Cervical Spine Manipulations Premanipulative Screening Upper Cervical Ligament




- Slides: 46
Cervical Spine Manipulations Pre-manipulative Screening
Upper Cervical Ligament Testing • When treating the upper cervical spine, stress tests should be done routinely, much like stress tests for knee ligaments are done routinely in a knee examination. • The original discovery of life threatening complications due to high velocity trauma is rare. • Even as rare as it is, if there exists even the suspicion of a life threatening instability, then the appropriate stress tests should obviously be performed.
Risk factors upper cervical instability • History of trauma (e. g. whiplash, football neck injury) • Congenital collagenous compromise (e. g. syndromes: Down’s, Ehlers-Danlos) • Inflammatory arthritides (e. g. rheumatoid arthritis, ankylosing spondylitis) • Recent neck/head/dental surgery.
Early presentation • • • Neck and head pain Feeling of instability Cervical muscle hyperactivity Constant support needed for head Worsening symptoms

Late presentation • Bilateral or quadrilateral limb paresthesiae, either constantly or reproduced/aggravated by head or neck movements. • Hyperreflexia • Clonus • Positive Babinski or Hoffman’s • Arm and leg weakness • Lack of coordination bilaterally
Active/patient generated tests Patient seated, minimal hands on required. Reduces the chance of exacerbating patient’s status. • Cervical rotation. Unable to move in presence of dens fracture, hangman’s fracture • Upper cervical sidebending • Active upper cervical flexion. If the neck is unstable, patient will be unable to flex the neck and will substitute with chin protrusion. Local symptoms are to be ignored. • Active upper cervical extension
Passive/therapist generated tests • Distraction O-A, C 1 -2. Patient seated • Alar ligament stress test • Compression lateral masses C 1 to rule out Jefferson fracture • Posterior shear occiput on C 1. • Anterior shear occiput on C 1, 2 • Transverse ligament - modified Sharp Purser test
Upper Motor Neuron Tests • • • Babinski Hoffman’s Dynamic Hoffman’s DTR’s Clonus Shimizu’s or Scapulo. Humeral Reflex
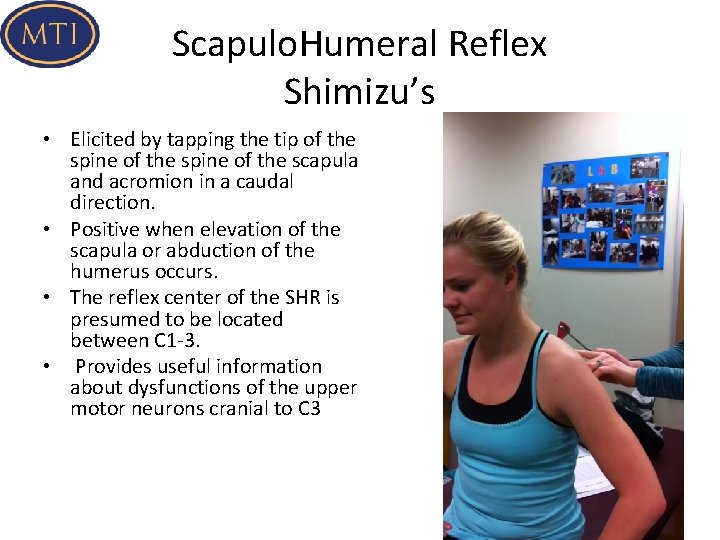
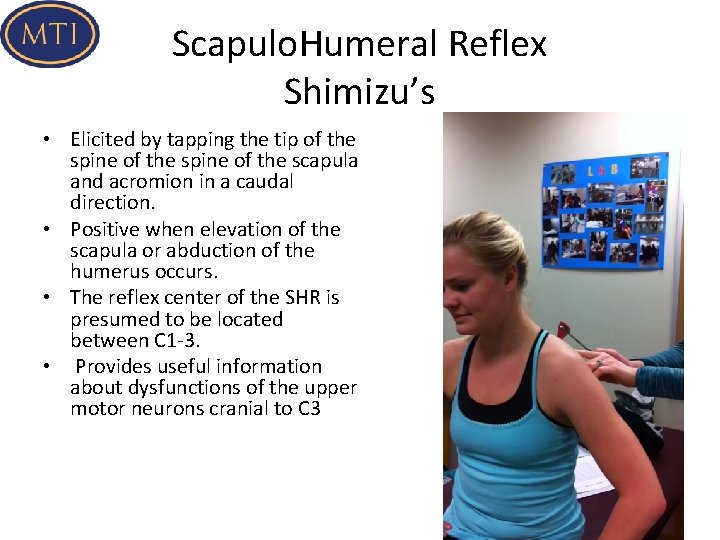
