Cervical Cancer Xin LU OBGYN Hospital Fudan University
Cervical Cancer Xin LU OB/GYN Hospital Fudan University
Contents General information u CINs u Spread pattern u FIGO staging u Clinical signs u Diagnosis and differential diagnosis u Principle for treatment u Prevention u Surveillance u
Key words n n n n Cervical cancer (Cxca) Human Papillomavirus (HPV) Radical Hysterectomy (RH) Radiotherapy (RT) Chemotherapy (CT) Neoadjuvant chemotherapy (NACT) Concurrent chemo-radiotherapy (CCCR) Radical Trachelectomy
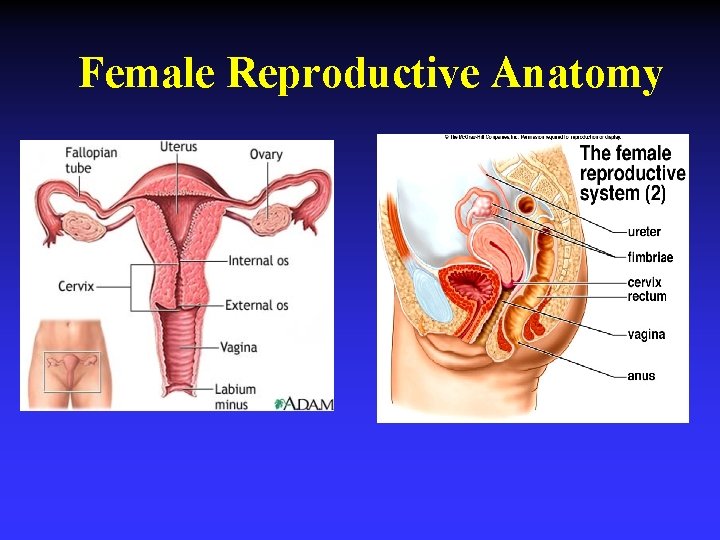
Female Reproductive Anatomy
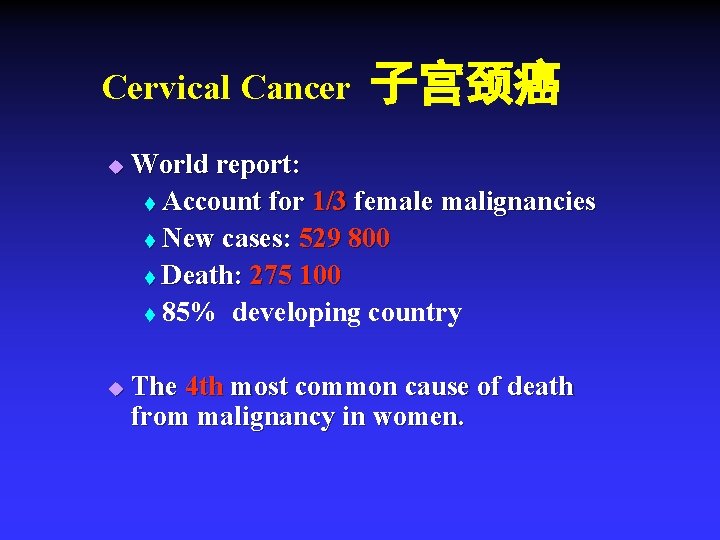
Cervical Cancer u u 子宫颈癌 World report: t Account for 1/3 female malignancies t New cases: 529 800 t Death: 275 100 t 85% developing country The 4 th most common cause of death from malignancy in women.
