Cervical Cancer Screening District I ACOG Medical Student
- Slides: 11
Cervical Cancer Screening District I ACOG Medical Student Education Module Last Updated: January 1, 2011
Cervical Cancer Screening Module Outline Ø Brief review of Cervical Cancer Ø Brief review of HPV Ø What is a Pap Smear? How To Perform? Ø Some Pap Terminology Ø Who to screen and when Ø Abnormal Pap What now?
Cervical Cancer Incidence/Prevalence Ø 3 rd most common GYN cancer in developed world l l Ø 11, 270 new cases in 2009 4, 070 deaths in 2009 Most common GYN cancer in developing countries l l 500, 000 new cases annually 240, 000 deaths annually Signs & Symptoms; Ø Abnormal Vaginal Bleeding Ø Postcoital Bleeding Ø Vaginal Discharge (watery, mucoid, purulent, malodorous)
Cervical Cancer Risk Factors; Ø Early onset of sexual activity Ø Multiple sexual partners Ø High-risk sexual partner Ø History of sexually transmitted diseases Ø Smoking (not adenocarcinoma) Ø High parity Ø Immunosuppression Ø Low socioeconomic status Ø Prolonged use of oral contraceptives Ø Hx of vaginal or vulvar cancer Vast majority of cases are caused by persistent high risk HPV infection Most common Histologies l l l Squamous Cell Carcinoma Adenocarcinoma Adenosquamous
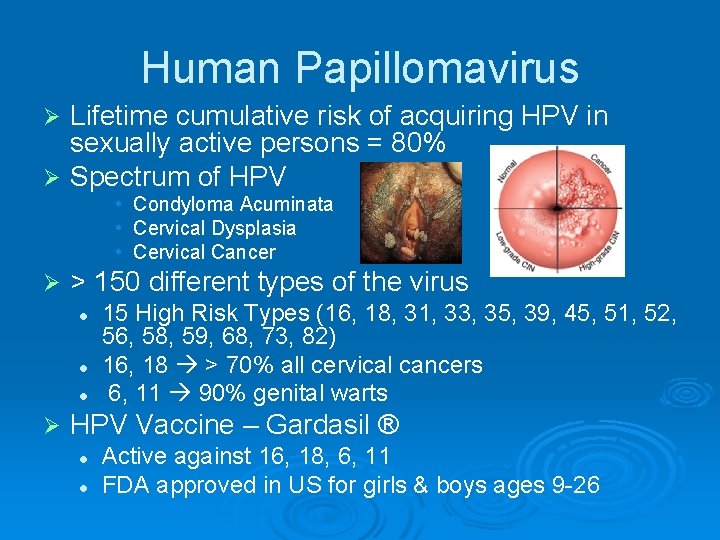
Human Papillomavirus Lifetime cumulative risk of acquiring HPV in sexually active persons = 80% Ø Spectrum of HPV Ø • Condyloma Acuminata • Cervical Dysplasia • Cervical Cancer Ø > 150 different types of the virus l l l Ø 15 High Risk Types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82) 16, 18 > 70% all cervical cancers 6, 11 90% genital warts HPV Vaccine – Gardasil ® l l Active against 16, 18, 6, 11 FDA approved in US for girls & boys ages 9 -26
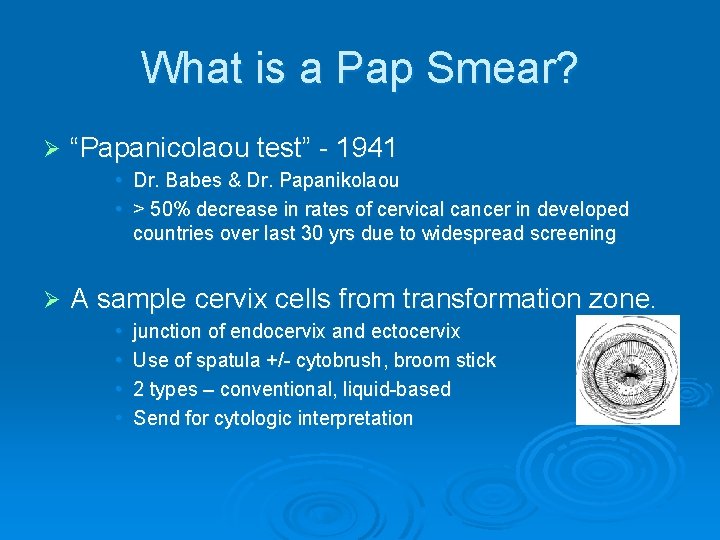
What is a Pap Smear? Ø “Papanicolaou test” - 1941 • Dr. Babes & Dr. Papanikolaou • > 50% decrease in rates of cervical cancer in developed countries