Certified Medical Board Investigator Training Event August 8
Certified Medical Board Investigator Training Event August 8, 2017 Elizabeth S. Grace, MD, FAAFP Medical Director, CPEP Assistant Clinical Professor, Department of Family Medicine University of Colorado
Introduction Elizabeth S. Grace, MD Medical Director CPEP – The Center for Personalized Education for Physicians • Independent, not-for-profit organization • Serving physicians and other healthcare professionals since 1990 • Mission To promote quality patient care and safety by enhancing the competence of physicians and other healthcare professionals
RESTORE clinicians to safe clinical practice RETAIN clinicians in the workforce Help clinicians REENTER practice after an absence
American Medical Association “… highly complicated and sensitive matter of providing help to physicians whose practice performance is sub-par. ”
Still relevant today…
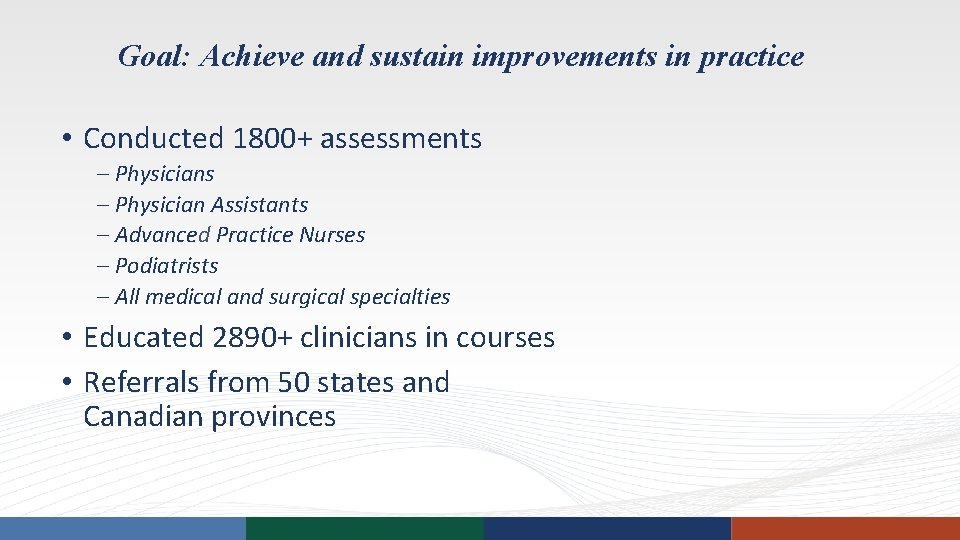
Goal: Achieve and sustain improvements in practice • Conducted 1800+ assessments – Physician Assistants – Advanced Practice Nurses – Podiatrists – All medical and surgical specialties • Educated 2890+ clinicians in courses • Referrals from 50 states and Canadian provinces
Alaska Hawaii
Alaska Hawaii
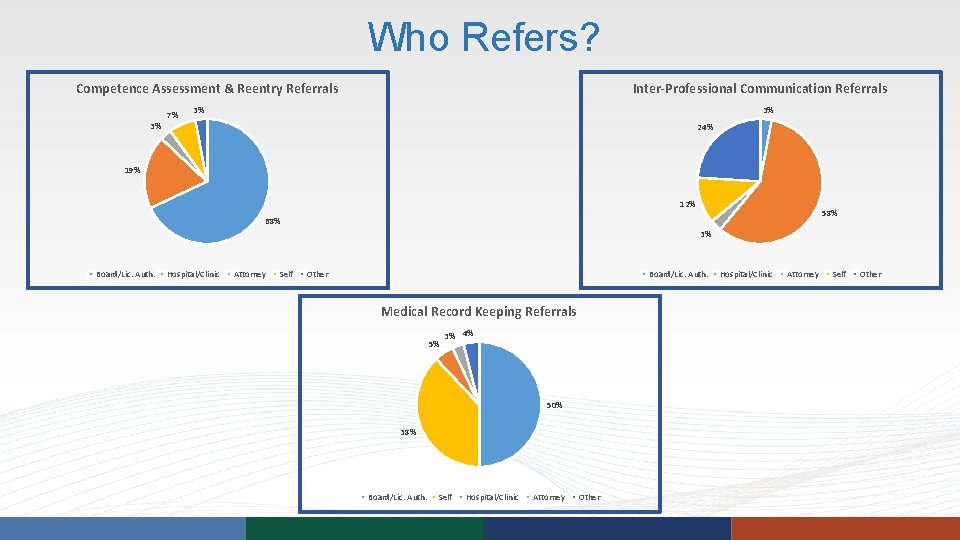
Who Refers? Competence Assessment & Reentry Referrals 3% 7% Inter-Professional Communication Referrals 3% 3% 24% 19% 12% 58% 68% 3% Board/Lic. Auth. Hospital/Clinic Attorney Self Other Board/Lic. Auth. Medical Record Keeping Referrals 5% 3% 4% 50% 38% Board/Lic. Auth. Self Hospital/Clinic Attorney Other Hospital/Clinic Attorney Self Other
Funding Sources Independent Non-Profit • Participant fees (92%) • Donations (6%) – Provide discounts to Colorado participants and support program development • Grants (2%) • No state/licensure funding
Fees* For program fees and CME: • Problems/Solutions Brochure • Website (www. cpepdoc. org) • Some programs vary by specialty or participant need • Call with questions 303 -577 -3232 Compare to: • Cost of litigation • Benefit of effective remediation
Who Pays? • Participant generally pays for services • Referring organization: – May pay a portion or all of cost for Assessment or course – Generally does not pay for educational intervention
Confidentiality Policy • Information shared only if written release – • Important to require participant to sign release in your order/agreement Release can be revoked – CPEP will notify parties involved • Participants may enroll without providing a release for referring organization • CPEP will notify state board if danger to patients • Regardless of referral organization/source
Testimony Upon request, CPEP will respond to requests for • Affidavits • Testimony by Medical Director or Executive Staff
Ethics Remediation, Rehabilitation, and Recommitment to Medical Professionalism: A Programmatic Approach Ethics and Behavior 2015 Predictors of Physician Performance on Competence Assessment Academic Medicine 2014 Physicians Reentering Clinical Practice: Characteristics and Clinical Abilities Journal of Continuing Education in the Health Professions 2010/Journal of Medical Regulation 2011 Do Physicians Referred for Competency Evaluations have Underlying Cognitive Problems? Academic Medicine 2009
Certified Medical Board Investigator Training Event August 8, 2017 Foundational Concepts of Assessment and Remediation