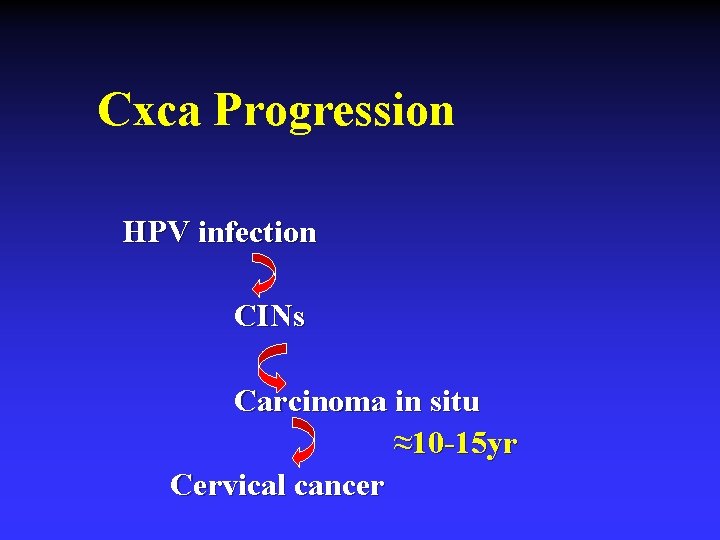
Cxca Progression HPV infection CINs Carcinoma in situ ≈10 -15 yr Cervical cancer
Etiology High-risk factors HR-HPV u Use of oral contraceptives u Smoking u Multiple sexual partners u History of herpes infection u History of STD u
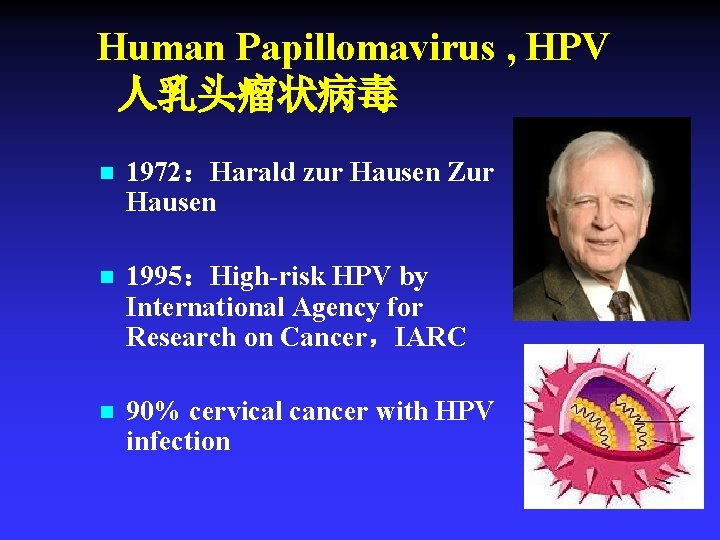
Human Papillomavirus , HPV 人乳头瘤状病毒 n 1972:Harald zur Hausen Zur Hausen n 1995:High-risk HPV by International Agency for Research on Cancer,IARC n 90% cervical cancer with HPV infection
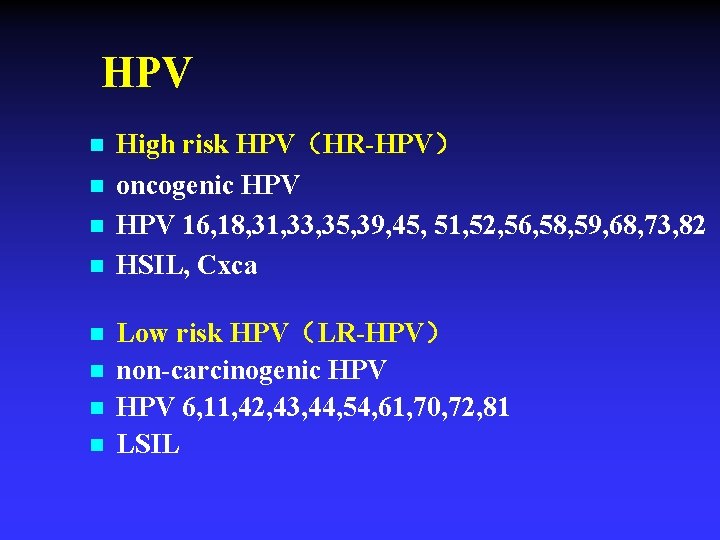
HPV n n n n High risk HPV(HR-HPV) oncogenic HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82 HSIL, Cxca Low risk HPV(LR-HPV) non-carcinogenic HPV 6, 11, 42, 43, 44, 54, 61, 70, 72, 81 LSIL
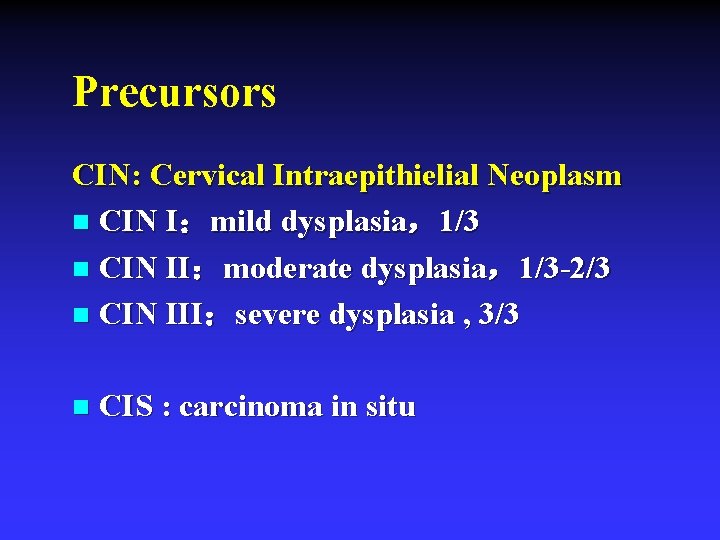
Precursors CIN: Cervical Intraepithielial Neoplasm n CIN I:mild dysplasia,1/3 n CIN II:moderate dysplasia,1/3 -2/3 n CIN III:severe dysplasia , 3/3 n CIS : carcinoma in situ
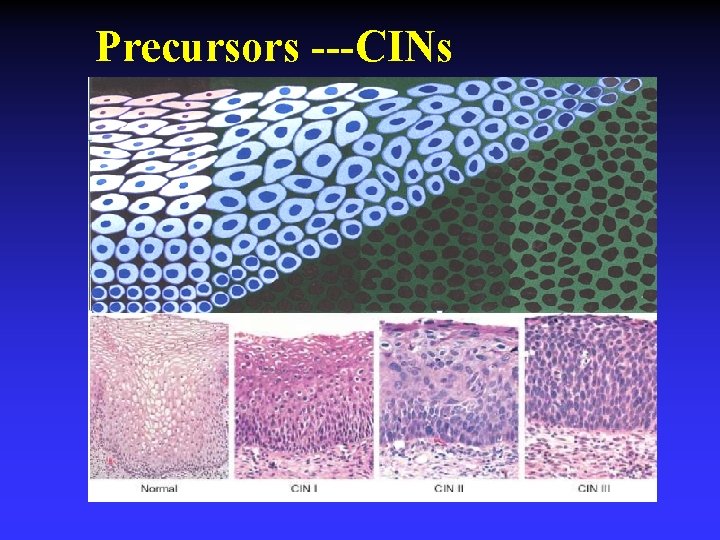
Precursors ---CINs
