Cervix Erosion A extension of the columnar epithelium


- Slides: 41
Cervix Erosion A extension of the columnar epithelium outward across the vaginal face of the cervix. v. Redder v. Soft velvety appearance v. Mucus secretion 1
Cervix Erosion A extension of the columnar epithelium outward across the vaginal face of the cervix. v. Redder v. Soft velvety appearance v. Mucus secretion 2
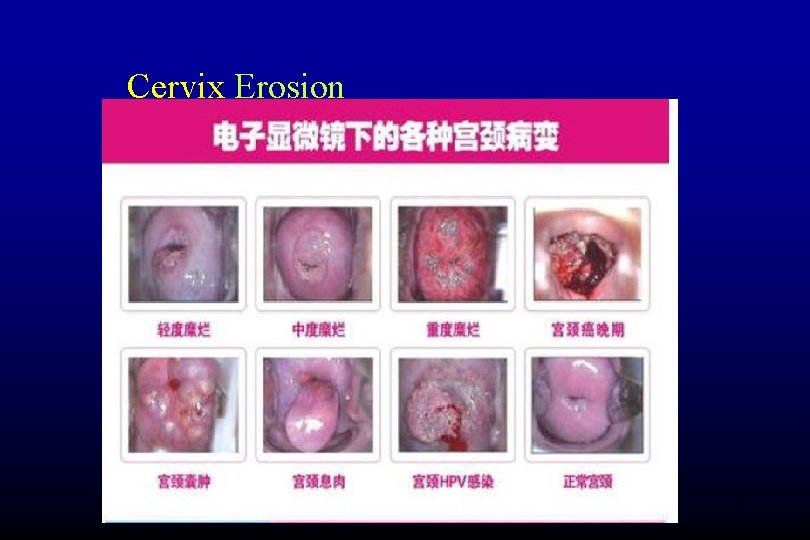
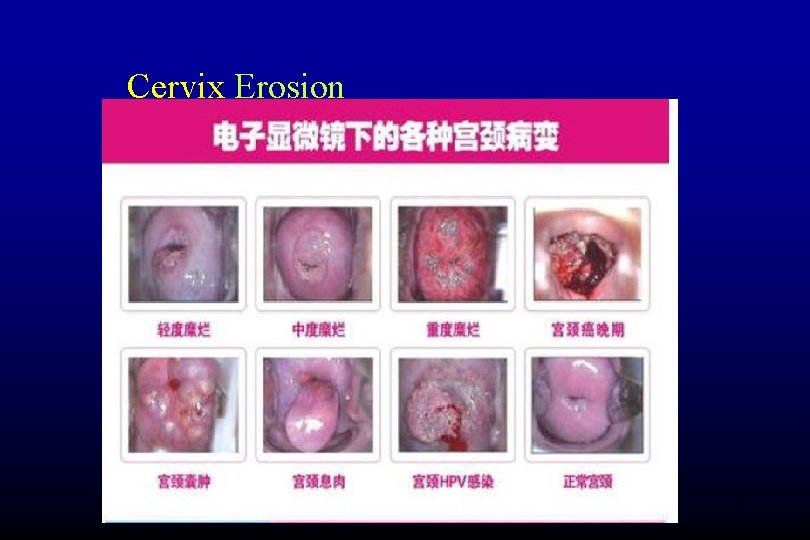
Cervix Erosion 3
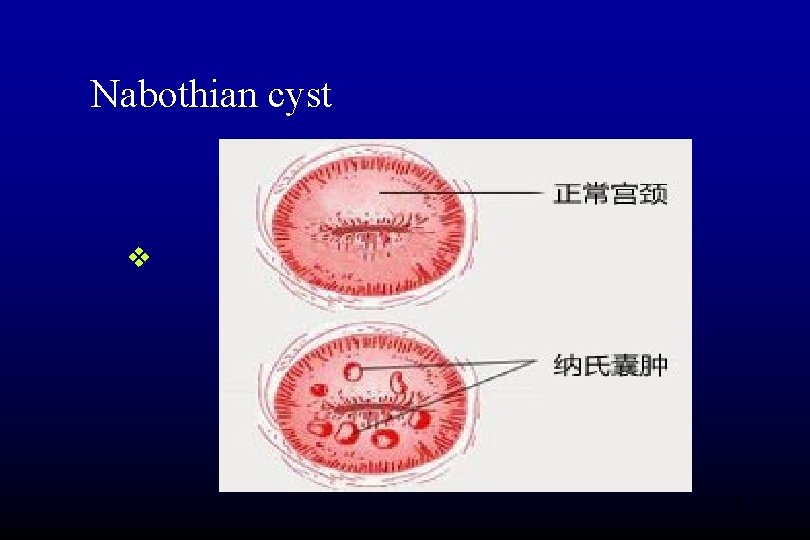
Nabothian cyst v. Dilated retention cyst v. Mucin filled cyst yellow to whitish, v. Domed protrusion from the exocervix. v. A few millimeters in diameter. v. Rare occasion the diameter may reach 1 cm or more v. Require no therapy 4
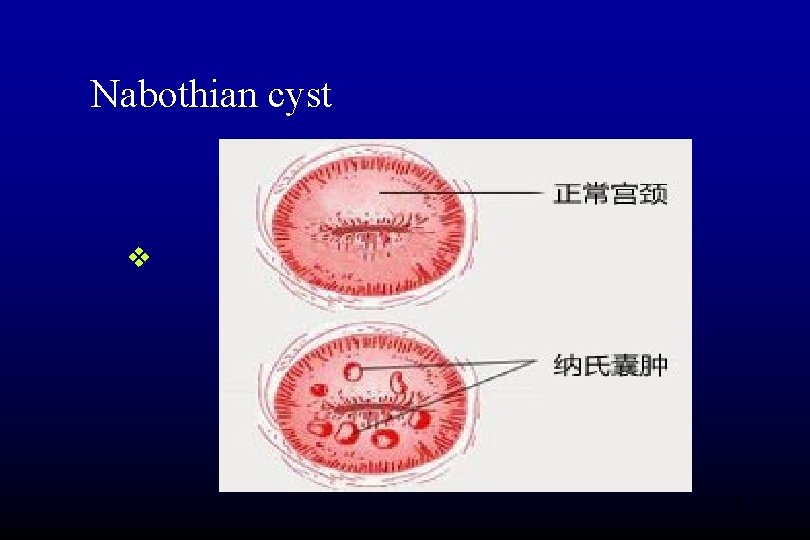
Nabothian cyst v 5
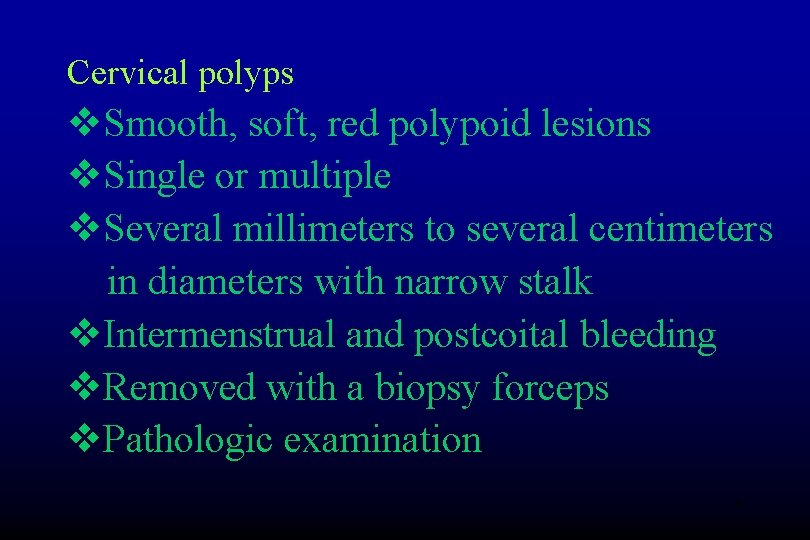
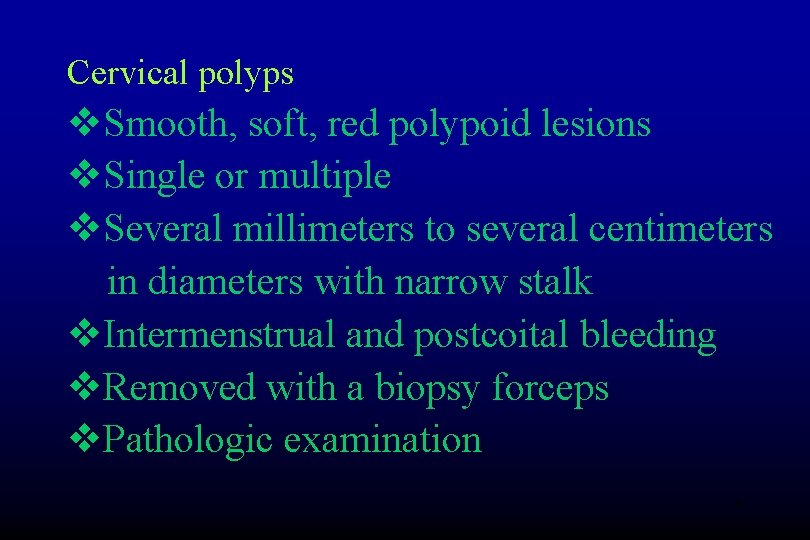
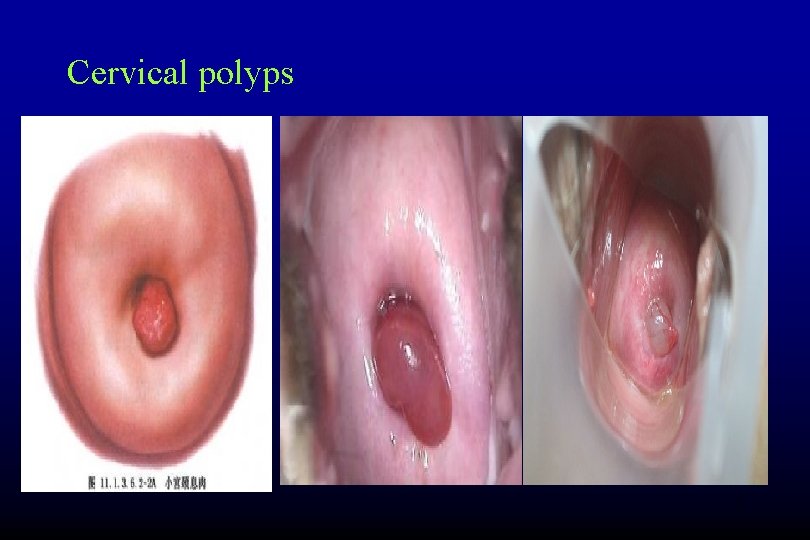
Cervical polyps v. Smooth, soft, red polypoid lesions v. Single or multiple v. Several millimeters to several centimeters in diameters with narrow stalk v. Intermenstrual and postcoital bleeding v. Removed with a biopsy forceps v. Pathologic examination 6
