Cervical Length Ultrasound Translating Knowledge Into Clinical Practice




















- Slides: 63
Cervical Length Ultrasound Translating Knowledge Into Clinical Practice
Goals § Review indications for cervical length measurement in the second and third trimester § Describe management of the short second trimester cervix based on fetal number and obstetrical history, including variations of routine management options § Describe evaluation and management of third trimester threatened preterm labor using cervical length and fetal fibronectin testing.
Indications for Cervical Length Measurement § Second Trimester § assess SPTB risk in women with or without prior SPTB § guide preventative care of SPTB in women with short cervix § Third Trimester § assess and guide care of women with threatened preterm labor
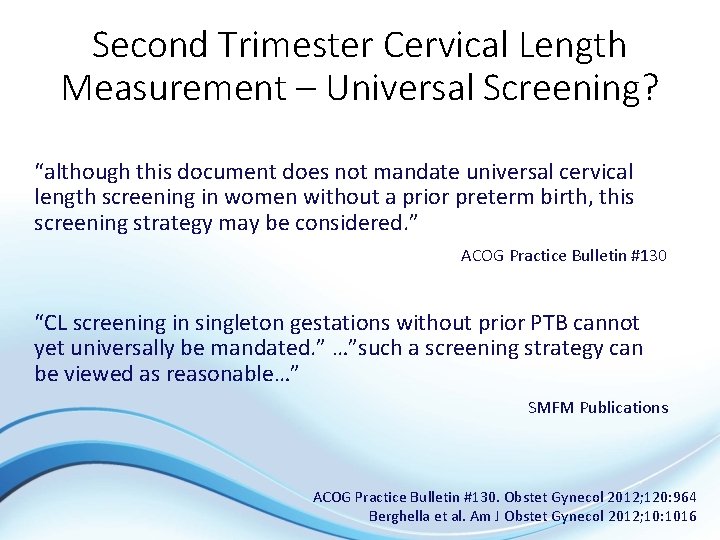
Second Trimester Cervical Length Measurement – Universal Screening? “although this document does not mandate universal cervical length screening in women without a prior preterm birth, this screening strategy may be considered. ” ACOG Practice Bulletin #130 “CL screening in singleton gestations without prior PTB cannot yet universally be mandated. ” …”such a screening strategy can be viewed as reasonable…” SMFM Publications ACOG Practice Bulletin #130. Obstet Gynecol 2012; 120: 964 Berghella et al. Am J Obstet Gynecol 2012; 10: 1016

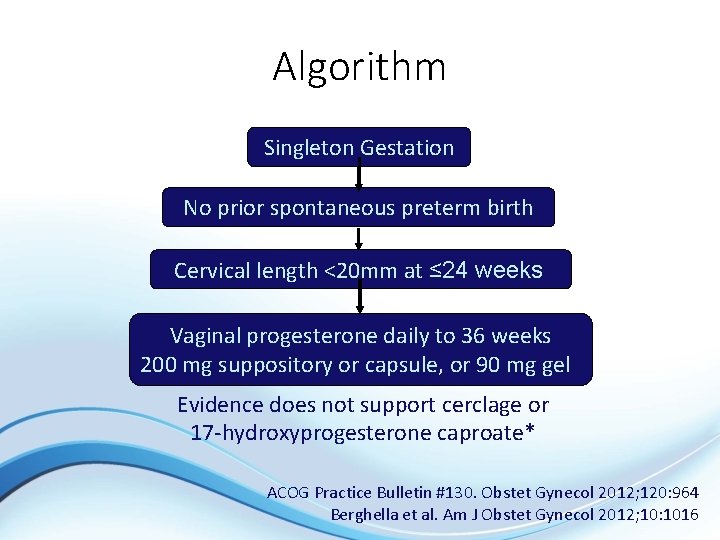
Singleton, no prior SPTB, short cervix (≤ 20 mm) ≤ 24 weeks § Is there an intervention to reduce prematurity risk? VAGINAL PROGESTERONE daily from diagnosis to 36 weeks 200 mg suppository or capsule, or 90 mg gel
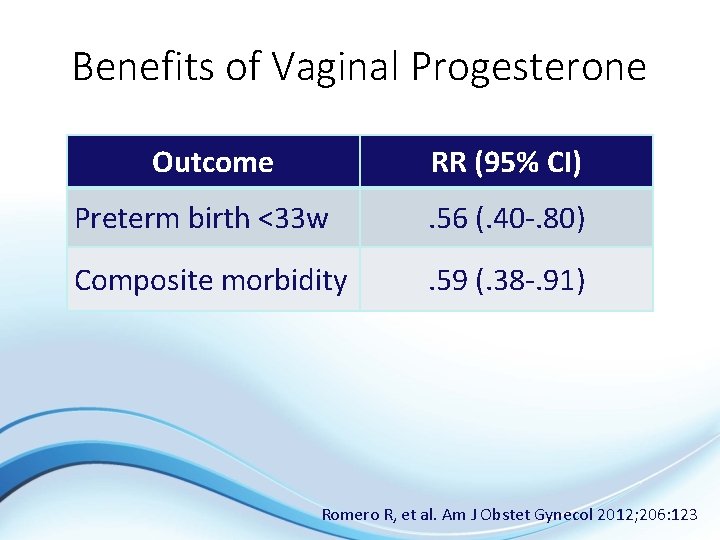
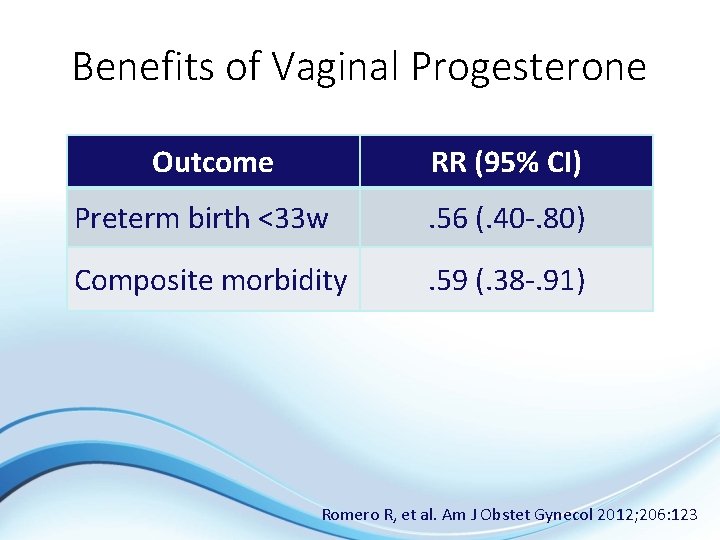
Benefits of Vaginal Progesterone Outcome RR (95% CI) Preterm birth <33 w . 56 (. 40 -. 80) Composite morbidity . 59 (. 38 -. 91) Romero R, et al. Am J Obstet Gynecol 2012; 206: 123