Objectives • Why do things go wrong in a medical environment? • What are the real goals of an investigation? • How does remediation fit in? • What are the best ways to approach remediation?
Mission of the Medical Licensing Boards Patient protection through the regulation of the practice of medicine
Why do things go wrong in a medical environment? • Institutional /regulatory • Organizational/management • Work environment • Team environment • Staffing • Task related • Patient characteristics • Combinations of factors https: //psnet. ahrq. gov/primers/primer/10/root-cause-analysis
Why do things go wrong in a medical environment? • Institutional /regulatory • Organizational/management • Work environment • Team environment • Staffing • Task related • Patient characteristics • Combinations of factors https: //psnet. ahrq. gov/primers/primer/10/root-cause-analysis
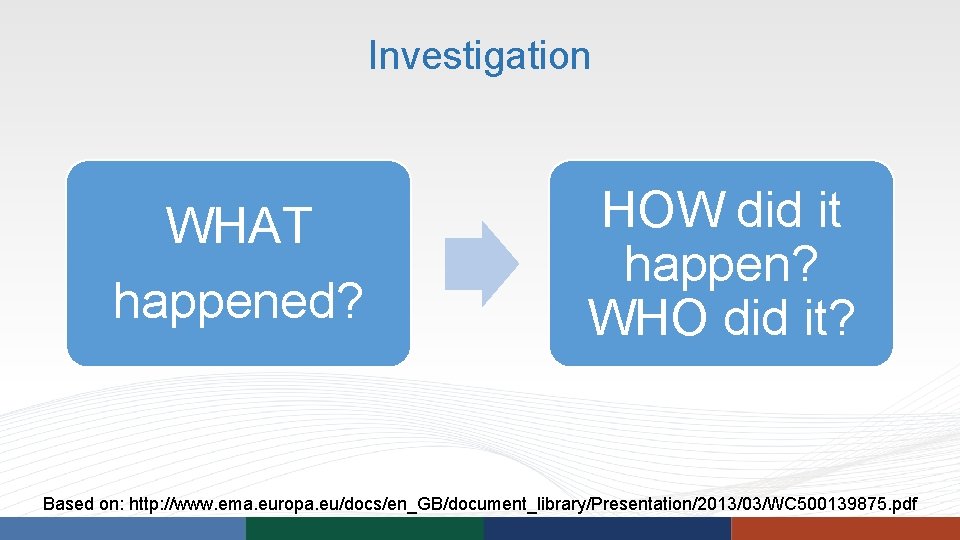
Investigation WHAT happened? HOW did it happen? WHO did it? Based on: http: //www. ema. europa. eu/docs/en_GB/document_library/Presentation/2013/03/WC 500139875. pdf
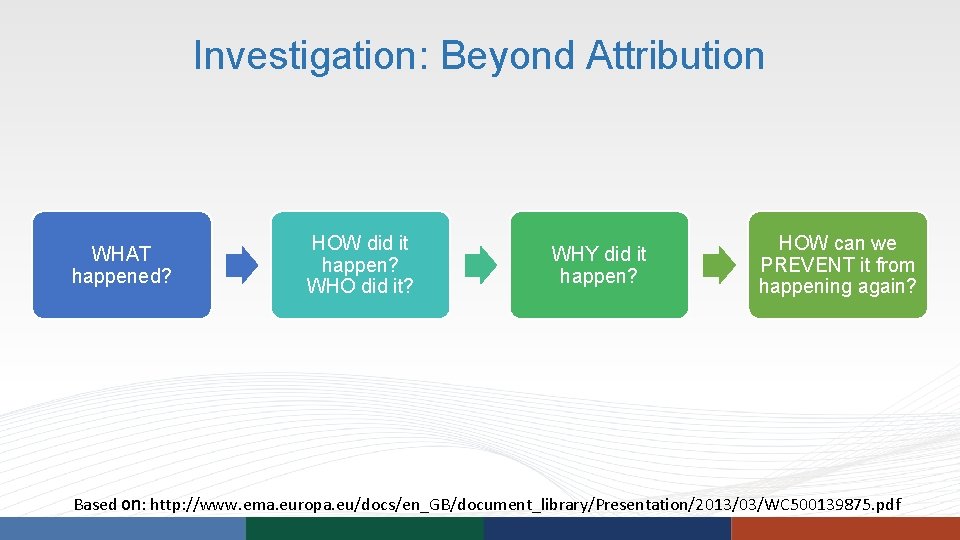
Investigation: Beyond Attribution WHAT happened? HOW did it happen? WHO did it? WHY did it happen? HOW can we PREVENT it from happening again? Based on: http: //www. ema. europa. eu/docs/en_GB/document_library/Presentation/2013/03/WC 500139875. pdf
Response to Substandard Care • Restraint • Punishment • Remediation
Remediation “Physician, heal thyself. ” Luke 4: 23
Remediation “The preponderance of evidence suggests that physicians have a limited ability to self-assess. ” Accuracy of Physician Self-assessment Compared With Observed Measures of Competence, JAMA, Vol. 296 No. 9, September 6, 2006
Remediation “I can’t fix it if I don’t know what’s broken. ” Highway Heartbreak Ridge (1986)
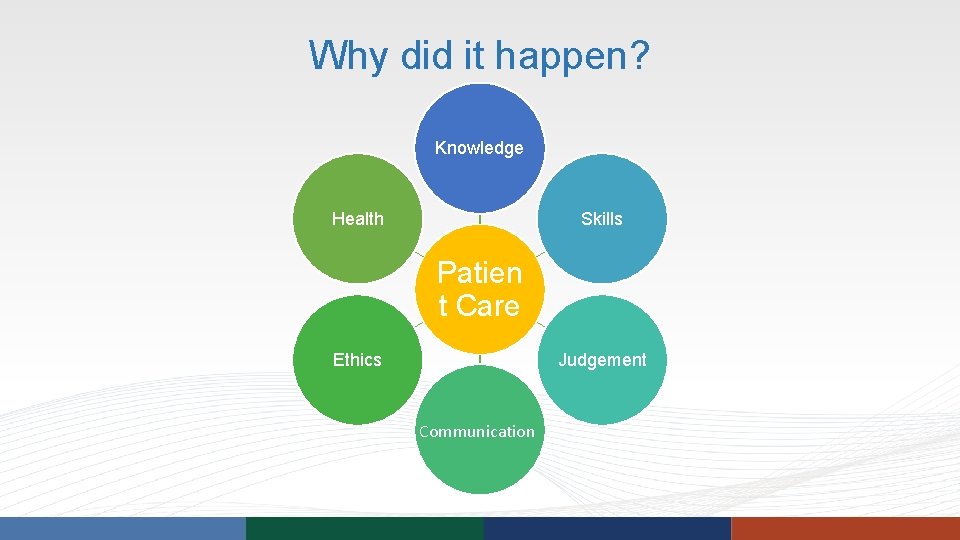
Why did it happen? Knowledge Health Skills Patien t Care Ethics Judgement Communication
How did it happen? Clinical Competence Assessment • First step in effective remediation is determining gaps • Physician assessment programs provide objective and comprehensive educational needs assessments • Typically the assessment is not limited to the specific area of concern • Remediation is then targeted to identified needs
How do we prevent it from happening again? Remediation: CME leads to greater improvement in participant performance if it… • Is interactive • Uses a variety of methods – Simulation technology, standardized patients, immediate feedback • Involves multiple exposures to content over longer duration • Focuses on outcomes that are considered important by the clinician (contextually relevant) Effectiveness of CME: Updated Synthesis of Systematic Reviews. Cervero, et al; ACCME 2014
How do we prevent it from happening again? Remediation: • Traditional continuing medical education • Intensive skill building courses • Structured and monitored educational intervention
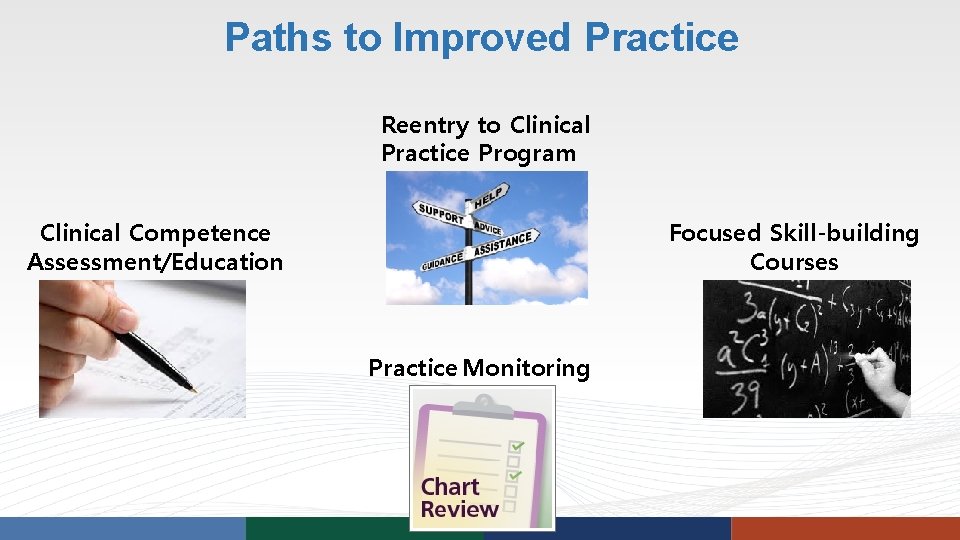
Paths to Improved Practice Reentry to Clinical Practice Program Clinical Competence Assessment/Education Focused Skill-building Courses Practice Monitoring
Competence Assessment Programs • Focus on physicians whose clinical competence has been questioned • Referred by a regulatory agency • Conduct comprehensive assessment • Relevant to core competencies • Provide remedial education that identifies specific expected activities and goals Guidelines for Physician Enhancement Programs Coalition for Physician Enhancement
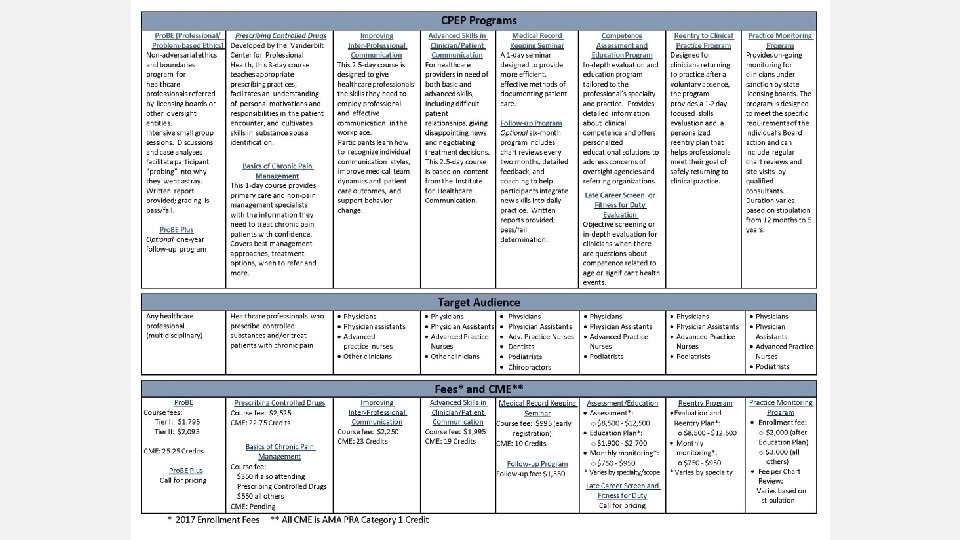
