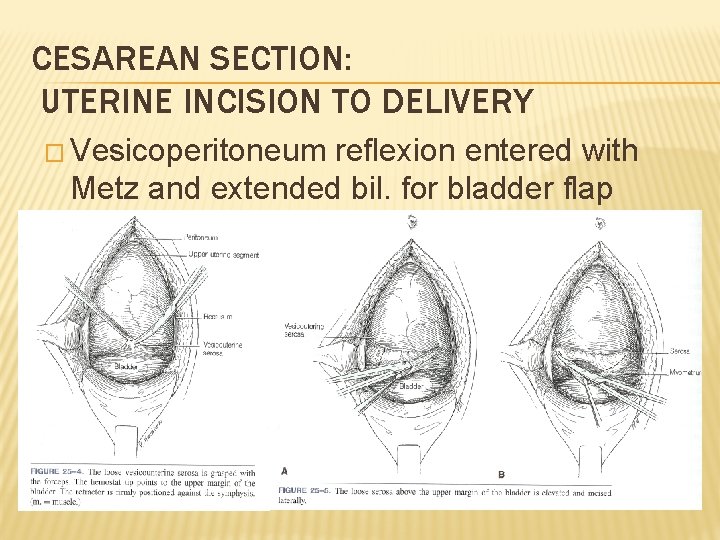
CESAREAN SECTION: UTERINE INCISION TO DELIVERY � Vesicoperitoneum reflexion entered with Metz and extended bil. for bladder flap
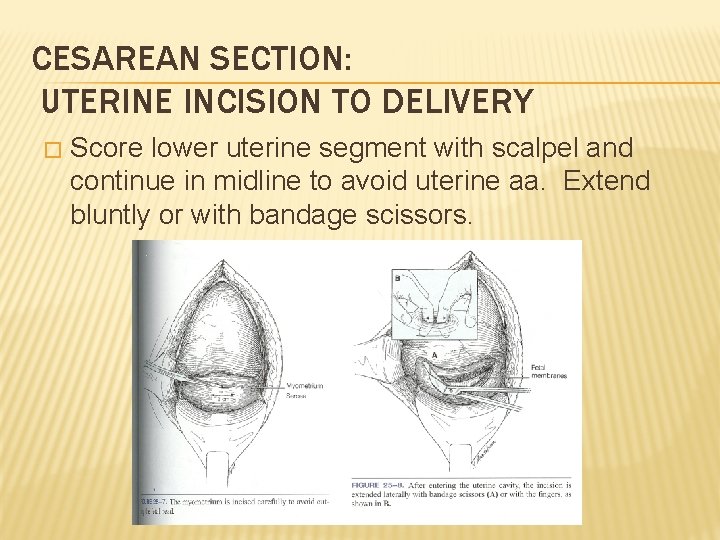
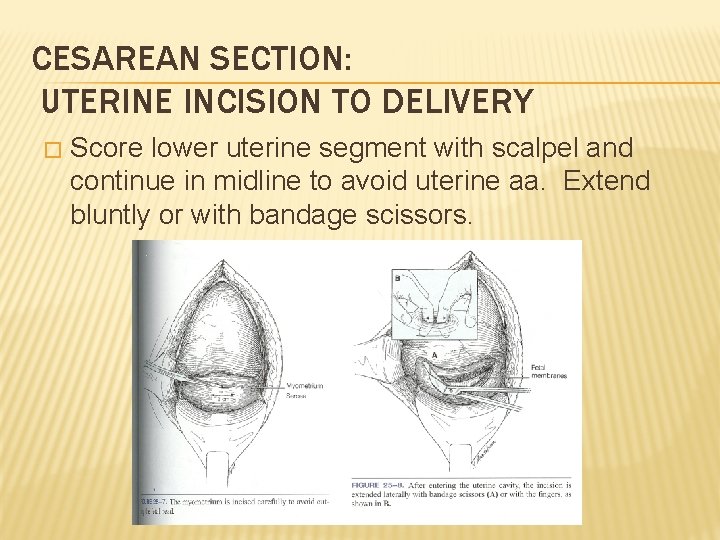
CESAREAN SECTION: UTERINE INCISION TO DELIVERY � Score lower uterine segment with scalpel and continue in midline to avoid uterine aa. Extend bluntly or with bandage scissors.
CESAREAN SECTION: UTERINE INCISION TO DELIVERY � Once delivering hand inserted, bladder blade removed � Bring head up to incision by flexing fetal head, without flexing wrist to avoid uterine incision extensions � Once infant delivered, collect cord gases if desired and cord blood sample � Deliver placenta manually or with uterine massage
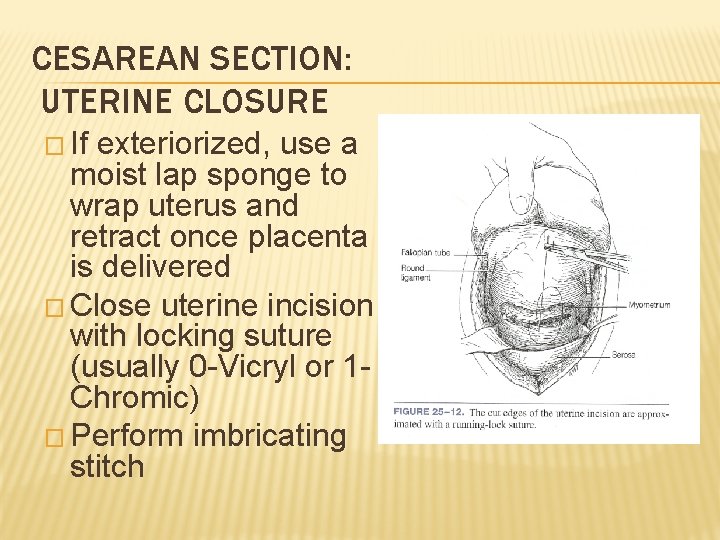
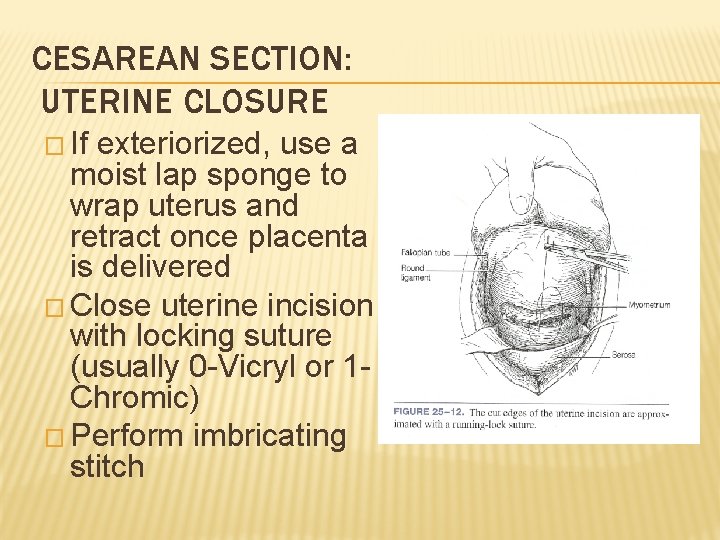
CESAREAN SECTION: UTERINE CLOSURE � If exteriorized, use a moist lap sponge to wrap uterus and retract once placenta is delivered � Close uterine incision with locking suture (usually 0 -Vicryl or 1 Chromic) � Perform imbricating stitch
CESAREAN SECTION: CLOSURE � Examine adnexa, irrigate rectouterine pouch and/or gutters and re-examine uterine incision � Ensure hemostasis of rectus then close fascia with non-locking suture to avoid vessel strangulation � Close subcut. space if over 2 cm, then skin � If needed, clear lower uterine segment and vagina of clots once skin is closed and dressed
POST-OPERATIVE CARE � Pt. must urinate within four hours of Foley removal, otherwise replace Foley for another 12 hours � Any fever post-op MUST be investigated � Wind: Atelectasis, pneumonia � Water: UTI � Walking: DVT, PE, Pelvic thromboembolism � Wounded: Incisional infection, endomyometritis, septic shock

