Cervical Spine Anatomy and Approaches Claris Shi Anatomy
- Slides: 26
Cervical Spine: Anatomy and Approaches Claris Shi
Anatomy • 7 vertebrae • C 1 and C 2 form a unique set of articulations providing mobility in C spine • 50% of flexion/extension occurs between occiput and C 1 • 50% of rotation occurs between C 1 and C 2 • Anatomic landmarks • C 1 – base of nose and hard palate • C 2 – teeth of closed mouth • C 3 – mandible/hyoid bone • C 4 – common carotid bifurcation • C 4/5 – thyroid cartilage • C 6/7 – cricoid cartilage • C 6 – carotid pulse palpated against C 6 transverse process
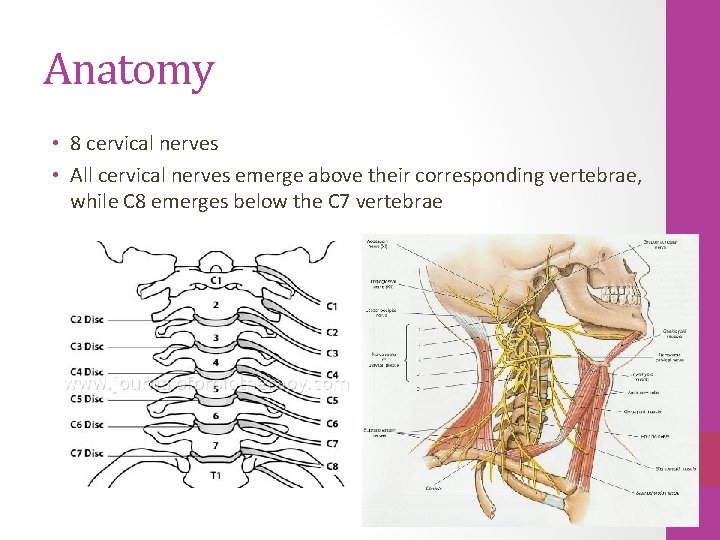
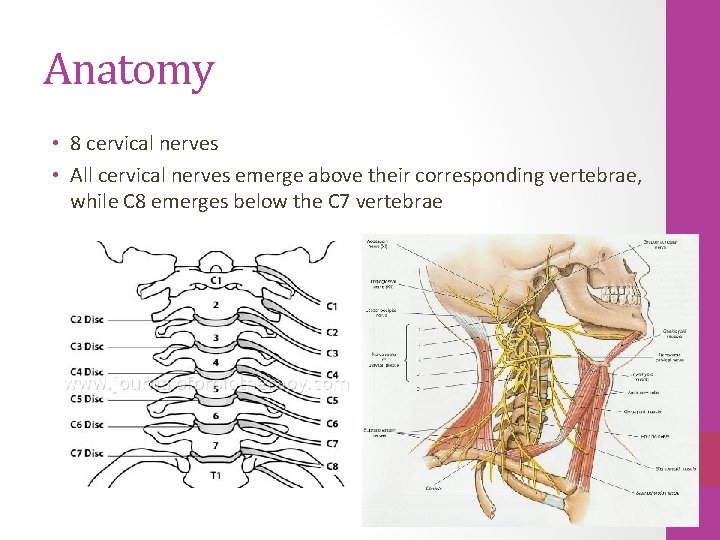
Anatomy • 8 cervical nerves • All cervical nerves emerge above their corresponding vertebrae, while C 8 emerges below the C 7 vertebrae
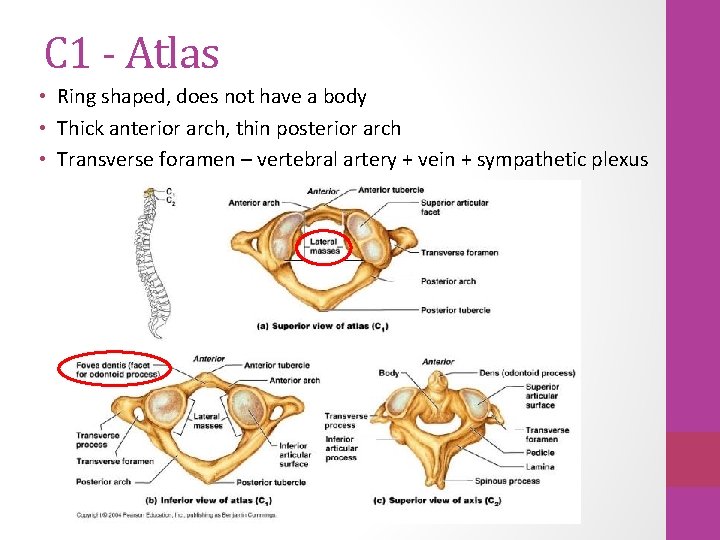
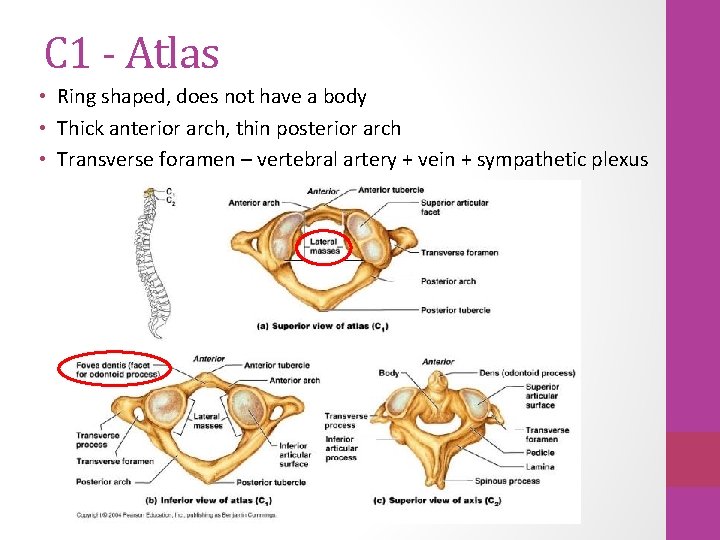
C 1 - Atlas • Ring shaped, does not have a body • Thick anterior arch, thin posterior arch • Transverse foramen – vertebral artery + vein + sympathetic plexus