Focused Remedial Courses Medical Record Keeping PROBE: Ethics Remediation Prescribing Controlled Drugs Basics of Chronic Pain Management Clinician-Patient Communications Inter-Professional Communications
Skill-Building Courses • Course characteristics – Small group, interactive format – Tailored to meet needs of participants – Faculty expertise • Incorporate personalized learning techniques – Practice skills with simulated patients – Develop personalized action plan – Performance reports from faculty and follow-up recommendations New courses developed with grant support provided by COPIC Medical Foundation and Pinnacol
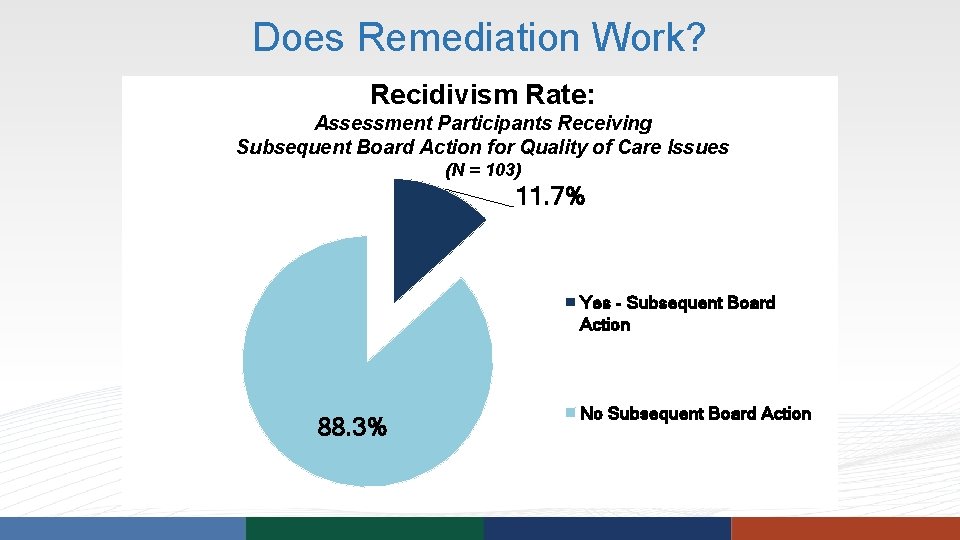
Does Remediation Work? Recidivism Rate: Assessment Participants Receiving Subsequent Board Action for Quality of Care Issues (N = 103) 11. 7% Yes - Subsequent Board Action 88. 3% No Subsequent Board Action
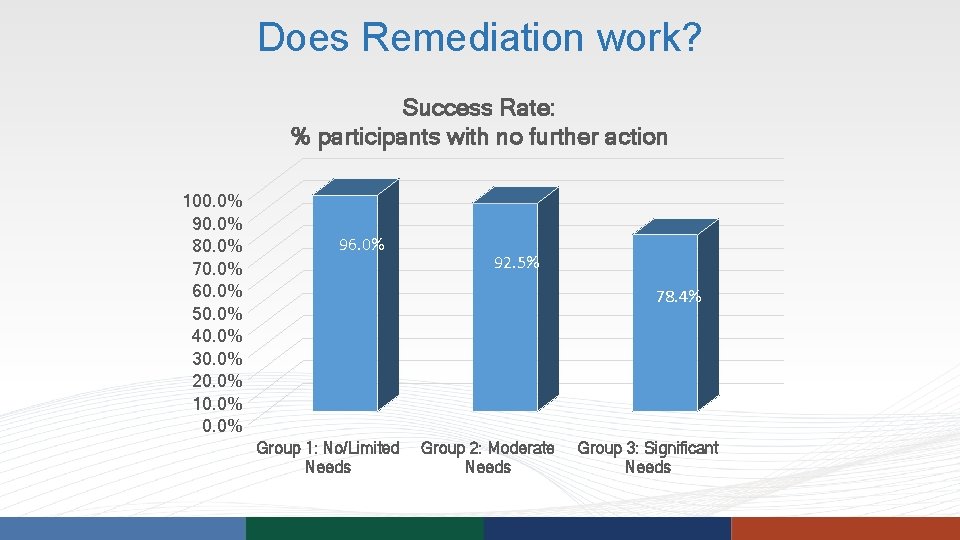
Does Remediation work? Success Rate: % participants with no further action 100. 0% 90. 0% 80. 0% 70. 0% 60. 0% 50. 0% 40. 0% 30. 0% 20. 0% 10. 0% 96. 0% 92. 5% 78. 4% Group 1: No/Limited Needs Group 2: Moderate Needs Group 3: Significant Needs
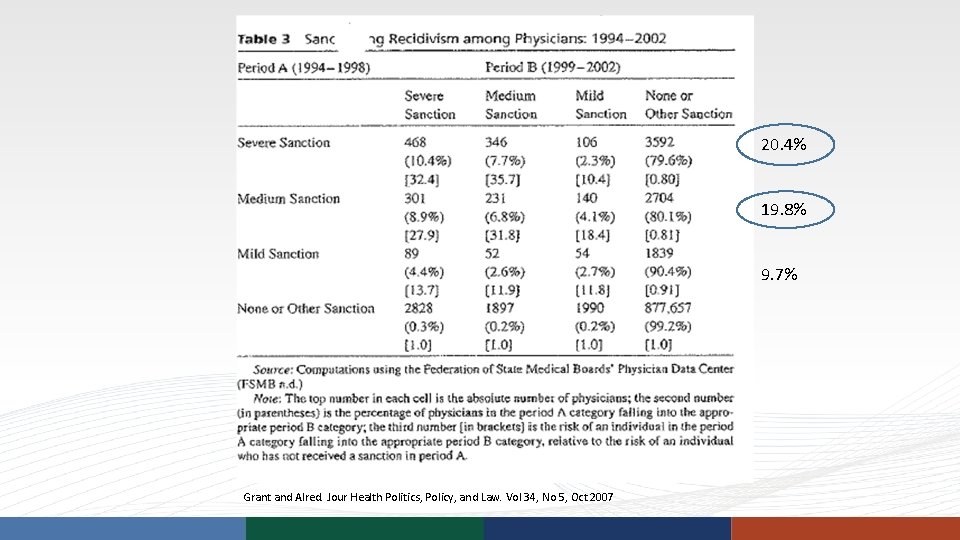
20. 4% 19. 8% 9. 7% Grant and Alred. Jour Health Politics, Policy, and Law. Vol 34, No 5, Oct 2007
Directory of Assessment and Education Programs FSMB Clinical Competence Assessment Resources http: //fsmb. org/licensure/spex_plas/plas_clinical FSMB Directory of Physician Assessment and Remedial Education Programs http: //fsmb. org/Media/Default/PDF/USMLE/Rem. Ed. Prog. pdf Coalition for Physician Enhancement http: //cpe. memberlodge. org/organizationalmembers
Summary • Ideally, investigations look into what the underlying cause(s) could be, to try to prevent additional occurrences • Remediation should always be considered • Physicians are not skilled at self-identifying educational needs • Competence assessment programs help identify needs • Structured education programs relieve boards of burden of evaluating and monitoring a physician’s plan for remediation
Certified Medical Board Investigator Training Event August 8, 2017 Clinical Competence Assessment and Remediation
Objectives • Overview of Competence Assessment and Education Programs • Determining scope of an Assessment: Board input • Testing components and modalities • Format of findings and outcomes • Overview of an Educational Intervention • What defines successful completion of remediation
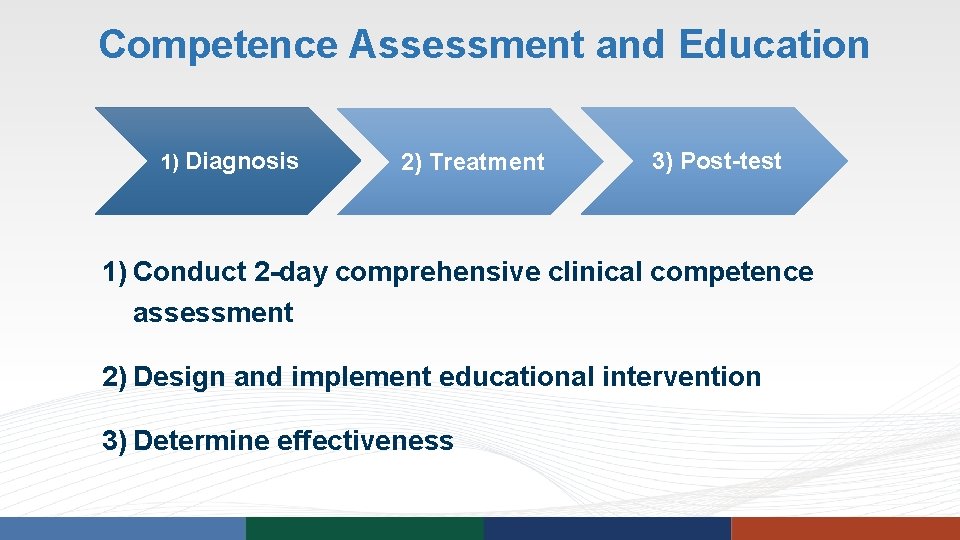
Competence Assessment and Education 1) Diagnosis 2) Treatment 3) Post-test 1) Conduct 2 -day comprehensive clinical competence assessment 2) Design and implement educational intervention 3) Determine effectiveness
Competence Assessment: Personalization CPEP Competence Assessments • Tailored to the profession • Physician – M. D. /D. O. • Physician Assistant, Advance Practice Nurse, Doctor of Podiatric Medicine • Specialty-specific • Tailored to the participant’s scope of practice
Information Gathering: Participant • Written intake materials • • • Education and training Job history Malpractice history Scope of practice Schedule of appointments, procedures, deliveries • Telephone interview conducted by Associate Medical Director • Participant’s perspective • Anticipated changes to practice
Information Gathering: Referring Organization • Referring organization information is key to assessment design • • • Public and confidential discipline Informal communication What are your questions? What is the participant’s history with the organization? If the participant’s license is restricted, is it temporary or permanent?