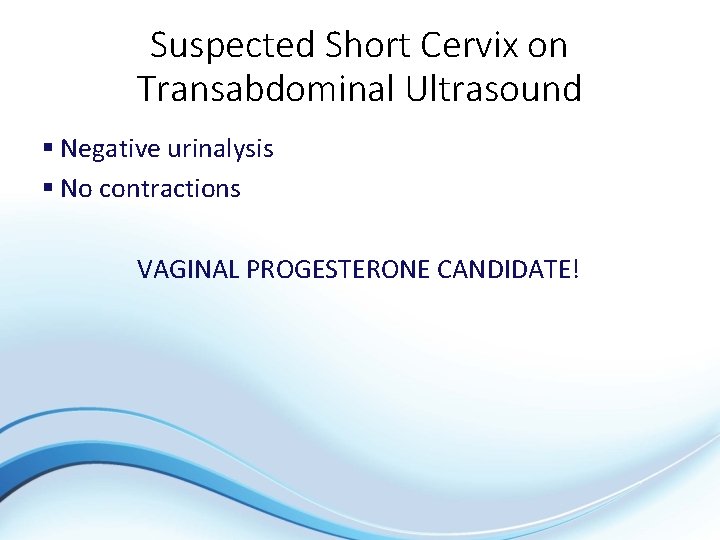
Suspected Short Cervix on Transabdominal Ultrasound § 34 year old G 1 P 0 at 22 -2/7 weeks § TVU CL 15 mm Cervical length 15 mm
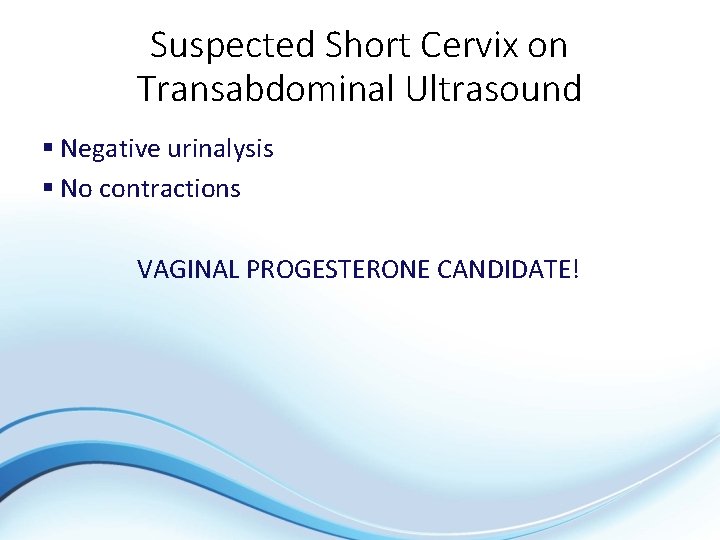
Suspected Short Cervix on Transabdominal Ultrasound § Negative urinalysis § No contractions VAGINAL PROGESTERONE CANDIDATE!
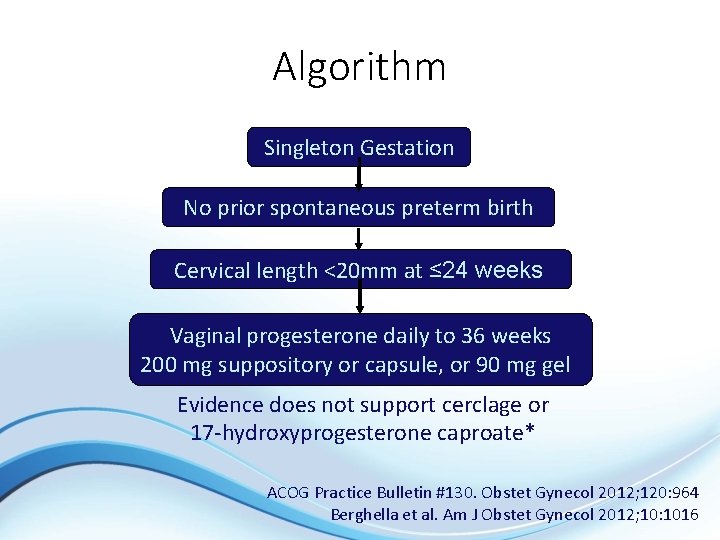
Algorithm Singleton Gestation No prior spontaneous preterm birth Cervical length <20 mm at ≤ 24 weeks Vaginal progesterone daily to 36 weeks 200 mg suppository or capsule, or 90 mg gel Evidence does not support cerclage or 17 -hydroxyprogesterone caproate* ACOG Practice Bulletin #130. Obstet Gynecol 2012; 120: 964 Berghella et al. Am J Obstet Gynecol 2012; 10: 1016

Prior Spontaneous Preterm Birth, Normal Transvaginal Cervical Length § Singleton, prior SPTB, unknown or normal (>25 mm) cervix ≤ 24 weeks § Is there an intervention to reduce prematurity risk? 17 -hydroxyprogesterone caproate (17 P) weekly 1636 weeks, 250 mg IM

Benefits of 17 P Delivery % RR (95% CI) NNT <37 w 36. 3 0. 66 (0. 54 -0. 81) 5 -6 <32 w 11. 4 0. 58 (0. 37 -0. 91) 12 Meis P et al. N Eng J Med 2003; 348: 2379