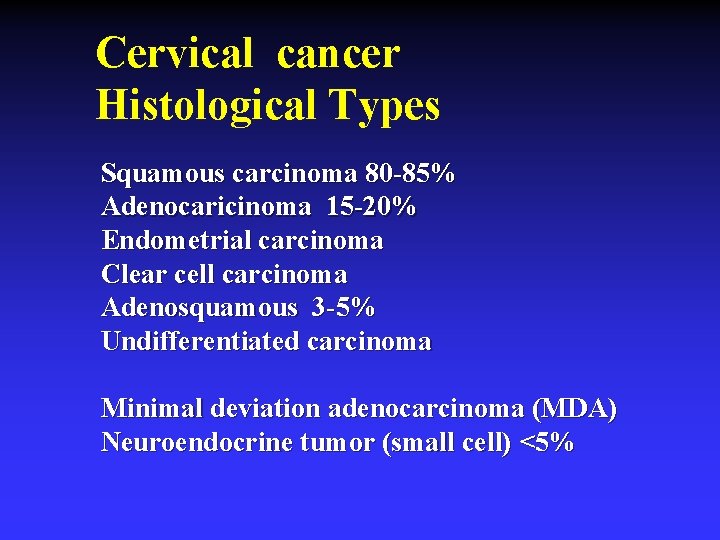
Cervical cancer Histological Types Squamous carcinoma 80 -85% Adenocaricinoma 15 -20% Endometrial carcinoma Clear cell carcinoma Adenosquamous 3 -5% Undifferentiated carcinoma Minimal deviation adenocarcinoma (MDA) Neuroendocrine tumor (small cell) <5%
Spread pattern n Transcelomic u most common n Lymphatic u retroperitoneal ( pelvic and paraaortic ) LN spreading is common in advanced- stage n Hematogenous u uncommon
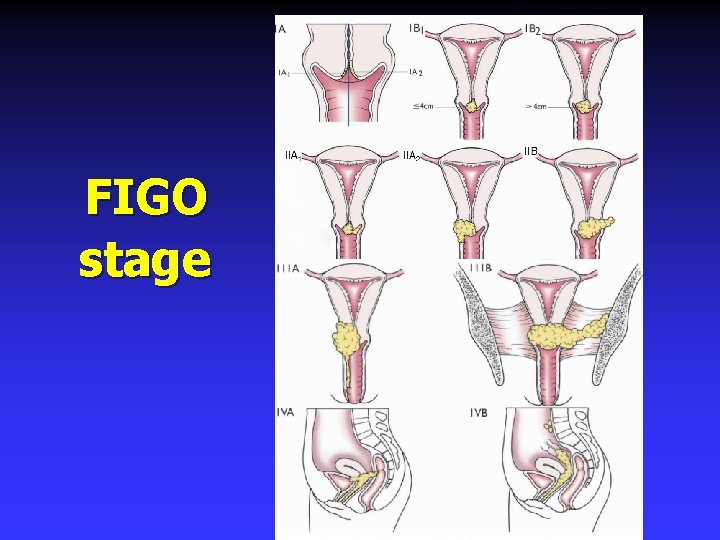
FIGO stage

FIGO Staging I The carcinoma is strictly confined to the cervix (extension to the uterine corpus should be disregarded). IA Invasive cancer identified only microscopically. Invasion is limited to measured stromal invasion with a maximum depth of 5 mmb and no wider than 7 mm. (All gross lesions even with superficial invasion are Stage IB cancers. ) IA 1: Measured invasion of stroma ≤ 3 mm in depth and ≤ 7 mm width. IA 2 : Measured invasion of stroma >3 mm and <5 mm in depth and ≤ 7 mm width. IB Clinical lesions confined