POST-OPERATIVE CARE � In the first 12 -24 hours, the dressing may become soaked with serosanguinous fluid – if saturated, replace dressing otherwise no action needed � After Foley is removed (usually within 12 hours post -op), encourage ambulation of halls, not just room � Dressing may be removed in 24 -48 hours post-op (attending specific), use maxipad � Ensure pt. is tolerating PO intake, urinating well and has flatus before discharge � Watch for post-op ileus
DELAYED COMPLICATIONS � Subsequent Pregnancies � Uterine rupture/dehiscence � Abnormal placental implantation (accreta, etc) � Repeat Cesarean section � Adhesions � Scaring/Keloids

WOUND DEHISCENCE Noted by separation of wound usually during staple removal or within 1 -2 weeks post-op � Must explore entire wound to determine depth of dehiscence (open up incision if needed) – if through rectus fascia, back to the OR � If dehiscence only in sub. Q layer, debride wound daily with 1: 1 sterile saline/H 2 O 2 mixture and pack with gauze � May use prophylactic abx – Keflex, Bactrim, Clinda � KEY: Close f/u and wound exploration �

POST-PARTUM COUNSELING: PHARM � Continue PNV � Colace � Motrin 800 mg q 8 � Percocet 1 -2 tabs q 4 -6 for breakthrough � OCP (start 4 -6 wks post-partum)
POST-PARTUM COUNSELING: ACTIVITY � No lifting objects over baby’s wt. � Continue ambulation � No strenuous activity � NOTHING by vagina (sex, tampons, douches, bathtubs, hot tubs) for 6 wks!!
POST-PARTUM COUNSELING: INCISION CARE � Only showers – light washing � If pt has steristrips, should fall off in 7 -10 days, otherwise use warm, wet washcloth to remove � If pt has staples – removal in 3 -7 days outpt. � Most attendings will have pt f/u in office in about 2 wks for wound check

POST-PARTUM COUNSELING: NOTIFY MD/DO � � � � Fever (100. 4)/Chills HA Vision changes RUQ/Epigastric pain Mastitis sx Increasing abd. pain Erythema/Induration/ increasing swelling around incision � � � Purulent drainage Serosanguinous drainage over half dollar size on pad Wound separation Purulent vaginal discharge Vaginal bleeding over 1 pad/hr or golf ball size clots Calf tenderness
SUMMARY � Indications � Surgical Technique � Post-operative management � Post-operative Complications � Post-partum counseling
REFERENCES �Cunningham, F. , Leveno, Keith, et al. Williams Obstetrics. 22 nd ed. , New York, 2005. �Gabbe, Steven, Niebyl, Jennifer, et al. Obstetrics: Normal and Problem Pregnancies. 4 th ed. , Nashville, 2001. �Gilstrap III, Larry, Cunningham, F. , et al. Operative Obstetrics. 2 nd ed. , New York, 2002. �www. uptodateonline. com