Prior Spontaneous Preterm Birth, Normal Transvaginal Cervical Length § Is there a role for cervical length surveillance? YES! § meta-analysis, 4 randomized trials § prior SPTB <37 w, cervix ≤ 25 mm Outcome Delivery <35 w Cerclage No Cerclage 23. 4% 39. 0% RR (95% CI) NNT 0. 61 (0. 40 -0. 92) 8 Berghella et al. Obstet Gynecol 2005; 106: 181
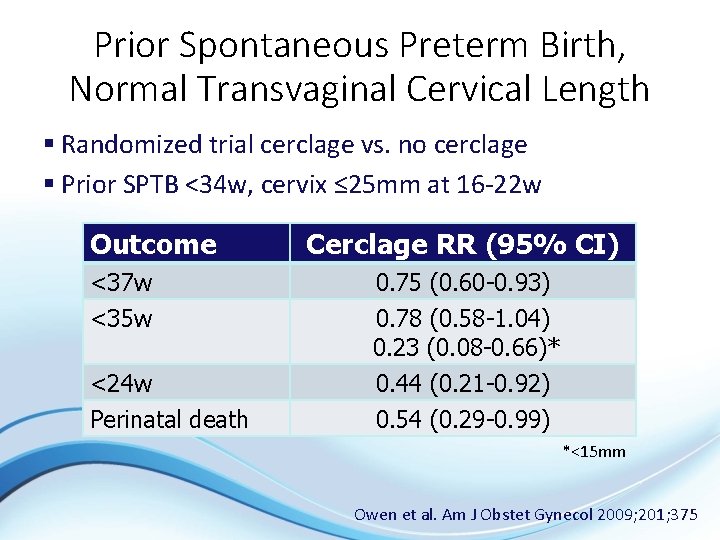
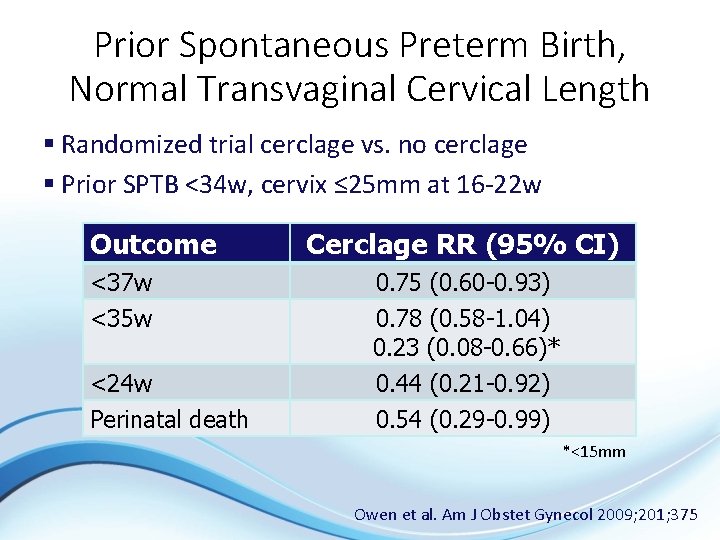
Prior Spontaneous Preterm Birth, Normal Transvaginal Cervical Length § Randomized trial cerclage vs. no cerclage § Prior SPTB <34 w, cervix ≤ 25 mm at 16 -22 w Outcome <37 w <35 w <24 w Perinatal death Cerclage RR (95% CI) 0. 75 (0. 60 -0. 93) 0. 78 (0. 58 -1. 04) 0. 23 (0. 08 -0. 66)* 0. 44 (0. 21 -0. 92) 0. 54 (0. 29 -0. 99) *<15 mm Owen et al. Am J Obstet Gynecol 2009; 201; 375
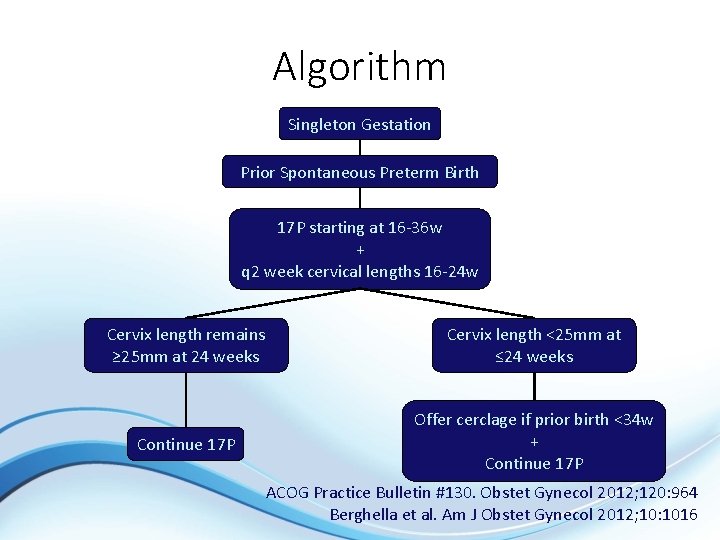
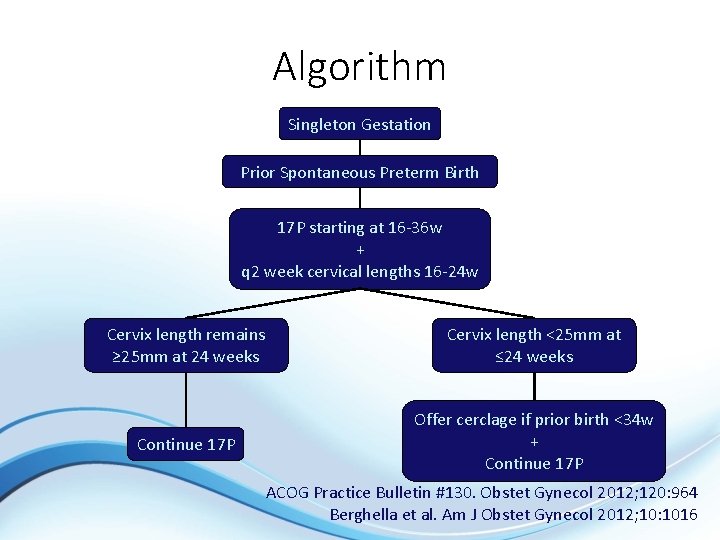
Algorithm Singleton Gestation Prior Spontaneous Preterm Birth 17 P starting at 16 -36 w + q 2 week cervical lengths 16 -24 w Cervix length remains ≥ 25 mm at 24 weeks Cervix length <25 mm at ≤ 24 weeks Continue 17 P Offer cerclage if prior birth <34 w + Continue 17 P ACOG Practice Bulletin #130. Obstet Gynecol 2012; 120: 964 Berghella et al. Am J Obstet Gynecol 2012; 10: 1016
Prior Spontaneous Preterm Birth with Prior Successful Cerclage § 26 -year old G 3 P 1102 at 11 5/7 weeks § Pregnancy #1 § short cervix § preterm labor at 26 weeks § delivery at 28 weeks § Pregnancy #2 § cerclage at 13 weeks § delivery at 40 weeks