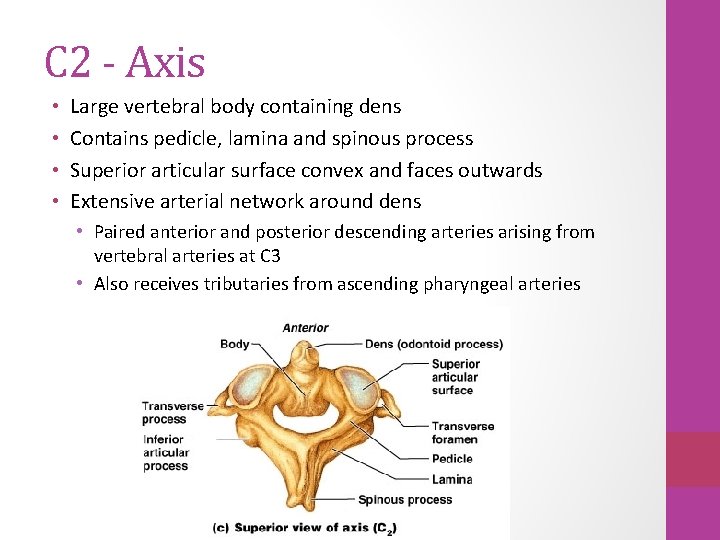
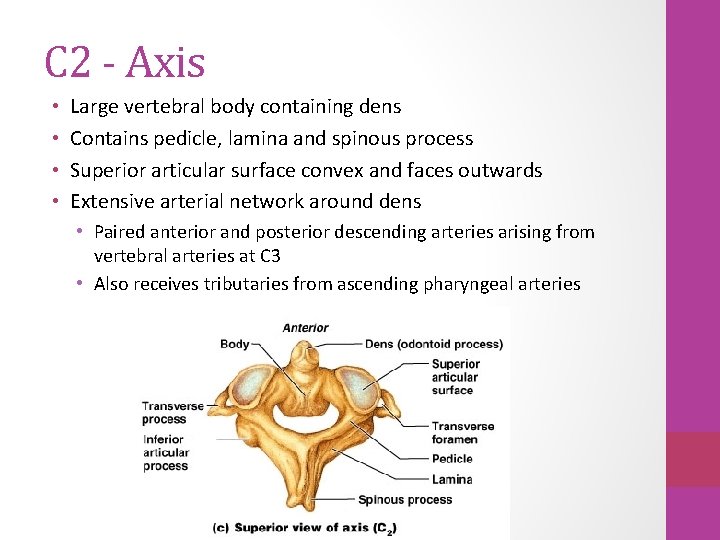
C 2 - Axis • • Large vertebral body containing dens Contains pedicle, lamina and spinous process Superior articular surface convex and faces outwards Extensive arterial network around dens • Paired anterior and posterior descending arteries arising from vertebral arteries at C 3 • Also receives tributaries from ascending pharyngeal arteries
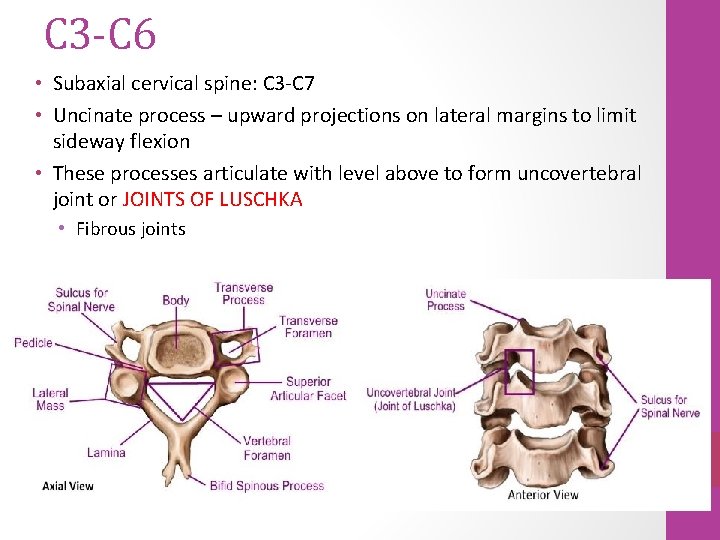
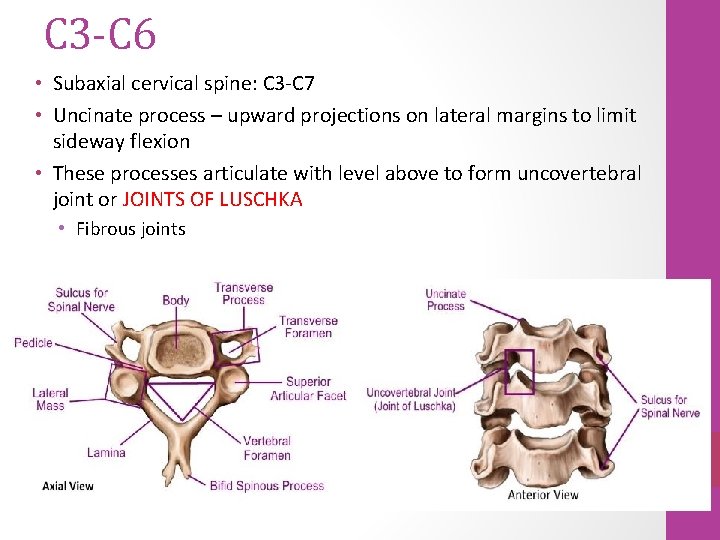
C 3 -C 6 • Subaxial cervical spine: C 3 -C 7 • Uncinate process – upward projections on lateral margins to limit sideway flexion • These processes articulate with level above to form uncovertebral joint or JOINTS OF LUSCHKA • Fibrous joints
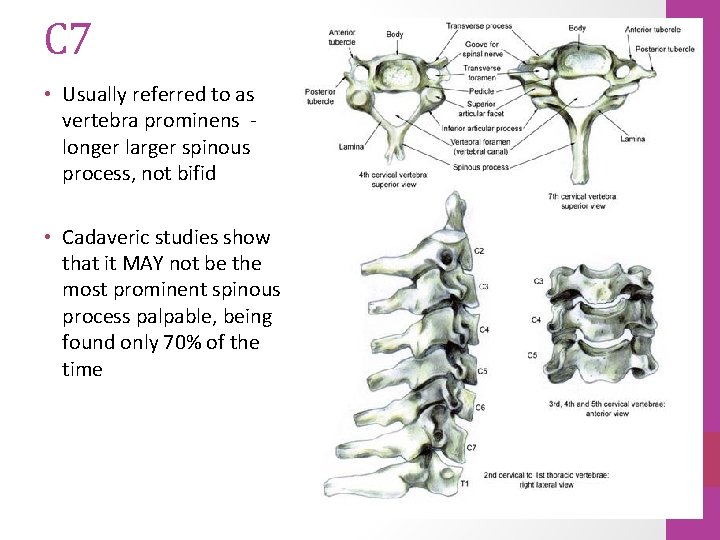
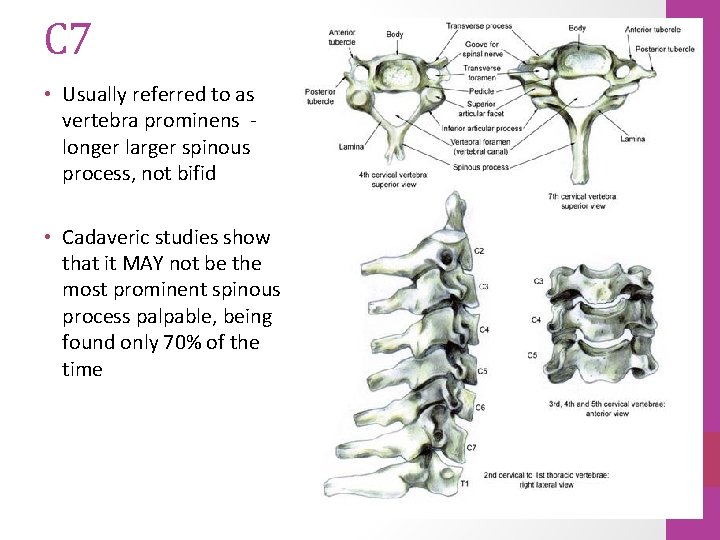
C 7 • Usually referred to as vertebra prominens longer larger spinous process, not bifid • Cadaveric studies show that it MAY not be the most prominent spinous process palpable, being found only 70% of the time
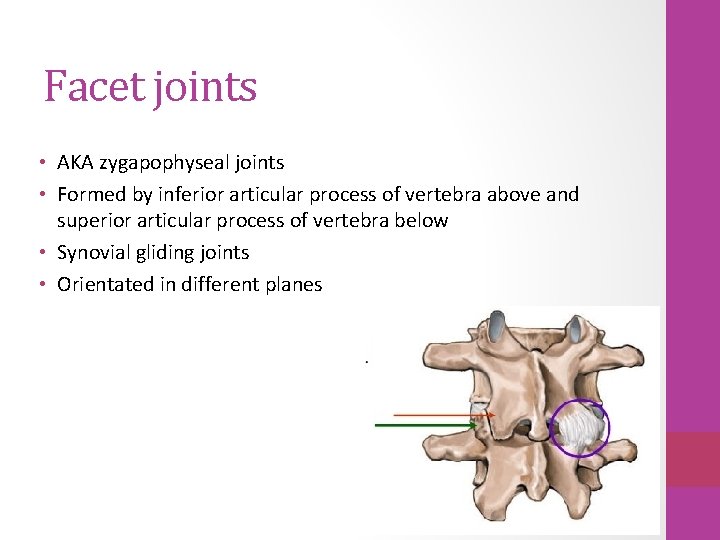