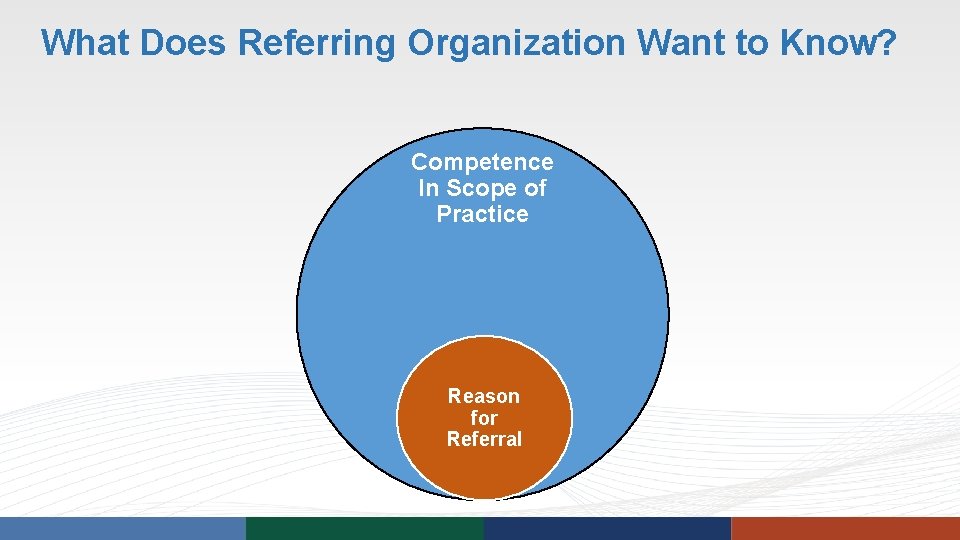
What Does Referring Organization Want to Know? Competence In Scope of Practice Reason for Referral
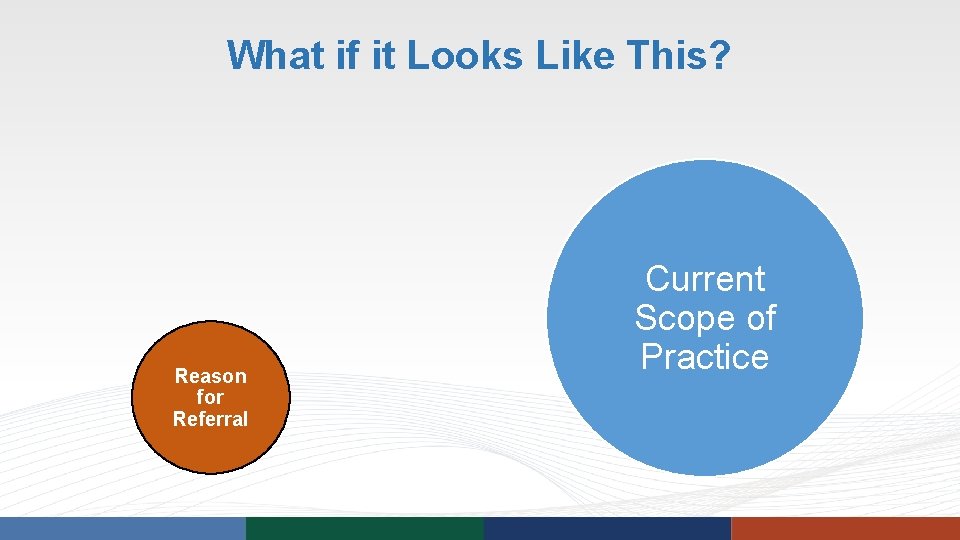
What if it Looks Like This? Reason for Referral Current Scope of Practice
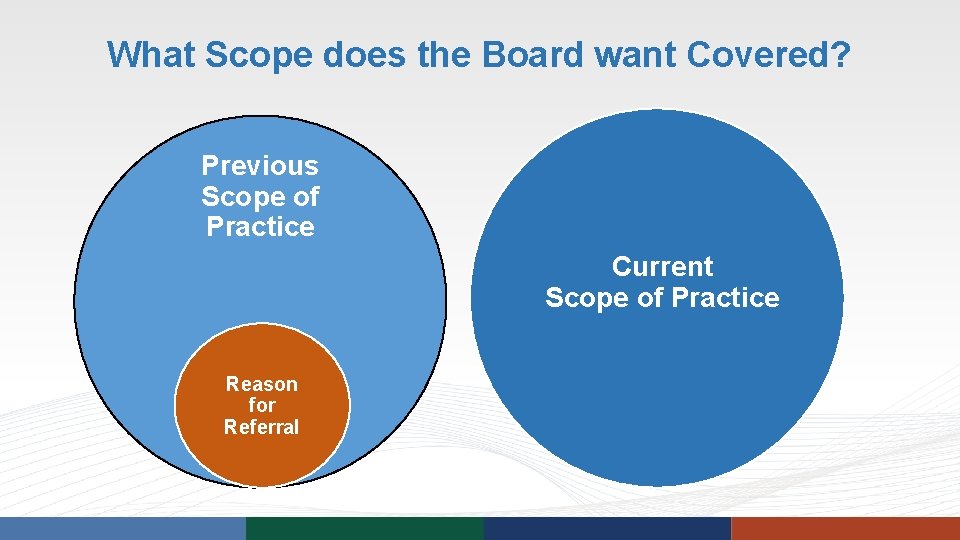
What Scope does the Board want Covered? Previous Scope of Practice Current Scope of Practice Reason for Referral
Focus of Competence Assessment • Cover participant’s scope of practice • Evaluate participant’s actual practice • Application of knowledge in practice • Address reason for referral
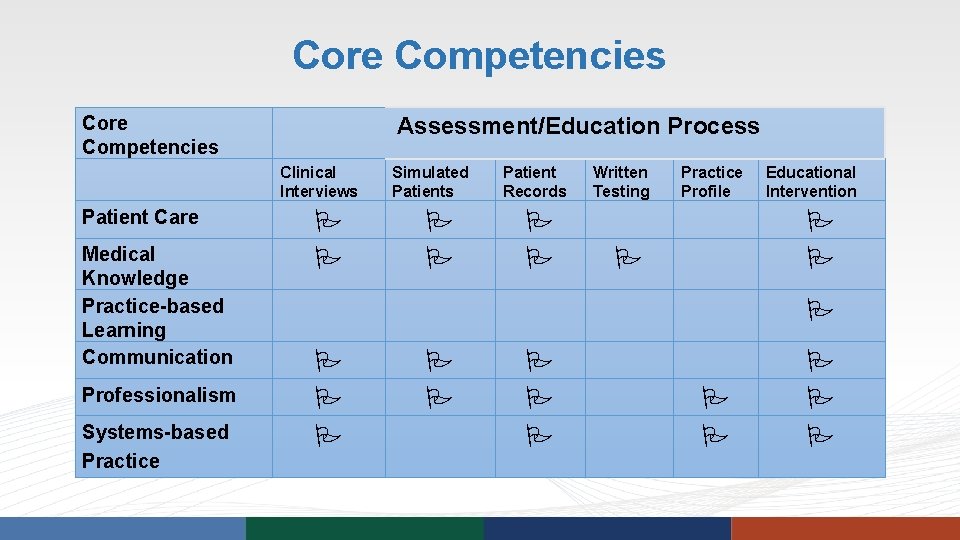
Core Competencies Assessment/Education Process Clinical Interviews Patient Care Medical Knowledge Practice-based Learning Communication Professionalism Systems-based Practice Simulated Patients Patient Records Written Testing Practice Profile Educational Intervention
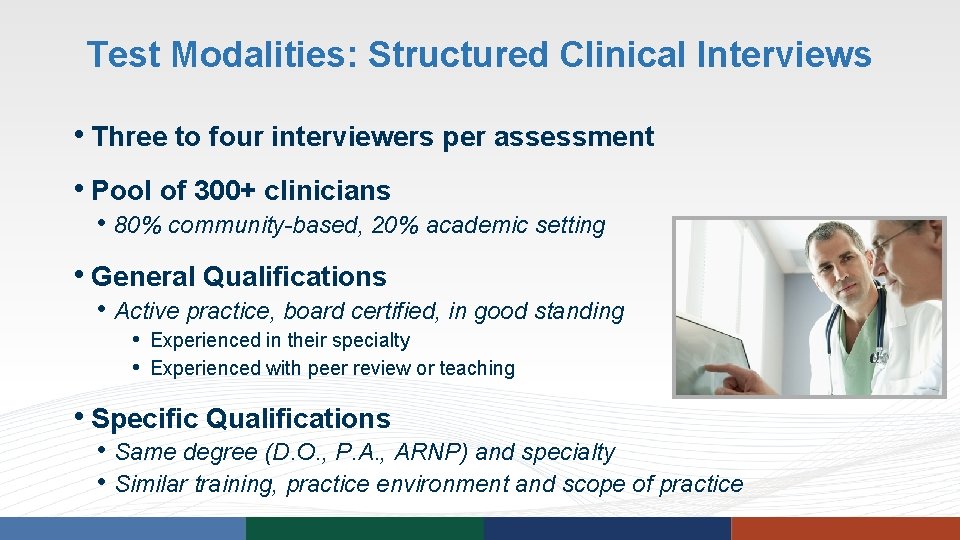
Test Modalities: Structured Clinical Interviews • Three to four interviewers per assessment • Pool of 300+ clinicians • 80% community-based, 20% academic setting • General Qualifications • Active practice, board certified, in good standing • Experienced in their specialty • Experienced with peer review or teaching • Specific Qualifications • Same degree (D. O. , P. A. , ARNP) and specialty • Similar training, practice environment and scope of practice
Components of Structured Clinical Interviews • Clinical interviews based on: • Patient records from participant’s practice or hypothetical cases • Topics pertinent to speciality • Chart reviews • Twenty to forty charts reviewed by interviewing clinical consultants • CPEP selects charts • Consultants do not review index cases • Charts selected to reflect scope of practice and areas of concern • Includes office, surgical, and procedural charts • Other information: e. g. , images, FMS, EKG, EEG
Value of Structured Clinical Interviews • Objective evaluation • Knowledge • Clinical judgement, rationale • Application of knowledge in practice • Quality of care provided • Documentation practices
Test Modalities: Written Testing and More • ECG Interpretation • Fetal monitor strip interpretation • Multiple choice testing • NBME: post licensure and clinical science exams • COMVEX • NCCPA practice exams • Cognitive function screen using Micro. Cog • Review of health information
Test Modalities: Simulated Patient Encounters • Components • • Interview and examine simulated patient Specialty-specific scenarios Trained actors Document a progress note • Evaluates • Communication and documentation skills
Test Modalities: Technical Skills Testing • Difficult Airway Simulation • Fundamentals of Laparoscopic Surgery • Fundamentals of Endoscopic Surgery • Emergency Medicine • In development: Obstetrics
Assessment Results • Formal report of results based on participant performance • • • Medical Knowledge Patient Care Documentation Communication Professionalism • Educational recommendations for remediation (if warranted)
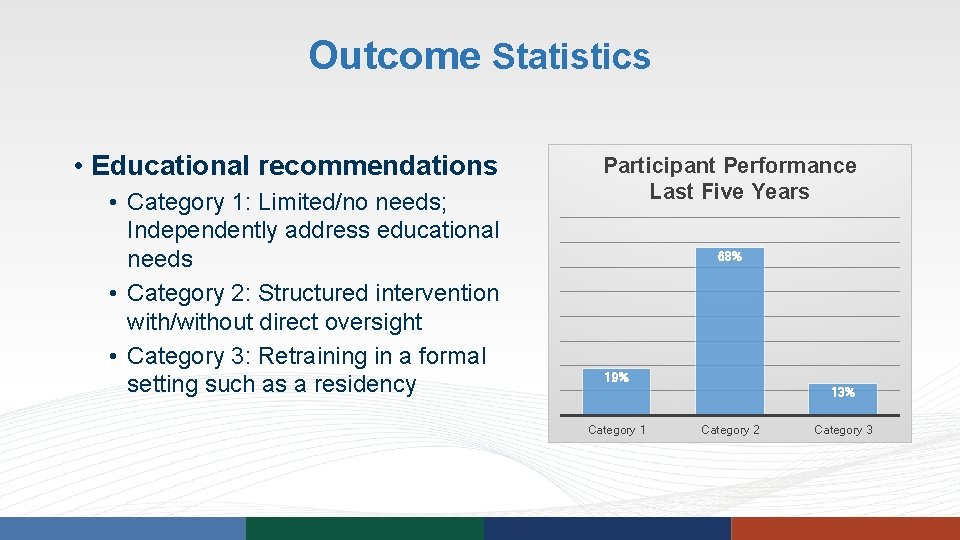
Outcome Statistics • Educational recommendations • Category 1: Limited/no needs; Independently address educational needs • Category 2: Structured intervention with/without direct oversight • Category 3: Retraining in a formal setting such as a residency Participant Performance Last Five Years 68% 19% 13% Category 1 Category 2 Category 3