to the cervix, or preclinical lesions greater than stage IA. IB 1: Clinical lesions no greater than 4 cm in size. IB 2: Clinical lesions >4 cm in size. II The carcinoma extends beyond the uterus, but has not extended onto the pelvic wall or to the lower third of vagina. IIA Involvement of up to the upper 2/3 of the vagina. No obvious parametrial involvement. IIA 1: Clinically visible lesion ≤ 4 cm IIA 2: Clinically visible lesion >4 cm IIB Obvious parametrial involvement but not onto the pelvic sidewall. III The carcinoma has extended onto the pelvic sidewall. On rectal examination, there is no cancer-free space between the tumor and pelvic sidewall. The tumor involves the lower third of the vagina. All cases of hydronephrosis or non-functioning kidney should be included unless they are known to be due to other causes. IIIA Involvement of the lower vagina but no extension onto pelvic sidewall. IIIB Extension onto the pelvic sidewall, or hydronephrosis/non-functioning kidney. IV The carcinoma has extended beyond the true pelvis or has clinically involved the mucosa of the bladder and/or rectum. IVA Spread to adjacent pelvic organs. IVB Spread to distant organs.
Platform of diagnosis for cervical diseases v Pap smear v TCT v HPV v Colposcopy--biopsy v LEEP TBS classification
Cervical cancer Symptoms No symptoms n Abnormal pap smear n Leukorrhea n Postcoital bleeding n Pelvic pain n
Cervical cancer Diagnosis History u Physical examination u Cytology (pap smear, TCT) u Biopsy (colposcopy) u Conization u Imaging u
Principle for treat cervical cancer n Evidence based medicine u FIGO ( International Federation of Gynecology and Obstetrics) u n NCCN (National Comprehensive Cancer Network) Individualized therapy;
Cervical Cancer Treatment Precursor- CINs n Micro-invasive cancer n Invasive cancer n
Treatment for CINs CIN I: follow up 3— 6 months n CIN II: u local therapy u conization n CIN III: u conization u hysterectomy n
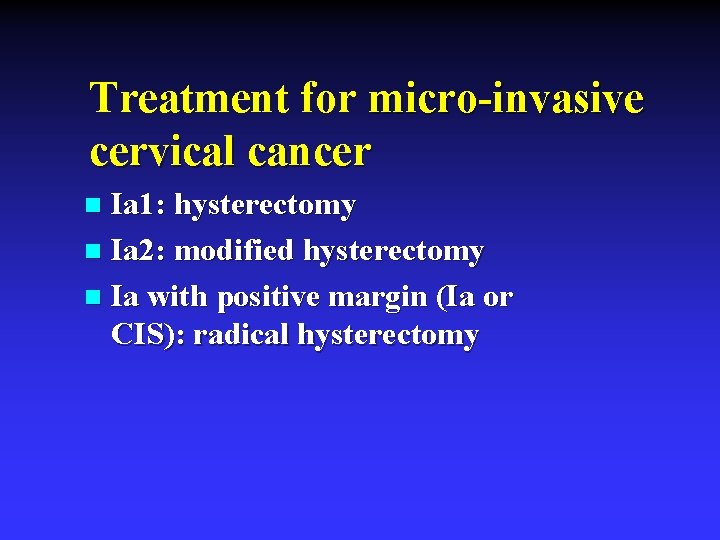