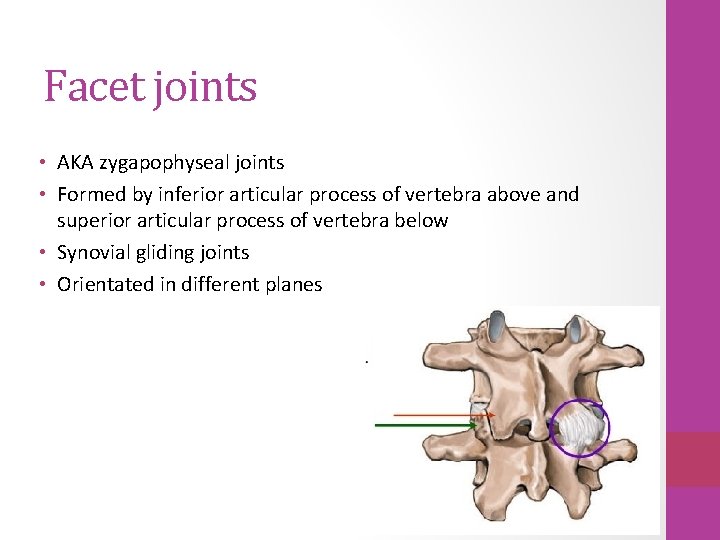
Facet joints • AKA zygapophyseal joints • Formed by inferior articular process of vertebra above and superior articular process of vertebra below • Synovial gliding joints • Orientated in different planes
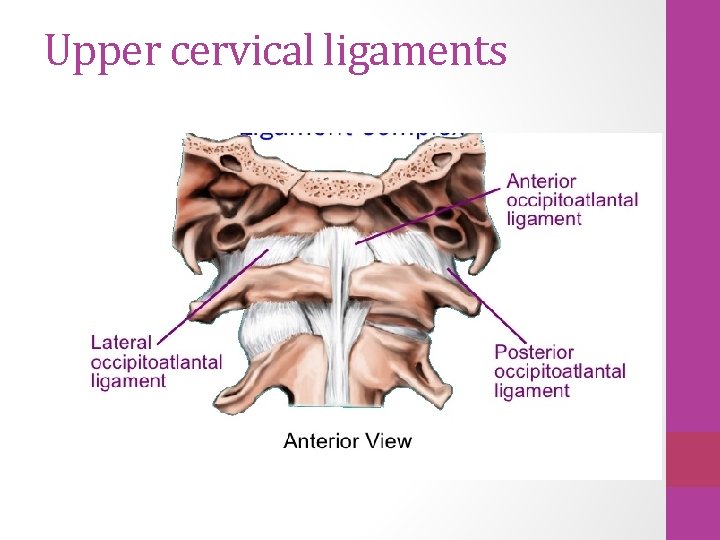
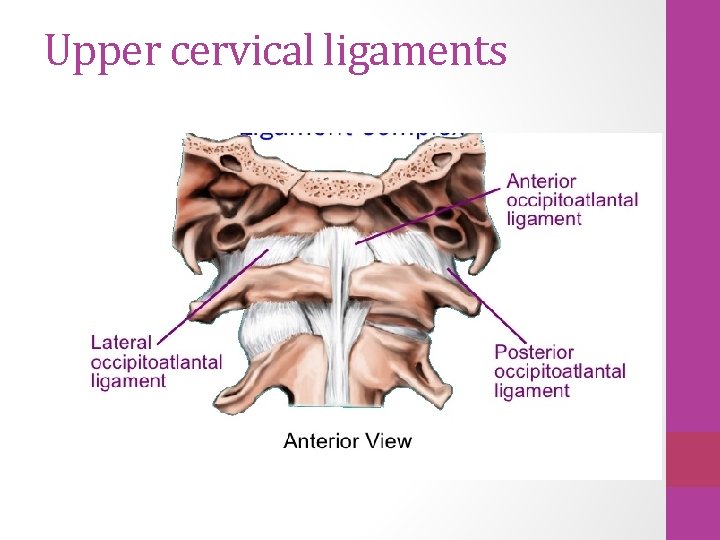
Upper cervical ligaments
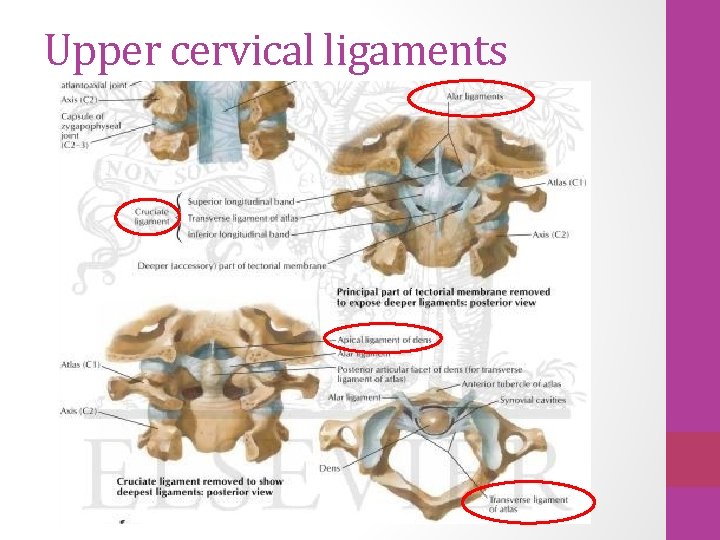
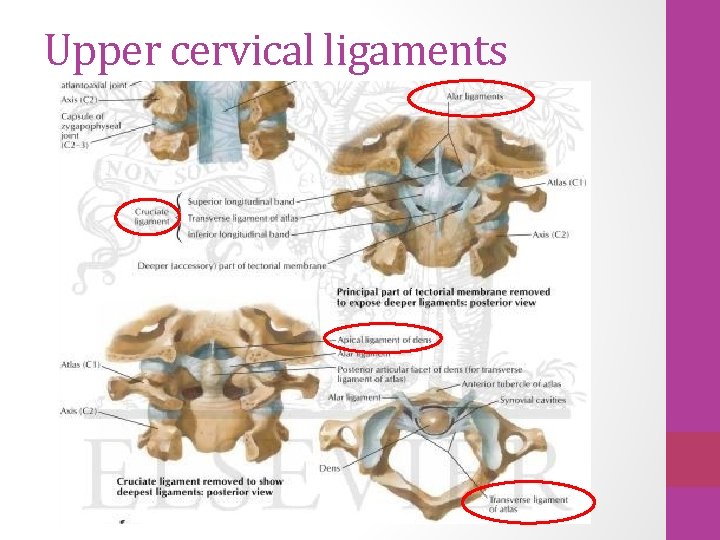
Upper cervical ligaments
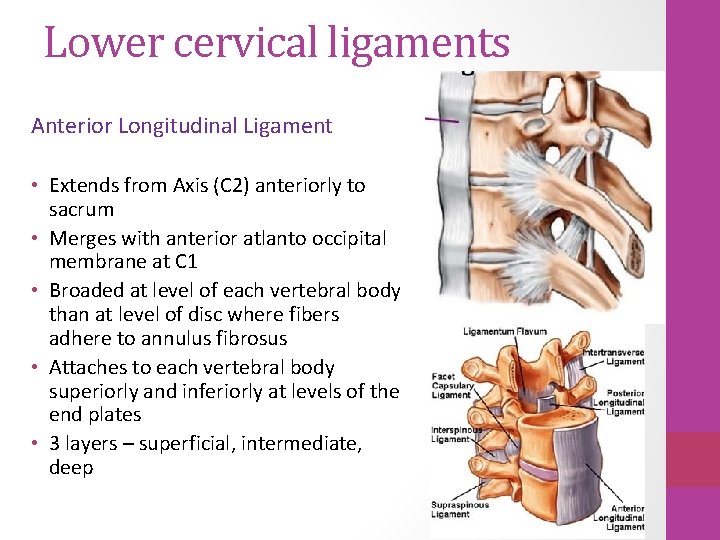
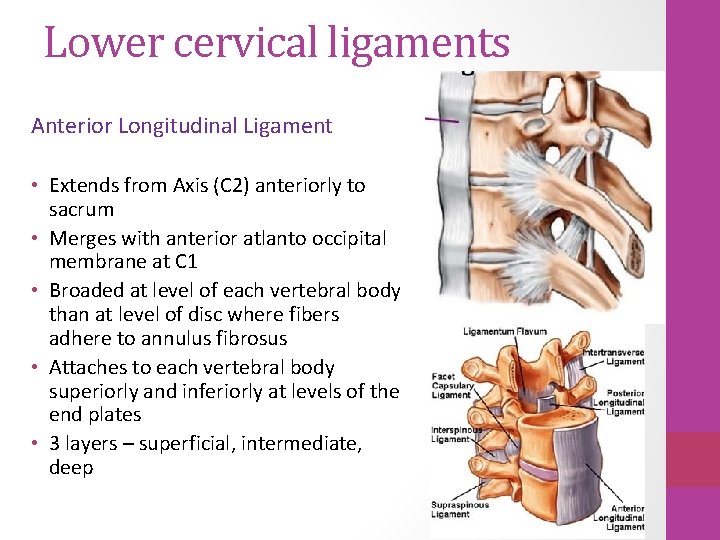
Lower cervical ligaments Anterior Longitudinal Ligament • Extends from Axis (C 2) anteriorly to sacrum • Merges with anterior atlanto occipital membrane at C 1 • Broaded at level of each vertebral body than at level of disc where fibers adhere to annulus fibrosus • Attaches to each vertebral body superiorly and inferiorly at levels of the end plates • 3 layers – superficial, intermediate, deep
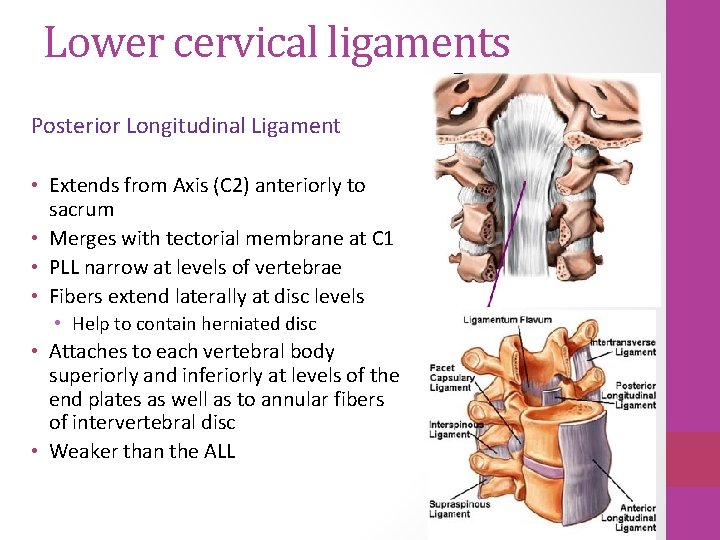
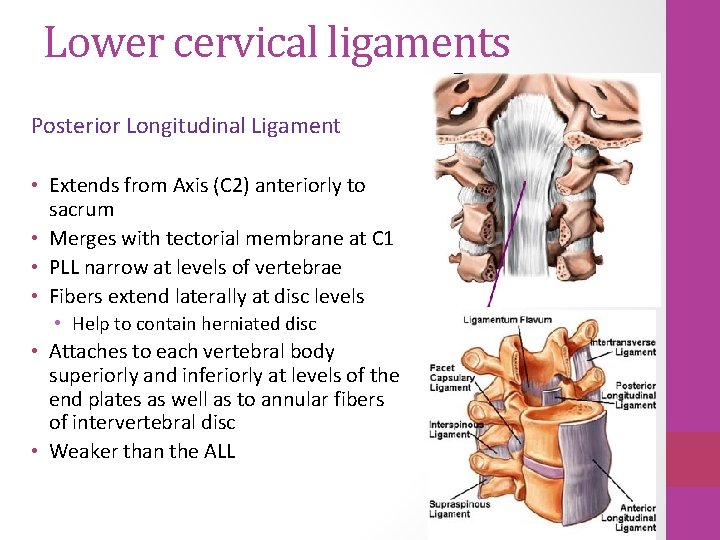