over last 30 yrs due to widespread screening Ø A sample cervix cells from transformation zone. • • junction of endocervix and ectocervix Use of spatula +/- cytobrush, broom stick 2 types – conventional, liquid-based Send for cytologic interpretation
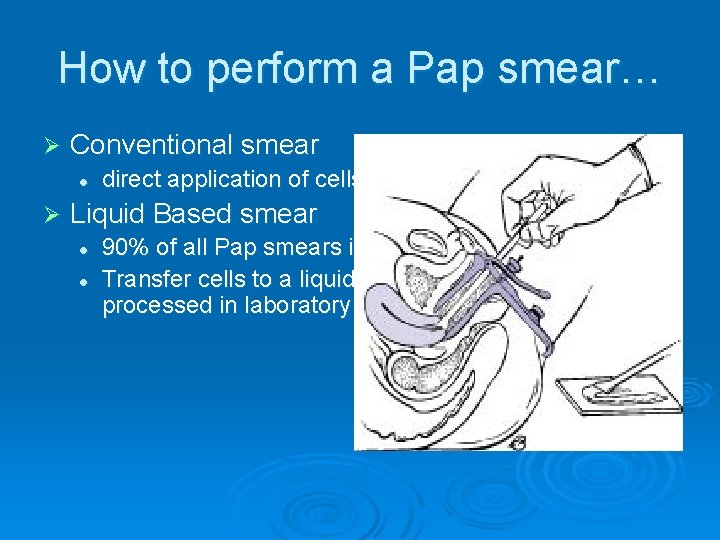
How to perform a Pap smear… Ø Conventional smear l Ø direct application of cells to a slide Liquid Based smear l l 90% of all Pap smears in US Transfer cells to a liquid preservative. Liquid processed in laboratory and transferred to a slide
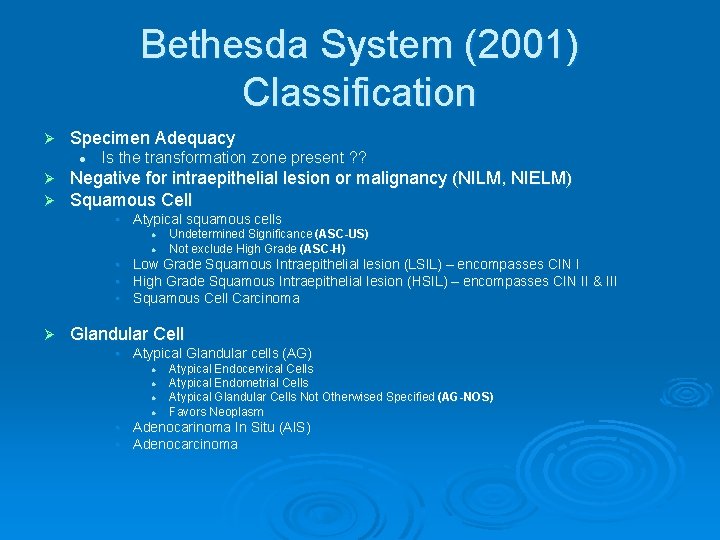
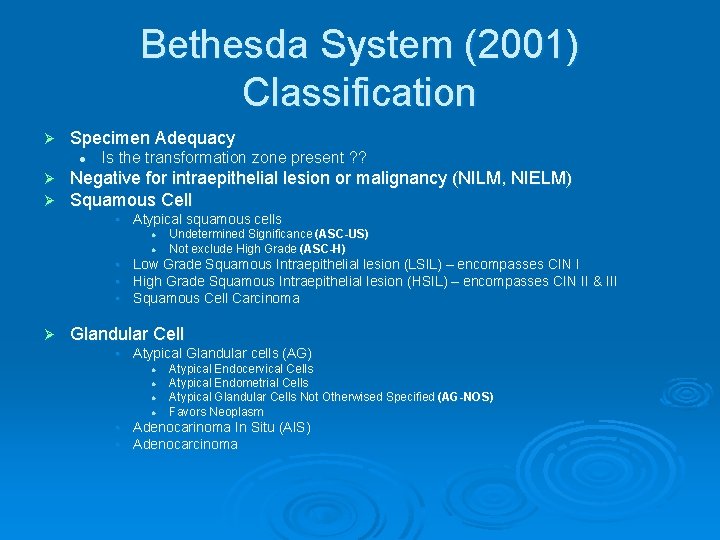
Bethesda System (2001) Classification Ø Specimen Adequacy l Ø Ø Is the transformation zone present ? ? Negative for intraepithelial lesion or malignancy (NILM, NIELM) Squamous Cell • Atypical squamous cells l l Undetermined Significance (ASC-US) Not exclude High Grade (ASC-H) • Low Grade Squamous Intraepithelial lesion (LSIL) – encompasses CIN