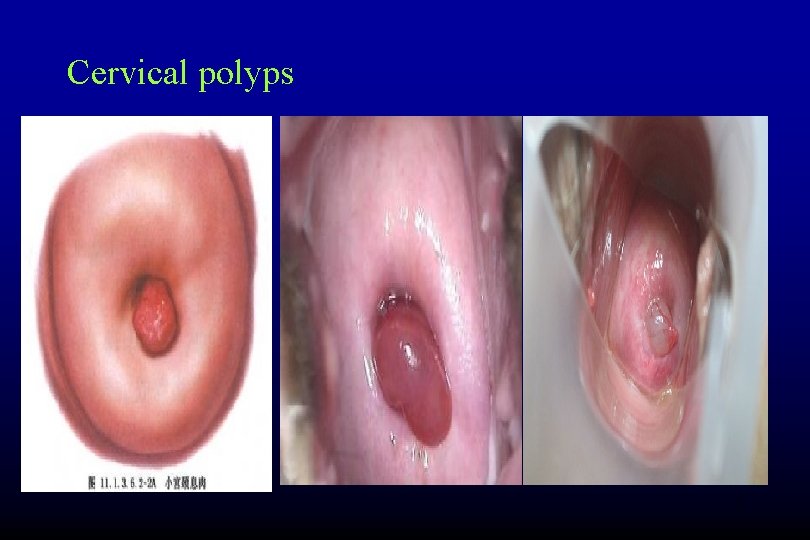
Cervical polyps 7
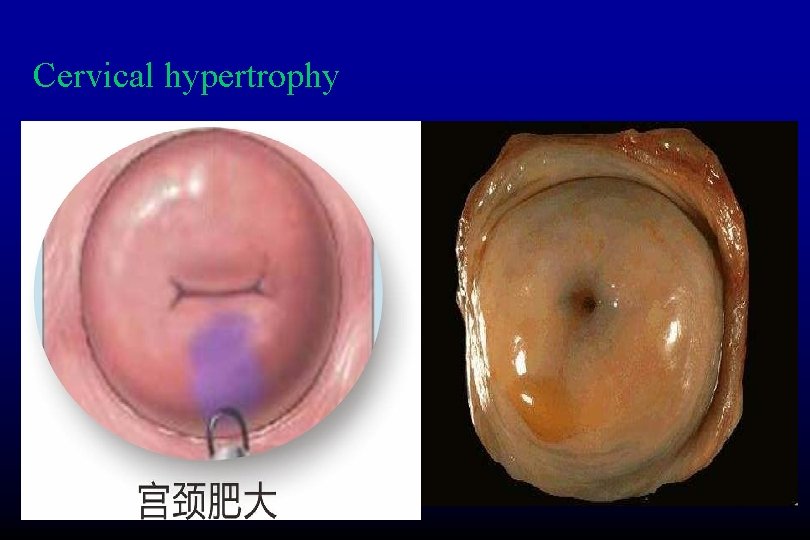
Cervical hypertrophy v. Both the diameter and the length of the cervix may increase several fold vedema, congestion 8
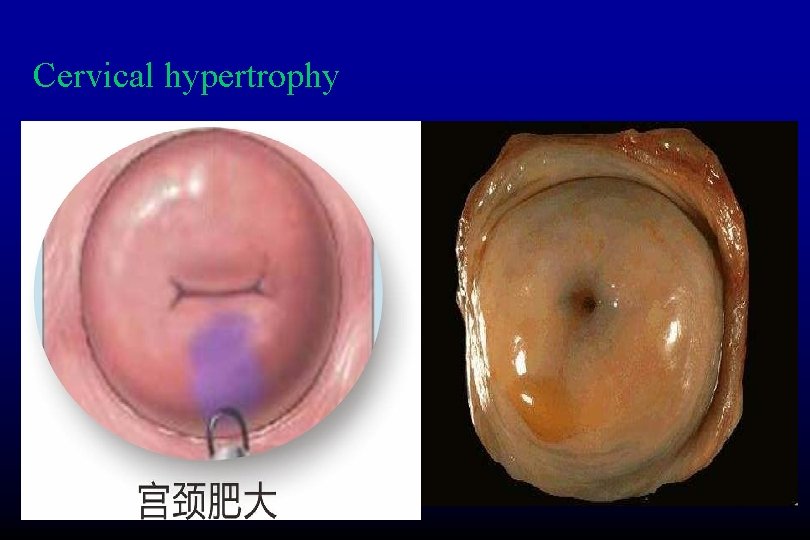
Cervical hypertrophy 9
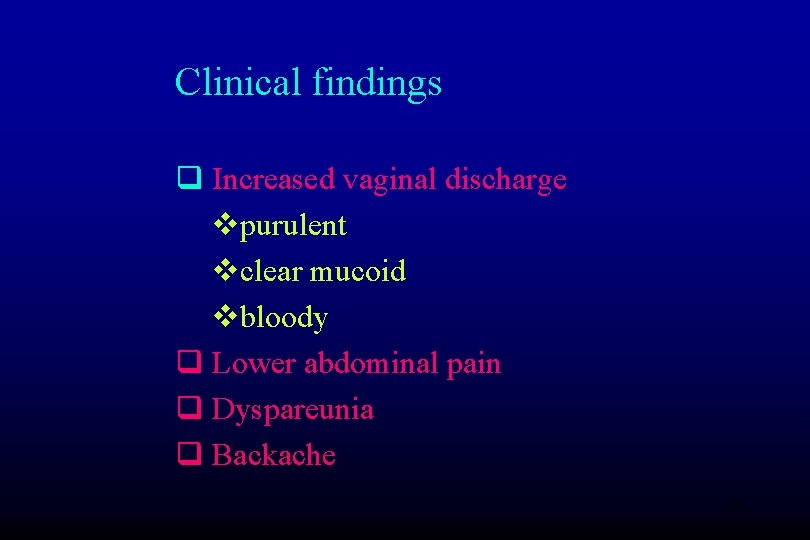
Clinical findings q Increased vaginal discharge vpurulent vclear mucoid vbloody q Lower abdominal pain q Dyspareunia q Backache 10
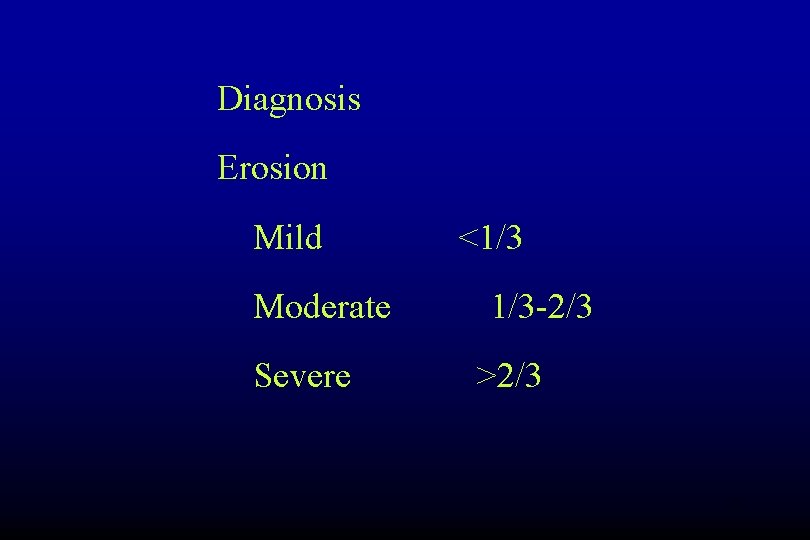
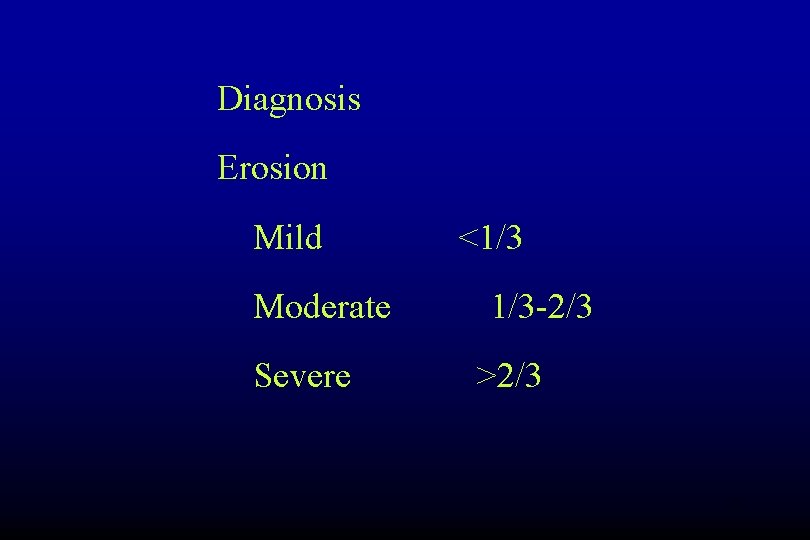
Diagnosis Erosion Mild Moderate Severe <1/3 1/3 -2/3 >2/3 11
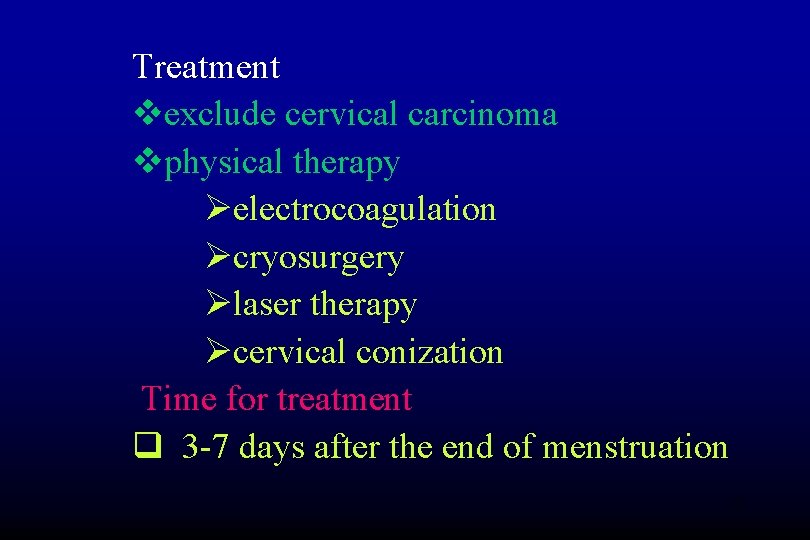
Treatment vexclude cervical carcinoma vphysical therapy Øelectrocoagulation Øcryosurgery Ølaser therapy Øcervical conization Time for treatment q 3 -7 days after the end of menstruation 12
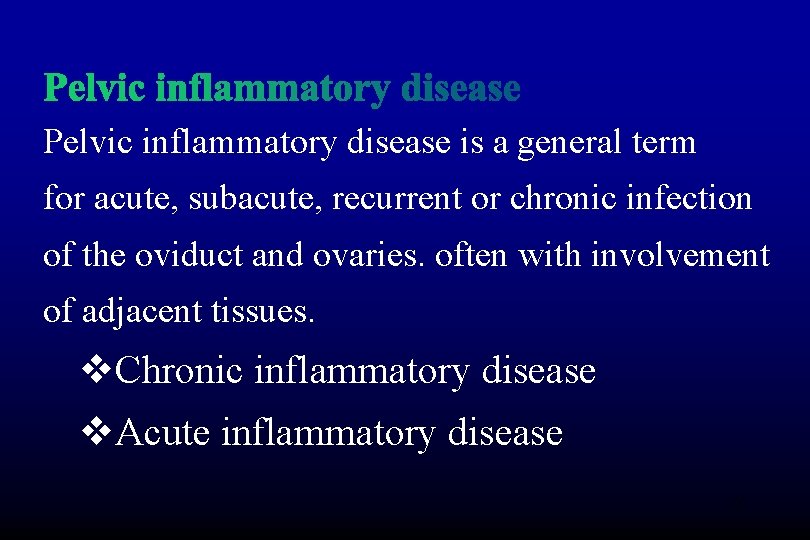
Pelvic inflammatory disease is a general term for acute, subacute, recurrent or chronic infection of the oviduct and ovaries. often with involvement of adjacent tissues. v. Chronic inflammatory disease v. Acute inflammatory disease 13