Scapulo. Humeral Reflex Shimizu’s • Elicited by tapping the tip of the spine of the scapula and acromion in a caudal direction. • Positive when elevation of the scapula or abduction of the humerus occurs. • The reflex center of the SHR is presumed to be located between C 1 -3. • Provides useful information about dysfunctions of the upper motor neurons cranial to C 3
Early Presentation Cervical Arterial Dysfunction • • • Mid-upper cervical pain Pain around ear and jaw Head pain (front- temporo- parietal) Occipital headache Acute onset of pain described as "unlike any other”
Late Presentation Cervical Arterial Dysfunction • • • Drop attacks Dizziness Dysphagia (difficulty swallowing) Dysarthria (speech change, either slurred or slowed) Diplopia (double vision) Nausea Nystagmus Facial lip paresthesiae/ facial numbness Cranial nerve dysfunction
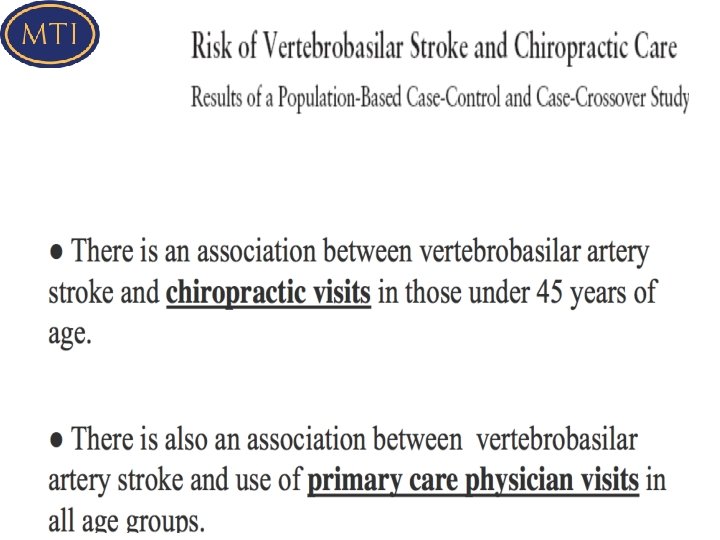
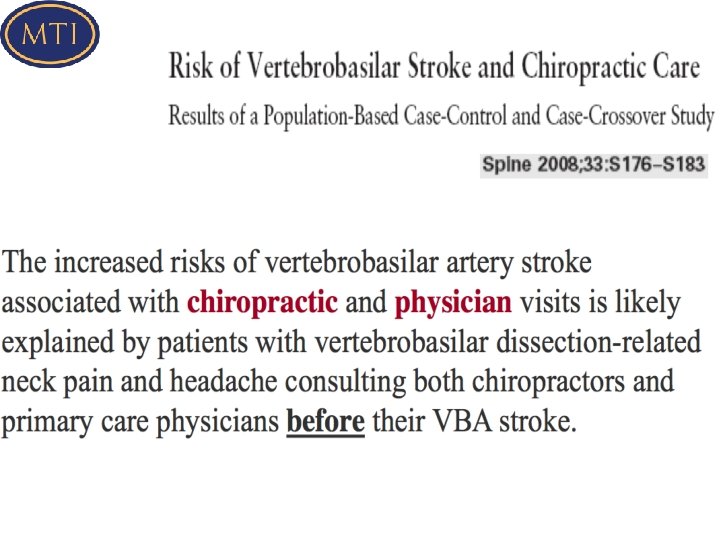
Clinical Reasoning • Estimated risk of serious complications resulting from HVT of the cervical spine has been reported to range between 1 in 4500 (Dunne et al. , 2000) to 6 in 10 million (Hurwitz et al. , 1996) • Precise risk of injury is indeterminable due to the unknown number of unreported cases (Ernst, 2004; Carlesso et al. 2010 a) and the paucity of methodologically sound research studies (Kerry et al. , 2008). • Minor to moderate adverse events following manual therapy may be as high as 50% • The risk of major adverse events with manual therapy is reported to be low (Carlesso et al. , 2010). • Nevertheless, given the limitations of known prevalence and the serious nature of the adverse event, manipulation of the upper cervical spine remains a contentious issue
Primary Presenting Features of Carotid/Vertebral Artery Dissection • A case control study by Rivett et al (2015) looked at 21 patients < 55 years with radiologically confirmed vertebral or carotid artery dissection • They were interviewed about risk factors, preceding events and clinical features of their stroke • Headache and neck pain, speech disturbance, limb weakness, were the primary presenting features • Balance disturbance and ptosis were mentioned, to a lesser extent
Primary Presenting Features of CAD • Importantly, a high proportion of participants (67%) with CAD reported transient ischemic features prior to their admission to hospital • This is considerably higher than rates reported prior to general stroke, which range between 4% and 16% • These transient ischemic features have not been identified in previous studies • Question patients carefully for such features!!