Lower cervical ligaments Posterior Longitudinal Ligament • Extends from Axis (C 2) anteriorly to sacrum • Merges with tectorial membrane at C 1 • PLL narrow at levels of vertebrae • Fibers extend laterally at disc levels • Help to contain herniated disc • Attaches to each vertebral body superiorly and inferiorly at levels of the end plates as well as to annular fibers of intervertebral disc • Weaker than the ALL
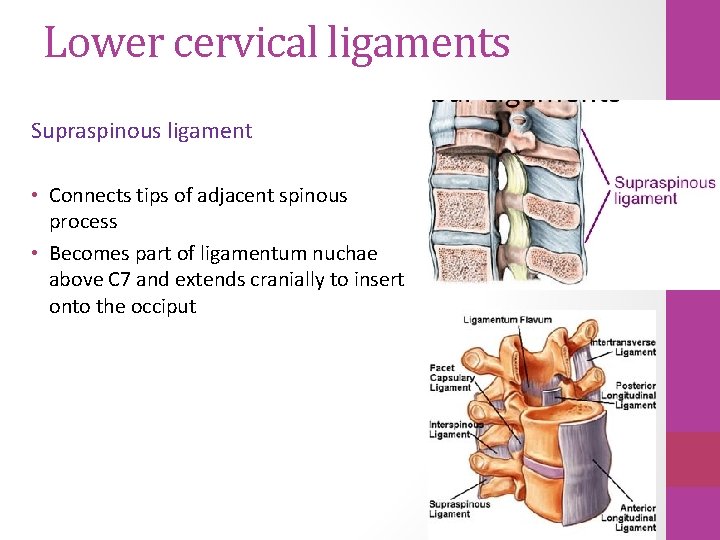
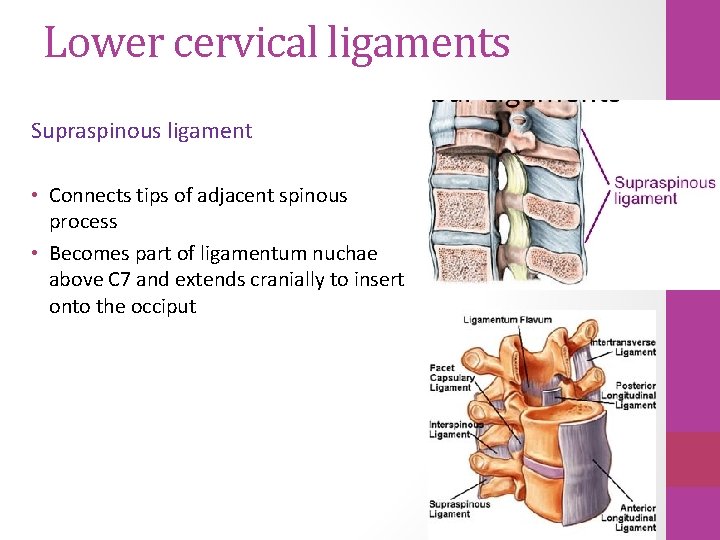
Lower cervical ligaments Supraspinous ligament • Connects tips of adjacent spinous process • Becomes part of ligamentum nuchae above C 7 and extends cranially to insert onto the occiput
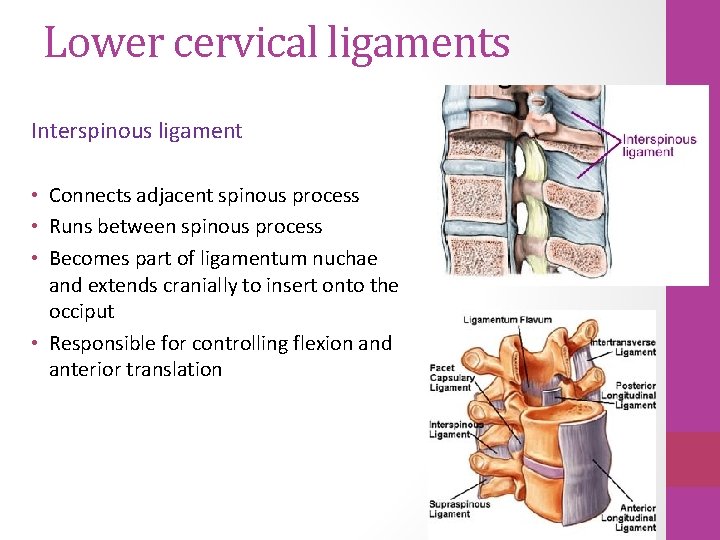
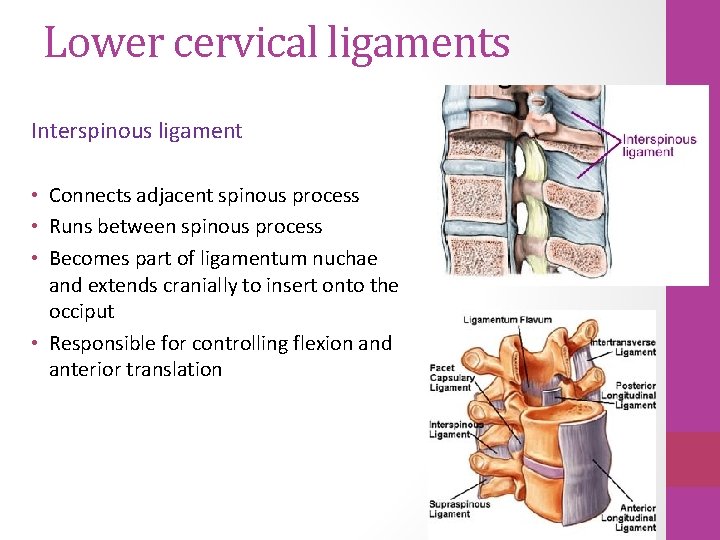
Lower cervical ligaments Interspinous ligament • Connects adjacent spinous process • Runs between spinous process • Becomes part of ligamentum nuchae and extends cranially to insert onto the occiput • Responsible for controlling flexion and anterior translation
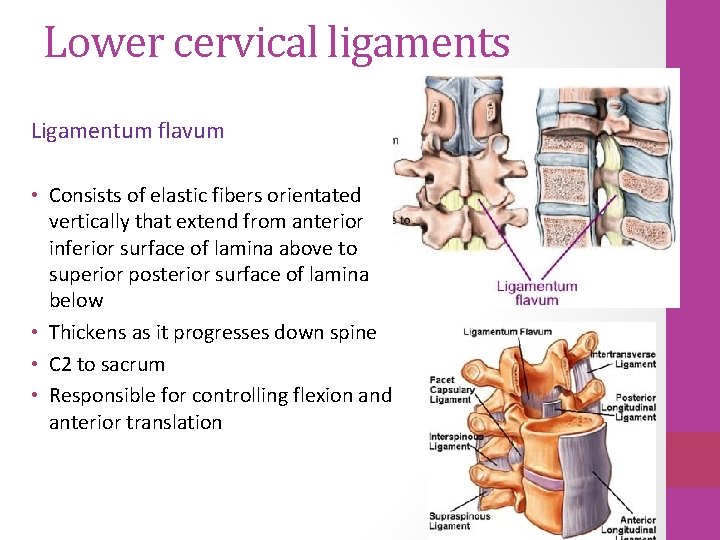
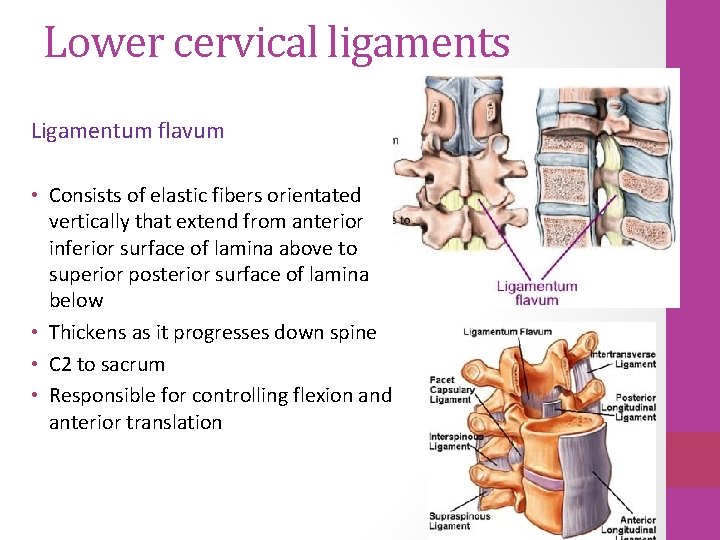