Prior Spontaneous Preterm Birth with Prior Successful Cerclage § 17 P 16 -36 weeks § Every 2 week cervix lengths 16 -24 weeks, weekly for cervical length 25 -29 mm 24 week cervix length = 37 mm
Prior Spontaneous Preterm Birth with Prior Successful Cerclage § Spontaneous labor at 39 weeks § Delivered 9 lb 6 oz infant, Apgars 9/9
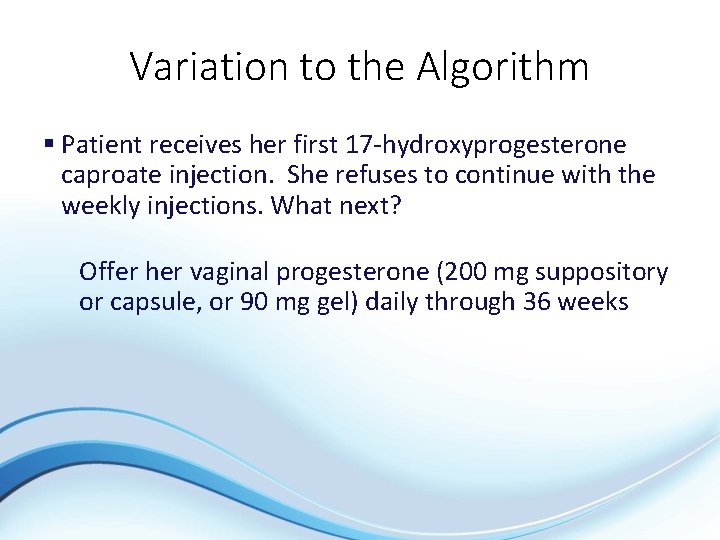
Variation to the Algorithm § Patient receives her first 17 -hydroxyprogesterone caproate injection. She refuses to continue with the weekly injections. What next? Offer her vaginal progesterone (200 mg suppository or capsule, or 90 mg gel) daily through 36 weeks
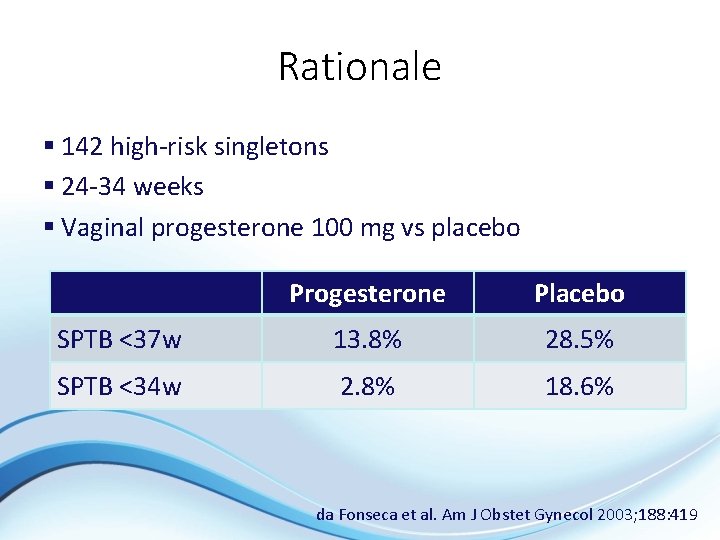
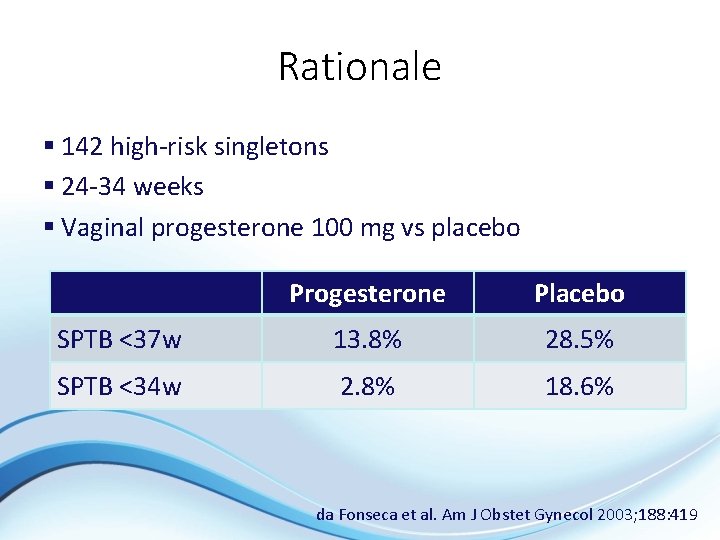
Rationale § 142 high-risk singletons § 24 -34 weeks § Vaginal progesterone 100 mg vs placebo Progesterone Placebo SPTB <37 w 13. 8% 28. 5% SPTB <34 w 2. 8% 18. 6% da Fonseca et al. Am J Obstet Gynecol 2003; 188: 419

Rationale § 502 subjects with prior 2 nd trimester spontaneous preterm birth or history of cerclage § Excluded: § Advanced dilation & effacement, cerclage in place § Short Cx < 25 mm or funneling at 14 -18 weeks § Randomized to 17 P vs. vaginal progesterone Outcome 17 -Progesterone Vaginal P SPTB <34 w SPTB 34 -37 w NICU 25. 7% 9. 3% 25. 7% 16. 6% 15. 4% Maher et al. Acta Obstet-Gynecol 2013; 92: 215
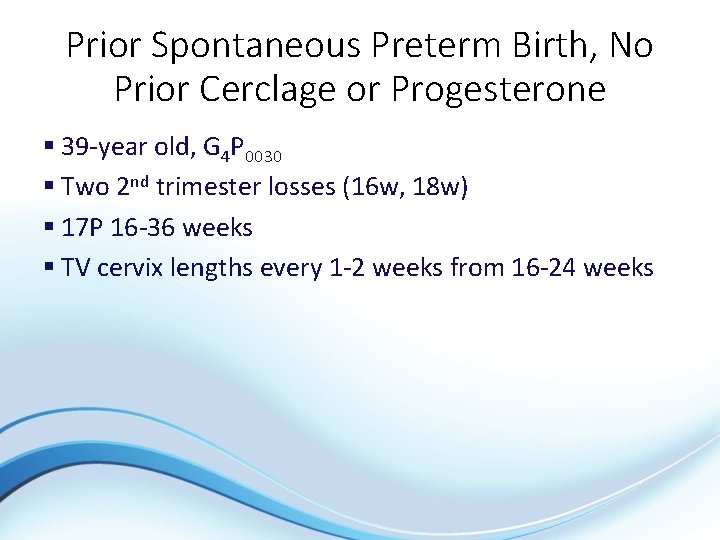
Prior Spontaneous Preterm Birth, No Prior Cerclage or Progesterone § 39 -year old, G 4 P 0030 § Two 2 nd trimester losses (16 w, 18 w) § 17 P 16 -36 weeks § TV cervix lengths every 1 -2 weeks from 16 -24 weeks