Treatment for micro-invasive cervical cancer Ia 1: hysterectomy n Ia 2: modified hysterectomy n Ia with positive margin (Ia or CIS): radical hysterectomy n

Treatment for invasive cervical cancer Surgical threatment Ib-IIa n Radiotherapy n Chemotherapy n Combined therapy n
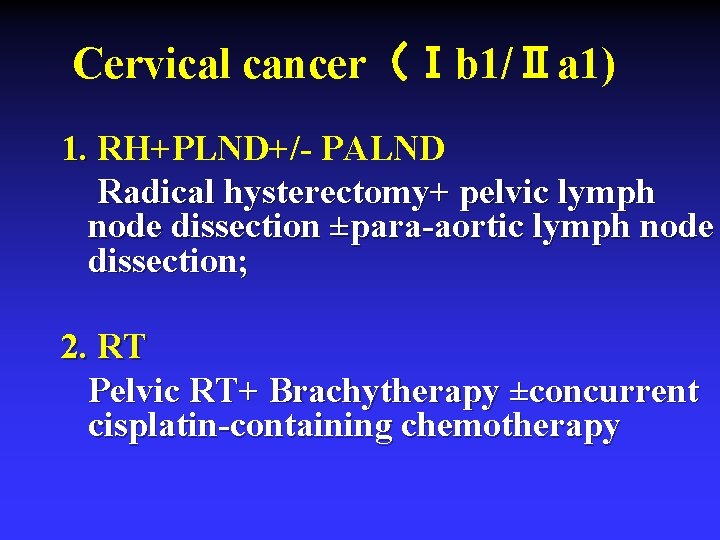
Cervical cancer(Ⅰb 1/Ⅱa 1) 1. RH+PLND+/- PALND Radical hysterectomy+ pelvic lymph node dissection ±para-aortic lymph node dissection; 2. RT Pelvic RT+ Brachytherapy ±concurrent cisplatin-containing chemotherapy
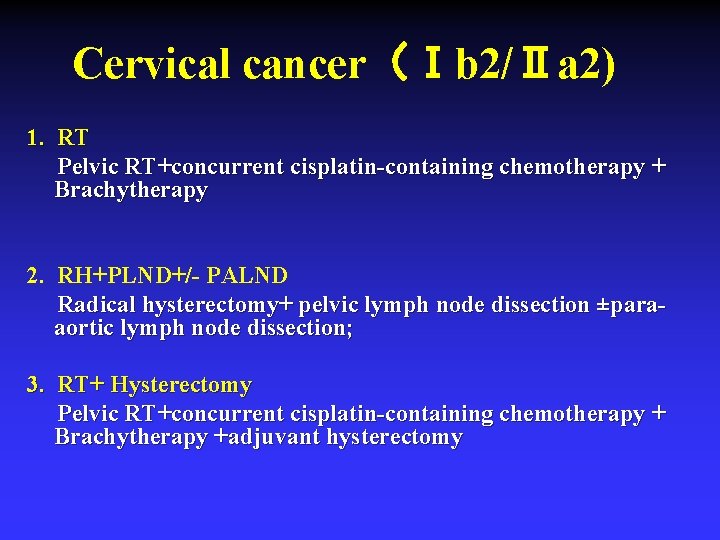
Cervical cancer(Ⅰb 2/Ⅱa 2) 1. RT Pelvic RT+concurrent cisplatin-containing chemotherapy + Brachytherapy 2. RH+PLND+/- PALND Radical hysterectomy+ pelvic lymph node dissection ±paraaortic lymph node dissection; 3. RT+ Hysterectomy Pelvic RT+concurrent cisplatin-containing chemotherapy + Brachytherapy +adjuvant hysterectomy
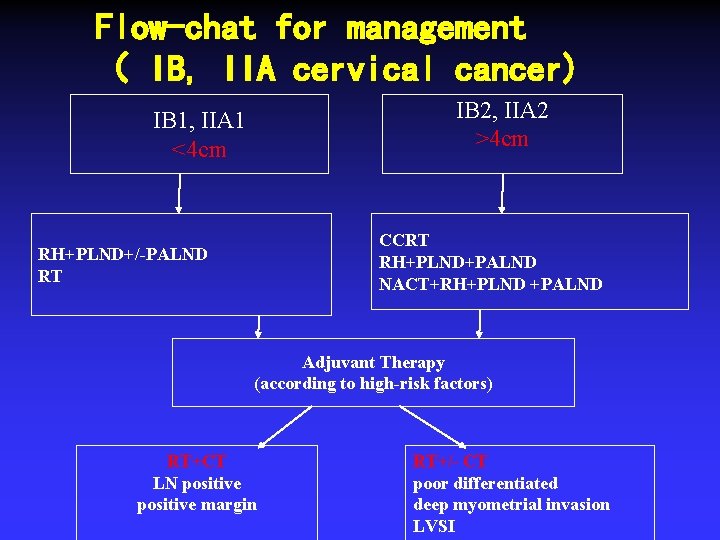
Flow-chat for management ( IB, IIA cervical cancer) IB 2, IIA 2 >4 cm IB 1, IIA 1 <4 cm CCRT RH+PLND+PALND NACT+RH+PLND +PALND RH+PLND+/-PALND RT Adjuvant Therapy (according to high-risk factors) RT+CT LN positive margin RT+/- CT poor differentiated deep myometrial invasion LVSI