Educational Intervention
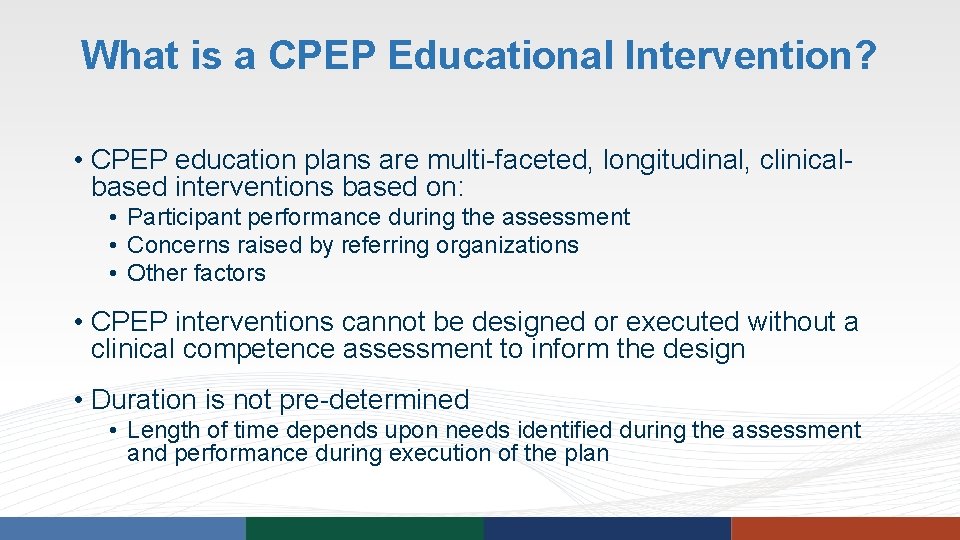
What is a CPEP Educational Intervention? • CPEP education plans are multi-faceted, longitudinal, clinicalbased interventions based on: • Participant performance during the assessment • Concerns raised by referring organizations • Other factors • CPEP interventions cannot be designed or executed without a clinical competence assessment to inform the design • Duration is not pre-determined • Length of time depends upon needs identified during the assessment and performance during execution of the plan
Overall Educational Intervention Goals § Reawaken intellectual ability § Learn how to manage ongoing professional development in contemporary practice § Seek to identify and address barriers to successful practice § Achieve and sustain improvements in practice § Gain skills in evaluating quality of resources and references, with emphasis on evidence-based medicine
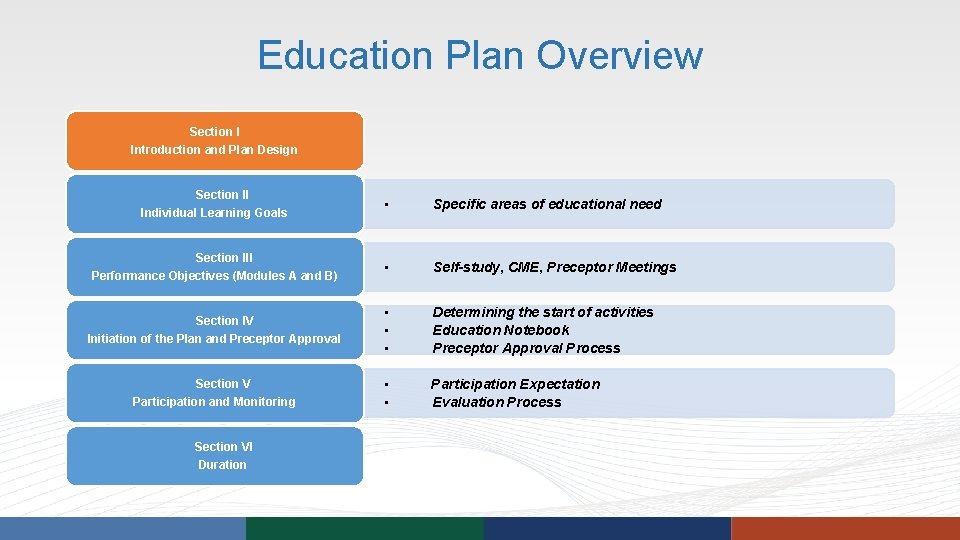
Education Plan Overview Section I Introduction and Plan Design Section II Individual Learning Goals Section III Performance Objectives (Modules A and B) Section IV Initiation of the Plan and Preceptor Approval Section V Participation and Monitoring Section VI Duration • Specific areas of educational need • Self-study, CME, Preceptor Meetings • • • Determining the start of activities Education Notebook Preceptor Approval Process • • Participation Expectation Evaluation Process
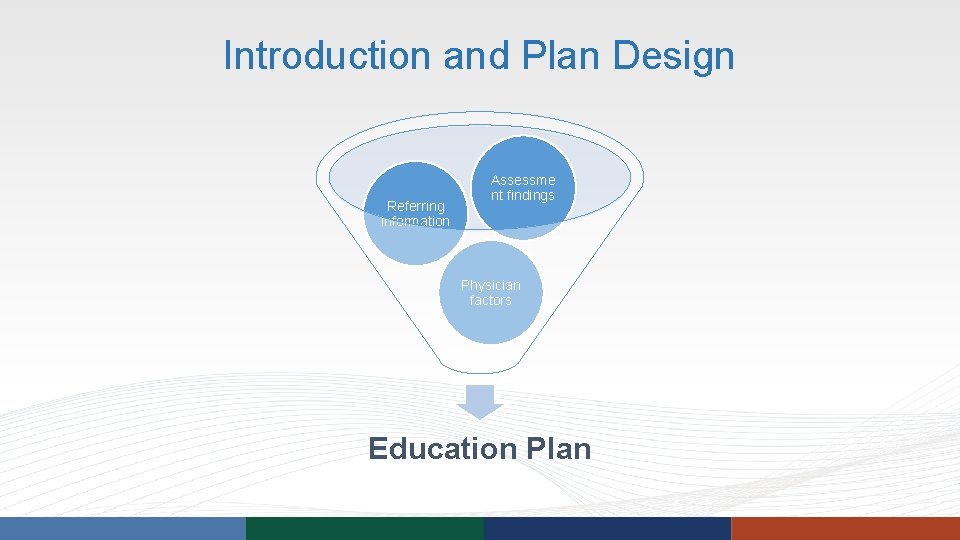
Introduction and Plan Design Referring information Assessme nt findings Physician factors Education Plan
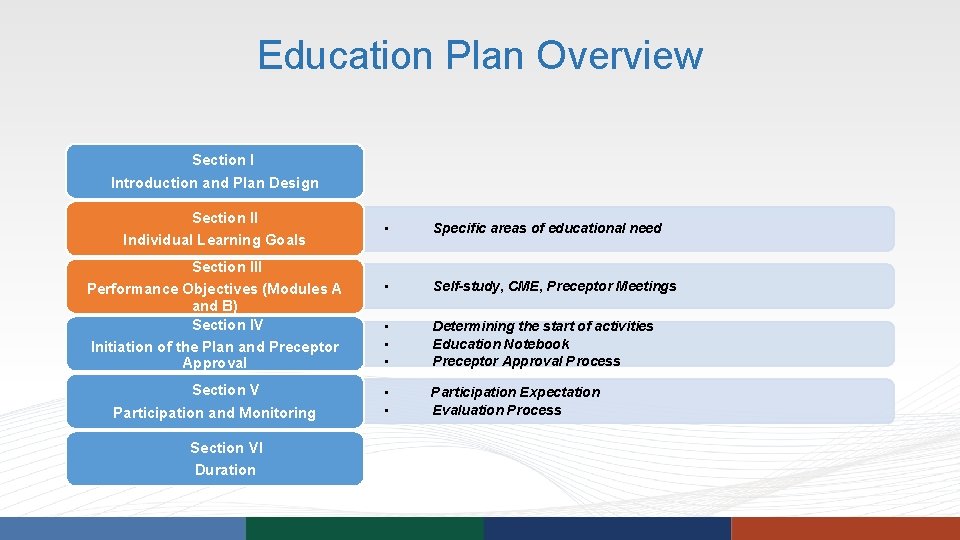
Education Plan Overview Section I Introduction and Plan Design Section II Individual Learning Goals Section III Performance Objectives (Modules A and B) Section IV Initiation of the Plan and Preceptor Approval Section V Participation and Monitoring Section VI Duration • Specific areas of educational need • Self-study, CME, Preceptor Meetings • • • Determining the start of activities Education Notebook Preceptor Approval Process • • Participation Expectation Evaluation Process
Goals and Objectives § Learning Goals are defined by the assessment report § Performance Objectives are the specific educational activities that provide focused learning experiences
Module A: Medical Knowledge Enhancement § Increase medical knowledge through a variety of modalities • • • Case-based learning CME Suggested readings Courses Self-study – peer-reviewed, evidence-based resources • May begin before Preceptor is identified • Benefit is maximized with Preceptor participation
Module B: Patient Care Enhancement • Completed with a Preceptor • Practice-based education • Chart reviews and preceptor meetings • Point-of-Care – graduated levels of oversight • Participant providing patient care in their home community, if possible
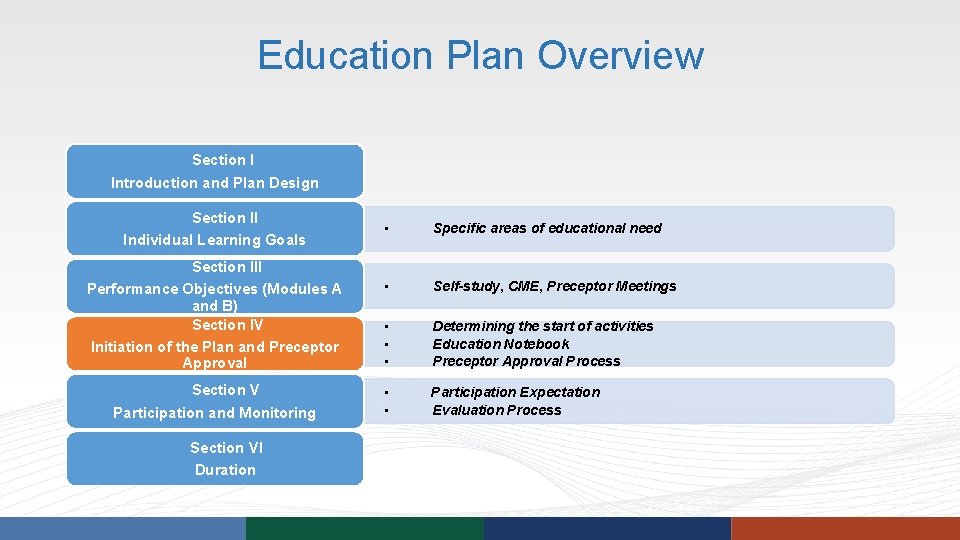
Education Plan Overview Section I Introduction and Plan Design Section II Individual Learning Goals Section III Performance Objectives (Modules A and B) Section IV Initiation of the Plan and Preceptor Approval Section V Participation and Monitoring Section VI Duration • Specific areas of educational need • Self-study, CME, Preceptor Meetings • • • Determining the start of activities Education Notebook Preceptor Approval Process • • Participation Expectation Evaluation Process