Risk Factors Cervical Arterial Dysfunction History of trauma to cervical spine History of migraine-type headache Hypertension Hypercholesterolemia / hyperlipidemia Cardiac disease, vascular disease, previous cerebrovascular accident or transient ischaemic attack • Diabetes mellitus • Blood clotting disorders • • •
Risk Factors Cervical Arterial Dysfunction • • Anticoagulant therapy Long-term use of steroids History of smoking Recent infection Immediately post partum Trivial head or neck trauma Absence of a plausible mechanical explanation for the patient’s symptoms
Risk Factors Trauma identified by participants fit into 3 main categories: 1. abrupt or jerky head movements 2. intense or unusual physical effort 3. activities involving sustained extended positions of the neck Question patients with recent-onset neck pain or headache about exposure to these types of activity within the last month
Risk Factors Trauma • Recent prior minor mechanical trauma or strain to the neck is an important feature in CAD. • This may include cervical manipulation, but less vigorous manual techniques or exercises should also be considered. • The finding that recent minor mechanical trauma or strain to the neck was associated with CAD is consistent with the findings of other reports.
Risk Factors Smoking • 21% of participants with CAD were smokers, reflecting the percentage of smokers for this age group in the general population • Smoking is associated with higher blood levels of inflammatory mediators, which may have implications for vessel-wall health • However, no participant had elevated blood levels of any inflammatory markers
Risk Factors Infection • 21% of participants reported a recent infection prior to CAD • Despite the low incidence in this current study, and in respect to the higher incidence found in other studies, we recommend that clinicians specifically question patients presenting with recent-onset neck pain or headache about recent infections
Risk Factors Blood Pressure • Hypertension is considered a risk factor for carotid and vertebral artery disease. • An increase in blood pressure may be related to acute arterial trauma • Evaluation of blood pressure as part of the physical examination may therefore be a valuable test to inform clinical reasoning. • Although hypertension is a strong predictor of cardiovascular disease, interpretation of readings must be in the context of other findings, and sound clinical reasoning
Risk Factors Cardiovascular Risk Factors • General cardiovascular risk factors, with the exception of diagnosed migraine, were not strongly represented in the CAD group, suggesting that they may not be useful indicators of risk of dissection. • This is inconsistent with current recommendations for general cardiovascular screening prior to any cervical manual treatment. • A history of diagnosed migraine may be a potential risk factor for dissection; however, it may be difficult to distinguish the clinical presentation of migraine headache from a dissection in progress
Risk Factors Prior Cervical Manipulation • Cervical manipulation was not a statistically significant factor in this study. • Of concern is that any manual treatment could potentially be implicated if a patient with CAD were to seek treatment for neck pain or headache.
Risk Factors Age • The major vascular complication after cervical manipulation occurred predominantly in young adults • This finding suggests that cervical osteoarthritic changes would not be the pathogenesis in the majority of these cases
Cervical Manipulation Trauma • Do not ignore the close temporal association between trauma and the number of cases of VA dissection, • Trauma can be from manipulation, trivial trauma, MVA’s, or strenuous activity. • Significantly, symptoms of VA dissection are acute neck pain and headache, which are exactly the symptoms for which patients seek treatment and for which they not uncommonly receive manipulation
Pre-screening Vertebral Artery • Current research does not support the contention that provocative positional testing can accurately identify patients at risk for cervical artery disease • Vertebral artery testing procedures have a sensitivity and specificity that approximates zero: high likelihood of false negative findings. • Test procedures for the vertebral artery also hold a certain risk, and screening tests will not identify all patients at risk of suffering adverse reaction to cervical manipulation
Vertebral Artery Test • There is no known method for testing the intrinsic anatomy of the vertebral artery • Doppler studies (Arnold, 2004) have shown that only full range cervical rotation and a premanipulative hold at C 1 -2 stresses the vertebral artery sufficiently to demonstrate reduction of bloodflow. • Clinical Guidelines of the Australian Physiotherapy Association recommend that only rotation be used to test for VBI.