Lower cervical ligaments Ligamentum flavum • Consists of elastic fibers orientated vertically that extend from anterior inferior surface of lamina above to superior posterior surface of lamina below • Thickens as it progresses down spine • C 2 to sacrum • Responsible for controlling flexion and anterior translation
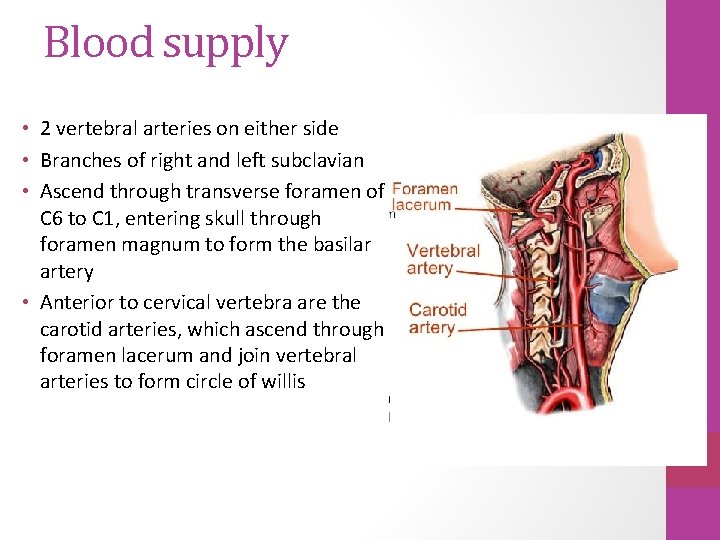
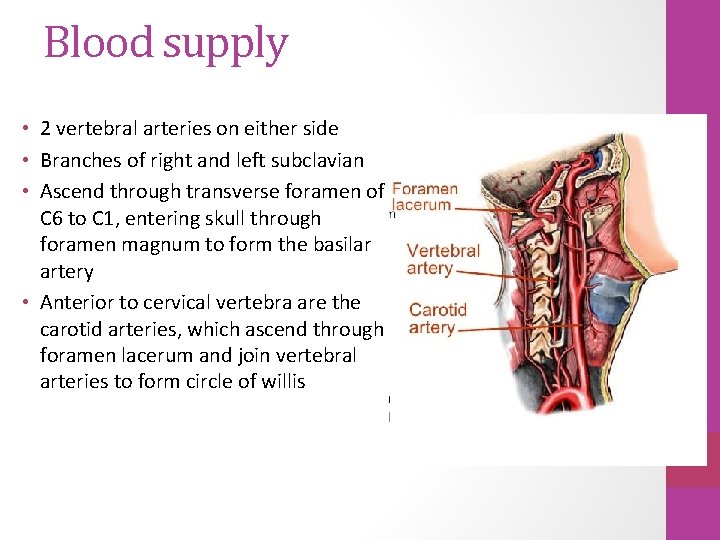
Blood supply • 2 vertebral arteries on either side • Branches of right and left subclavian • Ascend through transverse foramen of C 6 to C 1, entering skull through foramen magnum to form the basilar artery • Anterior to cervical vertebra are the carotid arteries, which ascend through foramen lacerum and join vertebral arteries to form circle of willis
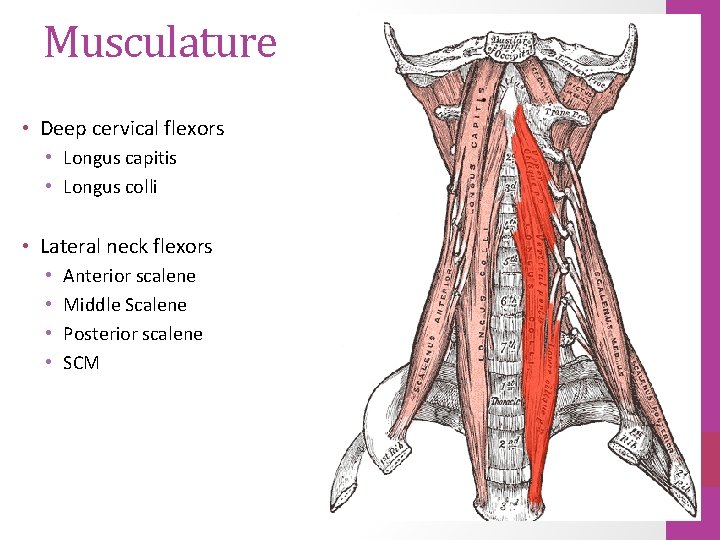
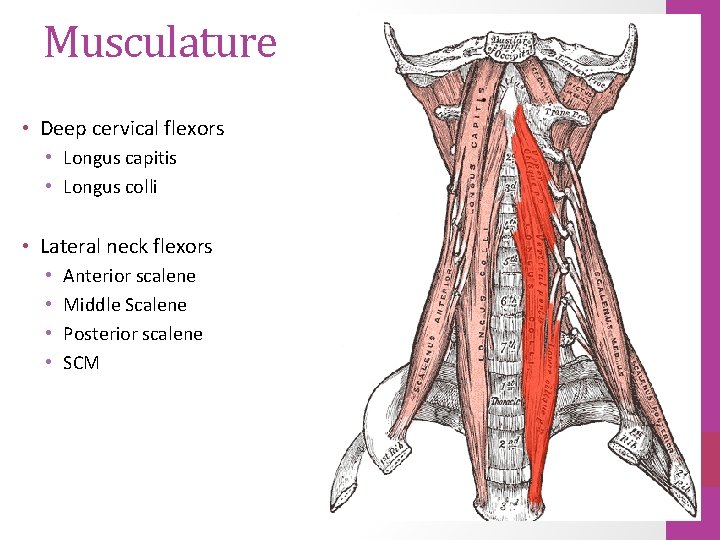
Musculature • Deep cervical flexors • Longus capitis • Longus colli • Lateral neck flexors • • Anterior scalene Middle Scalene Posterior scalene SCM
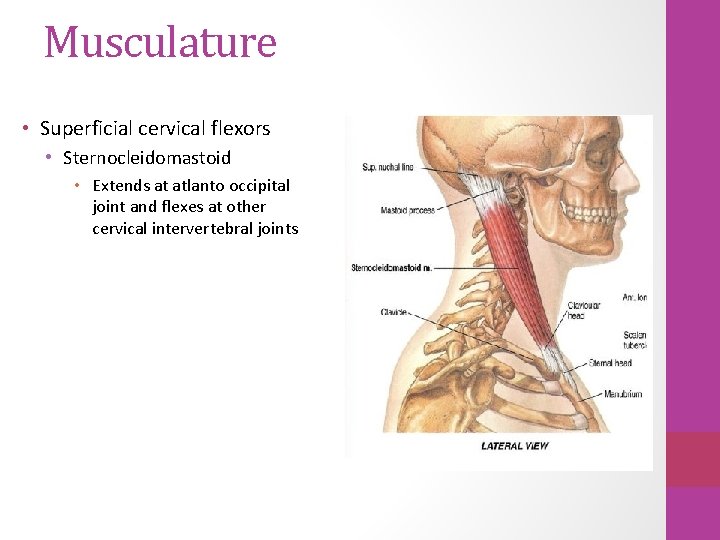
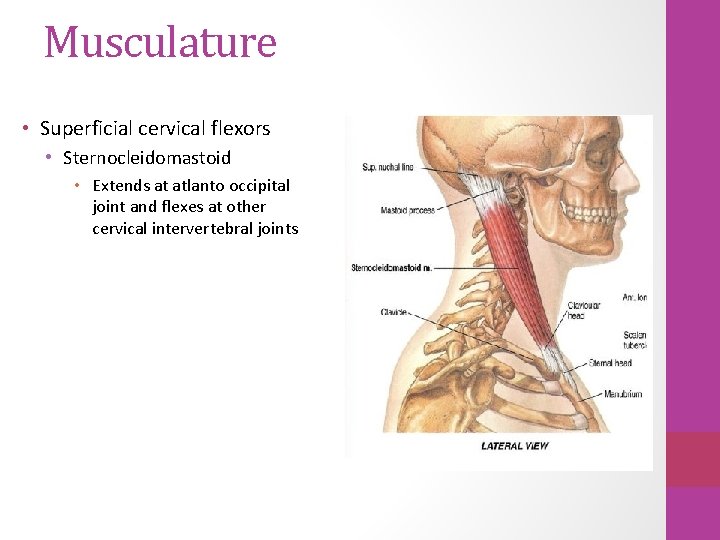