Prior Spontaneous Preterm Birth, No Prior Cerclage or Progesterone 16 18 19 weeks 32 mm cervix==27 mm 8 mm
Prior Spontaneous Preterm Birth, No Prior Cerclage or Progesterone § Patient continued 17 P and cerclage placed § Emergency cesarean at 34 weeks – abruption
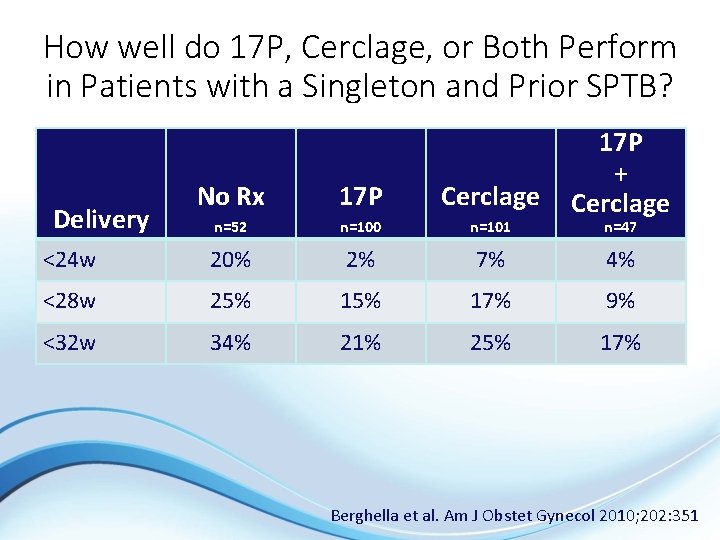
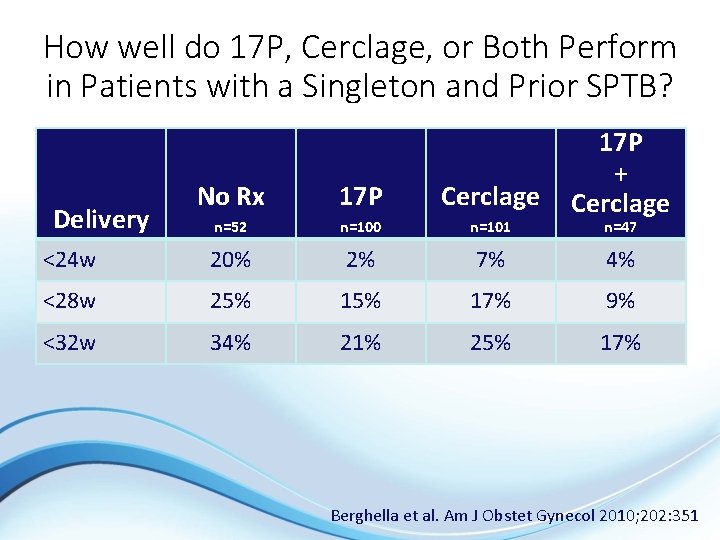
How well do 17 P, Cerclage, or Both Perform in Patients with a Singleton and Prior SPTB? 17 P + Cerclage No Rx 17 P Cerclage n=52 n=100 n=101 <24 w 20% 2% 7% 4% <28 w 25% 17% 9% <32 w 34% 21% 25% 17% Delivery n=47 Berghella et al. Am J Obstet Gynecol 2010; 202: 351
Prior Spontaneous Preterm Birth with History-Indicated Cerclage § 30 -year old, G 3 P 0111 § 1 st pregnancy was an 19 week loss consistent with cervical insufficiency § 2 nd pregnancy was a 34 week delivery secondary to spontaneous preterm birth with a history-indicated cerclage placed at 12 weeks § She’s now in her 3 rd pregnancy and already had her history-indicated cerclage at 12 weeks
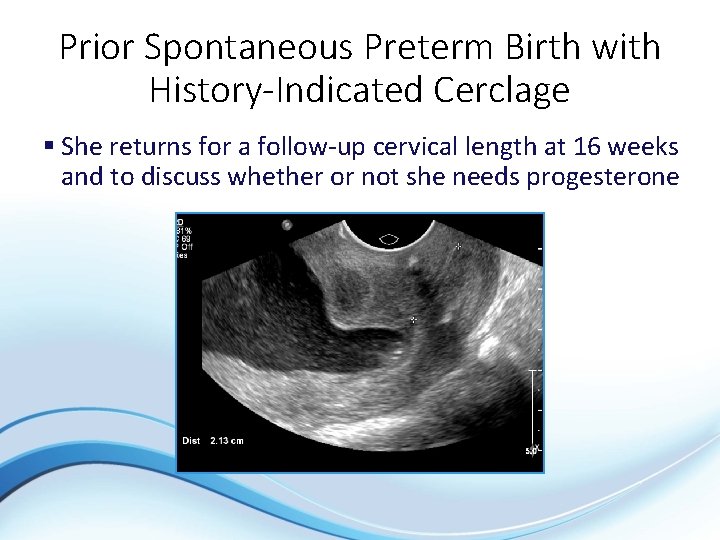
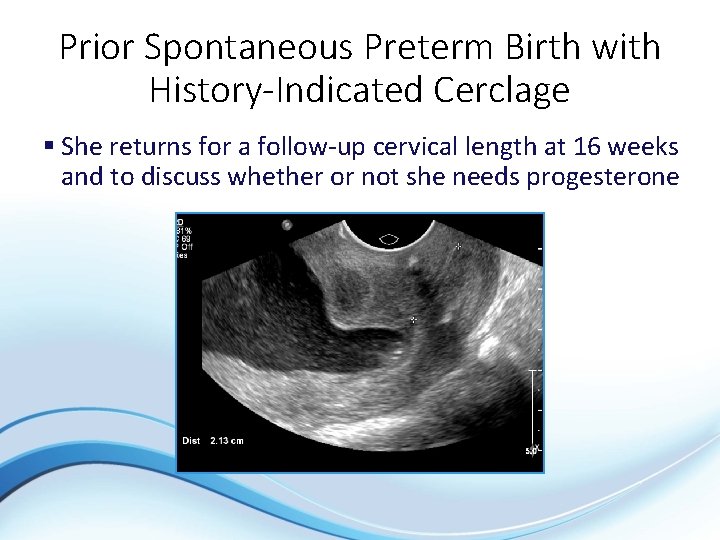
Prior Spontaneous Preterm Birth with History-Indicated Cerclage § She returns for a follow-up cervical length at 16 weeks and to discuss whether or not she needs progesterone

Prior Spontaneous Preterm Birth with History-Indicated Cerclage § Management questions: § Should she be initiated on progesterone? YES! § She qualifies based on her history and has a shortening cervix § If so, which route? Either IM or vaginal progesterone (but not both!) is acceptable § Should she continue to have cervical lengths? Individualize serial cervical length monitoring based on patient and clinical circumstances § Digital and speculum exams should be considered
What About Obesity and Progesterone? § Retrospective Cohort Study of 390 women with prior SPTB on 17 P § 216 women with BMI >25 § 174 women with BMI <25 § Increased risk for SPTB <32 weeks with BMI >25 § No differences in SPTB <35 weeks or <37 weeks § Success rate of 17 P at standard dosing may be impacted by BMI. Co AL et al. Am J Obstet Gynecol 2015
What About Obesity and Progesterone? § Secondary analysis of the MFMU 17 P (Meis) trial § No benefit for 17 P prevention of SPTB was noted with BMI >30 or maternal weight>165 lbs § Preterm Birth prevention by 17 P use may be ineffective in those with BMI >30 Heyborne KD et al. Am J Obstet Gynecol 2015