Initiation of the Plan
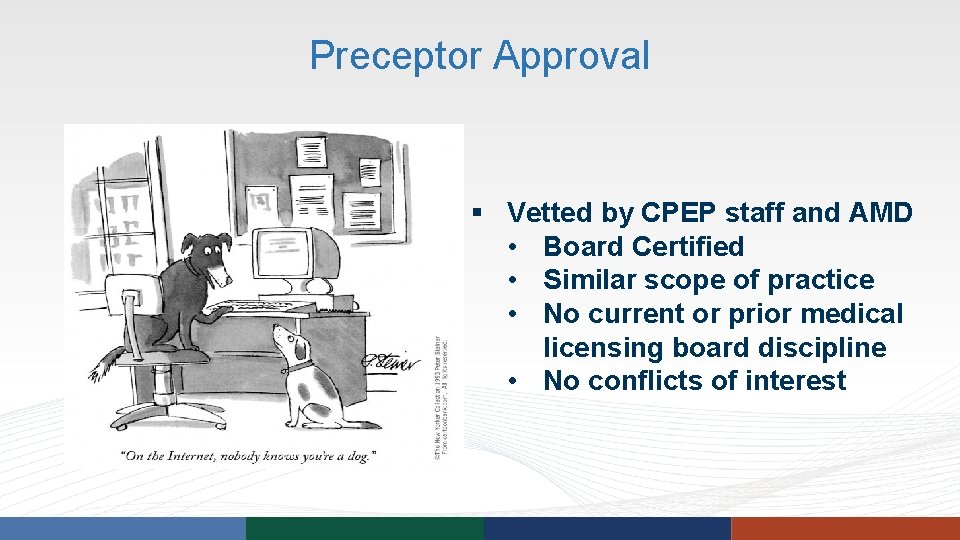
Preceptor Approval § Vetted by CPEP staff and AMD • Board Certified • Similar scope of practice • No current or prior medical licensing board discipline • No conflicts of interest
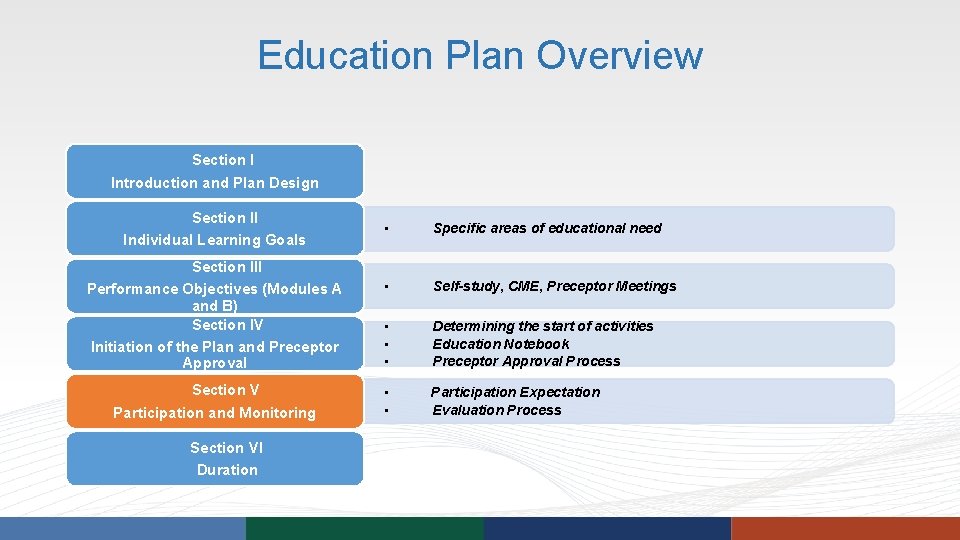
Education Plan Overview Section I Introduction and Plan Design Section II Individual Learning Goals Section III Performance Objectives (Modules A and B) Section IV Initiation of the Plan and Preceptor Approval Section V Participation and Monitoring Section VI Duration • Specific areas of educational need • Self-study, CME, Preceptor Meetings • • • Determining the start of activities Education Notebook Preceptor Approval Process • • Participation Expectation Evaluation Process
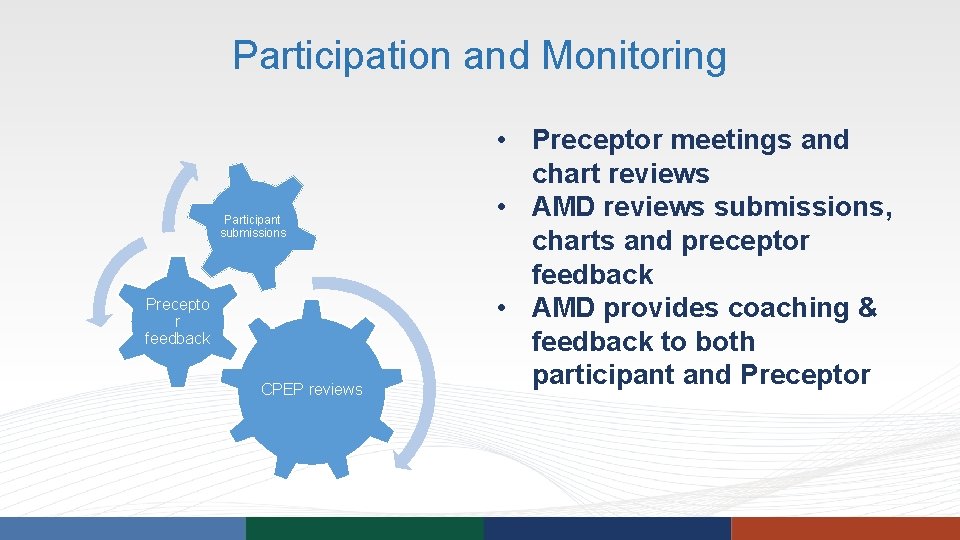
Participation and Monitoring Participant submissions Precepto r feedback CPEP reviews • Preceptor meetings and chart reviews • AMD reviews submissions, charts and preceptor feedback • AMD provides coaching & feedback to both participant and Preceptor
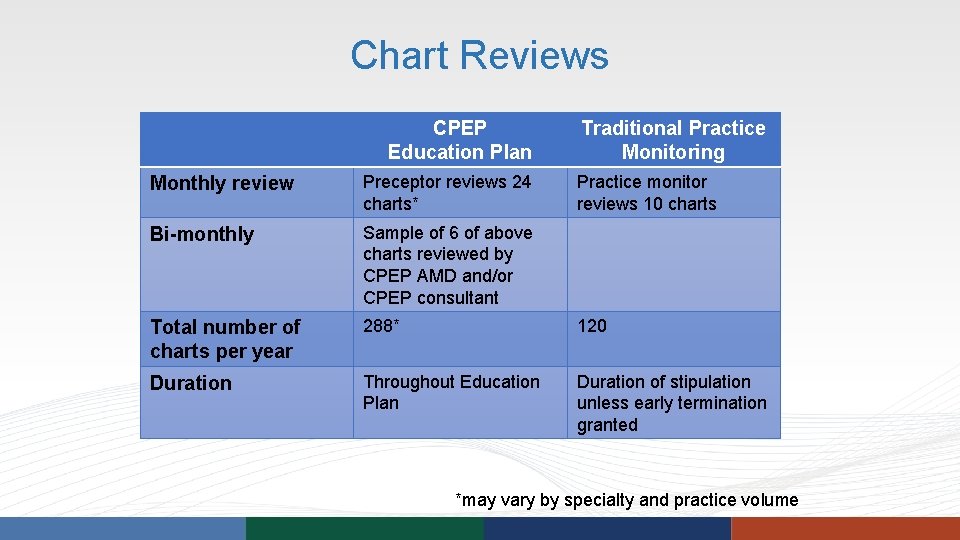
Chart Reviews CPEP Education Plan Traditional Practice Monitoring Monthly review Preceptor reviews 24 charts* Practice monitor reviews 10 charts Bi-monthly Sample of 6 of above charts reviewed by CPEP AMD and/or CPEP consultant Total number of charts per year 288* 120 Duration Throughout Education Plan Duration of stipulation unless early termination granted *may vary by specialty and practice volume
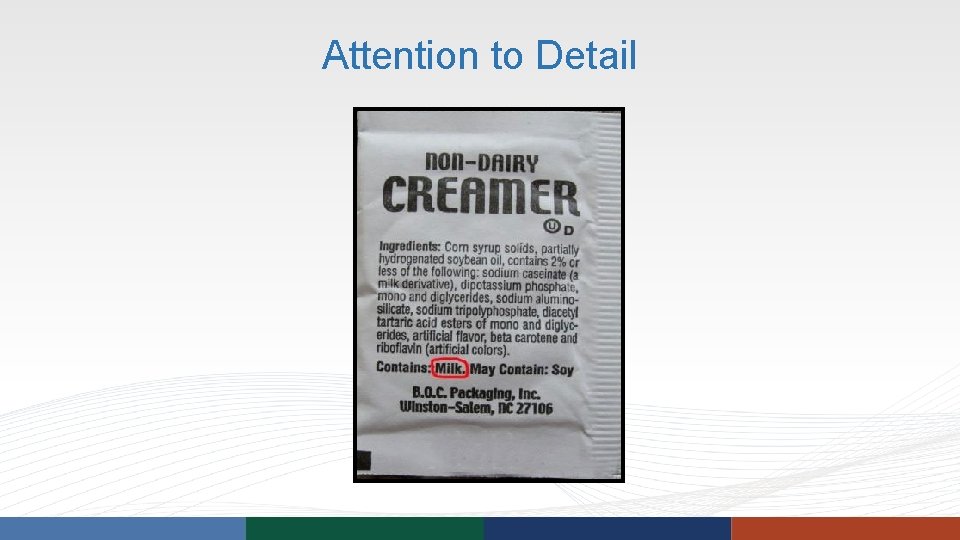
Attention to Detail
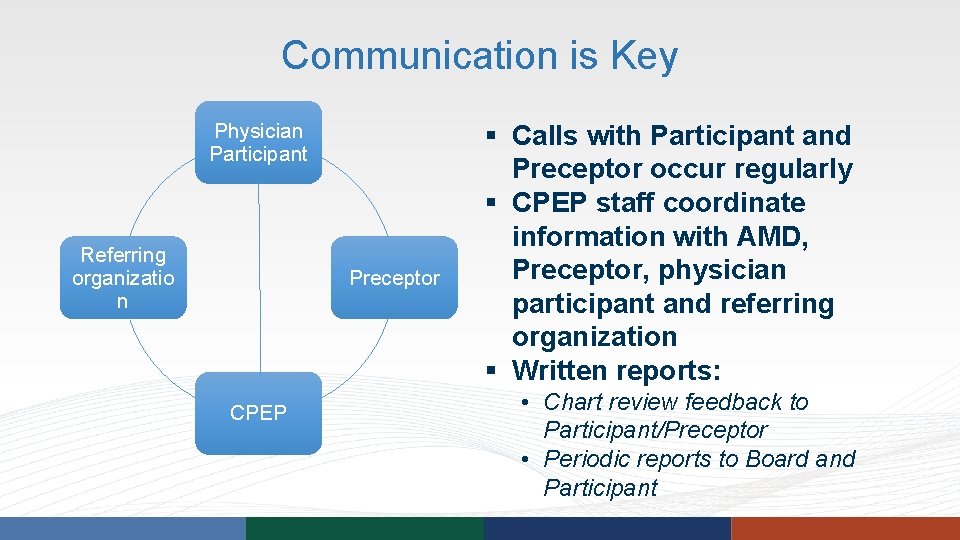
Communication is Key Physician Participant Referring organizatio n Preceptor CPEP § Calls with Participant and Preceptor occur regularly § CPEP staff coordinate information with AMD, Preceptor, physician participant and referring organization § Written reports: • Chart review feedback to Participant/Preceptor • Periodic reports to Board and Participant
Summative Assessment • Post-Education Evaluation • To demonstrate maintenance of improvements • Similar components to Assessment • What if they don’t pass?
Termination Rare, but can occur in circumstances of: • Non-compliance • Maximal educational benefit • Others
Summary • Educational needs assessment should be conducted before and after education intervention • Determining scope of Assessment is complicated and Board input is often needed • Assessment is by multiple means and involves chart review • Educational recommendations are based on performance • Structured education is clinically-based

Certified Medical Board Investigator Training Event August 8, 2017 Electronic Medical Records: New Challenges in Reviewing Medical Records
Objectives • Discuss why documentation is such a challenge to some physicians • Review general principles of good documentation • Discuss specific characteristics of the EMR that complicate chart and case review
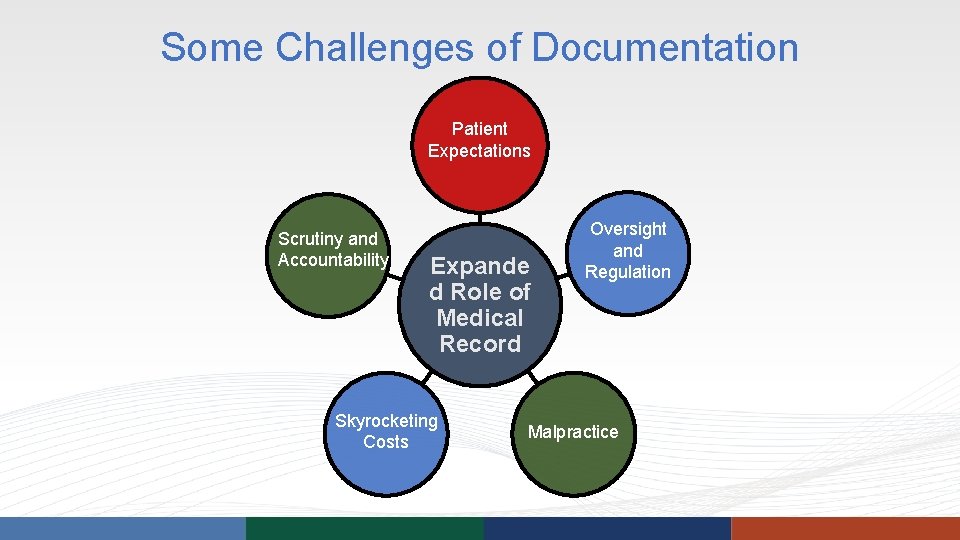
Some Challenges of Documentation Patient Expectations Scrutiny and Accountability Expande d Role of Medical Record Skyrocketing Costs Oversight and Regulation Malpractice
General Principles of Good Documentation Test #1 Could another provider reading any individual chart note: • See a complete and logical picture of each encounter? • Understand clinical reasoning without guessing?
General Principles of Good Documentation Test #2 Could another healthcare provider assume ongoing care of the patient without re-doing work?