Musculature • Superficial cervical flexors • Sternocleidomastoid • Extends at atlanto occipital joint and flexes at other cervical intervertebral joints
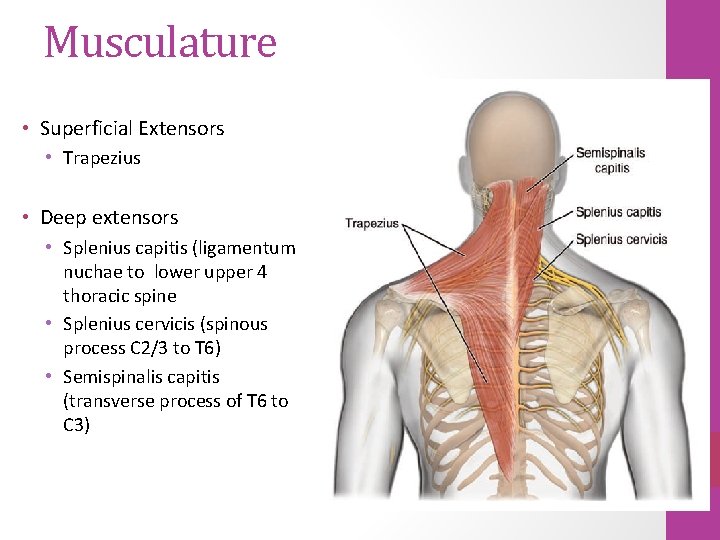
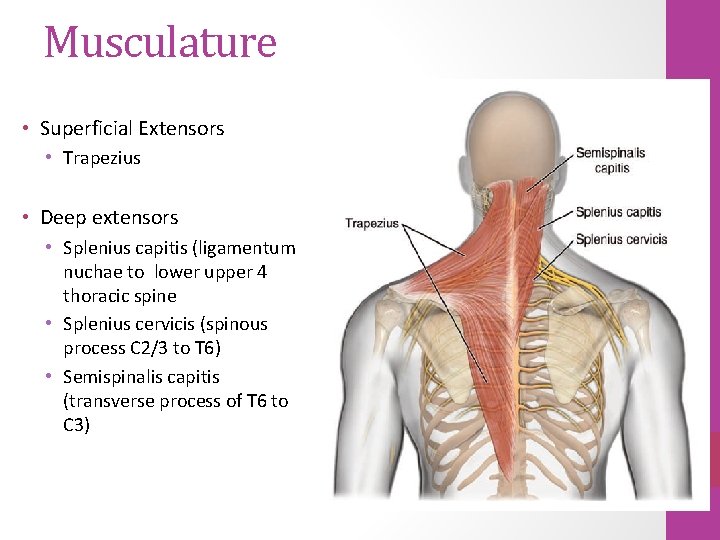
Musculature • Superficial Extensors • Trapezius • Deep extensors • Splenius capitis (ligamentum nuchae to lower upper 4 thoracic spine • Splenius cervicis (spinous process C 2/3 to T 6) • Semispinalis capitis (transverse process of T 6 to C 3)
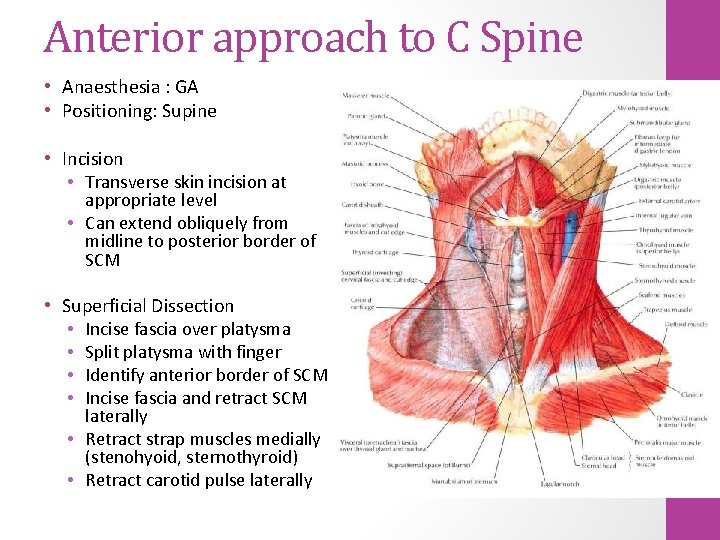
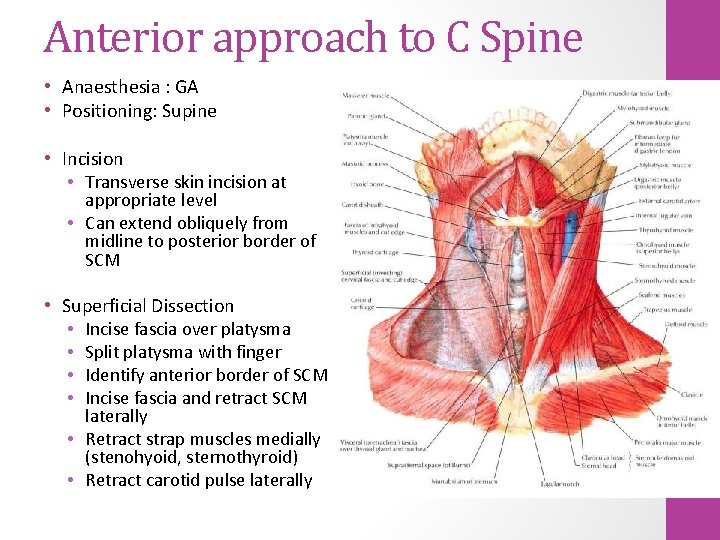
Anterior approach to C Spine • Anaesthesia : GA • Positioning: Supine • Incision • Transverse skin incision at appropriate level • Can extend obliquely from midline to posterior border of SCM • Superficial Dissection • Incise fascia over platysma • Split platysma with finger • Identify anterior border of SCM • Incise fascia and retract SCM laterally • Retract strap muscles medially (stenohyoid, sternothyroid) • Retract carotid pulse laterally
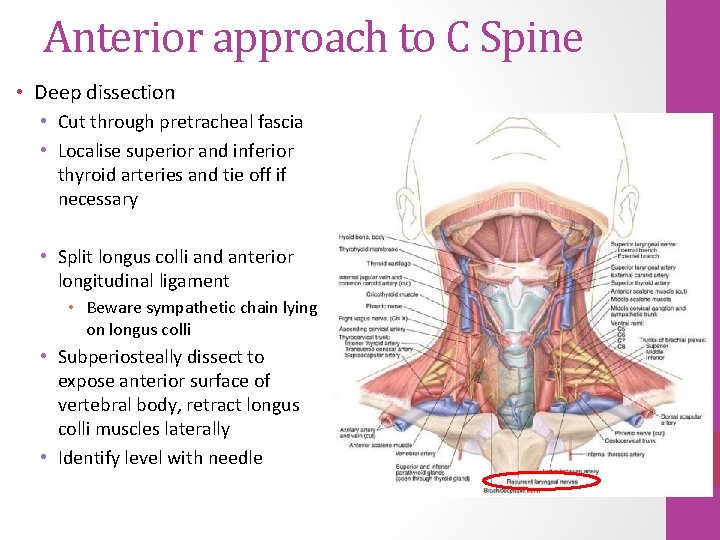