Do 17 P Plasma Levels Matter? § Secondary analysis of 315 patients § Increased risk of SPTB among subjects whose 17 P levels were in the lowest quartile § Did not evaluate by BMI § Need additional studies Caritis et al. Am J Obstet Gynecol 2014; 210: 128
Summary § Obesity may decrease success rate of 17 P for SPTB prevention § Low plasma levels of 17 P may increase risk of SPTB § Further research in these areas are needed § There is NO current recommendation at this time to alter the dose in the obese patient or to evaluate plasma levels
Twins, Normal Cervix Regardless of Prior Spontaneous Preterm Birth “No evidence of benefit to 17 P or vaginal progesterone”
Twins, No Prior Spontaneous Preterm Birth, Short Cervix § Vaginal progesterone may reduce neonatal composite morbidity, but small numbers RR 0. 52 (0. 29 -0. 93) Romero § “insufficient evidence to assess effect of progesterone” SMFM Publications § “available data regarding the efficacy of cerclage placement, progesterone supplementation, or both…do not support their use. ” ACOG Practice Bulletin Romero et al. Am J Obstet Gynecol 2012; 206: 123 Berghella et al. Am J Obstet Gynecol 2012; 10: 1016 ACOG Practice Bulletin #130. Obstet Gynecol 2012; 120: 964

Twins with Short Cervix § 17 P not efficacious § Avoid cerclage § meta analysis suggests increased adverse outcomes Outcome RR (95% CI) Delivery <35 w 2. 15 (1. 15 -4. 01) Perinatal mortality 2. 66 (0. 83 -8. 54) Berghella et al. Obstet Gynecol 2005; 106: 181
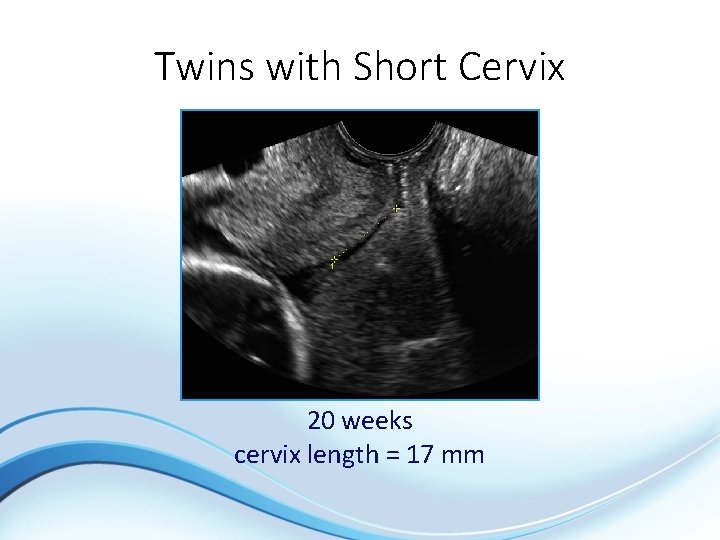
Twins with Short Cervix § 45 -year old, G 7 P 1051 § five 1 st trimester miscarriages § term cesarean § IVF dichorionic twins
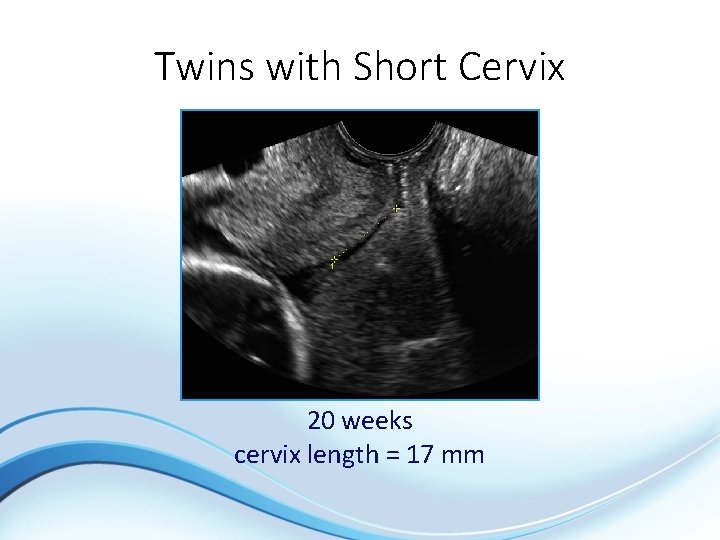
Twins with Short Cervix 20 weeks cervix length = 17 mm
Twins with Short Cervix § No contractions § Negative urinalysis § Expectant care § Outcome § spontaneous labor at 36 weeks
Preterm Labor: Importance of Early Diagnosis § Transfer to facility with NICU § Glucocorticoid administration § Group B streptococcal (GBS) prophylaxis § Tocolytic therapy
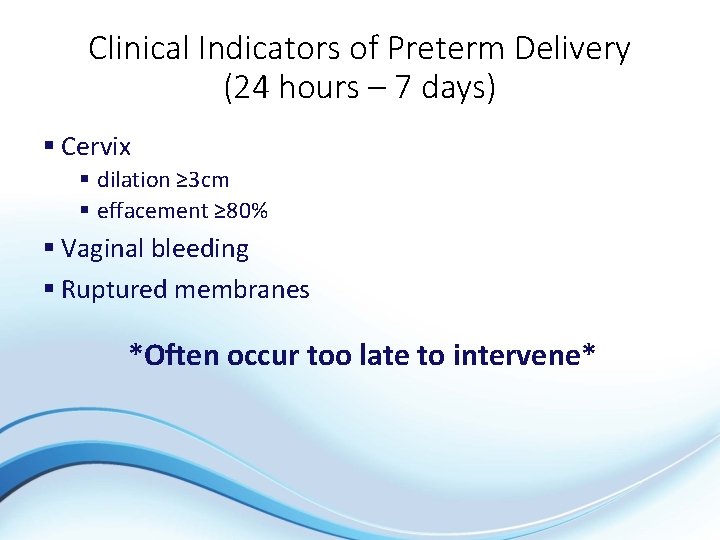
Clinical Indicators of Preterm Delivery (24 hours – 7 days) § Cervix § dilation ≥ 3 cm § effacement ≥ 80% § Vaginal bleeding § Ruptured membranes *Often occur too late to intervene*

Evaluation of the Symptomatic Patient § Two Goals: 1. Identify patient not likely to deliver preterm and avoid unnecessary intervention 2. Identify patient likely to deliver preterm, allowing time for effective interventions

Assessment of Symptomatic Patient. Speculum Exam § Obtain vaginal swab for fetal fibronectin (FFN) § Evaluate for presence of amniotic fluid § Obtain culture for GBS