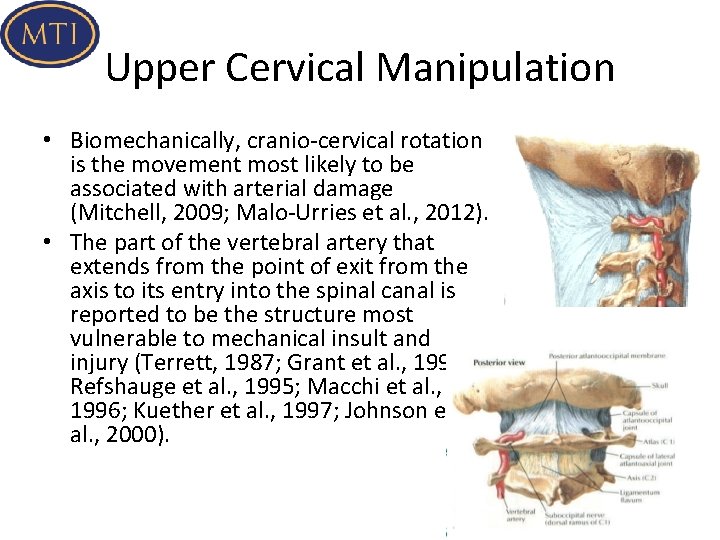
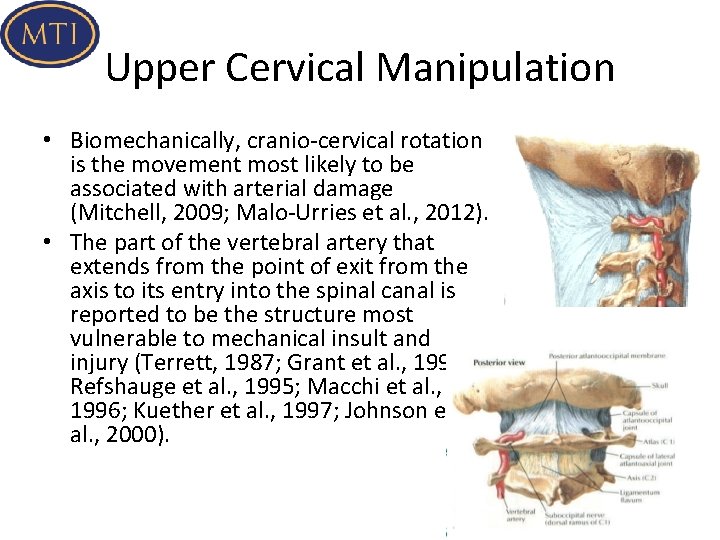
Upper Cervical Manipulation • Biomechanically, cranio-cervical rotation is the movement most likely to be associated with arterial damage (Mitchell, 2009; Malo-Urries et al. , 2012). • The part of the vertebral artery that extends from the point of exit from the axis to its entry into the spinal canal is reported to be the structure most vulnerable to mechanical insult and injury (Terrett, 1987; Grant et al. , 1994; Refshauge et al. , 1995; Macchi et al. , 1996; Kuether et al. , 1997; Johnson et al. , 2000).
Upper Cervical Manipulation • One underlying concern is that manipulation involving rotation may, at least momentarily, alter the velocity of blood flow in one or both of the vertebral arteries. However, this argument seems to be dispelled by a study by Erhardt et al (2015). • In this study they tried to quantify changes in blood flow velocity in the VA during manipulation of C 1 -2 (Manual Therapy 2015).
• Findings of this study indicate that in normal subjects, blood flow velocity of vertebral artery is not affected by manipulation of C 1 -2 Therefore, in apparently healthy vessels, manipulation of C 1 -2 does not appear to increase mechanical stress on the vertebral artery. • It remains unknown whether adverse haemodynamic responses would be recorded in the presence of vessel hypoplasia, vessel wall pathology or inherent weakness.