Pelvic inflammatory disease (PID) is an infectious and inflammatory disorder of the upper female genital tract, including the uterus, fallopian tubes, and adjacent pelvic structures. Infection and inflammation may spread to the abdomen, including perihepatic structures (Fitz. Hugh−Curtis syndrome). 14
Pelvic inflammatory disease PID is initiated by infection that ascends from the vagina and cervix into the upper genital tract. Chlamydia trachomatis is the predominant sexually transmitted organism associated with PID. Of all acute PID cases, less than 50% test positive for the sexually transmitted organisms such as Chlamydia trachomatis and Neisseria gonorrhea 15
Pelvic inflammatory disease The diagnosis of acute PID is primarily based on historical and clinical findings. Clinical manifestations of PID vary widely. Many patients exhibit few or no symptoms, whereas others have acute, serious illness. The most common presenting complaint is lower abdominal pain. Many women report an abnormal vaginal discharge. 16
Pelvic inflammatory disease The differential diagnosis includes appendicitis, cervicitis, urinary tract infection, endometriosis, ovarian torsion and adnexal tumors. Ectopic pregnancy can be mistaken for PID; indeed, PID is the most common incorrect diagnosis in cases of ectopic pregnancy. Consequently, a pregnancy test is mandatory in the workup of women of childbearing age who have lower abdominal pain. 17