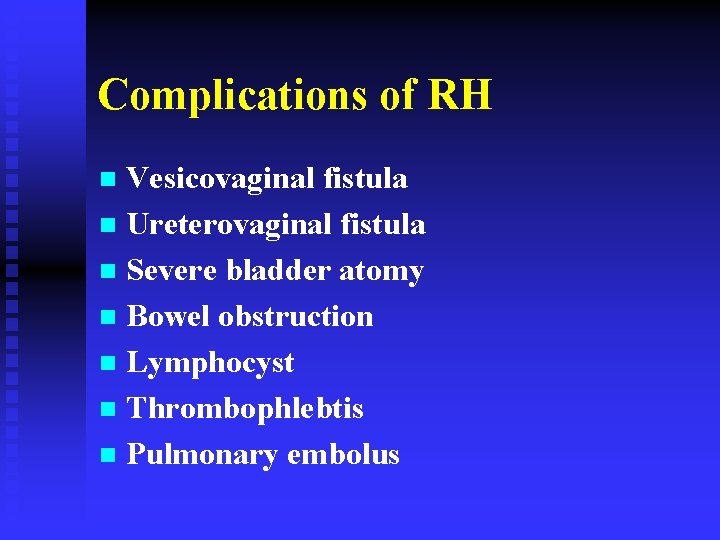
Complications of RH Vesicovaginal fistula n Ureterovaginal fistula n Severe bladder atomy n Bowel obstruction n Lymphocyst n Thrombophlebtis n Pulmonary embolus n
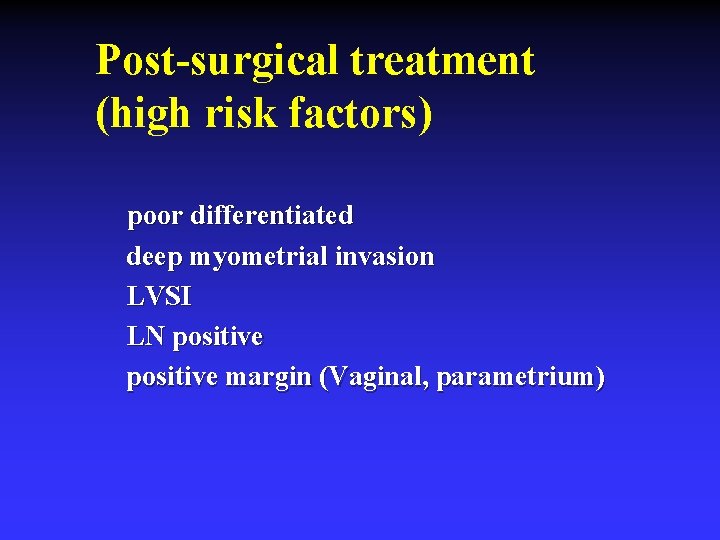
Post-surgical treatment (high risk factors) poor differentiated deep myometrial invasion LVSI LN positive margin (Vaginal, parametrium)
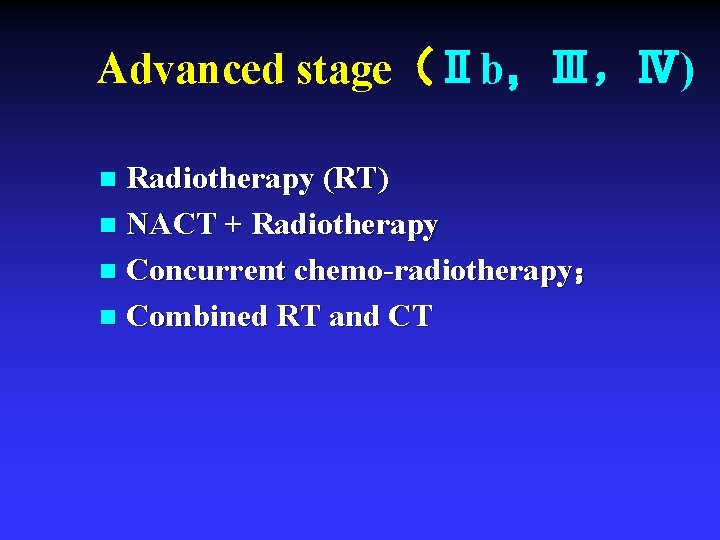
Advanced stage(Ⅱb,Ⅲ,Ⅳ) Radiotherapy (RT) n NACT + Radiotherapy n Concurrent chemo-radiotherapy; n Combined RT and CT n
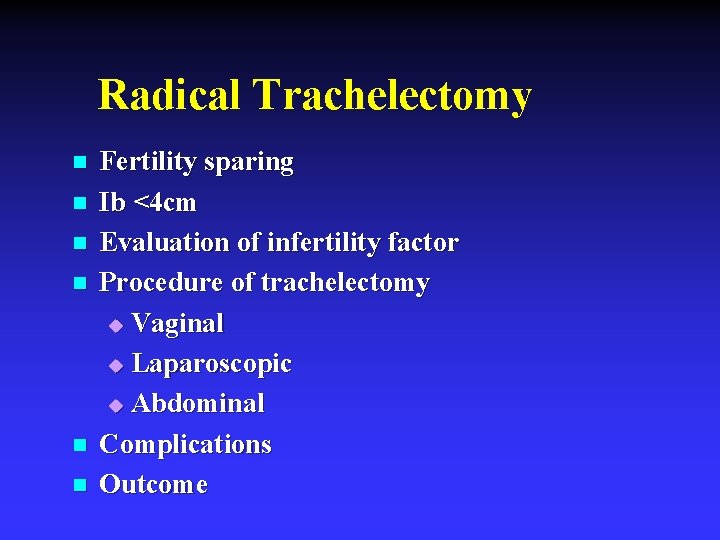
Radical Trachelectomy n n n Fertility sparing Ib <4 cm Evaluation of infertility factor Procedure of trachelectomy u Vaginal u Laparoscopic u Abdominal Complications Outcome
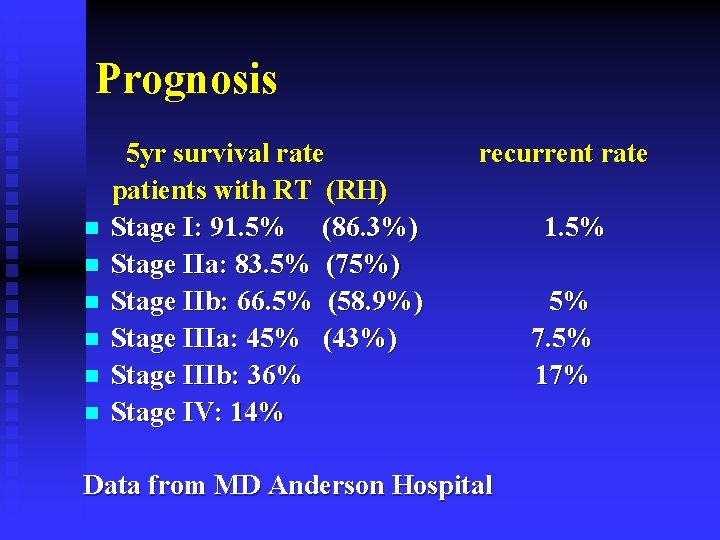