I • High Grade Squamous Intraepithelial lesion (HSIL) – encompasses CIN II & III • Squamous Cell Carcinoma Ø Glandular Cell • Atypical Glandular cells (AG) l l Atypical Endocervical Cells Atypical Endometrial Cells Atypical Glandular Cells Not Otherwised Specified (AG-NOS) Favors Neoplasm • Adenocarinoma In Situ (AIS) • Adenocarcinoma
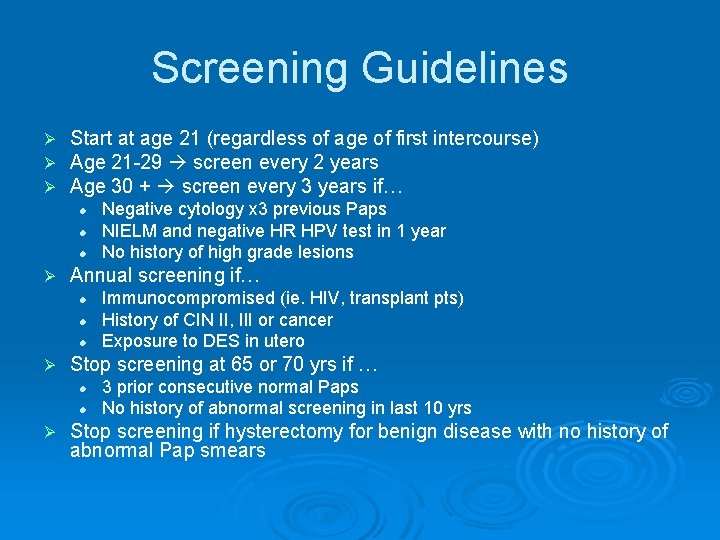
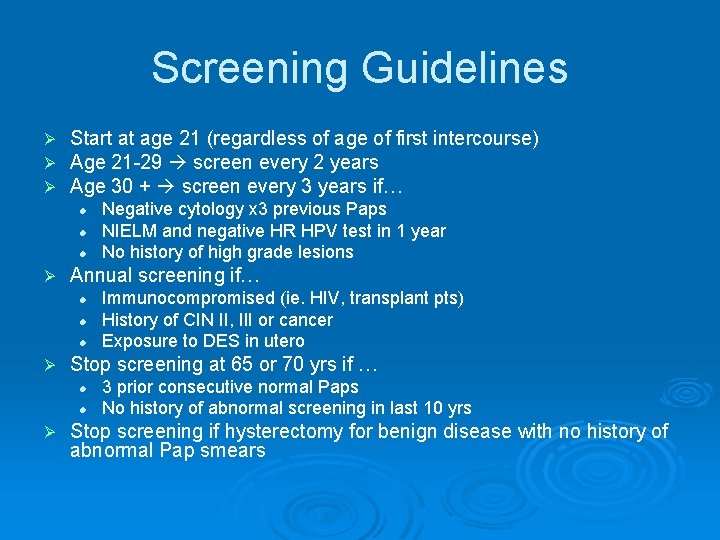
Screening Guidelines Ø Ø Ø Start at age 21 (regardless of age of first intercourse) Age 21 -29 screen every 2 years Age 30 + screen every 3 years if… l l l Ø Annual screening if… l l l Ø Immunocompromised (ie. HIV, transplant pts) History of CIN II, III or cancer Exposure to DES in utero Stop screening at 65 or 70 yrs if … l l Ø Negative cytology x 3 previous Paps NIELM and negative HR HPV test in 1 year No history of high grade lesions 3 prior consecutive normal Paps No history of abnormal screening in last 10 yrs Stop screening if hysterectomy for benign disease with no history of abnormal Pap smears