Pelvic inflammatory disease PID may produce tubo-ovarian abscess (TOA) and may progress to peritonitis and Fitz-Hugh−Curtis syndrome (perihepatitis; see the image below). Note that a rare but life-threatening complication of acute rupture of a TOA may result in diffuse peritonitis and necessitate urgent abdominal surgery. 18
Pelvic inflammatory disease Laparoscopy is the current criterion standard for the diagnosis of PID. No single laboratory test is highly specific or sensitive for the disease, but studies that can be used to support the diagnosis include the erythrocyte sedimentation rate (ESR), the C-reactive protein (CRP) level, and chlamydial and gonococcal DNA probes and cultures, endometrial biopsy, imaging studies (eg, ultrasonography, computed tomography [CT], and magnetic resonance imaging [MRI]) may be helpful in unclear cases. 19
Pelvic inflammatory disease Empirical antibiotic treatment is recommended for patients with otherwise unexplained uterine or adnexal tenderness and cervical motion tenderness, according to guidelines from the Centers for Disease Control and Prevention (CDC). Antibiotic regimens for PID must be effective against C trachomatis and N gonorrhoeae, as well as against gram-negative facultative organisms, anaerobes, and streptococci. 20
The preventive mechanism of female genital system v Vulva v. Vagina v. Cervix v. Menstruation v. Oviduct 21
Pathophysiology Most cases of PID are presumed to occur in 2 stages. The first stage is acquisition of a vaginal or cervical infection. This infection is often sexually transmitted and may be asymptomatic. The second stage is direct ascent of microorganisms from the vagina or cervix to the upper genital tract, with infection and inflammation of these structures 22
Pathophysiology The mechanism (or mechanisms) by which microorganisms ascend from the lower genital tract is unclear. Studies suggest that multiple factors may be involved. Although cervical mucus provides a functional barrier against upward spread, the efficacy of this barrier may be decreased by vaginal inflammation and by hormonal changes that occur during ovulation and menstruation. 23