Fetal Fibronectin (FFN) § Glycoprotein acts as a “glue” for membrane adherence § Presence in cervicovaginal fluid 20 -36 weeks associated with increased risk of SPTB § Absence of FFN associated with reduced risk of SPTB in next 714 d SPTB Detection (%) Singletons Symptomatic Asymptomatic Twins 76. 1 17 -19 71 PPV (%) NPV (%) 25. 9 13 -24 97. 6 97 97 Sanchez-Ramos L et al Obstet Gynecol 2009; 114: 631 Singer E et al Obstet Gynecol 2007; 109: 1083
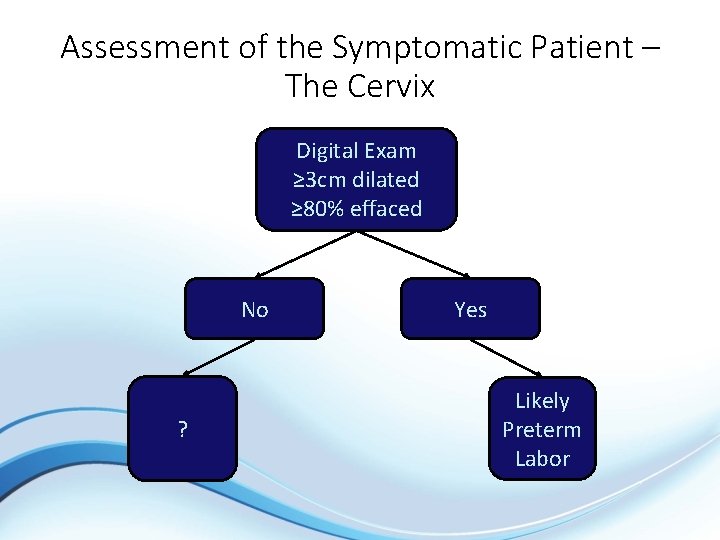
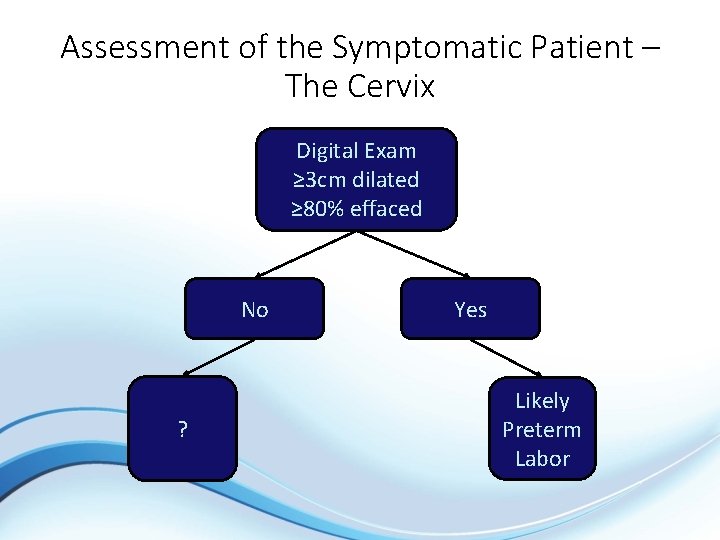
Assessment of the Symptomatic Patient – The Cervix Digital Exam ≥ 3 cm dilated ≥ 80% effaced No ? Yes Likely Preterm Labor
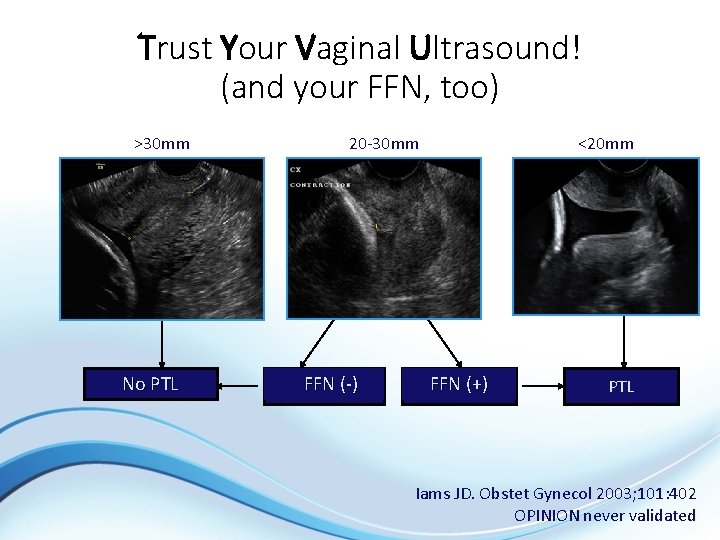
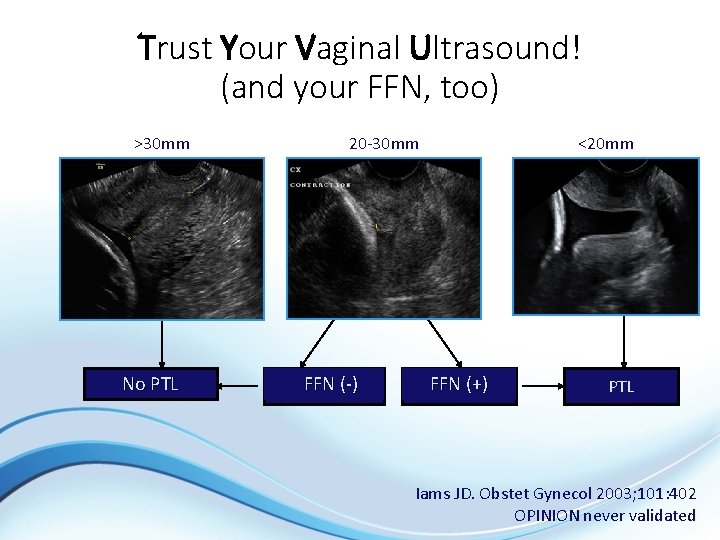
Trust Your Vaginal Ultrasound! (and your FFN, too) >30 mm No PTL 20 -30 mm FFN (-) <20 mm FFN (+) PTL Iams JD. Obstet Gynecol 2003; 101: 402 OPINION never validated
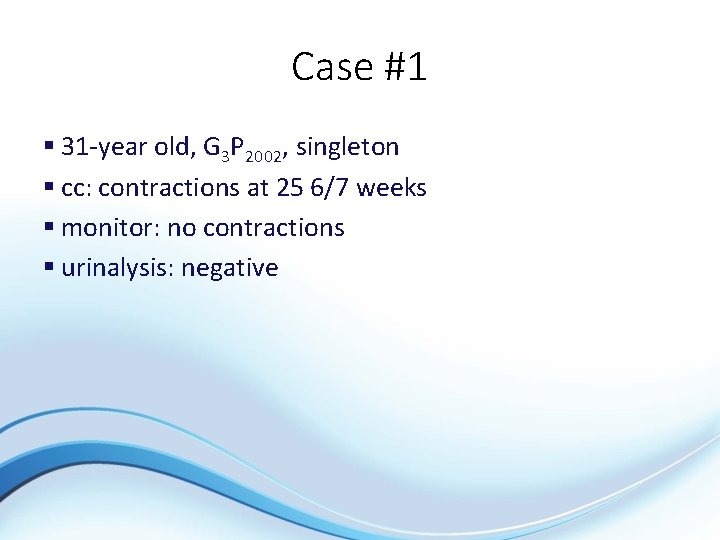
Case #1 § 31 -year old, G 3 P 2002, singleton § cc: contractions at 25 6/7 weeks § monitor: no contractions § urinalysis: negative
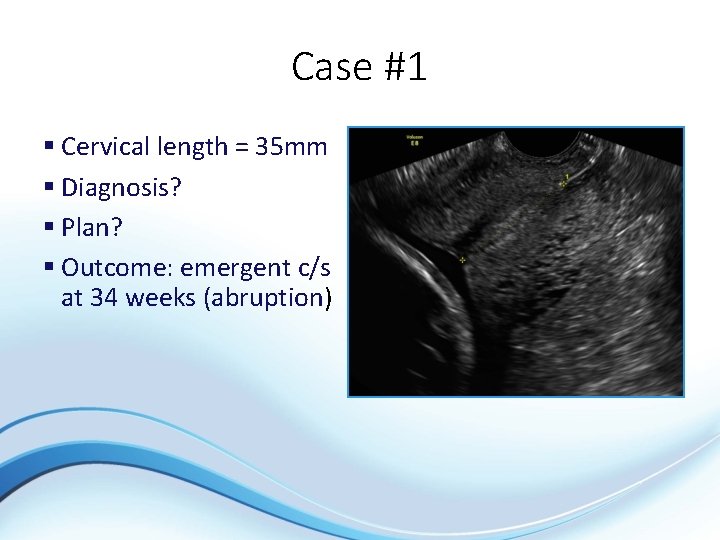
Case #1 § Cervical length = 35 mm § Diagnosis? § Plan? § Outcome: emergent c/s at 34 weeks (abruption)
Case #2 § 33 -year old, G 4 P 2012, singleton § cc: contractions at 28 3/7 weeks § monitor: contractions every 1 -3” § urinalysis: negative
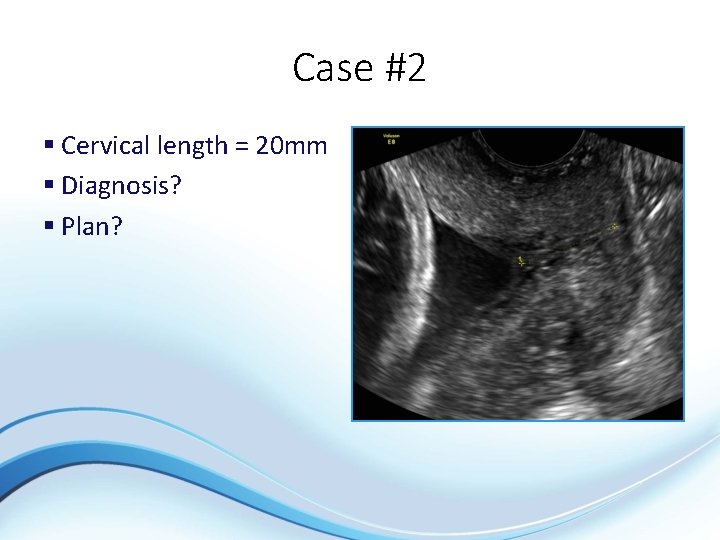
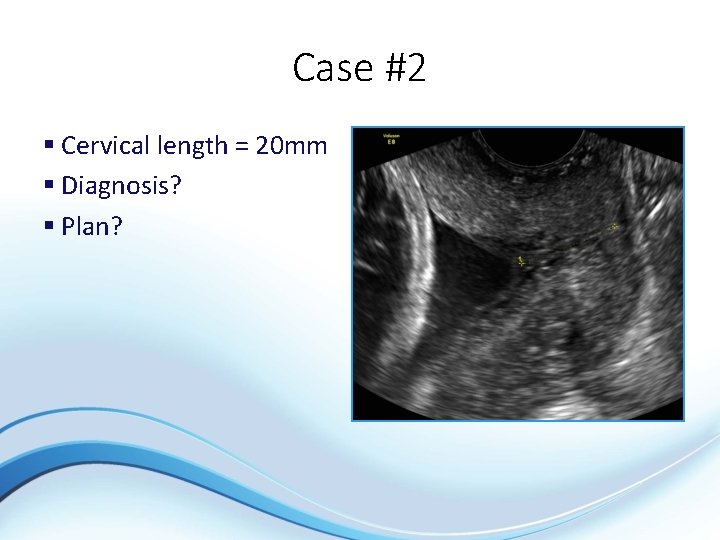
Case #2 § Cervical length = 20 mm § Diagnosis? § Plan?
Case #2 § FFN = negative § Outcome: repeat c/s in labor at 37 weeks
Case #3 § 27 -year old G 1 P 0, singleton § cc: contractions at 30 6/7 weeks § monitor: q 3” contractions § urinalysis: negative § cervix: 1 cm/70% effaced