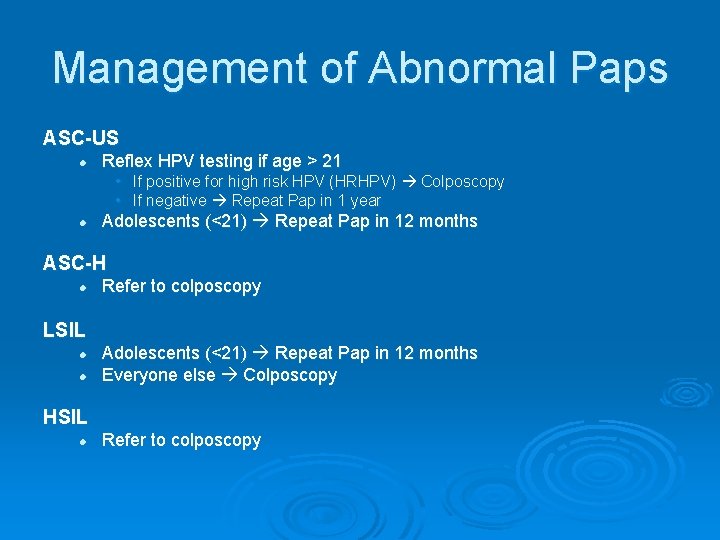
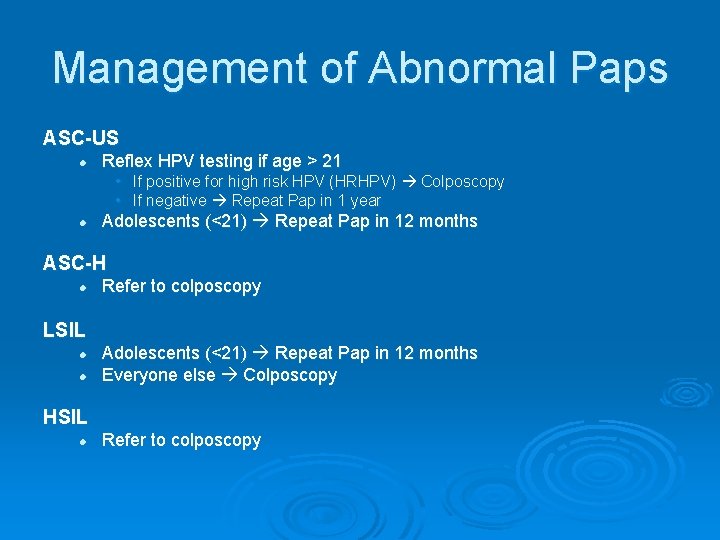
Management of Abnormal Paps ASC-US l Reflex HPV testing if age > 21 • If positive for high risk HPV (HRHPV) Colposcopy • If negative Repeat Pap in 1 year l Adolescents (<21) Repeat Pap in 12 months ASC-H l Refer to colposcopy LSIL l l Adolescents (<21) Repeat Pap in 12 months Everyone else Colposcopy HSIL l Refer to colposcopy
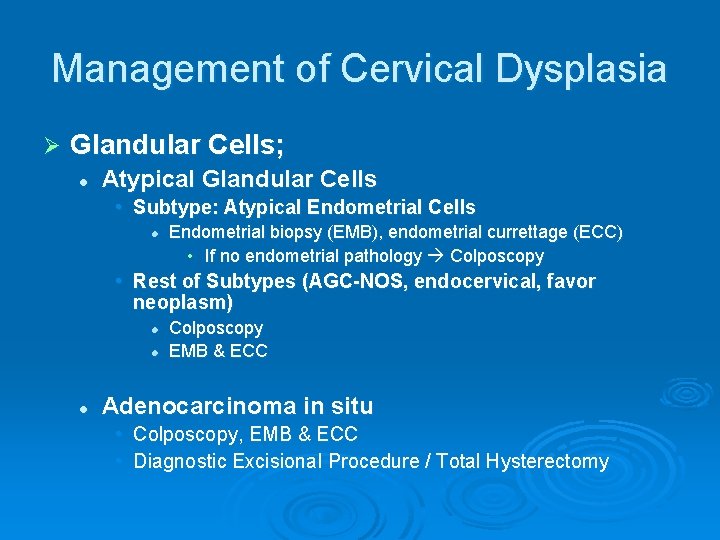
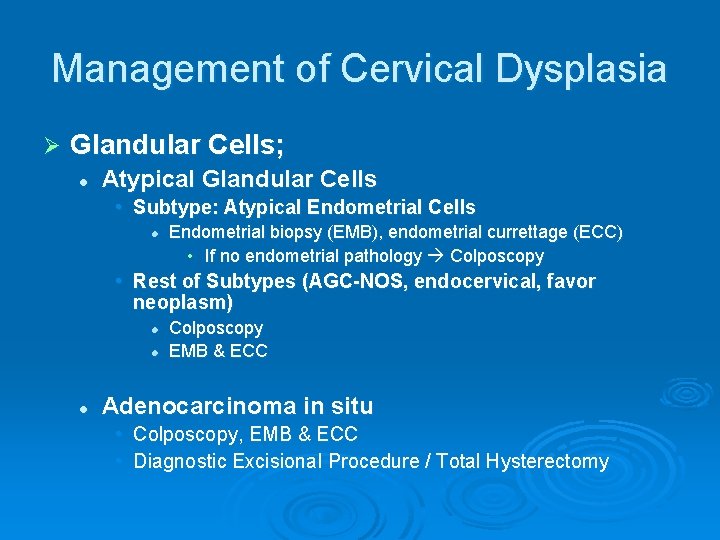
Management of Cervical Dysplasia Ø Glandular Cells; l Atypical Glandular Cells • Subtype: Atypical Endometrial Cells l Endometrial biopsy (EMB), endometrial currettage (ECC) • If no endometrial pathology Colposcopy • Rest of Subtypes (AGC-NOS, endocervical, favor neoplasm) l l l Colposcopy EMB & ECC Adenocarcinoma in situ • Colposcopy, EMB & ECC • Diagnostic Excisional Procedure / Total Hysterectomy