Prognosis n n n 5 yr survival rate patients with RT (RH) Stage I: 91. 5% (86. 3%) Stage IIa: 83. 5% (75%) Stage IIb: 66. 5% (58. 9%) Stage IIIa: 45% (43%) Stage IIIb: 36% Stage IV: 14% recurrent rate Data from MD Anderson Hospital 1. 5% 5% 7. 5% 17%
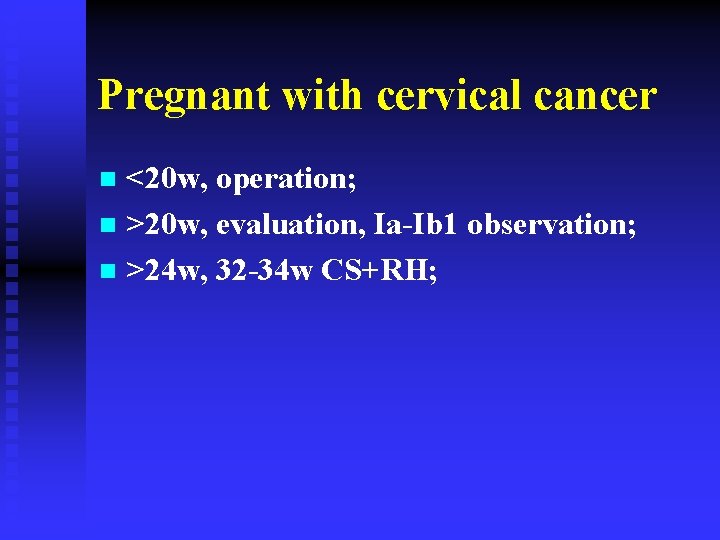
Pregnant with cervical cancer <20 w, operation; n >20 w, evaluation, Ia-Ib 1 observation; n >24 w, 32 -34 w CS+RH; n
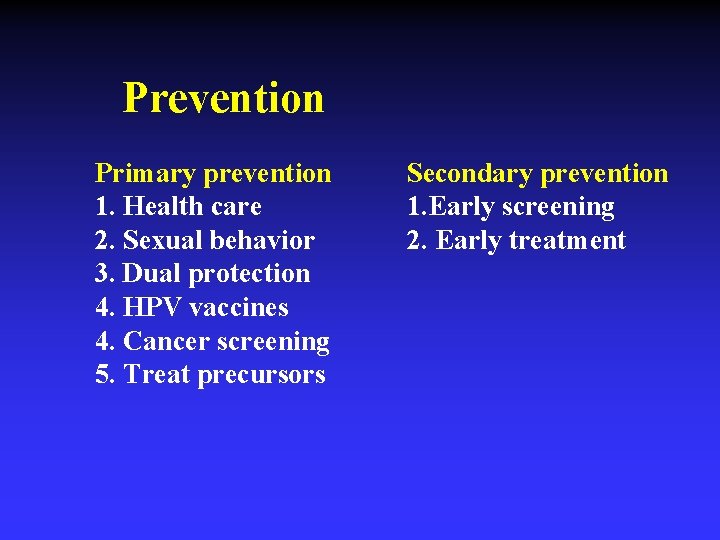
Prevention Primary prevention 1. Health care 2. Sexual behavior 3. Dual protection 4. HPV vaccines 4. Cancer screening 5. Treat precursors Secondary prevention 1. Early screening 2. Early treatment
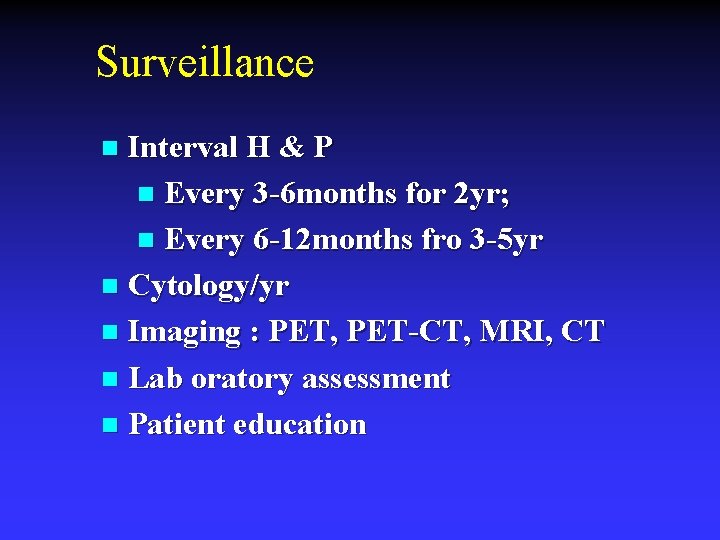
Surveillance Interval H & P n Every 3 -6 months for 2 yr; n Every 6 -12 months fro 3 -5 yr n Cytology/yr n Imaging : PET, PET-CT, MRI, CT n Lab oratory assessment n Patient education n
Take home message n n n n HPV (HR) CINs FIGO stage Surgery: Radical hysterectomy and PLND Post-operation treatment: high risk factors RT and CT Fertility sparing trachelectomy HPV Vaccine

THANKS OB/GYN Hospital of Fudan University
- Slides: 36