Organization of the Clinical Information • Subjective P A • Objective • Assessment • Plan S O
Understanding Clinical Rationale When a thing is true, there is no need to use any arguments to substantiate it. -Vinobe Bhave
EMR: Benefits for the Investigator/Reviewer • Legibility • Organization • Availability: not likely to be lost; easily accessible • Time stamps and identification of the “author” for entries to the record and when the encounter “closed” • Access is tracked • Metadata
EMR: Drawbacks for the Investigator/Reviewer • Ease of access: security concern • Availability dependent upon functioning hardware and system • Constantly changing format: difficult to recreate what the physician saw and had access to at the time • Pseudonarrative • Checklists • Ability to ‘cut and paste’ clinical information: difficult to determine what was actually done
EMR: Drawbacks for the Investigator/Reviewer • Takes entirely different skillset to review an electronic chart • More places to “store” information • Communication between providers • Communication with patient, e. g. , test results and follow-up recommendations • Error correction may be difficult to identify • Some parts of the record do not “exist” unless called upon • Data “noise”
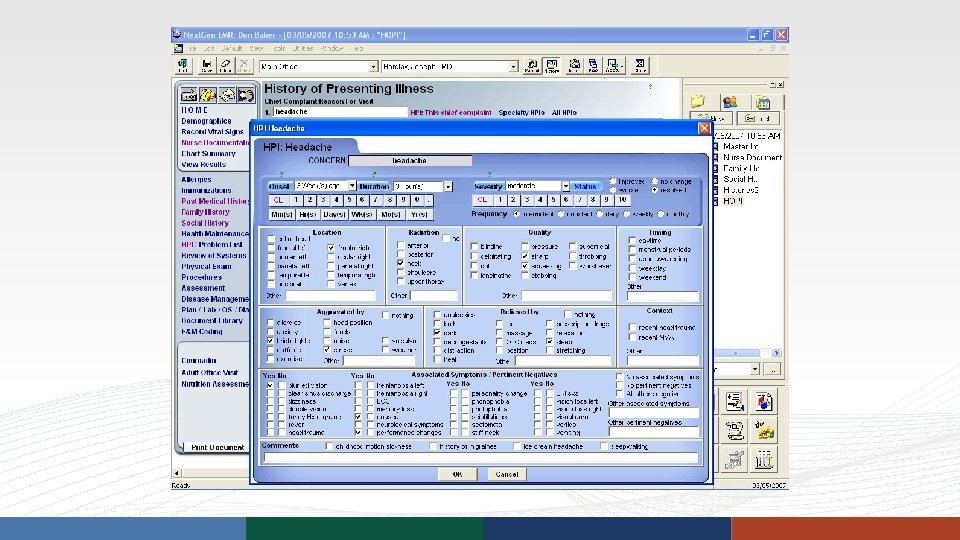
Specific EMR Challenges Subjective/Objective • EMR: Reliance on Structured Data • Different ways to capture data • Free text • Check boxes/radio buttons • Auto-populate • Makes it difficult to get a clear picture of who the patient is/what the problem is (lack of “personalization”)
Structured Data DRAWBACKS BENEFITS • Does not capture the patient • Population health narrative • Easier to share information • Not how we integrate • Data collection – research, QI information and formulate • Patient identification for medical ideas interventions
Specific EMR Challenges Medication Lists • Imported med list may not be an accurate reflection of what is being taken • May not include outside meds (or OTCs) • Short term meds remain on the list unless a stop date is indicated • Discontinued meds are not taken off the active med list unless specifically terminated • ‘Reconciliation’ of medication lists
Specific EMR Challenges Problem Lists • Exploding problem lists make it difficult to scan for important problems/conditions • One diagnosis may be on a list in 5 or 7 different forms
Specific EMR Challenges Assessment/Diagnosis • Often the provider is unable to find the precise diagnostic code and therefore “settles” on something close, but not exactly correct • This diagnostic “near miss” can carry forward • Forced to select a diagnosis to associate with an order (dx test) before the provider actually knows what is going on, leading to either imprecise diagnoses or multiple overlapping diagnoses at one visit
Specific EMR Challenges Increased Use of Scribes • Risk of impacting the quality of the documentation and ability to convey the physician’s thought process
Specific EMR Challenges Controlled Substance Prescribing • Providers may have a greater tendency to NOT include prescriptions in their progress notes because a record of same can be found elsewhere in the EMR • Med lists may look like patient is on multiple short and long acting opioids if discontinued mediations are not taken off the medication list • Be aware of vague recording of PDMP check and UDS (not specific to EMR)
Summary • Patient care documentation is complicated because the medical record serves so many different purposes • A strong medical record is one in which the data (S+O) support the diagnosis, and the treatment plan is substantiated by the data and diagnosis • The adoption of EMR enhances ease of access and legibility for the reviewer, but may make it more difficult to understand the patient’s status, the care that was provided, and the physician’s decision-making
Certified Medical Board Investigator Training Event August 8, 2017 Addressing Concerns About Controlled Substance Prescribing
Objectives • Scope of the problem of prescription drug abuse • How did we get where we are today? • What are the guidelines? • Red flags for prescribing concerns • Pertinent educational and monitoring offerings
Controlled Substances • Opioids • Sedative/hypnotics including benzodiazepines • Stimulants
Prescription Drug Abuse • A national problem • 17, 000 deaths from painkiller ODs annually • More deaths from Rx Drug OD than MVAs • More deaths from Rx Drug OD than OD from “street drugs” • A Colorado problem • 300 deaths in CO each year from Painkiller ODs • CO ranked 12 in the nation on self-reported nonmedical use of opioid painkillers: 224, 000 misuse Rx Drugs each year. • Annual deaths from painkillers more than tripled from 2000 to 2013 http: //takemedsseriously. org/
The Physician’s Dilemma • Chronic pain • 116 million US adults • Greater than heart disease, diabetes & cancer combined • These patients need and deserve effective treatment • Physicians remain the most common source of diverted controlled prescription drugs • Upper limits to dosing not defined
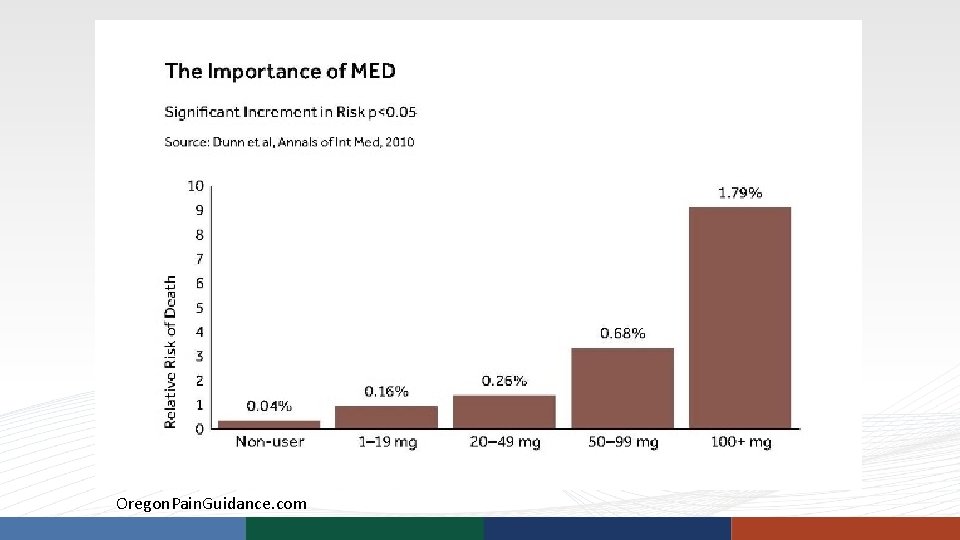
Oregon. Pain. Guidance. com
How did we get to this place? Physician Factors: • Inadequate training in taking a thorough substance use history; few ask about misuse of controlled prescription drugs • Inadequate training in the identification of drug diversion, abuse, and addiction • Inadequate training in how to address drug-seeking patients • Inadequate training in chronic pain management
How did we get to this place? Physician Factors (continued): • Lack of understanding of safe prescribing principles • Personality characteristics • Difficulty saying “no”
Why doctors can’t say no • Research (Kravitz, UCD) 10 - 25 percent of patients bring a specific request to their doctor (the high end is for PCPs). Patients who do not have their requests met rate their physician lower, are less likely to adhere to their doctor’s recommendations, and use more healthcare resources than those who do get their request. • These encounters are stressful and unsatisfying to the physician • http: //www. salon. com/2011/11/28/why_doctors_cant_say_no/
How did we get to this place? Environmental Factors: • Pain as the 5 th vital sign
How did we get to this place? Environmental Factors: • Misleading marketing
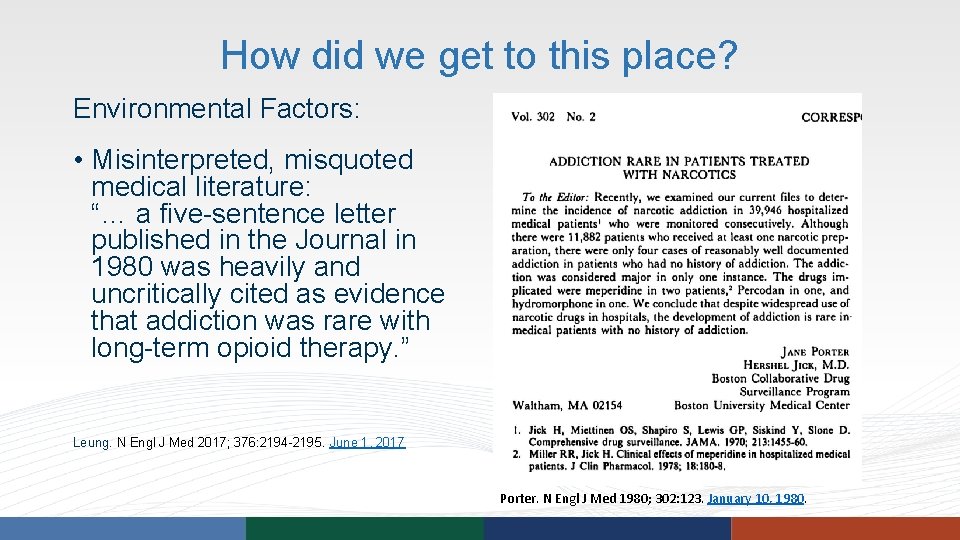
How did we get to this place? Environmental Factors: • Misinterpreted, misquoted medical literature: “… a five-sentence letter published in the Journal in 1980 was heavily and uncritically cited as evidence that addiction was rare with long-term opioid therapy. ” Leung. N Engl J Med 2017; 376: 2194 -2195. June 1, 2017 Porter. N Engl J Med 1980; 302: 123. January 10, 1980.
What are the current guidelines? The problem with guidelines: • Not the same as standard of care • Moving target
CDC Guideline Determining when to initiate or continue opioids for chronic pain Note: “…recommendations for primary care physicians…” 1. Non-pharmacologic and non-opioid therapy preferred. Benefits should outweigh the risks 2. Establish realistic treatment goals for pain and function 3. Revisit risks and benefits periodically
CDC Guideline Opioid Selection, dosage, duration, follow-up, and discontinuation 4. Initial prescribing with immediate release 5. Lowest effective dose; carefully reassess if ≥ 50 MED; avoid ≥ 90 MED 6. Acute Rx: 3 to 7 days 7. Evaluate benefits and harm 1 -4 weeks after initiating, and every 3 months; modify if harms outweigh risk
CDC Guideline Assessing risk and addressing harms of opioid use 8. Before starting and periodically after, evaluate risk factors for opioidrelated harm 9. Review PDMP when starting an opioid prescription for chronic pain and periodically (every prescription to every 3 months) 10. UDS before starting and at least annually 11. Avoid prescribing opioid and benzodiazepine concurrently (now an FDA “black box” warning) 12. Offer or arrange treatment for addiction What about CS agreements?
Standard of Care The watchfulness, attention, caution and prudence that a reasonable person in the same circumstances would exercise… The problem is that the "standard" is often a subjective issue upon which reasonable people can differ. http: //legal-dictionary. thefreedictionary. com/standard+of+care
Red Flags • Indication • Prescribing for a vague or poorly defined condition • Prescribing for conditions for which there is poor or no indication for opioids (migraines, fibromyalgia) • Treatment planning: • Lack of use of non-pharmacologic treatment • Lack of use of (or lack of documented treatment failure) of non-opioid medication alternatives • Lack of use of specialists and referrals (pain management, psychology, psychiatry, addiction medicine) • Lack of establishment of functional goals • What appears to be an unintentional transition from acute to chronic prescribing
Red Flags • Risk assessment: • Lack of assessment risk of addiction (current or future) prior to prescribing (e. g. , ORT, PDMP check, UDS) • Ongoing assessment of risk (COMM, UDT, PDMP) • Patient education: • Lack of informed consent of addiction, adverse effects such as sedation • Quantities • Large quantities • Quantities that exceed daily dosing • Escalating dosing
Red Flags • Drug formulation • Inappropriate use of LA/ER formulations • Dangerous combinations • More than one SA and one LA opioid • Opioid and benzodiazepine or other sedating drug • Certain muscle relaxants • Addiction and diversion • Failure to recognize and/or address
Red Flags • Duration • Prescribing for longer than planned • Failure to consider impact of comorbidities • Obstructive sleep apnea, mental health comorbidities, pregnancy, respiratory disease, renal disease, liver disease, age • Patterns of prescribing over time • Escalating dosing • Early refills • Failure to address aberrant behaviors (such as unexpected UDS results)
Caveats in Chart Review Medications • Medication lists can be misleading (missing information or containing medications that patients is no longer on) • Prescribers don’t always document prescriptions in the text of the progress note • May need to look multiple places (including the PDMP, if allowed) to get a complete picture
Caveats in Chart Review Urine Drug Testing • In-office testing (immunoassay) can result in false positives and false negatives • Send-out testing (liquid or gas chromatography) is much more precise and may need to be ordered to fully understand an inoffice screen • Prescribers may misinterpret urine drug screens
Caveats in Chart Review Prescription Drug Monitoring Program • Legitimate use of the PDMP defined by state legislation or statute • Search may be more complicated than it sounds (multiple names, addresses, states)
Caveats in Chart Review • Difference between MED calculators and dose conversion calculators • Some calculators do not properly convert methadone dosing due to non-linear metabolism
Educational Offerings Relevant to Prescribing • Competence Assessment and Education Programs • Courses • Practice Monitoring specific to prescribing/pain management
Prescribing Controlled Drugs: Critical Issues and Common Pitfalls • Curriculum developed by Vanderbilt Center for Professional Health • 3 day small group interactive course • For healthcare professionals who prescribe controlled substances • Cited for inappropriate prescribing • Those who wish for enhanced competence in managing patients seeking or on controlled substances • Self-referred or referred by medical boards, employers, others • Team-taught: physician, psychologist, addiction counselor • Not designed to: • Provide treatment for active drug dependence or misuse by the clinician • Address the illegal selling of drugs for profit
PCD Course Overview • Participants learn • • • The role of the state licensure board The role of the DEA and the Controlled Substances Act Current information on state Rx drug monitoring programs To identify and manage patients with chemical dependency To identify and manage drug-seeking patients Proper practices for prescribing CSs, screening for risk, monitoring for aberrant behavior • Participants achieve self-understanding • What makes a clinician vulnerable to poor prescribing • Participants engage in simulated patient encounters • Substance abuse screening • Risk assessment
I know a lot about what I shouldn’t be doing. But I don’t know what I SHOULD be doing.