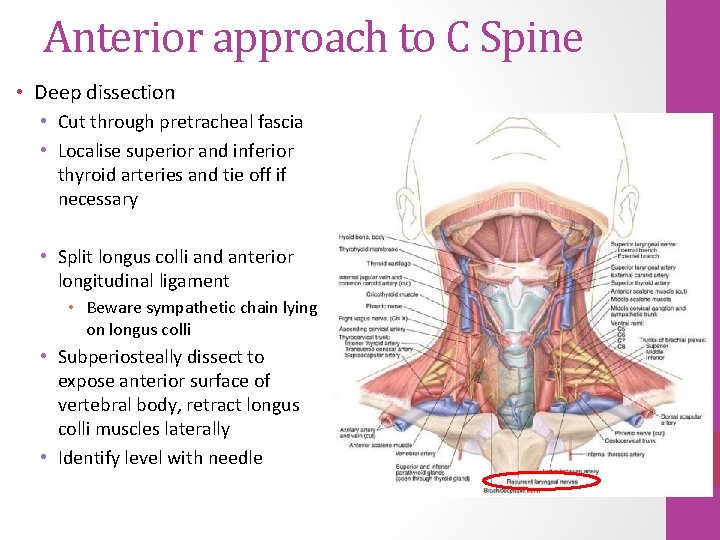
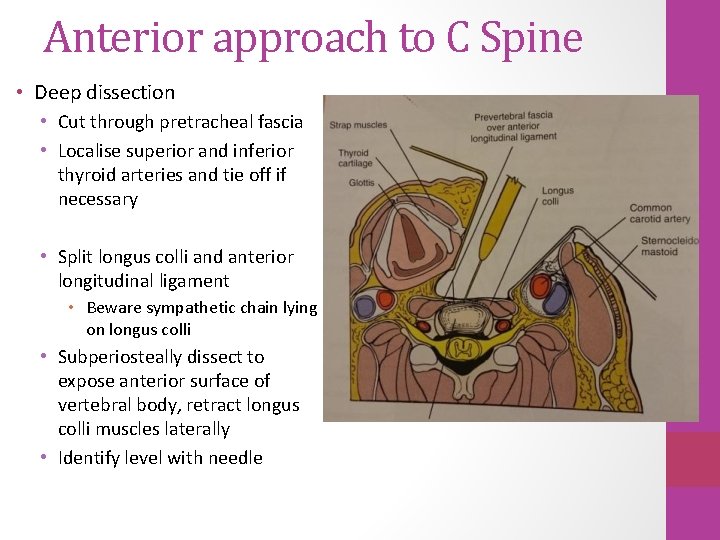
Anterior approach to C Spine • Deep dissection • Cut through pretracheal fascia • Localise superior and inferior thyroid arteries and tie off if necessary • Split longus colli and anterior longitudinal ligament • Beware sympathetic chain lying on longus colli • Subperiosteally dissect to expose anterior surface of vertebral body, retract longus colli muscles laterally • Identify level with needle
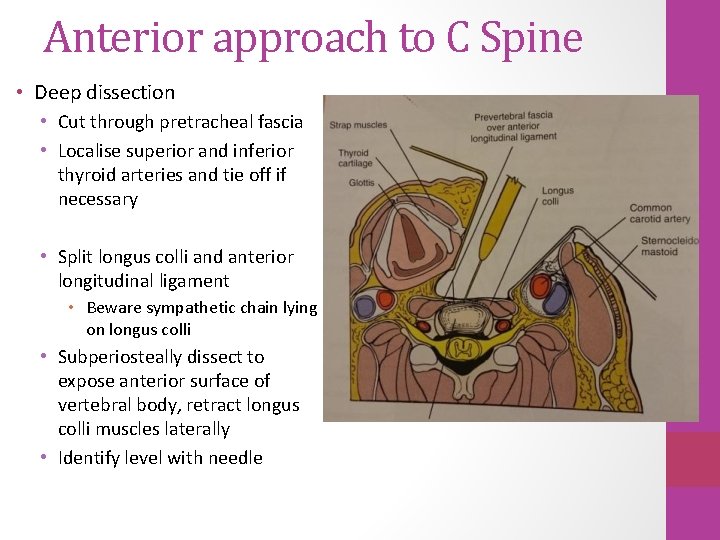
Anterior approach to C Spine • Deep dissection • Cut through pretracheal fascia • Localise superior and inferior thyroid arteries and tie off if necessary • Split longus colli and anterior longitudinal ligament • Beware sympathetic chain lying on longus colli • Subperiosteally dissect to expose anterior surface of vertebral body, retract longus colli muscles laterally • Identify level with needle
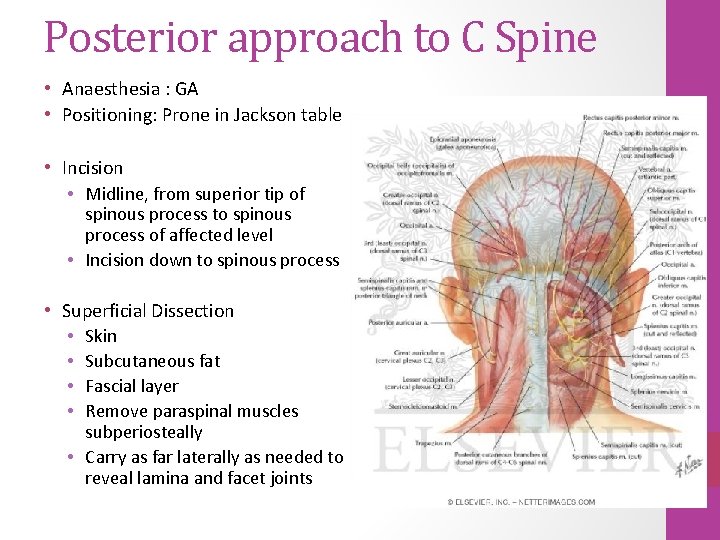
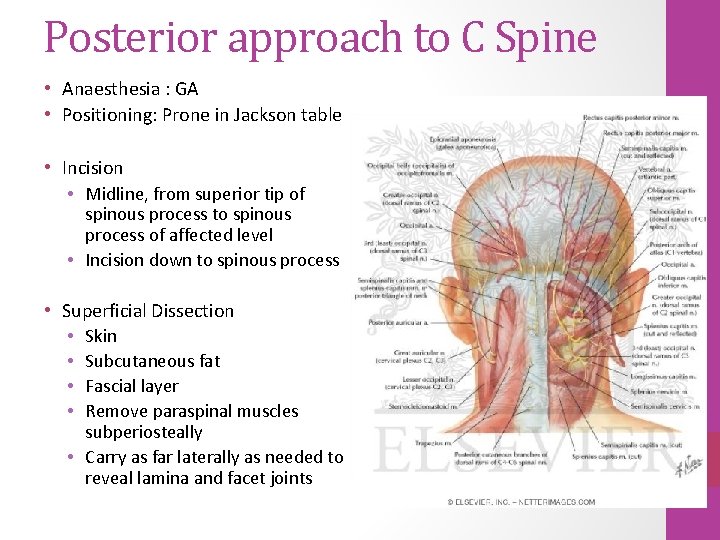
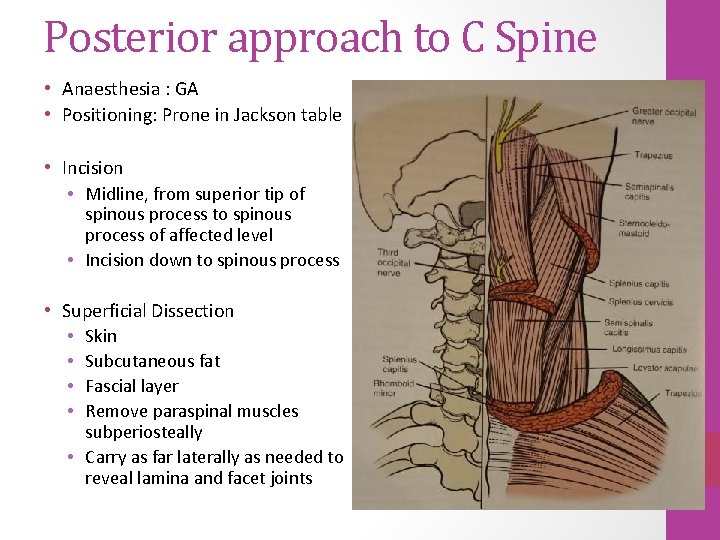