Pathophysiology Inflammation may extend to uninfected parametrial structures, including the bowel. Infection may extend via spillage of purulent materials from the fallopian tubes or via lymphatic spread beyond the pelvis to produce acute peritonitis and acute perihepatitis (Fitz-Hugh−Curtis syndrome). 24
Prognosis PID has 3 principal complications, as follows: Chronic pelvic pain Infertility Ectopic pregnancy 25
v. Lymphatics v. Blood vessels v. Mucosa v. Direct dissemination 26
Reason of pelvic infection v. Postpartum and associated abortion v. IUD-related v. Secondary to other infection site v. Infection during the period v. The acute onset of chronic inflammatory disease 27
Clinical findings A. symptoms and signs v. Abdominal and pelvic pain v. Pelvic pressure. back pain v. Purulent vaginal discharge v. Nausea and vomiting v. Fever with tachycardia v. Both lower quadrants abdominal tenderness 28
Pelvic examination v Inflammation of the periurithral and bantholin’s gland v Purulent cervical discharge. v Tenderness on movement of the cervix and uterus and palpation of the parametria 29
B laboratory findings v. Leukocytosis with a shift to the left v. Culdocentosis reaction fluid C. X-ray finding Signs of ileus , nonspecific. 30
Differential diagnosis v. Acute appendicitis v. Ectopic pregnancy v. Ruptured corpus luteum cyst v. Torsion of an adnexal mass v. Degeneration of a leiomyoma v. Endometriosis 31
Treatment v. Bed rest v. Restrict oral feeding v. Administer intravenous fluids to correct dehydration and acidosis v. Use nasogastric suction in the presence of abdominal distention or ileus v. Give antibiotics v. Exploratory laparotomy(operation) ØAbdominal symptoms persist ØClinical findings worsen ØThe patient’s condition deteriorates ØAbscess formation and have no response to conservative treatment 32
Chronic pelvic inflammatory disease Clinical findings A. symptoms and signs v. Pelvic pain. unilateral or bilateral v. Dyspareunia v. Dysfunctional uterine bleeding v. Infertility v. Fever reinfection v. Tenderness v. Thickening of the parametria 33
B. laboratory findings vleukocytosis Ddifferential diagnosis v. Endometriosis v. Ovarian tumor v. Ectopic pregnancy 34
Prevention: prompt and adequate treatment of acute pelvic infection Treatment v. General treatment v. Chinese herbs v. Physical treatment thermal therapy v. Surgery v. Hydrosalpinx v. Tubo-ovarian complexes 35