Basics of Chronic Pain Management: Essentials for the Non-Pain Management Specialist One-day (8 -hour) seminar • For any clinician who manages patients with chronic pain who is not a pain management specialist • Enhance knowledge of chronic pain management and improve the quality of care of patients with chronic pain • NOT designed to make clinicians into pain management specialists Faculty • Multidisciplinary: medical pain management/addiction, interventional pain management, and internal medicine/integrative medicine
Basics of Chronic Pain Management: Course Overview • Chronic Pain • Physiology • Overview of treatment • Non-Pharmacologic Treatment • Interventional Pain Management • Pharmacologic Pain Management • Non-opioids • Opioids • Pain States: recognizing common conditions • Special Populations • The Patient Encounter • Chart Review/Self-Audit
Which course do they need? • Prescribing Controlled Drugs • Safe prescribing • Identification of and management/response to risk, drug diversion, abuse, and addiction • Self understanding: difficulty saying “no” • Basics of Chronic Pain Management • Only one tool (opioids) in their toolbox • Evidence-based treatment for conditions that cause chronic pain
Practice Monitoring Program • Specific to CS prescribing • Chart selection • Review directed to only CS prescribing or CS prescribing and overall practice • Can be done after Assessment and Education or alone • If used alone, findings may warrant additional intervention
Summary • A number of factors have contributed to the current prescription drug abuse epidemic • A number of prescribing behaviors (red flags) can help you identify inappropriate prescribing • Tools for remediation include: • Assessment and Education Programs • Intensive skill building courses in Prescribing Controlled Drugs and Basics of Chronic Pain Management • Practice Monitoring Program
Certified Medical Board Investigator Training Event August 8, 2017 Practice Monitoring
Objectives • Describe Practice Monitoring Program • Differentiate PMP from Educational Intervention • Differentiate PMP from traditional practice monitoring

Practice Monitoring Program Quality Review Program
Practice Monitoring Program • Developed after a request from the Colorado Medical Board • Provide effective, consistent, reliable process for practice monitoring • Structured to address the clinician’s specific Board-ordered requirements • Two paths • After completion of CPEP assessment/education plan • For ANY physician required to undergo monitoring ‒ E. g. clinicians who have not participated in CPEP assessment/education Eyes and ears of the Board … Determine if meeting Standard of Care
Preceptor vs. Monitor • Preceptor • Definition: an instructor; teacher; tutor • Role: meet regularly with participant to guide educational process, discuss cases and help improve clinical knowledge and judgement, as well as address other educational goals • Chart review: in CPEP process, review at least 24 of the participant’s charts per month • Reporting: report any concerns about on-going patient care to CPEP • Monitor • • Definition: to observe, record, or detect; to oversee, supervise or regulate Role: eyes and ears of board to determine if care meets standard Chart review: generally 10 charts/month – based on requirements of referrer Reporting: report substandard care or danger to patients
How PMP Works • CPEP identifies monitor ‒ CPEP submits credentials to Board for approval if required • CPEP provides expectations/structure/forms for monitor to use • CPEP submits reports to Board • If monitor rates care as substandard, CPEP will have another physician review the chart to confirm the finding • Frequency of reviews and number of charts determined per Board order
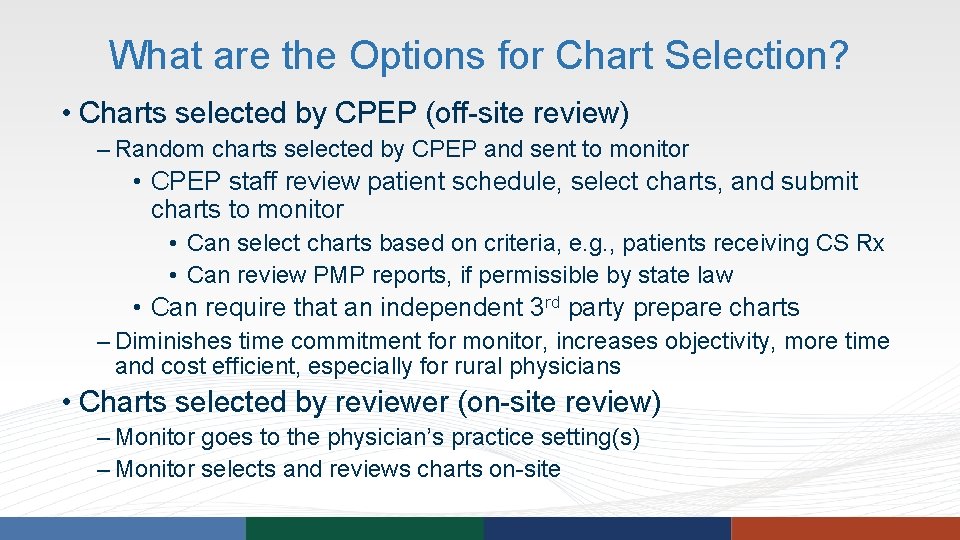
What are the Options for Chart Selection? • Charts selected by CPEP (off-site review) ‒ Random charts selected by CPEP and sent to monitor • CPEP staff review patient schedule, select charts, and submit charts to monitor • Can select charts based on criteria, e. g. , patients receiving CS Rx • Can review PMP reports, if permissible by state law • Can require that an independent 3 rd party prepare charts ‒ Diminishes time commitment for monitor, increases objectivity, more time and cost efficient, especially for rural physicians • Charts selected by reviewer (on-site review) ‒ Monitor goes to the physician’s practice setting(s) ‒ Monitor selects and reviews charts on-site
When is it Used? • As part of a remedial education agreement ‒ Undergo Competence Assessment ‒ Complete Educational Intervention ‒ Complete 18 months of monitoring ‒ As well as other requirements ‒ End of probation can be contingent on successful completion of this process
When is it Used? • As part of any board-ordered monitoring process ‒ Can be used in any situation where traditional monitoring is ordered ‒ Designed to meet the requirements of the stipulation ‒ Ends when clinician’s stipulation requirement is completed, usually 5 years
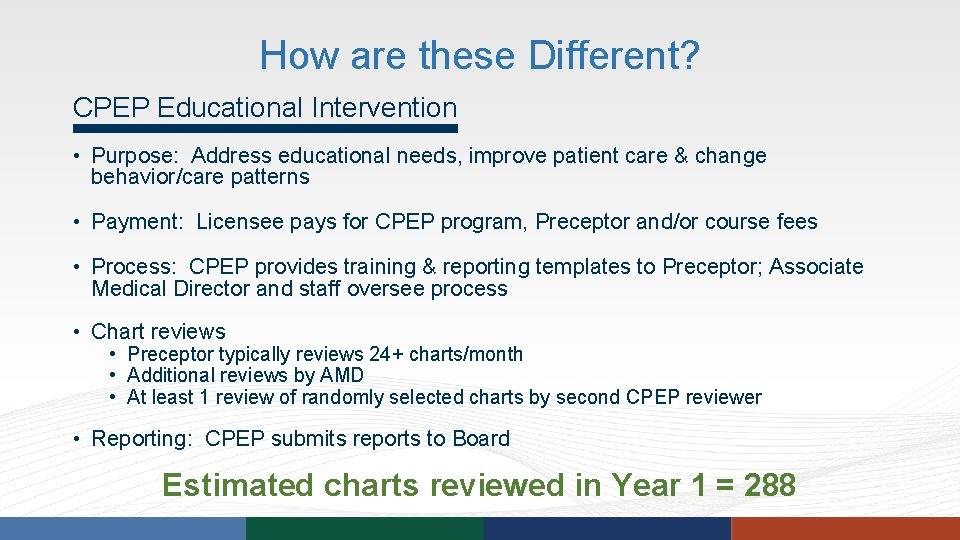
How are these Different? CPEP Educational Intervention • Purpose: Address educational needs, improve patient care & change behavior/care patterns • Payment: Licensee pays for CPEP program, Preceptor and/or course fees • Process: CPEP provides training & reporting templates to Preceptor; Associate Medical Director and staff oversee process • Chart reviews • Preceptor typically reviews 24+ charts/month • Additional reviews by AMD • At least 1 review of randomly selected charts by second CPEP reviewer • Reporting: CPEP submits reports to Board Estimated charts reviewed in Year 1 = 288
How are these Different? CPEP Practice Monitoring Program • Purpose: To report whether practice is within accepted standards based on chart review • Payment: Licensee pays for enrollment and monitoring fees; CPEP pays Reviewer • Process: CPEP provides training & reporting templates to Preceptor; Medical Director and staff oversee process • Typically chart reviews include: • 10 charts/month for first 3 months • 10 charts/quarter for remainder of stipulation • Charts rated as substandard are reviewed by another physician for agreement and quality control • Reporting: CPEP submits reports to Board Estimated charts reviewed in Year 1 = 60
How are these Different? Traditional Practice Monitoring • Purpose: To report whether practice is within accepted standards based on chart review • Payment: Monitor paid by licensee or volunteers time • Process: Follows Board guidelines, if available • Chart Reviews: Typically stipulations require 10 charts/month for first 3 months and then 10 charts/quarter for remainder of stipulation • Reporting: Monitor submits reports to Board • Quality of reporting varies Estimated charts reviewed in Year 1 = 60
What are the Benefits of PMP? • Provides structure and consistency to monitoring process • Ensures objectivity of monitor • Includes second review of charts rated as below standard • Provides consistent reporting and compliance with Board orders
Summary • Practice Monitoring Program can be useful alone or as a followup to or concurrent with an Educational Intervention • Primary purpose is to monitor for acceptable standard of care • Secondary purpose feedback to the physician • Specifics are dictated by Board preference or disciplinary requirements • Variables: number of charts, types of charts, how often, site of review, board approval of monitor
Certified Medical Board Investigator Training Event August 8, 2017 Digging Deeper: Understanding Quality of Care Concerns and Resources
Professionalism • Fiduciary responsibility • Beneficence – Nonmaleficence – Autonomy – Justice
Professionalism • Sexual boundaries • Fraudulent billing or documentation • Pill mill • Lapse in confidentiality
Professionalism • Inappropriate prescribing • Inadequate informed consent • Practicing outside competence (aesthetics, medical bariatrics) • Medical record deficiencies • Negligence
What are you struggling with?
Questions? Elizabeth Grace, MD esgrace@cpepdoc. org 303 -577 -3232
- Slides: 154