Posterior approach to C Spine • Anaesthesia : GA • Positioning: Prone in Jackson table • Incision • Midline, from superior tip of spinous process to spinous process of affected level • Incision down to spinous process • Superficial Dissection • Skin • Subcutaneous fat • Fascial layer • Remove paraspinal muscles subperiosteally • Carry as far laterally as needed to reveal lamina and facet joints
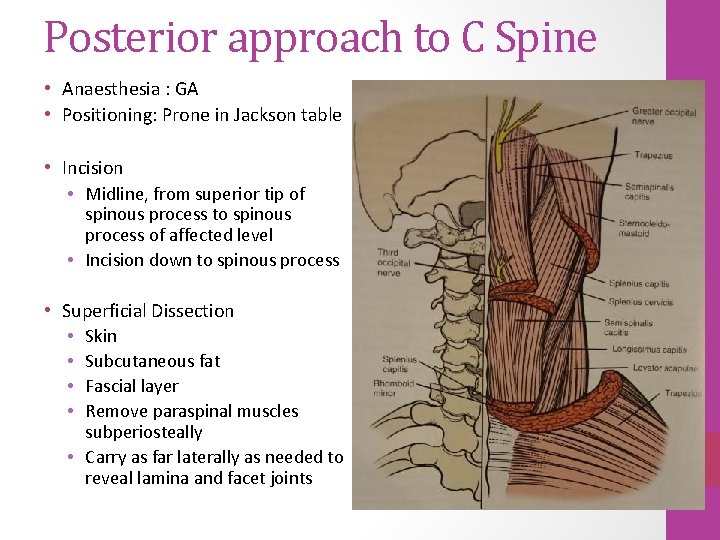
Posterior approach to C Spine • Anaesthesia : GA • Positioning: Prone in Jackson table • Incision • Midline, from superior tip of spinous process to spinous process of affected level • Incision down to spinous process • Superficial Dissection • Skin • Subcutaneous fat • Fascial layer • Remove paraspinal muscles subperiosteally • Carry as far laterally as needed to reveal lamina and facet joints
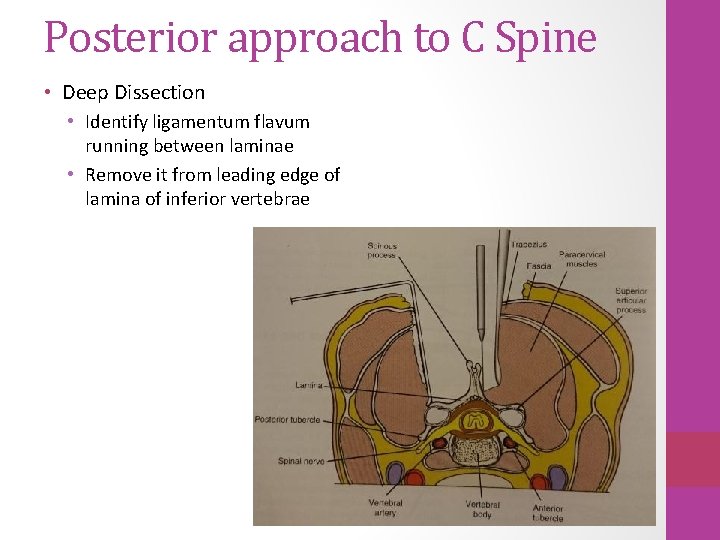
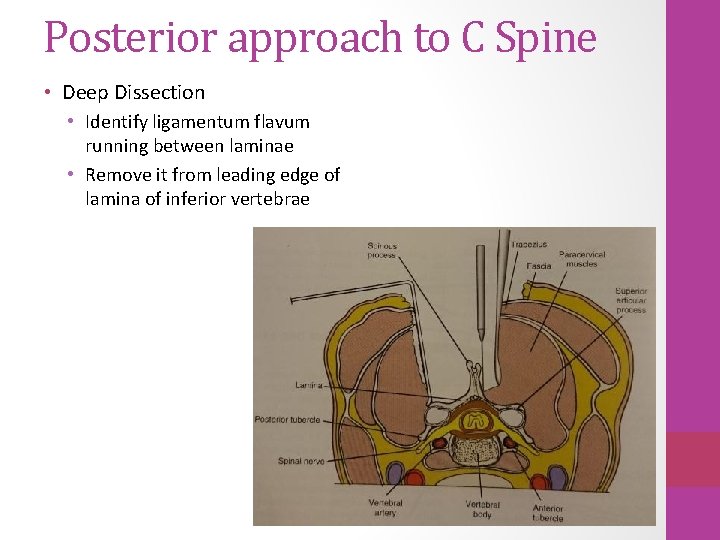
Posterior approach to C Spine • Deep Dissection • Identify ligamentum flavum running between laminae • Remove it from leading edge of lamina of inferior vertebrae
Thank You