• As such this study indirectly supports a stance taken by IFOMPT (Rushton et al. , 2012) that careful subjective and objective risk assessment combined with prudent clinical reasoning may be the way to progress for clinicians.
• A review by Puentedura et al in 2012 of 134 cases describing patients who experienced severe adverse events after cervical manipulation showed that, if all contraindications and red flags were ruled out, there was potential for a clinician to prevent 44. 8% of adverse events • Additionally, 10. 4% of the events were unpreventable, suggesting some inherent risk associated with cervical manipulation even after thorough exam and proper clinical reasoning.
Alternative Approach to Direct Cervical Treatment • Current evidence suggests a large likelihood of improved patient outcomes when thoracic manipulation is coupled with cervical active range of movement exercises • Subsequent sessions can then introduce more direct manual cervical treatments if warranted
How to proceed in the absence of certainty • Cervical artery strokes are rare, but are an important consideration as part of your assessment • Arterial dissection and other vascular presentations are fairly recognizable if the appropriate questions are asked during the patient history, • Based on the current evidence, there is no strong foundation for the claim that there is a causal relationship between cervical manipulation and vertebral artery dissection or stroke. • There is no strong empirical evidence to support the notion that upper cervical manipulation carries any greater risk of injury than middle or lower cervical manipulation, or that non thrust mobilization to any region of the cervical spine carries any less risk than manipulation to the same region
How to proceed in the face of uncertainty • Upper cervical manipulations, especially the ones involving rotation, should be used with caution. • Stay away from endrange techniques, especially extension and rotation • Develop a high index of suspicion for cervical vascular pathology, especially with cervical trauma

How to proceed in the absence of certainty • Consider limitations of current objective tests. • In cases of acute onset headache “unlike any other”, conservative treatment techniques are recommended in the early stages • Do not further examine or treat a patient with signs and symptoms of cervical artery disease
How to proceed in the absence of certainty • You cannot ignore the presence of cardinal signs and symptoms • A patient with cardinal signs and symptoms warrants a referral to a medical specialist for appropriate management • Incorporate T spine manipulation in the treatment of C spine disorders.
How to proceed in the absence of certainty • Patients may present for treatment of acuteonset headache or neck pain arising from a dissection in progress. • Individuals with CAD may have transient ischemic signs and symptoms as warning signs in the preceding few weeks. .

How to proceed in the absence of certainty • Carefully question patients presenting with recent onset, moderate to severe, or unusual neck pain or headache about minor trauma and any signs of visual disturbance, dizziness and balance deficits, arm paresthesia, or speech deficits • Arterial dissection is fairly recognizable if the appropriate questions are asked
VBI and Upper Cervical Stability Screening Protocol • Expert history taking. Questions should include the following: presence of neck trauma, presence of cardinal symptoms, RA, stroke, steroid use, symptom aggravation with movements or positions, worsening symptoms • Upper cervical ligamentous stability testing • Sustained end range cervical rotation to the left and the right. To be done in sitting first. If no problems, progress to supine. Maintain each position with overpressure for 10 seconds (or less if symptoms are provoked) and on release, a period of 10 seconds should elapse to allow for any latent response to the sustained position. The patient is asked about dizziness during each test, and the eyes are observed for the presence of nystagmus • The position or movement that provokes symptoms as described by the patient • Sustained mobilization position M Always assess prior and immediately after a technique involving endrange rotation, as well as first thing next visit…
Informed Consent • Obtain informed consent. • Document it as such in your notes. • Since specific requirement for informed consent differ from country to country and more importantly for us, from state to state, it is difficult to specify how this needs to be worded
Informed Consent • We recommend something along the following lines: • "I would like to perform a "quick stretch" on your neck to improve range of motion of a particular joint. This is likely to improve and/or eliminate your neck, shoulder symptoms (also could refer to arm or headache). You may sense a "popping" of the joint and may experience some local soreness due to the stretching procedure. Is it ok to perform this quick stretch? ” • The use of the term “quick stretch” circumvents the use of the word manipulation, which in many states can give rise to problems.

Cervical Manipulation Critical Rules • Don’t overlock • No follow through on the thrust • Low amplitude
Additional Good Advice Use minimal leverage Use non-torsional techniques There should be no pain Use multiple components so the main thrust can be minimal • Excessive force conceals weakness • •