Case #3 § Cervical length = 16 mm § Diagnosis? § Plan?
Case #3 § Treatment § steroids § tocolytic § Antibiotic § Outcome § recurrent PTL § delivery at 31 2/7 weeks
Case #4 § 31 -year old G 1 P 0, dichorionic twins 30 weeks § cc: contractions q 3” § monitor: q 3” contractions § urinalysis: negative § cervix: 1 -2 cm/50% effaced

Case #4 § Cervical length = 27 mm § Diagnosis? § Plan?
Case #4 § FFN negative § Every 2 week cervix length (stable) and FFN (-) to 34 weeks § Spontaneous labor at 36 weeks

Case #5 § 26 -year old G 2 P 0010, dichorionic twins 28 weeks § cc: q 4” contractions § monitor: q 4” contractions § urinalysis: negative § cervix: 2 cm/80% effaced

Case #5 § Cervix length = no measurable cervix, sludge present § Diagnosis? § Plan?
Case #5 § Tocolysis § Steroids § Antibiotics § Progressive labor § Cesarean delivery
Summary – Singletons § No prior SPTB § cervical length screening optional, but not mandatory § One measurement between 16 -24 weeks § treat short cervix with vaginal progesterone
Summary – Singletons § Prior SPTB § treat with 17 P 16 -36 weeks § Vaginal progesterone is a reasonable substitution § serial cervix lengths 16 -24 weeks § for short cervix § offer cerclage, continue 17 P or vaginal progesterone § vaginal progesterone without cerclage or 17 P

Summary – Twins § No current role for 17 P or cerclage § No prior SPTB, short cervix § expectant care
Summary – Threatened PTL § Cervical length with FFN effectively triages women with threatened PTL and an equivocal digital exam