Pelvictuberculosis Clinical findings A. symptoms and signs v. Infertility v. Amenorrhea v. Abdominal or pelvic pain v. Fever with low grade v. Weight loss v. Pelvic mass 36
B. laboratory findings Find the organism v. Menstrual discharge v. Curettage or biopsy v. Peritoneal biopsy X-ray finding v. Chest X-ray v. Hysterosalpingography (HSG) v. Laparoscopy 37
Differential diagnosis v. Chronic pelvic inflammatory v. Endometriosis v. Ovarian trmor v. Cervical carcinoma 38

Treatment Drugs v. Isoniazid (异烟肼INH) 0. 1 tid for 2 years v. Streptomycin 0. 5 -1 g im qd for 4 -6 months v. Ethambutol 乙胺丁醇片 15 -25 mg/kg v. Rifampin 400 -600 mg qd REGIMEN(方案) v. Combined therapy 39
Surgery v. Masses not resolving with medical therapy v. Resistant or reactivated disease v. Persistant menstrual irregularities. v. Fistuila formation 40
QUESTIONS: v. What is pelvic inflammatory disease (PID) and who is at high risk for developing the disorder? v. How is pelvic inflammatory disease (PID) diagnosed? v. Which conditions should be included in the differential diagnosis of pelvic inflammatory disease (PID)? v. What is the disease course of pelvic inflammatory disease (PID)? v. What is the role of laparoscopy in the diagnosis of pelvic inflammatory disease (PID)? 41